August 2008
Volume 24, Number 9
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State Department of Health
Deborah Bachrach, Deputy Commissioner
Office of Health Insurance Programs
Important Information
Editorial Message
Medicaid Update Newsletter Will Move to Electronic Distribution
In an effort to distribute the Medicaid Update newsletter in a more timely manner, reduce costs, and be more environmentally minded, beginning in January 2009, the Office of Health Insurance Programs will no longer produce a printed version of the newsletter. The Medicaid Update will ONLY be available electronically. This new delivery system will allow our providers to receive policy sensitive bulletins faster.
The newsletter will be delivered monthly to your designated e-mail address in a Portable Document Format (PDF). The electronic newsletter is the ideal way to have important policy information at your fingertips. Providers will be able to read, print, and share the newsletter with other interested colleagues at their convenience.
TO RECEIVE THE MEDICAID UPDATE ELECTRONICALLY
please send your e-mail address along with your provider ID #
by Friday, October 31, 2008 to:
medicaidupdate@health.state.ny.us
Providers who are unsure about receiving an electronic-only version of the newsletter should bear in mind that the PDF newsletter can always by printed and read in hard copy. In addition, the current and archived newsletters are posted on the DOH Web site at http://www.nyhealth.gov/health_care/medicaid/program/update/main.htm and are always available for your convenience.
You will receive your final printed newsletter by mail in December 2008 as we transition from print newsletters to electronic distribution.
The Office of Health Insurance Programs anticipates that most providers will take advantage of this new delivery system, however, for those few who cannot, arrangements are being considered for hard copy delivery. if you need to receive a hard copy of the Medicaid Update, please send your written request, along with your provider ID#, to the following address by Friday, October 31, 2008:
NYS Department of Health
Office of Health Insurance Programs, Attn: Kelli Kudlack
Corning Tower, Room 2029
Albany, New York 12237
We hope you will continue to find this newsletter to be a valuable source of information.
Don't be left out....send us your e-mail address and provider # today!
 Pharmacy News
Pharmacy News
Family Health Plus Pharmacy Benefit
Effective October 1, 2008, the pharmacy benefit for Family Health Plus managed care enrollees will be "carved-out" of the managed care plan benefit package.
Preferred Drug Program News
Changes are effective August 20, 2008.
Preferred Drug List
A guide detailing New York's list of preferred drugs.
EPIC Update - New York's Prescription Coverage for Seniors
On October 1, 2008 EPIC will require the substitution of brand name multi-source drugs with a generic equivalent.
 Policy and Billing Guidance
Policy and Billing Guidance
Nursing Home Transition and Diversion Medicaid Waiver Program
A new Medicaid waiver program for individuals 18 years of age and older with a physical disability and for seniors who choose to live in the community rather than in an institutional setting.
Learn About Medicaid's New Ambulatory Care Reimbursement Method
The Department of Health has created a new Web site to help providers prepare for Medicaid's new outpatient reimbursement method, Ambulatory Patient Groups (APGs).
Regional Perinatal Center Ambulance Transportation Providers
The cost of ambulance transportation of neonatal infants from community hospitals to facilities designated as Regional Perinatal Centers (RPC) is the financial responsibility of the RPC.
Inpatient Medicaid Claims Require POA Indicator
Reporting of Present on Admission (POA) indicators for each diagnosis submitted on all INPATIENT Medicaid claims are mandatory for all inpatient facilities.
 General Information
General Information
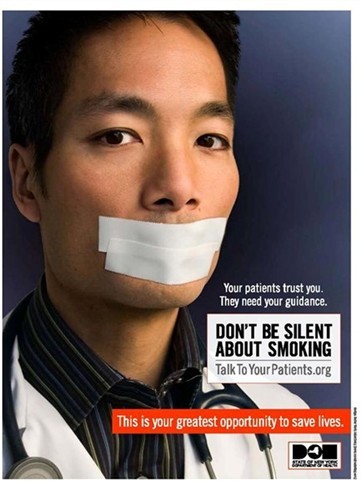
Don't Be Silent About Smoking
Talk to your patients about the dangers of smoking.
