Provider Bulletin 10-01 February 2010
Provider Bulletin
New York State EPIC - Prescription Protection for SeniorsP.O. BOX 15018
ALBANY, NY 12212-5018
1-800-634-1340
Bulletin No. 10-01
February 2010
Subject: New EPIC ID numbers & Cards
All EPIC members have been assigned new identification numbers in order to protect their privacy. Ask your EPIC customers to present their new cards when they drop off or pick up their prescriptions. Start submitting claims with the new ID numbers immediately. A picture of the new EPIC card is printed below.
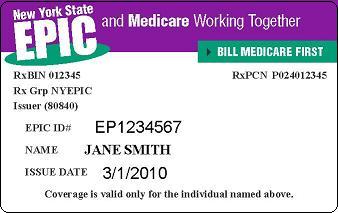
- The EPIC ID number format has changed. All ID numbers will have 9 characters and will begin with the letters EP and followed by 7 numbers (i.e. EP1234567).
- All EPIC members now have the same BIN (012345) and PCN (P024012345) numbers. Make sure that your customer profiles are updated and that you are only using these numbers.
- The card now shows an Issue Date instead of a Coverage Period.
- If seniors have any questions, refer them to the EPIC Helpline at 1-800-332-3742.
NOTE: The co-pay schedule has been removed from the back of the card; refer to the schedule on the EPIC web site.
In order to process EPIC claims correctly, the new ID number, BIN and PCN should be submitted by your pharmacy. Since most EPIC members are also enrolled in a Medicare Part D or other drug plan as their primary coverage, EPIC provides supplemental coverage for drug costs not paid by Part D or other prescription coverage. It is important that the primary coverage is being fully utilized so that EPIC is not paying costs that are the responsibility of the primary payer and seniors pay only the lowest possible co-pay. Thank you for your participation and support!
Subject: Mailing Drugs to Addresses Outside NYS
EPIC allows prescription drugs to be mailed to members’ temporary addresses that are located outside of New York State on a short-term basis or in emergency situations. Pharmacies should call the EPIC Provider Helpline when they are requested to mail or deliver drugs to an out-of-state location for more than six months or if they think a senior enrolled in EPIC is no longer a NYS resident. The EPIC Helpline staff will determine the senior’s residency status. Please be advised that only NYS residents are eligible for EPIC.
Subject: Claims Processing Reminders
Bill Part D or Other Primary Payer First
Many EPIC members changed their Medicare Part D plans as of January 1 due to plan formulary and benefit changes. Additionally, EPIC may have auto-enrolled certain members in a new plan due to premium increases. In some cases, the member may not have received their new Part D plan ID card in January, and might not have notified you of the change.
When billing Part D for an EPIC member, if the claim is denied for “coverage terminated” or “invalid cardholder ID”, before billing EPIC as primary with other Coverage Code (OCC) 3, please submit a Medicare eligibility transaction (E1) to obtain up-to-date information regarding the member’s enrollment in a Part D plan. This information also can be obtained by calling Medicare at 1-866-835-7595. Contact your software vendor or corporate office for technical assistance with the E1 transaction.
Adhere to primary Plan Quantity Limits
Claims denied by the Part D or other primary plan with reject code 76 (plan limitations exceeded) should be corrected to adhere to the quantity limits of the primary payer before being submitted to EPIC as secondary payer.
Claims with OCC 1 or 7 Denied if EPIC Records show Active Part D Coverage
If your records show the member has no other coverage, or if the member insists they do not have Part D coverage, before billing EPIC as primary with OCC 1 or 7, submit a Medicare eligibility transaction (E1) as noted above.
If the E1 transaction or Medicare helpline confirms there is currently no other coverage for the member, call the EPIC Provider Helpline at 1-800-634-1340 for an override of the EPIC denial.