April 2012 Medicaid Update Special Edition Volume 28, Number 4
Introducing Health Homes
Improving Care for Medicaid Recipients with Chronic ConditionsOverview
The Health Home program is a result of the efforts of the Medicaid Redesign Team (MRT), which was established by Governor Andrew Cuomo in January 2011 and charged with reducing costs while increasing quality and efficiency in New York's Medicaid program. Health Homes will improve the health care provided to both Fee-for-Service (FFS) and Managed Care Plan (MCP) members of the Medicaid Program (who are medically needy) and will save money by reducing preventable hospitalizations, emergency room visits and unnecessary care. It is anticipated that at least 975,000 of the more than five million Medicaid members meet the Federal criteria for Health Homes. The Centers for Medicare and Medicaid Services (CMS) approved the State Plan Amendment (NYS Health Home SPA for Individuals with Chronic Conditions 11-56) for Phase I of the Health Home program on February 3, 2012, with an effective date of January 1, 2012.
A Coordinated Effort
The Department of Health (DOH) Office of Health Insurance Programs (OHIP) (which includes Medicaid); Health Information Technology Transformation (OHITT) and the AIDS Institute; the NYS Office of Mental Health (OMH); the NYS Office of Alcoholism and Substance Abuse Services (OASAS) and the NYC Department of Health and Mental Hygiene have been working together with a provider advisory group to develop this new initiative. On January 1, 2012, DOH implemented the Health Home program. Health Homes provide a care coordination model for high-cost, high-need Medicaid recipients. Health Homes in New York State have been specifically designed to provide integrated care management focused on these individuals. The program is designed to reimburse specially selected providers meeting state and federal criteria for delivering care management services to members with chronic medical and behavioral health conditions. Beginning January 1, 2012, the state will convert existing case management programs: OMH Targeted Case Management (TCM), HIV COBRA and the OASAS Managed Addiction Treatment Services program (MATS) into Health Homes. Guidance to implement retroactive claiming under new rates for patients already receiving these case management services will be posted on, or linked to the Health Home web site as developed.
OMH guidance on TCM conversion is posted on the OMH web site at: http://www.omh.ny.gov/omhweb/adults/health_homes/.
OASAS guidance is forthcoming for the MATS conversion/billing and from the AIDS Institute for COBRA conversion/billing.
What is a Health Home?
A Health Home is a care management service model whereby all of the professionals involved in a member's care communicate with one another so that all needs (medical, behavioral health and social service) are addressed in a comprehensive manner. This is done primarily through a "care manager" who oversees and coordinates access to all of the services a member requires while ensuring that the member receives everything necessary to stay healthy. Oversight and care coordination will reduce unnecessary emergency department visits and inpatient stays, and health records will be shared among providers so that services are not duplicated or neglected. Health Home services are provided through partnerships between health care providers, health plans and community based organizations. When all the services and partners are considered collectively they effectively become a "Health Home." A Health Home is distinct from a Patient-Centered Medical Home or PCMH (see figure 1).
Identifying the Need
New York's Medicaid program currently serves individuals with a broad array of health care needs and challenges. The majority of Medicaid members are relatively healthy and only require access to primary care practitioners for episodic, acute and preventive health care. However, the Medicaid program has several population groups that have complex medical, behavioral, and long term care needs. These populations utilize a large volume of high cost services including inpatient and long-term institutional care. Navigating the current health care system can be difficult for healthy Medicaid members, and even more so for members who have complex chronic conditions.
The first Health Home program is designed specifically to provide care management for adults with chronic medical and behavioral conditions. Developmentally disabled individuals, children, and members in need of long-term care services will not be assigned to Health Homes initially, as other Health Home care management models will need to be developed for these populations. (see figures 2 & 3)
Recipients with Multiple Chronic Illnesses(PDF, 3KB, 1pg.)
Implementation
Health Homes will be implemented in three population waves, with each wave targeting a different eligible population. This first wave will focus on those with mental health/substance abuse and other chronic conditions as described above. Subsequent waves will be developed to focus on those with long-term care needs and developmental disabilities.
The long-term care population is targeted for the second wave and the approach for implementation includes two components that are still under development. The first component is to develop a Health Home using the existing managed long term care program (MLTCP) structure and work to leverage and improve the care management within that program. The second long-term care component would include building a care management network of nursing homes and non-institutional providers to manage services. The best way to implement Health Homes for the long-term care population is the subject of ongoing discussions between New York State staff, and the CMS Innovation Center.
