Overview of Final Health Home Application to Serve Children and Other Design Updates
- Overview also available in Portable Document Format (PDF)
November 5, 2014
Tailoring Health Homes to Serve Children ˜
Collaborative Effort of State Agency Partners and Stakeholders
- State Agency Partners
- Office of Mental Health (OMH)
- Office of Alcoholism and Substance Abuse Services (OASAS)
- Office of Children and Family Services (OCFS)
- Department of Health (DOH) (including Office of Health Insurance Programs, Center for Health–Division of Family Health, AIDS Institute)
- New York State Education Department
- Stakeholders
- Health Homes, Managed Care Plans and Care Managers
- Associations
- Advocates
- Local Government Partners (LDSS, LGU, SPOA, NYCDOHMH)
Draft Application, Comments and Letters of Interest
- State released Draft Application on June 30, 2014 for review and comment by Stakeholders
- Comments and Letters of Interest due July 30, 2014
- 34 Letters of Interests Submitted
- 21 Currently Designated Health Home (some of which indicated the potential formation of partnerships among Designated Health Homes)
- 12 New Organizations
- Proposed coverage areas span every county of the State
- Letters of Interest have been posted to DOH Health Home Website
- More than 40 Health Homes, Medicaid providers, children´s advocates and other stakeholders submitted comments
- Stakeholder comments were helpful, thoughtful and generally supportive of the overall concept and design of the Health Home model for children
- Comments covered a wide spectrum of topics, including:
- The Application process and timelines for Health Home designation and enrollment
- Operationalizing the design of the Health Home model for children
- Many of these comments/topics will be addressed as the details of the design of the Health Home model for children evolve over the next several months
- Today´s discussion will include status updates on many of these topics
- State will continue to seek stakeholder input and provide status updates as elements of design evolve
Schedule for Enrolling Children In Health Homes
- In response to comments received from Stakeholders to provide more time in the anticipated schedule, the State extended the schedule for enrollment from January 2015 to July 2015
- Based upon further analysis of the work required to implement elements of the design of the Health Home model for children the State has extend the begin enrollment date to October 2015
- As discussed in more detail throughout today´s Webinar, the additional three months will provide more time:
- For System Readiness
- Develop elements of the Medicaid Analytics Performance Portal relevant to Health Homes and children
- Modify and test CANS–NY Assessment tool
- To develop an approach to phase–in enrollment of children which will also phase–in the costs of Health Home rates which can support low case load ratios
- Investments would be approved as part of the Global Spending Cap in the 2015–16 Executive Budget
- To build network capacity, including care managers
- To resolve questions around the Standards and procedures for delivering Conflict Free Home and Community Based Services (HCBS) that may impact Health Home care managers (CFCM)
- Provide more time for identifying points and processes for connecting Health Home with systems of care (Early Intervention, Juvenile Justice, School Supportive Health, LGUs)
- For providers to form networks and partnerships
- For prospective lead Health Homes to submit Applications (note Applications required to be submitted electronically and due March 2, 2015)
- For the review and approval of Applications
- For Health Homes to enter into DEAAs with DOH and to enter into subcontractor agreements with care managers and network providers
- To develop and provide informational and training Webinars to Health Homes, care managers, and other systems of care
- For System Readiness
| Anticipated Schedule of Activities for Expanding Health Homes to Better Serve Children | Due Date |
|---|---|
| Draft Health Home Application to Serve Children Released | June 30, 2014 – Completed |
| Due Date to Submit Comments on Draft Health Home Application to Serve Children | July 30, 2014 – Completed |
| Due Date to Submit Letter of Interest | July 30, 2014 – Completed |
| Final Health Home Application to Serve Children Released | November 3, 2014 – Completed |
| Due Date to Submit Health Home Application to Serve Children | March 2, 2015 |
| Review and Approval of Health Home Applications to Serve Children by the State | March 2, 2015 to June 15, 2015 |
| HH and Network Partner Readiness Activities | June 15, 2015 to September 30, 2015 |
| State Webinars, Training and Other Readiness Activities | Through September 30, 2015 |
| Begin Phasing in the Enrollment of Children in Health Homes | October 2015 |
