Home Care Cost Report Instructions
- Instructions are also available in Portable Document Format (PDF)
Required for:
Licensed Home Care Services Agencies (LHCSA)
Certified Home Health Agencies (CHHA)
Fiscal Intermediaries (FI)
For the Period: January 1, 2021 to December 31, 2021
Contents
Introduction
The Home Care cost report is required to be completed by agencies who operate one or more of the following entities:
- Certified Home Health Agency (CHHA)
- Licensed Home Care Services Agency (LHCSA)
- Fiscal Intermediary (FI)
An agency is defined as an organization that operates one or more CHHA, LHCSA, or FI. Agencies that operate one or more of these facilities must complete certain parts of this cost report for each of these entities.
An entity is defined as a CHHA, LHCSA, or FI. An entity may be operated as part of a larger agency or may be free-standing.
Some of the schedules in the Home Care cost report will require information at the agency level, while other schedules require information at the entity level. The instructions explicitly state which schedules of the Home Care cost report require agency level information and which schedules require entity level detail (CHHA, LHCSA, or FI) to be reported. A note is included at the beginning of each section to indicate if agency or entity level information is required.
A The letter "A" indicates a schedule requires agency-level information to be reported.
E The letter "E" indicates a schedule requires entity-level information to be reported.
Reporting Guidance
Since Medicaid reimbursement rates for LHCSAs and FIs are calculated by county, entity level information will need to be broken out separately on schedules where this detail is required. For the purposes of this cost report, LHCSA and FI entities are required to be separated by county. For example, if a LHCSA provides services in two counties, then that agency is said to have two entities for the purposes of Home Care cost report submissions. This should not result in changes to the existing reporting practices, as the Personal Care Cost Report was previously completed by county for LHCSAs and FIs. Note that if an FI currently has a pending application status, has had an application approved, or has previously operated as part of a LHCSA, the FI entity should still be broken out separately for reporting purposes on the Home Care cost report. In addition, some agencies may have office locations that service multiple counties. An entity should not be identified based on the physical office locations, but rather the county served. A unique LHCSA or FI entity is associated with one county.
For CHHAs, the Operating Certificate will be used as the unique entity identifier and will be the driver for how the information should be reported on certain schedules. For example, if an agency holds three CHHA operating certificates, the agency is said to have three CHHA entities for the purposes of the cost report. CHHA entities are not classified based on county of operation, but rather solely based on their operating certificate.
Please note that all cost report schedules will be completed in the Home Care Tool. The Home Care Tool is a web-based platform that will create a customized view of only the schedules of the cost report required to be completed for your agency and the entities operated by the agency. Based on the information you enter in the "Reporting Hierarchy" tab of the Home Care Tool, only the required schedules will be visible to complete in the "Cost Report Schedules" tab. Note that further details related to the Home Care Tool can be found in the "Completion of Web-based Tool" portion of the Instructions tab.
The cost report schedule instructions specify that a standard set of rules be followed in order to provide consistent data for comparison purposes. The Department of Health (DOH) reserves the right to reject the information submitted if the instructions are not properly followed.
In addition to completing the Home Care cost report, agencies/entities will be required to provide questionnaire responses and participate in audit procedures performed by KPMG, LLP (KPMG).
Important Items to Note
- Allocation Methodology
There are some schedules of the cost report that require an allocation methodology to allocate agency costs or other information to the appropriate entities and service types. The DOH has prescribed the Total Operating Expenses allocation methodology to allocate information within the Home Care Cost Report. If a provider is unable to use this approach, they can explicitly document the allocation methodology they used (e.g., Hours of Service, Square Feet Occupied, Time Study). Note that this information will be reviewed by KPMG during the audit process. - Costs
Please note that you are required to report actual costs when completing the Home Care cost report. In addition, the Home Care cost report must include all agency costs (regardless of payor source, i.e., Medicaid, Medicare, third party insurance, or private pay). Revenue figures should not be reported in the Home Care cost report besides what is requested in Schedule 19 (Statement of Revenue and Expenses). - Contracting relationships
As part of the delivery of services, many agencies have contracting relationships with other agencies to perform direct care services. For example, there are instances where a CHHA will contract out the delivery of Home Health Aide (HHA) services to a LHCSA. If both the CHHA and LHCSA reported the costs of these services as allowable on the Home Care cost report, this would result in double counting. As such, only the agency contracting out the services should report them as allowable on the Home Care cost report. The agency acting as a subcontractor should not report these services as allowable. Instead, for all LHCSA schedules that require the reporting of information by service type, there is a line item for "Other non-allowable services." Any costs related to a LHCSA performing HHA services as part of a contract with a CHHA should be reported in this line. See below for detailed instructions on how to report costs on Schedule 3 as the subcontractor versus the contractor. Note that further instructions regarding contracting relationships are covered within the instructions for Schedule 3a, 3b, and 3c of this document.
Agency purchasing a direct care service from another agency (contractor)
The agency contracting out the direct care services should report the costs they incurred purchasing the service (e.g., the amount they paid the subcontractor) in the "Contracted Purchased Services" Column 009, within the applicable service type row on Schedule 3, as shown in the screenshot below.Agency providing a direct care service to another agency (subcontractor)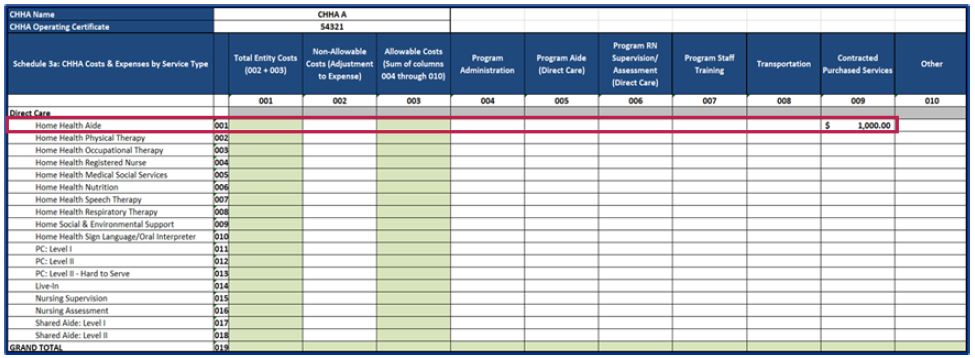
The agency acting as the subcontractor should report the expenses they incurred performing the direct care services (e.g., paying the direct care worker for the hours worked providing the service, transportation for the worker to get to the patient to provide the subcontractor services, etc.) in the "Other non-allowable services" row 009 in the "Program Aide (Direct Care)" Column 005 on Schedule 3, as shown in the screenshot below.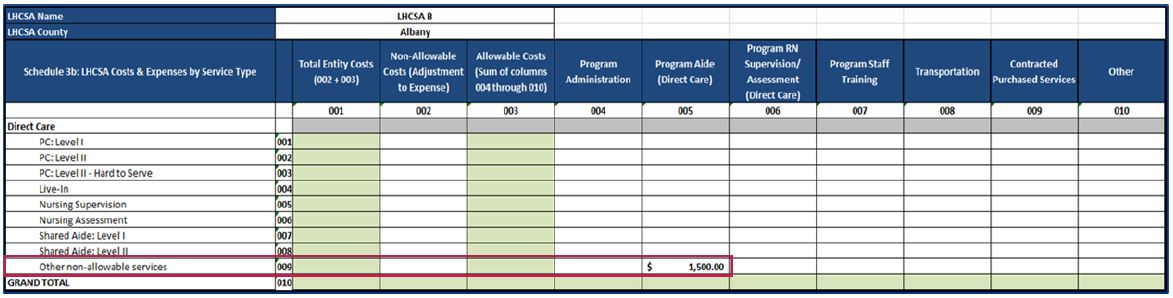
Note: Administrative-related contracted purchased services costs, such as cleaning, bookkeeping, administrative computer services, and other services not related to direct patient care, should be reported in Column 004 (Program Administration) within the Administration & General row. - CPA Certifications
The Home Care cost report does not need to be certified by a CPA prior to submission. DOH has engaged KPMG to conduct audits of the Home Care cost report submissions. Although CPA certification is no longer required, agencies may still use a vendor to assist with Home Care cost report preparation and submission. If an agency uses a vendor to support the cost report and/or audit process, the agency is still responsible for accurate and timely submissions and responses to any inquiries. Please also note that an executive-level individual will need to sign off on the completeness and accuracy of the cost report data prior to submission (e.g., CEO or CFO). - Accounting Methodology
The Home Care cost report should be completed using the accounting methodology used for your agency's financial statements (e.g., accrual or cash basis).
In addition, the Financial Statement Schedules of the Home Care cost report (Schedule 17, Schedule 18, and Schedule 19) should be completed using the reporting period of your agency. For example, if your agency's fiscal year is July 1st through June 30th, then Schedules 17, 18, and 19 can be completed in line with this reporting period. It is important to note that no matter the fiscal reporting period of your agency, all other schedules of the Home Care cost report (Schedule 1 through Schedule 16) should be reported on a calendar year basis. - Providers not required to complete the Home Care Cost Report
The following providers are not required to complete the Home Care Cost Report:- Assisted Living Program (ALP) only agencies
- Private pay only agencies
- Hospital-based CHHAs or LHCSAs
- Private duty nursing only agencies
- Agencies receiving no Medicaid reimbursement (through Fee-for-Service (FFS) or MLTC)
- LHCSAs who contract with CHHAs and provide no other home care services
- CHHAs who provide ONLY Hospice services
- Programs of All-Inclusive Care for the Elderly (PACE) program only facilities
- Nursing Home Transition and Diversion (NHTD) and Traumatic Brain Injury (TBI) program only facilities
- Procedural Recommendations
- Agencies should develop internal cost report policies and procedures to help ensure that costs and statistics are reported properly. Documented cost report policies and procedures will allow for consistent year-over-year reporting compliance in the event of staff turnover at the agency. The policy and procedures document should include cost report preparation instructions that are specific to the agency, such as the sources of data that are necessary to complete the cost report, how costs should be allocated on different schedules, and who is responsible for preparing and reviewing the report.
- A cost report policies and procedures template that agencies may leverage to prepare this document is located within the "Instructions" tab of the Tool, under the "Useful Links" section on the right-hand side of the screen.
- In an effort to demonstrate segregation of duties during the cost report submission process, agencies should have multiple individuals involved in the cost report preparation, review, and submission of the cost report.
- Agencies should develop internal cost report policies and procedures to help ensure that costs and statistics are reported properly. Documented cost report policies and procedures will allow for consistent year-over-year reporting compliance in the event of staff turnover at the agency. The policy and procedures document should include cost report preparation instructions that are specific to the agency, such as the sources of data that are necessary to complete the cost report, how costs should be allocated on different schedules, and who is responsible for preparing and reviewing the report.
- Workers' Recruitment & Retention (WR&R) Costs and Revenue
Per PHL - S.3614 (9) and SSL 367-q, all home care agencies receive an annual WR&R rate add-on. The WR&R rate add-on is additional revenue for home care agencies to spend on recruitment, training, and retention costs. On Schedules 3 and 4 of the Home Care Cost Report, only WR&R costs in excess of the WR&R revenue received through the WR&R rate add-on may be reported as allowable. Any portion of WR&R expenses that was covered by the WR&R rate add-on revenue should be reported as non-allowable in Column 002 on Schedules 3 and 4.
To calculate WR&R costs, the agency should sum all recruitment, training, and retention expenses from the specific cost report year. To properly report the WR&R costs on Schedules 3 and 4, the agency should subtract the WR&R revenue received in the specific cost report year from their total WR&R costs. The net amount of WR&R costs should be reported as allowable (in Column 004 Program Administration or Column 007 Program Staff Training), and the amount covered by the WR&R revenue should be reported as non-allowable (in Column 002 Non-allowable Costs) on Schedule 3 and Schedule 4.
Agencies can identify their WR&R rate add-on on their Medicaid FFS rate sheet. DOH understands that agencies may need to estimate their WR&R revenue for the 2021 Home Care Cost Report. Agencies may determine their own method of estimating the WR&R revenue for the 2021 cost report year; however, they must provide supporting documentation that documents how their WR&R revenue was calculated.
If an agency is unsure of how to estimate their WR&R revenue, DOH has provided an optional approach that agencies may leverage. This method is summarized below:- Assume that the WR&R rate add-on percentage in 2021 was 4.56%1 of your agency's Medicaid reimbursement rate.
- Divide the reimbursement rate (dollar value) by 1.0456. Then, subtract that value from the reimbursement rate (dollar value) to arrive at the WR&R rate add-on dollar value.
