Focus Area 3: Reproductive, Preconception and Inter-Conception Health
- Goal #6: Prevent unintended and adolescent pregnancy
- Goal #7: Increase utilization of preventive health care services
To achieve further improvement in birth outcomes, women must practice healthy behaviors and be engaged in primary and preventive health care services throughout their reproductive lives, including before they become pregnant (preconception) and between pregnancies (inter-conception). This focus on health across the life course encompasses family planning services to help women prevent or plan pregnancies. It also recognizes that approximately half of all pregnancies are unplanned, underscoring the importance of routine preventive care and promotion of women's health and wellness across the lifespan, regardless of pregnancy plans.
Two priority preconception/reproductive health outcomes were established for the 2013-2018 a Prevention Agenda and State Health Improvement Plan: prevention of unintended and adolescent pregnancy and use of preventive health services by women of reproductive age. These outcomes complement other sections of the State plan that influence reproductive, preconception and inter-conception health, including: injury and violence prevention, prevention and management of chronic diseases, prevention and cessation of tobacco use, HIV/STI prevention, maternal and infant health, use of preventive health care services during childhood and adolescence and promotion of mental health and prevention of substance abuse.
Goal #6: Prevention of Unintended and Adolescent Pregnancy
Defining the Problem
A pregnancy is considered unintended if it is mistimed, unplanned or unwanted at the time of conception. Unintended pregnancies can be associated with negative health and economic outcomes.93 Approximately half of all pregnancies in the United States are unintended.94 Unintended pregnancy may significantly impact a woman's life course, education and work plans, income potential and future relationships.
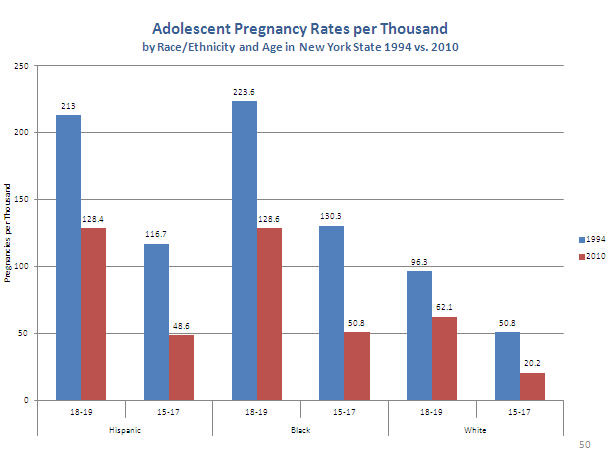
Significant attention has given to preventing pregnancy among adolescents. Four of five pregnancies among women age 19 and younger were unintended and three in ten girls get pregnant before the age of 20.95 Although the teen pregnancy rate is declining, significant racial, ethnic, educational and economic disparities remain. Non-Hispanic Black and Hispanic young women are twice as likely to have an unintended pregnancy as their non-Hispanic White counter parts. Studies have also shown that 20 percent of pregnant teens were enrolled in special education classes.96
Whether planned or not, there are significant public health and societal concerns about teen pregnancy. Adolescent mothers are more likely to drop out of school, remain unmarried and live in poverty. Adolescent fathers are more likely to have lower economic stability, income, educational attainment, and more turbulent relationships. Children born to single teen mothers have more emotional and behavioral problems; poorer physical health; are more likely to use drugs, tobacco and alcohol; more likely to enter the juvenile justice system, and less likely to do well in school.97 However, the most recent rigorous research on adolescent pregnancy challenges the prevailing view, teen-childbearing causes a life of poverty and disadvantage. The research instead demonstrates that the lives of teen mothers and fathers (compared to older parents) are more likely to be marked by poverty, poor academic performance, and low expectations before they become parents, factors that explain a substantial part of their later-life disadvantage.98,99,100 These findings emphasize the need to target profoundly disadvantaged youth with comprehensive interventions that can positively change their life opportunities and aspirations, and that support them to set and achieve their own goals.
