Attachment I - NY DSRIP Program Funding and Mechanics Protocol
- Attachment I is also available in Portable Document Format (PDF)
I. Preface
a. Delivery System Reform Incentive Payment Fund
On April 14, 2014, the Centers for Medicare and Medicaid Services (CMS) approved New York´s request for an amendment to the New York´s Partnership Plan section 1115(a) Medicaid demonstration extension (hereinafter "demonstration") authorizing the creation of a Delivery System Reform Incentive Payment (DSRIP) Fund. This demonstration is currently approved through December 31, 2014. DSRIP Funds will not be made available after December 31, 2014 unless the state´s demonstration renewal is approved by CMS.
Section IX of the Special Terms and Conditions (STC) describes the general rules and requirements of the Delivery System Reform Incentive Payment (DSRIP) Fund.
b. DSRIP Strategies Menu and Metrics and Program Funding and Mechanics Protocol
The DSRIP requirements specified in the STCs are supplemented by two attachments to the STCs. The Program Funding and Mechanics Protocol (this document, Attachment I) describes the State and CMS review process for DSRIP project plans, incentive payment methodologies, reporting requirements, and penalties for missed milestones. The DSRIP Strategies Menu and Metrics (Attachment J) details the specific delivery system improvement activities that are eligible for DSRIP funding.
This version of the DSRIP Program Funding and Mechanics Protocol is approved April 14, 2014. In accordance with STC 10.b in section IX, the state may submit modifications to this protocol for CMS review and approval in response to comments received during the post–award comment period and as necessary to implement needed changes to the program as approved by CMS.
II. DSRIP Performing Provider Systems
The entities that are responsible for performing a DSRIP project are called "Performing Provider Systems." Performing Provider Systems must meet all requirements described in the STCs, including the safety net definition described in STC 2 is section IX. This section provides more detail about the specific criteria that performing provider systems must meet in order to receive DSRIP funding and the process that the state will follow to assure that performing provider systems meet these standards.
The state will determine the types of providers eligible to participate as a Performing Provider System, as described in paragraph (a) below. All providers are required to form coalitions of providers that participate in DSRIP as a single Performing Provider System, as described in paragraph (b) below. Coalitions must specify their outpatient beneficiary population based on the attribution model described in paragraph (c) below.
a. Assessment of Safety Net Provider Status
The state will use data from DSH audits and other available information to make an assessment of which providers in the state could be eligible for DSRIP funding, consistent with STC 2 in section IX. This list of providers will be submitted to CMS and will be publicly available on the state´s website. Performing Provider Systems are expected to continue serving a high proportion of Medicaid and uninsured patients throughout the duration of the demonstration, and significant deviation from these standards will be cause to discontinue DSRIP funding for the Performing Provider System after the mid–point assessment.
b. Coalitions
Eligible major public general hospitals and other safety net providers are encouraged to form coalitions that apply collectively as a single Performing Provider System. The state will review each of the proposed Performing Provider Systems and may require additional connectivity to additional medical, behavioral health, long term care, developmental disabilities or social service providers as required to build a comprehensive regional performance network. Coalitions will be evaluated on performance on DSRIP milestones collectively as a single Performing Provider System. Coalitions are subject to the following conditions:
- Coalitions must designate a lead coalition provider who is primarily responsible for ensuring that the coalition meets all requirements of performing provider systems, including reporting to the state and CMS. In the process of formally approving each Performing Provider System, the state shall articulate a set of standards that each lead entity must follow including specific rules on project oversight, performance payment distribution and other required legal and operational obligations of the lead entity.
- Coalitions must establish a clear business relationship between the component providers, including a joint budget and funding distribution plan that specifies in advance the methodology for distributing funding to participating providers. The funding distribution plan must comply with all applicable laws and regulations, including, without limitation, the following federal fraud and abuse authorities: the anti–kickback statute (sections 1128B(b)(1) and (2) of the Act); the physician self– referral prohibition (section 1903(s) of the Act); the gainsharing civil monetary penalty (CMP) provisions (sections 1128A(b)(1) and (2) of the Act); and the beneficiary inducement CMP (section 1128A(a)(5) of the Act). CMS approval of a DSRIP plan does not alter the responsibility of Performing Provider Systems to comply with all federal fraud and abuse requirements of the Medicaid program.
- Coalitions must have a plan for reporting, decision–making, change management, and dispute resolution on performance and incentive payments.
- Each coalition must in the aggregate meet the minimum outpatient beneficiary requirements specified in paragraph (d) below.
- For coalitions that involve public hospitals that are providing Intergovernmental Transfer (IGT) funding for a project, the public entity providing IGT funding will generally be the lead coalition provider for the Performing Provider System that is directly using the IGT match. Private safety net providers can also service as coalition leads as provided in paragraph (d) below.
- Each coalition must have a data agreement in place to share and manage patient level data on system–wide performance consistent with all relevant HIPAA rules and regulations.
c. DSRIP Beneficiary Attribution Method
The goal of DSRIP is to have each Performing Provider System responsible for most or all Medicaid beneficiaries in the given geography or medical market area. It is expected that most of the Medicaid beneficiaries (including dually eligible members) in the state will be attributed to a Performing Provider System. The possible exceptions are beneficiaries that are primarily being served by providers not participating in any Performing Provider System in the region.
However, given the comprehensive nature of DSRIP, it is expected that each approved Performing Provider System will include all of the major providers of Medicaid services in their region, greatly reducing the number of beneficiaries not attributed to any Performing Provider System. A beneficiary will only be attributed to one Performing Provider System, based on the methodology described below.
Performing Provider Systems must include a proposed target population, including a specific geography for the overall performing provider effort. Each Performing Provider System will be approved for a specific geography, consisting of one or more counties, based on their application and the state´s review. This specific geography will be utilized to form a service area for the purpose of attribution. Utilizing the proposed geography, for each DSRIP Project Plan submitted by a given Performing Provider System, the department will identify the Medicaid and uninsured beneficiaries´ population (if applicable) that will be attributed to that system prospectively at the start of each measurement year. This prospective attribution denominator for DY 1 will be used in valuation for payment purposes without any adjustments applied, except at the midpoint evaluation as specified in section VI.d. The attributed members will be the collective focus for all projects.
Matching Goal – The aim of the attribution process is to help assign a DSRIP participants to the best Performing Provider System based on the recipient´s current utilization patterns, including assigned care management and primary care provider as well as the geographical appropriateness of that system. This means beneficiaries will be assigned to Performing Provider Systems, in their region, which include the providers most responsible for their care (as determined based on visits to primary service types –including PCP – as described below). The attribution logic will test for a plurality of visits within the Performing Provider System. Plurality, for DSRIP purposes, means a greater proportion of services as measured in qualifying visits within the Performing Provider System than from services outside the Performing Provider System.
Two Forms of Attribution:
DSRIP Attribution will come in two forms. The first form of attribution will be to initially assign a given cohort of patients to each Performing Provider System. This will be a 1 to 1 match between a Performing Provider System and each attributable Medicaid and uninsured member (uninsured members will be attached at the aggregate county level based on census data). This first form of attribution will be called Attribution for Initial Valuation. The second form of attribution will be for performance measurement purposes and will be done at the conclusion of each measurement year to create an appropriate group of members for DSRIP performance measurement purposes – this form of Attribution will be called Attribution for Performance Measurement.
Attribution for Initial Valuation:
This initial attribution is done for two basic purposes. The first purpose is to create a number of Medicaid and uninsured lives for use in the calculation of potential performance awards as part of the DSRIP valuation process. The second purpose is to create an initial group of Medicaid members only for initial performance benchmark development. Attribution for Initial Valuation will follow a logic flow based first on 1) the type of PPS and then 2) the population subcategory the given Medicaid member falls into.
PPS Type and Attribution:
Three PPS Types will be recognized for the purpose of attribution:
- Single PPS in a Region;
- Multi PPS in Region –Public Hospital Led/Involved; and
- Multi PPS – Non–Public Hospital Involved.
Single PPS in a Region – If a PPS is the only PPS approved by the state in a defined region then all the Medicaid members receiving services in that region will be attributed to that single PPS. As previously promised by the State, the single PPS in a region will also receive all the non– utilizing Medicaid members (i.e., members enrolled in Medicaid but not receiving any Medicaid paid services) residing in their approved region in their attribution. In addition, the single PPS will receive all the uninsured residing in their approved region if they agree to do the 11th DSRIP project targeted to the uninsured.
Multi PPS in Region – Public Hospital Led/Involved – If a PPS that includes a major public hospital in their network (as lead, co–lead, or network partner) is approved in a region where there is at least one other approved PPS, then the public led/involved PPS will receive all utilizing Medicaid members (with the exception of some low utilizing Medicaid members – see below) that get most of their services from the PPS network through the loyalty assignment methodology described below. This public led/involved PPS will also be given the first opportunity to develop an 11th project specifically designed to serve the uninsured in its region. If this public led/involved PPS opts to do that 11th project, they will then also have all the uninsured members residing in their approved region attributed to their PPS for initial valuation. This public led/involved PPS will also receive (for attribution for payment purposes and again only if they do the 11th project) a cohort of non–utilizing and low use Medicaid members in the region. Low use members are those that meet a state definition of lower use designed to target members with use patterns that appear to not be coordinated by PCP or care manager during the attribution period (e.g., ED visits with no evidence of PCP access, Inpatient visits with no primary care etc.). All of these low use members may however be included in the attribution denominators for measurement purposes (and baseline data) based on their current access patterns. This cohort of non–utilizing and low utilizing members will be utilized in attribution and valuation for all Public hospital Led/Involved PPSs and any non–public PPSs approved to do the 11th project as discussed below. This non–utilizing and low utilizing cohort will be determined at the conclusion of the DSRIP application review.
