July 2010 Volume 26, Number 9
New York State Medicaid Update
The official newsletter of the New York Medicaid Program
David A. Paterson, Governor
State of New York
Richard F. Daines, M.D. Commissioner
New York State DOH
Donna J. Frescatore, Medicaid Director & Deputy Commissioner
Office of Health Insurance Programs

In this issue....
POLICY AND BILLING GUIDANCE
Mandatory Managed Care for Beneficiaries with HIV/AIDS in New York City
Guidelines to Receive Medical Home Statewide Incentive Payments from Medicaid
Expanded Coverage of Telemedicine Specialist Consultations
Assistance for Pregnant Women Choosing a Medicaid Managed Care Plan
Reimbursement for Sterilization Procedure During Delivery for Fidelis Enrollees
UPDATE: Adult Day Health Care Transportation Methodology
Obstetrical Care Practitioner Billing Policy Update and Clarification
PHARMACY UDATES
Over-the-Counter Chelation Therapy Agents
Lead Poisoning Prevention Program Regional Lead Centers
Medicaid Pharmacy Prior Authorization Update
Early Fill Edit Update
Automatic Refills Update
Medicaid Offers Electronic Funds Transfer (EFT)
ALL PROVIDERS
Smoking Cessation Advertisement
Provider Directory
ATTENTION TRANSPORTATION PROVIDERS:
The Medicaid Transportation Policy Unit has changed its phone number to (518) 473-2160.
Mandatory Managed Care
for Beneficiaries with
HIV/AIDS in New York City
Health Plans and Medicaid
Return to Table of Contents
Effective September 1, 2010, Medicaid beneficiaries with HIV/AIDS who live in New York City and are not otherwise excluded will be required to enroll in a managed care plan. Individuals whose HIV/AIDS status is their only reason for exemption must enroll in Medicaid managed care unless they are eligible for another exemption (e.g., homelessness). Beneficiaries that need to enroll or request an exemption should contact Medicaid CHOICE at (800) 505-5678.
Managed Care Plan Enrollment: Mandatory enrollment mailings for current Medicaid beneficiaries will be phased-in by borough, beginning with Brooklyn. Beneficiaries with HIV/AIDS who receive a mandatory enrollment mailing must choose to enroll in a mainstream managed care plan or one of three HIV Special Needs Plans (SNPs) within the choice period specified in the mailing. HIV SNPs are managed care plans specifically designed to serve Medicaid beneficiaries with HIV/AIDS and their children. Non-SSI beneficiaries with HIV/AIDS will have 60 days to choose a plan but may request an additional 30 days for a total of 90 days to make a choice. As with current policy, all SSI beneficiaries will be given 90 days to choose a managed care plan. Individuals who do not choose a plan will automatically be assigned to a mainstream managed care plan. Auto-assigned individuals will have an opportunity to switch to another mainstream plan or an HIV SNP of their choosing during the 90 day grace period. All beneficiaries with HIV/AIDS may change from a mainstream managed care plan to an HIV SNP, or from an HIV SNP to another HIV SNP at any time. Information regarding switching plans is available from Medicaid CHOICE and in the mandatory mailing and enrollment letters.
Providers treating this population should encourage their patients to enroll in plans with which the provider participates to promote continuity of medical care. Providers are also encouraged to join the networks of Medicaid managed care plans and HIV SNPs in their community.
Managed Care Benefits: The benefit package for HIV positive individuals who join a mainstream managed care plan is the same as for all Medicaid beneficiaries. Services carved-out from managed care include but are not limited to: prescription medications, targeted case management, AIDS adult day health care services, some mental health and substance abuse services (including MMTP), HIV resistance tests, personal care, and hospice services.
The mainstream managed care plan contract is available online at: www.nyhealth.gov/health_care/managed_care/docs/medicaid_managed_care_and_family_health_plus_model_contract.pdf.
The benefit package for HIV SNPs is the same as the benefit package for regular managed care plans, with the exception of Mental Health and Chemical Dependence Inpatient Rehabilitation Services. For adults in a HIV SNP, detoxification services, most mental health services and inpatient rehabilitation services for chemical dependency are the responsibility of the HIV SNP. Outpatient services for chemical dependency, including MMTP, are carved-out.
