2022-2023 Value Based Payment Reporting Requirements
Technical Specifications Manual
- 2022-2023 Tech Spec Manual is also available in Portable Document Format (PDF)
____________________________________________________________
New York State Department of Health
Email Address: OQPSVBP@health.ny.gov
Last Revised March 2, 2023
Table of Contents
- INTRODUCTION
- VBP ARRANGEMENTS AND ASSOCIATED QUALITY MEASURES
- CATEGORIZATION OF QUALITY MEASURES
- CLASSIFICATION OF QUALITY MEASURES
- ORGANIZATIONS REQUIRED TO REPORT
- REPORTING GUIDELINES VBP MAINSTREAM & SUBPOPULATIONS
- WHERE TO SUBMIT VBP REPORTING DATA
- TABLE 1: 2022 VBP LIST OF REQUIRED MEASURES
- PATIENT ATTRIBUTION FILE
- REPORTING GUIDELINES VBP MLTC
- TABLE 2: 2023 MLTC VBP LIST OF REQUIRED MEASURES
- MLTC ATTRIBUTION FILE
- ATTRIBUTION METHODOLOGY
- FILE FORMAT
- FIELD DEFINITIONS
- FILE SUBMISSION
- TABLE 3: 2022 VBP LIST OF CATEGORY 2 MEASURES
- TABLE 4: 2023 VBP MLTC CATEGORY 2 MEASURES
- TABLE 5: NYS FIPS CODES BY COUNTY
- TABLE 6: SUBMISSION EXAMPLES
- Member Data, attributed to Provider 2 from 5/1/2022 to 12/31/2022
- TABLE 7: MCO ATTRIBUTION FILE - DATA QUALITY CHECKLIST
- TABLE 8: MLTC ATTRIBUTION FILE - DATA QUALITY CHECKLIST
| Important Dates & Contact Information | ||||
|---|---|---|---|---|
| Mainstream VBP | MLTC VBP | |||
| Contact | OQPSVBP@health.ny.gov | Contact | MLTCVBP@health.ny.gov | |
| Submission Date | All files must be received electronically by 11:59 p.m. EST Friday, July 28, 2023. | Submission Date | Plan/Provider-VBP Contractor performance to the State by Friday, July 28, 2022 | |
| MLTC VBP data files: All files must be received electronically by 11:59 p.m. EST Friday, July 28, 2023. | ||||
| Health Commerce System (HCS) | To: OQPS VBP Evaluation | Health Commerce System (HCS) | To: MLTC VBP Evaluation | |
I. Submission Requirements
INTRODUCTION
The purpose of this document is to make stakeholders aware of the quality measure reporting requirements for Medicaid Managed Care Organizations (MCOs) participating in the New York State (NYS) Medicaid Value-Based Payment (VBP) program. The 2022-2023 VBP Reporting Requirements refer to data for Measurement Year 2022 (MY2022).
Sections II, III, and IV of this document include guidance for the organizations responsible for reporting, the subset of measures for which reporting will be required by Mainstream VBP Arrangements, and the changes to the reportable set of MY2022 Quality Measure Sets (see TABLE 1: 2022 VBP LIST OF REQUIRED MEASURES). Sections V and VI provide guidance for Managed Long-Term Care (MLTC) VBP Arrangements.
The New York State Department of Health (NYS DOH) has completed the first phase of a health transformation effort, known as the State Innovation Model (SIM) award, which focused on the transformation of primary care delivery and payment models statewide. The New York State Patient Centered Medical Home (NYS PCMH) model was created as part of the SIM initiative. With NYS PCMH, a Primary Care (PC) Core measure set was developed, and multi-payer data is used to calculate results for practices for the measure. To reduce the burden on MCOs participating in both the NYS PC measure set model and Medicaid VBP, we are aligning the reporting for both programs and utilizing the NYS Primary Care Core Set Scorecard data request to fulfill reporting requirements for both programs, where possible.
VBP ARRANGEMENTS AND ASSOCIATED QUALITY MEASURES
The VBP Roadmap updated in June 2022, outlines five types of VBP arrangements to be included for MY2022:
- Total Care for the General Population (TCGP) Arrangement: Includes all costs and outcomes for care, excluding certain subpopulations (specified below).
- Total Care for Special Needs Subpopulation Arrangements: Includes costs and outcomes of total care for all members within a subpopulation exclusive of TCGP.
- Children's Subpopulation: to address the unique needs of children at different developmental stages
- Behavioral Health/Health and Recovery Plans (HARP): for those with Serious Mental Illness or Substance Use Disorders
- People Living with HIV/AIDS
- Managed Long Term Care (MLTC)
- Episodic Care Arrangements
- Maternity Care: Includes episodes associated with a pregnancy, including prenatal care, delivery and postpartum care through 60 days post-discharge for the mother, and care provided to the newborn from birth through the first 30 days post-discharge.
- IPC arrangements: All references to Integrated Primary Care (IPC) arrangements and associated requirements have been removed from the VBP Roadmap1.
CATEGORIZATION OF QUALITY MEASURES
Through a multi-group stakeholder engagement process, a set of quality measures was defined for each arrangement. Based on an analysis of clinical relevance, reliability, validity, and feasibility, each measure was placed into one of three categories:
- Category 1: Selected as clinically relevant, reliable, valid, and feasible. These measures are outlined in Table 1.
- REQUIREMENT: Only the Category 1 measures that are indicated in this document as "Required to Report" (✓) are to be reported by the MCO to the State.
- Category 2: Seen as clinically relevant, valid, and reliable, but where the feasibility could be problematic.
Category 2 measures are listed in the appendix (Table 3) of this guide. - Category 3: Rejected based on a lack of relevance, reliability, validity, and/or feasibility. These measures are not included in this manual.
CLASSIFICATION OF QUALITY MEASURES
Each Category 1 measure is classified as either Pay-for-Performance (P4P) or Pay-for-Reporting (P4R). P4P measures are intended to be used in the determination of shared savings amounts for which VBP Contractors are eligible. P4R measures are intended to be used by the MCOs to incentivize the VBP Contractors for reporting data to monitor the quality of care delivered to members in a VBP contract.
|table of contents|ORGANIZATIONS REQUIRED TO REPORT
Medicaid Managed Care Organizations with Level 1 or higher value-based contracting arrangements are required to report. All submissions must be received electronically by 11:59 p.m. EST on Friday, July 28, 2023.
|table of contents|REPORTING GUIDELINES VBP MAINSTREAM & SUBPOPULATIONS
II. Reporting Guidelines VBP Mainstream & Subpopulations
Mainstream & Subpopulation VBP Arrangements [Other than MLTC]
The State is requesting that Medicaid Managed Care (MMC) plans submit data files that leverage their 2022 Quality Assurance Reporting Requirements (QARR) (HEDIS®)2 submission which will be used to create aggregated quality results by VBP Contractor for all members in a VBP Arrangement. Specifically, the State is asking insurers to provide a modified version of the NYS Patient-Level Detail (PLD) file, along with provider and practice information. Submission of the NYS PCMH Patient-Level Detail file for all members in a Level 1 or higher VBP Arrangement will fulfill this reporting requirement. The NYS PCMH Patient-Level Detail File layout is included in Section IV of this manual. The State is also requesting a separate Patient Attribution file for all members in a Level 1 or higher VBP Arrangement. The Patient Attribution file layout is also included in Section IV.
Table 1: 2022 VBP List of Required Measures
- Lists, by arrangement, the 2022 VBP Category 1 Measure sets and indicates the 2022 measures the State is requiring for reporting.
- Section IV: File Specifications required for reporting.
- This manual describes reporting requirements only. For VBP reporting or contracting questions, please contact OQPSVBP@health.ny.gov.
- Organizations must purchase the HEDIS® 2022 Technical Specifications for descriptions of the required HEDIS® measures. For specifications for other non-HEDIS measures, please contact the measure steward for the correct version of the specification. NYS-specific measures are defined in the 2022 Quality Assurance Reporting Requirements (QARR) Technical Specifications Manual.
MEASURE CHANGES
- Changes to the Reporting Requirements for 2022 Measure Sets were made based on the feedback received by the DOH from the Clinical Advisory Groups, HEDIS measurement changes, and other stakeholder groups. Those changes are indicated below. In instances where a measure was moved from Category 1 in MY2021 to Category 2 in MY2022 or removed entirely, the State will not require reporting of the data related to those measures.
TCGP:
Category 1: Changes
- Comprehensive Diabetes Care (CDC): Eye Exam (retinal) Performed; replaced with Eye Exam for Patients with Diabetes (EED); as a Category 1 Measure
- Comprehensive Diabetes Care (CDC): Hemoglobin A1c (HbA1c) Poor Control (>9.0%); replaced with Hemoglobin A1c Control for Patients with Diabetes (HBD) as a Category 1 Measure.