Multi PPS – Non–Public Involved – If the PPS is approved in a region that contains at least one other PPSs approved for all or part of their approved region (Multi PPS) and this region does not include a major public hospital as a major partner in their network, then this non–public involved PPS will receive attribution of utilizing Medicaid members that get most of their services from their PPS network in the loyalty assignment methodology described below. This Multi–PPS (non–public) type is only eligible to receive uninsured and a cohort of low/non–utilizing Medicaid members under one of two scenarios – 1) there is no public PPS in the region or 2) there is a public PPS in the region but the public PPS has opted not to do the 11th project. If scenario 1 or 2 materializes, the Non–Public PPS(s) would then have the option to elect to pursue the 11th project. If the non–public PPS(s) decides to pursue the 11th project, they will then be eligible to receive uninsured and a cohort of low/non–utilizing Medicaid members in their attribution. If a public led/involved PPS is approved in the region and that public PPS opts not to do the 11th project, then the non–Public involved PPS(s) in the region will be offered an opportunity to do so. If the non–public PPS(s) selects the 11th project, under such circumstances then they will be assigned the uninsured members residing in their approved PPS region in the attribution for initial valuation based on the percentage of Medicaid members assigned to the PPSs in the region (e.g., if a given Non–Public PPS has 60 percent of the region´s Medicaid population attributed then they will get 60 percent of the uninsured members). So, if no public led PPS exists in the region or the public declines to do the 11th project, the uninsured members will be divided between any Non–public PPS(s) (once the opt to do the 11th project) based on the percentage of Medicaid members assigned to the PPSs in the region. Also, the cohort of the low/non–utilizing Medicaid population will be attributed to the any Non–public PPS(s) using the same method as the uninsured are distributed; again they will be assigned this population only if they opt to do the 11th project.
Attribution for Payment Logic based on PPS Type:
| PPS Type | Medicaid Regular 1 Utilizers Attribution | Medicaid Non/Low Utilizers Attribution |
Uninsured Attribution |
|---|---|---|---|
| Single PPS in Region | All in the defined region | All in the defined region | All in the defined region if the PPS opts for the 11th project. |
| Multi PPS in Region – Public Led/Involved | Based on attribution loyalty logic | Cohort in the defined region if the PPS opts for the 11th project | All in defined region if PPS opts for 11th project |
| Multi PPS – Non–Public Involved | Based on attribution loyalty logic | None – unless no public PPS in the region or the public PPS opts not to do the 11th project. In addition, this PPS would need to do the 11th project and Non/Low attribution will then be based on PPS MA attribution percentage in region. | None – unless no public PPS in the region or the public PPS opts not to do the 11th project. In addition, this PPS would need to do the 11th project and uninsured attribution will then be based on PPS MA attribution percentage in region. |
Attribution Logic – Loyalty Based Attribution for Regions with Multiple PPS
Utilizing Medicaid Members will be attributed first based on what population subcategory they belong to and second based on the attribution loyalty logic that has been specifically designed for that given subpopulation by the state.
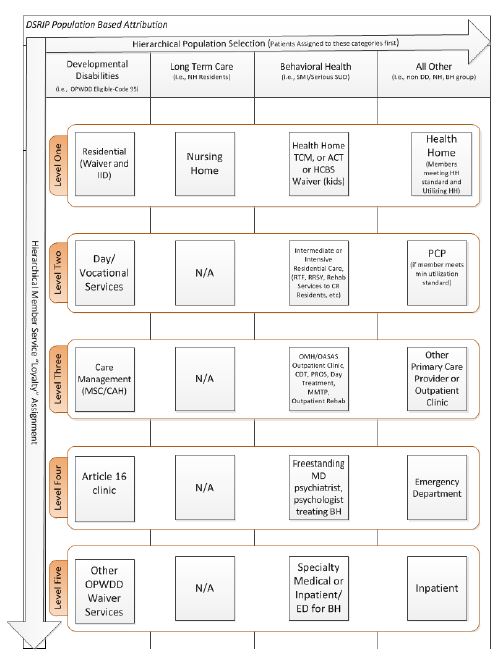
Four mutually exclusive population subcategory groupings have been set up for DSRIP purposes:
- Developmental Disabilities (OPWDD Service Eligible – Code 95)
- Long Term Care (Only NH residents)
- Behavioral Health (SMI/Serious SUD)
- All Other
Medicaid members will be placed into one of these population subcategories based on a mutually exclusive hierarchy in the order presented above. In other words, the logic will first look for evidence of Developmental Disabilities and if none exists then evidence of Long Term Care and if none exists then Behavioral Health and if none exists then the member will be assigned to All Other. So, for example, if the member meets criteria for developmental disabilities and long term care they will be assigned to development disabilities as that is first in the hierarchy.
Similarly, if a member does not meet criteria for developmental disabilities but does meet criteria for both long term care and behavioral health they will be assigned to long term care.
After a member is assigned to a population subcategory they will then been assigned to a PPS based on a loyalty algorithm that is specific to their population subcategory. For instance, if they have been assigned to the behavioral health subcategory the algorithm will check first for care management/health home connectivity and if none exists go on to look for residential connectivity and then ambulatory and so on in hierarchical order.
The following graphic helps to illustrate the overall process.
It should be noted that the majority of members will be attributed from within the "All other" category above. It is estimated that over 80 percent of Medicaid members will be attributed from within that category. Further, while some members in the All Other category with multiple chronic illness will be attributed based on their health home care management agency, clearly most of the All Other members are going to be attributed to a DSRIP network based on their health plan assigned PCP as most patients are in health plans and many of those members are utilizing their assigned PCP. If a non–health home member in the "All Other" is not utilizing the assigned PCP they will then be attributed based upon the primary care provider or clinic that they see most often for ambulatory care. If no ambulatory care exists they will then be attributed based upon emergency department and then inpatient use if necessary. Irrespective of the final attribution, each PPS will be required to make ongoing efforts to work with health plans and providers to align care management, PCP and specialty services for all attributed members in such a way to fully leverage existing positive clinical relationships.
The results of the preliminary attribution process above will be shared with the Medicaid Managed Care organizations for their enrolled members. The MCOs will review the state´s attribution logic/results and suggest any needed changes based on more current member utilization information including more recent PCP assignment or specialty service access. In advance of this attribution process the state will share the DSRIP Performing Provider System network with the plan to identify any network alignment gaps that may exist so that the DSRIP Performing Provider System and the MCOs can work together to align service delivery and plan contracted networks as appropriate.
PPS Networks and Attribution – Once the Performing Provider System network of service providers is finalized the each Performing Provider System service network will be loaded into the attribution system for recipient loyalty to be assigned based on visit counts to the overall Performing Provider System network in each of the above hierarchical population subcategories. Once the initial attribution is calculated for the purposes of setting DSRIP project values, the performing provider system network may only be changed with a DSRIP plan modification (as described in section X.a below). For each of these population subcategories, the algorithm will check the services provided by each provider and accumulate these visits to the Performing Provider System the given provider is partnered with. If a recipient is currently outside the Performing Provider System geographic area, the visits are excluded (e.g. recipient traveling from upstate to NYC for special surgery). Each Performing Provider System associated with the matched provider accumulates the total number of visits for each service/provider combination. Adjustments to attribution based on known variables (e.g. recent changes to the recipient´s address) may be made by the state with MCO input if deemed necessary by data. After all visits against all providers are tallied up for a given service type, the methodology finds the Performing Provider System with the highest number of visits for the recipient in each service loyalty level as appropriate. If a single provider is in more than one PPS network (e.g. PCP) then the tie breaking method below may be employed for final matching purposes. This overall process will be designed to ensure that the Performing Provider System that is the best fit for the recipient is chosen.
Finalizing Match and Ties – If more than one Performing Provider System has the highest number of visits based on the highest priority service loyalty types noted, the methodology re– runs the above logic across all Medicaid service types. This process could break a tie if additional visits in other service types cause one Performing Provider System to accumulate more visits. So for instance, Nursing Home residents that are in nursing homes with connectivity to multiple PPSs may be placed based on their utilization of hospital or other services. If, however, this still results in a tie, the methodology will place the recipient in a separate bucket to be assigned at the end of the process. Recipients who have no predominant demonstrated provider utilization pattern will be assigned to a PPS based on a special logic. If the member is not matched from within the Developmental Disabilities, Long Term Care or Behavioral Health population subcategories the Performing Provider System in their geographic region will be chosen by first looking to see if the beneficiary has any primary care provider (PCP) assigned by a Medicaid health plan; if the beneficiary has an assigned PCP the beneficiary will be matched to the Performing Provider System that has that PCP in their network (a method will be developed to address PCPs that are in more than one Performing Provider System). For all population subcategories, if the beneficiary cannot be matched by PCP, then the beneficiary will be assigned to the Performing Provider System with the most beneficiaries already assigned (by the visit attribution method) in their specific zip code or other relevant geographic area. Except for beneficiaries who are explicitly excluded because they receive the majority of their services (more than 50%) at providers that are not participating in DSRIP, all beneficiaries will be attributed.
Attribution for Performance Measurement Purposes
Although the patient populations targeted for Performing Provider System measurement are determined as of January 1 (or other date specified) of the measurement year for valuation purposes, patient attribution for Performing Provider System quality measurement for domain 2 and 3 metrics will be defined as of the measurement period. This is consistent with the CMS Medicare Shared Savings Program (MSSP), where there is an initial, prospective attribution at the start of the measurement year to determine the populations to be included and a final attribution at the end of the year for evaluation and measurement. Each patient will be assigned to only one PPS for measurement purposes. The patient population attributed for valuation will form the basis for quality measurement for all population–based measures (see Metric Specification guide) with the appropriate criteria applied for each measure. For episodic–based measures (see Metric Specification guide), the initial population attributed to each PPS will be limited to only those members seen for that episode of care within the PPS network during the measurement period. Episode of care refers here to all care provided over a period of time (as defined in the measurement specifications) for a specific condition (e.g. Diabetes – all diabetes care received in a defined time period for those members; HIV– all HIV care received in a defined time period for those members). Since PPS networks are non–binding and members can choose to receive care outside of network, it is necessary to protect patient confidentiality for certain highly sensitive medical conditions, as well as, ensure medical records are available to the PPS network for all hybrid measures. For institutional–based measures (see Metric Specification guide) the population for quality measurement will represent the population within that facility.
d. Minimum Outpatient Service Level
Performing Provider Systems must have a minimum of 5,000 attributed Medicaid beneficiaries a year in outpatient settings.
e. Performing Provider System Relation to IGT Entities
Intergovernmental transfer (IGT) entities are entities that are eligible to contribute allowable governmental funds or other non–federal funds for use by the state for the non–federal share of DSRIP payments for a Performing Provider System. They include government–owned Hospitals and other government entities such as counties.
