NURSING HOME TRANSITION and DIVERSION MEDICAID WAIVER
N.Y.S. DEPARTMENT OF HEALTH
Office of Health Insurance Programs Division of Long Term Care
Program Manual 2021
- Manual is also available in Portable Document Format (PDF)
Introduction
Introduction to the Home and Community-Based Services Nursing Home Transition and Diversion (NHTD) Medicaid Waiver
The Home and Community-Based Services (HCBS) Medicaid Waiver for Nursing Home Transition and Diversion (NHTD) is one of the options available to New Yorkers with disabilities, and seniors, so they may receive services in the most appropriate, least restrictive setting.
What is a Home and Community Based Services (HCBS) 1915(c) Medicaid Waiver?
In 1981, Congress authorized the waiver of certain federal requirements to enable a state to provide home and community services (other than room and board) to individuals who would otherwise require institutional/nursing facility services reimbursed by Medicaid. The waiver programs are called 1915(c) waivers, named after the section of the Social Security Act that authorized them. Under 1915(c) waiver authority, states can provide services not usually covered by the Medicaid program, as long as these services are required to keep the person from being institutionalized.
A 1915(c) waiver:
- Allows states to assemble a package of carefully tailored services to meet the needs of a targeted group in a community-based setting;
- Is an opportunity for comprehensive services to be available in the community rather than in an institution;
- Maintains the waiver participant's health and welfare through an individualized service plan; and
- Assures that the overall cost of serving the waiver participants in the community is less than the cost of serving this same target group in an institution.
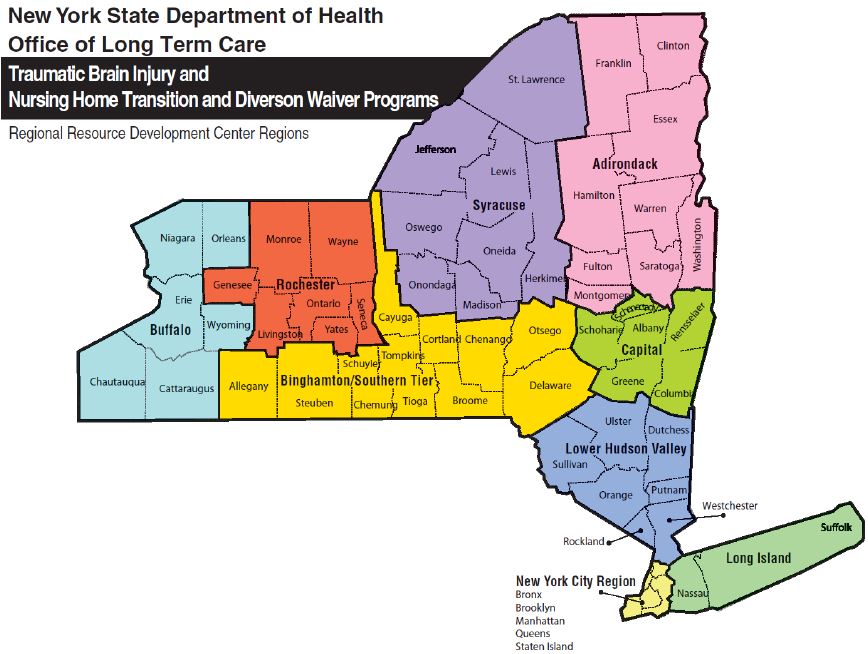
The Nursing Home Transition and Diversion (NHTD) 1915(c) Medicaid waiver is a Home and Community-Based Services (HCBS) program, administered by the New York State Department of Health (NYSDOH) through contractual agreements with Regional Resource Development Centers (RRDC). The RRDC employs a Regional Resource Development Specialist (RRDS) and a Nurse Evaluator (NE) and other qualified staff and serves designated counties in the state (refer to Section XIII).
The NHTD waiver provides services to assist individuals with disabilities, and seniors, toward successful inclusion in the community. Waiver participants may come from a nursing facility or other institution (transition) or choose to participate in the waiver to prevent institutionalization (diversion).
Waiver services are provided when informal supports, local, state, and other federally funded services are not sufficient to assure the health and welfare of the individual in the community.
The development of the NHTD Medicaid waiver was based on the philosophy that individuals with disabilities and/or seniors have the same rights as others. This includes the right to be in control of their lives, encounter and manage risks, and learn from their experiences. This is balanced with the waiver program's responsibility to assure the waiver participants' health and welfare.
The provision of the waiver services is based on the participant's unique strengths, needs, choices, and goals. The individual is the primary decision-maker and works in cooperation with providers to develop a service plan. This process leads to personal empowerment, increased independence, greater community inclusion, self-reliance, and meaningful productive activities. Waiver participant satisfaction is a significant measure of success of the NHTD waiver.
Program Manual - Purpose and Layout
This Program Manual was created to provide policies, procedures, and information about the Nursing Home Transition and Diversion (NHTD) Medicaid waiver program for waiver applicants/participants, stakeholders, Service Coordinators (SC) and other waiver service providers, Regional Resource Development Centers (RRDC), Regional Resource Development Specialists (RRDS), and Nurse Evaluators (NE). Upon request, it can also be shared with applicants and waiver participants.
Sections one (I) through eleven (XI) of this Program Manual outline the policies and procedures of the NHTD waiver. Section fourteen (XIV) contains the forms used in the various areas/components of the waiver program. Section twelve (XII) is the Glossary of Terms relevant to the waiver program. Section thirteen (XIII) contains the map outlining the regions served by the Regional Resource Development Centers (RRDC).
This manual replaces the 2008 and subsequent draft Program Manuals for the Nursing Home Transition and Diversion Medicaid Waiver.
This manual reflects the major changes in 1915(c) Medicaid waiver application approved by the Centers for Medicare and Medicaid Services (CMS) effective July 1, 2018; all subsequent amendments as well are new compliance requirements set forth by CMS.
These changes include and are not limited to:
- Update of service provider qualifications and/or service definitions for Service Coordination, Assistive Technology, Community Integration Counseling Services, Environmental Modifications, Independent Living Skills Training, Positive Behavioral Interventions and Supports, and Structured Day Program Services;
- Addition of Transportation Services (Social) as an extended state plan service; and
- Update/clarification of Serious Reportable Incidents.
Every section has been updated to include new operational policies and procedures
Special Note: Whenever the term 'applicant' or 'participant' is used in this Program Manual, it also includes reference, if applicable, to a duly authorized representative designated to act on behalf of the applicant/participant, unless specifically stated otherwise.
TABLE OF CONTENTS
Section I: Introduction to the NHTD Waiver
Foreward
This manual replaces the 2008 and subsequent draft Program Manuals for the Nursing Home Transition and Diversion Medicaid Waiver.
This manual reflects the major changes in the 1915(c) Medicaid waiver application approved by the Centers for Medicare and Medicaid Services (CMS) effective July 1, 2018, as well as new compliance requirements set forth by CMS. These changes include but are not limited to:
- Update of service provider qualifications and/or service definitions for Service Coordination, Assistive Technology, Community Integration Counseling Services, Environmental Modifications, Independent Living Skills Training, Positive Behavioral Interventions and Supports, and Structured Day Program Services;
- Addition of Transportation Services (Social) as an extended state plan service; and
- Update/clarification of Serious Reportable Incidents.
Every section has been updated to include new or existing policies and procedures for the NHTD waiver.
Basic Framework
Under the authority provided by Section 1915(c) of the Social Security Act and as approved by the Centers for Medicare and Medicaid Services (CMS), New York State has elected to provide home and community-based services (HCBS) under this Nursing Home Transition and Diversion (NHTD) waiver program.
Section II: Becoming a Waiver Participant
Introduction
The approved waiver application specifies the scope and features of the NHTD waiver program, including eligibility criteria and services offered through the program. This manual is intended for Regional Resource Development Centers (RRDCs), NHTD Providers, and stakeholders to assist with the implementation and operationalization of the processes, procedures, and other features of the NHTD waiver program, as approved in the waiver application.
A state must implement the waiver as specified in the approved application. If the state wants to change the waiver while it is in effect, it must submit an amendment to CMS for its review and approval. All requests for new waivers, waiver renewals and amendments must be submitted by the state Medicaid agency. There is no limit on the number of HCBS waivers that a state may operate.
In its application, a state must specify the unduplicated number of individuals that the state intends to serve each year the waiver is in effect. It is up to the state to determine this number, based on the resources that the state has available to underwrite the costs of waiver services. As state resources permit, this number may be modified by amendment while the waiver is in effect. The state may not exceed its approved enrollment without seeking an amendment to the application.
In its application and each year during the period that the waiver is in operation, the state must demonstrate that the waiver is cost neutral. In particular, the average per participant expenditures for the waiver and non-waiver Medicaid services must be no more costly than the average per person costs of furnishing institutional (and other Medicaid state plan) services to individuals requiring the same level of care.
HCBS Waiver Resources on the Web
In addition to the web-based application for 1915(c) waivers located here, CMS makes available assorted information and resources via its website (medicaid.gov) regarding the HCBS waiver program. The CMS web pages that are especially pertinent include:
General information about the HCBS waiver program along with links to other pertinent information is located here
Link to 1915(c) Application, Instructions, Technical Guide, and Review Criteria
The NHTD waiver makes every effort to promote the right of waiver applicants and participants to choose participation in the NHTD waiver, identify needed services, and select their service providers. Agencies that provide Service Coordination must adhere to conflict-of-interest (COI) requirements established by the Department. Compliance with these practices promotes the independence of the Service Coordinator (SC) and ensures participant choice. The Service Coordinator is responsible for providing unbiased and comprehensive information to the participant about available services and service providers. A Service Coordinator may not "steer" business and may not recommend or indicate a preference for a service provider. A waiver participant cannot get Service Coordination and another direct waiver service from the same provider.
NHTD Eligibility
This section of the Program Manual delineates the eligibility criteria, issues that impact eligibility, referral, intake, application, and determination processes.
A. Eligibility Criteria
Waiver applicants must meet all the following criteria in order to be approved for the NHTD waiver. The individual must:
- Be between age 18 and 64 with a physical disability, or age 65 and older upon application to the waiver; if under age 65, the physical disability must be documented. Documentation can be supported by award letters/determination and/or via confirmation with the Local Department of Social Services (LDSS).
Examples of award letters/determination may include:The LDSS refers individuals seeking a Medicaid disability determination to the State Disability Review Unit (SDRU) to complete a disability review. Confirmation of the disability determination is sent to the LDSS and the applicant. Confirmation of this determination is secured by the RRDC.
- Supplemental Security Income (SSI);
- Social Security Disability Insurance (SSDI); or
- Railroad Retirement letter for total permanent disability for SSI benefits.
For questions regarding disability documentation requirements call the State Disability Review Unit toll free number 1-866-330-0591 or go here.
If the individual is between the ages of 18-64, they must have a physical disability as a primary diagnosis.
For those without a disability review, documentation from the individual's physician, hospital summaries or nursing facility records may verify the physical disability. Documentation from a physician should be in the form of a written summary on physician letterhead, signed & dated by the physician, outlining the physical disability.- The individual must identify a Home and Community Based (HCB) Settings compliant residence in which they will reside when receiving waiver services. This can be their current residence or a residence they are planning to move to with the support of NHTD services. Residential settings of four or more unrelated individuals are excluded. Enrolled waiver participants residing in a setting of four or more unrelated individuals prior to the HCB settings compliance date will remain under the previous criteria until they move. The services and supports available through the waiver and other sources must be sufficient to maintain the individual's health and welfare in the community. Since the participant's residence is also the primary waiver services provision site, it must be Home and Community Based (HCB) Settings compliant and cannot be a congregate care setting. This includes certified and/or licensed residences such as assisted living, nursing facilities, supervised apartments, group homes, and adult care residences.
NOTE: Individuals residing in buildings/housing owned by waiver service provider agencies or waiver service provider staff may not be considered HCB settings compliant and may require another living arrangement in order to receive waiver services.- The individual and/or their legal guardian must choose to participate in the waiver by indicating consent on the Freedom of Choice form.
- Be a recipient of Medicaid coverage that supports community-based long-term care services. Such coverage includes:
NOTE: The type of Medicaid coverage the individual receives must be verified by providing a copy of Medicaid verification from the New York State system with the submission of the application packet (the Service Coordinator attaches this to the Initial Service Plan).
- 01 - Full Coverage
- 02 - Out-Patient Coverage
- 06 - Provisional Eligibility Excess Income (Case Type 20 Only)
- 08 - Presumptive Eligibility - Home Care (Case Type 20 Only)
- 10 - All Services except Long-Term Care (Case Types 20 and 22 Only)
- 11 - Legal/Alien - Full Coverage
- 19 - Community Coverage with Community-Based Long-Term Care
- 21 - Outpatient Coverage with Community-Based Long-Term Care
- 23 - Outpatient Coverage with no Nursing Facility Services
- 30 - PCP Full Coverage
It is not the responsibility of the RRDC and/or the Service Coordinator to facilitate application for Medicaid eligibility.- Be assessed to need a nursing facility level of care (LOC) and live safely in the community. The Uniform Assessment System for New York (UAS-NY) determines the applicant's nursing facility level of care (LOC). It is completed by a registered nurse certified to complete the UAS-NY. A score of 5 or greater is required for waiver eligibility. A UAS-NY assessment must be dated within ninety (90) calendar days prior to the Effective Date of the Notice of Decision (NOD) Authorization (DOH-5740) or Notice Date of the NOD Denial of Waiver Program (DOH-5737), as appropriate.
If the individual is in a hospital or nursing facility, their LOC may be determined by the Hospital and Community Patient Review (H/C PRI) (DOH-694) and SCREEN (/DOH-695) assessment tools. If an H/C PRI and SCREEN is completed for eligibility into the NHTD waiver program, the participant must be reassessed using the UAS-NY for LOC within ninety (90) days of their Enrollment Date into the NHTD waiver program.
Resource links for H/C PRI and SCREEN training: Hospital and Community Patient Review Instrument (H/C PRI) and School of Public Health
All future LOC reassessments for the NHTD waiver program must be completed at least annually through the use of the UAS-NY.
NOTE: If an applicant/participant does not meet nursing facility LOC as a result of their first LOC assessment/reassessment, then the RRDC will have the RRDC Nurse Evaluator (NE) complete the applicant/participant's second LOC assessment (UAS-NY). If it is found that the applicant/participant does not require a nursing facility LOC as indicated by the second LOC assessment, then the RRDC will issue a NOD Denial of Waiver Program to the applicant, or a NOD Intent to Discontinue from Waiver Program (DOH-5738) to the waiver participant.- The applicant must select a Service Coordination provider who will assist the applicant in the completion and submission of an Application Packet, including the Initial Service Plan (refer to section C below - Application), in cooperation with the Service Coordinator. This Initial Service Plan (ISP) must describe why the individual is at risk for nursing home placement without the provision of waiver services and indicate how the available supports and requested waiver services identified in the ISP will prevent institutionalization. Upon entry into the waiver program, the participant must participate in monthly service coordination in order to maintain their waiver eligibility (see section C below - Referral, Intake, Application, and Determination processes).
- Included in the Initial Service Plan, the applicant must have a completed Plan for Protective Oversight (PPO). Additionally, the applicant must be capable of directing their service plan or has a legal guardian or other duly designated health care agent available to direct the participant's service plan development and participation.
- Informal supports and Medicaid state plan and waiver services must be sufficient to safely serve the individual in the community. The individual must be able to live in the community with the services and supports available through the waiver and other resources without compromising their health and welfare, as determined by the Regional Resource Development Specialist (RRDS). Informal supports will be used to supplement waiver and state plan services whenever possible.
- Entrance to the waiver is further based on confirmation that the applicant chooses to participate in waiver services, completion of a service plan and applicable forms signed by the applicant, and confirmation that the applicant can be safely and appropriately cared for in a community setting. Applicants are enrolled in the NHTD program only when all necessary services are in place, and the health and welfare of the individual can reasonably be assured.
B. Issues That Impact Eligibility
An individual currently residing in or planning to reside in a facility certified under the Assisted Living Program (ALP) or other licensed or certified congregate care setting is not eligible for the NHTD waiver.
In addition, Medicaid regulations will not allow for duplication of services. Therefore, an individual enrolled in a Health and Recovery Plan (HARP), Health Homes, Managed Long Term Care Program (MLTC), a Program of all Inclusive Care for the Elderly (PACE) or receiving Comprehensive Medicaid Case Management (CMCM) through a targeted case management program is not eligible for the NHTD waiver unless they are disenrolled from the applicable programs. These managed care members must seek voluntary disenrollment from the plan and the managed care plan codes must be removed from the applicant's eMedNY profile before the effective date for waiver eligibility. Waiver services may not be billed while an applicant/participant is enrolled in one of these managed care products. The provision of care management/case management/service coordination cannot be duplicated.
The NHTD waiver may not serve individuals who would, but for the waiver, receive services in an Institution for Mental Disease (IMD).
NOTE: Forms are available in accessible formats upon request.
C. Referral, Intake, Application, and Determination Processes
The following describes the process for becoming a waiver participant:
Referral
A potential participant (applicant) or someone acting on their behalf, contacts the Regional Resource Development Center (RRDC) serving the region in which the individual resides or is seeking to reside. This communication may be completed via phone, email, or other correspondence. The date of first contact made to the RRDC from a potential participant, or someone acting on their behalf, is referred to as the referral date. The RRDC staff completes and signs the Referral form (DOH-5747).
There is an individual in the RRDC to accept and monitor referrals in the office. All calls/communication initiating referrals must be returned and documented within five (5) business days of the referral date and the RRDC continues to complete the Referral form with any additional information obtained. The call will confirm basic referral information such as phone number, address, CIN, etc.
It must first be confirmed that the individual is seeking waiver services and/or consents to the referral. Based on the response, the RRDC then determines whether to proceed to the intake process. For example, if the individual responds they are not interested in receiving services or they did not agree with the referral, the process terminates. During the call the RRDC will confirm that the individual meets the basic eligibility criteria to continue the intake process. If the individual does not meet the basic criteria for the waiver (e.g., the individual does not have the appropriate Medicaid for home and community-based services (HCBS), is under the age of 18 or indicates their preference not to pursue admission into the NHTD waiver program), the RRDC staff will confirm the referral will not move forward to intake and a letter will be provided to the individual within five (5) business days of the date of last contact (referral close-out date). This notification is a letter confirming the conversation and advises the individual of the opportunity to seek waiver services at a later date when basic eligibility criteria changes or individual's choices change. Included in this communication will be information about other programs/services, if appropriate. The RRDC must offer the potential applicant an Intake appointment within ten (10) business days of contact (date of referral contact).
NOTE: Applicants requiring spousal budgeting in order to meet Medicaid eligibility for waiver services will be referred to the LDSS for consideration prior to the referral moving to intake. The RRDC will provide the LDSS notification of the applicant's intent to seek waiver eligibility and apply spousal budgeting.
If the individual appears to meet the basic criteria during the initial call (age, Medicaid eligibility, physical disability) for the waiver, the RRDC will schedule the intake meeting or contact the individual at a later time via phone to schedule the intake. If the individual is unreachable by phone after two attempts, the RRDC will contact the individual in writing. This contact will be to schedule the intake. The letter will be addressed to the applicant, and if a nursing home resident, the discharge planner and/or Open Doors Transition Specialist will be copied. If the applicant does not respond to this letter within 10 business days, the RRDC will send a letter advising that the referral will not proceed to intake because the outreach attempt was unsuccessful.
For those proceeding to intake, an Intake meeting must be scheduled within thirty (30) calendar days of the date of last contact. The Intake meeting may include anyone the applicant chooses to be present. Any action, such as referral for housing or referral for additional assessments taken as a result of the intake meeting, must include notification to the legal guardian.
If the individual has a Legal Guardian or other duly designated individual, documentation of the authority to make decisions on behalf of the individual must be produced at the Intake meeting. If documentation cannot be secured by the date of the Intake meeting and the meeting was held, the RRDC staff will notify the applicant in writing after the Intake meeting that the application cannot proceed without the required document(s). If the documentation is not secured prior to the applicant's service coordination agency selection, the agency selection cannot proceed until the documentation is secured. The RRDC will issue a Notice of Decision (NOD) Denial.
If an Intake meeting was scheduled and the individual postpones the proposed Intake meeting on multiple occasions or for a period exceeding sixty (60) days from the date of referral, the applicant will be contacted in writing by the RRDC advising that due to the meeting cancellations, the referral will not proceed to Intake. The applicant may re-initiate referral at any time (a new referral is not required).
Waiver applicants/participants with limited fluency in English must have access to services without undue hardship. RRDC staff will take action to provide interpretation or translation services for applicants/participants who require these services. This may be accomplished through a variety of means, including employing bi-lingual staff, resources from the community (e.g., local colleges), and contracted interpreters.
Applicants/participants who speak a primary language other than English may bring a translator of their choice with them to meetings with waiver providers and/or the RRDS. However, applicants/participants are not required to bring their own translator, and applicants/participants cannot be denied access to waiver services on the basis of difficulty in obtaining qualified translators.
A complaint line is established for applicant/participants to call if they believe their rights related to waiver services are being violated. All calls will be investigated promptly.
The RRDC will maintain ongoing progress notes regarding the status of the case on the Referral Form. All Referral and Intake information will be tracked in the regional database.
Intake
The Regional Resource Development Specialist (RRDS) provides detailed information to the applicant and/or legal guardian during the intake process regarding the purpose of the NHTD waiver, the philosophy of the NHTD waiver, available services, the application and service plan development process, role of the Service Coordinator (SC), a list of available service coordination providers, and the complaint and Fair Hearing processes. The RRDC staff provides information regarding the Notice of Decision (NOD), Informal/Case Conference, and Fair Hearing processes. Additionally, upon selection, the Service Coordinator ensures that the waiver applicant understands their rights regarding Informal/Case Conferences and Fair Hearings as they proceed through the waiver enrollment process, and throughout the duration of the participant's waiver enrollment.
The RRDC staff completes the Intake form (DOH-5725) at the meeting with the applicant/Legal Guardian. Both the RRDC staff and the applicant/Legal Guardian then review and sign the form.
The RRDC staff must follow Health Insurance Portability and Accountability Act (HIPAA) compliance policies. The applicant and/or their Legal Guardian and a witness will complete and sign the Release of Information form.
The RRDC staff then reviews the Application for Participation, Initial Applicant Interview Acknowledgment (DOH-5729) and the Freedom of Choice forms (DOH-5728) with the applicant at the Intake meeting and has the applicant and the Legal Guardian sign the forms. All forms must be executed prior to the close of the Intake meeting.
Should it be discovered during Intake that the applicant is ineligible for the waiver: e.g., Medicaid eligibility has been suspended or indicates their preference not to pursue admission into the NHTD waiver program, the RRDC staff will provide available options for referrals to other programs/services. The RRDC staff closes the Intake process and issues a NOD Denial (DOH-5734) within ten (10) business days of the Intake meeting. Options for alternate services and/or resources will be included with the NOD.
The New York Association of Independent Living (NYAIL) is contracted by the Department of Health to provide the Open Doors program. Open Doors seeks to increase home and community-based services (HCBS) reduce the use of institutional services and support individuals with disabilities living in the community. Independent Living Center (ILCs) are disability-led grassroots organizations providing advocacy and supports to assist people with disabilities of all ages to live independently and fully integrated in their communities. NYAIL's Open Doors Transition Centers have transition specialists at ILCs across the state to directly assist people in nursing homes access the services they need to return to the community. The transition specialists also work with people to access needed supports and services in the community. This includes providing people with objective information about services and supports that are available in their local community. Additional information can be found at: The New York Association on Independent Living (NYAIL) Open Doors Transition Center. If the applicant is a nursing home discharge, the RRDC will confirm if the referral is known to the Open Doors Program. Upon consent of the applicant, the RRDC may share the referral information with Open Doors.
If the RRDC staff determines potential eligibility (e.g., the meets the basic eligibility criteria of age and Medicaid eligibility) and the applicant indicates their continued interest in pursuing admission into the NHTD waiver program, then the Intake process continues. Prior to the close of the Intake meeting RRDC staff will provide the applicant with a current list of approved and available service coordination agencies, and the Service Coordination Agency Selection form (DOH-5727). The RRDC will discuss the service coordination agency selection process with the applicant at the Intake meeting. The RRDC updates the Service Coordination list weekly. Although the provider has indicated an interest in providing services, the list does not guarantee provider availability or the provider's willingness to accept the case. If the provider has indicated that they are currently not accepting new cases, the name of the agency will be removed from the list until the provider notifies the RRDC of their availability. The RRDC will update the list anytime there is a change in providers and/or provider status. Throughout the service coordination selection process, the RRDC will encourage the applicant to interview potential service coordination agencies. Should the applicant indicate that they will require assistance with the selection of a service coordination agency, the RRDC will attempt to contact the applicant via phone to provide assistance, as needed. If contact by phone is not successful, the RRDC will attempt contact via other means, including a letter.
From the date of the Intake meeting, the applicant will have an initial thirty (30) days to initiate service coordination selection. Within the first fourteen (14) days, the applicant is expected to begin contacting and interviewing possible SC providers. The Nursing Home Discharge Planner, Open Doors Transition Specialist and/or family members may assist with this process. The RRDC will confirm within the first fourteen (14) days that the applicant has initiated the search process. If the RRDC does not receive a completed Service Coordination Agency Selection form within thirty (30) days of the intake meeting, the RRDC will contact the applicant to assist in selecting a service coordination agency. If the RRDC is unable to contact or discuss the selection of a service coordination agency with the applicant, it may determine that an NOD Denial is warranted or continue to assist the applicant with the selection process. Using data generated from the monthly referral and intake report, for those applicants pending service coordination selection for seventy-five (75) days or greater, NYSDOH will complete an audit of a sample to determine the reason for the delay.
An additional thirty (30) days may be provided to select a service coordination provider. At the end of the additional thirty (30) day period, the RRDC will reach out to the applicant to check on the status of their service coordination agency selection. Upon selection of a service coordination provider by the applicant, the Service Coordination Agency Selection form is sent to the RRDC within sixty (60) days of the Intake meeting, and the Intake process shall continue. Any approved support assisting the applicant with selection of a service coordination provider may forward the Service Coordination Agency Selection form to the RRDC. If the form is not timely received by the RRDC, the RRDC will contact the applicant to confirm the status of service coordination selection. If the applicant indicates they are still having a problem securing a Service Coordinator, the RRDC will help to facilitate the selection process.
Within two (2) days of receipt of the Service Coordination Agency Selection form from the applicant, the RRDC sends the Service Coordination Agency Selection form to the requested service coordination provider.
If the service coordination agency is willing and able to accept the potential participant, the agency assigns a Service Coordinator to the potential participant and an appropriate agency representative signs the Service Coordination Agency Selection form and returns it to the RRDC within five (5) business days of receipt of the form.
Upon receipt of the form, the RRDC approves the provider by signing the Service Coordination Agency Selection form and returns the form and Freedom of Choice form to the service coordination agency. If the applicant has a legal guardian, the guardianship information is also included. The applicant will receive written confirmation from the RRDC of the provider selection.
If, within the five (5) business days, the service coordination provider does not respond to the RRDC formally accepting the case, the RRDC will advise the applicant that the selection has not yet been approved. The RRDC will contact the provider to confirm the status of the provider selection request. If the provider is not going to proceed with accepting the case, the RRDC will contact the applicant via phone to provide assistance in selecting a new service coordination agency. If contact by phone is not successful, the RRDC will attempt contact via other means, including a letter. During contact, the RRDC will provide the applicant with an updated service coordination provider list, excluding the prior provider, and including a new Service Coordination Agency Selection form. The applicant will have an additional fourteen (14) days to select another provider. At the end of the fourteen (14) day period the RRDC will contact the applicant to confirm the status of their selection of a service coordination provider agency. If no service coordination agency has been selected or is available to provide services, the RRDC staff closes the Intake process, and the applicant will be issued an NOD Denial. If the applicant indicates continuing interest in the program, the RRDC may determine not to issue an NOD Denial and will continue working with the applicant to secure a service coordination provider. The NOD will be sent to the applicant with fair hearing rights and a copy to the NH Discharge Planner/Open Doors Transition Specialist, if applicable. An applicant is not barred from applying to the program in the future or seeking referral to other resources such as Managed Long Term Care (MLTC). An applicant may seek to re-apply for waiver services at any time.
NOTE: Applicants will not be denied solely based on service coordination provider or RRDC failure to meet deadlines in the intake and/or initial application process.
Application
The Service Coordinator (SC) assists the applicant in securing waiver eligibility, coordinates service provision, and monitors the delivery of all services in the service plan. Services may include Medicaid State Plan services, non-Medicaid federal, state and locally funded services, as well as educational, vocational, social, and medical services. Additionally, the SC must ensure the timely completion of the assessment or if an assessment is not available, secure the completion of the assessment. This information secures the individual's level of care and on-going development and review of the service plan.
The complete Application Packet contains the following:
- Application for Participation (DOH-5729) - completed with the RRDC staff;
- Waiver Participant Rights and Responsibilities;
- Level of care assessment - UAS-NY if in the community, or H/C PRI and SCREEN if in a nursing facility or hospital;
- ISP;
- Provider Selection form(s);
- Plan of Protective Oversight (PPO);
- Proof of Physical Disability Determination (if under age 65);
- Freedom of Choice (DOH-5728) - completed with the RDDC staff;
- Service Coordination Agency Selection (DOH-5727) - completed with the RRDC staff;
- NHTD Participant Instructions for the Complaint Process (DOH-5729);
- NHTD Medicaid Waiver Initiative;
- Current and appropriate Medicaid eligibility has been verified; and
- The individual meets the age requirement upon application.
The Initial Service Plan (ISP) addresses many aspects of the applicant's life, including safety, independent living skills, and medical and cognitive needs. As a result, family members, friends, and informal supports are encouraged to provide input into the applicant's service goals. The applicant may include any person of his/her choosing to assist in the development of the service plan.
The ISP contains an assessment of the individual's strengths, limitations, and goals. It identifies what services are necessary to support and maintain the individual in the community. For waiver applicants residing in a nursing/rehabilitation facility or hospital, the ISP includes current summaries of all services provided and a discharge summary from the facility, including relevant medical reports and assessments.
The assessment also includes an evaluation of risk factors that will be addressed in the Plan for Protective Oversight (PPO). The PPO explicitly states the individuals who are responsible for assisting the participant with daily activities/emergencies, medication management, financial transactions, fire/safety issues, and back-up plans are also included. The PPO establishes a plan to reduce risk and address safety issues. The PPO addresses back-up issues for activities that are directly related to health and welfare.
The Uniform Assessment System New York (UAS-NY) not only establishes nursing facility LOC, but also offers a summary of the individual's strengths, weaknesses, and level of functioning. This information is incorporated into the service plan as identified training or support goals. The UAS-NY, or PRI (if in a nursing facility) is completed within required time frames, identifies the applicant as needing a nursing home Level of Care (LOC score of 5 or greater) and that the home environment is the appropriate setting for the participant to receive services.
Assessments are completed by service providers or additional outside assessments and may be procured on behalf of the applicant/participant. The RRDC reviews each service plan to assure it meets the assessed needs of the applicant and reflects choice.
During Initial Service Plan development, risk factors and safety considerations are identified by the Service Coordinator (SC), the applicant, family members, and treating professionals. Interventions or assistive technology devices, or environmental modifications to minimize isolation, are incorporated into the service plan with consideration of the participant's assessed preferences. Individuals, family members and/or designated others participate in the service plan development to assure identification of realistic strategies that will mitigate foreseeable risk with consideration of the participant's unique desires and goals. All available informal supports and non- waiver services are utilized wherever appropriate.
When the waiver applicant's choices are such that the waiver program will not be able to assure their health and welfare in the community, the RRDC may deny waiver services. The waiver participant may present a risk to themselves, staff, family, and informal supports. This concern is discussed with the applicant. If the applicant's health and welfare can be assured, and services are in place at the time of eligibility, then the waiver application can proceed. If this is not possible, then the applicant is issued a Notice of Decision (NOD) of Denial with Fair Hearing rights attached.
If there is a delay in Application packet submission, the RRDC will contact the Service Coordinator to confirm what the reason is for the delay in submitting the application (e.g., locating housing). Service Coordinators are expected to respond within twenty- four (24) hours from this contact to respond with the reason for the delay. If the Service Coordinator does not call back within twenty-four (24) hours, the RRDC will follow up directly with the applicant. The RRDC will document the contact in a case note.
If during the development of the ISP it is determined that the applicant cannot identify a residence where waiver services are to be provided, the plan development will be suspended until a residence is identified. The Service Coordinator may assist the applicant in identifying a residence. Additionally, Community Transitional Services or Environmental Modifications may be utilized as a mechanism to support applicants in this endeavor if they are transitioning from a nursing home. If it becomes apparent that a living arrangement is not forthcoming within 60 days of the RRDC's approval of the service coordination provider, the RRDC issues a NOD Denial.
Waiver services cannot be initiated without an approved service plan and approval by the RRDC. Waiver service providers may only bill for waiver services upon waiver eligibility and at the time-of-service provision.
If, during plan development and application period, the service coordination provider is unable to continue providing services, the service coordination agency must issue a 30- day letter notifying the applicant in writing and including the reason for discontinuation of the service indicating they can no longer assist the applicant with waiver enrollment. This letter must note the date service will be discontinued and cannot be retroactive.
The RRDC also receives a copy of the letter. Upon receipt of the letter, the RRDC notifies the applicant that they must select another service coordination provider and provides the applicant an updated approved service coordination provider list, excluding the current provider. A new Service Coordination Agency Selection form will be included with the list. The RRDC will contact the applicant within fourteen (14) days to review the status of their new service coordination provider search. The applicant will have a total of an additional thirty (30) days from the receipt of the updated service coordination provider list to select a provider. If a new provider cannot be identified within that timeframe with the assistance of the RRDC, or the applicant fails to select a new service coordination agency, the RRDC issues a NOD Denial.
The waiver applicant has the right to select a new service coordination provider at any time during the application process.
Determination
The RRDS reviews the completed Application Packet, which includes the ISP, and either approves the Packet or sends the RRDS ISP Review form to the Service Coordinator with a written request for revisions and/or additional information needed for approval. The service plans submitted for potential participants who have medically complex cases must be reviewed by the RRDS and the NE. The final decision for waiver eligibility rests with the RRDC and is confirmed with a Notice of Decision (NOD). A Notice of Decision (NOD) is a written document that notifies an applicant/participant of an action being taken by the waiver program, including an explanation of the reasons for the action.
The RRDC will review the applicant´s Initial Service Plan, Plan of Protective Oversight, UAS-NY documentation, confirm Medicaid eligibility, guardianship status, and completed application packet. The RRDC has 14 days after receiving the complete application package to make an eligibility determination. The applicant will be determined eligible or provided a reason why they are not eligible via the NOD.
If approved for waiver services, a NOD Authorization (DOH-5740) is issued to the applicant by the RRDC. This NOD indicates the effective date of enrollment into the NHTD waiver program for the participant. The RRDC also forwards a copy of the Authorization NOD to the LDSS and to the Service Coordinator. Upon receipt of the NOD, the LDSS inputs program Restriction/Exemption (R/E) code 60 (NHTD) into the Welfare Management System (WMS)/eMedNY. The Service Coordinator is responsible for sending a copy of the NOD to all NHTD waiver service providers authorized in the approved service plan. A NOD Authorization cannot be effectuated until any existing Restriction/Exemption code that excludes NHTD waiver services is removed from the applicant's electronic record. Each waiver service identified in the service plan is approved upon approval of the service plan and the issuance of the NOD Authorization. Services are authorized based on the frequency and duration identified in the service plan.
A NOD Denial is issued to the applicant at any point in the application process when the RRDC determines that the individual is not eligible for waiver services and indicates the reason(s) for denial.
If, at any point during this process, the RRDC determines that the applicant cannot be safely served in the community with the services and supports available through the waiver and other resources, the RRDC will issue a NOD Denial.
If, at any point during the referral and intake process, an applicant chooses to relocate to a region covered by another RRDS, the current RRDC is responsible for making the initial contact with the RRDS in the relocation region. The RRDS from the new region will contact the applicant to provide the list of current approved service coordination providers in that region.
The RRDS is responsible for assuring the correct NOD is completed and sent out to each applicant/participant, legal guardian (if applicable), Authorized Representative (if applicable), Service Coordinator, NHTD waiver staff, and LDSS, as specified on the bottom of each form.
Applicants/participants have sixty (60) days from the date of the notice to request a Fair Hearing. OTDA notifies the appellant of the time and place of the hearing at least ten (10) calendar days prior to the hearing date.
The Service Coordinator provides follow-up in this process by contacting the applicant/participant to discuss the reasons for the NOD and to assure their understanding of the right to request an Informal/Case Conference and/or Fair Hearing (with aid continuing, if appropriate). The applicant/participant is also notified of their right to be represented by legal counsel, a relative, a friend or other person or to represent themselves. The applicant/participant is advised that they may be able to obtain legal assistance by contacting the Legal Aid Society or other legal advocacy groups. The Service Coordinator is responsible for sending a copy of the NOD to all waiver service providers in the Service Plan.
Applicants/Participants may request a Fair Hearing by calling a statewide toll-free number (1-800-342-3334), faxing a copy of the notice (on the back of the NOD) to OTDA, or by mailing the request to OTDA.
NOTE: Individuals placed out-of-state who have NYS Medicaid and are seeking waiver services proceed through the same referral, intake, and eligibility review process. RRDC staff, Open Doors Transition Specialists, and Service Coordinators travel to meet with out-of-state applicants and complete the eligibility process.
Section III: Becoming a Waiver Provider
Introduction
The NHTD waiver program is committed to providing high quality and cost-effective services offered through qualified waiver service providers. This section describes the waiver service provider's qualifications, the waiver service provider's responsibilities, steps in the application process, subcontracts, termination of contracts and housing.
The final Home and Community-Based Services (HCBS) regulations (known as the "Final Rule") were published in the Federal Register on January 16, 2014; they became effective March 17, 2014.
The regulation is designed to enhance the quality of HCBS, provide additional protections, and ensure full access to the benefits of community living. The intent is that individuals receiving Medicaid-funded HCBS have the opportunity to receive these services in a manner that protects individual choice and promotes community integration. All NHTD waiver service providers must meet this compliance criteria.
Home and Community-Based Settings Requirements
HCBS must be delivered in a setting that meets home and community-based setting requirements as set forth in the federal rule. Waiver participants must be living in and receive services in settings that comport with the HCBS setting requirements. Private residences where individuals receive Medicaid funded services are assumed to comply with the regulatory criteria. CMS considers the term "private home" to be "a residence owned or leased by an individual for his or her personal use".
Settings that are not Home and Community-Based are specified in the Final Rule:
- Nursing Facility
- Institution for Mental Disease
- Intermediate Care Facility for Individuals with Intellectual Disabilities
- Hospital
- Other locations that have qualities of an institutional setting, as determined by the Secretary
The regulations identify other settings that are presumed to have institutional qualities and do not meet the requirements for Medicaid Home and Community-Based Settings:
- Settings in a publicly or privately operated facility that provides inpatient institutional treatment.
- Settings in a building on the grounds of, or adjacent to, a public institution.
- Settings with the effect of isolating individuals receiving Medicaid HCBS from the broader community of individuals not receiving Medicaid HCBS.
Individuals receiving waiver services reside in their own home, residential settings of four or more unrelated individuals are excluded. Waiver participants residing in a setting of four or more unrelated individuals at the time of the approval of the waiver application will remain under the old criteria until they move, or the state transition plan is fully implemented.
The services and supports available through the waiver and other sources must be sufficient to maintain the individual's health and welfare in the community. The living environment must be fully integrated into the broader community and selected by the participant.
Waiver services provided outside the home should not be in a consolidated/congregate location or on the grounds or immediately adjacent to a public institution. New York State continues to move forward with its statewide transition plan to be fully compliant with the federal rule.
NYSDOH and the RRDCs are responsible for monitoring for Home and Community- Based Services (HCBS) settings compliance. Monitoring for compliance with the federal home and community-based setting requirements is in addition to, and does not replace, the waiver assurances for monitoring that are part of the HCBS 1915(c) waivers. All providers must meet HCBS settings requirements at the time of provider application. All existing waiver service providers must be in full compliance by March 17, 2023.
The NHTD Waiver application requires that waiver services cannot be provided in residences of four or more unrelated individuals.
A. Qualifications for Provider Agencies
All waiver service providers, including those already approved to provide services under the Medicaid State Plan or another Medicaid waiver are required to also be approved as an NHTD waiver service provider. Waiver service providers must be located in and able to provide services in New York State. Waiver service providers must meet all licensure and other qualifications of the service(s) they are applying for as specified in this Program Manual (refer to Section VI - Waiver Services). The specifications for waiver service providers are established in Appendix C of the approved 1915(c) waiver application.
In order to remain on the active provider list which is provided to applicants/participants for waiver service selection, the provider must be ready, willing and available to accept new cases.
Waiver service providers are responsible for knowing, understanding, and implementing the waiver in accordance with the policies and procedures established in this Program Manual, the approved 1915(c) waiver application and any updates or changes generated by NYSDOH. Waiver service providers are also responsible for knowing, understanding, and implementing the waiver in accordance with required billing and documentation standards established by CMS, NYSDOH, eMedNY and monitored by the Office of the Medicaid Inspector General (OMIG).
Waiver service providers may request approval to provide all waiver services for which they qualify in more than one region. The approval process to add services or regions supplements the initial application process (an eMedNY application is only required with the initial application). The provision of all services must be in full compliance with Conflict-of-Interest (COI) requirements (42 CFR 431.301(c)(1)(vi)) that were implemented by CMS on March 17, 2014.
Upon the provider's signature on the Provider Agreement form, the waiver service provider must report any subsequent change(s) in status to NYSDOH and its designees (RRDC). These changes may include: change of ownership and control; change of agents, managing employees and those with a controlling interest; change of address; and change of provider contact information. The provider, as the employer of waiver service staff, is responsible for verifying that the individual(s) maintain the needed license, registration or certification throughout the period of time they provide waiver services and are employed by the provider. The RRDC, Waiver Unit staff, NYSDOH Office of Primary Care and Health Systems Management (OPCHSM) surveillance staff and/or NYS Office of the Medicaid Inspector General (OMIG) staff verify employee qualifications and certifications through surveys and/or audits.
If at any time a waiver service provider is unable to maintain qualified staff, it will not be able to provide the service(s) performed by such staff. The waiver service provider must report any changes in staffing status to the appropriate RRDC. Waiver service providers must ensure that all provision of waiver services is completed by staff who meet the qualifications in this manual and the approved 1915(c) NHTD waiver application upon applying to become a waiver service provider and throughout the time-of-service provision. These requirements should be reviewed by the provider for all staff at least annually to ensure on-going compliance. Documentation of required staff qualifications must be maintained by the waiver service provider. Documentation may include: resume(s), license(s), registration and/or certification. This documentation is supported by the Employee Verification of Qualifications (EVQ) form and must be available upon audit, request and/or investigation by authorized agents.
Waiver service providers must adhere to all Medicaid confidentiality and Health Information Portability and Accountability Act (HIPAA) requirements and ensure the privacy of the waiver participant. Waiver service providers must adhere to all responsibilities and conditions delineated in the Provider Agreement.
B. Provider Responsibilities
- Agencies applying to provide Assistive Technology (AT), Community Transitional Services (CTS), Congregate and Home Delivered Meals, Environmental Modifications Services (E-mods), Home Visits by Medical Personnel, Moving Assistance and Respiratory Therapy must:
- Ensure participant's right of choice;
- Establish and maintain current safety and emergency policies and procedures;
- Establish and maintain personnel files on every employee, including resumes and job descriptions. If a waiver service provider has more than one office and the personnel files are housed in the main office when the other office(s) is/are surveyed by the New York State Department of Health (NYSDOH), the personnel files need to be provided to the surveyor(s) at the location being surveyed if requested by the surveyor(s);
- Have basic knowledge of the NHTD Waiver's Incident Reporting Policy regarding Serious Reportable Incidents (SRI) (refer to Section X - Incident Reporting Policy and Complaint Procedure), including the obligation to report to the Service Coordinator and to cooperate with the RRDC staff investigating a SRI;
- Establish and maintain a documentation system to ensure staff is providing the expected amount/type of service in accordance with the participant's Service Plan. This system must include documentation of date, type and to whom the service is provided;
- Establish and maintain a process for surveying participant satisfaction. This process includes obtaining information from the participant about their satisfaction with the services provided, whether the staff was able to make appointments, whether staff was on time for appointments and whether services were provided as agreed upon. This data will be summarized each calendar year. Satisfaction surveys are to be completed by the individual provider and the RRDC;
- Establish and maintain a method for recording and addressing complaints made by the waiver participants, families, legal guardians and others. This information must include the number and types of complaints made/received, including an analysis of these complaints and the waiver service provider's response to them and reported to the RRDC each calendar year;
- Establish and maintain a file for each participant served including: a copy of the Notice of Decision (NOD), the first page of the Service Plan and the page(s) describing the need for the requested waiver service(s) as provided by the Service Coordinator and approved by the RRDC and approved projected and final cost report forms. All services must be included in the participant's service plan and approved by the RRDC prior to the start of service provision; and
- Cooperate with NYSDOH, Office of Medicaid Inspector General (OMIG) and other government agencies with jurisdiction to conduct surveys and audits.
- Agencies applying to provide all other waiver services must satisfy the following conditions:
- Ensure participant's right of choice;
- Compliance with Conflict-of-Interest (COI) requirements;
- Establish and maintain current safety and emergency policies and procedures;
- Establish and maintain personnel files on every employee including resumes, job descriptions, licensure and training certifications, employee verification of qualification forms. If a waiver service provider has more than one office and the personnel files are housed in the main office, when the other office(s) is surveyed by NYSDOH, the personnel files must be provided to the surveyor(s) at that location if requested);
- Follow the NHTD Serious Reportable Incident (SRI) Policy and Procedure (refer to Section X - Incident Reporting Policy and Complaint Procedure);
- Establish and maintain policy and procedure for documenting Recordable Incidents (refer to Section X - Incident Reporting Policy and Complaint Procedure);
- Establish and maintain a tracking system to ensure that the staff is providing the expected amount/type of service in accordance with the participant's approved service plan;
- Establish and maintain an accurate system for documenting the goal/outcome of the service provided, the time and date of the service(s) provided and the date billed;
- Establish and maintain a method for self-appraisal of service provision including accepting suggestions and formulating methods for improvement;
- Establish and maintain a process for surveying participant satisfaction. This process includes obtaining information from the participant about their satisfaction with the services provided, whether the staff was able to make appointments, whether staff was on time for appointments and whether services were provided as agreed upon. This data will be summarized each calendar year. Satisfaction surveys are to be completed by the individual provider and the RRDC.
- Establish and maintain a method for recording and addressing concerns and complaints made by the waiver participants, families, legal guardians and others; this information must include the number and types of complaints made/received, including an analysis of these complaints and the waiver service provider's response to them;
- Establish and maintain records which include functional assessments, goals specific to the service, proof of the authorization of the service, Detailed Plans, notation of each participant encounter/contact and related billing, copies of all service plan related documents including Individual Service Reports (ISRs), team meeting summaries, documentation of all communication with the Service Coordinator, NODs, Contact sheet, Plan of Protective Oversight, and the current Waiver Participant Rights and Responsibilities (DOH-5732);
- Provide training using a curriculum approved by the RRDC and update the subject matter as directed by NYSDOH and/or the RRDC;
- Cooperate with the NYSDOH, OMIG and other state and federal agencies with jurisdiction to conduct surveys and audits; and
- Establish internal protocols and provide staff training as established by NYSDOH.
All approved waiver service providers are responsible for advising the appropriate RRDC and NYSDOH in writing of any agency changes. Notification must be submitted as soon as the agency is aware that such a change will occur. Examples of agency changes include but are not limited to: change of ownership and control; change in managing employees change of address; and change of provider contact information.
C. Provider Meetings
Each RRDC will hold at least eight (8) provider meetings each year. Meetings may be held in-person or through indirect means such as webinars and teleconferences. This will be at the discretion of the RRDC. Approved waiver service providers must attend at least eight (8) scheduled provider meetings in each region in which the waiver service provider is approved. These meetings address policies and procedures relevant to the health and welfare of the participants and provide critical updates related to the NHTD waiver. It is also an opportunity for waiver service providers within each region to share ideas, trends and issues. Failure of a provider to meet attendance requirements, as documented by the RRDC, will lead to restrictions in the provision of waiver service(s) and/or termination. The RRDC is required to maintain internal documentation to support proof of attendance which will be made available for audit and surveillance purposes. Attendance at provider meetings must include management and supervisory level staff.
The following providers are exempt from attending the mandatory provider meetings, unless the RRDC deems that the meeting is relevant to the waiver provider and informs them that their attendance is required:
- Assistive Technology (AT)
- Community Transition Services (CTS)
- Moving Assistance (MA)
- Congregate and Home Delivered Meals
- Environmental/Vehicle Modifications
- Home Visits by Medical Personnel
- Respiratory Therapy
NOTE: If a waiver staff person is employed at more than one waiver service agency, they may only represent one agency when attending provider meetings.
D. Application Process
The following steps describe the application process for becoming a waiver service provider:
Step 1: Provider Inquiries
The potential waiver service provider for the NHTD waiver will contact the RRDC in the region they are interested in providing services. A formal Letter of Intent must be submitted to the RRDC before any application can proceed.
Letter of Intent (on agency letterhead, signed and dated by management) must contain:
- A description of the agency's history of providing services to individuals with disabilities and/or seniors. If experience is limited, a description of how the agency proposes to develop the expertise to effectively provide services to NHTD participants must be included;
- A list of service(s) which the potential provider is seeking approval to provide; and
- Identification of the RRDC region(s) (and counties if applying for HCSS and/or Respite where licensed) where seeking to provide services.
After receipt of the Letter of the Intent by the potential waiver service provider, the RRDC will contact the provider within fifteen (15) days of receipt of the letter to discuss the application process, supply a copy of the NHTD Provider Agreement and Employee Verification of Qualifications (EVQ) form(s).
The potential waiver service provider must return the signed Provider Agreement to the RRDC indicating their continued intent to become a waiver service provider within thirty (30) days or the application will be identified as closed. The RRDC will advise the provider in writing of the closure.
After receipt of the signed Provider Agreement from the potential waiver service provider, the RRDC will forward the Letter of Intent and signed Provider Agreement to NYSDOH. Concurrent with the submission of the Letter of Intent and Provider Agreement, the potential waiver service provider must complete a "New York State Medicaid Enrollment Form" for Institutions and Rate-Based Providers (EMEDNY- 436601) to obtain a Medicaid Management Information System (MMIS) Provider ID. Waiver services may not be provided without this ID and assigned rate codes. The Category of Service for Respiratory Therapy and Home Visits by Medical Personnel is 0260; The Category of Service for all other waiver services is 0263. The eMedNY application and additional documents as outlined in the instructions as applicable to the provider, will be mailed directly to eMedNY. Refer to the Provider Enrollment section at www.emedny.org. A copy of the eMedNY application must be included in the provider enrollment package submitted to the RRDC.
After submission of the Letter of Intent, signed Provider Agreement and the eMedNY application, the potential waiver service provider will contact the appropriate RRDC(s) to continue the application process.
Step 2: Preparation for the Interview - Role of the RRDC
Each RRDC is responsible for recommending approval of the providers seeking to offer services in their region to NYSDOH. The RRDC must complete a preliminary interview and discussion with the potential provider. Provider interviews may be conducted in-person or via alternative means. The RRDC interview process is done concurrently with the processing of the eMedNY application.
Prior to arranging a formal interview, each RRDC will review the potential provider's policies and procedures. When a provider is seeking approval in two (2) or more regions, the RRDCs will conduct a collaborative review of the application documents and schedule a joint interview with the potential provider. Each RRDC must maintain a complete application packet of all providers approved, or seeking approval, in their region.
Agencies applying to provide Assistive Technology (AT), Community Transitional Services (CTS), Congregate and Home Delivered Meals, Environmental Modifications (E-mods), Home Visits by Medical Personnel, Moving Assistance and Respiratory Therapy must satisfy the following for policies and procedures:
- Maintain HIPAA compliance;
- Uphold safety and emergency procedures;
- Retain Human Resources policies/procedures;
- Have basic knowledge of Serious Reportable Incident Policy;
- Maintain a service provision tracking and billing system;
- Conduct participant satisfaction surveys;
- Address complaints and grievances from participants, advocates and family members;
- Record and address concerns/complaints of participants, the RRDC, Service Coordinator, and DOH waiver staff;
- Maintain recordkeeping/documentation for each participant;
- Cooperate with NYSDOH, OMIG and other government agencies with jurisdiction to conduct surveys & audits;
- Protocols for person-centered planning and procedures to protect participant choice; and
- Providers of Home Visits by Medical Personnel and Respiratory Therapy must also delineate protocols to ensure compliance with Conflict-of-Interest criteria.
Agencies applying to provide all other services must satisfy the following for policies and procedures:
- Maintain HIPAA compliance;
- Uphold safety and emergency procedures which include an "on-call" system;
- Establish Human Resource practices;
- Maintain a service provision tracking and billing system;
- Maintain participant communication logs;
- Plan for self-appraisal of service provision including accepting suggestions and formulating methods for improvement;
- Conduct participant satisfaction surveys;
- Handle complaints and grievances from participants, advocates and family members;
- Maintain a system for tracking serious reportable incidents and investigations;
- Form and maintain an Incident Reporting/SRI Committee;
- Protocols for quality assurance functions and service oversight;
- Delineate protocols to ensure compliance with Conflict-of-Interest criteria;
- Record and address concerns of the RRDS, Service Coordinator, and DOH waiver staff;
- Protocols for person-centered planning and procedures to protect participant choice;
- Maintain complete recordkeeping/documentation for each participant;
- Conduct waiver service training;
- Conduct additional training programs for staff; and
- Cooperate with NYSDOH, OMIG and other federal and state agencies with jurisdiction to conduct surveys & audits.
Note: HCSS providers must meet all Licensed Home Care Service Agency licensure and regulatory requirements.
During the preliminary interview, the RRDS(s) will review and discuss:
- The NHTD waiver, its philosophy and services;
- Home and Community-Based Services (HBCS) Final Rule federal regulation, how the regulation applies to the NHTD waiver program and how this Final Rule may affect the potential waiver service provider (i.e., Conflict-of-Interest, Person-Centered Planning and/or HCBS Settings requirements);
- The potential waiver service provider and complete applicable sections of the Waiver Service Provider Interview form;
- Qualifications of proposed staff for each service the provider is applying to provide; and
NOTE: A different staff profile must be submitted for each service. A staff profile may only be used for one provider per waiver service.- Training materials the provider will implement for each staff providing a specific waiver service (refer to Section VIII - Required Training for Waiver Service Providers). Providers may also choose to adopt NYSDOH training materials.
NOTE: Waiver service provider policies and procedures must be in place prior to the start of service provision.The potential waiver service provider will have ninety (90) days from the date of submission of their Letter of Intent (LOI) to complete an interview and submit a complete application packet to the RRDC. If the RRDC does not receive the complete documentation within ninety (90) days of receipt of the Letter of Intent and signed Provider Agreement, the RRDC will notify the provider that the application has been withdrawn. The provider will be advised that they may reapply at a later date by submitting a new Letter of Intent, a signed Provider Agreement and initiate the application process again.
Site Visits
Prior to submission of the final application packet to the NYSDOH, the RRDC must visit the proposed site for a Structured Day Program (SDP) and obtain a copy of the Certificate of Occupancy and Fire Inspection. The RRDC must obtain a copy of the SDP's sign-in/out policy which must follow the format outlined in Section VI - Waiver Services. The RRDC must also confirm that all service sites are compliant with the HCBS Settings Final Rule and will engage in activities to comply with HCBS Settings Federal regulation.
Providers must keep the RRDC and NYSDOH apprised of all service locations and any changes. Participant files must be available for inspection.
Step 3: Completing the RRDC Interview and Application Packet
The potential waiver service provider will work with the appropriate RRDC(s) to gather the following application packet contents:
- The Waiver Service Provider Interview form, which includes a Provider Address Grid and Employee Verification of Qualifications (EVQ) form(s). The Waiver Service Provider Interview form is completed during the in-person interview with the potential waiver service provider. When two (2) or more regions are involved in a joint application process, one (1) RRDC will lead by conducting the interview. The other RRDC(s) are required to participate in a joint interview. Each RRDC will complete Parts II, III and V of the Waiver Service Provider Interview form, region-specific EVQ form(s) and Address Grid. Providers seeking to provide the same service in multiple regions must present a different resume for each service in each region. The intent is that staff are available and ready to provide services at the time the provider is approved to offer services. During the interview, the RRDS(s) will:
- Interview the potential waiver service provider and complete the Waiver Service Provider Interview form;
- Review resumes of proposed staff and EVQ in comparison to provider qualifications established in the waiver application. (See Step 3.c. below for those waiver services that do not require an EVQ form.);
- Review training materials developed by the potential waiver service provider (refer to Section VIII - Required Training for Waiver Service Providers);
- Review the potential waiver service provider's policies and procedures that were submitted (refer to Step 2); and
- If the Provider is seeking to offer Structured Day Program Services, inspect the site to ensure HCBS settings compliance and occupancy, fire and safety requirements.
- All relevant potential waiver service staff of a potential waiver service provider must meet the staff qualifications listed within Section VI - Waiver Services and the approved NHTD waiver application. One (1) EVQ form must be submitted for at least one (1) qualified individual for each waiver service being requested. A separate EVQ form must be submitted for each waiver service being requested. The potential waiver service provider must select a different employee for each EVQ form submitted. An employee may only represent one employer/provider and waiver service. A resume highlighting relevant experience and proof of applicable qualifications (a copy of the diploma(s), license(s) and/or certification(s)) must be attached to the EVQ form(s). While an EVQ form is not needed for AT, CTS, Congregate and Home Delivered Meals or Moving Assistance, a copy of applicable contract and/or contractor(s) will need to be submitted to demonstrate adherence to waiver service qualifications. Once approved, providers are required to review staff qualifications for all staff on an annual basis and confirm they continue to qualify to provide assigned waiver services.
- A copy of the signed Provider Agreement form.
- A copy of the Federal Employee Identification Number (FEIN). The agency name on the FEIN documentation must match the agency name on the eMedNY application. The address on the FEIN must match one of the addresses on the eMedNY application (Independent providers are required to provide their social security number if they do not have a FEIN).
- A copy of the potential provider's licensure, certification, contract(s)/contractor(s) and/or any other requirements, as applicable, which support the requested waiver service(s) and satisfy the requirements for being a provider of the waiver service specified in the provider enrollment packet.
- A copy of the eMedNY "New York State Medicaid Enrollment Form" for Institutions and Rate-Based Providers (EMEDNY-436601) and additional forms as outlined in the instructions at www.emedny.org as applicable to the provider.
- Verification that a site visit has been completed for any applicable program site that requires HCBS settings compliance as outlined in the Final Rule.
Upon receipt of the complete provider application packet from the potential waiver service provider, the RRDC will make a recommendation for enrollment and must submit all required documentation to NYSDOH within thirty (30) days of receipt of the completed application package.
If documentation is not received by NYSDOH within one hundred twenty (120) days of the potential waiver service provider's signed Provider Agreement and Letter of Intent, the potential provider's application will be returned to the RRDC. At any point in time the potential waiver service provider may re-apply.
Step 4: RRDC Recommendations
The RRDC is responsible for making recommendations to NYSDOH regarding approval of the proposed waiver service(s) based on the applying agency's: personnel qualifications, capacity to develop and maintain high quality services, ability to meet federal requirements and the understanding of and willingness to adhere to the philosophy and policies of the NHTD waiver.
The RRDC must submit the completed Provider Enrollment Application Packet to NYSDOH waiver staff via e-mail, mail, or fax. The Waiver Service Provider Interview form describes the RRDS' decision and includes the RRDS' recommendations for whether to approve the potential waiver service provider and, if approved, which waiver service(s) the applicant will be approved to provide in that region.
If the potential waiver provider is applying to provide waiver services in more than one region, the applicable RRDCs will decide who will be the lead RRDC. The lead RRDC completes the interview as described in step 3 and will submit the fully completed Waiver Service Provider Interview form with the entire application packet to the NYSDOH waiver unit, this includes the lead RRDC's region-specific EVQ forms(s) and Address Grid. The other applicable RRDC(s) will only need to complete and submit to the NYSDOH waiver unit: Parts II, III and V of the Waiver Service Provider Interview form, the region-specific EVQ form(s) and Address Grid. Providers seeking to provide the same service in multiple regions must present a different resume for each service in each region. The intent is that staff are available and ready to provide services at the time the provider is approved to offer services.
If there is a difference of opinion between the potential waiver service provider and the RRDC about whether the waiver service provider should be approved and/or what services the waiver service provider will be able to provide, NYSDOH waiver staff will be responsible for the final decision.
Step 5: DOH Waiver Staff Decision
Once the complete application packet is received by NYSDOH, if any additional information, clarification, or corrections are needed, NYSDOH waiver staff will contact the RRDC and/or the potential waiver service provider to obtain such documentation. NYSDOH waiver staff audit employee qualifications against waiver requirements.
Prior to processing the application, NYSDOH waiver staff confirm that there are no adverse actions on record or pending regarding the provider: these actions may include but are not limited to surveillance deficiencies and pending corrective action plans, OMIG audits, action by the Office of Professional Conduct, licensure compliance by the NYS Department of Education etc.
Once the MMIS/Provider ID is assigned by the NYSDOH Bureau of Provider Enrollment and the application packet is approved, NYSDOH waiver staff prepares a Transmittal and Rate Sheet to upload approved rates to eMedNY for billing purposes.
NOTE : NYSDOH waiver staff notifies the Bureau of Provider Enrollment if additional Locator Codes need to be added for an additional RRDC Region or for the provision of the waiver service, HCSS. NYSDOH waiver staff must wait for confirmation that additional Locator Codes have been added before proceeding to the next step.
The Transmittal and Rate Sheet is forwarded to the Division of Finance and Rate Setting for approval. Once approved, the Transmittal and Rate Sheet is forwarded to the Rate Based Unit (RBU) and Medical Claims Audit BMLs for upload into eMedNY. A Batch report is received by NYSDOH waiver staff on a weekly basis to confirm rates have been added to an agency's eMedNY provider file. NYSDOH waiver staff then verifies that all information was uploaded correctly in eMedNY. NYSDOH waiver staff sends written notification to the provider and RRDC(s) indicating which, if any, services are approved and the effective date of the approval. If the waiver service provider disagrees with the decision, the provider may discuss its concerns with NYSDOH waiver staff.
NYSDOH waiver staff are responsible for making a judgment about the character and competency of each potential waiver service provider as these two factors impact the waiver service provider's ability to deliver waiver services. NYSDOH waiver staff must obtain reasonable assurances that the applicant is capable of delivering waiver services in accordance with the operational standards and intent of the NHTD waiver. NYSDOH waiver staff may contact other New York State agencies or their counterparts in other states, if applicable, to gather information about the current status and background of the potential waiver service provider; this includes any past experience in providing HCBS waiver or non-waiver services, prior audits and/or Medicaid violations.
Step 6: Lists of Approved Providers
NYSDOH waiver staff notifies the appropriate RRDC(s) of the Medicaid approval of a new waiver service provider and of the waiver services that the provider has been approved to provide. The RRDC adds the waiver service provider to the list of approved waiver service providers for the region and distributes the updated list to all service coordination agencies/Service Coordinators in their region. The updated list of approved waiver service providers is distributed each time a change in the provider list occurs. The RRDC is responsible for maintaining a current list of approved and available waiver service providers and for distributing a conflict-free provider list to the individual waiver participant, eliminating any providers which may be in conflict. The RRDC will update the provider list no less than weekly. The RRDC must authorize services and the designated provider via the approval of the service plan prior to service provision to a participant.
Adding a Waiver Service
Approved waiver service providers may apply to provide one (1) or more additional waiver services at any time. To request the approval of one (1) or more additional waiver services, an agency must submit a Letter of Intent (see Step 1. a.) and a copy of the FEIN document to the appropriate RRDC. After receipt of the Letter of Intent, the RRDC will forward the Letter of Intent to NYSDOH. The RRDC will schedule an interview and complete the Waiver Service Provider Interview form including an Address Grid and EVQ(s).
Depending on what service(s) are being requested, the following documentation may need to be submitted to the appropriate RRDC:
- Employee Verification of Qualifications (EVQ) form(s), including a resume highlighting relevant experience and a copy of the diploma(s), license(s) and/or certification(s), as applicable to the service. One (1) EVQ form must be submitted for at least one qualified individual for each waiver service being requested. While an EVQ form is not needed for AT, CTS, Congregate and Home Delivered Meals or Moving Assistance, a copy of applicable contract and/or contractor(s) will need to be submitted to demonstrate adherence to waiver service qualifications. Providers are responsible for reviewing staff qualifications for all staff providing services on an annual basis.
NOTE: A different employee must be submitted for each waiver service the provider is applying for. All employees must meet staff qualifications and the provider must complete an EVQ for all employees. Staff qualifications must be reviewed and confirmed by the provider on an annual basis.- A copy of the potential provider's licensure, certification, contract/contractor(s) and/or any other requirements, as applicable, which support the requested services and satisfy the requirements for being a provider of the waiver service specified in the provider enrollment packet.
NOTE: The RRDC must visit the proposed site for a Structured Day Program (SDP) and obtain a copy of the Certificate of Occupancy and Fire Inspection. The RRDS must obtain a copy of the SDP's sign-in/out policy which must follow the format outlined in Section VI - Waiver Services prior to waiver service provision at the site. The RRDS must also confirm that the site meets the HCBS Settings Final Rule requirements.- A copy of the "New York State Medicaid Enrollment Form" for Institutions and Rate-Based Providers (EMEDNY-436601) only if the additional service is under a different Category of Service from what the waiver service provider is currently approved (0260 for Respiratory Therapy and Home Visits by Medical Personnel; 0263 for all other waiver services).