The HIV SNP contract is available online at: www.nyhealth.gov/health_care/managed_care/docs/medicaid_managed_care_fhp_hiv-snp_model_contract.pdf
As a reminder, a breakdown of how coverage of mental health and chemical dependence inpatient rehabilitation services by population is provided below.
| Mental Health and Chemical Dependence Inpatient Rehabilitation | ||
|---|---|---|
| Covered by health plan for the following populations | Covered by Medicaid fee-for-service for the following populations | |
| Mainstream Plan | Non-SSI enrollees | SSI enrollees |
| HIV SNP | All adult enrollees All HIV+ children Non-SSI uninfected children | Uninfected SSI children |
Questions? Please e-mail omcmail@health.state.ny.us.
Guidelines to Receive Medical Home Incentive Payments from Medicaid
Return to Table of Contents
Providers recognized as a PPC®-PCMH™* by the NCQA (National Committee for Quality Assurance) must provide the 4-digit extension of the zip code for each NCQA recognized practice location to NCQA as soon as possible (directions are as follows).
IN ADDITION:
- If your practice site is a clinic (Article 28 facility), OR
- If you bill through a group practice:
You must also provide the "Practice Site NPI" to NCQA as soon as possible. This is defined as either:
- 1. The billing NPI of the clinic, OR
- 2. The billing NPI of the group practice.
Providers must report these critical data elements to NCQA to receive statewide medical home incentive payments from New York Medicaid. Incentive payments will not begin until this information is on file with NCQA. NCQA transfers this information monthly to the State Department of Health for the processing of incentive payments. Please submit your zip code INCLUDING THE 4-DIGIT EXTENSION, AND your Practice Site NPI (if you practice in a clinic, or if you bill through a group practice) to NCQA via e-mail at: ppc-pcmh@ncqa.org.
Note: If you are an NCQA recognized medical home provider practice, working in an office setting and billing under your individual NPI, you must provide your zip code and 4-digit zip code extension to NCQA. However, the "Practice site NPI" will not pertain to providers if they bill under their personal NPI which was submitted to NCQA during the certification process.
For more detailed information on the Medicaid Statewide Medical Home Program, please review the December 2009 and May 2010 Medicaid Update newsletters at the following links:
http://nyhealth.gov/health_care/medicaid/program/update/2009/2009-12spec.htm, and http://nyhealth.gov/health_care/medicaid/program/update/2010/2010-05.htm.Questions? Please contact the Division of Financial Planning and Policy at (518) 473-2160.
* NCQA Disclaimer:
The Physician Practice Connections-Patient Centered Medical Home (PPC®-PCMH™) Recognition Program is developed,
owned, and managed by the National Committee for Quality Assurance (NCQA). To learn more about the PPC®-PCMH™
Recognition Program, refer to the program's Website at www.ncqa.org/ppcpcmh.aspx. NCQA is not involved in any
determination of clinician incentive payments under the New York State Medicaid Medical Home Program.
Expanded Coverage of Telemedicine
Specialist Consultations
Return to Table of Contents
Telemedicine is an interactive audio and video telecommunications system that permits a "real time" interactive consultation between a physician and patient. The September 2006 Medicaid Update provided billing instructions for telemedicine consultations provided by physician specialists in hospital facilities.
Retroactive to February 1, 2010, Medicaid is expanding coverage for physician specialist telemedicine consultations to patients in hospital outpatient departments. Additionally, physicians may bill separately for their hospital services using the physician fee schedule in both the inpatient and outpatient setting, including for telemedicine consultations. Physician reimbursement for the telemedicine consultation will be for the same amount as an in-person specialist consultation. Telemedicine consultations are not limited to any specific physician specialty. Covered physician specialties include, but are not limited to, neurology, endocrinology, oncology, etc. Telemedicine consultations must be conducted using a real-time fully interactive, secure two-way audio and video telecommunications system that supports review of diagnostic tests integral to the consultation.
Physician specialist telemedicine consultations are covered when medically necessary and under the following circumstances:
- the patient is located at the spoke site and the physician specialist is located at the hub site;
- the spoke site is the hospital where the patient and referring physician are located;
- the hub site is the office or other hospital where the physician specialist is located;
- the patient is present during the telemedicine consultation;
- a specialist is not available at the spoke site to provide a timely consultation;
- the physician specialist is not conducting the telemedicine consultation at the spoke site;
- the telemedicine consult request and the rationale for the request are documented in the patient's medical record;
- the patient record includes documentation that the telemedicine consultation occurred and that the results and findings were communicated to the requesting provider;
- the consulting physician is licensed in NYS; is practicing within his/her scope of specialty practice; is enrolled in New York Medicaid; and is credentialed and privileged at the spoke site hospital.
