NY Changes in Ambulatory Patient Group (APG) Reimbursement
Changes in APG Reimbursement
- Presentation also available in Portable Document Format (PDF)
Effective January 1, 2010
Overview of APG Payment Changes for January 1, 2010
- Visit–based rate codes will be eliminated (except for ambulatory surgery services).
- Updated APG weights and revised base rates
- New enhanced hospital MR/DD/TBI base rate paying a 20% bump for patients with RE code 95 or RE code 81.
- Pharmacotherapy and chemotherapy classifications will expand from 5 to 6 levels (however, chemo drugs will continue to be carved out).
- A new "premium" drug APG was created comprising both pharmacotherapy and chemotherapy drugs. This APG, and its associated drugs, will be carved out of APGs and will be billable as ordered ambulatory.
- APGs will recognize units of service for some PT, OT, and nutrition procedure codes, as well as crisis management, patient education (including services rendered by CDEs & CAEs), and health/behavioral assessments.
- Medical visits will not package with significant ancillaries (e.g., MRIs), dental procedures, PT, OT, speech, and counseling services and will instead pay at the line level. All significant ancillaries will become "if stand alone, do not pay" procedures.
- Multiple same APG discounting (rather than consolidation) which currently applies to most dental services will be expanded to include dental sealants, OT, PT, speech, and most mental hygiene APGs.
- Genetic testing procedures will be carved out and paid using the ordered ambulatory services fee schedule.
- The no–blend APG list will be expanded to include cardiac rehabilitation (which comes off the never pay APG list in January), developmental testing, crisis management, medication administration, and medication management.
- The following new APGs were created:
- Physical Therapy – Group
- Speech Therapy – Group
- Crisis Intervention
- Medication Administration and Observation (primarily developed for MMTP, which will not move to APGs in January 2010)
- Mental Hygiene Assessment
- Mental Hygiene Screening and Brief Assessment
- Some procedures (e.g., provision of vision aids) will be paid based on procedure–specific weights rather than APG–specific weights.
- Capital add–on rules will change so that an add–on is paid for nearly all types of visits including those consisting entirely of ancillaries and dental examinations (currently, a capital add–on is not paid with ancillary only visits).
- However, a capital add–on will not be paid for visits consisting solely of medication administration, PT–group, speech–group, cardiac rehabilitation, immunization, and patient education.
Additional Major Program & Policy Changes
- Statewide Patient–Centered Medical Home Incentive Program (implementation on Federal approval).
- Physician Carve Out policy effective for OPDs (scheduled for February 1, 2010 implementation).
New Episode–Based Payment Will Replace Visit–Based Payment
- Beginning January 1, 2010 OPDs and SBHCs must use new episode–based rate codes (1432 and 1450) for Medicaid patients. Providers may continue to use visit based rate codes for dual eligible recipients.
- Under episode pricing, the APG Grouper Pricer will view all procedures coded on a claim as being part of the same visit, regardless of the coded dates of service.
- Providers will no longer have to "reassign" the actual date of service for related ancillaries to the same date of service as the initial medical visit or procedure.
- An episode is defined as all medical visits and/or significant procedures that occur on a single date of service, as well as any associated ancillaries that occurred on or after the date of the medical visit and/or significant procedure.
APG Billing Rate Codes In Effect for January 2010
| Service/Setting |
Facility Type |
Rate Codes ‐ Effective January 1, 2010 |
| Visit |
Episode |
| Outpatient Department * |
Hospital |
1400 |
1432 |
| OPD ‐ MR/DD/TBI |
Hospital |
NA |
1489 |
| Ambulatory Surgery |
Hospital |
1401 |
NA |
| Emergency Room |
Hospital |
NA |
1402 |
| School Based Health * |
Hospital |
1444 |
1450 |
|
| General Clinic * |
DTC ** |
1407 |
1422 |
| General Clinic ‐ MR/DD/TBI * |
DTC |
1435 |
1425 |
| Dental School * |
DTC |
1428 |
1459 |
| Renal Clinic * |
DTC |
1438 |
1456 |
| School Based Health * |
DTC |
1447 |
1453 |
| Free‐standing Surgery Center |
DTC |
1408 |
NA |
Notes:
* Rate codes being eliminated will continue to be active through December 31, 2009.
** DTC Rate Codes will be effective September 1, 2009 (pending CMS approval), except codes 1453, 1456, and 1459 which are effective 10/1/2009.