- Policies and Procedures if they differ for the additional waiver service being requested (see Step 2 above).
The remainder of the process to add a service is the same as the initial application/approval process. Providers should start from Step 4 onward to complete the application process for adding a waiver service.
Adding a Region
Approved waiver service providers may apply to provide waiver services in an additional region(s) at any time. To request approval of an additional region(s), an agency must submit a Letter of Intent to the new region (see Step 1. a.) and a copy of the FEIN document to the appropriate RRDC. After receipt of the Letter of Intent, the RRDC will forward the Letter of Intent to NYSDOH. The new RRDC will schedule an interview and complete the Waiver Service Provider Interview form, including an Address Grid.
Depending on what service(s) are being requested, the following documentation may need to be submitted to the appropriate RRDC:
- Employee Verification of Qualifications (EVQ) form(s), including a resume highlighting relevant experience and a copy of the diploma(s), license(s) and/or certification(s) as applicable to the service. One (1) EVQ form must be submitted for at least one qualified individual for each waiver service being requested. While an EVQ form is not needed for AT, CTS, Congregate and Home Delivered Meals or Moving Assistance, a copy of applicable contract and/or contractor(s) will need to be submitted to demonstrate adherence to waiver service qualifications.
NOTE: A different employee must be submitted for each waiver service the provider is applying for. These should not be the same staff provided in the currently approved region. All employees must meet staff qualifications and the provider must complete an EVQ for all employees. Staff qualifications must be reviewed and confirmed by the provider on an annual basis.- A copy of the potential provider's licensure, certification, contract/contractor(s) and/or any other requirements, as applicable, which support the requested services and satisfy the requirements for being a provider of the waiver service specified in the provider enrollment packet.
NOTE: The RRDC must visit the proposed site for a Structured Day Program (SDP) and obtain a copy of the Certificate of Occupancy and Fire Inspection. The RRDS must obtain a copy of the SDP's sign-in/out policy which must follow the format outlined in Section VI - Waiver Services prior to waiver service provision at the site. The RRDS must also confirm that the site meets the HCBS Settings Final Rule requirements.- A copy of the "New York State Medicaid Enrollment Form" for Institutions and Rate-Based Providers (EMEDNY-436601) only if the additional service is under a different Category of Service from what the waiver service provider is currently approved. (0260 for Respiratory Therapy and Home Visits by Medical Personnel; 0263 for all other services).
- Policies and Procedures if they differ for the additional waiver service being requested (see Step 2 above).
The remainder of the process to add a region is the same as the initial application/approval process. Providers should start from Step 4 to complete the application process for adding a region.
E. Subcontracting for Waiver Services
Subcontracting is defined as the approved waiver service provider's use of another agency to fulfill the responsibilities and services delegated to the approved waiver service provider in the Service Plan. All subcontractors are required to meet the staff qualifications for the waiver service. The approved waiver service provider must complete an EVQ for all subcontract staff and maintain appropriate personnel records for the staff. The approved provider is responsible for all claims submission and all wavier program compliance.
For these services, subcontracting may only occur when the approved waiver service provider seeks to supplement waiver service provision due to its own limited resources. However, the waiver service provider is responsible for supervising the completion of all service provision in accordance with the service plan, ensuring that all workers are skilled or appropriately licensed, and determining that the completed task meets State and Federal codes, including Conflict-of-Interest (COI) requirements. Subcontracting may not be employed in order to avoid COI requirements. The waiver service provider who is subcontracting is responsible for ensuring that their subcontractor(s) meet the appropriate waiver service staff qualifications at all times.
F. NYSDOH Restriction of a Waiver Service Provider
When NYSDOH waiver staff are informed by the RRDC of deficiencies or adverse action by an approved waiver service provider, NYSDOH may choose to restrict a waiver service provider's ability to expand services and/or accept new cases. This decision is based on identified performance issues by the RRDC, failure to comply with conflict-of-interest criteria, investigation findings, complaints and/or identified negative trends. The RRDC, in consultation with NYSDOH, will remove the provider from the list of available providers for the region until a plan of corrective action is submitted, reviewed, and approved by the RRDC. The RRDC is responsible for removing the provider from the list of available providers and re-instating the provider on the list when the deficiencies are resolved. The RRDC provides NYSDOH with the updated available provider list on a quarterly basis. The RRDC will distribute the updated list of providers to the Service Coordination agencies weekly. When a provider is removed from the list of available providers, the RRDC will not approve any service provider requests for the organization. This includes new referrals and case transfers. This restriction pertains to the agency as a whole and all services the provider is approved to provide. Examples of deficiencies may include, but are not limited to:
- Failure to meet COI criteria;
- Failure to meet HCBS Settings requirements;
- Failure to meet Person-Centered Planning requirements;
- Late Service Plans (refer to Section V - The Service Plan);
- Late ISRs (refer to Section V - The Service Plan);
- Unacceptable waiver service provider practices;
- Questionable quality of services;
- Failure to attend participant team meetings;
- Failure to attend RRDC provider meetings;
- Failure to secure/provide needed and timely assessments in order to fulfill services identified in the service plan and/or meet level of care requirements;
- Failure to provide waiver services as established in a participant's service plan;
- Trends in service provision that reflect inadequate or inappropriate service provision; and
- Waiver service provider's inability to follow the NHTD waiver policies and procedures.
The restriction will remain in place until the matter is resolved and within the designated time frame established by the RRDC.
NYSDOH may initiate a disenrollment process by sending the provider a letter advising the provider's waiver service identification (ID) will be terminated in sixty (60) days and the reason for the disenrollment. The letter also informs the waiver service provider that all service restrictions in place and remain in effect until final termination is implemented. NYSDOH will copy the RRDC on the letter. The RRDC will initiate contact with the provider and impacted waiver service participants in order to facilitate selecting a new waiver service provider(s) and to initiate the service transition process.
Upon initiation of the transition process, the current Service Coordinator must assist the participant(s) in choosing a new waiver service provider and completing the Request for Change of Provider form (DOH-5750). The Service Coordinator will assist the participant(s) and the terminating waiver service provider through the period of transition from current to new waiver service provider(s). The terminated waiver service provider is responsible for sending copies of all evaluations, ISRs, Detailed Plan(s) and an update on the participant's accomplished goals to the new waiver service provider(s) as applicable.
NOTE: All daily program documents and case notes remain the work product of the provider and do not transfer to the new provider. This includes, but is not limited to: time keeping records, activity lists, shift notes and case notes. The RRDC may request copies of these documents, as needed.
All participant records must be maintained for a period of six (6) years from the effective date of the provider's termination of their MMIS Provider ID. All files must remain available for audit purposes during this period.
In situations in which the service being terminated is Service Coordination, the letter must direct the participant to contact the RRDC to select another service coordination provider agency. The RRDC must assist the participant in completing the Change of Service Coordination Agency Request Form (DOH-5731). The RRDC must ensure that all applicable documents (e.g., ISP, current Service Plan, evaluations, current level of care, ISRs, Detailed Plans) are transferred from the current Service Coordinator to the new Service Coordinator.
The disenrollment process is a last resort and may only be rescinded if NYSDOH and the RRDC are presented sufficient evidence that the reason for the disenrollment has been addressed and remedied. Upon verification that the corrective action has been sufficiently completed, NYSDOH will initiate steps to withdraw the disenrollment action.
G. Waiver Provider Request to Voluntarily Terminate Provider Agreement
An approved waiver service provider may choose to terminate one or all of their approved waiver service(s) by submitting a Letter of Intent to terminate to the appropriate RRDC and NYSDOH. Written notice must be submitted at least sixty (60) calendar days prior to the date of termination in accordance with the Provider Agreement. This Letter of Intent must identify where service records will be kept for six (6) years post termination and must be made available upon request by NYSDOH and other oversight entities.
Upon notification to the RRDC and NYSDOH, the waiver service provider must also notify all participants that they will no longer continue to provide the service(s). For all waiver service providers, regardless of waiver service, the notice must be sent at least thirty (30) calendar days prior to the end of waiver service provision. The notice must direct the participant to contact their Service Coordinator to select other waiver service provider(s).
The Service Coordinator must assist the participant(s) in choosing a new waiver service provider and complete the Request for Change of Provider form (DOH-5750). The Service Coordinator will assist the participant(s) and the terminating waiver service provider through the period of transition from current to new waiver service provider(s). The terminating waiver service provider is responsible for sending the applicable new waiver service provider(s) the following copies of all evaluations: ISRs, Detailed Plans and an update on the participant's accomplished goals. The waiver service provider must continue all service provision until such time that all cases have been successfully transitioned to new service providers or the participant no longer seeks the service.
In situations where the service being withdrawn is Service Coordination, the notice must direct the participant to contact the appropriate RRDC to select another Service Coordination provider agency. The RRDC must assist the participant in completing the Change of Service Coordination Agency Request form (DOH-5731). The provider must ensure that all documentation, services and assessments are current at the time of the transition. The RRDC must ensure that all applicable documents (e.g., ISP, current Service Plan, evaluations, current level of care, ISRs, Detailed Plans) are transferred from the current Service Coordinator to the new Service Coordinator. The waiver service provider must continue all service provision until such time that all cases have been successfully transitioned.
NOTE: All daily program documents and case notes remain the work product of the provider and do not transfer to the new provider. This includes, but is not limited to: time keeping records, activity lists, shift notes and case notes. The RRDC may request these documents, as needed.
All participant records must be maintained for a period of six (6) years from the effective date of the provider's termination of their MMIS Provider ID. All files must remain available for audit purposes during this period.
H. Provider Termination of Waiver Services to an Individual Waiver Participant
An approved waiver service provider may choose to no longer serve an individual waiver participant. If this is the case, then the waiver service provider must send a letter to the waiver participant, the participant's Service Coordinator and the RRDC at least thirty (30) calendar days prior to discontinuing the provision of service(s). Providers must ensure that service provision has been successfully transitioned prior to the actual termination of services. The letter must be sent via priority mail or delivered directly to the participant. The reason(s) for terminating service(s) must be clearly identified in the letter and can include but are not limited to: inability to meet participant's service needs, staff safety or loss of staff. The letter must advise the participant to contact their Service Coordinator and/or RRDC for assistance with selecting another approved waiver service provider.
The current waiver service provider must follow the Change of Provider Process (refer to Section V - The Service Plan).
In situations in which the service being terminated is Service Coordination, the Service Coordinator should advise the participant of the change in advance by sending a letter thirty (30) days prior to the service termination. The letter should be sent directly to the participant advising they contact the RRDC to select another service coordination provider agency. The RRDC will provide the participant a list of all available conflict- free waiver service providers. The RRDC must assist the participant in selecting a new service coordination provider and in completing the Change of Service Coordination Agency Request form (DOH-5731). The RRDC must ensure that all applicable documents (e.g., ISP, current Service Plan, evaluations, current level of care, ISRs, Detailed Plans) are transferred from the current Service Coordinator to the new Service Coordinator. Services will not terminate until a new provider is identified and approved.
NOTE: All daily program documents and case notes remain the work product of the provider and do not transfer to the new provider. This includes, but is not limited to: time keeping records, activity lists, shift notes and case notes. The RRDC may request copies of these documents, as needed.
If the participant is currently seeking a Fair Hearing and has aid continuing, a provider is required to continue to provide services until such time that a decision is rendered, or a new provider selected. If the provider cannot continue service provision during this period, documentation explaining the reason why must be provided to the RRDC. This information will be included in the participant's fair hearing information. The termination of services may not place the participant at risk.
NOTE: All other NYSDOH regulations related to service provision and/or fair hearings will take precedent over waiver service protocols as related to discontinuing services to an individual.
Conflict-of-Interest Provision
Waiver service providers may not function as landlords or employ waiver participants. Waiver service providers may not maintain any fiduciary relationship with a waiver service participant it serves such as representative payee, trustee, executors, or power of attorney. Waiver service providers may not serve as guardians for waiver participants they serve. Waiver service providers also may not accept private pay arrangements from waiver participants on their caseload.
Conflict-of-Interest federal regulation also restricts the provision of Service Coordination and another direct waiver service to the same participant, more information regarding this can be found in Section IX - Quality Assurance. All waiver service providers must provide conflict-free waiver service provision.
Conflict-of-Interest is defined as a real or seeming incompatibility between one's private interests and one's public or fiduciary duties: where a person or party has two contradictory interests. The role of a Medicaid waiver service provider is to solely provide approved Medicaid waiver services.
Oversight
NYSDOH waiver staff obtain reasonable assurances that the applying agency is capable of delivering services in accordance with the operational standards and intent of this waiver. NYSDOH waiver staff contact other New York State agencies to gather information about the current status and background of the potential provider, including any past experience in providing HCBS waiver services. NYSDOH waiver staff review information about providers through Automated Survey Processing Environment (ASPEN), the Attorney General's (AG) office, Office of Medicaid Inspector General (OMIG), Office of Inspector General (OIG), New York State Office of the Professions and web searches prior to approving providers.
NYSDOH monitors non-licensed/non-certified providers to assure adherence to waiver requirements through the RRDC and the NYSDOH Office of Primary Care and Health Systems Management (OPCHSM). NYSDOH waiver staff review information about providers through Automated Survey Processing Environment (ASPEN), AG, OMIG, OIG and web searches. If there are questions about the provider's ability to meet the standards, the following action may be taken: request for a plan of corrective action, referral made to OMIG or request for an additional survey of the provider.
RRDCs maintain attendance sheets of all provider trainings. These documents are reviewed by NYSDOH during site visits. RRDCs include provider training data in the RRDC Quarterly Report.
Waiver providers are responsible for maintaining ongoing training for their staff to assure that waiver compliance standards are met. This information is reviewed upon survey.
RRDC staff provides NYSDOH with an annual schedule of all provider meetings. A master schedule is maintained by NYSDOH. Provider meetings are utilized as a mechanism for program updates and include at least one training topic per meeting. Samples of training materials and agenda are provided to NYSDOH.
If, at any time, a provider is unable to maintain qualified staff for a service, it is no longer able to provide that service. The waiver provider must report any changes in status to the appropriate RRDC.
Providers who have not provided waiver services in two (2) or more years and wish to resume providing services must contact the appropriate RRDC to reapply as a waiver provider with current and appropriate documentation.
NYSDOH waiver staff provide ongoing technical assistance to RRDC staff and providers about the qualifications and criteria necessary to be an approved NHTD waiver provider.
Provider enrollment practices are reviewed at Quarterly RRDC meetings.
A provider database system is maintained by NYSDOH to track information throughout the provider enrollment process as well as maintain critical information that facilitates the monitoring of providers and the survey process.
Information received via NHTD complaint lines is maintained and used as a source to identify ongoing issues or trends in service provision related to specific providers.
NYSDOH and/or RRDCs review training materials used by a waiver provider to train their staff and make recommendations for changes or improvement, or the provider may use NYSDOH core curriculum training modules.
NYSDOH and/or RRDCs attend waiver service provider trainings as necessary.
NYSDOH waiver staff designate time in each RRDC quarterly meeting to provide training by subject matter experts on a variety of waiver implementation issues.
Documentation of remediation activities is accomplished by the following measures: correspondence among NYSDOH waiver staff, the RRDC, participants and their legal guardians, and/or service providers; amended service plans; findings from retrospective record reviews and reports of follow-up meetings with participants; and the results of NYSDOH site visits.
Record Keeping
The record set maintained by each provider must include and is not limited to: name of participant, date of service, staff performing the activity, time and attendance records, the start and end time of each session, a description of the activities performed during the session, and the participant's service goals and the participant's progress toward attaining those goals.
Each Structured Day Program must maintain a daily log to reflect participant attendance. This document must be maintained at the program site and it must contain the following information: date and time the participant arrived/departed from the structured day program, and reason for departure if the participant leaves prior to assigned program hours (e.g., mid-day departure for lunch).
Per NYCRR Title 10 section 405.10 (a) (4), providers must maintain appropriate financial records supporting their determination of available resources, collection efforts, receipt of funds and application of monies received. Such records must be readily accessible to authorized officials for audit purposes. Providers must identify an office location where participant files are maintained.
Medical records shall be retained in their original or legally reproduced form for a period of at least six (6) years. The records shall be legible, accurately written, complete, properly filed, retained and accessible in a manner that does not compromise the security and confidentiality of the records.
For auditing purposes, records on enrollees must be maintained and be available to authorized Medicaid officials for six (6) years following the date of the waiver participant's termination from waiver services. Failure to conform to these requirements may affect payment and may jeopardize a provider's eligibility to continue as a Medicaid provider.
If a provider should wish to terminate services, all participant records must be maintained for a period of six (6) years from the effective date of the provider's termination of their MMIS Provider ID.
Provider records must adequately support billing for waiver services. Claims for NHTD waiver services are adjudicated by eMedNY. The eMedNY system identifies HCBS enrollees with a Restriction/Exemption/RE code that identifies the person as being enrolled in the NHTD waiver. Payment system edits require the client record to indicate active Medicaid eligibility and HCBS Waiver enrollment for all dates of service billed. All billings are processed either through eMedNY or through direct payment to the transportation contractors through the NYSDOH contracted transportation system.
Providers must complete an eMedNY Revalidation of their MMIS Provider ID every five (5) years.
NYSDOH is the single State agency responsible for monitoring payments made under the New York State Medicaid program. Statewide audits of Medicaid funded programs are conducted by the Office of the State Comptroller (OSC), the Office of the Attorney General (AG), the Department of Health, and the Office of the Medicaid Inspector General (OMIG).
Providers are required to file an annual Cost Report to the State within 120 days (150 with a requested extension) following the end of the provider's fiscal reporting period. Providers are not required to secure an independent financial audit. If a provider fails to file a complete and compliant Cost Report within 60 days of the due date, the State may impose a 2% penalty on all of the provider's Medicaid billing for the waiver.
Section IV: Roles and Responsibilities
Regional Resource Development Center
Regional Resource Development Specialist and Nurse EvaluatorIntroduction
The NYS Department of Health (NYSDOH) contracts with qualified not-for-profit agencies for the daily operations of the waiver in specified regions established by NYSDOH. These agencies serve as Regional Resource Development Centers (RRDCs) and employ Regional Resource Development Specialists (RRDS) and Nurse Evaluators (NEs) to enroll participants and service providers, approve service plans, develop regional resources, and administer the NHTD waiver in each respective region. The RRDCs serve as the authorizing agent on behalf of NYSDOH for all waiver services contained within the waiver participant's Service Plan. Additionally, the RRDC monitors all eligibility and Level of Care (LOC) determinations on behalf of waiver applicants/participants. RRDCs play a vital role in the success of the NHTD waiver; they work to ensure high quality service provision to all participants of the NHTD waiver. This section of the Program Manual defines and clarifies the roles and responsibilities of the RRDC.
Appendix A of the approved 1915(c) Waiver Application establishes that NYSDOH may use contracted entities to perform waiver operational and administrative functions on behalf of the Medicaid agency (NYSDOH). These include:
- Disseminating information about waiver services to community agencies, families, and potential waiver participants by conducting informational meetings and community outreach events.
- Oversight and implementation of waiver participant enrollment: RRDC staff meet with each potential waiver participant to discuss waiver services; explain participants' rights and responsibilities; discuss participant choice and determine if the individual meets waiver eligibility criteria. Those individuals choosing to apply for waiver services receive a list of approved Service Coordination agencies that will assist the individual to select needed services and develop an Initial Service Plan (ISP).
- Monitoring waiver services and expenditures: RRDC staff review all service plans to ensure cost effectiveness and track and ensure timely submission of Level of Care (LOC) assessments.
- Reviewing participant service plans: RRDC staff review and approve all ISPs to establish program eligibility. Revised Service Plans (RSPs) are reviewed and approved on an annual basis.
- Recruiting providers: RRDC staff assess the need for services in their regions and conduct outreach to potential providers. They encourage current providers to expand their scope of waiver services when appropriate. Potential providers are interviewed and referred to NYSDOH for enrollment.
- Conducting training and technical assistance: RRDC staff provide technical assistance to providers, participants, advocates, community services and other RRDCs.
- Receipt, oversight, and investigation of participant complaint calls: The RRDC is responsible for investigation, review, and resolution of complaints. By having the RRDC assess complaints at the local level, issues are addressed more quickly, and the complainant is contacted directly by the RRDC. Complaints related to the RRDC are received directly by NYSDOH and the phone number is maintained on the waiver participant contact sheet posted in the participant's home. A copy of the complaint protocol (DOH-5729) and complaint line phone numbers is maintained on the NYSDOH website. Participants are informed of the outcome of the review of the complaint in writing. NYSDOH reviews complaint data on a quarterly basis and analyzes the information for trends and recurring issues. The complaint protocol indicates: "if the subject of the complaint is the RRDC or another service within the New York State Department of Health (NYSDOH), NYSDOH NHTD waiver staff will address the complaint or initiate review of the matter. For such complaints, please call the NYSDOH NHTD Program at 518-474-5271." Any individual may contact NYSDOH to discuss concerns of any nature or if unsatisfied with the complaint resolution.
Regional Resource Development Center (RRDC)
The RRDCs are located in nine (9) designated regions across New York State (refer to Section XIII - RRDC Regions map).
Each RRDC administers the NHTD waiver program initiatives at the regional level under the direction of the NYSDOH. The RRDC is responsible for managing the waiver, with an emphasis on ensuring participant choice, availability of waiver service providers and cost effectiveness of waiver services within its region.
Qualifications of the RRDC
The RRDC must:
- Be a non-profit organization or agency secured via a competitive grant application process capable of supporting the work of the RRDS, Nurse Evaluator (NE), the conditions of the 1915(c) waiver application and all other requirements as designated by the RRDC contract;
- Be Health Insurance Portability and Accountability Act (HIPAA) and Medicaid confidentiality compliant to assure the privacy of all waiver participants;
- Have expertise in working with individuals with disabilities and seniors and be able to demonstrate commitment to ensuring the provision of integrated community-based services to these individuals, their family members and other informal supports;
- Possess extensive knowledge of providers of community-based long term services in the geographic area they serve; and
- Be financially stable and have the organizational capacity to administer RRDC responsibilities.
General Roles and Responsibilities of the RRDC
The RRDC will:
Employ a Lead RRDS, a NE, quality assurance and housing specialists and other staff who meet the qualifications and experience specified in its contract. The program specific clauses of the RRDC contract memorialize the minimum experience and qualifications for the Lead RRDS and Nurse Evaluator. The contract further defines that any candidate under consideration for Lead RRDS and Nurse Evaluator must be approved by NYSDOH prior to employment. All other RRDC staff hiring is subject to NYSDOH review;
- Function as an initial point-of-contact for referrals, potential applicants, their families, legal guardians, and/or authorized representatives;
- Administer the day-to-day activities of the waiver and make recommendations based on such activities to NYSDOH for improvements/revisions to NHTD waiver policies and procedures;
- Develop and maintain waiver resources and supports in the region it serves;
- Manage the service plan (SP) review process, and other monitoring functions using a database compatible with NYSDOH needs;
- Maintain databases to ensure efficient management of intakes and referrals, the service plan review process, level of care, Serious Reportable Incidents (SRIs), housing and other information determined necessary to maintain by DOH waiver staff;
- Ensure that data is conveyed timely and accurately;
- Maintain participant Application Packets, all service plans, reports, and other required documentation as specified by the NHTD waiver and in a manner consistent with State standards for e-file transfers and information sharing;
- Develop collaborative relationships with regionally based stakeholders including Local Departments of Social Services (LDSS) and other local government entities, providers, advocacy organizations and others necessary to assure a comprehensive coordinated approach to the targeted population;
- Receive, investigate, and provide oversight of applicant/participant complaint calls;
- Conduct training and provide technical assistance to applicants, participants, providers, advocates, community resources and other RRDCs;
- Reduce the incidence of unnecessary institutionalization through:
Transition: Assisting eligible individuals currently living in nursing homes to move to appropriate community-based settings.
Diversion: Preventing in-state and out-of-state facility placements through individual and systems advocacy and the
development of needed supports for eligible individuals.
Repatriation: Assisting individuals who have been in out-of-state facilities return home to New York State.- Cooperate with State and Federal audits;
- Complete annual participant satisfaction surveys;
- Attend quarterly RRDC meetings and participate in monthly conference calls with NYSDOH;
- Complete reports and maintain program data as established by NYSDOH;
- The RRDC is required to maintain sufficient provider capacity to ensure the delivery of waiver services in the region and offer sufficient participant choice;
- Manage other roles and responsibilities as defined by NYSDOH as indicated in the contract;
- Complete quarterly reports associated with the contract workplan in order to confirm contract deliverables;
- Monitor regional compliance with relevant NYS and Federal statues and report to NYSDOH as requested; and
- Approve, facilitate and monitor non-waiver housing supports and services for waiver participants/applicants as provided through the NHTD Housing Subsidy Program or separate grants and other programs. The RRDC must assist eligible waiver participants in securing appropriate housing. RRDCs are also responsible for ensuring that payments made through the NHTD Housing Subsidy Program, a state funded program, are correct and that placements remain appropriate for housing subsidy participants
NYSDOH monitors the performance of the RRDC on an ongoing basis. All requests for documents related to a waiver participant require the appropriate HIPAA release forms and encryption protocols. The RRDC will only release documents or medical records from participant files which were used for the sole use of determining waiver eligibility or were produced by the RRDC to provide waiver services. Requests for other third-party documents should be redirected to the source of the document. All discussions and documents regarding a waiver applicant/participant require a release from the individual prior to addressing any requests and/or information.
Regional Resource Development Specialist (RRDS)
The RRDS is the key staff member responsible for the development, management, administration, and monitoring of the NHTD waiver for the RRDC on a regional level. The RRDS promotes participant choice, ensures the delivery of high-quality services, assists in the development of needed waiver services, and oversees waiver cost- effectiveness.
The RRDS communicates regularly with NYSDOH, collaborates with local government entities, waiver service providers and advocacy groups in order to be an active member of the network of services and supports in the community.
Skills
The RRDS will have:
- Demonstrated expertise working with individuals with disabilities and seniors and extensive familiarity with the operation of Section 1915(c) waivers and community- based services;
- Knowledge, skills, and/or abilities to assess, identify and address gaps in services;
- Excellent screening and interviewing skills;
- Excellent communication and presentation skills;
- Ability to develop and maintain collaborative relationships with regionally based stakeholders, including the LDSSs, other local government entities, providers, advocacy organizations and others necessary to assure a comprehensive, coordinated approach to services for individuals with disabilities and seniors;
- Working knowledge of community-based resources for individuals with disabilities and/or seniors;
- Excellent problem-solving and investigating skills;
- Working knowledge of Medicaid, Medicare and/or other third-party payers;
- Skill in coordinating activities, evaluating data and establishing priorities; and
- All additional qualifications outlined in the RRDC contract.
Roles and Responsibilities of the RRDS
It is the responsibility of the RRDS to assist NYSDOH in ensuring that waiver participants in New York State, who are individuals with disabilities and seniors, are able to live as independently as possible in the community.
The RRDS works closely with NYSDOH to provide data and input as needed regarding the administration of the NHTD waiver in its region.
The RRDS may meet with the participant at any time or place as needed and allowed by the applicant/participant and has the right to access all records regarding the provision of waiver services and applicant/participant waiver eligibility.
The RRDS may access all provider offices and locations of service delivery at any time, including unannounced visits in order to monitor service delivery and to ensure the health and safety of service participants.
RRDS responsibilities include:
- Information, Resource and Referral
- Work closely with NYSDOH to disseminate public information regarding the waiver's ability to meet the needs of individuals with disabilities and seniors;
- Respond to calls from individuals with disabilities and seniors, family members, advocates, professionals and others requesting information regarding waiver services;
- Provide resource information and education regarding the community-based needs of individuals with disabilities and seniors;
- Ensure that all prospective participants who appear eligible for waiver services and have indicated interest in receiving waiver services are interviewed;
- Provide a timely response to inquiries and referrals. If the referral meets basic eligibility requirements (age, Medicaid status, residence), meet with prospective waiver participants to explain the waiver philosophy and services and make a preliminary non-financial determination of appropriateness for the waiver;
- Make referrals to available resources in the community as needed if an individual appears to be ineligible or is determined not eligible for the waiver;
- Track referrals and intakes and ensure timely contact;
- Effective and timely communication with applicants; and
- Maintain an informational database vital to the analysis of the effectiveness of the NHTD waiver.
- Development of Community Resources
- Assess and identify regional waiver and non-waiver service capacity to meet the demands for waiver participation in its service area and report to NYSDOH;
- Provide data to NYSDOH regarding regional needs, outcomes, quality assurance and improvement and cost savings as part of quarterly reports and upon request;
- Develop and implement mechanisms to recruit waiver service providers;
- Promote the quality and availability of services sufficient to allow waiver applicants/participants the opportunity of choosing waiver service providers;
- Develop linkages with Open Doors representatives, inpatient rehabilitation units and long-term care facilities to identify potential participants and to facilitate community re-entry from these institutions;
- Establish linkages with community-based health care providers to promote quality and availability of services;
- Maintain relationships with existing local and state entities, including point of entry, advocacy groups and providers of community-based services for people with disabilities and seniors and their families;
- Maintain an open, collaborative relationship with LDSSs to identify Medicaid eligibility for applicants/participants, access state plan services, and implement necessary service coding for waiver participants;
- Recommend surveillance and audit priorities to NYSDOH as related to waiver service providers; and
- Conduct independent site visits and oversight activities.
- Manage Provider Enrollment and Training
- Interview potential waiver service providers using the RRDS Provider Interview form;
- Make waiver service provider enrollment recommendations to NYSDOH based on factors such as the waiver service provider's understanding of the waiver philosophy, the waiver service provider's staff qualifications, the waiver service provider's established NHTD policies and procedures, participant choice and control, and the waiver service provider's ability to deliver quality services (refer to Section VI -Waiver Services);
- Provide oversight of provider training and offer training to potential waiver service providers regarding the philosophy, policies, and procedures of the waiver; participant needs; development and implementation of comprehensive waiver service plans; and standard documentation and reporting requirements as needed; and
- Meet new Service Coordinators within thirty days of employment with a Service Coordination agency and provide direct training as indicated.
NOTE: The RRDC will review each provider's training curricula upon application. This may include utilizing the NYSDOH core curriculum training. Subsequent to provider enrollment, each provider will submit an annual training plan to the RRDC delineating training topics and frequency for the calendar year. After initial orientation, each staff person must attend at least one annual training session in the calendar year of January 1 to December 31.- Interview and Preliminary Assessment of Potential Waiver Participants
- Confirm applicant's active Medicaid (MA) status;
- Meet with all prospective waiver participants to complete an Intake interview, review and sign the Initial Applicant Interview and Acknowledgement document (DOH-5729), explain the waiver's philosophy, goals and available services and determine if the individual is a candidate for the waiver;
- Recommend other available resources/services for individuals who appear to not be eligible for waiver services (e.g., age, disability, MA status);
- Offer individuals the choice of participation in the NHTD waiver and, when the individual chooses the waiver, provide a list of available Service Coordination providers;
- Obtain signed Application for Participation form (DOH-572), Freedom of Choice form (DOH-5728), and the Service Coordination Agency Selection form (DOH-5727);
- Assure each potential waiver participant receives a timely Level of Care (LOC) determination through the completion of the Uniform Assessment System for New York (UAS-NY) or PRI (if in a nursing facility) (DOH-694);
NOTE: If a PRI and Screen are completed for LOC determination, then a UAS-NY must be completed within 90 days of the individual's enrollment date into the NHTD waiver program.- Track all LOC assessments and outcomes in the participant database;
- Coordinate with the LDSS regarding the appropriate utilization of Medicaid State Plan and NHTD waiver services;
- Maintain contact with a potential waiver participant and document encounters until a Service Coordination agency is selected and accepts the potential waiver participant;
- Forward all applicant information to the Service Coordinator employed by the Service Coordination provider selected by the potential waiver participant;
- Maintain a current list of all approved waiver service providers in the region, updating the list of available providers at least weekly; and
- Monitor provider selection lists to ensure that applicants receive Service Coordination services that are compliant with federal Conflict-of-Interest requirements.
- Review of All Service Plans
- Ensure compliance with federal person-centered planning requirements that each individual receiving Medicaid HCBS has a person-centered service plan that ensures the delivery of services in a manner that reflects personal preferences and choices;
- Review all completed Application Packets and supporting documentation including the ISP (Initial Service Plan) (DOH-5726) submitted by the Service Coordinator to determine initial appropriateness for participation in the waiver;
- Ensure that waiver participants meet Nursing Facility Level of Care (NFLOC) and are assessed annually;
- Review all service plans (Initial, Revised and Addendum) for completeness, focusing on the needs and goals of the waiver participant, the ability of waiver services to support the health and welfare of the participant in the community, the timely provision of services, participant rights and choices, and the efficiency and cost effectiveness of the plan;
- Complete the RRDS Service Plan Review form and determine whether the ISP, Application Packet, subsequent RSP, or Addendum should be approved/disapproved. If needed, provide a written evaluation of the review to the Service Coordinator indicating any necessary revisions or additions needed to the service plan or Application packet;
- Request additional review of service plans by the Nurse Evaluator (NE) as deemed appropriate to assure the plan meets the medically complex needs of the potential active waiver participant, supports the participant's health and welfare and is consistent with needs identified in the UAS-NY Community Health Assessment;
- Track all timeframes related to the receipt of referral through intake interview and Service Coordination agency selection;
- Track timeliness of review process from receipt of ISP and Application Packet to issuance of Notice of Decision (NOD);
- Track timeliness of submission of all service plans for RRDS review and follow up as needed to ensure compliance;
- Track all approved service plans (ISP, Addendum(s), RSP) in the participant database;
- Send notification to the Service Coordinator of the late submission of service plans;
- Provide notification to NYSDOH regarding potential issues related to plan submission, provider selection and/or the application process; and
- Report status and timeliness of reviews via the RRDC monthly report.
- Administer Notices of Decision (NOD)
- Provide the potential waiver participant with information regarding NODs and their rights regarding Case Conferences with the RRDC and Fair Hearings during the initial interview process;
- Notify participants of their program status through utilization of the standard DOH NOD forms as outlined in this Program Manual;
- Provide each potential or active waiver participant an appropriate NOD. Forward a copy to all entities listed on the NOD form (DOH-5735, DOH-5737, DOH-5738, DOH-5739, DOH-5734 & DOH-5740);
- Track all NODs issued in the intake and participant database;
- Maintain open communication with NYSDOH regarding NODs that lead to a Case Conference or Fair Hearing process and all discontinuation notices issued by the LDSS due to loss of Medicaid coverage;
- Attend Case Conferences and Fair Hearings as a representative of the NHTD Waiver program (refer to Section II - Becoming a Waiver Participant); and
- Keep NYSDOH waiver staff informed of any concerns affecting the status of the Fair Hearing process.
- Review Implementation of Waiver Services
- Review all service plans for applicants/participants in the region to ensure that services and the projected cost of services meets the needs of the waiver participant and is an appropriate use of Medicaid funds;
- Review service plan grids to confirm that all approved services are indicated with the frequency and duration and confirm that projected annual costs are correct; and
- Complete home visits and attend Team Meetings and case conferences as needed.
- Incident Reporting
- Implements tasks and responsibilities described in the Incident Reporting Policy and Procedure (refer to Section X - Incident Reporting Policy and Complaint Procedure);
- Utilizes the SRI database to enter data for every SRI reported for participants of the NHTD waiver in the RRDC region. This includes:
- assignment of incident tracking numbers and provider assignment;
- tracking of all reports between the RRDC and waiver providers involved in the discovery and investigation of SRIs;
- the timeliness of report submissions;
- the outcomes of investigations to determine whether the allegations are substantiated;
- the closure of SRIs; and
- the follow up of participant contact(s).
- Assures proper notification is provided to NYSDOH regarding all pertinent incidents and issues (refer to Section X - Incident Reporting Policy and Complaint Procedure);
- Assures that changes to Service Plans and PPOs required as a result of SRI outcomes are implemented timely and effectively by the Service Coordinator;
- Analyzes waiver provider's quarterly SRI reports, annual SRI, and Recordable Incident reports for trends. Data regarding outcomes determined from review and analysis of these reports is submitted to NYSDOH in RRDC quarterly reports;
- Complete quarterly and annual SRI Trend reports for submission to NYSDOH; and
- Ensure compliance with performance measures established in the NHTD 1915(c) waiver application.
- Technical Assistance and Support to Participants, Family Members and Others
- Is available to applicants, participants, family members/informal supports, legal guardians, and designated representatives to answer questions and address concerns regarding the NHTD waiver;
- Supports a participant's right to be the decision-maker regarding life goals, activities, services and waiver service providers;
- Provides information regarding the NHTD waiver program to meet the needs of individuals with disabilities and/or seniors, their family members/informal supports, and the community in its region; and
- Provides direction to participants related to Conflict-of-Interest, person-centered planning and HCBS settings requirements.
- Technical Assistance to Providers
- Attends or coordinates Team Meetings as appropriate or upon request of the participant, the Service Coordinator or team, (refer to Section V - Service Plan);
- Provides training and technical assistance to waiver service providers on all aspects of the waiver program, including: the needs of waiver participants, all aspects of person-centered waiver service plans, policies and procedures and standard documentation/reporting requirements, HCBS settings requirements and Conflict-of-Interest;
- Conducts scheduled provider meetings 8-10 times per year in the region to review waiver policies and updates and provide waiver-related training;
- Assures appropriate providers participate in a minimum of eight (8) provider meetings per year as required; and
- Provides ongoing technical assistance and receives feedback from waiver service providers regarding the policy and procedures of the waiver.
- Technical Assistance to Other RRDCs, Community Agencies, and the State
- Attends and participates in quarterly RRDC meetings, conference calls and webinars;
- Provides cross training and technical assistance and shares areas of expertise with RRDCs in other regions as needed; and
- Provides information and assistance to public, State, and local agencies.
- Develop and Submit Reports to NYSDOH
- Prepare and submit monthly, quarterly, and annual reports on behalf of the contracted agency summarizing RRDC services provided and progress made toward contract deliverables detailing the use of assigned grant funds for program activities. Work closely with NYSDOH to provide information, records and statistical and narrative reports regarding regional needs, outcomes, quality assurance, improvements, and cost savings;
- Communicate regularly with NYSDOH by attending meetings, reviewing policies affecting the waiver and receiving ongoing technical assistance through phone calls and e-mails;
- Attends quarterly RRDS meetings and other meetings upon the request of NYSDOH;
- Makes recommendations based on experience with waiver activities and ongoing administration of the program to NYSDOH waiver staff for improvements to NHTD waiver policies and procedures;
- Assess the quality of services in the region and report findings to NYSDOH;
- Complete annual participant satisfaction surveys and file audits; and
- Maintain accurate and timely data regarding service provision and applicant/participant information.
Nurse Evaluator (NE)
The RRDC will employ, either directly or under contract, at least one Registered Professional Nurse (referred to as the "Nurse Evaluator") to assist the RRDC in the administration and monitoring of the NHTD waiver program. The role of the NE is not to duplicate the role of the RRDS, but to provide clinical expertise related to the care and needs of waiver applicants/participants and to support the RRDS and the successful implementation of the NHTD waiver.
Requirements
The NE must:
- Be a current New York State licensed registered professional nurse and be in good standing;
- Be New York State certified to complete the Hospital and Community Patient Review Instrument (H/C-PRI), SCREEN, Uniform Assessment System-New York (UAS-NY) and other clinical assessments as requested by NYSDOH; Possess excellent clinical assessment skills;
- Have excellent screening and interviewing skills;
- Have excellent problem-solving and investigating skills;
- Have two (2) years of satisfactory professional experience working with people with disabilities and/or seniors in a community setting;
- Possess excellent organizational and training skills;
- Have excellent written and verbal communication skills and the ability to resolve conflicts;
- Be able to coordinate activities, evaluate data and establish priorities;
- Have working knowledge of community-based resources for individuals with disabilities and/or seniors;
- Possess experience with developing relationships with institutional and/or community-based organizations;
- Maintain a working knowledge of services and supports available through Medicaid, Medicare and/or other third-party payers; and
- Meet all qualifications outlined in the agency contract with NYSDOH.
Roles and Responsibilities of the NE
NE responsibilities include:
- Technical Assistance and Support to the RRDC/RRDS and other Nurse Evaluators
- Assists the RRDS in reviewing service plans that are medically complex to assure the information is accurate and utilizes resources and available services to meet the health and welfare needs of the participant;
- Review and/or administer the UAS-NY, or PRI/SCREEN (if in a nursing facility), when there is a concern that the current UAS-NY or PRI does not reflect participant LOC (Level of Care) needs. (e.g., when the individual does not meet LOC requirement; or there appears to be a discrepancy regarding the outcome of a LOC assessment);
- Conduct annual LOC assessments for waiver participants as needed;
- Provide resource information and education regarding individuals with disabilities and seniors as requested by the RRDC;
- Participate in local activities and consortia on issues involving individuals with disabilities and seniors relevant to the NHTD waiver;
- Attend quarterly RRDC meetings, webinars, and training opportunities; and
- Provides training and technical assistance and share areas of expertise with other NEs.
- Resource to Providers
- Attend Team Meetings and case conferences where the participant's clinical needs may warrant further interpretation/assistance; and
- Provide training and technical assistance to waiver service providers on clinical aspects of the waiver program as needed.
- Technical Assistance to Participants, Family Members and Others
- Is available to participant's family members/informal supports and legal guardians to answer questions and address concerns of a clinical nature; and
- Support the participant's right to be the decision maker regarding life goals, serve as a liaison to nursing homes, discharge planners and other medical professionals facilitating the care and welfare of waiver applicants/participants.
- Incident Reporting
- Provide feedback to the RRDS during investigations of SRIs as requested;
- Participate in investigations as needed; and
- Review reports and analyze trends.
- Develop and Submit Reports to NYSDOH
- Maintains required documentation of visits, assessments, consultations recommendations, technical assistance, etc.;
- Prepares reports as requested by NYSDOH summarizing services provided and progress made toward attaining waiver program objectives in cooperation with RRDC requirements for submission of quarterly and annual reports to NYSDOH;
- Attends quarterly RRDC meetings and other meetings upon the request of NYSDOH waiver staff;
- Makes recommendations based on experience with waiver activities and ongoing administration of the program to DOH waiver staff for improvements to NHTD waiver policies and procedures;
- Assess the quality of services in the region and report findings to NYSDOH; and
- Monitors UAS-NY systems for case assignments and timely LOC assessments.
The Role of the NYSDOH
NYSDOH is responsible for assessing the performance of contracted and/or local/regional non-state entities that conduct waiver operational and administrative functions.
NYSDOH oversees the operation of the NHTD waiver, and the fulfillment of Regional Resource Development Center (RRDC) contractual obligations in accordance with section 366 (6-a) of the Social Service Law. NYSDOH waiver staff monitor RRDC contractors' administration of the program. The RRDCs employ Regional Resource Development Specialists (RRDSs). NYSDOH requires that each RRDC employ one full time RRDS who works exclusively on the NHTD waiver. This position is designated by NYSDOH as the Lead RRDS. NYSDOH also requires that each RRDC employ a Nurse Evaluator. Program-specific clauses of the RRDC contract memorialize the minimum experience and qualifications for the Lead RRDS and Nurse Evaluator. The contract further defines that any candidate under consideration for these positions must be approved by NYSDOH prior to employment. If the contractor fails to fill the vacancy with a qualified professional acceptable to NYSDOH, the contract may be terminated immediately. With reasonable notice and written justification, NYSDOH may require the contractor to remove from the contract any employee justified by NYSDOH as being incompetent, otherwise unacceptable, or whose employment on the contract is considered contrary to the best interests of the public or the State. The contract and the NHTD Program Manual also establish the roles and responsibilities of the RRDC. The RRDC is responsible for the development, management, administration, and monitoring of the NHTD waiver on a regional level.
NYSDOH monitors the performance of the RRDCs on an ongoing basis. NYSDOH waiver staff maintain daily contact with the RRDCs. Specifically, RRDC performance is assessed through the following activities:
- NYSDOH waiver staff, via the RRDC, conduct retrospective reviews of a random sample of service plans to assure quality performance of these entities. A standardized form is distributed by NYSDOH and utilized on a statewide basis. NYSDOH waiver staff monitor for correct completion of the Initial Applicant Interview and Acknowledgement, Level of Care, Freedom of Choice, Service Coordinator Selection, Provider Selection, Participant Rights and Responsibilities forms in the record. The service plan review is based on a statistically appropriate sample size to allow valid analysis and conclusions to be drawn from the results. Sample size will be set to ensure a ninety five percent (95%) confidence level with a margin of error of ± five percent (5%) as established by Raosoft.
- NYSDOH waiver staff conduct RRDC annual site visits, as needed, to assess operational and administrative performance and to assure quality performance of these entities on an annual basis, or as needed. During RRDC site visits or audit reviews, NYSDOH waiver staff review a random sample of participant records to assure the presence of a completed and signed Referral (DOH-5747), Intake (DOH-5725), Initial Applicant Interview and Acknowledgement (DOH-5729), Freedom of Choice (DOH-5728), Service Coordinator Agency Selection (DOH- 5727), Provider Selection (DOH-5730), and Participant Rights and Responsibilities forms (DOH-5732).
- Designated in the RRDC contract work plan is the requirement that each RRDC maintain a specific phone number to receive complaints. Service Coordinators are responsible to inform participants of the phone number and to review the process for filing a complaint with the participant. The complaint number is identified on the waiver participant's contact list posted in the participant's home. The complaint line is available to NHTD waiver participants, their families, and advocates for registering complaints and concerns. The complaint protocol (DOH-5729) and phone numbers are available on the NYSDOH website. Information can be found under the header entitled "Complaint Process for Medicaid Long Term Care Waivers." Information retrieved via complaint lines is reviewed by NYSDOH to monitor complaints.
- Each RRDC completes an annual participant satisfaction survey. NYSDOH issues the format and the RRDC is responsible for the distribution of the survey to all waiver participants and receipt of responses, to assure that a minimum statistically appropriate sample size of a ninety five percent (95%) confidence level with a margin of error of ± five percent (5%) is collected. NYSDOH compiles the statewide aggregate data collected from each RRDC and completes a comparative analysis to prior years' data.
- NYSDOH waiver staff regularly assess RRDC performance through review of required contractor quarterly reports on provider and participant enrollment activity and other contractual obligations. NYSDOH waiver staff review and analyze the reports, evaluate contractual performance and waiver implementation trends, and may request a financial audit if expenditure discrepancies cannot be resolved, or additional concerns are raised. Quarterly payments to RRDC contractors may be withheld pending the resolution of performance or compliance issues.
- NYSDOH waiver staff also meet with RRDC contractors on a quarterly basis to review NYSDOH policies, discuss community resources, review performance measures and for training.
- NYSDOH waiver staff conduct monthly statewide RRDC conference calls. Conference calls with individual RRDC contractors are conducted as needed. These calls are used to share methods to enhance program performance, evaluate training methods, discuss participant and provider issues, and review trends in research or services related to NHTD.
- NYSDOH reviews supplemental reports completed by the RRDSs. These reports include monthly statistical data reflecting intakes, referrals, plan reviews, discharges, and enrollments. Quarterly complaint reports and quarterly reports of Serious Reportable Incident data are completed by the RRDCs. These reports reflect aggregate data from approved providers in the region who submit an individual provider report to the RRDC. In addition to providing significant information related to waiver operations, the reports help NYSDOH evaluate the RRDC's contractual performance and statewide waiver implementation trends.
- NYSDOH waiver staff receive calls from waiver participants, Local Department of Social Services (LDSS) staff and other stakeholders that contribute to NYSDOH waiver staff's assessment of the RRDC.
- A standard statewide database of participant and provider enrollment, service plan development and cost of services enables NYSDOH waiver staff to evaluate and monitor program activity at the RRDC contractor level. NYSDOH staff complete random reviews of the participant database to ensure that RRDC staff are entering the required information and LOC determinations are completed per required time frames. NYSDOH waiver staff also analyze data to identify regional and statewide trends, to evaluate current policy, and to identify and implement programmatic changes.
- Each RRDC has established an internal tracking system for pertinent information such as intake, referrals, service plans and incidents to supplement existing NYSDOH data systems. NYSDOH staff review the RRDC contractors' internal tracking systems and discuss internal procedures.
- As established in their contracts, RRDCs are responsible for recruiting and maintaining NHTD waiver providers. NYSDOH monitors the number, type, and location of newly developed providers in each region by monitoring the database and reviewing each region's provider list on a quarterly basis. By contract, the RRDC is required to maintain sufficient provider capacity to ensure the delivery of waiver services in the region and offer sufficient participant choice in providers. NYSDOH reviews provider application packets to ensure that all appropriate transaction forms and letters of incorporation are complete, accurate and include correctly dated information prior to submission to OHIP's Bureau of Provider Enrollment.
- NYSDOH monitors participant requests for Fair Hearings and the disposition of the case. RRDCs are monitored by NYSDOH to ensure that they have properly determined the reason for the adverse action/decision, prepared and presented the case. This includes a review of the NODs, case summary, supporting documentation, and the reason for the action. All RRDC-related Fair Hearings are tracked by NYSDOH.
- RRDC and NYSDOH waiver staff work with NYSDOH Office of Primary Care and Health Systems Management (OPCHSM) surveillance staff to facilitate on-site surveys for a sample of providers. RRDCs are provided with a copy of the deficiency report and notification of the accepted plan of correction.
- Any RRDC contractor operational deficiency will be addressed in a timely manner, whether informally through direct communication with the contractor, or by a formal investigation. In the latter situation, NYSDOH waiver staff notify the RRDC Executive Director in writing of the findings and request a specified corrective action within ten (10) business days.
- Remediation of identified problems or risk factors specific to an RRDC is initiated immediately. Identified quality improvements and corrective action steps to address trends and at-risk practices are addressed statewide at RRDC quarterly meetings and during interim conference calls.
- NYSDOH monitors the RRDC to ensure the contractor fulfills its contractual obligations and performance measures. This oversight includes but is not limited to: technical assistance; monitoring of the RRDC administration of the program; identification of needed corrective action; and implementation and completion of those actions.
- NYSDOH may request a financial audit if program discrepancies cannot be resolved or additional concerns are raised.
- NYSDOH waiver staff review the discharge/enrollment data with the RRDCs at quarterly meetings in conjunction with projected enrollment data in the waiver application. If data presented indicates the RRDSs need to expedite intakes, monitor service coordination agency selection by applicants, and facilitate approval of initial service plans, then a plan to remedy the problem is established.
- Participant enrollment and discontinuation data is reviewed at each Quarterly RRDC meeting.
Section V: The Service Plan
Introduction
Section 2402(a) of the Affordable Care Act requires the Secretary of Health and Human Services to ensure all states receiving federal funds:
- Develop service systems that are responsive to the needs and choices of individuals receiving home and community-based services (HCBS) and community-based long-term services and supports (LTSS);
- Maximize independence and self-direction;
- Provide support coordination to assist with a community-based supported life;
- Achieve a more consistent and coordinated approach to administration of policies and procedures across programs; and
- Requires a Person-Centered Service Plan for each individual receiving Medicaid HCBS.
The person-centered planning process:
- Is driven by the individual;
- Includes people chosen by the individual;
- Provides necessary information and support to the individual to ensure that the individual directs the process to the maximum extent possible; and
- Is timely and occurs at times/locations of convenience to the individual.
Person-Centered service plans assist the person in achieving personally defined outcomes in the most integrated community setting, ensure delivery of services in a manner that reflects personal preferences and choices, and contribute to the assurance of health and welfare. The plan also includes risk factors and plans to minimize them.
Appendix D of the approved 1915(c) waiver application describes the process that is used to develop the person-centered service plan.
The NHTD waiver makes every effort to promote the right of waiver applicants and participants to choose participation in the NHTD waiver, identify needed services, and select their service providers. Agencies that provide service coordination must adhere to conflict-of-interest (COI) requirements established by the Department of Health. Compliance with these practices promotes the independence of the Service Coordinator (SC) and ensures participant choice. The SC is responsible for providing unbiased and comprehensive information to the participant about available services and service providers. A SC may not "steer" business and may not recommend or indicate a preference for a service provider.
The following safeguards ensure that the service plan development is conducted in the best interest of the waiver participant and promotes provider choice:
- The applicant first meets with staff from the RRDC, which is a contractual agent of NYSDOH. The RRDC staff provides information about the waiver services, waiver service providers and explains to the applicant that they have a choice of all available waiver service providers and encourages them to interview service coordination agencies in order to make an informed choice;
- If the applicant appears eligible, they select a service coordination provider and sign a Service Coordination Agency Selection Form (DOH-5727) indicating that they understand that they are entitled to choose a service coordination provider and choose approved providers for other waiver services;
- The applicant signs the Provider Selection Form (DOH-5730). By signing the form, the applicant is affirming that they were given a choice of approved waiver providers;
- On an annual basis, the participant reviews and signs the Participant Rights and Responsibilities Form (DOH-5732), which describes the right to choose and change waiver service providers as requested (it should be noted that choice of a service provider is not choice of specific staff). The participant maintains a copy of the signed form, as does the RRDC and SC in the participant's record;
- The applicant's signature is required on the Initial Service Plan (DOH-5726), Revised Service Plan(s), and any addenda to the service plan. The participant's signature indicates that the participant agrees with the information that is included in the service plan, and that it includes the services requested and the chosen providers of the services;
- The participant has the right to change waiver providers at any time during the period covered by an approved service plan. With the assistance of their SC, the participant completes a Change of Service Coordination Agency Selection Form (DOH-5731), which is then sent to the Regional Resource Development Specialist (RRDS). If the participant wishes to change their Service Coordination provider, the participant contacts the RRDS. The RRDS provides information to the participant about service coordination providers and assists the participant with completing the Change of Service Coordination Agency Request Form;
- The RRDS reviews each service plan to ensure it meets the assessed needs of the participant and reflects waiver participant choice;
- A complaint line is established for participants to call if they believe their rights are being violated or have concerns regarding their service provision. All calls will be investigated promptly;
- The participant is given a contact list that contains the phone numbers of the RRDS and NYSDOH waiver staff in case any concerns arise;
- Participants are surveyed using a uniform survey tool to obtain feedback about the services and supports that they receive under the NHTD waiver. This survey includes questions about the waiver participant's satisfaction with the amount of choice and control that the participant has over their services and over their providers of service;
- NYSDOH waiver staff, via the RRDC, conducts a random retrospective record review using a statistically appropriate sample size determined by the software program available at the Raosoft website to allow valid analysis and conclusions to be drawn from the results. Sample size will be based on a ninety-five (95%) confidence level with a margin of error of ± (five) 5% (p is less than or equal to .05);
- NYSDOH has the responsibility to ensure informed choice of providers for all participants. In the event of coercion by providers, the provider will be subject to corrective actions;
- The Regional Resource Development Specialist (RRDS) is responsible for the review of every service plan and addendum to ensure they are meeting the participant's health and welfare and that they are cost-effective. Authorization of the services identified in the service plan by the RRDC allow the provision of the service and claims billing by the provider;
- Once the service plan has been approved by the RRDS, the SC is responsible for ensuring that all service providers receive a copy of the approved service plan and are aware of the overall content of the plan and goals. The approved plan is forwarded to each service provider within three (3) calendar days of receipt of the approved plan by the SC. The provider must be in receipt of the approved plan prior to implementing services;
- The applicant/participant and their legal guardian, if applicable, reviews and signs the written plan before the SC submits it to the RRDS for review. The service plan is also signed by the SC and the SC supervisor prior to submission to the RRDC. Services are not implemented without a signed and executed service plan; and
- Participants are informed by the SC of their right to contact any waiver entity when there are concerns regarding the delivery of services. All waiver providers are responsible for maintaining open communication with the SC when concerns or changes with the participant occur that potentially affect the provision of services.
A. Types of Service Plans
There are two types of service plans utilized by the NHTD waiver: Initial Service Plan (ISP) (DOH-5726) and Revised Service Plan (RSP). Both documents may be updated or amended by an addendum to the existing service plan. The RSP is revised/rewritten annually. The Service Coordinator (SC) is responsible for completing the ISP/RSP.
Service plans are expected to evolve as the participant experiences community life, requests revisions, experiences significant life changes, or as new service options become available.
The service plan is an essential tool that clearly states responsibility for each of the services and supports that the waiver participant needs based on a comprehensive, person-centered assessment. The service plan includes the description of methods for addressing the participant's goals and objectives and identifies persons and/or services responsible for implementing and monitoring the plan. These methods are discussed and evaluated at each service plan review.
Each service plan includes an assessment of the individual to determine the services needed to prevent institutionalization or return to a facility. This assessment should include, in person-centered terms, a description of the individual, their psycho-social history and a description of their strengths and needs.
The assessment also includes an evaluation of risk factors that will be addressed in the individual's Plan of Protective Oversight (PPO). The PPO explicitly states the individuals who are responsible for assisting the participant with daily activities/emergencies, medication management, financial transactions, fire/safety issues, and back-up plans are also included. The PPO establishes a plan to reduce risk and address safety issues. The PPO addresses back-up issues for activities that are directly related to health and welfare.
The service plan identifies services for one year of waiver participation. If the waiver participant's level of skill changes, an adjustment in the type and amount of the waiver services may be required and an addendum to the plan is developed. The SC develops the addendum in collaboration with the participant, authorized representatives, and specific service provider(s).
The service plan specifies all supports to be provided to the waiver participant, this includes: informal caregivers (i.e., family, friends, and natural supports), federal and state funded services, Medicaid State Plan services, and waiver services. Waiver services are provided when informal or formal supports are not available to meet the participant's needs. Waiver services may also be accessed when it is more efficient or cost-effective than Medicaid State Plan services.
Initial Service Plan (ISP) - The ISP (DOH-5726) is developed when an individual is applying to become a waiver participant. The ISP is a collection of personal, historical, medical/functional and social information about the applicant gathered through interview and assessment of the individual by the Service Coordinator (SC), clinicians and service providers. It is the primary component of the Application Packet (refer to Section II of this manual: Becoming a Waiver Participant) and is due to the RRDC within sixty (60) calendar days from the date noted on the approved Service Coordination Agency Selection Form (DOH-5727) when there are no roadblocks to eligibility, e.g., need for community housing. The ISP provides justification for the individual's participation in
the NHTD waiver by describing the reason NHTD services are needed to assure the individual's health and welfare while in the community.
The Regional Resource Development Specialist (RRDS) provides detailed information to the applicant and/or their legal guardian during the intake process regarding the purpose of the NHTD waiver, the philosophy of the NHTD waiver, available services, the application and Initial Service Plan development process, role of the Service Coordinator (SC), a list of available waiver providers, and the fair hearing process. Service plans address many aspects of the applicant/participant's life, including safety, independent living skills, and medical and cognitive needs. As a result, family members, friends and informal supports are encouraged to provide input into the applicant/participant's service goals. The applicant/participant may include any person of their choosing to assist in the development of the service plan.
The focus of the ISP is on the individual, reflecting their choices and needs for supporting the individual's health and welfare while in the community. This includes information regarding significant relationships, current informal and community supports, desired living situation, and recreational and/or community activities. The ISP must also contain a description of the individual's strengths and limitations, including any cognitive, behavioral or physical concerns.
The ISP also details services necessary to safely maintain the individual in the community and defines the services and supports necessary to transition an individual residing in a facility-based setting to community life, if appropriate. The ISP will identify the services and supports necessary for the first year of waiver participation.
Revised Service Plan (RSP) - The RSP is developed through a collaborative effort between the participant, individual(s) selected by the participant to participate in the development of the RSP, the Service Coordinator (SC), current NHTD waiver service providers, non-waiver providers, and others, as appropriate. The focus of the RSP remains on the individual, reflecting their needs and choice of services that continue to support safe and successful community living.
The RSP contains a review and evaluation of the participant's previous twelve (12) months (365 calendar days) of waiver services. It addresses how waiver services continue to prevent institutionalization and indicates whether these services should continue unchanged, be modified or discontinued.
An RSP is required in the following situation:
- At least every twelve (12) months (365 calendar days) from the date on which the previous service plan was approved, the participant continues to need waiver services, continues to meet eligibility requirements and chooses to continue participation in the waiver.
An addendum or new RSP may be required:
- When the individual's needs change and an adjustment in the level or amount of services is indicated;
- When a change in the participant's living situation occurs that warrants a change in services; and
- When the participant seeks a change in services or content of the service plan.
The RSP must contain a review of the participant's current and previous services and identify the plans and goals for the next twelve (12) month service period. The goal and services should project the participant's service needs for one year following the termination date of the existing service plan. The RSP details the services necessary to maintain the individual safely in the community with available resources and informal supports and should be sufficient to prevent nursing home placement.
The approval of the service plan by the RRDC authorizes the provision and billing of the services identified in the plan. Failure to have an approved service plan at the time-of-service provision or deviation from the approved services identified in the plan will disallow the payment for the services. An applicant must have an approved service plan to be eligible for waiver services and an approved service plan is required to continue to receive waiver services after eligibility. Late submission and/or late approval of a service plan can result in the interruption of services to a participant and penalties to waiver service providers. A service plan cannot be backdated.
Addendum to the Service Plan - The Addendum to the service plan is developed by the Service Coordinator in collaboration with the participant and individual(s) selected to participate in the process and specific service provider(s) when there is a minor change needed in the frequency, duration, type, increase or decrease in existing services, or the addition of a new service that does not change the overall goals or intent of an existing service plan (e.g., the participant's residence has not changed and they wish to increase/decrease the amount of time at a Structured Day Program). These changes are not significant enough to warrant a change in the overall content of the plan. Generally, an addendum is done to increase or decrease a service due to participant choice, not due to a change in medical status or physical need.
General Information About Service Plans
The service plan reflects coordination between all providers involved with the applicant/participant. Input from agencies directly or indirectly involved in the provision of services is necessary. Participant choice is inherent to the service plan development process. The Service Coordinator is responsible for providing unbiased and comprehensive information to the applicant/participant about available services and service providers. This includes a summary of all waiver services available to the applicant/participant.
It is the responsibility of the Service Coordinator to invite representatives of the applicant/participant's choice to be involved in service plan development. The Service
Coordinator is required to include the applicant/participant, their advocate, and any other family or friends the applicant/participant selects. Additionally, at the mid-year Team Meeting, a representative from each of participant's service providers is required to attend the meeting. The SC coordinates the Team Meeting and plan development, but it is ultimately the decision of the participant and their advocate to decide who will participate in the service plan development process.
The Service Coordinator must provide a detailed explanation of the applicant/participant's choices and needs in the service plan, including information regarding relationships, desired living situation, recreation or community inclusion time activities, physical and mental strengths or limitations, spiritual needs and goals for vocational training, employment, or community service. A description of why the waiver services are needed to prevent placement in a nursing home must also be included.
Waiver applicants/participants with limited fluency in English must have access to services without undue hardship. RRDC staff in conjunction with the Service Coordinator must make arrangements to provide interpretation or translation services for applicants/participants who require these services. This may be accomplished through a variety of means, including employing bi-lingual staff, resources from the community (e.g., local colleges), and contracted interpreters. Non-English-speaking applicants/participants may bring an interpreter of their choice with them to meetings with waiver providers and/or the RRDS. However, applicants/participants are not required to bring their own interpreter, and applicants/participants cannot be denied access to waiver services due to an RRDC's difficulty in obtaining qualified interpreters.
The Service Coordinator must identify and coordinate all non-waiver services deemed appropriate and necessary for the applicant/participant. If the applicant/participant is not currently receiving necessary non-waiver services, the Service Coordinator must work with the individual and all necessary partners to obtain any necessary referrals, assessments, and approvals/authorizations.
If the applicant/participant is currently receiving non-waiver services, the Service Coordinator must work with the individual and all necessary parties to obtain any necessary referrals, reassessments, and re-authorizations for the continued provision of these services.
It is the Service Coordinator's responsibility to demonstrate an understanding of the processes required to obtain necessary referrals, reassessments and approvals for waiver and non-waiver services. This includes understanding the procedures necessary to secure services such as physician's orders, prior authorizations, and reauthorizations. When service plans include State Plan services, the Service Coordinator must work closely with the Local Department of Social Services (LDSS), assuring there is no duplication of services and that the necessary authorizations are received.
The Service Coordinator reviews the complete content of the service plan and related services with the applicant/participant. The applicant/participant must be informed of all the options for meeting their needs and preferences.
The service plan reflects coordination between all providers involved with the applicant/participant. It is necessary to obtain input from agencies directly or indirectly involved in the provision of services. Participant choice is inherent to the service plan development process. The Service Coordinator is responsible for providing unbiased and comprehensive information to the applicant/participant about available services and service providers. This includes a summary of all waiver services and service providers available to the applicant/participant.
The applicant/participant's signature is required on the Initial Service plan, Revised Service Plan(s), and any addenda to the service plan. The applicant/participant's signature indicates that the applicant/participant agrees with the information that is included in the service plan, and includes the services requested and the chosen providers of the services. The applicant/participant is the primary decisionmaker in the development of goals, and selection of supports and providers. The completed and approved plan is designed to address needs associated with their health and welfare, independence, productivity, and an ability to return to or remain in the community. The participant must be advised of any changes in the content of the plan.
The RRDS reviews each service plan to ensure it meets the assessed needs of the applicant/participant and reflects waiver participant choice. Once the applicant is enrolled in waiver services, the Service Coordinator monitors the provision of all services in the services plan.