| Children´s Behavioral Health Services and other Children´s Populations Transition to Managed Care | January 2016 |
Definition of a Child
- Stakeholders requested the State define child
- For purposes of the Application and in the context of the administration of Health Homes (e.g., children´s rates, Health Homes primarily serving children) a child is defined as an individual under the age of 21
- NOTE: Age is NOT an eligibility requirement for Health Homes (e.g., individuals that turn 21 and meet the chronic condition based criteria and are appropriate for Health Homes care management remain eligible for Health Homes)
Use of the Child and Adolescent Needs and Strengths Assessment of New York (CANS–NY)
- Stakeholders generally supported the use of the CANS–NY Assessment tool in the Health Home model
- CANS–NY is anticipated to be used:
- Determine need for Home Community Based Services
- Determine acuity for Health Home Rates
- Assist in determining if children meet HH eligibility functional criteria
- To address concerns the current CANS–NY tool may not adequately capture the various children´s populations that would be eligible for Health Home and HCBS services, including infants and toddlers and medically fragile children, the State is working to modify the CANS–NY to:
- Include modules specific to the 0–5 and 6–21 age groups
- Include a module related to sexuality and sexual orientation
- The State is working to modify the CANS–NY tool to:
- Include modules relating to Activities of Daily Living and Instruction on Activities of Daily Living to be in compliance with the Balancing Incentive Program;
- Make enhancements to better assess medically fragile children
- Modify the tool to determine functional limitations as provided by SED and Trauma HH eligibility criteria
- Develop an algorithm that will determine acuity tier (i.e., High, Medium, Low) for children´s Health Home rates
- The State anticipates it will begin testing the modifications to the CANS–NY tool mid– December
- No cost training is available on–line, State exploring possibility of providing more in– depth, in person training sessions
- CANS–NY data will eventually be warehoused on the Uniform Assessment System on DOH´s Health Commerce System and linked to the Medicaid Analytics Performance Portal
Expanding Health Home Eligibility to Better Serve Children – SED
- Stakeholders requested the State clarify the definition of Serious Emotional Disturbance (SED)
- Goal in developing the SED definition for Health Home is to be consistent with the OMH SED definition, which relies upon the Diagnostic and Statistical Manual of Mental Health Disorders (DSM), and the chronic condition eligibility requirements of the Health Home Program.
- Serious Emotional Disturbance (SED): A child or adolescent (under the age of 21) that has a designated mental illness diagnosis as defined by the most recent version of the DSM and, as grouped by the 3MTM Clinical Risk Groups (CRGs), is a chronic condition AND has experienced functional limitations due to emotional disturbance over the past 12 months (from the date of assessment) on a continuous or intermittent basis.
- The State is finalizing work to cross–reference the most recent DSM list (DSM–5) of designated mental health diagnoses to the OMH SED definition and then to the list of chronic conditions as determined by the 3MTM Clinical Risk Groups (CRGs).
- It is expected that that SED definition for Health Home will include diagnoses from the following DSM–5 categories:
- Bi–Polar and Related Disorders; Depressive Disorders; Feeding and Eating Disorders; Schizophrenia Spectrum and Other Psychotic Disorders; Obsessive–Compulsive Related Disorder; Disruptive, Impulse Control and Conduct Disorders; and Personality Disorders
- It is expected that that SED definition for Health Home will include diagnoses from the following DSM–5 categories:
- To meet the SED criteria functional limitations must exist in the following areas (unchanged from Draft Application)
- Ability to care for self (e.g. personal hygiene; obtaining and eating food; dressing; avoiding injuries); or
- Family life (e.g. capacity to live in a family or family like environment; relationships with parents or substitute parents, siblings and other relatives; behavior in family setting); or
- Social relationships (e.g. establishing and maintaining friendships; interpersonal interactions with peers, neighbors and other adults; social skills; compliance with social norms; play and appropriate use of leisure time); or
- Self–direction/self–control (e.g. ability to sustain focused attention for a long enough period of time to permit completion of age–appropriate tasks; behavioral self–control; appropriate judgment and value systems; decision–making ability); or
- Ability to learn (e.g. school achievement and attendance; receptive and expressive language; relationships with teachers; behavior in school).
