Partial Capitation Contract
- Contract is also available in Portable Document Format (PDF)
MISCELLANEOUS/CONSULTANT SERVICES
(Non–Competitive Award)
Managed Long Term Care Partial Capitation Contract
STATE AGENCY (Name and Address):
New York State Department of Health
Office of Health Insurance Programs
Division of Long Term Care
One Commerce Plaza
99 Washington Avenue, 16th Floor
Albany, NY 12210
______________________________________________
CONTRACTOR (Name and Address):
______________________________________________
CHARITIES REGISTRATION NUMBER:
CONTRACTOR HAS ( ) HAS NOT ( ) TIMELY FILED WITH THE ATTORNEY GENERAL´S CHARITIES BUREAU ALL REQUIRED PERIODIC OR ANNUAL WRITTEN REPORTS
FEDERAL TAX IDENTIFICATION NUMBER:
MUNICIPALITY NUMBER (if applicable):
______________________________________________
STATUS:
CONTRACTOR IS [ ] IS NOT [ ]
A SECTARIAN ENTITY
CONTRACTOR IS [ ] IS NOT [ ]
A NOT–FOR–PROFIT ORGANIZATION
CONTRACTOR IS [ ] IS NOT [ ]
A NY STATE BUSINESS ENTERPRISE
______________________________________________
NYS Comptroller´s Number:
Originating Agency Code: 3450000
______________________________________________
TYPE OF PROGRAM:
Managed Long Term Care
______________________________________________
CONTRACT TERM:
FROM: January 1, 2015
TO: December 31, 2016
FUNDING AMOUNT FOR CONTRACT TERM:
Based on approved capitation rates
______________________________________________
(X) IF MARKED HERE, THIS CONTRACT IS RENEWABLE FOR ONE ADDITIONAL TWO–YEAR PERIOD OR TWO ADDITIONAL ONE YEAR PERIODS SUBJECT TO THE APPROVAL OF THE NEW YORK STATE DEPARTMENT OF HEALTH AND THE OFFICE OF THE STATE COMPTROLLER
______________________________________________
|top of page|
APPENDICES TO THIS AGREEMENT AND
INCORPORATED BY REFERENCE INTO THE AGREEMENT
APPENDIX A. Standard Clauses for New York State Contracts
APPENDIX B. New York State Department of Health Guidelines For Contractor Compliance with the Federal Americans with Disabilities Act
APPENDIX C. Certification Regarding Lobbying
APPENDIX D. Standard Form LLL Disclosure of Lobbying Activities
APPENDIX E–1. Proof of Workers´ Compensation Coverage
APPENDIX E–2. Proof of Disability Insurance Coverage
APPENDIX F. Service Area and Ages of Population Served
APPENDIX G. Managed Long Term Care Covered and Non–Covered Services
APPENDIX H. Schedule of Capitation Rates
APPENDIX I. Reserved
APPENDIX J. Definitions
APPENDIX K. Grievance and Appeal System, Member Handbook Language and Service Authorization Requirements
APPENDIX L. Managed Long Term Care Enrollee Rights
APPENDIX M. Managed Long Term Care Plan Information Requirements
APPENDIX N. Managed Long Term Care Risk Corridor
APPENDIX O. Nursing Home Transition
APPENDIX P. Conflict Free Evaluation and Enrollment Center
APPENDIX X. Modification Agreement Form (to accompany modified appendices for changes in term or consideration
on an existing period or for renewal periods)
IN WITNESS WHEREOF, the parties hereto have executed or approved this AGREEMENT as of the dates appearing under their signatures.
CONTRACTOR SIGNATURE
By: _________________________________________
_________________________________________
Printed Name
Title: _________________________________________
Date: _________________________________________
STATE AGENCY SIGNATURE
By: _________________________________________
_________________________________________
Printed Name
Title: _________________________________________
Date: _________________________________________
State Agency Certification:
In addition to the acceptance of this contract, I also certify that original copies of this signature page will be attached to all other exact copies of this contract.
STATE OF NEW YORK )
) SS.:
County of ____________ )
On the _________ day of ___________________ in the year ____________, before me, the undersigned, personally appeared __________________________________________________________, personally known to me or proved to me on the basis of satisfactory evidence to be the individual(s) whose names(s) is (are) subscribed to the within instrument and acknowledged to me that he/she/they executed the same in his/her/their/ capacity(ies), and that by his/her/their signature(s) on the instrument, the individual(s), or the person upon behalf of which the individual(s) acted, executed the instrument.
______________________________________
Notary
Approved:
ATTORNEY GENERAL
______________________________________
Title: ______________________________________
Date: _______________________________________
Approved:
Thomas P. DiNapoli
STATE COMPTROLLER
______________________________________
Title: ______________________________________
Date: _______________________________________
TABLE OF CONTENTS
Article I Term of Contract, Renewal and Termination
- Term of Contract
- Renewal
- Termination of the Contract by the Department
- Termination of the Contract by the Contractor
- Other Termination Reasons
- Contract Expiration and Contractor Termination/Phase–out Plan
- Effect of Termination on New Enrollments
Article II Statutory and Regulatory Compliance
Article III Contractor Service Area and Ages of Population to Be Served
Article IV Eligibility for Managed Long Term Care
- Populations Eligible for Enrollment
- Eligibility Requirements
- Populations Excluded from Enrollment
- Populations Exempted from Enrollment
Article V Obligations of the Contractor
- Provision of Benefits
- Eligibility Activities of Contractor
- Enrollment Process
- Disenrollment Policy and Process
- Enrollee Protections
- Quality Assurance and Performance Improvement Program
- Marketing
- Information for Potential Enrollees, Applicants and Enrollees
- Member and Provider Services
- Person Centered Service Planning and Care Management
- Consumer Directed Personal Assistance Services
- Enrollee Health and Welfare
- Advance Directives
- Use of Health Information Technology (HIT) to Link Services
- Duplicate CINs
- Contractor Responsibilities Related to Public Health
- Fair Hearings
- Aid Continuing
- Contractor Responsibilities to the Department
Article VI Payment
- Capitation Payments
- Modification of Capitation Rates during Contract Period
- Rate–Setting Methodology
- Payment of Capitation
- Denial of Capitation Payments
- Department Right to Recover Premiums and Contractor Duty to Repay
- Third Party Health Insurance Determination
- Other Insurance and Settlements
- Contractor Financial Liability
- Spenddown and Net Available Monthly Income
- No Recourse Against Enrollees
- Notification Requirements to LDSS Regarding Enrollees
- Contractor´s Fiscal Solvency Requirements
- Prohibition on Payments to Institutions or Entities Located Outside of the United States
- Managed Long Term Care Risk Corridor
- High Cost High Need Risk Pool
- Nursing Home Price Mitigation Pool
Article VII Contractor Relationship with Providers
- Provider Relations
- Full Responsibility Retained
- Required Provisions
- Network Requirements for Covered Services
- Provider Termination Notice
- Recovery of Over Payments to Providers
- Optometry Services Provided by Article 28 Clinics Affiliated with the College of Optometry of the State University of New York
- Dental Services Provided by Article 28 Clinics Operated by Academic Dental Centers not Participating in Contractor´s Network
- Department Exclusion or Termination of Providers
- Health Home Service and Care Management Coordination
- Service Verification Process
- Withholding of Payments
- Home Care Services Worker Wage Parity Rules
- Fair Labor Standards Act
Article VIII Records, Reporting and Certification Requirements
- General Requirements
- Maintenance of Contractor Performance Records, Records Evidencing Enrollment Fraud and Documentation Concerning Duplicate CINs
- Maintenance of Financial Records and Statistical Data
- Access to Contractor Records
- Retention Periods
- Reporting Requirements
- Data Certifications
- Notification of Changes in Reporting Due Dates Requirements or Formats
- Ownership and Related Information Disclosure
- Role of Compliance Officer and Compliance Committee
- Public Access to Records
- Certification Regarding Individuals Who have been Debarred or Suspended Federal or State Government
- Conflict of Interest Disclosure
- OMIG´s Right to Audit and Recover Overpayments Caused by Contractor Submission of Misstated Reports
- OMIG´s Right to Audit and Recover Overpayments Which Were Caused by the Contractor´s Misstated Encounter Data
- OMIG Audit Authority
- OMIG Compliance Review Authority
Article IX Intermediate Sanctions
Article X General Requirements
- Authorized Representative With Respect to Contract
- Confidentiality
- Additional Actions and Documents
- Relationship of the Parties, Status of the Contractor
- Nondiscrimination
- Employment Practices
- Dispute Resolution
- Assignment
- Binding Effect
- Limitation on Benefits of this Contract
- Entire Contract
- Conflicting Provisions
- Modification
- Headings
- Pronouns
- Notices
- Partial Invalidity
- Force Majeure
- Survival
- State Standard Appendix A
- Indemnification
- Environmental Compliance
- Energy Conservation
- Prohibition on Use of Federal Funds for Lobbying
- Waiver of Breach
- Choice of Law
- AA. Executory Provision and Federal Funds
- BB. Renegotiation
- CC. Affirmative Action
- DD. Omnibus Procurement Act of 1992
- EE. Nondiscrimination in Employment in Northern Ireland
- FF. Contract Insurance Requirements
- GG. Minority And Women Owned Business Policy Statement
- HH. Provisions Related to New York State Information Security Breach and Notification Act
- II. Accessibility of State Agency Web–based Intranet and Internet Information and Applications
- JJ. New York State Tax Law Section 5–a
- KK. Provisions Related to New York State Procurement Lobbying Law
- LL. Piggybacking
- MM. Lead Guidelines
- NN. Payment
- OO. M/WBE Utilization Plan for Subcontracting and Purchasing
- PP. On–going Vendor Responsibility
- QQ. Veterans Protections
APPENDICES
APPENDIX A Standard Clauses for New York State Contracts
APPENDIX B New York State Department of Health Guidelines for Contractor Compliance with the Federal Americans with Disabilities Act
APPENDIX C Certification Regarding Lobbying
APPENDIX D Standard Form LLL Disclosure of Lobbying Activities
APPENDIX E–1 Proof of Workers´ Compensation Coverage
APPENDIX E–2 Proof of Disability Insurance Coverage
APPENDIX F Service Area and Ages of Population Served
APPENDIX G Managed Long Term Care Covered and Non–Covered Services
APPENDIX H Schedule of Capitation Rates
APPENDIX I Reserved
APPENDIX J Definitions
APPENDIX K Grievance and Appeal System, Member Handbook Language and Service Authorization Requirements
APPENDIX L Managed Long Term Care Enrollee Rights
APPENDIX M Managed Long Term Care Plan Information Requirements
APPENDIX N Managed Long Term Care Risk Corridor
APPENDIX O Nursing Home Transition
APPENDIX P Conflict Free Evaluation and Enrollment Center
APPENDIX X Modification Agreement Form (to accompany modified appendices for
changes in term or consideration on an existing period or for renewal periods)
MANAGED LONG TERM CARE CONTRACT
This CONTRACT is hereby made by and between the State of New York Department of Health, hereinafter called the "Department" and _________________________, hereinafter called the "Contractor" identified on the face page hereof.
WHEREAS, the Department is the single State agency charged with the responsibility for administration of the New York State Medical Assistance Program (Medicaid), Title 11 of Article 5 of the Social Services Law (SSL); and
WHEREAS, the Contractor has been certified as a managed long term care plan pursuant to New York State Public Health Law (PHL) §4403–f; and
WHEREAS, the Contractor represents that the Contractor is able and willing to provide and arrange for health and long–term care services on a capitated basis in accordance with PHL §4403–f;
NOW, THEREFORE, in consideration of the foregoing and of the covenants and agreements hereinafter set forth, the Parties hereto agree as follows:
ARTICLE I
TERM OF CONTRACT, RENEWAL AND TERMINATION
A. Term of Contract
Term: The Contract shall begin on and, unless terminated sooner as permitted by the terms of this Contract, end on the dates identified on the face page hereof.
B. Renewal
The Department, with the approval of the State Comptroller or his designee, may extend the term of the Contract for up to one (1) additional two (2) year term or two (2) additional one–year terms. Standard Appendix X is the form to be used in extension of this Contract. The Department will provide written notice to the Contractor of extension of the term of the Contract at least ninety (90) days prior to the end of the term.
C. Termination of the Contract by the Department
- The Department shall have the right to terminate this Contract, if the Contractor, in the Department´s determination:
- takes any action that threatens the health, safety, or welfare of any Enrollee;
- has engaged in an unacceptable practice under 18 of the New York Codes, Rules and Regulations (NYCRR) part 515, that affects the fiscal integrity of the Medicaid program, or has engaged in an unacceptable practice pursuant to section B of Article IX of this Agreement;
- has failed to substantially comply with applicable standards of the PHL and regulations or has had its certificate of authority suspended, limited, or revoked;
- materially breaches this Contract or fails to comply with any term or condition of this Contract and such breach or failure is not cured within twenty (20) days, or such longer period as the Department may allow, of the Department´s notice of breach or noncompliance;
- becomes unable to meet its obligations in the normal course of business including but not limited to circumstances beyond its control and changes to the provider network affecting Enrollee access; or
- brings a proceeding voluntarily, or has a proceeding brought against it involuntarily, under Title 11 of the U.S. Code (the Bankruptcy Code), and the petition is not vacated within thirty (30) days of its filing.
- The Department shall give the Contractor written notice of termination of this Contract, specifying the applicable termination provision(s) and the effective date of termination.
D. Termination of the Contract by the Contractor
- The Contractor shall have the right to terminate this Contract if the Department:
- fails to make agreed–upon payments in a timely and accurate manner; or
- materially breaches the Contract or fails to comply with any material term or condition of this Contract.
- Contractor shall allow thirty (30) days, or such longer period as the Contractor may permit, from the time of the Contractor´s written notice of deficiency, for the Department to cure the identified deficiency.
- The Contractor shall give the Department written notice specifying the reason(s) for and the effective date of the termination, which shall not be less time than will permit an orderly disenrollment of Enrollees to the Medicaid Fee–For–Service (FFS) program or transfer to another Managed Long Term Care Plan (MLTCP), but no more than ninety (90) days.
E. Other Termination Reasons
- This Contract may be terminated by the Contractor or the Department as of the last day of any month upon no more than ninety (90) days prior written notice to the other Party so as to ensure an orderly transition. Notwithstanding this provision, the Contractor agrees to comply with sections F and G of this Article.
- This Contract shall be terminated immediately if federal financial participation in the costs hereof becomes unavailable or if state funds sufficient to fulfill the obligation of the Department hereunder are not appropriated by the New York State Legislature. The Department will give the Contractor prompt written notice of such termination of this Contract.
- This Contract may be terminated in accordance with the provisions of section BB of Article X of this Contract.
F. Contract Expiration and Contractor Termination/Phase–Out Plan
- The Contractor hereby agrees that in the event this Contract is terminated by either Party that the Contractor will continue to provide Covered Services to Enrollees until Enrollees are reinstated to FFS care or transferred to another MLTCP. To the extent that such services are provided by the Contractor to Enrollees prior to their disenrollment into a FFS program or transfer to another MLTCP, the Contractor will continue to be reimbursed a premium for such Enrollee. Upon expiration and non–renewal or termination of this Contract, the Contractor shall comply with the termination plan that the Contractor has developed and that the Department has approved.
- In the event that the Contractor gives notice to terminate this Contract, the Contractor shall submit a termination plan for Department approval with the Contractor´s notice of termination.
- In the event that the Department gives notice to terminate this Contract, the Contractor shall submit within fifteen (15) days of notice or such longer period as the Department may allow a termination plan for Department approval.
- Sixty (60) days prior to the date of termination, the Contractor shall advise all current Enrollees of the termination by regular first–class mail. In the event that the termination date is established less than sixty (60) days in advance, letters shall be mailed by regular first–class mail within five (5) days of the establishment of the termination date.
- The Contractor shall communicate with Local Department of Social Services (LDSS) or entity designated by the Department within fifteen (15) days of the establishment of the termination date to offer LDSS(s) or entity designated by the Department, assistance and information necessary to reinstate each Enrollee´s Medicaid benefits through the FFS system or facilitate enrollment in another MLTCP.
- As soon as a termination date has been established and appropriate notice given pursuant to this Contract by either the Contractor or the Department:
- The Contractor shall work with the LDSS or entity designated by the state to ensure enrollees are informed of their MLTCP and FFS options, and to effectuate transfer to the plan or option selected by the enrollee.
- the Contractor shall contact other community resources to determine the availability of other programs to accept the Enrollees into their programs;
- the Contractor shall assist Enrollees by referring them and by making their care management record and other enrollee service records available as appropriate to health care providers and/or programs;
- the Contractor shall establish a list of Enrollees that is prioritized according to those Enrollees requiring the most skilled care; and
- based upon the Enrollee´s established priority and a determination of the availability of alternative resources, individual person–centered service plans shall be developed by the Contractor for each Enrollee in collaboration with the Enrollee, the Enrollee´s family and appropriate community resources.
- In conjunction with such termination and disenrollment, the Contractor shall provide such other reasonable assistance as the Department may request in affecting that transition.
Upon completion of the person–centered service plan and reinstatement of the Enrollee´s Medicaid benefits through the FFS system or enrollment in another MLTCP, an Enrollee shall be disenrolled from the Contractor´s MLTCP. - Within sixty (60) days of the date of termination of the Contract, an accounting shall be prepared and submitted to the Department by or on behalf of the Contractor for the establishment of a sum to be repaid to the Department by the Contractor of funds advanced by the Department, if any, for coverage of Enrollees for periods subsequent to the date of termination.
- The Contractor shall maintain all books, records and other documents that may be required pursuant to this Contract regarding the MLTCP and make such records available to the Department and all authorized representatives of the state and federal government throughout the period that such records are required to be maintained pursuant to this Contract.
G. Effect of Termination on New Enrollments
Once either Party has given notice of its intentions to terminate this Contract, the Contractor shall suspend enrollment into its MLTCP, and if operating in a mandatory county, will be removed from auto assignment.
|top of section| |top of page|ARTICLE II
STATUTORY AND REGULATORY COMPLIANCE
- The Contractor agrees to operate in compliance with the requirements of this Contract, legislative and regulatory requirements including, but not limited to, 42 Code of Federal Regulation (CFR) Parts 434 and 438 and PHL §4403–f and other applicable provisions of PHL Articles 44 and 49.
- Covered services provided by the Contractor under this Contract shall comply with all standards of the New York State Medicaid Plan established pursuant to New York State Social Services Law (SSL) § 363–a and satisfy all other applicable requirements of SSL and PHL.
- The Contractor agrees to comply with all applicable laws, regulations, and rules including:
- Title VI of the Civil Rights Act of 1964 as implemented by regulations at 45 CFR Part 80;
- The Age Discrimination Act of 1975 as implemented by regulations at 45 CFR Part 91;
- The Rehabilitation Act of 1973 as implemented by regulations at 45 CFR Part 84;
- The Americans with Disabilities Act (ADA);
- The Health Insurance Portability and Accountability Act (HIPAA);
- Other laws applicable to recipients of federal funds; and
- The New York City Health Code for Contractors operating in New York City.
- The Contractor must comply with Title II of the ADA and section 504 of the Rehabilitation Act of 1973 for program accessibility and must develop an ADA Compliance Plan consistent with the New York State Department of Health Guidelines for Contractor Compliance with the ADA set forth in Appendix B, which is hereby made a part of this Agreement as if set forth fully herein. Said plan must be approved by the Department, be filed with the Department, and be kept on file by the Contractor.
- The Contractor is receiving federal payments under this Contract. The Contractor and subcontractors paid by the Contractor to fulfill its obligations under this Contract are subject to certain laws that are applicable to individuals and entities receiving federal funds. The Contractor agrees to inform all subcontractors that payments that they receive are, in whole or in part, from federal funds.
- In the event that any provisions of this Contract conflicts with the provisions of any statute or regulations applicable to a Contractor, the provisions of the statute or regulations shall have control.
- The Contractor agrees to abide by any and all applicable guidance issued in writing by the Department to MLTC partial capitation plans.
ARTICLE III
CONTRACTOR SERVICE AREA AND AGES OF POPULATION TO BE SERVED
- For purposes of this Contract, the Contractor´s service area shall consist of the geographic area described in Appendix F of this Contract, which is hereby made a part of this Contract as if set forth fully herein. The Contractor must request written Department approval to reduce or expand its service area for purposes of providing Managed Long Term Care (MLTC) services. In no event, however, shall the Contractor modify its service area until it has received such approval. Any modifications made to Appendix F as a result of an approved request to expand and/or reduce the Contractor´s service area shall become effective fifteen (15) days from the date of the written Department approval without the need for further action on the part of the parties to this Contract.
- The age groups to be served by the Contractor are identified in Appendix F of this Contract, which is hereby made a part of this Contract as if set forth fully herein. The Contractor must request written Department approval to make any changes in the age groups it serves under the Contract. In no event, however, shall the Contractor make such a change until it has received such approval. Any modifications made to Appendix F as a result of an approved request to change the age groups served by the Contractor under this Contract shall become effective fifteen (15) days from the date of the written Department approval without the need for further action on the part of the parties to this Contract.
ARTICLE IV
ELIGIBILITY FOR MANAGED LONG TERM CARE
A. Populations Eligible for Enrollment
- Mandatory Enrollment Counties:
Upon approval of the Department and CMS, counties are designated as Mandatory for MLTC (Mandatory). The Contractor will be notified at least sixty days in advance when a county is designated as Mandatory. In these counties, dual eligible individuals (having both Medicare and Medicaid), who are age 21 and older and who are assessed as needing community based long term care services listed in section B subsection 6 of this Article for more than 120 days must enroll in MLTC in order to receive those services. These individuals are defined as MLTC Mandatory Persons.
In Mandatory counties, the following may voluntarily enroll in MLTC:- dual eligible individuals, age 18–20, who have been assessed as eligible for nursing home level of care at time of enrollment and also assessed as needing community based long term care services for more than 120 days; and
- non–dual eligible individuals, age 18 and older, who have been assessed as eligible for nursing home level of care at time of enrollment and also assessed as needing community based long term care services for more than 120 days.
- Non–Mandatory Enrollment Counties:
In Non–Mandatory Enrollment Counties, the following may voluntarily enroll in MLTC:- dual eligible individuals, age 18 and older, who have been assessed as eligible for nursing home level of care at time of enrollment and also assessed as needing community based long term care for more than 120 days may choose to enroll in MLTC;
- non–dual eligible individuals age 18 and older, who are not otherwise considered mandatory for managed care, who have been assessed as eligible for nursing home level; and
- dual eligible individuals who are age 21 or older, who are assessed as needing community based long term care services for more than 120 days, may choose to enroll in MLTC.
B. Eligibility Requirements
Except as specified in section C of this Article, an Applicant who completes an enrollment agreement shall be eligible to enroll under the terms of this Contract if he/she:
- meets the age requirements identified in Appendix F;
- is a resident in the Contractor´s service area;
- is determined eligible for Medicaid by the LDSS or entity designated by the Department;
- is determined eligible for MLTC by the MLTCP, or entity designated by the Department, using an eligibility assessment tool designated by the Department;
- with the exception of districts designated as Mandatory for permanent Nursing Home enrollment (as defined in Article IV and Appendix O), is capable, at the time of enrollment, of returning to or remaining in his/her home and community without jeopardy to his/her health and safety, based upon criteria provided by the Department; and
- is expected to require at least one (1) of the following Community Based Long Term Care Services (CBLTCS) covered by the MLTCP for more than 120 days from the effective date of enrollment:
- nursing services in the home;
- therapies in the home;
- home health aide services;
- personal care services in the home;
- adult day health care;
- private duty nursing; or
- Consumer Directed Personal Assistance Services
- During the initial assessment process utilizing the Uniform Assessment System, the Contractor should ensure the Applicant demonstrates a documented functional or clinical need for one of the CBLTCS and clearly identify the service(s) in the plan of care. Social Day Care, as a covered service in the benefit package, can contribute to the total care plan but cannot represent the sole service provided to an Applicant.
- The potential that an Applicant may require acute hospital inpatient services or nursing home placement during such 120 day period shall not be taken into consideration by the Contractor when assessing an Applicant´s eligibility for enrollment.
C. Populations Excluded From Enrollment
- The following individuals cannot receive benefits through the MLTCP:
- Residents of psychiatric facilities;
- Residents of residential health care facilities at the time of enrollment;
- Individuals expected to be Medicaid eligible for less than six (6) months;
- Individuals eligible for Medicaid benefits only with respect to tuberculosis–related services;
- Individuals with a "county of fiscal responsibility" code of 99 (i.e., eligible only for breast and cervical cancer services) in eMedNY;
- Individuals receiving hospice services at the time of enrollment;
- Individuals with a "county of fiscal responsibility" code of 97 (i.e., residing in a state Office of Mental Health (OMH) facility) in eMedNY;
- Individuals with a "county of fiscal responsibility" code of 98 (i.e., individuals in an Office for People with Developmental Disabilities (OPWDD) facility or treatment center) in eMedNY;
- Individuals eligible for the family planning expansion program;
- Individuals under sixty–five (65) years of age in the Centers for Disease Control and Prevention breast and/or cervical cancer early detection program and need treatment for breast or cervical cancer, and are not otherwise covered under creditable health coverage;
- Residents of intermediate care facilities for the mentally retarded (ICF/MR);
- Individuals who could otherwise reside in an ICF/MR, but choose not to do so;
- Residents of alcohol/substance abuse long term residential treatment programs;
- Individuals eligible for Emergency Medicaid;
- Individuals in the OPWDD Home and Community Based Services section 1915(c) waiver program;
- Individuals in the following section 1915(c) waiver programs: Traumatic Brain Injury, Nursing Home Transition & Diversion, and Long Term Home Health Care Program; (until such time as final approval is given to the Long Term Home Health Care Program 1915(c) waiver amendment;
- Residents of Assisted Living Programs (ALP);
- Individuals in receipt of Limited Licensed Home Care Services; and
- Individuals in the Foster Family Care Demonstration.
- The Department has the right to make further modification to the excluded populations as necessary to implement statewide Medicaid program initiatives, including Medicaid Redesign initiatives. Contractor will comply with the elimination of Nursing Home exclusion and implement Nursing Home Transition enrollment protocol outlined in Appendix O, and as further defined in guidance issued by the Department.
D. Populations Exempted From Enrollment
- The following may request an exemption from receiving benefits through the MLTCP:
- Individuals aged 18–21 who are nursing home certifiable and require more than 120 days of community based long term care services;
- Native Americans;
- Individuals who are eligible for the Medicaid buy–in for the working disabled and are nursing home certifiable; and
- Aliessa Court Ordered Individuals.
ARTICLE V
OBLIGATIONS OF THE CONTRACTOR
A. Provision of Benefits
- The Contractor shall provide covered services set forth in Appendix G in accordance with the coverage and authorization requirements of 42 CFR 438.210; comply with professionally recognized standards of health care and implement practice guidelines consistent with 42 CFR 438.236; and comply with the requirements of 42 CFR 438.114 regarding emergency and post–stabilization services to the extent that services required to treat an emergency medical condition are within the scope of covered services in Appendix G.
- Benefit package services provided by the Contractor under this Contract shall comply with all standards of the State Medicaid Plan established pursuant to SSL §363–a and shall satisfy all applicable requirements of the PHL and SSL. Non–covered services for which the Enrollee is eligible under the Medicaid Program will be paid by the Department on a fee–for–service basis directly to the provider of service. The parties acknowledge and accept that the Department has the right to make modifications to the benefit package services (set forth in Appendix G) with advance notice to the Contractor of at least sixty (60) days. Such modifications may include expansions of and/or restrictions to such benefit package services, the addition of new benefit package services, and/or the elimination of benefit package services. Such modifications will be made only as necessary to implement statewide Medicaid program initiatives, including Medicaid Redesign initiatives.
- The Contractor shall allow each Enrollee the choice of Participating Provider of covered service to the extent possible and appropriate.
- The Contractor shall maintain and demonstrate to the Department´s satisfaction, a sufficient and adequate network for the delivery of all covered services either directly or through a network of contracted providers that meets the requirements in section D of Article VII of this Contract. The Contractor shall meet the standards required by 42 CFR 438.206 for availability of services; 42 CFR 438.207 for assurances of adequate capacity; and applicable sections of PHL and regulations. If the network is unable to provide necessary services under this Contract for a particular Enrollee, the Contractor agrees to adequately and timely furnish these services outside of the Contractor´s network for as long as the Contractor is unable to provide them within the network.
- The Contractor is financially responsible for Urgently Needed Services. Urgently Needed Services are covered only in the United States, the Commonwealth of Puerto Rico, the Virgin Islands, Guam, American Samoa and the Northern Mariana Islands. The Contractor may require the Enrollee or the Enrollee´s designee to coordinate with the Contractor or the Enrollee´s Primary Care Physician prior to receiving care.
- Services for which Enrollees can self–refer:
- Vision Services: The Contractor will allow its Enrollees to self–refer to Article 28 clinics that provide optometry services and are affiliated with the College of Optometry of the State University of New York to obtain covered optometry services as described in Article VII Section G of this Agreement.
- Dental Services: The Contractor will allow its Enrollees to self–refer to Article 28 clinics operated by academic dental centers to obtain covered dental services as described in Article VII Section H of this Agreement.
B. Eligibility Activities of Contractor
- Mandatory Counties
- Transitioning Patients
In Mandatory counties, for individuals transitioning from a Medicaid community based long term care program, the Contractor must:- accept the enrollment of all individuals who choose the Contractor´s plan or who are auto–assigned to the Contractor. These individuals are presumed to meet the eligibility requirements for MLTC and are not required to be assessed prior to enrollment. The Contractor will be notified of all such enrolled individuals by the LDSS or entity designated by the Department;
- continue to provide services authorized under the Enrollee´s pre–existing service plan for a minimum of ninety (90) days after enrollment, but may conduct a person–centered service plan and care management assessment pursuant to section J of Article V of this Agreement within thirty (30) days of enrollment; and
- issue a notice of action for any restriction, reduction, suspension or termination of authorized services, which clearly articulates the Enrollee´s right to file an appeal (either expedited, if warranted, or standard), the right to a fair hearing and external appeal, and the right to have authorized services continue when requesting a fair hearing.
- The MLTCP must submit monthly reports (within ten (10) business days of the close of each month) to the Department identifying instances when the MLTCP has issued a notice of action that involves a reduction of split shift or live–in services or when the MLTCP is reducing hours by twenty–five percent (25%) or more.
- The MLTCP must also submit a monthly report (within ten (10) business days of the close of the month) to the Department identifying the number of appeals and fair hearings requested as a result of the above reductions.
Auto–Assignment only applies in a county approved for Mandatory enrollment. The LDSS or entity designated by the Department will assign MLTC Mandatory Persons who have not chosen a MLTCP within the required time period to a MLTCP. Initially, auto–assignment will be made sequentially among all plans eligible for auto–assignment. The Department reserves the right to initiate an algorithm based on quality or other such factors when data for its development are available.
The Department may suspend or terminate a Contractor´s ability to receive auto– assigned enrollments for cause such as, but not limited to, quality of care issues, inability to process referrals timely, network inadequacy, or other issues that affect the Contractor´s operations.
- Transition from Mainstream Managed Care (MMC) to MLTC
- For individuals who enroll in Contractor´s MLTCP who were in receipt of CBLTC services from an MMC plan, and who were disenrolled either due to a change in Medicaid eligibility status or receipt of Medicare, Contractor must continue to provide services as described in Article V, Section B, Subsections 1.a.ii and 1.a.iii.
- Contractor shall enroll members of the Contractor´s MMC plan(s), and of such plans run by any affiliated entity such as a sister or managing corporation unless said entities themselves also have an MLTC plan, into the Contractor´s MLTC plan that are in receipt of Medicare, as identified on the monthly disenrollment file sent to the Contractor by the MMC Enrollment Broker or LDSS, and meet the requirements for eligibility in the MLTC plan otherwise stated in this Agreement.
- New Patients
For individuals requesting enrollment who are not currently receiving services, the Contractor will use the assessment instrument specified by the Department (currently the Uniform Assessment System (UAS)), to assess each Applicant for MLTC enrollment. The MLTCP may use additional tools that have been approved by the Department in its evaluation of Applicants.- Contractor will comply with the Conflict Free Evaluation and Enrollment Center enrollment protocols and implementation plan outlined in Appendix P, and as further defined in guidance issued by the Department.
- The Contractor´s initial assessment for MLTC eligibility must be conducted within thirty (30) days of first contact by an individual requesting enrollment or of receiving a referral from the Enrollment Broker or other source. This assessment must be performed by a Registered Nurse (RN) in the individual´s home.
- The Contractor must provide a monthly report to the Department or entity designated by the Department listing all individuals for whom an assessment was completed in a format determined by the Department. The report must include the name of the individual; the date of initial contact to the plan for individuals that were not referred by the LDSS or entity designated by the Department; and the date the MLTCP conducted its assessment for program eligibility. The report must be submitted within ten (10) business days of the close of each month.
- Transitioning and New Patients
- The Contractor shall maintain adequate documentation (including the UAS) for at least three (3) years to support the enrollment decision, which is subject to post enrollment audit by the Department or contracted entity.
- The Contractor will transmit an enrollment form completed by the Contractor to the LDSS or entity designated by the Department for enrollment processing.
- Transitioning Patients
- Non–Mandatory Counties
- In non–Mandatory counties, the Contractor will use the assessment instrument specified by the Department (currently the UAS) to assess each Applicant for eligibility for MLTC enrollment. The MLTCP may use additional tools that have been approved by the Department in its evaluation of Applicants.
- The initial assessment for MLTC eligibility must be conducted within thirty (30) days of first contact by an individual requesting enrollment or of receiving a referral from the Enrollment Broker or other source. This assessment must be performed by an RN in the individual´s home.
- The Contractor shall maintain documentation (including the UAS) for at least three (3) years to support the enrollment decision, which is subject to audit by the Department or contracted entity.
- The Contractor will transmit an enrollment form completed by the potential member to the LDSS or entity designated by the Department for enrollment processing.
- Mandatory and Non–Mandatory Counties
- The Contractor is permitted to find that the Applicant does not meet the eligibility criteria identified in sections A, B and C of Article IV of this Contract and notify the Applicant of that finding. However, should such Applicant want to pursue enrollment the Contractor must transmit the application to the entity designated by the Department in accordance with section B.2.d of this Article.
- The Contractor also is permitted to advise the Applicant that he/she does not meet the eligibility criteria identified in sections A, B and C of Article IV of this Contract and that the Contractor will recommend denial of enrollment of the Applicant to the LDSS or entity designated by the Department if the Applicant does not choose to withdraw his/her application pursuant to section B.3.f of this Article. Only the LDSS or entity designated by the Department may deny enrollment.
- If the Contractor operates in a service area which encompasses more than one (1) county (other than those that make up the City of New York), and the Contractor has knowledge that an Enrollee proposes to change residence from one county to another within the service area, to necessitate continuing Medicaid eligibility, the Contractor must notify the original LDSS or entity designated by the Department of the pending move.
- The Contractor shall accept applications and enrollment agreement forms in the order they are received, without selecting among forms and without regard to the capitation rate the Contractor will receive for such person. The Contractor shall not discriminate against eligible Applicants on the basis of health status or need for health care services.
- The Contractor agrees to transmit the signed enrollment application of the Applicant to the LDSS or entity designated by the Department on a timely basis. Applications submitted to the LDSS or entity designated by the Department by noon on the 20th day of the month will be accepted for enrollment on the first of the following month provided that the application is complete, and the Applicant has active Medicaid eligibility. The Contractor must notify the LDSS or entity designated by the Department if the Contractor is aware of the existence of duplicate Client Identification Numbers (CINs).
- An Applicant may withdraw an application or enrollment agreement by noon on the 20th day of the month prior to the effective date of enrollment by indicating his/her wishes orally or in writing. All withdrawals must be acknowledged in writing to the Applicant by the Contractor.
- In counties where the Conflict–Free Evaluation and Enrollment Center has not been implemented, the Contractor must continue to abide by Article V Section B Subsections 3.a and 3.b.