- Follow-Up After Emergency Department Visit for Alcohol and Other Drug Dependence (FUA); name and specifications revised by NCQA to Follow-Up After Emergency Department Visit for Substance Use (FUA); as a Category 1 Measure.
- Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment (IET); measure name and specifications revised by NCQA to Initiation and Engagement of Substance Use Disorder Treatment (IET); as a Category 1 Measure.
Category 2: Changes
- There are no TCGP category 2 measures.
IPC: Arrangement type removed from VBP Roadmap.
Behavioral Health/HARP:
Category 1: Changes
- Completion of Home and Community Based Services Annual Needs Assessment; removed as a Category 1 Measure.
- Comprehensive Diabetes Care (CDC): Eye Exam (retinal) Performed; replaced with Eye Exam for Patients with Diabetes (EED); as a Category 1 Measure
- Comprehensive Diabetes Care (CDC): Hemoglobin A1c (HbA1c) Poor Control (>9.0%); replaced with Hemoglobin A1c Control for Patients with Diabetes (HBD) as a Category 1 Measure.
- Employed, Seeking Employment or Enrolled in a Formal Education Program; removed as a Category 1 Measure.
- Follow-Up After Emergency Department Visit for Alcohol and Other Drug Dependence (FUA); name and specifications revised by NCQA to Follow-Up After Emergency Department Visit for Substance Use (FUA); as a Category 1 Measure.
- No Arrests in the Past Year; removed as a Category 1 Measure.
- Percentage of Members Enrolled in a Health Home; removed as a Category 1 Measure.
- Stable Housing Status; removed as a Category 1 Measure.
Category 2: Changes
- No Category 2 Measures were changed, added, or removed from the Behavioral Health/HARP measure set.
HIV/AIDS:
Category 1: Changes
- Comprehensive Diabetes Care (CDC): Eye Exam (retinal) Performed; replaced with Eye Exam for Patients with Diabetes (EED); as a Category 1 Measure
- Comprehensive Diabetes Care (CDC): Hemoglobin A1c (HbA1c) Poor Control (>9.0%); replaced with Hemoglobin A1c Control for Patients with Diabetes (HBD) as a Category 1 Measure.
- Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment (IET); name and specifications revised by NCQA to Initiation and Engagement of Substance Use Disorder Treatment (IET) as a Category 1 Measure.
Category 2: Changes
- No Category 2 Measures were changed, added, or removed from the HIV/AIDs measure set.
Maternity:
Category 1 Changes
- Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment (IET); name and specifications revised by NCQA to Initiation and Engagement of Substance Use Disorder Treatment (IET) as a Category 1 Measure.
Category 2: Changes
- No Category 2 Measures were changed, added, or removed from the Maternity measure set.
Children's:
Category 1: Changes
- Adolescent Preventive Care Measures; removed as a Category 1 Measure.
- Follow-Up Care for Children Prescribed ADHD Medication (ADD); measure specifications revised by NCQA as a Category 1 Measure.
Category 2: Changes
- Follow-Up After Emergency Department Visit for Alcohol and Other Drug Dependence (FUA); name and specifications revised by NCQA to Follow-Up After Emergency Department Visit for Substance Use (FUA); as a Category 1 Measure.
WHERE TO SUBMIT VBP REPORTING DATA
- Electronically submit all files (no later than 11:59 p.m. EST on Friday, July 28, 2023) via a secure file transfer facility. Do not mail materials.
- Specific delivery instructions are given for each file.
WHAT TO SEND FOR VBP REPORTING
- The State is requesting a NYS PCMH file and a Patient Attribution file for ALL members in a VBP Level 1 or higher Arrangement.
*****All submissions must be received electronically by 11:59 p.m. EST on Friday, July 28, 2023.*****
QUESTIONS CONCERNING 2023 VBP REPORTING
Please submit all questions to OQPSVBP@health.ny.gov.
|top of section| |table of contents|III. Reporting Requirements
TABLE 1: 2023 VBP LIST OF REQUIRED MEASURES
| Measures | Notes | Arrangement Type | NQF ID | Specifications | Class | ||||
|---|---|---|---|---|---|---|---|---|---|
| TCGP | Maternity | HARP | HIV/AIDS | Children's | |||||
| Total Care for the General Population (TCGP) | |||||||||
| Adherence to Antipsychotic Medications for Individuals with Schizophrenia (SAA) | ✓ | NA | ✓ | NA | NA | 1879 | HEDIS 2022 | P4P | |
| Adherence to Mood Stabilizers for Individuals with Bipolar I Disorder | NR | NA | NA | NR | NA | 1880 | CMS 2022 | P4P | |
| Antidepressant Medication Management - Effective Acute Phase Treatment & Effective Continuation Phase Treatment (AMM) | ✓ | NA | NA | ✓ | NA | 0105 | HEDIS 2022 | P4P | |
| Asthma Medication Ratio (AMR) | ✓ | NA | ✓ | ✓ | ✓ | 1800 | HEDIS 2022 | P4P | |
| Breast Cancer Screening (BCS) | ✓ | NA | ✓ | ✓ | NA | 2372 | HEDIS 2022 | P4P | |
| Cervical Cancer Screening (CCS) | 2 | ✓ | NA | ✓ | ✓ | NA | 0032 | HEDIS 2022 | P4P |
| Child and Adolescent Well–Care Visits (WCV)** | ✓ | NA | NA | NA | ✓ | HEDIS 2022 | P4P | ||
| Childhood Immunization Status – Combination 3 (CIS) | 2 | ✓ | NA | NA | NA | ✓ | 0038 | HEDIS 2022 | P4P |
| Chlamydia Screening in Women (CHL) | ✓ | NA | ✓ | NA | ✓ | 0033 | HEDIS 2022 | P4P | |
| Colorectal Cancer Screening (COL)** | 2 | ✓ | NA | ✓ | ✓ | NA | 0034 | HEDIS 2022 | P4P |
| Controlling High Blood Pressure (CBP)** | 2 | ✓ | NA | ✓ | ✓ | NA | 0018 | HEDIS 2022 | P4P |
| Depression Remission or Response for Adolescents and Adults (DRR) | ✓ | NA | NA | ✓ | ✓ | HEDIS 2022 | P4P | ||
| Diabetes Screening for People with Schizophrenia or Bipolar Disorder Using Antipsychotic Medications (SSD) | ✓ | NA | ✓ | ✓ | NA | 1932 | HEDIS 2022 | P4P | |
| Eye Exam for Patients with Diabetes (EED) | ✓ | NA | ✓ | ✓ | NA | HEDIS 2022 | P4P | ||
| Follow-Up After Emergency Department Visit for Substance Use (FUA) | ✓ | NA | ✓ | NA | NA | 3488 | HEDIS 2022 | P4P | |
| Follow-Up After Emergency Department Visit for Mental Illness (FUM) | ✓ | NA | ✓ | NA | NA | 3489 | HEDIS 2022 | P4P | |
| Follow-Up After High-Intensity Care for Substance Use Disorder (FUI) | ✓ | NA | ✓ | NA | NA | HEDIS 2022 | P4P | ||
| Follow-Up After Hospitalization for Mental Illness (FUH) | ✓ | NA | ✓ | NA | NA | 0576 | HEDIS 2022 | P4P | |
| Hemoglobin A1c Control for Patients With Diabetes (HBD)** | ✓ | NA | ✓ | ✓ | NA | HEDIS 2022 | P4P | ||
| HIV Viral Load Suppression (VLS) | 1 | ✓ | NA | NA | ✓ | NA | 2082 | HRSA | P4P |
| Immunizations for Adolescents - Combination 2 (IMA) | ✓ | NA | NA | NA | ✓ | 1407 | HEDIS 2022 | P4P | |
| Initiation and Engagement of Substance Use Disorder Treatment | ✓ | ✓ | NA | ✓ | NA | 0004 | HEDIS 2022 | P4P | |
| Initiation of Pharmacotherapy upon New Episode of Opioid Dependence | ✓ | NA | ✓ | ✓ | NA | NYS 2022 | P4P | ||
| Kidney Health Evaluation for Patients With Diabetes (KED) | ✓ | NA | ✓ | ✓ | NA | HEDIS 2022 | P4P | ||
| Pharmacotherapy for Opioid Use Disorder (POD) | ✓ | NA | ✓ | CAT 2 | NA | HEDIS 2022 | P4P | ||
| Potentially Preventable Mental Health Related Readmission Rate 30 Days | ✓ | NA | ✓ | NA | NA | NYS 2022 | P4P | ||
| Prenatal and Postpartum Care (PPC)** | ✓ | ✓ | NA | NA | NA | 1517 | HEDIS 2022 | P4P | |
| Well-Child Visits in the First 30 Months of Life (W30) | ✓ | NA | NA | NA | ✓ | HEDIS 2022 | P4P | ||
| Maternity Care | |||||||||
| Contraceptive Care – Postpartum | NA | NR | NA | NA | NA | 2902 | US Office of Population Affairs | P4R | |
| C-Section for Nulliparous Singleton Term Vertex (NSTV) (PC-02) | NA | NR | NA | NA | NA | 0471 | TJC 2019 | P4R | |
| Depression Screening and Follow-Up for Adolescents and Adults (DSF-E) | NA | ✓ | NA | ✓ | ✓ | HEDIS 2022 | P4R | ||
| Exclusively Breast Milk Feeding (PC-05) | NA | NR | NA | NA | NA | 0480 | TJC 2017 | P4R | |
| Incidence of Episiotomy | NA | NR | NA | NA | NA | 0470 | Christiana Care Health System 2019 | P4R | |
| Low Birth Weight [Live births weighing less than 2,500 grams (preterm v. full term)] | NA | NR | NA | NA | NA | 0278 | AHRQ v7.0 | P4R | |
| Percentage of Preterm Births | NA | NR | NA | NA | NA | NYS 2022 Vital Statistics | P4R | ||
| Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention | NA | ✓ | ✓ | ✓ | NA | 0028 | AMA PCPI | P4R | |
| Health and Recovery Program (HARP) | |||||||||
| Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-Up Plan | NA | NA | NR | NR | NA | 0421 | CMS 2020 | P4R | |
| Preventive Care and Screening: Influenza Immunization | NA | NA | ✓ | ✓ | NA | 0041 | AMA PCPI | P4R | |
| Statin Therapy for Patients with Cardiovascular Disease (SPC) | NA | NA | ✓ | ✓ | NA | HEDIS 2022 | P4R | ||
| Use of Pharmacotherapy for Alcohol Abuse or Dependence | NA | NA | ✓ | ✓ | NA | NYS 2022 | P4R | ||
| Use of Spirometry Testing in the Assessment and Diagnosis of COPD (SPR) | NA | NA | ✓ | ✓ | NA | 0577 | HEDIS 2022 | P4R | |
| HIV/AIDS | |||||||||
| Potentially Avoidable Complication (PAC) in Patients with HIV/AIDS | 1 | NA | NA | NA | NA | NR | Altarum Institute | P4R | |
| Sexually Transmitted Infections: Screening for Chlamydia, Gonorrhea, and Syphilis | 1 | NA | NA | NA | NA | NR | NYS 2022 | P4R | |
| CHILDREN | |||||||||
| Annual Dental Visit (ADV) | NA | NA | NA | NA | ✓ | 1388 | HEDIS 2022 | P4R | |
| Asthma Admission Rate [PDI #14] | NR | NA | NA | NA | NR | 0728 | AHRQ v5.0 | P4P | |
| Developmental Screening in the First Three Years of Life | NA | NA | NA | NA | NR | 1448 | Oregon Health & Science University | P4R | |
| Follow–Up Care for Children Prescribed ADHD Medication (ADD)* | NA | NA | NA | NA | ✓ | 0108 | HEDIS 2022 | P4R | |
| Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents (WCC) | 2 | NA | NA | NA | NA | ✓ | 0024 | HEDIS 2022 | P4R |
✓ - Required to Report NA - Not Applicable to the Arrangement Shading - Purple - Not required to be reported
1 - There are no reporting requirements for this measure. NYS will calculate the measure result for MY2022
2 - For measures that you may have reported using the hybrid sample in the PLD for QARR,
we request that you report the administrative denominator and numerator for VBP.
IV. File Specifications - Mainstream VBP
NYS PCMH Scorecard Patient-Level Detail File
Please use your 2022 QARR/HEDIS data warehouse as the source for this information. Do not recalculate or update measure results. However, in addition to the measure elements that you reported for QARR/HEDIS for 2022, please include the provider/practice information that was attributed to the member using your plan's attribution methodology. Several fields regarding the provider and practice site of the service have been added to the layout request for this purpose, specifically two separate fields for TIN: Practice TIN and Contractor TIN. The NYS PCMH data file is modeled after the NYS 2022 Patient-Level Detail file (PLD) that you prepared as part of your QARR submission, and many of the data elements in the NYS PCMH file follow the same definitions and format as used to define the data elements in the PLD. You may find it helpful to use the PLD as a resource or starting point in completing the NYS PCMH file. We ask that you populate the NYS PCMH with all Lines of Business that you serve (e.g., Medicaid). Once completed, please upload the file to IPRO’s FTP site. A subfolder in the “QARR 2022” folder where you will upload your 2022 QARR files entitled “NYS PCMH 2022” will be created for your submission. If someone other than your QARR liaison will be responsible for NYS PCMH reporting, please contact the VBP Team at OQPSVBP@health.ny.gov for access to the FTP site. Please note that the deadline for submission is Friday, July 28, 2023.
Exceptions to the PLD file are noted below:
- The NYS PCMH file requests Medicare HEDIS data, which is not required for QARR reporting.
- The Plan ID is not your plan's QARR ID. The Plan ID field should be populated with the Organization ID that you used to submit the IDSS to NCQA.
- Note that the Organization ID is different from the Submission ID. Submission ID which is specific to a Line of Business.
- The Organization ID provides six digits. If your plan's ID is smaller, please right justify.
- For Medicaid, we are asking that you populate the member’s CIN in the ID field and not an internal ID number, for other products, please use an internally-defined ID number. In order to receive credit for VBP reporting, the Medicaid CIN must be populated for Medicaid members.
- Provider/Practice attribution information is required for NYS PCMH. This information is not required for QARR reporting.
Specific Instructions:
- Please be aware that although the member ID for all products except Medicaid is an internal number assigned by your plan, you will need to link the member to the provider of service. You should use a naming convention that will facilitate this process.
- If a member is reported for a specific measure in more than one product line (e.g., duals), please report the member for only one product, using the following priority: Commercial, then Medicare, then Medicaid. This instruction affects only members who may be reported twice in the same measure.
- A Member ID (Field #3) may be included on the file more than once if the member is in more than one product line during the reporting period.
- For hybrid measures that you reported to NCQA/NYS using the hybrid methodology, which requires calculating the measure based on a sample rather than the entire eligible population, for NYS PCMH only, we are requesting that you report the administrative denominator and administrative numerator (and not the hybrid data), which is populated on the IDSS.
- Members in the file must be in at least one measure.
- Measures that are not applicable to the member should be zero-filled.
- A valid Tax ID (TIN) is nine characters. If the TIN is not available, set the field value to "999999999".
- Practice Name must be populated in the Practice Name (Field #9) only.
- Practice Address Line 1 (Field #10) must contain the street address of the Practice, not the Practice Name.
- For Fields #7-22, leave these fields blank if the member cannot be attributed to any provider and you are not able to identify the provider.
- For Field #21, Populate with valid TINs only. If a member is NOT attributed to a VBP Contractor set to '999999999'.
- Initiation and Engagement of Alcohol and Other Drug Dependence Treatment (IET) has been updated to reflect the episodic language of the measure as a member can have more than one episode that contributes to the denominator and numerator. The IET Engagement numerator (Field #88 and 91) value must be less than or equal to the Initiation numerator (Field #87 and 90) value.
- The ADD Continuation and Maintenance (C&M) Phase denominator (Field #103) and numerator (Field #104) must be less than or equal to the Initiation Phase denominator (Field #101) and numerator (Field #102).
- For the AAB (Field #83) and LBP (Field #85) measures, provide the actual numerator (non-inverted) (e.g., for AAB, the numerator would be members receiving the antibiotic).
- For the AMB measure, please populate the fields with the number of events for each LOB you are reporting. Member Months is not required for 2022.
- For the IPU/AHU/EDU measures, please populate the fields with number of events for each LOB you are reporting. Member Months is not required for 2022.
- The AMR measure has replaced the MMA measure in fields 47-61. For MY2022, the Ratio of controller medications to total asthma medications of 0.75 or greater has been retired. Please zero fill these columns (Field #49, 52, 55, 58, 61). Additionally, the 65-85 years age group has been retired. Please zero fill these columns (Field # 59 and 60).
- For the retired Comprehensive Diabetes Care (CDC), please zero fill field #72, 73, 74, 75, and 76. The CDC measure has been replaced with new measures Hemoglobin A1c Control for Patients with Diabetes (HBD) (field #142 and 143), Eye Exam for Patients with Diabetes (EED) (field #144 and 145), and Kidney Health Evaluation for Patients with Diabetes (KED) (field #146 and 147).
