Ambulatory Patient Groups Implementation
Diagnostic & Treatment Centers and Free Standing Ambulatory Surgery Centers
August 18, 2010
- Presentation also available in Portable Document Format (PDF)
Presentation Outline
- Status of APG implementation in D&TCs
- APG retro–billing policies
- Overview of APGs & ancillary, laboratory and radiology billing policies
- Visit vs. episode payments
- Special payment rules and APG carve–outs
- 2010 APG Grouper Pricer updates
- APG resource materials for providers
- Questions and answers period
Speakers
Gregory Allen, Director
Division of Financial Planning and Policy
Office of Health Insurance Programs
Ronald Bass, Director
Bureau of Policy Development and Coverage
Division of Financial Planning and Policy
Office of Health Insurance Programs
Maria Payne, Asst. Director
Bureau of Strategic Planning and Policy Analysis
Division of Financial Planning and Policy
Office of Health Insurance Programs
Benefits to D&TCs
- APGs will replace outdated D&TC threshold payment rates (frozen in 1994)
- Additional $50 million in Medicaid revenue for D&TCs when fully annualized (only $12.5M currently approved by CMS, the balance is pending approval)
- Increased investment in community clinic rates will cover approximately 90% of average D&TC costs
- Approximately 90% of D&TC clinics stand to be positively or neutrally impacted by converting to APGs
- 2010 APG weight increases, particularly for low intensity services (e.g., +95% for physical therapy), will further benefit rehab providers
- Additional payments and payment enhancements for:
- weekend/evening hours
- diabetes/asthma educators
- medical homes
- smoking cessation counseling
- cardiac rehabilitation
- Mental health counseling by licensed social workers
New York Has Invested Over $600 M in Ambulatory Care
| (Gross $ in Millions) PROGRAM (effective date) |
Approved in SFY 08/09 Budget (Full Annual) |
Additional Funding Approved in SFY 09/10 Budget (Full Annual) |
Total Investment SFY 10/11 (Full Annual) |
|---|---|---|---|
| Hospital Programs | $178.00 | $92.00 | $270.00 |
| Outpatient Clinic (12/1/2008) | $88.00 | $92.00 | $180.00 |
| Ambulatory Surgery (12/1/2008) | $40.00 | $0.00 | $40.00 |
| Emergency Room (1/1/2009) | $50.00 | $0.00 | $50.00 |
| Freestanding Programs | $12.50 | $37.50 | $50.00 |
| Freestanding Clinic | |||
| Ambulatory Surgery Centers | |||
| Primary Care Investments | $38.00 | $90.10 | $128.10 |
| Asthma and Diabetes Education (1/1/2009) | |||
| Expanded "After Hours" Access (1/1/2009) | |||
| Social Worker Counseling (pending CMS approval) | |||
| Smoking Cessation (1/1/2009) | |||
| First Time Mothers/Newborns (4/1/2009) | |||
| Cardiac Rehabilitation (1/1/2010) | N/A | ||
| SBIRT (4/1/2009) | N/A | ||
| Smoking Cessation (1/1/2010) | N/A | ||
| Primary Care Standards/Medical Home (1/1/2010) | N/A | ||
| Adirondack Medical Home (pending CMS approval) | N/A | ||
| Physicians | $120.00 | $68.00 | $188.00 |
| Mental Hygiene Enhancements | N/A | $2.70 | $2.70 |
| Detoxification Services Reform (4/20/2009) | |||
| TOTAL | $348.50 | $290.30 | $638.80 |
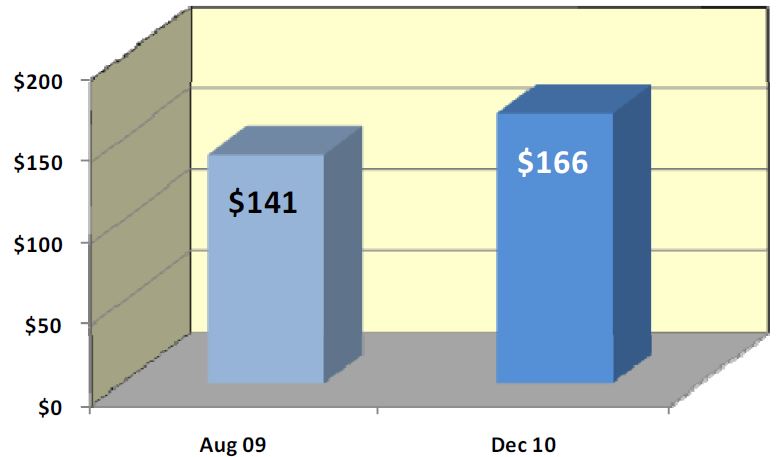
Impact of $50M Investment:
Diagnostic & Treatment Center Rates Up 18%
Retro–Billing for APG Claims
APG Retro–Billing for DTCs
- Providers may submit claims using APG rate codes starting July 18, 2010.
- Detailed billing guidance was issued July 1st
- DOH will end date the current D&TC and Ambulatory Surgery Center (ASC) rate codes December 1, 2010
- All D&TCs and most free–standing ASC claims (except for those ambulatory surgery claims that include both primary and secondary procedures during the same visit–––see next slide) received and processed by eMedNY prior to August 1, 2010, for dates of service on or after September 1, 2009, will be automatically reprocessed by eMedNY through the EAPG grouper/pricer resulting in an adjustment of payment based on the new APG payment methodology.
- The new APG base rates were loaded to the system and available for billing beginning on July 18, 2010.
- The "lock down" date for claims reprocessing will be August 1, 2010. Claims submitted to eMedNY on or after August 1, 2010 using the old rate codes will not be automatically reprocessed under the APG rate codes by eMedNY. Providers will have to reprocess those claims using the APG rate codes prior to December 1, 2010 (when the old rate codes are zeroed out).
- Providers and vendors will not have to resubmit most claims that were submitted prior to August 1, 2010 to receive the retroactive payment adjustment.
- As it may take eMedNY up to three and a half months to process the retroactive adjustments, providers may opt to adjust claims on their own when APG rate codes become active.
APG Retro–Billing for Free–standing Ambulatory Surgery Centers
- Claims for dates of service on or after September 1, 2009, that have only one surgical procedure on the claim will be automatically reprocessed through the APG Grouper Pricer and the payments will be adjusted accordingly.
- Claims for dates of service on or after September 1, 2009, which involved both primary and secondary surgical procedures during the same visit (i.e., rate code 1804 & 1805 claims) will not be able to be reprocessed.