 Pharmacy News
Pharmacy News
Family Health Plus Pharmacy Benefit
Return to Table of Contents
Effective October 1, 2008, the pharmacy benefit for Family Health Plus managed care enrollees will be "carved-out" of the managed care plan benefit package and will be administered by the Medicaid fee-for-service program. Family Health Plus enrollees will be issued a Medicaid Benefit Identification Card to obtain their pharmacy benefit.
If enrollees are already using a Medicaid Benefit Identification Card to obtain other benefits, they can use the same Benefit Identification Card to access their pharmacy benefits on or after October 1, 2008. If they currently use a Family Health Plus managed care identification card to access their pharmacy benefits, they must continue to do so until October 1, 2008.
The pharmacy benefit includes:
- Prescription drugs
- Insulin and diabetic supplies currently covered as a pharmacy benefit by Medicaid (e.g., insulin syringes, blood glucose test strips, lancets, alcohol swabs)
- Smoking cessation agents, including OTC products
- Select over-the-counter medications covered on the Medicaid Preferred Drug List (Prilosec OTC, loratadine, Zyrtec)
- Hearing aid batteries
- Enteral formulae with prior authorization (1-866-211-1736)
- Drug co-payments for Family Health Plus enrollees will not change.
Co-payments will remain at $6.00 for brand-name drugs, $3.00 for generic drugs, $1.00 for diabetic supplies, hearing aid batteries and enteral formulae, and $0.50 for covered over-the-counter drugs. For more information about Family Health Plus co-payments, please refer to the April 2006 Medicaid Update, "Family Health Plus Co-payment Information." - Prescriptions for Family Health Plus enrollees will be subject to all Medicaid program requirements.
Prescriptions may also be subject to prior authorization under Medicaid's Preferred Drug Program, Clinical Drug Review Program, and the Mandatory Generic Drug Program. Prior authorization is obtained through the Clinical Call Center at 1-877-309-9493. For more information see https://newyork.fhsc.com or http://www.nyhealth.gov/health_care/medicaid/program/pharmacy.htm - With the exception of controlled substances, prescriptions must be filled within 60 days and are valid for six months from original prescription date with up to five refills.
Drugs administered in the physician's office (J-Code drugs) remain in the managed care benefit package and should continue to be billed to the enrollee's Family Health Plus managed care plan.
Questions? Contact Medicaid Pharmacy Policy & Operations staff at (518)486-3209.
 Pharmacy News
Pharmacy News
Preferred Drug Program Update
Return to Table of Contents
Effective August 20, 2008, prior authorization requirements will change for some drugs in the following ten drug classes:
- Angiotensin Receptor Blockers (ARBs)
- Antihistamines - Second Generation
- Beta Blockers
- Calcium Channel Blockers (Dihydropyridine)
- Central Nervous System (CNS) Stimulants
- Corticosteroids - Intranasal
- HMG-CoA Reductase Inhibitors (Statins)
- Narcotics - Long Acting
- Sedative Hypnotics/Sleep Agents
- Triglyceride Lowering Agents
To obtain prior authorization for non-preferred drugs, call the pharmacy clinical call center at (877) 309-9493 and follow the appropriate prompts.
The New York State Medicaid Preferred Drug List can be accessed at https://newyork.fhsc.com/.
Please remember that preferred drugs do not require prior authorization!
For clinical concerns or preferred drug program questions, call (877) 309-9493.
For billing questions, call (800) 343-9000.
For Medicaid pharmacy policy and operations questions, call (518) 486-3209.
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Call: 1-877-87FRAUD
Your call will remain confidential.
Or complete a Complaint Form online at:
www.omig.state.ny.us
 Pharmacy News
Pharmacy News
UPDATE FROM EPIC
NEW YORK'S PRESCRIPTION PROGRAM FOR SENIORS
Return to Table of Contents

Mandatory Generic Program
Effective October 1, 2008, EPIC will require a prior authorization to cover brand name drugs when there is an A-rated generic available. Some exemptions will apply, consistent with those under the Medicaid Mandatory Generic Program. Mandatory generic requirements will apply only when EPIC is the primary payer, and no other drug coverage is available. Please keep this new requirement in mind when prescribing or dispensing prescriptions to seniors enrolled in EPIC. More information about the EPIC prior authorization process will be provided in upcoming issues.