- Only MCOs reporting their Medicaid Line of Business need report the following 8 VBP specific measures: Statin therapy for patients with cardiovascular disease, Use of Spirometry Testing in the Assessment and Diagnosis of COPD, Diabetes Screening for Schizophrenia or Bipolar Disorder Who Are Using Antipsychotic Medications, Initiation of Pharmacotherapy upon New Episode of Opioid Dependence, Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents (Administrative rate), Follow-Up Care for Children Prescribed ADHD Medication, Annual Dental Visits, and Well-Child Visits in the First 30 Months of Life. Medicaid plans submitting NYS PCMH data should add these additional variables to the NYS PCMH file layout and it will count towards the VBP reporting requirements.
For questions regarding this request, please contact the VBP Team of OQPS at: OQPSVBP@health.ny.gov or (518) 486-9012.
Patient Attribution File
The State is asking insurers to provide an attribution file for all members enrolled in a VBP arrangement during the 2022 Calendar Year per the methodology specified in your state-approved contract. The attribution file will be used in combination with other quality measure sources (e.g., 2022 NYS Patient-Level Detail File) to aggregate quality results for the 2022 Category 1 population-specific measures by VBP Contractor.
NOTE: MLTC attribution instructions are different than for other populations. Please follow the instructions in the MLTC attribution file subsection of this manual.
File Format:
Submit a text file that is either: fixed-width (TXT) or comma-separated values (CSV)
Fixed-width TXT files:
- Must have column start/end locations as documented in the following table.
- Data must not include column names. The first row in the file must be data.
- Numeric values should be right justified, and blank filled to the left of the value; text fields should be left-justified, and blank filled to the right of the value. Variable character (VARCHAR) fields should be treated as text.
CSV files:
- Must not have additional columns beyond those shown in the following table. (Refer to companion excel file.)
- Data must include column names. The first row in the file must be the column names as documented in the following table.
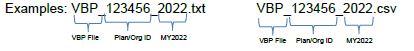
Naming Convention:
The file should be named VBP_PlanID_2022.txt or VBP_PlanID_2022.cvs (Refer to field 1 in table below.)
All files are due no later than Friday, July 28, 2023.
| Element # | Name | Direction | Allowed Values | Data Type | Required/Optional | Length | Start | End |
|---|---|---|---|---|---|---|---|---|
| 1 | Plan_ID# | Organization ID used to submit the IDSS to NCQA. This ID is consistent across all Lines. | ###### | VARCHAR | R | 6 | 1 | 6 |
| 2 | Product_Line | A member's product line at the end of the measurement period. | 1 = MEDICAID 2 = SNP 11 = HARP | NUMBER | R | 2 | 7 | 8 |
| 3 | Unique_Member_ ID# | Medicaid Client ID Number (CIN) *The field is alphanumeric and should be treated as a text field. This field is mandatory - do not leave it blank! | VARCHAR | R | 8 | 9 | 16 | |
| 4 | County_of_ Residence | Enter the 3-digit county FIPS code for each member's county of residence. | ### | NUMBER | R | 3 | 17 | 19 |
| 5 | Zip_Code_of_ Residence | ##### | NUMBER | R | 5 | 20 | 24 | |
| 6 | Practice_Tax_ID# | Populate with valid TINs only. This field is mandatory - do not leave it blank! | ######### | NUMBER | R | 9 | 25 | 33 |
| 7 | PCMH_Site_ID# | PCMH Site ID# - NCQA generated ID | NUMBER | O | 11 | 34 | 44 | |
| 8 | Practice_Site_ID# | Internal plan practice site ID# | VARCHAR | O | 13 | 45 | 57 | |
| 9 | Practice_Name | This field is mandatory - do not leave it blank! | TEXT | R | 50 | 58 | 107 | |
| 10 | Practice_Address_ Line_1 | TEXT | R | 35 | 108 | 142 | ||
| 11 | Practice_Address_ Line_2 | TEXT | O | 35 | 143 | 177 | ||
| 12 | Practice_Address_ Line_3 | TEXT | O | 35 | 178 | 212 | ||
| 13 | Practice_Address_ City | TEXT | R | 25 | 213 | 237 | ||
| 14 | Practice_Address_ State | TEXT | R | 2 | 238 | 239 | ||
| 15 | Practice_Address_ Zip_Code | ##### | NUMBER | R | 5 | 240 | 244 | |
| 16 | Practice_Telephone _Number | ########## | NUMBER | O | 10 | 245 | 254 | |
| 17 | Provider_NPI | National Provider Identifier - 10 Digit ID | ########## | NUMBER | R | 10 | 255 | 264 |
| 18 | Provider_First_ Name | TEXT | R | 15 | 265 | 279 | ||
| 19 | Provider_Middle_ Initial | TEXT | O | 1 | 280 | 280 | ||
| 20 | Provider_Last_ Name | TEXT | R | 35 | 281 | 315 | ||
| 21 | VBP_Contractor_ Tax_ID# | Populate with valid TINs only. Please include the TIN of the VBP Contractor (not the provider) If the member is NOT in a VBP level 1 or higher arrangement set to '999999999'. | ######### | NUMBER | R | 9 | 316 | 324 |
| 22 | VBP_Contractor_ DBA_Name | Enter the DBA name listed on your VBP contract/arrangement. | VARCHAR | R | 50 | 325 | 374 | |
| 23 | VBP_Contractor_ Type | 1 = Provider/ Hospital 2 = IPA 3 = ACO 9 = Unknown | NUMBER | R | 1 | 375 | 375 | |
| 24 | VBP_Arrangement_ Type | Refer to Section C, #2b of the DOH 4255 - Provider Contract Statement and Certification form. | 1 = TCGP 2 = IPC 3 = HARP 4 = HIV/AIDs 5 = Maternity 6 = Children's 7 = Off Menu | NUMBER | R | 1 | 376 | 376 |
| 25 * | DOH_VBP_Contract _ID# | The number provided by DOH in the Agreement approval letter begins with DOH ID ### | #### | NUMBER | R | 4 | 377 | 380 |
| 26 * | MCO_Unique_ Contract_ID# | Plan generated ID used to submit contract to DOH; Section A, #3 of the 4255. | VARCHAR | R | 50 | 381 | 430 | |
| 27 | Prov_Att_start_date | MMDDYYYY - Must be between 1/1/2022 and 12/31/2022 | MMDDYYYY | DATE | R | 8 | 431 | 438 |
| 28 | Prov_Att_end_date | MMDDYYYY - Must be between 1/1/2022 and 12/31/2022 | MMDDYYYY | DATE | R | 8 | 439 | 446 |
| 29 | MBR_Race | Enter the member's race | 1=White 2=Black or African American 3=American Indian/Alaskan Native 4=Asian 5=Native Hawaiian/Pacific Islander 6=Other Race 7=Two or more races 8=Asked but not answered 9=Unknown |
NUMBER | R | 1 | 447 | 447 |
| 30 | MBR_ Ethnicity | Enter the Member's ethnicity | 1=Hispanic or Latino 2=Non-Hispanic or Latino 9=Unknown 0=Asked but not answered |
NUMBER | R | 1 | 448 | 448 |
| Field | Field Name | Description/Specifications |
|---|---|---|
| 1 | Plan_ID# | Enter your Organization ID used to submit the IDSS to NCQA. This ID is consistent across all Lines of Business. |
| 2 | Product_Line | Enter the member's product line at the end of the measurement period. Enter the corresponding number (1) Medicaid, (2) SNP, (11) HARP. |
| 3 | Unique_Member_ID# | Enter member's Medicaid Client Identification Number (CIN). The field should be continuous without any spaces or hyphens. The field is alpha-numeric and should be treated as a text field. This field is mandatory- do not leave it blank! |
| 4 | County_of_Residence | Enter the Federal Information Processing Standard (FIPS) code for the member's county of residence. Please refer to Appendix VII, Table 5 - NYS FIPS Codes by County at the end of this manual for a complete listing of NYS FIPS codes. |
| 5 | Zip_Code_of_Residence | Enter the 5-digit zip code of the member's residence. |
| 6 | Practice_Tax_ID# | Enter the 9-digit Federally assigned Tax Identification Number for the Practice of the member's provider. Populate with valid TINs only. This field is mandatory - do not leave it blank! |
| 7 | PCMH_Site_ID# | Enter the NCQA assigned number associated with your Patient-Centered Medical Home (PCMH.) |
| 8 | Practice_Site_ID# | Enter your internal site ID assigned by the plan. |
| 9 | Practice_Name | Enter the complete name of the provider's practice. This field is required, do not leave blank. |
| 10 11 12 | Practice_Address_Line_1 Practice_Address_Line_2 Practice_Address_Line_3 | Enter the physical address of the practice location. (Enter up to 3 lines) |
| 13 | Practice_Address_City | Enter the city in which the practice is located. |
| 14 | Practice_Address_State | Enter the 2-digit abbreviation for the state in which the practice is located. |
| 15 | Practice_Address_Zip_Code | Enter the 5-digit zip code in which the practice is located. |
| 16 | Practice_Telephone_Number | Enter the practice's main phone line, it should be in the format of ########## with no intervening "-". |
| 17 | Provider_NPI | This is the unique 10-digit National Provider Identifier (NPI) of the provider the member was serviced by during the reporting period. This should be a provider organization that had frequent contact with the member and, therefore, could potentially affect the need for hospitalization or not. A member may be serviced by multiple providers during the same time period (provide one row of data for every provider a member was serviced by). |
| 18 | Provider_First_Name | Enter the provider full first name |