When selecting a waiver provider (including service coordination agency selection), the RRDC will provide the applicant/participant a current list of approved providers for that waiver service in the region. This current provider list will be individualized for each waiver applicant/participant to ensure conflict-of-interest federal requirements are met and that all providers on the individualized provider list are conflict-free for that individual (these conflict-of-interest requirements are listed in 42 CFR 441.301(c)(1)(vi) and can be found here. The RRDC will assist the applicant/participant in selecting a service coordination provider that meets COI compliance requirements. Once selected, a Service Coordinator will review the list of available and appropriate providers with the applicant. These providers will be identified in the service plan. In general, this regulation states that no provider of home and community-based services (HCBS) may provide HCBS and service coordination to the same individual. Due to the nature of certain waiver services in the NHTD waiver program, there are some exempt waiver services that an approved service coordination provider can provide to an individual who is on their service coordination caseload. These waiver services, listed below, are not subject to conflict-of-interest criteria:
- Assistive Technology (AT);
- Community Transitional Services (CTS);
- Congregate and Home Delivered Meals;
- Environmental Modifications (E-mods);
- Moving Assistance; and
- Transportation Services.
If an applicant/participant chooses a service coordination provider that also provides other waiver services (excluding those services listed above), the applicant/participant will be notified that they may not select this provider for any other waiver services (aside from service coordination). When this individual is choosing other waiver service providers, the current provider list provided by the RRDC will not include the individual's service coordination provider. If an individual is already receiving waiver services and must choose a new service coordination provider, any of that participant's current waiver service providers that also provide service coordination will be removed from the current approved service coordination provider list that the RRDC provides to the participant.
Requirements for all Service Plans to Meet Federal Compliance
Service plan development should align with federal, state, and program person- centered planning policies found in statute, regulations, and guidance, and should be driven by the waiver applicant/participant. The process includes identifying strategies for the waiver participant to lead their own planning if desired, resolving disagreements, addressing what is important to the participant and how the team will identify and plan for any known risks the individual may encounter.
The Final Rule, effective March 17, 2014, requires that each individual receiving Medicaid home and community-based services (HCBS) must have a person-centered service plan.
Person-centered planning assists people needing the HCBS construct and describe a service plan that will bring purpose and meaning to their life.
The applicant/participant will lead the person-centered planning process. The process should provide necessary information and support to ensure that the applicant/participant directs the process to the maximum extent possible and is enabled to make their own informed choices and decisions.
If the applicant/participant has a legal guardian, the guardian should have a participatory role, as needed, and as defined by the individual.
The person-centered planning process must only include those people chosen by the applicant/participant. For example, an applicant working on their Initial Service Plan with their Service Coordinator chooses who they would like included in their person-centered service plan process. These participants may include people such as family, friends and/or informal supports. Individuals chosen by the applicant/participant and their selected service providers participate in the applicant/participant's person-centered service planning process.
The person-centered planning process should:
- Be timely and occur at times and locations convenient to the applicant/participant;
- Reflect cultural considerations of the individual;
- Be conducted by providing information in plain language and in a manner that is accessible to applicants/participants with disabilities and/or persons who are limited English proficient;
- Offer informed choices to the applicant/participant regarding the services, and supports they receive and from whom;
- Record the alternative home and community-based settings that were considered by the individual; and
- Include a method for the applicant/participant to request updates to the plan as needed.
Person-Centered Service Plan
The person-centered service plan must reflect the services and supports that are important for the individual to meet their needs identified through an assessment of functional need, as well as what is important to the applicant/participant. This includes but is not limited to their service preferences and the means by which such services and supports will be delivered.
The written plan must confirm that the applicant/participant has chosen the setting where they reside. The setting must also be integrated and support full access to the greater community, this includes:
- Opportunities to seek employment and work in competitive integrated settings;
- Engagement in community life;
- Control of personal resources; and
- Access to services in the community to the same degree of access as individuals not receiving Medicaid HCBS.
The person-centered service plan must:
- Reflect the applicant/participant's strengths and preferences;
- Reflect clinical and support needs as identified through an assessment of functional need and presented by the applicant/participant;
- Include individually identified goals and desired outcomes;
- Reflect risk factors and measures in place to minimize them, including individualized back-up plans and strategies when needed;
- Reflect the services and supports (paid and unpaid) that will assist the individual to achieve identified goals, and providers of those services and supports, including natural supports;
NOTE: Natural/informal supports are unpaid supports that are provided voluntarily to the individual voluntarily in lieu of NHTD HCBS waiver services and supports.- Include those services the applicant/participant elects to self-direct;
- Identify the individual and/or entity responsible for monitoring the plan;
- Be finalized and agreed to, with the informed consent of the applicant/participant in writing and signed by all persons/providers responsible for its implementation; and
- Be distributed to the applicant/participant/providers and other people involved in the plan.
The following requirements must be documented in the person-centered service plan:
- Identify a specific and individualized assessed need;
- Document the positive interventions and supports used prior to any modifications to the person-centered service plan;
- Include a clear description of the person in relationship to their specific assessed need;
- Have measurable goals, objectives and timelines;
- Identify how data will be collected and reviewed to measure the ongoing effectiveness;
- Include a description of the need for the modification;
- Include established time limits for periodic reviews to determine if the modification is still necessary or can be terminated;
- Include informed consent of the applicant/participant; and
- Include an assurance that interventions and supports will cause no harm to the applicant/participant.
B. Plan for Protective Oversight (PPO)
Every service plan includes a Plan of Protective Oversight (PPO). The RRDC reviews every PPO as part of the service plan approval. Any consistent failure in a back-up plan identified in the PPO is reported through the Serious Reportable Incident process. The PPO indicates all key activities that directly impact the health and welfare of the participant and clearly identifies the individual(s) responsible for providing the needed assistance to the applicant/participant in the event of an emergency or disaster. These key activities may include instruction for Home and Community Support Services (HCSS) staff regarding specific oversight and/or supervision needs. If specific instruction for HCSS staff regarding oversight and/or supervision are not listed, HCSS staff will respect the waiver participant's right to privacy except under extenuating circumstances or unless a specific intervention is identified in a behavior plan. All staff working with a participant must read and be familiar with the content of the participant's PPO.
The PPO must be completed by the Service Coordinator with the applicant during the development of the ISP. The PPO must be signed and dated by the applicant and Service Coordinator and all individuals listed as informal supports to the waiver applicant. It is attached with the ISP packet and sent to the RRDC for review and signature. A copy of the PPO must be provided to the participant by the Service Coordinator and maintained in an easily accessible location of the participant's choice within their home. A copy is also provided to each waiver service provider listed in the ISP/RSP. The PPO must be available in the home as a resource to direct service providers.
A new PPO must be completed by the Service Coordinator with the participant each time an RSP is developed for submission with the RSP packet to the RRDS for review. The Service Coordinator, participant, and all individuals listed as informal supports to the participant must sign the PPO.
The PPO must be reviewed by the Service Coordinator with the participant at each Addendum. If there are no changes to the PPO, the participant and the Service Coordinator sign the last page of the Addendum indicating that the PPO was reviewed and there were no changes. If there are any changes, a new PPO must be completed and signed by the participant, Service Coordinator and any individuals listed as informal supports to the participant. The PPO must be attached to the Addendum for submission to the RRDS for review.
Should any information in the PPO change in the interim, the Service Coordinator is responsible for making updates at that time and acquiring signatures from the participant and any individuals listed as informal supports to the participant. The amended PPO must be sent to the RRDC for review and signature.
Once reviewed and signed by the RRDC, the PPO is returned to the Service Coordinator, who distributes it to the participant and any waiver service provider listed in the current service plan. The PPO should be available at the point of service to ensure that any required safety measures are in place at the time-of-service delivery.
If the participant's situation has changed and the participant has an appointed legal guardian, the Service Coordinator will request and obtain the guardian documentation. A copy of this guardian documentation is forwarded to the RRDC. The Service Coordinator is responsible for advising waiver service providers of the new legal guardian. The Service Coordinator, however, does not forward the guardian documentation to waiver service providers.
C. Development of the Initial Service Plan (ISP)
The development of the service plan is the key responsibility of the Service Coordinator. The development of the Initial Service Plan (ISP) begins upon acceptance of the applicant by their chosen service coordination provider. All waiver participants have a choice of their waiver service providers. The waiver participant may change their waiver service providers at any time during the approved service plan period, including Service Coordinators.
The Initial Service Plan (ISP) identifies the recommended services for the first twelve (12) months (365 calendar days) of waiver participation. For waiver applicants residing in a nursing/rehabilitation facility or hospital, the ISP includes current summaries of all services provided and a discharge summary from the facility, including relevant medical reports and assessments. As information is collected for the service plan, the Service Coordinator, taking into account the efficiency of service utilization, must determine whether services are available through informal supports, non-Medicaid local, state and federally funded programs, Medicaid State Plan services, and/or waiver services. Medicaid remains the payer of last resort.
When developing the ISP, the Service Coordinator must collaborate with Local Department of Social Service (LDSS) staff to understand the applicant's history, if any, of participation in Medicaid State Plan community-based services or adult protective services. This will ensure there is no duplication of services.
The Service Coordinator discusses the need for non-waiver options with the applicant to assure that appropriate referrals are made and ensures these services are identified and included in the ISP.
All necessary assessments and evaluations must be completed prior to initiating such services as Home and Community Support Services, Assistive Technology, Community Transitional Services and Environmental Modifications. The Service Coordinator must obtain, complete, and include all applicable supporting documentation with the plan. This includes, but is not limited to: a Home Assessment Abstract, physician's order(s), home evaluation(s), etc.
Upon selection of waiver service providers by the applicant, the Service Coordinator is responsible for contacting each waiver service provider to assure the availability and ability necessary to provide the service(s). In addition, the Service Coordinator coordinates the inclusion of non-waiver services in the individual's service plan. The Service Coordinator must work collaboratively with the applicant, NHTD and non-waiver providers and others to prepare the most accurate and complete service plan for submission to the RRDC. Open communication assists the Service Coordinator in establishing a projected weekly schedule of all services (including days, times and who will provide) with input from the applicant. The schedule also includes the availability of informal supports.
Once the ISP is reviewed with/by the applicant, they are asked to sign the document indicating an understanding of its contents and purpose as written. By signing the ISP, the applicant is consenting to the goals and services identified in the plan. The Service Coordinator then submits the completed ISP as part of the Application Packet to the RRDC for review (refer to Section II of this manual: Becoming a Waiver Participant).
Service plans are expected to evolve as the participant experiences life in the community, requests revisions, experiences significant changes in their condition, or as new service options become available.
D. Coordination of Non-Waiver Services
In addition to the scheduling of waiver services, the Service Coordinator also must identify and coordinate all non-waiver services deemed appropriate and necessary for the applicant. If the applicant seeks to receive or is currently receiving non-waiver services, the Service Coordinator must work to obtain any necessary referrals, assessments, and ensure that approvals/authorizations are completed and maintained.
The Service Coordinator must know the processes required to obtain necessary referrals, assessments, re-assessments and prior approvals and reauthorizations for non-waiver services. This includes understanding which services require physician's orders (e.g., personal care or private duty nursing) and prior approvals/re-authorizations (e.g., authorization from LDSS for personal care and/or prior approval from State DOH or the LDSS for private duty nursing). The RRDS and/or Service Coordinator may identify that the applicant/participant requires the provision of skilled tasks. These tasks are not provided by NHTD waiver services. They may be provided to Medicaid recipients under State Plan services through Certified Home Health Agencies (CHHA), Private Duty Nursing or the Consumer Directed Personal Assistance Program (CDPAP). When service plans include State Plan services, the Service Coordinator must work closely with the LDSS to ensure that there is no duplication of services and that roles and responsibilities are clearly defined.
Once all non-waiver services are identified in the service plan, the Service Coordinator must identify the frequency and duration of the service provision in the Projected/Recommended Weekly Schedule of the ISP. This will prevent unnecessary overlap and/or gaps in services. This schedule serves only as a guidance document and can be amended at the request of the participant or adjusted due to available staff and/or resources. Each service and provider must be identified in the schedule and is responsible to provide the indicated services.
E. Scheduling of Waiver Services
The service plan is the essential tool that clearly states responsibility for each of the services and supports that the participant needs based on a comprehensive, person-centered assessment. The service plan includes the description of methods for addressing the participant's goals and objectives and identifies persons and/or services responsible for implementing and monitoring the plan. These methods are discussed and evaluated at each service plan review. Part of the work in developing an ISP is the scheduling of anticipated services that the applicant will receive. The Projected/Recommended Weekly Schedule of All Services is a one (1) week per diem recommended schedule. The schedule indicates the type of the service (e.g., ILST, CIC, informal supports) and the day(s), time(s) and frequency that each service may be provided as identified in the service plan. The name of each waiver service provider must be documented in the service plan and related charts (e.g., the Waiver Service and Cost Projection form found in the service plan). The name(s) of informal support(s) and specific assistance they are responsible to provide is documented in the Current Supports and Services section of the ISP. The proposed schedule should be flexible to allow for preferences and limitations of the applicant such as a limited attention span or reduced stamina, balanced with the availability of formal and informal supports. It should be designed to meet the goals and needs of the applicant, not the availability of the provider, support the waiver's philosophy of choice, and provide for the health and welfare of the participant.
NOTE: The schedule is a guidance document and can be amended to meet the needs of the participant.
A Team Meeting will be held to review the content of the approved plan and to ensure that all services are in place within thirty (30) days of the date of the approved plan. Any addendum seeking to increase or decrease a service must be presented to, and approved by the RRDC, and confirmed with a Notice of Decision (NOD).
Negotiations for changes in service delivery that do not warrant an addendum will include the waiver participant, Service Coordinator, and impacted providers of waiver and non-waiver services and will be documented in service notes.
The service plan must document any situations in which two services will be provided at the same time to ensure consistent and effective service provision; situations must be clinically justified and time limited. The intent is that the provision of the two services is required to support the individual, not duplicate service. Example: When an Independent Living Skills Training (ILST) provider is assisting/training a participant with a specific task, a Home and Community Support Services (HCSS) staff may be required to assist with personal care during the training session. The overlap of services must be justified and documented in the service plan for both services to be reimbursed.
Services may be rescheduled if the participant is unable to participate or the provider is not available. When the participant requests that a service be suspended for an extended period of time (1 day or more) for any medical or non-medical reason, it is the responsibility of that participant and/or informal support to notify the Service Coordinator who, in turn, notifies the providers. If the participant notifies the provider(s), the participant must also notify their Service Coordinator.
A provider should notify the Service Coordinator when a participant consistently refuses a service. The Service Coordinator should review the service plan with the participant and provider to determine if it needs to be revised to more accurately reflect the goals and abilities of the participant. Revisions to the schedule should allow enough time for the provider to make the necessary arrangements. If a participant refuses significant services that have been determined to be necessary to maintain them in the community safely, it may be necessary to discontinue the individual from the waiver. If a provider routinely cancels a service, the participant should be encouraged to select a new provider. Upon eligibility, a waiver participant must actively participate in waiver services and must participate in Service Coordination on a monthly basis in order to maintain waiver eligibility.
F. Submission of the Application Packet and ISP
Once the potential participant selects a Service Coordination agency who agrees to accept the case, the Service Coordinator has sixty (60) calendar days from the date the RRDC signs the Service Coordination Agency Selection form to submit a completed Application Packet, including the ISP, to the RRDS.
The Service Coordinator must have the Service Coordination Supervisor review and sign the completed Initial Service Plan prior to submission to the RRDS for review. This ensures another level of professional review. If the Service Coordination Supervisor is the Service Coordinator for the applicant/participant, the Service Coordinator Supervisor is not required to obtain an additional supervisory signature. In this situation, the Service Coordination Supervisor must sign the signature page of the ISP as both Service Coordinator and Service Coordination Supervisor.
The Service Coordinator submits the Application Packet with the ISP to the RRDC for review. In addition to the ISP, the Application Packet includes the following documents:
- Freedom of Choice form (DOH-5728) (copy) - signed by the applicant during Intake with RRDS; the original document will be maintained by the RRDC and a copy provided to the selected Service Coordination provider;
- Application for Participation form (DOH-5729) (original) - signed by the applicant during Intake with RRDS; the original document will be maintained by the RRDC and a copy provided to the selected Service Coordination provider;
- Proof of a disability if under 65 years old;
- Written verification from the Medicaid Eligibility Verification System (MEVS) regarding Medicaid coverage that supports community-based long term care services;
- Verification of age (examples: birth certificate, passport, driver license);
- Service Coordination Agency Selection form (DOH-5727) (copy) - signed by the applicant and completed by RRDS;
- Provider Selection forms (DOH-5730) - signed by the applicant and waiver service provider;
- A Level of Care that must be dated within ninety (90) calendar days prior to the Effective Date of the Notice of Decision of eligibility (DOH-5740) and be completed by an individual certified by the State of New York to administer the tool. For individuals transitioning from a nursing home or hospital, the HC-PRI tool may be used to facilitate eligibility and the UAS-NY assessment will be conducted within ninety (90) days of enrollment into the waiver;
- Plan for Protective Oversight (PPO), completed by the Service Coordinator and signed by applicant;
- Waiver Participant's Rights and Responsibilities form (DOH-5732) (copy), signed by applicant during application process; and
- Any Description and Cost Projection form(s) and HCSS assessment form, if applicable, completed by the waiver service provider and submitted by the Service Coordinator.
All other forms and the ISP included in the Application Packet must be complete and signed by the applicant.
Service provision must meet federal conflict-of-interest and integrated settings requirements.
If for reasons beyond the control of the Service Coordinator, the submission of the enrollment package (including the ISP) application is delayed, the Service Coordinator must maintain consistent and open communication with the RRDC. The RRDC may choose to grant an extension. Reasons for extensions include but are not limited to: delay in establishing a residence, unexpected hospitalization, nursing home admission, or a change in the applicant's request for services.
If the Service Coordinator does not meet the sixty (60) calendar day-time frame for submission of the ISP packet, does not meet the criteria for an approved extension(s) period, or it appears the applicant will not become eligible for services within a reasonable period of time, the Service Coordinator and Service Coordination Supervisor receives written notification from the RRDC indicating that the Application Packet is past due. When submission of an Application Packet exceeds one hundred twenty (120) days, an NOD Denial (DOH-5737) will be issued.
If late submission of Application Packets becomes a repeated problem for an agency, the RRDC will notify NYSDOH of this problem. If remedial action is not imminent, NYSDOH will advise the RRDC to remove the Service Coordination agency from the list of available service providers indicating the intent to withhold new referrals until a written plan of action is submitted and approved by the RRDC. If this problem is not corrected, NYSDOH will initiate action to disenroll the provider from the waiver program.
G. Review and Determination Process for the ISP
Upon receipt of the Application Packet and ISP, the RRDC has fourteen (14) calendar days to review the information and issue a NOD.
The RRDS completes the Initial Service Plan Review form and reviews the ISP.
If the needs of the applicant appear to be medically complex, the Nurse Evaluator (NE) will review the ISP to ensure all options are explored and services are adequate to meet the needs of the individual prior to plan implementation.
If there are any discrepancies/concerns regarding the service plan, the RRDC must return it to the Service Coordinator for correction or additional information. This is documented on the RRDS Initial Service Plan Review form.
The Service Coordinator has fourteen (14) calendar days to respond to the RRDS's request for additional information or corrections and resubmit the Service Plan to the RRDS for final review and determination. Prior to resubmission of the ISP, the Service Coordinator must present the revised plan to the applicant for review and signature. Continued lateness will result in the provider being removed from the list of available providers. If the ISP is not returned within fourteen (14) calendar days or is returned and does not meet waiver requirements, an NOD Denial (DOH-5737) will be issued. In order to facilitate waiver services to an applicant, an ISP will not be withheld for non- substantive corrections (e.g., inappropriate formatting and grammatical errors). These errors will be noted on the Service Plan Review form. Upon final determination, the RRDS signs the Service Plan Review form and returns it with the service plan to the Service Coordinator who in turn sends it to the applicant. The Service Coordinator will make the corrections to the ISP as indicated in the Service Plan Review form and review the changes with the participant at the thirty (30) day Team Meeting; however, resubmission of the ISP to the RRDC is not required.
If the application packet is approved, the applicant is acknowledged as a 'participant'. The RRDC must complete the Notice of Decision (NOD) Authorization (DOH-5740) and distribute it to the participant and all others listed on the NOD (refer to Section II - Becoming a Waiver Participant and Section IX - Due Process). If an applicant is transitioning from Managed Long Term Care (MLTC) services, all MLTC codes must be removed from the case before waiver services can begin. The RRDC will return the Application Packet to the Service Coordinator, who must provide a copy of the ISP and PPO to the participant. The Service Coordinator communicates the authorization and the effective date to the facility (e.g., nursing home, hospital) if applicable, and to all non-waiver providers involved in the ISP. The Service Coordinator also sends a copy of the approved ISP and PPO to all NHTD waiver service providers responsible for delivery of the services and items identified in the ISP. A copy of the service plan and the PPO must be available in the participant's home as a resource for service providers. In order to ensure that all the services identified in the service plan are in place, a Team Meeting will be conducted within thirty (30) days of the effective date of the service plan.
If the RRDC determines that the applicant does not meet waiver eligibility criteria, the RRDC completes and sends a NOD Denial of Waiver Program to the applicant and Service Coordinator. The Service Coordinator, in consultation with the RRDC, will provide alternative referral options (e.g., names and phone numbers of other LTC programs) to the denied applicant. The Service Coordinator will notify all waiver and non-waiver providers involved in the development of the ISP of the denial decision.
H. Waiver Contact List
The Waiver Contact List is included in the waiver participant's service plan packet supplied by the Service Coordinator. The list contains a current listing of the waiver participant's waiver service providers as listed in the ISP/RSP. This list includes the services provided, names of the provider agencies, names of the persons providing the services and their phone numbers, names of the service providers' supervisors and the supervisors' phone numbers. This list must comply with Conflict-of-Interest rules. Also included in the contact information are all pertinent emergency phone numbers, the NHTD Complaint Line and contact information for the RRDC.
Waiver service providers are responsible for contacting the Service Coordinator when contact information pertinent to the participant changes. A copy of the Contact List should be posted in the home for easy access to the participant, family and staff.
The Service Coordinator retains a copy of the most updated contact list in the participant's file. The Contact List is amended each time a new waiver service is initiated; when changes in contact information occurs; annually when an RSP is submitted; or upon addendum of a service plan. The Service Coordinator must routinely review the Contact List with the participant to ensure it is correct and up to date. If changes are warranted, the Service Coordinator will make needed updates and redistribute the contact list.
I. Implementation of the Approved Service Plan
The RRDC confirms the effective date for the initiation of services with the Service Coordinator. Services may not be provided without the approval by the RRDC. The RRDC and the service providers must confirm that all required Medicaid eligibility and codes are in place prior to service provision. Prior to provision of waiver services, the Service Coordinator must ensure that the participant remains Medicaid eligible and appropriate program eligibility codes (Restriction/Exception (R/E) codes) are in place. Waiver services may only be provided by approved waiver service providers.
To ensure that the services identified in the service plan are in place, a team meeting will be conducted within thirty (30) days of the effective date of the service plan. Effective dates of service plans cannot be retroactive. The Service Coordinator documents the team meeting by completing a Team Meeting Summary form which must be submitted to the RRDC within fourteen (14) days of the date of the meeting. The Service Coordinator must also send a copy of the Team Meeting Summary form to the participant, and all active waiver service providers. Participation in Team Meetings is billable by the provider and meeting hours must be designated and approved in the service plan.
During the service plan's initial thirty (30) day period, the waiver service provider(s) will develop the Detailed Plan to be discussed at the thirty (30)-day Team Meeting.
Detailed Plan
A Detailed Plan is developed and implemented by the individual waiver service provider to identify the specific tasks and activities to be provided by the waiver provider in support of the participant's overall goals as identified in the service plan.
The Detailed Plan includes:
- All assessment(s) conducted by the waiver service provider;
- Participant's goal(s) as it/they relates to the specific waiver service that is the subject of the Detailed Plan;
- Milestones and activities needed to meet the goals identified in the Detailed Plan;
- Interventions needed by the waiver service provider to assist the participant in meeting their goals; and
- Timeframes in obtaining the participant's individualized goals.
Communication is critical to the success of a service plan. Waiver service providers must communicate with each other, informal supports and non-waiver providers at all times, especially when there is an overlap in the provision of services to the participant. Often, a participant has a personal goal that crosses over multiple service providers. An example of this is the provider of Positive Behavioral Interventions and Supports (PBIS) communicating with other waiver service providers on methods of working with a participant to address behavioral issues and needed supports.
If at any time a waiver participant or waiver service provider determines there is a need to change the amount, frequency or duration of services approved in the service plan, the Service Coordinator must be notified. No changes may be made to a service plan by the waiver service provider until the Service Coordinator is notified, and the participant and RRDC approve the changes or an Addendum or RSP is completed. The approval of the service plan by the RRDC is the prior authorization of the service and, in turn, authorizes billing.
Waiver service providers must recognize that Detailed Plans are ever-changing as the needs of the participant change. Therefore, re-assessment of a waiver participant's strengths and needs are on-going and the way in which services are provided may require adjustment and adaptation for the participant. These techniques are a critical element of the Detailed Plan.
J. Ongoing Review of the Service Plan
The Service Coordinator should regularly review the service plan with the participant. This review is a natural component of the meetings between the participant and Service Coordinator. Prior to approval of the Initial Service Plan, the Service Coordinator must contact the applicant monthly. Upon approval of the Initial Service Plan, the Service Coordinator must meet with the waiver participant face-to-face at least once a month.
One of these visits must occur in the participant's home no less than quarterly in order to assure receipt of required care. This is always a good opportunity to discuss the efficacy of the services offered with the waiver participant.
Service plan reviews should focus on all aspects of the participant's life, including:
- Satisfaction with the performance of providers and informal supports;
- Satisfaction with living situation;
- Adequacy of supports and services;
- Provision of the waiver services in accordance with the approved service plan, ensuring that at a minimum of one waiver service is provided per month;
- Sufficient opportunities to participant in community activities;
- Achievement of goals related to waiver services;
- Changes in function and behavior; and
- Changes in priorities or goals.
Any issues identified must be addressed by the Service Coordinator with the provider, other necessary parties and/or RRDC, as appropriate. This information must be documented in the Service Coordinator's case notes and made available to the RRDC as needed.
Other events that may trigger a service plan review include:
- The participant requests a change in services or waiver service providers;
- There are significant changes (improvement or decline) in the participant's physical, cognitive, and/or behavioral status;
- A new waiver service provider is approved for the NHTD waiver and the participant is interested in either changing to that waiver service provider or adding a newly available service;
- The expected outcomes of the services are either realized or need to be altered; and/or
- Notification from a non-waiver provider of the need to change amount, frequency and/or duration of services.
To ensure services are provided in the most integrated and efficient manner, providers attend regularly scheduled (at least every six (6) months from the last Team Meeting) Team Meetings to discuss progress toward the participant's goals, identify any impediments to achieving projected milestones and address any issues affecting the participant. After a Team Meeting, a Team Meeting Summary form is completed by the Service Coordinator. The Service Coordinator then sends a copy of the Team Meeting Summary form to the participant, the RRDC, and all active waiver service providers within fourteen (14) days of the Team Meeting. Regularly scheduled Team Meetings with the participant and service providers are an essential part of ensuring the participant's health and welfare.
For plans that include one or more non-waiver services, the review of the plan must include timely outreach and coordination with all involved parties (service providers, informal supports, family members and other advocates) to discuss the waiver participant's progress and need for services.
K. Development of the Addendum
Requests for changes to the service plan may come from the participant, family members, the Service Coordinator, other waiver service providers or other involved parties. The Service Coordinator is responsible for working with the participant and anyone chosen by the participant to participate in the development of the Addendum.
Once the Addendum has been written by the Service Coordinator, it must be reviewed and signed by the participant for submission to the RRDS for review and determination.
L. Submission of the Addendum
The Service Coordinator will submit to the RRDC the completed and signed Addendum and a copy of each of the following documents:
- Waiver Contact List, if revision is necessary;
- A new PPO, if revisions are made that impact the PPO or if no changes were required, a copy of the PPO with an updated signature page;
- Individual Service Report (ISR), only if a waiver service is being, increased, decreased, or discontinued; and
- Insurance, Resources and Funding Information sheet (if any information has changed).
M. Review and Approval Process for the Addendum
The RRDS must review the Addendum to determine the need for changes in the service(s).
There may be a need for an emergency increase of services to a participant to meet their health and welfare in the community; for example, the caregiver has an unplanned hospitalization. In these unexpected events, the Service Coordinator needs to contact the RRDS and obtain verbal approval for the increase in service(s). All communication between the RRDS and the Service Coordinator must be documented in their respective records and included in the service plan. If the emergency service(s) is intended to be ongoing, then the Service Coordinator must submit an Addendum to the RRDS for approval within two (2) business days.
Upon receipt of the Addendum, the RRDS will complete the RRDS Addendum Review form. The RRDS must review the Addendum within five (5) business days and send the review form to the Service Coordinator if any changes are necessary. The Service Coordinator resubmits the Addendum to the RRDS with the corrections made within five business days. If the Addendum is approved, the RRDS will send the approved Addendum and NOD to the participant and the Service Coordinator. The existing timeline and approval dates for the service plan remain in effect.
A Notice to increase, add, decrease, terminate or deny services (DOH-5735, DOH-5739, DOH-5734) will be issued after the Addendum is reviewed by the RRDS.
If an Addendum to the service plan is denied, the RRDC will issue a NOD Denial (DOH-5734) to the participant and Service Coordinator. The participant may choose to exercise due process related to the decision (refer to Section IX - Due Process of this manual). If no action is initiated, the Service Coordinator must work with the participant to find alternative solutions. Technical assistance from the RRDC may be requested at any time.
A copy of the Addendum is provided to all active waiver service providers involved in the current service plan by the Service Coordinator.
N. Development of the Revised Service Plan (RSP)
The Revised Service Plan (RSP) is re-written and approved by the RRDC annually. In preparation for the RSP, a Team Meeting will be conducted six (6) months from the last Team Meeting. If there is a significant change in the participant's needs for support and services or the participant's life situation, or it is requested by a participant, a new RSP may be developed. The Service Coordinator works with the participant, anyone the participant selects to participate, and other necessary parties in the development of the RSP. At this time, the activities of the current service plan period are reviewed to assess the participant's current status and to determine whether goals have been met successfully. Waiver participants must actively participate in waiver services to maintain waiver eligibility. The continued need for participation in the waiver program to avoid nursing home placement is also determined by the Service Coordinator. The participant must continue to need a nursing facility level of care to maintain waiver eligibility.
The Service Coordinator conducts a Team Meeting to develop the RSP; this is held six (6) months from the date of the last Team Meeting. Prior to this meeting, required waiver service providers will submit an Individual Service Report (ISR) to the Service Coordinator for review and consideration at the Team Meeting.
The RSP is due to the Regional Resource Development Center (RRDC) at least sixty (60) days prior to the last day of the twelve (12) months of the most recently approved service plan. Included in the submission of the RSP, the Service Coordinator must also submit the Team Meeting Summary and ISRs from the Team Meeting held to develop the RSP. This is necessary to prevent delays in service that would adversely affect the health and welfare of the participant.
To ensure this is done, the Service Coordinator must:
- Work with the participant to arrange for and facilitate a Team Meeting that must be held prior to the end of the current service plan period to develop the proposed RSP and ensure timely submission of the service plan. Attendees include the participant, waiver service providers, legal guardian and anyone invited by the participant, including informal supports, and other interested parties, which may include non-waiver providers involved in the Service Plan. The Team Meeting provides an opportunity to discuss issues that cut across services and discuss/resolve concerns regarding health and welfare; and
- Receive all current required waiver service providers' Individual Service Reports (ISRs) prior to the Team Meeting. The Service Coordinator also develops an ISR for Service Coordination. For the Service Coordinator to develop the RSP appropriately, it is imperative that all current required waiver service provider ISRs are complete and submitted timely.
An Individual Service Report (ISR) provides a summary and update of the waiver participant's progress to meet the goals identified in the service plan. Each ISR must contain the following information:
- Each of the participant's goal(s) for this service that have been addressed during the current service plan;
- The interventions used to address each goal as described in the Detailed Plan(s);
- Any progress made for each goal;
- Any barriers to progress toward each goal;
- The participant's goal(s), expected interventions and outcomes for this service in the next service plan;
- Recommendations for amount, frequency, and duration of this service in the next service plan; and
- An explanation of why this service is necessary to ensure the health and welfare of the participant in the next service plan.
The Service Coordinator also uses information from the current service plan, including addenda submitted during the service plan period. For new services, the Service Coordinator must collaborate with the provider(s) selected by the participant to ensure that there is appropriate documentation for the RSP, including the justification for the new service.
Providers must notify the Service Coordinator when a participant repeatedly refuses a service or repeatedly asks that the service be rescheduled. The Service Coordinator reviews the service plan with the participant to determine if it needs to be revised to more accurately reflect the goals and abilities of the participant and/or scheduling issues. Revisions to the schedule should allow enough time for the provider to make the necessary arrangements. When a participant refuses all waiver services, it is necessary to evaluate their continued participation in the waiver. Waiver participants must actively participate in waiver services to maintain eligibility.
For plans that include non-waiver service providers, the review of the plan must include timely outreach and coordination with all non-waiver providers identified in the service plan (e.g., review of plans including personal care, certified home health agency, or private duty nursing must be considered with those providers and the agencies responsible for approving/authorizing services).
The Service Coordinator must discuss any proposed changes to the service plan with the participant and the individual(s) who participated in the development of the RSP prior to submission of the plan to the RRDC.
The RSP must be signed by the participant or participant's legal guardian to indicate that the participant understands its contents and purpose as written.
The Service Coordinator Supervisor is expected to meet with any waiver participant prior to the completion of the RSP developed by a Service Coordinator under their supervision. The Supervisor and Service Coordinator are both expected to sign the RSP upon its completion. This provides a level of professional review identifying any inconsistencies or problems in the service plan that could impede the approval process.
As previously stated, the Service Coordinator submits the completed and signed RSP and any required documentation to the RRDS for review at least sixty (60) calendar days prior to the end of the current service plan period. The RRDS reviews the RSP within fourteen (14) calendar days of receipt utilizing the RRDS RSP Review Form. If corrections are needed, the RRDS sends the form back to the Service Coordinator. The Service Coordinator will resubmit the RSP with corrections in less than fourteen (14) calendar days. In order to facilitate waiver services to a participant, the RSP will not be withheld for non-substantive corrections (e.g., inappropriate formatting and grammatical errors). These errors will be noted on the Service Plan Review form. Upon final determination, the RRDS signs the Service Plan Review form and returns it with the service plan to the Service Coordinator who in turn sends it to the participant. The Service Coordinator will make the corrections to the RSP as indicated in the Service Plan Review form; however, resubmission of the RSP to the RRDC is not required. The Service Coordinator must still correct the plan and advise the participant of the correction(s).
O. Delinquent Individual Service Report (ISR) From Waiver Service Providers
Waiver service providers are responsible to submit their ISRs prior to the Team Meeting to the Service Coordinator to avoid interruption of service to the participant (with exceptions as noted in Section VII - Record Keeping).
NOTE: ISRs are not required for the initial 30-day Team Meeting.
The Service Coordinator is also required to submit a complete and timely ISR as part of the development of the RSP.
At the Team Meeting, if a waiver service provider determines that changes need to be made to the ISR to better reflect the participant's needs, that waiver service provider may request one (1) additional business day to revise and resubmit the ISR to the Service Coordinator. In some situations, an ISR can only be completed after decisions are reached during the Team Meeting.
NOTE: If at any time the RRDS feels the information provided in the ISR from any waiver service provider requires further explanation, the RRDC may request that the Service Coordinator obtain and submit a revised ISR that more accurately reflects the Detailed Plan. The RRDC may request any supporting documents necessary to review the service plan.
Each waiver service provider is responsible to develop and submit ISRs in accordance with timelines established in this section of the Program Manual. Therefore, when a waiver service provider does not submit a timely ISR and does not communicate the need for additional time to submit an ISR with the Service Coordinator, the Service Coordinator must notify the RRDC. The RRDC will contact the waiver service provider advising that the plan approval may not proceed without the ISR. Failure to submit the ISR within seven (7) calendar days of the date of contact may result in administrative action.
If at the end of the seven (7) calendar days the waiver service provider has not complied with the submission of the ISR, the Service Coordinator must contact the RRDC for further follow-up. Upon receipt of the ISR, the Service Coordinator notifies the RRDC. If a provider continues to fail to provide needed reports, the RRDC will contact NYSDOH to alert them of the trend and will remove the provider from the list of available waiver service providers in the region. The participant may be asked to select a new service provider.
In circumstances in which the waiver service provider may not be able to submit the ISR on time, the waiver service provider must maintain open communication with the Service Coordinator regarding the reasons for late submission. The Service Coordinator must contact the RRDS and communicate this delay. The Service Coordinator will provide an explanation that the ISR was not timely submitted in the RSP and copy the provider. The Service Coordinator should proceed with the development of the Service Plan to maintain the timeline for submission to the RRDS for review.
If a waiver service provider fails to comply with the timelines for submission of ISRs, the RRDC notifies DOH waiver staff of the waiver service provider's continued delinquency. DOH waiver staff will discuss the matter with the RRDC and determine if the provider should be removed from the list of available service providers in the region.
P. Submission of the RSP
The Service Coordinator must submit the completed RSP packet to the RRDS for review. The RSP packet includes the RSP and the following:
- Written verification from the Medicaid Eligibility Verification System (MEVS) regarding the participant's Medicaid status;
- Community Health Assessment Level of Care report;
- Team Meeting Summary held to develop the RSP;
- ISRs from all direct service waiver providers (see Section VI - Waiver Services for a list of direct and non-direct waiver service providers);
- Provider Selection forms (if applicable);
- Confirmation of reauthorizations/re-approvals of pertinent non-waiver services (e.g., Medicaid State Plan services);
- Plan of Protective Oversight (PPO) - newly written and signed;
- Insurance, Resources and Funding Information sheet completed and signed;
- Waiver Participant Rights and Responsibilities form, completed annually; and
- Description and Cost Projection forms and HCSS Assessment (if applicable).
Q. Delinquent Submission of the RSP by the Service Coordinator
Late submission of an RSP by the Service Coordinator can result in the interruption of services to a participant and potentially lead to discontinuation of the waiver participant from waiver services. A participant must have a current and approved service plan in order for services to continue and a provider bill for the service. Continued failure to submit timely RSPs will result in removal from the approved provider list for the region and possible disenrollment of the service coordination provider agency. A complete, acceptable RSP packet must be submitted to the RRDS for approval at least sixty (60) calendar days prior to the end date of the current service plan.
When the Service Coordinator is facing unforeseen circumstances that affect the submission of the service plan within the required timeframe, the Service Coordinator must make immediate contact with the RRDS for technical assistance. A plan must be established that will prevent disruption of services to the participant, potential penalties to the service coordination agency, and billing concerns for all waiver service providers.
When a RSP packet is not submitted to the RRDC by the Service Coordinator at least sixty (60) calendar days prior to the end date of the current service plan, the following protocol will be implemented:
Notification of Late Submissions
Notification will be sent to the service coordination agency supervisor by the RRDC via priority mail or return receipt e-mail anytime a RSP packet is not submitted by the required timeframe (sixty (60) calendar days prior to the end of the current service plan period). It informs the service coordination agency supervisor that communication with the RRDC is necessary to ensure that the RSP packet is submitted within seven (7) calendar days. It further informs the supervisor that failure to comply will lead to the provider being removed from the list of available service providers in the region. Failure to submit an acceptable RSP packet within this time frame constitutes breach of the Provider Agreement, leading to potential provider disenrollment. If there is a break in approved service plans due to failure to obtain an approved service plan, a provider cannot bill for any services provided during the period the plan dates are interrupted.
It is the responsibility of the Service Coordinator to contact all waiver service providers involved in the RSP that billing for waiver services is prohibited until the RRDS receives and approves the RSP packet. Without the approval of the service plan by the RRDC services are not authorized.
When NYSDOH waiver staff and/or the RRDC are informed of any issue(s) regarding the provision of services by an approved waiver service provider, NYSDOH waiver staff and the RRDC may choose to restrict a waiver service provider's opportunity level. This decision is based on performance evidence, conflict-of-interest criteria, investigation, complaints and/or identified trends. For more information on the opportunity level restriction, see "NYSDOH Restriction of a Waiver Service Provider" in Section III of the program manual.
The RRDC will remove the provider from the list of available providers for the region until a plan to remedy the deficiencies is submitted, reviewed and approved by the RRDC. The RRDC is responsible for distributing the new list of available providers. The RRDC will provide NYSDOH with the updated available provider list on a quarterly basis.
Repeated late submissions of RSP packets may result in the initiation of the provider disenrollment process whereby the service coordination agency will no longer be able to serve NHTD waiver participants. The RRDC will request that NYSDOH disenroll the provider. NYSDOH will notify the Provider Enrollment Unit that the provider be removed as an approved Medicaid waiver service provider.
NYSDOH will advise the provider of the date of disenrollment and advise the agency of the requirements for transitioning all waiver participants to new waiver service providers.
R. Review and Approval Process for the RSP
The RSP review process must be completed by the RRDS within fourteen (14) days of receipt of the service plan.
Upon receipt of the RSP packet, the RRDS uses the RRDS Revised Service Plan Review form while reviewing the RSP to determine if:
- The individuals' health and welfare were maintained in the previous service plan and, if not, what changes need to occur;
- The participant continues to need and receives a waiver service at least once a month;
- Written verification from the Medicaid Eligibility Verification System (MEVS) regarding Medicaid coverage that supports community-based long term care services is attached;
- The UAS-NY is current, and reflects a nursing facility Level of Care;
- The RSP is reasonable given the context of the participant's stated goals;
- All available informal supports and non-waiver services have been appropriately arranged and are utilized;
- The services/providers requested by the participant comply with Conflict-of-Interest criteria;
- Waiver services are being used in a reasonable and effective manner;
- The services described in the RSP will maintain the participant's health and welfare;
- The frequency and duration of the services requested are appropriate, adequately meet the person's needs and are not excessive;
- The goals and preferences described in previous service plans have been the focus of the activities in the last twelve (12) months (365 calendar days);
- The PPO is complete, provides sufficient protections while ensuring the participant's rights and signed by the participant;
- The Insurance, Resources and Funding Information Sheet is completed and signed;
- All other required forms (e.g., Cost Description and Projection forms, social transportation grid, HCSS assessment form, if applicable) are completed, signed by the participant, and attached to the RSP; and
- The participant and all identified providers in the plan have signed the RSP.
NOTE: If the needs of the participant appear to be medically complex in nature, the RRDS will request additional review of the RSP by the NE or request additional medical information.
The RRDC has fourteen (14) calendar days to review the RSP. If the RSP is submitted timely and the RRDC deems that corrections are necessary, the Service Coordinator has an additional fourteen (14) calendar days to respond to the RRDC's request for additional information or corrections and resubmit the Revised Service Plan to the RRDS for final review and determination. Prior to resubmission of the RSP, the Service Coordinator must present the revised plan to the participant for review and signature. Continued lateness will result in the provider being removed from the list of available providers. If the RSP is not returned within fourteen (14) calendar days or is returned and does not meet waiver requirements, an NOD Discontinuation may be issued. In order to facilitate waiver services to a participant, an RSP will not be withheld for non- substantive corrections (e.g., inappropriate formatting and grammatical errors). These errors will be noted on the Service Plan Review form. Upon final determination, the RRDS signs the Service Plan Review form and returns it with the service plan to the Service Coordinator who in turn sends it to the participant. The Service Coordinator will make the corrections to the RSP as indicated in the Service Plan Review form; however, resubmission of the RSP to the RRDC is not required.
If there are any discrepancies in the information provided in the RSP, or the RRDS is seeking changes and the RSP may not be approved, the RRDS will discuss required changes with the Service Coordinator. This is documented on the RRDS Revised Service Plan Review form which is sent with the RSP packet to the Service Coordinator for correction. The Service Coordinator discusses the issues and/or any alternative options with the participant.
The Service Coordinator returns the corrected/amended RSP packet to the RRDC for re-review. Upon approval, the RRDS signs the RSP and PPO and returns them to the Service Coordinator. The Service Coordinator provides a copy of the RSP and PPO to the participant, all waiver service providers included in the RSP and others as appropriate. The Service Coordinator may also need to discuss the content of the plan with other key parties who do not necessarily require a copy of the RSP.
The RRDS completes and issues the appropriate Notice of Decision (NOD) based on resulting changes to services from the previous Service Plan; e.g., increase, decrease, addition. Should the approval of the RSP indicate no changes in waiver service(s) from the previous service plan, a new NOD is not required. The approval of the service plan by the RRDS is sufficient authorization. The RRDS' signature on the service plan designates the service approval. If there is an increase/reduction or discontinuation of a service, a NOD indicating the change is issued. The Service Coordinator distributes a copy of the NOD form to the approved waiver service provider(s). The NOD informs the participant of their rights regarding the decision, including their right to a Case Conference and a Fair Hearing with aid continuing, if applicable (refer to Section IX - Due Process).
Upon denial of a service identified in the service plan, the RRDC must relay this to the Service Coordinator and issue the NOD Denial of Waiver Service and/or Denial of a Waiver Provider. The Service Coordinator is responsible to give a copy to the participant and others listed on the NOD form. It is the responsibility of the Service Coordinator to review Case Conference and Fair Hearing rights with aid continuing, if applicable, with the participant and document this in their record when they are reviewing the NOD.
The Service Coordinator discusses the reasons for denial and service alternatives with the participant. An appropriate transition/discharge plan will be developed and reviewed with the RRDS.
S. Process for Changing a Provider
The participant's ability to change a waiver service provider is an essential component of assuring participant choice. It also allows a waiver service provider the opportunity to recognize that it can no longer meet the participant's service needs.
NYSDOH has the responsibility to ensure informed choice of providers for all participants. Additionally, it is responsible to ensure available provider lists present conflict-free choices for the applicant/participant. In the event of coercion by providers, the provider will be subject to appropriate remedial actions. Such actions may include suspension of the ability to provide services to new participants or disenrollment of the agency as an approved HCBS/NHTD waiver provider. Service Coordinators are not permitted to recommend a provider or to "steer" a participant to a particular provider.
a. Participant Request to change a provider agency
If the participant chooses to change their waiver service provider, the Service Coordinator must utilize the following procedure:
- The participant or their current Service Coordinator informs the current waiver service provider of the participant's intent to change waiver service providers;
- The Service Coordinator will contact the RRDC and advise them of the participant's desire to change their provider agency;
- The RRDC will provide the participant with a list of approved and available waiver service providers for the participant to interview and make their choice;
NOTE: NHTD waiver applicants/participants are offered choice of provider and not of a specific staff person.- Upon selection of a new waiver service provider, the participant will inform the Service Coordinator of their preference. The Service Coordinator will complete the Change of Provider Request form (DOH-5750) with the participant and send the completed and signed form to the selected waiver service provider;
- The requested waiver service provider must review the form and complete the Statement of Requested Provider indicating the approval of the participant's request or the denial of the participant's request with a reason for denial. The form must then be returned to the Service Coordinator within five business days of receipt;
- If the requested waiver service provider declines the participant's request for services, the Service Coordinator must inform the participant and ask them to select another waiver service provider from the list. The selection process proceeds;
NOTE: Waiver service providers are voluntary and may decline service provision without cause. The Service Coordinator maintains all completed Change of Provider forms in the participant's record.- When the requested waiver service provider accepts the participant's request, the Service Coordinator submits the Change of Provider Request form to the RRDS for review and determination. The RRDS's decision is documented on the Change of Provider Request form and sent back to the Service Coordinator;
- If the RRDS approves the provider change, the Service Coordinator will establish a date and time for the Transition Meeting and documents this on the Change of Provider Request form. The RRDS may contact the waiver participant to confirm "free choice" of the provider;
NOTE: The Transition Meeting provides an opportunity for current provider(s) to meet with newly selected providers to exchange information ensuring the success of the new provider(s) with the least amount of disruption to the participant. The Service Coordinator documents this information on the Change of Provider Request form.- The RRDS reviews the request and upon approval, sets an effective date for the change. The RRDS will send the approved Change of Provider form to the participant, Service Coordinator, and all current and new waiver service providers;
- If the RRDS does not approve the request for a change of waiver service provider, the RRDS will indicate the reason why (e.g., the waiver service provider does not meet conflict-of-interest criteria or is no longer an approved provider of NHTD services) on the Change of Provider Request form and immediately notify the Service Coordinator, sending the form back to the Service Coordinator to be maintained in the participant's record. When this occurs, the RRDS will complete and send the NOD Denial of Waiver Provider/Waiver Service form to the participant and others designated on the form;
- The Service Coordinator must work with the participant to select another waiver service provider, which restarts the Change of Provider process;
- When the request for Change in Provider is approved by the waiver service provider and the RRDS, the Service Coordinator must facilitate the Transition Meeting during which participant information is reviewed and transferred to the new provider, ensuring a smooth transition occurs;
- Once this process is completed, the Service Coordinator must update the Waiver Contact List and provide a copy to the participant and other current waiver service providers as appropriate;
- If the participant chooses to change their service coordination provider, the RRDS must work directly with the participant through the above process; and
- The participant, Service Coordinator or any provider should contact the RRDS if this procedure is not followed.
NOTE: If the participant requests to remain with the same agency but change agency employee, the agency is responsible for ensuring the participant's choice in meeting this request. When a request in agency employee occurs, a change in provider form is not necessary. The process is internal within the provider agency. If the participant's request cannot be met by the agency, the agency must notify the Service Coordinator for assistance. The provider is not obligated to provide a specific staff assignment and may consider the needs of the organization when making staff assignments.b. Provider Request to discontinue an applicant/participant
When a waiver service provider is unable to or wishes to no longer provide services to a participant, the following procedures must be followed:
- The waiver service provider must inform the applicant/participant of its intent to terminate service provision. This must be done at a minimum of thirty (30) calendar days prior to stopping the provision of service(s);
- Notification must be sent via priority mail or hand-delivered to the participant. A copy of the letter must also be sent to the Service Coordinator and the RRDC;
- Reasons for the termination must be included in the letter;
- The RRDC will provide the applicant/participant with a list of available waiver service providers from which to interview and select;
- If it is the Service Coordination agency seeking to discontinue services to the applicant/participant, then the RRDC is responsible for providing the participant with a list of available conflict-free service coordination agencies from which to select;
- Upon selection of the new waiver service provider, the participant will inform the RRDC and the Service Coordinator of their selection in order to assist the participant through the completion of the Change of Provider Request form;
- The current waiver service provider must work closely with the newly requested waiver service provider and the Service Coordinator (or RRDS, as appropriate) to assure that a smooth transition occurs and that all appropriate documentation is provided to the new agency; and
- The Service Coordinator must amend the service plan to reflect the change in waiver service provider.
c. Staff no longer able to serve a participant
When a staff member of a waiver service provider will no longer be providing services to a participant due to reassignment or resignation, the following procedures apply:
- The staff member or agency supervisor must notify the participant of the employee's intent to leave their assignment and advise the participant to discuss the change with their Service Coordinator. The participant can remain with the agency or choose to change waiver service providers
- The staff member or the agency supervisor notifies the Service Coordinator of the staff departure.
- The Service Coordinator meets with the participant to determine if a new waiver service provider is desired. If the participant desires a new waiver service provider, the Service Coordinator will assist the participant through the Change of Provider process (refer to Changing Waiver Provider section above).
- If the participant chooses to remain with the current waiver service provider, the Service Coordinator must work with the participant and agency supervisor to assure that no lapse in staff coverage occurs.
- The Service Coordinator will amend the current service plan to reflect any change, if needed.
- When it is the Service Coordinator leaving the agency, the RRDS will talk with the participant about their continued interest in remaining with this service coordination agency. If the participant desires to change service coordination agencies, the RRDS will assist them through the change of service coordination provider process.
- If the participant chooses to remain with the current service coordination agency, the agency will work with the participant and the agency supervisor to ensure that no lapse in staff coverage occurs.
d. Establishing the date for change
As a final step in the process of changing waiver service providers, the RRDS will establish the date for the change in service provider to ensure that no lapse in service provision occurs. The following timeline applies. Due to billing requirements, Service Coordination must change on the first of the month (refer to Section VI - Waiver Services); and
- The provider must notify the participant with at least thirty (30) days' notice of the change. The RRDS may make the change of waiver service providers effective upon receipt of the Change of Provider Request form if it is determined that the health and welfare of the participant is at risk. This may be accomplished verbally or in writing.
During the transition period, the Service Coordinator will arrange for a Transition Meeting between the current and new providers and the participant to exchange information. In the event the Service Coordinator is the provider/staff changing, the RRDS will arrange for such a Transition Meeting. The current provider is responsible for providing the new provider with copies of all evaluations, ISRs, and an update of what has been accomplished since the last service plan. This process must comply with all laws, such as the Health Insurance Portability and Accountability Act (HIPAA), regarding confidentiality and the release of medical and NHTD waiver services material. A provider cannot terminate a case until the RRDC determines a successful transition has been implemented,
T. Transferring Regions
The participant may choose or need to relocate to a different region of NYS. To preserve continuity of services, meaningful exchange of information between the sending/receiving RRDC and waiver service providers is imperative. The following must occur to support the participant's relocation:
- The participant must inform the Service Coordinator of their desire/need to relocate. This notification must be at least thirty (30) days prior to the move date in order to ensure a proper transition of services;
- The Service Coordinator will meet with the participant to obtain information regarding the new residence, needed services in the new location, and anticipated date of transfer;
- The Service Coordinator must notify the current RRDC and provide details of the participant's request to relocate;
- The current Service Coordinator must assure a Release of Information is in place to assist in the transfer of information process;
- The current RRDC must contact the new RRDC in the new region to initiate the transfer of services and provide a copy of the Initial Service Plan and the current service plan, PPO and LOC assessment;
- The new RRDC must contact the participant to discuss service options and providers in the new area and make a preliminary determination as to whether the participant can be appropriately served in the new region;
- Upon preliminary approval by the new RRDC, the participant will select a new service coordination provider from the list of approved and available conflict-free service coordination agencies provided by the new RRDS;
- The participant maintains their right to interview service coordination providers or designate someone on their behalf to do so, whenever possible.
NOTE: It is always recommended that a face-to-face visit between the Service Coordinator and participant be made whenever possible. If this cannot be accomplished, it is imperative that the new Service Coordinator work closely with the participant and current Service Coordinator;- The participant works with the new RRDC to complete the Service Coordination Agency Selection form indicating their selection;
- The new Service Coordinator acquires needed additional documentation (e.g., current Level of Care, original Application Packet, PPO) for the development of the RSP;
- The new Service Coordinator assists the participant through the Provider Selection process;
- The participant maintains their right to interview waiver service providers or designate someone on their behalf to do so whenever possible;
- The new Service Coordinator develops a Revised Service Plan (RSP) with the participant and submits it to the new RRDC for review and approval; and
- Upon approval of the RSP by the new RRDS, the current Service Coordinator must inform the participant of their responsibility to contact the current LDSS and inform them of their transfer to a new county as a continued participant of the NHTD waiver and with the anticipated date of transfer. If requested by the participant, the Service Coordinator can assist in the contact to LDSS; in New York City, a new Medicaid number is required in order for a participant to continue to receive waiver service. The new Service Coordinator must contact the LDSS in the new county to ensure information regarding transfer of the participant's Medicaid eligibility status to the new region has occurred.
NOTE: If there is indication that the participant cannot be appropriately served in the new RRDC region, the receiving RRDC will be notified of that concern by the Service Coordinator. These concerns will be presented to the participant. If the participant still desires to relocate to the new region but cannot be served by the waiver in that region, the new RRDC communicates this to the current RRDC who will issue an NOD - Discontinuation of Waiver Program to the participant and others as indicated on the NOD. The current Service Coordinator discusses the NOD, Case Conference and Fair Hearing rights with the Participant. The current Service Coordinator works with the participant to develop a discharge plan.Each RRDC maintains a database for tracking service plan periods, service plan type (ISP/RSP), service plan due dates, and type of Notice of Decision (NOD) issued. The RRDC will work to meet the quality assurance performance measures established in the approved 1915(c) waiver application.
RRDC staff report the status of service plan reviews on a monthly basis to NYSDOH.
RRDCs generate reports from the database of upcoming and overdue service plan reviews. On an annual basis the RRDC completes a record audit of a statistically reliable sample of files to assess compliance. Regional data is provided to NYSDOH waiver staff who complete a statewide aggregate summary.
The Office of Primary Care and Health Systems Management (OPCHSM) completes surveys of approved providers as established in survey protocols. The Waiver unit works with the NYSDOH Surveillance staff throughout the year to address provider performance and concerns.
The Office of the Medicaid Inspector General (OMIG) has established protocols for the review of NHTD provider payment records as per NYSDOH Medicaid Update January 2005, Vol 20, No1, OMM. OMIG reports are posted on its website.
RRDC staff develop internal procedures to ensure participant choice and adequate services are provided in a timely manner. The providers are also required to respond to the participant's request for services in a timely manner. RRDC staff, in addition to NYSDOH Surveillance staff, complete site visits to providers and offer technical assistance.
Annual participant satisfaction surveys are completed to garner participant feedback regarding the quality and overall satisfaction of waiver services.
When the Service Coordinator is facing unforeseen circumstances that may prevent the submission of the LOC assessment and service plan within the required timeframe, the Service Coordinator immediately contacts the RRDS for technical assistance. A plan is established to prevent disruption of services to the participant, potential penalties to the service coordination agency, and billing concerns for all waiver service providers.
The RRDC contacts the service coordination agency supervisor any time a LOC assessment and service plan packet are not submitted to the RRDS within the required timeframe.
Repeated submission of late, incomplete and/or unacceptable service plan packets and/or LOC assessments results in the initiation of corrective action. Failure to comply may lead to NYSDOH waiver staff choosing to restrict a waiver service provider's opportunity level. When a provider's opportunity level is restricted, the waiver service provider will be ineligible to receive new referrals of waiver participants. This restriction pertains to the agency as a whole and all services the provider is approved to provide. For more information on the opportunity level restriction, see "NYSDOH Restriction of a Waiver Service Provider" in Section III of the program manual.
Section VI: Waiver Services
Introduction
NHTD Waiver Services are designed to address the unique needs of waiver participants. All other services and supports, including informal supports, non-Medicaid services, federally funded services, and Medicaid State Plan services must be explored before utilizing waiver services. The provision of waiver services must be cost-effective and necessary to avoid institutionalization.
This section describes each of the waiver services, provider qualifications, and reimbursement for the service.
The NHTD waiver program delineates its eighteen (18) waiver services as "direct" or "non-direct" waiver services.
Direct waiver services:
- Community Integration Counseling (CIC)
- Home and Community Support Services (HCSS)
- Home Visits by Medical Personnel
- Independent Living Skills and Training Services (ILST)
- Nutritional Counseling / Educational Services
- Peer Mentoring
- Positive Behavioral Interventions and Support Services (PBIS)
- Respiratory Therapy
- Respite
- Service Coordination
- Structured Day Program Services (SDP)
- Transportation Services
- Wellness Counseling
Non-direct waiver services:
- Assistive Technology (AT)
- Community Transitional Services (CTS)
- Congregate and Home Delivered Meals
- Environmental Modifications (E-Mods)
- Moving Assistance
NYSDOH will not make payment to a legally responsible individual, relatives, or legal guardians for furnishing waiver services. A legally responsible individual may include a designated representative. Individuals who fall under this category include, but are not limited to, a spouse, parent or individual(s) designated in the clinical record.
Service Coordination
Definition
Service Coordination is an individually designed service which provides primary assistance to the waiver applicant/participant in gaining access to needed waiver and Medicaid State Plan services, as well as other local, state, and federally funded educational, vocational, social, and medical services. These interventions are expected to result in assuring the waiver participant's health and welfare and increasing independence, integration, and productivity. The Service Coordinator assists the applicant in becoming a waiver participant and coordinates and monitors the provision of all services in the service plan once the individual is determined eligible. For individuals transferring from nursing facilities, the Service Coordinator assists the applicant in obtaining and coordinating services that are necessary to return to the community. For those individuals residing in the community, the Service Coordinator facilitates the necessary supports to maintain the individual's health and well-being sufficient to avoid unwanted nursing home placement.
There are four types of Service Coordination available to the waiver participant.
Roles and Responsibilities
The applicant/participant is the primary decision-maker in the development of goals, and selection of supports and individual service providers.
The Service Coordinator is responsible for:
- Facilitating the Initial Service Plan (ISP) and waiver program eligibility;
- Coordinating multiple services among multiple providers;
- Securing initial and annual level of care assessments;
- Assuring that Team Meetings are scheduled and held as designated in the service plan;
- Facilitating the acquisition, oversight, and delivery of service;
- Ensuring annual service plans (Revised Service Plans/RSPs) are completed in a timely manner;
- Facilitating the waiver applicant/participant's Plan of Protective Oversight (PPO) is completed and supports the service plan;
- Conducting monthly face-to-face visits and in-home visits with the participant no less than once a quarter;
- Maintaining records for at least six (6) years after termination of waiver services;
- Responding to participant crises and emergencies; and
- Addressing problems in service provision.
Each year the Service Coordinator will develop and submit the Revised Service Plan (RSP).
The Service Coordinator is responsible for the development of the service plan. The service plan contains an assessment of the individual's strengths, limitations, and goals. It identifies what services are necessary to maintain the individual in the community. The plan must include current summaries of all services provided, including relevant medical information and assessments. Contained within the service plan, the Service Coordinator must provide a detailed explanation of the applicant's/participant's choices and needs, including information regarding relationships, desired living situation, recreation or community activities, physical and mental strengths or limitations, goals for vocational training, and employment or community service. A description of why the waiver services are needed to prevent placement in a nursing home must also be included. The service plan identifies services in twelve (12) month intervals. The Service Coordinator is responsible for ensuring that the participant and all service providers receive a copy of the approved service plan and are aware of the content of the overall plan and goals. Services in a service plan cannot be initiated until prior approval is given by the RRDC. Service changes or additions proposed in an RSP cannot be initiated without prior approval from the RRDC.
A Service Coordinator must be knowledgeable about all waiver services, Medicaid State Plan services, and non-Medicaid services. Informal supports are often a crucial factor if the participant is to live a satisfying life and remain in the community. The Service Coordinator must be skilled in incorporating all of these resources into the waiver participant's service plan.
The Service Coordinator is responsible for assisting the waiver participant in the development of the individualized service plan and assuring that the participant, and those individuals chosen by the participant, are involved in the process.
The Service Coordinator is responsible for facilitating the Initial Service Plan (ISP) and waiver program eligibility.
The Service Coordinator is responsible for facilitating the acquisition of services, timely submission, and distribution of all Service Plans, and for the ongoing monitoring of services identified and approved in the participant's Service Plan through Service Coordinator oversight and coordination of multiple services among multiple providers.
The Service Coordinator is responsible for coordinating Team Meetings. Team Meetings facilitated by the Service Coordinator must occur, at a minimum, after the approval of the initial service plan, every six (6) months, and when an RSP is developed. Team Meetings are scheduled based on the service needs of the participant. At each Team Meeting, the Service Coordinator must discuss with the participant and other participating individual(s) any proposed changes to the participant's existing service plan.
The Team Meeting six (6) Month Timeline lays out the required team meetings for Service Coordinators. The first Team Meeting of the service plan year must be held within thirty (30) days after service plan approval. The next Team Meeting must be held six (6) months from that first Team Meeting (3 months before the RSP submission is due to the RRDC). Team meetings are also dictated by the needs of the participant. When there is a significant change in the participant's living arrangement, health, and safety status, when an addendum to the service plan is indicated, a Team Meeting must be held.
The Service Coordinator does not conduct initial and annual LOC assessments; however, they are responsible for ensuring that the assessments are completed and for reviewing service plans at such intervals as specified in Appendix D of this application. The goals and objectives within the service plan should be consistent with the strengths and needs reflected in the LOC assessments. The UAS-NY is the approved tool for assessing level of care.
Participation in the NHTD waiver is restricted to individuals who require a nursing facility level of care (LOC) as determined by completion of the UAS-NY for those who reside in the community. The purpose of this tool is to objectively evaluate an individual's functional status, strengths, care needs, and preferences using the needs assessment tools developed by the interRAI organization, which contain a comprehensive set of items, domains, scales, and other outcomes. The outcome of the assessment is used to guide the development of individualized long-term care service plans, which ensure that individuals receive needed care within their chosen setting and in a timeframe appropriate to their needs and wellbeing, as well as to maximize efficiency and minimize duplication.
The HC-PRI instrument is approved for use for individuals who are transitioning out of a nursing home or hospital. The HC-PRI instrument is used to identify medical events, including current medical diagnosis, prognosis, capabilities of the individual to perform Activities of Daily Living (ADL), and behavioral difficulties. The UAS-NY assessment will be conducted with these individuals within 90 days of their enrollment into the waiver.
Following the approval of the service plan, the Service Coordinator will assist the waiver participant in implementing the plan, as well as reviewing its effectiveness. The Service Coordinator is also responsible for addressing problems in service provision, should they arise. Throughout their involvement with the waiver participant, the Service Coordinator supports and encourages the waiver participant to increase their ability to problem-solve, be in control of life situations, and be independent. The Service Coordinator also assists the applicant/participant to complete their Plan of Protective Oversight (PPO). The PPO establishes the guidelines necessary to support the health and welfare of the participant in the home.
The Service Coordinator will conduct at least one face-to-face visit every month. At least quarterly, one of these face-to-face visits must occur in the participant's home, in order to ensure a safe and appropriate home environment. The Service Coordinator is also responsible for responding to participant crises and emergencies and associated incident reporting.
