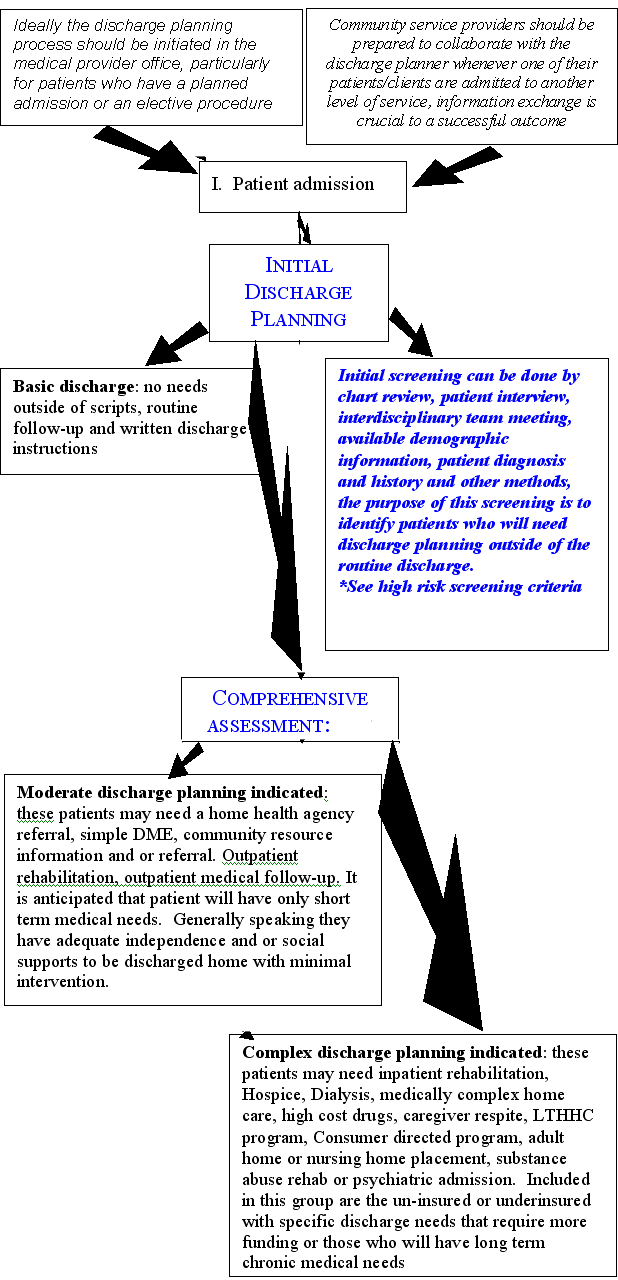
Suggested Model for Transitional Care Planning
Transitional Care Planning is a patient-centered, interdisciplinary process that begins with an initial assessment of the patient's potential needs at the time of admission and continues throughout the patient's stay. Ongoing consultation with the patient care team and reassessment of the patient's changing medical functional, social and cognitive capabilities assures that the comprehensive needs of the patient are addressed. Patients and families are apprised of the appropriate community resources available and encouraged to participate in all phases of the transitional care planning process. Referral mechanisms with community providers occur in a timely, systematic fashion in order for the patient to gain access to identified resources. The process concludes with the coordination and implementation of services and transition to the least restrictive level of care in keeping with the individual's wishes.
- Transitional Care Planning considers the patient's medical, physical, cognitive, economic and emotional strengths and abilities as well as their available support system
- Assessment of the patient's level of functioning prior to admission provides insight into resources available post discharge
- Ongoing collaboration between the patient, family and the interdisciplinary team provides an invaluable link, which facilitates the process of informed decision making
- Patients and families will receive verbal and written information of the range of services and available options available in the patient's community
- Patients and families will be given the opportunity to select the providers of services whenever possible
Initial Discharge Screen
These questions should allow the discharge planner to determine whether the patient is likely to need a more comprehensive assessment
- Was the patient independent prior to admission?
- Will this current episode of illness impact the patients independence
- Short term or long term?
- Does the patient have adequate informal supports to manage any loss of independence?
- Does the patient have adequate resources to provide for post discharge (Hospital, Nursing Home, Certified Home Health Agency) needs, such as meds, equipment, rehab, or follow up treatment? (Insurance, Private funds, Medicare, Medicaid).
- If the patient had prior home care services, were they adequate? Are they likely to be adequate after discharge?
- Are there any special requirements to access?
- Is there a different level of care needed and is there a different payor because of hospital stay?
- Has this patient had multiple hospital admissions?
High Risk Screening Criteria
Patients who fall into any of these categories should be targeted for a comprehensive assessment
- Over the age of 70
- Multiple diagnosis and co-morbidities
- Impaired Mobility
- Impaired self care skills
- Poor cognitive status
- Catastrophic injury or illness
- Homelessness
- Poor social supports
- Chronic illness
- Anticipated long term health care needs (e.g.,new diabetic)
- Substance abuse
- History of multiple hospital admissions
- History of multiple emergent care use
Comprehensive assessment
Patients who are identified as High Risk or those for whom a more comprehensive assessment is indicated should be evaluated using the following criteria
The screening process is dynamic and may include other information not listed below.
- Functional assessment (the patients ability to perform ADL's and IADL's)
- Cognitive assessment if indicated
- Who are the patient's informal supports?
- What are the abilities of the informal supports?
- What is the availability of the informal supports?
- What is the patient's living arrangement? (home, apartment, with family, congregate living, homeless)
This should include a description of the setting, such as stairs to enter, wheelchair accessibility, functional plumbing, heat, cooking facilities - What is the patient's understanding of their illness?
- Is the patient capable of participating in his or her own discharge planning, if not, do they have someone who can represent them in the process?
- What are the patient's goals for discharge?
- What does the patient need to achieve functionally to achieve these goals?
- What services might be available to the patient to achieve these goals?
- What services did the patient have prior to admission?
- Does the patient have a preference for service provider?
- Does the patients insurance have a preferred provider network?
- Does this patient have insurance or funds to pay for necessary care, if not what resources are available to them?
- Is the patient understanding of risks/benefits associated with their choices?
- Is there a history of non-compliance, which impacts the ability to be managed at home?
* This document refers to patient rather than individual/consumer because it is intended to be used by Hospitals for their patients.
Screening Andassessment Flow Chart