MRT 1115 Demonstration Annual Reports
- Report also available in Portable Document Format (PDF)
Demonstration Year: 20 (10/1/2016 – 9/30/2017) Federal Fiscal Quarter: 4 (7/01/2017 – 9/30/2017)
I. Introduction
In July 1997, New York State received approval from the Centers for Medicare and Medicaid Services (CMS) for its Partnership Plan Medicaid Section 1115 Demonstration. In implementing the Partnership Plan Demonstration, it was the State´s goal to:
- Improve access to health care for the Medicaid population;
- Improve the quality of health services delivered;
- Expand access to family planning services; and
- Expand coverage to additional low–income New Yorkers with resources generated through managed care efficiencies.
The primary purpose of the Demonstration was to enroll a majority of the State´s Medicaid population into managed care, and to use a managed care delivery system to deliver benefits to Medicaid recipients, create efficiencies in the Medicaid program and enable the extension of coverage to certain individuals who would otherwise be without health insurance.
The Partnership Plan Demonstration was originally authorized for a five–year period and has been extended several times. CMS had approved an extension of the 1115 waiver on September 29, 2006 for the period beginning October 1, 2006 and ending September 30, 2010. CMS subsequently approved a series of short term extensions while negotiations continued on renewing the waiver into 2016.
There have been a number of amendments to the Partnership Plan Demonstration since its initial approval in 1997. CMS approved three waiver amendments on September 30, 2011, March 30, 2012 and August 31, 2012, incorporating changes resulting from the recommendations of Governor Cuomo´s Medicaid Redesign Team (MRT). CMS recently approved the DSRIP and Behavioral Health amendments to the Partnership Plan Demonstration on April 14, 2014 and July 29, 2015, respectively.
New York State´s Federal–State Health Reform Partnership (F–SHRP) Medicaid Section 1115 Demonstration expired on March 31, 2014. Populations in the F–SHRP were transitioned into the 1115 Partnership Plan Waiver. A final draft evaluation report was submitted to CMS on February 11, 2015 and was approved by CMS on May 24, 2016.
On May 28, 2014, New York State submitted an application requesting an extension of the Partnership Plan 1115 Demonstration for five years. On May 30, 2014, CMS accepted New York´s application as complete and posted the application for a 30–day public comment period. A temporary extension was granted on December 31, 2014 which extended the waiver through March 31, 2015. Subsequent temporary extensions were granted through December 7, 2016.
New York is well positioned to lead the nation in Medicaid reform. Governor Cuomo´s Medicaid Redesign Team (MRT) has developed a multi–year action plan (A Plan to Transform the Empire State´s Medicaid Program) that when fully implemented will not only improve health outcomes for more than five million New Yorkers but also bend the state´s Medicaid cost curve.
Significant federal savings have already been realized through New York´s MRT process and substantial savings will also accrue as part of the 1115 waiver.
II. Enrollment: Fourth Quarter
MRT Waiver – Enrollment as of September 2017
| Demonstration Populations (as hard coded in the CMS 64) |
Current Enrollees (to date) |
# Voluntary Disenrolled in Current Quarter |
# Involuntary Disenrolled in Current Quarter |
|---|---|---|---|
| Population 1 – TANF Child 1 – 20 years in Mandatory Counties as of 10/1/06 | 798,988 | 7,781 | 81,403 |
| Population 2 – TANF Adults aged 21 through 64 in mandatory MC counties as of 10/1/06 | 114,283 | 2,372 | 8,182 |
| Population 3 – TANF Child 1 – 20 (´new´ MC Enrollment) | 16,779 | 226 | 11,801 |
| Population 4 – TANF Adults 21 – 64 (´new´ MC Enrollment) | 3,496 | 100 | 719 |
| Population 5 – Safety Net Adults | 571,496 | 14,474 | 70,419 |
| Population 6 – Family Health Plus Adults with Children | 0 | 0 | 0 |
| Population 7 – Family Health Plus Adults without Children | 0 | 0 | 0 |
| Population 8 – Disabled Adults and Children 0 – 64 (SSI 0–64 Current MC) | 31,070 | 1,052 | 163 |
| Population 9 – Disabled Adults and Children 0 – 64 (SSI 0–64 New MC) | 194,525 | 8,897 | 1,780 |
| Population 10 – Aged or Disabled Elderly (SSI 65+ Current MC) | 2,196 | 233 | 46 |
| Population 11 – Aged or Disabled Elderly (SSI 65+ New MC) | 59,659 | 3,596 | 1,704 |
MRT Waiver – Voluntary and Involuntary Disenrollment
| Voluntary Disenrollments | |
|---|---|
| Total # Voluntary Disenrollments in Current Demonstration Year | 38,731 or an approximate 6% decrease from last Q |
Reasons for voluntary disenrollment: Enrollment in another plan; approved enrollee request to qualify as either exempt or excluded; relocation to residence outside county of enrollment; and Local Department of Social Services (LDSS) approval to disenroll based upon appropriate cause.
WMS continues to send select closed cases to New York State of Health. Consequently, the disenrollment numbers now draw on a smaller WMS population contributing to general decline in voluntary disenrollment.
In this specific quarter, there was also a decrease in the "Enrolled in Other Plan" category of voluntary disenrollment. This would include a decrease in the mainstream plan´s passive enrollment of its own HARP eligible population into its own HARP offspring plan.
| Involuntary Disenrollments | |
|---|---|
| Total # Involuntary Disenrollments in Current Demonstration Year | 176,217 or an approximate 9% decrease from last Q |
Reasons for involuntary disenrollment: Loss of Medicaid eligibility including death, plan termination, and retro–disenrollment.
WMS continues to send select closed cases to New York State of Health. Consequently, the disenrollment numbers now draw on a smaller WMS population contributing to general decline in involuntary disenrollment.
As in the prior quarter, case closures in the WMS population decreased when compared to the prior quarter, but case closures remain high when compared to quarters in the prior fiscal year.
MRT Waiver – Affirmative Choices
| Mainstream Medicaid Managed Care | ||||
|---|---|---|---|---|
| July 2017 | ||||
| Region | Roster Enrollment | New Enrollment | Auto–assigned | Affirmative Choices |
| New York City | 1,242,673 | 19,339 | 2,450 | 16,889 |
| Rest of State | 638,187 | 12,962 | 1,422 | 11,540 |
| Statewide | 1,880,860 | 32,301 | 3,872 | 28,429 |
| August 2017 | ||||
| New York City | 1,227,308 | 22,825 | 3,091 | 19,734 |
| Rest of State | 604,954 | 14,910 | 1,420 | 13,490 |
| Statewide | 1,832,262 | 37,735 | 4,511 | 33,224 |
| September 2017 | ||||
| New York City | 1,209,385 | 18,729 | 2,335 | 16,394 |
| Rest of State | 569,784 | 12,639 | 1,035 | 11,604 |
| Statewide | 1,779,169 | 31,368 | 3,370 | 27,998 |
| Fourth Quarter | ||||
| Region | Total Affirmative Choices | |||
| New York City | 53,017 | |||
| Rest of State | 36,634 | |||
| Statewide | 89,651 | |||
| HIV SNP Plans | ||||
|---|---|---|---|---|
| July 2017 | ||||
| Region | Roster Enrollment | New Enrollment | Auto–assigned | Affirmative Choices |
| New York City | 13,294 | 144 | 0 | 144 |
| Statewide | 13,294 | 144 | 0 | 144 |
| August 2017 | ||||
| New York City | 13,317 | 218 | 0 | 218 |
| Statewide | 13,317 | 218 | 0 | 218 |
| September 2017 | ||||
| New York City | 13,323 | 169 | 0 | 169 |
| Statewide | 13,323 | 169 | 0 | 169 |
| Fourth Quarter | ||||
| Region | Total Affirmative Choices | |||
| New York City | 531 | |||
| Statewide | 531 | |||
MRT Waiver – Health and Recovery Plans Enrollment
| Health and Recovery Plans – New York City | |
|---|---|
| September 2017 | |
| Plan Name | Enrollment |
| Affinity Health Plan | 4,061 |
| Capital District Physicians Health Plan | 2,523 |
| Excellus Health Plan | 6,349 |
| HealthFirst | 21,246 |
| HealthPlus | 5,691 |
| HIP GNY | 4,748 |
| Independent Health Association | 1,637 |
| MetroPlus | 10,303 |
| Molina Healthcare (name change from Today´s Options) | 1,460 |
| MVP Health Plan | 4,131 |
| NYS Catholic Health Plan | 24,525 |
| United HealthCare | 5,821 |
| YourCare Health Plan | 1,538 |
| Total: | 94,033 |
| Health and Recovery Plans Disenrollment | |||
|---|---|---|---|
| FFY 17 – Q4 | |||
| Voluntary | Involuntary | Total | |
| July 2017 | 851 | 661 | 1,512 |
| August 2017 | 1,010 | 695 | 1,705 |
| September 2017 | 925 | 664 | 1,589 |
| Total: | 2,786 | 2,020 | 4,806 |
III. Outreach/Innovative Activities
A. Outreach Activities
New York Medicaid Choice (NYMC) Field Observations Federal Fiscal Quarter: 4
(07/01/2017 – 09/30/2017) Q4 FFY 2016–2017
As of the end of the fourth federal fiscal quarter (end of September 2017), there were 2,588,514 New York City Medicaid consumers enrolled in mainstream Medicaid managed care plans (MMC) and 52,579 Medicaid consumers enrolled in Health and Recovery Plans (HARP). MAXIMUS, the Enrollment Broker for the New York Medicaid CHOICE program (NYMC), conducted in person outreach, education, and enrollment activities in Human Resources Administration (HRA) facilities throughout the five boroughs of New York City. During the reporting period, MAXIMUS Field Customer Service Representatives (FCSRs) conducted outreach in 33 HRA facilities including six (6) HIV/AIDS Services Administration (HASA) sites, 10 Community Medicaid Offices (MA Only), and 17 Job Centers (Public Assistance). MAXIMUS reported that 12,309 clients were educated about their enrollment options and 6,954 (56%) clients made an enrollment choice. HRA´s Contract Monitoring Unit (CMU) observed a total of 2,059 presentations: 1,709 (83%) one–to–one presentations and 350 (17%) auto–assignment outreach presentations. The 2,059 presentations resulted in 646 (31%) completed managed care applications and generated a total of 818 enrollments. Also, FCSR provided 1,413 (69%) consumers with general information.
