Value Based Payment For Partially Capitated Plans
- Webinar also available in Portable Document Format (PDF)
MLTC VBP Refresher Webinar
- VBP Risk Levels
- SDH & CBO requirements & examples
- VBP Tracking Report (VBPTR)
March 8, 2019 – Updated 4/23/19
Agenda
- Introductions
- Review of MLTC VBP Risk Levels
- SDH & CBO Requirements and Examples
- VBPTR Review
- Other Contracting Questions
- Questions
VBP Risk Levels
MLTC VBP Risk Level Definitions
| VBP Level 0 | VBP Level 1 | VBP Level 2 | VBP Level 3 | |
|---|---|---|---|---|
| MLTC Partial Plans | An arrangement that includes a performance–based quality bonus that does not include the Potentially Avoidable Hospitalization (PAH) measure. | An arrangement that includes a performance–based quality bonus between an MLTC Partial Plan and a provider that is based on meeting performance targets for a set of specific quality measures agreed to in a VBP contract between an MLTC Partial Plan and provider. Such agreement must include the Potentially Avoidable Hospitalization (PAH) measure. |
A pay–for–performance agreement between MLTC Partial Plans and providers where incentive payments are based on meeting performance targets for quality measures agreed to in a VBP contract with the addition of a "downside" or quality withhold. To meet the Level 2 definition, Plans and providers should establish a minimum downside of 1% of total annual expenditures in the contract between the Plan and the provider. Requires inclusion of the PAH measure; and inclusion of at least one State approved long–term care measure recommended by the MLTC CAG Requires SDH and CBO inclusion |
To be determined at a future date. NOTE: No VBP requirements are targeted at achieving specifically VBP Level 3 contracting |
| Fully Integrated Plans (FIDA, MAP and PACE) | Arrangements that go beyond strict FFS but do not meet the requirements of VBP Level 1. Example: A shared savings arrangement that doesn´t make shared saving contingent upon quality outcomes. |
These arrangements continue the existing FFS payment methodology from MCO to providers but allows the VBP contractor to receive a percentage of the shared savings based on meeting sufficient efficiency and quality outcomes. | These arrangements allow the VBP contractor to receive a higher percentage of shared savings than in Level 1 because the VBP contractor is also required to share a percentage of losses that result from spending more than the ´target budget´. Requires SDH and CBO inclusion |
Arrangements that are fully capitated PMPM arrangements or prospectively paid bundles. Includes a quality component. Requires SDH and CBO inclusion |
Social Determinants of Health (SDH) & CBO Requirements for MLTC Programs
Quick Review of CBO and SDH Standards
All new and existing VBP Level 2 & 3 arrangements MUST include:
- At least one Social Determinant of Health Intervention.
- SDH Interventions must align with the five key areas of SDH outlined in the SDH Intervention Menu Tool, which includes:
- Education,
- Social, Family and Community Context,
- Health and Healthcare
- Neighborhood & Environment and
- Economic Stability
- Must have a contract with least one Tier 1 Community Based Organization (Non–Medicaid billing, non–profit social and human services organization).
- The Tier 1 Community Based Organization can be subcontract with a Tier 2 or 3 Community Based organization. This requirement does not have to be paired with the SDH requirement.
* VBP Level 2 & 3 contracts without SDH and CBO requirements will be categorized as Level I (so long as all other VBP requirements are met)
Tier 1, Tier 2, and Tier 3 CBO Definitions
- Tier 1 CBO
- Non–profit, non–Medicaid billing, community based social and human service organizations
- e.g. housing, social services, religious organizations, food banks
- All or nothing: All business units of a CBO must be non–Medicaid billing; an organization cannot have one component that bills Medicaid and one component that does not and still meet the Tier 1 definition
- Non–profit, non–Medicaid billing, community based social and human service organizations
- Tier 2 CBO
- Non–profit, Medicaid billing, non–clinical service providers
- e.g. transportation provider, care coordination provider
- Non–profit, Medicaid billing, non–clinical service providers
- Tier 3 CBO
- Non–profit, Medicaid billing, clinical and clinical support service providers
- Licensed by the NYS Department of Health, NYS Office of Mental Health, NYS Office for Persons with Developmental Disabilities, or NYS Office of Alcoholism and Substance Abuse Services.