Drug and Chemo Reclassifications for January 2010
| CPT |
Description |
Current APGs |
New 2010 APGs |
Description |
|
CPT |
Description |
Current APGs |
New 2010 APGs |
Description |
| J0130 |
Abciximab injection |
438 |
435 |
Class I Pharmacotherapy |
|
S0156 |
Exemestane, 25 mg |
435 |
430 |
Class I Chemotherapy Drugs |
| J1245 |
Dipyridamole injection |
435 |
436 |
Class II Pharmacotherapy |
S0187 |
Tamoxifen 10 mg |
435 |
430 |
Class I Chemotherapy Drugs |
| J1562 |
Vivaglobin, inj |
435 |
436 |
Class II Pharmacotherapy |
J9380 |
Vincristine sulfate 5 MG inj |
430 |
431 |
Class II Chemotherapy Drugs |
| J2185 |
Meropenem |
435 |
436 |
Class II Pharmacotherapy |
J9291 |
Mitomycin 40 MG inj |
432 |
431 |
Class II Chemotherapy Drugs |
| J0210 |
Methyldopate hcl injection |
435 |
436 |
Class II Pharmacotherapy |
J1327 |
Eptifibatide injection |
431 |
432 |
Class III Chemotherapy Drugs |
| J2248 |
Micafungin sodium injection |
438 |
436 |
Class II Pharmacotherapy |
J8520 |
Capecitabine, oral, 150 mg |
430 |
432 |
Class III Chemotherapy Drugs |
| 79005 |
Nuclear rx, oral admin |
436 |
437 |
Class III Pharmacotherapy |
J9120 |
Dactinomycin injection |
430 |
433 |
Class IV Chemotherapy Drugs |
| Q4081 |
Epoetin alfa, 100 units ESRD |
436 |
437 |
Class III Pharmacotherapy |
J9206 |
Irinotecan injection |
434 |
433 |
Class IV Chemotherapy Drugs |
| J1573 |
Hepagam b intravenous, inj |
436 |
438 |
Class IV Pharmacotherapy |
J9170 |
Docetaxel injection |
433 |
434 |
Class V Chemotherapy Drugs |
| J2820 |
Sargramostim injection |
437 |
438 |
Class IV Pharmacotherapy |
J9261 |
Nelarabine injection |
432 |
434 |
Class V Chemotherapy Drugs |
| J2353 |
Octreotide injection, depot |
438 |
439 |
Class V Pharmacotherapy |
J2278 |
Ziconotide injection |
433 |
441 |
Class VI Chemotherapy Drugs |
| J0850 |
Cytomegalovirus imm IV /vial |
439 |
440 |
Class VI Pharmacotherapy |
J9035 |
Bevacizumab injection |
434 |
441 |
Class VI Chemotherapy Drugs |
NOTE: The aforementioned are examples of drug reclassifications effective January 1, 2010. For a complete list consult the APG website.
New Premium "Class VII" APG for Select Chemotherapy and Pharmacotherapy Drugs
- There will be a new "premium" drug APG, consisting of certain chemotherapy and pharmacotherapy drugs. All drugs grouping to this class will be carved out of APGs and billable to the Ordered Ambulatory Fee Schedule.
| CPT |
Description |
Current APGs |
New 2010 APGs |
New 2010 APGs |
| J7311 |
Fluocinolone acetonide implt |
437 |
442 |
CLASS VII COMBINED CHEMOTHERAPY & PHARMACOTHERAPY |
| J1458 |
Galsulfase injection |
439 |
| J1785 |
Injection imiglucerase /unit |
439 |
| J1300 |
Eculizumab injection |
439 |
| J9300 |
Gemtuzumab ozogamicin inj |
434 |
| J0180 |
Agalsidase beta injection |
434 |
New Mental Hygiene APGs
- All providers that bill using APGs will have access to the following APG groups:
| APG |
APG Description |
APG Type Description |
| 321 |
Crisis Intervention |
Significant Procedure |
| 322 |
Medication Administration & Observation * |
| 323 |
Mental Hygiene Assessment |
| 324 |
Mental Health Screening & Brief Assessment |
| 274 |
Physical Therapy, Group |
| 275 |
Speech Therapy & Evaluation, Group |
New APG With Procedure Based Weights and APGs That Recognize Units of Service
- To recognize significant cost differentials in a single service, some procedures will be paid based on procedure–specific weights rather than APG–specific weight, including the following types of services:
- Select Mental Hygiene Services,
- Physical Therapy (for units–based procedures),
- Occupational Therapy (for units–based procedures), and
- Crisis Management.