Physician billing requirements:
- physicians billing for telemedicine consultations must include the modifier - GT "via interactive audio and video telecommunications systems" with the appropriate consultation E&M code to indicate services were performed via telemedicine;
- the place of service entered on the claim is the location of the patient. Use "21" for hospital inpatient, "22" for hospital outpatient, or "23" for hospital emergency room.
- the attending physician bills the appropriate E&M code without the GT modifier;
- payment will be made to only one physician for the professional component (reading and interpretation) of diagnostic tests such as radiological procedures and diagnostic assessments.
Questions? For additional information or assistance regarding Medicaid coverage of Telemedicine please contact the following:
Billing and claims submission, please contact the eMedNY Call Center at (800) 343-9000.
Medicaid telemedicine coverage, please contact the Division of Financial Planning and Policy at (518) 473-2160.
Funding for rural hospitals for purchasing of telemedicine equipment, please contact the Office of Rural Health at (518) 402-0102.
Credentialing and privileging requirements, please contact the Office of Health Systems Management at (518) 402-1003.
Procedure codes or fees, please refer to the Physician Fee Schedule, available at: http://www.emedny.org/ProviderManuals/Physician/index.html, or contact the Division of Provider Relations and Utilization Management at (518) 474-8161.
Assistance for Pregnant Women
Choosing a Medicaid Managed
Care Plan
Return to Table of Contents

Presumptive eligibility (PE) for pregnant women is a means of immediately providing Medicaid coverage for prenatal care services pending a full Medicaid eligibility determination. With the enactment of Chapter 484 of the Laws of 2009, all Medicaid enrolled licensed Article 28 providers that provide prenatal care are now required to perform presumptive eligibility (PE) determinations.
In addition to screening pregnant women for Medicaid presumptive eligibility, the provider must assist the pregnant woman who screens eligible in completing the Access NY Health Care application (DOH-4220). This includes helping the pregnant woman select a Medicaid managed care plan and submitting the completed Medicaid application to the appropriate local department of social services for a full Medicaid determination. The completed application must include a Medicaid managed care plan choice in Section I.
Prenatal care provider designated staff must be trained in the PE process prior to performing these determinations. On-line training is available at http://www.bsc-cdhs.org/eLearning/.
For a list of managed care plans by county, please visit: http://www.nyhealth.gov/health_care/managed_care/pdf/cnty_dir.pdf.
For further information regarding presumptive eligibility, please refer to the February 2010 Medicaid Update Prenatal Care Special Edition available online at: http://www.nyhealth.gov/health_care/medicaid/program/update/2010/2010-02_special_edition.htm.
Reimbursement for Sterilization
Procedure During Delivery for Fidelis Enrollees
Return to Table of Contents
Effective for dates of service beginning December 1, 2009, hospitals providing newborn delivery services combined with a sterilization procedure for enrollees of the New York State Catholic Health Plan, a.k.a. Fidelis Care New York, may bill Medicaid fee-for-service for the sterilization component of the service, only. The plan will continue to be responsible for payment of the newborn delivery.
The following billing instructions are valid for delivery and sterilization services provided to Medicaid managed care and Family Health Plus (FHPlus) enrollees of Fidelis. The billing hospital must participate in Fidelis' provider network or otherwise be approved by the health plan to provide delivery services to the enrollee.
Claims for the sterilization component of a combined delivery/sterilization inpatient stay may be submitted beginning April 22, 2010 and must include:
- Rate code 2290 Sterilization During Delivery;
- APR-DRG 541;
- A sterilization procedure code as primary or secondary (sterilization procedure codes are: 6621; 6622; 6629; 6631; 6632; 6639; 664; 6651; 6652; 6663; 6669; 6692; 6697);
- Date of admission as the date of service (must be a one day claim); and
- Primary diagnosis of birth/delivery and secondary diagnosis of sterilization.
Stays for combined delivery and sterilization services for enrollees of all other Medicaid managed care and FHPlus plans will continue to be billed to the health plan.
Additional information is available at www.emedny.org.
Questions on billing procedures should be directed to the eMedNY Call Center at (800) 343-9000.
