June 2008
Volume 24, Number 7
New York State
Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State Department of Health
Deborah Bachrach, Deputy Commissioner
Office of Health Insurance Programs
News for All Providers
Omni 3750 Medicaid Terminal Continues Warranty
Five-year warranty purchased with most Omni 3750 Medicaid terminals remains in effect.
National Provider Identifier Implementation September 2008
Continue to supply proprietary information during interim.
Important National Provider Identifier Information for Hospitals, Clinics, etc
NPI for attending providers must be submitted in place of the NYS license numbers.
Policy and Billing Guidance
Attention Pharmacy Providers: Are you using the correct National Drug Code (NDC)?
When validating a prior authorization you must use correct NDC.
Claims Will Require Present on Admission (POA) Indicator
Beginning July 17, 2008 reporting of Present on Admission (POA) indicators will be mandatory on all claims.
Unclassified Drug Code Now Available for Billing
Changes are coming effective July 1, 2008!
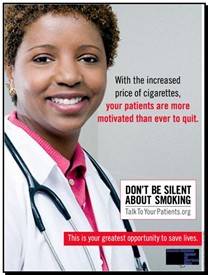
Don't Be Silent About Smoking
Talk to your patients about the dangers of smoking.
Reminder: Medicaid Enrollees Cannot be Billed
Medicaid enrollees, including those enrolled in Medicaid managed care plans, cannot be billed for services
New York City Ambulette and Livery Providers: Car Seat Policy Clarification
Vehicles licensed by the New York City Taxi and Limousine Commission (TLC) are exempt from car seat (and seat belt) regulations.
Supervising or Collaborating Physician(s) Must Be Identified
Important information for Registered Physician Assistants and Nurse Practitioners.
Dental Sealants To Require Prior Approval
Effective August 1, 2008 all dental sealants will require prior approval.
Dispensing Validation System Soon Available for Full Dentures and Dental Sealants
Effective August 1, 2008, prior authorization for full dentures and all dental sealants will be available electronically through the DVS system.
Policy on "Interrupted Treatment" for Dental Procedures
Read this article to learn about new policy on interrupted treatment for dental procedures.
National Drug Code Required on Claims for Physician Administered Drugs
A notice to Physicians, Nurse Practitioners, Licensed Midwives and Ordered Ambulatory Providers.
Medicaid Now Reimbursing for Viral Tropism Laboratory Test
The Medicaid program announces reimbursement for viral tropism testing.
Computer Sciences Corporation Offers Seminars - Sign Up Today!
Whether you are new to billing or need a refresher course, Computer Sciences Corporation offers training!
General Information
Information for all Providers...........

ePACES is a free internet-based program that allows NYS Medicaid providers to submit claims, eligibility requests (including service authorizations), claim status requests: electronic prior approval requests and view the associated responses.
Omni 3750 Medicaid Terminal Continues Warranty
Return to Table of Contents
VeriFone discontinued manufacturing Omni 3750 POS terminals in December 2007. New orders for POS terminals are fulfilled with VeriFone's Vx 570 devices.
The five-year warranty purchased with most Omni 3750 Medicaid terminals remains in effect and service will continue to be provided by VeriFone for the term of the warranty. Providers may continue using their Omni 3750 terminal even after its five-year warranty expires. However, should the terminal become inoperable, the provider will be responsible for repairs or replacement.
VeriFone offers repair services for the Omni 3750, as do other third party service companies. Another option would be to purchase a new Vx 570 Medicaid terminal. Visit www.emedny.org. Click on "Self Help"then on "Purchase a POS Device."
Medicaid eligibility verification will continue to be supported via the touch-tone telephone and the electronic Provider Assisted Claim Entry System (ePACES).
The Department of Health (DOH) Mandatory Swiper program will remain in effect for Mandatory Swiper providers required to use a card swipe device.
For questions about Medicaid terminals or to sign up for ePACES, call the eMedNY Call Center at (800) 343-9000.