The third wave of Health Home implementation targets the developmentally disabled population. This population currently is served in an existing targeted care management program that will most likely convert to Health Homes after work is completed on a Medicaid waiver, the People First waiver, being developed for this population. A separate Health Home for children is also under discussion. The remainder of this Medicaid Update article will focus on the first wave of Health Home implementation for those with mental health/substance abuse and other chronic conditions.
The first wave of Health Homes for those with chronic mental health/substance abuse and other chronic medical conditions will be rolled out in geographic phases across the state until the program is statewide. (see figure 4) Health care providers in areas designated for the Phase I roll out are located in Bronx, Kings (Brooklyn), Nassau, Warren, Washington, Essex, Hamilton, Clinton, Franklin and Schenectady counties.
On November 1, 2011, DOH received 61 Health Home applications to serve the Phase I counties and 12 provider-led applicants were conditionally approved as Phase I Medicaid Health Homes. The designated Health Homes are Community Based Organizations and Hospital Systems comprised of a provider network of partners that includes physical and behavioral health and community support partnerships. Contingent approvals for Phase II applications received on February 15, 2012 have been made. . Additional information about Phases I and II is included at the end of this article.
Provider Standards
Health Home provider qualification standards were developed to ensure that NY Health Homes meet the proposed federal Health Home model of service delivery and New York State standards. These standards were developed with input from a Provider Advisory Group made up of a variety of stakeholders including hospitals, clinics, physicians, mental health experts, chemical dependency treatment experts and housing providers. Representatives from the DOH Offices of Health Systems Management (OHSM), Office of Health Information Technology Transformation (OHITT), the AIDS Institute and the NYS OASAS and OMH also participated in the development of these standards. The standards set the groundwork for ensuring that Health Home members receive appropriate and timely access to medical, behavioral, and social services in a coordinated and integrated manner. Health Homes will be closely monitored to ensure that all standards are being met.
The Health Home standards are available online at:
http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/provider_qualification_standards.htm.
How it will Work
DOH will identify and assign Medicaid FFS members to Health Homes using a combination of clinical risk groups and an intelligent assignment algorithm that predicts for negative events (i.e., hospitalizations, nursing home, death) using prior claims and encounters. An ambulatory connectivity measure is also used to further assign risk.
This intelligent assignment model is further enhanced by a member "loyalty" matching algorithm. Medicaid members will be assigned to a specific Health Home, to the extent possible, based on existing relationships with care management, ambulatory care, emergency department and inpatient providers. The providers include both medical and behavioral health care providers. Further matching on housing providers and other factors is being explored.
Assignment Algorithm
Initial assignment to state-approved Health Home providers will be based on:
1) Provider Loyalty: Member Service Utilization (Ambulatory, Case Management, ED and Inpatient) within Health Home Provider Networks
2) Geographic Factors
Managed Care Plans (MCP) may use the DOH assignment algorithm to assign members to an appropriate Health Home.
New York State provided each Health Home and MCP with a list of Health Home eligible members, their DOH composite score, and other demographic information. Currently, the composite score is comprised of the risk score, which predicts the probability that a member will experience a negative outcome (e.g. inpatient admission, long term care, or death) in the following year and the DOH outpatient rank, which assigns a high score to members with little to no outpatient connectivity.
The goal is to assign and outreach to the highest risk (based on the predictive model) and highest cost members with the lowest primary and ambulatory care connectivity in each Health Home area.
Converting case management providers (OMH TCM, MATS, HIV COBRA TCM and CIDP) will assign their current members (both Medicaid FFS and MCP members) to a Health Home. Converting case management providers will determine which Health Home is appropriate to meet the needs of the member. Converting case management providers are responsible for obtaining the member signature on the DOH Health Home Patient Information Sharing Consent Form (DOH 5055) in order to allow data sharing. Health Homes will receive their member tracking files with these converting case management assignments already made and Health Homes and MCPs must respect these assignments to preserve the member’s existing care management relationship. The process for obtaining consent and using the member tracking files is covered in greater detail in the Member Consent and Member Assignment sections that follow.
Once members have been identified, DOH and the MCPs will move down the list using provider loyalty, PCP assignment (for MCPs), and geography (if needed) as markers for initial Health Home assignment. In the initial months, actual enrollment is expected to be lower due to several factors including the need to develop provider capacity and automation for billing and eligibility.