- Providers will have to void the "same visit" 1804 & 1805 claims and then resubmit a single APG claim for the visit which includes the CPT codes for both the primary and the secondary procedures performed during the visit.
- Voiding the 1805 claim and adjusting the rate code on the 1804 claim to 1408 and add the 1805 claim´s CPTs to the 1408 claim is another option.
- If providers have not voided (or adjusted) these claims prior to the start of eMedNY´s reprocessing of APG claims (August 1st), eMedNY will void same–visit 1804/1805 claims at that time, and providers may re–bill using the APG rate code as stated above.
APG Retro–Billing for DTCs (cont.)
- D&TC providers will be notified before episode rate codes are made available and billing guidance will be issued prior to the implementation of APG episode billing.
- Freestanding D&TCs should, but are not required to use episode rate codes once they are activated for all APG claims except for claims for Medicare/Medicaid dually eligible patients.
- Claims for dually eligible patients should always be submitted to eMedNY using APG visit rate codes.
APG Retro–Billing for Dialysis Centers
- Providers who, prior to APGs, used CPT 90999 (unlisted dialysis procedure) to bill for hemodialysis will have to use one of the CPT codes listed below for APG 168 to bill for hemodialysis, since 90999 groups to peritoneal dialysis in APGs.
- When DOH processes the September 1, 2009 to August 1, 2010 claims through the APG grouper–pricer, providers that used 90999 will be paid for peritoneal dialysis (APG 169: weight 0.4795), not hemodialysis (APG 168: weight 1.1155).
- Therefore, providers that used 90999 for hemodialysis since September 1, 2009 should recode their claims retroactively to DOS 9/1/2009 before August 1, 2010 if they want to avoid a "takeback" (recoupment).
- Even after DOH reprocesses the claims, providers will still be able to adjust their claims to correct improper coding and restore the correct funding level.
APG 168 Hemodialysis
- 4052F Hemodialysis via fistula
- 4053F Hemodialysis via AV graft
- 4054F Hemodialysis via catheter
- 90935 Hemodialysis, one evaluation
- 90937 Hemodialysis, repeated eval
- 90997 Hemoperfusion
- G0257 Unsched dialysis ESRD pt hos
- S9335 HT Hemodialysis
APG 169 Peritoneal Dialysis
- 4055F Pt revng peritoneal dialysis
- 90945 Dialysis, one evaluation
- 90947 Dialysis, repeated evaluation
- S9339 HIT peritoneal dialysis diem
- 90999 Unlisted dialysis procedure, inpatient or outpatient
APG Payment Methodology Overview
What are APGs?
- A classification system designed to explain the amount and type of resources used in ambulatory visits that:
- Predicts the average pattern of resource use for a group of patients by combining procedures, medical visits and/or ancillary tests that share similar characteristics and resource utilization;
- Provides greater reimbursement for higher intensity services and less reimbursement for low intensity services; and
- Allows more payment homogeneity for comparable services across all ambulatory care settings (e.g., outpatient department and diagnostic and treatment centers).
PRIMARY TYPES OF APGS
- ☐ SIGNIFICANT PROCEDURES: A procedure which constitutes the reason for the visit and dominates the time and resources expended during the visit. Examples include: excision of skin lesion, stress test, treating fractured limb. Normally scheduled.
- ☐ MEDICAL VISITS: A visit during which a patient receives medical treatment (normally denoted by an E&M code), but did not have a significant procedure performed. E&M codes are assigned to one of the 181 medical visit APGs based on the diagnoses shown on the claim (usually the primary diagnosis).
- ☐ ANCILLARY TESTS AND PROCEDURES: Ordered by the primary physician to assist in patient diagnosis or treatment. Examples include: immunizations, plain films, laboratory tests.
- ☐ OTHER TYPES OF APGs: Drugs, DME (not used in NYS, paid through fee schedule), Incidental to Medical Visit (always packaged), Per Diem, Inpatient–Only (not eligible for payment), Unassigned (not eligible for payment)
APG PAYMENT DEFINITIONS
- Consolidation (or Bundling)
- The inclusion of payment for a related procedure into the payment for a more significant procedure provided during the same visit.
- ➢ CPT codes that group to the same APG are consolidated.
- The inclusion of payment for a related procedure into the payment for a more significant procedure provided during the same visit.
- Packaging
- The inclusion of payment for related medical visits or ancillary services in the payment for a significant procedure.
- ➢ The majority of "Level 1 Ancillary APGs" are packaged.
- ➢ (i.e. pharmacotherapy, lab and radiology)
- ➢ Uniform Packaging List is available online at the DOH APG website.
- The inclusion of payment for related medical visits or ancillary services in the payment for a significant procedure.
- Discounting
- A discounted payment for an additional, but unrelated, procedure provided during the same visit to acknowledge cost efficiencies.
- ➢ If two CPT codes group to different APGs, 100% payment will be made for the higher cost APG, and the second procedure will be discounted (generally at 50%).
- A discounted payment for an additional, but unrelated, procedure provided during the same visit to acknowledge cost efficiencies.
Sample APG / HCPCS Crosswalk
| APG | APG Description | HCPCS Code |
HCPCS Description |
|---|---|---|---|
| 418 | Minor Cardiac And Vascular Tests |
36584 | Replace picc cath |
| 36589 | Removal tunneled cv cath | ||
| 36596 | Mech remov tunneled cv cath | ||
| 36860 | External cannula declotting | ||
| 37799 | Vascular surgery procedure | ||
| 93025 | Microvolt t‐wave assess | ||
| 93224 | ECG monitor/report, 24 hrs | ||
| 93225 | ECG monitor/record, 24 hrs | ||
| 93226 | ECG monitor/report, 24 hrs | ||
| 93230 | ECG monitor/report, 24 hrs |
Sample APGs and Weights
| APG | APG Name | Type | Weight |
|---|---|---|---|
| 30 | LEVEL I MUSCULOSKELETAL PROCEDURES EXCLUDING HAND AND FOOT | Sign. Proc. | 6.7781 |
| 40 | SPLINT, STRAPPING AND CAST REMOVAL | Sign. Proc. | 0.9264 |
| 112 | PHLEBOTOMY | Sign. Proc. | 0.7423 |
| 116 | ALLERGY TESTS | Sign. Proc. | 1.3107 |
| 271 | PHYSICAL THERAPY | Sign. Proc. | 0.6827 |
| 315 | COUNSELLING OR INDIVIDUAL BRIEF PSYCHOTHERAPY | Sign. Proc. | 0.6206 |
| 396 | LEVEL I MICROBIOLOGY TESTS | Ancillary | 0.1137 |
| 397 | LEVEL II MICROBIOLOGY TESTS | Ancillary | 0.2141 |
| 413 | CARDIOGRAM | Ancillary | 0.2274 |
| 414 | LEVEL I IMMUNIZATION AND ALLERGY IMMUNOTHERAPY | Ancillary | 0.2475 |
| 471 | PLAIN FILM | Ancillary | 0.4758 |
| 527 | PERIPHERAL NERVE DISORDERS | Medical Visit | 0.7377 |
| 562 | INFECTIONS OF UPPER RESPIRATORY TRACT | Medical Visit | 0.6284 |
| 575 | ASTHMA | Medical Visit | 0.7979 |
| 599 | HYPERTENSION | Medical Visit | 0.7924 |
| 808 | VIRAL ILLNESS | Medical Visit | 0.8734 |
| 826 | ACUTE ANXIETY & DELIRIUM STATES | Medical Visit | 0.6352 |
IMPORTANCE OF ACCURATE CODING
- Under APG payment methodology, all claims must include:
- the new APG rate codes;
- a valid, accurate ICD–9–CM primary diagnosis code(s)*; and
- valid CPT and/or HCPCS procedure code(s) reflecting service provided.
