Antibiotic Resistance

NYS STop Antibiotic Resistance Roadmap
Press Release: New York State Department of Health Issues Poster to Raise Awareness About Proper Antibiotics Use in Recognition of U.S. Antibiotic Awareness Week
Poster: Keep Andy-Biotic Strong… don’t use antibiotics wrong! (PDF) | Poster Order Form (PDF)
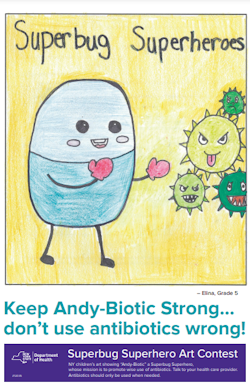
Superbug Superheroes Art Contest
The Story of AndyBiotic (PDF)
- Grade 3
Art Contest Drawing (PDF)- First place – (Cameron, Tarrytown, NY, attends Transfiguration School)
- Second place – (Emma, Yonkers, NY, attends St. Barnabus Elementary School)
- Third place - (Maxwell, Tarrytown, NY, attends Transfiguration School)
- Grade 4
Art Contest Drawing (PDF)- First place – (Lyla, Rome, NY, attends Westmoreland Upper Elementary School)
- Second place – (Addison, Franklinville, NY, attends Franklinville Elementary School)
- Third place - (Lillyana, Barker, NY, attends Pratt Elementary School)
- Grade 5
Art Contest Drawing (PDF)- First place – (Colleen, Yonkers, NY, attends St. Barnabus School)
- Second place – (Angelo, Bronx, NY, attends St. Barnabus School)
- Third place - (Miles, Nassau, NY, attends Donald P. Sutherland Elementary School)
What is antibiotic resistance?
Antibiotic resistance occurs when antibiotics (medicines used to treat infections caused by bacteria) don't work anymore. Antibiotics can be life-saving, but bacteria are becoming more resistant. If we're not careful about how we prescribe and use the antibiotics we've relied on for years, they might not work for us in the future.
What is antimicrobial resistance?
Antibiotic resistance is part of a broader threat called antimicrobial resistance, which is resistance to medicine used to treat all types of infections, including bacteria, parasites and fungi, for example.
Why is it happening?
Antibiotic resistance happens when antibiotics are inappropriately prescribed (for example, for viral infections, where they are not effective), or when inappropriately used (for example, using antibiotics without a health care provider's guidance). It can also result from inappropriate use of antibiotics in animals. Antibiotic resistant bacteria can then spread and become more common in the community.
Bacteria are only one type of germ that causes infections. Infections are also caused by viruses. Since antibiotics don't work against infections caused by viruses, using antibiotics for these infections, such as the common cold, the flu, bronchitis, most coughs, and most sore throats, can lead to antibiotic resistance. Antibiotics kill the healthy bacteria in the gut, allowing more harmful bacteria, such as C.difficile, to grow in its place. Taking antibiotics increases your risk of getting an antibiotic-resistant infection later.
Why should we care?
When bacteria become resistant, medicines may no longer work and infections can become difficult or impossible to treat. Antibiotic resistant germs can spread from one person to another leading to more antibiotic resistant infections.
How bad is the problem?
The Centers for Disease Control and Prevention (CDC) estimates that each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics, and at least 23,000 people die each year as a direct result of these infections. We are approaching a time when once easily-treated infections are no longer easy to treat or may be untreatable because of antibiotic resistance. As Dr. Thomas Frieden, head of the CDC, puts it, "The medicine cabinet is empty for some patients. It is the end of the road for antibiotics unless we act urgently."
Can animals spread antibiotic resistance?
- Antibiotic use in animals and agriculture can lead to antibiotic resistance in bacteria that can spread to humans and other animals through direct contact or contaminated food. Therefore, appropriate use of antibiotics is an important part of veterinary practice to protect animal and human health. Safe food handling, storage, and preparation is something everyone should practice to prevent illness.
What can you do about this health threat?
- Remember, antibiotics don't work for viral infections like the common cold, most coughs, and most sore throats. Taking antibiotics when they don't work can do more harm than good by causing stomach upset, diarrhea, or allergic reactions.
- Do not pressure your health care provider to prescribe antibiotics if they diagnose you with a viral infection.
- If your provider does prescribe antibiotics, make sure you take the entire course of medicine, even if you start to feel better. Do not stop unless your provider tells you it's OK to stop.
- Do not share antibiotics prescribed for you with another person.
- Don't save old doses of antibiotics for another time when you have an infection. Extra doses should be discarded as soon as you stop taking the medicine. The NYS Department of Environmental Conservation has information for households on drug disposal options.
What is the New York State Department of Health (NYSDOH) doing about this health threat? A few examples of key programs to address antibiotic resistance in NYS include:
- The New York State Department of Health (NYSDOH) has launched the NYS Antimicrobial Resistance Prevention and Control Task Force, which is a partnership of federal, state and local agencies. The mission of the NYS Antimicrobial Resistance Task Force is to develop new initiatives, create partnerships, and enhance collaboration to reduce the burden of illness due to antimicrobial resistance in NYS and improve the health and wellbeing of all New Yorkers. The task force will develop and implement a statewide strategic approach and a report of recommendations to combat antimicrobial resistance in New York. The work of the Task Force will shape New York's future response to this growing health threat.
- NYSDOH's Wadsworth Center is one of only seven CDC-designated Antimicrobial Resistance (AR) Regional Laboratories in the US. These strategically placed laboratories will have special capacity to rapidly detect and identify emerging antibiotic threats.
- NYSDOH is a state partner in the CDC's "Get Smart (Know When Antibiotics Work)" Campaign to educate health care providers and patients about antibiotic resistance and appropriate antibiotic use.
Information for Health Care Providers
- Talk to Your Health Care Provider About Antibiotics (PDF)
- CRE Information Card (PDF)
- Educating Patients About Antibiotic Resistance
- American College of Physicians/CDC Advice: Appropriate Antibiotic Use for Acute Respiratory Tract Infection in Adults
- Infectious Diseases Society of America Guidelines
- IDSA Antimicrobial Agent Use
- NYSDOH "Smart Use Guarantee" Poster
- "Smart Use Guarantee" Patient Postcard
- Adult and Pediatric Antibiotic Prescribing Guidelines - 8.5 x 11 (PDF, 4pg)
- Adult and Pediatric Antibiotic Prescribing Guidelines - 11 x 17 (PDF, 2pg) - Should you desire a hard copy version of the Antibiotic Guideline pocket reference (4.25" X 6.25", folded, accordion style) please email marybeth.wenger@health.ny.gov
- NYSDOH Hospital Acquired Infections Report
- NYS Get Smart Toolkit for Health Care Providers
- Viral Prescription pad (English)
- Advisories from the CDC
- CDC: Antibiotic- Resistant Gonorrhea