Health Home is a voluntary program for both FFS and MCP Medicaid recipients. The Health Home will send Medicaid FFS members a letter introducing the program and letting them know which Health Home they have been assigned to. In keeping with New York State protocols the template being used will be translated into seven languages including: Chinese, French, Haitian Creole, Italian, Korean, Russian and Spanish. Medicaid members will be given the option to select another Health Home where available or to opt out of the Health Home enrollment entirely. MCPs will assign their members to provider-led Health Homes. The MCPs will send an introduction/enrollment letter to their members
Member Consent
To allow data sharing, the member must sign a DOH Health Home Patient Information Sharing Consent Form (DOH -5055). This consent allows a member’s health information to be shared among the consented Health Home partners involved in their care and also serves as the Regional Health Information Organization (RHIO) consent form for Health Homes partnering with a RHIO. The Health Home should include a list of the core Health Home partners by corporate/agency name. Core Health Home partners are defined as the main institutional medical health and behavioral health providers and the care management agencies that are likely to serve the majority of Health Home members.
The consent should not include individual ordering or servicing practitioners, housing providers, social service support agencies, and criminal justice entities. Additional partners, such as housing, individual servicing or providing practitioners and social support agencies, etc., can be added as needed with an additional page 3 as necessary to the member's original Health Home consented partners. The additional page must include the patient's initials and the date the patient agreed to share information with the new participating partners. Please note that if a Health Home member is enrolled in a Managed Care Plan, the Managed Care Plan needs to be listed as one of the core partners on the Health Home consent form if the Health Home intends to share member information with the Plan for any out of plan or out of network benefits.
Converting OMH TCM, HIV COBRA TCM, and MATS programs should continue to work with existing members while they obtain the Health Home consent. Member disenrollment from a Health Home program requires a signed Withdrawal of Consent Form (DOH - 5058 available soon). Consent documents and detailed instructions are posted on the Health Home web site.
Member Assignment
DOH will provide each designated Health Home and MCP a monthly member tracking file of assigned members and their current demographic information. Initial assignments will be made for those Medicaid FFS members who qualify for Health Home services but currently may not have a meaningful primary care or case management connection. MCPs will assign their members to provider-led Health Homes. Starting in February, member tracking files were shared with Phase I provider-led Health Homes and MCPs via file transfer over the DOH Health Commerce System (HCS). Each Health Home and MCP must identify their HCS coordinator and maintain an active account with the HCS. Network partners will not need to access HCS for this program.
Health Home Referrals
Patient referral for Health Home services may come from a variety of sources. New York's decision to convert OMH and COBRA TCMs and MATS programs requires that individuals found eligible by local government units (LGUs) such as the OMH’s Single Point of Access (SPOA), Local Department of Social Services, NYC Human Resources Administration, NYC HIV AIDS Services Administration (HASA), health care facilities and other providers need to be referred for health home assignment on a priority basis.
In addition, Federal authority to conduct Health Homes mandates that hospitals refer individuals with chronic conditions who seek care or need treatment in a hospital emergency department to designated health home providers. Other referral sources may include the criminal justice system, court ordered clients for Assertive Outpatient Therapy (AOT), State prisons, county and city jails, Institutes for Mental Disease, managed care plans, designated Health Homes, clinics, family members, etc.
Individuals identified by the LGUs (OMH, COBRA, MATS, AOT) by the nature of their diagnosis will in the majority of cases meet Health Home criteria. For other referred clients with chronic conditions, a Referral Work Group made up of representatives from Health Homes and MCPs has recently been established to develop clinical guidelines and processes to assist providers in making referrals. For those clients in need of care management, the referring entity will first need to identify if the client receives their health care services from a managed care plan or through FFS. If the client is enrolled in managed care, the referring entity will then contact the client’s managed care plan for the Plan to make the Health Home assignment. If the client is FFS, the referring entity will call the DOH, who will make the Health Home assignment. Additional information on how make a referral and to complete the Health Home Member Tracking File for referred clients will be forthcoming.
Sharing Member Information
Each Health Home must have an approved Data Exchange Application and Agreement (DEAA) filed before member information (member tracking files) will be shared with the coordinator of each Health Home. The Health Homes must have an approved business associate subcontractor DEAA packet on file for each network partner prior to sharing member data with their network partners, e.g. with care management entities to do outreach and engagement with members. Once member consent has been obtained, member information can be shared with network partners, per the consent. In effect, each individual network partner does not need an approved subcontractor DEAA packet, however sharing of information as a Health Home with these non-DEAA-network-partners is dependent on a signed individual patient consent.
The sharing of personal health information (PHI), or other member information as it relates to Health Homes, must be sent securely in accordance with New York State and Federal laws and regulations. Guidance on the proper handling of PHI will be available on the Health Home web site. Furthermore, the DEAA must be updated as network partnerships evolve. Questions on the DEAA process can be directed to the Medicaid Privacy Officer.
