June 2010 Volume 26, Number 8
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State DOH
Donna J. Frescatore, Medicaid Director & Deputy Commissioner
Office of Health Insurance Programs

A new, free, 10-minute Provider Training Video has been produced by the Centers for Disease Control and Prevention (CDC) and the Safe Injection Practices Coalition. 1,000 copies are available to the first providers who request it at www.oneandonlycampaign.org.
In this issue....
POLICY AND BILLING GUIDANCE
Eligibility/Benefit Verification for Beneficiaries Enrolled in Medicare Health Plans/Medicaid
Change in Medicaid HIV Drug Resistance Billing Policy
Important Changes in the Care At Home I/II Medicaid Waiver
Treatment Of An Emergency Medical Condition New Statewide DOH-4471 Form Available
Provider Requirements in Medicaid Prenatal Care Standards Amended for Nurse Practitioner(s)
PHARMACY UDATES
Medicaid Pharmacy Prior Authorization Programs Update
Pharmacies Are Required to Submit Diagnosis Code on all Durable Medical Equipment,
Prosthetics, Orthotics, and Supplies (DMEPOS) Claims
Immediate Attention: Early Fill Edit
Use of Electronic Records by Pharmacy Providers
NCPDP SCRIPT 10.6 is Permitted for e-Prescribing
MATERNAL HEALTH CARE PROVIDERS AND FACILITIES
Breastfeeding Mothers' Bill of Rights: New Legislation Established
ALL PROVIDERS
Card Swipe Expansion Update
Tips to Prevent Rejection of Yearly Certification Forms
Medicaid Offers (EFT) for Provider Payments and PDF Paper Remittances
Group Practices and Individual Providers' 1099s
OMIG Bureau of Allegations & Complaints (BAC) Fact Sheet
Smoking Cessation Advertisement
Provider Directory
Eligibility and Benefit Verification
for Beneficiaries Enrolled in Medicare
Health Plans and Medicaid
Return to Table of Contents
Verifying Coverage Under Medicare Health Plans: Through the Medicare Modernization Act (MMA) and recent enhancements to eMedNY, Medicare is providing Medicaid with updated eligibility information for beneficiaries enrolled in Medicare Health Plans (also known as Medicare Advantage, Medicare Part C, and Medicare Managed Care Plans). Providers should expect to see this coverage more frequently on eligibility transactions.
Information available through the Medicaid Eligibility Verification System (MEVS) gives providers the eligibility status for a Medicaid beneficiary for a specific date (today or prior to today) and any Medicare, third party insurance, or HMO coverage that a beneficiary may have for the date of service. If the beneficiary is enrolled in a Medicare Health Plan, the MEVS response is:
- ePACES: Additional Payer Information - Carrier Code beginning with "H", "R", or "E" followed by four numeric digits.
- Verifone: Other Insurance - Plan Code beginning with "H", "R", or "E" followed by four numeric digits.
For further information, please see the MEVS manual available online at: http://www.emedny.org/ProviderManuals/AllProviders/supplemental.html#MEVSPM.
Medicare Health Plan Benefits May Include Dental and Vision Services: Some Medicare Health Plan benefit packages include certain dental and vision services not otherwise covered by traditional Medicare Part B. When a beneficiary is covered by a Medicare Health Plan, it is the provider's responsibility to verify the benefit package with the Plan directly.
For a listing of Medicare Health Plans, please visit: http://www.medicare.gov/MPPF/Include/DataSection/Questions/ListPlanByState.asp. (Scroll to bottom left of the page, and click on "New York" from the dropdown menu under "Learn More About Health Plans and Medigap Policies in Your Area.")
Medicaid As Secondary To A Medicare Health Plan: Medicaid requires that providers exhaust all existing benefits prior to billing Medicaid. Medicaid will then pay the applicable Medicare health plan coinsurance, co-payment and deductible. Providers must become network providers for Medicare health plans since plans must be billed first for all services included in the benefit package.
Please review the following editions of the Medicaid Update regarding billing instructions for Medicaid beneficiaries with coverage under a Medicare Health Plan:
http://www.health.state.ny.us/health_care/medicaid/program/update/2009/2009- 11.htm#enr
http://www.health.state.ny.us/health_care/medicaid/program/update/2010/2010- 01.htm#ben.
When required, providers must obtain prior authorization from the Medicare Health Plan and/or Medicaid.
For further questions on eligibility and claims transactions, please contact the eMedNY Call Center at (800) 343-9000.