HRA´s Contract Monitoring Unit (CMU) observed 1,709 one–to–one client informational sessions – 1,675 (98%) in HRA sites and 34 (2%) in nursing home facilities. CMU monitors reported the following:
- At HRA sites, 1,174 (70%) clients received general information that included and is not limited to plan transfer, enrollment options, and mandatory enrollment.
- 501 (30%) Fee–for–Service (FFS) clients made a voluntary enrollment choice for themselves and their family members.
- Of the 501 FFS clients that selected a plan during an informational session, 213 (43%) were randomly chosen to track for timely and correct processing. CMU reported that 100% of the clients were enrolled in a health plan of their choice and appropriate notices were mailed in a timely manner.
- At nursing homes, 28 (82%) residents made voluntary enrollment choice and 6 (18%) received general information.
Infractions were observed for 56 (11%) of the 529 Enrollment Counselling sessions conducted by NYMC Field Customer Service Representatives (FCSRs) at HRA and Nursing Home sites and 55 (98%) infractions were observed at HRA sites and 1 (2%) was observed at Nursing Home sites. Key messages most often omitted were failure to disclose or explain the following:
- Lock in policy;
- Good Cause Transfer;
- Emergency Room Services;
- Transitional Care.
NYMC Field Observations Demonstration Year: 20
(10/1/2016 – 9/30/2017) FFY 2016– 2017
During FFY 2016–2017, MAXIMUS Field Customer Service Representatives (FCSRs) conducted outreach in 33 HRA facilities including 6 HIV/AIDS Services Administration (HASA) sites, 10 Community Medicaid Offices (MA Only), and 17 Job Centers (Public Assistance). MAXIMUS reported that 59,301 clients were educated about their enrollment options and 31,188 (53%) clients made an enrollment choice. HRA´s Contract Monitoring Unit (CMU) observed a total of 8,450 presentations: 7,351 (86%) one–to–one presentations and 1,189 (14%) auto–assignment outreach presentations. The 8,450 presentations resulted in 2,597 (31%) completed managed care applications and generated a total of 3,145 enrollments. Also, FCSR provided 5,089 consumers with general information.
HRA´s Contract Monitoring Unit (CMU) observed 7,351 one–to–one client informational sessions – 7,212 (98%) in HRA sites and 139 (2%) in nursing home facilities. CMU monitors reported the following:
- At HRA sites, 5,043 (70%) clients received general information that included and is not limited to plan transfer, enrollment options, and mandatory enrollment.
- 2,169 (30%) Fee–for–Service (FFS) clients made a voluntary enrollment choice for themselves and their family members.
- Of the 2,169 FFS clients that selected a plan during an informational session, 857 (40%) were randomly chosen to track for timely and correct processing. CMU reported that 100% of the clients were enrolled in a health plan of their choice and appropriate notices were mailed in a timely manner.
- At nursing homes, 93 (67%) residents made voluntary enrollment choice and 46 (33%) received general information.
Infractions were observed on 151 (7%) of the 2,247 Enrollment Counselling sessions presented at HRA and Nursing Home sites and 149 (99%) were observed at HRA sites and 2 (1 %) were observed at Nursing Home sites. Key messages most often omitted were failure to disclose or explain the following:
- Lock in policy;
- Good Cause Transfer;
- Emergency Room Services;
- Transitional Care.
Auto–Assignment (AA) Outreach Q4 FFY 2016–2017
In addition to face–to–face informational sessions, FCSRs make outreach calls to FFS clients selected for plan auto–assignment. A total of 25,058 clients were reported on the auto– assignment list by NYMC. 3,728 (15%) clients responded to the call and 1,997 (54%) were enrolled. CMU monitored 350 (9%) completed outreach calls by FCSRs in HRA facilities. The following captures those observations:
- Phone Enrollment: 117 (33%) FFS clients made a voluntary phone enrollment choice for themselves and their family members.
- 38 were randomly chosen to track for timely and correct processing and CMU confirmed that consumers were enrolled in plan selected timely.
- Undecided: 233 (67%) FFS clients did not make an enrollment choice for several reasons that include having to consult a family member and/or physician. No infractions were observed for these calls.
Infractions were observed for eight (7%) of the 117 AA Phone Enrollment Counselling sessions conducted by NYMC Field Customer Service Representatives (FCSRs) at HRA. Key messages most often omitted were failure to disclose or explain the following:
- Failed to explain specialist, standing referral process;
- Use of plan ID card;
- Lock in Policy;
- Good Cause Transfer;
- Confirm Consumer Health Plan/PCP choice.
CMU also randomly selected 389 (2%) clients from the auto–assignment list of 25,058 clients to see if outreach calls were conducted; enrollment was chosen by consumer and notices were sent in a timely manner. CMU confirmed that appropriate notices were mailed in a timely manner to all 389 clients and clients were enrolled in their plan of choice.
Auto–Assignment (AA) Outreach FFY 2016–2017
In addition to face–to–face informational sessions, FCSRs made outreach calls to FFS clients selected for plan auto–assignment. A total of 86,659 clients were reported on the auto– assignment list. CMU monitored 1,189 completed outreach calls by FCSRs in HRA facilities. The following captures those observations:
- Phone Enrollment: 350 (29%) FFS clients made a voluntary phone enrollment choice for themselves and their family members.
- Undecided: 839 (71%) FFS clients did not make an enrollment choice for several reasons that include having to consult a family member and/or physician. No infractions were observed for these calls.
Infractions were observed on 34 (3%) of the 1,189 AA Phone Enrollment Counselling sessions presented at HRA sites. Key messages most often omitted were failure to disclose or explain the following:
- Failed to explain specialist, standing referral process;
- Use of plan ID card;
- Lock in Policy;
- Good Cause Transfer;
- Confirm Consumer Health Plan/PCP choice.
CMU also randomly selected 1,360 (2%) clients from the auto–assignment list of 86,659 clients to see if outreach calls were conducted; enrollment was chosen by consumer and notices were sent in a timely manner. CMU confirmed that appropriate notices were mailed in a timely manner to all 1,360 clients and clients were enrolled in their plan of choice.
NYMC Helpline Observations Q4 FFY 2016–2017
CMU is responsible for observing calls made by Downstate residents, including residents enrolled in managed care, and is committed to observe all Customer Service Representatives (CSRs) answering New York City calls every month. NYMC reported that 64,196 calls were received by the Helpline and 58,441 or 91% were answered. Calls answered were handled in the following languages: English: 43,013 (74%); Spanish: 9,333 (16%); Chinese: 3,150 (5%); Russian: 812 (1%); Haitian: 120 (.02%); and other: 2,013 (3%).