Procedure–based Weights & Units of Service Features in Some APGs
| All Procedure–Based and Units–Based APGs |
| APG |
APG Description |
| 118* |
Nutrition Therapy |
| 270** |
Occupational Therapy |
| 271*** |
Physical Therapy |
| 272**** |
Speech Therapy And Evaluation |
| 310 |
Developmental & Neuropsychological Testing |
| 312 |
Full Day Partial Hospitalization For Mental Illness |
| 315 |
Counseling Or Individual Brief Psychotherapy |
| 316 |
Individual Comprehensive Psychotherapy |
| 317 |
Family Psychotherapy |
| 320 |
Case Management & Treatment Plan Development – Mental Health Or Substance Abuse |
| 321 |
Crisis Intervention |
| 323 |
Mental Hygiene Assessment |
| 426 |
Psychotropic Medication Management |
| 427 |
Biofeedback And Other Training |
| 428 |
Education – Individual |
| 429 |
Education – Group |
| 490 |
Incidental To Medical, Significant Procedure Or Therapy Visit |
| APG |
APG Description |
Payment Action Flag Description |
HCPCS Code |
HCPCS code description |
| 118* |
Nutrition Therapy |
Alternate Weight – Not Units Based |
97804 |
Medical nutrition, group, each 30 min |
| G0271 |
Group MNT 2 or more 30 mins |
| Alternate Weight – Units Based |
97802 |
Medical nutrition, indiv, each 15 min |
| 97803 |
Med nutrition, indiv, subseq, each 15 min |
| G0270 |
MNT subs tx for change dx, each 15 min |
| 270** |
Occupational Therapy |
Alternate Weight – Units Based * |
97532 |
Cognitive skills development, 15 min |
| 97533 |
Sensory integration, 15 min |
| 271*** |
Physical Therapy |
Alternate Weight – Units Based * |
97032 |
Electrical stimulation, 15 min |
| 97033 |
Electric current therapy, 15 min |
| 272**** |
Speech Therapy And Evaluation |
Alternate Weight – Not Units Based |
92607 |
Ex for speech device rx, 1hr |
| 92608 |
Ex for speech device rx addl |
* For illustration purposes only. These APGs include additional procedures not shown in this table.
Medical Visits Will No Longer Package With Higher Intensity Significant Ancillaries
- Medical visits will no longer package with:
- more significant ancillaries (e.g., MRIs, mammograms, CAT scans, etc.);
- dental procedures;
- PT, OT, and speech therapies; and,
- counseling services.
- In these cases, a coded medical visit will separately pay at the line level.
Revised "If Stand Alone, Do Not Pay" List
- New additions to the "if stand alone, do not pay" list for January 2010 are as follows:
| New If Stand Alone Do Not Pay APGs for January 2010 |
| APG Type |
APG |
APG Desc |
| Significant Procedure |
118 |
Nutrition Therapy |
| Significant Procedure |
281 |
Magnetic Resonance Angiography ‐ Head And/Or Neck |
| Significant Procedure |
282 |
Magnetic Resonance Angiography ‐ Chest |
| Significant Procedure |
283 |
Magnetic Resonance Angiography ‐ Other Sites |
| Significant Procedure |
292 |
Mri‐ Abdomen |
| Significant Procedure |
293 |
Mri‐ Joints |
| Significant Procedure |
294 |
Mri‐ Back |
| Significant Procedure |
295 |
Mri‐ Chest |
| Significant Procedure |
296 |
Mri‐ Other |
| Significant Procedure |
297 |
Mri‐ Brain |
| Ancillary |
373 |
Level I Dental Film |
| Ancillary |
374 |
Level II Dental Film |
| Ancillary |
375 |
Dental Anesthesia |
| Drug |
440 |
Class VI Pharmacotherapy |
New (Additional) "No Blend APGs"
- The following new APGs will pay entirely based on the APG payment methodology and no existing payment will be factored into the operating component of the rate.
| APG |
APG Description |
APG Type |
| 94 |
Cardiac Rehabilitation |
Significant Procedure |
| 310 |
Developmental and Neuropsychological Testing |
Significant Procedure |
| 312 |
Full Day Partial Hospitalization for Mental Illness |
Per Diem |
| 321 |
Crisis Intervention |
Significant Procedure |
| 322 |
Medication Administration and Observation |
Significant Procedure |
| 426 |
Medication Management |
Ancillary |
Additional Significant Program & Policy Changes
Statewide Patient–Centered Medical Home Incentive Program
- This initiative will incentivize providers for developing patient–centered medical homes to improve health outcomes through better coordination and integration of patient care.
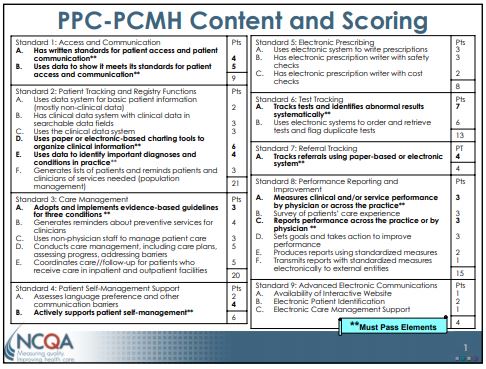
- New York Medicaid has chosen to adopt medical home standards consistent with the National Committee for Quality Assurance´s (NCQA) Physician Practice Connections® – Patient–Centered Medical Home Program (PPC–PCMH™).