For questions on Medicaid prior authorization, please call the Division of Provider Relations and Utilization Management at (800) 342-3005.
Change in Medicaid HIV Drug
Resistance Billing Policy
Return to Table of Contents
Modifications were recently made to the Medicaid billing policy for HIV drug resistance testing in response to Office of State Comptroller (OSC) recommendations to prevent overutilization for such testing.
New York Medicaid currently covers up to three HIV genotypic (87901) and HIV phenotypic (87903) drug resistance tests in any combination for beneficiaries within a 365 day period. For dates of service on or after January 1, 2010, Medicaid will reimburse laboratories for up to four HIV genotypic and phenotypic drug resistance tests in any combination within a 365 day period. This new policy will be enforced by payment edits that will apply across all laboratory providers. The frequency of HIV drug resistance testing was set in accordance with standard of care. Laboratories may wish to keep ordering practitioners updated as to each patients' utilization of these tests.
Note: The virtual phenotype drug resistance test (87900) is unaffected by this change and may continue to be billed a maximum of three times per recipient within a 365 day period, regardless of the number of HIV genotypic or HIV phenotypic drug resistance tests that have previously been provided the patient.
Billing questions? Please call the eMedNY Call Center at (800) 343-9000.
Policy questions? Please call the Bureau of Policy Development and Coverage at (518) 473-2160.
Important Changes in the Care
At Home I/II Medicaid Waiver
Return to Table of Contents
Care at Home (CAH) I/II is a Home and Community Based Services (HCBS) Medicaid waiver that enables physically disabled children to remain in the community instead of being institutionalized. The Department's waiver renewal, approved in 2009, included certain changes in eligibility as well as the addition of palliative care services designed to address end-of-life issues related to the child's illness.
The Department began enrolling providers effective February 25, 2010, for the palliative care waiver services:
- Family Palliative Care Education (Training); Bereavement Therapy; Pain and Symptom Management; Expressive Therapy (Art, Music and Play); and Massage Therapy.
The Department invites interested Hospices and Certified Home Health Agencies which meet certain eligibility and practice requirements, to apply to become a Care at Home (CAH) I/II Pediatric Palliative Care waiver service provider. Interested providers may apply to provide one or more palliative care waiver services. An application is available online at: http://nyhealth.gov/facilities/long_term_care/.
In addition to the palliative care services, there are several changes to the CAH I/II waiver. A 30- day inpatient stay is no longer required for eligibility, and children who are EITHER Medicaid eligible based on their parent's income OR who are ineligible for Medicaid, based on their parent's income and/or resources, may apply for enrollment in the waiver if they meet the following qualifications:
- Be under the age of 18;
- Be physically disabled, according to the Social Security Administration (SSA) program criteria;
- Require the level of care provided by a skilled nursing facility or hospital; and,
- Be capable of being cared for in the community safely.
For additional guidance please contact the Office of Long Term Care, Bureau of Medicaid Waivers, CAH I/II Program at (518) 486-6562, or via e-mail at: EAM04@health.state.ny.us.
Treatment Of An Emergency Medical
Condition New Statewide DOH-4471
Form Now Available
Return to Table of Contents
Form DOH-4471 "Certification of Treatment of an Emergency Medical Condition" has now replaced the Upstate form LDSS-3955 and New York City Medical Assistance Program (MAP) form MAP-2151. The new DOH-4471 form is available for download at: http://www.health.state.ny.us/health_care/medicaid/publications/docs/gis/10ma012att.pdf.
Please note this is a single page two-sided form. Effective July 1, 2010, local departments of social services (LDSSs) and the Medical Insurance and Community Services Administration (MICSA) are required to use form DOH-4471. Providers should not submit previous versions of the LDSS-3955 or the MAP-2151 form on or after July 1, 2010. Submission of the LDSS-3955 or MAP-2151 form after June 30, 2010, may result in a delay in payment. The most significant changes made to the form are in the "Authorization to Release Medical Information" section. This section appears on side two of the form and includes both the English and Spanish translation of the information. Provider instructions on how to complete the new DOH-4471 form have been added to side two.
The DOH-4471 form can now accommodate up to four coverage periods ("From-To" date(s) of Treatment/Hospital Stay). The date of Treatment/Hospital Stay entered on the form begins with the first day of the emergency. Medicaid reimbursement for emergency services is limited to the day the treatment was initiated through the period of time in which the need for the emergency services exists. The new DOH-4471 form must be completed, dated, and signed by the treating physician and the applicant/recipient for any subsequent treatment/hospital stay or continuing treatment for an emergency medical condition.