- Stakeholder concern: Verifying Criteria
- In addition to clinical assessments, the CANS–NY is being modified to help verify functional limitations
Expanding Health Home Eligibility to Better Serve Children – Trauma
- Stakeholder comments endorsed expanding Health Home eligibility criteria to include Trauma
- Definition of Trauma and at Risk for Another Condition remains unchanged from the definition included in the Draft Application
- Trauma is defined as exposure to a single severely distressing event, or multiple or chronic or prolonged traumatic events as a child or adolescent, which is often invasive and interpersonal in nature. Trauma includes complex trauma exposure which involves the simultaneous or sequential occurrence of child maltreatment, including psychological maltreatment, neglect, exposure to violence, and physical and sexual abuse.
- A child or adolescent who has experienced trauma would be defined to be at risk for another chronic condition if they have one or more functional limitations that interfere with their ability to function in family, school, or community activities, or they have been placed outside the home.
- Functional limitations are defined as difficulties that substantially interfere with or limit the child in achieving or maintaining developmentally appropriate social, behavioral, cognitive, communicative, or adaptive skills, or for a child who experienced trauma due to child maltreatment, a functional limitation is defined as a serious disruption in family relationships necessary for normal childhood growth and development.
- Stakeholder concern: Verifying Criteria
- In addition to clinical assessments, the CANS–NY is being modified to help verify functional limitations
Chronic Conditions for Health Home Eligibility
- Members that have two chronic conditions are eligible for Health Home
- The State has issued additional information regarding which conditions are chronic as grouped by the chronic the 3M™ Clinical Risk Groups (CRGs)
Expanding Health Home Eligibility to Better Serve Children – Overweight
- The Final Application includes a proposal to amend the Body Mass Index (BMI) > 25 to make the definition comparable to the CDC´s definition for overweight and to provide a comparable overweight measure for children as follows:
- Change "BMI > 25" to "BMI at or above 25 for Adults"
- Add "At or above the 85th percentile for children of the same sex and age"
- Children and adults that meet this revised overweight definition AND have one other chronic condition would be eligible for Health Home
Appropriateness Criteria for Health Homes
- In addition to meeting the chronic condition criteria for Health Home (i.e., SED, Trauma and At Risk for Another Condition, HIV, at least two chronic conditions) members must be "appropriate" for Health Home, i.e., they need the more intensive level of care management provided by Health Homes
- In response to stakeholder comments the appropriateness criteria for Health Homes was amended (new changes are in green, changes included in Draft Application are in bold) as follows:
- Appropriateness Criteria: Individuals meeting the Health Home eligibility criteria must be appropriate for Health Home care management. Assessing whether an individual is appropriate for Health Homes includes determining if the person is:
- At risk for an adverse event (e.g., death, disability, inpatient or nursing home admission, mandated preventive services, or out of home placement)
- Has inadequate social/family/housing support, or serious disruptions in family relationships;
- Has inadequate connectivity with healthcare system;
- Does not adhere to treatments or has difficulty managing medications;
- Has recently been released from incarceration, placement, detention, or psychiatric hospitalization;
- Has deficits in activities of daily living, learning or cognition issues, or
- Is concurrently eligible or enrolled, along with either their child or caregiver, in a Health Home.