| 19 | Provider_Middle_Initial | Enter the provider's middle initial. |
| 20 | Provider_Last_Name | Enter the provider's last name. |
| 21 | VBP_Contractor_Tax_ID# | This is the unique 9-digit tax identification number of the VBP Contractor (not the provider) that the member is assigned to a Level 1 or higher VBP arrangement during the reporting period. A member can only be assigned to one VBP contractor at a time. If not applicable, fill with 999999999. |
| 22 | VBP_Contractor_DBA_Name | The "Doing Business As" (DBA) name is the operating name of a company, as opposed to the legal name of the company. The VBP Contractor may be an ACO, IPA, individual provider, or hospital. |
| 23 | VBP_Contractor_Type | In this field, enter '1' if the contractor is a provider (provider includes hospitals), '2' if the contractor is an IPA, '3' if the contractor is an ACO, '9' if Unknown |
| 24 | VBP_Arrangement_Type | In this field, enter "1" if the VBP arrangement type is a TCGP arrangement, "2" if it is an IPC arrangement, "3" if it is a HARP arrangement, "4" if it is an HIV/AIDs arrangement, "5" if it is a Maternity arrangement, "6" if it is a Children's arrangement, "7"an Off-Menu arrangement. This information can be found in Section C, #2b of the DOH 4255 - Provider Contract Statement and Certification form. |
| 25 * | DOH_VBP_Contract_ID# | This is the number provided by DOH in the Agreement approval letter for your VBP arrangement, it begins with DOH ID ####. * You must populate either field 25 or 26, preferably both fields should be populated. If you need assistance obtaining your correct DOH VBP Contract Identifier, please email NYS DOH VBP mailbox at OQPSVBP@health.ny.gov |
| 26 * | MCO_Unique_Contract_ID# | This is the contract identifier created by your plan, which is a required component of all contracts submitted for review (it can be found in Section A, #3 of the DOH 4255, it is also typically in the footer of your contract documents. * You must populate either field 25 or 26, preferably both fields should be populated. If you need assistance obtaining your correct MCO Unique Contract Identifier, please email NYS DOH VBP mailbox at OQPSVBP@health.ny.gov |
| 27 | Prov_Att_start_date | This is the attribution start date with the provider when the member was first attributed to the provider. This date must be during the reporting period. It should be in the format of MMDDYYYY with no intervening "-" or "/". The format is the same if data is submitted via a fixed-width file or CSV. |
| 28 | Prov_Att_end_date | This is the attribution end date with the provider when the member was last attributed to the provider. This date must be during the reporting period. It should be in the format of MMDDYYYY with no intervening "-" or "/". The format is the same if data is submitted via a fixed-width file or CSV. |
| 29 | MBR_Race | Enter the member's race (either obtained by direct or indirect methods). Enter a value of '1' for White, '2' for Black or African American, '3' for AMerican Indian/Alaskan Native, '4' for Asian, '5' for Native Hawaiian/Pacific Islander, '6' for Other Race, '7' for Two or more races, '8' for Asked but not answered, or '9' for Unknown. This field is required and cannot be left blank. |
| 30 | MBR_Ethnicity | Enter the member's ethnicity (either obtained by direct or indirect methods). Enter a value of '1' for Hispanic or Latino, '2' for Non-Hispanic or Latino, '9' for Unknown, or '0' for Asked but not answered. This field is required and cannot be left blank. |
Submission Examples and Data Requirements Checklist
Please refer to section VII Appendix, Table 6 at the end of this manual, for layout examples of both TXT and CSV files.
Please refer to section VII Appendix, Table 7 at the end of this manual, for attribution file checklists for the MCO attribution file. The checklist is designed to ensure fields in the attribution file are standardized appropriately and are not required to be submitted with the attribution files.
File Submission:
Files for all arrangement types are to be submitted to the New York State Department of Health via the Secure File Transfer 2.0 of the Health Commerce System (HCS). Files should be submitted to OQPS VBP Evaluation or OQPSVBP@health.ny.gov via HCS.
Files must be received electronically by 11:59 p.m. ET; Friday, July 28, 2023.
|top of section| |table of contents|REPORTING GUIDELINES VBP MLTC
V. Reporting Guidelines VBP MLTC
INTRODUCTION
The State is requesting insurers to submit a Patient Attribution file, which will be used to create aggregated quality results by Provider or VBP Contractor. DOH will calculate all reportable Category 1 quality measure results for the arrangements. The attribution methodology and Patient Attribution file layout are included in Section VI of this document.
- Table 2: 2023 MLTC VBP List of Required Measures
- Lists, by arrangement, the 2023 MLTC VBP Category 1 Measure set and indicates the 2023 measures required for reporting.
Measure Changes
Changes to the Reporting Requirements for 2023 Measure Sets were made based on the feedback received by the DOH from the Clinical Advisory Groups, Measure Support Task Force and Sub-teams, and from other stakeholder groups. Those changes are indicated below. In instances where a measure was moved from Category 1 in MY2022 to Category 2 in MY2023 or removed entirely, the State will not require reporting of the data related to those measures.
MLTC:
Category 1: Change
- The following measures for MY2023 have been readded to the MLTC measure set:
- Percentage of members who remained stable or demonstrated improvement in pain intensity
- Percentage of members who remained stable or demonstrated improvement in Nursing Facility Level of Care (NFLOC) score
- Percentage of members who remained stable or demonstrated improvement in urinary continence
- Percentage of members who remained stable or demonstrated improvement in shortness of breath
Category 2: Change
- No Changes
Table 2: 2023 MLTC VBP List of Required Measures
| Measures | Notes | Arrangement Type | NQF ID | Specifications | Class |
|---|---|---|---|---|---|
| MLTC | |||||
| Managed Long-Term Care (MLTC) | |||||
| Percentage of members who did not have an emergency room visit in the last 90 days | 1 | ✓ | NYS 2023 | P4P | |
| Percentage of members who did not experience falls that resulted in major or minor injury in the last 90 days | 1 | ✓ | NYS 2023 | P4P | |
| Percentage of members who received an influenza vaccination in the last year | 1 | ✓ | NYS 2023 | P4P | |
| Percentage of members who did not experience uncontrolled pain | 1 | ✓ | NYS 2023 | P4P | |
| Percentage of members who were not lonely or were not distressed | 1 | ✓ | NYS 2023 | P4P | |
| Potentially Avoidable Hospitalizations (PAH) for a primary diagnosis of heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infection | 1, 2 | ✓ | NYS 2023 | P4P | |
✓ - Required to Report NA - Not Applicable to the Arrangement Shading - Purple - Not required to be reported
1 - There are no reporting requirements for this measure. NYS will calculate the measure result for MY2022/2023
2 - NYS will calculate this measure for the community-based providers.
VI. File Specifications - VBP MLTC
MLTC Attribution File
For MY2022, P4P Category 1 measures for the MLTC arrangement will be computed by DOH to reduce the burden on the MTLC plans. With the Public Health Emergency due to COVID, Community Health Assessment (CHA) based measure calculation will resume in MY 2022. Due to the COVID-19 public health emergency, the calculation of the MLTC VBP Category 1 measures, except for the Potentially Avoidable Hospitalization (PAH) measure, was not possible for MY2021. Calculation of rates for PAH and other Category 1 measures (except for the stable/improved over-time measures) will resume for MY2022. The other VBP Category 1 stable/improved over-time measures can be included in contracts starting in MY2023 and the DOH will resume calculating results for all P4P Category 1 measures.
Note - Starting with MY 2022, quality measures will only be calculated on an annual basis (e.g., MY2022 will reflect measurement period of January 1st - December 31st, 2022). Results will be distributed in Q3 of the following year (October 2023 for MY2022 results).
Attribution Methodology:
MAP/PACE: Plan enrollees who have four or more months of continuous enrollment from April 2022 through June 2023 should be submitted in this attribution file. This attribution should be to provider organizations of CHHA, LHCSA, and, VBP contractor (if applicable) which had the most frequent contact with the member and, therefore, could potentially affect quality measures. Services being received by the member through Consumer Directed Personal Assistance (CDPAS) should not be included in this attribution file.