The non–federal share of DSRIP payments to providers will be funded through the use of intergovernmental transfers (IGTs) from government owned or operated major public hospitals or their sponsoring government entity or other affiliated governmental entity, consistent with applicable federal law and regulations. Such IGTs will not be represented on any financial statement by the public hospital as a cost of patient care, overhead, tax, or administrative cost; instead it shall be reflected as a transfer to the state government. For purposes of this section, the major public hospital or their affiliated government or governmental entity are deemed to be one and the same.
No portion of a DSRIP payment paid to a Private Performing Provider system may be redirected to the public entity that is supplying IGTs to finance the non–federal share of such payments.
Also, no private provider that is included in a coalition of providers that includes public providers can transfer DSRIP funds to those public providers. Nothing herein precludes or restricts such private provider from making payments to a public provider for services performed or provided by the public provider including DSRIP related services.
The state encourages public and private providers to collaborate where appropriate and will work with Performing Provider Systems to clarify the flow of IGT funding to avoid impermissible provider donations.
III. Projects, Metrics, and Metric Targets
a. Projects
Performing provider systems will design and implement at least five and no more than 10 DSRIP projects, selected from the Strategies Menu and Metrics (Attachment J). Each project will be based on a particular strategy from Attachment J and will be developed to be responsive to community needs and the goal of system transformation, as defined by the objectives in STC 6 in section IX.
All the DSRIP projects for a Performing Provider System will be part of the Performing Provider System´s overall DSRIP Project Plan.
There are projects described in Attachment J that are grouped into different strategies, such as behavioral health, within each Domain (System Transformation Projects (Domain 2), Clinical Improvement Projects (Domain 3), and Population–wide Projects (Domain 4). For each strategy, there is a set of metrics that the performing provider system will be responsible for if they do any one of the projects within that strategy.
As described in Attachment J, Performing Provider Systems will select at least two system transformation projects (including one project to create integrated delivery systems as well as another project from either the care coordination or connecting settings strategies list), two clinical improvement projects (including a behavioral health project), and one population–wide project. The selection of all projects must be based on the community needs assessment of the baseline data and as the target population selected by the performing provider system.
Performing Provider Systems may choose additional projects as appropriate.
b. Metrics
In order to measure progress towards achieving each objective, each project must include metrics in all four of the following domains. Performing Provider Systems will report on these metrics in their semi–annual reports (described in VI.a below) and will receive DSRIP payment for achievement of these milestones (based on the mechanism described in VII.a below).
- Overall project progress metrics (Domain 1)
- System transformation metrics (Domain 2)
- Clinical improvement metrics (Domain 3)
- Population–wide metrics (Domain 4)
Performing Provider Systems that exceed their metrics and achieve high–performance by exceeding a preset higher benchmark for reducing avoidable hospitalizations or for meeting certain higher performance targets for their assigned behavioral health population will be eligible for additional DSRIP funds from the high performance fund, described in paragraph VIII.b. below.
The Strategies Menu and Metrics (Attachment J) describes the specific metrics that will be used to assess performance under each domain and specifies which metrics are pay–for–reporting and which are pay–for–performance. Additional measure specifications, including the process for addressing small n issues is described in the Metric Specification Guide supplement to Attachment J.
As described in STC 12.e. in section IX, the state or CMS may add domain 1 metrics to a project prospectively in order to address implementation concerns with at risk projects.
c. Metric Targets
All performing provider systems must have a target for all pay–for–performance metrics, which will be used to determine whether or not the performance target for the metric was achieved.
Performance targets should be based on the higher of top decile of performance for state or national data, or an alternative method approved by CMS. NY DSRIP goals for metrics may be based on NYS Medicaid results (preferred source) or national data where possible and on DSRIP DY1 results for metrics where state or national data are unavailable.
Annual improvement targets for Performing Provider System metrics will be established using the methodology of reducing the gap to the goal by 10%. The Performing Provider System baseline data will be established as soon as complete data is available for the baseline period (as specified in the Metric Specification Guide supplement to Attachment J) and will be used as the foundation to determine the gap to goal to set the improvement target.
For example, if the baseline data for a measure is 52 percent and the goal is 90 percent, the gap to the goal is 38. The target for the project´s first year of performance would be 3.8 percent increase in the result (target 55.8 percent). Each subsequent year would continue to be set with a target using the most recent year´s data. For example, should a PPS meet or exceed the first year´s target of 55.8 percent, the next annual target would be 10 percent of the new gap to the goal. This will account for smaller gains in subsequent years as performance improves toward the goal or measurement ceiling.
The PPS will know the annual performance target to be achieved at the beginning of the current DY and the method for determining the annual performance target will remain the same throughout the DSRIP years.
In general, Performing Provider System that achieve their target for the DY will be considered to have reached the annual milestone for the metric, and Performing Provider System that achieve 20 percent gap to goal or the 90th percentile of the statewide performance for the high–performance metrics listed in Attachment J may be eligible for additional payment for high–performance. If more frequent reporting (more than annual) of metric results are required for projects, the reported results for payment should be based on a standard twelve–month period.
IV. DSRIP Project Plan Requirements
a. Project Plan Development Process
The proposed project plans should be developed in collaboration with community stakeholders and responsive to community needs. Performing Provider Systems have the option to seek DSRIP design grants described in STC 10 in section IX.
According to a timeline developed by the state and CMS that aligns with the DSRIP deliverables schedule outlined in STC 40 in section IX, Performing Provider Systems must submit a final DSRIP Project Plan to the state for review with a complete budget and all other items described below, consistent with the requirements in STC 8 in section IX.
It is expected that the transformational nature of the activities to be undertaken in these projects will require a strict adherence to disciplined project management. The DSRIP Project Plan must provide evidence that the Performing Provider Systems has a clear understanding of the needs of the service area (based on objective data specific to the service area as well as community input), that the project will address these needs in a significant manner, that the Performing Provider System understands the metrics that will need to be monitored and the methodology that will be used to do such, and that the Performing Provider System has internal and/or external resources that will be available for project management and the required rapid cycle improvements inherently needed in these projects.
b. Organization of DSRIP Project Plan
DSRIP Project Plans must be submitted in a structured format agreed upon by the state and CMS. At a minimum, the plan shall include the following sections:
- DSRIP Face Sheet
This face sheet will list the documents included within the package and include the applicant´s name and a brief (no more than 1000 word) executive summary of the submitted project. - Provider Demographics including:
- Name, Address, Senior level person responsible for the DSRIP project and to whom all correspondence should be addressed
- The name of providers and their identification numbers participating in the project plan, including the lead provider in the case of a coalition.
- Definition of service area (according to the specifications in the DSRIP Strategies Menu and Metrics) and a discussion of how the providers in the coalition relate to (or inform) the service area definition. As further described in the DSRIP Strategies Menu and Metrics, Performing Provider Systems are accountable for improving the quality of care for all Medicaid and low–income uninsured beneficiaries in their service area as defined in the DSRIP Member Attribution Method above.
- Identification as a safety net provider with documentation supporting that identification as described in paragraph II.a above.
- Current patient population including demographic information, payer mix to document qualification as described in paragraph II.c above.
- Identification of Provider Overarching Goals: The Performing provider system will need to identify its goals for the project, as well as how the project contributes to achieving the overall goals (defined in STC 1 in section IX) to create and sustain an integrated, high performing health care delivery system that can effectively and efficiently meet the needs of Medicaid beneficiaries in their local communities by improving care, improving health and reducing costs. More specifically, the Performing provider system should demonstrate how the project will engage in system transformation (including linking across settings, ensuring appropriate capacity, and taking responsibility for a population), as demonstrated by achievement of avoidable events [including addressing behavioral health]. The Performing provider system will need to demonstrate that it has a governance strategy that ensures that participating providers work together as a "system" and not as a series of loosely aligned providers nominally committed to the same goal. Plans to progressively move from a loosely organized network of affiliated entities to an actual Integrated Delivery System must be evident in the goals.
The Performing provider system will need to provide objective data–driven evidence that this is a relevant goal for the Performing provider system and its service area. The performing provider system must demonstrate that all relevant Domain 3 metrics for the projects selected align with community needs and that these areas have room for improvement. With the exception of behavioral health Domain 3 measures, for which the following will not apply, if the Performing provider system´s performance on the most recent available data (as specified in the Metric Specification Guide supplement to Attachment J) for the majority of any chosen Domain 3 metric set is within 10 percentage points or 1.5 standard deviations to the high–performance goal described in section III.c above (whichever is greater), the project would not be approved. - Identification of Provider Project to meet identified goals, including brief rationale for project choice and summary (including citations) of existing evidence showing that project can lead to improvement on goals of project. Logic models such as driver diagrams may be helpful to demonstrate how the elements of the project all contribute to the central goals. Further information will be provided in the detailed assessment provided in (5) and must include all relevant domains outlined in the Strategies Menu and Metrics.
- Performance Assessment
- Current community health needs (population demographics, types and numbers of providers and services, cost profile, designation as Health Professional Shortage Area, mortality and morbidity statistics, and health disparities): Population demographics should include those who are institutionalized as well as those involved in the criminal justice systems. The assessment will include a discussion of a designated list of public health concerns determined by the state, including behavioral health. The selection of these concerns should be supported by baseline data on current performance on targeted health indicators and quality metrics. A review of the social determinates of health and assessment of disabilities consistent with Olmstead should also be included in such community assessment. Needs assessment should include a review of non–English languages spoken in the Performing Provider System catchment area to guide development of multi– language outreach and education material.
- Evidence of regional planning including names of partners involved in the proposed project (in addition to any coalition members in the Performing Provider System in accordance with the process described in paragraph II.b above) Detailed analysis of issues causing poor performance in the project area. These must include assessment of patient co–morbidities, patient characteristics, social system support, system capacity for primary care and disease management, and institutional issues such as finances, confounders to health care system improvement including fragmentation of services, competition, and assessment of regional planning issues.