Use the CBO list on DOH´s VBP website to find CBOs in your area
SDH Example: Medical Respite Program
- Goal: To shorten hospital stays; decrease readmission rates, and unnecessary emergency department visits.
- Program provides emergency shelter service for homeless adults being discharged from inpatient hospitalization with ongoing medical needs.
- Program allows plan members who are homeless or housing insecure to recover, while also working with a care manager to secure permanent housing.
- Average cost of $140/night per respite bed. This represents 6% of the average cost per night for a hospital admissions.
- Intervention also linked directly to reducing unnecessary hospitalizations.
- Return on investment in New York has been measured as high as 300%.
CBO Contracting Strategies
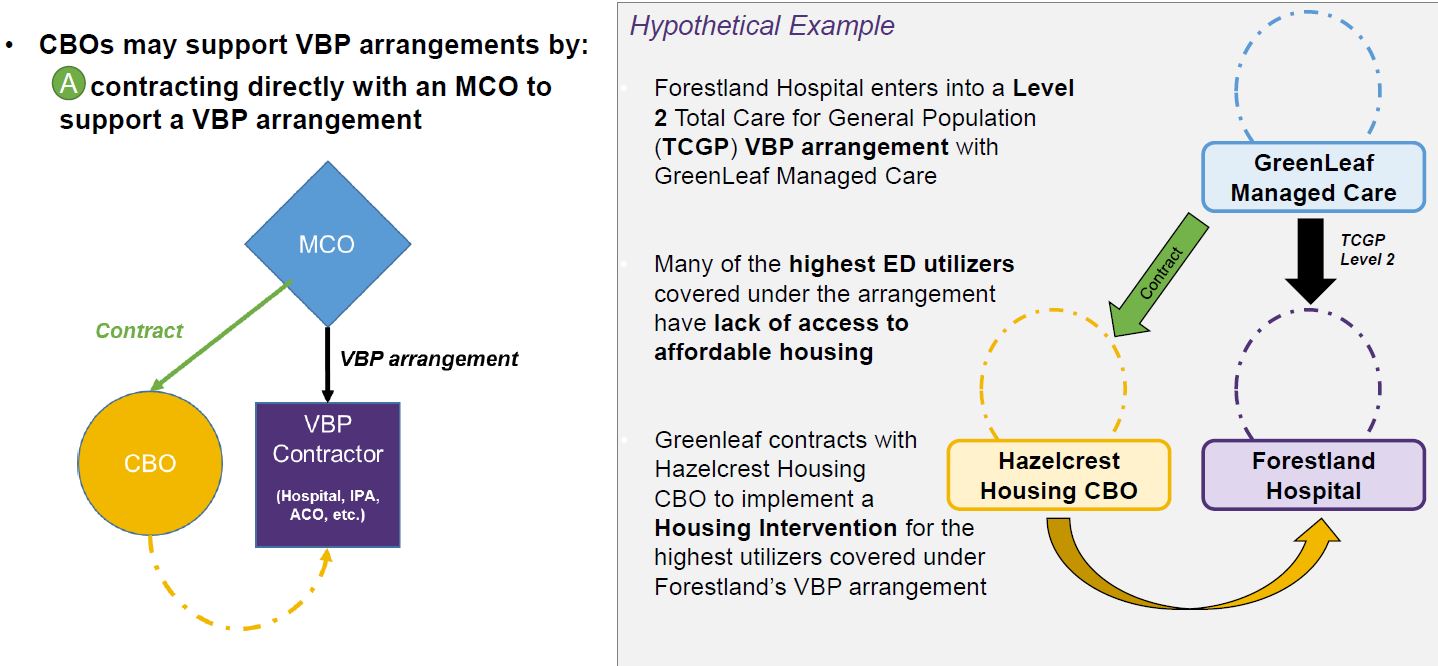
CBO Contracting Strategies – Scenario A
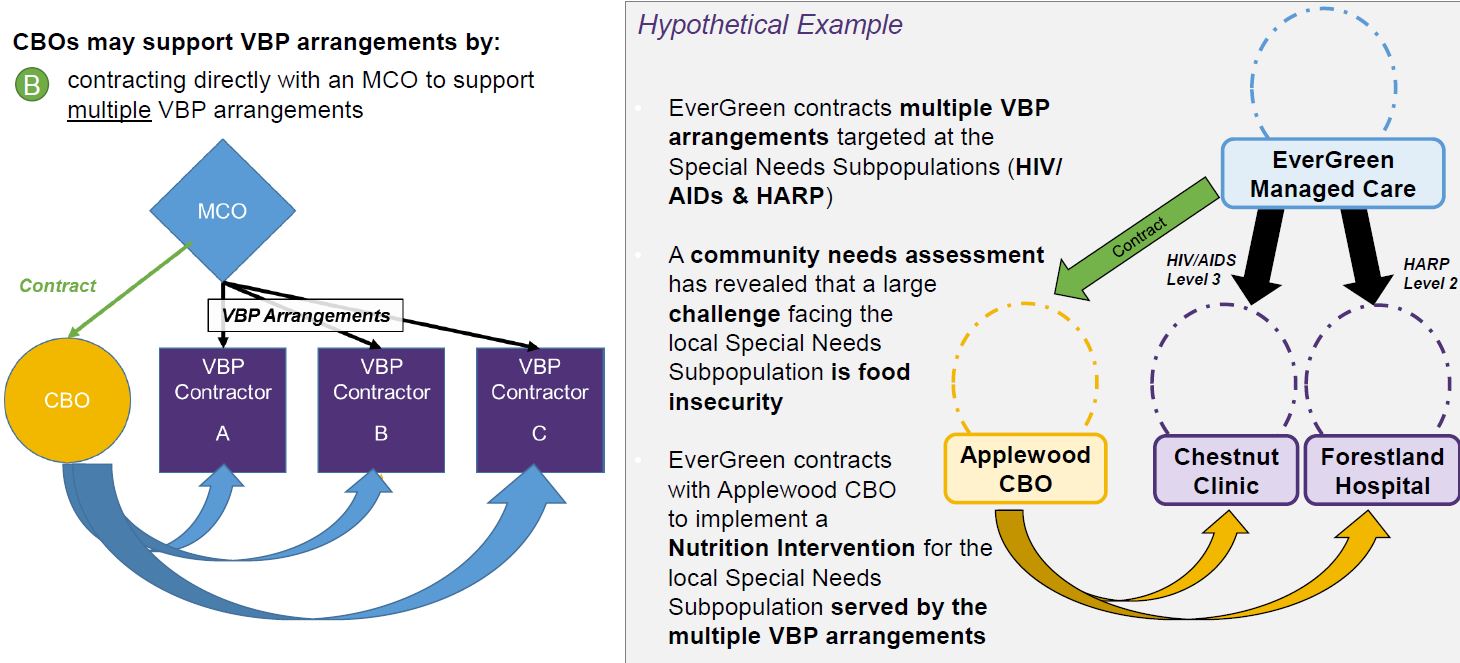
CBO Contracting Strategies – Scenario B
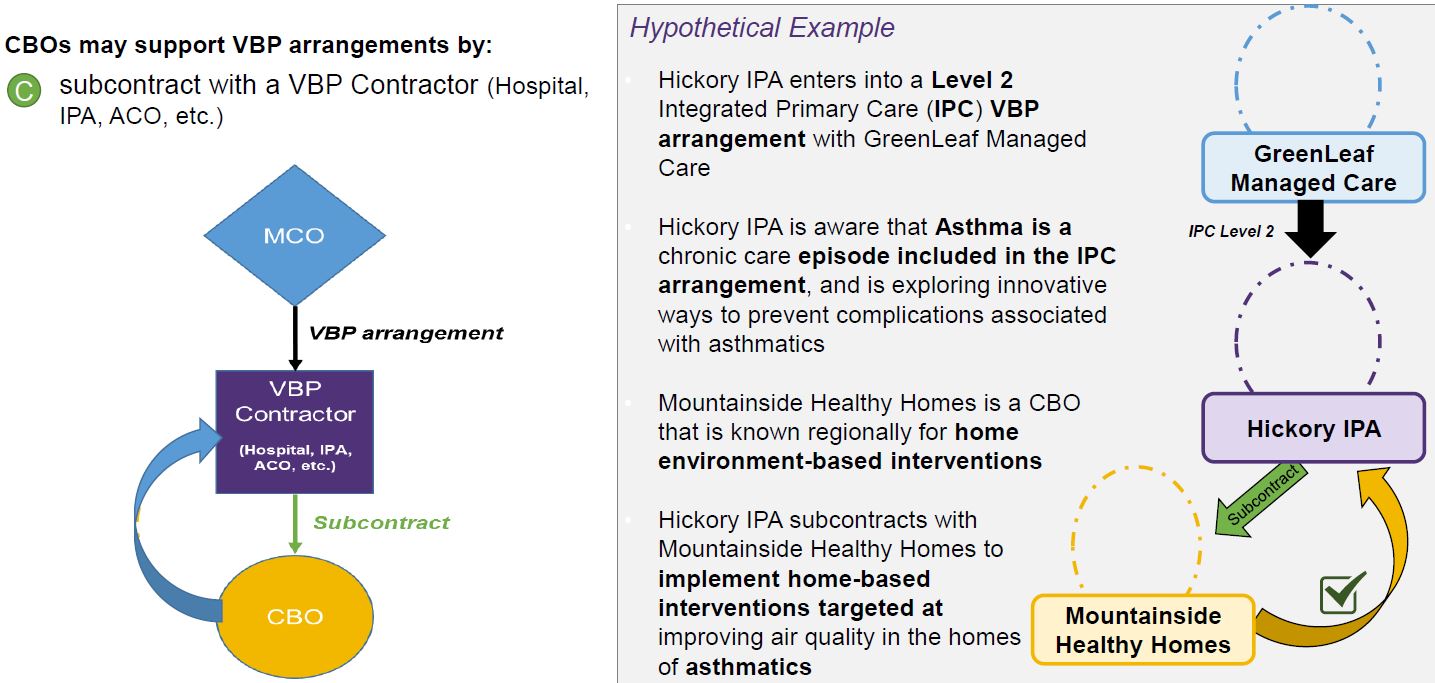
CBO Contracting Strategies – Scenario C
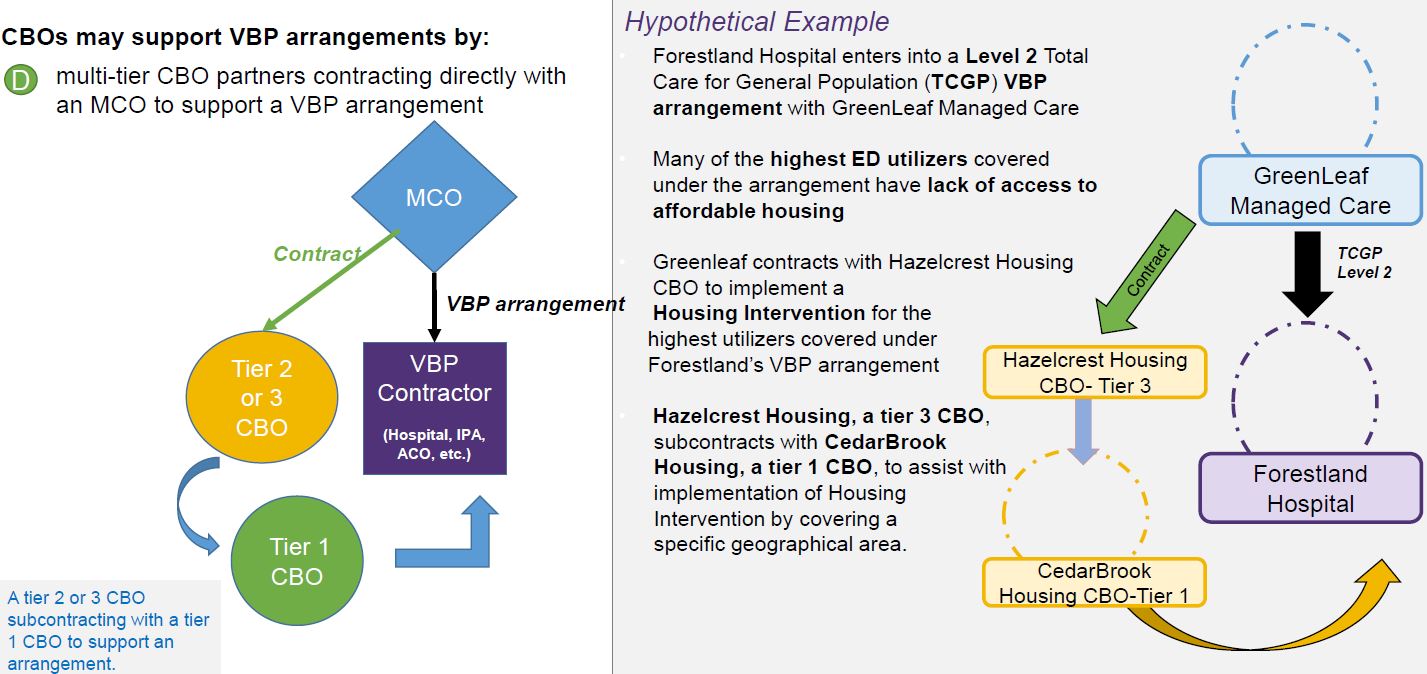
CBO Contracting Strategies – Scenario D
CBO Contracting Options
- CBO contracts are not required to include risk
