Conflict of Interest Compliant Models and Transition Discussion
- Presentation is also available in Portable Document Format (PDF)
Nursing Home Transition and Diversion (NHTD) Waiver Program And Traumatic Brain Injury (TBI) Waiver Program
March 6, 2019
Topics for Discussion
- Recap of Federal Conflict of Interest (COI) Rules and Requirements (January 11, 2019) Meeting
- Feedback from Stakeholders, Models that Meet (and do not Meet) CMS COI Requirements
- Important Timeframes and Next Steps
Conflict of Interest Defined
Providers of HCBS for the individual, or those who have an interest in or are employed by a provider of HCBS for the individual must not provide case management or develop the person–centered service plan.
Exception: Where the State can demonstrate that the only willing and qualified entity to provide case management and/or develop person–centered service plans in a geographic area also provides HCBS.
In these cases, the State must devise conflict of interest protections including separation of entity and provider functions within provider entities, which must be approved by CMS. Individuals must be provided with a clear and accessible alternative dispute resolution process.
In addition, certain NHTD and TBI services are NOT subject to COI.
- Source:42 CFR 441.301(c)(1)(vi)
| NHTD Waiver Services | TBI Waiver Services | ||||
|---|---|---|---|---|---|
| Exempt Services | Non–Exempt Services | Exempt Services | Non–Exempt Services | ||
| Assistive Technology (AT) | Service Coordination | Independent Living Skills and Training | Assistive Technology (AT) | Service Coordination | Independent Living Skills and Training (ILST) |
| Moving Assistance | Community Integration Counselling (CIC) | Structured Day Program Services | Community Transitional Services (CTS) | Structured Day Program Services | Positive Behavioral Interventions and Support Services (PBIS) |
| Community Transitional Services (CTS) | Nutritional Counseling/Educational Services | Transportation Services | Environmental Modifications (E–Mods) | Substance Abuse Program Services | |
| Congregate and Home Delivered Meals | Peer Mentoring | Wellness Counselling | Transportation Services | ||
| Environmental Modifications (E–Mods) | Positive Behavioral Interventions and Support Services (PBIS) | Home and Community Support Services (HCSS) | Community Integration Counselling (CIC) | ||
| Respiratory Therapy | Home Visits by Medical Personnel | Home and Community Support Services (HCSS) | |||
| Respite | Respite | ||||
Conflict of Interest Compliance
- The HCBS Final Rule is focused on the individual/participant not the provider.
- The individual may not receive service coordination (i.e., case management/planning) and direct waiver services from the same provider.
- Therefore, the rule does not necessarily preclude providers from offering both service coordination and other direct waiver services.
Case Management is …
- A "key" or "linchpin" service in the world of Long Term Supports and Services (LTSS)
- Both the human services system and the individual/family rely on case management.
- The "system" needs case management to keep the program running.
- The individual and family need case management to help them build and sustain their lives.
Case Management Activities and the Case Manager Role
- A case manager´s job is to help the individual and family become well–informed about all choices that may address the needs and outcomes identified in the plan
- The case manager’s activities and duties should be free of potential conflicts of interest that may promote conscious or unconscious "steering" (to particular services or service providers) of the member and their choices
- CMS uses the term "case management activities" to include the various functions specified in regulations with the assumption that these activities may be performed by individuals or entities other than the case manager or designated case management entity. In some programs/benefits, the entities who perform these functions may or may not be a case manager. Any activities that are case management must be performed by a person that is not providing other non–exempt waiver services to the same individuals to be COI compliant.
Suggested Models that Do Not Meet CMS COI Requirements
- Plan development and service oversight model
- Plan development agency develops initial, revised, and addenda to service plan; service broker identifies providers for the individual that are conflict–free, ready and willing.
- Plan development is included in the federal regulatory definition of Case Management. Therefore, a model that separates plan development from service coordination is not conflict free.
- This includes wellness checks and health and safety oversight.