MAXIMUS records 100% of the calls received by the NYMC helpline. CMU listened to 2,684 recorded calls. The call observations were categorized in the following manner:
- General Information: 1,403 (52%) Clients requested enrollment information and inquired about accessing plan services;
- Phone Enrollment: 512 (19%) FFS clients made a voluntary phone enrollment choice.
- Plan Transfer: 618 (23%) plan enrollees requested to change their plan;
- Public Calls: 151 (6%): Callers did not have MA eligibility and made inquiries regarding how to apply for coverage and plan enrollment or client did not want to provide CIN nor SS# to obtain non–case specific information.
Infractions/issues were identified for 657 (24%) of the recorded calls reviewed by CMU. The following summarizes those observations:
- Process: 359 (54%) – CSRs did not correctly document or failed to document the issues presented; did not provide correct information to the caller; or did not repeat the issue presented by the caller to ensure the information conveyed was accurately captured or correct;
- Key Messages: 109 (17%) – CSRs incorrectly explained or omitted how to navigate a managed care plan; use of emergency room; preventative care/explanation of PCP; and, referrals for specialists;
- Customer Service: 189 (29%) – Consumers were put on hold without an explanation or were not offered additional assistance.
NYMC is advised on a monthly basis of infractions observed and is required to develop, implement and submit a corrective action plan. Corrective actions include, but are not limited to, staff training and an increase in targeted CSR monitoring to ensure compliance.
NYMC HelpLine Observations FFY 2016–2017
CMU is responsible for observing calls made by Downstate residents, including residents enrolled in managed care, and is committed to observe all Customer Service Representatives (CSRs) answering New York City calls every month. NYMC reported that 279,718 calls were received by the Helpline and 259,780 or 93% were answered. Calls answered were handled in the following languages –English: 193,518 (74%); Spanish: 40,848 (16%); Chinese: 12,497 (5%); Russian: 3,972 (1%); Haitian: 553 (1%); and other: 8,392 (3%). MAXIMUS records 100% of the calls received by the NYMC helpline. CMU listened to 9,668 recorded calls. The call observations were categorized in the following manner:
- General Information: 5,802 (60%) Clients requested enrollment information and inquired about accessing plan services.
- Phone Enrollment: 1,490 (15%) FFS clients made a voluntary phone enrollment choice.
- Plan Transfer: 1,594 (17%) plan enrollees requested to change their plan.
- Public Calls: 782 (8%): Callers did not have MA eligibility and made inquiries regarding how to apply for coverage and plan enrollment or client did not want to provide CIN nor SS# to obtain case specific information.
Infractions/issues were identified for 2,263 (24%) of the recorded calls reviewed by CMU. The following summarizes those observations:
- Process: 1,283 (57%) – CSRs did not correctly document or failed to document the issues presented; did not provide correct information to the caller; or did not repeat the issue presented by the caller to ensure the information conveyed was accurately captured or correct.
- Key Messages: 449 (20%) – CSRs incorrectly explained or omitted how to navigate a managed care plan; use of emergency room; preventative care/explanation of PCP; and, referrals for specialists.
- Customer Service: 531 (23%) – Consumers were put on hold without an explanation or were not offered additional assistance.
NYMC is advised on a monthly basis of infractions observed and is required to develop, implement and submit a corrective action plan. Corrective actions include, but are not limited to, staff training and an increase in targeted CSR monitoring to ensure compliance.
IV. Operational/Policy Developments/Issues
Health Plans
A. Plan Expansions, Withdrawals and New Plans
- During Q4 FFY 2016–2017, there were no service area changes for Medicaid Managed Care Plans, HIV Special Needs Plans (HIV SNPs) or Health and Recovery Plans (HARPs).
- There were two approved plan expansions that occurred during the fiscal year:
- On January 9, 2017, MetroPlus Health Plan, Inc. was approved to expand its Medicaid Managed Care and HIV Special Needs Plan Service Area to include Richmond County.
- On April 3, 2017, United HealthCare of New York, Inc. was approved to expand its Medicaid Managed Care and HARP Service Area to include Franklin, Orleans, Schenectady, and Yates counties.
B. Medicaid Managed Care/Family Health Plus/HIV Special Needs Plan Model Contract
A large amendment to the 3/1/14 Medicaid Managed Care/Family Health Plus/HIV Special Needs Plan Model Contract has been under CMS review throughout most of the fiscal year. Included in this amendment are revisions related to implementation of the adult behavioral health redesign and the Health and Recovery Plan (HARP) product line, as well as new program integrity provisions and other necessary revisions related to implementation of various Medicaid Redesign Team (MRT) initiatives.
Specific milestone dates for the review of this amendment include:
- On November 18, 2016, New York State submitted the amendment to CMS for review.
- On April 11, 2017, the Department of Health received comments back from CMS regarding its review of the amendment. CMS identified several additional requirements that must be included in the amendment before CMS can approve it. Throughout the summer, the Department drafted this additional contract language, discussed these new provisions with the Health Plan Trade Associations and received Division of Legal Affairs (DLA) approval of the new language.
- On August 9, 2017, New York State submitted the CMS–requested additional contract revisions to CMS for approval. As of the close of the quarter, New York State was awaiting final CMS approval of the amendment.
C. Health Plans/Changes to Certificates of Authority
There were no changes to Certificates of Authority issued to Health Plans serving the Medicaid population during the first, third and fourth quarters of FFY 2016–2017.
The following changes occurred during the 2nd quarter FFY 2016–2017:
- Today´s Options of New York, Inc. executed a name change 1/18/17. The new name is Molina Healthcare of New York, Inc. d/b/a Molina Healthcare
- MetroPlus Health Plan, Inc. was approved to expand their Medicaid, CHP, and HARP lines of business into Richmond County effective 1/9/17.
United HealthCare of New York, Inc. was approved to expand their Medicaid and HARP lines of business into Franklin, Orleans, Schenectady, and Yates counties effective 3/31/17.
D. Surveillance Activities
Surveillance activity completed during the 4th Quarter FFY 2016–2017 (07/1/2017– 9/30/2017) include the following:
One (1) Comprehensive Operational Survey and one (1) Targeted Operational Survey were completed during the 4th Quarter FFY 2016–2017. SODs were issued and POCs were accepted for each of the following two (2) Plans.
- Healthnow (Comprehensive)
- IHA (Targeted)
Access and Availability Surveys were completed for sixteen (16) plans and Member Services Surveys were completed for eighteen (18) plans during the 4th Quarter FFY 2016–2017.
Access and Availability– An SOD was issued and a POC was accepted for fifteen (15) Plans. One (1) Plan was found in compliance:
- Affinity
- Amida Care
- CDPHP
- Excellus
- Fidelis
- HealthNow
- Healthplus (In Compliance)
- HIP
- IHA
- Metroplus
- Metroplus SNP
- Molina
- MVP
- VNS Choice
- Wellcare
- Yourcare
E. Surveillance activity completed during FFY 2016–2017 include the following:
Operational Surveys
Nine (9) Comprehensive Operational Surveys and eight (8) Targeted Operational Surveys were completed during FFY 2016–2017 (10/1/16–9/30/17). Statements of Deficiency (SODs) were issued to fourteen (14) Plans, for which Plans of Correction (POC) were received/accepted (note one plan IHA was surveyed twice in this year, receiving an SOD for each survey). Two (2) Plans were found in compliance.
1st Quarter FFY 2016–2017.
- Capital District Physicians´ Health Plan, Inc. – Targeted
- MetroPlus Special Needs Plan – Targeted (in compliance) *1
- MVP Health Plan, Inc. – Targeted (in compliance)
- Independent Health Association, Inc. – Comprehensive
2nd Quarter FFY 2016–2017
- YourCare – Targeted*
- HealthFirst Health Plan – Comprehensive*
- MetroPlus – Targeted*
- Amida Care. Inc. – Targeted
- Affinity Health Plan – Comprehensive
3rd Quarter FFY 2016–2017
- New York State Catholic Health Plan, Inc./Fidelis – Comprehensive
- WellCare of New York, Inc. – Comprehensive
- HealthPlus HP, LLC (d/b/a Empire Blue Cross Blue Shield HealthPlus) – Targeted
- VNS Choice – Comprehensive*
- Health Insurance Plan of Greater New York /Emblem – Comprehensive
- United Health Care – Comprehensive
4th Quarter FFY 2016–2017
- HealthNow New York Inc – Comprehensive
- Independent Health Association, Inc. – Targeted
Focus Surveys
Provider Directory Participation and Information Surveys were completed for the following eighteen (18) plans during the 1st Quarter FFY 2016–2017. SODs were issued to 16 plans, for which POCs were received/accepted. Two (2) plans were found in compliance.