Questions on managed care should be directed to the Bureau of Managed Care Program Planning & Implementation at (518) 473-0122.
UPDATE: Adult Day Health Care
Transportation Methodology
Return to Table of Contents
The following article describes the changes to adult day health care (ADHC) transportation reimbursement methodologies for fee-for-service and self-managed transportation to and/or from ADHC programs. Please note, ad hoc medical appointments may continue to be arranged by ADHC programs, but are always fee-for-service at the applicable county ad hoc medical transportation fee schedule.
Fee-for-Service ADHC Transportation: For transportation ordered through the local social services agency, and reimbursed through the county or State on a fee-for-service basis, the following applies:
- Taxi/livery fee-for-service fees remain unchanged.
Effective July 15, 2010:
- New York City ambulette - $50 round trip.
- Ambulette all other counties - new adult day health care ambulette transportation fee plus, where determined necessary and approved by the Department of Health, a mileage add-on commensurate with the county's existing mileage standards.
Self-Managed ADHC Transportation: For transportation managed and paid by the ADHC program, the following applies:
- If the program is now receiving the July 2009 established standardized round trip rate (New York City & surrounding metropolitan region $44.40, upstate $43.12) there will be no change.
- For programs that are now receiving an amount greater than the standardized rate, the July 2009 rate will not be changed. The Department of Health will request current contracts between ADHC programs and transportation providers and establish an administrative cap of 10%.
- For any self-managed program paying a contract rate lower than 85% of the reimbursement rate, the Department of Health will consider reducing the reimbursement rate for that program.
A letter to ADHC programs and county staff describing these changes is online at: http://www.emedny.org/ProviderManuals/Transportation/communications.html.
To request the Medicaid Transportation fee schedule, please email the Medicaid Transportation Policy Unit at: MedTrans@health.state.ny.us
Questions may be referred to the Medicaid Transportation Policy Unit at (518) 473-2160 or via e-mail to: MedTrans@health.state.ny.us
Obstetrical Care Practitioner Billing
Policy Update and Clarification
Return to Table of Contents
Antepartum Care: Effective April 1, 2010, Medicaid providers of antepartum care will no longer be required to prorate professional charges on their claims for procedure codes 59425 and 59426. Providers who perform fewer than four antepartum care visits to a single patient during the course of a pregnancy should bill the appropriate evaluation & management code for each date of service. This policy applies to all prenatal care providers who bill for professional services using the Medicaid fee schedule, including those enrolled in the MOMS program.
| Procedure Code | Description |
|---|---|
| Appropriate E&M code | If less than four antepartum visits are performed, providers should bill the appropriate E&M code for the visit. |
| 59425* | Antepartum care only; 4 - 6 visits (includes reimbursement for the initial antepartum encounter and up to five subsequent encounters - submit one unit). |
| 59426* | Antepartum care only; 7 or more visits (includes reimbursement for the initial antepartum encounter and six or more subsequent encounters - submit one unit). |
* Providers should bill the appropriate code after all antepartum care has been rendered using the last antepartum visit as the date of service. Only one antepartum care code will be reimbursed per pregnancy.
Global Fee: The global fee should still be billed in instances where the provider sees the patient for all antepartum care (7 or more visits), performs the delivery, and provides the postpartum care for the same patient. If the patient is seen for six or less antepartum visits, global care billing is not allowed under this policy and separate billing is required for the antepartum, delivery, and postpartum care.
Postpartum Care: There is no change to policy regarding postpartum visits. Only one outpatient postpartum visit can be billed with CPT code 59430 and should only be billed when the practitioner did not perform the delivery. Any subsequent medically necessary follow-up visit should be billed as an evaluation and management visit. In instances where the provider performs the delivery and provides postpartum care, the procedure codes 59410 (vaginal delivery and postpartum care) or 59515 (cesarean delivery and postpartum care) should be reported rather than the individual codes for delivery (59409 or 59514) and postpartum care (59430). There is an edit currently in place which will not allow a separate payment for the postpartum care.
Questions? Billing questions should be directed to the eMedNY Call Center at (800) 343-9000. Policy questions should be directed to the Division of Financial Planning and Policy at (518) 473-2160.