- Reimbursement for an Evaluation and Management (E & M) visit is determined by the primary ICD–9–CM diagnosis code. Diagnosis and procedure coding and billing must be supported by the documentation in the medical record.
- Secondary diagnoses or additional codes that describe any co–morbid (i.e., coexisting) conditions should also be coded, as certain significant conditions may supersede the primary diagnosis and cause the medical visit to group to Major Signs and Symptoms (APG 510), which could result in higher visit payment.
APG Payment Methodology
APG PAYMENT CALCULATION OVERVIEW
| APG Group Category | Weights | Packaging/Bundling or Discounting | Base Rate | Capital Add–on Payment | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CPT/HCPCS codes grouped according to procedure and/or diagnosis | → | Avg. cost for each APG visit/avg. cost for all APG visits | × | Weight multiplier applied to each APG | × | Established base rate by setting and peer group | + | Capital add–on for each patient visit | = | FINAL APG PAYMENT |
Weight Multiplier (Consolidating or Discounting Logic)
- 100% for primary (highest–weighted) APG procedure
- 100% unrelated ancillaries
- 150% for bilateral procedures
- 10%–50% for discounted lines (unrelated significant procedures performed in a single visit).
- 0% for bundled/consolidated lines (related ancillaries are included in the APG significant procedure payment)
Phasing and Blending
- Phasing: APG payments will be phased–in over time through blending.
- Blending: The Medicaid payment for a visit will include a percentage of the payment amount based on APGs and a complementary percentage of the payment amount based on the average facility clinic rate in 2007 as defined by DOH.
Hospital OPD and D&TC Transition and "Blend"
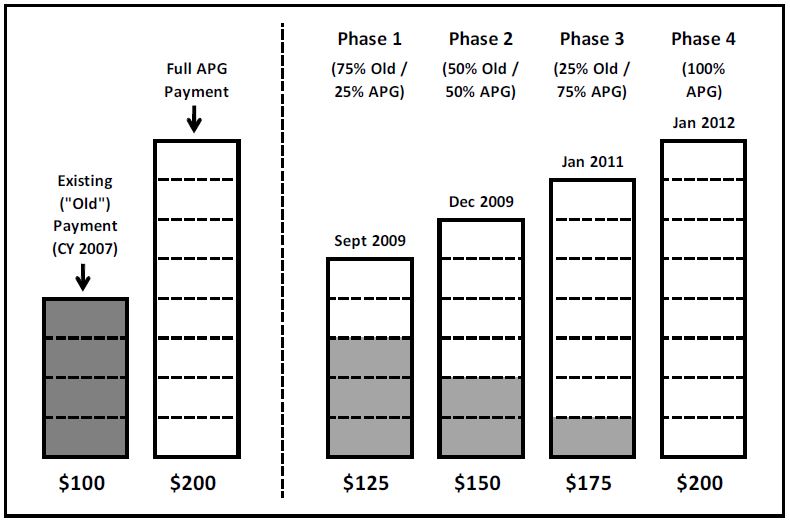
Note: Blend goes into effect on 9/1/09 for D&TCs and Free–Standing Ambulatory Surgery Centers and 12/1/2008 for hospital (OPDs).
Payment Example 1 – Medical Visit (Asthma)
DOS 5/1/2010
| APG Base Rate: $200.00 Rate Code: 1407 (DTC General Clinic) Existing Payment for Blend: $100.00 Region: Downstate Blend Percentage (APG): 50% Primary Dx Code (Description): 49390 (Asthma NOS) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Px Code | Procedure Description | APG | APG Description | Payment Action |
Units | Payment Percent |
Allowed Weight |
Full APG Payment |
APG Portion of Blend |
Existing Payment Portion of Blend |
Add–on Payment |
Total Payment |
| 99213 | Office/outpatient visit, est | 575 | Asthma | Full payment | 1 | 100% | 0.7979 | $ 160 | $ 80 | $ 50 | $ 20 | $ 150 |
| 82565 | Assay of creatinine | 400 | Level I Chemistry Tests | Packaged | 1 | 0% | 0.0000 | – | – | – | – | – |
| 71020 | Chest x–ray | 471 | Plain Film | Packaged | 1 | 0% | 0.0000 | – | – | – | – | – |
| TOTALS | 0.7979 | $ 160 | $ 80 | $ 50 | $ 20 | $ 150 | ||||||
Payment Example 2 – Medical Visit (HIV)
DOS 5/1/2010
| APG Base Rate: $200.00 Rate Code: 1407 (DTC General Clinic) Existing Payment for Blend: $100.00 Region: Downstate Blend Percentage (APG): 50% Primary Dx Code (Description): 42 (Human immuno virus dis) |
|||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Px Code | Procedure Description | APG | APG Description | Payment Action |
Units | Payment Percent |
Allowed Weight |
Full APG Payment |
APG Portion of Blend |
Existing Payment Portion of Blend |
Add–on Payment |
Total Payment |
|||||||||||||
| 99213 | Office/outpatient visit, est | 881 | Aids | Full payment | 1 | 100% | 1.0495 | $ 210 | $ 105 | $ 42 | $ 20 | $ 167 | |||||||||||||
| 85025 | Complete cbc w/auto diff wbc | 408 | Level I Hematology Tests | Packaged | 1 | 0% | 0.0000 | – | – | – | – | – | |||||||||||||
| 80076 | Hepatic function panel | 403 | Organ Or Disease Oriented Panels | Full payment | 1 | 100% | 0.1367 | 27 | 14 | 5 | – | $ 19 | |||||||||||||
| 90740 | Hepb vacc, ill pat 3 dose im | 416 | Level III Immunization | Full payment | 1 | 100% | 0.8428 | 169 | 169 | – | – | $ 169 | |||||||||||||
| 36415 | Routine venipuncture | 457 | Venipuncture | Full payment | 1 | 100% | 0.0602 | 12 | 5 | 2 | – | $ 7 | |||||||||||||
| TOTALS | 2.0892 | $ 418 | $ 292 | $ 50 | $ 20 | $ 362 | |||||||||||||||||||
Note: APG 416– Level III Immunization is on the No Blend APG List
Payment Example 3 – Ambulatory Surgery
DOS 5/1/2010
| APG Base Rate: $100.00 Rate Code: 1408 (Free–Standing Ambulatory Existing Payment for Blend: $500.00 Region: Downstate Blend Percentage (APG): 50% Primary Dx Code (Description): 5284 (Asthma NOS) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Px Code | Procedure Description | APG | APG Description | Payment Action |
Units | Payment Percent |
Allowed Weight |
Full APG Payment |
APG Portion of Blend |
Existing Payment Portion of Blend |
Add–on Payment |
Total Payment |
| 31545 | Remove vocal cord lesion w/scope | 63 | Level II Endoscopy Of The Upper Airway | Full payment | 1 | 100% | 7.0115 | $ 701 | $ 351 | $ 250 | $ 100 | $ 701 |
| 31515 | Laryngoscopy for aspiration | 62 | Level I Endoscopy Of The Upper Airway | Consolidated | 1 | 0% | 0.0000 | – | – | – | – | – |