Note: The maximum period of time that can be entered on a single DOH-4471 form is 90-days. This can be a combination of retroactive, current, and prospective coverage. Temporary nonimmigrants and undocumented aliens applying for coverage for treatment of an emergency medical condition are required to file a Medicaid application and must sign the DOH-4471, "Authorization to Release Medical Information" section on page 2. If the individual is unable to sign the certification form, the individual's authorized representative may sign on his/her behalf. The form is not valid without the required signature.
- Signing the form authorizes the LDSS to request information regarding the emergency medical treatment. It also gives the physician or facility permission to provide such information.
- A physician must, in all cases, make the decision as to whether or not the medical treatment is for an emergency medical condition.
Questions related to immigrant eligibility for Medicaid may be directed to the Bureau of Medicaid and Family Health Plus Enrollment at (518) 474-8887.
Provider Requirements in Medicaid
Prenatal Care Standards Amended for
Nurse Practitioner(s)
Return to Table of Contents

The New York State Medicaid Prenatal Care Standards have been revised to more accurately reflect the requirements for a nurse practitioner to be considered a qualified provider of prenatal and postpartum care. Prenatal care services, including prenatal diagnostic and treatment services, provided to pregnant women and postpartum women shall meet generally accepted standards of care as described by the most current American Academy of Pediatrics (AAP) and the American College of Obstetricians and Gynecologists (ACOG) guidelines for perinatal care. These services can be provided in New York State by a nurse practitioner in accordance with Article 139 of the New York State Education Law. Specialty certification in obstetrics/gynecology has been removed from the Prenatal Care Standards.
Medicaid Pharmacy Prior
Authorization Update
Return to Table of Contents
The following changes to the Preferred Drug Program (PDP) and Clinical Drug Review Program (CDRP) are effective June 17, 2010.
Prior authorization requirements will change for some drugs in the following four PDP drug classes:
- Angiotensin Receptor Blockers (ARBs); ARBs + Diuretics; HMG-CoA Reductase Inhibitors (Statins); Proton Pump Inhibitors (PPIs)
In addition to these changes, prior authorization will no longer be required under CDRP for the following medications:
- Byetta® (exenatide); Victoza® (liraglutide)
To obtain prior authorization for non-preferred drugs within the drug classes listed above, please contact the Clinical Call Center at (877) 309-9493 and follow the appropriate prompts. For an up-to-date Preferred Drug List (PDL), with a full listing of preferred and non-preferred drugs for each of the drug classes currently subject to the PDP, please visit: https://newyork.fhsc.com/downloads/providers/NYRx_PDP_PDL.pdf.
Additional information, such as a "Quick List" of only preferred drugs and updated prior
authorization forms, is available at each of the following Websites:
http://www.nyhealth.gov or http://www.eMedNY.org or https://newyork.fhsc.com
Note: Future changes to the Medicaid Pharmacy Prior Authorization Programs, including updates to the Preferred Drug List (PDL), will be communicated electronically through the Medicaid Update and the above mentioned Websites. If you wish to receive direct e-mail notification of changes, please send your request to: NYPDPNotices@magellanhealth.com.
Remember, unless otherwise indicated on the PDL or Quick List, prescribing preferred drugs requires no further action on your part.
For clinical concerns or preferred drug program questions, contact (877) 309-9493.
For billing questions, contact (800) 343-9000.
For Medicaid pharmacy policy and operations questions, contact (518) 486-3209.
Pharmacies Are Required to Submit
Diagnosis Code on all Durable Medical
Equipment, Prosthetics, Orthotics, and
Supplies (DMEPOS) Claims
Return to Table of Contents
New York Medicaid policy requires that prescribers provide a valid diagnosis code on all fiscal orders for durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS).
A valid diagnosis code is a minimum requirement for all DMEPOS fiscal orders. The diagnosis code must be submitted on all NCPDP pharmacy DMEPOS claims. The diagnosis code on the fiscal order must match the diagnosis code reported on the claim. Providers that bill using the 837 form should already be submitting the diagnosis code on all DMEPOS claims.