While continued attention to prevention of adolescent pregnancy is needed, the majority of unplanned pregnancies occur among unmarried women aged 20-29, highlighting the need for heightened attention to prevention of unintended pregnancy among young adults. A 2012 Guttmacher Institute report indicated that 73 percent of pregnancies among unmarried women age 20-24 were unintended.101 Unplanned pregnancy increases the risk for less-than-optimal health at the time of conception, including management of chronic diseases, such as diabetes and high blood pressure, which are increasingly common among young adults in the United States. Unintended pregnancy is associated with delayed use of prenatal care, reduced likelihood of breastfeeding and increased risk of maternal depression, low birth weight and birth defects.93,102,103 Poverty, race, class and educational attainment remain the greatest indicators of unintended pregnancy, coupled with the women's low expectations for their futures.
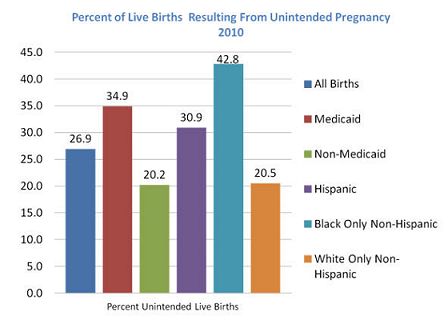
There are striking racial, ethnic and economic disparities in unintended pregnancy rates. In NYS in 2010, the percent of births that resulted from an unintended pregnancy was twice as high among Black women, and about 1.5 times higher among Hispanic women, compared to White women. Previous studies have shown that low-income young women are more than three times as likely to have unintended pregnancies as young women in the highest income group. Similarly, young women with some college education have half as many unintended pregnancies as high school graduates and one third that of non-graduates. Unmarried young women with no high school diploma have the highest unintended pregnancy rate.104
While the predictors and consequences of unintended pregnancy are well documented, more research is needed to better understand the factors that influence women's use of family planning services and methods to plan pregnancies.
Goals and Objectives
- Objective 6-1:
- By December 31, 2018, reduce the proportion of NYS births that result from unintended pregnancies by at least 10%.
- Objective 6-2:
- By December 31, 2018, reduce racial and ethnic disparities in unintended pregnancy rates by at least 10%.
- Objective 6-3:
- By December 31, 2018, reduce the rate of pregnancy among NYS adolescents age 15-17 years by at least 10%.
- Objective 6-4:
- By December 31, 2018, reduce racial and ethnic disparities in unintended and adolescent pregnancy rates by at least 10%.
- Tracking Indicators
-
- Percentage of live births resulting from a pregnancy that was unintended
-
- All live births.
- Target: 24.2%; Baseline: 26.9%; Year: 2010
- Source: NYSDOH Vital Statistics; Data Availability: State, county)
- Ratio of unintended pregnancy rates for Black non-Hispanics to White non-Hispanics.
- Target: 1.88; Baseline: 2.09; Year: 2010; Source: NYSDOH Vital Statistics; Data Availability: State, county
- Ratio of unintended pregnancy rates for Hispanics to White non-Hispanics.
- Target: 1.36; Baseline: 1.51; Year: 2010; Source: NYSDOH Vital Statistics; Data Availability: State, county
- Ratio of unintended pregnancy rates for Medicaid to non-Medicaid.
- Target: 1.56; Baseline: 1.73; Year: 2010
- Source: NYSDOH Vital Statistics; Data Availability: State, county)
- Adolescent pregnancy rate (number of pregnancies per 1,000 adolescents age 15-17 years):
-
- All adolescents age 15-17 years.
- Target: 25.6; Baseline: 28.5; Year: 2010
- Source: NYS Vital Statistics Data; Data Availability: State, county
- Ratio of pregnancies among adolescents age 15-17 for Black non-Hispanics to White non-Hispanics.
- Target: 4.9; Baseline: 5.47; Year: 2010
- Source: NYS Vital Statistics Data; Data Availability: s State, county)
- Ratio of pregnancies among adolescents age 15-17 for Hispanics to White non-Hispanics.
- Target: 4.1; Baseline: 4.58; Year: 2010
- Source: NYS Vital Statistics Data; Data Availability: State, county
- Additional Indicators
-
- Percentage of live births resulting from an unintended pregnancy.
- Target: TBD; Baseline: 34.4%; Year: 2010
- Source: Pregnancy Risk Assessment Monitoring System (PRAMS)
- Data Availability: State only)
- Ratio of births resulting from unintended pregnancy for Black non-Hispanics to White non-Hispanics.