Over-the-Counter Chelation
Therapy Agents
Return to Table of Contents
This notice contains important information for health care providers who are managing children with lead poisoning and autism spectrum disorders. Recently, the U.S. Food and Drug Administration (FDA) issued a statement concerning the use of over-the-counter (OTC) "chelation therapy" products promoted for home use to prevent or treat disease. The New York State Department of Health (NYSDOH) is sharing this important information because of concern about 1) the online marketing without FDA approval of these non-prescription chelation products for consumer purchase, and 2) the potential risks of side effects associated with use of these agents without the oversight of a licensed medical professional.
On February 4, 2010, the FDA issued the following statement in italics below, regarding OTC chelation therapy products.
The US Food and Drug Administration FDA advises consumers to be wary of so-called "chelation therapy" capsules, tablets, or suppositories marketed over-the-counter (OTC) that are promoted for home use to prevent or treat diseases. Various forms of "chelation" therapies are purported to cleanse the body of chemicals (such as mercury-containing chemicals) or to improve the cardiovascular system. "Chelation" has been proposed as a treatment for autism or hardening of the arteries; and for many other serious conditions. Many of these products are promoted on the internet.
FDA has never approved any marketing application for a nonprescription oral or rectal chelation product. Such products have not been studied in adequate and well-controlled clinical trials, and clinical data sufficient to support either the safety or efficacy of drugs used for these "chelation" purposes has not been reviewed by FDA. These products are illegally marketed and have not been subject to the rigorous manufacturing scrutiny required for FDA-approved products. FDA is concerned about the potential direct health risks posed by these products because of the lack of safety information, and because serious side effects can occur when a "chelation" product is used without the oversight of a licensed health-care professional. The products also pose serious indirect health risks to patients using these products that may be foregoing effective conventional medical treatment.
Families of children and adults with autism spectrum disorders are encouraged to speak to their health-care professional about treatment options, including pursuing new therapies with clinical investigators engaged in research monitored under an Institutional Review Board approved Investigational New Drug application, to make sure the risks are as low as possible and are worth any potential benefits.
Chelation therapy for lead poisoning requires management by medical practitioners aware of the potential side effects of treatment. The NYSDOH Lead Poisoning Prevention Program (LPPP) strongly recommends consultation with a Regional Lead Resource Center (RLRC) with questions concerning chelation therapy and/or other medical management considerations for lead poisoned children. Please see the following page for a listing of New York State Regional Lead Resource Centers.
For more information about lead poisoning prevention, please visit:
New York State Department of Health: www.health.state.ny.us/environmental/lead/.
New York City Department of Health and Mental Hygiene:
www.nyc.gov/html/doh/html/lead/lead.shtml.
For more information about early intervention and autism spectrum disorders, visit:
New York State Department of Health
http://www.nyhealth.gov/community/infants_children/early_intervention/index.htm.
http://www.nyhealth.gov/community/infants_children/early_intervention/autism.
New York City Department of Health and Mental Hygiene
http://www.nyc.gov/html/doh/html/earlyint/earlyint.shtml.
LEAD POISONING PREVENTION PROGRAM
REGIONAL LEAD RESOURCE CENTERS
Return to Table of Contents
(KALEIDA HEALTH/WOMEN & CHILDREN'S HOSPITAL OF BUFFALO)
Judge Joseph S. Mattina Community Health
300 Niagara Street
Buffalo, New York 14201
Medical Director: Melinda S. Cameron, MD
(716) 859-4199 Fax: (716) 859-4219
E-mail: MCamero@buffalo.edu
Project Coordinator: Stephanie Kellner
(716) 859-4199 Fax: (716) 859-4219
E-mail: SKellner@kaleidahealth.org
Sub Contractor
UNIVERSITY OF ROCHESTER Mailing Address:
Department of Pediatrics
Division of General Pediatrics University of Rochester Medical Center
601 Elmwood Avenue, Box 777
Rochester, New York 14642
Medical Director: Stanley J. Schaffer, MD, MS
