Provider Enrollment Feedback Sessions
ARCHIVE
- FAQs is also available in Portable Document Format (PDF)
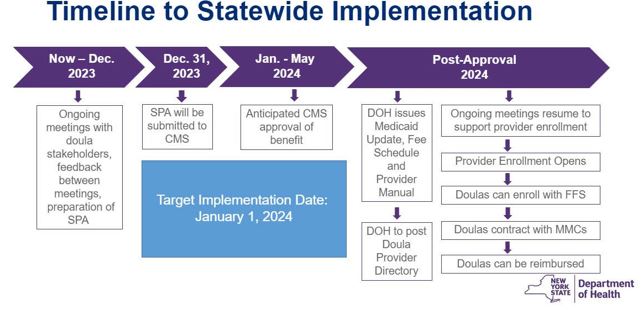
1. What is the projected implementation timeline for the New York State Medicaid doula services benefit?
The target implementation date for coverage of doula services under New York State Medicaid is January 1, 2024. A Medicaid State Plan Amendment (SPA) is required, and implementation of this new benefit is pending approval of the SPA from the federal Centers for Medicare & Medicaid Services (CMS).
2. What is a Medicaid State Plan Amendment (SPA) and why is it needed for doula services to be covered by Medicaid in New York?
The Medicaid State Plan is the official agreement between New York and the Federal government describing how New York administers its Medicaid program. The Medicaid State Plan defines groups of individuals to be covered, services to be provided, and methods for providers to be reimbursed. When a state is making a change to the Medicaid program policies or operations, a SPA must be submitted to CMS for review and approval.
3. When will doulas be able to receive reimbursement through New York State Medicaid for providing services to Medicaid-enrolled individuals?
Doulas will need to enroll as New York State Medicaid providers. At this time, only doulas who have participated in the Doula Services Pilot in Erie County have been able to enroll as New York State Medicaid providers, and enrollment is not yet open to additional doulas.
Medicaid provider enrollment will begin when the statewide policy is final and approved, and reimbursement for doula services will be available after the federal approval of the SPA.
A Medicaid Update will be published to announce the start date of availability of Medicaid reimbursement for doulas services provided by Medicaid-enrolled doulas. Medicaid Updates are published here.
4. What is the process for a doula to enroll as a provider with New York State Medicaid?
Doulas will first have to enroll with the New York State administered Medicaid program, "Medicaid fee-for-service (FFS)". Once enrolled as a Medicaid provider, a doula can then reach out to Medicaid Managed Care Organizations (MCOs) to apply to join the MCO's doula provider network. Most New York State Medicaid enrollees are members of (covered by) Medicaid MCOs. To be reimbursed for services provided to a Medicaid MCO member, a doula must be in the provider network of the MCO.
5. How are doulas being engaged in the New York State Medicaid doula services planning and design processes?
The NYS Medicaid team is hosting a series of virtual Medicaid Doula Town Hall meetings to discuss proposals for the doula services benefit and receive feedback and input from doulas and doula stakeholders. Doulas from the Medicaid Doula Services Pilot program in Erie County, as well as individual doulas, doula organizations, and doula advocates across the state have offered support, guidance, and information in the development of the benefit. A comprehensive evaluation of the Medicaid Doula Services Pilot program is being completed and findings will be considered in the design and planning for the benefit.
6. How can I participate?
To register for upcoming virtual Medicaid Doula Town Hall meetings, visit this website. Recordings and presentations from previous Town Hall meetings are also available at this link. The meetings are two hours long and held at various times of day and days of the week to accommodate different schedules. If you can't attend, you can send feedback to doulapilot@health.ny.gov.
Pilot
- Where can we find more information about the New York Medicaid Doula Pilot program?
To learn more about the Medicaid Doula Pilot program in Erie County, including eligibility, scope of services, enrollment, and evaluation, please visit this website.
Last updated October 2023