Status of CMS Discussions
- State Plan Amendment (SPA) required to amend the Health Home eligibility criteria to:
- Include trauma and at risk for another condition
- Amend the BMI at or above 25 and to include comparable definition for children
- Use the CANS–NY to determine acuity
- Establish legacy rates for TCM and Waiver Programs
- State had initial discussions and submitted informal, draft SPA to CMS
- Discussion was positive and supportive
- Next Steps:
- Respond to CMS questions (mostly technical)
- Discuss HH model for children with Substance Abuse and Mental Health Services Administration (SAMHSA) – Meeting scheduled for November 20, 2014
- Submit formal SPA for approval (per "sequencing" rules of CMS after the approval of the HH Resources ($190.6 million) Waiver SPA)
High Fidelity Wraparound Care Management
- Stakeholders generally endorsed employing the High Fidelity Wraparound model
- In early 2015, the State will work to explore how the High Fidelity Wraparound model can be integrated and phased into the Health Home model at a later date
- Considerations for integrating HFW in HH model for children include:
- Developing eligibility criteria for small subset of children,
- Operational and cost considerations for developing program and providing statewide access to a small group of children,
- Evaluation and quality monitoring (i.e., maintaining fidelity to the model)
Health Home Per Member Per Month Rates for Children
- The State is continuing to develop Health Home care management rates for children – Stakeholder comments focused on rate adequacy and low case load ratios
- The framework for the development of Per Member Per Month rates includes:
- Tiered rate structure (High, Medium, Low) based on acuity of child and the development of an algorithm using the modified CANS–NY (modifications to CANS–NY now under development)
- Low care manger to child ratios that are preliminarily anticipated to range from 1:12 to 1:40 and for HFW (1:10)
- Lower case loads tied to higher acuity and higher rates; higher case loads tied to lower acuity and lower rates
- Flat rate for "outreach" activities
- Phasing–in enrollment will help ensure the costs of Health Home rates predicated on low case load ratios can be accommodated in the Global Spending Cap
- Tiered rate structure would be in effect October 2015
- Tiered rate structure would be the mandated government rates in effect in the first two years of Managed Care (2016 and 2017)
- Legacy care management payments will be developed for children´s legacy providers (OMH TCM and B2H, CAH I/II, OMH Waiver Programs) and will remain in effect for two years
- Health Homes and managed care plans have the option of negotiating alternative payment arrangements if the Health Home, Plan and the State agree to such an alternative
Preliminary Estimates of HH Eligible and Health Home Rates for Children
- The State is working to make preliminary Health Home Rates, estimated number of children eligible for Health Home (including regional data) available in early January
- Next steps:
- Finalize SED definition and mapping to CRGs to identify potential Health Home eligible population
- Finalize modifications to CANS–NY Assessment Tool and development acuity algorithm (High, Medium and Low)
- Incorporate case load assumptions (1:12 to 1:40) to the data
Phasing in the Enrollment of Children into Health Homes
- Some stakeholders suggested the State consider phasing in the enrollment of children into Health Homes
- The State will work in collaboration with stakeholders on a Plan to phase–in enrollment
- Considerations for developing a phase–in plan will include:
- the "readiness" of designated Health Homes to begin serving children,
- identifying regions or populations of children under which to implement a phase–in approach
- accommodating the costs in the global spending cap
- It is anticipated the phase–in plan would continue to reflect the conversion of:
- Children enrolled in OMH´s TCM Program to Health Home on October 1, 2015
- Children enrolled in the OCFS Bridges to Health Waivers, the OMH SED Children´s Waiver, and the DOH Care at Home I/II Waiver will receive their care coordination through Health Home care management beginning on January 1, 2016.
Children with Developmental Disabilities
- Children receiving services from the Office for People with Developmental Disabilities (OPWDD), including children in the Care at Home III, IV, and VI Waivers will not be prioritized at this time for enrollment into Health Home.
- However, DOH is continuing to work with OPWDD to discuss approaches for beginning to enroll children in Health Homes that have a developmental delay diagnosis and one other Health Home chronic condition or a single qualifying Health Home chronic condition and require the level of care management services provided by Health Home and who are not currently receiving OPWDD services that require OPWDD service coordination
Assignment Lists and Referrals
- The State is considering procedures for identifying children and making initial assignments to Health Homes.
- Methods for identifying potentially eligible children include using Medicaid claims data create assignment lists and referrals from:
- Various entities [e.g., Early Intervention, primary care providers, Plans, LDSS, SPOA and Pre–Admission Certification Committee (PACC)].
- Systems of care (e.g., child welfare, foster care, educational system, Early Intervention, juvenile justice) which connect to children (often on a daily basis)
- To facilitate referrals, the design of Medicaid Analytics Performance Portal (MAPP) will include an internet portal that authorized users in these, and other systems can access to make referrals to a Health Home.