Changes to the NYS Long-Term Care VBP Initiative for 2021 and forward: MLTC Partial plans have been phased out of VBP as a result of the enacted SFY 2022-21 Budget. Plans are encouraged to continue to submit VBP arrangements for MAP and PACE consistent with standards outlined in the VBP Roadmap and the Provider Contract Guidelines for Article 44 MCOs, IPAs, and ACOs. Please note, MLTC Partial plans are not required to submit VBP attribution data beginning in 2022. As a result, Partial plans will not receive any attributed provider results or be included in the statewide denominator of any Category 1 P4P measures calculated by DOH.
File Format:
- Include only members who had 4 months or more continuous enrollment in an MLTC plan from April 2022 through June 2023.
- For each member from step 1, list all provider organization(s) that provided at least one service per month, for 4 or more continuous months from April 2022 through June 2023. The data should be formatted in a long form containing one row of data for each member/provider combination. Please provide at least one row of data for every provider a member was serviced by (see Examples 1 and 2 below). If a member does not have any providers from which they received 4 or more continuous months of care, THE MEMBER SHOULD NOT BE LISTED.
- The text file must be either: 1) fixed width and named PROVIDERS_MLTC.TXT, or 2) comma-separated values (CSV) and named PROVIDERS_MLTC.CSV.
- Fixed-width files
- Must have column start/end locations as documented in the following table.
- Data must not include column names. The first row in the file must be data.
- CSV files
- Must not have additional columns beyond those shown in the following table.
- Data must include column names. The first row in the file must be the column names as documented in the following table.
- Fixed-width files
- The following table provides instructions on the submission of member-level data.
# Field Name Data Type Length Start Colum End Column Details/Comments 1 CIN Varchar 8 1 8 A Participant's Medicaid client identification number. The field should be continuous without any spaces or hyphens. The field is alpha-numeric and should be treated as a text field. This field may not be NULL 2 MMIS_ID Varchar 8 9 16 The MLTC Plan's numeric eight-digit ID. This field may not be NULL. 3 Prov_NPI Varchar 10 17 26 The unique 10-digit National Provider Identifier (NPI) for the provider the member was serviced by during the reporting period. 4 Prov_start_ date Date 8 27 34 MMDDYYYY - Must be between April 2022 - June 2023 5 Prov_end_date Date 8 35 42 MMDDYYYY - Must be between April 2022 - June 2023 6 Contractor_TIN Varchar 9 43 51 The unique 9-digit tax identification number of the VBP Contractor. Only submit the TIN, if this member is included in a level 2 or higher arrangement with a VBP Contractor. If not applicable or level 1 arrangement, fill with 999999999. 7 Contractor_Type Varchar 1 52 52 1= CHHA, LHCSA, 2= IPA, 3= Hospital, 4= ACO, 8= Other, and 9 = NA. Only submit if this member is included in a level 2 or higher arrangement with a VBP Contractor. If not applicable or level 1 arrangement, fill 9 = NA. 8* DOH_VBP_ Contract_# Number 4 53 56 The number provided by DOH in the Agreement approval letter begins with DOH ID ###. *You must populate either field 8 or 9, preferably both fields should be populated. 9* MCO_Unique_ Contract_ID# Varchar 50 57 107 Plan generated ID used to submit contract to DOH; Section A, #3 of the 4255. *You must populate either field 8 or 9, preferably both.
Field Definitions:
Prov_NPI: This is the unique 10-digit National Provider Identifier (NPI) of the provider the member was serviced by during the reporting period. This should be a provider organization that had frequent contact with the member and, therefore, could potentially affect the need for hospitalization or not. A member may be serviced by multiple providers during the same time period (provide one row of data for every provider a member was serviced by).
Prov_start_date: This is the service start date with the provider. This date must be during the reporting period. It should be in the format of MMDDYYYY with no intervening "-" or "/". The format is the same if data is submitted via a fixed-width file or CSV.
Prov_end_date: This is the service end date with the provider. This date must be during the reporting period. It should be in the format of MMDDYYYY with no intervening "-" or "/". The format is the same if data is submitted via a fixed-width file or CSV.
Contractor TIN: This is the unique 9-digit tax identification number of the VBP Contractor (not the provider) that the member is assigned to for a Level 2 arrangement during the reporting period. A member can only be assigned to one level 2 or higher VBP contractor at a time. If not applicable or level 1, fill with 999999999.
Contractor_Type: The VBP Contractor may be an ACO, IPA, hospital, or large LHCSA/CHHA that is coordinating services for many LHCSAs or CHHAs. This field is for the VBP Contractor (not the provider) that the member is assigned to a level 2 or higher arrangement during the reporting period. A member can only be assigned to one level 2 or higher VBP contractor at a time. If not applicable or level 1 arrangement, fill with 9.
* DOH_VBP_Contract_#: This is the number provided by DOH in the Agreement approval letter for your VBP arrangement, it begins with DOH ID ####.
* MCO_Unique_Contract_ID#: This is the contract identifier created by your plan, which is a required component of all contracts submitted for review (it can be found in Section A, #3 of the DOH 4255, it is also typically in the footer of your contract documents.
*You must populate either field 8 or 9, preferably both fields should be populated.
Data Requirements Checklist
Please refer to section VII Appendix, Table 8 at the end of this manual, for attribution file checklists for the MLTC attribution file. The checklist is designed to ensure fields in the attribution file are standardized appropriately and are not required to be submitted with the attribution files.
File Submission:
Files are to be submitted to the New York State Department of Health via the Secure File Transfer 2.0 of the Health Commerce System. Files should be submitted to OQPS MLTC Evaluation mailbox. Files are to be submitted by close of business on Friday, July 28, 2023.
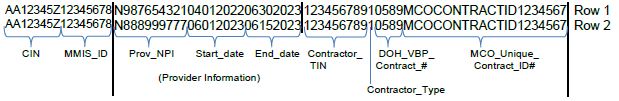
NOTE: When a Provider/NPI has overlapping service dates for a member, the service dates should be collapsed into one record with the earliest start date and furthest end date. Multiple rows for the same member/provider may be provided only if the provider/NPI has nonoverlapping service dates and each time frame meets the 4 months of service criterion. (see Example 3 below).
Submission Examples:
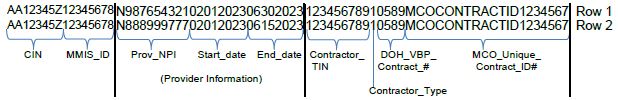
Example 1 and 2 below illustrate two different providers, with overlapping service dates, adding a single member from February through June 2023.
Example 1 not covered by level 2 or higher VBP contract:
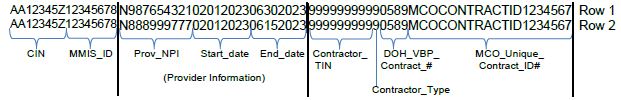
Example 2 covered by level 2 or higher VBP contract:
Example 3 below illustrates a member who was continuously enrolled for 4 or more months in the health plan and received at least one service per month from the same provider organization for 4 or more continuous months, for two separate non-overlapping time periods and is covered by level 2 or higher VBP contract during April 2022 through June 2023.
Fully Capitated Plans:
Because the HEDIS and CMS-based P4R category 1 measures cannot be calculated by the State, plans must calculate and report Plan/Provider-VBP Contractor performance to the State by July 28, 2023. Files are to be submitted to the New York State Department of Health via the Secure File Transfer 2.0 of the Health Commerce System. Files should be submitted to the OQPS MLTC Evaluation mailbox.
Plans should submit an Excel file with the following format. Submit a row for each measure being reported. Plans are required to report on all measures for each plan-provider combination.