| 00100 | Anesth, salivary gland | 380 | Anesthesia | Packaged | 1 | 0% | 0.0000 | – | – | – | – | – |
| TOTALS | 7.0115 | $ 701 | $ 351 | $ 250 | $ 100 | $ 701 | ||||||
NOTE: Pre–surgical testing ordered by D&TC or OPD clinic practitioner for clinic patients should be billed through APGs and non–clinic patients should be billed on an ordered ambulatory basis to the Medicaid fee schedule. All post–surgical testing should be billed on an ordered ambulatory basis to the Medicaid fee schedule.
Base Rates
- Base rates are established for peer groups.
- e.g. DTC, hospital OPD, hospital ED, free standing ambulatory surgery center, dental school, renal clinic etc.
- Within each peer group there are downstate and upstate regions that have differing rates.
- Peer group base rates are calculated based on case mix, visit volume, cost, and targeted investment.
- Base rates represent a "conversion factor" for multiplication by APG weights on a claim to arrive at the APG payment amount.
APG Base Rate Regions
- Downstate – New York City, Nassau, Suffolk, Westchester, Rockland, Putnam, Dutchess, Orange
- Upstate – The rest of the State
Base Rate Variables
- Case Mix Index (CMI)
- Coding Improvement Factor (CIF)
- Visit Volume
- Targeted Expenditure Level
- Base Year Expenditures
- Investment
- Reported Provider Cost by Peer Group (for scaling of investments)
Case Mix Index
- Definition – The average allowed APG weight per visit for a defined group of visits (based on peer group and time period of claims).
Coding Improvement Factor
- A numeric value used to adjust for the fact that the coding of claims subsequent to the implementation of APGs will become more complete and accurate.
Base Rate Formula
(for initial implementation)
Base Year Expenditures + Investment [see note]
___________________________________________
CMI × CIF × Base Year Visits
Note: When a "blend" payment methodology is being used, the investment must be divided by the APG blend percentage in order for the base rates to pay out the full investment. For example, if a $50M investment is to be paid out under a 25% APG blend then the investment used in the calculation shown above must be $200M.
Ancillary Payment Policy and Episode Payments
Delay in Ancillary Billing Policy for D&TCs
- The APG ancillary billing policy as originally proposed has been delayed for D&TCs until January 1, 2011.
- In January 2011, the Department will implement the ancillary policy, but with an option for providers that do not want to contract with ancillary vendors to code the ordered ancillary on the APG claim.
- Providers will be required to code all procedures associated with a visit weather they are performed on site or referred to an outside vendor.
- Providers will be given two billing options for "ordered" ancillaries:
- ➢ 1.) contract with outside providers for all their labs and radiology or
- ➢ 2.) have the labs and radiology providers bill directly off the ordered ambulatory fee schedule.
Ancillary Billing Policy for D&TCs
- All ancillary procedures (except APG carve outs), whether ordered of performed in–house, must be coded on the APG claim
- For ordered ancillaries, providers may either:
- contract with ancillary vendors and reimburse the vendors directly (from the APG proceeds), or
- not contract with ancillary vendors, in which case the ancillary vendors will bill Medicaid directly
- NOTE: The use of modifier 90 has been reversed from that which was described to providers during our training session on June 21st.
- If a provider desires reimbursement for any ancillary they must code modifier 90 on the same line as the ancillary. Again, all ancillaries must be coded on the APG claim (except APG carve outs)
- All providers may code modifier 90 on ancillaries performed in–house.
- Only those providers that contract with ancillary vendors may code modifier 90 on ordered ancillaries!
- Modifier 90 is only to be used for:
- In–house ancillaries performed by any APG biller, or
- Ancillaries ordered by contracting APG billers
- Ancillaries ordered by non–contracting providers must still be coded on the APG claim, but not with modifier 90
- Failure to code the ancillary or the inclusion of modifier 90 on the APG claim may subject the APG biller to OMIG action
- The effect of modifier 90:
- If modifier 90 is coded on a non–packaging ancillary (e.g., PET Scan), the provider will receive payment for the ancillary, subject to the usual APG payment logic. (IN–HOUSE ANCILLARY OR CONTRACTING PROVIDER)
- If modifier 90 is coded on a packaging ancillary (e.g., Plain Film), the provider will receive payment for the ancillary via "packaging" (i.e., payment will be included on the line for the E&M code).
- If modifier 90 is not coded on a non–packaging ancillary, no payment will be made for that ancillary. The ancillary vendor may bill Medicaid directly.
- If modifier 90 is not coded on a packaging ancillary, the value of the ancillary will be subtracted from the APG payment because the payment for that ancillary was included in the line for the E&M code. The APG biller was not entitled to that payment because an ancillary vendor will be billing Medicaid directly for the procedure.