- As has been anticipated in the Health Home model, the Plans will make assignments to Health Homes. Children not enrolled in a Plan will be assigned to a downstream care management agency by the Health Home. Each type of assignment will take into account existing relationships with health care providers or systems, geography and qualifying condition(s).
Standards for Care Managers and Engagement
- Stakeholders generally supported establishing qualifications for care managers, while noting the need to preserve flexibility to make operational decisions that best reflect the mix of children served
- Given the desired approach to keep case load ratios as low as practicable, particularly for those children with more intensive needs (acuity level of high or that may be in HFW when implemented) and the level of experience required to meet the care management needs of this group, the State is requiring that care managers that serve children with acuity level of "high" as determined by the CANS–NY or in HFW when implemented have:
- A Bachelor of Arts or Science with two years of relevant experience, or
- A Licensed Registered Nurse with two years of relevant experience, or
- A Masters with one year of relevant experience.
- Health Home Care Managers providing services to:
- High acuity children (as determined by the CANS–NY as modified) would be required to keep their caseload mix predominantly to children of the High acuity level (and HFW when implemented)
- Medium and high acuity children (as determined by the CANS–NY tool as modified) will be required to provide two Health Home services per month, one of which must be a face–to–face encounter with the child.
- Standards for children enrolled in the Early Intervention Program (EIP) and receiving Health Home services through a provider approved under EIP, the following minimum qualifications for EIP service coordinators, as set forth in Section 69–4.4 of 10 NYCRR will apply
- A minimum of one of the following educational or service coordination experience credentials:
- two years of experience in service coordination activities as delineated in this Subpart (voluntary or part–time experience which can be verified will be accepted on a pro rata basis); or
- one year of service coordination experience and an additional year of experience in a service setting with infants and toddlers with developmental delays or disabilities; or
- one year of service coordination experience and an Associates degree in a health or human service field; or
- a Bachelors degree in a health or human service field.
- Demonstrated knowledge and understanding in the following areas:
- infants and toddlers who may be eligible for early intervention services;
- State and federal laws and regulations pertaining to the Early Intervention Program;
- principles of family centered services;
- the nature and scope of services available under the Early Intervention Program and the system of payments for services in the State; and
- other pertinent information.
- A minimum of one of the following educational or service coordination experience credentials:
Potential Impact of Federal Rules for the Provision of HCBS on Health Home Care Managers and Standard Requirements
- As New York reviews the proposed 1115 amendment with CMS and negotiates terms and conditions, it is anticipated that some of the HCBS requirements will impact the responsibilities of Health Home Care Coordinators and may require a change in the standards described above.
- HCBS requirements that may impact Health Home care managers could include:
- Training requirements for care managers,
- Specific aspects of patient centered planning (e.g., who must sign the service plan) and
- Once HCBS and eligible and receiving services, person must receive at least one HCBS service per month
- Health Homes will be informed of these requirements as soon as they are determined and will be provided necessary training and information related to HCBS services and such requirements.
- HCBS requirements that may impact Health Home care managers could include:
Background Screening Requirements
- The State is interested in exploring the implementation of consistent practices for screening care coordinators who will work with children in Health Homes:
- Criminal History Records Checks against the NYS Division of Criminal Justice Services (DCJS)database, the NYS DCJS Sex Offender Registry, and the Statewide Central Register of Child Abuse and Maltreatment (SCR)
- Screening through the Medicaid Exclusion and Termination list
- The State will continue to update and consult Health Homes, providers and stakeholders as these requirements are developed over the next several months
Stakeholder Comment:
Children Currently Enrolled in Health Homes that Do Not Become Designated to Serve Children
- Health Home care management is an optional benefit, individuals have the right to choose a Health Home. There are more than 1,000 children currently enrolled across all Health Homes
- The designation of Children´s Health Homes is not intended to disrupt the continuity or provision of Health Home services now being provided to children, but is intended to ensure children receive services that meet their needs
- Health Homes that currently serve children that do not become a designated Health Home serving children will be required to:
- Disclose this information to the child/caregiver and discuss with the child/caregiver if:
- There is agreement that the Health Home is meeting the care management needs of the child and can continue to do so, or
- If it is in the best interests of the child to be reassigned to a Health Home designated to serve children.
