Ambulatory Health Care Facility (AHCF) Cost Report
- Attachment also available in Portable Document Format (PDF)
New York State Department of Health
Office of Health Insurance Programs
Division of Finance & Rate Setting
Bureau of Mental Hygiene Services, Hospital & Clinic Rate Setting (BMHRHC)
November 28, 2017
Agenda
- Centers for Medicare and Medicaid Services (CMS) data requirements & concerns
- Who is required to file an AHCF and why is it required?
- Calendar Year vs Fiscal Year reporting
- Selection of Services – Configuration Screen
- Total Cost Requirement
- DOH Rate Codes used in the UPL
- 2016 AHCF Cost Report Changes
- Visits & Procedures Clarification and Edits
- Timing for Cost Report Software & Completion
- Accessing the software on the Health Commerce System (HCS)
- Cost Report Document Filing Requirements
- APG website
- Contacts
Centers for Medicare and Medicaid Services (CMS) Data Requirements & Concerns
- Upper Payment Limit (UPL) Demonstration: A demonstration to CMS that what Medicaid pays is at or below what Medicare would pay.
- Method for clinic is cost compared to payment
- A review is completed by facility HOWEVER the final result is a statewide comparison of total costs vs total payments within the following groups: Voluntary, State Public & Non–State Public
- "UPL Room" = Costs – Payments (Costs must be greater than payments)
- New York State attempted to complete the 2012 UPL for freestanding clinics based on calendar year 2010 data.
- During the process of analyzing data, concerns arose about the accuracy of cost report and claims data submitted by providers
- CMS concluded that there was no UPL room after the inclusion of all APG State Plan Amendments (SPAs) for 2012 through 2017 and 12 SPAs were required to be withdrawn.
- CMS and the Department agreed that the Department would develop a Corrective Action Plan for improving the accuracy of the data going forward. (SPA 16–0002)
- The next full UPL calculation is required to use 2017 data for 2018 calendar year.
- If the Department can prove integrity of the data, a UPL may be able to be submitted earlier allowing the submission of SPAs.
- Data Issues
- Non–submission of cost reports
- CMS will no longer allow proxy costs be developed for a provider that did not submit their cost report. A provider’s payments will be included in the UPL calculation with $0 costs reducing "room".
- 100% compliance with cost report submission is needed
- Medicaid FFS claim counts in eMedNY not in agreement with Medicaid FFS Visits in the AHCF
- Medicaid FFS claim counts in eMedNY greater than Total Visits in the AHCF
- The Medicaid charge per visit should not equal the Medicaid rate. Facilities should have a uniform charge structure applied to all payors.
- Non–submission of cost reports
Who is required to file an AHCF?
- Part 86–4.3(a): "...treatment centers and/or diagnostic centers shall submit to the New York State Department of Health a certified Ambulatory Health Care Facility–1 form (AHCF–1)...."
- Part 86–4.3(b) states, "Each facility shall complete and file with the department and/or its agent annual financial and statistical report forms supplied by the department.... Each facility shall also file a copy of the audited financial statements..."
- Part 86–4.4 Certification of Reports
- Section (a): Certified by Independent CPA
- Section (b): CPA certification shall not apply to facilities operated by units of the NYS government whose total operating costs are less than $100,000
- Section (c): Certified by the operator of a proprietary facility, an officer of a voluntary facility or public official responsible for the operation of a public facility
- Part 86–4.4 Certification of Reports
- Failure to file: Part 86–4.3(h) states that the Commissioner shall reduce the facility’s current rate paid by state governmental agencies by 2%.
Why is the AHCF Cost Report required?
- Upper Payment Limit (UPL) calculation for CMS
- Capital component for APG rates or any rate component where cost data may be used
- FQHC Rate (appeals)
- Distribution calculations
- Safety Net Clinic distribution (Article 28 clinics providing comprehensive services as their principal mission)
- United Cerebral Palsy distribution (Article 28 clinics providing services to the developmentally disabled as their principal mission)
- Fiscal analysis
- State Budget proposals
- Cost vs Payment comparisons
- Certificate of Need application
- In any data analysis review you want your provider counted
AHCF Calendar Year vs Fiscal Year Reporting
➢ Calendar Year submission or Fiscal Year?
