Health and Recovery Plan (HARP)
Value Based Payment Quality Measure Set
Measurement Year 2024
- Measure Set is also available in Portable Document Format (PDF)
February 2024 NYS Medicaid Value Based Payment
INTRODUCTION
The Measurement Year (MY) 2024 Health and Recovery Plan (HARP) Quality Measure Set was created in collaboration with the Behavioral Health/HARP Clinical Advisory Group (CAG), the Primary Care (Physical Health) CAG, the New York State Department of Health (NYS DOH) CAG Strategy team, as well as subject matter experts from both the NYS Office of Mental Health (OMH) and NYS Office of Addiction Services and Supports (OASAS). The goal of this measure set is to align with measures put forth in the NYS Quality Assurance Reporting Requirements (QARR), the Healthcare Effectiveness Data and Information Set® (HEDIS)1 Technical Specifications for Health Plans, the Centers for Medicare & Medicaid (CMS) Core measure set, and the Merit-based Incentive Payment System (MIPS), where applicable. The measure set is designed to encourage providers to meet high standards of patient-centered clinical care and coordination across multiple care settings.
MEASURE SELECTION AND FEASIBILITY
Upon receiving recommendations from the CAGs, other NYS agencies, the release of guidelines from national measure stewards such as National Committee for Quality Assurance (NCQA)/HEDIS® and in accordance with the NYS Value Based Payment (VBP) Roadmap,2 the State defined a final list of measures to be included in the Behavioral Health/HARP Measure Set for MY2024. For MY2024, there are a total of thirty-one Category 1 and 2 HARP Quality Measures.
VBP ARRANGEMENT REQUIREMENTS FOR MY2024 - HEALTH EQUITY
In MY2022, NCQA added race and ethnicity stratification for five HEDIS measures to help promote transparency in health plan performance; another eight were added for MY2023. By doing so, NCQA hopes to better identify where disparities exist so they can be addressed. They also hope to identify and learn from top performers in areas where disparities don't exist. To align with this initiative, starting in July 2022, NYS requires payers and providers to incorporate race and ethnicity measure stratification in Value Based Payment (VBP) arrangements. For MY2024, HEDIS added nine additional measures, totaling 22 measures spanning numerous domains and VBP arrangement types.
Stratification Specifications:
- Payers are required to include at least one of the following measures in all level 1 or higher VBP contracts and stratify results by race and ethnicity categories as outlined in the HEDIS MY2024 specifications.3
| NQCA Measure Name | Measure Inclusion by Arrangement Type | |||||
|---|---|---|---|---|---|---|
| TCGP | HARP/BH | Maternity | HIV/AIDs | Children's | ||
| Adult Immunization Status (AIS-E)* | ✓ | |||||
| Asthma Medication Ratio (AMR)* | ✓ | ✓ | ✓ | ✓ | ||
| Breast Cancer Screening (BCS-E)* | ✓ | ✓ | ✓ | |||
| Cervical Cancer Screening (CCS; CCS-E)* | ✓ | ✓ | ✓ | |||
| Child and Adolescent Well-Care Visits (WCV) | ✓ | ✓ | ||||
| Childhood Immunization Status (CIS; CIS-E)* | ✓ | ✓ | ||||
| Colorectal Cancer Screening (COL; COL-E) | ✓ | ✓ | ✓ | |||
| Controlling High Blood Pressure (CBP) | ✓ | ✓ | ✓ | |||
| Eye Exam for Patients with Diabetes (EED)* | ✓ | ✓ | ✓ | |||
| Follow-Up After Emergency Department Visit for Mental Illness (FUM)* | ✓ | ✓ | ✓ | |||
| Follow-Up After Emergency Department Visit for Substance Use (FUA) | ✓ | ✓ | ||||
| Follow-Up After Hospitalization for Mental Illness (FUH)* | ✓ | ✓ | ||||
| Glycemic Status Assessment for Patients with Diabetes (GSD) (Formerly Hemoglobin A1c - HBD) | ✓ | ✓ | ✓ | |||
| Immunizations for Adolescents - Combo 2 (IMA, IMA-E) | ✓ | ✓ | ||||
| Initiation and Engagement of Substance Use Disorder Treatment (IET) | ✓ | ✓ | ✓ | |||
| Kidney Health Evaluation for Patients with Diabetes (KED)* | ✓ | ✓ | ✓ | |||
| Pharmacotherapy for Opioid Use Disorder (POD) | ✓ | ✓ | ||||
| Postpartum Depression Screening and Follow- Up (PDS-E)* | ✓ | |||||
| Prenatal and Postpartum Care (PPC) | ✓ | ✓ | ||||
| Prenatal Depression Screening and Follow-Up (PND-E)* | ✓ | |||||
| Prenatal Immunization Status (PRS-E)* | ✓ | ✓ | ||||
| Well-Child Visits in the First 30 Months of Life (W30) | ✓ | ✓ | ||||
*Added for MY2024
Stratification Requirements:
- Stratification of selected measures will be classified as pay-for-reporting (P4R).