- Comprehensive workforce strategy – this strategy will identify all workforce implications – including employment levels, wages and benefits, and distribution of skills – and present a plan for how workers will be trained and deployed to meet patient needs in the new delivery system based on the performance assessment of community health needs, and how the strengths of current workforce will be leveraged to the maximum degree possible under current state law and regulations.
- Review of Financial stability – A complete review of the financial condition of all financially challenged safety net and public providers in the performing provider system.
- Evidence of public input into the project including consumer engagement. This should include documentation of collaboration with local departments of public health, public stakeholders and consumers. In addition, the provider will need to document how there will be ongoing engagement with the community stakeholders, including active participation in any regional health planning activities currently underway in their community. Applicants will need to include workers and their representatives in the planning and implementation of their overall project with particular emphasis on the comprehensive workforce strategy. The Performing Provider System must specifically include evidence of consumer engagement in their needs assessment and planning process. The state may require Performing Provider Systems to maintain a website including contact information, overview of public comment opportunities, results of public processes, application materials, and required reporting.
- Work Plan Development: In this section the provider will provide an initial high–level work plan in a state–approved format using the domains of milestones identified in the DSRIP Strategies Menu and Metrics.
- Project progress milestones (Domain 1)
- System transformation and financial stability milestones (Domain 2)
- Clinical improvement milestones (Domain 3)
- Population–wide Milestones (Domain 4)
- Rapid cycle evaluation: The plan must include an approach to rapid cycle evaluation that informs the system of progress in a timely fashion, and how that information will be consumed by the system to drive transformation and who will be accountable for results, including the organizational structure and process to oversee and manage this process. The plan must also indicate how it will tie into the state´s requirement to report to CMS on a rapid cycle basis.
- Establishment of Milestones and Metrics: A section of the work plan must provide documentation of the monitoring strategy for the project including significant milestones and associated metrics, as specified in the DSRIP Strategies Menu and Metrics.
- Budget: Performing Provider Systems must provide a detailed budget for all 5 years of their DSRIP project. For Performing Provider Systems that were awarded HEAL grants, a detailed budget report along with a description of the similarities or differences must be included.
- Governance: The plan must include a detailed description of how the system will be governed and how it will evolve into a highly effective Integrated Delivery System. A clear corporate structure will be necessary and all providers that participate in the project will need to commit to the project for the life of the waiver. Weak governance plans that do not demonstrate a strong commitment to the success of the project will be rejected. Strong centralized project control will be encouraged especially for projects that require the greatest degree of transformation. The governance model should review the Performing Provider System´s need to pursue any state certificate of public advantage (COPA) and Accountable Care Organization (ACO) opportunities. Coalitions must define the members of the coalition and submit all supporting information about coalition governance including the business relationship, as described in Section II.b. The governance plan must address how the performing provider system proposes to address the management of lower performing members within the Performing Provider System network. This plan must include progressive sanctions prior to any action to remove a member from the performing provider system. The governance plan must also include a process by which the Performing Provider System will progressively advance from a group of affiliated providers to a high performing Integrated Delivery System. The state may provide governance template information for Performing Provider Systems to utilize in the development of their governance models and plans.
- Data sharing and confidentiality: Metrics will be collected in a uniform and valid fashion across all members of a Performing Provider System. The plan must include provisions for appropriate data sharing arrangements that permit this and appropriately address all privacy protections contained in federal law including HIPAA and New York Law.
- Expectation of Sustainability: Performing Provider Systems are asked to explain how the outcomes of this project will be sustained at the end of DSRIP and how gains can be continued after the conclusion of the project period. This should include a financial forecast of expected savings related to the implementation.
- Legal Compliance – Performing Provider Systems must comply with all relevant laws and regulations including compliance with Civil Rights Law and specifically all laws governing non–discrimination.
- Signed Attestations:
The Performing Provider System will submit a description of any initiatives that the provider is participating in that are funded by the U.S. Department of Health and Human Services and any other relevant delivery system reform initiative currently in place. The Performing Provider System will, by signature, attest that the submitted DSRIP project is not a duplication of a project from these other funded projects and does not duplicate the deliverables required by the former project (s). It should be noted if this project is built on one of these other projects or represents an enhancement of such a project that may be permissible, but it must be clearly identified as such in the DSRIP project plan.
The provider will submit an attestation statement documenting that the information provided in this document is accurate at the time of submission and that the provider, if accepted into the DSRIP, will cooperate fully with the state in the implementation and monitoring of this project and participate in the required learning collaboratives related to this project.
If the Performing Provider System is receiving funds from the Public DSRIP pool it will also provide a description of the IGT source identified for the project and attest that this IGT derives from local, public funds.
V. Project Valuation
The DSRIP project and application valuations will be calculated by the state (with assistance from the independent assessor) according to the methodology described below.
A maximum valuation for each DSRIP application is calculated based on the formula described in Section A below. Once the overall application value is determined, the value for the individual metrics of the DSRIP project plan is determined based on the distribution method described in Section B below. Project values are subject to monitoring by the state and CMS, as described in Section C below, and Performing Provider Systems may receive less than valuation described in their DSRIP plan if they do not meet metrics and/or if DSRIP funding is reduced because of the statewide penalty (described in Section IX.d below)
As a reminder, Performing Provider Systems are to submit a Project Plan with a minimum of 5 projects and (in most cases) a maximum of 10 projects for scoring purposes. In certain instance, a performing Provider System may be eligible to pursue a project plan containing 11 projects.
Please see below for project selection requirements per domain.
- Domain 2 Projects – Applicants must select at least two projects from this domain (one of which must be from sub–list A and one of which must be from sub–list B or C) but can submit up to 4 projects from Domain 2 for scoring purposes
- For eligible Performing Provider Systems pursuing 11 projects in their plan, they are allowed to select up to 5 projects from Domain 2 for scoring purposes. Domain 2 project selection must follow the same requirements listed above, but in these instances, there will also be the option for these systems to add project 2.d.i.
- Domain 3– Applicants must select at least two projects from this domain (one of which must be A. Behavioral Health), but can submit up to 4 projects from Domain 3 for scoring purposes
- Domain 4 – Applicants must select at least one project from this domain, but can submit up to 2 projects from Domain 4 for scoring purposes.
a. Valuation for DSRIP Application
The maximum DSRIP project and application valuation will follow a five–step process.
- The first step assigns each project in the Strategy Menu (Attachment J) a project index score which is a ratio out of a total of 60 possible points of each project (X/60 = project index score).
- The second step creates a project PMPM by multiplying the project index score by the state´s valuation benchmark. The valuation benchmark is pre–set by the state and varies based upon the number of projects proposed by an applicant.
- The third step determines the plan application score for the performing provider´s application based on a total of 100 points possible for each application (X/100 = Application Score)
- In the fourth step, the maximum project value is calculated by multiplying the project PMPM, the plan application score, the number of beneficiaries attributed to the project, and the duration of the DSRIP project (see example below).
- Once the maximum project values have been determined, the maximum application value for a Performing Provider System is calculated by adding together each of the maximum project values for a given Performing Provider System´s application.
The maximum application value represents the highest possible financial allocation a Performing Provider System can receive for their Project Plan over the duration of their participation in the DSRIP program. Performing Provider Systems may receive less than their maximum allocation if they do not meet metrics and/ or if DSRIP funding is reduced because of the statewide penalty (described in Section IX below).).
Step 1: Calculating Project Index Score
The value of a single project is expressed as an index score (see below). Project index scores are based upon a grading rubric that evaluated the project´s ability to transform the health care system. The State has assigned an index score to each project based on the grading rubric and the given project´s relative value to the other projects in the state´s menu. For application planning, index scores for each project are available to providers in the DSRIP Project Toolkit. These values have been made available to applicants in advance for their application submission.
The formula for the index score for each project on the menu consists of the following elements:
- Potential for achieving DSRIP goal of system transformation, including the three objectives, as described in STC 6 in section IX (Score 1 (lowest) – 30 (highest))
- Potential for achieving DSRIP goal of reducing preventable events, as described in STC 1a in section IX (Score 1– 10)
- Scope of project and capacity of project to directly affect Medicaid and uninsured population (1–10)
- Potential Cost Savings to the Medicaid Program (1–5)
- Robustness of evidence base (1–5)
Adding up the scores for each element for a given project will give each project an index score of X/60. The project index score (out of the 60 possible points) will be expressed in decimal form for calculation purposes.
Step 2: Calculating Project PMPM
Each project will be assigned a valuation benchmark based on the number of projects proposed in the application as described in Table 1 below.
By no later than 15 days after the public comment period for initial DSRIP applications, the state will establish a state–wide valuation benchmark based on its assessment of the cost of similar delivery reforms. This value will be expressed in a per member per month (PMPM) format and may not exceed $15 PMPM, as described in STC 9 in section IX.
For the purposes of the example described later in this section, an initial $8 PMPM valuation benchmark is used in Table 1 below. However, because projects serving more beneficiaries will have synergistic properties and economies of scale that will lower a project´s per member per month cost, the final valuation benchmark will be set based on the overall scope of applications received. Table 1 (below) will be updated to reflect the final valuation benchmark developed by the state in accordance with CMS´s guidelines.
Because additional projects will have synergistic properties, from leveraging shared infrastructure and resources, the valuation benchmark is discounted as follows for Performing Provider Systems selecting multiple projects. Although the project PMPM levels drop with the inclusion of additional projects, the overall Performing Project System valuation will generally increase (depending on the value of the actual projects selected) as more projects are added to the overall PPS effort. If the valuation benchmark is adjusted based on the process described above, the relative discount factor for additional projects beyond will remain the same.
Table 1. Valuation benchmark table (PMPMs may be revised according to the schedule described above, subject to the standards described in STC 9 in section Ix)
| Number of projects | Valuation Benchmark |
|---|---|
| 5 (minimum) | $8.00 |
| 6 | $7.20 |
| 7 | $6.80 |
| 8 | $6.65 |
| 9 | $6.50 |
| 10 | $6.50 |
| 11 (only for eligible PPS) | $6.50 |
The valuation benchmark is then multiplied by the project index score to create a project PMPM for each project.