- Multiply the WR&R add-on dollar value by the units of service provided in 2021, to arrive at the total WR&R revenue dollar amount for the year.
- If your agency provides multiple services (e.g., PC Level I and Nursing Supervision), then you will need to complete these steps for each service type and sum the total WR&R revenue dollar amounts.
- Agency A assumes that the WR&R rate add-on percentage in 2021 was 4.56%. of their Medicaid reimbursement rate.
- Agency A divides their Medicaid reimbursement rate by 1.0456 ($50/1.0456=$47.82). Then, Agency A subtracts that value from the Medicaid reimbursement rate to calculate their WR&R dollar value of $2.18 ($50-$47.82=$2.18).
- Agency A multiples 65,000 units of service by the rate add-on dollar value of $2.18 to calculate their total WR&R revenue dollar value of $141,700.
- This $141,700 should be offset from total WR&R costs and reported as non-allowable in Column 002 of Schedules 3 and 4. The remaining $58,300 that is net of the WR&R revenue should be reported as allowable in Column 004 (Program Administration) or Column 007 (Program Staff Training) on Schedules 3 and 4.
- Since Agency A only provided one service type in 2021, step 4 is not applicable. Note: Any WR&R costs in excess of this WR&R revenue may be reported as allowable on Schedule 3.
Note: Failure to submit all required schedules or failure to resubmit corrected schedules when requested may result in the imposition of sanctions or penalties.
Schedule 1: General Information - Agency
A Note: Schedule 1 contains agency-level information.
This General Information Schedule contains information on the agency-level. Information that will appear on this schedule includes the following:
Agency Information
- Name of Agency: Enter the legal name of the organization.
- Alternative agency name or DBA (if applicable): Enter any DBAs ("doing business as") or alternative names the agency may be used for identification purposes.
- Federal Tax ID: Enter the Federal Tax ID of the organization.
- Agency Type: Select the agency type (Proprietary, Voluntary, or Public).
- Address: Enter the street address of the agency headquarters.
- City: Enter the name of the city where the agency headquarters is located.
- State: Enter the state where the agency headquarters is located.
- Zip: Enter the zip code for the agency headquarters.
Contact Person Information
The name of the person that can answer questions regarding the cost report submission. Include this person's first and last name, job title, telephone number, and email address (required fields).
Entity Types
Information should be entered in for the total quantity of unique CHHA, LHCSA, and FI entities operated by the agency. For example, if an agency operates 2 CHHA, 2 LHCSA, and 2 FI entities, "2" should be entered for the CHHA, LHCSA, and FI line items. If an agency operates zero of one of the entity types, enter a value of "0." Do not leave any of these fields blank.
Notes: If an entity was not in operation during the given cost report year, then the entity should not be reported.
Please note that this information for Schedule 1 will be entered in the "Reporting Hierarchy" tab of the Home Care Tool. All information entered in this location will automatically populate in the "Cost Report Schedules" tab (location where the cost report schedules are to be completed).
Schedule 2: General Information - Entity
E Note: Schedule 2 contains entity-level information.
This General Information Schedule contains information at the entity level and will populate the below information for each of the entities (CHHA, LHCSA, or FI) operated by the agency. The number of tables that appear on this schedule will correlate with the total number of CHHA, LHCSA, and FI entities that appear on Schedule 1. For example, having 2 CHHA, 2 LHCSA, and 2 FI entities in Schedule 1 would result in six Schedule 2 tables appearing. These tables will populate automatically based on the information entered in the "Reporting Hierarchy" tab of the Home Care Tool.
Information that will appear on this schedule (depending on entity type) includes the following:
Entity Information
- Name of Entity: Enter the legal name of the organization.
- Type: Select the entity type (Proprietary, Voluntary, or Public) from the drop-down menu.
- Address: Enter the street address of the entity headquarters.
- City: Enter the name of the city where the entity headquarters is located.
- State: Enter the state where the entity headquarters is located.
- Zip: Enter the zip code for the entity headquarters.
- County Served: Select the county where services are provided by this entity from the drop-down box.
- MMIS ID Number: Enter the MMIS ID Number of each CHHA, LHCSA, or FI entity.
- Note: All Medicaid Management Information System ID numbers should be eight digits.
- Operating Certificate: Enter the Operating Certificate of any CHHA entities.
- Note: All operating certificates should be seven or eight digits.
- License Number: Enter the License Number of any LHCSA entities.
- Direct Care Standard Hours Per Work Week: Enter your entity's standard work week for a direct care worker (e.g., 40 hours per week). This would be the standard hours for an individual and would not include items like overtime.
- Program Administration Standard Hours Per Week: Enter your entity's standard work week for an administrative worker (e.g., 37.5 hours per week). This would be the standard hours for an individual and would not include items like overtime.
- Reporting Period (From and To): Enter time period during the cost report year that the data will be reported for the entity. For example, if an entity was only operational for July through December of the cost report year, this should be indicated here.
Contact Person
The name of the person that can answer questions regarding the cost report submission. Include this person's first and last name, job title, telephone number, and email address (required fields).
Schedule 3a, Schedule 3b, and Schedule 3c: Costs and Expenses
E Note: Schedule 3a, 3b, and 3c require entity-level information.
Schedule 3a, Schedule 3b, and Schedule 3c require the reporting of costs and expenses by service type for each CHHA, LHCSA, and FI entity operated by the agency. Note that an agency is required to complete more than one of the following schedules if they operate more than one of these entity types:
- Schedule 3a (for CHHA costs and expenses) - A separate Schedule 3a table should be completed for each unique CHHA entity.
- Schedule 3b (for LHCSA costs and expense) - A separate Schedule 3b table should be completed for each unique LHCSA entity.
- Schedule 3c (for FI costs and expenses) - A separate Schedule 3c table should be completed for each unique FI entity.
Please follow the below instructions while completing Schedule 3a, Schedule 3b, and Schedule 3c.
Note that in order to best complete these schedules, you should reference your facilities' trial balance, general ledger detail, payroll register, FTE report, and reconciliation between the general ledger and financial statements.
Note that you should enter data in Columns 002 and 004 through 010. Columns 001 and 003 will be automatically calculated based on the information entered into Columns 002 and 004 through 010.
Please note that you should report all costs on Schedules 3a, 3b, and 3c (includes direct care costs, administrative personnel costs, and nonpersonnel costs). These costs need to be allocated to the appropriate service type rows. The "Total Entity Costs" on Schedule 3 should reconcile to the total expenses per your agency's financial statements. Agencies are encouraged, but not required in 2021, to complete the "Financial Reconciliation" tab of the Tool after all cost report schedules have been completed. This tab will provide you with an opportunity to identify any reconciling items that may be causing the total expenses on Schedule 3 to differ from the total expenses per your financial documentation. Note that agencies selected for audit will be required to complete the "Financial Reconciliation" tab of the Tool.
- Column 001: Total Entity Costs - Column 001 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 002 (Non-Allowable Costs) and Column 003 (Total Allowable Costs). The Total Entity Costs value should reconcile to the total expenses per the agency's financial statements.
- Column 002: Non-Allowable Costs (Adjustment to Expenses) - Include in this column the reconciliation of interest offsets and recoveries of expense and non-allowable costs, which should not be included in Columns 004 through 010. To be considered as allowable in determining reimbursement rates, costs shall be properly chargeable to necessary patient care. Allowable costs shall be determined by the application of the principles of reimbursement developed for determining payments under Title XVIlI of the Federal Social Security Act (Medicare) program. Cost that are non-allowable in nature include, but are not limited to, the below list. When assessing whether or not a cost is allowable, note that allowable costs shall not include the following:
- Amounts in excess of reasonable or maximum title XVIII of the Federal Social Security Act (Medicare) costs or in excess of customary charges to the general public. This provision shall not apply to services furnished by public providers free of charge or at a nominal fee.
- Expenses or portions of expenses reported by individual entities which are determined by the commissioner not to be reasonable related to the efficient production of patient care services because of either the nature or the amount of the particular item.
- Costs not properly related to patient care or treatment which principally afford diversion, entertainment or amusement to owners, operators or employees of agencies or entities.
- Meal expenses and advertising costs for the purposes of attracting patients.
- Cash receipt assessment tax.
- Any interest charged related to rate determination or penalty imposed by governmental agencies or courts, and the costs of policies obtained solely to insure against the imposition of such a penalty.
- Costs of contributions or other payments to political parties, candidates or organizations and charities.
- The interest paid to a lender related through control, ownership, affiliation, or personal relationship to the borrower, except in instances where the approval of the Commissioner of Health has been obtained (For costs incurred on or after January 1, 1992).
- The expenses which were required to be funded from the Worker Recruitment and Retention Revenue received through the rate add-on. The CHHA Worker Recruitment and Retention add-on is calculated in accordance with Public Health Law 3614, Section 8. The CHHA Worker Recruitment, Training and Retention add-on is calculated in accordance with Public Health Law 3614, Section 9. The LHCSA Worker Recruitment and Retention add-on is calculated in accordance with Chapter 1 of the Laws of 2002, which added Section 367-q of the Social Services Law.
Note that non-allowable costs should be recorded as positive values. The portion of total costs that is non-allowable should be separated from the costs reported in Columns 004-010 and reported in Column 002. The total allowable plus non-allowable costs should add up to the agency's total costs. - Column 003: Allowable Costs - Column 003 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 004 through Column 010. Below is a description of allowable costs which are to be used when completing Columns 004 through 010. Allowable costs shall include, but are not limited to, the following:
- A monetary value assigned to services provided by religious orders and for services rendered by an owner or an operator of an entity
- The portion of the dues paid to any professional association which has been demonstrated, to the satisfaction of the commissioner, to be allocable to expenditures other than for public relations advertising or political contributions
- Costs reduced by income earned for Medicare Part B eligible services
- Those costs allocated to the patient care entity from a related organization to the extent that:
- Those costs are reasonably related to the efficient production of patient care services; and
- The base of allocation of such costs are consistent with regulations applicable to the cost reporting of the related organization.
- Column 004: Program Administration - All Program Administration (Personnel and Non-Personnel) costs should be reported in Column 004 on Schedule 3. This includes, but may not be limited to, the following:
- Criminal Background Check & Fingerprinting
- Capital Related - Building & fixtures, movable equipment
- Plant Operations & Maintenance
- Costs of operations, maintenance, and repairs to the provider entity facility
- Rent - Building, furnishings, vehicles
- Interest-Property
- Depreciation - Plant, equipment & furnishings, vehicles
- Administrative Worker Transportation
- Utilities - Gas, electricity, fuel, water
- Office Supplies & Materials
- Office Supplies and Expenses
- Postage/Freight/Messenger Service
- Copying/Printing
- Pencils/pens, folders, note pads, and the printing of office forms, letterhead and envelopes.
- Administrative employee physicals/uniforms/immunizations
- Administration & General expenses (examples in the sub-bullets below)
- Program Administration Worker salary/compensation costs
- Program Administration Worker fringe benefits and payroll tax:
- FICA taxes (Social Security + Medicare)
- Insurance (Life/Health)
- Pension & Retirement
- Workers' Compensation UID/Disability
- Employee Physicals
- Vacation Accrual
- Metropolitan Commuter Transportation (MTA) Tax
- Electronic Data Processing (EDP)/Computer Expenses
- Telephone Expenses
- Professional Fees (e.g., accounting services, legal services, maintenance services, cleaning, bookkeeping, administrative computer services, and other administrative-related contracted purchased services not related to direct patient care)
- Training/Education/Recruitment
- Books/Dues/Subscriptions
- Travel Expenses & Reimbursement
- Interest (non-capital)
- Insurance (non-capital)
- Billing services
- Medicaid Processing & Collections Services
- Payroll Processing Services
- Costs of advertising, public relations or promotion when such costs are specifically related to the provision of personal care services and are not for the purpose of attracting patients
The Grand Total row of Column 004 (Program Administration) on Schedule 3 should equal the Grand Total row of Column 004 (Program Administration) on Schedule 4. The Program Administration costs are the same on Schedules 3 and 4, but are being allocated in different ways. On Schedule 3, program administration costs should be allocated across the different service type rows that the agency provides using an allocation methodology (see on page 4 of this document for a description of allocation methodology). Note that an edit check exists within the Web-based Tool that will warn agencies if the values in Column 004 on Schedule 3 and Column 004 on Schedule 4 are not equal (at both the agency and entity level).
Additionally, note that taxes and benefits should be allocated appropriately to program administration workers in this column. Taxes and benefits for direct care workers should not be reported in this column.