| # | Field Name * | Data Type | Excel Column Placement | Details/Comments |
|---|---|---|---|---|
| 1 | MMIS_ID | Varchar | Column A | The MLTC Plan's numeric eight-digit ID. This field may not be NULL. |
| 2* | Prov_NPI | Varchar | Column B | The unique 10-digit National Provider Identifier (NPI) for the provider the member was serviced by during the reporting period. This field may not be NULL. |
| 3 | Measure ID | Varchar | Column C | Use the measure ID from the table below |
| 4 | Denominator for Measure | Varchar | Column D | Report the total number of members included in the denominator for the given measure |
| 5 | Numerator for Measure | Varchar | Column E | Report the total number of members that were included in the numerator for the given measure |
| 6 | Exclusions for Measure | Varchar | Column F | Report the number of members excluded from the given measure |
| 7 | Rate for Measure | Varchar | Column G | Report the rate to the hundredth decimal place |
| 8* | Contractor_TIN | Varchar | Column H | The unique 9-digit tax identification number of the VBP Contractor. Only submit the TIN, if this member is included in a level 2 or higher arrangement with a VBP Contractor. If not applicable or level 1 arrangement, fill with 999999999. |
| 9* | Contractor_Type | Varchar | Column I | 1= CHHA, LHCSA, 2= IPA, 3= Hospital, 4= ACO, 8= Other, and 9= NA. Only submit if this member is included in a level 2 or higher arrangement with a VBP Contractor. If not applicable or level 1 arrangement, fill 9 = NA. |
| 10 * | DOH_VBP_ Contract_# | Varchar | Column J | The number provided by DOH in the Agreement approval letter begins with DOH ID ####. *You must populate either field 10 or 11, preferably both. |
| 11 * | MCO_Unique_ Contract_ID# | Varchar | Column K | Plan generated ID used to submit the contract to DOH; Section A, #3 of the 4255. *You must populate either field 10 or 11, preferably both. |
| * See Field Definitions (page 29) under preceding MLTC Attribution File specifications | ||||
| Measure Name | Measure ID |
|---|---|
| MAP P4R measures (Measure Source/ Steward: NCQA/ HEDIS) | |
| Antidepressant Medication Management - Effective Acute Phase Treatment* | 1 |
| Antidepressant Medication Management - Effective Continuation Phase Treatment* | 2 |
| Colorectal Cancer Screening* | 3 |
| Eye Exam for Patients with Diabetes*,1 | 4 |
| Kidney Health Evaluation for Patients with Diabetes (KED)* | 5 |
| Follow-up After Hospitalization for Mental Illness - 7 Days^ | 6 |
| Follow-up After Hospitalization for Mental Illness - 30 Days^ | 7 |
| Initiation of Substance Use Disorder Treatment*,2 | 8 |
| PACE P4R measures (Measure Source/ Steward: CMS) | |
| PACE Participant Emergency Department Utilization Without Hospitalization | 9 |
| Percentage of Participants Not in Nursing Homes | 10 |
| Percentage of Participants with an Annual Review of Their Advance Directive or Surrogate Decision-Maker AND Percentage of Participants with an Annual Review of Their Advance Directive or Surrogate Decision-Maker | 11 |
| * Included in the TCGP measure set ^ Included in the Health and Recovery Plan (HARP) measure set 1. Replacement HEDIS measure 2. Measure specifications/name revised by NCQA/NYS for 2022 HEDIS Measure set |
|
VII. APPENDIX
TABLE 3: 2023 MAINSTREAM VBP LIST OF CATEGORY 2 MEASURES
| Measures | Notes | Arrangement Type | NQF ID | Measure Steward | ||||
|---|---|---|---|---|---|---|---|---|
| TCGP | Maternity | HARP | HIV/AIDS | Children | ||||
| Maternity Care | ||||||||
| Antenatal Steroids PC-03 | NA | Cat 2 | NA | NA | NA | 0476 | TJC | |
| Appropriate DVT Prophylaxis in Women Undergoing Cesarean Delivery | NA | Cat 2 | NA | NA | NA | 0473 | Hospital Corporation of America | |
| Experience of Mother with Pregnancy Care | NA | Cat 2 | NA | NA | NA | TBD | ||
| Hepatitis B Vaccine Coverage Among All Live Newborn Infants Prior to Hospital or Birthing Facility Discharge | NA | Cat 2 | NA | NA | NA | 0475 | Centers for Disease Control and Prevention | |
| Intrapartum Antibiotic Prophylaxis for Group B Streptococcus (GBS) | NA | Cat 2 | NA | NA | NA | 1746 | Massachusetts General Hospital | |
| Prenatal Depression Screening and Follow-Up | NA | Cat 2 | NA | NA | NA | NCQA | ||
| Postpartum Blood Pressure Monitoring | NA | Cat 2 | NA | NA | NA | Texas Maternity Bundle | ||
| Postpartum Depression Screening and Follow- Up | NA | Cat 2 | NA | NA | NA | NCQA | ||
| Vaginal Birth After Cesarean (VBAC) Delivery Rate, Uncomplicated | NA | Cat 2 | NA | NA | NA | NYS 2022 | ||
| Behavioral Health/HARP | ||||||||
| Adherence to Mood Stabilizers for Individuals with Bipolar I Disorder | NA | NA | Cat 2 | NA | NA | 1880 | CMS | |
| Asthma Action Plan | NA | NA | Cat 2 | Cat 2 | NA | AAAAI | ||
| Asthma: Assessment of Asthma Control – Ambulatory Care Setting | NA | NA | Cat 2 | Cat 2 | NA | AAAAI | ||
| Asthma: Lung Function/Spirometry Evaluation | NA | NA | Cat 2 | Cat 2 | NA | AAAAI | ||
| Continuing Engagement in Treatment (CET) Alcohol and Other Drug Dependence | NA | NA | Cat 2 | Cat 2 | NA | NYS TBD | ||
| Mental Health Engagement in Care – 30 Days | NA | NA | Cat 2 | NA | NA | NYS 2022 | ||
| Percentage of HARP Enrolled Members Who Received Personalized Recovery Oriented Services (PROS) or Home and Community- Based Services (HCBS) | NA | NA | Cat 2 | NA | NA | NYS 2022 | ||
| Use of Pharmacotherapy for Opioid Dependence | NA | NA | Cat 2 | Cat 2 | NA | NYS 2022 | ||
| HIV/AIDS | ||||||||
| Continuity of Care from Inpatient Detox to Lower Level of Care | NA | NA | NA | Cat 2 | NA | NYS 2022 | ||
| Continuity of Care from Inpatient Rehabilitation for Alcohol and Other Drug Abuse or Dependence Treatment to Lower Level of Care | NA | NA | NA | Cat 2 | NA | NYS 2022 | ||
| Diabetes Screening (HIV/AIDS) | NA | NA | NA | Cat 2 | NA | NYS DOH AIDS Institute | ||
| Hepatitis C Screening | NA | NA | NA | Cat 2 | NA | HRSA | ||
| Home Management Plan of Care (HMPC) Document Given to Patient/Caregiver (asthma) | NA | NA | NA | Cat 2 | NA | 0338 | The Joint Commission | |
| Housing Status | NA | NA | NA | Cat 2 | NA | HRSA | ||
| Linkage to HIV Medical Care | NA | NA | NA | Cat 2 | NA | NYS 2022 | ||
| Continuity of Pharmacotherapy for Opioid Use Disorder (POD) | NA | NA | NA | Cat 2 | NA | 3175 | NCQA | |
| Prescription of HIV Antiretroviral Therapy | NA | NA | NA | Cat 2 | NA | HRSA | ||
| Sexual History Taking: Anal, Oral, and Genital | NA | NA | NA | Cat 2 | NA | NYS DOH AIDS Institute | ||
| Substance Abuse Screening | NA | NA | NA | Cat 2 | NA | HRSA | ||
| Children | ||||||||
| Follow-up After Emergency Department Visit for Substance Use (FUA) | – | Cat 1 | NA | NA | Cat 2 | NA | 3488 | HEDIS 2022 |
| Follow-up After Emergency Department Visit for Mental Illness (FUM) | – | Cat 2 | NA | NA | Cat 3 | NA | 3489 | HEDIS 2022 |
| Maternal Depression Screening | NA | NA | NA | NA | Cat 2 | 1401 | HEDIS 2022 | |
| Screening for Reduced Visual Acuity and Referral in Children | NA | NA | NA | NA | Cat 2 | 2721 | CMS | |
| Topical Fluoride for Children | NA | NA | NA | NA | Cat 2 | 2528 | American Dental Association | |
| Use of First-Line Psychosocial Care for Children and Adolescents on Antipsychotics | NA | NA | NA | NA | Cat 2 | 2801 | HEDIS 2022 | |
TABLE 4. 2023 VBP MLTC CATEGORY 2 MEASURES
| Measures | Notes | Arrangement Type | Measure source/Steward |
|---|---|---|---|
| MLTC | |||
| Care for Older Adults - Medication Review | Cat 2 | NCQA | |
| Use of High-Risk Medications in the Elderly | Cat 2 | NCQA | |
| Percentage of members who rated the quality of home health aide or personal care aide services within the last 6 months as good or excellent | 1 | Cat 2 | MLTC Survey/New York State |
| Percentage of members who responded that they were usually or always involved in making decisions about their plan of care | 1 | Cat 2 | MLTC Survey/New York State |
| Percentage of members who reported that within the last 6 months the home health aide or personal care aide services were always or usually on time | 1 | Cat 2 | MLTC Survey/New York State |
- Included in the NYS DOH MLTC Quality Incentive measure set
TABLE 5 - NYS FIPS CODES BY COUNTY
| County Name | FIPS Code | County Name | FIPS Code | County Name | FIPS Code |
|---|---|---|---|---|---|
| Albany | 001 | Jefferson | 045 | Saratoga | 091 |
| Allegany | 003 | Kings | 047 | Schenectady | 093 |
| Bronx | 005 | Lewis | 049 | Schoharie | 095 |
| Broome | 007 | Livingston | 051 | Schuyler | 097 |
| Cattaraugus | 009 | Madison | 053 | Seneca | 099 |
| Cayuga | 011 | Monroe | 055 | St. Lawrence | 099 |
| Chautauqua | 013 | Montgomery | 057 | Steuben | 101 |
| Chemung | 015 | Nassau | 059 | Suffolk | 103 |
| Chenango | 017 | New York | 061 | Sullivan | 105 |
| Clinton | 019 | Niagara | 063 | Tioga | 107 |
| Columbia | 021 | Oneida | 065 | Tompkins | 109 |
| Cortland | 023 | Onondaga | 067 | Ulster | 111 |
| Delaware | 025 | Ontario | 069 | Warren | 113 |
| Dutchess | 027 | Orange | 071 | Washington | 115 |
| Erie | 029 | Orleans | 073 | Wayne | 117 |
| Essex | 031 | Oswego | 075 | Westchester | 119 |
| Franklin | 033 | Otsego | 077 | Wyoming | 121 |
| Fulton | 035 | Putnam | 079 | Yates | 123 |
| Genesee | 037 | Queens | 081 | Out of State | 000 |
| Greene | 039 | Rensselaer | 083 | Unknown/Missing | 999 |
| Hamilton | 041 | Richmond | 085 | ||
| Herkimer | 043 | Rockland | 087 |
TABLE 6: SUBMISSION EXAMPLES
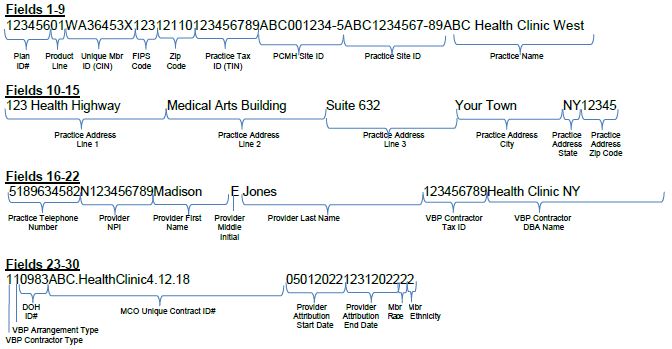
The example below illustrates one member attributed to two different providers, in the same VBP arrangement, within the reporting period submitted as a fixed-width TXT file.