Code Modifier 90?
| Contracting APG Biller | Non–contracting APG Biller | |
|---|---|---|
| Ancillary Service is Provided In–House (on site) |
YES | YES |
| Ancillary Service is Referred to Outside Vender |
YES | NO |
NOTE: Modifier 90 does not apply to APG carveouts which should never be coded on an APG claim.
Implementation of the APG Payment Policy For Ancillary Laboratory and Radiology Services
- Effective January 1, 2011, D&TCs must include all lab/radiology ancillary services on their APG claim.
- This includes any lab/radiology performed by the D&TC or referred to an outside lab/radiology provider.
- Prior to January 1, 2011, D&TCs should submit APG claims for only those ancillary procedures provided on site.
- Lab/radiology services referred by the D&TC to a provider not affiliated with the D&TC may be billed by that servicing provider directly to Medicaid using the appropriate fee schedule (unless those ancillary services were historically included in the D&TC´s clinic rate, in which case the clinic should reimburse the ancillary provider).
- There are, however, two exceptions to this policy for D&TCs:
- Ancillary tests and procedures performed on a patient referred by a community physician should be billed to the Medicaid fee schedule on an ordered ambulatory basis.
- Ancillary tests and procedures performed on a patient referred by a hospital–based clinic should be billed to the referring OPD.
Billing the Professional and Technical Component
- As with the clinic threshold rate, the physician professional component is always included in the APG payment to the D&TC.
- There are two exceptions to this policy;
- Ambulatory Surgery – The professional component should be billed by the attending physician (surgeon, anesthesiologist) using the Medicaid physician fee schedule.
- The professional component for ancillary radiology services should be billed by the radiologist using the Medicaid physician fee schedule when the radiology procedure is being done on an ordered ambulatory patient. (i.e., The patient is referred from either an Article 28 clinic or community physician)
- The D&TC must bill the radiology technical component to the referring clinic.
- There are two exceptions to this policy;
Visit vs. Episode Billing
Visit Billing
- Under visit APG billing, the APG grouper–pricer recognizes all procedures performed on the same day of service as a visit and applies grouping, discounting, etc. to that set of procedures accordingly.
- In order for the APG grouper to price the claim correctly, all dates of service for lab/radiology ancillary services provided the patient subsequent to the clinic visit must be adjusted so that they are the same date of service as the clinic visit during which they were ordered.
Episode Billing
- Under Episode APG billing, the grouper–pricer treats all lines on the claim as if they had the same date of service. Therefore, dates of service for lab/radiology ancillary services provided subsequent to the clinic visit may reflect the actual date of service for those ancillaries.
- Episode billing is the preferred billing method if there are multiple dates of service for the office visit and associated ancillaries since this method more accurately reflects when services are actually provided.
Visit APG Rate Code 1407
- The date of service for the medical visit/significant procedure and all associated lab/radiology ancillary procedures must be coded with the same date as the medical visit/significant procedure.
- Dates of service for lab/radiology ancillary services provided subsequent to the clinic must be adjusted by the clinic so that they are the same date as the clinic visit when they were ordered.
- This includes:
- ➢ Lab/radiology services provided by the D&TC.
- ➢ Lab/radiology services referred to outside ancillary providers.
- ➢ Lab/radiology services performed on same day and subsequent to the clinic visit.
- The "from/through" date in the header should encompass all of the dates of service for the medical visit/significant procedure.
Episode APG Rate Code 1422
- The date of service for the medical visit/significant procedure will be the date when the patient is seen in the clinic.
- The date of service for all lab/radiology ancillary services should be the date when those services were actually provided to the patient, as defined below.
- Lab date of service should be the date of specimen collection.
- Radiology date of service should be the date when the radiology procedure was provided to the patient.
- This includes:
- ➢ Lab/radiology services provided by the D&TC.
- ➢ Lab/radiology services referred to outside ancillary providers.
- ➢ Lab/radiology services performed on same day and subsequent to the clinic visit.
- The "from/through" date in the header should encompass the dates of service for the medical visit/significant procedure as well as all dates of service for the associated lab/radiology ancillary procedures provided the patient.
- Only a single episode (e.g., medical visit and associated ancillaries) may be coded on a claim.
- If procedures from two different episodes of care are coded on the same claim, unwarranted discounting or consolidation could occur, resulting in underpayment to the APG biller.
- As with the visit payment, if two claims are submitted by the same APG provider for the same patient using the same episode rate code and the same "from" date for the episode of care, only the first claim will be reimbursed.
APG Visit Payment and Assignment of Ancillary DOS
1407 APG Rate Code
| Claim | Date of Service (Line Level) | Service | Ancillary Service Provided | From/Thru Date (Header) |
|---|---|---|---|---|
| 1 | 1/1/2009 | E&M | Yes (See next row) | 1/1 ‐ 1/5 |
| 1 | 1/1/2009* | Ancillary | Provided on 1/5* | 1/1 ‐ 1/5 |
| 1 | 1/2/2009 | Dental | No | 1/1 ‐ 1/5 |
| 1 | 1/3/2009 | Physical Therapy | No | 1/1 ‐ 1/5 |
* Reassign ancillary to 1/1/2009 DOS on APG claim.
Note: Multiple DOS can be billed for same recipient/same DOS under APG rate code 1407.
APG Episode Payment and Assignment of Ancillary DOS (cont.)
1422 APG Rate Code
| Claim | Date of Service (Line Level) | Service | Ancillary Service Provided | From/Thru Date (Header) |
|---|---|---|---|---|
| 1 | 1/1/2009 | E&M | Yes (See next row) | 1/1 ‐ 1/5 |
| 1 | 1/5/2009* | Ancillary | Provided on 1/5* | 1/1 ‐ 1/5 |
| 2 | 1/2/2009 | Dental | No | 1/2 ‐ 1/2 |
| 3 | 1/3/2009 | Physical Therapy | No | 1/3 ‐ 1/3 |
*Use actual 1/5/2009 DOS on APG claim.
Note: A separate claim must be submitted for each separate DOS for same recipient/same DOS billed under APG rate code 1422.
APG Billing Rate Codes In Effect for January 2010
| Service/Setting | Facility Type | Rate Codes‐ Effective January 1, 2010 | |
|---|---|---|---|
| Visit | Episode | ||
| General Clinic | DTC | 1407 | 1422 |
| General Clinic‐ MR/DD/TBI | DTC | 1435 | 1425 |
| Dental School | DTC | 1428 | 1459 |
| Renal Clinic | DTC | 1438 | 1456 |
| School Based Health | DTC | 1447 | 1453 |
| Free‐Standing Surgery Center | DTC | 1408 | NA |
Note: D&TC Rate Codes will be effective September 1, 2009, except codes 1453,1456, and 1459 which are effective 10/1/2009.