- Target: TBD; Baseline: 1.87; Year: 2010
- Source: PRAMS; Data Availability: State only
- Closely Related Healthy People 2020 National Objectives
-
- FP-8.1:
- Pregnancies per 1,000 females ages 15-17.
- Target: 36.2; Baseline: 40.2; Year: 2005
- Source: Abortion Provider Survey, Guttmacher Institute; Abortion Surveillance Data, CDC, NCCDPHP; National Vital Statistics System-Natality (NVSS-N), CDC, NCHS; National Survey of Family Growth (NSFG), CDC, NCHS)
Interventions by Health Impact
| Goal #6: Prevention of Unintended and Adolescent Pregnancy | |
|---|---|
| Levels of Health Impact Pyramid | Interventions105 |
| Counseling and Education |
|
| Clinical Interventions |
|
| Long-Lasting Protective Interventions |
|
| Changing the Context to Make Individuals' Decisions Healthy |
|
| Socioeconomic Factors |
|
Interventions by Sector
NOTE: The chart below provides a sample of interventions that can be carried out by sector. Please refer to the 'Interventions by Health Impact' grid above for more interventions and references.
Health Care Delivery System
- Promote the use of the most effective contraceptive methods, including long-acting reversible contraceptives (LARCs).
- Provide patient education that focuses explicitly on correct, consistent use of highly effective contraception, use of dual protection (hormonal/LARC plus condoms) and teaching teens and young adults to negotiate contraceptive use with their partners.
- Educate sexually active patients on the use of and access to emergency contraception.
- Provide same-day post-abortion and post-partum contraception, including provision of LARC.
- Integrate preconception care, including strategies to prevent unintended pregnancy, into primary care delivered by pediatricians, obstetricians/gynecologists, adolescent medicine specialists and family practice physicians.
- Implement practices to expedite enrollment of low-income men and women family planning clients in public health insurance, including presumptive eligibility for Family Planning Benefit Program.
Employers, Businesses, and Unions
- Provide health insurance for employees and their families that covers preventive services, including effective contraceptives.
- Provide employees with paid time off, flextime and other incentives for preventive health care visits.
Media
- Help government and community-based organizations develop effective health communications/social marketing campaigns that promote planning pregnancies, delaying the onset of sexual activity, use of effective and emergency contraception and the availability of family planning services in the community for young men and women.
- Develop, evaluate and implement media literacy programs for adolescents to counteract prevalent media messages about sex.
- Increase time/space allotted for programming that supports health promotion messages targeting high-risk populations.
Academia
- Conduct research to better understand and develop interventions to address multiple dimensions of pregnancy intention.
- Conduct translational research to support effective evaluation, adaptation, replication, dissemination and implementation of evidence-based interventions to prevent unintended pregnancy among teens and young adults.
- Adapt training programs for medical students and residents to better integrate reproductive health care and family planning services into primary health care visits.
- Improve health services at two- and four-year colleges/universities to ensure a comprehensive approach that incorporates preconception care and reproductive/family planning services are integrated into primary care visits.
Community-Based Organizations
- Conduct enhanced outreach to engage high-risk populations in clinical family planning services and prevention programs.
- Implement comprehensive, evidence-based sexual health education programs in schools and other community settings.
- Establish referral relationships with facilitated enrollers and clinical family planning providers, and connect clients to health insurance and clinical pregnancy prevention services.
Other Governmental Agencies
- Implement comprehensive evidence-based, age-appropriate sexual health education in schools.
- Ensure that all youth in foster care have information about and access to comprehensive primary care services, including reproductive health/family planning services.
- Assess health insurance status and source of regular health care for all clients, and connect uninsured men and women to facilitated enrollers in the community.
- Eliminate the practice of sending Explanations of Benefits (EOBs) for reproductive health care services to protect confidentiality of patients.
Governmental Public Health
- Support the implementation of comprehensive evidence-based adolescent pregnancy prevention programming in targeted high-need communities.
- Support the delivery of comprehensive clinical family planning services, targeting resources to the highest-need communities and populations. At the local level, facilitate referral networks to link clients in need of services to available resources.