- Providers can elect to use a 12/31 or 6/30 year–end for cost reporting
- Election is made at the time of the initial cost report submission
➢ Historical Information
- In 1997, Section 2807 was amended for reporting requirements.
- Providers were contacted to make an election by 9/2/1997 for their cost reporting period.
- Once election was made, providers could not change it.
- Providers that opened after 1997 elect Calendar or Fiscal Year at the time of their first full year cost report submission.
Selection of Services – Configuration Screen
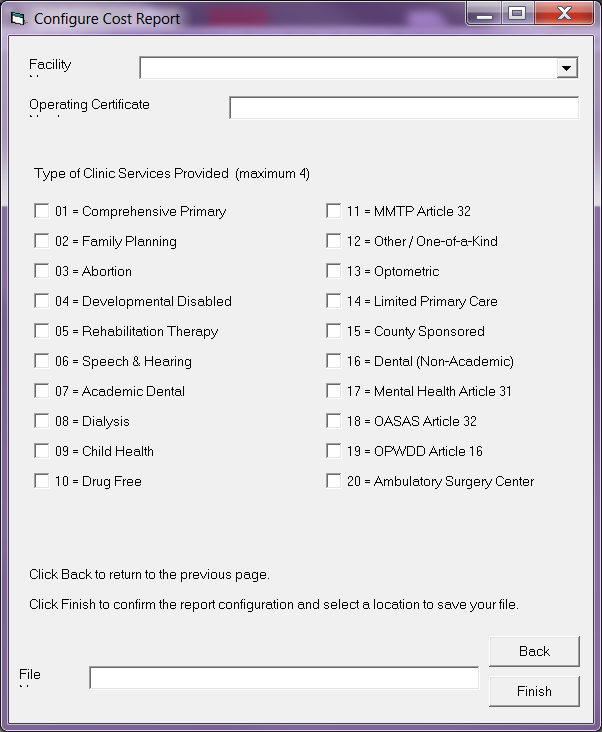
- Select appropriate services (the software will then provide the appropriate screens for each service).
- Services represents the different clinic environments.
- What is the clinic´s principal mission? (Part 86–4.13)
- The AHCF reports "Total Provider" costs.
- Dually/Jointly licensed providers:
- Report Article 28 (DOH Primary Care), Article 16 (OPWDD), Article 31 (OMH) & Article 32, Including OTP/MMTP (OASAS) separately.
- By selecting these services on the configuration screen, the software will provide the ability to separate the Article 28 costs from the Article 16, 31 & 32 costs.
- If selection is not labeled "Article 16, Article 31 & Article 32" the selections are to report the Article 28 primary care costs and statistics for your provider.
- Article 28 FQHC locations are Comprehensive.
Total Cost Requirement on the AHCF Cost Report
➢ Total facility clinic costs are to be reported
- Requirement to report entire agency clinic costs
- Overall look at a provider
- Percentage of business is primary care
- Capital rates historically developed on total provider clinic capital costs
- SPA 15–0059 submitted to use Article 28 costs only
- APG SPA and was not required to be withdrawn by CMS
- Delay of APG capital rate updates beginning 1/1/2016
- Federally Qualified Health Centers (FQHC)
- OMH and OASAS use the DOH calculated FQHC rate
- CMS Inquiry: Ability to separate FQHC and non–FQHC locations (non–FQHC should be included in the UPL calculation)
- 2017 AHCF: Further guidance to be provided at a later time for "FQHC Comprehensive" & "Non–FQHC Comprehensive"
- Separation of FQHC Comprehensive & Other Principal Mission Costs
DOH Rate Codes used in the UPL
➢ Only DOH Displayed – Many Mental Hygiene Rate Codes Used Also
| Rate Code |
Rate Code Description | Rate Code |
Rate Code Description |
|---|---|---|---|
| 1228 | COMPREHENSIVE WHEELCHAIR EVALUATION AND MANAGEMENT | 1498 | APG GEN CLINIC MR/DD/TBI (EDIT EXEMPT) |
| 1381 | SBHC FLU SEASONAL VACCINES – ADMINISTRATION ONLY | 1604 | MOMS HEALTH SUPPORTIVE SERVICE |
| 1382 | SBHC FLU H1N1 VACCINE – ADMINISTRATION ONLY | 1610 | INDIAN HEALTH SERVICES |
| 1383 | SBHC PNEUMO, VACCINES – ADMINISTRATION ONLY | 1850 | DAY HEALTH CARE SERVICE (HIV) |
| 1407 | D & T CLINIC APG | 3257 | INDIVID BRIEF PSYCHOTHERAPY 20–30 MIN WITH PATIENT |
| 1408 | D & T AMBULATORY SURGERY APG | 3258 | INDIVID COMPR PSYCHOTHERAPY 45–50 MIN WITH PATIENT |
| 1422 | DTC GENERAL CLINIC– APG EPISODE BASE RATE | 3259 | FAMILY PSYCHOTHERAPY WITH OR W/O PATIENT PRESENT |
| 1425 | DTC CLINIC MR/DD/TBI – APG EPISODE BASE RATE | 4257 | INDIVID BRIEF PSYCHOTHERAPY 20–30 MIN WITH PATIENT |