Coordination with Medicare Part D
EPIC helps seniors pay for their Part D deductibles, co-payments, and prescriptions during the coverage gap - as well as the monthly Part D premiums. EPIC also covers drugs not covered by the Part D plans, but pharmacies are expected to consult with prescribers about possible alternatives on the plan formulary. Effective October 1, 2008, pharmacies will need to certify that the prescriber was consulted, or was unable to be reached, before EPIC is billed as the primary payer. More information will be provided in the near future.
Pharmacists are reminded of the following when billing EPIC for seniors with Part D:
- Medicare Part D must always be billed first, or EPIC will deny the claim.
- Pharmacists can override the denial with an Other Coverage Code (field 308-C8) of 1, but only after submitting an eligibility transaction (E1) to Medicare that confirms there is currently no active Part D coverage.
- If Medicare Part D denies the claim, EPIC should be billed with an OCC of 3, along with the Other Payer Reject Code(s) (field 472-6E).
- If Medicare Part D approves the claim, EPIC should be billed for the Part D deductible or co-payment (Patient Pay Amount (field 505-F5)) with an OCC of 8. This includes "coverage gap" claims that are covered, but not paid, by Part D.
Calling all providers!! Do you have an elderly patient with Medicare Part D who is in the coverage gap? Or do you know a senior who could use help paying for their Medicare Part D premiums or co-payments? Please inform them or their caregivers about EPIC, and suggest they call the EPIC Helpline at (800) 332-3742.
 Policy & Billing Guidance
Policy & Billing Guidance
Nursing Home Transition and Diversion Medicaid Waiver Program
Return to Table of Contents
The New York State Department of Health (DOH) announces the "Nursing Home Transition and Diversion Waiver" (NHTD), a new Medicaid waiver program for individuals 18 years of age and older with a physical disability and for seniors who choose to live in the community rather than in an institutional setting.
PROGRAM INFORMATION
The NHTD waiver will provide community based services to individuals who are:
- Age appropriate;
- Assessed to be eligible for nursing home level of care;
- Capable of living in the community with needed assistance of at least one or more waiver services;
- Eligible for Community Based Long Term Care Medicaid;
- Not receiving services from another Home and Community Based Services Waiver;
- Considered part of an aggregate group that can be cared for at lower cost in the community than a similar group of Medicaid recipients in a nursing home.
DOH will administer this waiver program through nine Regional Resource Development Centers (RRDC) and three Quality Management Specialists (QMS) located throughout New York State. It is anticipated that a total of 5,000 participants will be served by this waiver between now and August 2010.
NHTD WAIVER SERVICES
Participants in the NHTD waiver are eligible to receive the following services:
- Service Coordination
- Assistive Technology
- Community Integration Counseling
- Community Transitional Services
- Congregate and Home Delivered Meals
- Environmental Modifications Services
- Home and Community Support Services (Physician order required)
- Home Visits by Medical Personnel
- Independent Living Skills Training Services
- Moving Assistance
- Nutritional Counseling/ Educational Services (Physician order required)
- Peer Mentoring
- Positive Behavioral Interventions and Supports
- Respiratory Therapy (Physician order required)
- Respite Services (Physician order required)
- Structured Day Program Services
- Wellness Counseling Service (Physician order required)
The NHTD Waiver Application and Program Manual can be accessed at
http://www.nyhealth.gov/facilities/long_term_care/waiver/nhtd_manual/nhtd_program_manual_with_forms.pdf
The Department of Health will be contacting physicians to further explain their responsibility for providing orders for the services specified above. For more information, please contact Bruce Rosen at (518) 486-3154.