- Payers are required to include the following detail in the Provider Contract Statement and Certification form and Contract language:
- Indicate what measure(s) will be included for race and ethnicity stratification.
- Indicate how the stratified measure results for applicable measures will be shared with the VBP contractor.
- Plans are required to include the race and ethnicity data to NYS using the following method:
- Race and ethnicity fields will be added to the annual VBP member attribution submission file specifications. This will allow the State to stratify measure performance by race and ethnicity categories for applicable performance measures at the VBP contract and VBP Contractor levels.
All new contracts submitted on or after July 1, 2022, must meet this requirement to be approved by NYS DOH. As of April 1, 2023, all other existing contracts were to be updated/amended at the end of the contract's current measurement period and before the contract's next measurement period began.
MEASURE CLASSIFICATION
Each measure has been designated by the State as Category 1, 2, or 3 with associated recommendations for implementation and testing for future use in VBP Arrangements. The measures below are classified by category based on an assessment of reliability, validity, and feasibility, and according to suggested method of use (either Pay for Reporting (P4R) or Pay for Performance (P4P)).
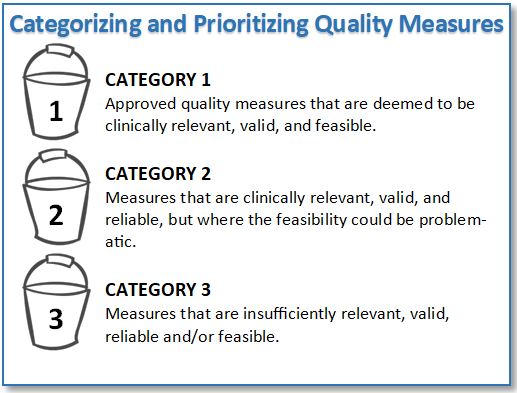
Category 1
Category 1 quality measures, as identified by the CAGs and accepted and deemed reportable by the State, are to be reported by VBP Contractors to the MCOs. These measures are also intended to be used to determine the amount of shared savings for which VBP contractors are eligible.4 At least one Category 1 P4P measure must be included in a VBP contract.
The State classified each Category 1 measure as either P4P or P4R:
- P4P measures are intended to be used in the determination of shared savings amounts for which VBP Contractors are eligible. Measures can be included in both the determination of the target budget and in the calculation of shared savings for VBP Contractors.
- P4R measures are intended to be used by the Managed Care Organizations (MCOs) to incentivize VBP Contractors to report data to monitor the quality of care delivered to members under the VBP contract. Incentives for reporting will be based on timeliness, accuracy, and completeness of data. Measures can be reclassified from P4R to P4P through annual CAG and State review or as determined by the MCO and VBP Contractor.
Not all Category 1 measures will be reportable for the measurement year, as reporting on some of these measures will be phased in over the next few years. Please refer to the 2024 Value Based Payment Reporting Requirements Technical Specifications Manual (MY2024) for details as to which measures must be reported for the measurement year. This manual will be updated annually each fall, in line with the release of the final VBP measure set for the subsequent year.
Categories 2 and 3
Category 2 measures have been accepted by the State based on the agreement of clinical importance, validity, and reliability, but flagged as presenting concerns regarding implementation feasibility.
Measures designated as Category 3 were identified as unfeasible at this time, or as presenting additional concerns, including accuracy or reliability, when applied to the attributed member population for an arrangement; therefore Category 3 measures are not included in the measure set.