C. Enrollment Process
- The Contractor shall comply with enrollment policies and procedures developed by the Contractor and approved by the Department. Such written policies and procedures shall address all aspects of application processing and shall contain the assessment tools identified in Subsection B.1.c of this Article and other materials to be used by the Contractor in the enrollment process. The Contractor will use a Department approved enrollment agreement, or the standardized enrollment agreement developed by the Department, to transmit enrollment information to the LDSS or entity designated by the Department on a timely basis. The Contractor must submit any proposed material revisions to the approved enrollment policies and procedures for Department approval prior to implementation of the revised procedures.
- The Contractor will notify enrollment referral sources, including the LDSS or entity designated by the Department, as appropriate if the Applicant does not enroll. The Contractor will also send a written confirmation to the Applicant if the Applicant does not enroll in the MLTCP.
- An Enrollee shall be entitled to receive Covered Services as provided for herein as of the effective date of enrollment in the Contractor´s MLTCP which will be the first day of the month following the processing of the enrollment by the LDSS or entity designated by the Department.
- The Department or entity designated by the Department will provide to the Contractor a WMS/eMedNY "Exception Report" for any processed applications that are not accepted by WMS/eMedNY when WMS/eMedNY does not show the Applicant as Medicaid eligible.
- The Contractor will request written permission from the Department to suspend enrollment when the Contractor determines that it lacks access to sufficient or adequate resources to provide or arrange for the safe and effective delivery of Covered Services to additional Enrollees. Resumption of enrollment will occur only with Department approval, not to be unreasonably delayed, after written notice from the Contractor that adequately describes how the situation precipitating the suspension was corrected.
- The Department may establish enrollment limits based either on a determination of readiness or on limits established pursuant to PHL §4403–f.
- The Department shall send copies of all notices regarding suspension and resumption of enrollment to the LDSS or entity designated by the State for processing of enrollments.
- The surplus amount (spenddown or NAMI amount) to be billed to an Enrollee by the Contractor must be the amount for which the Enrollee is responsible as determined by the LDSS or entity designated by the Department. The Enrollee must be billed for the full surplus amount each month. The method of collection of surplus amounts is subject to the terms of the Contractor´s agreement with the Nursing Facility.
D. Disenrollment Policy and Process
- Disenrollment Policy
- The Contractor shall comply with disenrollment policies and procedures developed by the Contractor as approved by the Department. Such written policies and procedures shall address all aspects of disenrollment processing and shall contain the disenrollment forms and materials used by the Contractor. The Contractor must submit any proposed material revisions to the policies and procedures for Department approval prior to implementation of the revised procedures.
- The effective date of disenrollment shall be the first day of the month following the month in which the disenrollment is processed through eMedNY.
- Disenrollment by the Contractor may not be based in whole or in part on an adverse change in the Enrollee´s health or on the capitation rate payable to the Contractor. Disenrollment may not be initiated because of the Enrollee´s high utilization of covered medical services, diminished mental capacity, or uncooperative or disruptive behavior resulting from his/her special needs except as may be established under section D subsection 5.a of this Article.
- The Contractor shall continue to provide and arrange for the provision of covered services until the effective date of disenrollment. The Department will continue to pay capitation fees for an Enrollee until the effective date of disenrollment.
- In consultation with the Enrollee and other individuals designated by the Enrollee, prior to the Enrollee´s effective date of disenrollment, the Contractor shall make all necessary referrals to the LDSS or entity designated by the Department, another MLTCP or alternative services for which the MLTCP is not financially responsible, to be provided subsequent to disenrollment, when necessary, and advise the Enrollee in writing of the proposed disenrollment date.
- If an Enrollee is transferring from the Contractor´s MLTCP to another MLTCP or Medicaid Managed Care plan, the Contractor must provide the receiving plan with the individual´s current person–centered service plan in order to ensure a smooth transition.
- If an Enrollee is disenrolling from the Contractor´s MLTCP to receive services through an Assisted Living Program (ALP), the Contractor must pay the applicable Medicaid rate for the level of care for which the Enrollee is assessed using the Patient Review Instrument (PRI) or successor tool until the disenrollment from the MLTCP is processed. The Contractor is responsible for all other medically necessary services covered by the MLTC benefit package that are not included in the ALP rate until the disenrollment takes place.
- Enrollee–Initiated Disenrollment
- An Enrollee may initiate voluntary disenrollment at any time for any reason upon oral or written notification to the Contractor. The Contractor must provide written confirmation to the Enrollee of receipt of an oral request and maintain a copy in the Enrollee´s record. The Contractor shall attempt to obtain the Enrollee´s signature on the Contractor´s voluntary disenrollment form but may not delay the disenrollment while it attempts to secure the Enrollee´s signature on the disenrollment form. The effective date of disenrollment must be no later than the first day of the second month after the month in which the disenrollment was requested.
- An Enrollee who elects to join and/or receive services from another managed care plan capitated by Medicaid, a 1915(c)–waiver program or OPWDD Day Treatment program is considered to have initiated disenrollment from the MLTCP
- The Contractor must provide information and referral to Enrollees who are requesting disenrollment without a transfer to another MLTCP, managed care plan capitated by Medicaid or alternative service who require such services in order to be safely maintained. Such assistance could include, but not be limited to, referral to the Enrollment Broker or Adult Protective Services (APS), if necessary.
- Contractor Initiated Disenrollment
- An involuntary disenrollment is a disenrollment initiated by the Contractor without agreement from the Enrollee.
- An involuntary disenrollment requires approval by the entity designated by the Department.
- The Contractor agrees to transmit information pertinent to the disenrollment request to the entity designated by the Department in sufficient time to permit the entity to affect the disenrollment pursuant to the requirements of 42 CFR 438.56 (e)(1).
- Reasons the Contractor Must Initiate Disenrollment
If an Enrollee does not request voluntary disenrollment, the Contractor must initiate involuntary disenrollment within five (5) business days from the date the Contractor knows:- an Enrollee no longer resides in the service area;
- an Enrollee has been absent from the service area for more than thirty (30) consecutive days;
- an Enrollee is hospitalized or enters an OMH, OPWDD or OASAS residential program for forty–five (45) consecutive days or longer;
- an Enrollee clinically requires nursing home care but is not eligible for such care under the Medicaid Program´s institutional rules;
- an Enrollee is no longer eligible to receive Medicaid benefits;
- an Enrollee is not eligible for MLTC because he/she is assessed as no longer demonstrating a functional or clinical need for community–based long–term care services or, for non–dual eligible Enrollees, in addition no longer meets the nursing home level of care as determined using the assessment tool prescribed by the Department. An Enrollee whose sole service is identified as Social Day Care must be disenrolled from the MLTC plan. The Contractor shall provide the LDSS or entity designated by the Department the results of its assessment and recommendations regarding disenrollment within five (5) business days of the assessment making such determination; or
- an Enrollee is incarcerated. The effective date of disenrollment shall be the first day of the month following incarceration.
- A Contractor May Initiate an Involuntary Disenrollment if:
- An Enrollee or an Enrollee´s family member or other person in the home engages in conduct or behavior that seriously impairs the Contractor´s ability to furnish services to either that particular Enrollee or other Enrollees; provided, however, the Contractor must have made and documented reasonable efforts to resolve the problems presented by the individual. Consistent with 42 CFR 438.56(b), the Contractor may not request disenrollment because of an adverse change in the Enrollee´s health status, or because of the Enrollee´s utilization of medical services, diminished mental capacity, or uncooperative or disruptive behavior resulting from his/her special needs.
- An Enrollee fails to pay for or make arrangements satisfactory to the Contractor to pay the amount, as determined by the LDSS or entity designated by the Department, owed to the Contractor as spenddown/surplus within thirty (30) days after such amount first becomes due, provided that during that thirty (30) day period the Contractor first makes a reasonable effort to collect such amount, including making a written demand for payment and advising the Enrollee in writing of his/her prospective disenrollment.
- An Enrollee knowingly fails to complete and submit any necessary consent or release.
- An Enrollee provides the Contractor with false information, otherwise deceives the Contractor, or engages in fraudulent conduct with respect to any substantive aspect of his/her plan membership.
E. Enrollee Protections
- The Contractor shall have and comply with Department–approved written policies and procedures regarding internal grievances, grievance appeals, and appeals processes that are consistent with the Department´s grievance, grievance appeals, and appeals policies contained in Appendix K of this Agreement. These include notifying Enrollees who receive an adverse appeal resolution about their right to a Medicaid Fair Hearing and/or an External Appeal through the Department of Financial Services, where applicable. The Contractor may not act in any manner so as to restrict the Enrollee´s right to a fair hearing or influence an Enrollee´s decision to pursue a fair hearing. The Contractor must submit any proposed material revisions to the approved policies and procedures for Department approval prior to implementation of the revised policies and procedures.
- The Contractor agrees to adopt and maintain arrangements satisfactory to the Department to protect its Enrollees from incurring liability for payment of any fees that are the legal obligation of the Contractor. To meet this requirement the Contractor must:
- ensure that all contracts with providers prohibit the Contractor´s providers from holding any Enrollee liable for payment of any fees that are the legal obligation of the Contractor; and
- indemnify the Enrollee for payment of any fees that are the legal obligation of the Contractor for services furnished by providers that have been authorized by the Contractor to serve such Enrollee, as long as the Enrollee follows the Contractor´s rules for accessing services described in the approved member handbook.
- The Contractor shall develop and implement written policies and procedures regarding Enrollee rights which fulfill the requirements of 42 CFR 438.100 and applicable state laws and regulations. These policies should include, but are not limited to:
- Protecting the Enrollee´s right to receive information about the Contractor and managed long–term care in a manner which does not disclose the Enrollee as participating in the MLTC Plan, provided that inclusion of the Contractor´s name is not considered a violation of this provision.
- The Contractor will distribute and otherwise make available information about Enrollee rights contained in Appendix L of this Agreement to all Potential Enrollees, Applicants and Enrollees.
- The Contractor shall provide Enrollees receiving CBLTC in MLTC with information and access to APS.
- The Contractor will cooperate with, and may not inhibit, the Participant Ombudsman in the exercise of its duties.
- The Participant Ombudsman is an independent organization that provides free ombudsman services to long term care recipients in the state of New York. These services include, but are not necessarily limited to:
- providing pre–enrollment support, such as unbiased health plan choice counseling and general program–related information,
- compiling enrollee complaints and concerns about enrollment, access to services, and other related matters,
- helping enrollees understand the fair hearing, grievance and appeal rights and processes within the health plan and at the State level, and assisting them through the process if needed/requested, including making requests of plans and providers for records, and
- informing plans and providers about community–based resources and supports that can be linked with covered plan benefits.
- The Contractor must include information about the Participant Ombudsman program, including its purpose, scope and nature of its services, and contact information, in the MLTC Plan member handbook, enrollee materials, action and adverse determination notices, and all grievance or appeal notices or communications.
- The Contractor must also, upon request, provide the Participant Ombudsman entity with a current list of Participating Providers in Contractor´s MLTC Plan.
- The Participant Ombudsman is an independent organization that provides free ombudsman services to long term care recipients in the state of New York. These services include, but are not necessarily limited to:
F. Quality Assurance and Performance Improvement Program
- The Contractor must have a quality assurance and performance improvement program which includes a health information system consistent with the requirements of 42 CFR 438.242, and a Department approved written quality plan for ongoing assessment, implementation, and evaluation of overall quality of care and services. The Contractor must submit any proposed material revisions to the approved quality plan for Department approval prior to implementation of the revised plan. The quality assurance and performance improvement program must identify specific and measurable activities to be undertaken by the Contractor. The Contractor´s written quality plan must meet the requirements of Article 44 of PHL and implementing regulations and address the standards in 42 CFR 438.240 regarding quality assurance and performance improvement and 42 CFR 438.242 regarding the health information system and the following additional elements:
- Board level accountability for overall oversight of program activities and review of the QA/PI program, annual review and approval of the program by the board and periodic feedback to the board on the review process by oversight committees.
- Goals and objectives that provide a framework for quality assurance and improvement activities, evaluation and corrective action. These goals and objectives should be reviewed and revised periodically and should be supported by data collection activities which focus on clinical and functional outcomes, encounter and utilization data, and client satisfaction data.
- Standards for access, availability and continuity of service including, but not limited to:
- length of time to respond to requests for referrals,
- timeliness of receipt of covered services,
- timeliness of implementation of person–centered service plan, and
- telephone consultation to assist Enrollees in obtaining health information and, on a twenty–four (24) hour basis, urgent care.
- Quality indicators that are objective, measurable and related to the entire range of services provided by the Contractor and which focus on potential clinical problem areas (high volume service, high risk diagnoses or adverse outcomes). The methodology should assure that all care settings (e.g., day center, nursing home and in–home settings) will be included in the scope of the quality assurance and performance improvement program.
- A process to review the effectiveness of the Contractor´s ability to assess an Enrollee´s care needs, sustain an Enrollee´s informal supports, identify an Enrollee´s treatment goals, assess effectiveness of interventions, evaluate adequacy and appropriateness of service utilization, including the social and environmental supports, and amend the care delivery process, as necessary.
- Enrollee and caregiver involvement in quality assurance and performance improvement activities and evaluation of satisfaction with services.
- Establishment of a review committee(s) to:
- evaluate data collected pertaining to quality indicators, performance standards, and client satisfaction;
- make recommendations to the board regarding the process and outcomes of the quality assurance and performance improvement program; and
- provide input related to processes to evaluate ethical decision–making including end–of–life issues.
- Policies and procedures of the review committee should:
- define qualifications of individuals participating on the committee(s);
- include a method for identifying, selecting and reviewing data and information to be used in the quality assurance and performance improvement program;
- integrate the findings of the grievance and appeals process;
- define a process for recommending appropriate action to resolve problems identified as part of quality assurance and improvement activities, including
- providing feedback to appropriate staff and subcontractors; for monitoring effectiveness of corrective actions taken; and for reporting QA/PI findings to the board on at least an annual basis; and
- incorporate review of the care delivery process to include appropriate clinical professionals and paraprofessionals as well as non–clinical staff, as appropriate.
- The Contractor agrees to cooperate with any external quality review conducted by or at the direction of the Department.
G. Marketing
- The Contractor shall conduct marketing activities for Potential Enrollees consistent with 42 CFR 438.104, applicable state law and implementing regulations, including but not limited to 18 NYCRR 360–10.9.
- Marketing materials include any information produced by or on behalf of the Contractor that references MLTC concepts, is intended for general distribution and is produced in a variety of print, broadcast and direct marketing mechanisms.
- The Contractor shall comply with a marketing plan which has received written prior approval by the Department. If there are any material changes to the marketing plan, they must be submitted to the Department before implementation. The marketing plan shall describe marketing and enrollment goals, the specific activities to be undertaken to achieve the enrollment goals and identify the personnel who will carry out the marketing functions. The marketing plan should address each of the following:
- a description of how the Contractor will distribute marketing material in its service area approved by the Department;
- a listing and copies of the specific marketing formats to be used (e.g., radio announcements, letters, posters, brochures, handbooks, websites) and the forums for distribution or presentation (e.g., health fairs, provider offices, community events);
- evidence that the material is written in twelve (12) point type at a minimum and prose written in clear, simple, understandable language at the 4th to 6th grade reading level;
- a description of how the Contractor will market to Potential Enrollees who speak other than English as a primary language;
- the methods of making alternate formats available to persons who are visually and/or hearing impaired;
- the method and timetable for updating and disseminating the list of Participating Providers available to Potential Enrollees;
- a description of how the Contractor will assure that its Participating Providers comply with these provisions;
- a discussion as to if or how the Contractor plans to provide nominal gifts for the target population, addressing application of such gifts to ensure they are not construed as an offer of financial gain or service incentive to induce either enrollment or transfer;
- description of the personnel qualifications, the training content, methods and mechanisms for evaluation, supervision and reimbursement of marketing personnel;
- clear identification of prohibited practices, to include prohibition against conducting marketing activities in any hospital emergency rooms, treatment rooms, hospital inpatient rooms, locations where services are delivered in medical professional offices, Nursing Home or Adult Care Facility resident rooms, areas of Adult Day Health Care Programs where care is provided to registrants, or Social Day Care Centers; and accepting referrals from Social Day Care Centers;
- a description of how the Contractor will assure that only marketing materials which have received prior approval from the Department will be distributed; and
- description of the methods to be used by the Contractor to monitor and assure compliance with the approved marketing plan.
- The Contractor shall conduct marketing activities consistent with the following provisions:
- The Contractor may use radio, television, billboards, newspapers, leaflets, brochures, the Internet, yellow page advertisements, letters, posters and verbal presentations by marketing representatives at health fairs and other appropriate events to market its product.
- The Contractor shall not mislead, confuse, or defraud Potential Enrollees or misrepresent itself, the Department or CMS.
- The Contractor shall not use a health assessment form or other means to select among otherwise eligible Applicants.
- The Contractor may distribute marketing materials in local community centers, pharmacies, hospitals, nursing homes, home care agencies, doctors´ offices and other areas where Potential Enrollees are likely to gather or receive long term care services.
- The Contractor may conduct marketing activities at provider sites only with the permission of the provider, and at sites not prohibited by subsection 3.j of this section.
- The Contractor may not directly or indirectly engage in door to door, telephone or other "Cold Call" marketing activities.
- The Contractor shall ensure, through its agreements with Participating Providers, compliance with the provisions of this section.
- The Contractor shall, with the consent of Potential Enrollees, provide for the participation of family members and other informal caregivers during marketing encounters.
- The Contractor, in its marketing materials, shall offer only benefits or services that are clearly specified in this Contract and available for the full Contract period being marketed.
- The Contractor shall not offer monetary incentives to Medicaid recipients to join the MLTCP. Nominal gifts of no more than $5.00 fair market value may be offered as part of promotional activities to stimulate interest in the MLTCP as long as such gifts are made available to everyone regardless of whether they enroll.
- Marketing representatives shall be trained in the concepts of MLTC and all facets of the plan using the subject outline of the member handbook as a minimal basis for the training curriculum.
- The Contractor shall not offer financial and other kinds of incentives to marketing representatives based on the number of Medicaid recipients a representative has enrolled in the program.
- The Contractor may not seek to influence enrollment in conjunction with the sale or offering of any private insurance.
- All written materials used in carrying out the functions of this section, including but not limited to marketing materials, the enrollment agreement and attestation, and the member handbook, must be reviewed and approved by the Department prior to use. The Contractor shall comply with all requests from the Department for periodic reports on the performance of the Contractor´s responsibilities pursuant to this Section. The Contractor shall submit these reports within thirty (30) days of receiving the request from the Department.
- Funds provided pursuant to this Agreement shall not be used for any partisan political activity, or for activities that may influence legislation or the election or defeat of any candidate for public office.
H. Information for Potential Enrollees, Applicants and Enrollees
- The Contractor shall provide information to all Potential Enrollees, Applicants and Enrollees consistent with 42CFR 438.10, applicable state laws and implementing regulations, and Appendix M of this Agreement.
- The Contractor shall provide Potential Enrollees, Applicants and Enrollees information consistent with the following provisions.
- The Contractor shall comply with the Department´s requirements for language and format standards for information pursuant to 42CFR 438.10 (c) and (d).
- The Contractor shall provide the member handbook and the provider network to all Applicants prior to enrollment and to Enrollees.
- The Contractor shall give Enrollees prior written notice of significant changes to the information identified in subsection 2.b of this Section. Such notice shall be at least thirty (30) days prior to the effective date of the change pursuant to 42 CFR 438.10(f)(4).
- The Contractor shall annually notify Enrollees in writing of their disenrollment rights and their right to request the information specified in 42CFR 438.10 (f) (6) and (g).
- The Contractor shall provide all Potential Enrollees who were not referred to the Contractor by an enrollment broker with information (in a format determined by the Department) describing MLTC, a list of available MLTCPs and information about how to reach an enrollment broker for questions or other assistance. The Contractor shall report to the Department the number of Potential Enrollees receiving these materials on a quarterly basis (within fifteen (15) days of the close of each quarter) in a format to be determined by the Department.
- The Contractor must submit to the Department for prior approval a description of how the Contractor will provide information and annual notification to its Enrollees as required by this section, including:
- evidence that the material is written in twelve (12) point type at a minimum and prose is written in clear, simple, understandable language at the 4th to 6th grade reading level;
- the methods the Contractor will use to provide information to Applicants and Enrollees who speak other than English as a primary language;
- the methods of making alternate formats available to persons who are visually and/or hearing impaired; and
- the method and timetable for updating and disseminating the list of Participating Providers.
- The Contractor shall obtain a signature on the Enrollment Agreement which will provide evidence that each Applicant/Enrollee has:
- received a member handbook which included the rules and responsibilities of plan membership and which expressly delineates covered and non–covered services;
- agreed to the terms and conditions for plan enrollment stated in the member handbook;
- understood the conditions for enrollment and disenrollment;
- received a copy of the Contractor´s current provider network listing and agreed to use network providers for covered services;
- has been advised of the projected date of enrollment;
- the Contractor is required to reimburse Article 28 outpatient departments, diagnostic and treatment centers, federally qualified health centers, and office–based practitioners that provide medical language interpreter services for Enrollees with limited English proficiency (LEP) and communication services for people who are deaf and hard of hearing;
- An Enrollee with limited English proficiency shall be defined as an individual whose primary language is not English and who cannot speak, read, write or understand the English language at a level sufficient to permit the Enrollee to interact effectively with health care providers and their staff. The need for medical language interpreter services must be documented in the medical record; and
- Medical language interpreter services must be provided during a medical visit by a third party interpreter who is either employed by or contracts with the medical provider. These services may be provided either face–to–face or by telephone. The interpreter must demonstrate competency and skills in medical interpretation techniques, ethics and terminology. It is recommended, but not required, that such individuals be certified by the National Board of Certification for Medical Interpreters (NBCMI).
- The Contractor must provide information and referral to Enrollees who are involuntarily disenrolled to assist the individual to transfer to another MLTCP or Medicaid Managed Care plan or alternative service. Such assistance could also include, but is not to be limited to, referral to the Enrollment Broker or APS, if necessary.
- The Contractor shall ensure that the member handbook includes a description of all services available to Enrollees, including benefit plan services indicated in Appendix G, and other services which Enrollees may access through Medicaid Fee for Service, such as Hospice services. The Contractor shall update its member handbook to reflect any changes to such services.
- Effective January 1, 2016, health care services delivered by telehealth are covered by the Contractor. Telehealth delivered services use electronic information and communication technologies by telehealth providers to deliver health care services, which include the assessment, diagnosis, consultation, treatment, education, care management and/or self– management of an Enrollee. Telehealth provider means: physician, physician assistant, dentist, nurse practitioner, registered professional nurse (only when such nurse is receiving patient–specific health information or medical data at a distant site by means of remote patient monitoring), podiatrist, optometrist, psychologist, social worker, speech language pathologist, audiologist, midwife, certified diabetes educator, certified asthma educator, certified genetic counselor, hospital, home care agency, hospice, or any other provider determined by the Commissioner of Health pursuant to regulation. The Contractor is responsible for covering services in the benefit package that are delivered by telehealth in accordance with Section 2999–cc of the Public Health Law.
I. Member and Provider Services
- The Contractor is responsible for providing the following member services:
- explaining the Contractor´s rules for obtaining services and assisting Enrollees in making appointments;
- fielding and responding to Enrollee questions and grievances, and advising Enrollees of the prerogative to complain to the Department, LDSS, or State designated entity at any time;
- clarifying information in the member handbook for Enrollees;
- advising Enrollees of the Contractor´s grievance and appeals system, the service authorization process, and Enrollee´s rights to a fair hearing and/or external review;
- accommodating Applicants and Enrollees who require language translation and communications assistance;
- conducting post enrollment orientation activities, including orientation of Enrollees, Enrollees´ families or representatives, employees, management principles and operating practices;
- health promotion and wellness initiatives; and
- assisting Enrollees with the renewal of their Medicaid benefits.
- The Contractor shall develop and implement written procedures and protocols to assure that member and provider services are provided in a manner that is responsive to cultural considerations and specific needs of its Enrollees.
- Member services staff assisting Enrollees with understanding how to access services; their covered benefits; notices of Action or Action Appeal determinations; their complaint, appeal, or fair hearing rights; or providing Enrollees with information on the status of Service Authorization Requests, will ask the Enrollee if their questions were answered to their satisfaction. If the Enrollee remains unsatisfied, the staff member must offer the Enrollee the option to file a Complaint with the Contractor. The Contractor shall investigate and respond to such Complaints in accordance with Appendix K of this Agreement, and any applicable federal and State rules, regulations, and guidance.
J. Person Centered Service Planning and Care Management
- Person centered service planning and care management entails the establishment and implementation of a written care plan and assisting Enrollees to access services authorized under the care plan. Person centered service planning includes consideration of the current and unique psychosocial and medical needs and history of the Enrollee, as well as the Enrollee´s functional level and support systems. Care management means a process that assists the Enrollee to access necessary covered services as identified in the Person–Centered Service Plan (PCSP). Care management services include referral, assistance in or coordination of services for the Enrollee to obtain needed medical, social, educational, psychosocial, financial and other services in support of the PCSP, irrespective of whether the needed services are included in the Benefit Package.
- The Contractor shall comply with policies and procedures consistent with 42 CFR 438.210, Article 49 of the PHL, 10 NYCRR Part 98 and Appendix K of this Agreement that have received prior written approval from the Department. The Contractor agrees to submit any proposed material revisions to the approved coverage and authorization of services policies and procedures for Department approval prior to implementation of the revised procedures.
- The Contractor shall have and comply with written policies and procedures for care management consistent with the coordination and continuity requirements of 42CFR 438.208. The Contractor shall submit to the Department any proposed material revisions to the care management system prior to the implementation of the revised procedures.
- Notwithstanding any benefit or population–specific Medicaid fee–for–service (FFS) to MLTC transitional care policy described in this Agreement, the Contractor shall authorize and cover CBLTCS and ILTSS at the same level, scope and amount as the Enrollee received under the FFS Program for 90 days following Enrollment or until the Contractor´s PCSP is in place, whichever is later.
- Except where a Participating Provider Agreement describes an alternate arrangement for authorization of transitional care, the Contractor may not deny payment to providers of transitional care CBLTCS and ILTSS solely on the basis that the provider failed to request prior authorization.
- Where an existing medical order has or is about to expire, and a new medical order is required for the continued provision of CBLTCS and ILTSS during the transitional period but cannot be obtained after reasonable effort, the Contractor shall work with the CBLTCS and ILTSS provider to arrange a safe transition for the Enrollee, which may be to a higher level of care.
- The Contractor´s care management system shall ensure that care provided is adequate to meet the needs of individual Enrollees and is appropriately coordinated and shall consist of both automated information systems and operational policies and procedures. The Contractor´s care management system must:
- Provide a minimum of one care management telephone contact per month for each enrollee;
- Provide a minimum of one care management home visit every six (6) months for each enrollee, which can be included as part of any re–assessment but cannot be accommodated via a delegated arrangement solely to meet the Uniform Assessment System requirement;
- Ensure that the level and degree of care management and the Plan of Care for each enrollee address the needs of the enrollee and are based upon the acuity and severity of enrollees´ physical and mental conditions;
- Identify the ratio of care managers to enrollees taking into consideration a hierarchical structure based on the acuity and severity of enrollees´ physical and mental conditions. If care management is provided in a "team approach," then the Care Management Protocols must address how the team operates;
- Identify methods to educate and inform the enrollee, as applicable, about Consumer Directed Personal Assistance Services (CDPAS) and other service options when creating the Plan of Care with the enrollee after the assessment and reassessments;
- Identify a reasonable minimum required response time to enrollee/member contacts. This should be based upon a hierarchy of need triage principle, that taking into consideration the enrollee´s needs and types of request;
- Identify the qualifications needed of care managers to demonstrate that care managers have the appropriate background in health care and/or long–term care, and degrees in social work, nursing, and/or a related field;
- The process for documentation in a record system of required phone contacts and home visits; and
- If Care Management responsibilities are delegated, the Care Management Protocols must provide that Contractor shall timely notify the applicable Administrator of any new enrollees in the MLTC Plan, and enrollees that are disenrolled from the MLTC Plan.
- Such notice shall be consistent with when and how the MLTC Plan is notified by the Department and/or the enrollment broker of this information.
- The Contractor may contract with another entity for the provision of Care Management Services to the Contractor´s MLTC Plan Enrollees by entering into a Care Management Administrative Services (CMAS) agreement with such entity, utilizing the guidelines issued by the Department.
- A comprehensive reassessment of the Enrollee and a person–centered service plan update shall be performed as warranted by the Enrollee´s condition but in any event at least once every six (6) months.
- The Contractor shall ensure, in accordance with NY PHL 4403–f, and applicable guidance issued by the Department, the proper coordination of care for enrollees who elect to receive Hospice benefits.
- The Contractor shall develop a person–centered service planning and care management system consistent with the following provisions:
- The Contractor shall arrange for health care professionals, as appropriate, including but not limited to, a registered nurse, social workers, and member services coordinator, to provide person–centered service planning and care management services to all Enrollees. Every effort should be made to involve the Enrollee´s physician(s) in person–centered service plan development and monitoring.
- The Contractor shall ensure that meetings related to an Enrollee´s person–centered service plan will be held at a location, date and time convenient to the Enrollee and his/her invited participants.
- Person Centered service planning and Care management services include, but are not limited to the following:
- Development of a person–centered service plan based on initial assessments and reassessments of the Enrollees. The assessments must use a person–centered process that identifies the strengths, capacities and preferences of the Enrollee as well as identifying the Enrollee´s long–term care needs and the resources available to meet those needs.
- The person–centered service plan must address all of the Enrollee´s assessed needs (including health and safety risk factors) and personal goals, emphasizing services being delivered in home and community–based settings and maintenance of community integration for the Enrollee.
- The person–centered service plan must include care management of covered services and coordination of non–covered services and any other services provided by other providers, community resources and informal supports.
- Development of a back–up plan to ensure that needed assistance will be provided in the event that the regular services in the person–centered service plan are temporarily unavailable.
- Development of individual person–centered service plans, in consultation with the Enrollee and his/her chosen informal supports, specifying personal and health care goals, the types, scope, amount and frequency of authorized covered services that will be delivered as part of the person–centered service plan as well as non–covered services and supports necessary to maintain the person–centered service plan.
- Assuring that Enrollees are offered a choice of network service providers.
- Have policies and procedures for monitoring the progress of each Enrollee to evaluate whether the covered services provided are appropriate and in accordance with the patient centered service plan.
- Evaluating whether the person–centered service plan continues to meet the Enrollee´s needs must occur and be documented at least every six (6) months or more frequently if the Enrollee´s condition changes.
- Enrollees who have been served by the Contractor and who subsequently elect hospice as a result of a qualifying illness or condition may continue to be enrolled in the MLTCP. Upon hospice enrollment, the Contractor must reevaluate its person–centered service plan in consultation with the hospice in order to coordinate person–centered service plans and avoid duplication or conflict.
- The person–centered service planning and care management system includes processes for:
- generating and receiving referrals among all providers (including health care and behavioral health providers);
- sharing clinical and treatment plan information;
- obtaining consent to share confidential medical and treatment plan information among providers consistent with all applicable state and federal laws and regulations;
- providing Enrollees with written notification of the person–centered service plan including authorized services;
- permitting Enrollees to request a change to the person–centered service plan if an Enrollee´s circumstances necessitate a change;
- enlisting the involvement of community organizations that are not providing covered services, but are otherwise important to the health and well–being of Enrollees;
- assuring that the organization of and documentation included in the care management record meet all applicable professional standards;
- providing care coordination of all services the Enrollee receives including transitions between care settings such as hospital to nursing home and nursing home to home; and
- Discharge planning so that the Contractor makes all reasonable attempts to work with all inpatient facilities and home care providers to develop discharge plans for their Enrollees. As part of discharge planning, the Contractor will arrange for and authorize covered services as medically necessary for the Enrollee´s care.
- The care management system requires care managers to have access to participating medical and social services professionals and para–professionals who on a routine basis provide direct care and services as required by the Enrollee´s status.
- The Contractor will make reasonable efforts to effectively communicate with providers and Enrollees during the PCSP development process regarding the need to obtain authorization for the services included in the PCSP, the timing of such reviews and when the Contractor has made its determination, so as to facilitate understanding of when any disagreements among the care planning team are to be resolved through the Contractor´s Grievance System.
K. Consumer Directed Personal Assistance Services (CDPAS)
- Pursuant to SSL § 365–f, CDPAS is a MLTCP covered benefit. The Department will notify the Contractor of the effective date of implementation of CDPAS as a covered benefit of the MLTCP. The Contractor must enter into agreements with Fiscal Intermediaries (FI) in its service area that provide payroll and other employer responsibilities for CDPAS. The FIs also assist CDPAS Enrollees with training, counseling and information for effectively directing and managing CDPAS. The Contractor must attest to the Department that it has an adequate network of FIs before covering CDPAS.
- The Contractor must ensure that all prospective and current Enrollees are:
- notified that CDPAS is an available voluntary benefit;
- provided with information explaining the CDPAS benefit;
- provided with information explaining available alternatives to the CDPAS benefit; and
- permitted to utilize the CDPAS benefit if requested.
- The Enrollee may designate a legal or non–legal representative to assist with or assume employer responsibilities for CDPAS. Such representative may not act as the Enrollee´s personal assistant.
- The Contractor is responsible for comprehensive assessment and development of a person–centered service plan for all MLTC services for Enrollees using CDPAS. However, the Contractor must permit CDPAS Enrollees (or an Enrollee´s representative) to have decision making authority regarding CDPAS staff:
- Recruitment;
- Training;
- Scheduling;
- Evaluation;
- Time sheet verification and approval; and
- Discharge.
- A CDPAS Enrollee may voluntarily disenroll from the self–directed option and receive traditional services through the MLTCP.
- A CDPAS Enrollee may be involuntarily disenrolled from the self–directed option if:
- continued participation in CDPAS would not permit the Enrollee´s health, safety or welfare needs to be met;
- the Enrollee demonstrates the inability to self–direct by consistently demonstrating a lack of ability to carry out the tasks needed to self–direct services; or
- there is fraudulent use of Medicaid funds such as substantial evidence that the Enrollee has falsified documents related to CDPAS.
- Any restriction, reduction, suspension or termination of authorized CDPAS (including CDPAS itself) or denial of a request to change CDPAS is considered an adverse determination which may be appealed by the Enrollee pursuant to 42 CFR Part 438 and for which the Enrollee may request a fair hearing or external appeal upon a final adverse determination.
- The Contractor shall inform FIs of its claim´s procedures. The Contractor shall process all claims and pay clean claims in a timely manner, as determined by the agreement with the FI, and notify FIs in writing as to the reason(s) claims are fully or partially denied. The Department may require a plan of correction, impose sanctions or take other regulatory action should it determine the Contractor consistently delays payments to FIs without due cause.
L. Enrollee Health and Welfare
- The Contractor must have policies and procedures for identifying, addressing and seeking to prevent critical incidents, which include instances of abuse, neglect and exploitation of its Enrollees, on a continuous basis. The Contractor is required to provide critical incident monitoring and investigations of critical incidents including but not limited to:
- wrongful death;
- use of restraints;
- medication errors that resulted in injury; and
- any other incidents as determined by the Department.
- The Contractor must submit critical incident reports to the Department regarding Enrollee health and welfare pursuant to Article VIII of this Contract.
M. Advance Directives
The Contractor must provide all directives and information to Enrollees with respect to their rights under PHL Articles 29–B and 29–C. The Contractor shall, in compliance with 42 CFR 438.6(i) and 422.128, maintain written policies and procedures for advance directives and provide written information to Enrollees with respect to their rights under PHL Articles 29–B and 29–C to formulate advance directives and of the Contractor´s policies regarding the implementation of such rights. The Contractor shall include in such written notice to the Enrollee materials relating to Advance Directives and health care proxies as specified in 10 NYCRR 98–1.14 (f) and 700.5.
N. Use of Health Information Technology (HIT) to Link Services
Contractors will make use of available HIT and access data through the regional health information organization/qualified entities to conduct these processes (as feasible) in order to comply with the Initial Standards detailed below. The Contractor must provide the Department with a plan to achieve the Final Standards detailed below within twenty–four (24) months of Contract execution.