| 1428 | D&T CLINIC APG – DENTAL CLINIC | 4258 | INDIVID COMPR PSYCHOTHERAPY 45–50 MIN WITH PATIENT |
| 1435 | D&T CLINIC APG – GEN CLINIC (MR/DD/TBI PATIENT) | 4259 | FAMILY PSYCHOTHERAPY WITH OR W/O PATIENT PRESENT |
| 1438 | D&T CLINIC APG – RENAL CLINIC | 5246 | COLLABORATIVE CARE MONTHLY CASE PAYMENT – YEAR 1 |
| 1447 | D & T CLINIC APG – SCHOOL BASED HEALTH CENTER | 5248 | COLLABORATIVE CARE RETAINAGE – YEAR 1 |
| 1453 | D&T CLINIC APG – SCHOOL BASED HEALTH (EPISODE) | 5313 | TB/DIRECTLY OBSERVED THERAPY–DNST LEVEL 2 |
| 1456 | D&T CLINIC APG – RENAL (EPISODE) | 5318 | TB/DIRECTLY OBSERVED THERAPY–UPST LEVEL 2 |
| 1459 | D&T CLINIC APG – DENTAL CLINIC (EPISODE) | 5388 | PRESCHOOL SUPPORTIVE HEALTH PROGRAM – IEP |
2016 AHCF Cost Report Changes
➢ Requirements:
- Develop a visit screen that will accommodate all services
- Calculate an appropriate capital rate
- Provide appropriate data for the UPL
➢ 2016 Exhibit Changes:
- Exhibit IC – Statistics by Patient Care
- Expanded detailing patient care services between capital and non–capital related
- Exhibit ID – Statistics & Revenue by Payer
- Changes on Exhibit IC did not require changes on Exhibit Id
- Revised to collect data for distribution payments
- Exhibit IIIA – Costs by Service
- Eliminated ability to remove School Based Health Care Center´s costs from Total Costs
- Adjusted formula for APG capital to use appropriate visits from Exhibit IC
- Exhibit IIIF – Statement of Revenue
- Revised to collect data for distribution payments
2016 AHCF Cost Report Changes – Exhibit IC
➢ Visits, Exhibit IC – Statistics by Patient Care
- Revised headers
- Moved School Based Health Centers from Section 2 to Section 3
- Receives a full APG payment + Capital
- Enhanced Section 3
- Row 025 used for APG Capital Rate development
- Does not include services that do not receive a capital payment
- Added "Other Visits By Patient Care"
- Payments do not receive a capital payment but are included in the UPL
- Moved OTP (formerly MMTP to a section within Section 3) [Configuration screen MMTP Article 32]
- Provided a line for OASAS Medical Visits [Configuration screen OASAS Article 32]
- New row 052 for Total Visits including OASAS
- Row 052 should = row 960 on Exhibit ID (Visits by Payer) [Fatal Edit]
- Section 4, Procedures – Added a row for Ambulatory Surgery
| Exhibit I – General & Statistical Information C. Statistics Name of Service |
|||
|---|---|---|---|
| ➢ Visits, Exhibit IC – Statistics by Patient Care (Sections 1 & 2) | |||
| Revised Text | Facilities should report ambulatory surgery, abortions, sterilization and dialysis as procedures in number 4 below. The threshold visits should not contain any visits related to these procedures. | ||
| 1. Total No. of Users | 001 | ||
| 2. Visit Statistics | |||
| No change to Edit: line 002 = line 025 | a. Total number of threshold visits | 002 | EDIT w Ln 025 |
| b. Off site visits | |||
| Home | 003 | ||
| Hospital | 004 | ||
| Nursing Home | 005 | ||
| Move row to threshold visits | Move (1) | ||
| Other: | |||
| 007 | |||
| 008 | |||
| 009 | |||
| Revised Header & Formula | TOTAL OFFSITE (Sum of 003 thru 005 + 007 thru 009) | 010 | Formula |
| ➢ Visits, Exhibit IC – Statistics by Patient Care (Section 3) | |||
| 3. Threshold visits by patient care cost center | |||