A participant's safety must always be the primary concern of the provider agency, Service Coordinator, and the RRDC. The Service Coordinator ensures appropriate measures are in place for the protection of a person from harm, injury, or abuse, and ensures the delivery of prompt and appropriate treatment or care.
The Service Coordinator is responsible for notifying the waiver participant and/or his/her legal guardian within twenty-four (24) hours of receiving a report that an incident has been reported and is being investigated. The Service Coordinator is also responsible for notifying other program or waiver providers of the incident when the evidence of injury or incident may impact services or the waiver provider.
The Service Coordinator is responsible for the completeness and accuracy of all documents presented to the RRDC on behalf of the applicant/participant.
The Service Coordinator is responsible for maintaining the primary service record for at least six (6) years after termination of waiver services for all participants assigned to their caseload.
A Service Coordinator's caseload may not exceed twenty-five (25) NHTD waiver participants. The Service Coordinator must complete a monthly face-to-face visit with each NHTD waiver participant on their caseload. A face-to-face meeting in the participant's home must occur at least quarterly.
The provision of Service Coordination must meet all federally required conflict-of-interest criteria.
All Service Coordination services must be documented in the service plan and provided by individuals or agencies approved as a provider of wavier services by NYSDOH.
Service Coordination has two basic components:
1. Initial Service Coordination; and
Initial Service Coordination encompasses the activities involved in assisting individuals applying for waiver services including developing the documentation to be submitted in the Application Packet. This component has three types of Service Coordination to meet the needs of various categories of waiver applicants/participants. The service provided generally remains the same, but the rate structure may vary due to the circumstances under which the applicant/participant seeks services:
- Initial Service Coordination, Diversion: Provided to individuals who are seeking enrollment and ultimately admitted to waiver services while residing in the community. Encompasses those activities involved in assisting individuals seeking application for waiver services and developing the documentation included in the Application Packet. Providers may only bill for this service upon the person's enrollment into the waiver. This will occur only once per waiver enrollment.
- Initial Service Coordination, Transition - Short Term Nursing Home Stay: Provided to individuals who are seeking waiver enrollment and ultimately enrolled who have been residing in a nursing home for fewer than six (6) months at the time of application. Assistance needed to transition from a nursing home, an individual, who has been institutionalized for less than six (6) months, is often less complicated than for those who have longer nursing facility stays. Encompasses those activities involved in assisting individuals seeking application for waiver services and developing the documentation included in the Application Packet. Providers may only bill for this service upon the person's enrollment into the waiver. Billing can occur only once per waiver enrollment.
- Initial Service Coordination, Transition - Long-Term Nursing Home Stay: Provided to individuals who are newly enrolled in the waiver who are residing in a nursing home for six (6) months or more at the time of application. Nursing home residents with lengthy stays need additional assistance to negotiate a safe discharge and a community care plan, often requiring many more cross agency interactions and a higher degree of coordination. It encompasses those activities involved in assisting individuals seeking application for waiver services and developing the documentation included in the Application Packet. This type of transition often requires more cross- agency interactions and a higher degree of coordination. Providers may only bill for this service upon the person's enrollment into the waiver. This will occur only once per waiver enrollment.
After the applicant selects a Service Coordinator, it is the Service Coordinator's responsibility to gain a full understanding of the applicant's needs, related life experiences, and goals. The Service Coordinator must interview all individuals who are stakeholders in the applicant's life. This requires obtaining information from community services and medical facilities/practitioners providing services to the individual, including information from a discharging facility, and incorporating it into the applicant's service plan.
In assisting the individual to develop the Initial Service Plan (ISP) (DOH-5726), the Service Coordinator must identify the following: sources of support, informal caregivers (family, friends, neighbors, etc.), non-Medicaid federal and state funded services (such as Adult Career and Continuing Education Services-Vocational Rehabilitation (ACCES- VR), Medicare, other third-party payers and Medicaid-funded services (such as medical, personal care, nursing). The waiver services included in the service plan are designed to complement other available supports and services available to Medicaid recipients. Waiver services can only be substituted for Medicaid State Plan services when there are greater efficiencies, such as the use of Congregate and Home Delivered Meals in lieu of a personal care assistant preparing a meal. A waiver service may not duplicate a state plan Medicaid service. If necessary, a Service Coordinator may have to assist the applicant/participant to locate a residence to live in the community. In order to be waiver eligible, an individual must choose to participate in the waiver, and be able to identify an HCBS compliant community residence where waiver services will be provided. The NHTD waiver supports the individual's right to choose where to live and to have access to integrated and accessible housing that falls within the individual's economic means. Residential settings of four (4) or more unrelated individuals are excluded from the waiver. Individuals residing in a living situation which is certified or licensed by the state (e.g., an Office of Mental Hygiene supported Residential Program for Adults, Assistive Living Arrangement, or an Adult Care Facility) will not be eligible for waiver services.
All levels of Initial Service Coordination are paid once per waiver enrollment.
2. Ongoing Service Coordination
Ongoing Service Coordination begins as soon as the individual is determined eligible for waiver services and issued a Notice of Decision (NOD) of Eligibility. The Service Coordinator is responsible for the timely and effective implementation of the approved service plan. The Service Coordinator is responsible for assuring that there is adequate coordination, effective communication, and maximum cooperation between all sources of support and services for the participant. This type of service coordination is provided to waiver participants on an ongoing, monthly basis. Billing for Initial Service Coordination cannot occur until after the initial service plan is approved, a Notice of Decision of Eligibility (DOH-5740) is issued, and the Local Department of Social Services (LDSS) has entered a Restriction/Exemption (RE) code of 60 in the Medicaid database.
On-going service coordination begins immediately after the Notice of Decision of Eligibility is issued and the R/E code is entered. The Service Coordinator will conduct face-to-face meetings with the waiver participant at least monthly to provide close monitoring of the participant's health and welfare needs. The Service Coordinator must conduct a face-to-face visit with the participant in the month following the issuance of the NOD of Eligibility. This does not include any face-to-face encounters completed while providing Initial Service Coordination.
At least quarterly, the Service Coordinator must conduct a face-to-face meeting in the participant's home in order to ensure receipt of required care. During face-to-face visits with the participant, the Service Coordinator discusses the provision of both waiver and non-waiver (Medicare, State Plan, or private insurance) services to confirm that the participant is receiving services in accordance with the approved service plan. The Service Coordinator assures that the participant is aware that they may contact the
Service Coordinator if issues/problems occur in between appointments. The ultimate responsibility for ensuring that the service plan is appropriately implemented rests with the Service Coordinator.
The NHTD waiver makes every effort to promote the right of waiver applicants and participants to choose participation in the NHTD waiver, identify needed services, and select their service providers. Agencies that provide Service Coordination must adhere to conflict-of-interest (COI) requirements established by the Department. Compliance with these practices promotes the independence of the Service Coordinator (SC) and ensures participant choice. The Service Coordinator is responsible for providing unbiased and comprehensive information to the participant about available services and service providers. A Service Coordinator may not "steer" business and may not recommend or indicate a preference for a service provider.
A Service Coordinator must be knowledgeable about all waiver services, Medicaid State Plan Services, and available non-Medicaid services. Informal supports are often a crucial factor if the participant is to live a satisfying life and remain in the community. The Service Coordinator's ability to make use of these informal supports is essential and offers the Service Coordinator and other providers the greatest opportunity for creativity. The Service Coordinator must be skilled in incorporating all of these resources into the participant's service plan. In addition, the Service Coordinator must be knowledgeable of the processes necessary to obtain needed referrals/orders, assessments, and approvals for non-waiver service(s).
The Service Coordinator is also responsible for:
- Formally reviewing, updating, and submitting all service plans to the Regional Resource Development Specialist (RRDS) for review in a timely manner (refer to Section V - The Service Plan);
- Facilitation of Team Meetings according to required timelines: after the approval of the Initial Service Plan and at least every six (6) months thereafter and/or on an as-needed basis;
- Providing the RRDC, all waiver providers, the participant, and others with written summaries of the Team Meetings within fourteen (14) days of the meeting. Submission of the Team Meeting Summaries with the Service Plan and/or any addendum to the RRDC is at the discretion of the RRDC (refer to page 12 for more information on Team Meetings);
- Maintaining records for at least six (6) years after termination of waiver eligibility or the termination of the authorization of the provider agency;
- Maintaining a tracking system for Level of Care evaluations and assuring that the UAS-NY, or PRI (if in a nursing facility) is completed:
- at least every twelve (12) months, or
- when the participant experiences a significant change;
- Maintaining all supporting documents and records necessary to secure services, such as waiver transportation requests, referral forms, Medicaid/Social Security documentation, etc.;
- Securing a signed Release of Information to disclose the service plan documents and other documents generated in the provision of services to the participant. This information will be shared, as needed, with waiver service providers and others as directed by the participant;
- Maintaining current knowledge of all approved waiver service providers in their region;
- Conducting monthly face-to-face meetings with the participant and at a minimum:
- Reviewing the service plan with the participant to determine if the services are meeting the participant's needs;
- Discussing the provision of services with the participant to determine the participant's level of satisfaction with the services they are receiving;
- Reviewing the Service Coordination Detailed Plan with the participant to discuss the participant's progress towards meeting his or her goals; and
- Reviewing the service plan with their Service Coordination Supervisor;
- Conducting in-home visits with the waiver participant at least quarterly.
On an annual basis, the Service Coordinator must review the Participant Rights and Responsibilities form (DOH-5732) with the participant and describe the participant's right to choose and change waiver service providers, as requested. The Service Coordinator must secure the participant's signature on the form and ensures the participant maintains a copy of the signed form and maintains a copy in the Service Coordination record;- Ensuring, on an annual basis, that the participant is provided with information regarding abuse/neglect prevention and how to report any incidents of abuse/neglect if that should occur;
- Ensuring, on an annual basis, that:
- The participant has a copy of the NHTD Participant Instructions for the Complaint Process (DOH-5729) in an easily accessible location; and
- The participant understands the complaint process well enough that they are able to make a complaint if necessary;
- Documenting all visits, contacts, meetings, etc. involving the participant in the Service Coordinator's record; and
- Working with the participant on a safe discharge/discontinuation plan upon termination of waiver services. In many cases, this will include collaboration with Local Department of Social Services (LDSS) to establish alternative services.
A Serious Reportable Incident (SRI) is any situation in which someone has knowledge that the safety and well-being of the waiver participant is compromised. It is a significant event or situation endangering a person's well-being, and because of the severity or sensitivity of the situation, must be reported to the Regional Resource Development Center (RRDC). The Service Coordinator is responsible for advising the RRDC of all SRIs. Recordable incidents such as hospital admissions and emergency room visits that do not result in admission will be discussed with the RRDC to determine if it qualifies as an SRI. Additionally, Recordable incidents are reported to the RRDC when a provider's SIRC identifies a trend of Recordables that may pose a health/safety risk. More information on SRIs and the SRI reporting process can be found in Section X - Incident Reporting Policy & Complaint Procedure.
The Service Coordinator must always provide unbiased assistance and act as a neutral advocate to the participant in the selection of providers and due process actions.
The Service Coordinator has the dual role of developing and monitoring the Service Plan. The agency/provider which employs the Service Coordinator may not provide any direct waiver service other than Service Coordination to any participant assigned to their Service Coordination caseload. The Service Coordinator is prohibited from providing any other direct waiver services to waiver participants assigned to their caseload, even if they are providing that service under the auspices of another provider. The Service Coordination provider may offer non-direct waiver services to applicants/participants on the Service Coordinator's caseload. These services include: Assistive Technology (AT), Community Transitional Services (CTS), Congregate and Home Delivered Meals, Environmental Modifications (E-mods), and Transportation Services and Moving Assistance. For more details on Conflict-of-Interest provisions, please see Section XI (- Quality Assurance) of this manual.
Caseload Limit:
Service Coordinators for NHTD waiver participants may not exceed a caseload of twenty-five (25) waiver participants.
Provider Qualifications
Independent providers and not-for-profit or for-profit health and human services agencies may provide Service Coordination. The agency must be approved by DOH as a NHTD waiver provider.
Service Coordinator staff qualifications are as follows:
- Persons self-employed or employed as Service Coordinators must be a/an:
An individual meeting any of the qualifications above must also have, at a minimum, one (1) year of experience providing case management/service coordination and information, linkages, and referrals regarding community-based services for individuals with disabilities and/or seniors.
- Licensed Master Social Worker (Licensed by the NYS Education Department);
- Licensed Clinical Social Worker (Licensed by the NYS Education Department);
- Individual with a Doctorate or Master of Social Work;
- Individual with a Doctorate or Master of Psychology;
- Individual with a Master of Gerontology;
- Physical Therapist (Licensed by the NYS Education Department);
- Registered Professional Nurse (Licensed by the NYS Education Department);
- Certified Teacher of Students with Disabilities (Certified by the NYS Education Department);
- Certified Rehabilitation Counselor (Certified by the Commission of Rehabilitation Counselor Certification);
- Licensed Speech Pathologist (Licensed by the NYS Education Department); OR
- Occupational Therapist (Licensed by the NYS Education Department).
- Persons self-employed or employed as Service Coordinators who have a Bachelor's degree must have three (3) years of experience providing case management/service coordination, information, linkages, and referrals regarding community-based services for individuals with disabilities and/or seniors.
- Persons self-employed or employed as Service Coordinators who have an Associate's degree must have five (5) years' experience providing case management/service coordination, information, linkages and referrals regarding community-based services for individuals with disabilities and/or seniors.
All agencies that employ two (2) or more Service Coordinators must provide supervision by an individual who fully meets the qualifications as a Service Coordinator. Service Coordination supervisors are responsible for providing ongoing supervision and training to staff.
For purposes of supervision, the supervisor is required to:
- Meet any potential participants face-to-face prior to the completion of the ISP developed by a Service Coordinator under their supervision, unless doing so would delay completion of the ISP;
- Meet any waiver participants face-to-face prior to the completion of the RSP developed by a Service Coordinator under their supervision;
- Have supervisory meetings with staff on at least a monthly basis and maintain notes on these meetings;
- Document progress of staff and conduct regular performance evaluations; and
- Review and sign-off on all service plans.
A Service Coordination supervisor may maintain an active caseload of waiver participants. However, this caseload should be reduced to accommodate the supervisory duties of the administrator.
The Service Coordination provider must have a communication system available with twenty-four (24) hours/seven (7) days per week coverage to assure any issues regarding a participant's services can be addressed.
Any currently employed waiver provider staff who met the waiver application qualifications which were in place on the date of their hire are approved to continue to provide services. Approved employees may receive a certificate of qualification to provide services. The issued certificate will allow that staff member to continue providing the same waiver service(s) at both their current location of employment and/or any change they have in future employment locations/agencies. This certificate has no expiration date and only applies to the waiver service they were qualified for upon hire. Certificates may be terminated at the discretion of NYSDOH.
Team Meetings
The Service Coordinator must be a strong and effective team leader. After the participant has selected all service providers, the Service Coordinator organizes the team to provide individualized services for the participant. The Service Coordinator needs to coordinate communication among all team members, including the participant. This becomes especially important when cognitive deficits affect the participant's memory. Maintaining good communication contributes towards effective coordination of services to support the participant in the community.
Team Meetings occur when:
- The annual review of the service plan is due;
- The participant requests a change in services or service providers;
- There are significant changes in the participant's physical, cognitive, or behavioral status;
- A new provider is approved, or the participant is interested in either changing providers or adding newly available services; and
- The expected outcomes of the services are either realized or need to be altered.
Team Meetings are scheduled based on the service needs of the participant but must be held at a minimum of every six (6) months from the date of the last Team Meeting. Service Coordinators must follow the Team Meeting six (6) Month Timeline when scheduling the required Team Meetings. This timeline provides that the first Team Meeting must be held within thirty (30) days after the approval of the service plan. The second Team Meeting should be held six (6) months after the first Team Meeting. An
ISR must be completed for the Team Meeting held prior to the submission of the RSP and submitted prior to, or at the Team Meeting. The Service Coordinator is required to complete an ISR following this timeline as well. Only one ISR is required annually unless there is a significant change in the participant and/or their related services. Timely submission of ISRs is imperative to maintain continuity of services to the participant.
All medication regimes are reviewed on an annual basis in conjunction with the service plan, upon discharges from hospitals, and rehabilitative services or when the needs/conditions of the participant change significantly.
A representative from each waiver direct-service provider must participate in Team Meetings as well as any individual's the applicant/participant seeks to invite. Failure to participate in the Team Meeting may jeopardize the continued approval of the waiver service provider. Providers of essential non-waiver services and anyone identified in the Plan for Protective Oversight (PPO) should also be invited to Team Meetings. Other potential members of the Team Meeting include advocates, family members, local department of social services staff, etc. If the waiver participant is receiving the same service from different waiver providers, all providers should attend the Team Meeting.
Providers of the following services are not required to participate in Team Meetings, but attendance may be requested by the Service Coordinator on the participant's needs:
- Assistive Technology (AT);
- Community Transition (CTS);
- Congregate and Home Delivered Meals;
- Environmental Modifications (E-mods);
- Home Visits by Medical Personnel;
- Moving Assistance;
- Waiver Transportation; and
- Respite.
These providers may submit progress reports and Individual Service Reports (ISRs) to the Service Coordinator, as needed.
The NHTD Waiver Program supports the philosophy of "For Me, With Me." The waiver applicant/participant should be present for all Team Meetings where their services and/or progress is discussed.
Team Meetings must be documented in the service plan by the Service Coordinator. Participation in Team Meetings must be documented in the notes of each active waiver service provider, including date, time, and location, and projected activities (refer to Section VII - Record Keeping).
The Service Coordinator completes the Team Meeting Summary form which includes:
- Date, time, and location of Team meeting;
- Participant's (or designated representative's) input and comments;
- Review of the participant's progress toward plan goals;
- Issues addressed;
- Recommendations for changes in the service plan (e.g., addition, decrease, increase or discontinuation of service(s));
- Attendance list; and
- Submission and acceptance of all required ISRs or documentation of reasons for any delay or resubmission.
The Service Coordinator distributes a copy of the completed Team Meeting Summary to all active waiver service providers and to the RRDS for review and acceptance. A final copy is then provided to the participant. Any concerns regarding the content of the Team Meeting Summary should be directed to the Service Coordinator. All active waiver service providers must maintain a copy of the Team Meeting Summary in the participant's record.
Team Meetings are not a substitute for the Service Coordinator's required face-to-face visits.
Team Meetings are organized and facilitated by the Service Coordinator as part of their responsibility to oversee services. Reimbursement for this activity is included in the monthly rate for Service Coordination. All other waiver service providers participating in a Team Meeting will be reimbursed for participation in the meeting. Attendance at the meeting is included in the total number of approved annual hours of service. Providers are not reimbursed for time spent writing reports and service plans. This is considered an administrative function.
Service Coordination must be provided by a DOH approved provider and must be included in the service plan to be reimbursed.
There are two (2) types of reimbursement for Service Coordination agencies:
- Initial Service Coordination is reimbursed on a one-time only basis for each participant after the individual is an approved participant in the waiver. Reimbursement is for the work, time, and travel expended in developing the Application Packet, including the Initial Service Plan.
There are three (3) rates for Initial Service Coordination. These are based on whether the person is in the community and how long an individual has been in a nursing home. These are:
- Diversion;
- Transition- Short-Term Nursing Home Stay - six (6) months or less in a nursing home; or
- Transition- Long-Term Nursing Home Stay - greater than six (6) months in a nursing home.
- Ongoing Service Coordination is reimbursed in monthly units. As with all waiver services, Service Coordination must be included in the service plan and can only be billed after the service is delivered. For reimbursement purposes, at a minimum, the Service Coordinator must have at least one face-to-face meeting with the participant in the month for which bills are being submitted.
Rates are based on Upstate and Downstate assignment.
Assistive Technology (AT)
Definition
Assistive technology is a service that directly assists a participant in the selection, acquisition, or use of an assistive technology device.
The Assistive Technology (AT) waiver service supplements the Medicaid (MA) State Plan Service for durable medical equipment and supplies not available under the State Plan. MA State Plan and all other resources must be explored and utilized before considering a request for Assistive Technology. All other sources must be explored utilized and/or exhausted before seeking Assistive Technology services. Durable Medical Equipment covered by the Medicaid State Plan can be found here under "DME."
An Assistive Technological device may include an item, piece of equipment, or product system, whether acquired commercially, modified, or customized, that is used to increase, maintain, or to improve the functional capabilities of the waiver participants.
Assistive Technology includes the costs associated with acquisition of the assistive technology; the evaluation of the assistive technology needs of a participant; implementation and oversight of the technology, including a functional evaluation of the impact of the provision of appropriate assistive technology to the participant in the customary environment of the participant; and/or the services consisting of the selecting, designing, project management, fitting, customizing, adapting, maintaining, repairing, or replacing Assistive Technology devices. In addition, the service may provide for training or technical assistance for the participant, family members, guardians, paid staff, advocates, or others who are utilizing or assisting with the implementation of the technology.
This service is only approved when the requested equipment and supplies are deemed medically necessary, and/or directly contribute to the participant's level of independence, ability to access needed supports and services in the community or are expected to maintain or improve the participant's safety and/or functional limitations as specified in the participant's service plan. The service includes the performance of assessments to identify the type of equipment needed by the participant.
Assistive technology provides for:
- Services consisting of purchasing, leasing, or otherwise providing for the acquisition of assistive technology devices for participants; and
- Services consisting of selecting, designing, fitting, customizing, adapting, applying, maintaining, repairing, or replacing assistive technology devices.
Justification for the Assistive Technology must indicate how the specific service/device will meet the medical and/or other needs of the participant in the most cost-effective manner.
Assistive Technology may be obtained at the time the individual becomes enrolled as a participant, no more than thirty (30) days in advance of community placement from a nursing home (prior to the initial NOD), or at the time of an approved service contained within a service plan. Requests for Assistive Technology must be less than $35,000 per two (2) year period, unless approved by NYSDOH waiver staff.
Requests for service must include all assessments made to identify the necessary Assistive Technology, including an assessment of the participant's unique functional needs, the intended purpose and expected use of the requested Assistive Technology, and documentation that the identified need has been matched to the features of the products requested, to assure the desired outcome. Justification must show how and why the service or product is needed and what rehabilitative or sustaining function it serves. It is anticipated that equipment loan programs or trial periods of non- customized equipment, if available, may be explored before extensive commitments are made to provide/purchase products.
Assistive Technology also includes Personal Emergency Response Systems (PERS) that are not supported through State Plan services: home devices that connect the person to a 24-hour call center with the push of a button. PERS are utilized as an integral part of a Medicaid personal care plan, and to supplement waiver services. If service is billed to Medicare or private insurance, the individual will not be eligible for PERS services through Assistive Technology.
Reimbursement is one hundred percent (100%) of the approved cost payable to the AT provider for coordinating the purchases on behalf of the participant.
Assistive Technology must be documented in the service plan, approved by the RRDC, and provided by agencies approved by NYSDOH waiver staff. The use of the device must be cost-effective.
Any currently employed waiver provider staff who met the waiver application qualifications which were in place on the date of their hire are approved to continue to provide services. Approved employees may receive a certificate of qualification to provide services. The issued certificate will allow that staff member to continue providing the same waiver service(s) at both their current location of employment and/or any change they have in future employment locations/agencies. This certificate has no expiration date and only applies to the waiver service they were qualified for upon hire. Certificates may be terminated at the discretion of NYSDOH. Due to the needs of the target population, provisions contained within this service allow for costs that may exceed corresponding State Plan services.
Devices such as tablets and laptops may be considered assistive technology and may be requested when the device is used to support the participant's ADL/IADL or habilitative needs. Devices considered experimental or used for intervention other than their prescribed/intended use will not be approved. Devices that require the administration and implementation of a skilled professional such as a physical therapist will not be approved for use in the home.
AT Services are not to be used to purchase non-essential devices such as recreational equipment (e.g., bicycles, swimming pool lifts), televisions, DVD players, entertainment systems, video games.
Provider Qualifications
AT Services are purchased through vendors who sell the needed medical, communication, and adaptive equipment or supplies.
Providers of Assistive Technology must be:
- Any not-for-profit or for-profit health and human service agency that has both the personnel and expertise to provide AT and is an approved Medicaid provider;
- An establishment registered as a pharmacy by the State Board of Pharmacy pursuant to Article 137 of the NYS Education Law; or
- Provider of PERS under contract with the Local Department of Social Services (LDSS);
Not-for-profit and for-profit health and human service agencies may provide AT or may subcontract with a qualified person or entity to provide AT.
Providers of AT must ensure that all devices and supplies meet standards established by Underwriters Laboratory and/or comply with Federal Communications Commission (FCC) Regulations, if appropriate.
The provider of this service is responsible for providing or securing training for the waiver participant, informal supports, and paid staff who will be assisting the waiver participant in using the equipment or supplies.
This is a non-direct waiver service.
Approval Process for AT Services
STEP 1
The participant and/or legal guardian may request AT from the Service Coordinator during the development of any service plan or any other time. The service must receive prior approval from the RRDC prior to responding to the request.
The request must be supported by an assessment to describe and justify the need for Assistive Technology and support that it will increase, maintain, or improve the functional capabilities of the participant. This must be conducted by a qualified professional who is knowledgeable about the full range of devices and/or technology to assist individuals with disabilities or seniors.STEP 2
The participant and Service Coordinator explore all available resources outside of the waiver to determine appropriateness of the requested AT and utilize all possible funding sources including: private insurance; community resources; non-Medicaid federal and state funding (e.g., Medicare); and/or other federal/State programs. Documentation by the Service Coordinator must include the resources explored and the outcome of the exploration. All other resources must be shown to have been utilized and/or exhausted before approval will be granted.STEP 3
If NHTD funding is required for the device(s), a dated physician's or related clinician's statement on practice letter head with statement of medical necessity is required and the Service Coordinator initiates the process for submission of the AT request to the RRDC using the Assistive Technology (AT) Description and Cost Projection form (DOH-5752). Information that must be included with the form includes but is not limited to:
- Justification for the AT indicating how the equipment will meet the needs and goals of the participant in an efficient and cost-effective manner.
Note: justification by the maker or provider of the device will not be accepted;- Copies of all assessments made to determine the necessary AT, including an assessment of the participant's unique functional needs and the intended purpose and expected use of the requested AT. The assessment must include a description of the ability of the equipment to meet the individual's needs in a cost-effective manner and completed by an independent assessor;
- When the AT will require modifications to the participant's residence, information must also include the name of the homeowner or landlord and their permission for the modifications/adaptations; and
- Date the AT is needed.
Assistive technology services may be used to support the costs of evaluating the participant and assessing devices. The cost of the assessment costs can be paid for prior to the initiation or completion of project.
STEP 4
The Service Coordinator and applicant select an approved AT provider and sign the Provider Selection form (DOH-5730).STEP 5
The Service Coordinator obtains bids for the device/service.
- For an item of AT costing less than $2,000, only one bid is required.
- For an item of AT costing $2,000 or more, three bids are required.
The Service Coordinator must select an approved provider based on reasonable pricing and obtain a written bid stating all terms and conditions of sale. The lowest bid among substantially equivalent bids that conform to the recommended plan must be selected. The Service Coordinator must review the bids and recommendations with the participant and/or legal guardian, obtain their input, and documents the outcome.
STEP 6
The Service Coordinator completes the AT Description and Cost Projection form and attaches the assessment and all bids obtained. The Service Coordinator reviews the form with the applicant/participant and both the Service Coordinator and applicant/participant sign.STEP 7
The Service Coordinator submits the completed AT Description and Cost Projection form along with the Initial or Revised Service Plan or Addendum, assessment, bids and supporting documentation to the RRDS.STEP 8
The RRDS reviews the AT Description and Cost Projection form, service plan, and attached documentation and may request more information. Approval is contingent upon available funding. The RRDS determines the appropriate bid for selection, notifies the Service Coordinator of the approval, signs the AT Description and Cost Projection form and sends the original AT Description and Cost Projection form back to the Service Coordinator.STEP 9
The Service Coordinator notifies the AT provider and provides them with a copy of the signed AT Description and Cost Projection form.STEP 10
After completion of the service, the AT provider completes and signs the Waiver Services Final Cost Form (DOH-5755) with the participant.STEP 11
The AT provider sends the original AT Description Cost Projection and the Waiver Services Final Cost forms to the Service Coordinator. The Service Coordinator must assure that the approved AT was appropriately provided. The participant will confirm satisfaction with the completed request in writing via their signature on the Waiver Services Final Cost form. The Service Coordinator then signs off and submits the Waiver Services Final Cost form to the RRDS. It is the responsibility of the Service Coordinator to advise the RRDC of any negative outcomes/concerns.If a participant presents concerns regarding the status of the request prior to completion, all action regarding the request will be suspended until the matter is resolved.
STEP 12
The RRDC reviews and completes the Waiver Services Final Cost Form and all supporting documentation and approves or denies the request. A copy of the final decision is provided to the Service Coordinator and/or AT Provider.STEP 13
The AT provider seeks reimbursement after receiving back the RRDC signed copy of the Waiver Services Final Cost form, indicating approval. Medically justified AT exceeding the service cap will also require approval from NYSDOH.NOTE: For AT that is provided and billed on a monthly basis (e.g., PERS units), the AT provider completes and signs the Waiver Services Final Cost and RRDS Approval of Final Cost form (DOH-5755) with the participant at the time of installation, indicating the installation fee and total projected monthly service fees for the length of the service plan. The RRDC reviews and completes this form, enabling the provider to bill on a monthly basis as long as the participant remains in the residence during any part of that month.
Repairs
Repairs to AT which are cost-effective may be allowed. Items that have worn out through normal use (keyboards, switches, etc.) may be replaced using the same procedures that were followed to initially acquire the item. There are situations where replacement or repair will be contingent on establishing a plan that would minimize repeated loss or damage. The Service Coordinator is responsible for working with the team to develop and implement a plan to prevent repeated loss or damage.
Reimbursement
AT must be provided by a DOH approved provider, included in the service plan and approved by the RRDC, to qualify for reimbursement. The service may only be provided to individuals who are NHTD waiver eligible at the time-of-service.
Requests for AT must be less than $35,000 per two (2)-year period. For example: if a participant needs more than one type of AT device during the two (2)-year period, the combined cost for this period may not exceed $35,000. It is expected that the Service Coordinator and the RRDC will exhaust all available resources prior to presenting the request. The service may not duplicate available Medicaid resources. With sufficient medical justification, a request that exceeds service limits may be presented to NYSDOH for consideration.
Reimbursement is one hundred percent (100%) of the approved cost payable to the AT provider for coordinating the purchases on behalf of the participant. This includes the cost for services consisting of purchasing, leasing, or otherwise providing for the acquisition of assistive technology devices for participants payable to the AT provider. These costs must be presented as an itemized bill/statement included in the total cost of the project.
AT is reimbursed based on the lowest of two costs: wholesale plus 50% or the retail cost. Repairs and replacement of parts are reimbursed at the retail cost. AT obtained no more than thirty (30) days prior to the initial NOD of eligibility are reimbursed after date of eligibility.
AT providers are required to submit projected cost estimates and final cost statements to the Service Coordinator. Each specific payment is made based on the tasks performed or the equipment or parts purchased on behalf of the participant. These reports are provided to the RRDC for approval. Claims for these services are reviewed by NYSDOH and the RRDC annually, to ensure the billed amount is the same as the approved amount. If in the process of completing a request there is a difference between the projected and actual costs, the RRDC requires an Addendum to the service plan and amended documents to support the change in the request.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate any Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Community Integration Counseling (CIC) Services
Definition
Community Integration Counseling (CIC) is an individually designed service intended to assist waiver participants who are experiencing significant problems in managing the emotional difficulties inherent in adjusting to a significant disability and/or living in the community. It is a counseling service provided to the waiver participant who is coping with altered abilities and skills, a revision of long-term expectations, or changes in roles in relation to significant others. This service does not duplicate other services available through the New York Medicaid State Plan. Therefore, once the counseling is no longer specific to community integration and becomes general therapeutic counseling, the service will terminate.
The service is designed for individuals experiencing significant problems in managing the emotional difficulties inherent in adjusting to a significant disability and living in the community. The efficacy of a treatment must be reviewed if successful intervention and significant progress has not occurred within two (2) years. At that time, alternative methods require consideration or continued services must be documented as a medical necessity. A transition plan will be implemented prior to the termination of services. Services may be extended in extraordinary cases with sufficient medical justification and upon review and approval of the RRDC.
Upon initiation of the service as a transition service, an initial assessment must be completed and include specific counseling goals. The assessment is limited to five (5) hours of direct service with the participant present. Goals must be reasonable and attainable, and services cannot extend beyond a two (2)-year period.
This service is primarily provided in the provider's office or the waiver participant's home. The participant must be present (face-to-face) at all CIC sessions.
While CIC services are primarily provided in a one-to-one session with either the waiver participant or a person involved in an ongoing relationship with the participant, there are times when it is appropriate to provide this service to the waiver participant or other(s) in a family counseling or group counseling setting. It is available to waiver participants and/or anyone involved in an ongoing significant relationship with the waiver participant when the issue to be discussed relates directly to the waiver participant. The waiver participant must provide consent for any individual to participate.
If CIC is provided to a person involved in an ongoing relationship with the participant in either a one-to-one session, or family counseling or group counseling setting, the participant must be present (face-to-face) in the location that the CIC session is being provided. "Collateral counseling" is not permitted without the participant present.
CIC is intended to be conducted on a short-term basis. The need for CIC could occur at the time of transition from a nursing home or at various times during the participant's involvement in the NHTD waiver. Goals must be reasonable and attainable. Services must be designed and implemented such that they do not extend beyond a two (2) year period. If significant progress has not occurred within two (2) years, the efficacy of a treatment must be reviewed. At that time, alternative methods require consideration. A request for continued CIC services must be accompanied by sufficient medical documentation and approved by the RRDC. A transition plan will be implemented prior to the termination of services.
The sharing of information obtained during a CIC session can only be disclosed in accordance with federal and accepted professional standards regarding client confidentiality.
CIC must not be used to assist the participant to become physically integrated into their environment. This function is the responsibility of other service providers, such as Service Coordinators, ILST and HCSS.
CIC may not exceed two hundred twenty (220) hours annually and four (4) hours weekly. However, in all cases, service limits are soft limits that may be exceeded due to medical necessity. If the participant's needs cannot be met within the established limits, a participant may request to exceed the limit by providing sufficient medical justification to the RRDC. The RRDC will approve or deny the request for additional services.
Provider Qualifications
CIC may be provided by any not-for-profit or for-profit health and human services agency.
Persons employed as a Community Integration Counselor must be a/an:
- Licensed Psychiatrist (licensed by the NYS Education Department);
- Licensed Psychologist (licensed by the NYS Education Department);
- Licensed Master Social Worker (Licensed by the NYS Education Department);
- Licensed Clinical Social Worker (Licensed by the NYS Education Department);
- Individual with a Doctorate degree in Psychology;
- Licensed Mental Health Practitioner (Licensed by the NYS Education Department). (This includes Creative Arts Therapists, Marriage and Family Therapists, Mental Health Counselors, and Psychoanalysts);
- Certified Rehabilitation Counselor (Certified by the Commission on Rehabilitation Counselor Certification);
- Individual with a Master of Social Work;
- Individual with a Master of Psychology;
- Certified Teacher of Students with Disabilities (Certified by the NYS Education Department); or
- Individual with a Master of Gerontology.
All Community Integration Counselors must have, at a minimum, two (2) years of experience providing adjustment related counseling to seniors and/or individuals with physical and/or cognitive disabilities and their families to be considered qualifying experience.
Any currently employed waiver staff who met the waiver application qualifications which were in place on the date of their hire are approved to continue to provide services. Approved employees may receive a certificate of qualification to provide services. The issued certificate will allow that staff member to continue providing the same waiver service(s) at both their current location of employment and/or any change they have in future employment locations/agencies. This certificate has no expiration date and only applies to the waiver service they were qualified for upon hire. Certificates may be terminated at the discretion of NYSDOH
Reimbursement
CIC services must be provided by a DOH approved provider and must be included in the service plan to be reimbursed. The assessment time is limited to five (5) hours of direct service with the participant present.
CIC is reimbursed in one (1) hour or partial units. Unless the rate is "grandfathered-in" for an existing provider, rates are assigned based on the county in which the service is provided.
If CIC is provided in a group setting, the hourly rate is divided evenly among the participants. For instance, if the participant is one (1) of four (4) people in the group, only one quarter (1/4) of an hour is billable to that participant. Providers may accumulate billable units until a whole hour is reached or may bill using partial units.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Community Transitional Services (CTS)
Definition
Community Transitional Services (CTS) are defined as individually designed services intended to assist a waiver participant to transition from a nursing home to living in the community. CTS is a one-time service per waiver enrollment. Should the waiver participant return to nursing home placement and later seek re-entry to waiver services, they may access the service again upon discharge. CTS may only be claimed upon waiver eligibility. This service is only provided when transitioning from a nursing home to the community. These funds are not available for when a participant moves within the community. Moving Assistance is a separate and distinct service available only for community-based moves and not nursing home transitions. The two services cannot be used at the same time in any approved service plan.
CTS provides funding for the reasonable costs of one-time set-up expenses for individuals transitioning from a nursing home to their own home or apartment in the community. Reasonable costs are defined as necessary expenses for an individual to establish their living space.
All CTS expenses must be included in the ISP, approved by the RRDC, and provided by agencies that are approved by NYSDOH. Reimbursement is not provided for items purchased prior to RRDC approval. CTS may not exceed $8,000 per waiver enrollment, which may include a project management fee, payable to the CTS provider. An itemized explanation for the project management fee must be included as an attachment to the Community Transitional Services (CTS) Description and Cost
Projection form. Approved costs will be covered by CTS up to thirty (30) days prior to the individual's discharge into the community.
This service includes: the cost of moving furniture and other belongings; security deposits; broker's fees required to obtain a lease on an apartment or home; purchasing of essential furnishings (e.g., bed, table, chairs, and eating utensils, including delivery and assembly); set-up fees or deposits for utility or service access (e.g., telephone, electricity, heating); and health and safety assurances such as pest removal, allergen control or one time cleaning prior to occupancy.
Security deposits funded through this service, and returned upon vacating the residence or dwelling, must be returned to the CTS provider. Upon return of the funds, the CTS provider must submit a paid claim void to eMedNY.
- The cost of moving essential furniture and other belongings must be provided by a licensed, certified (by NYS Dept. of Transportation) moving company;
- Payments for Security Deposits, including broker's fees, require a lease on an apartment or home unless provided by another housing source. All other payers must be exhausted. Upon return of security deposits to the CTS, a claim adjustment must be credited through eMedNY;
- Purchases of essential furnishings (e.g., bed, table, chairs, essential food preparation items and eating utensils, including delivery and assembly) require prior approval; and
- Health and safety assurances, such as pest removal, allergen control, one-time cleaning service or essential cleaning supplies necessary prior to occupancy, may be included when all other available resources are exhausted, and the service is necessary for occupancy.
This service will not be used to purchase non-essential or recreational items, such as television/VCRs/DVDs or music systems. CTS may not be used to purchase groceries, household appliances, clothing, or transportation of the participant from the nursing home into the community.
Purchases must be reasonable and not considered luxury or "designer" label items.
Security deposits funded through this service, and returned upon vacating the residence or dwelling, must be returned to the CTS provider. Upon return of the funds, the CTS provider must submit a claims adjustment (paid claim void) to eMedNY.
Provider Qualifications
Any for-profit or not-for-profit health and human service agency that has both the personnel and expertise to provide Community Transitional Services and is an approved Medicaid provider may provide CTS or may subcontract with a qualified person or entity to provide CTS.
Any not-for-profit housing agency or local housing authority that has both the personnel and expertise to provide CTS may provide CTS or may subcontract with a qualified person or entity to provide CTS. A not-for-profit housing agency or local housing authority upon application is eligible to provide CTS services.
Any licensed pharmacy, an establishment registered as a pharmacy by the State Board of Pharmacy pursuant to Article 137 of the NYS Education law, may provide CTS.
There are no minimum staff qualifications to provide Community Transitional Services. The qualifications are specific to the licensure and registration of the provider agency.
Approval Process for CTS
STEP 1
The applicant, Service Coordinator, and anyone selected by the applicant, determines what essential items are needed prior to discharge from the nursing home into the community.STEP 2
If appropriate, a comprehensive list of the essential items needed, or anticipated expenses, is developed by the applicant and Service Coordinator.STEP 3
The applicant and Service Coordinator explore all possible resources including informal supports and community resources for these items.STEP 4
After all other resources are explored and utilized, the Service Coordinator compiles a detailed list of any remaining essential items and anticipated expenses (including utility set-up, bids for pest control, and moving) using the Community Transitional Services Description and Cost Projection form.STEP 5
The Service Coordinator and applicant select an approved CTS provider and sign the Provider Selection form (DOH-5730).STEP 6
After completing the Community Transitional Services Description and Cost Projection Form, the applicant and Service Coordinator sign the form.STEP 7
The Service Coordinator sends the Community Transitional Services Description and Cost Projection Form and Provider Selection form to the CTS provider for their approval, signature, and Medicaid provider number.NOTE:
For moving costs and for services for health and safety assurances (e.g., cleaning), if the cost of either one of these services is greater than $1,000, three (3) bids must be obtained and submitted by the CTS provider, along with the CTS Description and Cost Projection form.STEP 8
The CTS provider returns the completed Community Transitional Services Description and Cost Projection form to the applicant's Service Coordinator, including the itemized list of cost-effective essential household furnishings.STEP 9
The Service Coordinator submits the complete Community Transitional Services Description and Cost Projection form with the ISP to the RRDS.STEP 10
The RRDC reviews and approves the costs detailed for CTS, reserving the right to question the necessity and/or deny any CTS items.The Service Coordinator must assure that the approved CTS request was appropriately provided and meets the participant's satisfaction. The applicant/participant will confirm satisfaction with the completed request in writing and if a participant presents concerns regarding the status of the request prior to completion, all action regarding the request will be suspended until the matter is resolved.
STEP 11
The RRDC notifies the Service Coordinator of approval or denial for CTS. A NOD of approval/denial is issued by the RRDC via approval of the ISP. It is the responsibility of the Service Coordinator to advise the RRDC of any negative outcomes/concerns. The Service Coordinator will advise the participant/legal guardian of their due process rights related to the decision.STEP 12
The Service Coordinator notifies the CTS provider that the applicant has been approved/denied for CTS.STEP 13
The CTS provider makes the approved payment directly to the broker, utility company and/or the landlord for a security deposit. The CTS provider purchases the approved essential furnishings with prior approval by the RRDS. All receipts and any remaining balance must be maintained by the CTS provider.STEP 14
The CTS provider completes the Waiver Services Final Cost and RRDS Approval of Final Cost form (DOH-5755), which certifies that the CTS was provided in accordance with the ISP. The CTS provider must maintain original receipts. A copy of the original receipts and an itemized list of items purchased is attached to the Waiver Services Final Cost and RRDS Approval of Final Cost form and submitted to the Service Coordinator.STEP 15
The Service Coordinator ensures that all items have been delivered to the waiver participant's residence and the provision of CTS has been appropriately furnished; the Service Coordinator attests to the completed CTS provision and signs the Waiver Services Final Cost and RRDS Approval of Final Cost form. The participant also confirms the request was completed as described and signs the Waiver Services Final Cost and RRDS Approval of Final Cost form indicating such. After the Waiver Services Final Cost and RRDS Approval of Final Cost form have been signed by the participant and Service Coordinator, the Service Coordinator and submits the form to the RRDS for approval.STEP 16
The RRDS reviews the Waiver Services Final Cost form, approves, and signs the RRDS Approval of Final Cost form, then provides a copy to the CTS provider and Service Coordinator.STEP 17
The CTS provider seeks reimbursement after receiving a copy of the NOD Authorization and RRDS signed and approved Waiver Services Final Cost and RRDS Approval of Final Cost forms from the Service Coordinator.Reimbursement
CTS must be provided by a DOH-approved provider and included in the Initial Service Plan to be reimbursed. Prior to making the purchases, if the cost is greater than one hundred ten percent (110%) of the estimate, another Community Transitional Services Description and Cost Projection form must be submitted to justify the request. Reimbursement will not be provided if the actual cost of the service exceeds ten (10) percent of the projected cost without prior approval.
This service is reimbursed on a cost basis. Total one-time reimbursement for CTS must not exceed $8,000 per waiver enrollment. This includes the cost for services consisting of purchasing, leasing, or otherwise providing for the acquisition of the items payable to the CTS provider. These costs must be presented as an itemized bill/statement included in the total cost of the project.
Approved costs are covered by CTS up to thirty (30) days prior to the individual's discharge from the nursing home into the community and issuance of a NOD of eligibility. Reimbursement is one hundred percent (100%) of the approved cost.
CTS providers are required to submit projected cost estimates and final cost reports to the Service Coordinator. Each specific payment is made based on the tasks performed or the equipment or parts purchased on behalf of the participant. These statements are provided to the RRDC for approval. Paid claims for these services are reviewed by NYSDOH and the RRDC annually, to ensure the billed amount is the same as the approved amount. If there is a difference between the projected and actual costs, the RRDC requires an Addendum to the Service Plan to justify the increase.
This is a non-direct waiver service.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Congregate and Home Delivered Meals
Definition
Congregate and Home Delivered Meals is an individually designed service which provides meals to waiver participants who cannot prepare or obtain nutritionally adequate meals for themselves, or when the provision of such meals will decrease the need for more costly supports to provide in-home meal preparation. While these meals will assist the waiver participant to maintain a nutritious diet, they do not constitute a full nutritional regimen. Therefore, the maximum number of meals the participant may receive per day is two (2). This service is not to be used to replace the regular form of "board" associated with routine living in an Adult Care Facility. Individuals eligible for non-waiver nutritional services should access those services first.
This service does not duplicate other services available through the New York Medicaid State Plan.
Provider Qualifications
Providers of Congregate and Home Delivered Meals are either contracted through Area Agencies on Aging (AAA) and/or those entities contracted through the AAA for Congregate and/or Home Delivered Meals.
Reimbursement
Congregate and Home Delivered Meals must be documented in the approved service plan and provided by agencies approved by DOH.
This service is reimbursed on a per meal basis as per the approved contract rate with the LDSS.
Attendance at Team Meetings for Congregate and Home Delivered Meal providers is not required. This is a non-direct waiver service.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Environmental Modifications Services (E-mods)
1.E-mods for Homes
Definition
Environmental Modifications (E-mods) are interior and exterior physical adaptations to the home that are necessary to ensure the health, welfare, and safety of the waiver participant. These modifications enable the waiver participant to function with greater independence in the community and help avoid institutionalization. E-mods include the performance of necessary assessments and project management to determine the type of modifications needed and the assessment that the adaptation has been completed according to the required specifications.
E-mod services must be made only to the primary full-time residence in which the waiver participant lives. However, if a waiver participant is moving to a new location that requires modifications, the modifications may be completed prior to the waiver participant's move. If an eligible individual is residing in an institution at the time of application to the waiver, the modifications may be completed no more than thirty (30) days prior to the initial NOD Discharge from the facility. When an E-mod is completed prior to a participant's move from an institution to the community, the E-mod will be reimbursed after the NOD is issued. Accordingly, when the waiver application is reviewed, a tentative discharge date from the institution must be designated.
An E-mod may alter the basic interior configuration of the waiver participant's home only if this alteration is necessary to successfully complete the modification. If the residence is not owned by the participant, the Service Coordinator must obtain documentation showing that the property owner supports and approves of the modification.
An E-mod may not add to the total square footage of the home.
An E-mod may not be furnished to adapt living arrangements that are owned or leased by providers of waiver services.
All E-mod services must be specified in the waiver participant's service plan and must be completed by agencies approved by DOH.
E-mod services must meet all State and local building codes and will be subject to independent review both prior to initiation and after completion.
Prior to submitting a request for a home adaptation, the property must have documentation of current assessed value and the homeowner must have sufficient insurance coverage.
Allowable E-mod services do not include improvements to the home (carpeting, roof repair, central air conditioning) that are not medically necessary or are not necessary to maintain the waiver participant's independence in the home or community.
The total cost of all E-mods, including vehicle modifications, must be less than $45,000 within a thirty-six (36) month period, unless approved by DOH. Any request for a modification with a total cost of $15,000 or more requires prior approval from NYSDOH.
Modifications with an estimated cost of $5,000 or more require a Home Evaluation.
The NHTD waiver program and the E-mod waiver service specifically will not reimburse for the cost of returning a modification to its original state, either in the case of a home modification or a vehicle modification.
Allowable E-mods
E-mods in the home include the purchase and/or installation of:
- Access ramps;
- Widening doorways and hallways;
- Handrails and grab bars;
- Automatic or manual door openers and doorbells;
- Backup generator for medical equipment; and/or
- Stair glides.
Allowable bathroom and kitchen modifications include:
- Roll-in showers;
- Sinks and tubs;
- Water faucet controls;
- Plumbing adaptations, e.g., cutouts, toilet/sink adaptations;
- Turnaround space changes/adaptations;
- Kitchen work surface adaptations;
- Cabinet and shelving adaptations; and/or
- Lighting and security adaptations.
Other home adaptations include:
- Electrical wiring and plumbing systems integral to the approved home adaptation; and
- Other adaptations necessary to facilitate accessible living arrangements for the participant's independence and daily functioning.
E-mods include the performance of necessary assessments and project management to determine the type of modifications needed and the assessment that the adaptation has been completed according to the required specifications. An itemized explanation for the project management fee must be included as an attachment to the signed Environmental Modification (E-Mod) Description and Initial Cost Projection form (DOH-5755).
E-mods are NOT to be used to:
- Build any portion of new housing construction;
- Build room extensions or additional rooms or spaces beyond the existing structure of a dwelling;
- Modify or build rooms for the use of physical therapy equipment;
- Purchase swimming pools, hot tubs, whirlpools, steam baths, or saunas for either indoor or outdoor use;
- Pave driveways or walkways;
- Purchase central air conditioning;
- Purchase and install elevators;
- Purchase service or maintenance contracts; and/or
- Purchase items or make modifications that primarily benefit members of the household other than the waiver participant.
Home Evaluation
For modifications with an estimated cost for $5,000 or more, a Home Evaluation is required. The evaluation is completed in three (3) phases:
Initial evaluation - The home evaluator/Home Evaluation Specialist visits the home to identify the current needs of the participant and any potential safety issues. The evaluator also assesses the structure of the home in order to identify any potential issues that may hinder the completion of the E-mod project. The home evaluator/Home Evaluation Specialist determines the specifications of the adaptation/modification.
Mid-project evaluation - The home evaluator/Home Evaluation Specialist visits the home to monitor the implementation of the project to ensure adequate progress is being made and to assess for any additional safety or functional issues.
Final evaluation - The final home visit is conducted at the completion of the project. The home evaluator/Home Evaluation Specialist inspects the project to ensure all E- mods are completed and accessible to the participant. This visit is required before payment is released to the service provider.
Provider Qualifications
Any not-for-profit or for-profit health and human services agency, not-for-profit housing agency or local housing authority that has both the personnel and expertise to complete an E-mod and is an approved Medicaid provider may provide Environmental Modifications or may subcontract with a qualified person or entity to provide Environmental Modifications.
Persons employed/contracted as a Home Evaluation Specialist must be a:
- Certified Aging in Place Specialist and have experience in recommending and implementing assistive technology or durable medical equipment in the home health care domain;
- Certified Environmental Access Consultant in the field of environmental modification with experience in recommending and implementing assistive technology or durable medical equipment in the home health care domain;
- Licensed Occupational Therapist (licensed by the NYS Education Department);
- Universal Design/Barrier Free/Accessibility Specialist;
- An independent contractor with expertise in universal design; or
- Licensed Physical Therapist (licensed by NYS Education Department).
A contractor cannot be paid to complete any E-mod project in a residence that they own. In order to receive payment for waiver services the contractor must be independent of the waiver participant and cannot be a relative.
In instances where the participant's Service Coordination Agency is also the chosen E- mod provider, the participant's Service Coordinator will only act in the capacity of Service Coordination and will not participate in the oversight and supervision of the project, including obtaining the bids. In this situation, the RRDC is responsible for ensuring that the E-mod provider follows this protocol.
The E-mod provider is responsible for the planning, supervision of the construction, and satisfactory completion of the project prior to billing for the modification. This includes the pre-, mid-, and post-evaluations of the modification, obtaining at least three (3) bids from qualified contractors for E-mods greater than $2,000, obtaining necessary permits, and, with the participation of the participant and/or their legal guardian, making recommendations for bid selection. The E-mod provider must ensure that the contractor is appropriately qualified and/or licensed in accordance with applicable State and local requirements. All materials and products used must meet all State or local construction requirements.
Providers must adhere to safety issues addressed in Article 18 of the New York State Uniform Fire Prevention and Building Code Act, as well as all local building codes.
Any currently employed waiver staff who met the waiver application qualifications which were in place on the date of their hire are approved to continue to provide services. Approved employees may receive a certificate of qualification to provide services. The issued certificate will allow that staff member to continue providing the same waiver service(s) at both their current location of employment and/or any change they have in future employment locations/agencies. This certificate has no expiration date and only applies to the waiver service they were qualified for upon hire. Certificates may be terminated at the discretion of NYSDOH.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate any Medicaid claims. These providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Approval Process for E-mods for a home
STEP 1
During the development of the service plan (SP), the applicant/participant and/or their legal guardian may request an E-mod. The request for service requires a dated physician's statement on MD letter head with statement of medical necessity.STEP 2
In order to determine the appropriateness of the requested E-mod, the applicant/participant, the Service Coordinator, and/or legal guardian must first assess all available resources outside of the waiver (i.e., informal supports, community resources and State/Federal agencies) and all other available funding sources to pay for the E-mod. Documentation by the Service Coordinator must include details of all resources assessed and the outcome of the assessment. All other resources must be shown in writing to have been exhausted before approval will be granted. If applicable, property owner permission for the E-mod must be obtained.STEP 3
The applicant/participant selects a waiver approved E-mod provider to be responsible for planning, oversight, and supervision of the project.STEP 4
The E-mod provider must arrange for the mandatory comprehensive evaluation of the property to be completed prior to commencement by a rehabilitative evaluation agency/Home Evaluation Specialist (for example, a United Cerebral Palsy or an Independent Living Center), or it may be performed by an independent building contractor who is well versed in Americans with Disabilities Act (ADA) compliance standards. The evaluation must contain a detailed description of the project, including:
- the scope of work to be done and specifications including the possible costs of necessary assessments and project management;
- the need for the requested E-mod;
- the utility of the proposed E-mod adaptation and any safety concerns;
- its expected benefit to the participant; and
- the most cost-effective approach to fulfilling the need.
It is important to remember that not all residences are suitable for E-mods (examples: insufficient structure on which to build a ramp; or not sound enough to support installation). Therefore, the evaluation must confirm that the residence can accommodate the modification. Modifications cannot exceed existing property lines or impinge public access.
The E-mod provider must also arrange for a mid-way and post-construction or installation evaluation of the E-mod with the evaluator. The post modification evaluation must occur within ten (10) calendar days of the completion, subject to project approval. The waiver applicant/participant must agree/accept the completed work throughout the stages of the project. Any disagreement must be brought to the immediate attention of the RRDC.
The E-mod provider must ensure a copy of the evaluation is provided to the Service Coordinator, participant, and RRDS prior to proceeding with the bidding process. The RRDS may request guidance from DOH in the review of the evaluation.
The Service Coordinator must assure that the approved E-mod request was appropriately provided and meets the participant's satisfaction. The participant will confirm satisfaction with the completed request in writing. A NOD of approval/denial is issued by the RRDC. It is the responsibility of the Service Coordinator to advise the RRDC of any negative outcomes/concerns.
After the Service Coordinator and E-mod provider receive written RRDC approval of the evaluation, the Service Coordinator is responsible to review the Agreement of Understanding with the participant and/or legal guardian and obtain required signatures indicating they understand the recommended plan for the adaptation, the bidding process, and their responsibility regarding maintenance and repair of the adaptations. The Service Coordinator provides a copy of the signed agreement to the E-mod provider.
STEP 5
In conjunction with the applicant/participant/Service Coordinator, the E-mod provider is responsible for obtaining the necessary bids from qualified contractors. Each bid must adhere to the following requirements:
- Use the specifications delineated in the evaluation;
- Specify the cost of each component in the scope of work, certifying that at a minimum, contractor grade materials are used. No upgrades to materials will be permitted by Medicaid or reimbursed under this waiver. This information must delineate cost of materials, permits, and labor;
- Provide at least three (3) references from people or entities for whom the contractor has done similar work, including verifiable photos and/or addresses, unless the E-mod provider will vouch for the quality of the contractor's work on previous E-mods;
- Have no outstanding judgments against them and/or their business and no unresolved complaints against them and/or their business on file with the New York State Department of Law or on file with the Better Business Bureau. This must be confirmed and documented by the E-mod provider;
- Submit proof of appropriate and adequate insurance coverage for the duration of the project;
- Certify that all work will comply with applicable building and zoning codes;
- Certify that they will obtain any permit required to make the modification;
- State clearly any work to be completed and/or equipment to be provided by the homeowner and/or landlord prior to commencement of the modification;
- Submit fully itemized bids with all associated material and labor costs; and
- Submit drawing plans and photographs provided of the area to be modified, as needed.
NOTE:
- For E-mods costing less than $2,000, only one (1) bid is necessary.
- For E-mods costing $2,000 or more, three (3) bids are necessary.
All bids must include the information delineated in the NHTD Sample Bid Submission form for E-mods.
The E-mod provider must show that reasonable efforts have been made to acquire the required three (3) bids. If the E-mod provider has been unable to obtain the required three (3) bids, all efforts made to fulfill this requirement and reasons why it was not met must be documented. The E-mod provider must contact the Service Coordinator, who in turn will inform the RRDS. The RRDS will consult with NYSDOH and will notify the Service Coordinator if the E-mod provider may proceed without the required three (3) bids. Both the RRDS and Service Coordinator must maintain complete documentation, including consultation with NYSDOH, in the participant's record.
STEP 6
The E-mod provider will review the bids with the participant and/or their legal guardian and document recommendations for bid selection.The E-mod provider submits the bids with its recommendations to the Service Coordinator for review and signature. The Service Coordinator submits the E-mod packet to the RRDS for approval.
Information that must be submitted in the packet includes, but is not limited to:
- Justification for the E-mod (dated physician's statement of medical necessity, written on appropriate letterhead);
- Documentation by the Service Coordinator of all other funding resources outside of the waiver assessed and the outcome of each assessment;
- All evaluations completed to determine the suitability and specifications of the E-mod;
- Information regarding the residence for which the E-mod is proposed, i.e., where the participant lives or intends to live, including the name of the homeowner or landlord. The owner's approval for the renovations, including any lease or rental contract, must be included. Funds will not be made available for the cost of removing an E-mod or restoring a site to its original configuration or condition. An E-mod will not proceed if this is a requirement of the property owner;
- Information verifying that the E-mod provider has fulfilled its responsibility as outlined in STEPS 4 and 5 above;
- If other renovations or repairs are being completed to the dwelling during the E-mod, the scope of work must only address the services/terms of the E-mod projects;
- Bids for the requested E-mod;
- Environmental Modification (E-Mod) Description and Initial Cost Projection form (DOH-5755);
- Agreement of Understanding;
- Completed service plan; and
- Photographs of the dwelling prior to the proposed modification.
STEP 7
The RRDC reviews the proposal and may request more information. Approval will be determined on a case-by-case basis, considering factors such as the appropriateness of the E-mod considering the participant's medical condition, their present or intended community living situation, quality of life, cost of the modification requested, available funding, and other limitations to the program.The lowest bid among substantially equivalent bids that conform to the bidding specifications must be selected unless there is an overriding issue with the lowest bid or bidder. If there are any issues, e.g., the equivalency of the bids, the reliability of the lowest bidder versus the reliability of the next lowest bidder, or whether one or more bids meet the bidding specifications, the RRDS must contact DOH before proceeding further. Exception to the lowest bid criteria may occur if there is sufficient justification for the preferred bid and prior approval is received from the RRDC.
STEP 8
Upon written approval or denial of the E-mod proposal from the RRDC, the RRDC will issue the Notice of Decision (NOD) and provide a copy of the NOD and the completed and signed Environmental Modification (E-Mod) Description and Initial Cost Projection form to the Service Coordinator and participant.
- If the E-mod proposal is denied, the Service Coordinator is responsible for sending a copy of the NOD Denial of a Waiver Service and/or Waiver Provider (DOH-5734) and a copy of the Environmental Modification (E- Mod) Description and Initial Cost Projection form to the E-mod provider in a timely manner.
- If the E-mod proposal is approved by the RRDS, the E-mod provider and chosen contractor sign and date the Agreement of Final Determination acknowledging agreement to the final determination. The E-mod provider forwards a copy to the Service Coordinator. The Service Coordinator will advise the participant/legal guardian of their due process rights related to the decision.
STEP 9
The Service Coordinator obtains the participant's signature under the Participant/Owner agreement portion of the Agreement of Final Determination, indicating they understand their responsibilities and forwards a copy to the RRDS. Upon receipt, the RRDS provides written approval to the E-mod provider that the work may begin.NOTE: If, during completion of the E-mod, the contractor finds that changes/additional work that will result in a cost difference from the original projected cost are necessary, the contractor must obtain approval of the changes before proceeding, or risk non-payment for such changes. The contractor must work with the E-mod provider to obtain the prior approval from the RRDS, which is done through an Addendum to the service plan.STEP 10
Upon completion of the E-mod and prior to final payment to the E-mod provider, the evaluating agency that conducted the initial mandatory comprehensive evaluation must evaluate the finished modification, ensuring the project's satisfactory completion and adherence to safety and code standards. The evaluator must submit the post-modification evaluation report to the E-mod provider stating whether there has been compliance with the initial evaluation. A summary of the work, including the actual cost of the modification, must be documented on the Final Cost for Environmental Modifications/Vehicle Modifications form (DOH-5754) by the E-mod provider. The completed form and post-modification evaluation are submitted to the Service Coordinator and participant who sign off acknowledging that the service was provided in accordance with the request. After all required signatures and forms have been collected, the Service Coordinator submits the forms to the RRDS.The E-mod provider must also obtain photographs of the completed modification and submit them to the Service Coordinator. The Service Coordinator obtains final signature(s) of the participant and homeowner (if applicable) on the Agreement of Final Determination, agreeing that the work has been satisfactorily completed, and submits the signed form and photographs to the RRDS.
STEP 11
The Service Coordinator reviews the Final Cost for Environmental Modifications/Vehicle Modifications form, post-modification evaluation, and photographs of the completed modification. The RRDS approves and signs the Final Cost for Environmental Modifications/Vehicle Modifications form and sends a copy to the Waiver Service Provider and Service Coordinator.STEP 12
The E-mod provider submits a claim for reimbursement after receiving the RRDS approved and signed copy of the Final Cost for Environmental Modifications/Vehicle Modifications form from the RRDS. All supporting documents including receipts for materials and sub-contractor billing must be included in the final reimbursement request.Repairs
Items purchased become the property of the homeowner, and maintenance and repairs are the responsibility of the homeowner. However, repairs for home modifications which are medically necessary to support the waiver participant's independence in the home or community and that are cost-effective may be allowed. Repair and/or replacement of environmental modifications must be contingent upon development and implementation of a plan to minimize repeated damage.
Removal of E-mods and returning property to its original state is not the responsibility of NYSDOH or the NHTD waiver. This matter must be resolved before work begins.
Reimbursement
All projects require prior approval from the RRDC for work to begin and payment to occur. The E-mod provider may make payments to contractors/sub-contractors and assessments. Payment will not be paid for work initiated prior to waiver eligibility if the applicant fails to become waiver eligible. Medicaid reimbursement will occur only when the individual is enrolled in the waiver. If the E-mod is for an individual transitioning from a nursing facility, the provider will not be reimbursed until the individual becomes enrolled as a participant and transitions into the community. Payment will not be made for services completed prior to approval of the project by the RRDC via an approved service plan.
E-mod providers may bill for reimbursement only after receiving a copy of the RRDS signed and approved Final Cost for Environmental Modifications/Vehicle Modifications form.
DOH will NOT provide reimbursement for any adaptation or modification that has not followed the process outlined above or which commenced prior to receiving approval.
E-mods include the performance of necessary assessments and project management to determine the type of modifications needed and the assessment that the adaptation has been completed according to the required specifications. An itemized explanation for any costs incurred related to project management must be included as a separate statement and included with the Final Cost for Environmental Modifications/Vehicle Modifications form.
E-mods (which includes both home and vehicle modifications) are reimbursed according to the final cost of the project approved by the RRDC and must not exceed $45,000 per thirty-six (36) month period. This total includes the amount of the approved bid, evaluation costs, project management costs and home evaluation services (which may not exceed ten percent (10%) of the total cost of the project). If a participant needs more than one type of E-mod during the thirty-six (36) month period, the combined cost for this period may not exceed $45,000. It is expected that the RRDS will exhaust all efforts in working with the participant, E-mod provider, and Service Coordinator to stay within the $45,000 limit. Only under certain extraordinary circumstances, with documentation of efforts, NYSDOH may consider approval of E-mods that exceed the $45,000 limit. However, NYSDOH reserves the right to refuse approval.
With the approval of the home evaluator and RRDC, payments may be made in three increments: 1) upon execution of the contract, 2) half-way through the completion of the project, and 3) upon completion of the project and approval of the project by the RRDC and Home Evaluator. All phases of a home modification must be inspected and approved by the home evaluator and/or RRDC or NYSDOH waiver staff prior to payment.
Initial: The home evaluator visits the home to identify the current needs of the participant and any potential safety issues. The evaluator also assesses the structure of the home in order to identify any potential issues that may hinder the completion of the E-mod project. The home evaluator determines the specifications of the adaptation/modification.