- Disclose this information to the child/caregiver and discuss with the child/caregiver if:
- Effective October 1, 2015, Health Homes that do not become designated to serve children may not enroll new members that are children (i.e., under the age of 21), unless there are documented extenuating circumstances (e.g. patient choice/preference, service needs of patient, patient circumstances, caregiver enrolled) indicating the provision of care management services by the non–child designated Health Home is in the child´s best interest.
Stakeholder Comment:
Concurrent Enrollment of Child and Caregiver in Health Homes
- In instances where both the caregiver and the child each meet the Health Home eligibility requirements, it is expected that Health Homes that serve both children and adults will offer Health Home care management to both the child and the caregiver and the care management will be appropriately coordinated.
- Health Homes designated to primarily serve children and thus do not have the care management expertise and a network sufficient to meet the needs of the care giver (i.e., the adult) must disclose this to the caregiver and the child and offer the child and caregiver the option of enrolling in another Health Home that can serve them both.
- Regardless of whether the child or caregiver are ultimately enrolled in the same or different Health Home, the Health Home or Health Homes must support the presentation of options and document the family´s choice and decision making process, and must collaborate to coordinate care management for the family and caregiver as appropriate.
Discharge from Health Home
- Children that no longer meet the chronic condition based criteria for enrollment, including whether they meet the appropriateness criteria and other functional criteria (i.e., as defined for Trauma and SED), and thus do not need the intensive level of care management provided by Health Homes, should be discharged from Health Home and transitioned to another level of appropriate care (e.g., patient centered medical home, HCBS care management).
- Stakeholder Comment: Children discharged from Foster Care should remain in Health Home for a period of time
- Eligibility for Health Home is determined by chronic condition criteria and appropriateness criteria
- Foster Care placement in itself does not make a child eligible for Health Home (it is not a chronic condition that makes an individual eligible for Health Home)
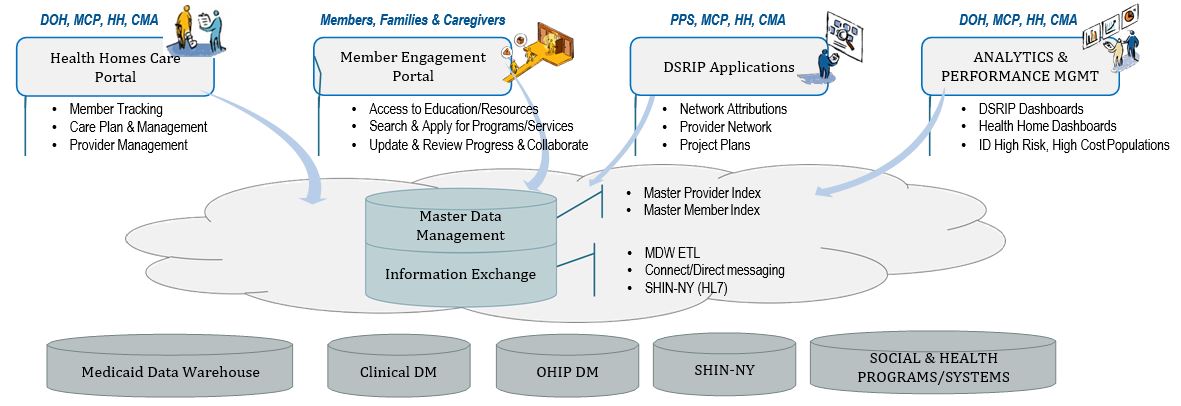
MAPP
- MAPP: Medicaid Analytics Performance Portal (MAPP) – Stakeholder Comments about how MAPP will impact Health Homes serving children
- MAPP supports both Health Homes and DSRIP per management technology needs
- MAPP Technology will be performance management system that will provide tools to the Health Home network to support providing care management for the Health Home population
- MAPP Technology will:
- Serve as retail front–end to the Medicaid Data Warehouse for PPS / Health Home community
- Robust dashboard capabilities provided by Salient
- Health Homes Business and Care Management Functionality
- Data management and analytics to drive performance and manage to quality outcomes
Medicaid Analytics Performance Portal Implemented Over 5 Phases through 2016 Long Term Vision
Phase 1: MAPP Member Tracking Go Live Date 2/27/15
- MEMBER TRACKING
- Member tracking and increased visibility (HHs, Plans and Care Managers)
- Assignments
- Referrals
- Transfer of individuals to between Health Homes
- Prioritization and workflow to support specialty programs
- Billing Support (develop Payment Assessment to evaluate member payment level, includes assessment, underlying logic and associated results)
- Capture Consent Management
- Self–administration of Health Homes and Managed Care Plans (users, provider network)
- INTEROPERABILITY (File Exchange)
- Maintain continuity of current file exchanges
- Long term planning for interoperability
- ANALYTICS & PERFORMANCE
- ID high risk, high cost populations for program(s) enrollment
- Evaluate program, member, provider, and community outcomes to goal