- CBO contracts could be structured as:
| Payment for services rendered | Upside only | Upside and Downside risk |
|---|---|---|
| Contracts without a risk–based component | ||
| No downside risk | Risk sharing contract | |
| If savings are achieved, CBO receives a portion of shared savings | If savings are achieved, CBO receives a portion of shared savings | |
| If losses are incurred, CBO would not take on any losses | If losses are incurred, CBO would take on some degree of loss |
- CBOs may be held to performance measure standards by the party they are contracting with (VBP Contractor or MCO) in order for contracting to continue
SDH Intervention Examples
SDH Example: Peer Mentoring and Wellness Coaching Program
- Goal: Promote the use of evidence–based care to manage chronic disease using trained peers
- Peer Mentors are recruited and matched with members based on their chronic conditions, language, and culture, etc.
- In–person or telephonic outreach to participant members to provide one–on–one support and encouragement for behavior change, leading to better self–management skills
- Supports include:
- Adhering to diet while being culturally sensitive
- Identifying and avoiding triggers that lead to negative outcomes
- Providing follow up and increased medication adherence
| SDH Domain | Intervention |
|---|---|
| Social and Community Context | Informal Support and Social Cohesion:
|
| Economic Stability | Social Transportation:
|
| Neighborhood and Environment | Healthy Homes:
|
| Economic Stability | Financial Security and Education:
|
VBP Tracking Report (VBPTR) Overview
VBPTR Reminders
- DOH requires that Managed Care Plans (partially capitated and fully integrated) submit their progress toward VBP implementation on a quarterly basis. (VBPTR)
- MCO reported Medicaid expenditure in VBP is used to:
- Report to CMS annually on the State´s progress in meeting VBP targets as defined in the Roadmap (VBP Roadmap, pg. 62)
- Calculate MCO incentives for rate setting year SFY 2018–19, as referenced in the VBP Roadmap (VBP Roadmap, pg. 47)
- Responses submitted via VBPTR should only include Medicaid expenditures
- Responses submitted via VBPTR should not include Medicare expenditures
- Fully Integrated products should not submit Medicare expenditures as part of their reporting
- The DOH is assessing MCO (including MLTC Plans) total Medicaid expenditure that transitions to VBP for the following:
- Partial capitation which includes LHCSA, CHHAs, SNF spend only
- Fully integrated products including MAP, PACE, FIDA
- Fully integrated products may have Levels 1, 2, or 3 VBP arrangements
- Partial capitation may have Levels 1 or 2 VBP arrangements
- An MCO´s VBP progress is measured by the following:
- Partial capitation: aggregate total expenditure captured in VBP for LHCSA, CHHA, SNF (i.e. "Total Medical Expense for Line of Business" on Table 1E should reflect the total expenditures for all LHCSA, CHHA and SNF providers regardless of VBP level or participation).
- Fully Integrated: aggregate total expenditure captured in VBP for the product lines held by a Plan, for example, (PACE, FIDA and mainstream)
- FIDA, MAP, and PACE should report all VBP dollars under "Total Care for MLTC Subpopulation" on Table 2F, 2D, and 2G, respectively. This enables the State to track spend for FIDA, MAP and PACE separately from the partial capitated spend (LHCSA, CHHA, SNF). Plans should report all of their Medicaid spending with all providers types on the respective Table 2.