- Direct care worker salary/compensation
- Direct care worker benefits & payroll taxes:
- FICA taxes (Social Security + Medicare)
- Life/Health Insurance
- Pension & Retirement
- Disability/Unemployment/Workers’ Compensation taxes
- Employee physicals
- Medical Supplies
- Other costs that can be directly attributable to the provision of care
- Program RN Supervision/Assessment worker salary/compensation
- Program RN Supervision/Assessment worker benefits & payroll taxes:
- FICA taxes (Social Security + Medicare)
- Life/Health Insurance
- Pension & Retirement
- Disability/Unemployment/Workers’ Compensation taxes
- Employee physicals
- Other costs that can be directly attributable to the provision of care related to nursing supervision and nursing assessment
Note: This Grand Total of this column does not need to equal the Grand Total of Column 007 (Program Staff Training) on Schedule 4.
- Direct care only costs (e.g., direct care wages associated with attending training) would not need to be reported in Column 007 (Program Staff Training) on Schedule 4.
- Only the associated administrative personnel and non-personnel portion of the costs would appear in Column 007 (Program Staff training) on Schedule 4.
Note: Costs associated with paying direct care workers to travel (travel time wages) should not be reported here, but rather should be reported in Column 005 (Program Aide [Direct Care]).
Important information on contracting relationships:
In a direct care contracting service relationship, only one of the two agencies involved in the relationship may report the expenses on the Home Care Cost Report.
- The subcontractor should report the expenses they incurred performing the direct care services (e.g., paying the direct care worker for the hours worked providing the service, transportation for the worker to get to the patient to provide the subcontractor services, etc.), not the revenue received for the services, on Schedule 3 within the “Other non-allowable services” row in Column 005 (Program Aide Direct Care).
- The agency contracting out the direct care service should report the cost they incurred purchasing the service (e.g., the amount they paid the subcontractor) in Column 009 Contracted Purchased Services, within the appropriate service type row on Schedule 3.
Example: For LHCSA entities acting as the subcontractor to a CHHA for the delivery of Home Health Aide services, these costs would be reported in the "Other non-allowable services" row in the "Program Aide (Direct Care)" column (Column 005).
Note: All administrative contracting service expenses (e.g., accounting services, legal services, maintenance services, etc.) should be reported in Column 004 (Program Administration) on Schedules 3 and 4.
For more information related to the Direct Care line items, please reference the Universal Billing Codes for Long Term Care Services in Appendix A. Note that Appendix A is related to Managed Care and does not contain information related to Fee-for-Service rate codes.
Schedule 4a, Schedule 4b, and Schedule 4c: General Service Cost Centers
E Note: Schedule 4a, 4b, and 4c require entity-level information.
Schedule 4a, Schedule 4b, and Schedule 4c require the reporting of general service cost centers for each CHHA, LHCSA, and FI entity operated by the agency. Note that an agency is required to complete more than one of the following schedules if they operate more than one of these entity types:
- Schedule 4a (for CHHA general service costs) - A separate Schedule 4a table should be completed for each unique CHHA entity.
- Schedule 4b (for LHCSA general service costs) - A separate Schedule 4b table should be completed for each unique LHCSA entity.
- Schedule 4c (for FI general service costs) - A separate Schedule 4c table should be completed for each unique FI entity.
Please follow the below instructions while completing Schedule 4a, Schedule 4b, and Schedule 4c.
Note that in order to best complete these schedules, you should reference your facilities' trial balance, general ledger detail, square footage reports, mileage logs, and allocation methodology.
Please note that Schedule 4 should contain administrative personnel costs and non-personnel costs. Direct care worker wages and benefits should not appear on Schedule 4. Costs in this schedule need to be allocated to the appropriate general service cost center.
- Column 001: Total Entity Costs - Column 001 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 002 (Non-Allowable Costs) and Column 003 (Total Allowable Costs). The "Total Entity Costs" amount should be greater on Schedule 3 than on Schedule 4, as Schedule 4 should not include any direct care worker wage and benefit costs.
- Column 002: Non-Allowable Costs (Adjustment to Expenses) - Include in this column the reconciliation of interest offsets and recoveries of expense and non-allowable costs. Allowable costs shall be determined by the application of the principles of reimbursement developed for determining payments under Title XVIlI of the Federal Social Security Act (Medicare) program.
For further guidance related to allowable costs, reference "Column 002: Non-Allowable Costs (Adjustment to Expenses)" in the instructions for Schedule 3a, Schedule 3b, and Schedule 3c.
Non-allowable costs should be recorded as positive values. The portion of total costs that is non-allowable should be separated from the costs reported in Columns 004-010 and reported in Column 002. - Column 003: Allowable Costs - Column 003 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 004 (Program Administration), Column 005 (Program Aide [Direct Care]), Column 006 (Program RN Supervision/Assessment [Direct Care]), Column 007 (Program Staff Training), Column 008 (Transportation), Column 009 (Contracted Purchased Services), and Column 010 (Other).
Note that bad debt should be reported as an offset to revenue and should not be reported with costs on Schedule 4a, Schedule 4b, or Schedule 4c. - Column 004: Program Administration - All Program Administration (Administrative personnel and non-personnel) costs should be reported in Column 004 on Schedule 4, within the appropriate cost center row. Examples of program administration costs include the following:
- Criminal Background Check & Fingerprinting
- Capital Related - Building & fixtures, movable equipment
- Plant Operations & Maintenance
- Costs of operations, maintenance, and repairs to the provider entity facility
- Rent - Building, furnishings, vehicles
- Interest-Property
- Depreciation - Plant, equipment & furnishings, vehicles
- Administrative Worker Transportation
- Utilities - Gas, electricity, fuel, water
- Office Supplies & Materials
- Office Supplies and Expenses
- Postage/Freight/Messenger Service
- Copying/Printing
- Pencils/pens, folders, note pads, and the printing of office forms, letterhead and envelopes.
- Administrative employee physicals/uniforms/immunizations
- Administration & General expenses (examples in the sub-bullets below)
- Program Administration Worker salary/compensation costs
- Program Administration Worker fringe benefits and payroll tax:
- FICA taxes (Social Security + Medicare)
- Insurance (Life/Health)
- Pension & Retirement
- Workers' Compensation UID/Disability
- Employee Physicals
- Vacation Accrual
- Metropolitan Commuter Transportation (MTA) Tax
- Electronic Data Processing (EDP)/Computer Expenses
- Telephone Expenses
- Professional Fees (e.g., accounting services, legal services, maintenance services, cleaning, bookkeeping, administrative computer services, and other administrative-related contracted purchased services not related to direct patient care)
- Training/Education/Recruitment
- Books/Dues/Subscriptions
- Travel Expenses & Reimbursement
- Interest (non-capital)
- Insurance (non-capital)
- Billing services
- Medicaid Processing & Collections Services
- Payroll Processing Services
- Costs of advertising, public relations or promotion when such costs are specifically related to the provision of personal care services and are not for the purpose of attracting patients
The Grand Total row of Column 004 (Program Administration) on Schedule 3 should equal the Grand Total row of Column 004 (Program Administration) on Schedule 4. The Program Administration costs are the same on Schedules 3 and 4, but are being allocated in different ways. On Schedule 3, program administration costs should be allocated across the different service type rows that the agency provides using an allocation methodology (see on page 4 of this document for a description of allocation methodology). Note that an edit check exists within the Web-based Tool that will warn agencies if the values in Column 004 on Schedule 3 and Column 004 on Schedule 4 are not equal (at both the agency and entity level).
Note: Also recorded here should be the proportional expenditures for administrative services of professional staff (i.e., nurses) who spend less than 100 percent of their time performing administrative services that apply to the total program. Included in this cost center are the expenditures for administrative supervision of aides.
- Criminal Background & Fingerprinting
- Employee physicals/uniforms/immunizations
- Medical supplies
- Other
- Criminal Background & Fingerprinting
- Employee physicals/uniforms/immunizations
- Other
- Criminal Background & Fingerprinting
- Employee physicals/uniforms/immunizations
- Medical Supplies
- Other
For the line items in Schedule 4a, Schedule 4b, and Schedule 4c, please reference the below guidance for details surrounding appropriate inclusion of costs. All items in this section deal largely with non-personnel expenses.
- Criminal Background Check & Fingerprinting - Expenditures related to conducting background check and fingerprinting of potential employees prior to hiring.
- Capital Related: Building & Fixtures - In this category, report the acquisition cost, freight, delivery, and installation charges to maintain or improve fixed assets, such as buildings.
- Capital Related: Movable Equipment - In this category, report the acquisition cost, freight, delivery and installation charges of minor equipment and furnishings, such as typewriters, adding machines, chairs, tables. Minor equipment and furnishings defined as costing less than $1,000. Individual items costing $1,000 or more are to be capitalized and the resultant depreciation charged to the "Depreciation: Equipment & Furnishings" line.
- Plant Operations & Maintenance - Include in this category, report all costs of operations, maintenance, and repairs to the provider entity facility. Expenditures for repairs costing $1000 or more, which prolong the useful life of an asset, increase its value, or adapt it to a different use shall be capitalized with the allowable depreciation and reported on the "Depreciation-Plant" line.
- Rent: Building - Rental charges as specified in the lease agreement are to be reported on this line.
- Rent: Furnishings - Include in this category all rental costs, including installation charges, if any, of leased equipment or furnishings, such as desks, chairs, computers, and copier machines. This account is restricted to items that are necessary for operating the provider entity.
- Rent: Vehicles - Include in this category rental costs of entity vehicles used in the provision of patient care services. Include any service or maintenance expenses if they are part of the rental/lease agreement.
- Interest: Property - Interest expense on bank loans, bonds, mortgages, or similar instruments is allowable if such expense was incurred to finance the purchase of fixed assets, major equipment, furnishings, or vehicles for providing patient care services.
- Depreciation: Plant - An allowance for depreciation of buildings based on accepted accounting principles using the original acquisition cost or donated value if title is held by the provider entity. The straight-line method should be used in conformity with the useful lives stated in "American Hospital Association Estimated Useful Lives of Depreciable Hospital Assets," latest edition.
- Depreciation: Equipment & Furnishings - An allowance for depreciation of equipment and furnishings using the same guidelines as stated above for buildings.
- Depreciation: Vehicles - An allowance for depreciation of vehicles using the same guidelines as stated above for buildings.
- Transportation - Expenditures for travel expenses incurred for administrative purposes only. These expenditures should include items such as gas and mileage, and not travel time wages paid to employees.
- Utilities - Expenditures for items such as gas, electricity, fuel and water necessary for the operation of the provider entity's facility.
- Office Supplies & Materials - Expenditures for consumable office supplies such as pencils/pens, folders, note pads, and the printing of office forms, letterhead and envelopes. Postage costs should also be included in this row.
- Insurance - Include in this category insurance costs including liability, fire and theft, burglary, plate glass, automobile, etc. Credit this line with any dividends, refunds, and rebates received from insurance carriers or agents. Insurance relating to employees' benefits should not be entered on this line.
- Administration & General - Expenditures for maintaining the daily operations of the provider entity. Specific examples of items that can be reported in this row can be found within the instructions for each of the columns.
- Medical supplies - Include any medical supplies such as masks and gloves.
- Employee physicals/uniforms/immunizations - Expenditures for employee physicals, uniforms, and immunizations.
- Other - Include any general service cost center expenditures that do not fall into one of the above categories. If an amount is entered into this line, an explanation/description to indicate the nature of the cost may be required.
Schedule 5a.1, Schedule 5a.2, Schedule 5b, and Schedule 5c - Service Statistics
E Note: Schedule 5a.1, 5a.2, 5b, and 5c require entity-level information.
Schedule 5a.1, Schedule 5a.2, Schedule 5b, and Schedule 5c include the service statistics broken down by service type and payor source at the entity level. Note that an agency is required to complete more than one of the following schedules if they operate more than one of these entity types:
- Schedule 5a.1 (for CHHA Pediatric service statistics) - A separate Schedule 5a.1 table should be completed for each unique CHHA entity reporting CHHA Pediatric service statistics.
- Schedule 5a.2 (for CHHA Episodic service statistics) - A separate Schedule 5a.2 table should be completed for each unique CHHA entity reporting CHHA Episodic service statistics.
- Schedule 5b (for LHCSA service statistics) - A separate Schedule 5b table should be completed for each unique LHCSA entity.
- Schedule 5c (for FI service statistics) - A separate Schedule 5c table should be completed for each unique FI entity.