Mid-Project: The home evaluator visits the home to monitor the implementation of the project to ensure adequate progress is being made and to assess for any additional safety or functional issues.
Final: The final home visit is conducted at the completion of the project. The home evaluator inspects the project to ensure all E-mods are completed and accessible to the participant. This visit is required before payment is released to the service provider.
All phases of a home modification must be inspected and approved by the home evaluator/Home Evaluation Specialist and/or RRDC or NYSDOH waiver staff prior to payment.
E-mod providers are required to submit projected cost estimates and final cost reports to the Service Coordinator. Each specific payment is made based on the tasks performed or the equipment or parts purchased on behalf of the participant. These reports are provided to the RRDC for approval. Payment reports for these services are reviewed by NYSDOH and the RRDC annually to ensure the claim amount is the same as the approved project amount. If there is a difference between the projected and actual costs, the RRDC requires an Addendum to the service plan to justify the increase.
This is a non-direct waiver service.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Provisions contained within this service allow for costs that may exceed comparable state plan services.
2. E-mods for Vehicles
Definition
Vehicle modifications provide the applicant/participant with the means to increase independence and access to services and supports in the community and may include adaptive equipment and/or vehicle modifications.
Equipment that is available from the dealer by factory installation as a standard or optional feature of the vehicle is not allowable for reimbursement as a waiver service. These items, as well as ongoing maintenance and repair of the vehicle, are the responsibility of the participant. Upkeep and maintenance of the modifications/adaptations made to the vehicle may be included in this waiver service with the approval of the RRDS, this does not include the routine maintenance of the vehicle.
Modifications will only be made to a vehicle if it is the primary source of transportation for the participant, is used to improve the waiver applicant/participant's independence and inclusion in the community, is available to the applicant/participant without restrictions, and is an alternative to Medicaid transportation. Vehicle modifications shall only be approved for one vehicle and must be done in the most cost-effective and least complicated manner while meeting the participant's functional capabilities and safety needs.
The adapted vehicle must be owned by the waiver applicant/participant, a family member who has consistent and ongoing contact with the waiver participant, or a non-relative who provides primary, long-term support to the participant, and who is not a paid provider of such services.
All vehicles modified under the waiver must be insured (collision and comprehensive) and meet New York State inspection and Adult Career and Continuing Education Services-Vocational Rehabilitation (ACCES-VR) standards, before and after the modifications are completed.
Reimbursement for vehicle modifications completed prior to waiver eligibility and RRDC approval is not allowed. The RRDC will not approve a request without an inspection, approval, and written recommendations of a Driver Rehabilitation Specialist. Payment will not be made prior to or in the absence of waiver eligibility.
All E-mods and vehicle modifications must be documented in the service plan and completed by providers approved by NYSDOH waiver staff.
The total cost of all E-mods, including home modifications, must be less than $45,000 within a thirty-six (36) month period, unless approved by NYSDOH. Any request for a modification with a total cost of $15,000 or more requires prior approval from NYSDOH. Driver Rehabilitation Specialist services may not exceed ten percent (10%) of the total cost of the project.
Provisions contained within this service allow for costs that may exceed CFCO State Plan services.
Allowable Vehicle Modifications
Adaptive equipment is designed to enable a participant to operate a vehicle, or be transported in the vehicle, but is not available as a routine option through the vehicle's manufacturer.
Adaptive equipment includes, but is not limited to, the following:
- Hand controls;
- Deep dish steering wheels;
- Spinner knobs;
- Wheelchair lock downs;
- Parking brake extensions;
- Foot controls;
- Wheelchair lifts; and/or
- Left foot gas pedals.
Vehicle modifications are adaptations and/or changes to the structure and internal design of existing vehicle equipment.
Vehicle modifications include, but are not limited to, the following:
- Replacement of a roof with an elevated fiberglass top;
- Floor cut-outs;
- Extension of steering column;
- Raised door;
- Repositioning of seats;
- Wheelchair floor; and/or
- Dashboard adaptations.
This service does not include general repairs or maintenance of a vehicle. All warranties and guarantees associated with the vehicle and adaptive device(s) must be fully utilized prior to seeking this service. Requests for repairs to E-mods for the vehicle must follow the same procedure as initial vehicle modification applications. This service will only support replacement items for damages beyond normal wear and tear. Consideration must be made to the cost-effectiveness of a repair vs replacement and/or new equipment.
The NHTD waiver program and the E-mod waiver service specifically, do not reimburse for the cost of returning a modification to its original state (whether this be for a home modification or a vehicle modification). This matter must be resolved prior to the service request is initiated.
Adaptive equipment and vehicle modifications may only be provided if the following conditions are met:
- The participant is not eligible for these services through any other resource (e.g., ACCES-VR, Veterans Administration, Workers Compensation, insurances, etc.). Any insurance claim for replacement equipment must be equal to or more than the cost of the modification;
- The vehicle was inspected by the RRDC prior to the approval of the modification request;
NOTE: The vehicle must also be inspected by the RRDC upon completion of the modification.- There is an acceptable written recommendation and justification submitted to the RRDC by a Driver Rehabilitation Specialist which states that the service(s) are essential for the participant to drive or be transported in a motor vehicle; and
- If the participant does not own the vehicle, the participant and the owner of the vehicle must sign the Agreement of Understanding form, confirming that the vehicle is available to the participant without restriction. The statement must include the owner's agreement to the modifications and that the participant will have full access to the vehicle.
Criteria for adaptive equipment and vehicle modifications:
- The Driver Rehabilitation Specialist will recommend the most cost-effective and least complicated adaptive equipment and vehicle modification(s) that meet the participant's functional capabilities and safety needs;
- A car driven by the participant may be considered for modification if the participant can (a) independently transfer themselves and a wheelchair into and out of the car, (b) has the functional ability to drive the car, and (c) does not have medical contraindications that preclude the ability to transfer from and/or drive the car;
- A van can only be considered for modification if a car cannot be modified to meet the participant's needs;
- Modifications to a vehicle that the participant will not be driving are limited to modifications that are essential to ensure safe transportation and access into and out of the vehicle; and
- Modifications may not exceed the Blue Book current market value of the vehicle. The value of the vehicle at the time of the modification must be equal to or more than the cost of the modification.
For New Vehicles
The participant (and/or family member) is expected to assume the cost of the vehicle purchase and all optional equipment available from the dealer through factory installation, i.e., air conditioning, sound systems. If an applicant/participant is planning to request a modification to a vehicle it is seeking to purchase, the vehicle must not be purchased prior to the determination that the vehicle can accommodate the modification and meet the participant's needs. The vehicle modification evaluation must be approved by the RRDC prior to purchasing the vehicle should this waiver service be requested.
For Used Vehicles
The NHTD waiver may cover the modification of used vehicles or the cost of modifications in a used vehicle only if the vehicle meets the above criteria and the following additional criteria:
- The vehicle must pass New York State inspection, and be registered and insured (for collision and comprehensive);
- Upon inspection by the Driver Rehabilitation Specialist, the vehicle must be structurally sound, without need of mechanical repairs and able to support/accommodate the needed adaptation;
- Upon inspection by the Driver Rehabilitation Specialist the vehicle must not have any rust or deficiencies in the areas to be modified or in the areas already modified; and
- The vehicle must be less than five years old or register fewer than 50,000 miles on the vehicle's odometer.
Used Adaptive Equipment
Used adaptive equipment and modification devices are sometimes available for purchase. To ensure the greatest safety and performance, NYSDOH will only approve used equipment purchased from licensed businesses dealing in the sale of vehicles or adaptive equipment. The equipment must be able to safely meet the participant's needs, as determined by an evaluation completed by a Driver Rehabilitation Specialist and be in good working condition, as determined by the vehicle modifier. It must be confirmed prior to purchase, that the equipment meets the specifications necessary for the vehicle in which it will be installed. The NHTD waiver will not contribute to the purchase of equipment previously purchased by the NYSDOH. Prior approval is required prior to the purchase.
Provider Qualifications
Any not-for-profit or for-profit health and human services agency, not-for-profit housing agency or local housing authority that has both the personnel and expertise to complete an E-mod and is an approved Medicaid provider may provide environmental Modifications or may subcontract with a qualified person or entity to provide Environmental Modifications.
Persons employed/contracted as a Driver Rehabilitation Specialist must be one of the following:
- Approved as a Driver Rehabilitation Specialist by Adult Career and Continuing Education Services- Vocational Rehabilitation (ACCES-VR);
- Licensed Occupational Therapist (Licensed by the NYS Education Department);
- Licensed Physical Therapist (Licensed by the NYS Education Department); or
- An individual with a Bachelor's degree certified as a Certified Driver Rehabilitation Specialist under the auspices of the Association of Driver Rehabilitation Specialists (ADED).
In addition, the individual must document three (3) years of experience providing driver rehabilitation services as defined by ACCES-VR.
The E-mod provider must ensure that individuals working on the E-mod are appropriately qualified and/or licensed to comply with any state or local rules. All materials and products used must meet any state and local construction requirements.
Providers must adhere to safety issues addressed in Article 18 of the New York State Uniform Fire Prevention and Building Code Act as well as local building codes.
Any currently employed waiver provider staff who met the waiver application qualifications which were in place on the date of their hire are approved to continue to provide services. Approved employees may receive a certificate of qualification to provide services. The issued certificate will allow that staff member to continue providing the same waiver service(s) at both their current location of employment and/or any change they have in future employment locations/agencies. This certificate has no expiration date and only applies to the waiver service they were qualified for upon hire. Certificates may be terminated at the discretion of NYSDOH.
Provider Role
The E-mod provider is responsible for the planning, oversight, supervision, and successful completion of the project. This includes the pre-, mid-way and post- evaluations of the modification, obtaining at least three (3) bids from qualified contractors for vehicle modifications costing $2,000 or more, and, with the participation of the participant and/or their legal guardian, making recommendations for bid selection.
Approval Process for Vehicle Modifications
STEP 1
During the development of the service plan, the applicant/participant and/or their legal guardian may request a vehicle modification. A dated physician's statement (on appropriate letterhead) of medical necessity is required.STEP 2
To determine the appropriateness of the requested vehicle modification, the applicant/participant, Service Coordinator, legal guardian and/or designated representative must first assess all other available resources to pay for the modifications (e.g., informal supports, community resources, State/federal agencies, ACCES-VR, Veterans Administration, Workers Compensation, insurances). Documentation by the Service Coordinator must include details of all resources assessed and the outcome of the assessment. All other resources must be shown to have been exhausted before approval will be granted.STEP 3
The applicant/participant selects a waiver approved E-mod provider to be responsible for planning, oversight, and supervision of the project.STEP 4
In conjunction with the applicant/participant and Service Coordinator, the E- mod provider must arrange for a mandatory comprehensive evaluation of the participant's needs for adaptive equipment or vehicle modifications that must be completed prior to commencement by a Driver Rehabilitation Specialist (who may be subcontracted by the E-mod provider). The evaluation must specify the most cost effective and least complicated vehicle modification that will ensure safe transportation, and exit/entrance into the vehicle for the participant. The evaluation must also include a dated and detailed scope of work and specifications.When arranging for the evaluation, the E-mod provider must also arrange for a post-modification evaluation within ten (10) calendar days of completion, subject to the modification being approved. Mid-project evaluations may also be required based on the complexity of the installation.
The E-mod provider must ensure that a copy of the evaluation is provided to the Service Coordinator, the participant, and the RRDC prior to proceeding with the bidding process.
After the Service Coordinator and E-mod provider receive written RRDC approval of the evaluation, the Service Coordinator is responsible for reviewing the Agreement of Understanding with the applicant/participant and/or legal guardian and obtaining the required acknowledgment of the participant and vehicle owner that the participant and vehicle owner understand the recommended plan for the adaptation, the bidding process, and their responsibility for maintaining the vehicle. The Service Coordinator provides a copy of the signed agreement to the E-mod provider.
STEP 5 The E-mod provider is responsible for obtaining the necessary bids from entities approved by ACCES-VR to provide vehicle modifications. The lowest bid among substantially equivalent bids that conform to the approved pre- evaluation must be selected.
- For modifications costing less than $2,000, only one (1) bid is required.
- For modifications costing $2,000 or more, three (3) bids are required.
All bids must include the information delineated in the NHTD Sample Bid Submission form for E-mods.
STEP 6
The E-mod provider will review the bids with the participant and/or their legal guardian and document recommendations for bid selection.The E-mod provider submits the bids with its recommendations to the Service Coordinator. The Service Coordinator then submits the request for the adaptive equipment or vehicle modification with all supporting documentation to the RRDS for approval. The supporting documentation must include:
- Justification (dated physician's statement) for the vehicle adaptive equipment or modification;
- All comprehensive assessments completed to determine the specifications of the vehicle modification;
- A copy of the selected bid and the projected costs;
- Vehicle Identification Number;
- Proof of the car ownership and insurance;
- Environmental Modification (E-Mod) Description and Initial Cost Projection form (DOH-5755);
- Agreement of Understanding;
- All documentation regarding bids;
- All documentation regarding participant's input;
- Completed service plan; and
- Photographs of the vehicle prior to the modification.
STEP 7
The RRDS reviews the proposal and may request more information. Approval is determined on a case-by-case basis, this is based on factors such as the reasonableness of the modification considering the applicant/participant's medical condition, cost of the modification requested, value and condition of the vehicle, compliance with the conditions and/or criteria listed above regarding modifications for new vehicles or used vehicles (whichever is applicable), and available funding.The lowest among substantially equivalent bids that conform to the bidding specifications must be selected, unless there is an overriding issue with the lowest bid or bidder, e.g., equivalency of the bids, reliability of the lowest bidder versus that of the next lowest bidder, or questions if one or more bids meet the bidding specifications. In such cases, the RRDS must contact DOH before proceeding further. Sufficient justification must be included in the request to the RRDC to accept a higher bid.
STEP 8
Upon RRDC written approval or denial of the vehicle modification, the RRDS will issue the Notice of Decision (NOD) and provide a copy of the NOD and the completed and signed Environmental Modification (E-Mod) Description and Initial Cost Projection form to the Service Coordinator and participant.If the vehicle modification proposal is denied, the Service Coordinator is responsible for sending a copy of the NOD and a copy of the Environmental Modification (E-Mod) Description and Initial Cost Projection form to the E-mod provider. The Service Coordinator will advise the participant/legal guardian of their due process rights related to the decision.
If the vehicle modification proposal is approved by the RRDS, the E-mod provider obtains a signature from the chosen contractor on the Agreement of Final Determination form acknowledging agreement with the final determination.
The E-mod provider forwards a copy of the signed Agreement of Final Determination form to the Service Coordinator.
NOTE: If the contractor finds that changes/additional work are necessary while completing the E-mod that will result in a cost difference from the original projected cost, the contractor must obtain approval of the changes before proceeding or risk non-payment for such changes. The contractor must work with the E-mod provider to obtain the prior approval from the RRDC through an Addendum to the service plan.STEP 9
The Service Coordinator obtains the participant's signature under the Participant/Owner agreement portion of the Agreement of Final Determination form indicating they understand their responsibilities and forwards a copy to the RRDC. Upon receipt, the RRDC provides written approval to the E-mod provider that the work may begin.STEP 10
Upon completion of the vehicle modification and prior to final payment, the Driver Rehabilitation Specialist must complete an evaluation of the finished modification to ensure that it has been satisfactorily completed and meets safety and code standards. The Driver Rehabilitation Specialist must submit the post-modification evaluation to the E-mod provider indicating compliance with the pre-modification assessment before the participant or member of the household takes possession of the vehicle. If the Driver Rehabilitation Specialist identifies a compliance issue, the contractor must correct the issue or contact the RRDC immediately if the contractor believes the issue cannot be remedied. Documentation must be obtained by the participant verifying the vehicle (including modification) is insured and has been inspected by New York State following the modification.The E-mod provider must obtain photographs of the completed vehicle modification and submit them to the Service Coordinator. The Service Coordinator obtains final signature(s) of the participant and vehicle owner (if applicable) on the Agreement of Final Determination form, agreeing the work has been satisfactorily completed, and submits the signed form to the RRDS.
STEP 11
The Service Coordinator submits the signed Final Cost for Environmental Modifications/Vehicle Modifications form (DOH-5754), the post-modification evaluation, photographs of the completed modification, all supporting documentation including receipts for equipment and billing statements for assessments, installation and labor, proof of updated insurance and inspection to the RRDC.STEP 12
The RRDC reviews the Final Cost for Environmental Modifications/Vehicle Modifications form and post-modification evaluation. Upon approval, the RRDC completes and signs the Final Cost for Environmental Modifications/Vehicle Modifications form. The RRDC sends a copy of this form to the E-mod provider and Service Coordinator. The Service Coordinator advises the applicant/participant of the approval.STEP 13
The E-mod provider submits a claim for reimbursement after receiving a copy of the Final Cost for Environmental Modifications/Vehicle Modifications form from the RRDS.Repairs
Modifications made to vehicles become the responsibility of the owner to maintain and repair. Additional items beyond those deemed necessary by NYSDOH are the responsibility of the participant.
Removing modifications or returning property to its original state is not the responsibility of NYSDOH or the NHTD waiver.
Reimbursement
Vehicle modifications must be provided by a NYSDOH approved provider, which may subcontract with a person or entity approved by ACCES-VR to provide vehicle modifications and included in the Service Plan to be reimbursed.
Medicaid reimbursement occurs only when the modification is for the use of an individual enrolled in the NHTD waiver.
DOH will NOT provide reimbursement for any adaptation or modification that has not followed the process outlined above or which commenced prior to receiving approval.
Home Evaluation services may not exceed ten percent (10%) of the total cost of the project.
Driver Rehabilitation Specialist services may not exceed ten percent (10%) of the total cost of the project.
E-mods include the performance of necessary assessments and project management to determine the type of modifications needed and the assessment that the adaptation has been completed according to the required specifications. An itemized explanation for these costs must be included as an attachment to the Final Cost for Environmental Modifications/Vehicle Modifications form.
The total cost of all E-mods, including home modifications, must be less than $45,000 within a thirty-six (36) month period, unless approved by NYSDOH. Any request for a modification with a total cost of $15,000 or more requires prior approval from NYSDOH.
It is expected that the Service Coordinator and RRDC will exhaust all available resources and make every effort to remain within the $45,000 limit. Only under certain extenuating circumstances, with documentation of efforts, will NYSDOH consider approval of any environmental modification totals that would exceed the $45,000 per thirty-six (36) month period limit. The RRDC is required to obtain prior approval from NYSDOH prior to exceeding any service limits. NYSDOH reserves the right to refuse approval of the request.
E-mod providers are required to submit projected cost estimates and final cost reports to the Service Coordinator. Each specific payment is made based on the tasks performed or the equipment or parts purchased on behalf of the participant. These statements are provided to the RRDC for approval. Claim reports for services are reviewed by NYSDOH and the RRDC annually to ensure the billed amount is the same as the approved amount. If there is a difference between the projected and actual costs, the RRDC requires an Addendum to the service plan to justify the increase.
This is a non-direct waiver service.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Home and Community Support Services (HCSS)
Definition
Home and Community Support Services (HCSS) are the combination of personal care services (Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs)) with oversight and/or supervision as a discrete service. Services are provided primarily in a participant's home. HCSS is provided to a waiver participant who requires assistance with personal care services tasks and whose health and welfare in the community is at risk because oversight and/or supervision of the participant is required even when no personal care task is being performed. Services may compliment, but not duplicate, other services.
HCSS is utilized when oversight and/or supervision as a discrete service is necessary to maintain the health and welfare of the participant living in the community. Oversight and/or supervision may be needed for safety monitoring to prevent an individual from harmful activities (for example, wandering or leaving the stove unattended). Oversight and/or supervision can be accomplished by cueing, prompting, direction, and instruction. HCSS is complementary but may not duplicate other services. HCSS is not to be used as a companion service. If the applicant/participant does not require oversight and/or supervision, HCSS is not appropriate.
HCSS can also be provided to participants needing oversight and/or supervision who also require assistance with personal care services. Personal care assistance provided by HCSS is defined as some or total assistance with ADLs such as dressing, bathing, hygiene/grooming, toileting, ambulation/mobility, transferring and eating; and IADLs such as housekeeping, shopping, meal preparation, laundry, escort to/from medical appointments, and assistance with telephone use essential to the maintenance of the participant's health and welfare in the community.
Since HCSS staff must be trained to the Personal Care Aide (PCA) Level II, they will be able to perform the scope of personal care tasks and functions necessary for an individual who also requires oversight and/or supervision. The HCSS worker is never allowed to exceed this scope of practice. HCSS differs from Personal Care Services provided under the Medicaid State Plan in that oversight/supervision is included in the service definition.
HCSS is provided under the direction and supervision of a Registered Professional Nurse (RN). The supervising RN is responsible for developing a plan of care and for orienting the HCSS staff providing this service. Dated physician orders must include documentation of the need for oversight and/or supervision as a discrete service based on medical diagnosis. The selected provider's supervising RN will be responsible for supervising HCSS staff.
HCSS is provided by Licensed Home Care Services Agencies (LHCSA) under Article 36 of New York State (NYS) Public Health Law. All regulations governing the LHCSA are in effect for the provision of this waiver service. Providers must have an approved license for each county in which services are provided. All staff must meet LHCSA training requirements, in addition to completing required waiver service training.
If during the service planning process, it is determined the applicant/participant will benefit from HCSS, a referral will be initiated. The applicant/participant begins by selecting an HCSS provider from the list of current qualified agencies provided by the Service Coordinator. Upon provider selection approval by the RRDC, the Service Coordinator contacts the selected HCSS provider to request an assessment.
If the applicant/participant's personal needs and/or goals do not warrant oversight and supervision and there are not sufficient informal supports to provide care, it may be more appropriate that the applicant/participant receive personal care services provided through the Medicaid State Plan. The RRDC and/or Service Coordinator may identify that the applicant/participant requires the provision of skilled tasks such as those provided under Certified Home Health Agency (CHHA) services or Private Duty Nursing. The Service Coordinator will work with the applicant/participant, their physician, and LDSS to secure the necessary evaluation to establish service eligibility. The approval of these services is provided by the LDSS, and the service is included in the applicant/participant's service plan. The same referral process would be completed for the Consumer Directed Personal Assistance Program (CDPAP) model. CDPAP may also be used for the delivery of skilled services. In cases involving a combination of HCSS and CDPAP for skilled services, the Service Coordinator must clearly articulate in the service plan the justification of the need for CDPAP and the task(s) CDPAP is(/are) providing to the participant.
If an applicant/participant requires HCSS due to the need for discrete oversight and/or supervision, this is an indicator that the individual is not self-directing and requires an appointed self-directed other to manage the CDPAP services. To avoid conflict of interest, the individual's HCSS worker, current NHTD waiver service providers, and/or NHTD contract staff (e.g., RRDS and NE) cannot serve as a self-directing other. In addition, any individual associated with an agency delivering Medicaid reimbursed services to the participant cannot serve as the self-directing other.
All HCSS must be documented in the service plan and provided by agencies approved as a provider of HCSS waiver services by the NYSDOH.
Assessment Process
Upon intake, if it appears the applicant/participant may benefit from HCSS, the Service Coordinator discusses the need for an assessment by an HCSS provider with the applicant/participant. The Service Coordinator provides the applicant/participant with a current conflict-free list of available HCSS providers. Upon selection of an HCSS provider, the applicant/participant completes the Provider Selection form (DOH-5730). The Service Coordinator submits the form to the RRDC for approval. Upon approval, the Service Coordinator arranges for a nursing assessment.
The Service Coordinator completes the designated sections of the Home Assessment Abstract (DSS-3139) and forwards the tool to the selected HCSS provider's supervising Registered Professional Nurse for completion. Upon receipt of the Home Assessment Abstract (DSS-3139) from the Service Coordinator, the HCSS provider's Registered Professional Nurse must complete the appropriate nursing-related sections of the Home Assessment Abstract (DSS-3139) and return the completed tool to the Service Coordinator within fourteen (14) calendar days. The Registered Professional Nurse must include in the Home Assessment Abstract (DSS-3139) documentation supporting the need for oversight and/or supervision. In addition, there must be clearly documented recommendations for the amount, frequency, and duration of HCSS for the participant and identification of any additional areas of support needed. The completed assessment tool must be provided to the Service Coordinator for review with the applicant/participant and to be included in the service plan. The RRDC will make the final determination regarding the total hours of service, frequency, and duration of HCSS to be provided.
An initial assessment may be completed by the RRDC Nurse Evaluator for an applicant/participant who is in a nursing home or hospital at the time service referral is made. The selected agency's supervising Registered Professional Nurse will need to complete the Home Assessment Abstract (DSS-3139) tool. For the section of the tool regarding the home environment, it is necessary to access the participant's residence. However, if this cannot be done prior to discharge from the hospital or nursing home, it must be completed on the first day HCSS is scheduled to begin. In this situation, HCSS may be approved to begin by the RRDC based on the information available in the preliminary and subsequent HCSS assessment.
The provider of HCSS must secure dated orders from the participant's medical practitioner supporting the need for services, including oversight and supervision, as outlined in LHCSA regulations 766.4 and 766.3.
These dated orders must include documentation of the need for oversight and/or supervision as a discrete service. If appropriate, the dated orders should also include documentation of the need for assistance with personal care tasks, the medical condition(s) and regimens involved in treatment, including medication regimens LHCSA regulations require the following:
"766.4 Medical orders.
……(b) For purposes of this Part, authorized practitioner shall refer to a doctor of medicine, a doctor of osteopathy, a doctor of podiatry, a licensed midwife or a nurse practitioner authorized under federal and state law and applicable rules and regulations to provide medical care and services to the patient except as may be limited by third party contract.
……(d) Medical orders shall reference all diagnoses, medications, treatments, prognoses, need for palliative care, and other pertinent patient information relevant to the agency plan of care; and
(1) shall be authenticated by an authorized practitioner within 12 months after admission to the agency; and
(2) when changes in the patient's medical orders are indicated, orders, including telephone orders, shall be authenticated by the authorized practitioner within 12 months."
The medical order must be supported by the plan of care (ISP/RSP) as described below:
"766.3 Plan of care.
The governing authority or operator shall ensure that:
……(b) a plan of care is established for each patient based on a professional assessment of the patient's needs and includes pertinent diagnosis, prognosis, need for palliative care, mental status, frequency of each service to be provided, medications, treatments, diet regimens, functional limitations and rehabilitation potential."
The RRDC is responsible to approve the service plan which includes the hours, frequency and duration of the service.
Other Considerations
Under the NHTD waiver, the selected provider's supervising Registered Professional Nurse will be responsible for supervising HCSS staff. The selected provider's supervising Registered Professional Nurse must conduct an initial home visit on the day and time HCSS staff begins providing services to the participant. The focus of this visit is for the selected provider's supervising Registered Professional Nurse to introduce the staff to the participant, ensure services established during the initial assessment continue to be sufficient and, if necessary, complete the environmental portion of the preliminary assessment tool. Any changes indicated will be communicated to the NHTD Service Coordinator and/or MD, as appropriate. If any activity requires on-the-job training, the selected provider's supervising Registered Professional Nurse will provide it during this visit.
All participants have a right to their own privacy within their home and should be afforded as such unless otherwise stated in their Plan of Protective Oversight (PPO). If a participant's personal care and oversight/supervision needs warrant HCSS during the night, the HCSS staff must remain awake throughout the duration of time assigned to the participant to ensure the appropriate level of oversight/supervision is provided. Dependent on the participant's need, it may be necessary for the participant to leave their bedroom door slightly ajar in order for adequate oversight and/or supervision to be provided. If this, or any other, assurances are necessary to ensure proper oversight and/or supervision, the specification(s) will be listed on the participant's Plan of Protective Oversight (PPO) and requires the participant's consent. If this, and/or any other specifications for proper oversight and/or supervision, are not listed on the participant's PPO, then the participant's right to privacy must be respected. Activities/goals included in the detailed plan should support these activities.
Often, when HCSS is being utilized, there may be other services involved such as Independent Living Skills Training (ILST), Positive Behavioral Intervention and Support (PBIS), and/or other waiver service providers assisting the participant to work toward their goals. For example, if ILST is utilized, an assessment will be completed and a Detailed Plan developed for cueing, prompting, or supervising the participant in ADLs and IADLs. The ILST will work cooperatively with the selected provider's supervising Registered Professional Nurse and HCSS staff to assure implementation of the Detailed Plan and provide needed guidance and/or additional training. Another example is the PBIS Specialist who may also train the HCSS staff in behavioral interventions based on a Detailed Plan. The provision of these types of complementary trainings will serve to enhance the level of consistency, cooperation, communication, and teamwork between providers and the participant. It is also important to note that HCSS may be provided concurrently with other services. If a participant requires personal care services while receiving another service, the service may be provided at the same time with sufficient justification and prior approval of the RRDC. The justification must be included and supported in the service plan.
Regularly scheduled Team Meetings with the participant and service providers are an essential part of ensuring the participant's health and welfare. This meeting is instrumental in the development and implementation of the service plan. Failure to attend Team Meetings may jeopardize the ability of the waiver provider to continue to provide waiver services. Participation at the Team Meeting is used to garner information from the participant and informal supports about needed services and change(s) in physical and/or cognitive status. The Team Meeting will also include discussion about the individual's progress and any service changes that may be warranted. It is a direct service to the participant. HCSS staff must attend Team Meetings as indicated by the Service Coordinator.
It is important to consider the interests and needs of the waiver participant when assigning HCSS support. The ability of the HCSS staff to support the strengths, interests, and needs of the participant will promote a better working relationship and help to meet the established goals for the service. When an applicant/participant selects a provider, they do not select the individual staff person. Due to administrative and staffing demands, providers work to ensure coverage, not a specific staff person. A participant may indicate staff preference to a provider; however, staff assignment is not guaranteed. Attempting to find the best match between the HCSS staff and participant remains a goal.
Given the critical need for continuity in oversight and/or supervision, HCSS providers are reminded of their responsibility for assuring sufficient back-up for the HCSS staff. Failure of staff to arrive to their assigned shift or to provide supervision during emergency room visits, may result in an SRI. Participants must also work to identify informal supports and back-up caregivers, should staff not be available or an emergency occurs. Additionally, the PPO should indicate those circumstances where a participant can be left alone or unsupervised in order to flex staff assignments and tasks; for example, leaving a participant alone in their apartment to go to the laundry room in the building.
Provider Qualifications
HCSS may only be provided by a Licensed Home Care Services Agency (LHCSA) licensed under Article 36 of the NYS Public Health law or exempt from licensure pursuant to 10 NYCRR Section 765-2.1(c). All regulations governing the LHCSA will be in effect for the provision of this service, e.g., patient rights, patient service policies and procedures, plan of care, medical orders, clinical supervision, patient care records, governing authority, contracts, personnel, records, and reports.
In accordance with Article 28-E of the Public Health Law and Executive Law 845-b, every residential health care facility (RHCF) which is licensed under Article 28 of the Public Health Law, and any certified home health agency, licensed home care services agency or long-term home health care program, certified, licensed or authorized under Article 36 of the Public Health Law, to provide services to patients, residents or clients shall request a criminal history record check, by the Department of Health (NYSDOH), for each prospective employee who will be providing direct care or supervision to patients, residents or clients. The term employee does not include persons licensed pursuant to Title 8 of the Education Law or Article 28-D of the Public Health Law such individuals as nurses, physical therapists, and occupational therapists, or volunteers. Part 402 of Title 10 of the Official Compilation of Codes, Rules and Regulations for the State of New York (NYCRR) establishes the process for conducting the background investigation and the standards for review by NYSDOH.
Each provider must develop and implement written policies and procedures that include protecting the safety of persons receiving services from temporary employees consistent with the regulations (e.g., appropriate direct observation and evaluation pending, review and employment eligibility determination). A provider requesting a criminal history record check obtains the fingerprints accompanied by two forms of identification to be submitted to NYSDOH. Providers must maintain and retain current records, including a roster of current employees who have been reviewed, to which NYSDOH shall have immediate and unrestricted access for the purpose of monitoring compliance.
Verification of compliance with the criminal history record check regulations are included in NYSDOH surveillance processes. At the time of surveillance, NYSDOH surveyors utilize a standardized tool to evaluate compliance with the criminal history background checks regulations. If a provider is found to be not in compliance with the regulations, a statement of deficiency(/ies) is issued for which the provider must provide a plan of correction. Licensed Home Care Agencies and Certified Home Health Agencies are surveyed every three (3) years, and RHCF entities are surveyed on average of once a year.
NYSDOH verifies that upon application, waiver providers meet required licensure and/or certification standards through an extensive review of documents submitted with the enrollment application, including resumes, licenses, certifications, or contracts.
Verification that service providers continue to meet required licensure and/or certification standards is conducted through the Department's three (3)-year surveillance cycle policy. In addition, licensure and/or certification may be reviewed during complaint investigations or at the request of NYSDOH waiver staff. If findings of the survey reveal deficient practices, the provider is required to submit a plan of correction or may be disenrolled as a provider of waiver services. Based on the scope and severity of deficiencies identified, NYSDOH may conduct a follow-up survey with the provider to determine if the plan of correction was implemented sufficiently and within the specified timeframes.
HCSS direct care staff members must:
- Be at least eighteen (18) years old;
- Be able to follow written and verbal instructions;
- Have the ability and skills necessary to meet the waiver participant's needs that will be addressed through this service;
- Have a valid certificate to indicate that they have successfully completed a forty (40)-hour PCA Level II Training program for Personal Care Aides or PCA Alternate Competency Demonstration equivalency testing that is approved by NYSDOH;
- Attend six (6) hours of in-service education per year, which includes NHTD waiver-specific training;
- Be in good physical health, including documentation of an annual (or more frequently if necessary) health status assessment and declaration that they are free from health impairments which pose potential risks to waiver participants or personnel, immunizations, and a yearly Mantoux skin test; and
- Be supervised in accordance with Licensed Home Care Service Agency (LHCSA) regulations.
Staff providing HCSS must meet all other requirements under Title 10 NYCRR 766.11 for the provision of Personal Care Aide services and have completed a criminal history check to the extent required by Title 10 NYCRR 402. HCSS staff must be supervised in accordance with LHCSA regulations. Program staff must act under the direction of an individual who meets the qualifications listed below.
NOTE: Section 10 NYCRR 400.23 is repealed effective November 13, 2019 and is now replaced with Title 10 NYCRR 402.
Nursing supervision must be provided by a Licensed Professional Nurse who:
Is licensed by the NYS Education Department pursuant to Article 139 of the NYS Education Law and is currently certified to practice as a registered professional nurse in New York State; and
Is in good physical health as required by NYSDOH for employees of LHCSA, that includes documentation of an annual health status assessment, immunizations, tuberculosis screening and testing, and a declaration that they are free from health impairments that pose potential risks to patients or personnel.The selected provider's supervising Registered Professional Nurse must attend approved Waiver Service training prior to providing billable services, and any additional training required by NYSDOH.
The HCSS agency must have a communication system available with twenty-four (24) hours/seven (7) days per week coverage to assure any issues regarding a participant's services can be addressed.
Note: requirements will change in conjunction with licensure and regulatory requirements for Licensed Home Care Service Agencies and/or Certified Home Health Care Agencies.
Reimbursement
HCSS services, including both direct care and selected provider's supervising Registered Professional Nurse Visits, must be provided by a NYSDOH approved provider and included in the service plan to be reimbursed. Each service plan contains an approved number of annual service units that a provider is authorized to deliver. The provider cannot exceed the number of approved annual hours of service contained in the service plan.
The provider must have a license for each county in which they are seeking to provide services. Rates are based on the county where the services are provided.
On-the-job training is considered administrative costs and is not billable as HCSS.
HCSS services are reimbursed on an hourly or partial unit basis. When HCSS is provided to more than one person at a time, the ratio of provider to participants must be stated in the service plan and the billing must be prorated. Example: HCSS is providing services to two individuals living together for six (6) hours. The service plan for everyone reflects a 1:2 ratio and billing reflects three hours per person.
HCSS staff must attend Team Meetings. Attendance at the meeting is included in the total number of approved annual hours of service. However, the provider may claim reimbursement for only one agency representative attending a Team Meeting. The assessment of the applicant/participant for the need for HCSS and providing recommendations for HCSS is considered an administrative cost and, therefore, is not discretely billable. The selected provider's supervising Registered Professional Nurse visit made on the day the HCSS begins is billable on a per visit basis. This visit will result in the development of the Detailed Plan and, if necessary, provide an opportunity for the completion of the environmental section of the preliminary assessment.
Providers are not reimbursed for time spent writing reports and/or service plans.
Subsequent visits made by the selected provider's supervising Registered Professional Nurse for supervision or on-the-job training of the HCSS staff are considered administrative costs and, therefore, are not billable.
A selected provider's supervising Registered Professional Nurse Visit made six (6) weeks prior to the development of a Revised Service Plan (RSP) to re-evaluate the participant for the continued need for HCSS and to complete the Individual Service Report (ISR) is a billable visit.
Section 12006(a) of the 21stCentury Cures Act (the Cures Act) requires that states implement Electronic Visit Verification (EVV) for all Medicaid Personal Care Services (PCS) and Home Health Care Services (HHCS) requiring an in-home visit by a provider. As a LHCSA, HCSS providers are required to implement an electronic visit verification system. The EVV system is required to capture the individual receiving the service and the date of service delivery.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate any Medicaid claims. These providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Home Visits by Medical Personnel
Definition
Home Visits by Medical Personnel are individually designed services to provide diagnosis, treatment, and wellness monitoring to preserve the waiver participant's functional capacity to remain in the community. Wellness monitoring is critical to the overall health of the waiver participant. Wellness monitoring includes disease prevention, the provision of health education, and the identification of modifiable health risks. Through increased awareness and education, the waiver participant is more apt to make healthy lifestyle choices, which will decrease the likelihood of unnecessary institutionalization. The frequency of wellness monitoring will be contingent on the waiver participant's needs.
Home visits by Medical Personnel are expected to decrease the likelihood of exacerbations of chronic medical conditions and unnecessary and costly emergency room visits, hospitalizations, and nursing facility placement. In addition to assessing the waiver participant, this service will also include the evaluation of the home environment from a medical perspective and the waiver participant's informal supports' ability to maintain and/or assume the role of caregiver. The provider's assessment of the informal supports/caregivers will focus on the relationship to the waiver participant in terms of the physical, social, and emotional assistance that is currently provided or may be provided in the future. Based on the outcome of this assessment, the provider of this service can make referrals for - or request that the Service Coordinator make referrals for - additional assistance as appropriate to maintain the waiver participant's ability to remain at home or in the least restrictive setting. This service will enhance the quality of medical care and the quality of life of the waiver participant.
Home Visits by Medical Personnel differs from what is offered under the New York Medicaid State Plan as this waiver service is used for wellness monitoring, the assessment of the informal supports'/caregivers' ability to aid the waiver participant, and/or the evaluation of the waiver participant's home environment from a medical perspective. This preventive activity decreases the likelihood of accidents in the home, lowers the waiver participant's and caregiver's stress levels, increases the quality of medical care provided to the waiver participant, and increases the efficiency of medication management, all of which promote the waiver participant's ability to remain at home.
This service is especially beneficial for those waiver participants who have significant difficulty traveling or are unable to travel for needed medical care provided by a physician, physician's assistant, or nurse practitioner because of:
- severe mobility impairments;
- terminal illness;
- a chronic condition that can be exacerbated by travel;
- severe pain;
- medical providers at a physician's office and/or transportation providers refusing to provide services due to an individual's disruptive behavior;
- the home visit is cost effective; and/or
- transportation to medical appointments is limited due to geographical or other considerations.
The Medical Personnel will perform a comprehensive assessment of the physical, psychosocial, environmental, and economic factors in the waiver participant's own environment that could affect the waiver participant's health and welfare and the ability to remain in the community. This comprehensive assessment and medical follow-up in the waiver participant's home is intended to improve the waiver participant's functioning. Because of this improved functioning, and by having the Medical Personnel complete a comprehensive assessment in the waiver participant's home, the Medical Personnel is more apt to detect conditions in the home environment that negatively affect the waiver participant's health and welfare and respond accordingly. This preventive activity is expected to decrease the likelihood of accidents in the home, lower the waiver participant's and caregiver's stress level, increase the quality of medical care provided to the waiver participant, and increase the efficiency of medication management which will promote the waiver participant's ability to remain at home.
As part of the home visit, the Medical Personnel will evaluate safety issues and other conditions in the home from a medical perspective. Medical Personnel will conduct a basic assessment of the home environment in relation to the waiver participant's health and welfare. Any concerns about the home environment that may affect the waiver participant's health and welfare will be shared with the Service Coordinator and other relevant members of the team.
The Medical Personnel are an integral part of the waiver participant's service provider team and have the responsibility to inform the Service Coordinator of any recommendations for services to meet the waiver participant's medical needs and/or other significant findings. The Service Coordinator will utilize this information in revising the waiver participant's service plan.
Provider Qualifications
Home Visits by Medical Personnel must be provided by a Physician in Private Practice. Persons providing Home Visits by Medical Personnel shall be a:
- Physician - Licensed and registered to practice medicine in New York State pursuant to Article 131 of the NYS Education Law;
- Nurse Practitioner - Certified as a nurse practitioner pursuant to Article 139 of the NYS Education Law, who must be working in a specialty area in collaboration with a licensed physician qualified to work in that specialty and in accordance with a written practice agreement and written practice protocols; or
- Physician Assistant - Registered as a physician assistant pursuant to Article 131-B of the New York State Education Law, who must be working under the supervision of a licensed physician and performing only such acts and duties within the scope of practice of such supervising physician.
Reimbursement
Home Visits by Medical Personnel must be provided by a DOH approved provider and must be included in the service plan to be reimbursed. Rates are based on Upstate/Downstate assignment.
Home Visits by Medical Personnel are provided on an individual basis and billed in twenty (20) minute units with a maximum of three (3) units per visit.
Home Visits by Medical Personnel providers participating in Team Meetings will be reimbursed at regular rate for attendance at these meetings.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Independent Living Skills Training (ILST)
Definition
Independent Living Skills Training Services (ILST) are individually designed to improve or maintain the ability of the waiver participant to live as independently as possible in the community. ILST assists in recovering skills that have decreased as a result of onset of disability. Also, ILST will primarily be targeted to those individuals with progressive illnesses to maintain essential skills. ILST may be provided in the waiver participant's residence and in the community. This service will primarily be provided on an individual basis. Only in the unique situation, in which the waiver participant will receive greater benefit from other than a 1:1 situation, will a group method of providing this service be approved. This arrangement requires prior approval from the RRDC.
ILST must be provided in the environment and situation that will result in the greatest positive outcome for the waiver participant. It is expected that this service will be provided in the waiver participant's environment; for example, in the participant's kitchen as opposed to a provider's kitchen. This expectation is based on the difficulty many participants experience with transferring or generalizing knowledge and skills from one situation to another. However, it is recognized that there is need for some practice of skills before using them in the waiver participant's environment. ILST cannot be provided in a structured day program setting without specific approval from the RRDC.
The ILST provider utilizes the comprehensive functional assessment of the waiver participant provided through the UAS-NY to identify the participant's strengths and weaknesses in performing Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) related to their established goals. The UAS-NY assessment is the basis for developing an ILST plan that describes the milestones and interim steps necessary to attain these goals. The UAS-NY assessment also includes a determination of the participant's manner of learning new skills and responses to various interventions. This comprehensive and functional assessment is conducted at least annually from the date of the last assessment and approved by the RRDS in conjunction with the service plan. The UAS-NY is used to develop the Detailed Plan and service goals for ILST services. The Detailed Plan will identify milestones to be met during the service plan period. Frequency, amount, and duration of ILST services are determined following completion of the initial and ongoing UAS-NY assessments.
ILST services may include assessment, training, and supervision of an individual with issues related to self-care, medication management, task completion, communication skills, interpersonal skills, socialization, sensory/motor skills, mobility, community transportation skills, reduction/elimination of maladaptive behaviors, problem solving skills, money management, pre-vocational skills, and ability to maintain a household.
ILST services may also be used to assist a waiver participant in returning to employment or expanding the waiver participant's involvement in meaningful activities such as volunteering. The utilization of this service for vocational support is only implemented after it is determined that the waiver participant is not eligible for services through either the New York State Education Adult Career and Continuing Education Services-Vocational Rehabilitation (ACCES-VR) or the Commission for the Blind and Visually Handicapped (CBVH); ACCES-VR and CBVH services have been exhausted; or the activity is not supported by ACCES-VR or CBVH services. ILST is not used as "job coaching," but to provide training in other skills that support vocational opportunities.
It is expected that ILST providers will train the waiver participant's informal supports, paid staff, and waiver providers to provide the type and level of supports that allows the waiver participant to act and become as independent as possible in ADLs and IADLs. ILST is used for training purposes and not for the provision of ongoing long-term care supports. This service may continue only when the waiver participant has reasonable and attainable goals. Justification to provide or continue this service must be clearly stated in the service plan within the context of clearly defined and reasonable goals. The provider cannot exceed the number of approved annual hours of service contained in the participant's service plan.
Each service plan contains an approved number of annual service units a provider is authorized to deliver. ILST providers must participate in Team Meetings. Meeting time is included in the total number of service hours included in the service plan. Regularly scheduled Team Meetings with the participant and service providers are an essential part of assuring the participant's health and welfare. This meeting is instrumental in the development and implementation of the service plan. Failure to attend Team Meetings may jeopardize the ability of the waiver provider to continue to provide waiver services. Participation at the Team Meeting is used to garner information from the participant and informal supports about needed services and change(s) in physical and/or cognitive status. The Team Meeting will also include discussion about the individual's progress and any service changes that may be warranted. It is a direct service to the participant.
ILST staff must complete and submit routine Individual Service Reports (ISRs) for review and discussion during Team Meetings and the service plan process.
Provider Qualifications
ILST may be provided by any not-for-profit or for-profit health and human services agency.
Persons employed as an Independent Living Skills and Training provider must be a/an:
- Licensed Master Social Worker (licensed by the NYS Education Department pursuant to Article 154 of the NYS Education Law);
- Licensed Clinical Social Worker (licensed by the NYS Education Department pursuant to Article 154 of the NYS Education Law);
- Individual with a Doctorate or Master of Social Work;
- Individual with a Doctorate or Master of Psychology;
- Licensed Physical Therapist (licensed by the NYS Education Department pursuant to Article 136 of the NYS Education Law);
- Registered Professional Nurse (registered by the NYS Education Department pursuant to Article 139 of the NYS Education Law);
- Certified Teacher of Students with Disabilities (certified by the NYS Education Department);
- Certified Rehabilitation Counselor (certified by the Commission on Rehabilitation Counselor Certification);
- Licensed Speech Pathologist (licensed by the NYS Education Department pursuant to Article 159 of the NYS Education Law);
- Registered Occupational Therapist (registered by the NYS Education Department pursuant to Article 156 of the NYS Education Law); or
- Individual with a Master of Gerontology;
AND
Must also have, at a minimum, one (1) year of experience completing functional based assessments of ADLs and IADLs, developing comprehensive treatment plans, and teaching individuals with disabilities and/or seniors to be more functionally independent.
OR- Be an individual with a Bachelor's degree and three (3) years of experience completing functional based assessments of ADLs and IADLs, developing comprehensive treatment plans, and teaching individuals with disabilities and/or seniors to be more functionally independent; or
- Be an individual with an Associate's degree and five (5) years of experience completing functional based assessments of ADLs and IADLs, developing a comprehensive treatment plan, and teaching individuals with disabilities and/or seniors to be more functionally independent.
The ILST provider agency must make every possible effort to match the skills and experience of the individual provider to the specific goals of the participant.
All agencies that employ two (2) or more ILST staff must provide supervision by an individual who fully meets the qualifications as an ILST provider. A supervisor may maintain an active caseload of waiver participants.
The supervisor is required to:
- Meet any potential waiver participants prior to the completion of the Detailed Plan developed by the ILST under their supervision;
- Work with the ILST to reevaluate the participant as needed, but not less than at the completion of the Revised Service Plans and whenever Addenda to the service plan are written;
- Have supervisory meetings with staff on at least a monthly basis;
- Provide ongoing supervision and training to staff; and
- Review and sign-off on all Detailed Plans.
Any currently employed waiver provider staff who met the waiver application qualifications which were in place on the date of their hire are approved to continue to provide services. Approved employees may receive a certificate of qualification to provide services. The issued certificate will allow that staff member to continue providing the same waiver service(s) at both their current location of employment and/or any change they have in future employment locations/agencies. This certificate has no expiration date and only applies to the waiver service they were qualified for upon hire. Certificates may be terminated at the discretion of NYSDOH.
Reimbursement
ILST services must be provided by a NYSDOH approved provider and must be included in the service plan to be reimbursed. The participant must be present at the time-of-service delivery.
Providers may not bill for hours used to complete initial, re-assessments, reviewing service data, and writing ILST plans and reports.
ILST services are not to exceed two hundred twenty (220) hours annually and no more than four (4) hours per day. In all cases, service limits are soft limits that may be exceeded due to medical necessity. If the individual's needs and goals cannot be met within the established limits, a participant may request to exceed the limit by providing sufficient medical justification to the RRDC. The RRDC will approve or deny the request for additional hours of service.
ILST is reimbursed in one (1) hour units or partial units. Rates are based on Upstate/Downstate assignment based on the county where the services are provided or as assigned by DOH.
Only in extraordinary situations where the participant benefits specifically from a group setting will this service be approved by the RRDS on other than an individual basis. This arrangement requires prior approval from the RRDC. In such situations, the provider may bill for a pro-rated percentage of the time spent with a participant (total hourly unit(s) divided by the total number of participants in the group). Training time provided to informal supports, waiver or non-waiver service providers must be designated in the service plan in order to be reimbursed and the participant must be present at the time of training.
This service does not duplicate other habilitative services available through the New York Medicaid State Plan.
Moving Assistance Services
Definition
Moving Assistance Services are individually designed services intended to pack and/or transport a waiver participant's possessions and furnishings within the state of New York when they must move from an inadequate or unsafe housing situation to a viable environment that more adequately meets the waiver participant's health and welfare needs. Moving Assistance may also be utilized when the waiver participant is moving to a location where there are more available resources and/or informal supports, thus allowing the waiver participant to remain in the community.
Moving Assistance is only available to waiver participants who already reside in the community. This service differs from Community Transitional Services (CTS) as CTS is only available to waiver applicants/participants who are transitioning from a nursing home. The funding limits for this service are separate and distinct. The two services cannot be used at the same time in any approved service plan.
Moving Assistance must be included in the service plan and approved by the RRDC. Billing for services may not exceed $5,000 per twelve (12) month period from the date of the move. If the cost of the move exceeds $1,000, the Service Coordinator must obtain three bids from licensed moving companies. If in extreme circumstances a contract for Moving Assistance exceeds $5,000, it must have prior approval from NYSDOH before the move may proceed.
Provider Qualifications
Any not-for-profit or for-profit health and human service agency that has both the personnel and expertise to provide Moving Assistance and is an approved Medicaid provider may provide Moving Assistance or may subcontract with a qualified person or entity to provide Moving Assistance. If the Moving Assistance provider chooses to subcontract, it must do so with licensed and certified (by NYS Dept. of Transportation) moving companies to provide this service. There are no minimum staff qualifications to provide Moving Assistance. The qualifications are specific to the licensure and registration of the provider agency as a whole. If due to extreme circumstances a licensed mover is not available, another sub-contractor may be utilized upon prior approval by the RRDC.
Approval Process for Moving Assistance
STEP 1
The participant, Service Coordinator, and anyone selected by the participant, establish the need for the move.STEP 2
If the move is deemed necessary, then the participant may choose an approved provider of Moving Assistance and completes the Provider Selection form (DOH-5730).STEP 3
The Service Coordinator provides the Provider Selection form to the selected Moving Assistance provider who works with the participant to select a moving company. The Provider Selection form is submitted to the RRDC for approval.STEP 4
The Service Coordinator, in conjunction with the Moving Assistance provider, identifies a moving company willing to accept the job. The moving company submits an estimate to the Moving Assistance provider, which must include all costs associated with the move (for example, packing of the participant's personal items).If the estimate is less than $1,000, the Moving Assistance provider submits the estimate to the participant's Service Coordinator. If the cost of this service is greater than $1,000, a total of three (3) bids must be obtained and submitted for approval.
If the bidding process delays the date of the move, the Service Coordinator will contact the RRDC to discuss the circumstances of the delay. The RRDC may suspend the bidding process. Upon NYSDOH approval, the move may proceed with the available bids.
STEP 5
The Service Coordinator completes the Moving Assistance Description and Initial Cost Projection form (DOH-5751), reviews the form and the terms and conditions of the mover's contract with the participant.STEP 6
The Service Coordinator secures the required information from the mover and/or Moving Assistance provider and returns it to the Service Coordinator.STEP 7
The Service Coordinator submits the completed Moving Assistance Description and Initial Cost Projection form, the bid(s) and mover's contract with the Revised Service Plan, or an Addendum to the RRDC for approval.STEP 8
The RRDC reviews and approves the costs for the move and sends a copy of the approved form back to the Service Coordinator.STEP 9
The Service Coordinator notifies the Moving Assistance provider that the participant has been approved for the move.STEP 10
The Moving Assistance provider completes and signs the Waiver Services Final Cost and RRDS Approval of Final Cost form (DOH-5755) and sends the form to the Service Coordinator. The Service Coordinator and participant must sign the form indicating that services were provided per the service request. After all needed signatures have been collected, the Service Coordinator and submits the signed and completed Waiver Services Final Cost and RRDS Approval of Final Cost form to the RRDC.STEP 11
The RRDC provides the final authorization and sends a copy to the Moving Assistance provider and Service Coordinator.STEP 12
The Moving Assistance provider may claim for the service once the NOD of approval is received, and it is confirmed the move has been successfully completed.Reimbursement
Moving Assistance must be documented in the service plan and/or addendum, approved by the RRDC, and provided by an approved waiver service provider.
This is a non-direct waiver service.
This service is reimbursed on a cost basis. Total reimbursement for Moving Assistance must not exceed $5,000 per twelve (12) month period. Requests above $5,000 must receive prior approval by the RRDC and NYSDOH. Moving Assistance is not a direct waiver service. Providers are not required to attend Team Meetings; therefore, there is no billing allowed for participation in Team Meetings.
Nutritional Counseling/Educational Services
Definition
Nutritional Counseling/Educational Services is an individually designed service which provides an assessment of the waiver participant's nutritional needs and food patterns, and the planning for the provision of food and drink appropriate for the waiver participant's conditions, or the provision of nutrition education, and counseling to meet normal and therapeutic needs. The services are generally provided in the participant's home.
In addition, these services may include:
- Assessment of nutritional status and food preferences;
- Planning for the provision of appropriate dietary intake within the waiver participant's home environment and cultural considerations;
- Nutritional education regarding therapeutic diets as part of the development of a nutritional treatment plan;
- Regular evaluation and revision of nutritional plans; and
- The provision of in-service education to the waiver participant, family, advocates, waiver, and non-waiver staff as well as consultation on specific dietary problems of the waiver participants.
Provider Qualifications
Nutritional Counseling/Educational Services may be provided by any not-for-profit or for- profit health and human services agency.
Staff providing Nutritional Counseling/Educational Services must be a:
- Registered Dietician (registered by the NYS Education Department pursuant to Article 157 of the NYS Education Law); or
- Registered Nutritionist (registered by the NYS Education Department pursuant to Article 157 of the NYS Education Law or certified by the Commission of Dietetic Registration).
Nutritional Counseling/Educational Services cannot be provided to a participant without a dated physician's written order which is obtained initially and every six (6) months thereafter by the Nutritional Counseling/Educational Services provider. Orders must contain number of hours of service, frequency, and duration of the service provided. The Nutritional Counseling/Educational Services provider must obtain and maintain all physician orders in the waiver participant's file at the agency according to existing regulations for Nutritional Counseling. Copies of all orders will be provided to the Service Coordinator for inclusion in the participant file.
Reimbursement
Nutritional Counseling/Educational Services must be provided by a NYSDOH approved provider and must be included in the service plan to be reimbursed. Rates are based on an Upstate/Downstate assignment based on where the services are provided.
Nutritional Counseling/Educational Services are provided on an individual, per visit basis. In-service education and consultation provided to informal supports or waiver, or non-waiver service providers must be included in the service plan in order to be reimbursed.
Nutritional Counseling/Educational Services providers participating in Team Meetings will be reimbursed at the per visit rate for their time at the Team Meeting.
This service does not duplicate other services available through the New York Medicaid State Plan.
Peer Mentoring
Definition
Peer Mentoring is an individually designed service intended to improve the waiver participant's self-sufficiency, self-reliance, and ability to access needed services, goods, and opportunities in the community. This is to be accomplished through education, teaching, instruction, information sharing, and self-advocacy training.
This service is for seniors and people with disabilities who are struggling to regain a self-satisfying life and may benefit from relating to another person who has been successful in this effort. A Peer Mentor is able to assist the waiver participant to overcome barriers that they may face in the community.
It is expected that Peer Mentoring will be conducted on a short-term basis and help facilitate referral to other resources that may provide on-going/longer-term services. This service may continue only when the waiver participant has reasonable and attainable goals.
The provider of this service should develop an ongoing relationship with a local provider of mental health services and other community resources in order to develop a network of support services for the waiver participant. The supervisor of the Peer Mentoring service is responsible for ensuring that this service is used appropriately and within the limits included in the service definition.
A waiver participant may receive this service as well as CIC or other mental health services as long as the need for more than one service is clearly documented in the service plan. This service is provided on an individual basis and specific goals must be established for the individual. Peer Mentoring will primarily be available to waiver participants who have recently transitioned into the community from a nursing home or as needed during times of crisis.
When available, Peer Mentors should participate in Team Meetings to discuss the waiver participant's progress.
This service does not duplicate other services available through the New York Medicaid State Plan.
Provider Qualifications
Peer Mentoring may be provided by any not-for-profit or for-profit health and human services agency. Persons providing Peer Mentoring must have:
- A disability or be a senior;
- Successfully demonstrated the ability to maintain a productive life in the community; and
- At least one (1) year of paid or unpaid experience providing peer mentoring or other equivalent experience working with seniors and/or people with disabilities.
Reimbursement
Peer Mentoring must be provided by a DOH approved provider and must be included in the service plan to be reimbursed. Rates are based on an Upstate/Downstate assignment based on where the services are provided.
Peer Mentoring is provided on an individual, face-to-face visit on an hourly basis. Participation in Team Meetings is reimbursed at the hourly rate for this service.
Positive Behavioral Interventions and Supports (PBIS) Respiratory Therapy
Definition
Positive Behavioral Interventions and Supports (PBIS) services are individually designed for waiver participants who have significant behavioral difficulties that jeopardize their ability to remain in the community. PBIS should be provided in the situation where the significant maladaptive behavior occurs.
PBIS services include but are not limited to:
- A comprehensive assessment of the individual's behavior, skills, and abilities, surrounding environment, network of informal and paid supports, family, and caregivers;
- The development and implementation of a holistic structured behavioral treatment plan (Detailed Plan) including specific realistic goals which can also be utilized by other providers and informal supports;
- The training of family, informal supports, and other providers so that they can also effectively use the basic principles of the behavioral plan;
- Regular reassessments and data collection of the effectiveness of the behavioral treatment plan; and
- Making adjustments to the plan as needed.
The comprehensive assessment of the individual's behavior is completed in the context of their medical diagnosis, abilities/disabilities, known reinforcers, antecedents of the behavior, and the environment in which the behavior occurs. The number of hours utilized to complete this assessment must be included in the service plan and may not exceed ten (10) hours. This assessment must be consistent with information contained within the UAS-NY assessment.
The participant must be present whenever PBIS services are provided, including training sessions and discussions with supports.
The primary goal of PBIS services is to decrease the intensity and/or frequency of the targeted behaviors and to teach safer and/or more socially appropriate behaviors. None of these activities shall fall within the scope of the practice of mental health counseling set forth in Article 163 of the NYS Education Law or invasive behavioral intervention.
The Detailed Plan must include a clear description of the targeted behavior(s), successive levels of intervention, starting with the most basic and least intrusive intervention. All plans must be written and presented using language that is easily understood and implemented by the staff, caregivers and informal supports surrounding the waiver participant. The plan must be consistent with the NYSDOH format. The provider must complete regular reassessments of the effectiveness of the Detailed Plan and modify the plan as needed.
Training of informal supports, waiver, and non-waiver service provider staff by the Behavior Specialist or PBIS Director will be provided to effectively use the basic principles of the behavioral plan. The number of training hours must be designated within the approved service plan in order to be reimbursed.
An emergency intervention plan is warranted when the waiver participant presents threatening or inappropriate behavior, which may be a threat to themself or others. This plan must be consistent with information presented in the Plan of Protective Oversight (PPO). The emergency intervention plan must be assessed on an ongoing basis and will be reviewed for efficacy at least every six (6) months at the Team Meeting, when significant changes in behavior occur or the medical status of the participant changes. Participation at the Team Meeting is used to garner information from the participant and informal supports about needed services and change(s) in physical and/or cognitive status. The Team Meeting will also include discussion about the individual's progress and any service changes that may be warranted. PBIS is a direct service to the participant.
Provider Qualifications
PBIS services may be provided by any not-for-profit or for-profit health and human services agency. The two key positions in PBIS service are the Program Director and the Behavioral Specialist.
The Program Director may perform the function of a Behavioral Specialist or supervise the Behavioral Specialist. The Behavioral Specialist may be responsible for the development and/or implementation of the Detailed Plan under the direction of the Program Director.
If a provider has more than one individual who meets the qualifications for Program Director, each of these qualified individuals can develop PBIS plans.
Any approved service provider with two (2) or more Behavioral Specialists must have a Program Director.
Persons employed as a PBIS Program Director must be a/an:
- Licensed Psychiatrist (Licensed by the NYS Education Department pursuant to Article 131 of the NYS Education Law);
- Licensed Psychologist (Licensed by the NYS Education Department pursuant to Article 153 of the NYS Education Law);
- Individual with a Doctorate or Master of Psychology;
- Licensed Master Social Worker (Licensed by the NYS Education Department pursuant to Article 154 of the NYS Education Law);
- Licensed Clinical Social Worker (Licensed by the NYS Education Department pursuant to Article 154 of the NYS Education Law);
- Master Level Certified Teacher of Students with Disabilities (Certified by the NYS Education Department);
- Licensed Behavior Analyst (Licensed by the NYS Education Department);
- Individual with a Master of Social Work; or
- Individual with a Master of Gerontology;
AND
Must have two (2) years of experience developing and implementing intensive behavioral plans.The Program Director is expected to meet any waiver participants prior to approving the behavior plan developed by a Behavior Specialist under their supervision, have supervisory meetings with staff on at least a monthly basis, and review and sign-off on all behavior plans. A supervisor may maintain an active caseload of waiver participants.
Provider Qualifications for Behavioral Specialists
The Behavioral Specialist is responsible for implementation of the Detailed Plan under the direction of the Program Director. The Behavioral Specialist must be a/an:
- Individual with a Bachelor's degree in psychology;
- Registered Professional Nurse (Registered by the NYS Education Department);
- Licensed Occupational Therapist (Licensed by the NYS Education Department);
- Licensed Physical Therapist (Licensed by the NYS Education Department);
- Certified Behavior Analyst Assistant (Certified by the NYS Education Department);
- Individual with a Bachelor's degree and a Certified TBI Specialist;
- Certified Rehabilitation Counselor (Certified by the Commission on Rehabilitation Counselor Certification);
- Individual with a Bachelor's degree and certified in Applied Behavioral Analysis (ABA);
- Individual with a Bachelor's degree and a Certified Dementia Practitioner; or
- Individual with a Bachelor's degree and a CARES Dementia Specialist;
AND
Must have two (2) years of experience developing and implementing intensive behavioral treatment plans.If there is only one Behavior Specialist employed by the provider, they must meet the qualifications of Program Director. The Program Director will provide ongoing training and supervision to the Behavioral Specialists.
PBIS staff must attend Team Meetings as needed. The provider cannot exceed the number of approved annual hours of service contained in the service plan. Regularly scheduled Team Meetings with the participant and service providers are an essential part of assuring the participant's health and welfare. This meeting is instrumental in the development and implementation of the service plan. Failure to attend Team Meetings may jeopardize the ability of the waiver provider to continue to provide waiver services. Participation at the Team Meeting is used to garner information from the participant and informal supports about needed services and change(s) in physical and/or cognitive status. The Team Meeting will also include discussion about the individual's progress and any service changes that may be warranted.
Any currently employed waiver provider staff who met the waiver application qualifications which were in place on the date of their hire are approved to continue to provide services. Approved employees may receive a certificate of qualification to provide services. The issued certificate will allow that staff member to continue providing the same waiver service(s) at both their current location of employment and/or any change they have in future employment locations/agencies. This certificate has no expiration date and only applies to the waiver service they were qualified for upon hire. Certificates may be terminated at the discretion of NYSDOH.
Reimbursement
Positive Behavioral Interventions and Supports services must be provided by a NYSDOH approved provider and must be included and approved in the service plan to be reimbursed. Rates are based on an Upstate/Downstate assignment based on where the services are provided or as assigned by DOH.
The number of hours utilized to complete the initial behavioral assessment must be included in the service plan and may not exceed ten (10) hours per service plan period. Hours are not provided to write the plan. PBIS is limited to two hundred forty (240) hours annually, not to exceed eight (8) hours per day.
This service is reimbursed on an hourly or partial unit basis.
Training hours cannot exceed ten (10) hours per service plan period and are contained in the approved number of annual service units a provider is authorized to deliver. The provider cannot exceed the number of approved annual hours of service contained in the service plan.