NYSDOH to Implement National Provider Identifier Requirement
Return to Table of Contents
The New York State Department of Health (NYSDOH) is planning to implement the National Provider Identifier (NPI) requirement on September 1, 2008. As a result, NYS Medicaid provider IDs and license numbers will continue to be required for processing until the NPI system release is installed.
The Office of Health Insurance Programs (OHIP) recommends that you and your information systems staff confirm that your vendors will be capable of processing HIPAA transactions using proprietary identifiers until September 1, 2008.
Questions? Please call the eMedNY Call Center at (800) 343-9000.
Important National Provider Identifier Information for Hospitals, Clinics, and other Facilities
Return to Table of Contents

As a result of the NPI final rule, the National Provider Identifier (NPI) for Attending Providers must be submitted in place of the NYS license numbers. In addition, both the NPI Final Rule and an Office of the Medicaid Inspector General (OMIG) initiative stipulate that the NPI of a clinic, hospital, or other facility can no longer be submitted as the Attending Provider.
Since it is critical for NYS Medicaid to use the Attending Provider's NPI for a variety of edits, including those that validate the Attending Provider's license and their relationship with the Billing Provider, it is essential that a method for associating the Attending Providers NPIs and license numbers with clinics, hospitals and other facilities be established.
It should be noted that OMIG has expressed their intent to review provider information reported in claim transactions, and that a claim will be denied if the Attending Provider's NPI is not on the roster of Attending Providers affiliated with the Billing Provider's NPI. Consequently, all clinics, hospitals and other facilities are now required to maintain an up-to-date "roster"of attending providers that may be included as a provider on claims submitted to NYS Medicaid.
The web based Attending Provider Reporting application allows clinics, hospitals and other facilities to maintain a roster of NPIs and licenses for their affiliated providers. Facilities with multiple NPIs must maintain a separate roster for each NPI. The Facilities Affiliated Practitioners NPI application can be accessed on the eMedNY Web site at http://www.emedny.org/hipaa/NPI/index.html
There is also a batch Facilities Practitioner's NPI Reporting (FPR) submission method, which was developed to accommodate facilities that have a large number of affiliations to record with NYS Medicaid. For information on the FPR, please visit http://www.emedny.org/hipaa/NPI/index.html
For manuals and additional information, please visit the eMedNY NY HIPAA Desk NPI Web site at http://www.emedny.org/hipaa/NPI/index.html
Questions? Please call the eMedNY Call Center at (800) 343-9000.
Policy and Billing Guidance........
Pharmacy Providers
Are you using the correct National Drug Code (NDC) when validating a prior authorization?
Return to Table of Contents

Please Remember:
- Prior authorizations validated with an inactive or invalid NDC will not be processed.
- The prior authorized NDC must exactly match the NDC of the drug you are dispensing.
- Prior authorization numbers and NDCs must be entered correctly on the claim.
If a prior authorization fails because the NDC used in validation does not match the NDC dispensed, it is the pharmacy's responsibility to request a new prior authorization number from the prescriber.
For clinical concerns or preferred drug program questions, contact (877) 309-9493.
For billing questions, contact (800) 343-9000.
For Medicaid pharmacy policy and operations questions, call (518) 486-3209.
The purpose of the POA indicator is to differentiate between conditions present at admission and conditions that develop during an inpatient admission. Example: Did a fracture occur before the patient was admitted or during the patient's care?
Five Indicator Codes Allowed
- Y- present at the time of IP admission
- N - not present at the time of IP admission
- U - documentation is insufficient to determine if condition is POA
- W - provider is unable to clinically determine whether condition was POA or not
- Exempt - leave blank if condition on the "not applicable" list; only reason why field should be blank
Medicaid Claims Will Require Present on Admission (POA) Indicator
Return to Table of Contents
Beginning July 17, 2008 reporting of Present on Admission (POA) indicators for each diagnosis submitted on all Medicaid claims will be mandatory for all inpatient facilities. After this date, claims that lack a valid POA indicator will be denied. In order to minimize the administrative burden of this requirement, Medicaid will use the POA definitions and reporting requirements as outlined by the Centers for Medicare & Medicaid Services (CMS).