Schedule 5a.1, Schedule 5a.2, Schedule 5b, and Schedule 5c are used to aggregate units of service by program type for all individual entities operated by the agency as related to CHHAs, LHCSAs, and FIs by cost reporting period. This section should not include units of service related to non-certifiable programs. Agencies should report all visits/hours on Schedule 5 within the appropriate payor source column and service type row, regardless of whether the provider was reimbursed for the visit.
Please follow the below instructions while completing Schedule 5a.1, Schedule 5a.2, Schedule 5b, and Schedule 5c:
Note that in order to best complete these schedules, you should reference your facilities' statistical payor data report that includes patients, visits, and hours and is separated by payor and service type.
Please review the below information related to Medicaid FFS and Medicaid Managed Care before completing Schedule 5a.1, Schedule 5a.2, Schedule 5b, and/or Schedule 5c.
- For Medicaid FFS, New York State provides direct reimbursement for the services provided (e.g., you receive a check or direct deposit from New York State).
- For Medicaid Managed Care, reimbursement is provided through contracts that providers have with MLTCs/MCOs (e.g., Empire, BlueCross, AgeWell, Aetna Better Health, etc.).
- Columns 001, 004, 013, 016, and 019: Patients - Data entered into these columns should represent the number of patients associated with the given column header (Medicaid Fee-for-Service [FFS], Medicaid Managed Care [MC], Medicare, Private Pay, or Other). Note the following:
- You should use the primary payor to determine where to report a patient (e.g., Medicaid versus Medicare for a dual-eligible patient).
- Note that the "Other" column should include commercial, government (such as Veterans Affairs and New York State Office for the Aging), workers' compensation, and no-fault insurance items. If any other items are included, agencies may be required to provide an explanation.
- Columns 002, 005, 014, 017, and 020: Visits/Days - Data entered in these columns should represent the total number of billable/paid visits or days of service associated with their given column header (Medicaid Fee-for-Service [FFS], Medicaid Managed Care [MC], Medicare, Private Pay, or Other). Note the following:
- You should use the primary payor to determine where to report the applicable visits/days (e.g., Medicaid versus Medicare for a dual-eligible patient).
- Note that the "Other" column should include commercial, government (such as Veterans Affairs and New York State Office for the Aging), workers' compensation, and no-fault insurance items. If any other items are included, agencies may be required to provide an explanation.
- Columns 003, 006, 012, 018, 021: Hours - Data entered in this column should represent the total hours for each service provided during the report period associated with their given column header (Medicaid Fee-for-Service [FFS], Medicaid Managed Care [MC], Medicare, Private Pay, or Other). Note the following:
- You should use the primary payor to determine where to report the applicable hours (e.g., Medicaid versus Medicare for a dual-eligible patient).
- Note that the "Other" column should include commercial, government (such as Veterans Affairs and New York State Office for the Aging), workers' compensation, and no-fault insurance items. If any other items are included, agencies may be required to provide an explanation.
- Dual-Eligible (Columns 010, 011, and 012) - Dual-eligible patients need to be captured in a specific way in Schedule 5a.1, Schedule 5a.2, Schedule 5b, and Schedule 5c. When reporting the patients (Column 010), visits/days (Column 011), and hours (Column 012) statistics for dual-eligible individuals, they should be reported in the Dual-eligible columns as well as the columns that are associated with the primary payor (e.g., Medicaid or Medicare). Since the Total Unique columns (022, 023, and 024) do not factor the dual-eligible columns into the calculation, this schedule can track dual-eligible statistics while also calculating the total unique patients, visits/days, and hours.
- Note that reporting a patient in the dual-eligible column would mean that the patient had Medicaid and Medicare dual coverage. A patient and the associated unit of service reported in the dual-eligible column should also be reported in either the Medicaid or Medicare columns. Reporting in this manner allows the dual-eligible information to be captured and also allows the automated calculated totals columns (022, 023, and 024) to calculate the total unique values since these automated calculations do not include the information from the dual-eligible columns.
- Column 007: Total Medicaid Patients - Column 007 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 001 (Medicaid Fee-for-Service Patients) and Column 004 (Medicaid Managed Care Patients).
- Column 008: Total Medicaid Visits/Days - Column 008 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 002 (Medicaid Fee-for-Service Visits/Days) and Column 005 (Medicaid Managed Care Visits/Days).
- Column 009: Total Medicaid Hours - Column 009 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 003 (Medicaid Fee-for-Service Hours) and Column 006 (Medicaid Managed Care Hours).
- Columns 022: Total Unique Patients - Column 022 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 001 (Medicaid Fee-for-Service Patients), Column 004 (Medicaid Managed Care Patients), Column 013 (Medicare Patients), Column 016 (Private Pay Patients), and Column 019 (Other Patients). Note that this column does not include the number of dual-eligible patients in the calculation. As such, Column 022 represents the total number of unique patients.
- Column 023: Total Unique Visits/Days - Column 023 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 002 (Medicaid Fee-for-Service Visits/Days), Column 005 (Medicaid Managed Care Visits/Days), Column 014 (Medicare Visits/Days), Column 017 (Private Pay Visits/Days), and Column 020 (Other Visits/Days). Note that this column does not include the number of dual-eligible visits/days in the calculation. As such, Column 023 represents the total number of unique visits/days.
- Column 024: Total Unique Hours - Column 024 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 003 (Medicaid Fee-for-Service Hours), Column 006 (Medicaid Managed Care Hours), Column 015 (Medicare Hours), Column 018 (Private Pay Hours), and Column 021 (Other Hours). Note that this column does not include the number of dual-eligible hours in the calculation. As such, Column 024 represents the total number of unique hours.
- Report Fields - There are some fields in Schedule 5a.1, Schedule 5a.2, Schedule 5b, and Schedule 5c that aren't applicable to certain parties that will be filling out the cost report. For example, for specific services, the unit of service is only measured by visits, not hours. All columns that should not have data entered in them are highlighted in gray.
If your agency tracks Home Health Registered Nurse services or Sign Language/Oral Interpreter units of service in hours, you will need to convert the service hours to visits to be able to report in the “visits/days” columns on Schedule 5. DOH determined the conversions for these two service types:- Home Health Registered Nurse - Assume that one RN visit/day is equal to one hour
- Sign Language/Oral Interpreter - Assume that one SL/OI visit/day is equal to one hour
When submitting supporting documentation for Schedule 5a.1, Schedule 5a.2, Schedule 5b, and/or Schedule 5c, agencies should note that this statistical data should be substantiated by third-party/system-generated reports to demonstrate the completeness and accuracy of the data included in the cost report. Additionally, agencies should clearly label the payor types (e.g., Medicaid Fee-for-Service versus Medicaid Managed Care) within the supporting documentation files submitted.
Schedule 6 - FI Tier Statistics
E Note: Schedule 6 requires entity-level information.
Schedule 6 includes the Fiscal Intermediary Medicaid tier statistics broken down by service type. As it pertains to Schedule 6, a member month is defined as a count of months that a patient has utilized services.
Please follow the below instructions while completing Schedule 6:
Note that in order to best complete this schedule, you should reference your facilities' statistical payor data report that includes member month hour ranges separated by Medicaid Fee-for-Service versus Medicaid Managed Care payors and service type.
- Column 001: Tier 1 FFS Member Months for 1–159 hours - Data entered into this column should represent the FFS Tier 1 member months for 1–159 hours.
- Column 002: Tier 2 FFS Member Months for 160–479 hours - Data entered into this column should represent the Tier 2 FFS member months for 160–479 hours.
- Column 003: Tier 3 FFS Member Months for 480+ hours - Data entered into this column should represent the Tier 3 FFS member months for 480+ hours.
- Column 004: Tier 1 MC Member Months for 1–159 hours - Data entered into this column should represent the Tier 1 Managed Care member months for 1–159 hours.
- Column 005: Tier 2 MC Member Months for 160–479 hours - Data entered into this column should represent the Tier 2 Managed Care member months for 160–479 hours.
- Column 006: Tier 3 MC Member Months for 480+ hours - Data entered into this column should represent the Tier 3 Managed Care member months for 480+ hours.
- Column 007: Tier 1 FFS + MC Member Months for 1–159 hours - Column 007 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 001 (Tier 1 FFS member months for 1–159 hours) and Column 004 (Tier 1 MC member months for 1–159 hours).
- Column 008: Tier 2 FFS + MC Member Months for 160–479 hours - Column 008 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 002 (Tier 2 FFS member months for 160–479 hours) and Column 005 (Tier 2 MC member months for 160–479 hours).
- Column 009: Tier 3 FFS + MC Member Months for 480+ hours - Column 009 does not require any information to be entered. This column is an automated calculation and reflects the sum of Column 003 (Tier 3 FFS member months for 480+ hours) and Column 006 (Tier 3 MC member months for 480+ hours).
Schedule 7a, Schedule 7b, and Schedule 7c - Current Charge to the General Public
E Note: Schedule 7a, 7b, and 7c require entity-level information.
Schedule 7a, Schedule 7b, and Schedule 7c include the current charge to the general public. Note that an agency is required to complete more than one of the following schedules if they operate more than one of these entity types:
- Schedule 7a (for CHHA Current Charge to the General Public) - A separate Schedule 7a table should be completed for each unique CHHA entity.
- Schedule 7b (for LHCSA Current Charge to the General Public) - A separate Schedule 7b table should be completed for each unique LHCSA entity.
- Schedule 7c (for FI Current Charge to the General Public) - A separate Schedule 7c table should be completed for each unique FI entity.
Please follow the below instructions while completing Schedule 7a, Schedule 7b, and Schedule 7c:
The Current Charge to the General Public information should be as of December 31st of the cost report year.
Note that in order to best complete these schedules, you should reference your facilities' chargemaster. Please ensure the unit of service from the chargemaster that is reported is consistent with the unit of service listed (i.e., hours, days, or visits).
- Column 001: Current Charge to the General Public - For each service that your entity provides, enter the public charges which have been approved by the governing authority. These charges are what an individual with no coverage would pay for a service and should reflect the charge per unit of service (i.e., visit, hours, days).
For any information entered in the "Other" line, an explanation may be required to indicate what service this amount relates to.
Schedule 8a, Schedule 8b, and Schedule 8c - Employee Compensation Analysis
E Note: Schedule 8a, 8b, and 8c require entity-level information.
Schedule 8a, Schedule 8b, and Schedule 8c include the compensation analysis for employees. Note that an agency is required to complete more than one of the following schedules if they operate more than one of these entity types:
- Schedule 8a (for CHHA employee compensation analysis) - A separate Schedule 8a table should be completed for each unique CHHA entity.
- Schedule 8b (for LHCSA employee compensation analysis) - A separate Schedule 8b table should be completed for each unique LHCSA entity.
- Schedule 8c (for FI employee compensation analysis) - A separate Schedule 8c table should be completed for each unique FI entity.
Please follow the below instructions while completing Schedule 8a, Schedule 8b, and Schedule 8c:
Note that in order to best complete these schedules, you should reference your facilities' FTE report with employee ID number, salaries/wages and hours by department and cost center grouping, pay code, and job type. In addition, you should reference your facilities' trial balance, general ledger detail, and employee benefits report with employee ID number by department and cost center grouping, and job type.
Additionally, the information entered on Schedule 8a, Schedule 8b, and Schedule 8c is similar but not identical to the information to Schedule 3a, Schedule 3b, and Schedule 3c. Information reported on 8a, 8b, and 8c should be reported on 3a, 3b, and 3c, but there will not be a direct tie out because the schedules are requesting information in a different manner.
Schedule 8a (CHHA) and Schedule 8b (LHCSA)
The FTE, Salary, and Employee Benefits columns should be completed for the applicable job title headers (Supervisors, Nurses, Aides, Clinical/Therapy, and Other) of employees who perform home care service-related duties. Employees who perform job duties for your agency that are not related to home care services should not be included in Schedule 8a or Schedule 8b. Any data reported as "Other" will need to be accompanied by documentation for supporting the nature of the work being reported.
- Columns 001, 004, 007, 010, and 013: FTE - Report the result of the total number of employee hours paid divided by the product of your entity's standard work week (e.g., 37.5 hours, 40 hours, etc.) times 52 weeks per year. Report FTE(S) to three decimal places.
- Columns 002, 005, 008, 011, and 014: Salary - This is the base salary amount and any other wages (e.g., overtime wages) paid to all employees in the job type title for the reporting period. The amount must be reported in whole dollars.
- Columns 003, 006, 009, 012, and 015: Employee Benefits - Report all costs for mandated and not mandated benefits made available to all employees that correspond to the job type title for the reporting period.
- Column 016: Total FTE - This column is an automated calculation and reflects the sum of Column 001, Column 004, Column 007, Column 010, and Column 013.