Outreach & Engagement
The DEAA agreement allows for initial Medicaid member information to be shared with Health Homes to facilitate outreach and engagement by the Health Home partnership. Existing intensive case management programs, OMH TCM, HIV COBRA TCM and the MATS programs, do not need to conduct outreach and engagement for their current members. These members will convert to Health Homes immediately and may continue to receive care management services while the OMH TCM, HIV COBRA TCM and MATS programs work with them to secure a signed Health Home consent form (DOH 5055). These programs will use outreach and engagement only for new members (see figure 5). OMH TCM, HIV COBRA TCM and MATS programs should continue to bill as they currently do until the Health Home rates are approved. Once approved, providers will bill for outreach and engagement (or active case management, if applicable) retrospectively, e.g., Phase I billing for services commencing in March would be billed in April, using the new Health Home rate codes and a March 1, 2012 date of service.
The outreach and engagement Per Member per Month (PMPM) payment will be available for three months. If outreach and engagement is unsuccessful (defined as not locating the member and/or not enrolling the member), the provider may continue outreach and engagement but may not bill again for these activities until the conclusion of a three-month interval. Health Homes may begin to work with new health home members while they obtain Health Home consent and bill the outreach and engagement PMPM. Members who opt-out by signing the Health Home Opt-out Form DOH - 5059 (which will be available soon) must be disenrolled.
Members who sign a Withdrawal of Consent Form (DOH - 5058 available soon) must also be disenrolled according to the Health Home's procedures. Health Homes are responsible for obtaining the signature on the withdrawal form and for notifying DOH through the member-tracking file, for FFS members, or to MCPs, for managed care plan members. As previously stated, converting OMH TCM, HIV COBRA and MATS programs should continue to work with existing members to obtain the Health Home consent.
All Health Home outreach and engagement activities are billable under the monthly PMPM as long as active outreach is occurring each month and at least one of the five core services (excluding HIT) described on page 13 are provided in each billed month. There will be no requirement for minimum face-to-face contacts; however, there must be evidence of activities each month that support billing, including:
- Active Outreach
- Contacts (face-to-face, mail, electronic, telephone)
- Health promotion activities
- Patient assessment
- Development of a care management plan; and/or
- Active work towards achieving care management plan goals
Examples of active outreach would include direct communications with the member (face-to-face, mail, electronic or by telephone), with their family or known associates (with appropriate provisions to assure patient privacy is protected); using the claim data provided as part of the initial member tracking file to contact providers the member uses or was known to use in the past; follow-up if the member presents to another partner in the Health Home network, etc. There should be evidence that outreach efforts are progressive and are escalated as appropriate, for example, if the member does not respond to letters another strategy should be used. Examples of acceptable and unacceptable outreach activities are described in figure 6a below.
Once a member has been assigned to a care manager and is actively engaged by the program, the full active care management PMPM may be billed using the first day of that service. DOH will monitor rates for sufficiency and may collect cost reports or other financial documentation.
EXAMPLES OF ACCEPTABLE AND UNACCEPTABLE OUTREACH
Acceptable Outreach Example
- Month One (letter to member followed by phone call to member).
- Month Two (phone call to member, outreach to care delivery partners and social service partners)
- Month Three (street level outreach)
- Month One (letter to member)
- Month Two (no outreach)
- Month Three (phone call to member)
The acceptable outreach example shows active, meaningful and progressive attempts at member engagement. The unacceptable outreach shows little outreach activity and little progression of activity.
Fee-for-Service Member Workflow and Manage Care Plan Member Workflow(PDF, 3KB, 2pgs.)
Health Homes will need to assure that care managers: (1) provide care management and patient assessment, and (2) develop and initiate a care management plan. In order to support billing there must be evidence of active care plan development or active care management according to the care plan and evidence that at least one of the five (excluding HIT) core Health Home services has been delivered each month. There must be evidence of care management activities that include face-to-face meeting(s), mailings, electronic communications and telephone calls. Ongoing and progressive care management activities must demonstrate active progress in moving the care management plan forward toward achieving member goals. New York State retains the right to review Health Home records as required.
DOH will send the names of eligible members to provider-led Health Homes. MCPs will be sent the name of eligible plan members and based on their experience with the member and encounter data will assign the member to a Health Home. Health Homes will not be required to enroll members they determine are not in need of the level of care management services provided under Health Homes. Health Homes will be required to develop care management stratification criteria that will determine if a member requires continued Health Home services or allows members to be discharged from a Health Home.
Health Home Member Tracking System
A detailed explanation of the Health Home Member Tracking System is available in the Specifications Document available on the Health Home web site: http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/rate_information.htm.