- Integrate Health home Dashboards in Portal
Phase 1B: Modifications to MAPP Member Tracking for Enrollment of Children, Summer of 2015
- MEMBER TRACKING
- Update flags and workflow for children (Identification, Assignment, Referral, Transfer, Prioritization)
- Capture / Manage Child Consent Management (alerts if no parental consent)
- Update Health Homes, Care Management Agency records (Provider Management) with child related specializations
- Develop Payment Assessment to evaluate member payment level (includes assessment, underlying logic and associated results)
- CARE COORDINATION
- Internet Portal for External Referrals
- CANS–NY Assessments for Children
- INTEROPERABILITY (File Exchange)
- Update file specifications to include child–related fields
- Begin integration with Early Intervention system
- ANALYTICS & PERFORMANCE
- Quality Measures
Measuring Quality and Performance
- The State is continuing to recommend the use of quality measures that do not initially require additional data to be collected and submitted by Health Homes and Care Managers
- The Final Application recommends:
- The addition of the following QARR Measures
- Use of Multiple Concurrent Antipsychotics in Children and Adolescents
- Use of First–Line Psychosocial Care for Children and Adolescents on Antipsychotics
- The replacement of the PSYCKES measure for Cardiometabolic Monitoring for Youth Using Atypical Antipsychotics with the QARR measure for Metabolic Monitoring for Children and Adolescents on Antipsychotics
- The integration of the CANS–NY to the UAS–NY and MAPP to facilitate the use of the CANS– NY data to evaluate outcomes of children enrolled in Health Home
- The addition of the following QARR Measures
- To facilitate ability to manage performance and monitor quality, the quality measures will be incorporated into MAPP
- The development of MAPP will help support the addition of new quality measures in the future
Integrating Early Intervention and Health Home Program
- Stakeholders generally support the State´s approach to leveraging the expertise of EI service coordinators and HH care managers by having the EI initial service coordinator continue to facilitate initial enrollment and the Health Home care manager provide ongoing care management, including the integration of EI services in the child´s comprehensive care plan
- State has discussed approach with Early Intervention Council and the New York State Association of County Health Officials
- Next Steps:
- Continue to work with stakeholders to discuss how to "operationalize" approach, including:
- Establishing clear, documented guidance regarding the roles of the EI initial service coordinator and the Health Home care manager, including ensuring EI program requirements are met
- Training on the roles and responsibilities of EI service coordinator and HH Care Management, including procedures for transitioning from initial EI coordination to HH Care Management, EI program requirements, HH program requirements
- Preliminary discussions with CMS and State Plan Amendment submission and approval
- Continue to work with stakeholders to discuss how to "operationalize" approach, including:
Establishing Linkages with Children´s Systems of Care
- State will continue to work with children´s systems of care to identify natural points in these systems where children can be identified and referred to Health Home (i.e., MAPP Internet Referral Portal) and to provide Health Home "101"and Eligibility Training
- Education: State working with State Education Department to schedule discussion with Commissioners Advisory Panel for Special Education
- Juvenile Justice: Initial discussions will cover juvenile probation, OCFS licensed detention programs, foster care agencies serving JDs, and OCFS facilities
- Local Government Units and Local Department of Social Services: Follow up to October 16, 2014 meetings
Consent for Minors and Health Home Health Information Technology (HIT) Requirements
- Children´s consent rules are complex and multi–faceted