- Affinity Health Plan, Inc.
- Amida Care, Inc.
- Capital District Physicians´ Health Plan, Inc.
- Excellus Health Plan, Inc.
- Health Insurance Plan of Greater New York
- HealthFirst PHSP, Inc.
- HealthPlus HP, LLC (d/b/a Empire Blue Cross Blue Shield HealthPlus)
- HealthNow New York Inc.
- Independent Health Association, Inc. (in compliance)
- MetroPlus Health Plan, Inc.
- MetroPlus Health Plan, Inc. Special Needs Plan
- MVP Health Plan, Inc.
- New York State Catholic Health Plan, Inc.
- Molina Healthcare of New York, Inc. d/b/a Molina Healthcare (in compliance)
- United HealthCare of New York, Inc.
- VNS CHOICE
- WellCare of New York, Inc.
- Yourcare
Access and Availability Surveys were completed for the following sixteen (16) plans during the 4th Quarter FFY 2016–2017. SODs were issued for sixteen (16) Plans, for which POCs were received/accepted.
- Affinity Health Plan, Inc.
- Amida Care
- Capital District Physicians´ Health Plan, Inc.
- Excellus Health Plan, Inc.
- Health Insurance Plan of Greater New York
- HealthPlus HP, LLC (d/b/a Empire Blue Cross Blue Shield HealthPlus)
- HealthNow New York Inc.
- Independent Health Association, Inc.
- MetroPlus Health Plan, Inc.
- MetroPlus Health Plan, Inc. Special Needs Plan
- Molina Healthcare of New York, Inc. d/b/a Molina Healthcare
- MVP Health Plan, Inc.
- New York State Catholic Health Plan, Inc.
- VNS Choice
- WellCare of New York, Inc.
- Yourcare
Member Services Surveys were completed for eighteen (18) plans during the 4th Quarter FFY 2016–2017. SODs were issued to fifteen (15) Plans, for which POCs were received/accepted. Five (5) Plans were found in compliance:
- Affinity Health Plan, Inc.
- Amida Care
- Capital District Physicians´ Health Plan, Inc. (in compliance)
- Crystal Run
- Excellus Health Plan, Inc.
- Health Insurance Plan of Greater New York
- HealthFirst PHSP, Inc.
- HealthPlus HP, LLC (d/b/a Empire Blue Cross Blue Shield HealthPlus, in compliance)
- HealthNow
- Independent Health Association, Inc. (in compliance)
- MetroPlus Health Plan, Inc. Special Needs Plan (in compliance)
- Molina Healthcare of New York, Inc. d/b/a Molina Healthcare (in compliance)
- MVP Health Plan, Inc.
- New York State Catholic Health Plan, Inc.
- United HealthCare of New York, Inc.
- VNS Choice
- WellCare
- Yourcare
V. Waiver Deliverables
A. Medicaid Eligibility Quality Control (MEQC) Reviews MEQC Reporting requirements under discussion with CMS
No activities were conducted during the quarter. Final reports have been submitted for all reviews, except for the one involved in an open legal matter.
Medicaid Eligibility Quality Control (MEQC) Reviews
- MEQC 2008 – Applications Forwarded to LDSS Offices by Enrollment Facilitators
No activities were conducted during the quarter due to a legal matter that is still open. - MEQC 2009 – Review of Medicaid Eligibility Determinations and Re– Determinations for Single and Childless Couple Individuals Determined Ineligible for Temporary Assistance
The final summary report was forwarded to the regional CMS office and CMS Central Office on July 1, 2015. - MEQC 2010 – Review of Medicaid Eligibility Determinations and Redeterminations for Persons Identified as Having a Disability
The final summary report was forwarded to the regional CMS office on January 31, 2014 and CMS Central Office on December 3, 2014. - MEQC 2011 – Review of Medicaid Self Employment Calculations
The final summary report was forwarded to the regional CMS office on June 28, 2013 and CMS Central Office on December 3, 2014. - MEQC 2012 – Review of Medicaid Income Calculations and Verifications
The final summary report was forwarded to the regional CMS office on July 25, 2013 and CMS Central Office on December 3, 2014. - MEQC 2013 – Review of Documentation Used to Assess Immigration Status and Coding
The final summary report was forwarded to the regional CMS office on August 1, 2014 and CMS Central Office on December 3, 2014.
B. Benefit Changes/Other Program Changes
Transition of Behavioral Health Services into Managed Care and Development of Health and Recovery Plans (HARPs)
In October 2015 New York State began transitioning the full Medicaid behavioral health system to managed care. The goal is to create a fully integrated behavioral health (mental health and substance use disorder) and physical health service system that provides comprehensive, accessible, and recovery oriented services. There are three components of the transition: expansion of covered behavioral health services in Medicaid Managed Care, elimination of the exclusion for Supplemental Security Income (SSI), and implementation of Health and Recovery Plans (HARPs). HARPs are specialized plans that include staff with enhanced behavioral health expertise. For Medicaid Managed Care (MMC), all Medicaid– funded behavioral health services for adults, with the exception of services in Community Residences, are part of the benefit package. Services in Community Residences and the integration of children´s behavioral health services will move to Medicaid Managed Care at a later date.
As part of the transition, the New York State Department of Health (DOH) began phasing in enrollment of current MMC enrollees throughout New York State into HARPs beginning with adults 21 and over in New York City in October 2015. This transition expanded to the rest of the state in July 2016. HARPs and HIV Special Needs Plans (HIV SNPs) now provide all covered services available through Medicaid Managed Care. NYS is monitoring plan–specific data in the three key areas of inpatient denials, outpatient denials, and claims payment.
Ongoing Monitoring of Adult Behavioral Health Transition
NYS is monitoring plan–specific data in the three key areas of inpatient denials, outpatient denials, and claims payment. These activities assist with detecting system inadequacies as they occur, and allow the State to initiate steps in addressing identified issues as soon as possible.
Inpatient Denial Report: Each month, MCOs are required to electronically submit a report to the State on all denials of inpatient behavioral health services based on medical necessity. The report includes aggregated provider level data for service authorization requests and denials, whether the denial was Pre–Service, Concurrent, or Retrospective, and the reason for the denial.
| NYS Mental Health (MH) & Substance Use Disorders (SUD) authorization requests and denials for Inpatient (07/01/2017 – 09/30/2017) | ||||
|---|---|---|---|---|
| Region | Total Authorization | Total Denials (Admin and Medical Necessity) | Utilization Review (Medical Necessity) Denials | Medical Necessity Denial Rate |
| NYC | 52,355 | 819 | 780 | 1.49% |
| ROS | 6,835 | 83 | 81 | 1.19% |
| Total | 59,190 | 902 | 861 | 1.45% |
Outpatient Denial Report: MCOs are required to submit on a quarterly basis a report to the State on ambulatory service authorization requests and denials for each behavioral health service. Submissions include counts of denials for specific service authorizations, as well as administrative denials, internal, and fair hearing appeals. In addition, HARPs are required to report authorization requests and denials of BH HCBS.
| NYS Mental Health (MH) & Substance Use Disorders (SUD) authorization requests and denials for Outpatient (07/01/2017 – 09/30/2017) | ||||
|---|---|---|---|---|
| Region | Total Authorization | Total Denials (Admin and Medical Necessity) | Utilization Review (Medical Necessity) Denials | Medical Necessity Denial Rate |
| NYC | 6,795 | 139 | 38 | 0.56% |
| ROS | 3,056 | 21 | 8 | 0.26% |
| Total | 9,851 | 160 | 46 | 0.47% |
Monthly Claims Report: On a monthly basis, MCOs are required to submit the following for all OMH and OASAS licensed and certified services. The State is not able to provide annual claims data at this time due to gaps in claims reporting in the 2nd Quarter 2017.