Step 3: Plan Application Score
Based on their submitted application, each project plan will receive a score based on the fidelity to the project description, and likelihood of achieving improvement by using that project. This plan application score will be used as a variable in calculating the maximum project value.
Each plan application score will be expressed as a score out of 100, which will drive the percent of the maximum project valuation for each project that will be allocated to that individual project plan. The plan application score (out of the 100) will be expressed in decimal form when calculating the maximum application valuation. The state will develop a rubric for the individual plan application score in collaboration with CMS. This rubric must include an assessment of whether each proposed project is sufficiently different from other DSRIP projects selected (and other existing projects being funded by other sources) so as to ensure that the Performing Provider System does not receive double–credit for performing similar activities.
Performing Provider Systems eligible for and approved to deliver project 2.d.i ("the 11th project") will be awarded an application bonus to reflect the extra effort needed to address the project´s target population. The total Project Plan application score, including the 11th Project Application bonus points, can´t exceed 100 points (i.e.: If an application score, before the addition of the bonus points, is a 95– then the maximum bonus added to that PPS application would be 5 point for a total score of 100). Applications will also be scored based on an applicant´s commitment to developing a capability to responsibly receive risk–based payments from managed care plans through the DSRIP project period.
Step 4: Calculating Maximum Project Value
The number of beneficiaries attributed to the project (based on the attribution method described in Section III above) and the anticipated duration (expressed in months) of the applicant´s participation in DSRIP program will also be used to calculate the maximum value for each project as follows.
Maximum Project Value = [Project PMPM] × [# of Beneficiaries] × [Plan Application Score] × [DSRIP Project Duration]
Step 5: Calculating Maximum Application Value
Once the Maximum Project Value for each of the projects in the Performing Provider System application is calculated, the maximum project values for each of the project are then added together to provide the Maximum Application Value for the DSRIP application.
Example: Putting it all together – Below is a simple example of the DSRIP valuation calculation:
For illustration purposes, a Performing Provider System submits six projects in their application. Two projects are from Domain Two; Creating an Integrated Delivery System, and Expand Access to Primary Care, and three projects from Domain Three; Integration of Behavioral Health in Primary care, Development of Evidence Based Medicine Adherence programs, and HIV Services Transformation and one project from Domain Four; Evidence Based Strategies to Prevent Substance Abuse and Other Mental/Behavioral Disorders. Scoring steps are included below but all numbers are for illustration purposes only and do not reflect on the actual values that the example projects will receive.
Step 1: Calculating Project Index Scores (for illustration purposes) Project Index Scores
- Project 1: Creating an Integrated Delivery System 56/60=.93
- Project 2: Create a Medical Village (Hospital) 54/60=.9
- Project 3: Integration of Behavioral Health in Primary care 39/60=.65
- Project 4: Evidence Based Medicine Adherence 29/60=.48
- Project 5: HIV Services Transformation 28/60=.47
- Project 6: Strategies to Prevent SUD and BH Disorders 20/60=.33
Step 2: Calculating Project PMPM (numbers below are for illustration only):
Since there are six projects in this example application, the valuation benchmark is $7.20 (for a six–project application – from the table in step 2 above). Each of the Project Index Scores (from Step 1) are then multiplied by Valuation Benchmark to compute the individual Project PMPMs.
[Project Index Score] × [Valuation Benchmark] = Project PMPM (see table below)
| Project Index Score | Valuation Benchmark | Project PMPM | |
|---|---|---|---|
| Project 1 | 0.93 | $7.20 | $6.70 |
| Project 2 | 0.9 | $7.20 | $6.48 |
| Project 3 | 0.65 | $7.20 | $4.68 |
| Project 4 | 0.48 | $7.20 | $3.46 |
| Project 5 | 0.47 | $7.20 | $3.38 |
| Project 6 | 0.33 | $7.20 | $2.38 |
Step 3: Calculating Plan Application Score
Performing Provider System submits a six project Performing Provider System application and receives a plan application score of 85/100. As part of the 15 point reduction from a perfect score, the Performing Provider System received a reduction because the Performing Provider System selected two projects that share the same metric set.
Step 4 and 5: Calculating Maximum Project Value and Maximum Application Valuation
The attribution assessment completed by the provider in their application (and subsequently verified by the State´s attribution method and independent assessors) shows 100,000 beneficiaries are expected to be served by the applicant´s DSRIP project.
As a result, the maximum application value is calculated as $138,108,000, as illustrated below.
| Project PMPM | # of Beneficiaries | Project Plan Application Score | # of DSRIP Months | Maximum Project Value | |
|---|---|---|---|---|---|
| Project 1 | $6.70 | 100,000 | 0.85 | 60 | $34,170,000 |
| Project 2 | $6.48 | 100,000 | 0.85 | 60 | $33,048,000 |
| Project 3 | $4.68 | 100,000 | 0.85 | 60 | $23,868,000 |
| Project 4 | $3.46 | 100,000 | 0.85 | 60 | $17,646,000 |
| Project 5 | $3.38 | 100,000 | 0.85 | 60 | $17,238,000 |
| Project 6 | $2.38 | 100,000 | 0.85 | 60 | $12,138,000 |
| Maximum Application Valuation | $138,108,000 | ||||
b. Metric valuation
Once the overall project valuation is set, incentive payment values will be calculated for each metric/milestone domain in the DSRIP project plan by multiplying the total valuation of the project in a given year by the milestone percentages specified below.
| Metric/Milestone Domains | Performance Payment* |
Year 1 (CY 15) |
Year 2 (CY 16) |
Year 3 (CY 17) |
Year 4 (CY 18) |
Year 5 (CY 19) |
|---|---|---|---|---|---|---|
| Project progress Milestones (Domain 1) |
P4R/ P4P | 80% | 60% | 40% | 20% | 0% |
| System Transformation and Financial Stability Milestones (Domain 2) |
P4P | 0% | 0% | 20% | 35% | 50% |
| P4R | 10% | 10% | 5% | 5% | 5% | |
| Clinical Improvement Milestones (Domain 3) |
P4P | 0% | 15% | 25% | 30% | 35% |
| P4R | 5% | 10% | 5% | 5% | 5% | |
| Population health Outcome Milestones (Domain 4) |
P4R | 5% | 5% | 5% | 5% | 5% |
* P4P is pay for performance; P4R is pay for reporting.
Within each metric/milestone domain and pay–for–performance/ pay–for–reporting grouping, the value for each metric/milestone will be equally divided between all metrics in a given grouping per the process that follows.
Providers will receive DSRIP payments based on achievement of reporting milestones (P4R) and/or performance targets for metrics (P4P) for a given project during a performance period. Within each project, the value for achieving each performance target/milestone is the same (evenly weighted) and will be calculated as "meeting" or "not meeting" the performance target/milestone. The points given for reaching a specified performance target/milestone will be called an Achievement value and will be calculated as a 0 or 1 value. If a performance target or reporting milestone is met, the Performing Provider System will receive an AV of 1 for that performance target/milestone in that reporting period. If the Performing Provider System does not meet its milestone or performance target, the Performing Provider System will receive an AV of 0 for that reporting period. This will be done across every project in every domain.
Performing Provider System improvement targets will be established annually using the baseline data for DY 1 and then annually thereafter for DY2–5. High level performance targets will be provided by the State using results from managed care reporting data in DY1 and using results from DSRIP projects in DY2–DY5 as described in metric targets in Section III c. The Achievement value for P4P metrics will be established by comparing the Performing Provider System result for the reporting period with the improvement target for the Performing Provider System. If the Performing Provider System meets the improvement target for the metric, the Performing Provider System will receive an AV of 1. If the Performing Provider System result also meets a high–performance threshold, there may be additional payment through high performance fund, which is not included in this part of the payment calculation.
AVs will then be grouped into either a pay–for–reporting (P4R) or a pay–for–performance (P4P) bucket for each domain. The P4P and P4R AVs in each domain will be summed to determine the Total Achievement Value (TAV) for the domain. A Percentage Achievement Value (PAV) will then be calculated by dividing the TAV by the maximum AV (the total number of metrics) for P4P and P4R in each domain. The PAV will demonstrate the percentage of achieved metrics within the P4R and P4P metrics for each domain for that reporting period.
Example: A Performing Provider System has a project in year one with a project level valuation of $100,000 for year one. If the Performing Provider System achieves two out of five of its metrics/milestones for that project it would receive 40 percent of the $100,000 or $40,000. The metrics/milestone value would be assigned AV and PAVs as follows:
| Metric/Milestone | Achievement | AV |
|---|---|---|
| Milestone 1 | Achieved | 1 |
| Milestone 2 | Achieved | 1 |
| Milestone 3 | Not Achieved | 0 |
| Milestone 4 | Not Achieved | 0 |
| Milestone 5 | Not Achieved | 0 |
| TAV | 2 | |
| PAV 2/5 | 40% |
The PAV will be used to determine the level of the total payment the provider has earned for that reporting period based upon the performance payment distribution provided under the metric valuation. The level of payment for a provider within a domain will be proportionate to the PAV allocated to that domain. Additionally, the Performing Provider System will be eligible for bonus payments by reaching separate high–performance targets described in Section III and Attachment J.
c. Project Value Monitoring
Performing Provider Systems will be required to develop budgets and report on DSRIP project spending throughout the demonstration. As described in paragraph VI.c below, CMS reserves the right to review project values to ensure that the project value index, the population denominator, and the overall project valuation are calculated correctly.
VI. DSRIP Project Plan Review Process
a. Overview of Review Responsibilities
Each Performing Provider System that elects to participate in the DSRIP program must submit a DSRIP Plan in accordance with the DSRIP Plan guidelines outlined in section IV of this Project Funding and Mechanics protocol, Attachment J: DSRIP Strategies Menu and Metrics, and the demonstration´s Special Terms and Conditions. Performing Provider Systems are expected to provide accurate information in their DSRIP plans and respond to the state and CMS´s requests for additional information and/or plan revisions in accordance with the timelines specified.