The following are the NCPDP 5.1 fields utilized to report diagnosis code:
| NCPDP FIELD | DESCRIPTION |
|---|---|
| Diagnosis Code (424-DO) | Code identifying the diagnosis of the patient |
| Diagnosis Code Count (491-VE) | Count of diagnosis occurrences 1-5 'Diagnosis Codes' may be sent |
| Diagnosis Code Qualifier (492-WE) | Code qualifying the 'Diagnosis Code' sent '01'= International Classification of Diseases (ICD-9) |
In September 2010, New York Medicaid will implement claims editing to validate that the diagnosis code is appropriate for the DMEPOS item reported. For example, claims for diabetic test strips must include the prescriber's diagnosis of diabetes.
Additional information on fiscal order requirements can be found in the Pharmacy and DME Provider Policy Manuals available online at: http://www.emedny.org/ProviderManuals/index.html.
For billing questions, please call the eMedNY Call Center at (800) 343-9000.
Immediate Attention: Early Fill Edit
Return to Table of Contents
Effective July 15, 2010, the "03" (Vacation Supply) Submission Clarification Code-Field 420- DK, currently in use, will not be acceptable as an override for the Early Fill edit. Beneficiaries should be instructed to make alternative arrangements when a temporary absence prevents them from picking up their prescriptions.
In cases of extenuating circumstances, the beneficiary should contact (518) 486-3209 at least seven days prior to departure. Approval will not be granted for controlled substances.
Use of Electronic Records by Pharmacy Providers
Return to Table of Contents
The guidelines for electronic records used in the Medicaid program were originally published in the November 2003 Medicaid Update. These guidelines permit, but do not require, the use of electronic records by Medicaid providers. General record keeping requirements for pharmacy providers will now include the following guidelines for the use of electronic records:
- Pharmacies must keep on file the signed prescription or fiscal order for which Medicaid payment is claimed for six years from the date of payment.
- Where original records are required (e.g. fiscal orders for supplies or durable medical equipment), providers may store them off-site and maintain copies (paper or electronically imaged) on-site. The original records must be accessible, made readily available upon a lawful request, and the location of the original records must be maintained in writing at the service location site (pharmacy).
- Electronic imaging of prescriptions and fiscal orders must result in an exact reproduction of the original order and may be required to be authenticated.
- A telephone order must be reduced to writing, either through written communication or electronic record, indicating the time of the call and initials of the pharmacist.
Effective immediately pharmacies are no longer required to generate and keep a hard copy of electronic prescriptions and fiscal orders. Original orders received in electronic format may be securely stored electronically. For Medicaid pharmacy policy questions, please call (518) 486- 3209.
NCPDP SCRIPT 10.6 is Permitted for e-Prescribing
Return to Table of Contents
Effective July 1, 2010, the Centers for Medicare and Medicaid Services will permit either NCPDP SCRIPT version 8.1 or version 10.6 for Medicare Part D e-prescriptions. Clinicians may use either NCPDP SCRIPT 8.1 or 10.6 for e-prescribing under the New York Medicaid e-Prescribing Incentive Program as of July 1, 2010.
Breastfeeding Mothers' Bill of Rights:
New Legislation Established
Return to Table of Contents

The U.S. Surgeon General recommends that babies be fed only breast milk for the first six months of their lives. The public health benefits of breastfeeding have long been recognized. Human milk is uniquely adapted to the nutritional needs of infants and provides for optimal growth and development. Breast milk is easy to digest and contains antibodies that help reduce the infant's risk of infection. Breastfed infants are at reduced risk for asthma, obesity, diabetes and other chronic illnesses throughout their lifetimes. Breastfeeding also benefits the mother, reducing postpartum bleeding, and reducing the risks of breast and ovarian cancers. Breastfeeding yields both health and economic benefits to the family and society.
In New York State, 70% to 80% of new mothers initiate breastfeeding. However, current New York rates of exclusive breastfeeding are approximately half the Healthy People 2010 goals of 40% at three months and 17% at six months. New York's rates are 26% and 8%, respectively. New York can and must do better.
To promote breastfeeding in New York State, the State Legislature has enacted into law the Breastfeeding Mothers' Bill of Rights, which covers all maternal health care providers and facilities, effective May 1, 2010.
This new legislation includes the right of pregnant women and new mothers:
- To be informed about the benefits of breastfeeding, and;
- To obtain support for breastfeeding during pregnancy, after delivery, and after discharge.