The table below provides a snap shot of claims data (total, paid and denied) for the period of 07/01/2017–09/30/2017.
| Mental Health (MH) & Substance Use Disorders (SUD) Claims (07/01/2017 – 09/30/2017) | ||||
|---|---|---|---|---|
| Region | Total Claims | Paid Claims (percentage of total claims reported) | Denied Claims (percentage of total claims reported) | |
| New York City | 1,452,894 | 85.75% | 15.04% | |
| Rest of State | 1,050,293 | 86.07% | 11.70% | |
| Statewide Total | 2,503,187 | 85.89% | 13.64% | |
Footnote: MCOs report monthly data. The volume of paid and denied claims could include pended claims from previous months.
HCBS Claims and Encounter Data
The tables below represent claims data for behavioral health Home and Community Based Services in NYC and Rest of State for the Quarter 4 2017 reporting period and for the annual reporting period.
Quarter 4 2017 BH HCBS Claims/Encounters Data
| HCBS Claims/Encounters: NYC, DOS: 07/01/2017 – 09/30/2017 | ||
|---|---|---|
| HCBS_SERV_GROUP | NUM_OF_CLAIMS | NUM_OF_RECIPIENTS |
| CPST | 35 | 20 |
| Education Support Services | 18 | 10 |
| Intensive Supported Employment | 27 | 12 |
| Peer Support | 102 | 27 |
| Pre–vocational | 9 | 5 |
| Provider Travel Supplement | 3 | 2 |
| Psychosocial Rehab | 54 | 21 |
| Residential Supports Services | 75 | 12 |
| Short–term Crisis Respite | 270 | 41 |
| TOTAL | 593 | 134 |
| HCBS Claims/Encounters: ROS, DOS: 07/01/2017 – 09/30/2017 | ||
|---|---|---|
| HCBS_SERV_GROUP | NUM_OF_CLAIMS | NUM_OF_RECIPIENTS |
| CPST | 5 | 2 |
| Education Support Services | 181 | 43 |
| Family Support and Training | 40 | 8 |
| Intensive Supported Employment | 22 | 11 |
| Peer Support | 665 | 110 |
| Pre–vocational | 41 | 16 |
| Provider Travel Supplement | 378 | 60 |
| Psychosocial Rehab | 275 | 63 |
| Residential Supports Services | 271 | 49 |
| Transitional Employment | 14 | 2 |
| TOTAL | 1,892 | 246 |
Note: Total of NUM_OF_RECEIPIENTS is Unique recipient, hence, not the Sum of column
Quarter 1 2016 – Quarter 4 2017 BH HCBS Claims/Encounters Data
Data reported date: 11/06/2017
| HCBS Claims/Encounters: NYC | N Recip. | ||||
|---|---|---|---|---|---|
| HCBS_SERV_GROUP | Annual Total Claims/Encounters | Q1: Oct16–Dec16 | Q2: Jan17–Mar17 | Q3: Apr17–Jun17 | Q4:Jul17–Sep17 |
| CPST | 251 | 11 | 15 | 23 | 20 |
| Education Support Services | 242 | 13 | 18 | 21 | 10 |
| Family Support and Training | 21 | 2 | 5 | 0 | 0 |
| Intensive Supported Employment | 316 | 4 | 12 | 17 | 12 |
| On–going Supported Employment | 10 | 2 | 1 | 0 | 0 |
| Peer Support | 753 | 38 | 55 | 51 | 27 |
| Pre–vocational | 400 | 17 | 17 | 27 | 5 |
| Provider Travel Supplement | 569 | 19 | 30 | 33 | 2 |
| Psychosocial Rehab | 401 | 12 | 22 | 23 | 21 |
| Residential Supports Services | 472 | 14 | 18 | 24 | 12 |
| Short–term Crisis Respite | 1406 | 37 | 35 | 45 | 41 |
| Transitional Employment | 25 | 1 | 3 | 3 | 0 |
| TOTAL | 4866 | 125 | 164 | 197 | 134 |
| HCBS Claims/Encounters: ROS | N Recip. | ||||
|---|---|---|---|---|---|
| HCBS_SERV_GROUP | Annual Total Claims/Encounters | Q1: Oct16–Dec16 | Q2: Jan17–Mar17 | Q3: Apr17–Jun17 | Q4:Jul17–Sep17 |
| CPST | 87 | 0 | 5 | 11 | 2 |
| Education Support Services | 539 | 2 | 17 | 48 | 43 |
| Family Support and Training | 137 | 2 | 7 | 11 | 8 |
| Intensive Supported Employment | 103 | 1 | 6 | 16 | 11 |
| On–going Supported Employment | 2 | 1 | 0 | 0 | 0 |
| Peer Support | 2003 | 12 | 57 | 133 | 110 |
| Pre–vocational | 265 | 4 | 16 | 28 | 16 |
| Provider Travel Supplement | 830 | 5 | 16 | 55 | 60 |
| Psychosocial Rehab | 940 | 16 | 44 | 74 | 63 |
| Residential Supports Services | 750 | 5 | 18 | 47 | 49 |
| Short–term Crisis Respite | 1 | 0 | 0 | 1 | 0 |
| Transitional Employment | 49 | 0 | 3 | 3 | 2 |
| TOTAL | 5706 | 26 | 123 | 292 | 246 |
Note: Total of "Num of Recipients" is by unique recipient, hence, not the Sum of column Data for past Quarters can be different to past data sent to CMS due to claim lags
Efforts to Promote Access to Behavioral Health Home Community Based Services (BH HCBS)
All HARP enrollees are eligible for individualized care management. In addition, Behavioral Health Home and Community Based Services (BH HCBS) have been made available to eligible HARP and HIV SNP enrollees. These services are designed to provide enrollees with specialized supports to remain in the community and assist with rehabilitation and recovery. Enrollees must undergo an assessment to determine BH HCBS eligibility. Effective January 2016 in NYC and October 2016 for the rest of the state, BH HCBS were made available to eligible individuals.
As discussed with CMS, New York experienced slower than anticipated access to BH HCBS for HARP members and has actively sought to determine the root cause for this delay. Following implementation of BH HCBS, the State and key stakeholders identified challenges, including: difficulty with enrolling HARP members in Health Homes (HH); locating enrollees and keeping them engaged throughout the lengthy assessment and Plan of Care development process; ensuring care managers have understanding of BH HCBS (including person–centered care planning) and capacity for care managers to effectively link members to rehab services; and difficulty launching BH HCBS due to low number of referrals to BH HCBS providers.
NYS is continuing its efforts to ramp up utilization and improve access to BH HCBS by addressing the challenges identified. These efforts include:
- Streamlining the BH HCBS assessment process
- Effective March 7th, 2017, the full portion of the New York State Community Mental Health assessment is no longer required. Only the brief portion (NYS Eligibility Assessment) is required to establish BH HCBS eligibility and provide access to these services.
- Ongoing development of training for care managers and HCBS providers to enhance the quality and utilization of integrated, person–centered plans of care and service provision
- Implementing rates that recognize low volume during implementation to help providers ramp up to sustainable volumes
- Enhancing Technical Assistance efforts for BH HCBS providers including workforce development and training
- Submitting a proposal to CMS to develop a pathway to BH HCBS for enrollees who are not enrolled in Health Home through MCO direct contracts with State Designated Entities to perform assessments and develop plans of care for BH HCBS
- Continuing efforts to increase HARP enrollment in HH including:
- Best practices for embedded care managers in ERs, Clinics, shelters, CPEPS and Inpatient units and engagement and retention strategies
- Existing quality improvement initiative within clinics to encourage HH enrollment
- Emphasis on warm hand–off to Health Home from ER and inpatient settings
- Ongoing work to strengthen the capacity of HH to serve high need SMI individuals and ensure their engagement in needed services through exploring the further expansion of Health Home Plus (HH+)
- Implementing Performance Management efforts, including developing and monitoring quality metrics to ensure HH care management is resulting in improved health outcomes and access to BH HCBS for HARP members
- Disseminating Consumer Education materials to improve understanding of the benefits of BH HCBS and educating peer advocates to perform outreach
- Exploring with CMS ways to utilize peers to help members understand the benefits of BH HCBS and facilitate linkage through the support of a person with lived experience.
As of November 22, 2017, 1,919 care managers in NYS have completed the required training for conducting the NYS Eligibility Assessment for BH HCBS. Also, as of, November 20, 2017, 13,804 eligibility assessments have been completed.