- Implement changes to expand and streamline access to public health insurance coverage for family planning services, including implementation of presumptive eligibility.
- Work with insurers to eliminate the practice of sending EOBs for reproductive health care services to protect the confidentiality of patients.
- Partner with State Education Department and local school districts to advance the implementation of evidence-based age-appropriate sexual health education in schools.
Non-Governmental Public Health
- Conduct enhanced outreach to engage high-risk populations in clinical family planning services and community-based prevention programs.
- Implement comprehensive, evidence-based sexual health educational programs in schools and other community settings.
- Directly provide, or establish referral relationships with, facilitated enrollment and clinical family planning services.
- Provide fertility education to family planning providers and federally qualified health centers.
Policymakers and Elected Officials
- Create economic and educational opportunities for women in high-risk communities and circumstances.
- Support the implementation of evidence-based, age-appropriate sexual health education in schools.
- Support continued access to comprehensive clinical family planning and reproductive health services.
Communities
- Disseminate facts and health promotion messages on pregnancy planning and prevention to members of organizations/ congregations.
- Engage affected populations in local strategies to raise awareness of health disparities and to identify, develop, implement and evaluate collective solutions to community health issues.
- Help identify and recruit 'natural helpers' from affected communities who can serve as trained paraprofessionals in health promotion programs, and individuals for professional education/training to serve as health care practitioners in their community.
Philanthropy
- Fund enhanced assessments of needs and challenges experienced by affected populations, such as community focus groups of women do not use contraception or family planning, and disseminate findings to State and local partners to help develop more effective interventions.
- Fund the development, evaluation, adaptation, replication and dissemination of evidence-based and innovative strategies to prevent unintended and teen pregnancy among affected populations.
- Fund training programs and quality improvement collaborating to strengthen capacity and improve effectiveness of health and human services providers related to reproductive health/family planning services.
Goal #7: Increase utilization of preventive health care services among women of reproductive ages.
Defining the Problem
Pre-conception health care is critical for women of reproductive age. Whether before a first or subsequent pregnancy, pre-conception care promotes women's health before conception, increasing the chances for a healthy, full-term birth.136 Health promotion, screening, and medical and psychosocial interventions addressed before conception can reduce risks that might affect future pregnancies. This enhanced approach to women's comprehensive primary and preventive care recognizes that whether planned or unplanned, approximately half the women in the United States experience at least one birth by age 25, and approximately 85 percent of them give birth by age 44. Although a central goal of pre-conception and inter-conception health care is to improve birth outcomes for women and their children, pre-conception care is fully consistent with broader goals of engaging all women in preventive health care services and promoting women's health and wellness across the lifespan. Use of preventive health care services by women of reproductive age thus may be viewed as part of a continuum that begins with well-child care during childhood and adolescence and continues throughout adult life.
Pre-conception care can identify key medical, behavioral, psychosocial and environmental risks for adverse birth outcomes and modify them before pregnancy (some risks must be addressed before conception). Pre-conception health status is one of many reasons for the persistent and widening racial, ethnic and economic disparities in birth outcomes.139 At least one study has demonstrated that pre- conception care can increase pregnancy planning and intention, which brings women into prenatal care services early in pregnancy.137,138 Addressing pre-conception health status in high-need populations could shrink the racial, ethnic and economic disparities in birth outcomes.139
Because many health factors can affect birth outcomes, women should obtain regular preventive care during their reproductive years.140 Rather than a single dedicated 'pre-pregnancy' planning visit, all health encounters during a woman's reproductive years should include counseling on medical care and behavioral changes that will optimize pregnancy outcomes. Care should include screening and risk assessment. The areas of inquiry should be for exposure to environmental hazards and toxins; medication use; nutrition, folic acid intake and weight management; genetic conditions and family history. Additionally, looking at substance use and social and mental health concerns, i.e., depression, social support, domestic violence and housing; identification and management of chronic medical conditions such as diabetes, hypertension and oral health; and immunizations; and discussion of child spacing, family planning and effective contraception methods. Women at risk may need additional counseling, testing, brief interventions (e.g., for smoking or alcohol), or referral to specialty care or supportive services. The approach is even more important for women who have endured an adverse birth outcome, to manage their contributing risks and reduce the likelihood of recurrence. In addition, women with disabilities often have not had access to reproductive health services and face barriers when seeking these services.141,142
An emerging appreciation for the fundamental importance of preconception health care is reflected throughout this Action Plan, highlighted by the decision to incorporate a specific priority focus on preconception preventive care. There is a significant need to develop further data systems and measures to support the development, implementation and evaluation of public health interventions to improve preconception and inter-conception health. The objectives and indicators selected for this component of the State Health Improvement Plan reflect currently available data, and should be expanded and refined as the evidence base and surveillance capacity related to preconception health further evolves.