- Initial Standards:
- Contractor has structured information systems, policies, procedures and practices to create, document, execute and update a person–centered service plan for every Enrollee.
- Contractor has a systematic process to follow–up on services and referrals which are incorporated into the Enrollee´s person–centered service plan.
- Contractor has a care management record system which allows the Enrollee´s health information and person–centered service plan to be accessible to the team of providers and which allows for population management and identification of gaps in care including preventive services.
- Contractor makes use of available HIT and accesses data through the regional health information organization/qualified entity to conduct these processes, as feasible.
- Final Standards:
- Contractor has structured interoperable HIT systems, policies, procedures and practices to support the creation, documentation, execution and ongoing management of a person–centered service plan for every Enrollee.
- Contractor uses an electronic health record system that qualifies under the Meaningful Use provisions of the HITECH Act, which allows the Enrollee´s health information and person–centered service plan to be accessible to the team of providers. If such a system is not currently available, a plan must be submitted for when and how it will be implemented.
O. Duplicate CINs
The Contractor, within five (5) business days of identifying cases where a person may be enrolled in the Contractor´s MLTCP under more than one CIN or has knowledge of an Enrollee with more than one active CIN, must convey that information in writing to the LDSS, or entity designated by the Department. Contractor must also notify the Department and must return any and all payments made to Contractor as a result of a duplicate CIN to the Department in a manner determined by the Department.
Notwithstanding the foregoing, the Department always has the right to recover managed care organization (MCO) premiums paid for persons who have concurrent enrollment in one or more MCO products under more than one CIN.
P. Contractor Responsibilities Related to Public Health
The Contractor shall provide the Department with information as requested to facilitate epidemiological investigations.
The Contractor shall make reasonable efforts to assure timely and accurate compliance by Providers with public health reporting requirements related to communicable diseases and conditions mandated in PHL Article 21 and, for Contractors operating in New York City, the New York City Health Code (24 RCNY 11.03 – 11.07).
The Contractor shall make reasonable efforts to assure timely and accurate compliance by Providers with other mandated reporting requirements.
The Contractor shall provide health education to Enrollees on an on–going basis through methods such as posting information on the Contractor´s web site, distribution (electronic or otherwise) of Enrollee newsletters, health education classes or individual counseling on preventive health and public health topics, such as:
- Injury prevention;
- Domestic violence;
- HIV/AIDS, including availability of HIV testing and sterile needles and syringes;
- STDs, including how to access confidential STD services;
- Smoking cessation;
- Asthma;
- Immunization;
- Mental health services;
- Diabetes;
- Screening for cancer;
- Chemical dependence;
- Physical fitness and nutrition;
- Cardiovascular disease and hypertension;
- Dental care, including importance of preventive services such as dental sealants; and
- Screening for Hepatitis C for individuals born between 1945 and 1965.
Q. Fair Hearings
- Contractor shall appear at all scheduled fair hearings concerning its clinical determinations and/or Contractor–initiated disenrollment´s, in conjunction with the LDSS or entity designated by the state, to present evidence as justification for its determination or submit written evidence as justification for its determination regarding the disputed benefits and/or services. If Contractor will not be making a personal appearance at the fair hearing, the written material must be submitted to OAH at least three (3) business days prior to the scheduled hearing and contain a phone number by which the hearing officer may contact a Contractor´s representative, who has knowledge of the issue under review, during the hearing. If the hearing is scheduled fewer than three (3) business days after the request, Contractor must deliver the evidence to the hearing site no later than one (1) business day prior to the hearing, otherwise Contractor must appear in person. Notwithstanding the above provisions, Contractor may be required to make a personal appearance at the discretion of the hearing officer and/or the Department.
- The Contractor must provide to the Enrollee or the Enrollee´s authorized representative copies of the documents the Contractor will present at the fair hearing, also known as the "evidence packet." Copies of the evidence packet must be provided without charge. Within ten (10) business days of receiving notification of a hearing request, the Contractor must mail copies of the evidence packet to the Enrollee or the Enrollee´s authorized representative. If, due to the scheduling of the fair hearing, the evidence packet cannot be prepared at least five (5) business days before the hearing, and there is not sufficient time for the evidence packet to be mailed, the Contractor must provide the Enrollee or the Enrollee´s authorized representative such copies no later than at the time of the hearing.
- Upon request, the Contractor must provide the Enrollee or the Enrollee´s authorized representative access to the Enrollee´s case file and provide copies of documents contained in the file. If so requested, copies of the case file must be provided without charge and within a reasonable time before the date of the hearing. If the request for copies of the case file is made less than five (5) business days before the hearing, the Contractor must provide the Enrollee and the Enrollee´s authorized representative such copies no later than at the time of the hearing. Such documents must be provided to the Enrollee and the Enrollee´s authorized representative by mail within a reasonable time from the date of the request if the Enrollee or the Enrollee´s authorized representative request that such documents be mailed; provided however, if there is insufficient time for such documents to be mailed and received before the scheduled date of the hearing, such documents may be presented at the hearing instead of being mailed.
- Despite an Enrollee´s request for a State fair hearing in any given dispute, Contractor is required to maintain and operate in good faith its own internal Complaint and Appeal processes as required under state and federal laws and by Article V and Appendix K of this Agreement. Enrollees may seek redress of Adverse Determinations simultaneously through Contractor´s internal process and the State fair hearing process. If Contractor has reversed its initial determination and provided the service to the Enrollee, Contractor may request a waiver from appearing at the hearing and, in submitted papers, explain that it has withdrawn its initial determination and is providing the service or treatment formerly in dispute.
- Contractor shall comply with all determinations rendered by OAH at fair hearings.
- Contractor shall cooperate with the Department efforts to ensure that Contractor is in compliance with fair hearing determinations. Failure by Contractor to maintain such compliance shall constitute breach of this Agreement. Nothing in this Section shall limit the remedies available to the Department, LDSS or the federal government relating to any non–compliance by Contractor with a fair hearing determination or Contractor´s refusal to provide disputed services.
- If the Contractor believes there is an error of law or fact in the fair hearing decision, pursuant to 18 NYCRR Part 358–6.6, the Contractor may not pend compliance with the fair hearing decision while seeking a correction or review of the decision from OAH.
- If the Department investigates a Complaint that has as its basis the same dispute that is the subject of a pending fair hearing and, as a result of its investigation, concludes that the disputed services and/or benefits should be provided to the Enrollee, Contractor shall comply with the Department´s directive to provide those services and/or benefits and provide notice to the Enrollee to which services have been authorized. The Contractor may request a waiver from appearing at the hearing and, in submitted papers, explain that it has withdrawn its initial determination and is providing the service or treatment formerly in dispute.
- If the Department, through its Complaint investigation process, or OAH, by a determination after a fair hearing, directs Contractor to provide a service that was initially denied by Contractor, Contractor may either directly provide the service, arrange for the provision of that service or pay for the provision of that service by a Non–Participating Provider. If the services were not furnished during the period the fair hearing was pending, the Contractor must authorize or furnish the disputed services promptly and as expeditiously as the Enrollee´s health condition requires.
- Contractor agrees to abide by changes made to this Section of the Agreement with respect to the fair hearing, Action, Service Authorization, Complaint and Appeal processes by the Department in order to comply with any amendments to applicable state or federal statutes or regulations.
- Contractor agrees to identify a contact person within its organization who will serve as a liaison to the Department for the purpose of receiving fair hearing requests, scheduled fair hearing dates and adjourned fair hearing dates and compliance with State directives. Such individual: shall be accessible to the State by e–mail; shall monitor e–mail for correspondence from the State at least once every business day; and shall agree, on behalf of Contractor, to accept notices to Contractor transmitted via e–mail as legally valid.
- The information describing fair hearing rights, aid continuing, Action, Service Authorization, utilization review, Complaint and Appeal procedures shall be included in all MLTC member handbooks and shall comply with this Agreement.
- Contractor shall bear the burden of proof at hearings regarding the restriction, reduction, suspension or termination of ongoing services. In the event that Contractor´s initial adverse determination is upheld as a result of a fair hearing, any aid continuing provided pursuant to that hearing request, may be recouped by Contractor.
R. Aid Continuing
- Pursuant to 42 CFR §438.420, SSL §365–a(8), and 10 NYCRR §360–10.8(g)(2), the Contractor is required to continue the provision of an Enrollee´s Benefit Package services that are the subject of a fair hearing (hereafter referred to as "aid continuing") if so ordered by the NYS Office of Administrative Hearings (OAH) under the following circumstances:
- Contractor has or is seeking to restrict, reduce, suspend or terminate a treatment or Benefit Package service currently being provided; and
- Enrollee has filed a timely request for a fair hearing with OAH; and
- There is a valid order for the treatment or service from a Participating Provider.
- If so ordered by OAH, the Contractor shall be responsible for providing aid continuing until one of the following occurs:
- the Enrollee withdraws the request for aid continuing or the fair hearing;
- OAH issues a fair hearing decision adverse to the Enrollee; or
- except in the case of a restriction or home bound Enrollee, the provider order has expired.
- The Contractor shall provide aid continuing in a manner and duration as ordered by OAH.
- The Contractor shall not cease to provide aid continuing until:
- OAH determines that the Enrollee is not entitled to aid continuing;
- the Enrollee withdraws the request for aid continuing or the fair hearing; or
- OAH completes the administrative process and/or issues a fair hearing decision.
- If the Contractor believes the Enrollee is not eligible for aid continuing, the Contractor may provide documentation of such to OAH and seek rescission of the aid continuing order.
- The Contractor shall not cease to provide aid continuing until:
- If the services and/or benefits in dispute have been restricted, terminated, suspended, or reduced and the Enrollee timely requests a fair hearing, Contractor shall, at the direction of either the Department or LDSS, restore the disputed services and/or benefits consistent with the provisions of this Agreement.
S. Contractor Responsibilities to the Department
Contractor agrees to identify a contact person within its organization who will serve as a Governmental relations liaison to the Department for the purpose of receiving Departmental inquiries, requests, and notifications regarding policy or programmatic matters.
Such individual: shall be accessible to the State by e–mail; shall monitor e–mail for correspondence from the State at least once every business day; and shall agree, on behalf of Contractor, to accept notices to Contractor transmitted via e–mail as legally valid.
|top of section| |top of page|ARTICLE VI
PAYMENT
A. Capitation Payments
- Compensation to the Contractor shall consist of a monthly capitation payment for each Enrollee.
- In compliance with PHL §4403–f, monthly capitation rates shall reflect savings to both state and local governments when compared to costs which would be incurred by such programs if Enrollees were to receive comparable health and long term care services on a fee–for–service basis in the geographic region for which services are provided.
- The monthly Capitation Rates are attached hereto as Appendix H and shall be deemed incorporated into this Contract without further action by the parties.
- The monthly capitation payment to the Contractor shall constitute full and complete payments to the Contractor for all services that the Contractor provides pursuant to this Agreement subject to the risk corridor provision that is detailed in section O of this Article for the period of January 1, 2012 through December 31, 2012.
- Capitation Rates shall remain in effect until such time as modifications are made pursuant to sections B and C of this Article.
B. Modification of Capitation Rates during Contract Period
- Any technical modification to Capitation Rates, during the term of the Agreement as agreed to by the Contractor, including but not limited to changes in Premium Groups, or Benefit Package, shall be deemed incorporated into this Contract without further action by the parties upon approval of such modifications by the Department and the U.S. Department of Health and Human Services (DHHS).
- Any other modification to Capitation Rates, as agreed to by the Department and the Contractor during the term of the Agreement, shall be deemed incorporated into this Contract without further action by the parties upon approval of such modifications by the Department, the State Division of the Budget and DHHS as of the effective date of the modified Capitation Rates as established by the Department and approved by the State Division of the Budget and DHHS.
- In the event that the Department and the Contractor fail to reach agreement on modifications to the monthly Capitation Rates, the Department will provide formal written notice to the Contractor of the amount and effective date of the modified Capitation Rates approved by the State Division of the Budget and DHHS. The Contractor shall have the option of terminating this Contract if such approved modified Capitation Rates are not acceptable. In such case, the Contractor shall give written notice to the Department and the LDSS, or entity designated by the Department, within thirty (30) days of the date of the formal written notice of the modified Capitation Rates from the Department specifying the reasons for and effective date of termination. The effective date of termination shall be ninety (90) days from the date of the Contractor´s written notice, unless the Department determines that an orderly disenrollment to Medicaid fee–for–service (FFS) or transfer to another MLTCP can be accomplished in fewer days. The terms and conditions in the Contractor´s phase–out plan specified in Article I of this Contract must be accomplished prior to termination. During the period commencing with the effective date of the Department´s modified Capitation Rates through the effective date of termination of the Contract, the Contractor shall have the option of continuing to receive capitation payments at the expired Capitation Rates or at the modified Capitation Rates approved by the Department and the State Division of the Budget and DHHS for the rate period.
- If the Contractor fails to exercise its right to terminate in accordance with this Section, then the modified Capitation Rates, approved by the Department and the State Division of the Budget, shall be deemed incorporated into this Contract without further action by the parties as of the effective date of the modified Capitation Rates as established by the Department and approved by the State Division of the Budget.
C. Rate–Setting Methodology
- Capitation rates shall be determined prospectively and shall not be retroactively adjusted to reflect actual Medicaid FFS data or Contractor experience for the time period covered by the rates. Capitated rates shall be certified to be actuarially sound in accordance with 42 CFR §438.6(c).
- Notwithstanding the provisions set forth in subsection 1 of this section, the Department reserves the right to terminate this Agreement in its entirety pursuant to section C of Article I of this Agreement, upon determination by the Department that the aggregate monthly Capitation Rates are not cost effective pursuant to PHL § 4403–f.
D. Payment of Capitation
- The monthly capitation payment for each Enrollee is due to the Contractor from the Effective Date of Enrollment until the Effective Date of Disenrollment of the Enrollee or termination of this Contract, whichever occurs first. The Contractor shall receive a full month´s capitation payment for the month in which disenrollment occurs. The roster generated by the Department, along with any modification communicated electronically or in writing by the Department, the LDSS, or entity designated by the Department, prior to the end of the month in which the roster is generated, shall be the enrollment list for purposes of eMedNY premium billing and payment. The Contractor, the LDSS, or entity designated by the Department may develop protocols for the purpose of resolving roster discrepancies that remain unresolved beyond the end of the month.
- Upon receipt by the fiscal agent of a properly completed claim for monthly capitation payments submitted by the Contractor pursuant to this Contract, the fiscal agent will promptly process such claim for payment through eMedNY and use its best efforts to complete such processing within thirty (30) business days from date of receipt of the claim by the fiscal agent. Processing of Contractor claims shall be in compliance with the requirements of 42 CFR 447.45. The fiscal agent will also use its best efforts to resolve any billing problem relating to the Contractor´s claims as soon as possible. In accordance with section 41 of the State Finance Law, the Department, LDSS, or entity designated by the Department shall have no liability under this Contract to the Contractor or anyone else beyond funds appropriated and available for payment of Medical Assistance care, services and supplies.
E. Denial of Capitation Payments
In the event that CMS denies payment for new or existing Enrollees based upon a determination that the Contractor failed to comply with federal statutes and regulatory requirements, the Department will deny capitation payments to the Contractor for the same Enrollees for the period of time for which CMS denies payment.
F. Department Right to Recover Premiums and Contractor Duty to Repay
- The parties acknowledge and accept that the Department has a right to recover premiums paid to the Contractor for Enrollees listed on the monthly roster who are later determined, for the entire applicable payment month, to have been incarcerated; to have moved out of the Contractor´s service area; or to have died. The Department has the right to recover premiums from the Contractor in instances where the Enrollee was inappropriately enrolled into the plan with a retroactive effective date, or when the enrollment period was retroactively deleted. Additionally, the Department may recover premiums in all cases where no services are provided during the applicable period, unless the Contractor demonstrates that it was at risk for provision of medical services for any portion of the payment period. Instances where the Contractor is not at risk include, but are not necessarily limited to, circumstances where the enrollee was not eligible for services, or where providers in fact refused or failed to render any services. Notwithstanding the foregoing, the Department always has the right to recover duplicate premiums paid for persons enrolled under more than one CIN in the Contractor´s MLTCP whether or not the Contractor has made payments to providers. All recoveries will be made pursuant to guidelines developed by the Department. The Department will not allow, under any circumstance, duplicate payments for an Enrollee.
- The parties acknowledge and accept that the Department has the right to recover premiums paid to the Contractor for Enrollees listed on the monthly roster where the Contractor has failed to initiate involuntary disenrollment in accordance with the timeframes and requirements contained in subsection 4. of Article V Section D of this Agreement. The Department may recover the premiums effective on the first day of the month following the month in which the Contractor was required to initiate the involuntary disenrollment.
- The Contractor, within five (5) business days of identifying cases where a person may be enrolled in the Contractor´s MLTCP under more than one CIN or has knowledge of an Enrollee with more than one active CIN, must convey that information in writing to the LDSS, or entity designated by the Department. Contractor must also notify the Department and must return any and all payments made to Contractor as a result of a duplicate CIN to the Department within five (5) business days and in a manner determined by the Department.
G. Third Party Health Insurance Determination
- Point of Service (POS)
- The Contractor will make diligent efforts to determine whether Enrollees have third party health insurance (TPHI). The LDSS or entity designated by the Department is also responsible for making diligent efforts to determine if Enrollees have TPHI and to maintain third party information on the WMS/eMedNY Third Party Resource System. If TPHI coverage is known at the POS, the MLTCP shall use the TPHI information to coordinate benefits (e.g., alert the provider and ask them to bill the TPHI that should be primary to the MLTCP).
- The Contractor shall make good faith efforts to coordinate benefits and must inform the LDSS or entity designated by the Department of any known changes in status of TPHI eligibility within five (5) business days of learning of a change in TPHI. The Contractor may use the Roster as one method to determine TPHI information.
- Post Payment and Retroactive Recovery
- The Department, and/or its vendor will also be vested with the responsibility to collect any reimbursement for Benefit Package services obtained from TPHI. In no instances may an Enrollee be held responsible for disputes over these recoveries. A recovery shall not exceed the encounter data paid claim amount.
- The Department will continue to identify available TPHI and post this information to eMedNY. The TPHI information will appear on the Contractor´s next roster and TPHI file. The Contractor will have six (6) months from the later of the date the TPHI has been posted (eMedNY transaction date) or the Contractor´s claim payment date to pursue any recoveries for medical services. All recoveries outside this period will be pursued by the Department.
- For Department–initiated and Department–identified recoveries, the Department will direct providers to refund the Department directly. In those instances where the provider adjusted the recovery to the Contractor in error, the Contractor will refund the adjusted recovery to the Department.
- TPHI Reporting
- The Contractor shall report TPHI activities through the Medicaid Encounter Data System (MEDS III), or its successor system, and Medicaid Managed Care Operating Report (MMCOR) in accordance with instructions provided by the Department. To prevent duplicative efforts, the Contractor shall, on a quarterly basis, share claim specific TPHI disposition (paid, denied, or recovered) information with the Department. If no information is received from the Contractor, the Department will assume there are no retroactive recoveries being pursued by the Contractor and will initiate recovery processing.
H. Other Insurance and Settlements
The Contractor is not allowed to pursue cost recovery against personal injury awards or settlements that the Enrollee has received. Any recovery against these resources is to be pursued by the Medicaid program and the Contractor cannot take action to collect these funds. Pursuit of Workers Compensation benefits and No–fault Insurance by the Contractor is authorized, to the extent that they cover expenses incurred by the Contractor.
I. Contractor Financial Liability
The Contractor shall not be financially liable for any services rendered to an Enrollee prior to his/her effective date of enrollment or subsequent to disenrollment.
J. Spenddown and Net Available Monthly Income
Capitation rates are adjusted to exclude Enrollee spenddown and NAMI as determined by the LDSS or entity designated by the Department. The surplus amount (spend down or NAMI amount) to be billed to an Enrollee by the Contractor must be the amount for which the Enrollee is responsible as determined by the LDSS or entity designated by the Department. The method of collection of NAMI is subject to the terms of the Contractor´s agreement with the nursing facility. The Contractor´s inability to collect funds from Enrollees will not change the MLTCP´s spenddown or NAMI adjustment. The Contractor shall report the gross amount of spenddown and NAMI for each Enrollee in accordance with the timeframes and in the format prescribed by the Department.
K. No Recourse Against Enrollees
Except for the rates and payments provided for in this Contract, the Contractor hereby agrees that in no event, including but not limited to nonpayment by the Medicaid agency, insolvency of the Contractor, loss of funding for this program, or breach of this Contract, shall the Contractor or a subcontractor bill, charge, collect a deposit from, seek compensation, remuneration, or reimbursement from, or have any recourse against any Enrollee or person acting on his/her behalf for covered services furnished in accordance with this Contract.
This section shall not prohibit the Contractor (or subcontractors as specified in their agreements with the Contractor) from billing for and collecting any applicable surplus amounts, NAMI, Medicare billable expenses, commercial insurance, Worker´s Compensation benefits, No–fault insurance, and coordination of benefit amounts. This section supersedes any oral or written contrary agreement now existing or hereinafter entered into between the Contractor and any Enrollee or persons acting on his/her behalf. This provision shall survive termination of this Contract for any reason.
L. Notification Requirements to LDSS or Entity Designated by the Department Regarding Enrollees
- The Contractor agrees to notify the LDSS or entity designated by the Department in writing when an Enrollee with a monthly spenddown is admitted to an inpatient facility so the spenddown can be recalculated and a determination made regarding the amount, if any, of the spenddown owed to the inpatient facility. The notification will include the Enrollee´s name, Medicaid number, hospital name and other information as directed by the Department.
- The Contractor agrees to notify the LDSS or entity designated by the Department in writing prior to admission of an Enrollee to a nursing facility, to allow Medicaid eligibility to be redetermined using institutional eligibility rules. The notification will include the Enrollee´s name, Medicaid number, nursing facility name and other information as directed by the Department. If such an Enrollee is determined by the LDSS or entity designated by the Department to be ineligible for Medicaid nursing facility services, the LDSS or entity designated by the Department will notify the Contractor of such determination.
M. Contractor´s Fiscal Solvency Requirements
The Contractor, for the duration of this Agreement, shall remain in compliance with all applicable state requirements for financial solvency for MCOs participating in the Medicaid Program. The Contractor shall continue to be financially responsible as defined in PHL §4403(1)(c) and shall comply with the contingent reserve fund and escrow deposit requirements of 10 NYCRR Part 98 and must meet minimum net worth requirements established by the Department and the New York State Department of Financial Services. The Contractor shall make provisions, satisfactory to the Department, to protect the Department and the Enrollees in the event of MCO or subcontractor insolvency, including but not limited to, hold harmless and continuation of treatment provisions in all provider agreements which protect the Department and Enrollees from costs of treatment and assures continued access to care for Enrollees.
N. Prohibition on Payments to Institutions or Entities Located Outside of the United States
Effective no later than June 1, 2011, the Contractor is prohibited under section 6505 of the Affordable Care Act (ACA), which amends section 1902(a) of the Social Security Act, from making or directing payments for Medicaid covered items or services to any financial institution or entity, such as provider bank accounts or business agents, located outside of the United States, District of Columbia, Puerto Rico, the Virgin Islands, Guam, the Northern Mariana Islands and American Samoa.
O. Managed Long Term Care Risk Corridor
For all enrollments into a MLTCP effective January 1, 2012 through December 31, 2012, the Contractor and the Department will participate in a risk sharing arrangement. The risk sharing between the Department and the Contractor will be an aggregate test of the cost (excluding administration costs) to the Contractor of caring for the new Enrollee cohort during 2012 versus the Medicaid premium (excluding administration costs) paid by the Department to the Contractor. The chart attached to this Contract as Appendix N represents an example of the possible structure for the risk corridor for risk sharing. The calculation of the monies owed to the Contractor by the Department (if any) or monies owed to the Department by the Contractor (if any) will be calculated approximately ninety (90) days following the end of the calendar year 2012 to allow for sufficient runout of claims. An assessment tool for all new Enrollees must be submitted on a monthly basis by the Contractor to the Department under the risk sharing arrangement. The Department will provide any applicable Medicaid FFS data on new Enrollees to the Contractor. The risk sharing arrangement may be renewed for an additional one (1) year if mutual interest exists.
P. High Cost High Need Risk Pool
During the period of April 1, 2014 through March 31, 2015, the Contractor will participate in a High Cost High Need Risk Pool which will be administered by the Department. The purpose of the Pool is to mitigate the additional costs incurred by MLTCP´s which have a disproportionate share of high needs members.
Disproportionate share is defined as a member mix, on a percentage basis, that is greater than average. High needs members are defined as those members requiring 12–24 hours per day of personal care service or community–based ventilator patients, as identified in encounter data or other reporting requirements provided by the Contractor as defined by the Department or entity designated by the Department.
The Pool will be funded by a 2% withholding from the monthly capitation payments which would otherwise be payable to the Plan for enrollments during the period of April 1, 2014 through March 31, 2015. All withheld funds will be distributed by the Department to MLTCPs which have a disproportionate share of high needs members. In the event that no disproportionate share exists, the Department shall remit payment of all withheld funds in its entirety.
The Department will evaluate the use of the Pool and other financing arrangements to validate that fund payments are not duplicative of each other. Capitation rates resulting from the implementation of the Pool, reflecting a 2% withholding and/or reflecting distribution of withheld funds, shall be certified to be actuarially sound in accordance with 42 CFR §438.6(c).
The Department shall have the right to terminate the Pool if another method to mitigate the risk of high needs patients is implemented, or if the Department determines for any other reason that the Pool is no longer necessary.
Q. Nursing Home Price Mitigation Pool
During the period of January 1, 2015 through December 31, 2016 or later subject to CMS approval, the Contractor will participate in a regional Nursing Home Price Mitigation (NHPM) Pool which will be administered by the Department. The purpose of the Pool is to mitigate the additional costs incurred by MLTCPs which have a disproportionate share of members residing in higher priced nursing homes in their provider networks. Distributions from the Pool will be calculated no less frequently than annually.
Plans will be required to provide the Department with data regarding their contract rates with nursing homes in their network, and the number of plan enrollees residing in each facility during each calendar month. The frequency of this reporting requirement will be determined by the Department. Average nursing home rates will be calculated for each managed care region.
Disproportionate share is defined as having a high number and/or percentage of members of a plan who are residing in nursing homes which have a per diem rate that is higher than the regional average.
The NHPM Pool will initially be funded by a 5% withholding from the nursing home component of the monthly capitation payments which would otherwise be payable to the Contractor for enrollments during the period of January 1, 2015 through December 31, 2016 or later subject to CMS approval. This percentage will be re–evaluated annually and may be reduced with appropriate notice to plans. The withheld percentage will not exceed 5%.
All withheld fund will be redistributed by the Department to MLTCPs which have a disproportionate share of nursing home–resident members residing in home with above average costs. Funds will be distributed by adjusting the per month rate for each impacted Contractor. In the event that no disproportionate share exists, the Department shall refund payment of all withheld funds in their entirety.
The Department will evaluate the use of the Pool and other financial arrangements to validate that fund payments are not duplicative of each other. Capitation rates resulting from the implementation of the Pool, reflecting a maximum 5% withholding and/or reflecting distribution of withheld funds, shall be certified to be actuarially sound in accordance with 421 CFR §438.6(c). The Department shall have the right to terminate the Pool if another method to mitigate the additional costs of higher priced nursing homes is implemented, or if the Department determines for any reason that the Pool is no longer necessary.
|top of section| |top of page|ARTICLE VII
CONTRACTOR RELATIONSHIP WITH PROVIDERS
A. Provider Relations
- Pursuant to 42 CFR 438.206, the Contractor must maintain a network of appropriate providers that is supported by written agreements and is sufficient to provide adequate access to all services covered under the Contract. To be considered accessible, the network must contain a sufficient number and array of providers to meet the diverse needs of the Enrollee population. This includes being geographically accessible and being physically accessible according to the ADA standards.
- The Contractor agrees to comply with applicable sections of PHL and regulation regarding provider contract requirements, provider relations and termination and federal requirements at 42CFR 434.6 and 438.6(l) regarding required provider contract provisions, 438.12 regarding provider discrimination prohibitions, 438.102 regarding provider–Enrollee communications, 438.214 regarding provider selection, and 438.230 regarding provider contract relationships and delegation.
- Provider Services
The Contractor is responsible to provide the following provider services through its Provider Manual and other mechanisms:- assisting providers with prior authorization and referral protocols;
- assisting providers with claims payment procedures;
- fielding and responding to provider questions and complaints;
- orientation of providers to program goals; and
- provider training to improve integrations and coordination of care.
- Communication with Patients
The Contractor shall instruct its Participating Providers regarding the following requirements applicable to communications with their patients about the MMC and FHPlus products offered by the Contractor and other MCOs with which the Participating Providers may have contracts:- Participating Providers who wish to let their patients know of their affiliations with one or more MCOs must list each MCO with whom they have contracts.
- Participating Providers who wish to communicate with their patients about managed care options must advise patients taking into consideration ONLY the managed care options that best meet the health needs of the patients. Such advice, whether presented verbally or in writing, must be individually based and not merely a promotion of one MLTCP over another.
- Participating Providers may display the Contractor´s outreach materials provided that appropriate material is conspicuously posted for all other MCOs with whom the Participating Provider has a contract.
- Upon termination of a Provider Agreement with the Contractor, a provider that has contracts with other MCOs that offer MMC and FHPlus products may notify their patients of the change in status and the impact of such change on the patient.
B. Full Responsibility Retained
- Notwithstanding any relationship(s) that the Contractor may have with providers, the Contractor shall maintain full responsibility for adhering to and otherwise fully complying with all applicable laws and regulations, this Contract, all standards and procedures approved by the Department for the MLTCP and the written instructions of the Department.
- The Contractor shall oversee and is accountable to the Department for all functions and responsibilities that are described in this Contract.
- The Contractor may only delegate activities or functions to a provider in a manner consistent with requirements set forth in this Contract, 42 CFR Parts 434 and 438 and applicable state laws and regulations.
- The Contractor may only delegate management responsibilities as defined by state regulation by means of a Department approved management services agreement. Both the proposed management services agreement and the proposed management entity must be approved by the Department pursuant to the provisions of 10 NYCRR 98–1.11, and in compliance with the Management Services Agreement Guidelines issued by the Department, before any such agreement may be implemented.
C. Required Provisions
- The Contractor shall have a formal process for credentialing providers on a periodic basis (initially and not less than once every three (3) years) and for monitoring provider performance. For providers that are not subject to licensure or certification requirements (other than Social Day Care), the Contractor shall establish alternative mechanisms to ensure the health and safety of Enrollees which could include such activities as criminal background checks or review of abuse registries. The Contractor shall enter into contracts only with providers who are in compliance with all applicable state and federal licensing, certification, and other requirements; and are generally regarded as having a good reputation; and have demonstrated capacity to perform the needed contracted services. All provider contracts must meet the requirements of this Contract and applicable state and federal laws and regulations.
- Although there is not a specific license or certification, in order to be assured of Enrollee health and safety, all providers of Social Day Care services must meet the standards and requirements of 9 NYCRR 6654.20.
- Prior to entering into contract with a provider of Social Day Care services, and on an annual basis thereafter, Contractors are required to conduct a site visit of each such provider in their network to review and assure compliance with:
- 9 NYCRR 6654.20,
- the terms of the contract between the provider and Contractor, and
- all other standards required by law or regulation for the operation of said provider, including but not limited to laws, codes, and regulations regarding the facility´ structure, labor requirements, and food quality.
- Contracts between Contractor and any provider of Social Day Care Service must specify that said provider will:
- adhere to and identify, in the contract between Contractor and said provider, all building laws, codes, and regulations applicable to the particular provider,
- adhere to all laws, codes, and regulations applicable to the provision of food,
- regularly report to the Contractor any issues related to appeals or grievances, and
- participate in applicable quality assurance and performance improvement initiatives.
- Prior to entering into contract with a provider of Social Day Care services, and on an annual basis thereafter, Contractors are required to conduct a site visit of each such provider in their network to review and assure compliance with:
- Provider contracts shall require the approval of the Department as set forth in PHL §4402 and in 10 NYCRR Part 98, and consistent with guidelines issued by the Department
- The Contractor shall impose obligations and duties on its providers, including its Participating Providers, that are consistent with this Contract, and that do not impair any rights accorded to the Department or DHHS, Office of the Medicaid Inspector General (OMIG), Office of the State Comptroller (OSC) or the New York State Office of the Attorney General.
- No contract, including any provider contract, shall limit or terminate the Contractor´s duties and obligations under this Agreement.
- Nothing contained in this Agreement between the Department and the Contractor shall create any contractual relationship between any provider of the Contractor, including Participating Providers, or with any Non–Participating Provider or third party and the Department. Nothing in this paragraph shall be construed to limit the authority of the New York State Office of the Attorney General to commence any action pursuant to 31 § 3729 et seq., State Finance Law § 187 et seq., Social Services Law § 145–b or other New York or Federal statutes, regulations or rules.
- Any contract entered into by the Contractor shall fulfill the requirements of 42 CFR Part 434 and 438 that are appropriate to the service or activity delegated under such contract.
- The Contractor shall also ensure that, in the event the Contractor fails to pay any provider, including any Participating Provider, in accordance with the contract or provider agreement, the contractor or Participating Provider will not seek payment from the Department, the Enrollees, or their eligible dependents.
- No contract between the Contractor and a health care provider shall contain any clause purporting to transfer to the health care provider, other than a medical group, by indemnification or otherwise, any liability relating to activity, actions or omissions of the Contractor as opposed to those of the health care provider.
- All contracts with providers of covered services (including management agreements, if applicable), shall include the following provisions:
- Any services or other activities performed by a provider in accordance with a contract between the provider and the Contractor will be consistent and comply with the Contractor´s obligations under this Contract and applicable state and federal laws and regulations.
- A provision that the Contractor will provide, no less than thirty (30) days prior to implementation, any new rules or policies and procedures regarding quality improvement, service authorizations, member appeals and grievances and provider credentialing, or any changes thereto, to a provider of covered services that is a subcontractor.
- No provision of the provider contract is to be construed as contrary to the provisions of PHL Article 44 and implementing regulations to the extent they do not conflict with federal law and 42 CFR Parts 434 and 438.
- Specific delegated activities and reporting responsibilities, including the amount, duration and scope of services to be provided.
- Satisfactory remedies, including termination of a provider contract when the Department or the Contractor determines that such parties have not performed adequately which includes but is not limited to egregious patient harm, significant substantiated complaints, submitting claims to the MLTCP for services not delivered, and refusal to participate in the plan´s quality improvement program.
- Provision for ongoing monitoring of the provider´s compliance with the provider contract by the Contractor. Such monitoring provision shall specify requirements for corrective action, revocation of the provider contract or imposing sanctions if the provider´s performance is inadequate.
- A procedure for the resolution of disputes between the Contractor and its providers. Any and all such disputes shall be resolved using the Department´s interpretation of the terms and provisions of this Contract and portions of provider contracts executed hereunder that relate to services pursuant to this Contract. If a provider contract provides for arbitration or mediation, it must expressly acknowledge that the Commissioner of the Department of Health is not bound by arbitration or mediation decisions. Arbitration or mediation must occur within New York State, and the provider contract must provide that the Commissioner will be given notice of all issues going to arbitration or mediation and copies of all decisions.
- A provision specifying how the provider shall participate in the Contractor´s quality assurance, service authorization and grievance and appeals processes, and the monitoring and evaluation of the Contractor´s plan.
- A provision specifying how the provider will insure that pertinent contracts, books, documents, papers and records of their operations are available to the Department, DHHS, the Comptroller of the State of New York and the Comptroller General of the United States and/or their respective designated representatives, for inspection, evaluation and audit, through six (6) years from the final date of the provider contract or from the date of completion of any audit, whichever is later.