Specifically, all hospitals and birthing centers providing maternity care services must:
- Conspicuously post the Breastfeeding Mothers' Bill of Rights;
- Include the Breastfeeding Mothers' Bill of Rights in the Maternity Information Leaflet, which is distributed during pre-booking or admission;
- After delivery, assure that new mothers have the appropriate conditions to support their decision to breastfeed their infants. This includes allowing the baby to stay with the mother immediately after birth, the right for the baby not to be bottle fed or be given pacifiers, and for provisions to be made to allow the baby to room-in;
- Make available trained staff who can provide to new mothers information on breastfeeding, breastfeeding support and expressing milk; updates on mothers' success with breastfeeding; and assistance to improve breastfeeding;
- In addition, upon leaving the facility, new mothers have the right to obtain breastfeeding information without commercial material, to be released without discharge packs containing infant formula, and to obtain information about community resources to support breastfeeding.
The NYS Department of Health encourages all maternal health care providers and facilities to review the new legislation and the Breastfeeding Mothers' Bill of Rights to determine the legislative requirements with which they must comply.
The NYS Department of Health encourages all maternal health care providers and facilities to review the new legislation and the Breastfeeding Mothers' Bill of Rights to determine the legislative requirements with which they must comply.
The documents are available online at: www.health.state.ny.us/community/pregnancy/breastfeeding/index.htm.
The Web page listed above includes the Breastfeeding Mothers' Bill of Rights in several languages. These materials can be used for posting at maternal health care facilities, and for inclusion in the Maternity Information Leaflet. The Department of Health calls on all maternal health care providers to promote breastfeeding by implementing this new Bill of Rights at your facility, and to look for additional opportunities to encourage and enable new mothers to breastfeed.
For questions about the Breastfeeding Mothers' Bill of Rights, contact the Department of Health's Bureau of Maternal and Child Health at (518) 474-0535, or email: promotebreastfeeding@health.state.ny.us.
The New York State WIC Program is a valuable resource for additional information on services for breast feeding support in the state. This is a supplementation nutrition program for lowincome pregnant and postpartum women (nursing and non-nursing), infants and children who meet certain medical or clinical criteria. One of the required services provided by the program is the promotion and support of breast feeding. Each local program has a trained breast feeding coordinator and a Peer Support program with trained peer counselors who provide education and other supports to assist women who decide to breast feed their infants.
For additional information about the WIC Program and requirements for client participation, please visit: www.health.state.ny.us/prevention/nutrition/wic/index.htm. To find out more about the WIC Breastfeeding Promotion and Support program, please contact the Growing Up Healthy Hotline to locate the WIC Local Agency nearest to you at (800) 522-5006.
Card Swipe Expansion Update
Return to Table of Contents
The New York State Office of the Medicaid Inspector General (OMIG) will be expanding the Card Swipe Program to include various pharmacies, dentists, physicians, private duty nurses, and transportation companies. In accordance with 18 NYCRR 514.4 and 514.5(e), providers who participate in the Card Swipe program are required to use the VeriFone terminal in a significant number of their weekly Medicaid transactions. Minimum compliance with this requirement calls for providers to swipe 85 percent of all eligibility transactions by passing the Medicaid beneficiary's benefit identification card through the VeriFone terminal. There is a 15 percent allowance designed to handle situations such as lost/stolen/forgotten cards, temporary cards, or cards that do not swipe.
Medicaid beneficiaries are required to carry their identification cards. The Department of Health regulation 18 NYCRR 360-6.2(b)(4) states that "A beneficiary must present the Medicaid (MA) identification card or a department-approved equivalent to the Medicaid provider before receiving medical services or supplies." Medicaid beneficiaries (outside New York City area) who do not have their card, or their card will not swipe, should be referred to their local Social Services Office or Medicaid office for a replacement card. New York City area Medicaid beneficiaries may call (877) 472-8411 or (718) 557-1399.
Designated Card Swipe providers will receive a free card swipe terminal. The terminal is the property of New York State. Pharmacies should swipe the Medicaid beneficiaries card when the prescription is picked up. If the Medicaid beneficiary is located in a foster care facility, they may not have been issued a card, they may be on a roster. The provider should check eligibility manually, but not refuse service to these beneficiaries based on the inability to swipe. If the Medicaid beneficiary does not provide the card, assuming that the provider is familiar with the Medicaid enrollee and can verify their ID number, service may be provided. The provider should instruct the Medicaid beneficiaries to bring their card the next time they require service(s). If a Medicaid beneficiary arrives with a temporary Medicaid ID card, the provider can use the card swipe terminal keypad to input information from the temporary card to access eligibility information. However, this will not count as a valid swipe transaction for the purpose of calculating the swipe percentage.