* Refer to pages 47 and 62 for a description of how MCO penalties are applied and how the State assess progress toward VBP implementation
VBPTR Reporting Requirements
Table 1 – 1G: Medical Expense Summary
| All Lines of Business |
|---|
|
Table 1–1G for both Fully & Partially Capitated Plans
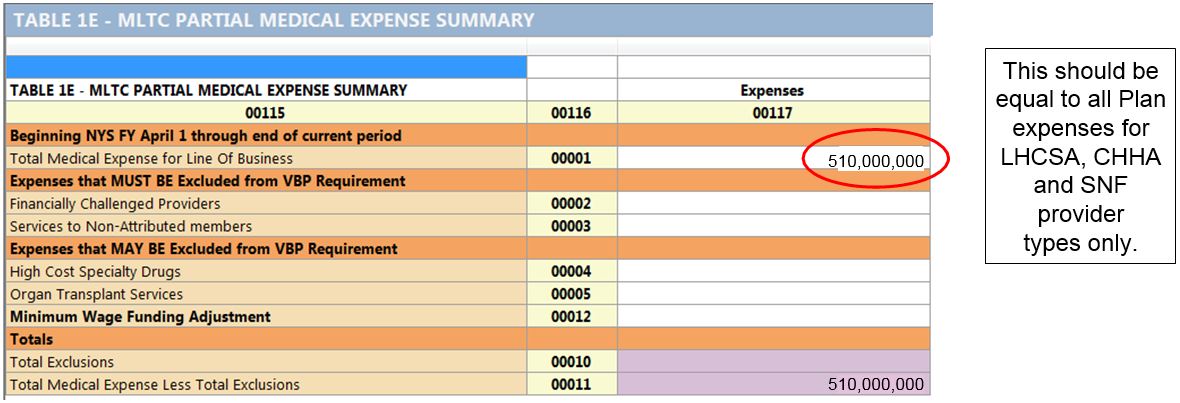
Table 2 – 2G: Medical Expense by Arrangement
| FIDA (Table 2F) MAP (Table 2D) PACE (Table 2G) |
MLTC Partial (Table 2E) |
|---|---|
|
|
Table 2E for Partially Capitated
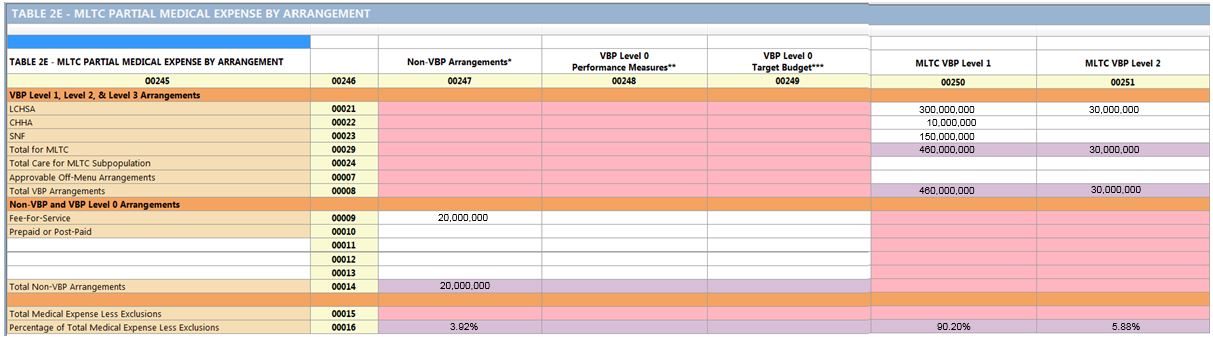
Reminder: For partially capitated plans, plans should not enter anything in the "Total Care of MLTC Subpopulation" line
Table 2 (D,F or G) for Fully Capitated Plans
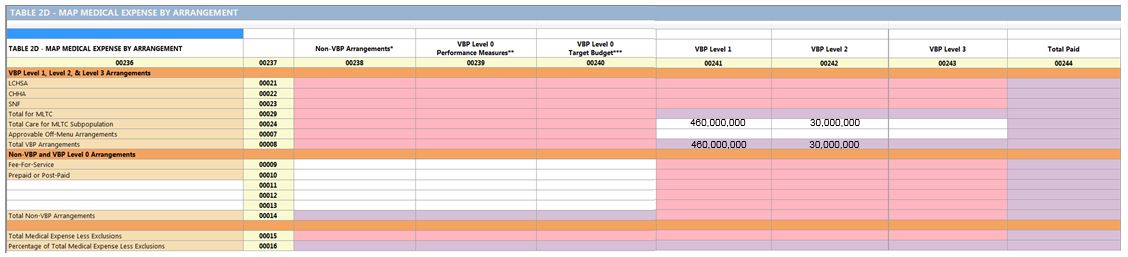
Table 3 – 3G: Medical Expense by Region
| All Lines of Business |
|---|
|
Table 4 – 4G: VBP Contract Specification Information
| Table 4 – All Lines of Business | Table 4–1 – All Lines of Business |
|---|---|
|
|
VBP Tracking Report (VBPTR) Examples
Examples based on contract submission and effective dates
Reporting Example 1
Scenario
- Plan ABC has a VBP Level 2 contract that was approved by DOH on October 1, 2018. The total medical expense for this contract is $5 million. How will Plan ABC report these dollars?