- Column 017: Total Salary - This column is an automated calculation and reflects the sum of Column 002, Column 005, Column 008, Column 011, and Column 014.
- Column 018: Total Employee Benefits - This column is an automated calculation and reflects the sum of Column 003, Column 006, Column 009, Column 012, and Column 015.
Schedule 8c (FI)
The FTE and Salary columns should be completed for the applicable job title headers (Assistant and Other) of employees who perform home care service-related duties. Employees who perform job duties for your agency that are not related to home care services should not be included in Schedule 8c. Any data reported as "Other" will need to be accompanied by documentation supporting the nature of the work being reported.
- Columns 001 and 004: FTE - Report the result of the total number of employee hours paid divided by the product of your entity's standard work week (e.g., 37.5 hours, 40 hours, etc.) times 52 weeks per year. Report FTE(S) to three decimal places.
- Columns 002 and 005: Salary - This is the base salary amount and any other wages (e.g., overtime wages) paid to all employees in the job type title for the reporting period. The amount must be reported in whole dollars.
- Columns 003 and 006: Employee Benefits - Report all costs for mandated and not mandated benefits made available to employees that correspond to the job type title for the reporting period.
- Column 007: Total FTE - This column is an automated calculation and reflects the sum of Column 001 and Column 004.
- Column 008: Total Salary - This column is an automated calculation and reflects the sum of Column 002 and Column 005.
- Column 009: Total Employee Benefits - This column is an automated calculation and reflects the sum of Column 003 and Column 006.
Schedule 9a and Schedule 9b - Contracted Staff Compensation Analysis
E Note: Schedule 9a and 9b require entity-level information.
Schedule 9a and Schedule 9b include the compensation analysis for contracted staff. Note that an agency is required to complete more than one of the following schedules if they operate more than one of these entity types:
- Schedule 9a (for CHHA contracted staff compensation analysis) - A separate Schedule 9a table should be completed for each unique CHHA entity.
- Schedule 9b (for LHCSA contracted staff compensation analysis) - A separate Schedule 9b table should be completed for each unique LHCSA entity.
Please follow the below instructions while completing Schedule 9a and Schedule 9b:
The FTE and Compensation columns should be completed for the applicable job title headers (Supervisors, Nurses, Aides, Clinical/Therapy, and Other) of contracted staff who perform home care service-related duties. Contracted staff who perform job duties for your agency that are not related to home care services should not be included in Schedule 9a or Schedule 9b. Any data reported as "Other" will need to be accompanied by documentation for supporting the nature of the work being reported.
Note that in order to best complete these schedules, you should reference your facilities' trial balance, general ledger detail, contracted staff invoices for dollars and hours, and contracts that specifies wage costs, hours, and non-labor costs.
Additionally, the information entered on Schedule 9a and Schedule 9b is similar but not identical to the information to Schedule 3a, Schedule 3b, and Schedule 3c. Information reported on 9a and 9b should be reported on 3a and 3b, but there will not be a direct tie out because the schedules are requesting information in a different manner.
- Columns 001, 003, 005, 007, and 009: FTE - Report the result of the total number of contracted staff hours paid divided by the product of your entity's standard work week (e.g., 37.5 hours, 40 hours, etc.) times 52 weeks per year. Report FTE(S) to three decimal places.
- Columns 002, 004, 006, 008, and 010: Compensation - This is the compensation amount paid to all contracted staff in the job type title for the reporting period. The amount must be reported in whole dollars.
- Column 011: Total FTE - This column is an automated calculation and reflects the sum of Column 001, Column 003, Column 005, Column 007, and Column 009.
- Column 012: Total Compensation - This column is an automated calculation and reflects the sum of Column 002, Column 004, Column 006, and Column 008, and Column 010.
Schedule 10a, Schedule 10b, and Schedule 10c - WR&R and Staff Turnover
E Note: Schedule 10a, 10b, and 10c require entity-level information.
Schedule 10a, Schedule 10b, and Schedule 10c include the WR&R and staff turnover analysis broken down by entity service type.
Note that an agency is required to complete more than one of the following schedules if they operate more than one of the below entity types.
- Schedule 10a (for CHHA WR&R and Staff Turnover) - A separate Schedule 10a table should be completed for each unique CHHA entity.
- Schedule 10b (for LHCSA WR&R and Staff Turnover) - A separate Schedule 10b table should be completed for each unique LHCSA entity.
- Schedule 10c (for FI WR&R and Staff Turnover) - A separate Schedule 10c table should be completed for each unique FI entity.
Please follow the below instructions while completing Schedule 10a, Schedule 10b, and Schedule 10c.
Note that in order to best complete these schedules, you should reference your facilities' payroll register run to include recorded date, employee ID number, job/pay code, and department description, etc. In addition, you should reference your facilities' trial balance, general ledger detail, and facility onboarding and termination report from HR.
Schedule 10a (CHHA)
- Column 001: WR&R Costs to Entity - Enter all allowable entity costs related to Worker Recruitment and Retention. The costs reported in this Schedule should directly relate to the recruitment and retention of non-supervisory home care service workers or any worker with direct patient care responsibility. Any funds determined to be used for activities other than recruitment, training, and retention of non-supervisory home care service workers or any worker with direct patient care responsibility shall be recouped. This recoupment will be in addition to any other penalties provided by law.
Reporting should be in accordance with Public Health Law 3614, Section 8:
" 8. (b) (i) Providers which have their rates adjusted pursuant to this subdivision shall use such funds solely for the purposes of recruitment and retention of non-supervisory home care services workers or any worker with direct patient care responsibility. Such purposes shall include the recruitment and retention of non-supervisory home care services workers or any worker with direct patient care responsibility employed in licensed home care services agencies under contract with such providers. Providers are prohibited from using such funds for any other purpose.
(ii) Each such provider shall submit, at a time and in a manner determined by the commissioner, a written certification attesting that such funds will be used solely for the purpose of recruitment and retention of non-supervisory home care services workers or any worker with direct patient care responsibility. The commissioner is authorized to audit each such provider to ensure compliance with the written certification required by this subdivision and shall recoup any funds determined to have been used for purposes other than recruitment and retention of non-supervisory home care services workers or any worker with direct patient care responsibility. Such recoupment shall be in addition to any other penalties provided by law.
(iii) In the case of services provided by such providers through contracts with licensed home care services agencies, rate increases received by such providers pursuant to this subdivision shall be reflected, consistent with the purposes of subparagraph (i) of this paragraph, in either the fees paid or benefits or other supports provided to non- supervisory home care services workers or any worker with direct patient care responsibility of such contracted licensed home care services agencies and such fees, benefits or other supports shall be proportionate to the contracted volume of services attributable to each contracted agency. Such agencies shall submit to providers with which they contract written certifications attesting that such funds will be used solely for the purposes of recruitment and retention of non-supervisory home care services workers or any worker with direct patient care responsibility and shall maintain in their file's expenditure plans specifying how such funds will be used for such purposes. The commissioner is authorized to audit such agencies to ensure compliance with such certifications and expenditure plans and shall recoup any funds determined to have been used for purposes other than those set forth in this subdivision. Such recoupment will be in addition to any other penalties provided by law.
(iv) Funds under this subdivision are not intended to supplant support provided by local government." - Columns 002: WRT&R Costs to Entity - Enter all allowable costs related to Worker Recruitment, Training and Retention. The costs reported in this Schedule should directly relate to the recruitment, training, and retention of non-supervisory home care service workers or any worker with direct patient care responsibility. Any funds determined to be used for activities other than recruitment, training, and retention of non-supervisory home care service workers or any worker with direct patient care responsibility shall be recouped. This recoupment will be in addition to any other penalties provided by law.
Reporting should be in accordance with Public Health Law 3614, Section 9:
"9. Notwithstanding any law to the contrary, the commissioner shall, subject to the availability of federal financial participation, adjust medical assistance rates of payment for certified home health agencies for such services provided to children under eighteen years of age and for services provided to a special needs population of medically complex and fragile children, adolescents and young disabled adults by a CHHA operating under a pilot program approved by the department, long term home health care programs, AIDS home care programs established pursuant to this article, hospice programs established under article forty of this chapter and for managed long term care plans and approved managed long term care operating demonstrations as defined in section forty-four hundred three-f of this chapter. Such adjustments shall be for purposes of improving recruitment, training and retention of home health aides or other personnel with direct patient care responsibility…"
- Column 003: Employees as of 1/1 - Enter the number of people employed by the entity as of January 1st of the reporting year.
- Column 004: Employees as of 12/31 - This column is an automated calculation and reflects the sum of Column 003 and Column 006 less Column 007.
- Column 005: Employees retained as of 12/31 who were employed on 1/1 - Enter the number of people employed by the entity as of December 31st of the reporting year who were also employed by the entity on January 1st of the same reporting year.
- Column 006: Employees Hired between 1/1 and 12/31 - Enter the number of employees hired between January 1st and December 31st of the reporting year.
- Column 007: Employees Separated from Entity During the Year - Enter the number of employees who were separated from the entity during the cost reporting period under review. Note that this column should include employees who were terminated or who voluntarily departed.
Schedule 10b (LHCSA) and Schedule 10c (FI)
- Column 001: WR&R Costs to Entity - Enter all allowable entity costs related to Worker Recruitment and Retention. The costs reported in this Schedule should directly relate to the recruitment and retention of non-supervisory home care service workers or any worker with direct patient care responsibility. Any funds determined to be used for activities other than recruitment, training, and retention of non-supervisory home care service workers or any worker with direct patient care responsibility shall be recouped. This recoupment will be in addition to any other penalties provided by law.
Reporting should be in accordance with Section 367-q of the Social Services Law:
" 4. Personal care services providers which have their rates adjusted pursuant to this section shall use such funds for the purpose of recruitment and retention of non- supervisory personal care services workers or any worker with direct patient care responsibility only and are prohibited from using such funds for any other purpose. Each such personal care services provider shall submit, at a time and in a manner to be determined by the commissioner of health, a written certification attesting that such funds will be used solely for the purpose of recruitment and retention of non-supervisory personal care services workers or any worker with direct patient care responsibility. The commissioner of health is authorized to audit each such provider to ensure compliance with the written certification required by this subdivision and shall recoup any funds determined to have been used for purposes other than recruitment and retention of non- supervisory personal care services workers or any worker with direct patient care responsibility. Such recoupment shall be in addition to any other penalties provided by law." - Column 002: Employees as of 1/1 - Enter the number of people employed by the entity as of January 1st of the reporting year.
- Column 003: Employees as of 12/31 - This column is an automated calculation and reflects the sum of Column 002 and Column 005 less Column 006.
- Column 004: Employees retained as of 12/31 who were employed on 1/1 - Enter the number of people employed by the entity as of December 31st of the reporting year who were also employed by the entity on January 1st of the same reporting year.
- Column 005: Employees Hired between 1/1 and 12/31 - Enter the number of employees hired between January 1st and December 31st of the reporting year.
- Column 006: Employees Separated from Entity During the Year - Enter the number of employees who were separated from the entity during the cost reporting period under review. Note that this column should include employees who were terminated or who voluntarily departed.
Schedule 11a, Schedule 11b, and Schedule 11c - Labor Costs
E Note: Schedule 11a, 11b, and 11c require entity-level information.
Schedule 11a, Schedule 11b, and Schedule 11c include the labor cost figures broken down by entity-level job type. Note that an agency is required to complete more than one of the following schedules if they operate more than one of these entity types:
- Schedule 11a (for CHHA Labor Costs) - A separate Schedule 11a table should be completed for each unique CHHA entity.
- Schedule 11b (for LHCSA Labor Costs) - A separate Schedule 11b table should be completed for each unique LHCSA entity.
- Schedule 11c (for FI Labor Costs) - A separate Schedule 11c table should be completed for each unique FI entity.
Please follow the below instructions while completing Schedule 11a, Schedule 11b, and Schedule 11c.
The information in these schedules should be completed for employees who perform home care service related duties. Employees who perform job duties for your agency that are not related to home care services should not be included in Schedule 11a, Schedule 11b, or Schedule 11c.
Note that in order to best complete these schedules, you should reference your facilities' trial balance, general ledger detail, and payroll register run to include employee ID number, pay codes, and department description, etc.
Additionally, the information entered on Schedule 11a, Schedule 11b, and Schedule 11c is similar but not identical to the information to Schedule 3a, Schedule 3b, and Schedule 3c. Information reported on 11a, 11b, and 11c should be reported on 3a, 3b, and 3c, but there will not be a direct tie out because the schedules are requesting information in a different manner.