In all cases, service limits are soft limits that may be exceeded due to medical necessity. If the individual's needs cannot be met within the established limits, a participant may request to exceed the limit by providing sufficient medical justification to the RRDC. The RRDC will approve or deny the request for additional services.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Respiratory Therapy Services
Definition
Respiratory Therapy Services is an individually designed service, specifically provided in the home, intended to provide preventative, maintenance, and rehabilitative airway- related techniques and procedures.
Respiratory Therapy Services include:
- Application of medical gases, humidity, and aerosols;
- Intermittent positive pressure;
- Continuous artificial ventilation;
- Administration of drugs through inhalation and related airway management;
- Individual care; and
- Instruction administered to the waiver participant and natural supports.
The services provided cannot duplicate services offered through the New York Medicaid State Plan.
Provider Qualifications
Respiratory Therapy may be provided by a Certified Home Health Agency licensed under Article 36 of the New York Public Health Law or a provider of Respiratory Therapy and Equipment and approved as a provider of this waiver service by NYSDOH.
Respiratory Therapy services cannot be provided to a participant without a dated physician's written order which is obtained by the Respiratory Therapy agency. The Respiratory Therapy provider must obtain all physician's orders initially and every six (6) months thereafter and maintain them in the waiver participant's file at the agency according to existing regulations for Respiratory Therapy. Orders must contain amount, frequency, and duration of the service provided.
Staff providing Respiratory Therapy must be currently licensed as a Respiratory Therapist pursuant to Article 164 of the NYS Education Law.
Reimbursement
Respiratory Therapy must be provided by a NYSDOH approved provider and must be included in the approved service plan to be reimbursed. Rates are based on an Upstate/Downstate assignment based on where the services are provided.
Respiratory Therapy is provided on an individual, per visit basis.
Respiratory Therapy providers participating in Team Meetings will be reimbursed at the per visit rate for their time at the Team Meeting.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Respite Services
Definition
Respite Services are provided to participants unable to care for themselves that are furnished on a short-term basis because of the absence or need for relief of those persons who normally provide care for the participant. Respite Services are individually designed services intended to provide scheduled relief to informal, non-paid supports who provide primary care and support to a waiver participant. Respite Services are provided in a 24-hour block of time, not to exceed thirty (30) days per year. This is usually provided for participants who are in need of oversight and supervision as a discrete task. Participants approved to receive Respite Services do not necessarily need to be receiving HCSS, as the oversight and supervision is being provided by their informal/non-paid supports on a regular basis. However, receipt of Respite Services does not preclude a participant from receiving other services on the same day.
Providers of Respite Services must meet the same standards and qualifications as the direct care providers of Home and Community Support Services (HCSS). All HCSS/Respite Services are provided by Licensed Home Care Services Agencies (LHCSA) under Article 36 of NYS Public Health Law. All regulations governing the LHCSA are in effect for the provision of Respite services. The LHCSA providing Respite Services must be licensed in the county where services are provided. The type of care and services supported in the service plan are also to be included in the plan for Respite Services and will be reimbursed separately from Respite Services.
With sufficient justification in the service plan, receipt of Respite Services does not preclude a participant from receiving other services on the same day.
The primary location for the provision of this service is in the waiver participant's home, but Respite Services may also be provided in another non-congregate care community dwelling acceptable to the waiver participant.
Respite Services are documented in the service plan, approved by the RRDC prior to implementation, and provided by agencies approved as a provider of waiver services by NYSDOH.
Provider Qualifications
Providers of Respite Services must be approved to provide and meet the same standards and qualifications as Home and Community Support Services (HCSS).
The Respite provider must have a communication system available with twenty-four (24) hours/seven (7) days per week coverage to assure any issues regarding a participant's services can be addressed.
Section 12006(a) of the 21stCentury Cures Act (the Cures Act) requires that states implement EVV for all Medicaid PCS and HHCS requiring an in-home visit by a provider. As such, LHCSA Respite providers are required to implement an electronic visit verification system. The EVV system is required to capture the individual receiving the service and the date of service delivery.
Reimbursement
Respite Services must be provided by a NYSDOH approved provider of HCSS and included in the service plan to be reimbursed. Each service plan contains an approved number of annual service units a provider is authorized to deliver. The provider cannot exceed the number of approved annual hours of service contained in the approved service plan. It is anticipated that Respite Services may be needed during a time of emergency. The RRDC may approve services on an emergency basis with the expectation that an addendum to the service plan will be submitted to the RRDC within twenty-four (24) hours of the emergency approval.
Respite Services are provided in blocks of twenty-four (24) consecutive hours, not to exceed thirty (30) days per year, billed on a daily-rate basis. Since Respite Services is provided on an intermittent basis, the Service Coordinator must determine when participation in Team Meetings is appropriate. The provider must have a license for each county in which they are seeking to provide services. Rates are assigned based on the county where the services are provided.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Structured Day Program Services (SDP)
Definition
Structured Day Program (SDP) services are individually designed services provided to facilitate acquisition, retention, or improvement in self-help, socialization, and adaptive skills and takes place in a non-residential setting separate from the participant's private residence or other living arrangement.
Activities and environments are designed to foster the acquisition of skills, appropriate behavior, greater independence, and personal choice.
Structured Day Program services focus on enabling the participant to attain or maintain their maximum functional level and shall be coordinated with other services included in the service plan. In addition, structured day program services may serve to reinforce skills or lessons taught in other settings.
Services may include assessment, training, supervision, or assistance to an individual with self-care, task completion, communication skills, interpersonal skills, problem- solving skills, socialization, sensory/motor skills, mobility, community transportation skills, and the development of other coping strategies and skills. Unlike ILST services, SDP services are provided in a socialized group setting outside of the home. This service may only continue when the waiver participant has reasonable and attainable goals. It is used for training purposes and not ongoing long-term supports. Justification to provide or continue this service must be clearly stated in the service plan and approved by the RRDS.
SDP services may be used to reinforce aspects of other NHTD services and Medicaid State Plan services. This is addressed due to the difficulty many individuals have with transferring or generalizing skills learned in one setting to other settings and the need for consistent reinforcement of skills. The service plan should address how the services are complimentary but not duplicative and how this service is necessary to avoid institutionalization. This service is intended to provide an opportunity for the waiver participant to continue to strengthen skills that are necessary for greater independence, improved productivity and/or increased community inclusion.
SDP services may be provided within a variety of settings and with very different goals. However, SDP may not be provided in the participant's home. Waiver participants may choose to participate in a Structured Day Program that emphasizes basic work skills, such as punctuality, problem solving, and effectively communicating with co-workers and supervisors. Other Structured Day Programs may focus on specific job skills, such as computer operation or cooking. When employment is not an immediate or long-term goal, services may focus on socialization skills.
The Structured Day Program is responsible for providing appropriate and adequate space to meet the functional needs of the waiver participants served. The program must provide adequate safety protection for the program waiver participants, including fire drills twice a year and maintain documentation of those drills. The Structured Day Program must be located in a building that meets all provisions of the New York State Uniform Fire Prevention and Building Codes. In addition, access to the program must meet and adhere to the requirements of the Americans with Disabilities Act (ADA). NYSDOH recognizes that SDP services may focus on community-based activities integrated in the community at large. However, each program must have a physical location where services will be provided should the participant choose not to participate in outside activities. All waiver participants must begin and end their service day at the Structured Day Program location. The RRDC or NYSDOH may determine the appropriateness of the physical space for the NHTD waiver participants.
SDP staff must attend Team Meetings as needed. Team Meetings are participant- centered and not staff meetings or staff trainings. Regularly scheduled Team Meetings with the participant, family, informal supports, and service providers are an essential part of assuring the participant's health and welfare. This meeting is instrumental in the development and implementation of the service plan. Failure to attend Team Meetings may jeopardize the ability of the waiver provider to continue to provide waiver services. Participation at the Team Meeting is used to garner information from the participant and informal supports about needed services and change(s) in physical and/or cognitive status. The Team Meeting will also include discussion about the individual's progress and any service changes that may be warranted. It is a direct service to the participant and scheduled at least every six (6) months or when the needs or the condition of the participant warrant review and potential amendment to their service plan. Structured Day Program staff are required to submit ISRs in conjunction with the service plan review process and Team Meetings.
This service differs from adult day health care services available under the New York Medicaid State Plan in that services are not required to be provided under the direct order of a physician.
Provider Qualifications
Structured Day Programs may be provided by any not-for-profit or for-profit health and human services agency. All Structured Day Programs must be identified in the service plan and provided by agencies approved as a provider of this waiver service by NYSDOH.
Each day program must provide a site where participants can meet when arriving and departing from the day program. There must also be a site available where participants can receive services if they choose not to go out into the community. The program must provide adequate protection for waiver participants' safety and must be located in a building that meets all provisions of the NYS Uniform Fire Prevention and Building Codes. Access to the program must adhere to the requirements of the ADA. The RRDS and/or NYSDOH staff determine the appropriateness of the physical space for NHTD waiver participants by completing a site visit.
All SDPs must adhere to the Home and Community-Based Settings Requirements and cannot be located in, or adjacent to, an institutional/congregate care setting. The RRDC will complete a site visit to the program location to confirm compliance with the regulation. If the location fails to meet the criteria a plan to establish a new program site and/or other remediation activities will be developed. The setting must be fully integrated into the community and does not isolate participants from the community at- large. Guidance regarding Home and Community Based Services (HCBS) Rule requirements for SDPs can be found here.
All SDPs must also have a sign-in and sign-out policy in place which contains the following:
Sign-in/sign-out protocols should be reviewed with the participant at their six (6) month team meeting, as a change in service hours may be warranted.
- Each Structured Day Program must maintain a daily log to reflect participant attendance. This document must be maintained at the program site and it must contain the following information: date and time the participant arrived/departed from the Structured Day Program, and reason for departure if the participant leaves prior to assigned program hours (e.g., mid-day departure for lunch). All exit and re-entry must be documented.
- When participants arrive at the Structured Day Program, they are to be verbally prompted by staff to sign-in the date and time of arrival and signature on the sign-in and sign-out log. If help is required, staff should provide verbal assistance to ensure accurate date and time is recorded.
- At the end of the Structured Day Program session, participants are to be verbally prompted by staff to sign-out with the date and time of departure and signature on the sign-in and sign-out log. If help is required, staff should provide verbal assistance to ensure accurate date and time is recorded.
- If a participant leaves for any reason other than at the end of the Structured Day Program, staff should prompt the participant to sign-out on the sign-in and sign-out log, ensuring accurate date and time, and include reason for leaving. If the participant requires supervision, the Structured Day Program must continue to provide supervision until the participant is confirmed safe. A system for supervising the participant outside of the program site must be in place. If the participant returns to the Structured Day Program, staff must prompt the participant to sign back in on the sign-in and sign-out log, ensuring accurate date and time are entered. At the end of the week, the total number of hours each participant was on site for services should be noted. If it is suggested that the participant is not attending the number of Structured Day Program hours prescribed in their approved service plan, a review of the schedule and needed hours of service should be discussed at the Team Meeting and services should be also be reviewed with the participant's Service Coordinator. An amendment to the service plan may be required.
Note: In situations where the participant is unable to sign the log, Structured Day Program staff may complete this information for the participant; as such, the Structured Day Program Director or their designee must sign each entry to validate the information that the staff entered.- All attendance records must be maintained with participant files according to Medicaid requirements.
Each Structured Day Program must have a Program Director who must be a/an:
- Licensed Master Social Worker (Licensed by the NYS Education Department pursuant to Article 154 of the NYS Education Law);
- Licensed Clinical Social Worker (Licensed by the NYS Education Department pursuant to Article 154 of the NYS Education Law);
- Individual with a Doctorate or Master of Social Work;
- Individual with a Doctorate or Master of Psychology;
- Licensed Physical Therapist (Licensed by the NYS Education Department pursuant to Article 136 of the NYS Education Law);
- Registered Professional Nurse (Licensed by the NYS Education Department pursuant to Article 139 of the NYS Education Law);
- Certified Teacher of Students with Disabilities (Certified by the NYS Education Department);
- Certified Rehabilitation Counselor (Certified as a Certified Rehabilitation Counselor (CRC) by the Commission on Rehabilitation Counselor Certification);
- Licensed Speech Pathologist (Licensed by the NYS Education Department pursuant to Article 159 of the NYS Education Law);
- Licensed Occupational Therapist (Licensed by the NYS Education Department to Article 156 of the NYS Education Law); or
- Individual with a Master of Gerontology;
AND
Must have one (1) year of experience developing and implementing day habilitation plans; providing vocational education services; providing residential habilitation services; or providing job coaching or supportive employment services.
OR
Individual with a bachelor's degree and two (2) years of experience developing and implementing day habilitation plans; providing vocational education services; providing residential habilitation service; or providing job coaching or supportive employment services.The Structured Day Program must be available to provide hands-on assistance to participants receiving services. Therefore, the Program must have at least one (1) employee with previous training and current Personal Care Aide (PCA) or Certified Nursing Assistant (CNA) certification available to all participants while at the program location. While SDPs are required to have at least one (1) employee with valid certification as a PCA or CNA, this employee does not have to fall under the staff qualifications listed for the Program Director or program staff positions. The only required qualifications for this individual are previous training and a current certificate certifying the person as a PCA or CNA. In addition to a required Program Director and staff with PCA/CNA training, a Structured Day Program may employ additional program staff.
Persons employed as Program Staff must:
- Be at least eighteen (18) years old with a minimum of a High School Diploma or equivalent (i.e., GED);
- Be able to follow written and verbal instructions; and
- Have the ability, skills, training, and supervision necessary to meet the waiver participant's needs that will be addressed through this service to assure the health and welfare of the waiver participant.
Any currently employed waiver provider staff who met the waiver application qualifications which were in place on the date of their hire are approved to continue to provide services. Approved employees may receive a certificate of qualification to provide services. The issued certificate will allow that staff member to continue providing the same waiver service(s) at both their current location of employment and/or any change they have in future employment locations/agencies. This certificate has no expiration date and only applies to the waiver service they were qualified for upon hire. Certificates may be terminated at the discretion of NYSDOH.
Reimbursement
Structured Day Program services must be provided by a NYSDOH approved provider and must be included in the approved service plan to be reimbursed. Each service plan contains an approved number of annual service units a provider is authorized to deliver services. The provider cannot exceed the number of approved annual hours of service contained in the service plan. The SDP may only bill for those hours that the participant is physically in attendance and actively engaged in Structured Day Program services. For example, if a participant is approved for eight (8) hours of Structured Day Program services but is signed out for one (1) hour to go to lunch outside of the SDP, then that participant was only in attendance at the SDP for seven (7) hours and the SDP may only bill for those seven (7) hours that the participant was in attendance at the SDP. Attendance at the program should be consistent with the program schedule included in the service plan.
NOTE: The federal Home and Community Based Settings regulation establishes that all recipients of Medicaid Home and Community Based Services (HCBS) are afforded the opportunity to move freely throughout the program site and to enter and leave at their own discretion as long as it does not present a health and safety issue and/or disruption to services.
Structured Day Program services are reimbursed on an hourly basis and not to exceed ten (10) hours per day. Participation in Team Meetings organized by the Service Coordinator is reimbursed at the hourly rate and included in the total number of approved annual hours of service.
Structured Day Program rates are assigned based on the county in which the SDP site is physically located.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Transportation Services (Social Transportation)
Definition
Waiver transportation (Social Transportation) is offered as a direct service to waiver participants in order to enable individuals to gain access to identified community resources, other community services, and activities as specified in their service plan. This service is offered in addition to medical transportation required under CFR 431.53 and transportation services under the Medicaid State Plan, defined in 42 CFR 440.170(a) (if applicable), and shall not replace them. NHTD waiver transportation services include transportation only for non-medical activities which support the participant's integration into the community. All other options for transportation, such as informal supports and community services that provide this service without charge, are utilized prior to seeking this service. The least costly and most medically appropriate mode of transportation is utilized.
If there is an established need for transportation to and from non-medical services, activities or events, the waiver participant and the Service Coordinator must first explore the use of informal supports to provide the transportation without charge and the use of existing transportation. If these are not viable options, transportation may be included in the participant's service plan as a waiver service.
Waiver transportation services/locations are subject to NYSDOH prior approval. A description of required social transportation services is included in each participant's service plan. The RRDC approves the total number of annual units for trips and destinations as part of the service plan approval. The trip cost is derived from NYS approved Medicaid transportation rates and may be a calculation of a base rate, approved mileage, and other approved New York State costs. NYSDOH contracts with a transportation provider to arrange and provide services. The Transportation Manager will use the Transportation Grid coupled with Medicaid transportation policies to arrange travel as appropriate.
Transportation services are administered by a contracted Medicaid Transportation Manager. When a friend or family member is available to transport a waiver participant, this friend or family member should be used for social transportation. Within reason, the same mode of transportation used by the waiver participant for standard medical trips should be used for social trips. The most cost-effective method of transportation needs to be considered. The mode of transportation should support the needs of the participant identified in the service plan.
Waiver transportation is available to all persons enrolled in the waiver program where providers are available. A determination must be made by the appropriate prior authorization official prior to utilizing this service. Prior approval by NYSDOH and the RRDC must be obtained for all identified trips contained within the service plan. Transportation will only be available to a location that is identified in the service plan and/or the approved Transportation Service Request grid and is directly related to the functional needs and/or goals identified in the service plan. Each service plan should identify the common market area commutation. Travel outside the common marketing area can be allowed when acceptable justification is presented. The Service Coordination agency is ultimately responsible to ensure that the travel identified in a waiver participant's individualized service plan is an appropriate and judicious use of public funds. Reimbursement for travel can be denied when the prior authorization official determines that the destination does not support the participant's integration into the community. The RRDC approves the service and the service limits with the approval of the plan. The RRDC needs to maintain an open line of communication with the Transportation Contractor and Service Coordinator to discuss usage and appropriateness of the request. The prior authorization official can always request additional information from the Service Coordinator to assist with the decision to approve or disapprove the request for social transportation services.
The need for transportation must be documented in the service plan. Specific justification for trips must be included and the use of transportation services must be supported by goals in the service plan. Whenever possible, family members, neighbors, friends, or community agencies which can provide this service without charge will be utilized. A waiver participant's service plan outlines the general parameters of his or her social transportation needs. However, these needs can change or be amended based upon the waiver participant's stated goals and/or successful ongoing integration into the community.
Payment is not made for waiver transportation if the participant does not receive prior authorization for the transport. Prior authorization is obtained from the contracted Medicaid Transportation Manager and must be included in the service plan and approved by the RRDC.
All documentation is reviewed by the Service Coordinator prior to submission to the RRDC and Transportation Management Contractor.
Requests for service are submitted to the RRDC and upon approval by the RRDC, is forwarded to the Transportation Management Contractor.
The Service Coordinator, RRDC, and the Transportation Contractor are responsible for maintaining complete and current records related to the request and provision of waiver transportation services.
The duration of the service should be specified in the participant's service plan. Waiver transportation services may be used to help initiate a new activity or skill for a participant. An individual may also use transportation services for a reoccurring activity if it is detailed in their service plan; however, the time frame and frequency for using transportation in this capacity must be outlined. There must be an articulated frequency, start and endpoint for using waiver transportation services to achieve a specific goal. Once the specific goal is met, the service or that activity should be discontinued. If the participant has more than one goal in their service plan that includes the use of waiver transportation services, it is reasonable to expect a participant to complete their needs tied to each goal in the same location, if possible, on the same day during the week, on the same trip.
Guidelines for Approving Requests for Social Transportation
Waiver (social) transportation is available to all persons enrolled in the NHTD waiver program where providers are available as long as the need for the service is supported by the participant's service plan.
1. The prior authorization official (Regional Resource Development Center/RRDC) approves the waiver participant's service plan which identifies the need for social transportation services
A waiver participant's service plan outlines the general parameters of his or her social transportation needs. There must be specific goals in the waiver participant's service plan that identify the need for social transportation. The needs can change or be amended based on the waiver participant's stated goals. The goals must demonstrate and support the waiver participant's need for integration into the community. The RRDC should only approve a travel request when the travel meets the guidelines for approval and are consistent with the participant's goals contained in the service plan.
The RRDC can always request additional information from the Service Coordinator to assist with the decision to approve or disapprove social transportation reimbursement.
The Service Coordinator will complete the Transportation Grid based on the participant's service plan and provide it to the RRDC with the service plan. The Grid includes the following information:
- Participant information;
- Service Coordinator information;
- Medical Justification form submission;
- Waiver Transportation services requested;
- Trip destination/location;
- Start date and end date;
- Frequency; and
- Projected Trip cost.
The RRDC will use the Grid coupled with Medicaid transportation policies to approve travel as appropriate. The eMedNY Transportation Manual is available here. The Grid will be submitted to the Transportation Contractor/Manager, who may request additional information from the RRDC or Service Coordinator in order to effectuate the request. It is not required to submit a copy of the service plan with the transportation request. However, the Transportation Contractor may request additional information prior to approving the request.
Additionally, the cost projection for waiver transportation services will be reflected in the waiver services grid, located in the service plan, as a waiver service.
While a service plan may include a defined number of miles for a participant to travel during a given period of time, it is not the role of the RRDC to maintain a running tally of miles and cap the trips when the mileage has been reached. This is the role of the Service Coordinator.
The RRDC approves the service and the service limits (including waiver transportation) upon their approval of the service plan. The RRDC needs to maintain an open line of communication with the Transportation Contractor and Service Coordinator to discuss on-going usage and appropriateness of the request.
The Transportation Contractor is responsible for authorizing transportation services as approved by the RRDC in accordance with Medicaid policy and the approved service plan. This information is indicated on the Transportation Grid. A Verification Form is required to be on file with Transportation Manager for each waiver participant that requires Ambulette or a higher level of service. The Transportation Manager will notify the RRDC upon receipt and approval of the request. All questions regarding the request will be directed to the RRDC.
2. Use of personal transportation
Transportation must be tied to the goals in the service plan. Use of transportation to non-medical locations not typically covered for the Medicaid population may only be requested when such transportation is necessary to meet a goal identified in the participant's service plan.
The first consideration prior to seeking waiver transportation must be all informal supports, community services, and public transit. When friends or family members are available to transport a participant, the friends or family members should be used to provide transportation. The individual friend or family member's name must be listed in the service plan; the individual must maintain a current New York State driver's license in good standing and drive an insured vehicle registered and licensed by New York State. It is expected that local travel to family events can be performed by one's family.
Transportation should be provided in the most cost-effective way and using the appropriate mode of transport. This service is not intended to replace/duplicate other services provided by ACCES-VR or any other existing vendor/waiver service providers.
3. Use of the medically appropriate mode of transportation
Within reason, the same mode of transportation used by the waiver participant for standard medical trips should be used for social trips, and vice versa.
The most cost-effective means of transportation needs to be considered. The mode of transportation should support the needs of the participant identified in the service plan. The Department requires a medical justification form for any mode of transport above taxi in upstate NY and public transit in NYC.
4. Travel within the common marketing area
Trips to grocery or department stores, church, restaurants, etc., should be within the same area that is frequented by others in the same community as the waiver participant. Travel outside the common marketing area can be allowed when acceptable justification is presented.
Prior approval by the Medicaid transportation contractor is necessary and justification should be sufficient to support the request. Each service plan should identify the common market area commutation. There must be goals in the service plan which support a trip outside of the common marketing area.
5. Travel to similar destinations in a short time period can be questioned
It is reasonable to expect a waiver participant to travel to a grocery, department, office supply, electronics or other type of store and expect that all of their weekly shopping needs for that specific type of store can be completed at the same store. Travel to multiple similar type stores on the same day and/or during the same week can be questioned. Waiver transportation is to be used to support skill development. There must be an identified and measurable outcome to the waiver service.
It is not reasonable to expect that all shopping can be accomplished in the same location. However, trips must be planned in advance with expected outcomes of time, location, and appropriateness.
6. Where possible, trips should be combined
For example, travel to return empty bottles for the deposit should be made at the same time the participant travels to a grocery store for shopping, and/or where a grocery store operates a pharmacy within, the participant can also pick up their prescriptions while grocery shopping.
If the RRDS does not agree with the travel usage, the travel request should be denied.
The Service Coordination agency is ultimately responsible to ensure that the travel contained in a waiver participant's individualized service plan is an appropriate and judicious use of public funds.
The duration of the service should be specified in the participant's service plan. Social Transportation may be used to help initiate a new activity or skill for a participant. An individual may also use social transportation for a reoccurring activity if it is detailed in their service plan; however, the time frame and frequency for using transportation in this capacity must be outlined. There must be an articulated frequency and start and endpoint for using social transportation to achieve a specific goal. Once the specific goal is met, the service for that activity should be discontinued. If the participant has more than one goal in their service plan that includes the use of waiver transportation, it is reasonable to expect a participant to complete their needs tied to each goal in the same location, if possible, on the same day during the week.
Before a transport is provided to a waiver participant, the transportation provider verifies the person's eligibility for Medicaid on the date of service. Reimbursement is not made for services rendered to ineligible persons. The Service Coordinator and/or RRDC must consult the Transportation Management Contractor prior to requesting a trip. Trip cost is derived from using the NYS Fee Schedule.
The RRDS ultimately approves the travel as part of the service plan approval. As a result, the RRDS is providing prior authorization of the service in conjunction with the Transportation Contractor.
Record Keeping for the Service Coordinator
The Service Coordinator is responsible for maintaining complete and current records of the waiver transportation requested and provided. This includes dates of transportation, destination, cost, and reason for use of waiver transportation services.
7. Reimbursement for travel can be denied when the prior authorization official determines that the destination does not support the participant's integration into the community
Absent adequate justification, travel to destinations such as casinos, "smoke shops" on a Native American reservation, off-track betting parlors, adult entertainment businesses, hunting clubs, or bars will not be approved.
It is the choice of the waiver participant to travel to these destinations; however, other transportation supports in the community should be used. Medicaid funds cannot be used for these activities.
The participant, Service Coordinator, and the RRDS must exercise good judgment when requesting and approving transportation services. Examples of approved trips need to be included in the service plan and consideration must be given to the fact that the trip is funded with Medicaid dollars.
8. Any utilization of waiver transportation must be supported by the individual's goals in their service plan
Waiver transportation is an individualized service and should not be used for group trips, outings, and/or social events. Activities must be socially integrated and HCBS compliant.
For any participant who requires a mode of transport that exceeds ambulette, a Form 2015 must be completed.
Services provided through Waiver transportation exceed New York Medicaid State Plan transportation.
Provider Qualifications
Transportation services can be provided by a NYSDOH approved Common Carrier and specialized transportation providers. To participate in the New York State Medicaid Program, a provider must meet all applicable state, county, and municipal requirements for legal operation. Department regulation at Title 18 of the New York Code of Rules and Regulations (NYCRR) Section 505.10, which applies to Medicaid transportation services, can be found here. Title 18 NYCRR §505.10(e)(6) indicates that providers must, regardless of Medicaid enrollment status, comply with applicable regulatory requirements. For ambulette, taxi, and livery companies, this may include local licensure by a municipality or a Taxi and Limousine Commission.
Reimbursement
Before transportation is provided to a waiver participant, the transportation provider verifies the person's eligibility for Medicaid on the date of service. Reimbursement is not made for services rendered to ineligible persons. The Service Coordinator and/or RRDC must consult the Transportation Management Contractor prior to requesting a trip. Trip costs are derived from using the NYS Fee Schedule.
Reimbursement for travel is denied when the prior authorization official determines that the destination does not support the participant's integration into the community and is not reflected in the service plan.
Transportation providers will only be reimbursed when acceptable records verifying a trip's occurrence are complete and available to auditors upon request. All payments are made through eMedNY as authorized by the Medicaid Transportation Contractor.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Wellness Counseling Service
Definition
Wellness Counseling Service is an individually designed service intended to assist the medically stable waiver participant in maintaining an optimal health status. It is intended to be available to a waiver participant who does not otherwise have access to nursing services. Through Wellness Counseling, a Registered Professional Nurse assists the waiver participant to identify their health care needs and provides guidance to the waiver participant to minimize, or in some cases, prevent acute episodes of disease and utilize health care resources efficiently and effectively. This service differs from Medicaid (MA) State Plan Nursing Service as wellness counseling is provided as a discrete service to medically stable individuals.
Through Wellness Counseling, a Registered Professional Nurse (RN) can reinforce or teach healthy habits such as the need for daily exercise, weight control, or avoidance of smoking. Additionally, the RN will be able to offer support for control of diseases or disorders such as high blood pressure, diabetes, morbid obesity, asthma, or high cholesterol.
In addition to these services, the Registered Professional Nurse can assist the waiver participant to identify signs and symptoms that may require intervention to prevent further complications from the disease or disorder. If potential complications are identified, the RN will counsel the waiver participant about appropriate interventions including the need for immediate medical attention or contact the waiver participant's physician for referral to traditional Medicaid State Plan services.
Wellness Counseling Service will be limited to no more than twelve (12) visits in a calendar year and will occur on an as needed basis.
This service does not duplicate other services available through the New York Medicaid State Plan.
Provider Qualifications
Wellness Counseling Service must be provided by a Certified Home Health Agency (CHHA) or a Licensed Home Care Service Agency (LHCSA). Staff providing Wellness Counseling Service must be a Registered Professional Nurse licensed by the NYS Education Department pursuant to Article 139 of the NYS Educational Law. All regulations governing the LHCSA will be in effect for the provision of this service.
Wellness Counseling Service cannot be provided to a participant without a dated physician's written order, which is obtained by the Wellness Counseling Service agency initially, and every six (6) months thereafter. Orders must contain amount, frequency and duration of the service provided. The Wellness Counseling Service provider must obtain and maintain all physician orders in the waiver participant's file at the agency.
Reimbursement
Wellness Counseling Service must be provided by a DOH approved provider and be included in the service plan to be reimbursed. Rates are assigned upstate/downstate based on the county where the services are provided.
Wellness Counseling Service is provided on an individual, per visit basis. It is limited to no more than twelve (12) visits in a calendar year and will occur on an as needed basis as prescribed by a physician.
Wellness Counseling Service providers participating in Team Meetings will be reimbursed at the per visit rate for their time at the Team Meeting.
All NHTD waiver service providers are responsible for keeping records sufficient to substantiate all Medicaid claims. Providers are audited on the accuracy and validity of such records to ensure that claim amounts are accurate and valid.
Section VII: Record Keeping
Introduction
All Nursing Home Transition and Diversion Waiver Service providers are responsible for maintaining records sufficient to substantiate all Medicaid claims.
NYCRR Title 10 section 405.10 (a) (4), establishes that providers must maintain appropriate financial records to support utilization of available resources, receipt of Medicaid funds, and confirmation of all Medicaid funds received. Such records must be readily accessible to authorized officials for audit purposes. In addition to financial records, providers must identify an office location where participant files are maintained for survey and audit purposes. Providers are audited on the accuracy and validity of such records to ensure that all submitted claims are accurate, valid, and consistent with Medicaid billing policy.
Federal law and State regulations require all Medicaid providers to maintain records necessary to fully disclose the extent of services, care, and supplies provided to Medicaid enrollees. As stated in Section 504.3, Title 18 of the New York Codes, Rules and Regulations: "By enrolling the provider agrees: (a) To prepare and maintain contemporaneous records demonstrating its right to receive payment under the Medicaid program and to keep for a period of six years from the date the care, services or supplies were furnished, all records necessary to disclose the nature and extent of services furnished and all information regarding claims for payment submitted by, or on behalf of, the provider and to furnish such records and information, upon request".
All applicant/participant records must be maintained for the entire period that an applicant/participant is actively receiving waiver services. The records shall be legible, accurately written, complete, properly filed, retained and accessible in a manner that does not compromise the security and confidentiality of the records. Upon termination of waiver services records will be available to authorized Medicaid officials for six (6) years following the date of the waiver participant's termination from waiver services. Failure to meet these requirements may affect payment and may jeopardize a provider's eligibility to continue as a Medicaid provider.
Third party documents such as financial or medical records received by service providers, NYSDOH and its authorized representatives on behalf of an applicant/participant will not be released to anyone other than the applicant/participant/legal guardian. All requests should be made directly to the originator of the document/report. Investigation reports and supporting documents are not maintained in the participant record and are not subject to release. A summary of information may be provided at the request of the applicant/participant/complainant.
Each waiver service provider and contractor are responsible for the storage and maintenance of applicant/participant records. Records must be stored in a secure location which maintains the physical integrity of the records in addition to safeguarding the records from the potential for environmental damage. Should an unexpected event occur in which records are damaged, the provider/contractor must immediately notify
NYSDOH and/or the RRDC and take the necessary actions to salvage the damaged records. Actions at a minimum should include: relocating the records to a safe environment, contacting a restoration company, and taking appropriate steps to remediate the problem to prevent additional damage. Providers are responsible to maintain documentation and evidence of any documents that have been lost due to an unexpected event. In the event of an audit by the Office of the Medicaid Inspector General (OMIG), OMIG will evaluate, on a case-by-case basis, whether there are mitigating circumstances for all missing or damaged documents.
Medicaid providers agree, as a condition of continued enrollment, to notify the Department of Health (NYSDOH) immediately of any changes supplied in the provider's enrollment agreement, including a change in service location and/or ownership. To keep the enrollment agreement up-to-date, providers must use the maintenance forms found on the Provider Enrollment tab here.
The New York State Medicaid Management Information System (MMIS), Electronic Medicaid System of New York (eMedNY) system is a computerized system for claims processing. Claims for all HCBS waiver services are adjudicated by eMedNY. The eMedNY system identifies HCBS enrollees with codes (Restriction/Exception (R/E) codes) that identify the person as HCBS enrolled and the effective date of the enrollment. Payment system edits require the client record to indicate active Medicaid eligibility and HCBS Waiver enrollment for all dates of service billed. All billings are processed either through eMedNY or through direct payment to the transportation contractors through the NYSDOH contracted transportation system.
It is highly recommended that all Medicaid providers conduct an annual self-assessment of their compliance programs and record keeping to maximize a provider's opportunity to make improvements, corrections or refinements to their record keeping and business systems. All providers must comply with compliance standards established by the Office of the Medicaid Inspector General (OMIG).
Electronic medical records and ordering systems are accepted by CMS if documentation received is otherwise in compliance with CMS record keeping requirements. With electronic systems, CMS may request a copy of a protocol, policy or procedure that describes how electronic health records are signed and dated in order to verify that the documentation has been electronically signed by the ordering/treating professional. Providers need a system and software products that are protected against modification. Providers that maintain electronic records must have the ability to produce electronic records in a paper format within a reasonable time, upon request of the RRDC, NYSDOH, and audit authorities.
Each waiver provider is assigned a provider identification number in eMedNY, which is dedicated solely to the NHTD waiver and ensures only enrolled waiver providers can bill for services. Each waiver service is assigned a unique rate code.
Providers must verify a participant's Medicaid eligibility prior to provision of services and obtain prior authorization for specific services. A participant must present an official Common Benefit Identification Card (CBIC) to the provider when requesting services. The issuance of an Identification Card does not constitute full authorization for provision of medical services and supplies. The participant's eligibility must be verified through eMedNY to confirm the participant's eligibility for services and supplies. A provider not verifying eligibility prior to provision of services will risk the possibility of nonpayment for those services.
Authorized state and federal agencies, and their authorized representatives, may audit or examine provider records. This examination includes all records the agency finds necessary to determine if services were provided in accordance to program guidelines and NYSDOH policy. This requirement applies to the provider's records and records for which the provider is the custodian.
A separate case record must be maintained for each participant served and for whom reimbursement is claimed.
All waiver service providers must maintain policies and procedures that assure the appropriate safeguarding of all records containing any identifiable information regarding waiver applicants and participants. These policies and procedures must be disseminated to all staff.
The policy must include, but is not limited to:
- Maintaining records in a secured environment (e.g., locked files or locked room) when they are not in use;
- Preventing exposure of information when records are in use;
- Identifying all information transmitted from one location to another as "confidential" in an appropriately secured manner;
- Obtaining prior authorization from the appropriate supervisory staff before taking records outside of the agency, and the return of records within one (1) business day;
- Properly informing applicants/participants of record collection procedures, access, utilization, and dissemination of information;
- Specifying procedures related to employee access to information; and
- Specifying the disciplinary actions for violations of confidentiality statutes, regulations, and policies.
Accurate and up-to-date record keeping is required of all Medicaid providers to substantiate Medicaid billing. The need to maintain the necessary records is described in the Provider Agreement, the eMedNY Provider Manual, and in this Program Manual. The waiver service provider is responsible for having clear and accurate documentation to support all Medicaid claims.
Waiver service providers must adhere to all Medicaid confidentiality and Health Information Portability and Accountability Act (HIPAA) requirements and ensure the privacy of the waiver participant.
In the case of the NHTD waiver program, all waiver service providers must maintain waiver participant records for at least six (6) years from the effective date of the termination of their MMIS Provider ID. These records must be available upon audit, request, and/or investigation.
A waiver service provider must also maintain other pertinent records associated with service delivery, including, but not limited to:
- Employment and personnel records which show staff qualifications, and time worked;
- Statistical records of services provided;
- Any other records required as a result of any agreements with either the Department of Health or a local social services district office; and
- Referrals, provider selection forms, sub-contractor, and provider agreements
If a waiver service provider has more than one office and the personnel files are housed in the main office when the other office(s) is/are surveyed by the New York State Department of Health (NYSDOH) or other audit authorities, the personnel files must be provided to the surveyor(s)/auditor(s) at the location where the review is being conducted.
Record keeping is required both for clinical reasons and documentation of the expenditures of Medicaid funds.
Clinically structured record keeping assists the waiver service provider in documenting the participant's desired goals and the accomplishment of these goals. The participant and waiver service provider work together to develop a provider-specific Detailed Plan that reflects the participant's goals, identifies strategies for intervention, and reviews the effectiveness of these interventions. This provides a better understanding of whether the goals have been met and when interventions and/or goals need to be revised.
Record Keeping Components
The Initial Waiver Application Packet Includes:
- Waiver Initiative Form (2018);
- Application for Participation;
- Freedom of Choice Form;
- Applicant Interview Acknowledgment (2009);
- Instructions for the Complaint Process (2019);
- Intake and Referral Form (2018) (2019);
- List of available Service Coordination Agencies provided to the applicant at intake;
- Service Coordination Agency Selection Form(s) (2009) (2018); and
- Release of Information form.
Eligibility
- Proof that the applicant is over the age of 18 upon application;
- If between 18-64 upon application, medical verification of a physical disability as a primary diagnosis;
- Verification of Medicaid, appropriate for community-based services;
- Proof of Level of Care: UAS-NY (required after 2013) (if Transition, completed within 90 days of enrollment with a PRI/SCREEN);
- Initial PRI Completion date (if NH/hospital transition or admitted prior to 2013);
- Provider Selection Form(s);
- Plan of Protective Oversight;
- Participant Rights and Responsibilities;
- Waiver Services Contact List; and
- Proof of receipt of Complaint Process protocols (2019).
Service Plan
- All necessary functional assessments and related detailed plans and Individual Service Reports (ISRs);
- The Service Plan Cover Sheet and Signature page;
- Proposed Schedule;
- Transportation grid, if a requested service;
- Team Meeting Summary (effective 3/2009) (revised 2018);
- Documentation of Eligibility; and
- Date of NOD (eligible/non-eligible).
Waiver service providers of Assistive Technology (AT), Community Transitional Services (CTS), Congregate and Home Delivered Meals, Environmental Modifications Services (E-mods), and Moving Assistance are considered as "non-direct" waiver service providers and, as such, are exempt from certain components of record keeping, but are required to maintain other types of documentation (refer to "Record Keeping for Specific Waiver Service Providers" later in this section). However, all NHTD waiver service providers are responsible for keeping records sufficient to substantiate any Medicaid claims. This would include initial and final cost forms and related assessments. These providers are audited on accuracy and validity of such records, to ensure that claim amounts are accurate and valid.
Waiver transportation is offered as a direct service through Medicaid contracted providers for waiver participants to enable individuals to gain access to identified community resources, community services, and specific activities identified in their service plan. Waiver Transportation supplements transportation provided by the Medicaid State Plan. It includes transportation for non-medical activities which support the waiver participant's integration into the community. Services must have prior approval using the transportation request form.
1. Detailed Plans
All direct waiver service providers must develop a Detailed Plan for each waiver participant it is serving. The Detailed Plan identifies the participant's goals for each waiver service and describes the interventions to be provided to assist the participant to achieve their goals. The Detailed Plan is an essential component of a participant's efforts to remain in their community of choice.
The development of the Detailed Plan begins with the waiver service provider interviewing the participant to establish the specific goals they want to achieve through this service. Once these goals are established, information must be obtained regarding the participant's current level of functioning. Information regarding the participant's current level of functioning should be garnered from the UAS-NY and other current clinical/medical assessments available in the participant's file that supported the participant's waiver eligibility. The provider will also obtain information regarding the participant's current level of functioning through discussions between the waiver service provider, the participant, informal supports, other treating professionals, and significant others involved with the participant. If the individual has been in a facility or has been receiving services in the community, it is essential to obtain any formal assessments that have been completed, including discharge summaries. This may require discussions with staff from nursing homes, hospitals, certified home health agencies, and licensed home care service agencies. The method for gathering baseline information may vary according to the particular waiver service. The waiver service provider is responsible for completing a thorough evaluation of the participant's basic skills and abilities related to their selected goals. The methods and techniques identified in the detailed plan must be consistent with the participants skills, abilities and needs and support the overall goals of the person-centered service plan.
Even after the Detailed Plan is developed, there must be an ongoing process in which waiver service providers must objectively and consistently review the Plan's goals with the participant and document progress. This allows the waiver service provider to fully and accurately evaluate the participant's strengths and weaknesses, address any areas of concern, and make needed revisions to the Detailed Plan. Each Detailed Plan must contain: the date of the plan, desired goals, outcomes and milestones, methods and/or interventions implemented, risks or challenges which may impede goal attainment, projected timeframes, and signature(s) of the participant and/or guardian. The Detailed Plan must be reviewed at least every six (6) months. Documentation of this review must be in the participant's record, but the Plan does not need to be re-written unless there is/are significant change(s) in the participant's condition and/or goals.
All activities and goals in the Detailed Plan must support the goals and objectives indicated in the participant's service plan and address the choices and wishes of the participant.
The Detailed Plan should include three components:
- Milestones/Progress Indicators
Milestones are defined as component, intermediate steps that must be accomplished to achieve a larger goal. Goals should be realistic, attainable and in the best interest of the participant. For example, a participant's goal is to resume participation in preparing meals for their family. A milestone would be established through the planning, preparing, and serving of dinner for three consecutive days. Milestones may indicate the sequential steps necessary to attain the goal.- Interventions/Methods and Techniques
Once milestones are established, the waiver service provider determines what interventions/techniques will assist the participant to achieve the milestones and, eventually, the selected goal. A thorough understanding of the participant's unique strengths, deficits, interests, and abilities will help guide the waiver service provider in the development of interventions. For example, ILST would work with the participant on the steps needed to plan a meal. This would include creating a menu, making a shopping list for items needed to make the meal, and purchasing needed items.- Timeframes
Timeframes include the frequency and length of the interventions and how long the participant and waiver service provider expect it will take for the participant to achieve the selected goal. Setting realistic timeframes is essential to determine the success of an intervention and the stated goal. Equally important is assisting a participant to recognize that a particular goal may not be attainable, but that the outcome of the goal can be accomplished through another means. For example, if a participant is not successful in achieving the milestone of planning and preparing one meal within the designated timeframe then a re-evaluation of the milestone, interventions and/or timeframe must occur. This includes determining what other means can be utilized to help the participant accomplish the goal of participating in meals with his/her family. If a participant is unable to attain success within the timeframes identified in the plan, documentation must be provided to support why the milestone/service should remain in place and what elements impeded the participant's success.2. Documentation of Encounters/Case Notes/Service Notes/Progress Notes
The waiver service provider must maintain documentation of each face-to-face encounter with the participant, for reimbursement. This documentation should provide a measure of how effective the service has been in supporting the participant in meeting their goals. It should contain a clear description of the staff's action, a description of the techniques employed in the service delivery, the participant's response to that action, and progress toward the goals/milestone. All professional and direct care staff must document the service encounter. Documentation of this encounter must include:
- The waiver service provider agency's name;
- The name of the waiver service provider staff conducting the encounter;
- The date of the encounter;
- The location of the encounter;
- The time and duration of the encounter; and
- A description of the service(s) provided that is/are related to the goal(s) established in the Detailed Plan.
The frequency and duration of the service also requires review. If a participant fails to actively participate in a waiver service, the plan should address if continued service is required and the reasons why participation did not occur as approved.
In the case of Structured Day Program services, providers are required to maintain an additional sign-in and sign-out log which must be used to document the time spent on location. When a participant enters or leaves the Structured Day Program, they must sign in or out as appropriate. The sign-in and sign-out log must be signed and written by the participant. Staff may provide assistance when necessary. The total hours of participation must be evaluated in comparison to the total hours of approved service. If it does not appear that the participant requires the approved hours of service due to departures from the program, then an addendum to the service plan may be warranted. For more information on this sign-in and sign-out policy, refer to Structured Day Program Services in Section VI - Waiver Services of this program manual.
This information must be recorded as soon as possible after each contact and reviewed for completeness each month. In addition to documenting encounters, waiver service providers must keep case notes which reflect:
- Communication with participants' family, friends, waiver and non-waiver providers;
- Health and welfare issues follow-up; and
- Concerns expressed by the participant or others and the actions taken to address them.
All waiver service providers are responsible for maintaining open communication with other providers serving the same participant when concerns or changes in condition of the participant potentially affect the overall care and provision of services. Each waiver service provider must be respectful of the participant's right to privacy and confidentiality regarding the sharing of information and have policies and procedures in place that support these rights.
All submission of claims for reimbursement must match the information included in the waiver service provider's documentation of encounters/case notes/service notes/progress notes. The number of service hours billed must be consistent with the hours of service documented.
Any health and welfare issues or concerns expressed by the participant, or someone on their behalf, must be documented by professional and direct care staff, including notification to the appropriate supervisor. The supervisor must maintain documentation of any issues referred to and the follow-up actions taken. The supervisor will also evaluate the effectiveness of services in meeting the participant's goals at each service plan review period.
Electronic Visit Verification Requirements Specific to HCSS Providers
New York Medicaid is required by federal law to implement an Electronic Visit Verification (EVV) system for certain home and community-based services. The law, referred to as the 21st Century Cures Act can be found in Public Law 114-255, Section 12006(a)(4)(B). The goals of EVV are to ensure timely service delivery for members, including real-time service gap reporting and monitoring, to reduce the administrative burden associated with paper timesheet processing, and generate cost savings from the prevention of fraud, waste, and abuse. Under this regulation, within the NHTD waiver, providers of Home and Community Support Services (HCSS) must implement an EVV system for the provision and oversight of EVV services.
EVV is an electronic system that verifies when provider visits occur and captures:
- The date and time of the visit;
- The location of the visit;
- The person who received the services;
- The person who provided the services; and
- The services provided.
In most cases, a signature or voice verification from the individual receiving the services can also be captured.
For more information on the New York State Department of Health's (NYSDOH's) EVV policy, please go here.
3. Individual Service Reports (ISR)
The ISR provides an opportunity for the waiver service provider to describe its activities during the period of the service plan and describes the participant's future goals and continued need for the service. As such, an ISR is not submitted for the first Team Meeting completed after the approval of the Initial Service Plan (ISP) or Revised Service Plan (RSP). All subsequent Team Meetings will include review of ISRs and will be amended as needed. A new ISR must be completed with the annual review of the service plan. Copies will be included in the service plan packet submitted to the RRDC for approval of the service plan (subsequent Team Meetings are held every six months after the first team meeting). Unless there is a significant change in the participant's condition or goals, no additional ISRs or Team Meetings are required until the approval of the next service plan. RSPs are submitted sixty (60) days prior to the end of the service plan period.
The ISRs will support the goals of the Service Plan. The ISR includes information provided by the participant, informal supports, and any assessments completed during the plan period. The Service Coordinator must clearly describe the anticipated costs and need for each of these services in the service plan. Failure to provide a timely ISR may result in administrative action against the waiver service provider and/or Service Coordinator, such as restricting a waiver service provider's opportunity level or Disenrollment (refer to Section V - The Service Plan of this Program Manual and Section III of the Program Manual for information on restricting a waiver service provider's opportunity level).
The following waiver service providers are required to submit ISR(s):
- Community Integration Counseling (CIC);
- Home and Community Support Services (HCSS);
- Home Visits by Medical Personnel;
- Independent Living Skills Training Services (ILST);
- Nutritional Counseling/Educational Services;
- Peer Mentoring;
- Positive Behavioral Interventions and Supports Services (PBIS);
- Respiratory Therapy Services;
- Respite Services;
- Service Coordination (SC);
- Structured Day Program Services; and
- Wellness Counseling Services.
The ISR is directly related to the Detailed Plan and ongoing documentation of encounters with the participant. The Detailed Plan sets the overall design of the interventions/methods/techniques to be implemented. The notes and encounter data regarding interactions and participant performance provide the information necessary to complete the ISR.
The ISR documents the progress of the participant in relation to the identified goals and services provided and describes the need for the continuation of the service or supports the decision to discontinue the service. Inclusion of this information in the service plan supports authorization for continued services. The completion of the ISR involves a thorough review of the Detailed Plan, a discussion of the participant's goals and accomplishments during the review period, and supports the overall goals included in the service plan.
To justify re-approval/continuation of a service, the ISR must clearly describe why the continuation of this service is warranted and supports the provision of services in the community as an alternative to institutional care.
The ISR must identify responses to the following questions:
- What goals presented in the current service plan support the information provided in the ISR?
- What interventions/methods/techniques were used to address goals?
- Is the frequency and duration of the service sufficient to meet the needs of the participant and support the service plan goals?
- What documented progress has been made towards the goals?
- Were there any barriers to service provision that impact the participant's progress and what steps were implemented to overcome the impediment?
- Do the current goals require amendment and what are the expected outcomes for the next service plan period?
- Is the frequency and duration of this service sufficient to meet the needs of the participant? If not, why? What are the recommended hours and duration of the service?
- How does the provision of this service support the health and welfare of the participant and avoid institutionalization?
- What recommendations need to be addressed in the next service plan?
Providers of the following waiver services are not required to complete an ISR for these services:
- Assistive Technology (AT);
- Community Transitional Services (CTS);
- Congregate and Home Delivered Meals;
- Environmental Modifications Services (E-mods);
- Vehicle Modifications; and
- Moving Assistance.
Record Keeping for Specific Waiver Service Providers
- Requirements for Service Coordinators
The Service Coordinator shall maintain a file for each participant that includes:
- The Application Packet, including the Initial Service Plan (ISP) (DOH-5726);
- The original and all subsequent UAS-NY Outcome reports, (and PRI, if the participant transitioned from a nursing facility);
- All RSP(s), including all required documentation and ISR(s) submitted from other waiver service providers;
- All functional assessments and related medical documentation (physician's orders) completed to support requested services in the service plan;
- All Addendums;
- All copies of Notices of Decision (NODs) forms provided to the participant, with documentation that the participant has received the NOD and been informed about their right to a Case Conference and/or Fair Hearing;
- If waiver transportation is requested: required documentation as established in the service guidelines;
- Documentation of Case Conference and Fair Hearing actions when requested by an applicant/participant;
- Summaries of all Team Meetings;
- Initial and annual Waiver Participant's Rights and Responsibilities form (DOH5732) with the original signature and date;
NOTE: The Waiver Participant's Rights and Responsibilities form must be signed and dated by the applicant/participant. The original document is included in the Application Packet. A copy is given to the participant to be maintained in an accessible location in the individual's home. The document is reviewed with them on an annual basis.- Annual review with participant regarding Abuse and Neglect reporting through the SRI process;
- Annual review with participant regarding the NHTD complaint process and review of the NHTD Instructions for the Complaint Process (DOH-5729);
- Current Waiver Contact List;
- All Plans for Protective Oversight (PPOs);
- Documentation of proof of the participant's current Medicaid eligibility each time the service plan is submitted to the RRDS;
- Documentation of Release of Information forms;
- Documentation of the provision of Service Coordination services; and
- Documentation of all other contacts and attempted contacts with:
- The participant and/or Legal Guardian;
- Family and informal supports;
- Local Departments of Social Services (LDSS);
- Providers of waiver services;
- Providers of non-waiver services;
- Regional Resource Development Center (RRDC) staff;
- DOH waiver staff;
- Any other significant contacts which affect the service plan and/or reflect a change in the participant's situation; and
- Any housing documents that are related to the NHTD/Olmstead Housing Subsidy Programs.
In addition, providers of Service Coordination must maintain the following separate from the participant's record:
- Documentation of any complaints or grievances and subsequent investigations generated as an outcome of these situations; and
- Documentation reflecting any involvement in the Serious Reportable and Recordable Incident processes.
Serious Reportable Incidents (SRIs) and related investigations are not considered part of the participant record and therefore are not subject to distribution. Copies of incident reports and subsequent investigations will not be released and are treated as confidential. Summary of the investigation process and related findings may be provided upon request by participants and their guardians.
NOTE: A copy of the full eligibility package must be maintained by all current and previous Service Coordination providers. A copy of the Application Packet must be obtained from the previous Service Coordination agency or the RRDC and be maintained by the current Service Coordination agency in the participant's record. The Service Coordinator is responsible for maintaining information that has been obtained and/or written since approved by the RRDC as the assigned provider.
The Service Coordinator is responsible for distributing approved service plans to all waiver service providers and ensuring that each waiver service provider receives all participant information relevant to the delivery of services to their assigned participant.
- Assistive Technology (AT), Community Transitional Services (CTS), Congregate and Home Delivered Meals, Environmental Modifications Services (E-mods), and Moving Assistance providers may maintain an "abridged" participant file specific to the service provided.
These "non-direct" waiver service providers are responsible for maintaining the following in the participant's record:
- Provider Selection form (DOH-5730);
- Copy of the service plan cover page and the pages regarding the need for the waiver service they are approved to provide;
- A copy of the participant's Notice of Decision (NOD) (DOH-5740) for waiver eligibility and service approval;
- A copy of the Participant's Rights and Responsibilities form for the current year, as applicable;
- A description of all services provided and related approvals by the RRDC;
- All functional assessments and evaluations necessary to provide the requested services including, but not limited to, physician's orders and prescriptions;
- Any bids required to provide the approved service and related supporting documentation, such as receipts and service evaluations and assessments;
- Release of Information forms; and
- Documentation of all contacts or attempted contacts (through an encounter, or verbal/written communication) with:
- The participant and/or legal guardian;
- Family and informal supports;
- Providers of State Plan, non-waiver and waiver services;
- RRDC; and
- Any other significant contacts related to the delivery of services in the approved service plan or change in circumstance impacting the delivery of those services in a timely manner.
In addition, these waiver service providers must maintain the following documentation separate from the participant's record:
- Documentation of any complaints or grievances and subsequent investigations generated as an outcome of their service delivery; and
- Documentation reflecting any direct involvement in the reporting and/or investigation of Serious Reportable and Recordable Incidents.
- Requirements for All Other Waiver Service Providers
All other "direct" waiver Service Providers are required to maintain a complete participant file:
- ISP (Initial Service Plan);
- All RSP(s) Revised Service Plans;
- All Addendum(s), if applicable;
- All copies of Notices of Decision (NOD) forms sent from the Service Coordinator;
- Documentation of all Team Meetings attended and a copy of the completed Team Meeting Summary received from the Service Coordinator;
- Initial and annual, as applicable, Participant's Rights and Responsibilities form;
- Current Waiver Contact List;
- All Plan for Protective Oversight (PPO) forms received during provision of service(s);
- Release of Information forms, as appropriate;
- Documentation of the provision of services;
- Documentation of all other contacts and attempted contacts with:
- The participant and/or legal guardian;
- Family and informal supports;
- Local Departments of Social Services;
- Other providers of waiver services;
- Providers of state plan and non-waiver services;
- RRDC staff;
- NYSDOH; and
- Any other significant contacts that affect the participant and related goals in the Service Plan and/or reflect a change in the participant's health, welfare or living situation;
- Service-specific assessments conducted or acquired, if applicable; and
- Signed and dated physician orders necessary for service provision.
Not included in the participant record:
- Any documentation of complaints or grievances and subsequent investigations generated as an outcome of these situations; and
- All supporting documentation related to the investigation such as staff statements, medical reports, case notes.
A standard investigation format is used by all providers. The format contains a series of questions/issues that must be addressed in the report. The RRDC reviews the report and the supporting document to determine if the investigation process has been sufficient. If the RRDC has a question about the substance of the investigation it will refer the report to NYSDOH for review and guidance. The RRDC returns the investigation report to the provider, requesting additional clarification or information. The investigation is not closed until the RRDC determines it is closed.
Each approved NHTD waiver provider must submit a report detailing its SRIs on a quarterly basis. These reports are submitted to the RRDC for inclusion in a regional report. The regional summary is then submitted to NYSDOH for review and compilation of statewide data and trend analysis.
Each agency's SIRC must submit an annual report to the RRDC regarding Serious and Recordable Incidents, corrective, preventive and/or disciplinary action pertaining to identified trends. This report must include the name and position of each of the members of the SIRC, documentation of any changes in the membership during the reporting period, and the dates of the SIRC meetings
NOTE: If a current waiver service provider was not the original waiver service provider agency involved at the time the ISP was approved, a copy of the ISP, current PPO, current RSP, any Addendum issued during the current RSP period, and NOD form(s) must be obtained from the Service Coordination agency and maintained in the waiver service provider's record for the waiver participant. For all other information, the waiver service provider is responsible for maintaining information that has been obtained and/or written since becoming involved as a waiver service provider for the participant.
Section VIII: Required Training for Waiver Service Providers
Introduction
This section of the Program Manual describes the training requirements for waiver service provider staff and how best to meet those training requirements.
The provision of high-quality services on a consistent basis will result in providing the waiver participant with the greatest opportunity to achieve their individual goals for living in the community.
Required training for all waiver service providers includes three components:
- Basic Orientation Training
- Service Specific Training
- Annual Training
An eMedNY listserv notice indicates that, effective January 1, 2020, NHTD and TBI waiver service providers are responsible for:
- Developing a written training curriculum for each training component noted above;
- Ensuring that all waiver service staff attend required training;
- Providing Basic Orientation Training and Service Specific Training to all staff prior to their unsupervised contact with a waiver participant;
- Providing required annual training to all waiver service staff who have direct contact with a waiver participant; and
- Documenting all training participation in the employee file, including training opportunities that staff have attended outside of the organization.
NHTD and TBI waiver service providers will be responsible to develop and implement provider specific Basic Orientation and Service Specific training curricula which must then be reviewed and approved by the Regional Resource Development Center (RRDC) prior to implementation. In addition, all Home and Community Support Services (HCSS) staff, in order to maintain LHCSA compliance, must attend at least 6 hours of in-service training annually, based on the calendar year. All waiver service annual training is to be provided based on the calendar year (January to December) regardless of the date of hire or initial training. HCSS staff are expected to complete both LHCSA training in addition to waiver service training. Environmental/Vehicle Modifications, Moving Assistance, Nutritional Counseling, Wellness Counseling, Respiratory Therapy, Congregate Meals, and Home Visits by Medical Personnel are not required to receive additional training beyond their professional experience and/or licensure. All other staff are required to attend Basic, Service Specific and Annual training. Waiver Transportation staff are required to fulfill the terms and conditions as a contracted Medicaid Transportation provider.
NOTE: Personal Care Regulation 18 NYCRR 505.14 states:
"(ii) In-service training shall be provided, at a minimum, for three hours semiannually for each person providing personal care services to develop specialized skills or knowledge not included in basic training or to review or expand skills or knowledge included in basic training."Licensed Home Care Service Agency Regulation states:
"766.11 Personnel.The governing authority or operator shall ensure for all health care personnel:
……(i) that all personnel receive orientation to the policies and procedures of the home care services agency operation and in-service education necessary to perform his/her responsibilities. At a minimum:
- home health aides must participate in 12 hours of in-service education per year;
- personal care aides must participate in six hours of in-service education per year; and
- advanced home health aide must participate in 18 hours of in-service education per year which must include medication management, infection control, and injection safety, and must be directly supervised by a registered professional nurse."
The Regional Resource Development Center staff must review and approve all training curricula and related materials prior to implementation using criteria established by NYSDOH and may observe training sessions as needed. Providers will be responsible to provide the RRDC with monthly training schedules or indicate if training is not offered in that month. On audit, OMIG will obtain the RRDC training curriculum approval document(s) for Basic Orientation and Service Specific curriculum.
Training may be conducted as a group or on a one-on-one basis. Staff who have not successfully completed the required training will not be left unsupervised with waiver participants until Basic Orientation and Service Specific training is completed. The Basic Orientation and Service Specific training must be completed within thirty (30) days of employment with the provider.
If a staff person has completed Basic Orientation and Service Specific training offered by another provider, prior to their current employment, the employer must have proof of the employee's successful completion of the training. A certificate of successful completion of the training must be maintained in the prior and current employer's staff personnel file. If the certificate of training completion is more than two years old, the staff person must be re-trained.
All employee personnel records must contain Basic Orientation and Service Specific training documentation, as follows: 1) a description of the course content; 2) dates of training attendance and copies of the sign-in sheet(s) verifying attendance at all trainings; 3) pre- and post-tests; and 4) certificates of training completion. For HCSS Annual training, the topic(s), training sheets and attendance sheets for at least 6 hours of training should be included. Annual training documentation for other waiver services should include the training curriculum and attendance sheets. For all trainings that were not conducted by the provider, the employee will need to provide verification of continued education credits or a training session that has met prior approval from the employer.
In addition to participation at provider training, all new Service Coordinators will be required to meet with Regional Resource Development Center (RRDC) staff within one (1) month of employment. The type of training and supervision offered during that session is at the discretion of the RRDC and will be fully documented with sign-in sheets and certificates of completion.
All staff are required to meet the professional qualifications established in the 1915(c) waiver applications.
All providers are required to attend at least eight (8) provider meetings conducted by the RRDC per year. Provider representation at the meetings must reflect the organization's administrative staff or mid-level supervisors.
All staff must receive training related to person-centered planning as related to 42 CFR §441.725. Information regarding the training initiative may be found here.
Basic Training should also include information about the philosophy of the HCBS/TBI/NHTD waiver programs and Serious Incident Reporting protocols.
Training must be provided by individuals who are knowledgeable about waiver programs, the needs of specialized service populations, incident reporting and record keeping requirements. Any staff person providing training must meet the service qualifications established in the waiver application for their related profession.
The RRDC will have established criteria for the review and approval of training curricula and will discuss additional training criteria with providers at the time of approval of the training materials.
The approved training certificate will be distributed to providers by the Regional Resource Development Centers (RRDCs).
All trainings held must have a sign-in and sign-out log indicating attendance for every day of training. Training participants must sign-in and sign-out for each day of training attended.
Staff from the RRDC may audit all training sessions at their discretion. Providers are required to provide their training schedules to the RRDC prior to implementation. The RRDC will establish the time frames for training calendar submission.
1. Basic Orientation Training
Definition
All qualified waiver service provider staff must complete Basic Orientation training prior to having any unsupervised contact with a waiver participant and within thirty (30) days of beginning service provision to a NHTD participant.
The training consists of one-on-one and/or group training to instruct new employees of waiver service providers about the general needs of individuals with disabilities and/or seniors, the philosophy, and policies of the NHTD waiver, waiver services and waiver participants' rights and responsibilities. The RRDC will utilize a checklist (RRDC Training Curricula Checklist) when reviewing and approving all provider training curriculum.
The Regional Resource Development Center (RRDC) may provide training when there are not a sufficient number of providers approved to conduct their own training in the region. If a provider does not have an approved curriculum, they may ask another provider who is approved to include their staff in their training sessions. This accommodation is strictly voluntary.
2. Service Specific Training
Definition
Service specific training prepares the waiver service provider staff for the roles and responsibilities specific to the waiver service they are qualified to provide. This training must be completed by a staff person prior to having any unsupervised contact with a waiver participant and within thirty (30) days of beginning service provision to a NHTD participant.
Service specific training consists of one-on-one and/or group training to instruct individual staff about their role as providers of a specific service. All staff must understand the description of each waiver service written in the Program Manual (refer to Section VI - Waiver Services).
All waiver service providers for this group must include the following information in the curriculum for Service Specific Training:
- Definition and goals of the service and a detailed job description;
- Roles and responsibilities of the provider of the specific service;
- Procedures for completing service-specific assessments;
- Procedures for effective communication and coordination between staff and the Service Coordinator and all waiver and non-waiver service providers;
- Basic understanding of NHTD waiver services and other available community services and funding sources;
- The prior approval process;
- Record keeping responsibilities of the specific waiver service providers, including NHTD Service Plans, Detailed Plans, documentation of encounters, and Individual Service Reports ;
- Team Meeting requirements;
- Waiver Participant Rights and Responsibilities (DOH-5732);
- Effective interventions during crisis, including behavioral and medical, natural disasters, severe weather, and lack of replacement staff;
- Basic safety and emergency procedures (e.g., choking, loss of consciousness, breathing difficulties); and
- Identifying and reporting any changes in the participant's routine use of medication, usual behaviors, mood, personality, sleep patterns, functional and cognitive abilities, appearance and/or lifestyle.
NOTE: Home and Community Support Services (HCSS) staff are required to attend all training requirements established in LHCSA regulations and must attend the additional hours of waiver training (Basic and Service Specific).
3. Annual Training
Definition
Annual Training is provided to keep waiver service provider staff up to date regarding their roles and responsibilities specific to the waiver service they are qualified to provide. Annual Training must be provided during each calendar year (January to December) regardless of the date of hire of the staff. Waiver service provider staff must complete this training, and this may consist of one-on-one and/or group training.