The policy, described in MLN Matters 5499, is available at: http://www.cms.hhs.gov/transmittals/downloads/r1240cp.pdf

Please Note: Facilities should continue to report POA indicators on Statewide Planning and Research Cooperative System (SPARCS) submissions. Please be advised that the Department of Health will reject records and inform facilities if there are problems with missing or incorrect indicators. We will include retrospective case reviews to determine the accuracy and validity of POA indicators submitted.
Important: Please make certain that your billing staffs are aware of this requirement, and that your physicians and other practitioners and coders are collaborating to ensure complete and accurate documentation, code assignment and reporting of diagnoses and procedures.
Questions? Please contact Dr. Foster Gesten at (518) 486-6865 or John E. Ulberg, Jr. at (518) 474-6350.
Provider Bulletin
Physicians, Nurse Practitioners, Podiatrists, and Article 28 Ordered Ambulatory Providers
Unclassified Drug Code Now Available for Billing
Return to Table of Contents
Effective for dates of service on and after July 1, 2008, J3490 (unclassified drugs) will be available for billing. The previous code used to bill unlisted drugs, 90779, will be discontinued.
The intent of this change is to be consistent with the definitions of the codes in CPT and HCPCS. Documentation of medical necessity, identification of dose administered and evidence of acquisition cost will be required with submission of a paper claim.
Questions? Please call the Pre-Payment Review Group at (518) 474-8161.
Resources
Return to Table of Contents
NYS SMOKERS' QUITLINE
(866) NY-QUITS or (866-697-8487)
AMERICAN CANCER SOCIETY
(800) 227-2345
AMERICAN LUNG ASSOCIATION
(800) 586-4872
CENTERS FOR DISEASE CONTROL AND PREVENTION
(800) CDC-4636 or (800-232-4636)
NATIONAL CANCER INSTITUTE
(800) 4-CANCER or (800-422-6237)
For more information on the New York State Medicaid Smoking Cessation policy,
please call the Bureau of Pharmacy Policy and Operations at: (518) 486-3209.
Important Reminder
Medicaid Enrollees Cannot be Billed
Return to Table of Contents
This is a reminder to all Medicaid providers about requirements of the Medicaid program related to requesting compensation from Medicaid enrollees, including Medicaid and Family Health Plus enrollees who are enrolled in a managed care plan. For purposes of this article "Medicaid Managed Care enrollees"also includes enrollees eligible for Family Health Plus.
Acceptance and Agreement
When a provider accepts a Medicaid enrollee as a patient, the provider agrees to bill Medicaid for services provided or, in the case of a Medicaid managed care enrollee, agrees to bill the enrollee's managed care plan for services covered by the contract.
The provider is prohibited from requesting any monetary compensation from the enrollee, or his/her responsible relative, except for any applicable Medicaid co-payments.
Private Pay Arrangements
A provider may charge a Medicaid enrollee, including a Medicaid enrollee enrolled in a managed care plan, only when both parties have agreed prior to the rendering of the service that the enrollee is being seen as a private pay patient.
Note that due to the requirement that PRIOR agreement be made for payment, Medicaid enrollees may never be charged for services rendered in the emergency room (except for applicable Medicaid co-payments).
This must be a mutual and voluntary agreement. It is suggested that the provider maintain the patient's signed consent to be treated as private pay in the patient record.
Medicaid Managed Care vs. Medicaid Fee-for-Service
A provider who participates in Medicaid fee-for-service but does not participate in the enrollee's Medicaid managed care plan may not bill Medicaid fee-for-service for a benefit covered in the managed care plan, with the exception of family planning services.
Such a provider may not bill the enrollee for services that are covered by the enrollee's Medicaid managed care contract unless there is prior agreement with the enrollee that he/she is being seen as a private patient as described above. The provider must inform the enrollee that the services may be obtained at no cost to the enrollee from a provider that participates in the enrollee's managed care plan.
In addition, if a Medicaid provider delivers care or services to a person covered by Medicaid and Medicare, Medicaid and Medicare must be billed. The patient cannot be billed for any covered services, except for Medicaid co-payments (if applicable).