| Primary Medical Care | 011 | ||
| Revised Header | Dental (Including Mobile Dental Unit) | 012 | |
| Family Planning | 013 | ||
| Mental Health | |||
| Psych Social Work Group Visit (Number of Clients seen in group setting) | 037 | ||
| Psych Social Work Individual Visit (FQHC only) | 038 | ||
| Mental Health other visit | 039 | ||
| Total Mental Health (Sum of lines 038 + 039) | 014 | Formula | |
| Speech & Hearing | 015 | ||
| Physical Therapy | 016 | ||
| Occupational Therapy | 017 | ||
| Other Rehabilitation Therapies | 018 | ||
| Other Health | 019 | ||
| Added row from above | School Based Health Centers (SBHC´s) | 006 | From Above (1) |
| Move to new section and Revise Header | 020 | Move (2) | |
| Revised Header | Other Threshold Visits: | ||
| 021 | |||
| 022 | |||
| 023 | |||
| 024 | |||
| 036 | |||
| Revised header & formula | TOTAL THRESHOLD (Sum of 006 + 011 thru 019 + 021 thru 024 + 036) | 025* | Formula |
| ➢ Visits, Exhibit IC – Statistics by Patient Care (Section 3 – New) | |||
| New Section | OTHER VISITS BY PATIENT CARE | ||
| New Row | Collaborative Care (Monthly & Retainage) | 043 | New |
| New Row | FQHC Group Therapy (# of clients in group setting) | 044 | New |
| New Row | LCSW/LMSW (Clinic & SBHC) | 045 | New |
| New Row | MOMS Health Supportive Service | 046 | New |
| New Row | SBHC Vaccines (Administration Payment Only) | 047 | New |
| New Row (Header Only) | Other: | ||
| New Row | 048 | New | |
| New Row | 049 | New | |
| New Row and Formula | TOTAL VISITS (Sum of 025 + 043 thru 049) | 050 | Formula |
| Row from above w new header | Opioid Treatment Program (formerly MMTP: Article 32) | 020 | From Above (2) |
| New Row | OASAS Medical Visit (Article 32 MMTP & OP Rehab) | 051 | New |
| New Row and Formula | TOTAL VISITS INCL OASAS (Sum of 050 + 020 + 051) | 052** | EDIT w Exh ID |
| ➢ Visits, Exhibit IC – Statistics by Patient Care (Section 4) | |||
| 4. Procedures | |||
| Abortions | 031 | ||
| Sterilization | 032 | ||
| Dialysis | 033 | ||
| New row | Ambulatory Surgery | 053 | New |
| Other: | |||
| 026 | |||
| 027 | |||
| 028 | |||
| 029 | |||
| 030 | |||
| 034 | |||
| 040 | |||
| 041 | |||
| 042 | |||
| Revised Header & Formula | TOTAL PROCEDURES (Sum of 026 thru 034 + 040 thru 042 + 053) | 035*** | EDIT w Exh Id |
* Line 025 used to develop APG Capital Rate
** For Visits, Row 052 should equal Line 960 on Exhibit Id
*** For Procedures, Row 035 should equal Line 960 on Exhibit Id
2016 AHCF Cost Report Changes – Other Exhibits
➢ Exhibit ID – Visits/Revenue & Exhibit IIIF – Revenue
- Added Lines for distributions collected
- Line 78: Clinic Safety Net distribution (For eligible providers began 4/1/2016)
- Line 79: Vital Access Provider (VAP) distribution
- Line 80: Delivery System Reform Incentive Payment (DSRIP)
➢ Exhibit IIIA – Costs
- Removed ability to adjust out School Based Health Center´s costs
- Costs should be included
- 2017 AHCF will eliminate column
Visits & Procedures Clarification
➢ Threshold Visits
- According to part 86–4.9(b), a threshold visit, including all part–time clinic visits, shall occur each time a patient crosses the threshold of a facility to receive medical care without regard to the number of services provided during that visit.