The state is responsible for reviewing all DSRIP plans using a CMS–approved checklist and other review process requirements described below. The state´s review will be supplemented by an independent assessment of DSRIP plans and a public engagement period, which should inform the state´s decision of whether to approve a DSRIP plan.
CMS will monitor the state´s review process and approve projects in accordance with section VI.c. below.
All Performing Provider Systems will be subject to addition review during the mid–point assessment, at which point the state may require DSRIP plan modifications and may terminate some DSRIP projects, based on the feedback from the independent assessor, the public engagement process and the state´s own assessment of project performance. CMS will also monitor this mid–point assessment review process and make determinations in accordance with V.d
b. State–level Review Process
i. DSRIP plan review checklist
On or before September 1, 2014, the state will submit the state´s approach and review criteria for reviewing DSRIP Project Plans, as well as a draft DSRIP Plan Initial Review Checklist that will be used in the state´s initial review of DSRIP Plans to CMS.
CMS and the state will work collaboratively to refine the criteria, approach, and DSRIP Plan Checklist to support a robust review process and compelling justification for approval of each project. The state (with support from the independent assessor) will apply the CMS approved review process to ensure that DSRIP Plans are thoroughly and consistently reviewed.
At a minimum, the DSRIP Plan Checklist shall include the following criteria:
- The plan is in the prescribed format and contains all required elements described herein and is consistent with special terms and conditions.
- The plan conforms to the requirements for Domains 1, 2, 3, and 4 as described herein, as well as in Attachment J: DSRIP Strategies Menu and Metrics
- The plan clearly identifies goals, milestones, metrics, and expected results.
- The description of the project is coherent and comprehensive and includes a logic model clearly representing the relationship between the goals, the interventions and the measures of progress and outcome.
- The project selection is grounded in a demonstrated need for improvement at the time that the project is submitted and is sufficiently comprehensive to meaningfully contribute to the CMS three–part aim for better care for individuals, better health for the population, lower costs through improvement (i.e. Triple Aim), and while at the same time charting a path towards future sustainability.
- The likelihood for success of this intervention is based on, where available, accurate and robust citations to the evidence base.
- The plan includes an approach to rapid cycle evaluation that informs the system of progress in a timely fashion, and how that information will be consumed by the system to drive transformation and who will be accountable for results, including the organizational structure and process to oversee and manage this process. The plan must also indicate how it will tie into the state´s requirement to report to CMS on a rapid cycle basis.
- The plan includes a detailed description of project governance. Included in the description will detailed accounting of how decisions will be made and what corporate structure will be used throughout the life of the project. A clear description of the powers granted to the project´s corporate entity by participating providers must be described as well as what the governance plan is beyond the waiver period. The governance plan must address how the Performing Provider System will address management of lower performing providers in the Performing Provider System network.
- The goals are mapped to a robust and appropriate set of research hypotheses to support the evaluation.
- There is a coherent discussion of the Performing Provider System´s participation in a learning collaborative that is strongly associated with the project and demonstrates a commitment to collaborative learning that is designed to accelerate progress and mid– course correction to achieve the goals of the project and to make significant improvement in the outcome measures specified.
- The amount and distribution of funding is in accordance with Section V of this protocol "Project Valuation."
- The plan, project, milestones, and metrics are consistent with the overall goals of the DSRIP program.
- The plan where necessary includes specific goals, projects, milestones and metrics focused on directly and aggressively addressing any provider financial stability issues.
ii. Independent assessment and public engagement process
The state must identify an independent entity ("independent assessor") to conduct an impartial review of all submitted DSRIP plans. The independent assessor will first conduct an initial screen of DSRIP plans to ensure that they meet the minimum submission requirements.
The independent assessor will notify the Performing Provider System in writing of any initial questions or concerns identified with the provider´s submitted DSRIP Plan and provide an opportunity for Performing Provider Systems to address these concerns.
After determining which DSRIP plans meet the minimum submission criteria, the independent assessor will convene a panel of relevant experts and public stakeholders to assist with the scoring of projects, in a manner similar to a federal grant review process. The independent assessor will ensure that standards are followed to prevent conflict of interest in the panel scoring process.
iii. Consumer Education Campaign
The state will conduct a statewide consumer education campaign through a competitively selected contractor with a proven track record in conducting large public education campaigns. The consumer education campaign will focus on development of educational materials and marketing efforts to help educate Medicaid and uninsured members about the benefits of the DSRIP program and the services available through local Performing Providers Systems.
Campaign materials will be developed in multiple languages.
iv. State assessment
According to a timeline developed by the state and CMS that aligns with the DSRIP deliverables schedule outlined in STC 40 in section IX, the state will make its official, initial determination on each timely submitted DSRIP Plan based on the findings of the independent assessor and the outside review panel. Any deviations from the independent assessor´s recommendations should be clearly explained to CMS.
The state will notify the provider system in writing that the plan has been approved and submitted to CMS.
During the state review process, including by the independent assessor and before the state notifies the provider system of an approval, the state will make adjustments to these reviews to accommodate any systemic gaps that CMS identifies in its review of a sample of plans as provided in VI.c. Any revisions to the reviews will be applied to all plans.
c. CMS Monitoring Process
In addition to approving the review protocol, CMS will review a sample of plans reviewed by the independent assessor and by the state to determine whether the protocol was followed, will identify any systematic gaps between the protocol and the actual reviews, and will provide such findings to the state to address these gaps in reviews by the independent assessor and by the state. CMS reserves the right to do a second sampling following notification by the state that the review processes were revised and after the independent assessor and the state complete additional reviews. Assuming that CMS finds that the reviews are consistent with the review protocol, CMS will accept the state´s recommendations for approval with the following possible exceptions which will be applied at CMS´s discretion:
- The state´s decision about approval is not consistent with the independent assessor
- The plan is an outlier in the valuation schema
- There is evidence in the plan, or exogenous information made available to CMS that calls into question for the independent assessor or the state of funding duplication
- There is evidence in the plan, or exogenous information made available to CMS calls into question whether the project is new or significantly expanded or enhanced from a project already underway.
CMS will complete its review according to a timeline developed by the state and CMS that aligns with the DSRIP deliverables schedule outlined in STC 40 in section IX. CMS reserves the right to conditionally approve plans, and to allow modifications to plans to resolve issues it identifies in its review provided that the modifications are made to the plan and found acceptable by CMS according to the timeline provided by CMS.
d. Mid–point Assessment
The state´s mid–point assessment review will be developed in collaboration with CMS. All DSRIP plans initially approved by the state must be re–approved by the state in accordance with the CMS approved review protocol in order to continue receiving DSRIP funding in DY 4 and 5.
The state will use and independent assessor and public engagement process similar to the process used for the initial approval of projects, described in paragraph b.ii above.
The state will submit to CMS for approval, on or before October 1, 2016, draft mid–point assessment review criteria, a description of its approach to review, and a draft DSRIP Plan Mid– point Assessment Checklist that will reflect the approved criteria and will be used in the assessment. CMS and the state will work collaboratively to refine the criteria, approach, and DSRIP Plan Checklist. The state will apply these criteria to ensure that DSRIP projects are thoroughly and consistently reviewed. Where possible, the state will notify providers in advance of the mid–point assessment if providers need to make changes in order to comply with the approved review criteria.
During DY 3, the independent assessor will work with the state to conduct a transparent mid– point assessment of all DSRIP projects using CMS–approved criteria. This review will provide an opportunity to modify projects and/or metrics in consideration of learning and new evidence. The independent assessor will conduct a focused review of certain high–risk projects identified by the state, CMS or the independent entity based on information provided for all projects in the provider´s monitoring reports.
The mid–point assessment review will, at a minimum, include an assessment of the following elements:
- Compliance with the approved DSRIP project plan, including the elements described in the project narrative;
- Compliance with the required core components for projects described in the DSRIP Strategies Menu and Metrics, including continuous quality improvement activities;
- Non–duplication of Federal funds;
- An analysis and summary of relevant data on performance on metrics and indicators to this point in time;
- The benefit of the project to the Medicaid and uninsured population and to the health outcomes of all patients served by the project (examples include number of readmissions, potentially preventable admissions, or adverse events that will be prevented by the project);
- An assessment of project governance including recommendations for how governance can be improved to ensure success. The composition of the performing provider system network from the start of the project until the midpoint will be reviewed. Adherence to required policies regarding management of lower performing providers in the network will be reviewed with a special focus on any action with regard to removing lower performing members prior to DY 4 and 5. (Note: Modifying coalition members requires a plan modification);
- The opportunity to continue to improve the project by applying any lessons learned or best practices that can increase the likelihood of the project advancing the three part aim; and
- Assessment of current financial viability of all providers participating on the DSRIP project.
Based on the recommendations by the independent assessor, the state or CMS may require prospective plan modifications that would be effective for DYs 4 and 5, including adjustments to project metrics or valuation. Significant changes to the number of Medicaid beneficiaries attributed to a Performing Provider System will require adjustments to the project valuation.
The state will review all modifications resulting from the mid–point assessment prior to CMS review and consideration, consistent with the process for review of plan modifications, described in section X. Future DSRIP payment for a provider may be withheld until the necessary changes as identified by the mid–point assessment are submitted (and all other requirements for DSRIP payment are met).
VII. Reporting Requirements and Ongoing Monitoring
Performance management and assessment of DSRIP will occur throughout its duration and will take several forms. Each area of assessment is interrelated to ensure a continuous cycle of quality improvement and shared learning. The final project work plans will provide the basis for monitoring each project.
- Ongoing provider–level evaluations will occur on a regular basis, as described below, and seek to provide timely and actionable feedback on the initiative´s progress, in terms of infrastructure changes, implementation activities and outcomes. The formative evaluation, or performance management, will track and report regularly on actions, performance on objective attainment and overall progress towards achieving a health care system based on the improving health, improving care, and reducing costs, and progress toward achieving the primary goals of DSRIP, to reduce avoidable hospitalization and seek improvements in other health and public health measures by transforming systems.
- Learning collaboratives will be implemented to seek peer–to–peer (provider–to– provider) and community stakeholder input on project level development of action plans, implementation approaches and project assessment. New York will be responsible for leading the collaborative approach to ensure effective sharing of information (e.g. best practices, case studies, challenges, results). The schedule for the collaboratives meeting will be shared with CMS.