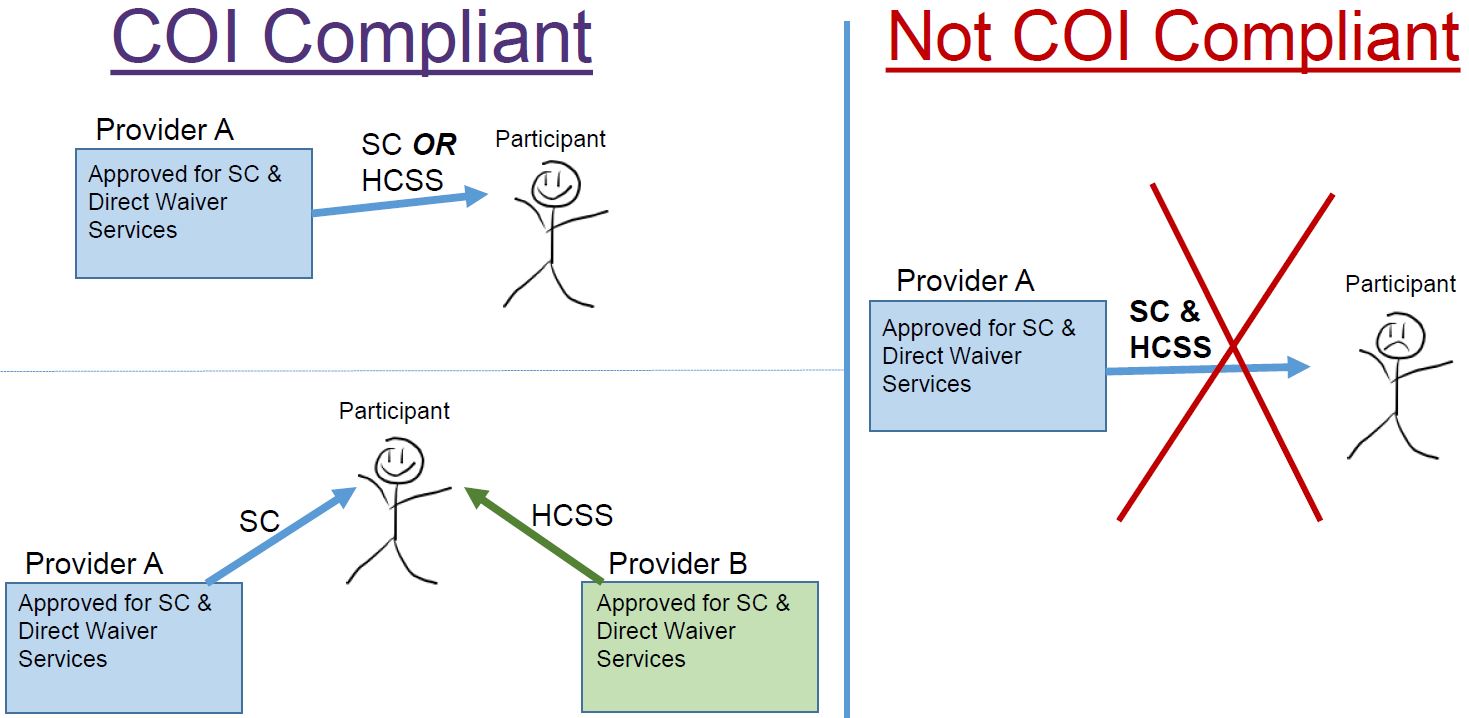
- CMS has indicated that providers of multiple services may continue to offer multiple services. However, they may only provide EITHER direct waiver services OR service coordination to any one participant. Providers cannot provide direct waiver services and service coordination to any one participant.
Models that Comply with CMS COI Requirements
- Service Coordination separation model
- Providers continue to provide multiple services but cannot provide service coordination and other direct waiver services to the same individual.
- Functions of Service Coordinators (SCs) may remain the same.
- An individual’s SC cannot be employed by a provider who is also offering direct waiver services to that individual.
- Service Coordination only providers and those who offer Service Coordination and other exempt services may continue business as usual.
- DOH/RRDC maintains authority over provider designation and final plan approval.
- Providers continue to provide multiple services but cannot provide service coordination and other direct waiver services to the same individual.
Service Coordination Separation Model: Pros/Cons – Stakeholder Feedback
| Pros | Cons |
|---|---|
| Functions of Service Coordinators may remain the same. | Participants may be required to change either their service coordination provider or their direct service provider and this may cause a disruption. |
| Providers can continue to provide service coordination services. | May create a significant capacity issue. Providers have commented that service coordination is not typically financially sustainable on its own |
| Service coordination only providers and those who offer service coordination and other exempt services may continue business as usual. | Participant choice is limited. |
| Prevents significant change to the system. | Potential for disruption in staffing. |
Models that Comply with CMS COI Requirements
- CMS has indicated that providers of multiple services may continue to offer multiple services. However, they may only provide EITHER direct waiver services OR service coordination to any one participant. Providers cannot provide direct waiver services and service coordination to any one participant.
- Service Coordination activities must be independent of direct waiver service provision.
- Conflict occurs not just if the entity is a provider but if the entity:
- Has an interest in a provider, or
- Is employed by a provider.
- Requirements are located at42 CFR 441.301(c)(1)(vi).
Models that Comply with CMS COI Rules
- Statewide organization model
- A statewide organization provides Service Coordination only.
- Service Coordination provider enrollment is limited to statewide Service Coordination agency/agencies.