- A provision that the statutes, rules and regulations, and applicable Medicaid Updates of the Medicaid program and of the Department related to the furnishing of medical care, services, or supplies provided directly by, or under the supervision of, or ordered, referred, or prescribed by Participating Providers enrolled in an MCO, apply to such Participating Providers and any subcontractors, regardless of whether the Participating Provider or subcontractor is an enrolled Medicaid provider, including 18 NYCRR 515.2, except to the extent that any reference in the regulations establishing rates, fees, and claiming instructions will refer to the rates, fees and claiming instructions set by the MCO.
- The Contractor agrees to comply with State Insurance Law §3224–appertaining to prompt payment to providers of covered services.
- The Contractor shall not enter into any agreement with any Participating Provider, Non– Participating Provider, subcontractor or third party that would limit any right to commence an action or to obtain recovery from such providers by the State, including, but not limited to, the New York State Office of the Attorney General, the Department, OMIG and OSC, even under circumstances where the Contractor has obtained an overpayment recovery from a provider. Nothing in this Agreement shall be construed to limit the amount of any recovery sought or obtained by the New York State Office of the Attorney General, The Department, OMIG, and OSC from any Contractor, Participating Provider, Non– Participating Provider, subcontractor, or from any third party.
- The Contractor must enter into alternate payment arrangements with providers. The arrangements must be an alternative to fee for service such as shared savings, capitation, pay–for–performance, etc. The Contractor must submit a proposed plan to the Department by December 1st of each year to identify which providers will be impacted by the alternate payment arrangements, the type of arrangements the Contractor has implemented or plans to implement, and the percent of provider payments impacted. The Contractor must increase the percent of total provider payments that are made using a model of reimbursement that is an alternative to traditional fee for service in a manner determined by the Department.
D. Network Requirements for Covered Services
- The Contractor must demonstrate and maintain, to the Department´s satisfaction, a sufficient and adequate network for delivery of all covered services.
- The Contractor shall provide documentation to demonstrate capacity to serve the expected enrollment in its service area. The documentation shall be submitted quarterly through the Health Commerce System (HCS) in such format specified by the Department which will permit the Department to review accessibility compliance. Such submission must comply with the requirements of 42 CFR 438.207 and applicable sections of state law and implementing regulations.
- The Contractor shall have a minimum of two (2) providers that are accepting new Enrollees in each county in its service area for each covered service in the benefit package unless the county has an insufficient number of providers licensed, certified or available in that county as determined by the Department.
- Providers of covered services to which an Enrollee must travel must be geographically accessible for the enrolled population. Travel times shall must not exceed:
- Thirty (30) minutes from the Enrollee´s residence in metropolitan areas; or
- Thirty (30) miles from the Enrollee´s residence in non–metropolitan areas.
- If the Contractor is unable to provide necessary services through its contracted network for a particular Enrollee, the Contractor agrees to adequately and timely furnish these services outside of the Contractors´ network for as long as the Contractor is unable to provide them within the network.
- Contractor shall post its provider directory on the Contractor´s website to enable Prospective Enrollees, Enrollees, family members and supports, or others providing guidance and assistance to Prospective Enrollees and Enrollees to review the contracted network. The website must clearly identify to which MLTC product the network applies if the Contractor offers more than one MLTC product.
- Provider contracts and material amendments thereto shall require the approval of the Department as set forth in PHL § 4402 and 10 NYCRR Part 98, and consistent with guidelines issued by the Department.
E. Provider Termination Notice
The Contractor shall provide the Department at least sixty (60) days´ notice prior to the termination of any Provider Contract, the termination of which would preclude an Enrollee´s access to a covered service by provider type under this Contract and specify how services previously furnished by the Provider will be provided. In the event a Provider Contract is terminated on less than sixty (60) days´ notice, the Contractor shall notify the Department immediately but in no event more than seventy–two (72) hours after notice of termination is either issued or received by the Contractor.
F. Recovery of Overpayments to Providers
- Consistent with the exception language in State Insurance Law §3224–b, the Contractor shall have and retain the right to audit participating providers´ claims for a six (6) year period from the date the care, services or supplies were provided or billed, whichever is later, and to recoup any overpayments discovered as a result of the audit. This six (6) year limitation does not apply to situations in which fraud may be involved or in which the provider or an agent of the provider prevents or obstructs the Contractor´s auditing.
- The parties acknowledge that the New York State Office of the Attorney General, the Department, the Office of the Medicaid Inspector General (OMIG) and the Office of the State Comptroller (OSC) have the right to recover overpayments, penalties, and other damages from Participating Providers, Non–Participating Providers, Contractors, subcontractors, and third parties in the Contractor´s network as a result of any investigation, audit or action commenced by the New York State of the Attorney General, the Department, OMIG, and OSC, including, but not limited to any litigation brought pursuant to State Finance Law § 187 et seq. or 31 U.S.C. § 3729 et seq. The Contractor shall not have a right to recover from the State any recovery obtained by the State pursuant to 31 U.S.C. § 3729 et seq., State Finance Law § 187 et seq., or other New York or Federal statutes, regulations or rules.
- The parties agree that where the Contractor has previously recovered overpayments, by whatever mechanism utilized by the Contractor, from a Participating Provider, said overpayment recovery shall not be recovered from that Participating Provider for any such previously recovered identifiable claims that are the subject of a further investigation, audit or action commenced by the agencies listed in Section 22.7b.
- The parties agree that where the Contractor has recovered overpayments from a Participating Provider, the Contractor shall retain said recoveries.
- Nothing in this Agreement shall be construed to limit the authority of the New York State Office of the Attorney General, OMIG, OSC, or the Department to investigate, audit or otherwise obtain recoveries from any Participating Provider, Non–Participating Provider, Contractor, subcontractor, or third party.
G. Optometry Services Provided by Article 28 Clinics Affiliated with the College of Optometry of the State University of New York.
- Consistent with Chapter 37 of the Laws of 2010 amending SSL § 364–j, optometry services provided by Article 28 clinics affiliated with the College of Optometry of the State University of New York may be accessed directly by Enrollees without the Contractor´s prior approval and without regard to network participation.
- The Contractor will reimburse non–participating Article 28 clinics affiliated with the College of Optometry of the State University of New York for covered optometry services provided to Enrollees at Article 28 Medicaid fee–for–service (FFS) clinic rates.
H. Dental Services Provided by Article 28 Clinics Operated by Academic Dental Centers not Participating in Contractor´s Network.
- Consistent with Chapter 697 of the Laws of 2003 amending SSL § 364–j, dental services provided by Article 28 clinics operated by academic dental centers may be accessed directly by Enrollees without prior approval and without regard to network participation.
- The Contractor will reimburse non–participating Article 28 clinics operated by academic dental centers for covered dental services provided to Enrollees at approved Article 28 Medicaid clinic rates in accordance with the protocols issued by the Department.
I. Department Exclusion or Termination of Providers
- If the Department excludes or terminates a provider from its Medicaid program, the Contractor shall, upon learning of such exclusion or termination, immediately terminate the Provider Agreement with the Participating Provider, and agrees to no longer utilize the services of the subject provider, as applicable. The Contractor shall access information pertaining to excluded Medicaid providers through the Department´s Health Commerce System (HCS). Such information available to the Contractor on the HCS shall be deemed to constitute constructive notice. The HCS should not be the sole basis for identifying current exclusions or termination of previously approved providers, as further defined in Subsection 3.p.ii of Article VIII Section F. Should the Contractor become aware, through the HCS or any other source, of a Departmental exclusion or termination, the Contractor shall validate this information with the Office of Health Insurance Programs and comply with the provisions of this Section.
- If Medicaid payments are made by the Contractor to an excluded or terminated provider for dates of service after the provider´s exclusion or termination effective date, the Contractor shall report and explain within 60 days of identifying the payment, in a form and format to be determined by OMIG in consultation with the Department, when and how the payment was identified, and the date on which the encounter data was adjusted to reflect the recovery.
J. Health Home Service and Care Management Coordination
- Eligible individuals enrolled in Contractor´s MLTC Plan may also be enrolled in a Health Home consistent with guidance issued by the Department.
- The Contractor shall utilize the Administrative Service Agreement (ASA) template approved by the Department and must comply with any applicable guidance from the Department.
- The Contractor shall retain primary care management responsibility for those services in the MLTC benefit package.
- While the template ASA provided by the Department may not be altered, if necessary, a Health Home and the Contractor may agree to elaborate their respective roles via an appendix–provided that it does not conflict with the terms of the ASA–providing an opportunity to further ensure that care coordination services are not duplicated.
K. Service Verification Process
Pursuant to 42 CFR 455.20, the Contractor will implement a service verification process that accurately evaluates the delivery of billed services to the recipient population by using statistically valid sample sizes and timeframes that determine whether Enrollees received services billed by Providers.
L. Withholding of Payments
The Contractor must, if directed by the Department or OMIG, withhold payments to Participating Providers, in whole or in part, when the Department or OMIG has determined or has been notified that a Participating Provider is the subject of a pending investigation of a credible allegation of fraud unless the Department or OMIG finds good cause not to direct the Contractor to withhold payments in accordance with 18 NYCRR § 518.7.
- The Contractor shall provide notice to the Participating Provider of the withhold as directed by the Department or OMIG and in accordance with 18 NYCRR § 518.7(b) and § 518.7(c).
- The Contractor shall direct all appeals of the withhold to:
Office of the Medicaid Inspector General
Office of Counsel
800 North Pearl Street
Albany, New York 12204
ATTN: Withhold Appeal
M. Home Care Services Worker Wage Parity Rules
The Contractor is required to comply with the home care worker wage parity law at Section 3614–c of the Public Health Law and all applicable notices and regulations issued pursuant to subdivisions 8 and 9 therein. These requirements apply to New York City, Nassau, Suffolk, and Westchester Counties.
The Contractor shall certify to the Department annually, on forms provided by the Department, that all home care aide services, whether provided by the Contractor or through a subcontractor, are in compliance with PHL § 3614–c.
The Contractor shall require subcontractors employing home care aides to certify to the Contractor annually, on forms provided by the Department, that all home care aide services provided through the subcontractor are in compliance with PHL § 3614–c.
The Contractor shall quarterly collect, and require subcontractors to provide, sufficient information to verify that subcontractors employing home care aides are in compliance with PHL § 3614–c. The Contractor shall develop protocols to establish a verification system to demonstrate compliance with requirements. Such verification system must be sufficient to verify that home care aide wages provided by each subcontractor meet or exceed the local wage requirements pursuant to subdivision 3 and applicable notices and regulations. Solely collecting the certification or an attestation of compliance is not sufficient to meet this requirement. The local wage requirements are subject to change pursuant to subdivision 3 and applicable notices and regulations, all wages provided must comply with the current rate in effect.
Failure to fully comply with the home care worker wage parity requirements may result in non–payment of services rendered, as required by PHL § 3614–c (2).
N. Fair Labor Standards Act
The Contractor is required to comply with all applicable provisions of the Fair Labor Standards Act (FLSA). The Contractor shall develop protocols to establish a verification system to demonstrate compliance with requirements. Such protocols shall include appropriate record keeping methodologies, tracking of aide travel time, hours worked on live–in cases, and appropriate rate of reimbursement. Such verification system and protocols are subject to audit by DOH, OMIG, and the Department of Labor.
|top of section| |top of page|ARTICLE VIII
RECORDS REPORTING AND CERTIFICATION REQUIREMENTS
A. General Requirements
- The Contractor shall maintain a health information system that collects, analyzes, integrates and reports data that meets the requirements of 42 CFR 438.242 and PHL Article 44. The system must be sufficient to provide the data necessary to comply with the requirements of this Agreement. The system must provide information on areas including, but not necessarily limited to:
- utilization;
- amounts paid to providers and subcontractors relating to patient care services and medical supplies; and
- Complaints, Appeals, and Disenrollments for other than loss of Medicaid eligibility.
- The Contractor must take the following steps to ensure that data received from Participating Providers is accurate and complete:
- verify the accuracy and timeliness of reported data;
- screen the data for completeness, logic and consistency; and
- collect utilization data in standardized formats as requested by the Department.
- The Contractor must also take the following steps to reasonably ensure that data received from Non–Participating Providers is accurate and complete:
- verify the accuracy and timeliness of reported data;
- screen the data for completeness, logic and consistency; and
- collect utilization data in standardized formats as requested by the Department.
- The Contractor must make all requested information available to CMS and the Department.
B. Maintenance of Contractor Performance Records, Records Evidencing Enrollment Fraud and Documentation Concerning Duplicate CINs
- The Contractor shall maintain and shall require its subcontractors, including its Participating Providers, to maintain appropriate records relating to performance under this Agreement, including:
- appropriate records related to services provided to Enrollees, including a separate Medical Record for each Enrollee;
- all financial records and statistical data that the LDSS or entity designated by the Department, the Department and any other authorized governmental agency may require including books, accounts, journals, ledgers, and all financial records relating to capitation payments, TPHI recovery, and other revenue or payments received, any reserves related thereto, and expenses incurred under this Contract;
- appropriate financial records to document fiscal activities and expenditures, including records relating to the sources and application of funds and to the capacity of the Contractor or its providers, including its Participating Providers, if relevant, to bear the risk of potential financial losses;
- all documents concerning enrollment fraud or the fraudulent use of any CIN;
- all documents concerning duplicate CINs; and
- appropriate records identifying every subcontract to a subcontractor, including any and all agreements arising out of said subcontract.
- Credentials for network providers shall be maintained on file by or in a manner accessible to the Contractor and furnished to the Department, upon request.
- The Contractor shall take reasonable steps to ensure that it notify Non–Participating Providers–upon payment of first claim–requesting the Non–Participating Provider to comply with the requirements of this Section of this Agreement.
- For every claim submitted to or paid by the Contractor, the Contractor shall maintain appropriate records identifying every subcontractor, person or entity performing the services under said claim, including amounts paid.
- The record maintenance requirements of this Section shall survive the termination, in whole or in part, of this Agreement.
C. Maintenance of Financial Records and Statistical Data
The Contractor shall maintain all financial records and statistical data according to generally accepted accounting principles and/or Statutory accounting principles where applicable.
D. Access to Contractor Records
The Contractor shall provide the LDSS or entity designated by the Department, the Department, the Comptroller of the State of New York, the Office of the Medicaid Inspector General (OMIG), the Attorney General of the State of New York, DHHS, the Comptroller General of the United States, and their authorized representatives with access to all records relating to Contractor performance under this Agreement for the purposes of examination, audit, and copying of such records. The Contractor shall give access to such records on two (2) business days prior written notice, during normal business hours, unless otherwise provided or permitted by applicable laws, rules, or regulations. When records are sought in connection with an investigation, all costs associated with the production and reproduction shall be the responsibility of the Contractor.
E. Retention Periods
The Contractor shall preserve and retain all records relating to Contractor performance under this Contract in readily accessible form during the term of this Contract and for a period of six (6) years thereafter. All provisions of this Contract relating to record maintenance and audit access shall survive the termination of this Contract and shall bind the Contractor until the expiration of a period of six (6) years commencing with termination of this Contract or if an audit is commenced, until the completion of the audit, whichever occurs later.
F. Reporting Requirements
- The Contractor shall be responsible for fulfilling the reporting requirements of this Agreement. Reports shall be filed in a format specified by the Department and according to the time schedules required by the Department.
- The Contractor shall furnish all information necessary for the Department to assure adequate capacity and access for the enrolled population and to demonstrate administrative and management arrangements satisfactory to the Department. The Contractor shall submit periodic reports to the Department in a data format and according to a time schedule required by the Department to fulfill the Department´s administrative responsibilities under PHL §4403–f and other applicable State and federal laws, and regulations or to meet federal waiver reporting requirements. Reports may include but are not limited to information on: availability, accessibility and acceptability of services; enrollment; Enrollee demographics; disenrollment; Enrollee health and functional status (including the UAS data set or any other such instrument the Department may request); service utilization; encounter data; Enrollee satisfaction; marketing; grievance and appeals; and fiscal data. The Contractor shall promptly notify the Department of any request by a governmental entity or an organization working on behalf of a governmental entity for access to any records maintained by the Contractor or a subcontractor pursuant to this Agreement.
- The Contractor shall submit the following specific reports to the Department.
- Financial Reports:
- Quarterly Financial Statements:
The Contractor shall submit Quarterly Financial Statements to the Department. The due date for quarterly reports shall be forty–five (45) days after the end of the calendar quarter. - Annual Financial Statements:
In accordance with 10 NYCRR Part 98–1.16, the Contractor shall file with the Department a financial statement each year in the form prescribed by the Commissioner known as the MMCOR. The MMCOR shows the condition at last year–end and contains the information required by PHL § 4408. The due date for annual statements shall be April 1 following the report closing date. - Other Financial Reports:
The Contractor shall submit financial reports, including certified annual financial statements, and make available documents relevant to its financial condition to the Department in a timely manner as required by State laws and regulations including but not limited to PHL §§ 4403–f, 4404 and 4409, 10 NYCRR § 98–1.11, 98–1.16, and 98–1.17 and applicable State Insurance Law §§ 304, 305, 306, and 310.
- Quarterly Financial Statements:
- Encounter Data:
- The Contractor shall prepare and submit encounter data on a bimonthly (twice a month) basis, as specified by the Department, to the Department through its designated fiscal agent. Each provider is required to have a unique identifier. Submissions shall be comprised of encounter records or adjustments to previously submitted records which the Contractor has received and processed from provider encounter or claim records of any contracted or directly provided services rendered to the Enrollee in the current or any preceding months.
Encounter Data submissions must be received by the fiscal agent in accordance with the time frames specified in the MEDS III data element dictionary, or its successor system´s equivalent, as posted on the Health Commerce System (HCS) to assure the submission is included in the fiscal agent´s monthly production processing.
The Contractor shall submit an annual notarized attestation that the encounter data submitted through the designated fiscal agent is, to the best of the Contractor´s information, knowledge and belief, accurate and complete. The encounter data submission must comply with the MEDS III data element dictionary, or its successor system´s equivalent, and shall include the name and provider number of any ordering, referring, prescribing, or attending provider and information on the rendering/operating/other professional. Generic Provider IDs set forth in MEDS III data element dictionary, or its successor system´s equivalent, shall be used only when specific Provider IDs remain unknown after reasonable inquiry. NPI numbers of providers not enrolled in Medicaid must be reported. If the NPI is not available, the Contractor shall report the Tax Payer ID of the provider or professional.
The Contractor may report encounter data records that have not been adjudicated from the provider submitted claim/encounter in the regular claims system, such as data collected through medical record review, if the following conditions are met:- The Contractor shall ensure that medical records, notes and documentation constituting the source of the submitted data be available for review by the Department for a period of six (6) years from the date of service.
- Proof is maintained by the Contractor that an Explanation of Benefits (EOB) was sent to the provider for all Medicaid Encounter Data collected and submitted to MEDS III, or its successor system, with the diagnosis and procedures clearly specified.
- The internal data system storing these records is subject to audit.
- All records created or modified through this information gathering process must be made identifiable to the Department using unique encounter control numbers (ECNs). Algorithms used to assign ECNs for these records must be sent to the Department prior to data submission.
- Contractor shall ensure to the best of the Contractor´s knowledge, information, and belief, that all required encounter data fields are submitted to the Fiscal Agent and are populated with accurate and complete data.
- The Contractor shall maintain information as to the ordering/referring, prescribing or attending provider and information on the rendering/operating/other professional relating to an encounter and the Contractor shall report such ordering/referring, prescribing or attending provider and information on the rendering/operating/other professional information via data provided to the Fiscal Agent in accordance with Subsection 3.b of Article VIII Section F of this Agreement.
- Consistent with the procedures established and, in a format, to be developed by the Department, the Contractor shall report the NYS provider license number and NPI of any subcontractor performing services. Where the subcontractor performing services does not have a NYS provider license number or NPI, the Contractor shall report the Tax Payer ID of the subcontractor.
- The Contractor acknowledges that the Department may, in its discretion, assess penalties for untimely, incomplete or inaccurate submission of encounter data pursuant to SSL 364–j (32).
- The Contractor shall prepare and submit encounter data on a bimonthly (twice a month) basis, as specified by the Department, to the Department through its designated fiscal agent. Each provider is required to have a unique identifier. Submissions shall be comprised of encounter records or adjustments to previously submitted records which the Contractor has received and processed from provider encounter or claim records of any contracted or directly provided services rendered to the Enrollee in the current or any preceding months.
- Grievance and Appeal Reports:
- The Contractor must provide the Department on a quarterly basis, and within fifteen (15) business days of the close of the quarter, a summary of all grievance and appeals received during the preceding quarter using a data transmission method that is determined by the Department.
- The Contractor also agrees to provide on a quarterly basis, within fifteen (15) business days of the close of the quarter, the total number of grievance or appeals that have been unresolved for more than thirty (30) days. The Contractor shall maintain records on these and other grievances or appeals, which shall include all correspondence related to the grievance or appeal, and an explanation of disposition. These records shall be readily available for review by the Department or entity designated by the Department upon request.
- Nothing in this Section is intended to limit the right of the Department and the entity designated by the Department to obtain information immediately from a Contractor pursuant to investigating a particular Enrollee grievance or appeal, or provider complaint.
- Fraud and Abuse Reports:
- If the Contractor has an enrolled population of 10,000 or more persons in the aggregate in any given year, the Contractor must comply with 10 NYCRR Part 98–1.21. This includes development and submission to the commissioner of a fraud and abuse prevention plan as well as designation of an officer or director who has responsibility and authority for carrying out provisions of the plan, and who reports directly to senior management.
- If the Contractor has fewer than 10,000 Enrollees or is otherwise not subject to 10 NYCRR § 98–1.21(a), the Contractor shall submit annually to the Department and OMIG, in a form and format to be determined by the Department or OMIG, a report of overpayments recovered.
- The Contractor, regardless of the size of its enrolled population, must submit to the Department and OMIG the following information on an ongoing basis for each reasonably suspected case of fraud and abuse it identifies through complaints, organizational monitoring, contractors, providers, beneficiaries, Enrollees, or any other source:
- The name of the individual or entity that committed, or is reasonably suspected of committing the fraud or abuse;
- The source that identified the reasonably suspected fraud or abuse;
- The type of provider, entity or organization that committed, or is reasonably suspected of committing the fraud or abuse;
- A description of the reasonably suspected fraud or abuse;
- The approximate dollar amount of the reasonably suspected fraud or abuse;
- The legal and administrative disposition of the case, if available, including actions taken by law enforcement officials to whom the case has been referred;
- No disposition of any case by the Contractor shall limit the authority of the New York State Office of the Attorney General, the Department, OMIG, or the Office of the State Comptroller (OSC) to investigate, audit or obtain recoveries from any Participating Provider, Non–Participating Provider, Contractor, subcontractor, or third party; and
- Other data/information as prescribed by the Department.
- Such report shall be submitted when cases of fraud and abuse are confirmed and shall be reviewed and signed by an executive officer of the Contractor.
- The Contractor will report to the Department and OMIG, any reasonably suspected criminal activity, fraud, or abuse committed by an Enrollee, provider, or the Contractor´s or subcontractor´s employee or management, or third party where there is a suspicion of such activity, within seven (7) days.
- Such report will be in a manner prescribed by the Department, in consultation with OMIG. For the purposes of this Section, criminal activity includes but is not limited to, submitting claims for services not rendered, providing unnecessary services, or possessing forged documents including prescriptions.
- Compliance Plan and Report
The Contractor shall conduct an annual assessment and submit to OMIG and the Department an annual report, in a form and format to be determined by the Department and OMIG, of the status of their conformity with all Contractor regulatory and contractual obligations (list to be developed by the Department and OMIG) by December 31 of each calendar year, to start in 2015.
The Contractor shall also establish and adhere to a process for reporting to the Department credible information of violations of law by the Contractor subcontractors or Enrollees for a determination as to whether criminal, civil or administrative action may be appropriate. With respect to Enrollees, this reporting shall be restricted to credible information on violations of law with respect to enrollment in the plan or the provision of, or payment for, health services. - Comprehensive Provider Report
The Contractor shall submit to the Department or OMIG quarterly, in a form and format to be determined by the Department or OMIG, a report which shall include the total dollar amount of claims submitted by Participating and Non–Participating Providers under the MLTC Partial Capitation Program to the Contractor or any agent of the Contractor, the total dollar amount paid to Participating and Non–Participating Providers under the MLTC Partial Capitation Program by the Contractor or any agent of the Contractor, and the total dollar amount of services ordered, referred or prescribed by Participating and Non–Participating Providers under the MLTC Partial Capitation Program during the reporting period. - Performance Improvement Projects:
The Contractor will be required to conduct performance improvement projects that focus on clinical and non–clinical areas consistent with the requirements of 42 CFR 438.240. The purpose of these studies will be to promote quality improvement within the MLTCP. At least one (1) performance improvement project each year will be selected as a priority and approved by the Department. Results of each of these annual studies will be provided to the Department in a required format. Results of other performance improvement projects will be included in the minutes of the quality committee and reported to the Department upon request. - Enrollee Health and Functional Status Report:
The Contractor shall submit Enrollee health and functional status data for each of their Enrollees in the format and according to the timeframes specified by the Department. The data shall consist of the UAS or successor instrument and any other such instrument the Department may request. The data shall be submitted at least semi–annually or on a more frequent basis if requested by the Department. - MLTCP Eligibility Assessments Reports:
The Contractor shall submit to the Department, within fifteen (15) days of the close of each quarter, a MLTCP Eligibility Assessments Report, in a format specified by the Department, which includes the following:- The total number of initial assessments requested by individuals referred or requesting new service.
- The number of such assessments that were conducted within thirty (30) days of the request or referral.
- The number of such assessments for individuals who did not meet MLTC eligibility requirements.
- The number of people who were not referred by an enrollment broker and contacted the MLTCP directly and were provided MLTC materials.
- Critical Incident Report:
The Contractor shall submit to the Department, within fifteen (15) days of the close of each quarter, a Critical Incident Report, in a format specified by the Department, which includes the following:- The number of critical incidents (as set forth in section L of Article V of this Contract) that were investigated by the Contractor, including the Enrollee outcome.
- Marketing Materials Report:
The Contractor shall submit to the Department, within fifteen (15) days of the close of each quarter, a Marketing Materials Report, in a format specified by the Department, which includes the following:- A listing of new marketing materials approved for use by the Department.
- Rebalancing Efforts Report:
The Contractor shall submit to the Department, within fifteen (15) days of the close of each quarter, a Rebalancing Efforts Report, in a format specified by the Department, which includes the following:- The number of individuals who were enrolled in the MLTCP from a nursing home.
- The number of Enrollees who were admitted to a nursing home but returned to the community.
- The number of Enrollees who were permanently admitted to a nursing home.
- Auto–Assigned Population – Notice of Action Report:
For initial implementation of the auto–assigned population, the MLTCPs must submit monthly reports (within ten (10) business days of the close of each month) identifying instances when the MLTCP has issued a notice of action that involves a reduction of split shift or live–in services or when the MLTCP is reducing hours by twenty–five percent (25%) or more.
The MLTCP will also submit a monthly report (within ten (10) business days of the close of the month) to the Department identifying the number of appeals and fair hearings requested as a result of the above reductions. - Ownership and Related Information Disclosure:
- Ownership and/or control interest in the Contractor/disclosing entity must be collected in accordance with this section. For the purposes of Article XIII Section F, a disclosing entity is any entity other than an individual practitioner or group of practitioners, as defined by 42 CFR § 455.101, that is a Participating Provider in the Contractor´s network. A person with an ownership or control interest means a person or corporation that:
- has an ownership interest totaling five (5) percent of more in the Contractor/disclosing entity;
- has an indirect ownership interest equal to five (5) percent or more in the Contractor/disclosing entity;
- has a combination of direct and indirect ownership interests equal to 5 percent or more in the Contractor/disclosing entity;
- owns an interest of five (5) percent or more in any mortgage, deed of trust, note or other obligation secured by the Contractor/disclosing entity if that interest equals at least five (5) percent of the value of the property or assets of the Contractor/disclosing entity;
- is an officer or director of the Contractor/disclosing entity that is organized as a corporation; or
- is a partner in a disclosing entity that is organized as a partnership?
- Consistent with 42 CFR 455.104, the Contractor must disclose complete ownership, control, and relationship information to the Department as specified in (iii)(A)(1)– (6) below:
- upon execution of a contract with the Department;
- upon execution of a renewal or extension of the contract with the Department;
or - within 35 days after any change in ownership of the Contractor.
- Consistent with 42 CFR 455.104, the Contractor will obtain a disclosure of complete ownership, control, and relationship information from all Participating Providers and other disclosing entities per this Agreement.
- The Contractor must require each Participating Provider and other disclosing entities, per this Agreement, to disclose:
- the name and address of each person (individual or corporation) with an ownership or control interest in the disclosing entity or in any subcontractor in which the disclosing entity has direct or indirect ownership;
- the date of birth and Social Security number for any individual with an ownership or control interest;
- whether any of the persons named, in compliance with (A) of this section, is related to another as spouse, parent, child, or sibling;
- a tax identification number (in the case of a corporation) with an ownership or control interest in the disclosing entity as a spouse, parent, child, or sibling; or whether the person (individual or corporation) with an ownership or control interest in any subcontractor in which the disclosing entity has a five (5) percent or more interest is related to another person with ownership or control interest in the disclosing entity as a spouse, parent, child or sibling;
- the name of any other disclosing entity in which a person with an ownership or control interest in the disclosing entity also has an ownership or control interest; and
- The name, address, date of birth and social security number of any managing employee of the disclosing entity.
- In order to minimize the Provider´s reporting requirements, the Contractor must accept the following:
- For New York State fee for service providers who also participate in Medicaid fee for service, the Contractor shall accept a copy and/or update of the standard Medicaid fee for service enrollment form to satisfy this requirement.
- If the provider is not a Medicaid fee for service provider, but participates in any Medicaid managed care program, such information will be provided in a format prescribed by the Department.
- The Contractor must keep evidence of all requests to obtain this information and copies of the information obtained from disclosing entities and make this information available to the State upon 35 days of the request.
- A disclosing entity must supply the information specified in (ii) of this section to the Contractor upon:
- application for participation;
- execution of an agreement with Contractor; and/or
- within 35 days after a change in ownership of the disclosing entity.
- The Contractor must require each Participating Provider and other disclosing entities, per this Agreement, to disclose:
- Ownership and/or control interest in the Contractor/disclosing entity must be collected in accordance with this section. For the purposes of Article XIII Section F, a disclosing entity is any entity other than an individual practitioner or group of practitioners, as defined by 42 CFR § 455.101, that is a Participating Provider in the Contractor´s network. A person with an ownership or control interest means a person or corporation that:
- Professional Discipline:
- Pursuant to PHL § 4405–b, the Contractor shall have in place policies and procedures to report to the appropriate professional disciplinary agency within thirty (30) days of occurrence of any of the following:
- the termination of a health care Participating Provider Agreement pursuant to PHL §4406–d for reasons relating to alleged mental and physical impairment, misconduct or impairment of patient safety or welfare;
- the voluntary or involuntary termination of a contract or employment or other affiliation with such Contractor to avoid the imposition of disciplinary measures; or
- the termination of a health care Participating Provider Agreement in the case of a determination of fraud or in a case if imminent harm to patient health.
- The Contractor shall make a report to the appropriate professional disciplinary agency within thirty (30) days of obtaining knowledge of any information that reasonably appears to show that a health professional is guilty of professional misconduct as defined in Articles 130 and 131–A of the New York State Education Law (Education Law).
- Pursuant to 42 CFR 1002.3(b), the Contractor will report to the Department and OMIG any adverse actions taken for program integrity reasons against Providers. The Contractor will notify the Department of any Provider denied credentialing or termination of the Provider´s contract for program integrity related reasons such as being on the excluded Provider list and/or having existing fraud, licensing or Office of Professional Medical Conduct (OPMC) issues.
- Pursuant to 42 CFR 1002.3, prior to the Contractor entering into or renewing any agreement with a Participating Provider or Subcontractor, or at any time upon written request by the Department, the Participating Provider or Subcontractor must disclose to the Contractor the identity of any person described in 42 CFR § 1001.1001(a)(1). The Contractor must notify the Department of any such disclosures within 20 working days from the date it receives the information.
- Unless otherwise authorized by the Department, under 18 NYCRR 515, the Contractor must exclude an entity (as defined in 42 CFR 1001.1001(a)(1)) if:
- a person with a relationship with such entity:
- has been convicted of a criminal offense as described in sections 1128(a)(b)(1)–(3) of the Act;
- has had civil money penalties or assessments imposed under section 1128A of the Act;
- has been excluded from participation in Medicare or any of the New York State health care programs; or if
- a person with a relationship with such entity:
- has a direct or indirect ownership interest (or any combination thereof) of 5 percent or more in the entity;
- is the owner of a whole or part interest in any mortgage, deed of trust, note or other obligation secured (in whole or in part) by the entity or any of the property assets, thereof, in which whole or part interests equal to or exceeds 5 percent of the total property and assets of the entity;
- is an officer or director of the entity, if the entity is organized as a corporation;
- is a partner in the entity, if the entity is organized as a partnership;
- is an agent of the entity;
- is a managing employee, that is, an individual (including a general manager, business manager, administrator or director) who exercises operational or managerial control over the entity or part thereof, or directly or indirectly conducts the day–to–day operations of the entity or part thereof; or
- is not currently described in A) through F) but was formerly described in and is no longer so described because of a transfer of ownership or control interest to an immediate family member or a member of the person´s household in anticipation of or following a conviction, assessment of a civil monetary penalty, or imposition of an exclusion.
- Contractor Notification Requirements of this Section
The Contractor must notify the Department within 20 working days of any negative action it takes on an individual´s or entity´s application to or participation in the Contractor´s MLTCP provider network, regardless of what such an action is called. This includes, but is not limited to, denial of application, suspension actions, settlement agreements, and situations where an individual or entity voluntarily withdraws from the program to avoid a formal sanction. - Contractor Refusal Rights to Providers Under this Section
- The Contractor may refuse to enter into or renew an agreement with a provider if any person who has ownership or control interest in the provider, or who is an agent or managing employee of the provider, has been convicted of a criminal offense related to that person´s involvement in any program established under Medicare, Medicaid or Title XX services program.
- The Contractor may refuse to enter into, or may opt to terminate, a Participating Provider agreement if it determines that the provider did not fully and accurately make the required disclosures.
- a person with a relationship with such entity:
- Pursuant to PHL § 4405–b, the Contractor shall have in place policies and procedures to report to the appropriate professional disciplinary agency within thirty (30) days of occurrence of any of the following:
- Certification Regarding Individuals Who Have Been Excluded, Debarred or Suspended By Federal or State Government:
- Contractor will certify to the Department initially and immediately upon changed circumstances from the last such certification that it does not knowingly have an individual who has been debarred or suspended by the federal, state or local government, or otherwise excluded from participating in procurement activities:
- as a director, officer, partner or person with beneficial ownership of more than five percent (5%) of the Contractor´s equity; or
- as a party to an employment, consulting or other agreement with the Contractor for the provision of items and services that are significant and material to the Contractor´s obligations in the Medicaid managed care program, consistent with requirements of SSA § 1932 (d)(1).
- Pursuant to 42 CFR 455.436, the Contractor shall:
- confirm the identity and determine the exclusion status of any employee in the capacity of general manager, business manager, administrator, director, or other individual who exercises operational or managerial control over, or who directly or indirectly conducts the day–to–day operations at initial hiring and any person with an ownership or control interest or who is an agent or managing employee of the provider through routine checks of Federal and State databases. These include the Social Security Administration´s Death Master file, and the National Plan and Provider Enumeration System (NPPES), and the Excluded Parties List System (EPLS), and either the List of Excluded Individuals and Entities (LEIE) or the Medicare Excluded Database (MED), the NYS OMIG Exclusion List, and any such other databases as the Secretary may prescribe; and
- check the LEIE (or MED), the EPLS, and NYS OMIG Exclusion List no less frequently than monthly.