Collections
A Medicaid enrollee, including a Medicaid managed care enrollee, must not be referred to a collection agency for collection of unpaid medical bills or otherwise billed, except for applicable Medicaid co-payments, when the provider has accepted the enrollee as a Medicaid patient. Providers may use any legal means to collect applicable unpaid Medicaid co-payments.
Emergency Medical Care
A hospital that accepts a Medicaid enrollee as a patient, including a Medicaid enrollee enrolled in a managed care plan, accepts the responsibility of making sure that the patient receives all medically necessary care and services.
Other than for legally established co-payments, a Medicaid enrollee should never be required to bear any out-of-pocket expenses for medically necessary inpatient services or medically necessary services provided in a hospital based emergency room (ER). This policy applies regardless of whether the individual practitioner treating the enrollee in the facility is enrolled in the Medicaid program.
Claim Submission
The prohibition on charging a Medicaid enrollee applies when a participating Medicaid provider fails to submit a claim to Computer Sciences Corporation (CSC) or the enrollee's managed care plan within the required timeframe. It also applies when a claim is submitted to CSC or the enrollee's managed care plan and the claim is denied for reasons other than that the patient was not Medicaid eligible on the date of service.
Claiming Problems
If a problem arises with a claim submission, the provider must first contact CSC or, if the claim is for a service included in the Medicaid managed care benefit package, the enrollee's Medicaid managed care plan.
If CSC or the managed care plan is unable to resolve an issue because some action must be taken by the enrollee's local Department of Social Services (e.g., investigation of enrollee eligibility issues), the provider must contact the Social Services Department for resolution.
For questions regarding claim submissions or denied claims,
please call the CSC Call Center at (800) 343-9000.
For questions regarding Medicaid managed care, please call the
Division of Managed Care and Program Evaluation at (518) 473-0122.
For questions regarding Medicaid fee-for-service, please call the
Office of Health Insurance Programs at (518) 473-2160.

NYC Ambulette
and Livery Providers
Car Seat Policy Clarification
Return to Table of Contents
Vehicles licensed by the New York City Taxi and Limousine Commission (TLC), i.e., ambulette and livery vehicles, are exempt from car seat (and seat belt) regulations.
However, passengers with children are encouraged to bring their own car seats, which the driver must allow the passenger to install. Regardless of the exemption from law, the TLC encourages everyone to buckle up! Source: http://home2.nyc.gov/html/tlc/html/passenger/faq_pass.shtml
Do you suspect that an Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Call: 1-877-87FRAUD
Your call will remain confidential.
Or complete a complaint form available at:
www.omig.state.ny.us
Important Information for Registered Physician Assistants and Nurse Practitioners
Supervising or Collaborating Physician(s) Must Be Identified
Return to Table of Contents

As a condition of enrollment in the NYS Medicaid program, Registered Physician Assistants (RPAs) must identify their supervising or collaborating physician(s). The provisions in Article 131A of the New York State Education Law and Article 37 of the New York State Public Health Law state that a physician may supervise no more than two physician assistants in his/her private practice and no more than six physician assistants employed by a hospital. Nurse Practitioners must have a minimum of one collaborating physician on file.
A nurse practitioner can have multiple specialties which would result in multiple collaborating physicians. Whenever there is a change in the status of the supervising physician(s) or collaborating physician, the RPA or nurse practitioner must notify the NYS Medicaid program of the change.
RPAs who want to add supervising physicians should complete the supervising physician certification and registered physician assistant enrollment questionnaire. Both forms must be sent in together along with detailed salaried arrangements for the RPA. Nurse Practitioners should complete the collaborating physician form.
These forms are available at: www.emedny.org/info/ProviderEnrollment/index.html
and should be submitted to:
Computer Sciences Corporation
Box 4610
Rensselaer, NY 12144-4610
Failure to update this information with the NYS Medicaid Program/ Provider Enrollment Unit may cause DME, Labs and Pharmacy providers who rendered services ordered by a RPA or Nurse Practitioner to receive the following edit denial:
01239 - Supervising Provider of the submitted order/prescriber was excluded prior to service date: This edit will fail a claim if the ordering/prescribing provider is a Registered Physician Assistant or a Nurse Practitioner.