Health Home Member information will be communicated between New York State, MCPs, Health Homes and downstream care management agencies through Health Home member tracking files. Health Homes and MCPs will be responsible for logging on to the Medicaid OHIP Datamart through the Health Commerce System (HCS) to receive and transmit these tracking files via file transfer. The outgoing DOH assignment file is comprised of information regarding the Health Home eligible member. Once a member is engaged in the Health Home program, the Health Home/MCP will provide DOH with specified information outlined in the Health Home Patient Tracking System Specifications Document (see figures 6a & 6b).
It is expected that Health Homes will provide the MCP with the required information about a member's care. Health Homes will be accountable to the MCP for the accuracy of the information the Health Home provides about the plan member. Health Homes will be responsible for receiving and submitting patient tracking information directly with DOH, for FFS members. Eventual amendments to State eligibility and payment systems (WMS and eMedNY) will allow providers to see a member's Health Home assignment.
Core Health Home Services
Health Home providers must have the capacity to perform core services specified by CMS. Billing under the monthly PMPM is supported as long as active outreach and engagement or active care management (including care plan development) occurs in each billed month and one of the first five core services is provided in each billed month. Note that Health Homes have 18 months to meet the sixth core service requirement, use of HIT technology. The DOH Office of Health Information Technology Transformation (OHITT) is working actively with Health Homes to identify opportunities to enhance HIT capacity.
The six core services are:
1) Comprehensive Care Management
2) Care Coordination and Health Promotion
3) Comprehensive Transitional Care
4) Patient and Family Support
5) Referral to Community and Social Support Services
6) Use of Health Information Technology to Link Services
The following tasks are examples of work carried out by the care manager/Health Home team that should be used to document claims submitted for the Health Home program.
HEALTH HOME SERVICES MINIMUM BILLING STANDARDS
Health Homes must provide at least one of the five core (exclusive of HIT) Health Homes services per month to meet minimum billing requirements. The mode of contact may include, but is not limited to: face to face meeting(s) (no minimum requirement), mailings, electronic media, telephone calls, and case conferences. Active, ongoing and progressive engagement with the client must be documented in the care management record to demonstrate active progress toward outreach and engagement, care planning and/or the client achieving their personal goals. The State retains the right to review Health Homes care records as required to assure that active services were being provided in each month for which a Medicaid payment was made for Health Home services.
| CORE HEALTH HOME SERVICES | EXAMPLES OF CORE HEALTH HOME SERVICES INTERVENTIONS/ACTIVITIES | Comprehensive Care Management | Complete a comprehensive health assessment/reassessment inclusive of medical/behavioral /rehabilitative and long term care and social service need |
|---|---|
| Complete/revise an individualized patient centered plan of care with the patient to identify patient's needs/ goals, and include family members and other social supports as appropriate. | |
| Consult with multidisciplinary team on client's care plan/needs/goals. | |
| Consult with primary care physician and/or any specialists involved in the treatment plan. | |
| Conduct client outreach and engagement activities to assess on-going emerging needs and to promote continuity of care & improved health outcomes. | |
| Prepare client crisis intervention plan. | |
| Care Coordination & Health Promotion | Coordinate with service providers and health plans as appropriate to secure necessary care, share crisis intervention (provider) and emergency info. |
| Link/refer client to needed services to support care plan/treatment goals, including medical/ behavioral health care; patient education, and self help/recovery and self management. | |
| Conduct case reviews with interdisciplinary team to monitor/evaluate client status/service needs. | |
| Advocate for services and assist with scheduling of needed services. | |
| Coordinate with treating clinicians to assure that services are provided and to assure changes in treatment or medical conditions are addressed. | |
| Monitor/support/accompany the client to scheduled medical appointments. | |
| Crisis intervention, revise care plan/goals as required. | |
| Comprehensive Transitional Care | |
| Follow up with hospitals/ER upon notification of a client's admission and/or discharge to/from an ER, hospital/residential/rehabilitative setting. | |
| Facilitate discharge planning from an ER, hospital/residential/rehabilitative setting to ensure a safe transition/discharge that ensures care needs are in place. | |
| Notify/consult with treating clinicians, schedule follow up appointments, and assist with medication reconciliation. | |
| Link client with community supports to ensure that needed services are provided. | |
| Follow-up post discharge with client/family to ensure client care plan needs/goals are met. | |
| Patient & Family Support | |
| Develop/review/revise the individual's plan of care with the client/family to ensure that the plan reflects individual's preferences, education and support for self management. | |
| Consult with client/family/caretaker on advanced directives and educate on client rights and health care issues, as needed. | |
| Meet with client and family, inviting any other providers to facilitate needed interpretation services. | |
| Refer client/family to peer supports, support groups, social services, entitlement programs as needed. | |
| Referral to Community &; Social Support Services | Collaborate/coordinate with community base providers to support effective utilization of services based on client/family need. |
For additional information regarding Health Home services, please refer to the provider standards at:
http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/provider_qualification_standards.htm.