For example, an employee is hired March 1, 20XX and completes the required initial training. The agency's annual training is set for June of that year. Therefore, the new employee must also attend the scheduled June annual training, as well as all subsequently scheduled annual trainings from that point forward.
Annual Training requirements include, at a minimum:
- A review of NHTD Participant Rights and Responsibilities (DOH-5732);
- A review of the NHTD Incident Reporting Policy and Complaint Procedure;
- A review of all new policies and/or procedures required by the NHTD waiver that impact the services provided; and
- Additional topics relating to findings of satisfaction surveys, incident reports and trend analyses.
Training must be provided by individuals who are:
- Knowledgeable about the needs of individuals with disabilities and/or seniors or knowledgeable regarding one of the specific areas of required training;
- Familiar with the philosophy, policies and procedures of the NHTD waiver (i.e., knowledgeable about the NHTD waiver program);
- Knowledgeable regarding the waiver service that is the subject of the service specific training; and
- Knowledgeable about incident reporting and record keeping requirements.
Any staff person providing training must meet the service qualifications established in the NHTD waiver application for their related profession.
Documentation of All Training By Providers
For all waiver service providers, the required documentation includes:
- Documentation in each waiver service provider employee's file of all NHTD- related trainings provided by the waiver service provider or other entities.
This documentation must contain:
- Name of the trainer and affiliation/qualifications;
- Verification of staff person's attendance at trainings;
- Date and place of training;
- Goals and objectives of training;
- Evaluation instruments that measured the success of the training; and
- Certificate of Attendance.
Agencies are responsible for ensuring that individuals providing waiver services have also completed Basic Orientation Training and Service Specific Training. Individuals with documented successful completion of prior training (DOH Training Certificate) in the content area(s) specified in Basic Orientation Training and/or Service Specific Training may be exempt from such training upon approval of the RRDC. If the DOH Certificate of Completion is more than two (2) years old, the employee must attend a new session (Basic and Service Specific).
Section IX: Due Process
Introduction
Under State and federal law, an applicant or participant has the right to seek review of certain determinations or actions of NYSDOH and its administrative designee, the Regional Resource Development Center (RRDC). Review can be requested in the form of a Case Conference with the RRDC or in the form of a Fair Hearing before an independent Hearing Officer. As established in 18 NYCRR 358, the NYS Office of Temporary and Disability Assistance's (OTDA) Office of Administrative Hearings (OAH) presides over the Fair Hearing process.
This section describes these rights and procedures and provides information about how applicants and participants can exercise their rights, including how and when to request a Fair Hearing. Additionally, both the RRDC and the Service Coordinator (SC) will provide information about the Case Conference and Fair Hearings processes to waiver applicants/participants. Reiteration and accessibility of this information is important to ensure applicants/participants are aware of and understand important consumer rights and options. In particular, the RRDC and the SC will review the Applicant Interview Acknowledgement (DOH-5729) and Waiver Participant Rights and Responsibilities (DOH-5732) forms, which include information about the Case Conference and Fair Hearing processes, with the applicant/participant. These forms are signed by the applicant/participant, legal guardian, or Authorized Representative to acknowledge receipt and understanding. The SC will also review the Waiver Participant Rights and Responsibilities form with the participant annually and will give it to the participant to be maintained in an accessible location in the home.
Waiver Participant's Rights and Responsibilities
During the initial face-to-face Intake meeting with the potential waiver participant, the Regional Resource Development Specialist (RRDS) provides information regarding the Notice of Decision (NOD), Case Conference, and Fair Hearing processes. Additionally, the Service Coordinator (SC) ensures that the waiver applicant understands his/her rights regarding Case Conferences and Fair Hearings as they proceed through the waiver enrollment process, and throughout the duration of the participant's waiver enrollment. The NOD regarding participation in the waiver program provided by the RRDS to the participant includes a description of Fair Hearing rights.
Both the RRDS initially, and the Service Coordinator, thereafter, provide information to waiver applicants to assure their awareness and understanding of the Fair Hearing process. This is important, as the application process can be lengthy, and reiteration of certain information provides assurance that important consumer rights and activities are understood by waiver applicants and participants.
An individual has the right to seek a Medicaid Fair Hearing for many reasons including issues related to the NHTD waiver. Decisions regarding Medicaid eligibility are addressed through the Fair Hearing process with the Local Department of Social Services (LDSS). As established in 18 NYCRR 358, the NYS Office of Temporary and Disability Assistance (OTDA) Office of Administrative Hearings presides over the Fair Hearing process.
A waiver participant may file a grievance/complaint through the NHTD Complaint Line at any time. All calls received through the NHTD Complaint Line are forwarded to NYSDOH waiver staff responsible for the operation of this grievance/complaint system.
Information regarding the State Grievance/Complaint System is provided by the Service Coordinator (SC) to the potential waiver participant during the enrollment process, and at other times throughout enrollment, as appropriate. The participant/legal guardian is informed that filing a complaint/grievance is not a prerequisite or substitute for a Fair Hearing.
The Regional Resource Development Center (RRDC) is responsible for receiving complaints and grievances on the regional complaint phone line. Approved NHTD service providers must also establish a method for receiving and addressing complaints. NYSDOH also receives complaints and monitors the response and outcomes of the RRDC and provider complaint processes.
The following information is on the participant's Waiver Contact List, which is maintained in the participant's home:
Waiver Complaint Line (Name of RRDC)
NYS Department of Health NHTD Waiver Program
NYS Department of Health Home Care Complaint Line (LHCSA issues)
NYS Department of Health Medicaid Helpline
NYS Office of Temporary and Disability Assistance Fair Hearings
NYS Justice Center
Poison Control CenterAdditionally, NYSDOH maintains the following call centers:
Adult Home Complaint Hotline
Home Care/Hospice Hotline
Nursing Home Abuse HotlineEvery waiver participant has certain rights and must agree to certain responsibilities related to the NHTD waiver program. As part of the approval process, the potential participant is presented with a copy of the Waiver Participant's Rights and Responsibilities (DOH-5732) for the waiver program.
The Service Coordinator is responsible for explaining the rights and responsibilities of being a waiver participant to the individual and/or legal guardian during the person- centered service planning process. The applicant and/or legal guardian must also sign and date the document during this process. These rights and responsibilities should be reviewed during the development of the application, at any time the service plan is revised, and any time the Service Coordinator is aware that the participant does not understand their rights or responsibilities.
The Waiver Participant's Rights and Responsibilities form must be signed and dated by the applicant and/or legal guardian at least annually thereafter. The signed original document is maintained with the Application Packet in the Service Coordinator's record. The Service Coordinator gives a copy to the participant to be maintained in an accessible location in the participant's home.
The Waiver Participant has the right to:
- Be informed of their rights prior to receiving waiver services;
- Receive services without regard to race, religion, color, creed, gender, national origin, sexual orientation, marital status, or disability;
- Be treated as an individual with consideration, dignity, and respect, including but not limited to, their person, residence and possessions;
- Have services provided that support their health and welfare;
- Assume reasonable risks and have the opportunity to learn from these experiences;
- Be provided with an explanation of all services available in the Nursing Home Transition and Diversion (NHTD) waiver and other health and community resources that may be of their benefit;
- Participate or designate an individual to participate on their behalf in the development, review and approval of all service plans, including any changes to the service plan;
- Select a Service Coordination provider;
NOTE: Waiver participants are afforded the right to choose provider agencies, not specific provider staff.- Receive assistance from their Service Coordinator to select service providers from other agencies. The participant may not choose to receive most other services from the same agency where their Service Coordinator works;
NOTE: Waiver participants are afforded the right to choose provider agencies, not specific provider staff.- Request a change in services (add, increase, decrease or discontinue) at any time;
- Be fully informed of the process for requesting a Conference with the RRDC and/or Fair Hearing upon receipt of a Notice of Decision or at any time while a participant of the NHTD waiver;
- Be informed of the name and duties of any person providing services approved in their service plan;
- Have the freedom and support to control their own schedule and activities;
- Receive services from approved, qualified individuals;
- Receive from the Service Coordinator, in writing, a list of names, telephone numbers, hours of operation, and supervisors for all waiver services providers, the RRDS, and the Waiver Complaint line;
- Refuse care, treatment and services after being fully informed of and understanding the potential risks and consequences of such actions;
- Have their privacy respected, including the confidentiality of personal records, and have the right to refuse the release of the information to anyone not authorized to have such records, except in the case of their transfer to a health care facility or as required by law or Medicaid requirements;
- Submit complaints about any concerns regarding services provided;
- Receive support and advice from the Service Coordinator to resolve their concerns and complaints about services and waiver service providers;
- Receive additional support and advice from the RRDC and DOH waiver staff as desired or in the event that their Service Coordinator is not successful in resolving concerns and complaints about services and waiver service providers;
- Have their complaints responded to and be informed of the outcome;
- Have their waiver service providers protect and promote their ability to exercise all rights identified in this document without fear of reprisal;
- Have all rights and responsibilities outlined in this document forwarded to their court appointed legal guardian, advocate or anyone they choose to act on their behalf;
- Participate in surveys inquiring about their experiences as an NHTD waiver participant. This also includes the right to refuse to participate in surveys without jeopardizing your continued participation in the waiver program; and
- Exercise all rights listed without fear of reprisal.
Waiver Participant's Responsibilities
The participant is responsible to:
- Work with their Service Coordinator to develop/revise their service plan to assure timely reauthorization of the service plan;
- Direct and actively participate in waiver services as identified in their service plan and receive Service Coordination a least monthly;
- Follow their service plan and notify their Service Coordinator if problems occur;
- Talk to their Service Coordinator and other waiver providers if they want to change their services or goals;
- Provide to the best of their knowledge, complete and accurate medical history, including all prescribed and over-the-counter medications they are taking and understand the risk(s) associated with their decisions about care;
- Inform the Service Coordinator about all treatments and interventions in which they are involved;
- Maintain their home in a manner which enables them to safely live in the community;
- Secure and maintain an appropriate community residence;
- Ask questions when they do not understand their services;
- Not participate in any criminal behavior. The participant understands that, if they do, their waiver service provider(s) may leave, the police may be called, and their continuation in the waiver program may be jeopardized;
- Report any changes in their medical condition, circumstances, informal supports, and formal supports to their Service Coordinator;
- Provide accurate information related to their coverage under Medicaid, including any notices from the Local Department of Social Services regarding their Medicaid, Medicare or other medically-related insurance programs to their Service Coordinator;
- Work with their Service Coordinator to maintain active Medicaid;
- Notify all waiver service providers as soon as possible if the scheduled service visit needs to be rescheduled or changed;
- Notify appropriate person(s) should any problems occur, or if the participant is dissatisfied with services provided; and
- Treat the RRDS and their service providers with consideration, dignity and respect. Show respect and consideration for staff and their property. Do not create an environment which is hostile for the RRDS or their service providers.
The Notice of Decision
The RRDC, as the administrative designee for NYSDOH, is required to provide the applicant/participant and the identified legal guardian or Authorized Representative, if applicable, with a Notice of Decision (NOD) when the RRDC takes certain actions. Actions that give rise to such notice include when:
- An individual is determined eligible for waiver participation;
- An individual is denied or discontinued from waiver participation;
- Waiver services are added, increased, decreased, or discontinued; or
- An individual's choice of provider is denied or discontinued.
The NOD is a standardized form that informs the applicant or participant of the action taken or intended. The NOD informs the applicant/participant of their right to a Case Conference to review the actions described in the NOD, their right to request a Fair Hearing if the applicant/participant believes the decision is incorrect, the methods and time frames for requesting a conference or Fair Hearing, and if applicable how a participant can maintain their benefits throughout the Fair Hearing process ("aid continuing" or "aid to continue"). The notice also provides guidance for acquiring free legal assistance and explains how to obtain copies of relevant documents including the applicant/participant case file.
The RRDC provides a copy of the NOD to the applicant/participant and to the SC, if the applicant/participant has an SC at the time of the decision. The SC will review the NOD with the applicant/participant and/or legal guardian, including the instructions provided in the notice, to ensure the applicant/participant's understanding of the decision and right to request a Case Conference and/or Fair Hearing. The SC will advise the applicant/participant that a request for a Fair Hearing must be submitted within sixty (60) days of the Notice Date indicated in the NOD. If applicable, the SC also reviews the participant's right to aid continuing while a Fair Hearing decision is under consideration, and that such requests must be made within ten (10) days of the Notice Date.
A copy of the NOD is kept in the applicant's/participant's record maintained by the RRDS and Service Coordinator. If applicable the case conference and fair hearing will be included.
Participants and providers must adhere to the effective date of the decision when implementing or terminating services. The RRDC approval of a service plan authorizes the provision of services documented in the plan.
Timely notice is a notice which is mailed at least ten (10) days before the date upon which the proposed action is to become effective.
The Notice of Decision Types
The following describes each type of Notice of Decision (NOD) used in the NHTD Waiver program (DOH-5740, DOH-5737, DOH-5738, DOH-5735, DOH-5739, DOH-5734). An applicant/participant may seek a remedy for an adverse decision specifically related to waiver services through the Fair Hearing process.
- NOD - Waiver Eligibility Denial or Discontinuation (DOH-5737 or DOH-5738) will be provided when an individual is not eligible to receive waiver services for such reasons, including but not limited to:
NYSDOH/RRDC may include other reasons for the action based on individual case circumstances.
- NYSDOH/RRDC determines the applicant/participant chooses not to receive waiver services.
- NYSDOH/RRDC determines the applicant/participant is not at least eighteen (18) years of age upon application.
- NYSDOH/RRDC determines the applicant/participant is not a recipient of Medicaid coverage that supports community-based long-term care services.
- NYSDOH/RRDC determines the applicant/participant is not able to identify an HCBS compliant community residence where waiver services will be provided.
- NYSDOH/RRDC determines that informal supports, non-Medicaid supports, State Plan Medicaid services, and/or waiver services are not sufficient to safely serve the individual in the community.
- NYSDOH/RRDC determines that the applicant/participant does not require nursing home Level of Care (LOC), based on the LOC assessment.
- NYSDOH/RRDC determines the services and supports available through the waiver and all other sources are not sufficient to maintain the individual's health and welfare in the community.
- NYSDOH/RRDC determines the applicant/participant chooses to receive services, or may be more appropriately served, by another home and community-based services Medicaid waiver.
- NYSDOH/RRDC determines the participant is hospitalized for more than thirty (30) days and there is no scheduled discharge date.
- NYSDOH/RRDC determines the participant is admitted to a nursing home, psychiatric, rehabilitation, assistive living, or other congregate care/institutional setting for other than a short term.
- NYSDOH/RRDC determines the participant is incarcerated for more than thirty (30) days.
- NYSDOH/RRDC determines the participant is residing outside the State of New York for more than thirty (30) days.
- NYSDOH/RRDC determines the participant is not actively participating in waiver services and/or does not receive ongoing Service Coordination.
- NYSDOH/RRDC determines that the applicant/participant is residing in a congregate care living arrangement of four or more unrelated individuals.
In the case of a discontinuation, a copy of the NOD is provided to the Local Department of Social Services (LDSS) to advise that the program designation (R/E code 60) must be removed from the individual's Medicaid ID.- NOD - Waiver Eligibility Authorization (DOH-5740) is provided to an applicant when they are approved to receive waiver services. This NOD includes the effective date of eligibility for services. A copy of the NOD is provided to the Local Department of Social Services (LDSS) to enter the determination in the Medicaid history of the individual and to assign the program designation to the participant's Medicaid ID. This authorization confirms providers may initiate services. Waiver services may not be provided without this authorization.
A copy of the NOD is provided to the Local Department of Social Services (LDSS) to advise that the program designation (R/E code 60) be assigned to the applicant's Medicaid ID., or in the case of a discontinuation, the program designation be removed.- NOD - Reduction and/or Discontinuation of Waiver Service(s) (DOH-5739) is provided to a participant when there is a reduction in the hours/frequency/duration of a waiver service(s) and/or elimination/discontinuation of specific waiver service(s).
- NOD - Denial of a Waiver Provider (DOH-5734) is provided to a participant when their request for a specific waiver service provider is denied due to conflict of interest; or the provider is no longer approved/available to provide services.
NHTD waiver participants may only select a waiver service provider from the list of currently approved and conflict-free providers presented to the participant by the RRDC. Approval of a waiver service provider does not mean authorization of specific staff employed by the provider. Participants are not ensured that specific staff will be assigned to a case or can continue to work with a specific participant.
Authorization of a waiver service provider is completed through a signed Provider Selection Form (DOH-5730) completed by the RRDC prior to service delivery. This authorization does not require an NOD and is not subject to Fair Hearing. A provider selection form is executed each time a participant selects a new provider and the RRDC approves the request. When the waiver service provider is unable/unwilling to accept a participant, an NOD is not required and the RRDC will advise the applicant/participant they must select another provider. The provider will confirm denial/lack of availability of service provision in writing to the applicant/participant.- NOD Addition and/or Increase of Waiver Service(s) (DOH-5735) authorizes the provision of services to a participant when there is an increase in the hours/frequency/duration of a waiver service(s), and/or when a new waiver service(s) is approved in the participant's service plan. Services may not be initiated without this NOD unless the RRDC approves emergency services.
- NOD Notification of Death of a Waiver Participant is provided to the Local Department of Social Services when a participant has died. All waiver services terminate at the death of a participant and the Service Coordinator is responsible to inform waiver service providers when services are to cease. A copy of the NOD is provided to the Local Department of Social Services (LDSS) to enter the determination in the Medicaid history of the individual and to remove the program designation to the participant's Medicaid ID.
NOTE: This notice is not sent to the participant's home, legal guardian, or to any family/designated representatives. It is only sent to the Service Coordinator, NHTD waiver staff and LDSS in the county of residence and with fiscal responsibility as noted on the bottom of the form. The service coordination agency sends a copy to the other active waiver service providers to complete close out of their records.Case Conferences and Fair Hearings
Applicants/participants who receive an NOD may request either a Case Conference and/or a Fair Hearing. If the applicant/participant, or their representative, contacts the RRDC to discuss an applicable action, the RRDC should remind them about their right to a Conference and Fair Hearing, and work with the applicant/participant to reach an understanding of the action or other appropriate resolution. If a consensus cannot be reached, the RRDC reminds the applicant/participant about their right to request a Case Conference and/or Fair Hearing and aid continuing, if applicable, and should provide information (such as contact information for requesting a Fair Hearing) to enable the applicant/participant to exercise their rights.
Case Conferences
An applicant/participant may request a Case Conference with the RRDC to review the RRDC's decision. The applicant/participant may request a Case Conference regardless if they request a Fair Hearing. Requesting a Case Conference does not affect the participant's ability or right to request a Fair Hearing and is not a prerequisite/or substitute for a Fair Hearing. A request for a Case Conference does not entitle a participant to aid continuing. Aid continuing is only available to participants for certain actions and can only be obtained when requesting a Fair Hearing.
The Case Conference is an opportunity for the applicant/participant and/or legal guardian to review with the RRDC the reasons for the action and address information they feel has not been accurately or sufficiently presented. At the conference, if the RRDC discovers that an incorrect/inaccurate decision was made or when a different decision is appropriate because of additional information provided by the applicant/participant, the RRDC may revoke or revise the decision to reflect the updated understanding, which may warrant a new NOD. Through discussion, it may be possible to resolve issues without a Fair Hearing. Applicants/participants utilizing the Case Conference process are still entitled to a Fair Hearing.
Requesting a Fair Hearing
A Fair Hearing is a hearing held in the presence of a Hearing Officer, a specially trained Administrative Law Judge (ALJ) from the New York State Office of Temporary and Disability Assistance (OTDA). Information about OTDA and the Fair Hearing process may be found here. The purpose of the Fair Hearing is to allow the applicant/participant or legal guardian to present evidence and arguments to the Administrative Law Judge (ALJ) so that the ALJ may consider the evidence and arguments presented by the RRDC and determine whether to affirm or disconfirm the RRDC's decision. The applicant/participant may secure their own legal counsel to represent them throughout the appeal process, but it is not necessary to proceed. Service Coordinators may assist an applicant/participant through the hearing process, however, may not represent the participant for the purposes of the Fair Hearing. Information further explaining this role may be found here.
A waiver applicant/participant has the right to seek a Fair Hearing for many reasons including issues related to the NHTD waiver. Applicants/participants have sixty (60) days from the Notice Date indicated on the NOD to request a Fair Hearing. OTDA will notify the appellant of the time and place of the hearing at least ten (10) calendar days prior to the hearing date. Applicants/participants may request a Fair Hearing by calling a statewide toll-free number (1-800-342-3334), faxing a copy of the notice (on the back of the NOD) to OTDA, mailing the request to OTDA or through completion and submission of the online request form found here.
The applicant/participant may also request in person at the following locations:
New York City
Office of Temporary and Disability Assistance
Office of Administrative Hearings
14 Boerum Place, 1st Floor
Brooklyn, New York 11201 Albany
Office of Temporary and Disability Assistance
Office of Administrative Hearings
40 North Pearl Street
Albany, New York 12243For applicants/participants who are speech and/or hearing impaired, they may contact the New York Relay Service at 711 and request that the operator call OTDA at 1 (877) 502-6155. Service at this number will only be provided to callers using Telecommunications Device for the Deaf (TDD) equipment. For more information on the New York Relay Service, please visit their website here. Decisions regarding Medicaid eligibility are addressed through the Fair Hearing process with the LDSS.
Aid Continuing
Aid continuing offers the participant an opportunity to continue Medicaid benefits received prior to the adverse action while they pursue a Fair Hearing until a final determination is made. If the participant indicates the need for aid continuing until the Fair Hearing decision is received, the participant must: a) request the Fair Hearing before either the intended effective date of the action or ten (10) days after the notice is mailed, whichever is later, and b) indicate that they want their services to continue. If this time period elapses and the participant can no longer request aid continuing, they may still request a Fair Hearing if it is done within sixty (60) calendar days of the NOD Notice Date.
The decision to grant aid continuing is made by OTDA. If approved, OTDA will issue an aid continuing order to the RRDC to continue services in question. Upon approval of OTDA, services subject to aid continuing must be maintained until OTDA issues the Fair Hearing decision. If the Fair Hearing decision supports the action taken by the RRDC and the participant received aid continuing, NYSDOH may determine the participant is responsible for the cost of services provided during the Fair Hearing process.
Fair Hearing Process
When OTDA receives notification from the applicant/participant and/or legal guardian of their intent to pursue a Fair Hearing, OTDA notifies NYSDOH of the request including if aid continuing has been requested and approved. NYSDOH notifies the responsible RRDC of the request for Fair Hearing. If the request for aid continuing is approved, the RRDC notifies the Service Coordinator. Upon approval of aid continuing, all services in place at the time of the request for Fair Hearing will remain in place until a Fair Hearing decision is rendered. Providers will maintain proof of the Fair Hearing and aid continuing in the participant record as authorization to continue service provision during the Fair Hearing process. The RRDC will provide the Service Coordinator a copy of the Fair Hearing notice with the notation of "AC" so that providers are aware that services are approved to continue pending the hearing outcome.
Once the RRDC has been notified that a person or organization has been authorized to represent the applicant/participant at the Fair Hearing, such representative will receive copies of all correspondence between the RRDC and the applicant/participant relating to the Case Conference and Fair Hearing.
At any reasonable time before the date of the Fair Hearing and also at the Fair Hearing, the applicant/participant or their authorized representative has the right to examine the contents of their case record and all documents and records to be used by the RRDC at the Fair Hearing. This information may also be provided in conjunction with and at the time of the Case Conference. As a matter of course, the RRDC will provide the appellant with copies of such documents at no cost, which may be mailed or emailed, and are available for review at the RRDC.
At the hearing, appellants are afforded the opportunity to present written or oral evidence to demonstrate why the action should not be taken, as well as the opportunity to question any persons who appear at the hearing. Appellants have the right to bring witnesses to speak in favor of their position. Any documents that may be helpful in supporting the appellant's case may be presented. Appellants are also advised that they have the right to be represented by legal counsel, a relative, a friend or other person, or to represent themselves. Appellants may be able to obtain legal assistance by contacting the Legal Aid Society or other legal advocacy groups.
Who may be present at the Fair Hearing
The following persons may be present at a Fair Hearing:
- The applicant/participant who has requested the Fair Hearing;
- The applicant/participant's representative;
- Counsel or other representatives of the RRDC;
- Witnesses of either party and any who may be called by the hearing officer;
- An interpreter; and/or
- Any other person admitted at the hearing officer's discretion, with the consent of the appellant.
To conduct the hearing the applicant/participant or their representative must be present.
A representative of the RRDC must also appear at the Fair Hearing along with the case record and a written summary of the case. Such representative must:
- Have reviewed the case; and
- Be prepared to present evidence in support of the action, including:
- The case number;
- A brief description of the facts, evidence and reasons supporting the RRDC decision, including identification of the specific provisions of law, program manual and approved policies which support the action; and
- A copy of the applicable Notice of Decision (NOD).
Role of the Service Coordinator and Other Waiver Providers
A Service Coordinator, other waiver providers or employing agency, may discuss and provide additional information in response to a preliminary decision in which there is disagreement. Once a written determination to deny, discontinue, or reduce one or more waiver services is executed, any advocacy or appearance on behalf of the participant by waiver providers to challenge the decision is beyond the scope of the provider's role. Such activity constitutes a conflict-of-interest for the Service Coordinator, other waiver provider or employing agency.
Advocating for the participant against the Department is not consistent with the role of "advocate" as presented in the Program Manual. In the case of service coordination, for example, their duties are to facilitate the acquisition of needed services on behalf of the applicant/participant. Once action is initiated by the RRDC and a Fair Hearing decision rendered, the participant and providers are bound by that decision.
A waiver provider, for example, a service coordinator, may assist a participant and their family in seeking a Case Conference to help resolve a discrepancy, making a Fair Hearing request and/or by referring the participant and their family to legal services providers. Waiver providers may also support the participant by performing tasks such as filing, mailing and/or managing paperwork for their participant's case and care. Such assistance is appropriate and permissible, but the practice of advocacy by a Medicaid provider who is in the position to receive financial gain by the advocacy is a conflict of interest, or an appearance of a conflict of interest.
The Role of the RRDC in the Fair Hearing process
- Works in conjunction with NYSDOH to prepare for the hearing;
- Prepares an Evidentiary Packet containing copies of all required documentation and examples that explain the reasons for the NOD and address the applicant's/participant's concerns;
An Evidentiary Packet includes copies of the following:
- Verification of current Medicaid coverage/eligibility, indicating eligibility for community-based long term care;
- Notice of Decision(s) sent to applicant/participant resulting in the request for Fair Hearing;
- Current UAS-NY or PRI (if in a nursing facility or hospital) completed by an individual(s) certified/trained to administer the tools;
- Freedom of Choice form (DOH-5728), signed by the applicant/participant;
- Relevant case notes;
- Current service plan, RSP and/or Addendum approved and signed by RRDS;
- Plan for Protective Oversight (PPO);
- Service provider notes/records which serve as documentation of recurring issues, if applicable;
- Applicable pages from the NHTD Program Manual and program directives related to the case with section and page number(s) noted; and
- Case history/timeline indicating action taken to respond to the applicant/participant's dispute/issues.
- Responds in a timely manner to an applicant/participant's request for access to and/or copies of documents from the applicant/participant's record;
- Attends the Fair Hearing and presents information to the Administrative Law Judge. NYSDOH may request that its legal counsel or another entity (e.g., waiver service provider) attend the Fair Hearing and present information as appropriate; and
- Keeps NYSDOH informed of any issues that occur during the Fair Hearing process.
Generally, within ninety (90) days of the hearing request, OTDA will send a formal written decision to the participant, NYSDOH and the LDSS with the final decision of the hearing. NYSDOH provides a copy of this response to the RRDC.
The RRDC then:
- Notifies the Service Coordinator of the outcome of the hearing so that appropriate follow-up can occur;
- Ensures that any changes to the service plan are made accordingly; and
- Ensures that if discontinuation from the waiver is indicated for the participant, the Service Coordinator establishes a safe and appropriate discharge plan.
A copy of all NODs and related Conference and Fair Hearing decisions is maintained in the participant's record at both the RRDC and Service Coordination provider office.
NYSDOH staff monitor all Fair Hearing requests and dispositions and serves as a liaison to OTDA if there are any issues regarding the tracking and facts related to the Fair Hearing process.
Section X: Incident Reporting Policy and Complaint Procedure
Introduction
As part of its obligation to promote the well-being of every participant being served, the Nursing Home Transition and Diversion (NHTD) waiver must ensure safeguards are in place to prevent, to the extent possible, circumstances/situations that can result in harm to the participant.
The purpose of reporting, investigating, correcting and/or monitoring certain events or situations is to enhance the quality of care provided to participants and to protect them (to the extent possible) from further harm. The following process serves to identify, investigate and remedy potentially harmful situations and minimize the possibility of future occurrences.
Incident Reporting Policy
The process for Incident Reporting begins with the occurrence of an 'Event,' which is defined as an occurrence with a negative impact to the participant, or actual harm to the participant that has come to the attention of a waiver service provider. Once a provider has become aware of an 'Event,' the provider must evaluate what has occurred to determine at what level an investigation must be conducted. The safety of the participant must be immediately ensured upon discovering an event. The two categories of 'Events' are as follows:
- Recordable Incidents are events that do not pose an immediate threat to the participant and do not meet the level of severity of Serious Reportable Incidents but may compromise the participant's safety and well-being if not noted, reported and addressed. These incidents warrant an internal investigation by the provider and are monitored by the provider agency's quality assurance unit for trends and outcomes, including the necessity for a more in-depth investigation (e.g., a Serious Reportable Incident). Recordable incidents are not reported to NYSDOH. These incidents are reported annually to the RRDC and are subject to review upon site visit by the RRDC and/or NYSDOH.
Investigations of Recordable Incidents are conducted at the provider level in accordance with the agency's own internal investigation process. As part of the investigation, the agency must determine ways to improve its policies, procedures, and practices to prevent reoccurrence of Recordable Incidents.- Serious Reportable Incidents (SRI) are significant events or situations endangering a participant's well-being, and because of the severity or sensitivity of the situation, must be reported to the Regional Resource Development Center (RRDC) and/or NYSDOH.
The RRDC is the administrator of the SRI process within its region. The RRDCs assure that: (a) the process is initiated, investigated, and completed in a timely manner; (b) outcomes are appropriate; and (c) the waiver service provider investigating the SRI conducts appropriate follow-up.
SRI investigations are conducted at the provider level as designated by the RRDC. Each waiver service provider must determine ways to improve its own policies and procedures to prevent the reoccurrence of SRIs. Through the provision of technical assistance, monitoring, and trend analysis, the RRDC will make recommendations to providers for improvements in the provision of services. Outcomes from analyses of regional SRI trends will be provided to DOH waiver staff for statewide analysis and improvement activities. These activities include ensuring the quality of care provided to participants and maintaining the participant's health and welfare. DOH waiver staff identify specific areas of concern or trends related to incidents. This information assists DOH waiver staff in identifying and developing training and policies aimed at increasing provider skills in the prevention, identification, and investigation of incidents.
Serious Reportable Incidents (SRI) Classification
SRI classifications include:
- Abuse is defined as the maltreatment or mishandling of a participant that would endanger their physical or emotional well-being through the action or inaction of anyone associated with the participant, whether or not the participant is or appears to be injured or harmed.
The type of allegation of abuse must be classified in the SRI report as one of the following:
- Physical Abuse is defined as physical actions, such as hitting, slapping, pinching, kicking, hurling, strangling, shoving, unauthorized or unnecessary use of physical interventions, or other mishandling of a participant. Physical contact that is not necessary for the safety of the person and causes discomfort to the participant, or the use of more force than is reasonably necessary is also considered to be physical abuse.
Emergency situations in which physical intervention is used to assure the health and welfare of the participant or others must also be reported as an SRI.- Sexual Abuse is defined as any sexual contact between a participant and any employee, intern, volunteer, consultant, or contractor of the waiver service provider providing services to the participant. Sexual abuse may also occur with any other person living in the community if it is non-consensual or if, according to New York State law, the participant is not competent to consent. Sexual contact is defined as the touching or fondling of the sexual or other body parts of a person for the purpose of gratifying the sexual desire of either party, whether directly or through clothing. Sexual contact also includes causing a person to touch someone else for the purpose of arousing or gratifying personal sexual desires. Forcing or coercing a participant to watch, listen to, or read material of a sexual nature is also considered sexual abuse. A situation in which one participant has a sexual contact with another participant who is either not capable of consent to or did not agree to participate in the relationship, is considered to be an SRI.
- Psychological Abuse is defined as the infliction of anguish, emotional pain, or distress. Emotional or psychological abuse includes, but is not limited to, verbal assaults, insults, threats, intimidation, ridicule, humiliation, scorn, contempt, dehumanization or harassment, or any other acts that are otherwise denigrating or socially stigmatizing. Manipulation, isolating an individual from family, friends, or regular activities, and enforcing social isolation are further examples. The use of language and/or gestures and a tone of voice, such as screaming or shouting at or in the presence of a participant may, in certain circumstances, constitute psychological abuse.
- Seclusion is defined as the placement of the waiver participant alone in a locked room or area from which they cannot leave at will, or in which their normal egress is prevented by someone's direct and continuous physical action.
The act of seclusion should not be confused with a limited quiet time procedure prescribed and/or included in a behavior intervention plan. Quiet time is a procedure in which a waiver participant is accompanied by staff away from an activity for a brief period of time to help the participant recompose themselves. In addition, the participant may request time alone for this same purpose. In removing the participant from ongoing activity, the objective is to offer a changed environment in which the individual may calm down. The use of quiet time is not considered to be an incident unless it is excessive or used as a punishment.- Restraint is defined as the act of limiting or controlling a person's actions or behavior through the use of any device (physical or chemical) that prevents the free movement of any limb; immobilizes a person; or renders the person unable to participate satisfactorily in services, community inclusion time or other activities.
This does not preclude the use of mechanical supports to provide stability necessary for therapeutic measures such as immobilization of fractures, administration of intravenous fluids or other medically necessary procedures.- Mistreatment is defined as a deliberate decision to act toward the participant in a manner that violates the participant's individual human rights, the service plan (SP), and/or is not generally considered acceptable professional practice.
An allegation of financial or material exploitation that can compromise the safety and well-being of a participant should be filed as an Allegation of Abuse, subcategory Mistreatment.- Aversive Conditioning is defined as the use of unpleasant or uncomfortable procedures when trying to change the behaviors of a participant.
- Neglect is defined as a condition of deprivation in which the participant receives insufficient, inconsistent, or inappropriate services, treatment or care to meet their needs; failure to provide an appropriate and/or safe environment; and/or failure to provide appropriate services, treatment or care by gross error in judgment, inattention or ignoring. For example, neglect occurs if a Service Coordinator is aware that an agency listed in a service plan cannot or did not provide the requested services and does not seek an alternate waiver service provider to meet the participant's needs.
The NHTD waiver program recognizes that the failure of staff to attend a scheduled shift may not always put the participant at serious risk; however, to ensure and maintain the health and safety of participants, the need for staff coverage in certain circumstances must be documented in the plan of protective oversight (PPO). Failure to meet the conditions of the PPO should be reported as an SRI.- Violation of a Participant's Civil Rights is defined as any action or inaction that deprives a participant of the ability to exercise their legal rights under State or federal law (e.g., the Americans with Disabilities Act (ADA)).
- Missing Person is defined as an unexpected or unauthorized absence of a participant, taking into consideration their habits, deficits, health problems and capabilities.
When the absence of a participant constitutes a recognized danger to the well- being of that individual or others, a formal search must be initiated immediately. This includes contacting informal supports, the Service Coordinator (if not the one discovering the participant's absence), and the police.
For a participant not believed to be in immediate danger, consideration should be given to the missing person's habits, deficits, capabilities, health problems, etc., in making the decision of when to begin a formal search, but a search must be initiated no more than twenty-four (24) hours after discovery that the participant is missing.- Death of a Waiver Participant is defined as death due to circumstances unrelated to the natural causes of illness, disease or proper treatment in accordance with accepted medical standards; an apparent homicide or suicide; or an unexplained or accidental death. Deaths due to natural causes must be reported to the RRDC within 24 hours; the RRDC will determine if it will be categorized as an SRI.
The follow-up report of the investigation submitted to the RRDC must include information concerning the death, and if obtainable, medical records, death certificate, police reports, autopsy reports, Emergency Medical Services (EMS) records, emergency room records and any other information deemed relevant.- Unplanned Hospitalization is defined as any injury or illness that results in a hospital admission of a participant for treatment or observation for greater than twenty-four (24) hours due to the injury/illness.
Regardless of the participant's admission status, if they are in the hospital over twenty-four (24) hours, an SRI must be filed.
NOTE: If a participant who requires oversight and supervision is brought to a hospital while under the care of a waiver service provider staff, then that staff person is obligated to remain with the participant until they are admitted; until they return home; or until a family member/informal support arrives. If staff leave the participant prior to their admission to the hospital; before the participant returns home; or before the arrival of family member/informal support, an SRI Neglect must be filed.- Possible Criminal Action is defined as any actions by participants which are, or appear to be, a crime under New York State or federal law. Improper action taken by staff is to be included in Violation of a Participant's Civil Rights or other related categories.
- Medication Error/Refusal is defined as any situation in which a participant displays marked adverse effects, or their health or welfare is in jeopardy due to incorrect dosage, administration, or refusal to take prescribed medication.
Consideration must always be given to a participant's right to make choices for themselves and their right to accept risks. If an action by either a waiver service provider or by a participant may have jeopardized a participant's health or welfare even though it did not result in an adverse reaction, the waiver service provider still must investigate the situation and record the action as a Recordable Incident (refer to the Recordable Incident process found in this section). The investigating agency will maintain documentation of the incident investigation and its outcome.
The Recordable Incident will rise to the level of an SRI if the investigation uncovers that the participant did, in fact, experience an adverse reaction (refer to the SRI protocol in this section).Serious Reportable Incident Reporting Procedure
Reporting Responsibilities
When a waiver service provider discovers that an 'Event' has occurred, the agency has twenty-four (24) business hours to initiate an investigation to determine whether the 'Event' is an SRI. If the agency determines the 'Event' is an SRI, the discovering agency then becomes the 'reporter' and initiates the SRI process (refer to procedure below). The agency must complete and submit the "24-Hour Provider Report" to the RRDC within twenty-four (24) hours of knowledge/discovery of the incident.
As part of the investigation of the 'Event', the agency must recognize that a variety of individuals associated with a waiver service provider may be involved in the 'Event,' or may be a witness to the 'Event' and therefore obligated to inform their supervisor. The supervisor determines who will investigate the 'Event' for the agency. If there is a question about whether the 'Event' meets the definition of an SRI, the provider must contact the RRDC to discuss the matter.
In situations in which only a family member or other informal support has witnessed the 'Event' or in which there were no witnesses to the 'Event,' the waiver service provider employee who was made aware of the 'Event,' or their supervisor, becomes the 'discoverer.' They are responsible for investigating the 'Event' to determine whether it is an SRI and reporting the 'Event,' if it is an SRI, to the RRDC within twenty-four (24) hours of discovery.
The RRDC has the responsibility of assigning the investigation to the waiver service provider it feels is most appropriate to conduct the investigation. If the incident does not involve a waiver service provider's employee, the RRDC has the discretion to assign the responsibility of the investigation to any of the participant's waiver service providers or to undertake the investigation itself.
The RRDC must request technical assistance from DOH waiver staff when there are any concerns regarding the investigation of an SRI.
In the event an employee of an Assistive Technology (AT), Community Transitional Services (CTS), Congregate Home and Delivered Meals, Environmental Modifications Services (E-mods), Moving Assistance or Transportation Services provider witnesses an incident or has any concerns involving the participant, that employee must notify their agency's supervisor. The subcontractor and/or the waiver service provider is responsible to report the incident to the participant's Service Coordinator. The Service Coordinator is responsible to initiate and/or conduct the investigation. Contracted
Medicaid Transportation providers must adhere to the terms and conditions of their contract. If an incident is witnessed by an employee of a Home Visits by Medical Personnel waiver provider, that employee must notify the Service Coordinator directly.
Upon notification by any of these providers, the Service Coordinator becomes the 'discoverer' of the incident and is responsible for the reporting process with RRDC.
Procedure
To ensure compliance with the Health Insurance Portability and Accountability Act (HIPAA), all reports and communication containing Protected Health Information (PHI) must be sent via encrypted email.
- Within twenty-four (24) hours of discovering an 'Event' has occurred, the discovering waiver service provider must:
- Determine if the 'Event' rises to the level of a SRI;
- Complete the 24-Hour Provider Report and send it via encrypted email to the RRDC; and
- Provide a copy via encrypted email of the 24-Hour Provider Report to the participant's Service Coordinator (if the discovering waiver service provider is other than the service coordination agency).
If the Service Coordinator is alleged to be involved in the incident, the 24-Hour Provider Report is sent to the Service Coordination Supervisor.
If the 'discoverer' of the incident is a NYSDOH or RRDC employee, staff may assign the responsibility to complete the 24-Hour Provider Report to the most appropriate professional with knowledge of the applicant/participant and/or incident.
A participant's safety must always be the primary concern of the provider agency, Service Coordinator and the RRDC. Whatever measures appear to be reasonable and prudent to ensure the protection of a person from further harm, injury, or abuse, and to provide prompt treatment or care are taken.
Any employee, intern, volunteer, consultant, or contractor alleged to have abused a person shall be removed from immediate proximity to, or responsibility for, the participant and may not work with other participants until the investigation is completed. The immediate removal of this individual will be confirmed in the 24-hour report.
When appropriate, any waiver service provider or waiver entity may contact Adult Protective Services (APS) related to an 'Event' involving a waiver participant at any time during the SRI Reporting process. In addition, a waiver service provider, Service Coordinator or RRDS must ensure that the waiver participant is reminded of their right to notify the police as appropriate. The RRDC will assure that any known contact made by the provider with APS or with the police has been appropriately documented in the 24-Hour Provider Report, Provider Follow-Up Report, or subsequent Provider Follow-Up Reports.
Upon request, RRDC staff provides NYSDOH with any additional documentation obtained during an investigation for cases of abuse, neglect, death, or any event that is determined to be an SRI.- Upon receipt of the 24-Hour Provider Report, the Service Coordinator must contact the participant and/or legal guardian and inform them that an investigation is under way. In addition, the Service Coordinator must notify any other waiver or non-waiver provider currently involved in the service plan when there is visible evidence of injury to the waiver participant or when the incident or response to the incident may impact services or activities. Consideration of the individual's privacy should be balanced against the need to notify only waiver service providers for the purpose of service delivery. Contact with the waiver participant and/or legal guardian and/or other waiver service providers must be documented using the Service Coordinator 24- Hour Notification Report form. The Service Coordinator sends this report to the RRDC.
If the Service Coordinator is alleged to be involved in the incident, the Service Coordination Supervisor is responsible for contacting the participant and following Step 2.
All waiver service providers must ensure that during the investigation, if the person alleged to be involved in the incident serves the participant (e.g., the Service Coordinator), that person must not continue to serve the participant. The agency's supervisor must work with the participant to assure selection of an alternate individual to work with the participant. In addition, the participant must be offered the choice to select a different waiver service provider agency if one is available. The removal/suspension of this individual shall be reported in the 24-Hour report.- Within twenty-four (24) hours of receiving the 24-Hour Provider Report, the RRDC will review the form and then complete the RRDC Initial Response form. Upon entry into the database, an incident number is automatically assigned to the incident. This number must be included in all future reports and correspondence relating to the incident.
- Classification and Category Verification
The RRDC will document on the RRDC Initial Response acceptance of the original classification or, if indicated, the re-classification of the incident.
If the RRDC determines that the incident does not meet the definition of an SRI and re-categorizes the incident as a Recordable Incident, this must be noted on the RRDC Initial Response. In this instance, the case is considered CLOSED.
The RRDC also completes the RRDC Status Report form.
The RRDC will send the participant/legal guardian a close-out letter within seven (7) calendar days, indicating that the incident has been closed as an SRI and re-categorized as a Recordable Incident, which will be investigated internally by the waiver service provider.
If a waiver service provider is involved in the Recordable Incident, that agency must conduct an internal investigation and maintain documentation regarding the investigatory process and outcomes on file at the agency.
The RRDC provides a copy of the RRDC Initial Response and the RRDC Status Report to the discovering waiver service provider (if different from the investigating waiver service provider) and the Service Coordinator. The RRDC will also send a copy of the close-out letter to the Service Coordinator.- Assigning the Investigation
The RRDC will determine which waiver service provider will be responsible for conducting the investigation and will contact the waiver service provider to discuss the waiver service provider's plan for investigating the incident. The RRDC will forward the RRDC Initial Response and the 24-Hour Provider Report to the investigating waiver service provider. The RRDC will also send a copy of the RRDC Initial Response to the discovering waiver service provider (if different from the investigating waiver service provider) and the Service Coordinator.
The RRDC will provide technical support to the waiver service provider and may request assistance from DOH waiver staff in the process, if necessary. The RRDC will document contact on the RRDC Initial Response and provide the dates of the expected seven (7) calendar day and thirty (30) calendar day Provider Follow-Up Reports.
If there is concern regarding a potential conflict-of-interest or appearance of a conflict, the RRDC will assign another waiver provider who provides services to the individual to conduct the investigation.
The RRDS and/or Nurse Evaluator will conduct the investigation if the scope of the incident goes beyond one waiver service provider, there is an appearance of conflict-of-interest among the providers, the provider has demonstrated non- compliance with program manual standards or improper procedures, or the NYSDOH requests the RRDC complete the investigation.
NOTE: The RRDC must notify NYSDOH of any extraordinary events within 24 hours of receipt of the 24-Hour Provider Report.- The investigating waiver service provider must designate at least one (1) individual to be responsible for conducting a thorough and objective investigation or may choose to contract with another agency to conduct the investigation. The investigator is required to have documented experience and/or training in conducting investigations. Those conducting the investigation must not be directly involved in the incident; an individual whose testimony is incorporated in the investigation; or individuals who are the supervisor, supervisee, spouse, significant other or immediate family member of anyone involved in the investigation.
At the same time, the investigating waiver service provider must notify its Serious Incident Review Committee (SIRC) (refer to the section below - Provider's Serious Incident Review Committee (SIRC)) that an investigation has been assigned.- Within seven (7) calendar days of receiving the RRDC Initial Response and the 24-Hour Provider Report, the investigating waiver service provider must complete and submit the Provider Follow-Up Report to the RRDC, including all formal investigating agency reports, interview statements, and any contact made with the SIRC.
- Within seven (7) calendar days of receiving the Provider Follow-Up Report (7-day), the RRDC will review the form and provide a written response to the investigating waiver service provider as to whether the information received is sufficient to close the incident or whether it must remain open for further investigation, using the RRDS/NE for consultation as needed. The RRDC will complete the RRDC Status Report form indicating whether the case:
- Is re-classified (with explanation);
- Remains open (and the reason why); and/or
- Is closed, including documentation of whether the incident was substantiated or not, and why.
If left open for further investigation, the investigating waiver service provider must continue the investigation process and prepare information for submission of the completed Provider Follow-Up Report (30-day).
The RRDC will send a copy of the RRDC Status Report to the Service Coordinator and the investigating waiver service provider.
- If the investigation remains open, the investigating waiver service provider must submit a Provider Follow-Up Report to the RRDC within thirty (30) calendar days (as designated on the RRDC Initial Response) for review, with copies of all reports, statements, and supporting documentation attached.
- Within seven (7) calendar days of receipt of the Provider Follow-Up Report (30-day), the RRDC will decide to close the case or continue the investigation. The RRDC will complete the RRDC Status Report indicating whether the case:
The RRDC will send a copy of the RRDC Status Report to the Service Coordinator and the investigating waiver service provider.
- Is re-classified (with explanation);
- Remains open (and the reason why); and/or
- Is closed, including documentation of whether the incident was substantiated or not, and why.
- If further investigation is deemed appropriate by the RRDC, a Provider Follow-Up Report must be submitted by the investigating waiver service provider monthly (every thirty (30) calendar days). The due date is based on the designated thirty (30) day due date indicated in the RRDC Initial Response.
In each case, the RRDC staff has seven (7) calendar days to review the monthly report and provide a completed RRDC Status Report to the investigating waiver service provider indicating whether the incident remains open or is closed and why, including documentation of whether the incident was substantiated or not. A copy of each RRDC Status Report is forwarded to the Service Coordinator by the RRDC.
For the RRDC to consider an investigation to be closed:The RRDC reviews the final investigation report and the supporting document(s) to determine if the investigation process has been sufficient. If the RRDC has a question about the substance of the investigation it will refer the report to DOH for review and guidance. If the investigation is to remain open, the reasons for that decision must be identified by the RRDC in the RRDC Status Report along with directions for further investigative action. The RRDC returns the investigation report to the provider, requesting additional clarification and/or information.
- The final investigation report must be submitted to the RRDC, along with the Provider Follow-Up Report; and
- The provider's Serious Incident Review Committee (SIRC) must have met, reviewed the investigation, and recommended that the incident be closed. The SIRC must also provide the RRDC with suggestions post review.
No incident investigation may remain open for more than ninety (90) days from the date of the 24-Hour Provider Report without the approval of the SIRC, the RRDC and/or NYSDOH. This approval will occur in only the most atypical circumstances, e.g., criminal investigation, civil litigation.
SRI investigations pertaining to unplanned hospitalizations must be closed within the timeframe of ninety (90) days from the date of the 24-Hour Provider Report, not after discharge from the hospital.
The investigation is not closed until the RRDC determines it is closed.
When the case is deemed closed, the RRDC must complete the RRDC Status Report, sending a copy to the Service Coordinator and the investigating waiver service provider.
Once the investigating provider receives the final RRDC Status Report, it must send written notice to the participant/legal guardian within seven (7) days that the investigation has completed, indicating the final outcome without disclosing the details of the investigation. The provider must forward a copy of the letter to the RRDC and Service Coordinator.
If the case is re-classified, the investigation must continue under the same protocol as if open, until the RRDC can determine that the investigation has been completed and the case can be closed, including documentation supporting the determination.- Once the investigation is closed, the RRDC must also notify the participant/legal guardian within seven (7) calendar days via a close-out letter indicating the investigation is completed and forward a copy to the Service Coordinator. Although details of the investigation are not disclosed, the final outcome is provided to the participant/legal guardian. A summary of the investigation findings will be included in the letter.
- Any further contact with the participant will be made at the discretion of the RRDC, depending on the type and outcome of the investigation, consistent with the plan of corrective action or recommendations included in the final investigation report. When indicated, the RRDC will consult with NYSDOH waiver staff to determine what, if any, additional action is required.
All providers and the RRDC must maintain an SRI database, tracking all SRIs reported.
All documentation related to SRIs and subsequent investigations are not considered to be part of the participant's file. All information is treated with the highest level of confidentiality with limited access. NYSDOH and other authorities may request information for purposes of additional investigation or referral to authorities. Should a participant and/or their legal guardian seek the outcome of an investigation, a summary of the investigation and its outcome will be provided.
If, at any time during an SRI investigation, a waiver service provider does not comply with time frames outlined for reporting and/or has failed to comply with necessary documentation requirements, the RRDC will notify NYSDOH. This may include, but is not limited to, the waiver service provider's failure to submit any of the required documents to the RRDC (e.g., the seven (7) or thirty (30) day Provider Follow-Up Report and closure of the investigation within ninety (90) days). NYSDOH will determine an appropriate response and course of action, including but not limited to restriction of a waiver service provider's opportunity level or other plan of corrective action, such as removal from the list of available service providers. The notice to the Executive Director will outline the need for immediate attention to the incident and a plan of corrective action. Restriction of a waiver service provider's opportunity level will not be lifted until NYSDOH is assured that all deficiencies have been adequately addressed and alleviated.
Investigation of Serious Reportable Incidents
The waiver service provider assigned by the RRDC must designate at least one individual to be responsible for conducting a thorough and objective investigation. The investigator must have experience and/or training in conducting investigations.
A waiver service provider may choose to use another agency to perform the investigation. However, the investigating agency must not have any involvement or stake in the outcome of the investigation. The decision of the investigating agency is binding. The results of the investigation are presented to the SIRC, which will determine if the investigation is complete, any remaining appropriate action to take and any necessary follow-up.
People conducting the investigation must not include:
- Individuals directly involved in the incident;
- Individuals whose testimony is incorporated in the investigation; or
- Individuals who are supervised by the person being investigated, or the spouse, significant other or immediate family member of anyone involved in the investigation.
The investigating waiver service provider must utilize the statewide investigation format developed by NYSDOH for completing the investigation report.
The investigative report of an SRI must contain the following information:
- A clear and objective description of the event under investigation. This must include a description of the alleged victim, all people involved in the alleged incident, the names and contact information of all witnesses and the time and place the incident occurred;
- Details of structured interviews with all individuals involved in the events and all witnesses;
- Identification of whether this was a unique occurrence or if there is a pattern of such incidents apparently related to previous activities or reported incidents;
- The investigator's conclusions regarding whether the allegation is substantiated, unsubstantiated or whether no definitive conclusions can be reached. The reasoning behind this decision must be included; and
- The investigator's recommendations for action(s). The action(s) may be directed towards individual employees or the participant, and/or may address larger program concerns such as training, supervision, or agency policy.
Investigations by NYSDOH
As described in the NHTD Waiver Provider Agreement, NYSDOH and its representative(s) (i.e., the RRDC or others identified as such by NYSDOH) have the authority to investigate the conduct, performance and/or alleged neglect of duties of administrators or employees of any organization serving as an NHTD waiver service provider. This level of intervention will occur when there are concerns that the provider has not followed the procedures described in this policy. If the waiver service provider is found to have failed to comply with the SRI procedures described in this Program Manual, necessary steps to remedy the deficiency will be implemented.
The RRDC, provider and NYSDOH will work cooperatively with other State agencies with investigative responsibilities to ensure a thorough investigative process.
Upon discovery of an incident, any individual subject to investigation is not permitted to provide services to any NHTD waiver participant. They are to be removed from service provision until the investigation is completed.
Provider's Serious Incident Review Committee (SIRC)
Approved NHTD waiver service providers must have a Serious Incident Review Committee (SIRC) to provide oversight and review of the investigation process, evidence generated by the investigation and investigation outcomes. Independent waiver service providers, regardless of the size of their caseload, must also form a SIRC; this can be accomplished by partnering with other independent provides or existing agencies.
Providers of:
- Assistive Technology (AT);
- Community Transition Services (CTS);
- Moving Assistance (MA);
- Congregate and Home Delivered Meals;
- Environmental/Vehicle Modifications;
- Respiratory Therapy; and
- Home Visits by Medical Personnel;
are not responsible to maintain a SIRC unless the provider is also approved to provide other waiver services. These providers will utilize the SIRC in place by the Service Coordination provider.Contracted Medicaid Transportation providers will comply with the terms and conditions of their Medicaid contract.
The investigating waiver service provider is responsible for notifying its SIRC that an investigation has been initiated and that committee review is required.
1. Organization and Membership of the Serious Incident Review Committee
- The Committee may be organized on an agency-wide, multi-program or program- specific basis;
- Independent waiver service providers may partner with other independent providers or existing agencies;
- Participation of a cross section of staff, including professional staff, direct care staff and at least one member of the administrative staff is strongly recommended;
- The Committee must contain at least five (5) active members. Participation of a cross section of staff, including professional staff, direct care staff and at least one member of the administrative staff is strongly recommended. A minimum of five (5) members must be present any time the Committee convenes;
- The individual assigned to conduct investigations for the agency can be a part of the Committee but may not serve on the Committee at the same time that they are involved in an active investigation for the agency;
- The Executive Director of the agency shall not serve as a member of the Committee but may be consulted by the Committee in its deliberations;
- The Program Administrator for NHTD waiver services may be designated as a member only if the Committee is an agency-wide or multi-program committee; and
- The Committee must meet at least quarterly, and always within thirty (30) days of the date of the initial report of an SRI involving a NHTD waiver participant.
2. Responsibility of the Serious Review Committee
This Committee is responsible for reviewing the investigation of every SRI and Recordable Incident. The SIRC will evaluate whether the investigation has been thorough and objective. It will determine whether the conclusions and recommendations of the investigator comply with generally accepted professional standards in the guidelines of the NHTD waiver. The SIRC is also responsible for determining if the investigation was appropriately reported, investigated, and documented.
In addition, the Committee will:
- Assure that the waiver service provider's Incident Reporting Policies and Procedures comply with DOH NHTD Incident Reporting Policy as detailed in this Program Manual;
- Ascertain that necessary and appropriate corrective, preventive, and/or disciplinary action has been taken in accordance with the Committee's recommendations. If other actions are taken, the Committee must document the original recommendations and explain why these recommendations were revised;
- Develop recommendations, if warranted, for changes in provider policy and procedure to prevent or reduce occurrences of similar situations. These recommendations must be presented to the appropriate administrative staff;
- Identify trends in SRI (by type, client, site, employee, involvement, time, date, circumstance, etc.), and recommend appropriate corrective and preventive policies and procedures to the agency administration;
- Submit quarterly reports to the RRDC regarding SRIs. These reports must be submitted by the end of the month following the end of each quarter. For example, if the quarter runs from January 1 to March 31, the report must be received by the RRDC no later than April 30. The report must contain information of all SRI investigations conducted by the waiver service provider and identified trends that might negatively impact participants and remediation effects. For example, the agency identified a trend that warranted changes in the waiver service provider's policies, procedures, and practices. The RRDC reviews the report for regional trend analysis, makes recommendations for interventions and subsequently forwards the report with its analysis and outcomes to DOH waiver staff for further review. DOH waiver staff may also request reports at any time;
NOTE: If the provider agency has not been involved in any SRI investigations during the quarter, it is still necessary to submit a quarterly report stating no incidents occurred or were investigated; and- Report annually to the RRDC regarding SRIs, all Recordable Incidents and all corrective, preventive and/or disciplinary actions taken pertaining to identified trends. This report reflects the activities of the agency's SIRC in the investigation process, investigation outcomes, and remediation activities. It provides details on incidents by type, trends identified, and the effectiveness of any changes or improvements in policies and/or practices that occurred during the year (this report must include the name and position of each of the members of the SIRC and documentation of any changes in the membership during the reporting period).
This report must be submitted to the RRDC in each waiver service provider's region in which it is authorized to provide waiver services by January 31 of each year for the prior year. The RRDC reviews the report for regional trend analysis and makes recommendations for interventions. DOH waiver staff may also request reports at any time.3. Documentation of Serious Incident Review Committee Activity
- The chairperson shall ensure that minutes are kept for all meetings and maintained in one location;
- Minutes are to be maintained in a manner that ensures confidentiality and are not included in the participant's record;
- Minutes addressing the review of SRI shall state: (a) the identification number of the incident (provided by RRDC); (b) the participant's name and CIN; (c) a summary of the situation that caused the report to be generated, including date and type of incident; (d) Committee findings and recommendations; and (e) actions taken on the part of the agency/program as a result of such recommendations; and
- NYSDOH and the RRDC may request to review minutes at any time.
All information regarding SRI reports, including but not limited to the information collected to complete the investigation, the investigation report and minutes of the standing SIRC, must be maintained separately from the participant's records.
Recordable Incidents
A Recordable Incident is an event that does not present an immediate threat to the participant and does not meet the level of severity of an SRI but may compromise the participant's safety and well-being. These incidents warrant an internal investigation by the provider and are monitored by the provider agency's quality assurance unit for trends and outcomes. Recordable incidents are not reported to NYSDOH but may be audited as needed. Recordable Incidents are reported annually to the RRDC and are subject to review upon site visit by the RRDC and/or NYSDOH Office of Primary Care and Health Systems Management (OPCHSM). NYSDOH reserves the right to review these incidents at any time.
Recordable incidents may include, but are not limited to, the following:
Injury: any suspected or confirmed harm to a participant caused by an act or person accidental in nature or one that the cause cannot be identified which results in a participant requiring medical or dental treatment and such treatment is more than first aid. The RRDC will determine if it will be categorized as a Recordable Incident or re- classified as an SRI.
Death of a waiver participant: due to natural causes when in a treatment facility or hospice environment. Deaths due to natural causes must be reported to the RRDC within twenty-four (24) hours and the RRDC will determine if it will be categorized as a Recordable Incident.
Sensitive Situation: any situation related to a waiver participant that needs to be monitored for a potential adverse outcome. This includes events that attract media attention or inappropriate activity which could threaten the participant's ability to remain in the community. The RRDC will determine if it will be categorized as a Recordable Incident.
Emergency room visits and planned admissions that do not result in hospital admission or a prolonged stay may be determined recordable at the discretion of the RRDC.
Medication refusal that is not prolonged or results in an adverse reaction may be determined recordable at the discretion of the RRDC.
Provider policies and Procedures for Recordable Incidents
<Provider policies and procedures regarding Recordable Incidents must include an explanation or identification of the:
- Process for reporting, investigating and resolving Recordable Incidents within the agency;
- Process for identifying patterns of incidents that involve a specific participant or staff within the agency that threaten the health and welfare of participants in general;
- Staff person responsible for the oversight and assessment of Recordable Incidents within the organization;
- System for tracking the reporting, investigation and the outcome of all Recordable Incidents which includes:
- Name and CIN of the participant;
- Identity of any individuals associated with the participant at the time of the incident;
- Date(s) and time of the incident; and
- Description of Incident; and
- Action(s) taken by the waiver service provider, including recommendations for changes in the circumstances associated with the incident criteria used to determine when a Recordable Incident should be upgraded to an SRI to be reported to the RRDC.
The RRDC reviews the agency policies and procedures pertaining to SRI and Recordable Incidents during the provider enrollment process to ensure it meets the requirements set forth in the program manual and waiver application.
The RRDC may request Recordable Incidents at any time if deemed necessary, for instance, when investigating a complaint.
NHTD Complaint Process
There are a number of ways in which a complaint can be filed, or information can be sought about NHTD waiver services. These methods include, but are not limited to: phone call, email, letter, and face-to-face/in person contact. Each RRDC maintains a designated phone line to accept inquiries or complaints on behalf of waiver applicants/participants. The NHTD complaint contact list and instructions for participants on the complaint process (DOH-5729) can be found here under "Complaint Process for Medicaid Long Term Care Waivers".
To file a complaint or request information, the complainant should call the specific RRDC complaint number noted on the contact list. If the complainant requires an accommodation due to a hearing loss, they may use the TeleTYpe (TTY) numbers listed for each region or call the New York State TTY Relay Service at 711 or 1-800-662-1220, and an operator will assist them in contacting the RRDC or DOH.
If the complainant prefers to provide a written complaint via letter or email to any staff person associated with the NHTD Waiver program, email and mailing address information can also be found on the NHTD complaint contact list or the NYSDOH NHTD email box at nhtdwaiver@health.ny.gov.
At any time, the complainant can seek the assistance of a staff person such as the Service Coordinator, waiver service provider, informal supports or family member when filing a complaint. The complainant's concerns will remain confidential.
If the complaint is against the RRDC or a Medicaid service provider, the complainant may contact DOH directly. NHTD waiver staff will accept the complaint and initiate a review. If the complainant cannot call NYSDOH directly, they may call the RRDC or their Service Coordinator for assistance. They will contact the Department of Health on behalf of the complainant.
Staff responsible for the complaint follow-up will contact the complainant within two (2) business days to acknowledge receipt of the complaint and to advise that the matter is under review. Once a resolution is reached, the RRDC/DOH will contact the complainant to discuss the outcome of the investigation, pursuant to HIPAA confidentiality regulations, and will provide confirmation of the discussion.
Once the complaint investigation/review is completed, the complainant will be notified of the investigation findings as "substantiated," "unsubstantiated," or "inconclusive." This notification will also notify the complainant of any actions required to remedy the problem. Due to confidentiality requirements, copies of investigations are not distributed, but the complainant may request a summary of the investigation process and findings.
If the matter is determined by the RRDC to be a Serious Reportable Incident (SRI), the complaint will be reclassified as an SRI. The RRDC will send a letter to the complainant advising them of the reclassification of the complaint as an SRI. The protocols for SRIs will be implemented.
The RRDC will assign the investigation to the most appropriate organization to conduct the investigation, e.g., Service Coordination agency or Service Provider (ILST, CIC) or may conduct the investigation directly. The RRDC and NYSDOH have the discretion to assign the responsibility for an investigation to any organization associated with the applicant/participant or undertake its own investigation.
NYSDOH and the RRDC seek to equitably and timely address all applicant/participant concerns and issues.
Waiver Service Provider's Internal Complaint Procedure
Each waiver service provider must develop and implement a process for responding to complaints made by participants or other(s) on their behalf (e.g., guardian, family members or advocates). This process must be clearly written, easy to navigate and provided to the participant.
The complaint policy must include:
- A description of how to register a verbal or written complaint, that registering a complaint in no way jeopardizes the participant's right to receive services, who in the provider agency is responsible for receiving and responding to the complaint, and the timeframe for making initial contact with the participant (no more than two (2) days) upon receipt of complaint;
- A time frame for completing a complaint investigation and providing a written response to the complainant (maximum of thirty (30) calendar days from receipt of initial complaint);
- An appeals process, including timeframes, if the person who registered the complaint is not satisfied with the response;
- An additional appeals process, in which the complaint is forwarded to the waiver service provider's governing authority for review and recommendations; and
- Notification to the participant of their right to contact the RRDS if not satisfied with the outcome of the waiver service provider's response to their complaint.
If the RRDS is not able to resolve the issue, the RRDC forwards the matter to NYSDOH for review and final resolution.