Potential Causes: If a MMIS provider ID or a registered license number of a RPA or Nurse Practitioner is entered in the prescribing or ordering provider field of a DME, LAB or pharmacy claim, the status of the supervising provider(s) is also verified. If the supervising provider or any member of the group affiliation has an enrollment status indicating they have been excluded/disqualified, this edit will be failed.
Solution: The ordering/prescribing provider - RPA or Nurse Practitioner - must update the enrollment status of their supervising provider(s) with the NYS Medicaid Program/Provider Enrollment Unit. To remove an affiliation with a supervising or collaborating provider, correspondence (on letterhead) requesting disaffiliation with the excluded/disqualified provider(s) should be sent to the address above. Include the RPA or Nurse Practitioner's MMIS ID and name and the affiliated provider's name and either MMIS ID or license number.
Questions? Please contact the Division of Provider Relations and Utilization Management,
Fee for Service Provider Enrollment Department at (800) 342-3005 (option 4 ).
Dental Sealants will Soon Require Prior Authorization
Return to Table of Contents

Effective for dates of service on or after August 1, 2008, all dental sealants (procedure code D1351) will require prior approval in order to ensure that services do not exceed maximum limits. Prior authorization can be obtained by:
- Electronic submission through the DVS system (as noted below); or
- Electronically via a HIPAA 278 transaction by using a PC and ePACES or similar HIPAA compliant software; or
- By submitting an eMedNY prior approval request form 361401
Information on ePACES and instructions on DVS can be obtained at:
http://www.emedny.org/HIPAA/SupportDocs/ePACES.html
Verifone Omni 3750 terminal information and instructions on DVS can be obtained at:
http://www.emedny.org/ProviderManuals/AllProviders/Omni_3750_Supplemental_Guide/1_3/Omni3750_Supplemental_Guide.htm
Complete instructions are available in the "Dental Prior Approval Guidelines"section of the MMIS Dental Provider Manual which can be obtained at:
http://www.emedny.org/ProviderManuals/Dental/PDFS/Dental_PA_Guidelines.pdf
Dispensing Validation System Soon Available
for Full Dentures and Dental Sealants
Return to Table of Contents
Effective with dates of service on or after August 1, 2008 full dentures (procedure codes D5110 & D5120) and all dental sealants (procedure code D1351) can be approved automatically through the electronic Dispensing Validation System (DVS).
The DVS will substantially reduce the time and effort required to determine if the service can be rendered. This is because a DVS request is submitted in "real time". Real time means that the status of the request will be available by the end of your DVS session.
DVS submission is the fastest and easiest way to submit requests and is highly recommended.
DVS can be accessed through:
- A PC using ePACES software;
- By using the VeriFone Omni 3750 POS card-swipe terminal; or,
- By use of a VeriFone Vx570 device.
The current manual review process will continue as in the past for those providers who do not have access to ePACES, VeriFone, or if DVS is declined.
For DVS technical assistance or to obtain eMedNY prior approval request form 361401,
Please contact Computer Sciences Corporation (CSC) at (800) 343-9000.
Questions? Please contact the Division of Provider Relations and Utilization Management, Dental Bureau at (800) 342-3005 option #2.
Policy on "Interrupted Treatment" for Dental Procedures
Return to Table of Contents
Claims are normally submitted when the product or service is completed and delivered to the client. Therefore, the appropriate procedure code (not the "billing code" used for interrupted treatment) should be used along with the date that the service is actually completed and delivered.
All claims submitted using the interrupted treatment billing codes will be pended for manual review. Payment in full may be considered if the supporting documentation demonstrates that the service was completed and delivered.
Payment, either in full or pro-rated, may be considered if the service is NOT completed and delivered. The amount of compensation will be determined based on the documentation provided. If the "decisive appointment" has not been met, or the client was not eligible on the date of the "decisive appointment", no compensation is available.