Care Management Metrics
Care management metrics are integral to evaluate the care provided by each Health Home. Care management metrics will be broken into two sections: process metrics and quality metrics. The process metrics will be collected to assess the level of care management services provided and the degree to which five of the six core Health Home services are delivered. For managed care members, the servicing Health Home will send individual member metric information to DOH through the MCP. For Medicaid FFS members, the provider-led Health Homes will report metric information directly to DOH.
DOH has set a goal to utilize a uniform platform that will satisfy MCPs, Health Homes and DOH data collection and reporting requirements. DOH is evaluating the Case Management Annual Reporting Tool (CMART), currently used by MCPs, to report member data. Use of this tool will standardize the data collected for managed care members and Medicaid FFS members and streamline the reporting for provider-led Health Homes.
Care management metrics will be reported to DOH documenting the performance of these five core services, and to support billing claims. New York State expects that Health Home providers will strive to incorporate all of the core services into their program, with the exception of Health Information Technology (HIT). Health Home providers will be allowed eighteen (18) months from program implementation to meet the HIT final core service. The Care Coordination and Health Promotion core service is anticipated to be the most widely used core service for the outreach and engagement of members. See the Health Home web site at: http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/nys_implementation.htm.
Quality Metrics
Guidance from CMS is expected in the summer of 2012 for seven Health Home core quality metrics. New York State outcome metrics are included in the SPA. Initially, quality metrics will be derived from encounter and claim data. Please see the Health Home web site at:
http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/docs/chronic_conditons_spa_11-56_phase.pdf.
BILLING INFORMATION
Provider Enrollment
Designated provider-led Health Homes that are not enrolled in Medicaid must first obtain an NPI and then enroll in New York Medicaid as a provider to enable billing to eMedNY. Designated provider-led Health Homes already enrolled in Medicaid that do not have the Category of Service (COS) 0265 (Case Management) must apply to add this COS for Health Home services. Designated provider-led Health Homes (and targeted case management agencies that will bill directly for legacy slots) that already have COS 0265 must update their enrollment application to include the provision of Health Home services.
A guide to Health Home Provider Enrollment is posted on the Health Home web site.
Health Home Rate Code Definitions
Converting Legacy Slots
1851: Health Home/OMH TCM
1852: Health Home Outreach /OMH TCM
1880: Health Home/AIDS/HIV Case Management
1881: Health Home Outreach/ AIDS/HIV Case Management
1882: Health Home/ MATS
1883: Health Home Outreach/MATS
1885: Health Home/CIDP Case Management
New Health Home Slots
1386: Health Home Services (Plans and FFS)
1387: Health Home Outreach (Plans and FFS)
Claim Submission
MCPs and provider-led Health Homes will be notified by the state's fiscal agent, Computer Sciences Corporation (CSC), through an automatically generated rate letter that new Health Home rates (see figure 7a) have been added to their rate file. Health Home billing should not occur until a provider receives this rate letter.
Claims can only be submitted once per month and must be dated the first of the month for assigned members. Claims are submitted electronically using the 837-I format institutional claim type. Guidance for converting case management (e.g. OMH TCM and HIV COBRA) programs is under development. Converting case management providers should continue to bill as they do now. Once converting case management providers transition to the new Health Home rates, they will use the new Health Home rate codes for billing for care management services (see figure 7a).
Rate Sharing
Managed Care Plans are paid for Health Home services outside of regional premiums using a monthly care management fee paid under the Health Home rate code. The plan must bill eMedNY for Health Home payments using the rate codes 1386 and 1387. Plans may retain a portion of this payment for administrative services, as negotiated in individual contracts between the Plan and the Health Home. Plans need to contract with provider-led Health Homes to assign their plan members to Health Homes as appropriate.
Plan payments should be shared commensurate with the Health Home services being delivered. Health Homes receive payments from the Plans and then distribute payments to network partners comparable to relative effort. Payments downstream to care management agencies from provider-led Health Homes also must be shared proportionally with delivered services.