Ongoing Stakeholder Engagement Activities
DOH, the New York State Office of Mental Health (OMH), and the New York State Office of Alcoholism and Substance Abuse Services (OASAS) are continuing to meet regularly with managed care plans and behavioral health providers across the State to discuss stakeholder concerns and implementation challenges. The State plans to continue these meetings throughout the transition period. These stakeholder engagement efforts have included the following:
- Regional Planning Consortium (RPC) meetings for stakeholders to discuss and monitor issues related to access and availability of behavioral health services in managed care. Each RPC represents natural local patterns of access to care, and include representatives from counties, the State, consumers and families, peers and advocates, behavioral health service providers, hospitals, Health Homes and MCOs.
- In addition to the quarterly RPC board meetings, an RPC Co–Chairs Meeting occurred on October 30th, 2017 where co–chairs from each of the 11 regions across the State came together to meet with State leadership to share local impact and propose solutions related to the transition to Medicaid Managed Care.
- Examples of issues addressed at RPC meetings:
- Increasing Access to HCBS: Several RPC regions hosted HARP/HCBS networking events held to help build relationships among the MCOs, Health Homes, Care Management Agencies and HCBS providers in the regions. In addition, the RPC committees are working together to identify potential barriers to accessing HCBS what can be done to address these barriers. Other areas under review are reasons why some individuals are refusing services after the HCBS assessment is completed.
- MCO– Provider Communication: Providers expressed difficulty contacting the appropriate MCO reps in an efficient and timely manner to address HCBS billing issues. As a result, RPCs are working with MCOs to develop region– specific directory lists with updated contact info of appropriate MCO reps.
- Peer/ Family Advocate Education: Education is lacking for Peer/Family Advocates regarding HARP/HCBS services and how to access these services. To resolve this issue, multiple RPC regions are also working closely with New York Association Psychiatric Rehabilitation Services (NYAPRS) to help host Peer to Peer trainings, which provide an opportunity to inform consumers about HARP and HCBS.
- Plan Behavioral Health Clinical Directors meetings are monthly meetings convened by the New York State (NYS) Office of Mental Health (OMH), Office of Alcoholism and Substance Abuse Services (OASAS), and DOH with New York City (NYC) and Rest of State (ROS) Managed Care Organization (MMCO) Behavioral Health (BH) Medical Directors to review clinical operations issues. Covered subject matter includes announcements and updates from NYS OMH and NYS OASAS, Clinical Transformation Goals, Utilization and Care Management, Performance Measurement and Improvement, High–Need Populations, and Training. These meetings for NYC MMCO BH Medical Directors commenced in January 2015. Meetings for ROS BH MMCO Medical Directors started in May 2016. Meeting minutes are captured and follow–up items are tracked and resolved.
- A HARP–HCBS Subcommittee Workgroup was implemented by the NYS Health Home/Managed Care Organization (HH/MCO) Workgroup charged with developing recommendations for further streamlining the BH HBCS workflow and improve access to services.
- Managed Care Technical Assistance Center (MCTAC) continues to provide technical assistance to behavioral health providers and care managers in New York State, including technical assistance around billing managed care, contracting with managed care plans, and the new BH HCBS. See below for annual participation rates.
Annual Participation Rates (FY16–17)
- MCTAC offered 108 webinars and in–person events between September 1, 2016 and August 31, 2017
- 9,876 total participants
- 4,964 unique participants
- From September 1, 2016 through August 31, 2017, 281 unique OASAS agencies (67.1%) and 393 unique OMH agencies (71.3%) have participated in MCTAC.
- New York City:
- 152 OMH agencies (71.4%)
- 103 OASAS agencies (61.3%)
- Rest–of–state:
- 256 OMH agencies (72.3%)
- 190 OASAS agencies (72%)
- New York City:
- Since MCTAC´s first offering, it has engaged 343 unique OASAS agencies (81.9%) and 466 unique OMH agencies (84.6%).
- New York City:
- 186 OMH agencies (87.3%)
- 133 OASAS agencies (79.2%)
- Rest–of–state:
- 295 OMH agencies (83.3%)
- 223 OASAS agencies (84.5%)
- New York City:
Transition of School–based Health Center Services from Medicaid Fee–for–Service:
During the 4th Quarter of FFY 2016–2017, the New York State Department of Health, School Based Health Center (SBHC) providers, Medicaid managed care plans and other stakeholders continued to work together on the process of transitioning SBHC services from Medicaid fee–for–service to Medicaid managed care. The scheduled implementation date is July 1, 2018. During the quarter, three subgroups of the larger SBHC stakeholder workgroup (Credentialing and Contracting, Claims and Billing, and Quality Improvement, Utilization Management and Care Coordination), continued to meet to further discuss implementation issues and explore possible solutions. Each subgroup is co–chaired by a Managed Care Plan representative and a School Based Health Center representative and facilitated by a Department of Health staff person. During the August 25, 2017, meeting, the full SBHC workgroup met, with the co–chairs presenting the outcomes of their respective subgroup meetings. Full workgroup and subgroup activities will continue throughout 2017 and continue into 2018. The next full SBHC workgroup meeting date is to be determined. The SBHC transition guidance document and Frequently Asked Questions (FAQs) are posted to the MRT 8401 page on the DOH website.
During FFY 2016–2017 (10/1/16–9/30/17), the full SBHC Stakeholder Workgroup meetings were held on December 15, 2016, March 16, 2017, June 15, 2017 and August 25, 2017.
The workgroup was split into three subgroups: Credentialing and Contracting, Claims and Billing, and Quality Improvement, Utilization Management and Care Coordination.
Throughout the year, the small workgroups met, as needed, to work toward resolving potential implementation issues and plan for a seamless transition from Medicaid fee–for– service to Medicaid managed care on July 1, 2018.
Clotting Factor Transition from Medicaid Fee–for–service
On July 1, 2017, outpatient clotting factor products and services were transitioned into the Medicaid managed care (MMC) benefit package. All clotting factor recipients received a letter from both DOH and the recipient´s Medicaid managed care plan alerting the recipient regarding this transition and providing instruction on how the service will be covered by the MMC Plan. The recipients were also given a number to call for further guidance for any unresolved issues with this benefit transition into Medicaid managed care. DOH confirmed that all MMC Plans have established contracts with or have entered into single case agreements/letter of agreement with non–participating provider for the provision of clotting factor products. Initially, DOH held daily calls with MMC Plans and clotting factor provider. To date; there have been no substantive issues reported. The Clotting Factor transition guidance, FAQs and other clotting factor resources are posted to the MRT 8401 page on the DOH website.
Annual
During FFY 2016–2017 (10/1/16–9/30/17), the clotting factor stakeholder meetings were held on February 2, 2017, and March 2, 2017.
In addition; the DOH met with Plans and Plan Trade Associations, Clotting Factor Providers, and Clotting Factor manufacturers over the past several months, with the expectation of providing a seamless transition from Medicaid FFS to Medicaid managed care on July 1, 2017. Ongoing activities related to implementation include CMS notification, continued stakeholder engagement, rate setting, enrollee notification, and plan and provider readiness, including network development and contracting. Several clotting factor guidance documents were developed and other clotting factor resources were posted to the MRT 8401 page on the DOH website.
C. Federally Qualified Health Services (FQHC) Lawsuit
The Southern District of New York upheld the primary elements of DOH´s methodology for reimbursing FQHCs, and the Court of Appeals affirmed except it remanded for the purpose of determining whether DOH´s supplemental rate methodology adequately accounts for visits not paid for by the MCOs. In September 2016, the SDNY reopened discovery on the limited question of what information is included in the Managed Care Visit and Revenue Report and how DOH treats such information in calculating the FQHCs´ supplemental rates.
D. Managed Long Term Care Program (MLTCP)
All MLTCP models provide a person–centered plan of care, integration of health care, environmental and social services, and a supportive transition from the previous, fragmented, FFS process to coordinated managed care.
1. Accomplishments
During the July 2017 through September 2017 quarter, one MAP plan was approved for a service area reduction in two counties (Nassau and Suffolk) and, with sufficient capacity remaining, one partial capitation plan was approved to withdraw from six counties (Nassau, Suffolk, New York, Richmond, Queens, and Kings counties). There was no new plan activity in terms of plan openings or service area expansions. During the annual period of October 2016 through September 2017, the Department approved a total of six service area reductions (five partial capitation plans and one MAP plan) and five service area expansions (two partial capitation plans, two MAP plans and one PACE plan).