General terminal care information:
- Terminals should be kept in a clean, dry location.
- The terminal may need to be cleaned.
- Magnetic card swipe terminal cleaner kits can be purchased on-line or through VeriFone.
- To limit the number of Medicaid eligibility cards that will not swipe properly, Medicaid beneficiaries should be advised to keep their Medicaid ID card away from their cell phone. NOTE - Cards with improved magnetic strips will soon be available.
Providers that require technical assistance may contact the eMedNY Call Center at (800) 343- 9000. All other Card Swipe program questions may be directed to (518) 402-1470. For additional information on the Card Swipe program, please visit the OMIG Website at: www.omig.state.ny.us.
Tips to Prevent Rejection of Yearly
Certification Forms
Return to Table of Contents
New York Medicaid policy requires that each provider annually certify their connection with their Electronic Transmitter Identification Number (ETIN). If the certification is not renewed annually, claims and other transactions will be rejected on the expiration date.
During each 12-month period, eMedNY distributes two renewal notices accompanied by a preprinted certification statement with the provider and ETIN information listed on the form. The first notice is sent 45 days prior to the date the yearly decertification will take place and a second notice is sent 30 days prior to the decertification date.
For providers who are applying for a new ETIN, the certification must accompany the ETIN application. The ETIN application and the certification form that must accompany it can be found at www.emedny.org. Please adhere to the following instructions to prevent the rejection of your certifications and the rejection of claims:
- All information entered on the form should be legible; and red ink is prohibited.
- If the certification you have completed from the Web site has no ETIN entered in the upper left-hand corner, it is assumed you are applying for a new ETIN. In this case the certification must be sent in with the ETIN application form.
- Please make certain that the name of the provider and the provider number match. For example, if you are submitting a certification for an individual practitioner ID, the name of the individual must be entered on the form. If you are certifying a group practice ID, the group practice name and group provider number must match.
- For most providers, the National Provider Identifier (NPI) is now required on certification forms. If you are a provider that is exempted from the NPI rule, your NY Medicaid MMIS Provider ID should be entered. NPIs are 10 digits in length and Medicaid numbers are 8 digits.
- All signatures (provider's and notary's) must be original ink signatures.
- The name of the person signing before the notary must be entered in the blank line right after the words: "before me personally came."
- The notary should use the official notary stamp, however, if the stamp is not available, the written information in place of the stamp must include the notary's number, expiration date, and signature.
Questions? Please contact the eMedNY Call Center at (800) 343-9000.
Medicaid Offers Electronic Funds
Transfer (EFT) for Provider Payments
and PDF Paper Remittances
Return to Table of Contents
Thousands of providers have signed up to have their Medicaid funds deposited directly into their checking or savings account. Providers that have not yet signed up for EFT are urged to take advantage of the benefits that EFT offers - benefits include:
- Eliminates the possibility of lost checks;
- Eliminates delays that may be caused by misdirected checks;
- Eliminates mail time;
- Funds are secure;
- Save trips to the bank to deposit your checks from Medicaid.
In addition to EFT, providers who currently receive paper remittance statements from Medicaid can elect to receive a PDF version of the paper remittance delivered electronically through eMedNY's secure Website. PDF remittances have many advantages over paper remittances such as:
- The remittance will not be held with your Medicaid check or EFT release for two weeks but released to you two weeks earlier.
- You will know when the PDF is available in your eXchange account and not have to wait for the mail.
- The remittance can be downloaded and stored electronically for ease of retrieval and you can still print a hard copy.
- The remittance can be word searched to help locate specific claims.
- The PDF will look exactly like the paper remittance you may be use to receiving.
- Remittances can be printed with Adobe Reader® (6.0 release or higher required), which is available free of charge.
Both the EFT and PDF remittance applications are available online at: http://www.emedny.org/info/ProviderEnrollment/index.html.
Questions? Please contact the eMedNY Call Center at (800) 343-9000.
Group Practices and Individual
Providers' 1099s
Return to Table of Contents
Each year, the eMedNY Call Center receives calls from individual practitioners who have been contacted by the Internal Revenue Service (IRS) for underreporting their income. The following tips were developed to help assist individual practitioners who are employed by group practices.