Goals and Objectives
- Objective 7-1:
- By December 31, 2018, increase the percentage of reproductive-age women who have health insurance to the Healthy People 2020 target of 100%.
- Objective 7-2:
- By December 31, 2018, increase the percentage of women of reproductive age who receive routine primary and preventive health care services before or between pregnancies by at least 10%.
- Objective 7-3:
- By December 31, 2018, improve birth spacing by at least 10%.
- Tracking Indicators
-
- Percentage of women ages 18-64 who report they have any kind of health coverage (as a proxy for women of reproductive age using data that are available).
- Target: 100%; Baseline: 86.1, Year: 2010
- Data Source: U.S. Census Bureau, Small Area Health Insurance Estimates; Data Availability: State, county
- Percentage of live births that occur within 24 months of a previous pregnancy.
- Target: 17.0%; Baseline: 18.9%; Year: 2010
- Data Source: NYSDOH Vital Statistics; Data Availability: State, county)
- Additional Indicators
-
- Percentage of women ages 18-44 who report that they have any kind of health care coverage.
- Target: TBD; Baseline: 86.8%; Year: 2008-2010
- Data Source: NYS BRFSS; Data Availability: State only [county level approximately every 5 years]
- Percentage of women ages 18-44 who report that they have seen a doctor for a routine checkup within the last year.
- Target: TBD; Baseline: 70.8%; Year: 2008-2010
- Data Source: NYS BRFSS; Data Availability: State only [county level approximately every 5 years]
- Percentage of women ages 18-44 who report that they had a dental visit within the last year.
- Target: TBD; Baseline: 74.9%; Year: 2006, 2008, 2010 combined
- Data Source: NYS BRFSS; Data Availability: State only [county level approximately every 5 years]
- Closely Related Healthy People 2020 National Objectives
-
- AHS-1.1:
- Proportion of people with health insurance.
- Target: 100%; Baseline: 83.2%; Year: 2008; Data Source: National Health Interview Survey (NHIS), CDC, NCHS)>
- FP-1:
- Proportion of pregnancies that are unintended.
- Target : 56.0%; Baseline: 51.0%; Year: 2002
- Data Source: National Survey of Family Growth (NSFG), CDC, NCHS; National Vital Statistics System (NVSS), CDC, NCHS; Abortion Provider Survey, Guttmacher Institute; Abortion Surveillance Data, CDC, NCCDPHP
- FP-5:
- Percentage of pregnancies conceived within 18 months of a previous birth.
- Target: 31.7%; Baseline: 35.3%; Year: 2008. Data Source: National Survey of Family Growth, CDC, NCHS
Interventions by Health Impact
| Goal #7: Increase utilization of preventive health care services among women of reproductive ages. | |
|---|---|
| Levels of Health Impact Pyramid | Interventions |
| Counseling and Education |
|
| Clinical Interventions |
|
| Long-Lasting Protective Interventions |
|
| Changing the Context to Make Individuals' Decisions Healthy |
|
| Socioeconomic Factors |
|
Interventions by Sector
NOTE: The chart below provides a sample of interventions that can be carried out by sector. Please refer to the 'Interventions by Health Impact' grid above for more interventions and references.
Healthcare Delivery System
- Provide routine preconception/inter-conception care for women of reproductive age that includes screening and follow up for risk factors, management of chronic medical conditions and use of contraception to plan pregnancies. Preconception/inter-conception care should be integrated in routine primary care delivered by family practice, pediatric, OB-GYN and internal medicine primary and specialty care practitioners.
- Make available examination tables that can be raised and lowered to ensure that women with physical disabilities can obtain routine screening and preventive care.
- Implement reminder systems for routine preventive health and follow-up visits.