Member Data, attributed to Provider 1 from 1/1/2022 to 04/30/2022
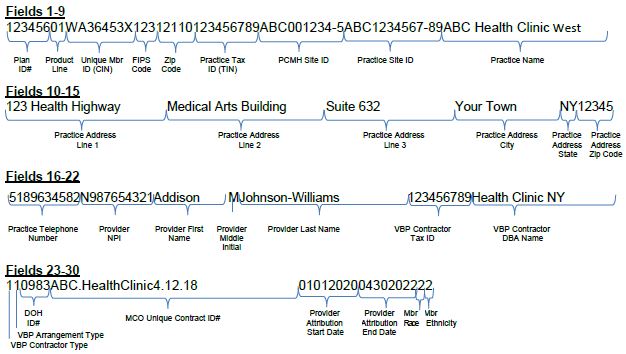
Member Data, attributed to Provider 2 from 5/1/2022 to 12/31/2022
The example below illustrates one member's data submitted as a CSV file.
Fields 1-9:
| Plan ID# | Product Line | Member ID (CIN) | FIPS Code | Zip Code | Practice Tax ID (TIN) | PCMH Site ID | Practice Site ID | Practice Name |
|---|---|---|---|---|---|---|---|---|
| 123456 | 01 | WA12345X | 123 | 12110 | 123456789 | ABC001234-5 | ABC1234567-89 | ABC Health Clinic West |
Fields 10-16:
| Practice Address Line 1 | Practice Address Line 2 | Practice Address Line 3 | Practice Address City | Practice Address State | Practice Address Zip Code | Practice Telephone Number |
|---|---|---|---|---|---|---|
| 123 Health Highway | Medical Arts Building | Suite 632 | Your Town | NY | 12345 | 5189634582 |
Fields 17-23:
| Provider NPI | Provider First Name | Provider Middle Initial | Provider Last Name | VBP Contractor Tax ID# | VBP Contractor DBA Name | VBP Contractor Type |
|---|---|---|---|---|---|---|
| N987654321 | Addison | M | Johnson-Williams | 123456789 | Health Clinic NY | 1 |
Fields 24-30:
| VBP Arrangement Type | DOH VBP Contract ID | MCO Unique Contract ID# | Provider Attribution Start Date | Provider Attribution End Date |
|---|---|---|---|---|
| 1 | 0983 | ABC.HealthClinic4.12.18 | 01/01/2022 | 12/31/2022 |
TABLE 7: MCO ATTRIBUTION FILE - DATA QUALITY CHECKLIST
| Data Quality Check | Value | Notes |
|---|---|---|
| Value used for Plan_ID# is the Organization ID used to submit IDSSto NCQA | ☐ Yes ☐ No |
|
| Every record includes a valid Medicaid Client Identification Number (CIN) | ☐ Yes ☐ No |
The field is alpha-numeric and must be a valid CIN. Do not use internal organization member identification numbers. This field is mandatory for every record. |
| Total number of records submitted | ||
| Number of unique members included in file | ||
| Number of unique members by product line | MC (1) = SNP (2) = HARP (2)= |
|
| All records include a valid Practice_Tax_ID# | ☐ Yes ☐ No |
This field is mandatory for every record. |
| All records include a valid Practice_Name | ☐ Yes ☐ No |
This field is mandatory for every record. |
| All records include a valid VBP_Contractor_Tax_ID# (if the member is not in a VBP level 1 or higher then the value is set to '999999999') | ☐ Yes ☐ No |
This field is mandatory for every record. |
| For members in a VBP level 1 or higher arrangement, the VBP_Contractor_Tax_ID# represents the higher umbrella Tax ID # of the Contractor organization | ☐ Yes ☐ No |
|
| All records include a valid VBP_Contractor_DBA_Name (if the member is not in a VBP level 1 or higher than the value is set to '999999999') | ☐ Yes ☐ No |
This field is mandatory for every record. |
| Number of members assigned toeach VBP_Contractor_Type | Provider/Hospital (1) = IPA (2) = ACO (3) = Unknown (9)= |
|
| Number of members in each VBP_Arrangement_Type | TCGP (1) = IPC (2) = HARP (3) = HIV/AIDs (4) = Maternity (5) = Children's (6) = Off Menu (7) = |
|
| Every record includes either a valid DOH_VBP_Contract_ID# OR a valid MCO_Unique_Contract_ID# | ☐ Yes ☐ No |
You must populate either the DOH_VBP_Contract_ID# field or the MCO_Unique_Contract_ID# field. Preferably both fields should be populated. If you need assistance obtaining your correct DOH VBP Contract Identifier, please email NYS DOH VBP mailbox at OQPSVBP@health.ny.gov |
TABLE 8: MLTC ATTRIBUTION FILE - DATA QUALITY CHECKLIST
| Data Quality Check | Value | Notes |
|---|---|---|
| Value used for MMIS_ID is the MLTC Plan's numeric eight-digit ID. | ☐ Yes ☐ No |
This field is mandatory for every record. |
| Every record includes a valid Medicaid Client Identification Number (CIN) | ☐ Yes ☐ No |
The field is alpha-numeric and must be a valid CIN. Do not use internal organization member identification numbers. This field is mandatory for every record. |
| Total number of records submitted | ||
| Number of unique members included in file | ||
| All records include a valid Prov_NPI number | ☐ Yes ☐ No |
The Prov_NPI is the unique 10-digit National Provider Identifier (NPI) for the provider the member was serviced by during the reporting period This field is mandatory for every record. |
| All records include a valid VBP_Contractor_Tax_ID# (if member is not in a VBP level 1 or higher, set the value to '999999999') | ☐ Yes ☐ No |
This field is mandatory for every record. |
| All records include a valid VBP_Contractor_DBA_Name (if member is not in a VBP level 1 or higher then the value is set to '999999999') | ☐ Yes ☐ No |
This field is mandatory for every record. |
| Number of members assigned to each VBP_Contractor_Type | CHHA, LHCSA (1) = IPA (2) = Hospital (3) = ACO (4) = Other (8) = NA (9) = |
|
| Every record includes either a valid DOH_VBP_Contract_# OR a valid MCO_Unique_Contract_ID# | ☐ Yes ☐ No |
You must populate either the DOH_VBP_Contract_ID# field or the MCO_Unique_Contract_ID# field. Preferably both fields should be populated. If you need assistance obtaining your correct DOH VBP Contract Identifier, please email NYS DOH MLTC VBP mailbox at mltcvbp@health.ny.gov |
| All members are assigned to only one Level 2 (or higher) VBP Contractor at a time | ☐ Yes ☐ No |
_________________________________
1. NYS Department of Health Updated VBP Roadmap Executive Summary - May 2022 1
2. HEDIS® is a registered trademark of the National Committee for Quality Assurance2
Follow Us