- Pursuant to 42 CFR 455.436, the Contractor shall:
- confirm, through routine checks of Federal and State databases, the identity and determine the exclusion status of new Participating Providers, re–enrolled Participating Providers, and all current Participating Providers, including any Non–Participating Providers, subcontractors, or persons with an ownership or control interest in, or who is an agent or managing employee of, any Participating Provider. These include the Social Security Administration´s Death Master (SSDM) file, the National Plan and Provider Enumeration System (NPPES), the Excluded Parties List System (EPLS), either the List of Excluded Individuals and Entities (LEIE) or the Medicare Excluded Database (MED), the NYS OMIG Exclusion List, and any such other databases as the Secretary may prescribe;
- confirm the identity and determine the exclusion status of Non–Participating Providers, upon payment of first claim through routine checks of Federal and State databases. These include the SSDM file, the NPPES, the EPLS, either the LEIE or the MED, the NYS OMIG Exclusion List, and any such other databases as the Secretary may prescribe;
- check the SSDM and NPPES for new providers, re–enrolled providers and any current provider who were not checked upon enrollment into Contractor´s Medicaid program; and
- check the LEIE (or the MED), the EPLS, and the NYS OMIG Exclusion List no less frequently than monthly;
- The Contractor shall:
- Confirm that providers have procedures in place to identify and determine the exclusion status of managing employees through routine checks of Federal databases. These include the Social Security Administration´s Death Master file, The National Plan and Provider Enumeration System (NPPES), The Excluded Parties List System (EPLS), either the List of Excluded Individuals and Entities or the Medicare Excluded Database (MED), and any such other databases as the Secretary may prescribe; and
- check the LEIE (or the MED), the EPLS, and the NYS OMIG Exclusion List no less frequently than monthly.
- Contractor will certify to the Department initially and immediately upon changed circumstances from the last such certification that it does not knowingly have an individual who has been debarred or suspended by the federal, state or local government, or otherwise excluded from participating in procurement activities:
- Business Transaction Disclosures
- Pursuant to 42 CFR 455.105(b)(2), the Contractor and its contracted providers must submit, within 35 days of the date of request by the Department or Secretary of DHHS, full and complete information about:
- the ownership of any subcontractor with whom the Contractor has had a business transaction(s) totaling more than $25,000 during the 12–month period ending on the date of the request; and
- the ownership of any subcontractor with whom any contracted provider has had a business transaction(s) totaling more than $25,000 during the 12–month period ending on the date of the request; and
- any significant business transactions between the Contractor and any wholly owned supplier, or between the Contractor and any subcontractor, during the 5–year period ending on the date of the request; and
- any significant business transactions between the Contractor´s provider and any wholly owned supplier, or between the provider and any subcontractor, during the 5–year period ending on the date of the request.
- For the purposes of Article VIII Section F, a "wholly owned supplier" shall mean a supplier of services or items under this Agreement whose total ownership is held by the Contractor/provider or by a person, persons, or other entity with an ownership or control interest in the Contractor/provider.
- A supplier means an individual, agency, or organization from which a Contractor/provider purchases goods and services used in carrying out its responsibilities under Medicaid.
- A Subcontractor means an individual, agency or organization to which the Contractor or disclosing entity has contracted or delegated some of its management functions or responsibilities.
- Pursuant to 42 CFR 455.105(b)(2), the Contractor and its contracted providers must submit, within 35 days of the date of request by the Department or Secretary of DHHS, full and complete information about:
- Disclosure of Criminal Activity:
- Pursuant to 42 CFR 455.106, the Contractor will disclose to the Department any criminal convictions by managing employees related to Medicare, Medicaid, or Title XX programs at the time the Contractor applies or renews an application for participation in the Medicaid managed care program or Family Health Plus program or at any time on request. For the purposes of this section, managing employee means a general manager, business manager, administrator, director, or other individual who exercises control or who directly or indirectly conducts the day–to–day operation of an institution, organization, or agency.
- Pursuant to 42 CFR 455.106, before the Contractor enters into or renews a provider agreement, or at any time upon written request by the State, the Contractor must disclose to the State the identity of any person who:
- has ownership or control interest in the provider, or is an agent or managing employee of the provider; and
- has been convicted of a criminal offense related to that person´s involvement in any program under Medicare, Medicaid, or the Title XX services program since the inception of those programs.
- Notification to the U.S. Department of Health and Human Services (DHHS) Inspector General.
- The Department shall notify the DHHS Inspector General of any disclosures made under this Subsection within 20 working days from the date it receives the information; and
- The Department shall also promptly notify the DHHS Inspector General of any action it takes with respect to the provider´s participation in the program.
- Denial or Termination of Provider Participation
- The Contractor may refuse to enter into or renew an agreement with a provider if any person who has an ownership or control interest in the provider, or who is an agent or managing employee of the provider, has been convicted of a criminal offense related to that person´s involvement in any program established under Medicare, Medicaid or Title XX services program; and
- The Contractor may refuse to enter into or may terminate a provider agreement if it determines that the provider did not fully and accurately make any disclosure required under Subsection 3.s of this Section.
- Such denial or termination of a provider´s participation under this section may afford the provider a right to a hearing pursuant to Public Health Law § 4406–d(2).
- Additional Reports:
Upon request by the Department, the Contractor shall prepare and submit other operational data reports. Such requests will be limited to situations in which the desired data is considered essential and cannot be obtained through existing Contractor reports. Whenever possible, the Contractor will be provided with ninety (90) days´ notice and the opportunity to discuss and comment on the proposed requirements before work is begun. However, the Department reserves the right to give thirty (30) days´ notice in circumstances where time is of the essence.
- Financial Reports:
G. Data Certification
The Contractor shall comply with the data certification requirements in 42 CFR 438.604 and 438.606.
- The types of data subject to certification include, but are not limited to, enrollment information, encounter data, the premium proposal, annual network submissions, contracts and all other financial data. The certification shall be in a format prescribed by the Department and must be sent at the time the report or data are submitted.
- The certification shall be signed by the MLTCP´s Chief Executive Officer, the Chief Financial Officer or an individual with designated authority; and, the certification shall attest to the accuracy, completeness and truthfulness of the data.
H. Notification of Changes in Reporting Due Dates Requirements or Formats
The Department may extend due dates or modify report requirements or formats upon a written request by the Contractor to the Department, where the Contractor has demonstrated a good and compelling reason for the extension or modification. The Department will issue a written response to the request for a modification or extension of the due date.
I. Ownership and Related Information Disclosure
The Contractor shall report ownership and related information to the Department, and upon request to the Secretary of DHHS and the Inspector General of DHHS, in accordance with 42 U.S.C. §1320a–3 and 1396b(m) (4) and SSA §1124 and 1903(m)(4)).
J. Role of Compliance Officer and Compliance Committee:
- The Contractor shall designate a compliance officer and establish a compliance committee pursuant to 42 CFR 438.608 (b) (2). It is the obligation of the compliance officer and compliance committee to:
- monitor the plan reporting obligations and ensure that the required reports are accurate and submitted in a timely manner;
- develop written policies, procedures and standards of conduct that articulate the MLTCP´s commitment to adhere to all applicable federal and state standards;
- conduct appropriate staff training activities in an atmosphere of open communication;
- establish provisions for internal monitoring and auditing; and
- have provisions for prompt responses to deleted offenses with provisions for corrective action initiatives where appropriate.
- Pursuant to and in accordance with 42 CFR § 438.608, the Contractor must have administrative and management arrangements or procedures, including a mandatory compliance plan, that are designed to prevent fraud and abuse and ensure prompt organizational response to detect offenses and development of corrective action initiatives. These arrangements or procedures must include the following:
- written policies, procedures, and standards of conduct that articulate the organization´s commitment to comply with all Federal and State standards;
- the designation of a compliance officer and a compliance committee that are accountable to senior management;
- effective training and education for the compliance officer and the organization´s employees; effective lines of communication between the compliance officer and the organization´s employees;
- enforcement of standards through well publicized disciplinary guidelines;
- a provision for internal monitoring and auditing; and
- a provision for prompt response to detected offenses, and for the development of corrective action initiatives relating to the MCOs contract.
K. Public Access to Reports
Any data, information, or reports collected and prepared by the Contractor and submitted to New York State authorities in the course of performing their duties and obligations under this Contract will be deemed to be records of the Department and may be disclosed subject to and consistent with the requirements of Freedom of Information Law.
L. Certification Regarding Individuals Who Have Been Debarred or Suspended By Federal or State Government
The Contractor will certify to the Department initially and immediately upon changed circumstances from the last such certification that it does not knowingly have an individual who has been debarred or suspended by the federal or state government, or otherwise excluded from participating in procurement activities:
- as a director, officer, partner or person with beneficial ownership of more than five percent (5%) of the Contractor´s equity; or
- as a party to an employment, consulting or other agreement with the Contractor for the provision of items and services that are significant and material to the Contractor´s obligations in the MLTCP consistent with requirements of SSA §1932 (d)(1).
M. Conflict of Interest Disclosure
The Contractor shall report to the Department in a format specified by the Department documentation, including but not limited to the identity of and financial statements of person(s) or corporation(s) with an ownership or contract interest in the MLTCP or with any subcontract(s) in which the MLTCP has a five percent (5%) or more ownership and interest, consistent with requirements of SSA § 1903 (m)(2)(a)(viii) and 42 CFR§ §455.100 and 455.104.
N. OMIG´s Right to Audit and Recover Overpayments Caused by Contractor Submission of Misstated Reports
The OMIG can perform audits of financial reports filed by Contractors after the Department reviews and accepts the Contractor´s report. If the audit determines that the Contractor´s filed report contained misstatements of fact, causing the Contractor and/or other Contractors to receive an inappropriate capitation rate, the OMIG will recover any and all overpayments. The Contractor will be entitled to the audit rights afforded to providers in 18 NYCRR 517, 518 and 519. Nothing in this section shall limit the Department, OMIG, or any other auditing entity from the development of alternative audit and/or recovery rights for time periods prior to the Contract period, during the Contract period, or subsequent to the Contract period, or limit other remedies or rights available to the Department, OMIG, or any other auditing entity relating to the timeliness, completeness and/or accuracy of the Contractor´s reporting submission.
O. OMIG´s Right to Audit and Recover Overpayments Which Were Caused by the Contractor´s Misstated Encounter Data
The OMIG can perform audits of the Contractor´s submitted encounter data after the Department has reviewed and accepted the Contractor´s encounter data submission. If the audit determines the Contractor´s encounter data was incorrectly submitted, and the Contractor received additional or higher Medicaid managed care capitation rate payments due to the incorrect encounter data, OMIG can recover from the Contractor the additional Medicaid funds that the Contractor received because of the encounter data misstatement. The Contractor will be entitled to the audit rights afforded to providers in 18 NYCRR 517, 518 and 519. Nothing in this section shall limit the Department, OMIG or any other auditing entity from the development of alternative audit and/or recovery rights for time periods prior to the Contract period, during the Contract period, or subsequent to the Contract period or limit other remedies or rights available to the Department, OMIG or any other auditing entity relating to the timeliness, completeness and/or accuracy of the Contractor´s reporting submission.
P. OMIG Audit Authority
In accordance with New York State Public Health Law sections 30 – 36, and as authorized by federal or state laws and regulations, OMIG may review and audit contracts, cost reports, claims, bills and all other expenditures of medical assistance program funds to determine compliance with federal and state laws and regulations and take such corrective actions as are authorized by federal or state laws and regulations.
Q. OMIG Compliance Review Authority
In accordance with New York State Public Health Law sections 30 – 36, and as authorized by federal or state laws and regulations, OMIG may conduct reviews of Participating Providers´ compliance programs, as well as Contractors´ compliance with the requirements of 42 U.S.C. § 1396a(a)(68) and 18 NYCRR Part 521.
|top of section| |top of page|ARTICLE IX
INTERMEDIATE SANCTIONS
- The Contractor is subject to the imposition of sanctions as authorized by state law and regulation, including the Department´s right to impose sanctions for unacceptable practices as set forth in 18 NYCCR Part 515 and civil and monetary penalties pursuant to 18 NYCRR Part 516 and 42 CFR 438.700 and such other sanctions and penalties as are authorized by local laws and ordinances and resultant administrative codes, rules and regulations related to the Medical Assistance Program or to the delivery of the contracted services.
- Unacceptable practices for which the Contractor may be sanctioned include, but are not limited to:
- Failing to provide medically necessary services that the Contractor is required to provide under its Contract with the Department.
- Imposing premiums or charges on Enrollees.
- Discriminating among Enrollees on the basis of their health status or need for health care services.
- Misrepresenting or falsifying information that it furnishes to an Enrollee, Applicant, Potential Enrollee, health care provider, the Department or to CMS.
- Distributing directly or through any agent or independent contractor, Marketing materials that have not been approved by the Department or that contain false or materially misleading information.
- Violating any other applicable requirements of SSA § 1903(m) or 1932 and any implementing regulations.
- Violating any other applicable requirements of 18 NYCRR or 10 NYCRR Part 98.
- Failing to comply with the terms of this Agreement.
- Intermediate Sanctions may include but are not limited to:
- Civil monetary penalties.
- Suspension of all new enrollment after the effective date of the sanction.
- Termination of the contract, pursuant to Article I of this Agreement.
- The Department shall have the right, upon notice to the LDSS or entity designated by the Department, to limit, suspend or terminate enrollment activities by the Contractor and/or enrollment into the MLTCP upon ten (10) days written notice to the Contractor. The written notice shall specify the action(s) contemplated and the reason(s) for such action(s) and shall provide the Contractor with an opportunity to submit additional information that would support the conclusion that limitation, suspension or termination of enrollment activities or Enrollment in the Contractor´s MLTCP is unnecessary. The Department reserves the right to suspend enrollment immediately in situations involving imminent danger to the health and safety of Enrollees. Nothing in this paragraph limits other remedies available to the Department under this Agreement.
- The Contractor will be afforded due process pursuant to federal and state laws and regulations, including 42 CFR 438.710, 18 NYCRR Part 516, and Article 44 of the PHL.
ARTICLE X
GENERAL REQUIREMENTS
A. Authorized Representatives With Respect to Contract
Upon commencement of performance under this Contract, the Department and the Contractor shall each designate a contract representative under this Contract and shall promptly so notify the other Party in writing. The contract representative shall be the contact person for all matters arising under this Contract. Each Party shall notify the other Party if it designates a new contract representative.
B. Confidentiality
- All individually identifiable information relating to Applicants and Enrollees that is obtained by the Contractor shall be safeguarded pursuant to 42CFR 431 and applicable sections of 45CFR parts 160 and 164, 42CFR part 2, 42 U.S.C. Section 1396a(a)(7) (Section 1902(a)(7) of the SSA ), and regulations promulgated thereunder, and applicable sections of State law and regulation including but not limited to PHL § 27–F, SSL 369, and section 33.13 of Mental Hygiene Law. Information shall be used or disclosed by the Contractor pursuant to appropriate consent only for a purpose directly connected with performance of Contractor obligations under this Contract.
- Medical records of Applicants and Enrollees shall be confidential and shall be disclosed to and by other persons within the Contractor´s organization, including subcontractors, only as necessary to provide health care and quality, peer, or complaint and appeal review of health care under the terms of this Contract.
- The provisions of this Section shall survive the termination of this Contract and shall bind the Contractor so long as the Contractor maintains any individually identifiable information relating to Applicants or Enrollees.
C. Additional Actions and Documents
Each Party hereby agrees to use its good faith and best efforts to cooperate with the other and to take or cause to be taken such further actions to execute, deliver, and file or cause to executed delivered, and filed such further documents and instrument, and to use best efforts to obtain such waivers and consents as may be necessary or as may be reasonably requested in order to effectuate fully the purposes, terms, and conditions of this Contract and the purposes of the plan.
D. Relationship of the Parties, Status of the Contractor
The Parties agree that the relation of Contractor to the Department will be that of an independent Contractor. The Parties also agree and acknowledge that Contractor is authorized to operate and to perform its obligations under this Contract pursuant to the provisions of PHL Article 44, Article 43 of State Insurance Law and section 402 of the Social Security Amendments of 1967, as amended by section 222(b) of the Social Security Amendments of 1972, 42 U.S.C. 1395b–1. The Parties further agree and acknowledge that Contractor will not, by virtue of its operation, of its performance of its obligations hereunder, of its compensation hereunder, or of any other provisions of this Contract: (1) be deemed to be an agent or instrumentality of the State of New York, the United States, or any agency of either, or (2) be deemed to be a preferred provider organization, third party administrator, or an independent practice association.
E. Nondiscrimination
The Contractor shall not unlawfully discriminate on the basis of age, race, color, gender, creed, religion, disability, sexual orientation, source of payment, type of illness or condition or place of origin. The Contractor shall operate the program in compliance with all applicable state and federal non–discrimination laws.
F. Employment Practices
- The Contractor shall comply with the nondiscrimination clause contained in Federal Executive Order 11246, as amended by Federal Executive Order 11375, relating to Equal Employment Opportunity for all persons without regard to race, color, religion, sex or national origin, the implementing rules and regulations prescribed by the Secretary of Labor at 41 CFR Part 60 and with the Executive Law of the State of New York, section 291–299 thereof and any rules or regulations promulgated in accordance therewith. The Contractor shall likewise be responsible for compliance with the above–mentioned standards by subcontractors with whom the Contractor enters into a contractual relationship in furtherance of this Contract.
- The Contractor shall comply with regulations issued by the Secretary of Labor of the United States in 20 CFR Part 741, pursuant to the provisions of Executive Order 11758, and with the Federal Rehabilitation Act of 1973 and the ADA of 1990. The Contractor shall likewise be responsible for compliance with the above–mentioned standards by subcontractors with whom the Contractor enters into a contractual relationship in furtherance of this Contract.
G. Dispute Resolution
The Contractor and the LDSS or entity designated by the Department shall jointly develop and use a process for resolving disputes with regard to the accuracy of assessments performed for enrollment, involuntary disenrollment´s and for continued stay decisions when the Enrollee no longer meets the nursing home level of care as determined at the last comprehensive assessment of the calendar year.
H. Assignment
This Contract may not be assignable by the Contractor without the prior written consent of the Commissioner of Health.
I. Binding Effect
Subject to any provisions hereof restricting assignment, this Contract shall be binding upon and shall inure to the benefit of the Parties and their respective successors and permitted assignees.
J. Limitation on Benefits of this Contract
It is the explicit intention of the Parties that no Enrollee, person or other entity, other than the Parties, is or shall be entitled to bring any action to enforce any provision of this Contract against the other Party, and that the covenants, undertakings, and agreements set forth in this Contract shall be solely for the benefit of, and shall be enforceable only by the Parties, or their respective successors and assignees, as permitted hereunder; provided, however, that the covenants, undertakings, and agreements set forth in section K of Article VI of this Contract hereof shall be construed for the benefit of the Enrollees.
K. Entire Contract
This Contract (including the Schedules and Appendices hereto) constitutes the entire Contract between the Parties with respect to the subject matter hereof, and it supersedes all prior oral or written agreements, commitments, or understandings with respect to the matters provided for herein. This Contract shall not be deemed to apply to individuals who are not Enrollees.
L. Conflicting Provisions
In the event of any conflict between the provisions of the main body of this Contract and the provisions of any Appendix or Schedule(s) attached hereto, the provisions of the main body of this Contract shall govern, unless a provision of an Appendix or a Schedule explicitly states that it shall supersede the main body of this Contract. State Appendix A takes precedence over the provisions of any other Appendix.
M. Modification
This Contract is subject to amendment or modification only upon mutual consent of the Parties reduced to writing. Attached Appendix X is the form to be used in modification of this Contract. Any such amendment or modification is not binding on the Parties unless and until approved by the Comptroller of the State of New York.
N. Headings
Article and section headings contained in this Contract are inserted for convenience of reference only, shall not be deemed to be a part of this Contract for any purpose, and shall not, in any way, define or affect the meaning, construction, or scope of any of the provisions hereof.
O. Pronouns
All pronouns and any variations thereof shall be deemed to refer to the masculine, feminine, neuter, singular or plural as the identity of the person or entity may require.
P. Notices
All notices permitted or required hereunder shall be in writing and shall be transmitted either:
- via certified or registered United States mail, return receipt requested;
- by facsimile transmission;
- by personal delivery;
- by expedited delivery service; or
- by e–mail.
Such notices shall be addressed as follows or to such different addresses as the parties may from time to time designate:
State of New York Department of Health
Name: Jason Helgerson
Title: Medicaid Director
Address: Office of Health Insurance Programs One Commerce Plaza
99 Washington Avenue, 1620 Albany, NY 12210
Telephone Number: 518–402–5673
Facsimile Number: 518–474–6961
E–Mail Address: jason.helgerson@health.ny.gov
[Insert Contractor Name]
Name:
Title:
Address:
Telephone Number:
Facsimile Number:
E–Mail Address:
Any such notice shall be deemed to have been given either at the time of personal delivery or, in the case of expedited delivery service or certified or registered United States mail, as of the date of first attempted delivery at the address and in the manner provided herein, or in the case of facsimile transmission or e–mail, upon receipt.
The parties may, from time to time, specify any new or different address in the United States as their address for purpose of receiving notice under this Agreement by giving fifteen (15) days written notice to the other party sent in accordance herewith. The parties agree to mutually designate individuals as their respective representative for the purposes of receiving notices under this Agreement. Additional individuals may be designated in writing by the parties for purposes of implementation and administration/billing, resolving issues and problems, and/or for dispute resolution.
Q. Partial Invalidity
Should any provision of this Contract be declared or found to be illegal, invalid, ineffective, unenforceable or void, then each Party shall be relieved of any obligation arising from such provision; the balance of this Contract, if capable of performance, shall remain in full force and effect.
R. Force Majeure
Each Party shall use all efforts to perform its obligations under this Contract but shall be excused for failure to perform or for delay in performance hereunder due to unforeseeable circumstances beyond its reasonable control or which could not have been prevented by it, including but not limited to acts of God, floods, hurricanes, earthquakes, acts of war, civil unrest, or embargoes; provided, that acts of any governmental body shall be deemed not to be a force majeure.
S. Survival
The termination or expiration of this Agreement shall not affect vested or accrued rights or obligations of the Parties existing as of the date of such termination or expiration or other obligations expressly intended to survive the termination or expiration hereof. Without limiting the generality of the foregoing, the following provisions of this Agreement shall survive any expiration or termination of this Agreement: entire Article VI; entire Article VIII; Article V Section D.; Article I Sections E, F and G; Article X Sections B, E, H, K, L, M, V, and AA, Appendix A and all definitional provisions of this Agreement to the extent that they pertain to any other surviving provisions or obligations.
T. State Standard Appendix A
The Parties agree to be bound by the terms and conditions of "Standard Clauses for New York State Contracts" attached hereto and incorporated herein as Appendix A. State Appendix A takes precedence over the provisions of this Agreement and any other Appendix.
U. Indemnification
- Indemnification by Contractor
- The Contractor shall indemnify, defend and hold harmless the Department, the State, its officers, agents and employees and the Enrollees and their eligible dependents from:
- any and all claims and losses incurred by or accruing or resulting from the acts or omissions of all Contractors, subcontractors, materialmen, laborers and any other person, firm or corporation furnishing or supplying work, services, materials, or supplies in connection with the performance of this Contract;
- any and all claims and losses incurred by, accruing, or resulting to any person, firm or corporation who may be injured or damaged by the acts or omissions of the Contractor, its officers, agents and employees or subcontractors, including Participating Providers, in connection with the performance of this Contract; and
- against any liability, including costs and expenses, for violation of proprietary rights, copyrights, or rights of privacy, arising out of publication, translation, reproduction, delivery, performance, use or disposition of any data furnished by the Contractor under this Contract or based on any libelous or otherwise unlawful matter contained in such data.
- The Department shall provide the Contractor with prompt written notice of any claim made against the Department and the Contractor, at its sole option, shall defend or settle said claim. The Department shall cooperate with the Contractor, to the extent necessary for the Contractor to discharge its obligations hereunder. Notwithstanding the foregoing, the State reserves the right to join any such claim, at its sole expense, when it determines there is an issue of significant public interest.
- The Contractor shall have no obligation hereunder with respect to any claim or cause of action for damages to persons or property to the extent caused by the Department, its employees or agents, when acting within the course and scope of their employment.
- The Contractor shall indemnify, defend and hold harmless the Department, the State, its officers, agents and employees and the Enrollees and their eligible dependents from:
- Indemnification by the Department
Subject to the availability of lawful appropriations as required by State Finance Law §41 and consistent with §8 of the State Court of Claims Act, the Department shall hold the Contractor harmless from and indemnify it for any final judgment of a court of competent jurisdiction to the extent attributable to the negligence of the Department or its officers or employees when acting within the course and scope of their employment. Provisions concerning the Department´s responsibility for any claims for liability as may arise during the term of this Contract are set forth in the New York State Court of Claims Act, and any damages arising for such liability shall issue from the New York State Court of Claims Fund or any applicable, annual appropriation of the Legislature of the State of New York.
V. Environmental Compliance
The Contractor shall comply with all applicable standards, orders or regulations issued pursuant to the Clean Air Act, 42 U.S.C. 7401 et seq., and the Federal Water Pollution Control Act, as amended, 33 U.S.C. 1251 et seq. The Contractor shall report violations to the Department, DHHS and to the appropriate Regional Office of the Environmental Protection Agency.
W. Energy Conservation
The Contractor shall comply with any applicable mandatory standards and policies relating to energy efficiency which are contained in the State Energy conservation plan issued in compliance with the Energy Policy and Conservation Act of 1975, Pub. L. 94–163 42 U.S.C. 6321 et seq., and any amendment thereto.
X. Prohibition on Use of Federal Funds for Lobbying
- The Contractor agrees, pursuant to U.S.C. 1352and 45 CFR Part 93 not to expend federally appropriated funds received under this Contract to pay any person for influencing or attempting to influence an officer or employee of an agency, a member of Congress, an officer or employee of Congress, or an employee of a member of Congress in connection with the awarding of any federal contract, the making of any federal grant, the making of any federal loan, the entering into of any cooperative agreement, and the extension, continuation, renewal, amendment, or modification of any federal contract, grant, loan or cooperative agreement.
- The Contractor agrees to complete and submit the "Certification Regarding Lobbying", attached hereto as Appendix C and incorporated herein, if this Contract exceeds $100,000.
- If any funds other than federally appropriated funds have been paid or will be paid to any person for influencing or attempting to influence an officer or employee of an agency, a member of Congress, an officer or employee of Congress, or an employee of a member of Congress in connection with this Contract or the underlying federal grant and the agreement exceeds $100,000 the Contractor agrees to complete and submit Standard Form– LLL, "Disclosure of Lobbying Activities", attached hereto as Appendix D and incorporated herein, in accordance with its instructions.
- The Contractor shall include the provisions of this section in all subcontracts under this Contract and require that all subcontractors whose contract exceeds $100,000 certify and disclose accordingly to the Contractor.
Y. Waiver of Breach
No term or provision of this Contract shall be deemed waived and no breach excused, unless such waiver or consent shall be in writing and signed by the Party claimed to have waived or consented. Any consent by a Party to, or waiver of, a breach under this Contract shall not constitute consent to, a waiver of, or excuse for any other, different or subsequent breach.
Z. Choice of Law
This Contract shall be interpreted according to the laws of the State of New York, without reference to choice of law principles. The Contractor shall be required to bring any legal proceeding against the Department or the State arising from this Contract in New York State courts.
AA. Executory Provision and Federal Funds
Section 112 of New York State Finance Law requires that any contract made by a State Department which exceeds fifty thousand dollars ($50,000) in amount be first approved by the Comptroller of the State of New York before becoming effective. The Parties recognize that this Agreement is wholly executory and not binding until and unless approved by the Comptroller of the State of New York. The Parties also agree that the effectiveness of this Agreement is conditioned upon receipt of any approval required pursuant to federal law to permit full Federal financial participation in the costs hereof. Contractor agrees to comply with all applicable federal audit requirements including but not limited to OMB Circular A–87 and other applicable federal rules and procedures concerning use of federal funds.
BB. Renegotiation
In the event any part of this Agreement is found to be invalid or unenforceable under applicable law and alters the general scope of contractual performance or a change occurs in applicable state or federal law, rules or regulations or federal or state interpretations thereof which requires alteration of the general scope of contractual performance to remain in compliance therewith, or the Department obtains a waiver of such applicable Federal law, rule or regulation, either Party may initiate re–negotiation of the terms and conditions of this Agreement to preserve the benefit bargained for. If the Parties are unable to agree on a revision of contractual terms and conditions consistent with the altered scope of contractual performance, either Party may terminate this Agreement as of the last day of the month following the month in which written notice of termination is given, subject to the provisions of Sections F and G of Article I of this Agreement.
CC. Affirmative Action
The Contractor agrees to comply with all applicable Federal and State nondiscrimination statutes including:
- The Civil Rights Acts of 1964, as amended; Executive Order No. 11246 entitled "Equal Employment Opportunity," as amended by Executive Order 11375, and as supplemented in Department of Labor Regulation 41 CFR Part 60; Executive Law of the State of New York, Sections 290–299 thereof, and any rules or regulations promulgated in accordance therewith; Section 504 of the Rehabilitation Act of 1973 and the Regulations issued pursuant thereto contained in 45 CFR Part 84 entitled "Nondiscrimination on the Basis of Handicap in Programs and Activities Receiving or Benefiting from Federal Financial Assistance"; and the Americans with Disabilities Act (ADA) of 1990, 42 U.S.C. Section 12116, and regulations issued by the Equal Employment Opportunity Commission which implement the employment provisions of the ADA, set forth at 29 CFR Part 1630.
- The Contractor is required to demonstrate effective affirmative efforts and to ensure employment of protected class members. The Contractor must possess and may upon request be required to submit to the Department a copy of an Affirmative Action Plan which is in full compliance with applicable requirements of federal and State statutes.
- Contractors and subcontractors shall undertake or continue existing programs of affirmative action to ensure that minority group members and women are afforded equal employment opportunities without discrimination because of race, creed, religion, color, national origin, sex, age, disability or marital status. For these purposes, affirmative action shall apply in the areas of recruitment, employment, job assignment, promotion, upgrading, demotion, transfer, layoff, or termination and rates of pay or other forms of compensation.
- Prior to the award of a State contract, the Contractor shall submit an Equal Employment Opportunity (EEO) Policy Statement to the Department within the time frame established by the Department.
- The Contractor´s EEO Policy Statement shall contain, but not necessarily be limited to, and the Contractor, as a precondition to entering into a valid and binding State contract, shall, during the performance of the State contract, agree to the following:
- The Contractor will not discriminate against any employee or Applicant for employment because of race, creed, religion, color, national origin, sex, age, sexual orientation, disability or marital status, will undertake or continue existing programs or affirmative action to ensure that minority group members and women are afforded equal employment opportunities without discrimination, and shall make and document its conscientious and active efforts to employ and utilize minority group members and women in its work force on State contracts.
- The Contractor shall state in all solicitations or advertisements for employees that, in the performance of the State contract all qualified applicants will be afforded equal employment opportunities without discrimination because of race, creed, religion, color, national origin, sex, age, disability or marital status.
- At the request of the contracting agency, the Contractor shall request each employment agency, labor union, or authorized representative of workers with which it has a collective bargaining of other agreement or understanding, to furnish a written statement that such employment agency, labor union, or representative will not discriminate on the basis of race, creed, religion, color, national origin, sex, age, sexual orientation, disability or marital status and that such union or representative will affirmatively cooperate in the implementation of the Contractor´s obligations herein.
- Except for construction contracts, prior to an award of a State contract, the Contractor shall submit to the contracting agency a staffing plan of the anticipated work force to be utilized on the State contract or, where required, information on the Contractor´s total work force, including apprentices, broken down by specified ethnic background, gender, and Federal Occupational Categories or other appropriate categories specified by the contracting agency. The form of the staffing plan shall be supplied by the contracting agency.
- After an award of a State contract, the Contractor shall submit to the contracting agency a work force utilization report, in a form and manner required by the agency, of the work force actually utilized on the State contract, broken down by specified ethnic background, gender, and Federal Occupational Categories or other appropriate categories specified by the contracting agency.
- In the event that the Contractor is found through an administrative or legal action, whether brought in conjunction with this Contract or any other activity engaged in by the Contractor, to have violated any of the laws recited herein in relation to the Contractor´s duty to ensure equal employment to protected class members, the Department may, in its discretion, determine that the Contractor has breached this Contract.
- Additionally, the Contractor and any of its subcontractors shall be bound by the applicable provisions of Article 15–A of the Executive Law, including Section 316 thereof, and any rules or regulations adopted pursuant thereto. The Contractor also agrees that any goal percentages contained in this Contract are subject to the requirements of Article 15–A of the Executive Law and regulations adopted pursuant thereto. For purposes of this Contract the goals established for subcontracting/purchasing with Minority and Women–Owned business enterprises are 0% to 5%. The employment goals for the hiring of protected class persons are 5% to 10%.
The Contractor shall submit reports as required by the Department, in a format determined by the Department, concerning the Contractor´s compliance with the above provisions, relating to the procurement of services, equipment and or commodities, subcontracting, staffing plans and for achievement or employment goals. The Contractor agrees to make available to the Department upon request, the information and data used in compiling such reports.
It is the policy of the Department to encourage the employment of qualified applicants/recipients of public assistance by both public organizations and private enterprises who are under contractual agreement to the Department for the provision of goods and services. The Department may require the Contractor to demonstrate how the Contractor has complied or will comply with the aforesaid policy.
DD. Omnibus Procurement Act of 1992
It is the policy of New York State to maximize opportunities for the participation of New York State business enterprises, including minority and women–owned business enterprises as Contractors, subcontractors, and suppliers on its procurement contracts. The Omnibus Procurement Act of 1992 requires that by signing this Contract, the Contractor certifies that whenever the total contract is greater than $1 million:
- The Contractor has made reasonable efforts to encourage the participation of New York State Business Enterprises as suppliers and subcontractors on this project, and has retained the documentation of these efforts to be provided upon request to the State;
- The Contractor has complied with the Federal Equal Opportunity Act of 1972 (Pub. L. 92–261), as amended;
- The Contractor agrees to make reasonable efforts to provide notification to New York State residents of employment opportunities on this project through listing any such positions with the Job Service Division of the New York State Department of Labor, or providing such notification in such manner as is consistent with existing collective bargaining contracts or agreements. The Contractor agrees to document these efforts and to provide such documentation upon request;
- The Contractor acknowledges notice that New York State may seek to obtain offset credits from foreign countries as a result of this Contract and agrees to cooperate with the State in these efforts.
EE. Nondiscrimination in Employment in Northern Ireland
In accordance with Chapter 807 of the Laws of 1992, the Contractor agrees that, if it or any individual or legal entity in which the Contractor holds a ten percent (10%) or greater ownership interest, or any individual or legal entity that holds a ten percent (10%) or greater ownership in the Contractor, has business operations in Northern Ireland, the Contractor, or such individual or legal entity, shall take lawful steps in good faith to conduct any business operations it has in Northern Ireland in accordance with MacBride Fair Employment Principles relating to nondiscrimination in employment and freedom of workplace opportunity, and shall permit independent monitoring of its compliance with such Principles.
FF. Contract Insurance Requirements.
The Contractor must, without expense to the State, procure and maintain, for the full term of the Contract, insurance of the kinds and in the amounts hereinafter provided, in insurance companies authorized to do such business in the State of New York covering all operations under this Contract, whether performed by it or by subcontractors. Before commencing the work, the Contractor shall furnish to the Department of Health a certificate or certificates, in a form satisfactory to said Department, showing that it has complied with the requirements of this Section, which certificate or certificates shall state that the policies shall not be changed or canceled until thirty (30) days written notice has been given to said Department. The kinds and amounts of required insurance are:
- A policy covering the obligations of the Contractor in accordance with the provisions of Chapter 41, Laws of 1914, as amended, known as the Workers´ Compensation Law, and the Contract shall be void and of no effect unless the Contractor procures such policy and maintains it for the full term of the Contract.
- Policies of Bodily Injury Liability and Property Damage Liability Insurance of the types hereinafter specified, each within limits of not less than $500,000 for all damages arising out of bodily injury, including death at any time resulting therefrom sustained by one person in any one occurrence, and subject to that limit for that person, not less than $1,000,000 for all damages arising out of bodily injury, including death at any time resulting therefrom sustained by two or more persons in any one occurrence, and not less than $500,000 for damages arising out of damage to or destruction of property during any single occurrence and not less than $1,000,000 aggregate for damages arising out of damage to or destruction of property during the policy period.