Medicaid Fee-For-Service Providers
The "Interrupted Treatment" procedure code ("billing code" in the below chart) can be used with the date of the "decisive appointment" as the date of service if the following conditions are met:
- The client was eligible for fee-for-service Medicaid on the date of the "decisive appointment;" however,
- The service is completed and delivered, but the client lost FFS Medicaid eligibility after the date of the "decisive appointment" (eg. lost Medicaid entirely or was switched to a managed care plan with dental coverage); or,
- The service is NOT completed and delivered (eg. client died, was incarcerated, moved away, etc.).
Managed Care Plans
Medicaid managed care and Family Health Plus plans offering dental services must continue to cover any remaining treatments required to complete the procedures listed below if a managed care enrollee is disenrolled from the plan for any reason (including, but not limited to, losing Medicaid eligibility, transferring to another plan or voluntary disenrollment) after a decisive appointment. Such coverage is required even if the number does not qualify for guaranteed eligibility.
| Service | Approved/Multiple Visit Procedures | Billing Code | Decisive Appointment |
|---|---|---|---|
| Space Maintainers | D1510, D1515 | D0999 | Tooth Preparation |
| Crowns | D2710-D2792, D2952, | D2999 | Tooth Preparation |
| Root Canal Therapy | D3310-D3348 | D3999 D3999 | Initial Root Canal Apexification/Recalcification |
| Complete Dentures | D5110-D5120 | D5899 | Final Impression |
| Partial Dentures | D5211-D5214 | D5899 | Final Impression |
| Denture Repairs | D5510-D5660 | D5899 | Acceptance of denture for repair |
| Denture Rebase | D5710-D5721 | D5899 | Final Impression |
| Denture Relining | D5750-D5761 | D5899 | Final Impression |
| Other Prosthetic Services | D5820-D5899 | D5899 | Final Impression |
| Maxillofacial Prosthetics | D5911-D5999 | D5999 | Final Impression |
| Bridge Pontics | D6210-D6252 | D6999 | Preparation of abutment teeth |
| Bridge Retainers | D6545-D6792 | D6999 | Preparation of abutment teeth |
| Other Fixed Prosthetic Services | D6970, D6972 | D6999 | Tooth preparation |
| Orthodontic Treatment | D8670, D8070, D8080, D8090 | D8999 D8999 | Placement of appliances and beginning of active treatment Date of initial appliance treatment |
| Orthodontic Retention | D8680 | D8999 | Completion of active treatment |
| Occlusal Guards | D9940 | D8999 | Final Impression |
Questions? Please call the Division of Provider Relations and Utilization Management, Dental Bureau at (800) 342-3005, option #2.
Important Information for Physicians, Nurse Practitioners, Licensed Midwives, and Ordered Ambulatory Providers
Providers Must Report National Drug Code on Claims for Physician Administered Drugs
Return to Table of Contents
The 2005 Federal Deficit Reduction Act (DRA) requires providers to report the National Drug Code (NDC) when billing for physician administered drugs on Medicaid claims in addition to existing reporting requirements (i.e. Healthcare Common Procedure Coding System - HCPCS).
Electronic claims require a valid 11-digit NDC number for payment. NDCs are not required on claims submitted for 340b drugs billed at their acquisition cost.
The NDC is maintained by the Food and Drug Administration and contains identifying information for the labeler/manufacturer and drug product. Medicaid is required to use this information to maximize federal drug rebates.
NDC Reporting
The NDC can be found on the drug invoice and/ or product package.
The Health Insurance Portability and Accountability Act standard code set for an NDC is 11-digits, in a 5-4-2 configuration. The first five digits represent the labeler/manufacturer, the next four digits represent the drug and strength and the last two represent the package size.
Therefore, when submitting an NDC to the Department, a leading zero may need to be added. When the NDC is listed in a ten digit configuration, where the zero is added depends upon the configuration of the NDC. Examples of the NDC and leading zero placements follow:
| NDC# Configuration | Leading Zero Placement for 5-4-2 Configuration |
| XXXX-XXXX-XX 4 - 4 - 2 | 0XXXX-XXXX-XX 5 - 4 - 2 |
| XXXXX-XXX-XX 5 - 3 - 2 | XXXXX-0XXX-XX 5 - 4 - 2 |
| XXXXX-XXXX-XX 5 - 4 -1 | XXXXX-XXXX-0X 5 - 4 - 2 |
A listing of the drug labelers/vendors currently participating in the Medicaid program is available at: http://www.cms.hhs.gov/MedicaidDrugRebateProgram/10_DrugComContactInfo.asp
Questions? Please call the eMedNY Call Center at (800) 343-9000.