New York´s Enrollment Broker, NYMC, conducts the MLTC Post Enrollment Outreach Survey which contains questions specifically designed to measure the degree to which consumers could maintain their relationship with the services they were receiving prior to mandatory transitions to MLTC. For the July 2017 through September 2017 quarter, post enrollment surveys were completed for 15 enrollees. Nine of the fourteen enrollees who responded to the question (64%) indicated that they continued to receive services from the same caregivers once they became members of an MLTCP. This represents a slight decrease in affirmative responses from 70% during the previous quarter. While the number of enrollees responding to the question varied each quarter during the period October 2016 through September 2017, the percentage of those that continued to receive services from the same caregiver once they became members of an MLTCP varied within a range of 11%.
Enrollment: Total enrollment in MLTC Partial Capitation Plans grew from 181,914 to 189,071 during the July 2017 through September 2017 quarter. For that period, 13,981 individuals who were being transitioned into Managed Long Term Care made an affirmative choice, a number that is relatively consistent with the previous three quarters and that brings the 12–month total for affirmative choice to 53,409. Monthly plan–specific enrollment for the October 2016 through September 2017 annual period is submitted as an attachment.
2. Significant Program Developments
The Managed Long Term Care (MLTC) Surveillance Unit was created to monitor and improve the quality of MLTC Plan operations and service delivery. The ultimate purpose of these efforts is to ensure that the health and welfare of MLTC Plan service recipients is protected and the services received are fair and consistent.
This unit was still a relatively new unit during the annual period October 2016 through September 2017; therefore, the survey structure, monitoring activity and processes are still undergoing development and refinement. A policies and procedures manual was created, and various tracking systems have been implemented.
Surveillance activity during the year concentrated on partial capitation plans, with the first round of audits having been completed for all 31 MLTC plans. The development of monitoring systems and training for the oversight of Medicaid Advantage Plus (MAP) plans continues. Routine surveillance of MAP plans and implementation of a sanctions/monetary penalty/fining system are anticipated to begin during the coming year.
During the July 2017 through September 2017 quarter, three operational surveys and one focused survey were finalized, with Plans of Correction accepted. In addition:
- The MLTC surveillance program´s plan of correction process is under revision.
- The Year 2 survey process remains in redesign phase and the Year 2 survey schedule in development due to staffing changes, coupled with the anticipation of a new surveillance software system.
3. Issues and Problems
There were no issues or problems to report for the July 2017 through September 2017 quarter or for the annual period of October 2016 through September 2017.
4. Summary of Self–Directed Options
The transition of consumers receiving Consumer Directed Personal Assistance Service (CDPAS) was achieved during the October 2013 through September 2014 period. Self– direction is provided within the MLTCP as a consumer choice and gives individuals and families greater control over services received. Plans continue to be required to contract with a minimum of two (2) Fiscal Intermediaries in each county. The requirement continues to be monitored on a quarterly basis, and all plans are meeting that requirement.
5. Required Quarterly Reporting
Critical incidents: There were 277 critical incidents reported for the July 2017 through September 2017 quarter, an increase of three incidents over the last quarter. Critical incidents by plan for this quarter are attached. For the annual period October 2016 through September 2017, the growth in critical incidents remained in relative proportion to the growth of overall enrollment.
Grievances and Appeals: For the July 2017 through September 2017 quarter, the top reasons for the grievance/appeal remain dissatisfaction with transportation, dissatisfaction with quality of home care, home care aides late/absent on scheduled day of services, dissatisfaction with quality of other covered services, and then miscellaneous reasons.
| Period: 7/01/17 – 9/30/17 (Percentages rounded to nearest whole number) |
|||
|---|---|---|---|
| Number of Recipients: 200,869 | Grievances | Resolved | Percent Resolved |
| # Same Day | 5,260 | 5,260 | 100% |
| # Standard/Expedited | 2,997 | 2,689 | 90% |
| Total for this period | 8,257 | 7,949 | 96% |
| Appeals | 10/16–12/16 | 1/17–3/17 | 4/17–6/17 | 7/17–9/17 | Average for Four Quarters |
|---|---|---|---|---|---|
| Average Enrollment | 179,583 | 186,567 | 193,019 | 200,869 | 190,010 |
| Total Appeals | 1,055 | 1,507 | 1,433 | 1,433 | 1,357 |
| Appeals per 1,000 | 6 | 8 | 7 | 7 | 7 |
| # Decided in favor of Enrollee | 278 | 286 | 295 | 295 | 289 |
| # Decided against Enrollee | 642 | 1,000 | 1,021 | 1,021 | 921 |
| # Not decided fully in favor of Enrollee | 98 | 126 | 92 | 92 | 102 |
| # Withdrawn by Enrollee | 23 | 29 | 19 | 19 | 23 |
| # Still pending | 289 | 364 | 358 | 358 | 342 |
| Average number of days from receipt to decision | 15 | 11 | 15 | 15 | 14 |
| Grievances and Appeals per 1,000 Enrollees By Plan and Product Type July 2017 – September 2017 | ||||||
|---|---|---|---|---|---|---|
| Enrollment | Total Grievances |
Grievances per 1,000 |
Total Appeals |
Appeals per 1,000 |
||
| Partial Capitation Plan Total | 186,847 | 6,567 | 35 | 1,302 | 7 | |
| Medicaid Advantage Plus (MAP) Total | 8,325 | 559 | 67 | 220 | 26 | |
| PACE Total | 5,697 | 1,131 | 199 | 15 | 3 | |
| Total for All Products: | 200,869 | 8,257 | 41 | 1,537 | 8 | |
Total Grievances increased slightly from 8,145 during the last quarter to 8,257 during the July 2017 through September 2017 quarter. The total number of appeals also increased slightly from 1,433 during the last quarter to 1,537 during the July 2017 through September 2017 quarter. For the October 2016 through September 2017 annual period, the growth in grievance and appeals represents a smaller percentage than the growth of enrollment, and the top reasons for the grievances and appeals has remained constant during the year.
Technical Assistance Center (TAC) Activity
During the October 2016 through September 2017 annual period, the TAC Unit took in a total of 3,909 cases (calls, emails, physical mail, and faxes). Seventy–one percent of the cases were resolved within the same month of receipt. As indicated throughout this past year´s quarterly reports, the largest number of cases relate to dissatisfaction with home health care or with the enrollee´s interdisciplinary team at the plan. Questions from providers regarding billing, eligibility, and coverage also make up many cases.
The TAC Unit continually looks for ways to better capture data in a changing environment.
During the July 2017 through September 2017 quarter, the number of calls received by the TAC unit was 864, down from 980 last quarter, and down for the second quarter in a row. Again, there was a noticeable number of cases related to plan transfers, and this is likely still due to plans reducing their service areas during previous quarters.
Call volume:
- Substantiated Complaints: 291
- Unsubstantiated Complaints: 332
- Complaints Resolved Without Investigation: 45 Inquiries: 196
- Total Calls: 864
The five most common types of contacts were related to:
- Interdisciplinary Team: 18%
- Home Health Care: 17%
- Billing – Claims Denied in Error: 8%
- Billing – Provider Questions on Coverage: 4%
- Billing – Lack of Authorization: 3%
It should be noted that home health care complaints are investigated based upon a member´s subjective experience; they do not necessarily represent neglect or abuse.
Evaluations for enrollment: The Conflict Free Evaluation and Enrollment Center (CFEEC) operations were fully implemented statewide by June 30, 2015. For the July 2017 through September 2017 quarter, 10,839 people were evaluated, deemed eligible and enrolled into plans. This brings the total for the October 2016 through September 2017 annual period to 39,420.
Referrals and 30–day assessment: For the July 2017 through September 2017 quarter, MLTC plans conducted 13,264 assessments. The total number of assessments conducted this quarter has increased; however, the percentage of assessments conducted within the 30–day time frame has decreased from 86% during Q3 to 74% during Q4. This is likely related to the service area reductions and expansions that occurred during the year. During the annual period October 2016 through September 2017, a total of 44,687 assessments were completed, with 82% of those assessments being conducted within 30 days of the request. The Department continues to monitor data collection, evaluation and reporting of CFEEC activity.