- Contractor´s Liability Insurance issued to and covering the liability of the Contractor with respect to all work performed by it under this proposal and the Contract.
- Protective Liability Insurance issued to and covering the liability of the People of the State of New York with respect to all operations under this Contract, by the Contractor or by its subcontractors, including omissions and supervisory acts of the State.
- Automobile Liability Insurance issued to and covering the liability of the People of the State of New York with respect to all operations under this Contract, by the Contractor or by its subcontractors, including omissions and supervisory acts of the State.
GG. Minority and Women Owned Business Policy Statement
The New York State Department of Health recognizes the need to take affirmative action to ensure that Minority and Women Owned Business Enterprises are given the opportunity to participate in the performance of the Department of Health´s contracting program. This opportunity for full participation in our free enterprise system by traditionally, socially and economically disadvantaged persons is essential to obtain social and economic equality and improve the functioning of the State economy.
It is the intention of the New York State Department of Health to fully execute the mandate of Executive Order–21 and provide Minority and Women Owned Business Enterprises with equal opportunity to bid on contracts awarded by this agency in accordance with the State Finance Law.
To implement this affirmative action policy statement, the Contractor agrees to file with the Department of Health within 10 days´ notice of award, a staffing plan of the anticipated work force to be utilized on this Contract or, where required, information on the Contractor´s total work force, including apprentices, broken down by specified ethnic background, gender, and Federal occupational categories or other appropriate categories specified by the Department. The form of the staffing shall be supplied by the Department, after an award of this Contract, the Contractor agrees to submit to the Department a work force utilization report, in a form and manner required by the Department, of the work force actually utilized on this Contract, broken down by specified ethnic background, gender and Federal occupational categories or other appropriate categories or other appropriate categories specified by the Department.
HH. Provisions Related to New York State Information Security Breach and Notification Act
Contractor shall comply with the provisions of the New York State Information Security Breach and Notification Act (General Business Law Section 899–aa; State Technology Law Section 208). Contractor shall be liable for the costs associated with such breach if caused by Contractor´s negligent or willful acts or omissions, or the negligent or willful acts or omissions of agents, officers, employees or subcontractors.
II. Accessibility of State Agency Web–based Intranet and Internet Information and Applications
Any web–based intranet and internet information and applications development, or programming delivered pursuant to the contract or procurement, will comply with New York State Enterprise IT Policy NYS–P08005, Accessibility of Web–Based Information and Applications, as such policy or standard may be amended, modified or superseded, which requires that state agency web–based intranet and internet information and applications are accessible to persons with disabilities. Web content must conform to New York State Enterprise IT Policy NYS–P08–005 as determined by quality assurance testing. Such quality assurance testing will be conducted by the Department and the awarded contractor and the results of such testing must be satisfactory to the Department before web content will be considered a qualified deliverable under the contract or procurement.
JJ. New York State Tax Law Section 5–a
Section 5–a of the Tax Law, as amended, effective April 26, 2006, requires certain contractors awarded state contracts for commodities, services and technology valued at more than $100,000 to certify to the New York State Department of Taxation and Finance (DTF) that they are registered to collect New York State and local sales and compensating use taxes. The law applies to contracts where the total amount of such contractors´ sales delivered into New York State are in excess of $300,000 for the four quarterly periods immediately preceding the quarterly period in which the certification is made, and with respect to any affiliates and subcontractors whose sales delivered into New York State exceeded $300,000 for the four quarterly periods immediately preceding the quarterly period in which the certification is made.
This law imposes upon certain contractors the obligation to certify whether or not the contractor, its affiliates, and its subcontractors are required to register to collect sales and compensating use tax and contractors must certify to DTF that each affiliate and subcontractor exceeding such sales threshold is registered with DTF to collect New York State and local sales and compensating use taxes. The law prohibits the State Comptroller, or other approving agencies, from approving a contract awarded to an offerer meeting the registration requirements but who is not so registered in accordance with the law.
Contractor must complete and submit directly to the New York State Department of Taxation and Finance, Contractor Certification Form ST–220–TD. Unless the information upon which the ST–220–TD is based changes, this form only needs to be filed once with the DTF. If the information changes for the Contractor, its affiliates(s), or its subcontractors(s), a new form (ST–220–TD) must be filed with the DTF.
Contractor must complete and submit to the Department of Health the form ST–220–CA certifying that the Contractor filed the ST–220–TD with DTF. Failure to make either of these filings may render an offerer non–responsive and non–responsible. Offerers shall take the necessary steps to provide properly certified forms within a timely manner to ensure compliance with the law.
KK.Provisions Related to New York State Procurement Lobbying Law
The State reserves the right to terminate this Contract in the event it is found that the certification filed by the Contractor in accordance with New York State Finance Law §139–k was intentionally false or intentionally incomplete. Upon such finding, the State may exercise its termination right by providing written notification to the Contractor in accordance with the written notification terms of the Contract.
LL. Piggybacking
New York State Finance Law Section 163(10)(e) [see also http://www.ogs.state.ny.us/procurecounc/pgbguidelines.asp] allows the Commissioner of the NYS Office of General Services to consent to the use of this Contract by other New York State Agencies, and other authorized purchasers, subject to conditions and the Contractor´s consent.
MM. Lead Guidelines
All products supplied pursuant to this agreement shall meet local, state and federal regulations, guidelines and action levels for lead as they exist at the time of the State´s acceptance of this Contract.
NN. Payment
Payment for claims/invoices submitted by the Contractor shall only be rendered electronically unless payment by paper check is expressly authorized by the Commissioner, in the Commissioner´s sole discretion, due to extenuating circumstances. Such electronic payment shall be made in accordance with ordinary State procedures and practices. The Contractor shall comply with the State Comptroller´s procedures to authorize electronic payments. Authorization forms are available at the State Comptroller´s website by email at epunit@osc.state.ny.us or by telephone at 518–474–6019. The Contractor acknowledges that it will not receive payment on any claims/invoices submitted under this Agreement if it does not comply with the State Comptroller´s electronic payment procedures, except where the Commissioner has expressly authorized payment by paper check as set forth above.
In addition to the Electronic Payment Authorization Form, a Substitute Form W–9, must be on file with the Office of the State Comptroller, Bureau of Accounting Operations. Additional information and procedures for enrollment can be found at http://www.osc.state.ny.us/epay.
Completed W–9 forms should be submitted to the following address:
NYS Office of the State ComptrollerBureau of Accounting Operations
Warrant & Payment Control Unit
110 State Street, 9th Floor
Albany, NY 12236
OO.M/WBE Utilization Plan for Subcontracting and Purchasing
The Department encourages the use of Minority and/or Women Owned Business Enterprises (M/WBEs) for any subcontracting or purchasing related to this contract. Contractors who are not currently a New York State certified M/WBE must define the portion of all consumable products and personnel required for this proposal that will be sourced from a M/WBE. The amount must be stated in total dollars and as a percent of the total cost necessary to fulfill the Agreement requirements. Supportive documentation must include a detailed description of work that is required including products and services.
The goal for usage of M/WBEs is at least 10% of monies used for contract activities. In order to assure a good–faith effort to attain this goal, the State requires that Contractors complete the M/WBE Utilization Plan and submit this Plan.
Contractors that are New York State certified MBEs or WBEs are not required to complete this form. Instead, such Contractors must simply provide evidence of their certified status.
Failure to submit the above referenced Plan (or evidence of certified M/WBE status) will result in disqualification of the vendor from consideration for award.
PP. On–going Vendor Responsibility
- General Responsibility Language
- The Contractor shall at all times during the Contract term remain responsible. The Contractor agrees, if requested by the Commissioner of Health or his or her designee, to present evidence of its continuing legal authority to do business in New York State, integrity, experience, ability, prior performance, and organizational and financial capacity.
- Suspension of Work (for Non–Responsibility)
- The Commissioner of Health or his or her designee, in his or her sole discretion, reserves the right to suspend any or all activities under this Contract, at any time, when he or she discovers information that calls into question the responsibility of the Contractor. In the event of such suspension, the Contractor will be given written notice outlining the particulars of such suspension. Upon issuance of such notice, the Contractor must comply with the terms of the suspension order. Contract activity may resume at such time as the Commissioner of Health or his or her designee issues a written notice authorizing a resumption of performance under the Contract.
- Termination (for Non–Responsibility)
- Upon written notice to the Contractor, and a reasonable opportunity to be heard with appropriate Department of Health officials or staff, the Contract may be terminated by the Commissioner of Health or his or her designee at the Contractor´s expense where the Contractor is determined by the Commissioner of Health or his or her designee to be non– responsible. In such event, the Commissioner of Health or his or her designee may complete the contractual requirements in any manner he or she may deem advisable and pursue available legal or equitable remedies for breach.
QQ. Veterans Protections
The Contractor shall contract with at least one veteran´s home that operates in its service area, provided that at least one veteran´s home operates in its service area.
Before March 31, 2015, and thereafter upon enrollment into Contractor´s MLTC Plan, the Contractor shall notify each veteran, spouse of a veteran, or Gold Star parent enrollee in need of long–term placement about the availability, or lack thereof, of a veteran´s home in Contractor´s network.
If Contractor´s MLTC Plan does not operate in an area with an accessible veteran´s home, or does not have one in its network, and unless otherwise indicated by the enrollee, the plan shall direct the enrollee to the enrollment broker. The Contractor must inform the enrollment broker of the matter and provide the enrollment broker with the applicable enrollee contact information.
If an applicable enrollee desires to receive care from a veteran´s home, the Contractor must allow the enrollee to access the veteran´s home services and must pay out of network until the enrollee has transferred to an MLTC Plan with an in–network veteran´s home.
The Contractor must inform enrollee about veteran´s home services available to them in the member handbook, including who is eligible for said services and their rights to receive said services, including, but not limited to, the rights outlined in this section.
|top of section| |top of page|APPENDIX A
STANDARD CLAUSES FOR NEW YORK STATE CONTRACTS
|top of section| |top of page|APPENDIX B
New York State Department of Health Guidelines for Contractor Compliance with the Federal Americans with Disabilities Act
I. OBJECTIVES
Title II of the ADA (Title II) and section 504 of the Rehabilitation Act of 1973 (Section 504) provides that no qualified individual with a disability shall, by reason of such disability, be excluded from participation in or denied access to the benefits of services, programs or activities of a public entity, or be subject to discrimination by such an entity. Public entities include state and local government and ADA and Section 504 requirements extend to all programs and services provided by state and local government. Since Medicaid is a government program, health services provided through Medicaid Managed Care, including MLTC, must be accessible to all that qualify for them.
MCO responsibilities for compliance with the ADA are imposed under Title II and Section 504 when, as a contractor in a Medicaid program, a plan is providing a government service. If an individual provider under contract with the MCO is not accessible, it is the responsibility of the MCO to make arrangements to assure that alternative services are provided. The MCO may determine it is expedient to make arrangements with other providers, or to describe reasonable alternative means and methods to make these services accessible through its existing Participating Providers. The goals of compliance with ADA Title II requirements are to offer a level of services that allows people with disabilities access to the program in its entirety, and the ability to achieve the same health care results as any Enrollee.
MCO responsibilities for compliance with the ADA are also imposed under Title III when the MCO functions as a public accommodation providing services to individuals (e.g. program areas and sites such as Marketing, education, member services, orientation, Complaints and Appeals). The goals of compliance with ADA Title III requirements are to offer a level of services that allows people with disabilities full and equal enjoyment of the goods, services, facilities or accommodations that the entity provides for its customers or clients. New and altered areas and facilities must be as accessible as possible. Whenever MCOs engage in new construction or renovation, compliance is also required with accessible design and construction standards promulgated pursuant to the ADA as well as State and local laws. Title III also requires that public accommodations undertake "readily achievable barrier removal" in existing facilities where architectural and communications barriers can be removed easily and without much difficulty or expense.
The State uses Plan Qualification Standards to qualify MCOs for participation in the MLTCP pursuant to the State´s responsibility to assure program access to all Enrollees, the Plan Qualification Standards require each MCO to submit an ADA Compliance Plan that describes in detail how the MCO will make services, programs and activities readily accessible and useable by individuals with disabilities. In the event that certain program sites are not readily accessible, the MCO must describe reasonable alternative methods for making the services or activities accessible and usable.
The objectives of these guidelines are threefold:
- To ensure that MCOs take appropriate steps to measure access and assure program accessibility for persons with disabilities;
- To provide a framework for MCOs as they develop a plan to assure compliance with the Americans with Disabilities Act (ADA); and
- To provide standards for the review of the MCO Compliance Plans.
These guidelines include a general standard followed by a discussion of specific considerations and suggestions of methods for assuring compliance. Please be advised that, although these guidelines and any subsequent reviews by state and local governments can give the Contractor guidance, it is ultimately the Contractor´s obligation to ensure that it complies with its Contractual obligations, as well as with the requirements of the ADA, Section 504, and other federal, state and local laws. Other federal, state and local statutes and regulations also prohibit discrimination on the basis of disability and may impose requirements in addition to those established under ADA. For example, while the ADA covers those impairments that "substantially" limit one or more of the major life activities of an individual, New York City Human Rights Law deletes the modifier "substantially".
II. DEFINITIONS
- "Auxiliary aids and services" may include qualified interpreters, note takers, computer– aided transcription services, written materials, telephone handset amplifiers, assistive listening systems, telephones compatible with hearing aids, closed caption decoders, open and closed captioning, telecommunications devices for Enrollees who are deaf or hard of hearing (TTY/TDD), video test displays, and other effective methods of making aurally delivered materials available to individuals with hearing impairments; qualified readers, taped texts, audio recordings, Braille materials, large print materials, or other effective methods of making visually delivered materials available to individuals with visual impairments.
- "Disability" means a mental or physical impairment that substantially limits one or more of the major life activities of an individual; a record of such impairment; or being regarded as having such an impairment.
III. SCOPE OF CONTRACTOR COMPLIANCE PLAN
The MCO Compliance Plan must address accessibility to services at MCO´s program sites, including both Participating Provider sites and MCO facilities intended for use by Enrollees.
IV. PROGRAM ACCESSIBILITY
Public programs and services, when viewed in their entirety must be readily accessible to and useable by individuals with disabilities. This standard includes physical access, non–discrimination in policies and procedures and communication. Communications with individuals with disabilities are required to be as effective as communications with others. The MCO Compliance Plan must include a detailed description of how MCO services, programs, and activities are readily accessible and usable by individuals with disabilities. In the event that full physical accessibility is not readily available for people with disabilities, the MCO Compliance Plan will describe the steps or actions the MCO will take to assure accessibility to services equivalent to those offered at the inaccessible facilities.
A. PRE–ENROLLMENT MARKETING AND EDUCATION STANDARD FOR COMPLIANCE
Marketing staff, activities and materials will be made available to persons with disabilities. Marketing materials will be made available in alternative formats (such as Braille, large print, and audiotapes) so that they are readily usable by people with disabilities.
Suggested Methods for Compliance
- Activities held in physically accessible location, or staff at activities available to meet with person in an accessible location as necessary
- Materials available in alternative formats, such as Braille, large print, audio tapes
- Staff training which includes training and information regarding attitudinal barriers related to disability
- Activities and fairs that include sign language interpreters or the distribution of a written summary of the marketing script used by plan marketing representatives
- Enrollee health promotion material/activities targeted specifically to persons with disabilities (e.g. secondary infection prevention, decubitus prevention, special exercise programs, etc.)
- Policy statement that Marketing Representatives will offer to read or summarize to blind or vision impaired individuals any written material that is typically distributed to all Enrollees
- Staff/resources available to assist individuals with cognitive impairments in understanding materials
Compliance Plan Submission
- A description of methods to ensure that the MCO´s Marketing presentations (materials and communications) are accessible to persons with auditory, visual and cognitive impairments
- A description of the MCO´s policies and procedures, including Marketing training, to ensure that Marketing Representatives neither screen health status nor ask questions about health status or prior health care services
B. MEMBER SERVICES DEPARTMENT
Member services functions include the provision to Enrollees of information necessary to make informed choices about treatment options, to effectively utilize the health care resources, to assist Enrollees in making appointments, and to field questions and Complaints, to assist Enrollees with the Complaint process.
B1. ACCESSIBILITY
STANDARD FOR COMPLIANCE
Member Services sites and functions will be made accessible to and usable by, people with disabilities.
SUGGESTED METHODS FOR COMPLIANCE (include, but are not limited to those identified below):
- Exterior routes of travel, at least 36" wide, from parking areas or public transportation stops into the Contractor´s facility
- If parking is provided, spaces reserved for people with disabilities, pedestrian ramps at sidewalks, and drop–offs
- Routes of travel into the facility are stable, slip–resistant, with all steps > ½" ramped, doorways with minimum 32" opening
- Interior halls and passageways providing a clear and unobstructed path or travel at least 36" wide to bathrooms and other rooms commonly used by Enrollees
- Waiting rooms, restrooms, and other rooms used by Enrollees are accessible to people with disabilities
- Sign language interpreters and other auxiliary aids and services provided in appropriate circumstances
- Materials available in alternative formats, such as Braille, large print, audio tapes
- Staff training which includes sensitivity training related to disability issues [Resources and technical assistance are available through the NYS Office of Advocate for Persons with Disabilities – V/TTY (800) 522–4369; and the NYC Mayor´s Office for People with Disabilities – (212) 788–2830 or TTY (212)788–2838]
- Availability of activities and educational materials tailored to specific conditions/illnesses and secondary conditions that affect these populations (e.g. secondary infection prevention, decubitus prevention, special exercise programs, etc.)
- MCO staff trained in the use of telecommunication devices for Enrollees who are deaf or hard of hearing (TTY/TDD) as well as in the use of NY Relay for phone communication
- New Enrollee orientation available in audio or by interpreter services
- Policy that when member services staff receive calls through the NY Relay, they will offer to return the call utilizing a direct TTY/TDD connection
COMPLIANCE PLAN SUBMISSION
- A description of accessibility to the member services department or reasonable alternative means to access member services for Enrollees using wheelchairs (or other mobility aids)
- A description of the methods the member services department will use to communicate with Enrollees who have visual or hearing impairments, including any necessary auxiliary aid/services for Enrollees who are deaf or hard of hearing, and TTY/TDD technology or NY Relay service available through a toll–free telephone number
- A description of the training provided to the member services staff to assure that staff adequately understands how to implement the requirements of the program, and of these guidelines, and are sensitive to the needs of persons with disabilities
B2. IDENTIFICATION OF ENROLLEES WITH DISABILITIES STANDARDS FOR COMPLIANCE
The Contractor must have in place satisfactory methods/guidelines for identifying persons at risk of, or having, chronic diseases and disabilities and determining their specific needs in terms of specialist physician referrals, durable medical equipment, medical supplies, home health services etc. The Contractor may not discriminate against a Prospective Enrollee based on his/her current health status or anticipated need for future health care. The Contractor may not discriminate on the basis of disability, or perceived disability of an Enrollee or their family member.
SUGGESTED METHODS FOR COMPLIANCE
- Appropriate post Enrollment health screening for each Enrollee, using an appropriate health screening tool
- Patient profiles by condition/disease for comparative analysis to national norms, with appropriate outreach and education
- Process for follow–up of needs identified by initial screening; e.g. referrals, assignment of case manager, assistance with scheduling/keeping appointments
- Enrolled population disability assessment survey
- Process for Enrollees who acquire a disability subsequent to Enrollment to access appropriate services
COMPLIANCE PLAN SUBMISSION
A description of how the Contractor will identify special health care, physical access or communication needs of Enrollees on a timely basis, including but not limited to the health care needs of Enrollees who:
- are blind or have visual impairments, including the type of auxiliary aids and services required by the Enrollee
- are deaf or hard of hearing, including the type of auxiliary aids and services required by the Enrollee
- have mobility impairments, including the extent, if any, to which they can ambulate
- have other physical or mental impairments or disabilities, including cognitive impairments
- have conditions which may require more intensive case management
B3. NEW ENROLLEE ORIENTATION
STANDARD FOR COMPLIANCE
Enrollees will be given information sufficient to ensure that they understand how to access medical care through the plan. This information will be made accessible to and usable by people with disabilities.
SUGGESTED METHODS FOR COMPLIANCE
- Activities held in physically accessible location, or staff at activities available to meet with person in an accessible location as necessary
- Materials available in alternative formats, such as Braille, large print, audio tapes
- Staff training which includes sensitivity training related to disability issues [Resources and technical assistance are available through the NYS Office of Advocate for Persons with Disabilities – V/TTY (800) 522–4369; and the NYC Mayor´s Office for People with Disabilities – (212) 788–2830 or TTY (212)788–2838]
- Activities and fairs that include sign language interpreters or the distribution of a written summary of the Marketing script used by plan marketing representatives
- Include in written/audio materials available to all Enrollees information regarding how and where people with disabilities can access help in getting services, for example help with making appointments or for arranging special transportation, an interpreter or assistive communication devices
- Staff/resources available to assist individuals with cognitive impairments in understanding materials
COMPLIANCE PLAN SUBMISSION
- A description of how the MCO will advise Enrollees with disabilities, during the new Enrollee orientation on how to access care
- A description of how the MCO will assist new Enrollees with disabilities (as well as current Enrollees who acquire a disability) in selecting or arranging an appointment with a Primary Care Practitioner (PCP)
- This should include a description of how the MCO will assure and provide notice to Enrollees who are deaf or hard of hearing, blind or who have visual impairments, of their right to obtain necessary auxiliary aids and services during appointments and in scheduling appointments and follow–up treatment with Participating Providers
- In the event that certain provider sites are not physically accessible to Enrollees with mobility impairments, the MCO will assure that reasonable alternative site and services are available
- A description of how the MCO will determine the specific needs of an Enrollee with or at risk of having a disability/chronic disease, in terms of specialist physician referrals, durable medical equipment (including assistive technology and adaptive equipment), medical supplies and home health services and will assure that such contractual services are provided
- A description of how the MCO will identify if an Enrollee with a disability requires on–going mental health services and how the MCO will encourage early entry into treatment
- A description of how the MCO will notify Enrollees with disabilities as to how to access transportation, where applicable
B4. COMPLAINTS, COMPLAINTS AND APPEALS STANDARDS FOR COMPLIANCE
The MCO will establish and maintain a procedure to protect the rights and interests of both Enrollees and the managed long–term care plans by receiving, processing, and resolving Complaints and Appeals in an expeditious manner, with the goal of ensuring resolution of Complaints/Appeals and access to appropriate services as rapidly as possible.
All Enrollees must be informed about the Grievance System within their plan and the procedure for filing Complaints and/or Appeals. This information will be made available through the Member Handbook, the Department´s toll–free Complaint line [1–(800) 206–8125] and the plan´s Complaint process annually, as well as when the MCO denies a benefit or referral. The MCO will inform Enrollees of: the MCO´s procedures; Enrollees´ right to contact the LDSS or the Department with a Complaint, and to file an Appeal or request a fair hearing; the right to appoint a designee to handle a Complaint or Appeal; and the toll–free Complaint line. The MCO will maintain designated staff to take and process complaints and be responsible for assisting Enrollees in complaint resolution.
The MCO will make all information regarding the Grievance System available to and usable by people with disabilities and will assure that people with disabilities have access to sites where Enrollees typically file Complaints and requests for Appeals.
SUGGESTED METHODS FOR COMPLIANCE
- Toll–free Complaint phone line with TDD/TTY capability
- Staff trained in Complaint process, and able to provide interpretive or assistive support to Enrollee during the Complaint process
- Notification materials and Complaint forms in alternative formats for Enrollees with visual or hearing impairments
- Availability of physically accessible sites, e.g. member services department sites
- Assistance for individuals with cognitive impairments
COMPLIANCE PLAN SUBMISSION
- A description of how the MCO´s Complaint and Appeal procedures shall be accessible for persons with disabilities, including:
- procedures for Complaints and Appeals to be made in person at sites accessible to persons with mobility impairments
- procedures accessible to persons with sensory or other impairments who wish to make verbal Complaints or Appeals, and to communicate with such persons on an ongoing basis as to the status or their Complaints and rights to further appeals
- description of methods to ensure notification material is available in alternative formats for Enrollees with vision and hearing impairments
- A description of how the Contractor monitors Complaints and Appeals related to people with disabilities.
C. Case Management
STANDARD FOR COMPLIANCE
MCOs must have in place adequate case management systems to identify the service needs of all Enrollees, including Enrollees with chronic illness and Enrollees with disabilities, and ensure that medically necessary covered benefits are delivered on a timely basis. These systems must include procedures for standing referrals, specialists as PCPs, and referrals to specialty centers for Enrollees who require specialized medical care over a prolonged period of time (as determined by a treatment plan approved by the MCO in consultation with the primary care provider, the designated specialist and the Enrollee or his/her designee), out–of–network referrals and continuation of existing treatment relationships with out–of–network providers (during transitional period).
SUGGESTED METHODS FOR COMPLIANCE
- Procedures for requesting specialist physicians to function as PCP
- Procedures for requesting standing referrals to specialists and/or specialty centers, out–of–network referrals, and continuation of existing treatment relationships
- Procedures to meet Enrollee needs for, durable medical equipment, medical supplies, home visits as appropriate
- Appropriately trained MCO staff to function as case managers for special needs populations, or sub–contract arrangements for case management
- Procedures for informing Enrollees about the availability of case management services
COMPLIANCE PLAN SUBMISSION
- A description of the MCO case management program for people with disabilities, including case management functions, procedures for qualifying for and being assigned a case manager, and description of case management staff qualifications
- A description of the MCO´s model protocol to enable Participating Providers, at their point of service, to identify Enrollees who require a case manager
- A description of the MCO´s protocol for assignment of specialists as PCP, and for standing referrals to specialists and specialty centers, out–of–network referrals and continuing treatment relationships
- A description of the MCO´s notice procedures to Enrollees regarding the availability of case management services, specialists as PCPs, standing referrals to specialists and specialty centers, out–of–network referrals and continuing treatment relationships
D. Participating Providers
STANDARD FOR COMPLIANCE
MCO´s networks will include all the provider types necessary to furnish the Benefit Package, to assure appropriate and timely health care to all Enrollees, including those with chronic illness and/or disabilities. Physical accessibility is not limited to entry to a provider site, but also includes access to services within the site, e.g. exam tables and medical equipment.
SUGGESTED METHODS FOR COMPLIANCE
- Process for the MCO to evaluate provider network to ascertain the degree of provider accessibility to persons with disabilities, to identify barriers to access and required modifications to policies/procedures
- Model protocol to assist Participating Providers, at their point of service, to identify Enrollees who require case manager, audio, visual, mobility aids, or other accommodations
- Model protocol for determining needs of Enrollees with mental disabilities
- Use of Wheelchair Accessibility Certification Form
- Submission of map of physically accessible sites
- Training for providers re: compliance with Title III of ADA, e.g. site access requirements for door widths, wheelchair ramps, accessible diagnostic/treatment rooms and equipment; communication issues; attitudinal barriers related to disability, etc. [Resources and technical assistance are available through the NYS Office of Advocate for Persons with Disabilities –V/TTY (800) 522–4369; and the NYC Mayor´s Office for People with Disabilities – (212) 788–2830 or TTY (212) 788–2838].
- Use of ADA Checklist for Existing Facilities and NYC Addendum to OAPD ADA Accessibility Checklist as guides for evaluating existing facilities and for new construction and/or alteration.
COMPLIANCE PLAN SUBMISSION
- A description of how the MCO will ensure that its Participating Provider network is accessible to persons with disabilities. This includes the following:
- Policies and procedures to prevent discrimination on the basis of disability or type of illness or condition
- Identification of Participating Provider sites which are accessible by people with mobility impairments, including people using mobility devices. If certain provider sites are not physically accessible to persons with disabilities, the MCO shall describe reasonable, alternative means that result in making the provider services readily accessible.
- Identification of Participating Provider sites which do not have access to sign language interpreters or reasonable alternative means to communicate with Enrollees who are deaf or hard of hearing; and for those sites describe reasonable alternative methods to ensure that services will be made accessible
- Identification of Participating Providers which do not have adequate communication systems for Enrollees who are blind or have vision impairments (e.g. raised symbol and lettering or visual signal appliances), and for those sites describe reasonable alternative methods to ensure that services will be made accessible
- A description of how the MCO´s specialty network is sufficient to meet the needs of Enrollees with disabilities
- A description of methods to ensure the coordination of out–of–network providers to meet the needs of the Enrollees with disabilities
- This may include the implementation of a referral system to ensure that the health care needs of Enrollees with disabilities are met appropriately
- MCO shall describe policies and procedures to allow for the continuation of existing relationships with out–of–network providers, when in the best interest of the Enrollee with a disability
- Submission of the ADA Compliance Summary Report or MCO statement that data submitted to the Department is an accurate reflection of each network´s physical accessibility
E. POPULATIONS WITH SPECIAL HEALTH CARE NEEDS
STANDARD FOR COMPLIANCE
MCOs will have satisfactory methods for identifying persons at risk of, or having, chronic disabilities and determining their specific needs in terms of specialist physician referrals, durable medical equipment, medical supplies, home health services, etc. MCOs will have satisfactory systems for coordinating service delivery and, if necessary, procedures to allow continuation of existing relationships with out–of–network provider for course of treatment.
SUGGESTED METHODS FOR COMPLIANCE
- Procedures for requesting standing referrals to specialists and/or specialty centers, specialist physicians to function as PCP, out–of–network referrals, and continuation of existing relationships with out–of–network providers for course of treatment
- Linkages with behavioral health agencies, disability and advocacy organizations, etc.
- Adequate network of providers and sub–specialists and contractual relationships with tertiary institutions
- Procedures for assuring that these populations receive appropriate diagnostic work–ups on a timely basis
- Procedures for assuring that these populations receive appropriate access to durable medical equipment on a timely basis
- Procedures for assuring that these populations receive appropriate allied health professionals (Physical, Occupational and Speech Therapists, Audiologists) on a timely basis
- State designation as a Well Qualified Plan to serve the OPWDD population and look–alikes
COMPLIANCE PLAN SUBMISSION
A description of arrangements to ensure access to specialty care providers and centers in and out of New York State, standing referrals, specialist physicians to function as PCP, out–of–network referrals, and continuation of existing relationships (out–of–network) for diagnosis and treatment of rare disorders
ADDITIONAL ADA RESPONSIBILITIES FOR PUBLIC ACCOMMODATIONS
Please note that Title III of the ADA applies to all non–governmental providers of health care. Title III of the Americans with Disabilities Act prohibits discrimination on the basis of disability in the full and equal enjoyment of goods, services, facilities, privileges, advantages or accommodations of any place of public accommodation. A public accommodation is a private entity that owns, leases or leases to, or operates a place of public accommodation. Places of public accommodation identified by the ADA include, but are not limited to, stores (including pharmacies) offices (including doctors´ offices), hospitals, health care providers, and social service centers.
New and altered areas and facilities must be as accessible as possible. Barriers must be removed from existing facilities when it is readily achievable, defined by the ADA as easily accomplishable without much difficulty or expense. Factors to be considered when determining if barrier removal is readily achievable include the cost of the action, the financial resources of the site involved, and, if applicable, the overall financial resources of any parent corporation or entity. If barrier removal is not readily achievable, the ADA requires alternate methods of making goods and services available. New facilities must be accessible unless structurally impracticable.
Title III also requires places of public accommodation to provide any auxiliary aids and services that are needed to ensure equal access to the services it offers, unless a fundamental alteration in the nature of services or an undue burden would result. Auxiliary aids include but are not limited to qualified sign interpreters, assistive listening systems, readers, large print materials, etc. Undue burden is defined as "significant difficulty or expense". The factors to be considered in determining "undue burden" include, but are not limited to, the nature and cost of the action required and the overall financial resources of the provider. "Undue burden" is a higher standard than "readily achievable" in that it requires a greater level of effort on the part of the public accommodation.
Please note also that the ADA is not the only law applicable for people with disabilities. In some cases, State or local laws require more than the ADA. For example, New York City´s Human Rights Law, which also prohibits discrimination against people with disabilities, includes people whose impairments are not as "substantial" as the narrower ADA and uses the higher "undue burden" ("reasonable") standard where the ADA requires only that which is "readily achievable". New York City´s Building Code does not permit access waivers for newly constructed facilities and requires incorporation of access features as existing facilities are renovated. Finally, the State Hospital code sets a higher standard than the ADA for provision of communication (such as sign language interpreters) for services provided at most hospitals, even on an outpatient basis.
|top of section| |top of page|APPENDIX C
Certification Regarding Lobbying
The undersigned certified, to the best of his or her knowledge, that:
- No Federal appropriated funds have been paid or will be paid to any person by or on behalf of the Contractor for the purpose of influencing or attempting to influence an officer or employee of any agency, a Member of Congress, an officer or employee of a Member of Congress in connection with the awarding of any Federal loan, the entering into any cooperative agreement, or the extension, continuation, renewal, amendment, or modification of any Federal contract, grant, loan or cooperative.
- If any funds other than Federal appropriated funds have been paid or will be paid to any person for influencing or attempting to influence an officer or employee of any agency, a Member of Congress, in connection with the award of any Federal contract, the entering into of any cooperative agreement, or the extension, continuation, renewal, amendment, or modification of any Federal contract, grant, loan or cooperative agreement, and the Agreement exceeds $100,000, the Contractor shall complete and submit Standard Form–LLL, "Disclosure Form to Report Lobbying," in accordance with its instructions.
- The Contractor shall include the provisions of this section in all provider Agreements under this Agreement and require all Participating Providers whose provider agreements exceed $100,000 to certify and disclose accordingly to the Contractor.
This certification is a material representation of fact upon which reliance was placed when this transaction was made or entered into. Submission of this certification is a prerequisite for making or entering into this transaction imposed pursuant to U.S.C. 1352 The failure to file the required certification shall subject the violator to a civil penalty of not less than $10,000 and no more than $100,000 for each such failure.
Date: ____________________________________________
Name (Printed): _______________________________
______________________________________________
(Signature)
Title: ______________________________________
Organization: _____________________________________________
APPENDIX D
Standard Form LLL Disclosure of Lobbying Activities
|top of section| |top of page|APPENDIX E–1
Requirements for Proof of Workers´ Compensation Coverage
Unless the Contractor is a political sub–division of New York State, the CONTRACTOR shall provide proof, completed by the Contractor´s insurance carrier and/or the Workers´ Compensation Board, of coverage for:
Workers´ Compensation, for which one of the following is incorporated into this contract as Appendix E–1:
- CE–200, Affidavit For New York Entities And Any Out–Of–State Entities With No Employees, That New York State Workers´ Compensation And/Or Disability Benefits Insurance Coverage Is Not Required; OR
- C–105.2 – Certificate of Workers´ Compensation Insurance. PLEASE NOTE: The State Insurance Fund provides its own version of this form, the U–26.3; OR
- SI–12 – Certificate of Workers´ Compensation Self–Insurance, OR GSI–105.2 – Certificate of Participation in Workers´ Compensation Group Self–Insurance.