- On a quarterly basis, the state will publish on its website project–by–project status updates which will show available data that reflects each strategy´s progress on metrics and indicators, as relative to pre–approved targets.
- A mid–point assessment (end of the third year) will be completed by an independent assessor. The midpoint assessment which will provide independent quantitative analysis of DSRIP planning and implementation through December 2016, as well as timely qualitative research findings which will provide context for reports on provider´s progress in planning and implementing selected DSRIP programs. The qualitative findings will contribute to understanding implementation issues which go beyond the quantitative analyses. In addition, the qualitative analysis will inform and sharpen analytic plans for the summative evaluation. The mid–point assessment will be submitted by the end of June 2017.
- In addition to monitoring, an interim and final summative statewide evaluation of DSRIP will be completed by the independent evaluator to examine the effect of DSRIP activities on achieving the State goals of (1) safety net system transformation at both the system and state level; (2) accountability for reducing avoidable hospital use and improvements in other health and public health measures at both the system and state level; and (3) efforts to ensure sustainability of delivery system transformation through leveraging managed care payment reform. The data and findings of the mid–point assessment will be among the information used by the independent evaluator for the interim evaluation. Among other things, the interim evaluation will provide broad learning both within the state and across the nation. Part of this interim evaluation will examine issues overlapping with ongoing provider– level evaluations, and part of this effort will examine questions overlapping with the final evaluation.
a. Semi–annual Reporting on Project Achievement
Two times per year, Performing Provider Systems seeking payment under the DSRIP program shall submit reports to the state demonstrating progress on each of their projects as measured by the milestones and metrics described in their approved DSRIP plan. The reports shall be submitted using the standardized reporting form approved by the state and CMS. Based on the reports, the state will calculate the incentive payments for the progress achieved in accordance with Section VII "Disbursement of DSRIP Funds". The Performing Provider System shall have available for review by the state or CMS, upon request, all supporting data and back–up documentation. These reports will be due as indicated below after the end of each reporting period:
- Reporting period of January 1 through June 30: the reporting and request for payment is due July 31.
- Reporting period of June 30 through December 31: the reporting and request for payment is due January 31.
These reports will serve as the basis for authorizing incentive payments to Performing Provider Systems for achievement of DSRIP milestones. The state shall have 30 days to review and approve or request additional information regarding the data reported for each milestone/metric and measure. If additional information is requested, the Performing Provider System shall respond to the request within 15 days and the state shall have an additional 15 days to review, approve, or deny the request for payment, based on the data provided. The state shall schedule the payment transaction for each Performing Provider System within 30 days following state approval of the Performing Provider System´s semi– annual report.
As part of CMS´s monitoring of DSRIP payments, CMS reserves the right to review a sample of the Performing Provider System Reports and withhold or defer FFP if DSRIP milestones have not been met.
Note: Because many domain 2, 3, and 4 metrics are annual measures, these annual measures will only be available to be reported once a year for purposes of authorizing and determining incentive payments.
b. State Monitoring Reports
The state, or its designee, will conduct robust monitoring and assessment of all submitted reports, Performing Provider System progress, challenges and completion no less frequently than quarterly, and as appropriate in order to monitor DSRIP implementation and activities.
Upon this review, an analysis will be made regarding:
- the extent of progress each Performing Provider System is making towards meeting each milestone
- the specific activities that appear to be driving measurable change
- the key implementation challenges, including governance issues, associated with specific activities designed to drive improvement
- the identification of adjustments to the DSRIP program, and/or projects as observed through the analysis of submitted provider–level data and/or onsite findings as they occur
Comparative analysis and findings will be performed and summarized into actionable reports that provide the right level of information to various project stakeholders to help facilitate learning at the Performing Provider System level, as well as the DSRIP program level. The reports will be used to drive peer–to–peer discussion regarding opportunities for improvement and methods for course correction through the use of the Learning Collaborative. The results of these assessments will be disseminated to the independent DSRIP evaluation contractor and CMS. This information is expected to inform the DSRIP evaluation during both the mid–point and summative evaluations to understand key factors related to the performance and progression of the DSRIP program to date.
The state, or its designee, will take effective action, as needed, to remedy a finding to promote fulfillment of the DSRIP goals. This may include providing feedback to the health care industry at–large, or individual project participants if significant issues are observed.
- Operational Report
An operational report at the project level will be the primary report to manage and report DSRIP performance. The operational report will have the functionality to report on project–level data related to Performing Provider Systems performing the same project. This report will also include an Executive Summary which will be used by CMS, senior state officials and the public as a means of following the overall progress of the DSRIP demonstration. This report will include the following data elements:- Identification of participating providers
- Completion factor of providers, by provider
- Dashboard of project–specific measure results, aggregated at project, plan, regional and state levels
- Summary of applied interventions
- Summary of pilot models
- Summary of reported challenges
- Summary of reported successes
- Update on governance
- Noted best practices
- Summary of approved payments (compared to the valuation in the DSRIP project plan), which should reconcile to the DSRIP funding reported on the CMS–64
This level of reporting may also show progress of the learning process itself by tracking the frequency of meetings by activity and participation in order to confirm that the learning collaborative activity is being fulfilled by the Performing Provider System.
It will be the responsibility of each project participant to ensure effective diffusion of learning amongst Performing Provider Systems who have selected the same project focus area. This includes discussing the types of innovations, strategies and Plan–Do– Study–Act (PDSA) cycles that have been implemented throughout the demonstration. - Consumer Level Report
A consumer level report will have the functionality to report on high–level geographic and project–specific data elements in order to understand which providers in their area are driving to improve quality and the area of focus for that Performing Provider System. The report may include:- County–level map that indicates all New York hospitals
- County–level map that indicates all participating hospitals and participating outpatient providers
This report may also have drill–down functionality to learn summary detail about the objective, methodology, current performance, and expected results of each Performing Provider System.
c. Learning Collaboratives
One facet of the DSRIP program is the development of the Learning Collaborative. The purpose of the Learning Collaborative is to promote and support a continuous environment of learning and sharing based on data transparency within the New York healthcare industry in an effort to bring meaningful improvement to the landscape of healthcare in New York.
The Learning Collaborative will be managed by the state and/or its independent assessor through both virtual and in–person collaboration that both builds relationships as well as facilitates project analysis and measurement. The Learning Collaborative will be designed to promote and/or perform the following:
- Sharing of DSRIP project development including data, challenges, and proposed solutions based on the Performing Provider Systems´ quarterly progress reports
- Collaborating based on shared ability and experience
- Identifying key project personnel
- Identification of best practices
- Provide updates on DSRIP program and outcomes
- Track and produce a "Frequently Asked Questions" document
- Encourage the principles of continuous quality improvement cycles
There will be multiple collaboratives developed based on the number and type of projects chosen by Performing Provider Systems. Each learning Collaborative will include key personnel from the Performing Provider Systems and selected members of the stakeholder community including provider association representation. For each collaborative, the state will designate personnel to be responsible for guiding and facilitating the Learning Collaborative.
An online, web–based tool will be utilized in order to effectively manage the collection and the dissemination of information related to the DSRIP and projects. A key component of the online tool will be a reporting feature that allows tiered–level reporting that conveys key information to the various levels of stakeholder groups interested in learning and tracking performance of the DSRIP program. This tool will act as a repository with reporting capability for various audiences including that of the general public, the Department, CMS, and the healthcare industry.
The tool will deliver data in ways that can be 1) easily interpreted by various stakeholders, 2) promote self–evaluation, and 3) promote the diffusion of effective intervention models.
d. Program Evaluation
As described in STC 10.e. in section IX, the state will identify an independent evaluator to provide an interim and summative evaluation. The interim evaluation will consider among other things the findings of the mid–point assessment conducted by the independent assessor. The evaluations must be in accordance with the evaluation STCs 19–30 in section IX and as approved by CMS through the evaluation design phase provided in STC 20 in section IX.
The interim evaluation will be due one year prior to the expiration of the demonstration and will include data from DY 1, 2, and 3. The final, summative evaluation will be completed by the end of March 2020.
The interim and summative evaluation will meet all standards of leading academic institutions and academic peer review, as appropriate for both aspects of the DSRIP program evaluation, including standards for the evaluation design, conduct, interpretation, and reporting of findings.
e. Overall Data Standards
The state will collect data from providers often as is practical in order to ensure that project impact is being viewed in as "real time" a fashion as possible. Collecting and analyzing data in this fashion will allow for rapid, life–cycle improvement which is an essential element of the DSRIP project plan.
Since managed care is an important component of the state´s quality improvement strategy, the state will implement a provider/plan data portal that will allow access to appropriately permissioned patient and provider specific data in the Medicaid Data Warehouse. Role based access to this portal will allow providers and their partnering health plans access to current Medicaid claims and encounters data and eventually real time EMR and care management data provided through connectivity with local regional health organizations (RHIOs). Faster access to more real time clinical and managed care data will be particularly relevant to this project and is also the rationale for using state–measured health plans metrics or Quality Assurance Reporting Requirements (QARR) as a major data source for this project. In addition, providers and their partnering health plans will have access to the analytical capabilities of 3M and Salient suite of performance tools through the portal. This will allow DSRIP providers and the health plans to partner with the state to measure case mix adjusted avoidable hospitalization metrics at the local level using standardized definitions and eventually with more real time updates. More information on DSRIP performance and the portal will be posted on the state´s DSRIP website.
The state will use the Quality Committee, established in 2013 to assist NYSDOH on quality measurement and improvement that will be responsible for supporting the clinical performance improvement cycle of DSRIP activities. The Quality Committee includes representatives from various sectors of healthcare including hospitals, nursing homes, managed care plans, provider organizations and consumer representation. Additional members will be added specifically to reflect DSRIP including representatives from local governmental units and additional consumer representation. The current charge of the Committee is to provide NYSDOH with expertise in various sectors of health care quality, assist on proposed quality improvement goals and provide guidance on measuring and reporting quality information to the public. The Quality Committee will serve as an advisory group for DSRIP offering expertise in health care quality measures, clinical measurement and clinical data used in performance improvement initiatives.