- Service Coordination only providers and those who offer Service Coordination and other exempt services may continue business as usual.
- The provider(s) offer no other direct waiver services.
- A statewide organization provides Service Coordination only.
Example: Jordan is applying for NHTD waiver services. He selects DEFCo as his Service Coordination provider. DEFCo is approved statewide and connects Jordan with a conflict–free SC in his region who he meets with to develop his person–centered service plan. DEFCo provides no other direct waiver services.
Statewide Service Coordination Model: Pros/Cons – Stakeholder Feedback
| Pros | Cons |
|---|---|
| Functions of Service Coordinators may remain the same. | Providers have indicated that due to the supervision requirements for individual service coordinators, the geographic area would have to be broken down in order to have sufficient administrative coverage. |
| Sub–contract arrangements may allow service coordinators to maintain current caseloads. | Service coordinators would have to change employers. |
| Option may serve as back–up in areas where there are not a sufficient number of providers. | Participant choice is limited. |
| Prevents significant change to the system. | Potential for disruption in staffing. |
SC Only and SC & Exempt* Provider Capacity
| Region As of February 2019 | NHTD SC Only | TBI SC Only | NHTD SC & Exempt | TBI SC & Exempt |
|---|---|---|---|---|
| Adirondack | 0 | 1 | 0 | 0 |
| Binghamton | 2 | 3 | 1 | 1 |
| Buffalo | 0 | 1 | 0 | 0 |
| Capital | 0 | 0 | 0 | 0 |
| Long Island | 1 | 0 | 0 | 0 |
| Lower Hudson Valley | 0 | 0 | 0 | 0 |
| NYC | 0 | 1 | 1 | 0 |
| Rochester | 1 | 1 | 1 | 0 |
| Syracuse | 0 | 1 | 0 | 0 |
| Total (February 2019): | 4 | 8 | 3 | 1 |
| (Total in 2018) | 5 | 5 | 7 | 2 |
*NHTD: AT, E–Mods, CTS, Moving Assistance and Congregate and Home Delivered Meals TBI: AT, E–Mods and CTS
SurveyMonkey Results
- NYSDOH received:
- 72 responses for NHTD out of 167 unduplicated providers for a rate of 42%
- 87 responses for TBI out of 203 unduplicated providers for a rate of 43%
- This survey was intended to assess provider capacity for waiver services (care management and other waiver services) on a county level in a way that the Conflict of Interest Compliance Implementation Plans (COICIPs) did not – and perhaps provide insight to potential solutions and partnerships.
- CMS requires county–level data to consider rural exemptions:
- County must have one or none willing and qualified service coordination providers.
- CMS requires county–level data to consider rural exemptions:
- The nature of the survey and the low response rate renders the results unreliable.
Stakeholder Review of COI Models
- There is support for the service coordination separation model, however, there are concerns regarding how a waiver participant will decide which services to continue to receive (waiver services or service coordination) from his/her current provider.
- There is support for a Plan Development Agency/Service model in which NYSDOH will contract with designated entities to develop the service plan. This would include:
- A separation of "field services" from other case management functions.
- An interim service coordination function performed by the RRDC (or as a separate discrete waiver service).
- Supporting a rate adjustment for service coordination services.
- There is a recommendation for a care coordination model that would be comparable to Health Homes (i.e., used by HARP members) – need more explanation from Stakeholders.
Stakeholder Concerns
Providers raised the following issues with implementing models that are compliant with the COI requirements:
- Loss/disruption of income for the case managers that must find new employers
- Loss/disruption of either a case manager or a provider for the participant and guardian
- Loss of income from case management services for agencies that employed case managers
- Loss/disruption of benefits for case managers employed by agencies that had built up retirement and/or insurance
- Loss of qualified case managers
What options can we employ to mitigate these concerns?
|top of section| |top of page|Stakeholder Input – Next Steps
- Is there a path that minimizes disruption to participants and providers that combines implementing both the service coordination separation model and statewide organization model?
- Can providers work within in their regions to develop relationships and referral mechanisms to provide applicants/participants with choices that are conflict free?
- Is there data providers would be willing to share (quickly) to help us collectively asses options or pathways of implementing models that are conflict free?
- Other?
Brief Overview of Important Deadlines*
| Compliance Readiness Action | Due Date |
|---|---|
| CMS is anticipating that NYSDOH will present its final model for review. | 4/1/2019 |
Operationalize single option for meeting COI, includes:
|
1/6/2020 |
| Establish transition steps to operate under new service model. | 4/13/2020 |
| CMS wants the transition of cases to the new model to begin. | 6/1/2020 |
| Full implementation | 1/1/2021 |
*Per the approved CAP
|top of section| |top of page|
Follow Us