- To direct payments to a Group Practice Tax ID Number, claims must be submitted with the GROUP Practice NPI in the appropriate Group ID field of a claim. Failure to submit a valid group NPI will cause Medicaid payments to be directed to the Individual Practitioner's NPI. Funds paid to the individual will appear on the individual's 1099 tax form and are reported to the IRS under the individual's social security number.
- When a group practice receives a payment for an individual practitioner's NPI, the funds should be either directed to the individual practitioner or the claims should be voided and rebilled with a valid Group Practice NPI before the end of the year. Group practices are urged not to deposit checks made out to individual practitioners to group practice bank accounts without notifying the individual practitioner as the individual will receive a 1099 tax report showing the funds paid to the individual. This could cause problems for the individual as eMedNY reports these funds to the IRS as paid to the individual practitioner.
- Once the 1099 is issued for funds paid to the individual practitioner, eMedNY cannot alter the 1099 information. If this occurs, individual practitioners should work with the group practice to satisfy any IRS requirements. If the practitioner did not receive the 1099, a duplicate can be requested, at no charge, by sending a written, signed request that includes the provider number and tax year to the following address:
Computer Sciences Corporation
PO Box 4611
Rensselaer, NY 12144-8611
For a fee, eMedNY can provide a list of checks that were included in the 1099 amount and copies of canceled checks to show where the funds were deposited. The fee for a check listing is $30.00 and canceled check copies are $10.00 each. Requests for these documents can be sent to the address above with the appropriate payment.
Questions? Please contact the eMedNY Call Center at (800) 343-9000.
NYS Office of the Medicaid Inspector
General (OMIG) Bureau of Allegations &
Complaints (BAC) Fact Sheet
Return to Table of Contents
The New York State Office of the Medicaid Inspector General's (OMIG) Bureau of Allegations and Complaints (BAC) receive all Medicaid allegations and complaints and refer them to the appropriate entity for further action/investigation.
HOW TO REPORT MEDICAID COMPLAINTS AND FRAUD ALLEGATIONS:
Phone: Toll-free (877) 873-7283 or (518) 402-1378 Fax: (518) 486-7192
E-mail: BAC@omig.ny.gov.
OMIG Website: http://www.omig.ny.gov
Mailing Address: NYS Office of the Medicaid Inspector General (OMIG), Bureau of Allegations and
Complaints, 800 North Pearl Street, Albany, New York 12204
WHAT SHOULD BE REPORTED?
Providers are urged to alert the OMIG should they suspect or observe Medicaid misconduct. Some examples include:
- Giving or receiving bribes or kickbacks
- Unacceptable medical and/or billing practices
- Misuse or abuse of Medicaid services
- Falsifying records or giving false information
WHAT INFORMATION IS NEEDED?
- Who is involved
- What wrongdoing occurred
- When it occurred
- Whether there are witnesses to the misconduct
Please describe in as much detail as possible what a person or business did to commit Medicaid Fraud. Please enclose copies (never originals) of supporting documentation, when available.
WILL MY COMPLAINT REMAIN CONFIDENTIAL?
When providers contact the OMIG with a complaint they are not required to identify themselves, however, we encourage them to do so should we need to ask additional questions during our evaluation. If providers choose to identify themselves when filing a complaint, it should be noted that it is our strict policy to protect your identity during the course of our evaluation or investigation.
WHAT HAPPENS AFTER I REPORT MY COMPLAINT?
After your complaint is received, the OMIG (BAC) will evaluate and take appropriate action. If you submit your name and contact information on the complaint, you will receive an acknowledgement from the OMIG.
If you think it's wrong, it should be reported!
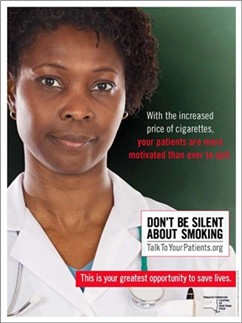
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting. For more information, please visit www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Please Call: 1-877-87FRAUD or (212 417-4570)
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us

Provider Directory
Return to Table of Contents
Office of the Medicaid Inspector General:
http://www.omig.state.ny.us or call (518) 473-3782 with general
inquiries or 1-877-87FRAUD with suspected fraud complaints or allegations.
This contact information can also be used for Provider Self-Disclosures.
Questions about billing and performing MEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Does your enrollment file need to be updated because you've experienced a change in ownership?
Fee-for-Service Providers please call (518) 402-7032
Rate-Based/Institutional Providers please call (518) 474-3575
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.