- The PPC–PCMH™ is a model of care that seeks to strengthen the physician– patient relationship by promoting improved access, coordinated care, and enhanced patient/family engagement.
- A medical home also emphasizes enhanced care through open scheduling, expanded hours and communication between patients, providers and staff.
- Care is also facilitated by registries, information technology, health information exchange and other means to ensure that patients obtain the proper care in a culturally and linguistically appropriate manner.
To be recognized as a medical home, providers need to demonstrate they can meet at least five of the following 10 criteria (i.e. achieve a minimum of 25 points out of 100 possible to attain the first of three levels of recognition):
- Written standards for patient access and patient communication;
- Use of data to show standards for patient access and communication are met;
- Use of paper or electronic charting tools to organize clinical information;
- Use of data to identify important diagnoses and conditions in practice;
- Adoption and implementation of evidence–based guidelines for three chronic conditions;
- Active patient self–management support;
- Systematic tracking of test results and identification of abnormal results;
- Referral tracking, using a paper or electronic system;
- Clinical and/or service performance measurement, by physician or across the practice; and
- Performance reporting, by physician or across the practice.
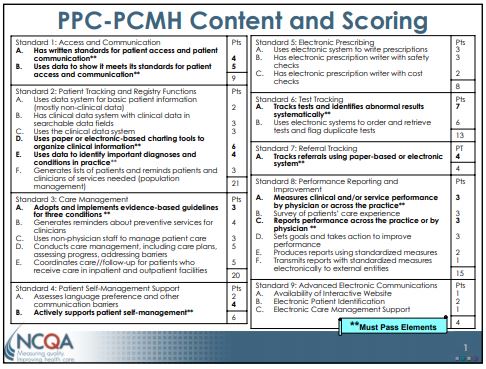
- There are three levels of medical home recognition that providers can achieve based on the following NCQA scoring scale:
| PPC–PCMH Scoring |
| Level of Qualifying |
Points |
Must Pass Elements
at 50% Performance Level |
| Level 3 |
75 – 100 |
10 of 10 |
| Level 2 |
50 – 74 |
10 of 10 |
| Level 1 |
25 – 49 |
5 of 10 |
| Not Recognized |
0 – 24 |
< 5 |
Levels: If there is a difference in Level achieved between the number of points and "Must Pass", the practice will be awarded the lesser level; for example, if a practice has 66 points but passes only 7 "Must Pass" Elements the practice will achieve at Level 1.
Practices with a numeric score of 0 to 24 points or less than 5 "Must Pass" Elements do not Qualify.
- Medicaid FFS claims with appropriately coded Evaluation and Management (E&M) codes 99201–99205, 99211–99215, or Preventive Medicine codes 99381–99386, 99391–99396 will be eligible for one of three enhanced payment levels (shown below), commensurate with the level of NCQA recognition received by the provider.
| Medical Home Pervisit Payment Add–ons |
| Setting |
Level I |
Level II |
Level III |
| Article 28 clinics |
$5.50 |
$11.25 |
$16.75 |
| Office‐based practitioners* |
$7.00 |
$14.25 |
$21.25 |
* Includes physicians and registered nurse practitioners
- NCQA recognized providers that participate in Medicaid and Family Health Plus health plans will receive details on the payment amounts they can expect for services provided to plan enrollees.
Physician Carve Out Policies for OPDs
- Reimbursement for physician professional services provided by hospital OPDs will be carved out of APGs beginning February 1, 2010.
- Note, there will be no change to current Medicaid policy which disallows payment for interns and/or residents, yet allows payment for supervisors and/or teaching physicians under specified conditions.
Supporting Materials
- The following is available on the DOH website
- Provider Manual
- PowerPoint Presentations
- APG Documentation
- APG Types, APG Categories, APG Consolidation Logic
- Revised Rate Code Lists
- Uniformly Packaged APGs
- Inpatient–Only Procedure List
- Never Pay and If Stand Alone Do Not Pay Lists
- Carve–Outs List
- List of Rate Codes Subsumed in APGs
- Paper Remittance
- Frequently Asked Questions
- Ambulatory Surgery List
Contact Information
- Grouper / Pricer Software Support
- 3M Health Information Systems
- Billing Questions
- Computer Sciences Corporation
- Policy and Rate Issues
- New York State Department of Health
Office of Health Insurance Programs
Div. of Financial Planning and Policy 518–473–2160