(585) 275-0267/Fax: (585) 273-1037
E-mail: Stanley_Schaffer@urmc.rochester.edu
Co-Director: James R. Campbell, MD, MPH
(585) 922-3919 (Direct #) Fax: (585) 922-3929
E-mail: James.Campbell@RochesterGeneral.org
Project Coordinator: Judy McMaster
E-mail: Judy_McMaster@urmc.rochester.edu
(585) 276-3105/Fax: (585) 273-1037
MONTEFIORE MEDICAL CENTER
Environmental Sciences Lead Program
111 East 210th Street
Bronx, New York 10467
Medical Director: John F. Rosen, MD
(718) 547-2789/ext. 217
Fax: (718) 547-2881/8251
E-mail: Jrosen5@ix.netcom.com
Program Administrator: Dana Politis
(718) 547-2789/ext. 216
Fax: (718) 547-2881/8251
E-mail: dpolitis@montefiore.org
Nancy Redkey
Cell: (914) 475-2793 E-mail: nredkey@aol.com
SUNY UPSTATE MEDICAL UNIVERSITY
Pediatric Medical Services Group
Department of Pediatrics
750 East Adams Street
Syracuse, New York 13210
Medical Director: Howard L. Weinberger, MD
(315) 464-5450 Fax: (315) 464-7564
E-mail: Weinberh@upstate.edu
Project Coordinator: Maureen Butler, BSN
(315) 464-7584 Fax: (315) 464-7564
E-mail: ButlerMJ@upstate.edu
Sub Contractor
ALBANY MEDICAL COLLEGE
Department of Pediatrics
43 New Scotland Avenue
Albany, New York 12208
Medical Director: Carrin Schottler-Thal, MD
(518) 262-7860- AMC Pediatric Group
Fax: (518) 262-5589
E-mail: schottc@mail.amc.edu
Lead Coordinator: Paul Moss
(518) 262-7860
E-mail: mossp@mail.amc.edu
Medicaid Pharmacy Prior
Authorization Update
Return to Table of Contents
The following changes to the Preferred Drug Program (PDP) are effective July 28, 2010. Prior authorization requirements will change for some drugs in the following five PDP drug classes:
- Anticoagulants - Injectable
- Serotonin Receptor Agonists (Triptans)
- Sulfasalazine Derivatives
- Corticosteroids-Intranasal
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)-Ophthalmic
The PDP is also expanding to include additional drug classes. Prescriptions for nonpreferred drugs in the following four drug classes will require prior authorization:
- Biguanides
- Xanthine Oxidase Inhibitors
- Beta Blockers-Ophthalmic
- Platelet Inhibitors
To obtain prior authorization for non-preferred drugs within the drug classes listed above, please contact the Clinical Call Center at (877) 309-9493 and follow the appropriate prompts. Following is the most up-to-date Preferred Drug List (PDL), with a full listing of preferred and non-preferred drugs for each of the drug classes currently subject to the PDP: https://newyork.fhsc.com/downloads/providers/NYRx_PDP_PDL.pdf.
Additional information, such as a "Quick List" of only preferred drugs and updated prior authorization forms, is available at each of the following Websites:
http://www.nyhealth.gov or
http://www.eMedNY.org or
https://newyork.fhsc.com.
Please note that future changes to the Medicaid Pharmacy prior authorization programs, including updates to the Preferred Drug List (PDL), will be communicated electronically through the Medicaid Update and the above mentioned Websites. If you wish to receive direct e-mail notification of changes, send your request to NYPDPNotices@magellanhealth.com.
Remember, unless otherwise indicated on the PDL or Quick List, prescribing preferred drugs requires no further action on your part.
For clinical concerns or preferred drug program questions, please contact (877) 309- 9493. For billing questions, contact (800) 343-9000. For Medicaid pharmacy policy and operations questions, call (518) 486 -3209.
Early Fill Edit Update
Return to Table of Contents
Effective immediately, claims submitted with the "03" (Vacation Supply) Submission Clarification Code-Field 420-DK, will deny. New York Medicaid's refill policy ensures an ample supply to accommodate for most temporary absences. Beneficiaries that do not have an adequate supply of medication due to a temporary absence should make alternative arrangements, such as relying on a trusted friend or family member.
In cases of extenuating circumstances, beneficiaries should contact (518) 486-3209 at least seven days prior to departure. Approval will not be granted for controlled substances.
Questions? Please contact the Medicaid Pharmacy Policy and Operations staff at (518) 486-3209.
Automatic Refills Update
Return to Table of Contents
Refilling of prescriptions or fiscal orders for Medicaid beneficiaries without the knowledge or permission of the beneficiary or their designated caregiver is NOT allowed under the Medicaid program. Automatic-refill programs offered by pharmacies are NOT an option for Medicaid beneficiaries.