- According to the Policy Guidelines Manual for Article 28 Clinics, "a qualifying threshold visit is one where the registered clinic patient has an encounter with a physician, physician assistant, nurse practitioner or licensed midwife for services that include comprehensive primary care."
- Is a visit with an RN a threshold visit?
- Even though a registered nurse (RN) is not a qualified licensed practitioner, if an RN administers chemotherapy or other infusion drugs under a physician´s order in a clinic setting (and an APG claim is to be filed to Medicaid with an infusion procedure code for the administration of the infusion drug), this encounter with an RN does qualify as a threshold visit for cost reporting purposes
- The following shall not constitute a threshold visit if the visit was solely for (86–4.9(c)):
- Ordered Ambulatory Services, Pharmacy, Respiratory Therapy, Nutrition, Recreation Therapy, Medical Social Services
➢ Procedures
- If included in Procedures, do NOT include in Visits.
- Per Part 86–4.9(a): The unit of service used to establish rates of payment shall be the threshold visit, except for dialysis, abortion, sterilization services and freestanding ambulatory surgery, for which rates of payment shall be established for each procedure.
- For reimbursement purposes, all the visits related to the procedure, regardless of the number of visits are to be considered and counted as part of one procedure. They are not billable as separate visits. [Procedure = Pre–Visit, Actual Procedure, Post–Visit]
➢ Reporting of OTP (formerly MMTP)
- Example: 5 daily visits in 1 week: Report the 5 daily visits
➢ Ordered Ambulatory Services
❖ Ordered ambulatory services are defined as specific services provided to non–registered clinic patients at the facility upon order and referral.
- If the service is billed and reimbursed as an Ordered Ambulatory Services, it should be reported as an Ordered Ambulatory Service.
- These services cannot be billed using the clinic rate.
- When a provider submits an APG claim, all ancillaries ordered by the Diagnostic and Treatment Center must be coded on the claim and must code the modifier U6 at the line level for each ancillary for which they are requesting payment.
- Modifier U6 will provide payment to the clinic for the ancillary service. If the service is contracted and not provided at the clinic, the U6 modifier is not included and APG payment is reduced.
- Statistics for ordered ambulatory services must be maintained by each facility as a matter of record:
- Visits are not included as threshold visits.
- Costs associated with these services must be identified and removed from operating costs.
- Visits and Revenue are reported on Exhibit 1D
Visit & Procedure Data Edits
➢ Exhibit IC: Line 002 = Line 025
2. Visit Statistics a. Total number of threshold visits 002 3. Threshold visits by patient care cost center TOTAL THRESHOLD (Sum of 006 + 011 thru 019 + 021 thru 024 + 036) 025
➢ Exhibit IC and Exhibit ID:
- Visit Edit: Exhibit IC Line 052 = Exhibit ID Line 960
- Exhibit IC
TOTAL VISITS INCL OASAS (Sum of 050 + 020 + 051) 052 - Exhibit ID – Visits Column
TOTAL SOURCE OF PAYMENT 960
Note: AHCF FFS Medicaid reported visits should = eMedNY claims used in the UPL
- Exhibit IC
- Procedures Edit: Exhibit IC Line 035 = Exhibit ID Line 960
- Exhibit IC
TOTAL PROCEDURES (Sum of 026 thru 034 + 040 thru 042 + 053) 052 - Exhibit ID – Procedures Column
TOTAL SOURCE OF PAYMENT 960
Note: AHCF FFS Medicaid reported procedures should = eMedNY claims used in the UPL
- Exhibit IC
Timing for Cost Report Software & Completion
➢ Starting with 2015 Survey
- If the Department can provide good data to CMS, there is a possibility of completing a UPL earlier than 2018.