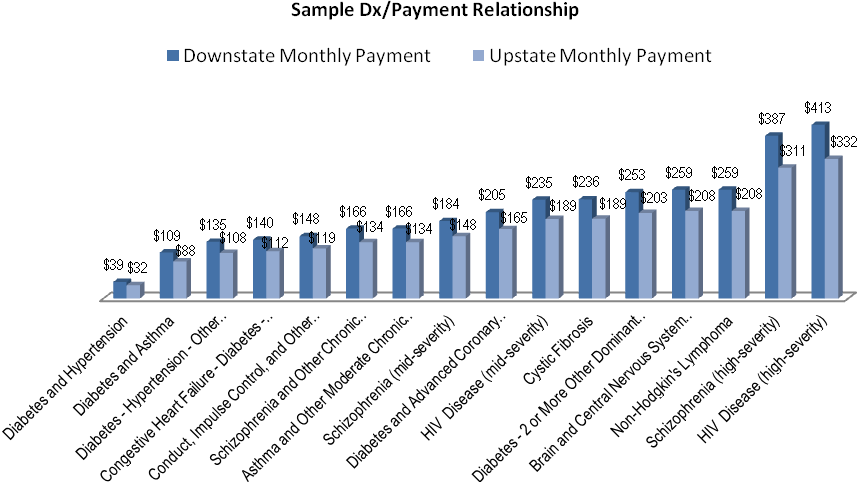
Rate Information & Determination
The Health Home care management rates were calculated using three main variables: caseload variation (scaled from 12:1 at highest intensity to 140:1 at lowest intensity), case management cost and patient specific acuity. Caseload variation (from 12:1 to 140:1) was derived from a combination of sources including existing targeted case management programs, chronic illness demonstration programs and other demonstrations of chronic illness management from other states (e.g. MA and WA).Case management cost was derived from cost data reported to DOH from existing programs. Patient specific acuity factors were obtained by using 3M Clinical Risk Group software. These raw acuity scores were then adjusted for a predicted functional status factor (e.g. mental health, substance abuse and higher medical acuity groups were "up-weighted") until functional status data becomes available to more accurately adjust clinical acuity. Patient specific adjusted acuity scores were utilized to "predict" case management need based on a regression formula.
Health Home rates by regions are available at:
http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/rate_information.htm.
Billing for Health Home Services
Health Home services for new Health Home members can be billed under one of two Health Home rate codes: outreach and engagement or active care management. The outreach and engagement for Medicaid FFS and managed care members will be paid at a reduced percentage (80%) of the active care management PMPM. Providers should submit one claim Per Member per Month using the first of the month as the date of service, regardless of when during the month the service was provided. Monthly payments to MCPs (for MCP members), provider-led Health Homes (Medicaid FFS members) and converting case management programs (both MC and Medicaid FFS members) will all be made through eMedNY. Determination of whether to bill the outreach and engagement or the active care management rate for assigned Health Home eligible members should be based on the information reported to the Health Home Patient Tracking System. While the consent to share personal health information (described on page 6 under member consent) is not required for individuals to begin to receive Health Home care management services or to bill for these services, it is expected that consent will be obtained in a timely manner to ensure the integration of services needed to improve outcomes.
Special Rules for Converting Case Management Billing
Legacy/Existing Slot BillingFor the first year, existing case management programs converting to Health Home partners (OMH TCMs, HIV COBRA TCM and MATS programs) will bill eMedNY directly for existing (or "legacy") slots using the specific Health Home rate codes (see figure 7a).These legacy rates have been calculated by OMH and will pay an amount equivalent to the average historical rate. Converted OMH TCM, COBRA, and MATS programs receive 100% of the Per Member per Month (PMPM) for outreach and engagement and active case management for existing/legacy slots. In year two, converting TCM providers will bill eMedNY directly for "legacy" slots using a blended rate averaging historical rate and new health home rate. (codes for these two rates: blended Outreach and Engagement – O/E – and active case management "legacy" slots will be determined at a later date.)
For the first year, Chronic Illness Demonstration Projects (CIDP) will bill eMedNY directly for CIDP members as of termination of contract on March 29, 2012. Any new members enrolled will be billed at the Health Home rate by the Health Home. In the second year, the legacy CIDP members also will be billed by the Health Home at the Health Home rate.
Chronic Illness Demonstration Program (CIDP)
- CIDP contracts ended on March 29, 2012.
- By March 29 all CIDPs must be in a Health Home partnership to continue to provide care management services.
- For one year as of the effective date of appropriate SPA, CIDPs, converting to Health Homes, may bill eMedNY directly for existing CIDP members converting to Health Homes with the new CIDP/Health Home rate code.