Automatic refilling of prescriptions/orders for prescription drugs, over-the-counter products, medical surgical supplies and enteral products is NOT allowed under the Medicaid program.
Requests for a refill: A Medicaid beneficiary or designated caregiver may contact the pharmacy to request necessary refills.
Provider inquiry: A provider may initiate contact with a Medicaid beneficiary to determine if a refill is necessary. Documentation of the need for a refill shall be maintained in the patient record and must include the date and time of contact, Medicaid beneficiary or designated caregiver's name and contactor's identification. This documentation must be available for audit purposes.
Reminder: Compliance with HIPAA privacy guideline is mandatory.
Questions? Please contact the Medicaid Pharmacy Policy and Operations staff at (518) 486-3209.
Medicaid Offers Electronic Funds
Transfer (EFT) for Provider Payments
and PDF Paper Remittances
Return to Table of Contents
Thousands of providers have signed up to have their Medicaid funds deposited directly into their checking or savings account. Providers that have not yet signed up for EFT are urged to take advantage of the benefits that EFT offers - benefits include:
- Eliminates the possibility of lost checks;
- Eliminates delays that may be caused by misdirected checks;
- Eliminates mail time;
- Funds are secure; and
- Saves trips to the bank to deposit your checks from Medicaid.
In addition to EFT, providers who currently receive paper remittance statements from Medicaid can elect to receive a PDF version of the paper remittance delivered electronically through eMedNY's secure website. PDF remittances have many advantages over paper remittances:
- The remittance will not be held with your Medicaid check or EFT release for two weeks but released to you two weeks earlier.
- You will know when the PDF is available in your eXchange account and not have to wait for the mail.
- The remittance can be downloaded and stored electronically for ease of retrieval and you can still print a hard copy.
- The remittance can be word searched to help locate specific claims.
- The PDF will look exactly like the paper remittance you may be use to receiving.
- Remittances can be printed with Adobe Reader® (6.0 release or higher required), which is available free of charge.
Both the EFT and PDF remittance applications are available online at: http://www.emedny.org/info/ProviderEnrollment/index.html.
Questions? Please contact the eMedNY Call Center at (800) 343-9000.
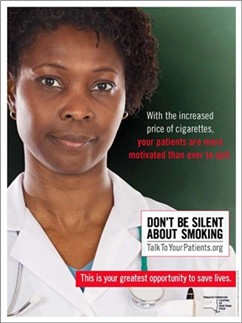
By providing counseling, pharmacotherapy, and referrals, you can double your patients' chances of successfully quitting. For more information, please visit www.talktoyourpatients.org or call the NY State Smokers' Quitline at 1-866-NY-QUITS (1-866-697-8487).
Do you suspect that a Medicaid provider or an enrollee has engaged in fraudulent activities?
Return to Table of Contents
Please Call: 1-877-87FRAUD or (212 417-4570)
Your call will remain confidential.
You can also complete a Complaint Form online at:
www.omig.state.ny.us

Provider Directory
Return to Table of Contents
Office of the Medicaid Inspector General:
http://www.omig.state.ny.us or call (518) 473-3782 with general
inquiries or 1-877-87FRAUD with suspected fraud complaints or allegations.
This contact information can also be used for Provider Self-Disclosures.
Questions about billing and performing MEVS transactions?
Please contact eMedNY Call Center at: (800) 343-9000.
Provider Training
To sign up for a provider seminar in your area, please enroll online at:
http://www.emedny.org/training/index.aspx
For individual training requests, call (800) 343-9000 or email: emednyproviderrelations@csc.com
Enrollee Eligibility
Call the Touchtone Telephone Verification System at any of the numbers below:
(800) 997-1111 (800) 225-3040 (800) 394-1234.
Address Change?
Questions should be directed to the eMedNY Call Center at: (800) 343-9000.
Fee-for-Service Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Rate-Based/Institutional Providers
A change of address form is available at:
http://www.emedny.org/info/ProviderEnrollment/index.html
Does your enrollment file need to be updated because you've experienced a change in ownership?
Fee-for-Service Providers please call (518) 402-7032
Rate-Based/Institutional Providers please call (518) 474-3575
Comments and Suggestions Regarding This Publication?
Please contact the editor, Kelli Kudlack, at:
medicaidupdate@health.state.ny.us
Medicaid Update is a monthly publication of the New York State Department of Health containing information regarding the care of those enrolled in the Medicaid Program.