MY2024 HARP QUALITY MEASURE SET
The measures and State-determined classifications provided on the following pages are recommendations for MY2024. Note that measure classification is a State recommendation, and implementation is to be determined between the MCO and VBP Contractor.
Measure sets and classifications are considered dynamic and will be reviewed annually. Updates will include measure additions, deletions, recategorizations, and/or reclassifications from P4R to P4P or vice versa, based on experience with measure implementation in the prior year. Please see Appendix A for a full list of these changes.
Category 1
The table below displays the Category 1 MY2024 Behavioral Health/HARP Quality Measure Set, arranged alphabetically, and includes measure title, measure steward, and State-recommended measure classification. The measure set is redlined to highlight changes made between MY2023 and MY2024; please refer to the key at the end of this table for an explanation of redlined formatting.
| Behavioral Health/HARP Measures | Measure Steward | Classification |
|---|---|---|
| Adherence to Antipsychotic Medications for Individuals with Schizophrenia (SAA) | Centers for Medicare & Medicaid Services (CMS) |
P4P |
| Adult Immunization Status - Electronic (Influenza)(AIS- E)** | National Committee for Quality Assurance (NCQA) |
P4P |
| Asthma Medication Ratio (AMR) | NCQA | P4P |
| Breast Cancer Screening (BCS-E)^ | NCQA | P4P |
| Cervical Cancer Screening (CCS; CCS-E)^ | NCQA | P4P |
| Chlamydia Screening in Women (CHL) | NCQA | P4P |
| Colorectal Cancer Screening ( |
NCQA | P4P |
| Continuing Engagement in Treatment Alcohol and Other Drug Dependence (CET)* | NYS | P4R |
| Controlling High Blood Pressure (CBP) | NCQA | P4P |
| COVID-19 Immunization Measure (CVS)^ | NYS | P4P |
| Diabetes Screening for People with Schizophrenia or Bipolar Disorder Who Are Using Antipsychotic Medications (SSD) | NCQA | P4P |
| Eye Exam for Patients With Diabetes (EED)^ | NCQA | P4P |
| Follow-Up After Emergency Department Visit for Mental Illness (FUM) | NCQA | P4P |
| Follow-Up After Emergency Department Visit for Substance Use (FUA) | NCQA | P4P |
| Follow-Up After High-Intensity Care for Substance Use Disorder (FUI) | NCQA | P4P |
| Follow-Up After Hospitalization for Mental Illness (FUH) | NCQA | P4P |
| NCQA | P4P | |
| Initiation of Pharmacotherapy upon New Episode of Opioid Dependence (POD-N) | NYS | P4P |
| Kidney Health Evaluation for Patients with Diabetes (KED)^ | NCQA | P4P |
| Pharmacotherapy for Opioid Use Disorder (POD) | NCQA | P4P |
| Potentially Preventable Mental Health-Related Readmission Rate 30 Days | NYS | P4P |
| Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-Up Plan | CMS | P4R |
| Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention^ | NCQA | P4R |
| Social Need Screening and Intervention (SNS-E)^ | NCQA | |
| Statin Therapy for Patients with Cardiovascular Disease (SPC)^ | NCQA | |
| Use of Pharmacotherapy for Alcohol Abuse or Dependence | NYS | P4R |
Retired/Removed for MY2024
*New Measure MY2024
^Measure Revised for MY2024
Category 2
The table below displays the Category 2 MY2024 Behavioral Health/HARP Quality Measure Set and includes the measure title and measure steward. All Category 2 measures are classified as P4R in MY2024. Category 2 measures were reviewed in detail this year and streamlined to include only those with an active measure steward and/or potential for movement to Category 1 in subsequent years. The measure set is redlined to highlight changes made between MY2023 and MY2024; please refer to the key at the end of this table for an explanation of redlined formatting.
| BEHAVIORAL HEALTH/HARP Measures | Measure Steward |
|---|---|
| Asthma Action Plan | American Academy of Allergy, Asthma & Immunology (AAAAI) |
| Asthma: Assessment of Asthma Control - Ambulatory Care Setting | AAAAI |
| Mental Health Engagement in Care 30 Days | NYS |
| Percentage of HARP Enrolled Members Who Received Personalized Recovery Oriented Services (PROS) or Home and Community-Based Services (HCBS) | NYS |
| Use of Opioid Dependence Pharmacotherapy | NYS |
Retired/Removed for MY2024
Appendix A
The table below identifies the changes to the Category 1 and Category 2 measures for the MY2024 HARP Quality Measure Set.