- Column 001: Base Wages for Hours Worked - Enter the base wages for employee hours worked. No other wages should be included in this column (i.e., travel wages, overtime wages, holiday wages, differentials should not be included in Column 001)
- Column 002: In-Service Wages - Enter the wages associated with employer sponsored trainings, such as continuing education or other mandated activities, for which employees are paid for the time spent completing.
- Column 003: Travel Wages - Enter the wages paid associated with traveling as part of the defined job function. For example, 1 hour of travel time to a client site would be captured in this column. Items such as gas and mileage should not be reported in this column.
- Column 004: Overtime Wages - Enter the wages paid to employees for hours worked greater than your entity's standard work week.
- Column 005: Weekend and Mutual Differentials - Dollars - Enter the wages paid to employees for weekend and mutual differentials resulting from non-standard shifts.
- Column 006: Holiday Worked Wages - Enter the wages paid to employees for hours worked on days considered to be Holidays. Any Holiday wages paid to employees where services were not physically provided should be reported in Column 007 of this Schedule (Other Wages).
- Column 007: Other Wages - Enter the wages paid to employees for hours worked other than the categories listed for Column 001 through Column 006. Included in this column should be any Holiday wages paid to employees where services were not physically provided. If an amount is entered into this line, an explanation/description may be required to indicate the nature of the wage.
- Column 008: Personal Time Off (PTO) - Dollars - Enter the total amount paid to employees for PTO used and for any PTO that was paid out.
- Column 009: Jury Duty & Bereavement - Dollars - Enter the total amount paid to employees for jury duty and bereavement.
- Column 010: Non-Taxable Fringe - Dollars - Enter the employer contribution portion of non-taxable fringe paid to employees. This column should include items such as retirement accounts or health flexible spending accounts.
- Column 011: FICA Taxes - Enter the employer contribution portion of Social Security and Medicare taxes.
- Column 012: Disability/Unemployment/Workers' Compensation Taxes - Enter the amount paid by the employer for disability, unemployment, and workers' compensation taxes.
- Column 013: Other Fringes - Enter any other fringe amounts in this column that were not covered on the other columns of Schedule 11a, Schedule 11b, or Schedule 11c. If an amount is entered into this line, an explanation/description may be required to indicate the nature of the item.
- Column 014: Total Wages - This column is an automated calculation and reflects the sum of Column 001 through Column 009.
Note that the salaried labor costs for job titles that perform tasks as part of a larger agency will be reported in Schedule 15.
Schedule 12a, Schedule 12b, and Schedule 12c - Labor Utilization
E Note: Schedule 12a, 12b, and 12c require entity-level information.
Schedule 12a, Schedule 12b, and Schedule 12c include the labor utilization figures broken down by entity-level job type. Note that an agency is required to complete more than one of the following schedules if they operate more than one of these entity types:
- Schedule 12a (for CHHA Labor Utilization) - A separate Schedule 12a table should be completed for each unique CHHA entity.
- Schedule 12b (for LHCSA Labor Utilization) - A separate Schedule 12b table should be completed for each unique LHCSA entity.
- Schedule 12c (for FI Labor Utilization) - A separate Schedule 12c table should be completed for each unique FI entity.
Please follow the below instructions while completing Schedule 12a, Schedule 12b, and Schedule 12c.
The information in these schedules should be completed for employees who perform home care service related duties. Employees who perform job duties for your agency that are not related to home care services should not be included in Schedule 12a, Schedule 12b, or Schedule 12c.
Note that in order to best complete these schedules, you should reference your facilities' trial balance, general ledger detail, and FTE report.
- Column 001: FTE - Report the result of the total number of employee hours paid divided by the product of your entity's standard work week (e.g., 37.5 hours, 40 hours, etc.) times 52 weeks per year. Report FTE(S) to three decimal places.
- Column 002: Base Hours Worked - Enter the base hours worked for employees. No other hours should be included in this column (i.e., travel hours, overtime hours, personal time off (PTO) should not be reported in Column 002).
- Column 003: Overtime Hours Worked - Enter the hours worked by employees that are greater than your entity's standard work week.
- Column 004: Travel Time - Hours - Enter the hours associated with traveling as part of the defined job function. For example, 1 hour of travel time to a client site would be captured in this column.
- Column 005: Holiday Hours - Enter Holiday hours for employees. This includes hours worked on days considered to be Holidays as well as any Holiday hours where services were not physically provided.
- Column 006: Total Hours Worked - This column is an automated calculation and reflects the sum of Column 002 through Column 005.
Schedule 13a, Schedule 13b, and Schedule 13c - Average Compensation
E Note: Schedule 13a, 13b, and 13c contains entity-level information.
Schedule 13a, Schedule 13b, and Schedule 313c include the average compensation broken down by entity type.
- Schedule 13a (for CHHA Average Compensation) - A separate Schedule 13a table will be completed for each unique CHHA entity.
- Schedule 13b (for LHCSA Average Compensation) - A separate Schedule 13b table will be completed for each unique LHCSA entity.
- Schedule 13c (for FI Average Compensation) - A separate Schedule 13c table will be completed for each unique FI entity.
Note that these schedules are automated calculations and are derived from data on Schedule 11 and Schedule 12. No data entry is required. The following items are calculated on Schedule 13a, Schedule 13b, and Schedule 13c:
- Column 001: Average Base Hourly Wage
- Formula: Base Wages for Hours Worked (Schedule 11, Column 001) / Base Hours Worked (Schedule 12, Column 002)
- Column 002: Average Total Hourly Compensation
- Formula: Total Wages (Schedule 11, Column 014) / Total Hours Worked (Schedule 12, Column 006)
- Column 003: Average Fringe
- Formula: Sum of Column 008 through 013 on Schedule 11 / FTE (Schedule 12, Column 001)
Schedule 14a, Schedule 14b, and Schedule 14c - Live-In Services
E Note: Schedule 14a, 14b, and 14c require entity-level information.
Schedule 14a, Schedule 14b, and Schedule 14c include the live-in information for each entity type. Note that an agency is required to complete more than one of the following schedules if they operate more than one of these entity types:
- Schedule 14a (for CHHA Live-In) - A separate Schedule 14a table should be completed for each unique CHHA entity.
- Schedule 14b (for LHCSA Live-In) - A separate Schedule 14b table should be completed for each unique LHCSA entity.
- Schedule 14c (for FI Live-In) - A separate Schedule 14c table should be completed for each unique FI entity.
Note that all days, hours, and wages reported should be for actual services.
Note that Continuous Care cannot be identified using billing for services but should be identified by the service authorizations for each patient.
Definitions
Live-in: the provision of care by one personal care aide for a patient who, because of the patient's medical condition, needs assistance during a calendar day with toileting, walking, transferring, turning and positioning, or feeding and whose need for assistance is sufficiently infrequent that a live-in 24-hour personal care aide would be likely to obtain, on a regular basis, five hours daily of uninterrupted sleep during the aide's eight-hour period of sleep.
Continuous Care (Split Shift): the provision of uninterrupted care, by more than one personal care aide, for more than 16 hours in a calendar day for a patient who, because of the patient's medical condition, needs assistance during such calendar day with toileting, walking, transferring, turning and positioning, or feeding and needs assistance with such frequency that a live-in 24-hour personal care aide would be unlikely to obtain, on a regular basis, five hours daily of uninterrupted sleep during the aide's eight hour period of sleep.
Please follow the below instructions while completing Schedule 14a, Schedule 14b, and Schedule 14c.
Note that in order to best complete these schedules, you should reference your facilities' census reports generated with the appropriate service type criteria.
- Column 001: Number of Unique Individuals Served - Enter the total number of unique individuals served for Live-In and Continuous Care (Split Shift) services.
- Column 002: Total Days of Service - For Live-In Services, this column is an automated calculation and reflects the sum of Column 003, Column 004, and Column 005. For Continuous Care (Split Shift) services, this column is not applicable, and no data should be entered.
- Column 003: Days of Service at 13 Hours Per Diem Only - For Live-In Services, enter the days of service at 13 hours per diem only. For Continuous Care (Split Shift), this column is not applicable, and no data should be entered.
- Column 004: Days of Services With Over 13 Hours But Less Than 16 Hours - For Live-In Services, enter the days of service with over 13 hours but less than 16 hours. For Continuous Care (Split Shift), this column is not applicable, and no data should be entered.
- Column 005: Days of Services With 16 or More Hours - For Live-In Services, enter the days of service with 16 or more hours. For Continuous Care (Split Shift), this column is not applicable, and no data should be entered.
- Column 006: Total Hours Worked - For Live-In Services, this column is not applicable, and no data should be entered. For Continuous Care (Split Shift) services, this column is an automated calculation and reflects the sum of Column 007, Column 008, and Column 009.
- Column 007: Hours for Days of Service at 13 Hours Per Diem Only - For Live-In Services, this column is not applicable, and no data should be entered. For Continuous Care (Split Shift) services, enter the hours for days of service at 13 hours per diem only.
- Column 008: Hours for Days of Service With Over 13 Hours But Less Than 16 Hours - For Live-In Services, this column is not applicable and no data should be entered. For Continuous Care (Split Shift) services, enter the hours for days of services with over 13 hours but less than 16 hours.
- Column 009: Hours for Days of Service With 16 or More Hours - For Live-In Services, this column is not applicable, and no data should be entered. For Continuous Care (Split Shift) services, enter the hours for days of services with 16 or more hours.
- Column 010: Average Hours Per Day Per Case - For both Live-In and Continuous Care (Split Shift) Services, this column is an automated calculation and reflects Average Hours Per Day Per Case.
- Column 011: Total Wages - Enter the total wages for both Live-In and Continuous Care (Split Shift) services.
Schedule 15 - Salaried Labor Costs
A Note: Schedule 15 requires agency-level information.
Schedule 15 includes the salaried labor costs at the agency level. Figures should be reported in this Schedule based on resources that provide administrative and executive-level services that cover one or more entity (CHHA, LHCSA, or FI).
Please follow the below instructions while completing Schedule 15:
Note that in order to best complete this schedule, you should reference your facilities' FTE reports with employee name and wage information by department and cost center grouping, pay code, and job type.
- Column 001: FTE - Report the result of the total number of employee hours paid divided by the product of your entity's standard work week (e.g., 37.5 hours, 40 hours, etc.) times 52 weeks per year. Report FTE(S) to three decimal places.
- Column 002: Salary - Report the base salary for the employees that are part of the defined job title.
- Column 003: Fringe Benefits - Enter the total fringe benefits received by the employees that are part of the defined job title.
- Column 004: Bonuses - Enter the total amount of bonuses paid to the employees that are part of the defined job title.
- Column 005: Other Compensation - Enter the total amount of other compensation paid to the employees that are part of the defined job title that does not fall under the categories in Column 002, 003, or 004. If an amount is entered into this line, an explanation/description may be required to indicate the nature of the items included.
Please note that any employee job title that you would like to include on this schedule other than what is included should be entered in an "Other" line. For any data entered in an "Other" job title line, the specific job title needs to be entered in the "Title (if Other)" column. An example of this would be if information needs to be entered for a Chief Technology Officer.
For Direct Care, an example of an applicable job title includes Supervisor. For Program Administration, examples of applicable job titles include CEO, CFO, COO, CTO, Director, Administrator, Scheduler, etc.
Schedule 16 - Top 10 Highest Paid Administrative Officials
A Note: Schedule 16 requires agency-level information.
Schedule 16 requires agencies to report information on their highest paid administrative employees, including name, position, and total compensation figures at the agency-level. Note that this information should be all inclusive and should not represent an allocated amount.
Please follow the below instructions while completing Schedule 16:
Note that in order to best complete this schedule, you should reference your facilities' FTE reports with employee name and wage information by department and cost center grouping, pay code, and job type.
- Officer Name - Enter the first and last name of the individual.
- Position - Enter the individual's job title.
- Salary Compensation - Enter the base salary for the employee.
- Fringe Benefits - Enter the total fringe benefits received by the employee.
- Bonuses - Enter the total amount of bonuses paid to the employee.
- Other Compensation - Enter the total amount of other compensation paid to the employee that does not fall under the salary compensation, fringe benefits, or bonuses categories. If an amount is entered into this line, an explanation/description may be required to indicate the nature of the items included.
Schedule 17 - Balance Sheet (Assets)
A Note: Schedule 17 requires agency-level information.
Schedule 17 requires agencies to report the components of their Total Assets. Agencies will be required to submit supporting documentation to verify the Home Care Cost Report submissions, including annual certified financial statements or other financial documentation that demonstrates reconciling items.
