Value Based Payment Innovator Program
Application Overview
- Webinar also available in Portable Document Format (PDF)
July 2017
Agenda
- Innovator Overview
- Intake Process
- Application Review Criteria and Procedures
VBP Innovator Program Summary
- Applies to experienced VBP providers interested in engaging in full or near full risk VBP Level 2 (L2) or VBP Level 3 (L3) arrangements with MCOs
- Total Care for General Population (TCGP) and/or Subpopulation arrangements
- Voluntary program: applications for designation accepted ongoing (no deadline)
- Designated Innovators will engage with their contracted health plans to amend or develop new contracts to reflect the additional functions and risk the Innovator takes on in conjunction with 90–95% of premium pass through
- Innovator arrangements are subject to the same DOH and DFS regulatory and financial solvency requirements as all other MCO-Provider contracts.
Application and Intake
- The Application, Templates and Instructions for Innovator Designation are available on DOH website, VBP Resource Library
- Part A Program Summary
- Part B Application
- Part C Financial Viability Template
- Part D Financial Viability Template Instructions
- Part E Financial Viability Certification
- Part F Acknowledgement
- Part G Quarterly Reporting Template
- Innovator completes application and supporting documents and email package to bmcfhelp@health.ny.gov, subject line "Innovator Application Submission"
- Applicant receives notice that their application has been received within one business day
Part B: Application Sections
The Innovator Application must include complete responses in order for a review to be made:
Section I: Introduction and Overview Section II: Applicant Information Section III Contracting Information Section IV: Attribution and Network Section V: Innovator Readiness and Network Adequacy
Financial Viability Template & Certification and Acknowledgement must be submitted with Application
Review Criteria
The review of Innovator applications will evaluate if there is sufficient documentation to demonstrate proficiency across five criteria:
- A commitment to contracting for a high or full risk VBP L2 or L3;
- Upholding health plan network adequacy;
- Past success in VBP contracting for TCGP or Subpopulation arrangements;
- The ability to meet minimum attribution thresholds; and
- Financial solvency and appropriate net worth.
Criteria 1: VBP Commitment
The application must demonstrate all of the following:
- List and Level(s) of potential VBP arrangements;
- Either TCGP or Subpopulation arrangement;
- If L2, the minimum % of potential losses to be allocated to the provider is 60%, with a minimum threshold of at least 35% of the target budget; and
- If applicant is not currently contracting at high risk L2 or L3, it must include a written plan demonstrating how it will do so.
Criteria 2: Network Adequacy
Applicant must attest that it will:
- Comply with all health plan network adequacy requirements;
- Not limit or impede patient choice;
And must describe:
- The scope of services provided to Medicaid members; and
- How the services described reflect the needs of the community served, including addressing Social determinants of health and CBO contracting
Criteria 3: Successful VBP Experience
Applicant must describe its VBP experience in TCGP or Subpopulation arrangements and how this will be leveraged successfully as an Innovator.
- Sufficient experience means demonstrated positive quality and financial outcomes in either a:
- L1 type arrangement (3 or more years); or
- L2 or L3 type arrangements (2 or more years).
- Examples of acceptable arrangements may include, but are not limited to:
- Medicare models: ACOs, Bundled Payment for Care Improvement, Independence at Home, Primary Care innovation models;
- Commercial models: Alternative Payment Contract, bundled payment, partial/full capitation, gain sharing;
- Medicare and Medicaid Managed Care models: partial/full capitation, gain–sharing
Criteria 4: Attribution Thresholds
Prospective Innovators must provide National Provider Identifier (NPI) information suitable to demonstrate their ability to meet the following minimum attribution thresholds aggregated across all plans:
- TCGP: ≥ 25,000 Medicaid non–dual members
- Subpopulation: ≥ 5,000 Medicaid members:
- non–dual members for HIV/AIDS and Health and Recovery Plans (HARP); or
- dual and non–dual members for Managed Long–Term Care (MLTC)
Criteria 5 – Financial Solvency
Prospective Innovators must include
- Historical and current year financial statements demonstrating solvency (operating margin, days cash on hand, operating cash flow margin, and current ratio)
- Detailed plan to maintain financial viability if maximum loss occurs under proposed arrangement(s)
- Estimate of, and ability to fund, the financial security deposit
Designated Innovators will be required to submit quarterly financial information
Innovator Functions
Application must specify the delegated management and administrative functions the prospective Innovator is to perform:
- Mandatory: Utilization Review, Utilization Management and Disease Management.