NOTE: ACORD forms are NOT acceptable proof of coverage.
|top of section| |top of page|APPENDIX E–2
Requirements for Proof of Disability Insurance Coverage
Unless the Contractor is a political sub–division of New York State, the CONTRACTOR shall provide proof, completed by the Contractor´s insurance carrier and/or the Workers´ Compensation Board, of coverage for:
Disability Benefits coverage, for which one of the following is incorporated into this contract as Appendix E–2:
- CE–200, Affidavit For New York Entities And Any Out–Of–State Entities With No Employees, That New York State Workers´ Compensation And/Or Disability Benefits Insurance Coverage Is Not Required; OR
- DB–120.1 – Certificate of Disability Benefits Insurance; OR
- DB–155 – Certificate of Disability Benefits Self–Insurance
NOTE: ACORD forms are NOT acceptable proof of coverage.
|top of section| |top of page|APPENDIX F
SERVICE AREA AND AGES OF POPULATION TO BE SERVED
The service area of the Contractor is:
The Contractor will serve the following age group(s):
__________ ages 18 and older
__________ ages 21 and older
|top of section| |top of page|APPENDIX G
MANAGED LONG TERM CARE COVERED & NON–COVERED SERVICES
| Services When Provided, Would be Covered by the Capitation 1, 2 | Non–Covered Services; Excluded From The Capitation; Can Be Billed Fee–For–Service |
|---|---|
| Care Management | Inpatient Hospital Services |
| Nursing Home Care (Residential Health Care Facility) | Outpatient Hospital Services |
Home Care
|
Physician Services including services provided in an office setting, a clinic, a facility, or in the home.3 |
| Adult Day Health Care | Laboratory Services |
| Personal Care | Radiology and Radioisotope Services |
| DME – including Medical/Surgical Supplies, Enteral and Parenteral Formula,4 and Hearing Aid Batteries, Prosthetics, Orthotics, and Orthopedic Footwear | Emergency Transportation |
| Personal Emergency Response System | Rural Health Clinic Services |
| Non–emergent Transportation | Chronic Renal Dialysis |
| Podiatry | Mental Health Services |
| Dentistry | Alcohol and Substance Abuse Services |
| Optometry/Eyeglasses | OPWDD Services |
| PT, OT, SP or other therapies provided in a setting other than a home. Limited to 20 visits of each therapy type per calendar year, except for children under 21 and the developmentally disabled. MLTC plan may authorize additional visits. | Family Planning Services |
| Audiology/Hearing Aids | Prescription and Non–Prescription Drugs, Compounded Prescriptions |
| Respiratory Therapy | All other services listed in the Title XIX State Plan |
| Nutrition | |
| Private Duty Nursing | |
| Consumer Directed Personal Assistance Services | |
| Services Provided Through Care Management: | |
| Home Delivered or Congregate Meals | |
| Social Day Care | |
| Social and Environmental Supports | |
_______________________________
1. The capitation payment includes applicable Medicare coinsurance and deductibles for benefit package services. 1
2. Any of the services listed in this column, when provided in a diagnostic and treatment center, would be included in and covered by the capitation payment. 2
3. Includes nurse practitioners and physician assistants acting as "physician extenders." 3
4. Enteral formula limited to nasogastric, jejunostomy, or gastrostomy tube feeding; or treatment of an inborn error of metabolism 4
APPENDIX H
Schedule of Capitation Rates
Effective Date: ______________________________
|top of section| |top of page|APPENDIX I
Reserved
|top of section| |top of page|APPENDIX J
DEFINITIONS
Terms used in this Contract, which are not otherwise defined, shall have the meanings set forth below.
Definitions of covered services are intended to provide general information about the level of care available through the Medical Assistance Program. The full description and scope of services specified herein are established by the Medical Assistance Program as set forth in the applicable eMedNY Provider Manual. Managed care organizations may not define covered services more restrictively than the Medicaid Program. Contractors are expected to provide services for individual Enrollees as described in each Enrollee´s plan of care. Services may be provided either directly or through a sub–contract.
834 Electronic Data Interchange Transmission file (834 File). A HIPAA 5010 compliant transaction enacted as part of the Affordable Care Act (P.L. 111–148 and 111–152). The 834 is an electronic Benefit Enrollment and Maintenance document generated by the New York State of Health. The 834 file contains new enrollments, changes in enrollments, reinstatement of enrollments and disenrollment´s.
Abusive, as it relates to cause for involuntary disenrollment, means subjecting program staff to physical abuse or criminal activity which exposes staff to imminent danger or verbal threats which create in staff a reasonable concern for physical safety.
Action. An activity of a Contractor or its subcontractor that results in: a denial or limited authorization of a requested service (including the type or level of service); a restriction, reduction, suspension, or termination of a previously authorized service; denial, in whole or in part, of payment for a service; failure to provide services in a timely manner; determination that a requested service is not a covered benefit (does not include requests for services that are paid for fee–for–service outside the plan); or failure to act within the timeframes for resolution and notification of determinations regarding grievances, appeals, and grievance appeals, as provided in this Appendix and applicable law.
Alcohol and substance abuse services includes both inpatient and outpatient care. Inpatient services include but are not limited to: assessment, management of detoxification and withdrawal conditions, group, individual or family counseling, alcohol and substance abuse education, treatment planning, preventive counseling, discharge planning, and services to significant others provided in–home, office or the community. The following care is also provided: outpatient alcoholism rehabilitation services through programs certified by the Office of Alcoholism and Substance Abuse Services (OASAS) under 14 NYCRR Part 380.3 or 380.8; medically supervised ambulatory substance abuse treatment in 1035 facilities certified by OASAS under 14 NYCRR Part 1035; and Methadone Maintenance Treatment Program (MMTP) through facilities which provide MMTP as their principle mission and are certified by OASAS under 14 NYCRR Part 1040.
Adult day health care is care and services provided in a residential health care facility or approved extension site under the medical direction of a physician to a person who is functionally impaired, not homebound, and who requires certain preventive, diagnostic, therapeutic, rehabilitative or palliative items or services. Adult day health care includes the following services: medical, nursing, food and nutrition, social services, rehabilitation therapy, leisure time activities which are a planned program of diverse meaningful activities, dental pharmaceutical, and other ancillary services. Adult day health care providers must notify the Department of election to provide an unbundled service or payment option to MLTC enrollees, however enrollee participation in an ADHC and authorized for a limited service or payment option does not constitute need for CBLTCS and eligibility for plan enrollment.
Appeal: a request for a review of an action taken by the Contractor.
Applicant: An applicant is an individual who has expressed a desire to pursue enrollment in a MLTCP.
Audiology/hearing aids: Audiology services include audiometric examination or testing, hearing aid evaluation, conformity evaluation and hearing aid prescription or recommendations if indicated. Hearing aid services include selecting, fitting and dispensing of hearing aids, hearing aid checks following dispensing and hearing aid repairs. Products include hearing aids, earmolds, batteries, special fittings and replacement parts.
Auto–assignment means a process by which a MLTC Eligible Person, who is mandated to enroll in MLTC, but who has not selected and enrolled in a MLTCP within sixty (60) days of receipt of the mandatory notice sent by the Enrollment Broker, is assigned to a MLTCP offering a MLTCP product in the Eligible Person´s county of fiscal responsibility.
Balancing Incentive Program (BIP) is the New York State Balancing Incentive Program grant awarded by CMS under Section 10202 of the Affordable Care Act for the program period of April 1, 2013 through September 30, 2015 and includes all funding and programs offered through BIP and subject to the general and programmatic terms and conditions governing the grant.
Benefit package shall mean those medical and health–related services identified in Appendix G which Enrollees are entitled to receive pursuant to Article V. A. They are also known as the Benefit Package services or Covered Services.
CMS means the U.S. Centers for Medicare and Medicaid Services, formerly known as HCFA.
Care management is a process that assists Enrollees to access necessary covered services as identified in the care plan. It also provides referral and coordination of other services in support of the care plan. Care management services will assist Enrollees to obtain needed medical, social, educational, psychosocial, financial and other services in support of the care plan irrespective of whether the needed services are covered under the capitation payment of this Agreement.
Community Based Long Term Care Services (CBLTCS) means health care and supportive services provided to individuals of all ages with functional limitations or chronic illnesses who require assistance with routine daily activities such as bathing, dressing, preparing meals, and administering medications. CBLTCS is comprised of services such as Home Health Services, Private Duty Nursing, Consumer Directed Personal Assistance Services, Adult Day Health Care Program, Personal Care Services.
Contract period is the term of the contract plus any extensions.
Covered services shall mean those medical and health–related services identified in Appendix G which Enrollees are entitled to receive pursuant to Article V. A. They are also known as the Benefit Package or Benefit Package services.
Chronic renal dialysis includes services provided by a renal dialysis center.
DHHS: The Department of Health and Human Services of the United States.
Dentistry includes but shall not be limited to preventive, prophylactic and other dental care, services and supplies, routine exams, prophylaxis, oral surgery, and dental prosthetic and orthotic appliances required to alleviate a serious health condition including one which affects employability.
Durable Medical Equipment (DME), includes medical/surgical supplies, prosthetics and orthotics, and orthopedic footwear, enteral and parenteral formula and hearing aid batteries. Durable medical equipment are devices and equipment, other than prosthetic or orthotic appliances and devices, which have been ordered by a practitioner in the treatment of a specific medical condition, and which have the following characteristics:
- can withstand repeated use for a protracted period of time,
- are primarily and customarily used for medical purposes,
- are generally not useful in the absence of an illness or injury; and
- are not usually fitted, designed or fashioned for a particular individual´s use. Where equipment is intended for use by only one patient, it may be either custom–made or customized.
Medical/surgical supplies are items for medical use other than drugs, prosthetic or orthotic appliances and devices, durable medical equipment or orthopedic footwear which treat a specific medical condition and which are usually consumable, non–reusable, disposable, for a specific purpose and generally have no salvageable value.
Prosthetic appliances and devices are appliances and devices, which replace any missing part of the body.
Orthotic appliances and devices are appliances and devices used to support a weak or deformed body member or to restrict or eliminate motion in a diseased or injured part of the body.
Orthopedic footwear are shoes, shoe modifications or shoe additions which are used to correct, accommodate or prevent a physical deformity or range of motion malfunction in a diseased or injured part of the ankle or foot; to support a weak or deformed structure of the ankle or foot or to form an integral part of a brace.
Medicaid coverage of enteral formula and nutritional supplements is limited to individuals who cannot obtain nutrition through any other means, and to the flowing three conditions: 1) individuals who are fed via nasogastric, jejunostomy, or gastrostomy tube; 2) individuals with rare inborn metabolic disorders; and 3) Children up to age 21 who require liquid oral enteral nutritional formula when there is a documented diagnostic condition where caloric and dietary nutrients from food cannot be absorbed or metabolized. Coverage of certain inherited disease of amino acid and organic acid metabolism shall include modified solid food products that are low protein, or which contain modified protein.
Emergency condition means a medical or behavioral condition, the onset of which is sudden, that manifests itself by symptoms of sufficient severity, including severe pain, that a prudent layperson, possessing an average knowledge of medicine and health, could reasonably expect the absence of immediate medical attention to result in: (a) placing the health of the person affected with such condition in serious jeopardy, or in the case of a behavioral condition placing the health of such person or others in serious jeopardy; (b) serious impairment to such person´s bodily functions; (c) serious dysfunction of any bodily organ or part of such person; or (d) serious disfigurement of such person.
Emergency transportation is transportation by ambulance as a result of an emergency condition.
Enrollee shall mean a person enrolled in the plan who is entitled to covered services in accordance with the provisions of this Agreement from the effective date of his/her enrollment until the effective date of his/her disenrollment.
Enrollee agreement shall mean the written agreement provided to Enrollees, which agreement is to be signed by Enrollees and by the Contractor.
Grievance – An expression of dissatisfaction by the member or provider on member´s behalf about care and treatment that does not amount to a change in scope, amount or duration of service. A grievance can be verbal or in writing. Plans cannot require that members put grievances in writing. Plans must designate one or more qualified personnel who were not involved in any previous level of review or decision–making to review the grievance, and if the grievance pertains to clinical matters, the personnel must include licensed, certified or registered health care professionals.
HCFA shall mean the Health Care Financing Administration of Department of Health and Human Services (DHHS), now known as the Centers for Medicare and Medicaid Services.
Home care includes the following services which are of a preventive, therapeutic rehabilitative, health guidance and/or supportive nature: nursing services, home health aide services, nutritional services, social work services, physical therapy, occupational therapy and speech/language pathology.
Home health aide means a person who carries out health care tasks under the supervision of a registered nurse or licensed therapist and who may also provide assistance with personal hygiene, housekeeping and other related supportive tasks to an Enrollee with health care needs in his home. Qualifications of home health aides are defined in 10 NYCRR 700.2 (b)(9).
Hospice is a coordinated program of home and inpatient care that provides non–curative medical and support services for persons certified by a physician to be terminally–ill with a life expectancy of twelve (12) months or less. Hospice programs provide patients and families with palliative and supportive care to meet the special needs arising out of physical, psychological, spiritual, social and economic stresses which are experienced during the final stages of illness and during dying and bereavement.
Hospices are organizations that must be certified under PHL Article 40. All services must be provided by qualified employees and volunteers of the hospice or by qualified staff through contractual arrangement to the extent permitted by federal and state requirements. All services must be provided according to a written plan of care that reflects the changing needs of the patient/family.
HCS shall mean the Health Commerce System, an internet–based communications infrastructure of the New York State Department of Health designed to allow the secure and efficient exchange of reporting, surveillance, statistical, and general information with its public health and health provider partners.
Inpatient hospital services are those items and services, provided under the direction of a physician, physician´s assistant, nurse practitioner, or dentist, ordinarily furnished by the hospital for the care and treatment of inpatients. Inpatient hospital services include care, treatment, maintenance and nursing services as may be required on an inpatient hospital basis. Among other services, inpatient hospital services encompass a full range of necessary diagnostic and therapeutic care including medical, surgical, nursing, radiological and rehabilitative services.
Institutional Long Term Services and Supports (ITLSS) mean Residential Health Care Facility (Nursing Home) services as included in the Benefit Package and provided by the Contractor when medically necessary.
LDSS shall mean Local Department of Social Services or the Human Resources Administration of the City of New York.
Laboratory services include medically necessary tests and procedures ordered by a qualified medical professional and listed in the Medicaid fee schedule for laboratory services. Physicians providing laboratory testing may perform specific laboratory testing procedures identified in the Physician´s eMedNY Provider Manual.
Long Term Placement (Permanent Placement) Status means the status of an individual in a Residential Health Care Facility (RHCF) when the entity designated by the State determines that the individual is not expected to return home based on medical evidence affirming the individual´s need for long term (permanent) RHCF placement.
Managed Long Term Care Quality Incentive means a monetary incentive in the form of an add–on to managed long term care capitation payment rates that is awarded to MLTCs with superior performance in relation to a predetermined set of measures which may include quality of care, consumer satisfaction and compliance measures.
Managed Long Term Care Workforce Development Program is a program of the New York State Department of Health that is designed to support initiatives that attract, train, retrain, and retain Long Term Care workers in the types of skills that will be needed to support health care transformation, service integration and provider communication and coordination. The program will also address issues of health disparities by training and placing needed workers in Medically Underserved Areas.
Meals: Home–delivered and congregate meals provided in accordance with each individual Enrollee´s plan of care.
Medically necessary shall mean necessary to prevent, diagnose, correct or cure conditions in the Enrollee that cause acute suffering, endanger life, result in illness or infirmity, interfere with such Enrollee´s capacity for normal activity, or threaten some significant handicap.
Medical social services, means assessing the need for, arranging for and providing aid for social problems related to the maintenance of a patient in the home where such services are performed by a qualified social worker and provided within a plan of care. These services must be provided by a qualified social worker as defined in 10 NYCRR 700.2(b)(24).
Mental health services include both inpatient and outpatient care. Inpatient services include medically necessary voluntary and involuntary admission to State psychiatric centers, Article 31 inpatient psychiatric hospitals and Article 28 hospitals. Outpatient service include but are not limited to: assessment (stabilization), treatment planning, discharge planning, verbal therapies, medication therapy and education, symptom management, case management services, crisis intervention (and outreach services), chlozapine monitoring and collateral services as certified by OMH, rehabilitation services in OMH licensed community residences and family–based treatment programs certified under 14 NYCRR Part 586.3. Mental health services include: intensive psychiatric rehabilitation treatment programs under 14 NYCRR Part 587; day treatment services certified by OMH under 14 NYCRR Part 587; continuing day treatment services certified by OMH under 14 NYCRR Part 587; intensive case management for seriously and persistently mentally ill individuals; and partial hospitalization services certified by OMH under 14 NYCRR Part 587. Fee–for–service Medicaid does not cover inpatient mental health services in an Institution for Mental Disease (IMD) for individuals age 21 through 64.
New York State of Health (NYSoH) means an office located within the New York State Department of Health that functions as the state´s official health insurance marketplace. The NYSoH was established in accordance with the Patient Protection and Affordable Care Act of 2010. NYSoH provides a web portal through which individuals may apply for and enroll in Medicaid and other government sponsored health insurance or purchase standardized health insurance that is eligible for federal subsidies.
NAMI shall mean the amount of net available monthly income determined by the Department that a nursing home resident must pay monthly to the nursing home (or to the Contractor if stipulated in the Subcontract agreement) in accordance with the requirements of the medical assistance program.
Nurse practitioner services mean services provided under a practice agreement and practice protocol with a collaborating physician (agreement and protocol available to the Department during Medicaid audits) which meet the definitions for nurse practitioner services in the eMedNY Provider Manual, generally services considered to be primary care.
Nursing services include intermittent, part–time and continuous nursing services provided in accordance with an ordering physician´s treatment plan as outlined in the physician´s recommendation. Nursing services must be provided by RNs and LPNs in accordance with the Nurse Practice Act. Nursing services include care rendered directly to the individual and instructions to his family or caretaker in the procedures necessary for the patient´s treatment or maintenance.
Nursing home care is care provided to Enrollees by a licensed facility as specified in Chapter V, 10 NYCRR.
Nutrition means the assessment of nutritional needs and food patterns, or the planning for the provision of foods and drink appropriate for the individual´s physical and medical needs and environmental conditions, or the provision of nutrition education and counseling to meet normal and therapeutic needs. In addition, these services may include the assessment of nutritional status and food preferences, planning for provision of appropriate dietary intake within the patient´s home environment and cultural considerations, nutritional education regarding therapeutic diets as part of the treatment milieu, development of a nutritional treatment plan, regular evaluation and revision of nutritional plans, provision of in–service education to health agency staff as well as consultation on a specific dietary problems of patients and nutrition teaching to patients and families. These services must be provided by a qualified nutritionist as defined in 10 NYCRR 700.2(b)(5).
Occupational therapy: Rehabilitation services provided by a licensed and registered occupational therapist for the purpose of maximum reduction of physical or mental disability and restoration of the Enrollee to his or her best functional level. Medicaid coverage of occupational therapy provided in a setting other than a home is limited to 20 visits per calendar year, except for children under age 21 and the developmentally disabled. A MLTC plan may authorize additional visits.
OPWDD (Office for People with Developmental Disabilities) services include: long term therapy services provided by Article 16 clinic treatment facilities, certified by OPWDD under 14 NYCRR, Part 679 or provided by Article 28 D&TCs explicitly certified by the Department as serving primarily persons with developmental disabilities: day treatment services provided in an ICF or comparable facility and certified by OPWDD under 14 NYCRR, Part 690; Comprehensive Medicaid Case Management services; and home and community–based waiver program services for the developmentally disabled.
Optometry includes the services of an optometrist and an ophthalmic dispenser and includes eyeglasses; medical necessary contact lenses and polycarbonate lenses, artificial eyes (stock or custom made) and low vision aids. The optometrist may perform an eye exam to detect visual defects and eye disease as necessary or as required by the Enrollee´s condition. Examinations which include refraction are limited to every two years unless otherwise justified as medically necessary.
If the Contractor does not provide upgraded eyeglass frames or additional features (such as scratch coating, progressive lenses or photo–gray lenses) as part of its covered vision benefit, the Contractor cannot apply the cost of its covered eyeglass benefit to the total cost of the eyeglasses the Enrollee wants and bill only the difference to the Enrollee. For example, if the Contractor covers only standard bifocal lenses and the Enrollee wants no–line bifocal lenses, the Enrollee must choose between taking the standard bifocal or paying the full price of the no–line bifocal lenses (not just the difference between the cost of the bifocal lenses and the no–line lenses). However, the Enrollee may pay for upgraded lenses as a private customer and have the Contractor pay for the frames or pay for upgraded frames as a private customer and have the Contractor pay for the lenses. The Enrollee must be informed of this fact by the vision care provider at the time that the glasses are ordered.
An ophthalmic dispenser fills the prescription of an optometrist or ophthalmologist and supplies eyeglasses or other vision aids upon the order of qualified practitioner. Coverage includes the replacement of lost or destroyed eyeglasses. The replacement of a complete pair of eyeglasses should duplicate the original prescription and frames. Coverage also includes the repair or replacement of parts in situations where the damage is the result of causes other than defective workmanship. Replacement parts should duplicate the original prescription and frames. Repairs to and replacement of frames and/or lenses must be rendered as needed. Eyeglasses do not require changing more frequently than every two years unless medically indicated, such as a change in correction greater than ½ diopter, or unless the glasses are lost, damaged, or destroyed.
If the Contractor does not provide upgraded eyeglass frames or additional features (such as scratch coating, progressive lenses or photo–gray lenses) as part of its covered vision benefit, the Contractor cannot apply the cost of its covered eyeglass benefit to the total cost of the eyeglasses the Enrollee wants and bill only the difference to the Enrollee. For example, if the Contractor covers only standard bifocal lenses and the Enrollee wants no–line bifocal lenses, the Enrollee must choose between taking the standard bifocal or paying the full price of the no–line bifocal lenses (not just the difference between the cost of the bifocal lenses and the no–line lenses). However, the Enrollee may pay for upgraded lenses as a private customer and have the Contractor pay for the frames or pay for upgraded frames as a private customer and have the Contractor pay for the lenses. The Enrollee must be informed of this fact by the vision care provider at the time that the glasses are ordered.
Outpatient hospital services are services which are provided by a hospital division or department primarily engaged in providing services for ambulatory patients, by or under the supervision of a physician, for the prevention, diagnosis or treatment of human disease, pain, injury, deformity or physical condition.
Participating Provider means a provider of care and/or services that has a Provider Agreement with the Contractor.
Party shall mean either the Department or the Contractor.
Personal care means some or total assistance with such activities as personal hygiene, dressing and feeding, and nutritional and environmental support function tasks. Personal care must be medically necessary, ordered by the Enrollee´s physician and provided by a qualified person as defined in 10 NYCRR 700.2(b)(14), in accordance with a plan of care.
Person Centered Service Plan (or plan of care) is a written description in the care management record of member–specific health care goals to be achieved and the amount, duration and scope of the covered services to be provided to an Enrollee in order to achieve such goals. The person–centered individual service plan is based on assessment of the member´s health care needs and developed in consultation with the member and his/her informal supports. The plan includes consideration of the current and unique psycho–social and medical needs and history of the Enrollee, as well as the person´s functional level and support systems. Effectiveness of the person–centered service plan is monitored through reassessment and a determination as to whether the health care goals are being met. Non– covered services which interrelate with the covered services identified on the plan and services of informal supports necessary to support the health care goals and effectiveness of the covered services should be clearly identified on the person–centered service plan or elsewhere in the care management record.
Personal Emergency Response System (PERS): PERS is an electronic device which enables certain high–risk patients to secure help in the event of a physical, emotional or environmental emergency. A variety of electronic alert systems now exist which employ different signaling devices. Such systems are usually connected to a patient´s phone and signal a response center once a "help" button is activated. In the event of an emergency, the signal is received and appropriately acted on by a response center.
Physical therapy: Rehabilitation services provided by a licensed and registered physical therapist for the purpose of maximum reduction of physical or mental disability and restoration of the Enrollee to his or her best functional level. Medicaid coverage of physical therapy provided in a setting other than a home is limited to 20 visits per calendar year, except for children under age 21 and the developmentally disabled. A MLTC plan may authorize additional visits.
Physician services include the full range of preventive care services, primary care medical services and physician specialty services that fall within a physician´s scope of practice under New York State Law. Physician services include the services of physician extenders, e.g., physician´s assistants, social workers. Physician services may be provided in the office, home and facilities including but not limited to hospitals and diagnostic treatment centers.
Podiatry: Podiatry means services by a podiatrist which must include routine foot care when the Enrollee´s physical condition poses a hazard due to the presence of localized illness, injury or symptoms involving the foot, or when they are performed as necessary and integral part of medical care such as the diagnosis and treatment of diabetes, ulcers, and infections. Routine hygienic care of the feet, the treatment of corns and calluses, the trimming of nails, and other hygienic care such as cleaning or soaking feet, is not covered in the absence of pathological condition.
Potential Enrollee means a Medicaid recipient who is eligible to voluntarily elect to enroll in a managed long–term care plan but is not yet an Enrollee of managed long term care plan.
Prescription and non–prescription drugs: Include drugs on the "New York State List of Medicaid Reimbursable Drugs: Non–Prescription Drugs and Prescription Drugs" (inclusive of those agents such as blood products) as well as supplies which appear on the list of "Allowable Medical and Surgical Supplies" which are ordered by a qualified practitioner.
Private duty nursing services are medically necessary services provided to Enrollees at their permanent or temporary place of residence, by properly licensed registered professional or licensed practical nurses (RNs or LPNs), in accordance with physician orders. Such services may be continuous and may go beyond the scope of care available from certified home health care agencies (CHHAs).
Provider Contract: shall mean a written contract with the Contractor pursuant to which a person or entity provides certain services or items the Contractor deems necessary or advisable to the operation of the plan.
Provider: shall mean a person or entity with whom the Contractor has entered into a written Provider Contract.
Radiology and radioisotope services include medically necessary services provided by qualified practitioners in the provision of diagnostic radiology, diagnostic ultrasound, nuclear medicine, radiation oncology, and magnetic resonance imaging (MRI). These services are performed upon the order of a qualified practitioner.
Respiratory therapy means the performance of preventive, maintenance and rehabilitative airway–related techniques and procedures including the application of medical gases, humidity, and aerosols, intermittent positive pressure, continuous artificial ventilation, the administration of drugs through inhalation and related airway management, patient care, instruction of patients and provision of consultation to other health personnel. These services must be provided by a qualified respiratory therapist as defined in 10 NYCRR 700.2(b)(33).
Rural health clinic services are services provided by a clinic certified as a "rural health center" under 42 CFR 491.
Same Day Grievance means a grievance that is resolved by the Plan to the satisfaction of Enrollee the same day the grievance is lodged. A Same Day Grievance does not require written acknowledgement from the plan; however, information about the Same Day Grievance must be documented by the plan in its records.
Service area shall mean the geographic area for which the Contractor has been approved by the DOH to provide services.
Social and environmental supports are services and items that support the medical needs of the Enrollees and are included in an Enrollee´s plan of care. These services and items include but are not limited to the following: home maintenance tasks, homemaker/chore services, housing improvement, and respite care.
Social day care is a structured program which provides functionally impaired individuals with socialization; supervision and monitoring; and nutrition in a protective setting during any part of the day, but for less than a 24–hour period. Additional services may include and are not limited to personal care maintenance and enhancement of daily living skills, transportation, caregiver assistance, and case coordination and assistance.
Social services are information, referral, and assistance with obtaining or maintaining benefits which include financial assistance, medical assistance, food stamps, or other support programs provided by the LDSS, Social Security Administration, and other sources. Social services also involve providing supports and addressing problems in an Enrollee´s living environment and daily activities to assist the Enrollee to remain in the community.
Speech–language pathology: A licensed and registered speech–language pathologist provides rehabilitation services for the purpose of maximum reduction of physical or mental disability and restoration of the Enrollee to his or her best functional level. Medicaid coverage of speech therapy provided in a setting other than a home is limited to 20 visits per calendar year, except for children under age 21 and the developmentally disabled. A MLTC plan may authorize additional visits.
Surplus amounts: shall mean the amount of medical expenses the Department determines a "medically needy" individual must incur in any period in order to be eligible for medical assistance (as currently described in 18 NYCRR 360–4.8). Surplus amounts are also referred to as spenddown.
Third Party Health Insurance (TPHI) means comprehensive health care coverage or insurance (including Medicare and/or private MCO coverage) that does not fall under one of the following categories:
- accident–only coverage or disability income insurance;
- coverage issued as a supplement to liability insurance;
- liability insurance, including auto insurance;
- Workers Compensation or similar insurance;
- automobile medical payment insurance;
- credit–only insurance;
- coverage for on–site medical clinics;
- dental–only, vision–only, or long–term care insurance;
- specified disease coverage;
- hospital indemnity or other fixed dollar indemnity coverage; or
- prescription–only coverage.
Transportation: shall mean transport by ambulance, ambulette, taxi or livery service or public transportation at the appropriate level for the Enrollee´s condition for the Enrollee to obtain necessary medical care and services reimbursed under the New York State Plan for Medical Assistance or the Medicare Program. The Contractor is required to use only approved Medicaid ambulette vendors to provide ambulette transportation services to Enrollees.
Urgent care shall mean medically necessary services required in order to prevent a serious deterioration of an Enrollee´s health that results from an unforeseen illness or injury.
|top of section| |top of page|APPENDIX K
GRIEVANCE AND APPEAL SYSTEM, MEMBER HANDBOOK LANGUAGE, AND SERVICE AUTHORIZATION REQUIREMENTS
1. GRIEVANCE SYSTEM REQUIREMENTS
The Grievance System regulations in Subpart F of 42 CFR Part 438 apply to both "expressions of dissatisfaction" by Enrollees (grievances) and to requests for a review of an "action" (as defined in 438.400) by a managed long–term care plan (an appeal). For managed long–term care plans, the Grievance System processes identified in Subpart F have been combined with the grievance requirements in New York State Public Health Law (PHL) 4408–a and the utilization review and appeal requirements in Article 49 of the PHL.
A. Grievances
Grievance – An expression of dissatisfaction by the member or provider on member´s behalf about care and treatment that does not amount to a change in scope, amount or duration of service. A grievance can be verbal or in writing. Plans cannot require that members put grievances in writing. Plans must designate one or more qualified personnel who were not involved in any previous level of review or decision–making to review the grievance, and if the grievance pertains to clinical matters, the personnel must include licensed, certified or registered health care professionals.
Grievances that can be immediately (same day) decided to the member´s satisfaction do not need to be responded to in writing. Plans are required to document the grievance and decision, and log and track the grievance and decision for quality improvement purposes. If the grievance cannot be decided immediately (same day), the plan must decide if grievance is expedited or standard.
Expedited Grievance – the plan determines, or the provider indicates that a delay would seriously jeopardize the Enrollee´s life or health or ability to attain, maintain or regain maximum function. A member may also request an expedited review of a grievance.
Expedited and Standard Grievances
- Plan must send written acknowledgement of grievance within 15 business days of receipt. If a decision is reached before the written acknowledgement is sent, the plan may include the written acknowledgement with the notice of decision (one notice).
- Must be decided as fast as member´s condition requires, but no more than:
- Expedited: 48 hours from receipt of all necessary information, but no more than 7 calendar days from the receipt of the grievance.
- Standard: 45 calendar days from receipt of all necessary information, but no more than 60 calendar days from receipt of the grievance.
- Up to 14 calendar day extension. Extension may be requested by member or provider on member´s behalf (written or verbal). Plan may also initiate extension if it can justify need for additional information and if extension is in member´s interest. In all cases, extensions must be well documented.
- Plan must notify the member of decision by phone for expedited grievances and provide written notice of decision within 3 business days of decision (expedited and standard).
Grievance Appeal – Member has 60 business days after receipt of notice of grievance decision to file a written appeal. Appeal may be submitted by letter or on a form supplied by the plan. Upon receipt of a written appeal, the plan must decide if the appeal is expedited or standard appeal. A member or provider may also request an expedited review of a grievance appeal. The determination of a grievance appeal on a non–clinical matter must be made by qualified personnel at a higher level than the personnel who made the grievance determination. Grievance appeal determinations with a clinical basis must be made by personnel qualified to review the appeal, including licensed, certified or registered health care professionals who did not make the initial determination, at least one of whom must be a clinical peer reviewer.
Grievance Appeal – Expedited and Standard
- Plan must send written acknowledgement of grievance appeal within 15 business days of receipt of request. If a decision is reached before the written acknowledgement is sent, the plan may include the written acknowledgement with notice of decision (one notice).
- Must be decided as fast as member´s condition requires, but no more than:
- Expedited: 2 business days of receipt of all necessary information.
- Standard: 30 business days receipt of necessary information.
- Plan must provide written notice of decision. Notice must include reason for determination, and in cases where the determination has a clinical basis, the clinical rationale for the determination.
- No further appeal.
Necessary Written Notices for Grievances and Grievance Appeals
| Notices | Grievance | Grievance Appeal |
|---|---|---|
Written acknowledgement
|
X X |
X X X |
Notice of plan–initiated extension, if applicable. (May be combined with acknowledgement)
|
X X |
|
Plan Decision
|
X X X |
X X |
|
X | |
|
X |
Required Plan Documentation on Grievances and Grievance Appeals
The plan must maintain a file on each grievance and associated appeal, if any, that must include (at a minimum):
- the date the grievance/grievance appeal was filed and a copy of the grievance/grievance appeal;
- the date of receipt of and a copy of the Enrollee´s acknowledgement letter, if any, of the grievance/grievance appeal;
- all member/provider requests for expedited grievances/grievance appeals and plan decision about the request;
- necessary documentation to support any extensions, and
- the determination made by the plan, including the date of the determination, titles, and in the case of a clinical determination, the credentials of the plan´s personnel who reviewed the grievance/grievance appeal.
B. APPEALS
An Appeal is a request for a review of an action taken by a plan.
Expedited Appeal – the plan determines, or the provider indicates that a delay would seriously jeopardize the Enrollee´s life or health or ability to attain, maintain or regain maximum function or the action was the result of a concurrent review of a service authorization request. A member may also request an expedited review of an appeal. If an expedited review is not requested, the appeal will be treated as a standard appeal.
Plans must designate one or more qualified personnel who were not involved in any previous level of review or decision–making to review the appeal, and if the appeal pertains to clinical matters, the personnel must include licensed, certified or registered health care professionals.
The plan may deny a request for an expedited review, but it must make reasonable efforts to give oral notice of denial of an expedited review and send written notice within 2 calendar days of oral request. The appeal is then handled as a standard appeal. A member´s disagreement with plan´s decision to handle as a standard appeal is considered a grievance – see Grievance Procedures.
An appeal may be filed orally or in writing. If oral, the plan must provide the member with a summary of the appeal in writing as part of acknowledgement or separately. The date of the oral request for both standard and expedited appeals is treated as the date of the appeal.
Appeal – Expedited and Standard
- Appeal must be requested within 60 business days of postmark date of notice of action, or the intended effective date of the proposed action, whichever is later.
- Plan must send written acknowledgement of appeal within 15 days of receipt. If a decision is reached before the written acknowledgement is sent, the plan may include the written acknowledgement with the notice of decision (one notice).
- Must be decided as fast as member´s condition requires, but:
- Expedited: within 2 business days of receipt of necessary information, but no later than 3 business days of receipt of appeal request.
- Standard: no later than 30 calendar days of receipt of appeal request.
- Up to 14 calendar day extension. Extension may be requested by member or provider on member´s behalf (written or verbal). Plan may also initiate extension if it can justify need for additional information and if extension is in the member´s interest. In all cases, extension reason must be well–documented
- Plan must make a reasonable effort to give oral notice for expedited appeals and must send written notice within 2 business days of decision for all appeals. If dissatisfied, members may file both State Fair Hearing and External Appeal. If both are filed, the State Fair Hearing decision is the one that counts.
Necessary Templates for Written Notices for Appeals – Expedited and Standard
The Contractor shall ensure that all notices are in writing and in easily understood language and are accessible to non–English speaking and visually impaired enrollees. Notices shall include that oral interpretation and alternate formats of written material for enrollees with special needs are available and how to access the alternate formats.
All notices must include up–to–date contact information for the Independent Consumer Advocacy Network (ICAN), along with the following statement: "You can also call the Independent Consumer Advocacy Network (ICAN) to get free, independent advice about your coverage, complaints, and appeals´ options. They can help you manage the appeal process. Contact ICAN to learn more about their services:"
- Letter indicating the plan will not make a determination on the appeal because the appeal request was not submitted by the member within 60 business days of the notice of action.
- Written acknowledgement
- Name, address and telephone number of the individual or department designated by the plan to respond to the appeal.
- If a member has requested an expedited appeal and the plan has decided not to expedite the appeal, the acknowledgement must indicate that the appeal will be handled on a standard basis, and inform the member of his/her right to file a grievance and how to do so.
- The acknowledgement must identify any additional information required by the plan from any source to make the appeal decision.