- Reporting Correctly:
- Updated 4/23/19:
For the annual reporting period (April 1, 2018 – March 31, 2019) the full $5 million should be reported in Table 2 under Level 2. If a contract is submitted and effective during the SFY reporting period, the total medical for the contract is counted as VBP.
- Updated 4/23/19:
- Reporting Correctly:
Reporting Example 2
Scenario
- Plan ABC enters into a contract with a retroactive start date of January 1, 2019. The contract was approved in July 2019. Can Plan ABC count this contract on their 4/1/18–3/31/19 VBPTR submission?
- Reporting Correctly:
- Updated 4/23/19:
Yes. If a contract is submitted by and has an effective date on or before 3/31 of the respective SFY reporting period (April 1 – March 31), it can be counted as VBP for that annual reporting period. - The contract must be approvable within the 3 day (Tier 1 contracts) or 90 day (Tier 2 & 3 Contracts) timeframe as outlined in the Provider Contract Guidelines.
- Updated 4/23/19:
- Reporting Correctly:
Reporting Example 3
Scenario
- Plan ABC amended a Non–VBP arrangement in December 2018, and it is now considered a Level 2 arrangement moving forward. Does Plan ABC need to split the contract expenses between the two levels?
- Reporting Correctly:
- Updated 4/23/19:
No, contract expenses should not be split among different arrangement levels. - If a contract amendment was submitted by and had an effective date on or before 3/31 of the respective SFY, then the total amount of the contract should be entered in Level 2.
- Updated 4/23/19:
- Reporting Correctly:
Reporting Example 4
Scenario
- Plan ABC, an MLTC Partial Plan, is entering information on Table 1E. What expenditure should be entered for "Total Medical Expense for Line of Business"?
- Reporting Correctly:
- For partially capitated plans, the Total Medical Expense for Line of Business should only include total spend for LHCSA, CHHA, SNF in both VBP & non–VBP arrangements. It should NOT include other services or provider types (unless the Plan has a DOH approved Off–menu arrangement).
- Reporting Correctly:
Other Contracting Questions
Other Questions Asked by Plans
Q: Can the VBP contract between the Plan & Provider include a contingency that the Plan receive VBP quality performance dollars from the State in order to award upside funding to the Provider?
A: No, payment cannot be contingent upon the Plan receiving VBP Quality Performance dollars from the State.
Q: To meet the Level 2 definition, the amount of risk allocated to the provider must be at least 1% of total annual expenditures in the contract between the Plan and the provider.
A: Plans and providers may use the total annual expenditure of the previous year´s contract (between the same provider and Plan) to determine 1% risk or Plans and providers may calculate 1% risk based on the annual expenditure of the current year´s contract. Either method is acceptable.
Q: How should Plans encourage Providers to enter into a Level 2 arrangement?
A: The State does not dictate how these arrangements should be set up in your Plan to provider contracts. For example, Plans may choose to increase the upside in Level 2 arrangements to incentivize provider participation. (i.e. Plans are encouraged to share more data, pass down the VBP performance adjustment, etc.)
Q: Can bonus monies or penalties be applied using retrospective lookback and assessed after the performance year?
A: The methodology for assessing provider performance to calculate upside or downside is not defined by the State and can be negotiated between the Plan & Provider.
Please direct any additional questions or feedback to:
vbp@health.ny.gov
Follow Us