APG Carve–Outs and Special Payment Rules
APG Carve–Outs
- All items that were carved–out of the threshold visit rate will continue to be carved–out and paid off the referred ambulatory services fee schedule – with a single exception...
- MRIs will no longer be carved–out of the threshold visit, but instead must be billed under APGs.
- The following slides list select APG carve–outs, but for a complete see DOH APG website.
Current APG Carve–Outs
(for complete list see DOH APG website)
- Certain therapeutic injections (e.g., Botulinum Toxin A & B and Epogen for ESRD dialysis patients)
- Blood Factors/Hemophilia, Medical Abortion Pharmaceuticals (Misoprostol/Mifepristone), & Family Planning Devices (IUDs & Contraceptive Implant)
- Certain specific laboratory tests (e.g., lead screen, hepatitis C viral load, HIV drug resistance tests)
- Tuberculosis DOT
- All drugs grouping to the Chemotherapy Drug APGs
- Level VII (Combined Chemotherapy/Pharmacotherapy) Drugs
- Mental Health Counseling by LCSW and LMSWs (new)
- All genetic laboratory tests
- Newborn Hearing/Screening Services (3139)
- "Carved in" for July 1, 2010
- FQHC Group Psychotherapy (4011)/Off–site Services (4012)
- Screening for Orthodontic Treatment (3141)
- TB/Directly Observed Therapy (5312, 5313, 5317, 5318)
- MOMS Health Supportive Services (1604)
- HIV Counseling and Testing by HIV Primary Care Medicaid Providers (1695, 1802, 3109)
- Day Health Care Service (HIV) (1850)
- Dialysis/Medicare Crossover (3107)
Never Pay APGs
- "Never Pay" APGs are those services that are not covered under APG reimbursement.
- Examples of Never Pay APGs include:
- Respiratory Therapy
- Artificial Fertilization
- Biofeedback
- Please see a complete list of Never Pay APGs on the Department´s website.
"If Stand Alone, Do Not Pay" APGs
- "If Stand Alone, Do Not Pay" APGs generally consist of procedures performed as follow–up to an initial clinic visit for which APGs will not pay. These consist primarily of tests and other ancillaries.
- Mirroring the current reimbursement system, these procedures will also not pay under APGs when they are the only items claimed for a given date of service
- For example:
- ➢ Follow–up laboratory and diagnostic radiology testing (except MRIs) related to an initial patient encounter.
- Providers should still claim for these procedures in order to maximize the available data that can be used for future reweighting and rebasing.
- Please see a complete list on the Department´s website.
Claiming for "Never Pay" and "If Stand Alone Do Not Pay" APGs
- If the only items on a claim for a particular date of service (APG visit) are "Never Pays" and/or "If Stand Alone, Do Not Pays", then the visit will be paid at zero.
Modifiers in APGs
- APGs will recognize several billing modifiers.
- 25 – distinct service
- Separately identifiable E&M service on the same day as a significant procedure (subject to DOH policy requirements)
- 27 – additional medical visit
- Separate medical visit with another practitioner on the same date of service (subject to DOH policy requirements)
- 52 – terminated procedure
- Discontinued outpatient hospital/ambulatory surgery procedure that does not require anesthesia
- 73 – terminated procedure
- Discontinued outpatient hospital/ambulatory surgery procedure, after some preparation, but prior to the administration of anesthesia
- 59 – separate procedure
- Distinct and separate multiple procedures (with same APG)
- 50 – bilateral procedure
- 25 – distinct service
2010 APG Grouper Pricer Changes
Overview of APG Payment Changes for January 1, 2010
- Updated APG weights and revised base rates
- Pharmacotherapy and chemotherapy classifications expanded from 5 to 6 levels (however, chemo drugs will continue to be carved out).
- A new "premium" drug APG was created comprising both pharmacotherapy and chemotherapy drugs. This APG, and its associated drugs, was carved out of APGs and is billable as ordered ambulatory.
- APGs recognizes units of service for a discrete list of services, e.g., physical therapy, occupational therapy, diabetes and asthma education (provided by a Certified Diabetic Educator/Certified Asthma Educator).
- Medical visits no longer package with significant ancillaries (e.g., MRIs), dental procedures, PT, OT, speech, and counseling services and instead pay at the line level.
- Multiple same APG discounting (rather than consolidation) which formerly applied to most dental services was expanded to include dental sealants, OT, PT, speech, and most mental hygiene APGs.
- Genetic testing procedures have been carved out. Laboratories should bill Medicaid using the laboratory fee schedule.
- The no–blend APG list now includes cardiac rehabilitation, which came off the "never pay" APG list in January.
- The following new APGs were created:
- Physical Therapy – Group
- Speech Therapy – Group
- Some procedures (e.g., provision of hearing aids) are now paid based on procedure–specific weights rather than APG–specific weights.
- Capital add–on rules will change so that an add–on is paid for nearly all types of visits including those consisting entirely of ancillaries and dental examinations (currently, a capital add–on is not paid with ancillary only visits).
- However, a capital add–on will not be paid for visits consisting solely of PT–group, speech–group, cardiac rehabilitation, and immunization.
New Premium "Class VII" APG for Select Chemotherapy and Pharmacotherapy Drugs
- There will be a new "premium" drug APG, consisting of certain chemotherapy and pharmacotherapy drugs. All drugs grouping to this class will be carved out of APGs and billable to the Ordered Ambulatory Fee Schedule.