- Mandatory four of seven: DUR, Appeals/Grievances, Member Services, Network Management, Provider Services Helpdesk, Provider Relations, Data Sharing
- Optional for maximum premium pass through: Claims Administration and Credentialing
Certification & Acknowledgment
- CEO or CFO must certify the financial report: Value Based Payment Innovator Interim Financial Report Certification form
- CEO, COO, General Counsel or other executive authority must accept and acknowledge Innovator Program requirements: Applicant Acknowledgement form
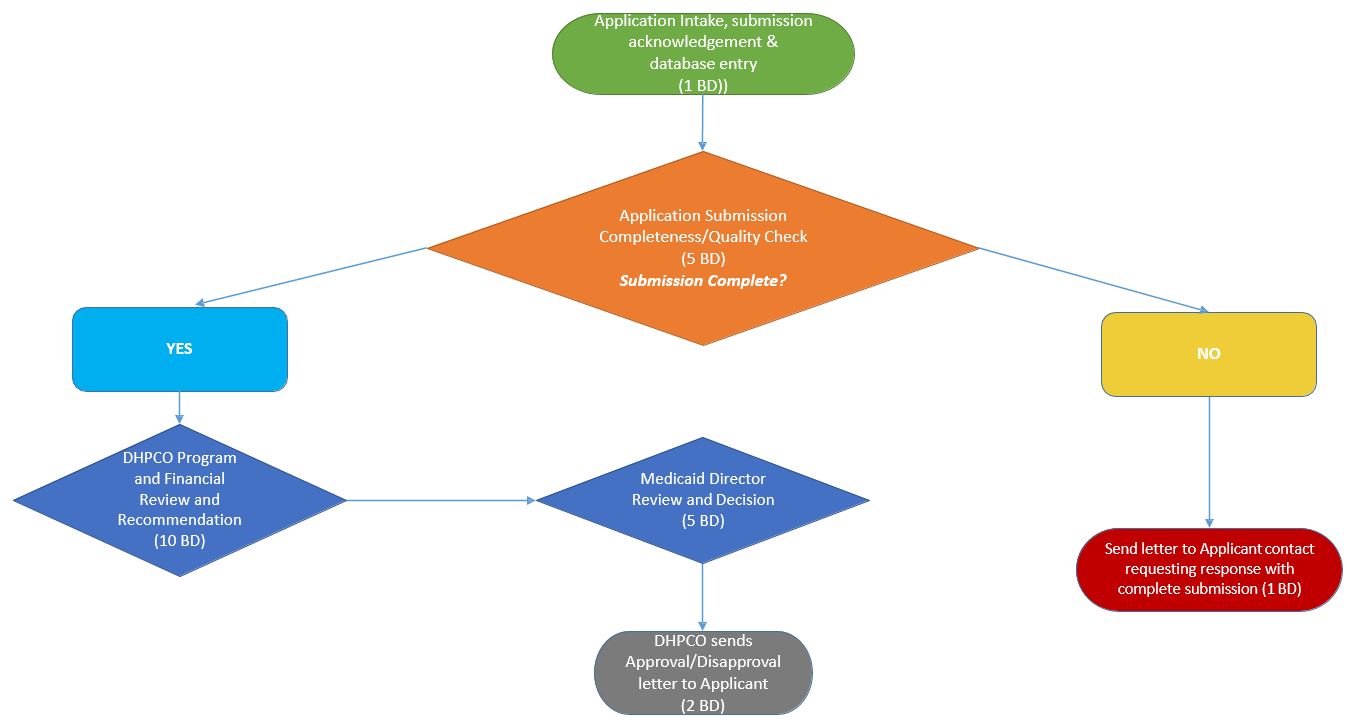
Innovator Application
Review Process
Questions?
- Written questions can be sent to bmcfhelp@health.ny.gov with the subject line "Innovator Application Question"
- Innovator FAQs will be posted to the VBP Library on the DOH Website.
Follow Us