- The State Agency Partners, including representatives from their legal departments, have been working to develop an approach to obtaining consent for the enrollment of children in Health Homes and the appropriate sharing of protected health information of children enrolled in Health Homes with parents and network providers
- The goal of the approach for children´s consent will recognize both the rights of parents/guardians to consent to the treatment of their children (re: parental/guardian consent to provide care management services to their child) and the rights of minors to consent to certain services (e.g., family planning, HIV/AIDS, mental health services, substance abuse services), and in those circumstances, to withhold such treatment/services from their parents
- The State plans to share draft children´s consent forms with Stakeholders for review and comment in early December
- The HIT technology requirements of the Health Home program for Health Homes serving children also recognize the inability to segment electronic health care information may require health information for minors be shared by non–electronic means
State Webinars, Training and Other Readiness Activities
| Health Home Operations and Other Training and Informational Webinars | Calendar Quarter |
|---|---|
| Overview Health Home Application to Serve Children and Other Design Updates | November 5, 2014 |
| Data Exchange Agreements and Subcontractor Packages Informational/Training | Q4, 2014 – Q1, 2015 |
| Consent Policy (Review of Draft Consent Form with Stakeholders, Informational Webinars) | Q4, 2014 – Q1, 2015 |
| Health Home Rates, Projected Estimates of HH Eligible Children, Updates on Eligibility Criteria (SED) , Begin Developing Plan for Prioritizing Enrollment | Q1, 2015 |
| HH Requirements, Health Information Technology (HIT), Electronic Health Records (EHR) – Informational Webinar | Q1 – Q2, 2015 |
| Managed Care Plan Administrative Services Agreement | Q2 – Q3, 2015 |
| Transition of OMH TCM Providers to Health Home | Q2 – Q3, 2015 |
| MAPP: HH Tracking, Billing, Health Home Outreach, Engagement, Assignment Lists, Referrals, Internet Referral Portal, HH–CMART, Dashboards | Q1 – Q3, 2015 |
| CANS–NY Online and Other Training Sessions | Beginning Q2, 2015 |
| Conflict Free Case Management (CFCM) | Q1 – Q2, 2015 |
| Health Home Training and Informational Webinars | Calendar Quarter |
| Early Intervention Program | Q1 – Q3, 2015 |
| Committee Special Education/SSHSP | Q1 – Q3, 2015 |
| Pediatricians "HH 101 / Eligibility" | Q2, 2015 |
| Foster Care System and Health Home | Q2, 2015 |
| Health Home Care Management Training for Voluntary Foster Care Agencies | Q2 – Q3, 2015 |
| Juvenile Justice Systems and Health Home | Q2 – Q3, 2015 |
| OASAS Program Information | Q2 – Q3, 2015 |
| OMH Program Information | Q2 – Q3, 2015 |
| Transition of Waivers (B2H, CAH I/II, OMH HCBS) | Q3 – Q4, 2015 |
| HCBS Services | Q3 – Q4, 2015 |
| Other Suggested Training Sessions? | |
Health Home Development Resources
- SPA submitted to CMS on September 30, 2014
- Consistent with Waiver Amendment, $190.6 million of Health Home Development Funds would support:
- Member Engagement and Health Home Promotion
- Workforce Training and Retraining
- HIT Implementation – Clinical Connectivity
- Joint Governance Technical Assistance and Implementation Funds
- Health Home Development Funds will be distributed through a rate add on; methodology and guidance to be developed.
Electronic Submission of Health Home Application to Serve Children
- Health Home Applications to Serve Children due March 2, 2015
- The Application consists of two Parts: Part I and Part II
- Part I includes Background and Policy Information
- Part II is the Health Home Application to Serve Children and must be submitted Electronically – see webpage and application for instructions
Resources and Questions and Answers
- Please send any questions, comments or feedback on Health Homes Serving Children to: hhsc@health.ny.gov
- Stay current by visiting our website.
- Open up today´s Webinar to Questions and Answers