| CPT | Description | Current APGs | New 2010 APG | New 2010 APG Description |
|---|---|---|---|---|
| J7311 | Fluocinolone acetonide implt | 437 | 442 | CLASS VII COMBINED CHEMOTHERAPY & PHARMACOTHERAPY |
| J1458 | Galsulfase injection | 439 | ||
| J1785 | Injection imiglucerase /unit | 439 | ||
| J1300 | Eculizumab injection | 439 | ||
| J9300 | Gemtuzumab ozogamicin inj | 434 | ||
| J0180 | Agalsidase beta injection | 434 |
New Procedure–Based Weights
- Beginning January 1, 2010 some procedures will be paid based on procedure–specific weights rather than APG– specific weights, including the following types of services:
- Select Mental Hygiene Services (OMR and OMH Certified clinics only),
- Physical Therapy (for units–based procedures),
- Occupational Therapy (for units–based procedures), and
- Nutritional Counseling
APGs That Contain Procedure–Based Weights
(some or all procedures use procedure–based weights)
| APG | APG Description |
|---|---|
| 118 | NUTRITION THERAPY |
| 270 | OCCUPATIONAL THERAPY |
| 271 | PHYSICAL THERAPY |
| 272 | SPEECH THERAPY AND EVALUATION |
| 310 | DEVELOPMENTAL & NEUROPSYCHOLOGICAL TESTING |
| 312 | FULL DAY PARTIAL HOSPITALIZATION FOR MENTAL ILLNESS |
| 315 | COUNSELLING OR INDIVIDUAL BRIEF PSYCHOTHERAPY |
| 316 | INDIVIDUAL COMPREHENSIVE PSYCHOTHERAPY |
| 317 | FAMILY PSYCHOTHERAPY |
| 320 | CASE MANAGEMENT & TREATMENT PLAN DEVELOPMENT ‐ MENTAL HEALTH OR SUBSTANCE ABUSE |
| 321 | CRISIS INTERVENTION |
| 323 | MENTAL HYGIENE ASSESSMENT |
| 426 | PSYCHOTROPIC MEDICATION MANAGEMENT |
| 427 | BIOFEEDBACK AND OTHER TRAINING |
| 428 | PATIENT EDUCATION, INDIVIDUAL |
| 429 | PATIENT EDUCATION, GROUP |
| 490 | INCIDENTAL TO MEDICAL, SIGNIFICANT PROCEDURE OR THERAPY VISIT |
Some Procedures are Based on Units of Service
- For some procedures, units of service are also recognized in the calculation of the payment. For example:
- Physical Therapy – 97032 – Electrical Stimulation, each 15 min (max 3 units)
- Occupational Therapy – 97532 – Cognitive Skills development, each 15 min (max 3 units)
- Nutrition Therapy – 97802– Medical Nutrition, ind., each 15 min (max 2 units)
- Note: All of these procedures are also paid based on procedure–specific weights
Sample Procedure–Based Weights
| APG | APG Description | Payment Action Flag Description |
HCPCS Code |
HCPCS Code Description | Weight | Units Limit |
|---|---|---|---|---|---|---|
| 118 | Nutrition Therapy | Alternate Weight‐ Not Units Based* |
97804 | Medical nutrition, group, each 30 min | 0.3448 | 1 |
| G0271 | Group MNT 2 or more 30 mins | 0.1517 | 1 | |||
| Alternate Weight‐ Units Based* |
97802 | Medical nutrition, ind, each 15 min | 0.1793 | 2 | ||
| 97803 | Medical nutrition, ind, subseq, each 15 min | 0.1793 | 2 | |||
| G0270 | MNT subs tx for change dx, each 15 min | 0.1793 | 2 | |||
| 270 | Occupational Therapy | Alternate Weight‐ Units Based* |
97532 | Cognitive skills development, 15 min | 0.2414 | 3 |
| 97533 | Sensory integration, 15 min | 0.2414 | 3 | |||
| 271 | Physical Therapy | Alternate Weight‐ Units Based* |
97032 | Electrical stimulation, 15 min | 0.2276 | 3 |
| 97033 | Electric current therapy, 15 min | 0.2276 | 3 | |||
| 272 | Speech Therapy And Evaluation |
Alternate Weight‐ Not Units Based |
92607 | Ex for speech device rx, 1hr | 0.8827 | 1 |
| 92608 | Ex for speech device rx addl | 0.8827 | 1 |
* For Illustration purposes only. These APGs include additional procedures not shown in this table. Any codes paid off the APG–based weight are not shown.
Medical Visits Will No Longer Package With Higher Intensity Significant Ancillaries
- Effective January 1, 2010 Medical visits will no longer package with:
- more significant ancillaries (e.g., MRIs, mammograms, CAT scans, etc.);
- dental procedures;
- PT, OT, and speech therapies; and,
- counseling services.
- In these cases, a coded medical visit will separately pay at the line level.
Revised "If Stand Alone, Do Not Pay" List
- Additions to the "If stand alone, do not pay" list for January 2010:
| APG Type | APG | APG Description |
|---|---|---|
| Sign. Proc. | 118 | Nutrition Therapy |
| Sign. Proc. | 281 | Magnetic Resonance Angiography‐ Head And/Or Neck |
| Sign. Proc. | 282 | Magnetic Resonance Angiography‐ Chest |
| Sign. Proc. | 283 | Magnetic Resonance Angiography‐ Other Sites |
| Sign. Proc. | 292 | Mri‐ Abdomen |
| Sign. Proc. | 293 | Mri‐ Joints |
| Sign. Proc. | 294 | Mri‐ Back |
| Sign. Proc. | 295 | Mri‐ Chest |
| Sign. Proc. | 296 | Mri‐ Other |
| Sign. Proc. | 297 | Mri‐ Brain |
| Ancillary | 373 | Level I Dental Film |
| Ancillary | 374 | Level II Dental Film |
| Ancillary | 375 | Dental Anesthesia |
| Drug | 440 | Class VI Pharmacotherapy |
New "No Blend APGs"
- The following new APGs will pay entirely based on the APG payment methodology (at 100%) and no existing payment will be factored into the operating component of the rate.
| APG | APG Description | APG Type |
|---|---|---|
| 94 | Cardiac Rehabilitation | Significant Procedure |
| 310 | Developmental and Neuropsychological Testing | Significant Procedure |
| 312 | Full Day Partial Hospitalization for Mental Illness | Per Diem |
| 321 | Crisis Intervention | Significant Procedure |
| 322 | Medication Administration and Observation | Significant Procedure |
| 426 | Medication Management | Ancillary |
- NOTE: D&TC providers licensed solely by DOH should not be routinely using certain mental hygiene therapy services (e.g., APG 310, APG 312, APG 321, APG 322 and APG 426).
APGs With Discounting Other than 50%
| APG | APG Description | Discount Percentage |
|---|---|---|
| 118 | NUTRITION THERAPY | 25% |
| 257 | AUDIOMETRY | 25% |
| 270 | OCCUPATIONAL THERAPY | 25% |
| 271 | PHYSICAL THERAPY | 25% |
| 272 | SPEECH THERAPY AND EVALUATION | 25% |
| 274 | PHYSICAL THERAPY, GROUP | 25% |
| 275 | SPEECH THERAPY & EVALUATION, GROUP | 25% |
| 315 | COUNSELLING OR INDIVIDUAL BRIEF PSYCHOTHERAPY | 10% |
| 316 | INDIVIDUAL COMPREHENSIVE PSYCHOTHERAPY | 10% |
| 317 | FAMILY PSYCHOTHERAPY | 10% |
| 318 | GROUP PSYCHOTHERAPY | 10% |
Note: This is a partial list, for a complete list please go to the Department´s website.