- Notice of plan–initiated extension, if applicable (may be combined with acknowledgement)
- Reason for extension
- How the delay is in the best interest of the member
- Any additional information that the plan requires from any source to make its determination
- Final Determination (Action Appeal) Notices
Notice to the Enrollee of Action Appeal determinations shall be dated and include:- Date the Action Appeal was filed and a summary of the Action Appeal;
- Date the Action Appeal process was completed;
- The results and the reasons for the determination, including the clinical rationale, if any;
- If the determination was not wholly in favor of the Enrollee, and:
- the Contractor upheld its original action, a statement that reminds the Enrollee of their right to request a fair hearing, including:
- that a request for a fair hearing must have been made to the State within 60 days of the initial action notice;
- the date by which such request must have been made; and
- if time remains for a fair hearing to be requested, instructions on how to request a fair hearing; or a statement that time to request a fair hearing has expired.
- the Contractor modified its original action in any way, a statement that the Action Appeal determination constitutes a new action, and the Enrollee has a right to request a fair hearing, including:
- that a request for a fair hearing must be made to the State within 60 days of the date of the Action Appeal notice; and
- a completed Department standard "4687 MLTC Action Taken –Denial, Reduction or Termination of Benefits (211)" notice for denial of benefits or for termination or reduction in benefits, as applicable, containing the Enrollee´s fair hearing and aid continuing rights.
- the Contractor upheld its original action, a statement that reminds the Enrollee of their right to request a fair hearing, including:
- The right of the Enrollee to contact the New York State Department of Health regarding his or her Complaint, including the Department´s toll–free number for Complaints; and
- For Action Appeals involving personal care services, the number of hours per day, number of hours per week, and the personal care services function (Level I/Level II):
- that were previously authorized, if any;
- that were requested by the Enrollee or their designee, if so specified in the request;
- that are authorized for the new authorization period, if any; and
- the original authorization period and the new authorization period, as applicable.
- For Action Appeals involving medical necessity or an experimental or investigational treatment, the notice must also include:
- a clear statement that the notice constitutes the final adverse determination and specifically use the terms "medical necessity" or "experimental/investigational;"
- the Enrollee´s coverage type;
- the procedure in question, and if available and applicable the name of the provider and developer/manufacturer of the health care service;
- statement that the Enrollee is eligible to file an External Appeal and the timeframe for filing, and if the Action Appeal was expedited, a statement that the Enrollee may choose to file a standard Action Appeal with the Contractor or file an External Appeal;
- a copy of the "Standard Description and Instructions for Health Care Consumers to Request an External Appeal" and the External Appeal application form;
- the Contractor´s contact person and telephone number;
- the contact person, telephone number, company name and full address of the utilization review agent, if the determination was made by the agent; and
- if the Contractor has a second level internal review process, the notice shall contain instructions on how to file a second level Action Appeal and a statement in bold text that the timeframe for requesting an External Appeal begins upon receipt of the final adverse determination of the first level Action Appeal, regardless of whether or not a second level of Action Appeal is requested, and that by choosing to request a second level Action Appeal, the time may expire for the Enrollee to request an External Appeal.
(Plans must notify members of the availability of assistance (for language, hearing, speech issues) if a member wants to file Fair Hearing request and/or an External Appeal and how to access that assistance.)
Required Plan Documentation for Appeals
The plan must maintain a file on each action and associated appeal (both expedited and standard), if any, that includes (at a minimum):
- a copy of the notice of action;
- the date the appeal was filed;
- a copy of the appeal;
- member/provider requests for expedited appeals and the plan´s decision;
- the date of receipt of and a copy of the Enrollee´s acknowledgment letter of the appeal (if any);
- necessary documentation to support any extensions, and
- the determination made by the plan, including the date of the determination, the titles and, in the case of clinical determinations, the credentials, of the plan´s personnel who reviewed the appeal.
2. MODEL MEMBER HANDBOOK GRIEVANCE AND APPEAL LANGUAGE
The following language relating to the managed long–term care demonstration grievance and appeal process must appear in the Contractor´s Member Handbook.
__________________ (plan name) will try its best to deal with your concerns or issues as quickly as possible and to your satisfaction. You may use either our grievance process or our appeal process, depending on what kind of problem you have.
There will be no change in your services or the way you are treated by (insert plan name) staff or a health care provider because you file a grievance or an appeal. We will maintain your privacy. We will give you any help you may need to file a grievance or appeal. This includes providing you with interpreter services or help if you have vision and/or hearing problems. You may choose someone (like a relative or friend or a provider) to act for you.
To file a grievance or to appeal a plan action, please call: xxxxxxx or write to: xxxxxxx When you contact us, you will need to give us your name, address, telephone number and the details of the problem.
What is a Grievance?
A grievance is any communication by you to us of dissatisfaction about the care and treatment you receive from our staff or providers of covered services. For example, if someone was rude to you or you do not like the quality of care or services you have received from us, you can file a grievance with us.
The Grievance Process
You may file a grievance orally or in writing with us. The person who receives your grievance will record it, and appropriate plan staff will oversee the review of the grievance. We will send you a letter telling you that we received your grievance and a description of our review process. We will review your grievance and give you a written answer within one of two timeframes.
- If a delay would significantly increase the risk to your health, we will decide within 48 hours after receipt of necessary information
- For all other types of grievances, we will notify you of our decision within
45 days of receipt of necessary information, but the process must be completed within 60 days of the receipt of the grievance. The review period can be increased up to 14 days if you request it or if we need more information and the delay is in your interest.
Our answer will describe what we found when we reviewed your grievance and our decision about your grievance.
How do I Appeal a Grievance Decision?
If you are not satisfied with the decision we make concerning your grievance, you may request a second review of your issue by filing a grievance appeal. You must file a grievance appeal in writing. It must be filed within 60 business days of receipt of our initial decision about your grievance. Once we receive your appeal, we will send you a written acknowledgement telling you the name, address and telephone number of the individual we have designated to respond to your appeal. All grievance appeals will be conducted by appropriate professionals, including health care professionals for grievances involving clinical matters, who were not involved in the initial decision.
For standard appeals, we will make the appeal decision within 30 business days after we receive all necessary information to make our decision. If a delay in making our decision would significantly increase the risk to your health, we will use the expedited grievance appeal process. For expedited grievance appeals, we will make our appeal decision within 2 business days of receipt of necessary information. For both standard and expedited grievance appeals, we will provide you with written notice of our decision. The notice will include the detailed reasons for our decision and, in cases involving clinical matters, the clinical rationale for our decision.
What is an Action?
When (insert plan name) denies or limits services requested by you or your provider; denies a request for a referral; decides that a requested service is not a covered benefit; restricts, reduces, suspends or terminates services that we already authorized; denies payment for services; doesn´t provide timely services; or doesn´t make grievance or appeal determinations within the required timeframes, those are considered plan "actions". An action is subject to appeal. (See How do I File an Appeal of an Action? below for more information.)
Timing of Notice of Action
If we decide to deny or limit services you requested or decide not to pay for all or part of a covered service, we will send you a notice when we make our decision. If we are proposing to restrict, reduce, suspend or terminate a service that is authorized, our letter will be sent at least 10 days before we intend to change the service.
Contents of the Notice of Action
Any notice we send to you about an action will:
- Explain the action we have taken or intend to take;
- Cite the reasons for the action, including the clinical rationale, if any;
- Describe your right to file an appeal with us (including whether you may also have a right to the State´s external appeal process);
- Describe how to file an internal appeal and the circumstances under which you can request that we speed up (expedite) our review of your internal appeal;
- Describe the availability of the clinical review criteria relied upon in making the decision, if the action involved issues of medical necessity or whether the treatment or service in question was experimental or investigational;
- Describe the information, if any, that must be provided by you and/or your provider in order for us to render a decision on appeal.
The notice will also tell you about your right to a State Fair Hearing:
- It will explain the difference between an appeal and a Fair Hearing;
- It will say that that you do not have to file an appeal before asking for a Fair Hearing;
- It will explain how to ask for a Fair Hearing; and
- If we are reducing, suspending, or terminating an authorized service and you want your services to continue while your appeal is decided, you must ask for a Fair Hearing within 10 days of the date on the notice or the intended effective date of the proposed action, whichever is later.
How do I File an Appeal of an Action?
If you do not agree with an action that we have taken, you may appeal. When you file an appeal, it means that we must look again at the reason for our action to decide if we were correct. You can file an appeal of an action with the plan orally or in writing. When the plan sends you a letter about an action it is taking (like denying or limiting services, or not paying for services), you must file your appeal request within 60 business days of the date on our letter notifying you of the action.
How do I Contact my Plan to file an Appeal?
We can be reached by calling XXX–XXX–XXXX or writing to (address). The person who receives your appeal will record it, and appropriate staff will oversee the review of the appeal. We will send a letter telling you that we received your appeal, and how we will handle it. Your appeal will be reviewed by knowledgeable clinical staff who were not involved in the plan´s initial decision or action that you are appealing.
For Some Actions You May Request to Continue Service During the Appeal Process
If you are appealing a restriction, reduction, suspension or termination of services you are currently authorized to receive, you must request a Fair Hearing to continue to receive these services while your appeal is decided. We must continue your service if you ask for a Fair Hearing no later than 10 days from the date on the notice about the restriction, reduction, suspension or termination of services or the intended effective date of the proposed action, whichever is later. To find out how to ask for a Fair Hearing, and to ask for aid to continue, see the Fair Hearing Section below.
Although you may request a continuation of services, if the Fair Hearing is not decided in your favor, we may require you to pay for these services if they were provided only because you asked to continue to receive them while your case was being reviewed.
How Long Will it Take the Plan to Decide My Appeal of an Action?
Unless you ask for an expedited review, we will review your appeal of the action taken by us as a standard appeal and send you a written decision as quickly as your health condition requires, but no later than 30 days from the day we receive an appeal. (The review period can be increased up to 14 days if you request an extension or we need more information and the delay is in your interest.) During our review you will have a chance to present your case in person and in writing. You will also have the chance to look at any of your records that are part of the appeal review.
We will send you a notice about the decision we made about your appeal that will identify the decision we made and the date we reached that decision.
If we reverse our decision to deny or limit requested services, or restrict, reduce, suspend or terminate services, and services were not furnished while your appeal was pending, we will provide you with the disputed services as quickly as your health condition requires. In some cases, you may request an "expedited" appeal. (See Expedited Appeal Process Section below.)
Expedited Appeal Process
If you or your provider feels that taking the time for a standard appeal could result in a serious problem to your health or life, you may ask for an expedited review of your appeal of the action. We will respond to you with our decision within 2 business days after we receive all necessary information. In no event will the time for issuing our decision be more than 3 business days after we receive your appeal. (The review period can be increased up to 14 days if you request an extension or we need more information and the delay is in your interest.)
If we do not agree with your request to expedite your appeal, we will make our best efforts to contact you in person to let you know that we have denied your request for an expedited appeal and will handle it as a standard appeal. Also, we will send you a written notice of our decision to deny your request for an expedited appeal within 2 days of receiving your request.
If the Plan Denies My Appeal, What Can I Do?
If our decision about your appeal is not totally in your favor, the notice you receive will explain your right to request a Medicaid Fair Hearing from New York State and how to obtain a Fair Hearing, who can appear at the Fair Hearing on your behalf, and for some appeals, your right to request to receive services while the Hearing is pending and how to make the request.
Note: You must request a Fair Hearing within 60 calendar days after the date on the Initial Determination Notice. This deadline applies even if you are waiting for us to make a decision on your Internal Appeal.
If we deny your appeal because of issues of medical necessity or because the service in question was experimental or investigational, the notice will also explain how to ask New York State for an "external appeal" of our decision.
State Fair Hearings
You may also request a Fair Hearing from New York State. The Fair Hearing decision can overrule our original decision, whether or not you asked us for an appeal. You must request a Fair Hearing within 60 calendar days of the date we sent you the notice about our original decision. You can pursue a Plan appeal and a Fair Hearing at the same time, or you can wait until the Plan decides your appeal and then ask for a Fair Hearing. In either case, the same 60 calendar day deadline applies.
The State Fair Hearing process is the only process that allows your services to continue while you are waiting for your case to be decided. If we send you a notice about restricting, reducing, suspending, or terminating services you are authorized to receive, and you want your services to continue, you must request a Fair Hearing. Filing an internal or external appeal will not guarantee that your services will continue.
To make sure that your services continue pending the appeal, generally you must request the Fair Hearing AND make it clear that you want your services to continue. Some forms may automatically do this for you, but not all of them, so please read the form carefully. In all cases, you must make your request within 10 days of the date on the notice, or by the intended effective date of our action (whichever is later).
Your benefits will continue until you withdraw the appeal; the original authorization period for your services ends; or the State Fair Hearing Officer issues a hearing decision that is not in your favor, whichever occurs first.
If the State Fair Hearing Officer reverses our decision, we must make sure that you receive the disputed services promptly, and as soon as your health condition requires. If you received the disputed services while your appeal was pending, we will be responsible for payment for the covered services ordered by the Fair Hearing Officer.
Although you may request to continue services while you are waiting for your Fair Hearing decision, if your Fair Hearing is not decided in your favor, you may be responsible for paying for the services that were the subject of the Fair Hearing.
You can file a State Fair Hearing by contacting the Office of Temporary and Disability Assistance:
- Online Request Form
- Mail a Printable Request Form:
NYS Office of Temporary and Disability Assistance
Office of Administrative Hearings
Managed Care Hearing Unit
P.O. Box 22023
Albany, New York 12201–2023 - Fax a Printable Request Form: (518) 473–6735
- Request by Telephone:
Standard Fair Hearing line – 1 (800) 342–3334
Emergency Fair Hearing line – 1 (800) 205–0110
TTY line – 711 (request that the operator call 1 (877) 502–6155) - Request in Person:
14 Boerum Place, 1st Floor
Brooklyn, New York 11201
40 North Pearl Street, 15th Floor
Albany, New York 12243
For more information on how to request a Fair Hearing, please visit: here.
State External Appeals
If we deny your appeal because we determine the service is not medically necessary or is experimental or investigational, you may ask for an external appeal from New York State. The external appeal is decided by reviewers who do not work for us or New York State. These reviewers are qualified people approved by New York State. You do not have to pay for an external appeal.
When we make a decision to deny an appeal for lack of medical necessity or on the basis that the service is experimental or investigational, we will provide you with information about how to file an external appeal, including a form on which to file the external appeal along with our decision to deny an appeal. If you want an external appeal, you must file the form with the New York State Department of Financial Services within four months from the date we denied your appeal.
Your external appeal will be decided within 30 days. More time (up to 5 business days) may be needed if the external appeal reviewer asks for more information. The reviewer will tell you and us of the final decision within two business days after the decision is made.
You can get a faster decision if your doctor can say that a delay will cause serious harm to your health. This is called an expedited external appeal. The external appeal reviewer will decide an expedited appeal in 3 days or less. The reviewer will tell you and us the decision right away by phone or fax. Later, a letter will be sent that tells you the decision.
You may ask for both a Fair Hearing and an external appeal. If you ask for a Fair Hearing and an external appeal, the decision of the Fair Hearing officer will be the "one that counts."
3. SERVICE AUTHORIZATIONS & ACTION REQUIREMENTS
Definitions
Prior Authorization Review: review of a request by the Enrollee, or provider on Enrollee´s behalf, for coverage of a new service (whether for a new authorization period or within an existing authorization period) or a request to change a service as determined in the plan of care for a new authorization period, before such service is provided to the Enrollee.
Concurrent Review: review of a request by an Enrollee, or provider on Enrollee´s behalf, for additional services (i.e., more of the same) that are currently authorized in the plan of care or for Medicaid covered home health care services following an inpatient admission.
Expedited Review: An Enrollee must receive an expedited review of his or her Service Authorization Request when the plan determines, or a provider indicates that a delay would seriously jeopardize the Enrollee´s life, health, or ability to attain, maintain, or regain maximum function. The Enrollee may request an expedited review of a Prior Authorization or Concurrent Review. Appeals of actions resulting from a Concurrent Review must be handled as expedited.
General Provisions
Any Action taken by the Contractor regarding medical necessity or experimental or investigational services must be made by a clinical peer reviewer as defined by PHL §4900(2)(a).
Adverse Determinations, other than those regarding medical necessity or experimental or investigational services, must be made by a licensed, certified, or registered health care professional when such determination is based on an assessment of the Enrollee´s health status or of the appropriateness of the level, quantity or delivery method of care. This requirement applies to determinations denying claims because the services in question are not a covered benefit when coverage is dependent on an assessment of the Enrollee´s health status, and to Service Authorization Requests including but not limited to: services included in the Benefit Package, referrals, and out–of–network services.
The plan must notify members of the availability of assistance (for language, hearing, speech issues) if member wants to file appeal and how to access that assistance.
The Contractor shall utilize the Department´s model MLTC Initial Adverse Determination and 4687 MLTC Action Taken notices.
Timeframes for Service Authorization Determination and Notification
- For Prior Authorization requests, the Contractor must make a Service Authorization Determination and notice the Enrollee of the determination by phone and in writing as fast as the Enrollee´s condition requires and no more than:
- Expedited: three (3) business days after receipt of the Service Authorization Request
- Standard: three (3) business days after receipt of necessary information, but no more than fourteen (14) days after receipt of request for Service Authorization Request.
- For Concurrent Review Requests, the Contractor must make a Service Authorization Determination and notice the Enrollee of the determination by phone and in writing as fast as the Enrollee´s condition requires and no more than:
- Expedited: one (1) business day after receipt of necessary information, but no more than three (3) business days of receipt of the Service Authorization Request
- Standard: one (1) business day after receipt of necessary information, but no more than fourteen (14) days of receipt of the Service Authorization Request
- In the case of a request for Medicaid covered home health care services following an inpatient admission, one (1) business day after receipt of necessary information; except when the day subsequent to the Service Authorization Request falls on a weekend or holiday, then seventy–two (72) hours after receipt of necessary information; but in any event, no more than three (3) business days after receipt of the Service Authorization Request.
- Up to 14 calendar day extension. Extension may be requested by Enrollee or provider on Enrollee´s behalf (written or verbal). The plan also may initiate an extension if it can justify need for additional information and if the extension is in the Enrollee´s interest. In all cases, the extension reason must be well documented.
- The MLTC Plan must notify enrollee of a plan–initiated extension of the deadline for review of his or her service request. The MLTC Plan must explain the reason for the delay, and how the delay is in the best interest of the Enrollee. The MLTC Plan should request any additional information required to help make a determination or redetermination and help the enrollee by listing potential sources of the requested information.
- Enrollee or provider may appeal decision – see Appeal Procedures.
- If the plan denied the Enrollee´s request for an expedited review, the plan will handle as standard review.
- The Contractor must notice the Enrollee if his or her request for expedited review is denied, and that Enrollee´s service request will be reviewed in the standard timeframe.
Other Timeframes for Action Notices
- When the Contractor intends to restrict, reduce, suspend, or terminate a previously authorized service within an authorization period, whether as the result of a Service Authorization Determination or other Action, it must provide the Enrollee with a written notice at least ten (10) days prior to the effective date of the intended Action, except when:
- the period of advance notice is shortened to five (5) days in cases of confirmed Enrollee fraud; or
- the Contractor may mail notice not later than date of the Action for the following:
- the death of the Enrollee;
- a signed written statement from the Enrollee requesting service termination or giving information requiring termination or reduction of services (where the Enrollee understands that this must be the result of supplying the information);
- the Enrollee´s admission to an institution where the Enrollee is ineligible for further services;
- the Enrollee´s address is unknown, and mail directed to the Enrollee is returned stating that there is no forwarding address;
- the Enrollee has been accepted for Medicaid services by another jurisdiction; or
- the Enrollee´s physician prescribes a change in the level of medical care.
- For CBLTCS and ILTSS, when the Contractor intends to reduce, suspend or terminate a previously authorized service, or issue an authorization for a new period that is less in level or amount than previously authorized, it must provide the Enrollee with a written notice at least ten (10) days prior to the effective date of the intended Action, regardless of the expiration date of the original authorization period, except under the circumstances described in 1(a)–(b).
- For CBLTCS and ILTSS, when the Contractor intends to reduce, suspend, or terminate a previously authorized service, or issue an authorization for a new period that is less in level or amount than previously authorized, the Contractor will not set the effective date of the Action to fall on a non–business day, unless the Contractor provides "live" telephone coverage available on a twenty–four (24) hour, seven (7) day a week basis to accept and respond to Complaints, Complaint Appeals and Action Appeals
- The Contractor must mail written notice to the Enrollee on the date of the Action when the Action is a denial of payment, in whole or in part,
- When the Contractor does not reach a determination within the Service Authorization Determination timeframes described in this Appendix, it is considered an Adverse Determination, and the Contractor must send notice of Action to the Enrollee on the date the timeframes expire.
Contents of Action Notices
- The Contractor must utilize the model 4687 MLTC Action Taken – Denial, Reduction or Termination of Benefits (211) notice for all actions.
- The Contractor must utilize the model MLTC Initial Adverse Determination notice for all actions, except for actions based on an intent to restrict access to providers under the recipient restriction program.
- For actions based on an intent to restrict access to providers under the recipient restriction program, the action notice must contain the following as applicable:
- the date the restriction will begin;
- the effect and scope of the restriction;
- the reason for the restriction;
- the recipient´s right to a fair hearing;
- instructions for requesting a fair hearing including the right to receive aid continuing if the request is made before the effective date of the intended action, or 10 days after the notices was sent, whichever is later;
- the right of Contractor to designate a primary provider for recipient;
- the right of the recipient to select a primary provider within two weeks of the date of the notice of intent to restrict, if the Contractor affords the recipient a limited choice of primary providers;
- the right of the recipient to request a change of primary provider every three months, or at an earlier time for good cause;
- the right to a conference with Contractor to discuss the reason for and effect of the intended restriction;
- the right of the recipient to explain and present documentation, either at a conference or by submission, showing the medical necessity of any services cited as misused in the Recipient Information Packet;
- the name and telephone number of the person to contact to arrange a conference;
- the fact that a conference does not suspend the effective date listed on the notice of intent to restrict;
- the fact that the conference does not take the place of or abridge the recipient´s right to a fair hearing;
- the right of the recipient to examine his/her case record; and
- the right of the recipient to examine records maintained by the Contractor which can identify MA services paid for on behalf of the recipient. This information is generally referred to as "claim detail" or" recipient profile" information.
APPENDIX L
MANAGED LONG TERM CARE ENROLLEE RIGHTS
The following identifies, at a minimum, managed long–term care Enrollee rights, and the language that must be used when communicating these rights to Potential Enrollees, Applicants and Enrollees in written material.
- You have the Right to receive medically necessary care.
- You have the Right to timely access to care and services.
- You have the Right to privacy about your medical record and when you get treatment.
- You have the Right to get information on available treatment options and alternatives presented in a manner and language you understand.
- You have the Right to get information in a language you understand; you can get oral translation services free of charge.
- You have the Right to get information necessary to give informed consent before the start of treatment.
- You have the Right to be treated with respect and dignity.
- You have the Right to get a copy of your medical records and ask that the records be amended or corrected.
- You have the Right to take part in decisions about your health care, including the right to refuse treatment.
- You have the Right to be free from any form of restraint or seclusion used as a means of coercion, discipline, convenience or retaliation.
- You have the Right to get care without regard to sex, race, health status, color, age, national origin, sexual orientation, marital status or religion.
- You have the Right to be told where, when and how to get the services you need from your managed long–term care plan, including how you can get covered benefits from out–of–network providers if they are not available in the plan network.
- You have the Right to complain to the New York State Department of Health or your Local Department of Social Services; and, the Right to use the New York State Fair Hearing System and/or a New York State External Appeal, where appropriate.
- You have the Right to appoint someone to speak for you about your care and treatment.
You have the Right to seek assistance from the Participant Ombudsman program.
|top of section| |top of page|APPENDIX M
MANAGED LONG TERM CARE PLAN INFORMATION REQUIREMENTS
Information and Language Requirements Pursuant to 42 CFR 438.10 State and Plan Responsibilities
Written Materials
Reg – Establish a methodology for identifying the prevalent non–English languages spoken by enrollees and potential enrollees throughout the State. "Prevalent" means a non–English language spoken by a significant number or percentage of potential enrollees and enrollees in the State. The State must make available written information in each prevalent non–English language.
Reg – the State must require each MCO, PIHP, PAHP, and PCCM to make its written information available in the prevalent non–English languages in its particular service area.
- For Statewide materials, DOH has defined prevalent language of Potential Enrollees for written material as primary language of 5% or more of 65+ population (based on 65+ population in NYS from 2010 census) for Potential Enrollees. Those languages are English and Spanish.
This standard applies to the State MLTC Consumer Guide which will be translated into Spanish. It has been distributed through SOFA, the LDSS, plans and included on the Department Website.- All plans are required to translate all written materials into Spanish if 5% or more of the population in a county which it serves speaks Spanish as a primary language (according to 2010 U.S. Census data). If plan doesn´t meet census criteria for Spanish translation, but Spanish is defined as a prevalent language under other criteria, then plan will be required to translate all written materials into Spanish.
- Additionally, all plans are required to translate all written materials into prevalent languages.
- DOH defines a prevalent language as a language spoken by at least 5% of the plan´s enrolled population or 50 members, whichever is less. Census data are used as the basis for defining prevalent languages.
- DOH requires in the MLTCP/DOH contract that plans meet the necessary requirements.
- For foreign language translations of member handbooks, brochures, and pamphlets, the Contractor must submit a certification/attestation of translation from a professional translation service that attests the translator has used his/her best efforts to accurately translate the material into the specified languages. At a minimum, the translation service must perform a reverse translation (translate the foreign language version back into English and compare to original document). Translated materials must meet the readability standards described in Subsection 4 of Article V Section H of this Agreement.
- With respect to all other outreach/advertising materials, the Department will have the discretion to decide if the materials prepared by the Contractor in languages other than English require a certification of translation. If the Department determines a certification of translation is required, the Department will inform the Contractor to submit a certification of translation from a professional translation service or from the Contractor´s staff person that performed the translation.
- All such certifications of translation prepared by or for Contractor, must:
- be prepared on the Contractor´s letterhead;
- include a statement that the translator attests to the best of his/her knowledge that the Non–English version of the materials submitted convey the same information and level of detail as the corresponding English version; and
- include the name of the translator, the translator´s signature and the translator´s job title.
Oral Translation
Reg – State must make oral interpretation services available and require each MCO, PIHP, PAHP, and PCCM to make those services available free of charge to each potential enrollee and enrollee.
- Oral interpretation services (via ATT Language Line, staff capabilities, etc.) are available through every LDSS. In DOH all BCCI staff have access to telephone interpretation services.
- All plans currently have capability for oral translation services, through staff, telephone translation, electronic translation device, etc.
- DOH requires in the MLTCP/DOH contract that plans meet necessary requirements for oral translation services.
Notifying Potential and Actual Enrollees About Translation Services
Reg –The State must notify enrollees and potential enrollees, and require each MCO, PIHP, PAHP, and PCCM to notify its enrollees: (i) That oral interpretation is available for any language and written information is available in prevalent languages and (ii) How to access those services.
- There are statements about oral translation service availability and the right to free language assistance services in the State MLTC Consumer Guide and the plan member handbooks.
- DOH requires in the MLTCP/DOH contract that plans meet necessary requirements for notification of availability of oral translation services.
Alternative Formats
Reg – Written material must (i) Use easily understood language and format; and (ii) Be available in alternative formats and in an appropriate manner that takes into consideration the special needs of those who, for example, are visually limited or have limited reading proficiency.
- DOH makes materials available in an alternative format.
- Plans must select the alternative format(s) to be used (e.g., audiotapes, reading content of written materials to prospective applicants/Enrollees) and obtain DOH approval of the selection.
- Plans will ensure that their member services staff screen calls for those individuals who might need materials in alternative formats.
- Plan guidelines require written material in easily understood and readable formats.
Information for Potential Enrollees
|top of section| |top of page|Reg: (1)The State or its contracted representative must provide the information specified in paragraph (2) to each potential enrollee as follows: (i)At the time the potential enrollee first becomes eligible to enroll in a voluntary program, or is first required to enroll in a mandatory enrollment program.(ii)Within a timeframe that enables the potential enrollee to use the information in choosing among available MCOs, PIHP, PAHPs, or PCCMs. (2) The information for potential enrollees must include the following: Names, locations, telephone numbers of, and non–English language spoken by current contracted providers.
- DOH defines Potential Enrollee as an individual who makes inquiry of the plan.
- The State MLTC Consumer Guide includes a statement that indicates the reader should check with the plan in which s/he is interested to find out which languages are spoken by which providers.
- Plan provider directories are required to identify the languages spoken by providers.
- Plan handbooks also must include a statement (in Spanish and other prevalent languages as appropriate) that directs Potential Enrollees to call the plan to obtain the most current information about languages spoken by participating providers.
- The State MLTC Consumer Guide includes information on all plans in the State, their service areas and contact numbers.
- Plans are required to provide information on all plans in the State, their service areas and contact numbers. This will be accomplished by the plans´ distribution of the State MLTC Consumer Guide with their handbooks.
- DOH requires in the MLTCP/DOH contract that plans meet necessary requirements for notifying Potential Enrollees and Enrollees about the availability of non–English speaking providers.
APPENDIX N
FOR ILLUSTRATION PURPOSES ONLY
Managed Long Term Care Risk Corridor
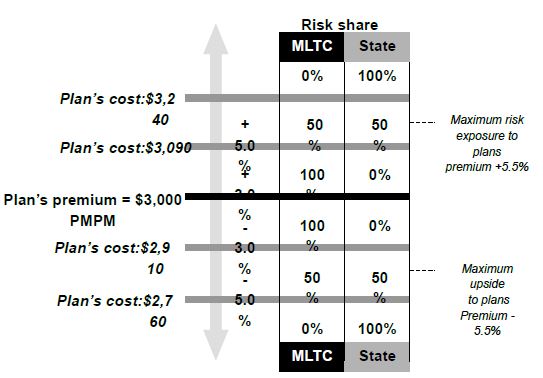
APPENDIX O
NURSING HOME TRANSITION
- In addition to the provisions found in this Appendix, Contractor must adhere to the Department´s "Transition of Nursing Home Benefits and Population into Managed Care policy," and any future amendments there to, which is hereby made part of this Appendix as if fully set forth herein.
- In accordance with the phased schedule outlined below, and in a time and manner described by the Department, all dual eligible persons 21–years–old and over seeking or referred for permanent nursing home placement must be enrolled into a Managed Long Term Care Plan. Contractor must implement this new enrollment policy in counties designated by the Department. The Department will designate counties in three phases.
- The Contractor must implement this new enrollment policy in the applicable service areas:
- Phase I
Immediately upon the enactment of this Appendix, unless otherwise indicated by the Department;
Within the Bronx, Kings, New York, Queens, Richmond, Nassau, Suffolk, and Westchester counties; - Phase II
At the time determined by the Department;
Within the counties designated for mandatory MLTC enrollment at the determined time;
In addition, permanent nursing home residents may voluntarily enroll in an MLTCP in Phase I and Phase II counties at this time; - Phase III
After Phase II, each time the Department announces implementation of mandatory MLTC enrollment for a county (or counties);
Within the county (or counties) contained in the Department´s announcement(s);
Permanent nursing home residents may voluntarily enroll in MLTC in counties contained in the Department´s announcement(s).
- Phase I
- The Contractor must implement this new enrollment policy in the applicable service areas:
- The Department reserves the right to change or amend, in its sole discretion and at any time upon reasonable notice, the manner, policies, and or timeframe(s) for the implementation of the Nursing Home Transition.
- Individuals not enrolled in an MLTCP who are in need of permanent Nursing Home care shall obtain a long–term care Medicaid eligibility determination from the LDSS or entity designated by the State prior to enrollment into an MLTCP.
- Dual eligible individuals who are 21–years–old or older and who have been determined eligible for Long Term Placement in a nursing home are allowed sixty (60) days to select an MLTCP for enrollment. Individuals who do not enroll in an MLTCP within the allotted time shall be auto–assigned to an MLTCP which contracts with the nursing home where the individual is currently placed.
- Contractor shall otherwise interact with potential applicants seeking or referred for nursing home placement in a manner determined by the Department. Such potential applicants shall also be directed to the Enrollment Broker for education and assistance regarding all MLTC Plan options available to them, including Community Based Long–Term Care alternatives.
- If an MLTCP does not have a nursing home to meet the needs of its members, the MLTCP must authorize out of network placement. If beds are not available at the time placement is indicated, the plan must authorize out of network placement.
- To the extent that any provisions in this Agreement are in conflict with the provisions of this Appendix, the provisions of this Appendix prevail.
APPENDIX P
CONFLICT FREE EVALUATION AND ENROLLMENT CENTER
- Where the Contractor operates in a county designated for mandatory enrollment into Managed Long Term Care (MLTC), all initial eligibility determinations for MLTC plans will be made by a Conflict–Free Evaluator, or other entity designated by the Department. All persons seeking information about the Contractor´s MLTC plan, or seeking enrollment into such product(s), should be forwarded to the Conflict–Free Evaluator in accordance with Departmental rules and guidance. If and when the Conflict–Free Evaluator determines persons to be eligible for MLTC, they will forward said person to the MLTC plan of his or her choice.
- In counties designated for mandatory enrollment into MLTC, the Conflict–free Evaluator will be implemented in a manner determined by the Department. Contractor will comply with the implementation of the Conflict–Free Evaluator based on guidance issued by the Department.
- Effective January 1, 2015, the Contractor must remove all contact information to the Contractor´s eligibility assessment staff, agents, subcontractors, and any entities that perform eligibility assessments on behalf of the Contractor, from all MLTC plan marketing materials and member handbooks.
- Upon submission to the Department for approval, the Contractor may seek a waiver of this provision from the Department. In doing so, the Contractor should provide the reason why the contact information should remain on the material in question. For example, the Contractor might utilize a single, general purpose phone number to handle all or most Enrollee or Potential Enrollee questions or concerns, in which case the Contractor should indicate what steps they have taken to capture and forward persons seeking enrollment/eligibility determinations to the Conflict–Free Evaluator. The Department reserves the sole right to determine whether to waive this provision.
- Effective January 1, 2015, the Contractor must provide the contact information for the Conflict–Free Evaluator, or other entity designated by the Department, on all MLTC plan materials that can reasonably be interpreted as intended to market to Potential Enrollees.
- To the extent that any provisions in this Agreement are in conflict with the provisions of this Appendix, the provisions of this Appendix prevail.
APPENDIX X
Modification Agreement Form
APPENDIX X
Agency Code ___________________________________
Period ________________________________________
Contract No __________________________________
Funding Amount for Period _______________________
This is an AGREEMENT between THE STATE OF NEW YORK, acting by and through _________________________ having its principal office at _________________________, (hereinafter referred to as the STATE), and ________________________ (hereinafter referred to as the CONTRACTOR), for modification of Contract Number _____________________ as amended in attached Appendix(ices).
All other provisions of said AGREEMENT shall remain in full force and effect.
IN WITNESS WHEREOF, the parties hereto have executed or approved this AGREEMENT as of the dates appearing under their signatures.
CONTRACTOR SIGNATURE
By: _________________________________________
_________________________________________
Printed Name
Title: _________________________________________
Date: _________________________________________
STATE AGENCY SIGNATURE
By: _________________________________________
_________________________________________
Printed Name
Title: _________________________________________
Date: _________________________________________
State Agency Certification:
In addition to the acceptance of this contract, I also certify that original copies of this signature page will be attached to all other exact copies of this contract.
STATE OF NEW YORK )
) SS.:
County of ____________ )
On the _________ day of ___________________ in the year ____________, before me, the undersigned, personally appeared __________________________________________________________, personally known to me or proved to me on the basis of satisfactory evidence to be the individual(s) whose names(s) is (are) subscribed to the within instrument and acknowledged to me that he/she/they executed the same in his/her/their/ capacity(ies), and that by his/her/their signature(s) on the instrument, the individual(s), or the person upon behalf of which the individual(s) acted, executed the instrument.
______________________________________
Notary
Approved:
ATTORNEY GENERAL
______________________________________
Title: ______________________________________
Date: _______________________________________
Approved:
Thomas P. DiNapoli
STATE COMPTROLLER
______________________________________
Title: ______________________________________
Date: _______________________________________