- New Health Home members assigned to a CIDP for Care Management will be billed for by the Provider-led Health Home or Managed Care Organization.
At a date yet to be determined, claims back to January 1, 2012, will be automatically reprocessed for Phase I county OMH TCM and HIV COBRA providers, to adjust to the new Health Home rate codes and rates. Providers may wish to revisit their billing from January 1, 2012 onward to ensure they have billed accurately. More specific guidance on retroactive billing is being developed.
New Health Home Slot Billing
These converting case management programs will also bill eMedNY for any new Health Home slots, using the Health Home rate codes. They will receive 80% of the Health Home active care management PMPM, for members assigned to new Health Home slots until that new member is in active case management. New Health Home slots will bill at 100% of the PMPM for active case management.
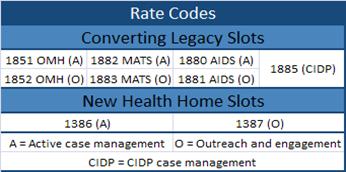
In summary, existing targeted case management programs bill eMedNY directly for both FFS and MCP members, using their specific rate codes for their legacy slots and the Health Home rate codes for new Health Home slots. Existing targeted case management programs bill directly to ensure they are accountable for managing the number of existing or "legacy slots", which have different billing rules. (See the rate codes listed in figure 7b).
Rate Adjustment
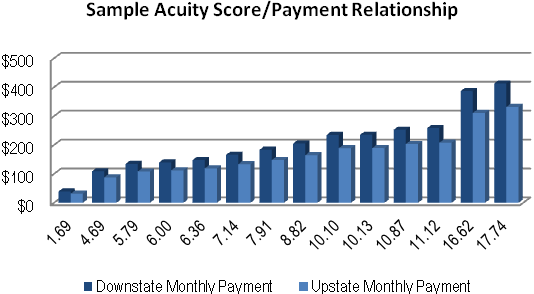
Payment rates will be based on region and average case mix (e.g. clinical acuity) as discussed previously, and initially will change monthly by Health Home and Managed Care Plan (see figures 8a & 8b). Rates will eventually be calculated and paid at a member specific level directly by eMedNY and then monthly provider and plan specific rate calculations will not be necessary.
When functional status data becomes available, rates will be adjusted based on member functional status (e.g. impairment in physical and/or behavioral functioning, housing status, and self management abilities). New York State is evaluating the Functional Assessment of Cancer Therapy for General Populations (FACT-GP) tool, with some additional questions.
A draft version of the assessment tool is available on the Health Home web site at:
http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/nys_implementation.htm.
Administration of the tool would be face-to-face and will be required at initial activation (enrollment), annually, and at disenrollment. Assessment outcomes will be reported to DOH by MCPs and the provider-led Health Homes.
Expansion Timeline
In November 2011, there were a total of 165 Letters of Intent or LOIs submitted from parties interested in being designated Health Homes. Health Homes are being expanded statewide through phases. Health Homes in Phase I counties have already been designated. A total of 37 unique applications were submitted on February 15 for evaluation for Phase II implementation in the following counties: Dutchess, Erie, Manhattan, Monroe, Orange, Putnam, Queens, Richmond (Staten Island), Rockland, Suffolk, Sullivan, Ulster and Westchester and Health Homes have been contingently designated.
There are 39 counties included in Phase III: Albany, Alleghany, Broome, Cattaraugus, Cayuga, Chautauqua, Chemung, Chenango, Columbia, Cortland, Delaware, Fulton, Genesee, Greene, Herkimer, Jefferson, Lewis, Livingston, Madison, Montgomery, Niagara, Ontario, Oneida, Onondaga, Orleans, Oswego, Otsego, Rensselaer, Saratoga, Schoharie, Schuyler, Seneca, St. Lawrence, Steuben, Tioga, Tompkins, Wayne, Wyoming and Yates. Implementation is anticipated to begin in July 2012.
Discontinuing Services
Any Health Home that wants to discontinue services is required to provide DOH with a minimum of six months notice. Services may not be discontinued without a DOH approved closure/services cessation plan, which includes proper procedures for clinically appropriate patient transition.
Additional Information
Sign up for e-mail alerts to keep updated on the Health Home program. Enroll online at: http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/listserv.htm.
General Health Home program information is posted on the Health Home web site at: http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/index.htm.
If you have any questions regarding Health Homes you may submit them electronically via e-mail to: hh2011@health.state.ny.us.
For more general Health Home direction please contact the Medicaid Call Center at (800) 541-2831. Providers with billing questions should contact the eMedNY Call Center at (800) 343-9000.