Special Payment Policy
Medicare and Commercial Insurance
- For Medicaid recipients who are also covered by Medicare or commercial insurance:
- If the lab or radiology provider is required to bill Medicare or the commercial insurance directly, the lab/radiology provider should do so.
- The lab/radiology provider should then bill Medicaid for the balance due.
- If Medicare or the commercial insurance denies payment for the laboratory test, the laboratory should bill Medicaid fee–for–service by the lab/radiology provider.
- The clinic should not report these ancillary lab/radiology services on their APG claim.
- Additionally, claims for dual eligible Medicare/Medicaid recipients may be billed using visit–based APG rate codes (e.g., 1407, 1408, 1428, 1435, 1438, and 1447).
Ambulatory Surgery Services
- The following applies only to free–standing providers that have been assigned both the ambulatory surgery base rate and the clinic base rate:
- Effective December 1, 2008 through June 30, 2010, an APG visit may be billed against an ambulatory surgery rate code if the visit includes at least one procedure from the Ambulatory Surgery Procedures List (see link below).
- The APG Ambulatory Surgery Procedures List will be eliminated on July 1, 2010 (see below). The list can be found here.
- Effective July 1, 2010 – if a visit is provided in an operating room, an ambulatory surgery rate code must be used on the claim.
- If a visit is provided to a patient under general anesthesia or intravenous sedation, outside the operating room, the visit may be billed against the ambulatory surgery rate code (again, only if the provider/location has been assigned the ambulatory surgery base rate).
- All other visits must be billed using a clinic APG rate code.
Ambulatory Surgery Dental Policy
- Effective January 1, 2010, any dentistry that is done in the operating room with the patient under general anesthesia and/or requiring intravenous sedation may be billed using the ambulatory surgery APG rate code.
- This policy will allow dental services provided in an operating room to be billed against the ambulatory surgery base rate.
- Note: dental procedures (HCPCS codes beginning with a "D"), except for orthodonture codes, are not separately billable against the practitioner´s fee schedule in the clinic setting. That policy extends into the operating room setting.
- Apart from D codes for orthodonture, D codes are only billable against the practitioner fee schedule in the office setting, not in the clinic, ambulatory surgery, or ED settings.
Pre & Post Surgery Testing
- Pre–Surgical Testing: Pre–surgical testing for ambulatory surgery ordered by an OPD or D&TC clinic practitioner for a clinic patient during an APG reimbursable clinic visit should be billed using an APG rate code.
- Pre–surgical testing ordered by a hospital ambulatory surgery unit or ambulatory surgery center practitioner for a patient referred to the ambulatory surgery facility should be billed by the ancillary provider on an ordered ambulatory basis using the Medicaid fee schedule.
- Post–surgical Testing (e.g., pathology): All post–surgical tests ordered by the hospital ambulatory surgery unit or ambulatory surgery center practitioner should be billed by the ancillary provider on an ordered ambulatory basis using the Medicaid fee schedule.
Inpatient Only Services
- Under APG payment rules, certain surgical procedures may only be performed in the hospital inpatient setting. These procedures may not be performed on an ambulatory surgery or clinic outpatient basis.
- These designated ´inpatient only´ procedures will not be reimbursed under the APG payment methodology.
- They will continue to be paid through the All Patient Refined – Diagnosis Related Groups (APR–DRG) payment methodology.
- The APG Grouper will automatically reject these procedures for payment.
- The list of these procedures is available at the Department´s Web site, please visit: here.
Payment for Services Provided by RNs and LPNs
- Clinics should never bill an E&M if the patient only sees an RN or an LPN.
- Patient encounters with only a RN or LPN are only billable to APGs for the following services:
- Chemotherapy or other infusions (an E&M may not be coded)
- Immunizations/Vaccinations (including Gardasil, allergy shots, and applicable administration codes)
- Note: Seasonal flu, pneumococcal and H1N1 vaccinations are APG carve– outs and must be billed to the ordered ambulatory category of service.
- The following services are billable to APGs only when the patient sees a physician and billable to ordered ambulatory when a patient only sees an RN or LPN:
- Urine pregnancy test
- Depo–Provera
- RNs and LPNs may provide service only within their respective scope of practice as defined by the State Education Department laws, rules and regulations.
- e.g., an LPN may not perform a patient assessment.
- Providers may obtain specific information about practitioner scope of practice at the SED Office of the professions website located here.
FQHCs
- Ancillary lab/radiology APG billing and payment policy applies to FQHCs that have opted into APGs.
- But, like other providers, they will have the ability to opt out of the contracting aspect of the ancillary policy
- If an FQHC has not opted into APGs and continues to be reimbursed under the prospective payment system (PPS):
- In general, lab is carved out of the PPS rate and may be billed to Medicaid by the testing lab using the laboratory fee schedule.
- Radiology provided on–site at the FQHC is included in the PPS rate, other than MRI which is carved out and may be billed to Medicaid fee– for–service.
- Services provided to patients referred off–site to a radiology provider may be billed by the radiology provider using the ordered ambulatory radiology fee schedule.
Supporting Materials & Contact Information
Supporting Materials
- The following is available on the DOH website
- Provider Manual – updated June 2010
- PowerPoint Presentations
- APG Documentation
- APG Types, APG Categories, APG Consolidation Logic
- Revised Rate Code Lists
- Uniformly Packaged APGs
- Inpatient–Only Procedure List
- Never Pay and If Stand Alone Do Not Pay Lists
- Carve–Outs List
- List of Rate Codes Subsumed in APGs
- Paper Remittance
- Frequently Asked Questions (currently under revision)
- Ambulatory Surgery List
Contact Information
- Grouper / Pricer Software Support
- 3M Health Information Systems
- Grouper / Pricer Issues 1–800–367–2447
- Product Support 1–800–435–7776
- http://www.3mhis.com
- 3M Health Information Systems
- Billing Questions
- Computer Sciences Corporation
- eMedNY Call Center: 1–800–343–9000
- Send questions to: eMedNYProviderRelations@csc.com
- Computer Sciences Corporation
- Policy and Rate Issues
- New York State Department of Health Office of Health Insurance Programs
Div. of Financial Planning and Policy 518–473–2160- Send questions to: apg@health.state.ny.us
- New York State Department of Health Office of Health Insurance Programs