Medicaid Now Reimbursing for Viral Tropism Laboratory Test
Return to Table of Contents

Medicaid now reimburses for viral tropism testing. This test identifies patients who are likely to respond to the new HIV entry inhibitor drug, Selzentry. Currently, one method (Trofile assay) is eligible for coverage; other methods may be covered in the future.
Laboratories are required to use MMIS procedure code 87999 to bill for a viral tropism assay test. The laboratory test is a covered service when clinically indicated, up to a maximum of two tests per 12-month period-per-patient. The test is billable fee-for-service even when ordered for a registered clinic patient.
Clinical laboratories, designated AIDS centers, hospital outpatient services, residential health care facilities, and ordering practitioners are reminded of the following payment policies applicable to all laboratory testing, including viral tropism assay tests:
- Laboratories may not bill for tests performed when patients are hospitalized. Medicaid payment to the hospital includes all necessary laboratory services.
- All ordered tropism assays are reimbursable fee-for-service directly to the testing laboratory. This includes tests ordered for:
- Inpatients of Article 28 residential health care facilities,
- Patients of designated AIDS centers operating under the 7 Tier AIDS payment structure,
- Patients of Article 28 certified outpatient clinics, and
- Patients of Article 28 certified free-standing diagnostic and treatment centers.
Only Medicaid-enrolled clinical laboratories with Department of Health approval to perform viral tropism assays are entitled to reimbursement.
Questions? Please call the Bureau of Policy Development and Coverage at (518) 473-2160.
Computer Sciences Corporation Offers
Seminars - Sign Up Today!
Return to Table of Contents

- Do you have billing questions?
- Are you new to Medicaid billing?
- Would you like to learn more about ePACES?
If you answered YES to any of these questions, please consider registering for a Medicaid seminar. Computer Sciences Corporation (CSC) offers various types of seminars to providers and their billing staff. Many of the seminars planned for the upcoming months offer detailed information and instruction about Medicaid's web-based billing and transaction program - ePACES.
ePACES is the electronic Provider Assisted Claim Entry System which allows enrolled providers to submit the following type of transactions:
- Claims
- Eligibility Verifications
- Utilization Threshold Service Authorizations
- Claim Status Requests
- Prior Approval Requests
Professional providers such as physicians, nurse practitioners and private duty nurses can even submit claims in "REAL-TIME" via ePACES.
Real-time means that the claim is processed within seconds and professional providers can get the status of a real-time claim, including the paid amount without waiting for the remittance advice.
Fast and easy seminar registration, locations and dates are available online at: http://www.emedny.org/training/index.aspx
Please review the seminar descriptions carefully to identify the seminar appropriate for your training needs. Registration confirmation will instantly be sent to your e-mail address.
If you are unable to access the Internet to register, you may also request seminar schedule and registration information through CSC's Fax on Demand service at:
(800) 370-5809; request document number 1002
for a list of seminars and registration information to be faxed to you.
CSC Regional Representatives look forward to meeting with you at upcoming seminars!
Questions? Please call the eMedNY Call Center at (800) 343-9000.

PROVIDER SERVICES
Return to Table of Contents
Missing Issues?
The Medicaid Update, indexed by subject area, can be accessed online at:
http://www.nyhealth.gov/health_care/medicaid/program/update/main.htm
Hard copies can be obtained upon request by emailing: medicaidupdate@health.state.ny.us
Office of the Medicaid Inspector General: http://www.omig.state.ny.us (518) 473-3782
Questions about an Article?
Each article contains a contact number for further information, questions or comments.
Questions about billing and performing EMEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at: http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email:emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to CSC at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.