Category 1 Measure Changes from 2023 to 2024
| Measure Name | Change | Rationale for Change |
|---|---|---|
| Adult Immunization Status - Electronic (Influenza)(AIS-E) | New Measure | Measure added to list of CAT1 recommended measures |
| Breast Cancer Screening (BCS-E) | Measure reporting specifications revised by NCQA for HEDIS MY2024 | Implemented gender- inclusive language |
| Cervical Cancer Screening (CCS; CCS-E) | Measure reporting specifications revised by NCQA for HEDIS MY2024 | Implemented gender- inclusive language |
| Cervical Cancer Screening (CCS; CCS-E) | HEDIS Stratified Measure | Added to NCQA list of Race and Ethnicity measures - New for MY2024 |
| Colorectal Cancer Screening ( |
Measure reporting specifications revised by NCQA for HEDIS MY2024 | ECDS Reporting only |
| Continuing Engagement in Treatment Alcohol and Other Drug Dependence (CET) | Category Change | Measure added to list of CAT1 recommended measures |
| COVID-19 Immunization Measure (CVS) | Measure reporting specifications revised by NYS for MY2024 | Refer to Quality Assurance Reporting Requirements (QARR) Technical Specifications for MY2024. |
| Eye Exam for Patients with Diabetes (EED) | Measure reporting specifications revised by NCQA for HEDIS MY2024 | Revised diabetes denominator |
| Eye Exam for Patients with Diabetes (EED) | HEDIS Stratified Measure | Added to NCQA list of Race and Ethnicity measures - New for MY2024 |
| Follow-Up After Emergency Department Visit for Mental Illness (FUM) | HEDIS Stratified Measure | Added to NCQA list of Race and Ethnicity measures - New for MY2024 |
| Follow-Up After Hospitalization for Mental Illness (FUH) | HEDIS Stratified Measure | Added to NCQA list of Race and Ethnicity measures - New for MY2024 |
| Hemoglobin A1c Control for Patients with Diabetes (HBD) | Name and specifications revised for MY2024, now: Glycemic Status Assessment for Patients with Diabetes (GSD) | Revised diabetes denominator; Inclusion of Glucose Management Indicator (GMI) |
| Kidney Health Evaluation for Patients with Diabetes (KED) | HEDIS Stratified Measure | Added to NCQA list of Race and Ethnicity measures - New for MY2024 |
| Preventive Care and Screening: Influenza Immunization | Removed for MY2024 | DOH/CAG recommended removal for MY2024 |
| Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention | Measure reporting specifications revised by CMS for MY2024 | Revised age group of initial population. |
| Social Need Screening and Intervention (SNS-E) | Classification change | Second year measure; changed to P4P. |
| Statin Therapy for Patients with Cardiovascular Disease (SPC)^ | Classification change | Second year measure; changed to P4P. |
| Use of Spirometry Testing in the Assessment and Diagnosis of COPD (SPR) | Measure removed | HEDIS/NCQA retired measure for MY2024 |
Category 2 Measure Changes from 2023 to 2024
| Measure Name | Change | Rationale for Change |
|---|---|---|
| Adherence to Mood Stabilizers for Individuals with Bipolar I Disorder | Measure removed from HARP/BH MY2024 CAT 2 measure set | Steward no longer supports measure. |
| Asthma: Spirometry Evaluation | Measure removed from HARP/BH MY2024 CAT 2 measure set | Steward no longer supports measure. |
| Continuing Engagement in Treatment Alcohol and Other Drug Dependence (CET) | Measure removed a CAT 2 measure for MY2024 | Measure added to list of CAT1 recommended measures |
__________________________________________________________
1. HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). 1
2. New York State Department of Health, Medicaid Redesign Team, Value Based Payment: Update, May 2023. (Link) 2
3. HEDIS® Measurement Year 2024 Volume 2 Technical Specification for Heath Plans, General Guidelines section 31. 3
4. New York State Department of Health, Medicaid Redesign Team, Value Based Payment: Update, May 2023. (Link) 4
Follow Us