- Survey distributed using same design as Minimum Wage
- Will be for Exhibit IC and Exhibit ID
- Not recasting any distributions or rates developed using the 2015 survey data.
- ONLY USED FOR THIS PURPOSE.
- Exhibit IIIA for Costs should not need to be resubmitted
- All costs should already have been reported.
- School Based Health Centers costs were to be included in total and adjusted out providing the added costs needed.
➢ 2016 Software release and completion
- Software in development
- Providers receive 60 days from release of the software to complete
- The Department will take into consideration the upcoming holidays
- Can begin developing data based on layout of the screens provided
Accessing the AHCF Software on the HCS
➢ In order to retrieve the software, providers must have an HCS account
➢ The Health Commerce System (HCS) is a communication tool
- Email blasts
- Keep email address current
- Provider responsibility
- Email blast separate from public website Electronic Mailing List
- Removal of employee when leave provider´s employment
- Secure network for posting provider specific information
- AHCF Cost Report software download and upload
- Rate Sheets (APG capital & FQHC)
- Distribution calculations
➢ An HCS account is required to access the software
- BMHRHC cannot establish an HCS account
- Accounts are person specific not provider specific
- Providers that have an HCS coordinator:
- The coordinator can set up an HCS account for an individual at their facility
- For new providers as well as existing providers:
- If no coordinator at the facility, contact the NYS Department of Health Commerce Accounts Management Unit Support (CAMU) at 1–866–529–1890
- HCS accounts gets you access to the HCS but not access to the AHCF Cost Report Application on the HCS
- Must complete an Access Application Form
➢ Access Application Form
- HCS homepage
- Click "Applications" from the Title Bar at the top of the screen
- Find "D&TC Cost Report" application by clicking "D" at the top "Browse by"
- Click "i" in the Profile column of "D&TC Cost Report" application
- Scroll down to find "DFRS D&TC Access Application Form" in "Access Information"
- Print out and complete the Form
➢ The individual user must complete Section I of the form and an HCS coordinator must complete Section II.
➢ Signatures for the user and the HCS coordinator must be notarized.
➢ Email the completed Form to dtcffsunit@health.ny.gov
|top of section| |top of page|Cost Report Document Filing Requirements
- What should be submitted?
- Electronic AHCF using the HCS
- CEO Certification
- CPA Certification
- Audited Financial Statements (AFS)
❖ CEO and CPA certifications are the first pages of AHCF Cost Report. Providers must print out these certification pages and complete. Alternative certification forms will not be accepted by NYS DOH.
❖ A complete submission includes not only the electronic AHCF submission but also the CEO & CPA certification and AFS. Without these required documents, the reporting requirement has not been met.
➢ When should they be submitted?
- The Certifications and AFS should be filed within 5 business days following the electronic submission of AHCF Cost Report.
➢ How should they be submitted?
- Certifications and AFS should be submitted by email to dtcffsunit@health.ny.gov
- Subject Line: 2016 AHCF Documentation_Name of Your Facility
- No longer requiring hardcopy submissions
- Naming Convention:
- Opcert#_CEO_2016.pdf
- Opcert#_CPA_2016.pdf
- Opcert#_AFS_2016.pdf
APG Website
➢ APGs (Ambulatory Patient Groups):
- Contact information (including O Agencies)
- Rates – both APG & FQHC
- Method of communication to providers
- APG Electronic Mailing List for website updates
https://www.health.ny.gov/health_care/medicaid/rates/apg/
|top of section| |top of page|Contacts
➢ Questions regarding completing the AHCF Cost Report:
- Email dtcffsunit@health.ny.gov
- Please identify yourself in the email:
- Your name
- Name of facility
- Facility Operating Certificate Number
- Telephone number
- Please identify yourself in the email:
➢ Should you experience any problems with the electronic submission, a toll–free HCS helpline is available at 1–866–529–1890.
Questions:
D&TC Fee–for–Service Unit:
A Q&A will be provided based on questions received from the webinar
|top of section| |top of page|