- Obtain NCQA Patient-Centered Medical Home (PCMH) certification.
- Adopt electronic health records and connect to regional health information systems to improve quality and coordination of services.
Employers, Businesses, and Unions
- Provide comprehensive health insurance for employees and their families that covers preventive, disease management and home visiting services.
- Provide employees with paid time off, flextime and other incentives for preventive health care visits.
Media
- Help government and community-based organizations develop effective marketing campaigns that promote norms of wellness, healthy behaviors and regular use of preventive health care services throughout the lifespan.
- Make increased advertising space and resources available for health promotion campaigns.
Academia
- Adapt training programs for medical students and residents, and continuing education programs for current practitioners, to better integrate preconception and reproductive health in routine care.
- Include disability literacy when training health practitioners in women's reproductive health.
- Conduct research to develop and evaluate educational messages and vehicles that have demonstrated improvement in knowledge, attitudes/beliefs, skills and behaviors related to health and wellness and the use of preventive health care services across the lifespan.
Community-Based Organizations
- Engage members of at-risk populations, including adolescents, LGBQT, women with disabilities, low- income women, immigrant women and others, to provide input and feedback on strategies to improve their use of health care services.
- Use peer counselors, lay health advisors, community health workers and promotoras to reinforce health education and health care service utilization and enhance social support to high-risk preconception and inter-conception women.
- Expedite enrollment of low-income reproductive-age women in Medicaid, including presumptive eligibility for family planning coverage.
- Use health information technology to facilitate more robust intake/enrollment, screening/risk assessment, referral, follow up and care coordination practices across health and human service providers.
Other Governmental Agencies
- Identify and promote educational messages and vehicles that have demonstrated to improve knowledge, attitudes, skills and/or behavior.
- Provide comprehensive, evidence-based health education that includes health literacy and consumer skills for use of health care services, for children and youth in schools.
- Assess health insurance status and source of regular health care for all clients served in other government programs, and connect families in need to facilitated enrollers within the community.
Governmental Public Health
- Expand the development and tracking of preconception and inter-conception health indicators and data sources to support public health program and policy development and evaluation.
- Support requirements for health insurance coverage of preconception/inter-conception health care services.
- Expand support for community-based programs that engage paraprofessionals from the community health workers to enhance social support to high-risk preconception and inter-conception women.
- Develop and disseminate evidence-based clinical guidelines and tools for health care providers to promote optimal well-being through utilization of preventive health services.
- Support or conduct public health detailing to improve health care providers' knowledge, beliefs and skills related to delivery of comprehensive, integrated preconception and inter-conception preventive health care services.
Non-Governmental Public Health
- Use home visiting programs to reinforce importance of inter-conception preventive health care services, including family planning.
- Conduct public health detailing to improve health and human service providers' knowledge, beliefs and skills related to delivery of comprehensive, integrated preconception and inter-conception preventive health care services.
- Streamline and simplify processes for health insurance enrollment and renewal for low-income women.
- Support development and implementation of local service networks, use of health information technology and coordination strategies to ensure that women with identified risk factors are linked to appropriate community resources and that follow-up occurs.
Policymakers and Elected Officials
- Implement Affordable Care Act reforms to ensure comprehensive, affordable health insurance for all NYS women, including coverage for family planning and reproductive health care services.
Communities
- Raise awareness about health disparities, and empower teens and young adults to demand access to preventive health care and to make decisions about reproductive health.
- Gather direct input from affected populations to understand better why some women do not use recommended preventive health care services, and share information with practitioners and policymakers to inform improvements.
- Disseminate information about community resources for health insurance, health care and other supportive services.
Philanthropy
- Fund the development, evaluation, replication and dissemination of evidence-based and innovative strategies to improve use of preventive health care among affected populations.
- Fund training programs and quality improvement collaboration to strengthen capacity and improve health care providers' effectiveness in delivering comprehensive and integrated preconception/inter-conception care as part of primary and specialty health care services.
- Provide leadership and funding to support community-wide, cross-sector practices, networks and systems to ensure that all women enrolled in health insurance and have a usual source of primary health care.
a The Prevention Agenda 2013-2017 has been extended to 2018 to align its timeline with other state and federal health care reform initiatives.