Final decision–making authority will be retained by the state and CMS, although all recommendations of the committee will be considered by the state and CMS.
Specifically, the Quality Committee will provide feedback to the state regarding:
- Development of attribution models
- Selection of metrics
- Selection of the high–performance target goals including the behavioral health high–performance avoidable hospitalization threshold for bonus payment purposes.
Data and metrics that form the basis of incentive payments in DSRIP should have a high degree of accuracy and validity. Consistent with current requirements for MCO and PIHPs under 438.242, the state must ensure, through its contracts with the Performing provider systems, that each Performing provider system receiving payments under DSRIP maintains (or participates in) a health information system that collects, analyzes, integrates, and reports data and can achieve the objectives of this DSRIP. The state must require that each Performing provider system ensure that data received from providers within the system is accurate and complete by ensuring that Performing Provider Systems have appropriate data agreements in place (as described in section IV.b) and verifying the accuracy and timeliness of reported data (including such data that contributes to chart review metrics), screening the data for completeness, logic, and consistency.
To the degree that the data and metrics are generated and obtained via managed care systems already subject to 438.242, no additional validation of the data is required.
For data and metrics reported in systems not subject to 438.242, these agreements between the state and Performing provider systems should also be accompanied by validation process performed by the independent assessor to ensure that the processes are generally valid and accurate. Penalties will be applied to Performing provider systems that are not reporting data that are valid and accurate as described.
VIII. DSRIP Funding Limits
a. Statewide limit on DSRIP Funding
Total DSRIP Fund expenditures are limited as specified in STC 14 in section IX. In addition to this limit, DSRIP Fund expenditures cannot exceed the lesser of the aggregate valuation of DSRIP projects as adjusted to include DSRIP planning funding and funds allocated to the High Performance Fund. Allowable expenditures are further limited by the availability of non–federal funding (through proper IGT or other funding), and provider performance on DSRIP milestones and metrics.
b. Public Hospital and Safety Net Provider Performance Provider System Transformation Funds
All Performing Provider Systems with approved DSRIP Project Plans will be eligible to apply for funding from one of two DSRIP pools. The first, Public Hospital Transformation Fund, will be open to applicants led by a major public hospital system. The public hospital systems allowed to participate in this fund include:
- Health and Hospital Corporation of New York City
- State University of New York Medical Centers
- Nassau University Medical Center
- Westchester County Medical Center
- Erie County Medical Center
The second fund Safety Net Performance Provider System Transformation Fund, would be available to all other DSRIP eligible providers.
Allocation of funds between the two pools will be determined after applications have been submitted, based on the valuation of applications submitted to each pool.
c. High Performance Fund
A portion of the Public Hospital Transformation Fund and Safety Net Performance Provider System Transformation Fund will be set aside to reward high performing systems according to the process specified below. The high performance fund will be made up of the following funds:
- For DY 2–5, up to 10 percent of the total DSRIP funds set aside for the high performance fund
- Target Funds that are forfeited from providers that do not achieve project milestones and metrics, less any prior year appealed forfeited funds where the appeal was settled in the current demonstration year in favor of the Performing Provider System.
The total amount of funding allocated for the high performance fund shall be distributed to qualifying providers based on meeting a specific set of Domain 2 and 3 metrics identified as a high–performance metrics by the state with input from the quality and measures committee. The metrics for the high performance fund are specified in Attachment J.
Additional funds will be set aside within each fund for performing provider systems reaching stretch/ bonus level targets (set by the state with input from the quality and measures committee) for significant improvement in avoidable hospitalization reduction for their attributed behavioral health population.
IX. Disbursement of DSRIP Funds
a. Total Available DSRIP Incentive Payments for a Project based on Project Valuation
Aggregate incentive payments available over the 5–year demonstration period to a Performing Provider System will be based on the project valuation approved by the state, subject to the limits set forth in section V above
b. Payment Based on Milestone Achievement for DY 1 – DY 5
Incentive payments are calculated separately for each project. The amount of the incentive funding paid to a provider will be based on the amount of progress made within specific milestones and the valuation of those milestones.
Half of the incentive funding for Domain 1 in DY 1 will be awarded for approval of the DSRIP plan. Fifteen percent will be paid upon the delivery of an acceptable first semiannual report.
Fifteen percent will be paid upon the delivery of an acceptable second semiannual report.
For each metric, the provider will include in the required DSRIP provider report the progress made in completing each metric along with sufficient supporting documentation. Progress for a given metric will be categorized as fully achieved or not achieved. If a provider has previously reported progress in a domain and received partial funding after the first semi–annual reporting period, only the additional amount is eligible for funding in the second semi–annual reporting period.
c. Payments from the High Performance Fund
Performing Provider Systems who have achieved performance improvement beyond the stated target improvement value in their approved DSRIP project plan will be eligible for additional payment from the DSRIP high performance fund, not to exceed 30 percent of their DSRIP project value.
A half of the high performance fund will be available for tier 1 payments, and half will be available for tier 2 payments which will be distributed as follows:
- Higher performing participating providers whose performance closes the gap between their current performance and the high–performance level by 20 percent shall receive Tier 1 level reward payments.
- Higher performing participating providers whose performance meets or exceeds the high–performance level (90th percentile of statewide performance) shall receive Tier 2 level reward payments.
High performance fund payments shall be adjusted based on Medicaid and indigent population size served by the project being implemented by the provider. The percentages above may be adjusted up or down by the State for each metric as appropriate to account for volume of demand on the high performance fund.
The state, working with the quality committee, will set a high–performance threshold for the measures described in attachment J specifically avoidable hospitalizations for the entire attributed population and separate high–performance targets (physical and behavioral metrics) for the behavioral health population subset. high–performance payments will be based on attaining 20 percent gap to goal or the 90th percentile of statewide performance on the high–performance metrics listed in attachment J.
d. Accountability for state performance
As described in STC 14 in section IX, providers and the state are accountable for statewide performance. DSRIP funding for providers may be reduced based on poor performance statewide described below.
If any of the four milestones below are not met, then DSRIP payments to providers will be reduced by the amount specified in STC 14 in section IX. DSRIP payment reductions will be applied proportionately to all DSRIP Performing Provider Systems based on the valuation of their DSRIP project plans. DSRIP reductions will not be applied to the DSRIP high performance fund payments.
Achievement of the statewide milestones is calculated as follows:
- Statewide performance on universal set of delivery system improvement metrics. The core set of delivery system improvement metrics in domain 2 of attachment J will be assigned a direction for improving or worsening and will be calculated to reflect the performance of the entire state. This milestone will be considered passed in any given year if more metrics in this domain are improving on a statewide level than are worsening (i.e. the performance level is the same or better, no error bar applied), as compared to the prior year as well as compared to initial baseline performance (DY 1).
- A composite measure of success of projects statewide on project–specific and population– wide quality metrics. The number of metrics met by each Performing Provider System in a given year based on the project–specific improvement standards specified in their approved DSRIP project plan will be added together to determine the composite success of all DSRIP projects. For the purposes of this addition, pay for reporting measures will only be counted once in the aggregate for each domain. This statewide milestone will be considered passed in any given year if the number of metrics met by all Performing Provider Systems in the aggregate is greater than the number of metrics that were not met.
- Growth in statewide total Medicaid spending that is at or below the target trend rate. As further described in STC 14 in section IX, statewide performance on this milestone will be considered passed if the state improves on the following two metrics on a per member per month (PMPM) basis, comparing the most recent state fiscal year to the year that immediately precedes it:
- Growth in statewide total inpatient and emergency room spending that is at or below the target trend rate (Measure applies in DSRIP Year3, DSRIP Year 4 and DSRIP Year 5).
- Growth in statewide total Medicaid spending that is at or below the target trend rate (measure applies in DSRIP Year 4 and DSRIP Year 5). PMPM amounts will be adjusted to exclude growth in federal funding associated with the Affordable Care Act. The state will not be penalized if it uses these higher FMAP rates generated by the ACA to reinvest in its Medicaid program.
- Implementation of the managed care plan. This milestone will be measured by targets agreed upon by CMS and the state after receipt of the managed care strategy plan in STC 39 in section IX related to reimbursement of plans and providers consistent with DSRIP objectives and measures. These targets will include one associated with the degree to which plans move away from traditional fee for service payments to payment approaches rewarding value.
e. Intergovernmental Transfer Process
The state will calculate the nonfederal share amount to be transferred by an IGT Entity in order to draw the federal funding for the incentive payments related to the milestone achievement that is reported by the Performing Provider System and approved by the IGT Entity and the State.
Within 14 days after notification by the state of the identified nonfederal share amount, the IGT Entity will make an intergovernmental transfer of funds. The state will draw the federal funding and pay both the nonfederal and federal shares of the incentive payment to the Performing Provider System. If the IGT is made within the appropriate 14–day timeframe, the incentive payment will be disbursed within 30 days. The total computable incentive payment must remain with the Performing Provider System.
X. DSRIP Project Plan Modifications
a. Modifying Existing Project Plans in Limited Circumstances
No more than once a year, Performing Provider Systems may submit proposed modifications to an approved DSRIP project plan for state and CMS review. These modifications may not decrease the scope of the project unless they also propose to decrease the project´s valuation.
Removal of any Performing Provider System member organization requires a proposed modification and removal of any such lower performing member must follow the required governance procedures including progressive sanction requirements.
The state and CMS will follow the same review process described in section VI above, except that the independent assessor will not be expected to convene review panels.
b. Reinvestment of Unused DSRIP Funds in DY4 and DY5
Unused DSRIP funding for DY 4 and 5 (including funding allocated to projects that were terminated as part of the midpoint assessment) may be directed towards further replicating high performing DSRIP projects that have proven to be particularly successful and can be implemented elsewhere (in approved Performing Provider System´ that are not currently employing such projects) and achieve results within two years. The state will develop its methodology for expanding successful projects and submit this to CMS in DY 2 for review and approval before the midpoint assessment is completed in DY 3.
Partnership Plan – Approval Period: August 1, 2011 – December 31, 2014; as Amended April 14, 2014
Follow Us