NOTE: At any time, the participant has the right to notify their Service Coordinator that they have made a complaint to a waiver service provider. The participant may request that the Service Coordinator act as an advocate by assisting them through the complaint process with the waiver service provider. The Service Coordinator and/or participant may contact the RRDC for assistance when the complaint process does not lead to a satisfactory resolution.
There may be times when a complaint must be converted to a Serious Reportable or Recordable Incident report. A waiver service provider must inform the individual filing the complaint that this has occurred, explaining the reason for converting the complaint, and document the incident review process.
Information regarding complaints must be made available to NYSDOH upon request and during a survey of the agency.
Section XI: Quality Assurance
Introduction
In accordance with 42 CFR §441.302, in order to ensure continued operation of the NHTD Waiver Program, NYS must provide the following assurances to CMS:
- Health & Welfare: The state assures that necessary safeguards have been taken to protect the health and welfare of persons receiving services under this waiver. These safeguards include:
- Adequate standards for all types of providers that provide services; and
- Assurance that the licensure/certification standards are met for services prior to service provision and are met on the date that the services are furnished.
- Financial Accountability: The state assures financial accountability for funds expended for home and community-based services.
- Evaluation of Need: The state assures that it provides for an initial evaluation (and periodic reevaluations, at least annually) of the need for nursing home level of care.
- Choice of Alternatives: The state assures that when an individual is determined to be likely to be eligible for waiver services, the individual (or, legal representative, if applicable) is: informed of any feasible alternatives available through waiver services and other Medicaid resources and is given the choice of either institutional or home and community-based waiver services.
NYSDOH Office of Health Insurance Programs (OHIP), Division of Long Term Care (DLTC) contracts with qualified not-for-profit organizations known as Regional Resource Development Centers (RRDCs) in regions established by NYSDOH across the state for the local administration of the waiver program. Each RRDC must demonstrate experience in working with individuals with physical disabilities and/or the elderly, extensive knowledge of community-based long term care services, an understanding of person-centered planning and choice, and the ability to provide culturally competent services.
NYSDOH has the responsibility to ensure informed choice of providers for all participants. The waiver participant is the primary decision-maker in the development of goals, and selection of supports and individual service providers. The RRDC has the principal role in providing participant choice between community-based services and institutional care. This includes information regarding the applicant/participant's right to choose home and community-based care and to select and/or change waiver service providers. All providers, including those already approved to provide Medicaid State Plan or services under another Medicaid waiver, are required to be enrolled specifically as an NHTD waiver provider, and to meet all state licensure and credentialing requirements specific to the services for which they apply as established in this program manual. NYSDOH utilizes several audit functions to review and confirm these processes. These include file reviews, review of information contained on the statewide database, desk audits of billing practices, RRDC quarterly reports and meetings, participant satisfaction surveys, incident, and complaint monitoring.
As contractually stipulated, the Regional Resource Development Center (RRDC) staff determine applicants' nonfinancial eligibility for waiver participation, enroll applicants and service providers, organize local outreach and informational efforts, develop regional resources, train waiver service providers about waiver-related processes and procedures, and otherwise assist in administering, under NYSDOH's direction, the NHTD waiver in each respective region. NYSDOH provides direct oversight of the RRDCs and their operations. Each RRDC provides a quarterly report that describes the measurable outcomes identified in the contract workplan. Additionally, every month each RRDC provides a statistical report of intakes, discharges, enrollment, and service plan reviews. This information is reviewed by NYSDOH waiver staff on a daily and ongoing basis. Level of Care evaluations, service plan approvals, and service authorizations are tracked using available data base and reporting mechanisms and monitored by NYSDOH daily.
NYSDOH oversees the operation of the NHTD waiver, and the fulfillment of Regional Resource Development Center (RRDC) contractual obligations in accordance with section 366 (6-a) of the Social Service Law. NYSDOH waiver staff monitor RRDC contractors' administration of the program. NYSDOH requires that each RRDC employ one full-time Regional Resource Development Specialist (RRDS), who works exclusively on the NHTD waiver, who is designated by NYSDOH as the Lead RRDS. NYSDOH also requires that each RRDC employ a Nurse Evaluator. Program specific clauses of the RRDC contract memorialize the minimum experience and qualifications for the Lead RRDS and Nurse Evaluator. The contract further defines that any candidate under consideration for these positions must be approved by NYSDOH prior to employment. If the contractor fails to fill the vacancy with a qualified professional acceptable to NYSDOH, the contract may be terminated. With reasonable notice and written justification, NYSDOH may require the contractor to remove from the contract any employee justified by NYSDOH as being incompetent, otherwise unacceptable, or whose employment on the contract is considered contrary to the best interests of the public or the state. The contract and the NHTD Program Manual also establish the roles and responsibilities of the RRDC. The RRDC is responsible for the development, management, administration, and monitoring of the NHTD waiver on a regional level.
NYSDOH monitors the performance of the RRDCs on an ongoing basis. NYSDOH waiver staff maintain daily contact with the RRDCs. Specifically, RRDC performance is assessed through the following activities:
- NYSDOH and/or the RRDC conduct retrospective reviews of a random sample of service plans to assure quality performance of these entities. A standardized form is distributed by NYSDOH and utilized on a statewide basis. NYSDOH waiver staff monitor for correct completion of the Initial Applicant Interview and Acknowledgement (DOH-5729), Level of Care, Freedom of Choice (DOH-5728), Service Coordination Agency Selection (DOH-5731), Provider Selection (DOH-5730), Participant Rights and Responsibilities (DOH-5732) forms in the record. The service plan review is based on a statistically appropriate sample size to allow valid analysis and conclusions to be drawn from the results.
- NYSDOH waiver staff conduct RRDC annual site visits, as needed, to assess operational and administrative performance and to assure quality performance of these entities. During RRDC site visits or audit reviews, NYSDOH waiver staff review a random sample of participant records to assure the presence of a completed and signed Referral (DOH-5747), Intake (DOH-5725), Initial Applicant Interview and Acknowledgement, Freedom of Choice, Service Coordination Agency Selection, Provider Selection (DOH-5730), and Participant Rights and Responsibilities forms.
- Designated in the RRDC contract work plan is the requirement that each RRDC maintain a phone number to receive complaints. Service Coordinators are responsible to inform participants of the phone number and to review the process for filing a complaint with the participant. The complaint number is identified on the waiver participant's contact list posted in the participant's home. The complaint line is available to NHTD waiver participants, their families, and advocates for registering complaints and concerns. The complaint protocol and phone numbers are available on the NYSDOH website and can be found here. Information can be found under the header entitled "Complaint Process for Medicaid Long Term Care Waivers." Information retrieved via complaint lines is reviewed by NYSDOH to monitor complaints.
- Each RRDC completes an annual participant satisfaction survey. NYSDOH issues the format and the RRDC is responsible for the distribution of the survey to all waiver participants and receipt of responses, to assure that there is a minimum statistically appropriate sample size. Additionally, each provider conducts a participant satisfaction survey.
- NYSDOH waiver staff regularly assess RRDC performance through review of required contractor quarterly reports on provider and participant enrollment activity and other contractual obligations. NYSDOH waiver staff review and analyze the reports, evaluate contractual performance and waiver implementation trends, and may request a financial audit if expenditure discrepancies cannot be resolved or additional concerns are raised. Quarterly payments to RRDC contractors may be withheld pending the resolution of performance or compliance issues.
- NYSDOH waiver staff also meet with RRDC contractors on a quarterly basis to review NYSDOH policies, discuss community resources, review performance measures and for training.
- NYSDOH waiver staff conduct monthly statewide RRDC conference calls. Conference calls with individual RRDC contractors are conducted, as needed. These calls are used to share methods to enhance program performance, evaluate training methods, discuss participant and provider issues, and review trends in research or services related to NHTD.
- NYSDOH reviews supplemental reports completed by the RRDCs. These reports include monthly statistical data reflecting intakes, referrals, plan reviews, discharges, and enrollments. Quarterly complaint reports and quarterly reports of Serious Reportable Incident data are completed by the RRDCs. These reports reflect aggregate data from approved providers in the region who submit an individual provider report to the RRDC. In addition to providing significant information related to waiver operations, the reports help NYSDOH evaluate the RRDC's contractual performance and statewide waiver implementation trends. All Serious Incident Report information is maintained in specific data base and monitored regularly.
- NYSDOH waiver staff receive calls from waiver participants, Local Department of Social Services (LDSS) staff, and other stakeholders that contribute to NYSDOH waiver staff's assessment of the RRDC.
- A standard statewide database of participant and provider enrollment and service plan development enables NYSDOH waiver staff to evaluate and monitor program activity at the RRDC contractor level. NYSDOH staff complete random reviews of the participant database to ensure that RRDC staff are entering the required information and LOC determinations are completed per required time frames. NYSDOH waiver staff also analyze data to identify regional and statewide trends, to evaluate current policy, and to identify and implement programmatic changes.
- Each RRDC has established an internal tracking system for pertinent information such as intake, referrals, service plans, and incidents to supplement existing NYSDOH data systems.
- As established in their contracts, RRDCs are responsible for recruiting and maintaining NHTD waiver providers. NYSDOH monitors the number, type, and location of newly developed providers in each region by monitoring the database and reviewing each region's provider list on a quarterly basis. By contract, the RRDC is required to maintain sufficient provider capacity to ensure the delivery of waiver services in the region and offer sufficient participant choice in providers. NYSDOH reviews provider application packets to ensure that all appropriate transaction forms and letters of incorporation are complete, accurate, and include correctly dated information prior to submission to OHIP's Bureau of Provider Enrollment.
- NYSDOH monitors participant requests for Fair Hearings and the disposition of the case. RRDCs are monitored by NYSDOH to ensure that they have properly prepared and presented the case. This includes a review of the case summary, supporting documentation, and the reason for the action. All RRDC-related Fair Hearings are tracked by NYSDOH.
- RRDC and NYSDOH waiver staff work with NYSDOH Office of Primary Care and Health Systems Management (OPCHSM) surveillance staff to facilitate on-site surveys for a sample of providers. RRDCs are provided with a copy of the deficiency report and notification of the accepted plan of correction.
- Any RRDC contractor operational deficiency will be addressed in a timely manner, whether informally through direct communication with the contractor, or by a formal investigation. In the latter situation, NYSDOH waiver staff notify the RRDC Executive Director in writing of the findings and request a specific corrective action within ten (10) business days.
- Regional Resource Development Specialists (RRDSs) complete site visits to waiver service providers to discuss issues and to complete a random sample review of participant files. Any issues discovered by the RRDS are presented to NYSDOH waiver staff and may prompt additional review by the Office of Primary Care and Health Systems Management (OPCHSM) surveillance staff.
Record Keeping
All Nursing Home Transition and Diversion Waiver Service providers are responsible for maintaining records sufficient to substantiate all Medicaid claims.
If a provider should wish to terminate services, all participant records must be maintained for a period of six (6) years from the effective date of the provider's termination of their Medicaid Management Information System (MMIS) Provider ID.
The provider enrollment application includes a series of forms, and a signature of affirmation that the provider signs and agrees to comply with all Medicaid rules, regulations, and directives. Furthermore, to submit claims, the provider must obtain the Electronic/Paper Transmitter Identification Number and submit a notarized certification statement. The statement is renewed annually by the provider. Failure to renew the statement results in denial of the provider's claims by the eMedNY system.
The Medicaid provider is responsible for ensuring the accuracy of appropriate Medicaid data, such as the Medicaid provider ID, Medicaid recipient ID, date of service, that the service was provided to an approved waiver participant, and the rate code for the services provided. The eMedNY system adjudicates the claim and reimbursement is issued directly to the provider.
All Medicaid claims submitted to eMedNY are subject to a series of edits to ensure validation of data, including waiver participant Medicaid eligibility, enrollment of the service recipient in the waiver on the date of service, and enrollment of the waiver service provider at the time-of-service. In addition, all waiver claims paid through eMedNY are subject to all the common payment integrity edit tests, as well as those specific to waiver transactions. Claims submitted after two (2) years from the date of service will be rejected.
To ensure that claims meet the essential test that billed waiver services were provided to waiver participants, the OMIG conducts waiver provider audits to verify that all Medicaid claims for reimbursement are supported with a record of the services provided. The record includes: name of participant; date of service; staff performing the activity; time and attendance records; the start and end time of each session; a description of the activities performed during the session; the participant's service goals that are being worked on; and the participant's progress toward attaining those goals.
Upon completion of each OMIG audit, final reports are written disclosing deficiencies pertaining to claiming, record keeping, and provision of service. These final audit reports are sent to the waiver provider and are available on the OMIG website for routine review by NYSDOH waiver staff.
As part of the claim submission process, providers must sign a Claim Certification Statement which includes certification that services were furnished and records pertaining to services are kept for a minimum of six (6) years.
NYSDOH and/or the RRDC conduct retrospective reviews of a random sample of applicant/participant records in order to complete audits/quality performance reviews of these entities. Data is generated, analyzed, and summarized consistent with the performance measures established in the approved 1915(c) waiver application.
More information and details on record keeping responsibilities can be found in section VII - Record Keeping.
Cost Reporting
NYSDOH is the single State agency responsible for monitoring payments made under the New York State Medicaid program. Statewide audits of Medicaid funded programs are conducted by the Office of the State Comptroller (OSC), the Office of the Attorney General (AG), the Department of Health, and the Office of the Medicaid Inspector General (OMIG).
The cost report is utilized by all government and non-government providers to communicate annual costs incurred as a result of operating waiver services, along with related participant utilization and staffing statistics. Providers are required to file an annual Cost Report to the State within 120 (one hundred twenty) days (150 (one hundred fifty) days with a requested extension) following the end of the provider's fiscal reporting period. Providers are not required to secure an independent financial audit. If a provider fails to file a complete and compliant Cost Report within 60 (sixty) days of the due date, the State will impose a two percent penalty on the provider's Medicaid billing for the waiver.
Providers receiving $100,000 or less in Medicaid reimbursement for services provided under the NHTD waiver must submit a complete and compliant Abridged Cost Report, which must include state-approved financial documentation. All Abridged Cost Reports must contain data demonstrating that costs were incurred for the provision of waiver services to waiver eligible individuals, in accordance with their care plans.
The Bureau of Mental Hygiene Services, Hospital and Clinic Rate Setting, within the Division of Finance and Rate Setting (DFRS) in the NYSDOH Office of Health Insurance Programs (OHIP), is the office responsible for rate setting and rate oversight and cost report review.
The Centers for Medicare & Medicaid Services (CMS) requires records of providers submitting cost reports be retained in their original or legally reproduced form for a period of at least 5 (five) years after the closure of the cost report. This requirement is found at 42 CFR 482.24[b][1], which can be located online at www.ecfr.gov.
NYSDOH gives public notice required by the State Administrative Procedure Act (SAPA) and other State laws of any amendment to its regulations regarding the rate- setting methodology. SAPA requires that a Notice of Proposed Rulemaking include a name, public office address, and telephone number for an agency representative to whom written views and arguments may be submitted.
Rate information is made available to waiver participants in their service plans. Each service plan describes the frequency and duration of each service, the annual unit amounts, the rate per unit, and the total annual cost of each service. All approved waiver providers receive notice of the rates for their approved services at the time of provider enrollment.
Remediation of financial issues begins immediately upon the discovery of any impropriety. Remediation may include voiding payments, adjusting paid claims, assigning penalties, and sanctioning providers through collaboration with OMIG and the Attorney General.
Documentation of remediation activities is accomplished by the following measures: correspondence among NYSDOH waiver staff, the RRDC, participants and their parents/legal guardians, and/or service providers; amended plans of care; and the results of NYSDOH annual reviews. All such documents are maintained in the participant's case file and, as appropriate, by NYSDOH/DLTC.
Person-Centered Service Plan
In accordance with 42 CFR §441.301(b)(1)(i), a participant-centered service plan (of care) is developed for each participant. All waiver services are furnished pursuant to the service plan. The service plan describes: (a) the waiver services that are furnished to the participant, their projected frequency and the type of provider that furnishes each service and (b) the other services (regardless of funding source, including state plan services) and informal supports that complement waiver services in meeting the needs of the participant. The service plan is subject to the approval of the Medicaid agency or its designee (RRDC).
Person-centered planning assists individuals in need of HCBS services and supports to construct a plan and describe what resources they need and desire to bring purpose and meaning to their lives. The person-centered planning process conducted with the applicant/participant leads to the development of the person-centered service plan.
The following safeguards ensure that the service plan development is conducted in the best interest of the waiver participant and assurance of provider choice:
- The applicant first meets with staff from the RRDC, which is a contractual agent of NYSDOH. The RRDC staff provides information about the waiver services, waiver service providers, and explains to the applicant that he/she has a choice of all waiver service providers and encourages him/her to interview SC agencies in order to make an informed choice;
- The applicant selects a Service Coordination provider and signs a Service Coordination Agency Selection form (DOH-5727) indicating that they understand that they are entitled to choose a Service Coordination provider and choose approved providers for other waiver services;
- The Service Coordinator (SC) is responsible for providing unbiased and comprehensive information to the participant about available services and service providers. The SC provides the applicant with a list of all approved waiver providers;
- The applicant signs the Provider Selection form (DOH-5730). By signing the form, the applicant is affirming that they were given a choice of approved waiver providers;
- On an annual basis, the participant reviews and signs the Participant Rights and Responsibilities form (DOH-5732), which describes the right to choose and change waiver service providers as requested. The participant maintains a copy of the signed form, as do the RRDC and SC in the participant's record;
- The applicant's signature is required on the Initial Service Plan (DOH-5726), Revised Service Plan(s), and any addenda to the service plan. The participant's signature indicates that the participant agrees with the information that is included in the service plan, and includes the services requested and the chosen providers of the services;
- The participant has the right to change waiver providers at any time during the period covered by an approved service plan. With the assistance of their SC, the participant completes a Change of Provider Request form (DOH-5750), which is then sent to the RRDC. If the participant wishes to change SCs, the participant contacts the RRDC. The RRDC provides information to the participant about SC providers and assists the participant with completing the Change of Service Coordination Agency Request form (DOH-5731);
- The RRDS reviews each service plan to assure it meets the assessed needs of the participant and reflects waiver participant choice;
- A complaint line has been established for participants to call if they believe their rights are being violated. All calls will be investigated promptly;
- The participant is given a contact list that contains the phone numbers of the RRDC and NYSDOH in case any concerns arise;
- Participants are surveyed using a standardized survey tool to obtain feedback about the services and supports that they receive under the NHTD waiver. This survey includes questions about the waiver participant's satisfaction with the amount of choice and control that the participant has over their services and over their providers of service; and
- NYSDOH waiver staff, and/or the RRDC, conduct a random retrospective record review using a statistically appropriate sample size.
The person-centered planning process should be characterized by the following:
- Is timely and occurs at times and locations of convenience to the applicant/participant;
- Reflects cultural considerations of the individuals; and
- Is conducted by providing information in plain language and in a manner that is accessible to applicants/participants with disabilities and/or persons who are limited English proficient.
Centers for Medicare and Medicaid Services (CMS) Home and Community Based (HCB) Settings Requirements
NHTD waiver services must comply with HCB Settings requirements at 42 CFR 441.301(c)(4)-(5) and associated CMS guidance. Individuals receiving waiver services reside in their own home. Residential settings of four or more unrelated individuals are excluded. Waiver participants residing in a setting of four or more unrelated individuals at the time of the approval of the waiver application will remain under the old criteria until they move or the state transition plan is fully implemented. The services and supports available through the waiver and other sources must be sufficient to maintain the individual's health and welfare in the community. The living environment must be fully integrated into the broader community and selected by the participant. Waiver services provided outside the home should not be in a consolidated/congregate location or on the grounds or immediately adjacent to a public institution.
The setting qualities for any residential or non-residential setting where individuals live and/or receive HCBS must have the following five qualities:
- Is integrated in and supports full access of individuals to the greater community;
- Provides opportunities to seek employment and work in competitive integrated settings, engage in community life, control personal resources; and
- Ensures that individuals receive services in the community, to the same degree of access as individuals not receiving HCBS.
- Is selected by the individual from among setting options including non-disability specific settings and options for a private unit in a residential setting;
- Person-centered Service Plans document the options based on the individual's needs, preferences, and for residential settings, resources available for room and board.
- Ensures an individual's rights of privacy, dignity and respect, and freedom from coercion and restraint;
- Optimizes individual initiative, autonomy, and independence in making life choices, including, but not limited to, daily activities, physical environment, and with whom to interact; and
- Facilitates individual choice regarding services and supports, and who provides them.
Institutional settings and settings presumed to have the qualities of an institution do not meet the requirements for Medicaid home and community-based settings. Institutional settings include, as specified in the Final Rule:
- Nursing Facility;
- Institution for Mental Disease;
- Intermediate Care Facility for Individuals with Intellectual Disabilities;
- Hospital; and
- Rehabilitation, assistive living, certified residence/group home, or other congregate care/institutional setting for other than a short term.
Other locations that have qualities of an institutional setting, as determined by the Secretary are described as:
- Settings in a publicly or privately operated facility that provides inpatient institutional treatment;
- Settings in a building on the grounds of, or adjacent to, a public institution; and
- Settings with the effect of isolating individuals receiving Medicaid HCBS from the broader community of individuals not receiving Medicaid HCBS.
CMS' Guidance on Settings that Have the Effect of Isolating Individuals Receiving HCBS from the Broader Community states two (2) characteristics that alone might, but not necessarily, have the effect of isolating individuals:
- The setting is designed specifically for people with disabilities, or for people with a certain type of disability; and
- Individuals in the setting are primarily or exclusively people with disabilities and the on-site staff that provides services to them.
Settings that isolate individuals receiving HCBS from the broader community may have any of the following characteristics:
- The setting is designed to provide people with disabilities multiple types of services/activities on-site such as housing, day services, medical, behavioral and therapeutic services, and/or social and recreational activities;
- People in the settings have limited, if any, interaction with the broader community; and
- The setting uses/authorizes interventions/restrictions used in institutional settings or deemed unacceptable in Medicaid institutional settings (e.g., seclusion).
Conflict-of-Interest
The Final Rule also addresses Conflict-of-Interest in relation to the provision of HCBS. The Conflict-of-Interest language is located at 42 CFR 441.301(c)(1)(vi) and can be found at this link
To avoid Conflict-of-Interest, waiver service providers, waiver service provider staff and/or NHTD contract staff (e.g., RRDS and NE) may not have any fiduciary relationship(s) with any participants in the NHTD waiver program regardless of service provision. Examples of fiduciary relationships include: being the Representative Payee or trustee for a waiver participant's financial interests and/or receiving any financial benefit other than employment from service provision. Family (whether by blood or marriage) of waiver service provider staff and/or NHTD contract staff may apply for the waiver and receive services if they are found to be eligible and choose to participate in the NHTD waiver program.
To avoid Conflict-of-Interest, waiver service providers, waiver service provider staff and/or NHTD contract staff may not serve as a guardian, Power of Attorney, or Health Care Proxy.
To avoid Conflict-of-Interest, Service Coordinators and Service Coordination Supervisors may not complete functional assessments for individuals on their caseloads.
Due to Conflict-of-Interest federal regulation, applicants/participants may not receive service coordination and other direct waiver services from the same provider. Waiver services which are non-direct may be offered by the same provider. These include: Assistive Technology (AT), Community transitional Services (CTS), Congregate and Home Delivered Meals, Environmental Modifications (E-mods), and Moving Assistance. For example, if a waiver provider is approved to provide Service Coordination, Home and Community Support Services (HCSS) and AT, they may provide both Service Coordination and AT to the same individual. However, they may not provide both service coordination and HCSS to the same individual.
CMS Waiver Assurances
This section explains the waiver assurances required by CMS and the NHTD activities related to meeting these assurances, including performance measures and the entity(s) responsible for each activity.
A. Nursing Facility Level of Care (LOC) Assurance
- An evaluation for LOC is required for all applicants for whom there is reasonable indication that waiver eligibility is forthcoming.
42 CFR §441.303(c)(1) requires that the waiver specify the credentials (minimum qualifications) of level of care evaluators. NYSDOH requires that all UAS-NY and PRI/SCREEN assessments be completed by a Registered Professional Nurse who has completed the required training in the assessment tool.
Activities:
- The RRDC is responsible for ensuring applicants are informed about the waiver application process, including the need for a LOC evaluation. A LOC evaluation is completed using the UAS-NY or H/C PRI (if the applicant is in a nursing facility);
- As part of the application process, the Service Coordinator ensures a current UAS-NY or PRI (if applicant is in a nursing facility) is completed within 90 (ninety) days of waiver eligibility. The assessment must indicate that the applicant has attained a LOC score of 5 (five) or greater. The RRDC reviews 100% of all applications for compliance with waiver eligibility criteria, including LOC;
- If the finding of a LOC evaluation indicates a score of less than 5 (five), a second assessment will be completed. This may include an assessment by the Nurse Evaluator assigned to the RRDC. If the applicant does not meet waiver eligibility criteria the RRDC will issue a Notice of Denial of waiver services (DOH-5737). The RRDC will work with the individual to facilitate referrals to other community resources. All NODs and referral information will be documented by the RRDC. Applicants who receive a NOD Denial are informed of their right to a Case Conference and/or a Fair Hearing if they disagree with the determination as indicated on the NOD form. The Service Coordinator will also advise the applicant of the content of the NOD and ensure they understand their rights;
- NYSDOH monitors for regional trends via monthly and quarterly reports and will provide direction and request remedial action when evidence suggests that the RRDC has not implemented required protocols or timeframes; and
`- NYSDOH will complete random retrospective record reviews to assess that protocols and timelines have been maintained by the RRDC and providers.
- The LOC of enrolled participants are reevaluated at least annually or as specified in the approved waiver.
42 CFR §441.303(c)(4) requires that the state specify how often level of care re-evaluations are performed. Level of care must be re-evaluated no less frequently than annually. Re-evaluation of level of care may be performed at any time due to a change in a person's condition or service needs.
Timely re-evaluation requires that the re-evaluation is completed prior to the end date of the previous evaluation to prevent a break in the continuity of a participant's services. Eligibility for waiver services hinges on the determination of the need for a level of care specified in the waiver. If a re-evaluation is not performed in a timely manner, it may have an adverse impact on the participant.
Activities:
- Waiver participants are reevaluated at least annually for LOC through completion of the UAS-NY. This is done no later than the annual anniversary date of the last LOC determination date. The RRDC reviews 100% of all Revised Service Plans (RSP) to assure ongoing compliance with waiver standards regarding LOC determinations. A UAS-NY score of 5 (five) or greater indicates the individual requires nursing facility LOC;
- The RRDC and Service Coordinator maintain a tracking system to assure timely LOC reevaluations;
- Team Meetings to review the service plan are completed after the Initial Service Plan (DOH-5726) is approved and at least every six months. The Service Coordinator is responsible to ensure that timely meetings are held;
- In conjunction with the annual review of the participant's RSP, the RRDC confirms that the updated UAS-NY has been completed and the LOC score indicates that the participant continues to require a nursing facility level of care;
- If the individual's LOC has changed and a score of less than 5 (five) is indicated, a second assessment will be completed to confirm the score;
- If the second UAS-NY completed by the NE determines that the waiver participant meets LOC, and the waiver participant continues to meet all other waiver eligibility criteria, the waiver participant will remain eligible on the waiver. Continued eligibility is noted by the RRDC's approval of the RSP;
- If the second UAS-NY completed by the NE establishes a LOC less than 5 (five), the RRDC issues a NOD - Discontinuation from the Waiver Program (DOH-5738). The NOD informs the waiver participant of their right to a Case Conference and/or a Fair Hearing and aid continuing if they disagree with the determination. The Service Coordinator works with the waiver participant to ensure they understand their rights;
- Before a participant is discontinued from the waiver, the Service Coordinator assists the participant with referrals for other services and will facilitate transition to new providers as needed;
- The RRDC tracks data regarding all LOC reevaluations to monitor this assurance is being met;
- NYSDOH requires the RRDC to conduct an annual random retrospective record review. NYSDOH reviews the findings for trends and advises the RRDC of individual, regional, or systemic changes or improvements;
- NYSDOH requires the RRDC to conduct random record reviews of service coordination agencies during site visits to confirm LOC determinations were timely and appropriate; and
- The data gathered regarding this assurance is included in the RRDC Quarterly Reports for review by NYSDOH. Based on review of this information, NYSDOH will advise the RRDC of needed changes and remedial activities to improve practices/policies/procedures.
- The processes and instruments described in the approved waiver are applied appropriately and according to the approved description to determine participant LOC.
Eligibility for waiver services hinges on the determination of the need for nursing facility level of care (LOC) specified in the waiver application. If an evaluation/re-evaluation is not performed in a timely manner, it may have an adverse impact on the participant. In addition, the state will not be able to claim for federal participation for the services furnished to the participant, nor should a provider bill for services until waiver eligibility is restored.
Activities:
- The UAS-NY or PRI (if applicant is in a nursing facility) are designated tools for documenting LOC and can only be completed by individuals properly trained and certified by the NYSDOH, as appropriate. The completed UAS- NY or PRI must be signed/attested by the assessor, verifying the validity of the assessment. NYSDOH can verify the credentials of the qualified assessor completing the UAS-NY or PRI;
- The RRDC reviews 100% of all initial UAS-NY or PRI, and subsequent UAS-NY(s), for timeliness and to verify the waiver participant meets LOC requirements;
- Each RRDC maintains a system to track the timeliness and appropriateness of all LOC evaluations/reevaluations; and
- The data gathered regarding this assurance is included in the RRDC Quarterly Reports for review by NYSDOH. Based on review of this information NYSDOH will advise the RRDC of needed changes and remedial activities to improve practices/policies/procedures.
B. Service Plan Assurance
- Service plans address all participants' assessed needs (including health and safety risk factors) and personal goals, either by the provision of waiver services or through other means.
An effective service plan development process provides the waiver participant the opportunity to actively lead and engage in the development of the plan, including identifying individuals who will be involved in the process. The participant should be furnished with supports that are necessary to enable the participant to actively engage in the planning process, including providing information about the range of services and supports offered through the waiver in advance of service plan development and engaging individuals to assist the participant or facilitate a person-centered planning process.
The service plan is the fundamental tool for assuring the participant's health and welfare. As such, it must be subject to periodic review and update. Such reviews determine the ongoing appropriateness and adequacy of the services and supports identified in the plan and ensure that the services furnished are consistent with the nature and severity of the individual's disability and continue to be responsive to the individual's needs and preferences. A service plan must be reviewed and updated no less than annually.
Activities:
- The RRDC conducts an intake meeting prior to the development of the ISP (Initial Service Plan). This provides the RRDC with information regarding the potential waiver participant's unique strengths and needs. The information acquired by the RRDC staff during Intake is documented on a standardized Intake form (DOH-5725) which is shared with the selected service coordination agency and used to develop the ISP.
For an individual to be eligible and maintain waiver eligibility they must: meet LOC criteria, require at least one waiver service, Service Coordination (as evidenced by the service plan), and actively participate in waiver services on a monthly basis;- The Service Coordinator works with the waiver participant to establish the ISP, RSP, and any Addenda. The service plan includes the range of services needed by the waiver participant including waiver and non-waiver services. It combines all services needed to address the waiver participant's health and welfare, personal goals, preferences, and cultural traditions;
Waiver participants have the right to freely select from among any willing and qualified provider of waiver services that is "conflict-free." In order to effectively exercise this right, participants should have ready access to accessible information about the qualified waiver providers that are available to furnish the services included in the plan. Such information will be furnished as part of the service plan development process by the RRDC and/or Service Coordinator;- The waiver participant's signature on the service plan indicates they have read it, or it has been read to them, and they understand its contents and purpose. Failure to sign the service plan suggests that the individual does not agree with the content and should be addressed by the RRDC;
- The service plan should include a backup plan to address contingencies such as emergencies, including the failure of a support worker to appear when scheduled to provide necessary services when the absence of the service presents a risk to the participant's health and welfare. An effective back-up plan is one that is crafted to meet the unique needs and circumstances of each waiver participant. The information should also describe the types of back-up arrangements that are employed to ensure the waiver participant's health and welfare. A Plan of Protective Oversight (PPO) is completed with the waiver participant and the Service Coordinator during the development of the ISP and at each RSP;
- The PPO is reviewed with the waiver participant by the Service Coordinator during the development of an Addendum. Any changes in the PPO will result in the completion of a new PPO for submission to the RRDS with the Addendum. If no changes are indicated, the PPO is signed, indicating the contents remain the same, and attached to the Addendum. The PPO will be posted/available in the home to ensure access by all service providers and family members;
- All service plans are forwarded to the RRDC for final review and approval. The RRDC conducts a comprehensive review of 100% of all service plans assuring the waiver participant's goals and preferences are recognized and the plan meets their health and welfare needs;
- If the RRDC finds the service plan does not reflect the waiver participant's needs and goals, support health and welfare or follow the program's policies, immediate corrective action must be requested from the Service Coordinator and completed before the service plan can be resubmitted to the RRDS for re-review. The corrections and subsequent review will be completed in a timely manner to ensure service delivery to the individual;
- Waiver service providers assess waiver participant satisfaction by conducting annual Participant Satisfaction Surveys and by investigating all complaints/grievances received. These surveys and complaint/grievance investigations are monitored by the RRDC and are reviewed by NYSDOH. In addition to the provider satisfaction survey, the RRDC will conduct an independent survey annually;
- All calls received by NYSDOH related to the individual's services and/or providers are directed to the RRDC unless the complaint is about the RRDC. Complaint and SRI protocols will be implemented. All issues that do not require the direct intervention of NYSDOH will be referred to the RRDC for investigation/follow-up. As a result of the investigation, changes may be required to the participant's service plan and/or providers;
- NYSDOH requires the RRDC to conduct annual Participant Satisfaction Surveys. The findings of these surveys are reviewed by NYSDOH and compiled into a statewide report. A comparative review of this data over multiple years is completed to identify trends and assist in future planning of waiver services. An RRDC may be required to take remedial action regarding issues specific to a region; and
- At the direction of NYSDOH, the RRDC will complete annual random retrospective record reviews. This includes a specific review of at least 5% of approved service plans completed in the year. This data is reviewed by NYSDOH and is included in the RRDC Quarterly Reports. Should deficiencies by identified by NYSDOH, the RRDC will be required to implement a remedial plan.
- NYSDOH monitors Service Plan development in accordance with its policies and procedures.
42 CFR §441.301(b)(1)(i) requires that waiver service plans must be subject to the approval of the Medicaid agency. The administrative authority for this activity is assigned to the RRDC by NYSDOH. The RRDC has responsibility to actively oversee the operation of the waiver and ensure the health and welfare of waiver participants.
Activities:
- The RRDC is responsible to review 100% of all service plans to assure the plans are developed in accordance with waiver participant needs and goals, meet health and welfare, and reflect the policies and procedures of the waiver program. Any discrepancies in the service plan must be referred to the Service Coordinator by the RRDC for further assessment and/or modification before re-review by the RRDS for approval. All reviews and corrections must be completed in a timely manner in order to ensure service delivery;
- Each service plan submitted to the RRDC for review and approval must be signed and dated by the waiver participant to assure the waiver participant has read it or it has been read to them and that they understand its contents and purpose. Failure to sign the service plan suggests that the individual does not agree with the content and should be addressed by the RRDC;
- The RRDC may assure all service plans for individuals who are medically complex or have a high rate of services are reviewed by the NE;
- The Service Coordinator is responsible to ensure that a safe and effective service plan is established with the waiver participant's involvement and support. Plans are formulated initially and revised at least every twelve (12) months or with an Addendum, as needed. The Service Coordinator must maintain a tracking system to guarantee the timeliness of service plans;
- The Service Coordinator is responsible for facilitating Team Meetings with the waiver participant and all key parties to review the service plan for revisions to ensure the waiver participant is involved and that their preferences are reflected in the service plan. The applicant/participant may choose other interested parties to attend the meeting;
- The Service Coordinator submits the service plan to the RRDC for review to ensure the service plan is appropriate and to avoid any lapse in service;
- NYSDOH may place restrictions on waiver service providers for late submission of RSPs and/or Individual Service Reports (ISR). Restrictions may include the written notification of deficiencies, or suspension of the waiver service provider from the list of available providers, which prevents the waiver service provider from accepting new waiver participants until the deficiencies are remedied. In addition, the waiver service provider may be required to submit a plan of corrective action to address the deficiencies; and
- The data gathered during quality assurance reviews will be included in the RRDC Quarterly Reports for review by NYSDOH. The RRDC is required to evaluate and assess the need to change and/or improve policies/procedures.
- Service plans are updated/revised at least annually or when warranted by changes in the waiver participant's needs.
The service plan (plan of care) identifies the waiver services as well as other services and supports that a person needs to live successfully in the community and, therefore, avoid institutionalization. In accordance with 42 CFR §441.301 (b)(1)(i), all waiver services must be furnished pursuant to a written service plan that is developed for each waiver participant. The service plan must reflect the full range of a participant's service needs and include both the Medicaid (waiver and State Plan) and non-Medicaid services along with informal supports that are necessary to address those needs.
Billing may be claimed only for those waiver services identified in the waiver application that are included in the service plan and may not be claimed for services furnished prior to the approval of the plan or for services not included in the service plan. The RRDC will make every attempt to ensure available service providers. Waiver service providers are voluntary and may choose to not serve or discontinue services to an applicant/participant. The RRDC will make every attempt to identify a new provider within the region's resources. The waiver administering agency (RRDC) is not responsible for ensuring their availability or actual delivery. As necessary and appropriate, activities should be undertaken to link, refer or advocate for such services. When non-waiver services and supports are needed to meet the needs of the participant, their provision must be monitored during the implementation of the service plan.
Activities:
- The Service Coordinator must ensure that Team Meetings are held after initial approval of the ISP and at least every six (6) months with the waiver participant, key parties, and anyone the waiver participant requests, to review the service plan. Needed revisions and development of an RSP are discussed during the Team Meeting. The service plan will be completely re- written on an annual basis;
- An Addendum is used when there is a need for minor adjustments in the service plan and there is no significant change of status in the participant and/or living conditions. An RSP is completed when there are major changes in the types and amounts of waiver services needed to assure health and welfare;
- All RSPs and Addenda must be reviewed and approved by the RRDC prior to implementation of services;
- A waiver participant may request a review of their service plan at any time and the Service Coordinator must comply with this request. If needed, a Team Meeting will be held with all appropriate persons in attendance. The waiver participant must be provided a copy of their approved service plan;
- The Service Coordinator and RRDC track the submission and review of all service plans according to policy and procedure;
- In the event service plans are consistently delinquent, the RRDC will seek a plan of corrective action from the provider and notify NYSDOH (refer to Section V - Service Plan; and
- The data gathered during quality assurance reviews will be included in the RRDC Quarterly Reports for review by NYSDOH. The RRDC is required to evaluate and assess the need to change and/or improve policies/procedures.
- Services are delivered in accordance with the service plan, including in the type, scope, amount, duration, and frequency specified in the service plan.
Activities:
- The Service Coordinator maintains regular contact with the waiver participant to discuss the delivery of services as approved in the participant's service plan;
- Discrepancies between service plans and actual service utilization may be discovered through a range of methods including a random retrospective review by NYSDOH of service plans against claims data acquired through eMedNY, OMIG audits of waiver service providers, NYSDOH surveys and audits of waiver service providers, NHTD Complaint Line calls, waiver service provider Participant Satisfaction Surveys, and NYSDOH Participant Satisfaction Surveys regarding waiver participant experiences with service provision. If issues are discovered, further investigation will be pursued. If it is found services are not being delivered in accordance with the service plan, NYSDOH will take appropriate action which may include changes to a waiver service provider's opportunity level or termination of the Provider Agreement;
- The data gathered regarding this assurance must be included in the RRDC Quarterly Reports and appropriate remedial action implemented; and
- A provider may bill only for those waiver services that are included in the approved service plan and may not claim for services furnished prior to the development of the service or for services not included in the service plan.
- Participants are afforded choice between/among waiver services and providers.
As provided in §1915(c)(2)(C) of the Act and 42 CFR §441.302(d), individuals have freedom of choice in the selection of home and community-based services or institutional services.
Activities:
- In the Intake interview with the potential waiver participant, the RRDC staff provides waiver services definitions and service limitations;
- During the Intake interview, the RRDC staff assures individuals are offered choice of Service Coordination by providing a list of available service coordination agencies. The applicant is encouraged to interview service coordination agencies prior to selecting an agency. Upon selection of a service coordination agency, the RRDC assures the Service Coordination Agency Selection form (DOH-5727) is completed and signed by the applicant and maintained in their record. The choice of a Service Coordinator must be conflict-free;
- The applicant is informed during the initial interview and again by the Service Coordinator that at any time they may request a change in waiver service providers, including service coordination agencies. This is executed using a Change of Provider Request form (DOH-5750) or the Change of Service Coordination Agency Request form (DOH-5731). The RRDC and/or the Service Coordinator assures each applicant receives a list of available qualified and conflict-free waiver service providers. Upon selection of waiver service provider(s), the Service Coordinator assures the agency can accept the potential waiver participant and sends the Provider Selection form (DOH-5730) to the RRDC. Upon approval by the RRDC, the form is sent to the provider and the Service Coordinator both of whom maintains the completed and signed form in the applicant's record;
- The applicant/participant may request a change of provider at any time during application and ongoing service provision. The Service Coordinator will provide the applicant/participant a Change of Provider Request Form and the applicant/participant may select a provider from the list of available and conflict-free service providers. The form is sent to the RRDC. The RRDC approves the selection and returns the form to the applicant/participant and service provider;
- The Service Coordinator assures the waiver participant signs the service plan indicating their acceptance of waiver service providers and waiver services;
- On an annual basis, the Service Coordinator assures the waiver participant reviews and signs a Waiver Participant Rights and Responsibilities form (DOH-5732) which includes information regarding a waiver participant's right to choose among waiver services/providers. A copy is kept in the waiver participant's record and is given to the waiver participant. This information is reviewed during the record review process;
- During data collection from annual Participant Satisfaction Surveys, NYSDOH notes any indicators that may suggest a waiver applicant/participant may have been denied the right to choose waiver services and waiver service providers. NYSDOH will initiate action to further investigate any deficiencies or issues and implement appropriate remedial action;
- All waiver service providers are responsible for conducting annual Participant Satisfaction Surveys containing questions about "choice." These surveys may be reviewed by NYSDOH and the RRDC;
- NYSDOH directs the RRDC to conduct annual random retrospective reviews to assure Provider Selection forms have been appropriately completed and to monitor deficiencies and/or trends that may warrant changes in protocol; and
- The data gathered during quality assurance reviews will be included in the RRDC Quarterly Reports for review by NYSDOH. The RRDC is required to evaluate and assess the need to change and/or improve policies/procedures.
- Participants are afforded due process.
The opportunity to request a Case Conference and/or Fair Hearing is a fundamental protection that is afforded TO waiver participants and applicants.
Activities:
- Applicant/participants are afforded the opportunity to request a Fair Hearing when they: (a) are not provided the choice of home and community-based services as an alternative to institutional care; (b) are denied the service(s) of their choice; and/or, (c) their services are denied, reduced or terminated;
- In order to ensure that the applicant/participant is fully informed of their right to Fair Hearing, it may be appropriate and even necessary for the Service Coordinator to supplement the written information included in the Notice of Decision with a verbal explanation of the Right to Fair Hearing by discussing the notice with the applicant/participant;
- The RRDC will issue timely notification to the individual and track the status of all NODs;
- Prior to the Fair Hearing process, the RRDC will afford the applicant/participant the opportunity to discuss the action at a Case Conference;
- The RRDC is responsible to represent NYSDOH at Fair Hearings. With guidance from NYSDOH, the RRDC will compile and present the Fair Hearing packet to the Court and the applicant/participant;
- NYSDOH monitors the status of all Fair Hearings, distributes Fair Hearing decisions and notices to the RRDC, and notifies the RRDC of any compliance issues associated with Fair Hearing decisions; and
- NYSDOH tracks all Fair Hearings and monitors for trends.
C. Qualified Providers
- NYSDOH verifies that providers initially and continually meet required licensure and/or certification standards and adhere to other standards prior to their furnishing waiver services.
The waiver assurances at 42 CFR §441.302(a) require that: (a) there are adequate standards for all types of providers that provide services under the waiver and (b) that the standards must be met when services are furnished. In other words, waiver services may only be furnished by providers who have been found to meet all applicable qualifications.
In addition, it is important to keep in mind that §1902(a)(27) of the Act (as further specified in 42 CFR §431.107(b)) requires that each provider of a Medicaid service have a provider agreement in effect with the Medicaid agency. This requirement applies to the provision of waiver services and assures accountability in the provision of Medicaid services. Provider standards or qualifications are the criteria that a provider must meet in order to provide the waiver service.
It is important to keep in mind that claiming is only available for waiver services that are furnished by providers who have been determined to be qualified when the service is furnished. These providers must have specific waiver provider IDs to bill for services.
Provider-managed means that the service provider is responsible for managing all elements of service provision in accordance with the participant's Service Plan, including taking into account any directives contained within the Service Plan regarding how and when the service is to be furnished and the expressed preferences of the participant.
Activities:
- NYSDOH only enters into Provider Agreements with agencies that meet the requirements for qualified staff for specific waiver services;
- Prior to approval of waiver service providers, the RRDC conducts interviews of potential waiver service providers, which include evaluation of employee resumes to ensure employees meet the required qualifications (refer to Section III - Becoming a Waiver Provider);
- Waiver service providers are responsible for assuring their staff meets all qualification requirements set by the waiver;
- The RRDC submits recommendations to NYSDOH waiver staff regarding qualified waiver service providers;
- Character and competency verification are obtained by NYSDOH through direct contact with other state agencies, where applicable;
- Certain waiver service providers (Home and Community Support Services (HCSS)/LHCSAs) are mandated to obtain Criminal History Record reports from the U.S. Attorney General's Office for all prospective direct care and supervisory staff prior to employment other than those persons licensed under Title 8 of the Education law or Article 28-D of the Public Health Law;
- If licensure or certification is a requirement for a waiver service provider, NYSDOH verifies waiver service provider agency qualifications before approving the agency as an NHTD waiver service provider;
- The waiver service provider must report any subsequent change in status to NYSDOH and/or the appropriate RRDC (e.g., the waiver service provider is unable to maintain qualified staff and therefore is unable to provide the waiver service(s), or if license or certification status changes);
- NYSDOH Office of Primary Care and Health Systems Management (OPCHSM) surveillance staff and/or NYS Office of the Medicaid Inspector General (OMIG) staff as well as other authorized oversight agencies survey licensed and/or certified and non-licensed/non-certified waiver service provider agencies to assure they adhere to licensure and/or certification standards, staff qualifications, policies and procedures including Incident Reporting, Detailed Plans and Individual Service Reports, concerns/grievances, and service plans;
- The RRDC communicates specific concerns regarding waiver service provider practices to NYSDOH waiver staff, possibly leading to NYSDOH survey, audit by OMIG or other further action;
- If a waiver service provider is found not to have met licensure/certification requirements (including the mandatory statutes for employee criminal history record checks), DOH waiver staff reserves the right to take administrative action regarding the provider, including but not limited to, removing the provider from the list of available waiver service providers in the region;
- Many processes allow the RRDC and NYSDOH to develop an understanding of waiver service provider capabilities and competencies. This includes, but is not limited to: review of service plans, SRI reports, annual reports of waiver service provider Incident Reports, training materials, and staff interactions; and
- The data gathered during quality assurance reviews will be included in the RRDC Quarterly Reports for review by NYSDOH. The RRDC is required to evaluate and assess the need to change and/or improve policies/procedures.
- NYSDOH implements policies and procedures for verifying that provider training has been conducted in accordance with state requirements and the approved waiver.
Activities:
- NYSDOH provides ongoing training and educational programs for the RRDC staff, providers, stakeholders, and participants;
- This Program Manual sets forth areas of training and competencies required for all staff of each waiver service provider;
- The RRDC will meet with all new Service Coordinators within the first thirty days of employment with the approved provider;
- An approved provider agency is responsible for:
- Developing a written training curriculum to meet the requirements identified in this section and Section VIII - Training;
- Ensuring that individuals providing the training meet the qualifications specified;
- Providing Basic Orientation Training and the appropriate Service Specific training to all waiver providers prior to any unsupervised contact with a waiver participant;
- Providing required annual training to all service staff; and
- Documenting all training in the employee file, including all related HCBS training, seminars and conferences attended, whether offered by the provider or other entities.
- The RRDC will review and approve a new provider's training curricula prior to recommending the provider for enrollment as a waiver service provider and subsequently on an annual basis to ensure that information is updated and kept current with NYSDOH policy and procedures;
- The RRDC may participate in audit training sessions, as needed, and without prior notification to the provider;
- All provider staff must have verification of completion of current and relevant training on record with the provider agency;
- The RRDC conducts 8-10 training programs per year to waiver service providers in its region;
- Documentation of training includes training curriculum, qualifications and name of trainer, attendance records, date and place of training, goals, and evaluation tools by waiver service providers;
- During NYSDOH surveys and audits of waiver service providers, documentation is reviewed to ensure compliance with training standards. If compliance is not met, a plan of correction is required and, if unsatisfactory, administrative action by NYSDOH;
- NYSDOH and/or RRDC staff examine waiver service provider's training curriculum or training records at any time; and
- The data gathered during quality assurance reviews will be included in the RRDC Quarterly Reports for review by NYSDOH. The RRDC is required to evaluate and assess the need to change and/or improve policies/procedures.
D. Health and Welfare
- The DOH waiver staff, on an ongoing basis, identifies, addresses, and seeks to prevent instances of abuse, neglect, exploitation, and unexplained death. An incident system is in place that effectively resolves those incidents and prevents similar incidents to the extent possible.
An effective incident management system entails conducting oversight to make sure that applicable policies and procedures are being followed for the reporting of critical incidents or events and that necessary follow-up is being conducted on a timely basis. A critical element of effective oversight is the operation of data systems that support the identification of trends and patterns in the occurrence of critical incidents or events in order to identify opportunities for improvement and thus support the development of strategies to reduce the occurrence of incidents in the future.
Activities:
- This Program Manual provides the RRDC and each waiver service provider with the policies and procedures for Serious Reportable Incidents (SRIs), including: abuse, neglect, exploitation and unexplained death reporting, investigating, and monitoring of outcomes;
- The Program Manual describes the waiver service providers' requirement for a Serious Incident Reporting Committee (SIRC), which has the responsibility for the final review and oversight of SRI and Recordable Incidents and investigations, assuring appropriate and immediate corrective or disciplinary action has been taken and preventive measures are in place. Waiver service providers must submit an annual report for review to the RRDC. The RRDC analyzes the data for trends and makes recommendations for changes/improvements on a provider and regional level. This data is compiled and sent by the RRDC to NYSDOH;
- The RRDC is the primary party to provide oversight and/or training regarding the SRI policy;
- During site visits, audits, and survey of waiver providers, NYSDOH and other audit agencies evaluate incident processes to assure the waiver providers have complied with all policies/procedures regarding incidents, incident review committees, and reporting timeframes. If non-compliance is evident, the waiver provider is issued a statement of deficiencies and must submit a plan of correction to NYSDOH;
- The RRDC is the entity responsible for the management of the NHTD SRI Policy and is responsible for alerting NYSDOH of atypical or outstanding serious reports of allegations;
- To measure system performance and to identify active or potential instances of abuse, neglect and/or exploitation, NYSDOH conducts annual Participant Satisfaction Surveys to all active waiver participants, analyzes incident trends, reviews investigations, and monitors provider performance;
- Upon request, RRDC staff provides NYSDOH any additional documentation obtained during an investigation for cases of abuse, neglect, death or any event that is determined to be an SRI and/or is of particular interest or concern; and
- NYSDOH serves as a centralized collection site to receive data compiled from NHTD Complaint Line calls, SRI, provider survey outcomes, as well as quarterly and annual reports. Data is analyzed by staff for regional and statewide trends. Outcomes are reviewed with the RRDC for needed interventions which may include additional training programs, changes and/or improvements in policy/procedure, restriction of provider opportunity level, administrative action and/or termination of provider agreement.
- The DOH waiver staff established overall health care standards and monitors those standards based on the responsibility of the service provider as stated in the approved waiver.
System-wide oversight methods include gathering information about types of incidents, participant characteristics, providers, how quickly reports are reviewed and investigated, how promptly follow-up takes place, the results of investigations, and whether participants are informed of the investigation results. Oversight includes using information to reduce the occurrence of incidents in the future.
Activities:
- The Service Coordinator serves as a liaison between waiver service providers facilitating communication regarding issues pertinent to the waiver participant's health and welfare;
- The Service Coordinator provides all waiver participants with a Waiver Contact Sheet with Service Coordinator contact information for the following: waiver service providers, RRDS, and DOH waiver staff. This information is updated and is provided to the waiver participant if any entity should change. These contacts allow for easier accessibility for waiver participants to communicate concerns regarding health and welfare;
- The Service Coordinator must review with the participant, at least annually, the Participant's Rights and Responsibilities (DOH-5732) and Complaint Protocols (DOH-5729). Annual review of the Participant's Rights and Responsibilities and Complaint Protocols helps to facilitate the ongoing health and safety of the participant;
- After the approval of the ISP and at least every six (6) months thereafter, the Service Coordinator facilitates Team Meetings with the waiver participant, anyone they choose to attend, waiver service providers, and other key parties to review and revise the service plan;
- Every service plan and Plan of Protective Oversight (PPO) is reviewed by the RRDC to assure the waiver participant's health and welfare needs are met;
- The Service Coordinator conducts monthly face-to-face visits with the waiver participant, based on the participant's health and welfare needs. The Service Coordinator must complete a home visit on a quarterly basis;
- All waiver service provider staff are trained to observe and report changes in the waiver participant's behavioral, physical, and cognitive functioning and the process to follow if concerns arise;
- Waiver service providers conduct a random sample of Participant Satisfaction Surveys annually, including health and welfare issues. Findings on this information is provided to the RRDC;
- NYSDOH waiver staff monitors calls received from the NHTD Complaint Line for trends;
- All SRI reports received are investigated according to policy and procedure (refer to Section X - Incident Reporting Policy and Complaint Procedure);
- On an ongoing basis, the RRDC staff review the quarterly SRI reports for trends, as needed. RRDC staff may provide technical assistance to waiver service providers;
- Waiver service providers submit quarterly and annual reports to the RRDC to review and analyze the information in their region and provides a regional summary report to NYSDOH;
- The data gathered during quality assurance reviews will be included in the RRDC Quarterly Reports for review by NYSDOH. The RRDC is required to evaluate and assess the need to change and/or improve policies/procedures;
- If warranted, NYSDOH and the RRDC may initiate additional remedial actions, including restriction of a waiver service provider's opportunity level for providing services to participants, termination of a provider agreement or other administrative action; and
- NYSDOH provides oversight and monitors system performance on an on- going basis, based on the outcome of trend analysis, including SRI, complaints/grievances, and Participant Satisfaction Surveys.
E. Administrative Authority
- The Medicaid (NYS Department of Health) agency retains ultimate administrative authority and responsibility for the operation of the waiver by exercising oversight over the performance of waiver functions by other state and local/regional non-state agencies (if appropriate) and contracted entities.
In accordance with 42 CFR §431.10, the Medicaid agency is responsible for ensuring that a waiver is operated in accordance with applicable federal regulations and the provisions of the waiver itself.
A state also may arrange for the performance of waiver operational and administrative functions by contracted entities, in this case, the Regional Resource Development Centers (RRDCs). NYSDOH must provide consistent, uniform administration and operation of the waiver across all geographic areas where the waiver is in operation.
Activities:
- NYSDOH maintains overall authority and responsibility for the operation of the waiver by exercising oversight of the performance of waiver functions by contractors, such as the RRDC staff;
- In order to effectuate a strong, compliant service delivery mechanism, NYSDOH has established clear and strong lines of communication between the RRDCs, providers, stakeholders, and participants;
- NYSDOH manages and oversees the performance of the contractors (RRDC) through annual random retrospective reviews of the service plans, NHTD Complaint Line calls, quarterly and annual reports, complaints/grievances, and annual on-site visits. If NYSDOH determines a decision by the RRDC staff does not reflect established policy, corrective actions will be initiated;
- NYSDOH has the final authority regarding acceptance/denial of an applicant and discontinuance of a waiver participant from the NHTD waiver;
- NYSDOH and other Medicaid authorities have the final authority regarding approval and termination of waiver service providers;
- NYSDOH waiver staff maintains open discussion with waiver participants, RRDC staff, waiver service providers, Local Department of Social Services (LDSS), participant advocates, and other community-based organizations who serve seniors and people with disabilities, to understand and evaluate the functioning of contractor's staff;
- NYSDOH gathers, evaluates, and monitors data collected from reports, audits, and surveys and requires a Plan of Correction when trend analysis and evidence indicate the need for program changes or improvements;
- NYSDOH receives complaint calls from waiver participants, stakeholders, providers, and others;
- NYSDOH conducts Quarterly RRDC Meetings, monthly conference calls, and daily interaction to review policies, network, present new policies/procedures, discuss regional trends, and address waiver issues; and
- Any data gathered regarding quality assurance reviews is included in the RRDC quarterly, monthly, and ad hoc reports for review by NYSDOH. Program remediation is at the direction of NYSDOH in consultation with RRDC.
F. Financial Accountability
- Claims are coded and paid for in accordance with the reimbursement methodology specified in the approved waiver and only for services rendered.
NYSDOH's audit system(s) ensure the integrity of provider billings for Medicaid payment of waiver services, including the methods, scope and frequency of audits conducted by the state. This includes, but is not limited to, testing a sample of provider billings to ensure that they are properly supported by documentation of the actual provision of waiver services or the review of provider cost accounting systems to ensure that, when rates are based on provider costs, costs have been properly recorded and do not include unallowable expenses.
Activities:
- The claims for federal financial participation (FFP) for NHTD waiver services are subject to the same policies and procedures that the NYSDOH Office of Health Insurance Programs (OHIP), through the eMedNY system, uses to claim federal financial participation for all other Medicaid services;
- Each waiver service provider is assigned a separate waiver service provider identification number in eMedNY to assure only qualified waiver service providers are billing for services. Each waiver service is assigned a unique rate code. Each waiver participant is assigned a unique program code (Restriction/Exemption/RE code 60);
- Upon approval of the waiver participant's ISP, a waiver participant Restriction/Exception Code 60, which is unique to the NHTD waiver, is assigned by the LDSS to assure that claims are paid only for individuals enrolled in the waiver on the date of service;
- All Medicaid claims submitted to eMedNY are subject to a series of edits to ensure validation of data. These edits include: whether the waiver participant is Medicaid eligible, whether the individual was enrolled in the waiver on the date of service, and whether the waiver service providers are enrolled waiver service providers;
- Billing validation as conducted by OMIG and/or NYSDOH entails using the Medicaid Management Information System (MMIS) to validate claims (e.g., verifying that the individual for whom the billing was made was eligible for Medicaid on the date of service). Additionally, NYSDOH and/or OMIG verify that the service billed was included in the participant's service plan. For the NHTD waiver, billing validation processes are conducted post-payment (e.g., surveillance and utilization review), including verification that the service billed was actually rendered. When a validation process that is conducted post- payment reveals a problem with a billing, NYSDOH removes the problem billing from its claim for FFP and recoups the inappropriate payment from the provider;
- NYSDOH performs a random retrospective review of claims to service plans and compares services identified in the service plan to billed claims. This review verifies waiver services are provided as authorized in the service plan. The NYSDOH waiver reviews paid claims in the eMedNY system to service plans according to the plan period. Discrepancies may be referred to OMIG. A comparable more in-depth audit is completed by OMIG;
- The responsibilities of the OMIG include, among other responsibilities, the Medicaid audit function. OMIG has developed and implemented an audit protocol in conjunction with NYSDOH and audits providers as established in its annual audit plan. Additionally, NYSDOH may present concerns regarding provider performance to OMIG for review and consideration;
- Upon completion of each audit, final audit reports are presented to identify deficiencies pertaining to claiming, record keeping, and provision of service. Providers participate in exit meetings and are offered the opportunity to remedy or challenge issues. OMIG audit reports are publicly posted; and
- Remediation efforts may include additional waiver service provider audits by OMIG, NYSDOH provider surveys, RRDC site visits, restriction of waiver service provider opportunity level, administrative action and/or termination of Provider Agreements.
- Rates remain consistent with the approved rate methodology throughout the five-year waiver cycle.
State financial oversight exists to assure that claims are coded and paid for in accordance with the reimbursement methodology specified in the approved waiver. NHTD waiver rates are established on a Fee for Service (FFS) basis. Billing for waiver services flow directly from providers to the state's claim payment system: eMedNY.
Activities:
- The Bureau of Mental Hygiene Services, Hospital and Clinic Rate Setting, which is housed within the Division of Finance and Rate Setting (DFRS) in the NYSDOH Office of Health Insurance Programs (OHIP), is the office responsible for rate setting and rate oversight;
- Cost reporting for non-profit waiver services will be subject to review. A standard cost reporting tool is used to reconcile the Medicaid payments for waiver. The process will demonstrate that NYS' costs are economic and efficient;
- Waiver service providers submit a cost report to NYSDOH annually;
- The Cost Report will be submitted to CMS within sixteen (16) months after the close of the reporting period;
- The use of retrospective reimbursement, using service provider cost requires a reconciliation of any and all interim payments to the final allowable Medicaid cost for each rate year; and
- If a provider has not filed a complete and compliant annual cost report for the reporting period, the provider will be considered delinquent.
Section XII: Glossary of Terms
Glossary of Terms for the NHTD Waiver Program
Abbreviation Definition AAA Area Agencies on Aging ACCES-VR Adult Career and Continuing Education Services-Vocational Rehabilitation ADA Americans with Disabilities Act ADL Activities of Daily Living AG Attorney General ALJ Administrative Law Judge ALP Assisted Living Program APS Adult Protective Services ADRC Aging and Disability Resource Center ASPEN Automated Survey Processing Environment AT Assistive Technology CBIC Common Benefit Identification Card CBVH Commission for the Blind and Visually Handicapped CDC Centers for Disease Control CDRS Certified Driver Rehabilitation Specialist CDBG Community Development Block Grant CDPAP Consumer Directed Personal Assistance Program CDPAS Consumer Directed Personal Assistance Services CFCO Community First Choice Options CFR Code of Federal Regulations CFR Consolidated Fiscal Report CHHA Certified Home Health Agency CIC Community Integration Counseling CIN Client Identification Number CMS Centers for Medicare and Medicaid Services CMCM Comprehensive Medicaid Case Management CNA Certified Nursing Assistant COI Conflict-of-Interest CTS Community Transitional Services DLTC Division of Long Term Care DME Durable Medical Equipment DOH Department of Health E-mods Modifications Services eMedNY Electronic Medicaid of New York EMS Emergency Medical Services EVQ Employee Verification of Qualifications EVV Electronic Visit Verification FEIN Federal Employee Identification Number FCC Federal Communications Commission FFP Federal Financial Participation GDIT General Dynamics Information Technology GED General Education Diploma HARP Health and Recovery Plan HBV Hepatitis B Virus HCV Hepatitis C Virus H/C PRI Hospital and Community Patient Review Instrument HCBS Home and Community-Based Services HCSS Home and Community Support Services HEAP Home Energy Assistance Program HHA Home Health Aide HIPAA Health Insurance Portability and Accountability Act HIV Human Immunodeficiency Virus HUD U.S. Department of Housing and Urban Development IADL Instrumental Activities of Daily Living ICF/IDD Intermediate Care Facility for Individuals with Developmental Disabilities ILC Independent Living Center ILST Independent Living Skills Training Services ISP Initial Service Plan ISR Individual Service Report LCM Local Commissioners Memorandum LDSS Local Department of Social Services LHCSA Licensed Home Care Services Agency LOC Level of Care LOI Letter of Intent LTC Long Term Care MA Medicaid MEVS Medicaid Eligibility Verification System MD A Doctor of Medicine MLTC Managed Long Term Care MMIS Medicaid Management Information System NYAIL New York Association of Independent Living NE Nurse Evaluator NFLOC Nursing Facility Level of Care NHTD Nursing Home Transition and Diversion Waiver NYCRR New York Code of Rules and Regulations NYS New York State NYSDOH New York State Department of Health NYSOFA New York State Office for Aging NOD Notice of Decision OHIP Office of Health Insurance Programs OIG Office of Inspector General OMH Office of Mental Health OMIG Office of Medicaid Inspector General OPCHSM Office of Primary Care and Health Systems Management OPWDD Office for People with Developmental Disabilities OSC Office of the State Comptroller OT Occupational Therapy OTDA Office of Temporary and Disability Assistance PACE Program of All-Inclusive Care for the Elderly PBIS Positive Behavioral Interventions and Supports PCA Personal Care Aide PCP Person-Centered Planning PCS Personal Care Services PERS Personal Emergency Response System PHI Protected Health Information POE Point of Entry PPO Plan for Protective Oversight PT Physical Therapy QA Quality Assurance QI Quality Improvement QIS Quality Improvement Strategy QMP Quality Management Program RBU Rate Base Unit R/E Restriction Exception RHCF Residential Health Care Facility (nursing home) RN Registered Professional Nurse RRDC Regional Resource Development Center RRDS Regional Resource Development Specialist RSP Revised Service Plan SAPA State Administrative Procedure Act SC Service Coordinator SDP Structured Day Program Services SIRC Serious Incident Reporting Committee SNF Skilled Nursing Facility SP Service Plan SRI Serious Reportable Incident SS Social Security SSI Social Security Income SSDI Social Security Disability Insurance SSI Supplemental Security Income TBI Traumatic Brain Injury TDD Telecommunications Device for the Deaf TOT Training-Of-Trainer TTY TeleTYpe UAS-NY Uniform Assessment System for New York USDA United States Department of Agriculture WMS Welfare Management System
Section XIII: RRDC Regions Map