In Schedule 17, accumulated depreciation amounts include the depreciation accumulated on the related assets used in operations. Enter these amounts as a positive.
Accumulated amortization amounts include the cumulative amount of all amortization expense that has been charged against an intangible asset.
- Cash and Cash Equivalents - Report the total of (1) the currency on hand, demand deposits with banks or other financial institutions, and other kinds of accounts that have the general characteristics of demand deposits in that the customer may deposit additional funds at any time and also effectively may withdraw funds at any time without notice or penalty and (2) the cash equivalents which are short term (generally less than three months), highly liquid investments that have both of the following characteristics:
- Readily convertible to known amounts of cash; and/or
- So near their maturity that they present insignificant risk of changes in value because of changes in interest rates.
- Temporary Investments (market value) - The amounts on this line represent current securities evidenced by certificates of ownership or indebtedness. Typical accounts would be marketable securities and other current investments.
- Patient Accounts Receivables - Include on this line all unpaid billings.
- Allowances and Adjustments for Uncollectables - These are valuation (or contra asset) accounts whose credit balances represent the estimated amount of uncollectible receivables from patients and third-party payers. Enter this amount as a positive.
- Other Accounts Receivables - An account receivable is a legally enforceable claim for payment held by a business against its customer/clients for goods supplied and/or services rendered. Report the sum total of Accounts Receivable, Grants Receivable, Contracts Receivable, Patient Services Receivable, Pharmacy Receivable and any other Receivable, except for related-party receivables, that is in substance an accounts receivable, less the allowance for doubtful accounts.
- Inventory - Enter the costs of unused patient care supplies. Perpetual inventory records maybe maintained and adjusted periodically to physical count. The extent of inventory control and detailed record keeping will depend upon the size and organizational complexity of the organization. Inventories may be valued by any generally accepted method, but the method must be consistently applied from year to year.
- Due from Other funds - Report amount due to the agency.
- Prepaid Expenses and other Current Assets - Enter the costs incurred which are properly chargeable to a future accounting period.
- Other Current Assets - These balances include other current assets not included in other assets categories.
- Total Current Assets - Total current assets is an automated calculation.
- Patient Funds Held in Trust (proprietary facilities only) - Enter the value of the patient funds being held in a trust.
- Land - This balance reflects the cost of land used in operations. Included here is the cost of off-site sewer and water lines, public utility, charges for servicing the land, governmental assessments for street paving and sewers, the cost of permanent roadways and of grading of a non-depreciable nature. Unlike building and equipment, land does not deteriorate with use or with the passage of time; therefore, no depreciation is accumulated.
- Land Improvement - Amounts on this line include structural additions made to land, such as driveways, parking lots, sidewalks, as well as the cost of shrubbery, fences and walls, landscaping, on-site sewer and water lines, and underground sprinklers. The cost of land improvements includes all expenditures necessary to make the improvements ready for their intended use.
- Buildings and Fixed Equipment - This line includes the cost of all buildings and subsequent additions used in operations (including purchase price, closing costs, attorney fees, title insurance and real estate broker commission). Included are all architectural, consulting and legal fees related to the acquisition or construction of buildings, and interest paid for construction financing.
- Automobiles and Trucks - The lease and/or rental expense for vehicles used exclusively in program/site and/or program administration functions.
- Major Moveable Equipment - Costs of equipment included on this line has the following general characteristics:
- Ability to be moved, as distinguished from fixed equipment (but not automobiles or trucks).
- A more or less fixed location in the building.
- A unit cost large enough to justify the expense incident to control by means of an equipment ledger and greater than or equal to $5,000.
- Sufficient individuality and size to make control feasible by means of identification tags.
- A minimum life of usually three years or more.
- Used in operations.
- Leasehold Improvements - The expense associated with program/site and/or program administration costs of improvements to leased property that are the service provider's responsibility under the lease terms.
- Minor Equipment (Non-Depreciable) - Costs of equipment included on this line has the following general characteristics:
- Ability to be moved, as distinguished from fixed equipment.
- A more or less fixed location in the building.
- A unit cost large enough to justify the expense incident to control by means of an equipment ledger but less than $5,000.
- Sufficient individuality and size to make control feasible by means of identification tags.
- A minimum life of usually three years or more.
- Used in operations.
- Total Fixed Assets - Total fixed assets is an automated calculation.
- Investments - Report the total investments as defined under U.S. GAAP.
- Mortgage Expense - Any agency administration mortgage expenses.
- Other Assets - These balances include other assets not included in any other assets categories in this Schedule.
- Total Other Assets - Total other assets is an automated calculation.
- Total Assets - Total assets is an automated calculation.
Schedule 18 - Balance Sheet (Liabilities)
A Note: Schedule 18 requires agency-level information.
Schedule 18 requires agencies to report the components of their Total Liabilities, Fund Balances, and Equity. Agencies will be required to submit supporting documentation to verify the Home Care Cost Report submissions, including annual certified financial statements or other financial documentation that demonstrates reconciling items.
- Notes and Loans Payable (Short-Term) - The amounts on this line represent current amounts owing as evidenced by certificates of indebtedness coming due in the next 12 months.
- Accounts Payable - This amount reflects the amounts due trade creditors and others for supplies and services purchased.
- Accrued Compensation and Related Liabilities - Report expenses that a business has incurred but has not yet paid.
- Accrued Expenses Payable - Report the total amount owed to creditors for delivered goods or completed services plus accrued expenses such as salaries payable, accrued payroll taxes, and other accrued liabilities.
- Deferred Revenue - Deferred income is received or accrued income which is applicable to services to be rendered within the next accounting period. Deferred income applicable to accounting periods extending beyond the next accounting period is included as other current liabilities. These amounts also reflect the effects of any timing differences between book and tax or third-party reimbursement accounting.
- Due to Other Funds (Short-Term) - Report any amounts of deposits currently held at another company to be paid within 12 months.
- Other Current Liabilities - Report any other amounts due to be paid to creditors within 12 months.
- Total Current Liabilities - Total current liabilities is an automated calculation.
- Mortgage Payable - This amount reflects the long-term financing obligation used to purchase real estate/property.
- Notes and Loans Payable (Long-Term) - The amounts on this line represent current amounts owing as evidenced by certificates of indebtedness which are not due in the next 12 months.
- Due to Other Funds (Long-Term) - Report any amounts of deposits currently held at another company to be paid in a period not within the next 12 months.
- Due to Related Parties - Report the total payables in which the payer and payee are related parties as defined under U.S. GAAP.
- Other Non-Current Liabilities- Report any other amounts due to be paid to creditors after 12 months.
- Total Long-Term Liabilities - Total long-term liabilities is an automated calculation.
- Total Liabilities (current and long-term) - Total liabilities (Current and Long-Term) is an automated calculation.
- General Fund Balance - Report the amount of any general funds.
- Special Purpose Fund Balance - Report the amount of any special purpose funds.
- Endowment Fund Balance - Report the amount of any endowment funds.
- Other Fund Balances - Report the amount of any other funds.
- Total Fund Balances - Total fund balances is an automated calculation.
- Owner's Capital - Report owner's investment plus the net income earned by the organization minus the draws made by the owner.
- Retained Earnings - Report the accumulated undistributed earnings of an organization retained at the end of the accounting period for future needs.
- Total Other Equity - Total other equity is an automated calculation.
- Total Liabilities, Fund Balances, Equity - Total liabilities, fund balances, and equity is an automated calculation.
Schedule 19 - Statement of Revenues & Expenses
A Note: Schedule 19 requires agency-level information.
Schedule 19 requires agencies to report the components of their Total Revenues and Expenses. Agencies will be required to submit supporting documentation to verify the Home Care Cost Report submissions, including annual certified financial statements or other financial documentation that demonstrates reconciling items.
- Home Care Service Revenue
- Medicaid
- FFS - Report Medicaid Fee-for-Service revenue only. If your agency provides Medicaid FFS services, then there should be FFS revenue reported in row 002 on Schedule 19 and statistics reported on Schedule 5 in Columns 001-003.
- Managed Care - Report Medicaid Managed Care revenue only. Report Medicaid Managed Care revenue only. If your agency provides Medicaid MC services, then there should be MC revenue reported in row 003 on Schedule 19 and statistics reported on Schedule 5 in Columns 004-006.
- Medicare - Report Medicare revenue only.
- Private Pay - Report Private Pay revenue only.
- Commercial - Report Commercial revenue only.
- Other Government Programs - Report other local, state, or federal home care service revenue not already captured above, such as revenue from the Office of the Aging.
- Other - Report any home care service revenue that does not fall into one of the above categories.
Note: If your agency has Medicaid surplus billing, the portion of the revenue that is from Medicaid FFS only should be reported in row 002 "Medicaid Fee-for-Service" and the private pay revenue portion should be reported in row 005 "Private Pay."
- Medicaid
- Total Home Care Service Revenue - Total home care service revenue is an automated calculation that sums rows 001, 004, 005, 006, 007 and 008.
- Total Other Operating Revenue - Report the revenues from the organization's ongoing major or central operations related to LHCSA, CHHA, and FI operations only. If other operating revenue exceeds 10% of the total revenue, you are required to complete an additional schedule breaking out these revenues.
- Total Operating Revenue - Total operating revenue is an automated calculation.
- Non-Revenue Support Services - Report the operating expenses associated with non- revenue support services.
- Ancillary Service Revenue Centers - Report operating expenses associated with revenue that is derived from goods or services other than an organization's primary offering.
- Program Services Revenue Centers - Report operating expenses associated with revenue received by an organization while charging for the services for which it received tax-exemption.
- Total Operating Expenses - Total operating expenses is an automated calculation.
- Excess (Deficiency) of Operating Revenues Over Expenses - This is an automated calculation.
- Income from Investments - Report the total income from investments as defined under U.S. GAAP.
- Interest Income - Report revenue earned for the use of funds or an investor on their investment over a period of time.
- Gain on Sale of Fixed Assets - Report the amount by which the proceeds from the sale of the fixed asset (that had been used in the business) exceeded its carrying amount at the time it is sold.
- Other Non-Operating Revenue - Report revenue generated by activities outside of an organization's primary operations.
- Total Non-Operating Revenue - Total non-operating revenue is an automated calculation.
- Federal, State, and Local Taxes - Report the total amount of Federal, State, and Local Taxes paid.
- Other Non-Operating Expenses - Report expenses generated by activities outside of an organization's primary operations.
- Excess (Deficiency) of Non-Operating Revenues over Non-Operating Expenses - This is an automated calculation.
- Excess of Total Revenues over Total Expenses (Expenses over Revenues) Before Extraordinary Gain (Loss) - This is an automated calculation.
- Extraordinary Gain (Loss) - Report any gain/loss as result of an unforeseen and generally unforeseeable event.
- Excess of Total Revenues over Total Expenses (Expenses over Revenues) after Extraordinary Gain (Loss) - This is an automated calculation.