Bulletin
Learn About Medicaid's New Ambulatory Care Reimbursement Method
Return to Table of Contents
The Department of Health has created a new Web site to help providers prepare for Medicaid's new outpatient reimbursement method, Ambulatory Patient Groups (APG's). APG's will be phased in beginning in December 2008 and will replace the current reimbursement methods for outpatient and community clinic, ambulatory surgery and emergency department services
To access the Department's new APG Web site go to http://health.state.ny.us/health_care/medicaid/rates/apg/index.htm or go to the http://www.nyhealth.gov and click on "Medicaid" in the left column and then on "Rates"
Bulletin
Ambulance Providers
Return to Table of Contents

The cost of ambulance transportation of neonatal infants from community hospitals to facilities designated as regional Perinatal Centers (RPC) is the financial responsibility of the RPC. Prior authorization of transportation from community hospitals to an RPC will not be granted.
Upon discharge of the infant, transportation from the RPC back to the community hospital is paid by Medicaid fee-for-service. Prior authorization from the appropriate county department of social services may be required. Questions? E-mail the medicaid Transportation Policy Unit at MedTrans@health.state.ny.us or call (518) 474-5187.
The purpose of the POA indicator is to differentiate between conditions present at admission and conditions that develop during an inpatient admission. Example: Did a fracture occur before the patient was admitted or during the patient's care

CMS Reporting Options and Definitions
Five Indicator Codes Allowed
- Y = present at the time of inpatient admission
- N = not present at the time of inpatient admission
- U = documentation is insufficient to determine if this condition os POA at the time of inpatient admission
- W = provider is unable to clinically determine whether the condition was POA
- Exempt - provider must enter "1" if condition is on the "not applicable" List
 Policy & Billing Guidance
Policy & Billing Guidance
CLARIFICATION:
Inpatient Medicaid Claims Require Present on Admission (POA) Indicator
Return to Table of Contents
In the past month, the Department of Health received some calls from providers seeking clarification on reporting responsibilities and requirements that were outlined in the June Medicaid Update article entitled "Medicaid Claims Require Present on Admission Indicators."
As of July 17, 2008 reporting of Present on Admission (POA) indicators for each diagnosis submitted on all INPATIENT Medicaid claims are mandatory for all inpatient facilities. This includes hospitalizations for substance abuse treatment, mental health admissions (including those from OMH licensed Article 31 and OASAS licensed Article 32 facilities), and all medical inpatient services. This also includes inpatient claims from 'Critical Access' Hospitals. All claims that lack a valid POA indicator as of September 17, 2008 will be denied.
In order to minimize the administrative burden of this requirement, Medicaid is using the POA definitions as outlined by the Centers for Medicare & Medicaid Services (CMS) for Medicare. However, the Medicaid POA requirement applies to a broader range of inpatient providers, as described above. The policy, described in MLN Matters 5499, is available at: http://www.cms.hhs.gov/transmittals/downloads/r1240cp.pdf
Inpatient providers should be mindful of the following requirements when submitting a claim:
- Claims without valid POA indicator codes will be denied
- This requirement applies to all INPATIENT bills - including inpatient MH, substance abuse treatment, critical access hospitals, etc.
- POA reporting is required for ALL claims filed after July 17; including claims for hospitalizations that happened prior to that date
- This does NOT apply to physician bills or outpatient billing.
Please Note: Facilities should continue to report POA indicators on Statewide Planning and Research Cooperative System (SPARCS) submissions. Please be advised that the Department of Health will reject records and inform facilities if there are problems with missing or incorrect indicators. We will include retrospective case reviews to determine the accuracy and validity of POA indicators submitted.
Questions? Please contact Dr. Foster Gesten at (518) 486-6865 or John T. Franklin at (518) 473-8822.
Don't Be Silent About Smoking
Return to Table of Contents

PROVIDER SERVICES
Return to Table of Contents
Missing Issues?
The Medicaid Update, indexed by subject area, can be accessed online at:
http://www.nyhealth.gov/health_care/medicaid/program/update/main.htm
Hard copies can be obtained upon request by emailing: medicaidupdate@health.state.ny.us
Office of the Medicaid Inspector General: http://www.omig.state.ny.us (518) 473-3782
Questions about an Article?
Each article contains a contact number for further information, questions or comments.
Questions about billing and performing EMEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to CSC at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.