Appendix A - Universal Codes for Long-Term Care Services with Respective Modifiers
| HOME CARE BILLING CODES AND MODIFIERS | ||||
|---|---|---|---|---|
| Service Type | Unit of Measurement | Procedure Code | Procedure Code Description | Modifier |
| Personal Care Aide Leve I (Homemaker/Housekeeper) | ||||
| PCS Level I - 15 Minutes | Per 15 minutes | $5130 | Homemaker service, NOS; per 15 minutes | U1 |
| PCS Level I Two Client | Per 15 minutes | S5130 | Homemaker service, NOS; per 15 minutes | U2 |
| PCS Level I Multiple Client | Per 15 minutes | S5130 | Homemaker service, NOS; per 15 minutes | U3 |
| PCS Level I | Per 15 minutes | 55130 | Homemaker service, NOS; per 15 minutes | TV |
| Personal Care Aide Level II | ||||
| PCS Level II Basic-15 Minutes | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for aninpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment {code may not be used to identify services provided by home health aide or certified nurse assistant) | U1 |
| PCSLevel II BasicTwo Client | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for an inpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | U2 |
| PCS Level 11 Multiple Client | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for anInpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment {code may not be used to identify services provided by home health aide or certified nurse assistant) | U3 |
| PCS Level II Weekend/Holiday | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for an inpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment {code may not be used to identify services provided by home health aide or certified nurse assistant) | TV |
| PCS Level 11 Hard to Serve | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for aninpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | U4 |
| PCS Level II Two Client Hard to Serve | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for aninpatient or resident of a hospital, nursingfacility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | us |
| PCS Level II Live in | Per diem {13 hours) | T1020* | Personal care services, per diem, not for an inpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | NONE |
| PCS Level II Live in Two Client | Per diem (13 hours) | T1020 * | Personal care services, per diem, not for an inpatient or resident of a hospital, nursingfacility, JCF/MR or IMD, part of the individualized plan of treatment {code may not be used to identify services provided by home health aide or certified nurse assistant) | U2 |
| HOME CARE BILLING CODES AND MODIFIERS | ||||
| Service Type | Unit of Measurement | Procedure Code | Procedure Code Description | Modifier |
| Personal Care Aide Level II | ||||
| PCS Level II Live in Weekend/Holiday | Per diem (13 hours) | T1020 * | Personal care services, per diem, not for an inpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | TV |
| PCS Level II Live in Two Client Hard to Serve | Per diem (13 hours) | T1020* | Personal care services, per diem, not for an inpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant\ | U5 |
| Consumer Directed Personal Assistant | ||||
| CDPA Basic - 15 Minutes | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for aninpatient or resident of a hospital, nursingfacility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | U6 |
| CDPA Enhanced | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for aninpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | U8 |
| CDPA Two Consumer | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for aninpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | U7 |
| COPA Two Consumer Enhanced | Per 15 minutes | T1019 | Personal care services, per 15 minutes, not for aninpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | U9 |
| COPA Live in | Per diem (13 hours) | T1020 * | Personal care services, per diem, not for an inpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | U6 |
| CDPA Live in Enhanced | Per diem (13 hours) | T1020 * | Personal care services, per diem, not for an inpatient or resident of a hospital, nursingfacility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant! | U8 |
| COPALivein TwoConsumer | Per diem (13 hours) | T1020 * | Personal care services, per diem, not for an inpatient or resident of a hospital, nursing facility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | U7 |
| COPALive in Two Consumer Enhanced | Per diem (13 hours) | T1020 * | Personal care services, per diem, not for an inpatient or resident of a hospital, nursingfacility, ICF/MR or IMD, part of the individualized plan of treatment (code may not be used to identify services provided by home health aide or certified nurse assistant) | U9 |
| *T1020 Per diem rate code may not be used if a personal care aide or personal assistant is not able to meet the sleep requirements required in | ||||
| Home Health Aide | ||||
| HHA - 15 minutes | Per 15 minutes | S5125 | Attendant care services; per 15 minutes | NONE |
| HHA | Per hour | S9122 | Home health aide or certified nurse assistant, providing care in the home - Per hour | NONE |
| HHA Two Client | Per 15 minutes | S5125 | Attendant care services; per 15 minutes | U2 |
| HHA - Live in | Per diem (13 hours) | S5126 | Attendant care services; per diem | NONE |
| HHA Live in Two Client | Per diem (13 hours) | S5126 | Attendant care services; per diem | U2 |
| Advanced Home Health Aide | Per hour | S9122 | Home health aide or certified nurse assistant, providing care in the home - per hour | U1 |
| Nursing Services | ||||
| Nursing Assessment/Evaluation | Per visit | T1001 | Nursing Assessment/evaluation | NONE |
| UAS Assessment | Per visit | T2024 | T1001-Nursing Assessment/evaluation. T2024-Service Assessment/plan of care development. | NONE |
| UAS Reassessment | Per visit | T2024 | T1001-Nursing Assessment/evaluation. T2024-Service Assessment/plan of care development. | NONE |
| Nursing Care in Home (RN) | Per diem (13 hours) | T1030 | Nursing care, in the home, by registered nurse, per diem | NONE |
| RN | Per hour | 59123 | Nursing care, in the home; by registered nurse, per hour (use for general nursing care only, not to be used when CPT codes 99500- 99602 can be used) | NONE |
| RN - 15 minutes | Per 15 minutes | T1002 | RN services, up to 15 minutes | NONE |
| Nursing Care in Home (LPN) | Per diem (13 hours) | T1031 | Nursing care, in the home, by licensed practical nurse, per diem | NONE |
| LPN | Per hour | 59124 | NursingCare, in the home; by licensed practical nurse, per hour | NONE |
| LPN - 15 minutes | Per 15 minutes | T1003 | LPN/LVN services, up to 15 minutes | NONE . |
| Home Health Care Services | ||||
| Occupational Therapy | Per visit | S9129 | Occupational therapy, in the home, per diem | NONE |
| Physical Therapy | Per visit | S9131 | Physical therapy, in the home per diem | NONE |
| Speech Therapy | Per visit | S9128 | Speech therapy, In the home, per diem | NONE |
| Respiratory Therapy | Per 15 minutes | 60237 | Therapeutic procedures to increase strength or endurance of respiratory muscles, one-on-one, face-to-face, per 15 minutes (includesmonitoring) | NONE |
| Respiratory Therapy | Per 15 minutes | G0238 | Therapeutic procedures to improve respiratory function, other than described by 60237, one-on-one, face-to-face, per 15 minutes (includes monitoring) | NONE |
| Nutritional Counseling | Per visit | 59470 | Nutritional counseling, dietician visit | NONE |
| Medical Social Services | Per visit | S9127 | Social work visit, in the home, per diem | NONE |
| Sign Language/Oral interpreter | Per 15 minutes | T1013 | Sign language or oral interpretive services, per 15 minutes | NONE |
| Social and Environmental Supports -Home Modification | Per service | S5165 | Home modifications; per service | NONE |
| Social and Environmental Supports -Assessment | Per service | T1028 | Assessment of home, physical andfamily environment, to determine suitability to meet patients medical needs | NONE |
| Telehealth | ||||
| Installation | Per service | S9110 | Telemonitoring of patient in their home, including all necessary equipment; computer system, connections, and software; maintenance; patient education and support; per month | NONE |
| Monitoring | Monthly | S9110 | Telemonitoring of patient in their home, including all necessary equipment; computer system, connections, and software; maintenance; patient education and support; per month | U1 |
| Medication Dispensers | ||||
| Installation | One Time | T1505 | Electronic medication compliance management device, includes all components and accessories, not otherwise classified | NONE |
| Monitoring | Monthly | S5185 | Medication reminder service, nonface-to-face; per month | NONE |
Note: For modifiers that state "as defined by each state," please refer to the column labeled NYS Definition. Each program utilizes modifiers for their specific program. Modifiers may be utilized more than once and are unique based on individual program.
| Modifier Descriptions | |||
|---|---|---|---|
| Personal Care Aide Level I (Homemaker/Housekeeper) | |||
| Modifier | Modifier Description | NYS Definition | Notes |
| U1 | Medicaid level of care 1, as defined by each state | This rate code modifier will be used for the provision of personal care Level I for basic services. | |
| U2 | Medicaid level of care 2, as defined by each state | This rate code modifier will be used for the provision of personal care Level I services to one of two clients In the same household where both clients are receiving personal care services from the same aide. | |
| U3 | Medicaid level of care 3,as defined by each state | This rate code modifier will be used for the provision of personal care Level I services for each personal care recipient who resides with other personal care recipients In a designated geographic area, such as In the same apartment building. | |
| TV | Special payment rate, holidays/weekends | This rate code modifier will be used for the provision of personal care Level I services on weekends (defined as between Saturday 8 a.m. to Monday 8 a.m.) and designated holidays. | |
Note: For modifiers that state "as defined by each state," please refer to the column labeled NYS Definition. Each program utilizes modifiers for their specific program. Modifiers may be utilized more than once and are unique based on individual program.
| Modifier Descriptions | |||
|---|---|---|---|
| Personal Care Aide Level II | |||
| Modifier | Modifier Description | NYS Definition | Notes |
| U1 | Medicaid level of care 1, as defined by each state | This rate code modifier will be used for the provision of personal care Level II for basic services. | |
| U2 | Medicaid level of care 2, as defined by each state | This rate code modifier will be used for the provision of personal care Level II services to one of two clients in the same household where both clients are receiving personal care services from the same aide. | |
| U3 | Medicaid level of care 3,as defined by each state | This rate code modifier will be used for the provision of personal care Level II services for each personal care recipient who resides with other personal care recipients in a designated geographic area, such as in the same apartment building. | |
| U4 | Medicaid level of care 4, as defined by each state | This rate code modifier will be used for the provision of personal care Level II services for clients who have exceptional needs and/or are in exceptional circumstances, such as the following situations: (1) a client ls left alone in the community In a life-threatening situation, and services must be provided within four hours; (2) a client has severe mental or physical diagnosis or has several documented social and/or behavioral problems which make him or her extremely difficult to serve; or (3) a client resides in a problematic environment which may include housing or geography or be influenced by the behavior or problems of family members residing with the client. | |
| U5 | Medicaid level of care 5, as defined by each state | This rate code modifier will be used for the provision of personal care Level II careservices to one of two clients In the same household where both clients are receiving personal care services from the same aide and where at least one of the clients has exceptional needs and/or Is In exceptional circumstances, such as the following situations: (1) a client is leftalone in the community in a life-threatening situation, and services must be provided within four hours; (2) a client has severe mental or physical diagnosis or has several documented social and/or behavioral problems which make him or her extremely difficult to serve; or (3) a client resides In a problematic environment which may Include housing or geography or be Influenced by the behavior or problems of family members residingwiththe client. | |
| TV | Special payment rate, holidays/weekends | This rate code modifier will be used for the provision of personal care Level I or Level II services on weekends (defined as between Saturday 8 a.m. to Monday 8 a.m.) and designated holidays. | |
Note: For modifiers that state "as defined by each state," please refer to the column labeled NYS Definition. Each program utilizes modifiers for their specific program. Modifiers may be utilized more than once and are unique based on individual program.
| Modifier Descriptions | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Consumer Directed Personal Assistant | |||||||||
| Modifier | Modifier Description | NYS Definition | Notes | ||||||
| U6 | Medicaid level of care 6, as defined by each state | This rate code modifier will be used for the provision of consumer directed personal assistance services for basic services, | |||||||
| U7 | Medicaid level of care 7 , as defined by each state | This rate code modifier will be used for the provision of consumer directed personal assistance services to one of two consumers In the same household where both consumers are receiving personal assistance servicesfrom the same personal assistant. | |||||||
| U8 | Medicaid level of care B, as defined by each state | This rate code modifier will be used for the provision of consumer directed personal care services for consumers who have exceptional needs and/or are In exceptional circumstances, such as the following situations: (1) a consumer has a documented inability to hire or retain sufficient staff, where the consumer can document that attempts have been made and that the wage rate Is directly responsible for the inability to hire or retain staff and provided further that the consumer Is at a nursing home level of care and therefore the lack of sufficient staff will result In institutionalization; (2) a consumer has severe mental and/or physical diagnosis or hasseveral documented social and/or behavioral problems which make him or her extremely difficult to serve; or (3) a consumer resides In a problematic environment which may include housing or geography, or be influenced by the behavior or problems of family members residing with the consumer. | |||||||
| U9 | Medicaid level of care 9, as defined by each state | This rate code modifier will be used for the provision of consumer directed personal assistance services to one of two consumers in the same household where both consumers are receiving personal assistance servicesfrom the same personal assistant and where at least one of the consumers has exceptional needs and/orls ln exceptional circumstances, such as the following situations: (1) a consumer has a documented inability to hire or retain sufficient staff, where the consumer can document that attempts have been made and that the wage rate ls directly responsible for the inability to hire or retain staff and provided further that the consumer is at a nursing home level of care and therefore the lack of sufficient staff will result In Institutionalization; (2) a consumer has severe mental and/or physical diagnosis or has several documented social and/or behavioral problems which make him or her extremely difficult to serve; or (3) a consumer resides in a problematic environment which may include housing or geography, or be influenced by the behavior or problems of family members residing with the consumer. | |||||||
Note: For modifiers that state "as defined by each state," please refer to the column labeled NYS Definition. Each program utilizes modifiers for their specific program. Modifiers may be utilized more than once and are unique based on individual program.
| Modifier Descriptions | |||
|---|---|---|---|
| Telehealth | |||
| Modifier | Modifier Description | NYS Definition | Notes |
| U1 | Medicaid level of care 1, as defined by each state | This rate code modifier would be used for the monthly fee of telemonitoring of patient. | |
| Home Health Aide | |||
| Modifier | Modifier Description | NYS Definition | Notes |
| U1 | Medicaid level of care 1, as defined by each state | This rate code modifier would be used for the provision of Advanced Home Health Aide services on an hourly basis. | |
| U2 | Medicaid level of care 2, as defined by each state | This rate code modifier will be used for the provision of personal care Level I or Level II services to one of two clients In the same household where both clients are receiving personal care services from the same aide. | |
________________________
1. In calendar year 2020, DOH provided a standard rate add-on percentage of 4.56% to all Medicaid Fee-for-service agencies.1