Referrals outside enrollment broker: During the July 2017 through September 2017 period, the number of people who were not referred by the enrollment broker and who contacted the plan directly was 20,805, an increase from 19,578 during the previous quarter. The October 2016 through September 2017 annual period saw a steady increase (53%) in this number, which, again, is likely due to the service area reductions and expansions that occurred during the year.
| Rebalancing Efforts | 7/17–9/17 | |||||
|---|---|---|---|---|---|---|
| New Enrollees to the Plan from a nursing home transitioning to the community | 527 | |||||
| Plan Enrollees admitted to a nursing home (for any length of stay) and return to the community | 2,924 | |||||
| Current plan Enrollees permanently placed in a nursing home | 15,216 | |||||
| New Enrollees permanently placed in a nursing home who remain in a nursing home | 3,168 | |||||
During the July 2017 through September 2017 quarter, the number of current plan enrollees permanently placed in a nursing home was 15,216, an increase of 2,164. The total number for the October 2016 through September 2017 annual period was 44,468. It continues to be expected that the number of plan enrollees in a nursing home will continue to grow as new nursing home patients are required to join a managed care plan.
VI. Evaluation of the Demonstration
Comments on the draft evaluation plan were received from CMS on March 15, 2017. DOH program staff worked to address questions and comments and to finalize the analytic framework. A revised evaluation plan was submitted to CMS on May 12, 2017. Comments on revisions were received from CMS on June 15, 2017. DOH program staff worked to address questions and comments and to finalize the analytic framework and procurement of an independent evaluator. Continued questions and need for clarification delayed submission of a revised evaluation plan.
In July, DOH staff compiled a series of questions and points of clarification which were sent to the CMS evaluation team on July 13, 2017. The CMS evaluation team returned their responses to DOH questions on September 6, 2017 and revisions were made accordingly to the evaluation plan. A revised plan was submitted in October to the CMS evaluation team, however questions remain regarding the specifics needed for the analytical methods as well as the process for contracting with an independent evaluator.
VII. Consumer Issues
I. All complaints
Medicaid managed care organizations (MMCOs) are required to report the number and types of complaints on a quarterly basis. The following table outlines the complaints received by managed care product line.
| MMCO Product Line | Total Complaints 7/1/17–9/30/17 | Total Complaints FFY 17 |
|---|---|---|
| Medicaid Managed Care | 5,824 | 22,675 |
| HARP | 375 | 1,024 |
| HIV/SNP | 183 | 721 |
| Total MMCO Complaints | 6,382 | 24,420 |
As described in the table above, total MMCOs complaints/action appeals reported for the quarter equal 6,382. This represents an 8.1% increase from the prior quarter. The most frequent category of complaint is balance billing disputes representing 22% of the quarterly total (24% annually).
The top 6 most frequent categories of complaints were as follows:
| Description of Complaint | Quarter 7/1/17–9/30/17 | Annual 10/1/16–9/30/17 |
|---|---|---|
| Balance Billing | 22% | 24% |
| Reimbursement/Billing | 17% | 16% |
| Problems with Advertising/Consumer Education/Outreach/Enrollment | 6% | 10% |
| Dissatisfaction with Quality of Care | 8% | 8% |
| Difficulty with Obtaining: Dental/Orthodontia | 7% | 7% |
| Pharmacy/Formulary | 7% | 7% |
The category of problems with advertising/consumer education/outreach and enrollment has been steadily declining 60% since the first quarter of FFY 17, and currently represents 6% (6th most reported) of the complaints quarterly. Annually, this category contains 10% of the reporting and was the 3rd most reported category. This category could include allegations of improper advertising, facilitated enrollment or marketing practices; lack of education regarding MMCO procedures for obtaining services, lack of follow–up by the MMCO to determine satisfaction with services and treatment; lack of handbook distribution; and problems with ID cards, except contacts concerning non–receipt of an ID card when the contractually allowable MMCO processing time period has not yet expired.
Monitoring of Plan Reported Complaints
The Department engages in the following analysis to identify trends and potential problems:
The observed/expected ratio is a calculation is developed for each MMCO, which represents a comparison of the number of observed complaints to the number that were expected, based on the MMCO´s average enrollment for the quarter, as a portion of total enrollment among all MMCOs. For example, an observed/expected of 6.15 means that there were more than six times the number of complaints reported than were expected. An observed/expected of 0.50 means that there were only half as many complaints reported as expected.
Based on the observed/expected ratio, the Department requests that MMCOs review and analyze categories of complaints where higher than expected complaint patterns persist. In FFY 17, four plans had observed/expected ratios greater than 2.0 and include: Affinity Health Plan, Amida Care, Inc., Independent Health Association, Inc. and Molina Healthcare of New York, Inc.
MMCO Outliers January–June 2017 Observed Expected Ratio Calculations
| Plan | o/e All Categories Combined |
|---|---|
| Affinity Health Plan | 2.8 |
| Amida Care, Inc. | 13.7 |
| Independent Health Association, Inc. | 2 |
| Molina Healthcare of New York, Inc | 4.7 |
All plans have engaged in conference calls with the State and/or submitted written explanations of any surges or changes in reporting and a corrective action plan to address any trends or issues was identified.
- Affinity Health Plan: Affinity was contacted to explain slightly higher than expected reporting in the several areas including: access to family planning services, reimbursement and billing, transportation, balance billing and difficulty with obtaining Consumer Directed Personal Assistance Services (CDPAS). Affinity responded that the increased in complaints was related to faulty communication of a policy change to require greater utilization review for some benefits, including physical therapy, speech therapy, and occupational therapy. The plan implemented a corrective action plan to improve vendor oversight, provider education and enrollee notification, including re– adjudicating claims, as necessary. The Department will continue to monitor the plan´s corrective actions.
- Amida Care Inc.: Amida reported higher than expected complaints related to dental, pharmacy, and transportation. Amida performed a comprehensive review of each complaint category and has committed to monitoring more closely for improvement opportunities. Amida cited State law changes and Medicaid benefit limitations as reasons for pharmacy and dental complaints, and received increased enrollee complaints related to the State change in transportation vendors in April 2017 (the transportation benefit is not managed by the plan). As discussed in the HIV/SNP section, below. Amida has already taken several corrective actions to address complaint findings and will continue with these efforts.
- Independent Health Association, Inc.: Independent Health identified eye care, mental health/substance abuse services/treatment, and appointment availability for behavioral health home and community based services as concerns, suggesting the vendors need to improve customer service. Their corrective action plans include monthly auditing and monitoring of the member´s experience with vendors and their administrative staff. The Department will continue to monitor implementation of these efforts and outcomes.
- Molina Healthcare Of New York, Inc.: Molina Healthcare reported higher than expected complaints in that pharmacy/formulary category. Upon investigation, the plan uncovered errors in their manual reporting process, which grossly exaggerated complaints in this area. Molina Healthcare implemented new data collection systems effective July 1, 2017 and expects improvements. Other categories also had reporting discrepancies. The Department will continue to monitor the accuracy of Molina Healthcare´s complaint reporting.
If no reduction is noted following several quarters of the implementation of the corrective action, an alternate or more prescriptive response will be requested to address the issues. The Department is committed to identifying trends and to ensure MMCOs take corrective action as appropriate.
Health and Recovery Plan (HARP) Complaints/Action Appeals:
Of the total 6,382 complaints, 375 were reported by Health and Recovery Plans (HARPs). New York State began offering HARP enrollment option two phases. The first occurred October 1, 2015 for New York City enrollees and the second began on July 1, 2016 for the rest of the state. This is the third quarter for HARP complaint data reporting as a separate submission, precluding an annualized review. The greatest percentage (16% or 61 complaints) was categorized as dissatisfaction with quality of care during this quarter.
HIV/SNPS
During the quarter, 183 complaints/action appeals were reported by HIV Special Needs Plans (HIV SNPs). This represents a 4.2% decrease in the number reported in the previous quarter. The greatest percentage (19% or 34 complaints) was categorized as dissatisfaction with Provider Services (Non–medical) or MCO Services.
There are three HIV SNPs, which are specifically designed to serve Medicaid beneficiaries with HIV/AIDS, the homeless, and their children, all located in New York City. We have been in discussion with the largest of the three plans, Amida Care, to discuss their reporting over the last few quarters, as we have observed higher than expected complaints in the areas of dental, transportation and pharmacy.
Amida Care identified areas of concern and engaged in several complaint correction action plans. Amida Care has partnered with its dental vendor, HealthPlex to develop education materials and conducted an outreach education campaign to build awareness regarding oral health and educate members on dental services. In 2017, New York State enacted legislation to address the opioid epidemic, including new restrictions on prescription pain medication. The plan developed an innovative pain management program in conjunction with Beacon Health Options to design strategies for pharmacy/formulary management to reduce dissatisfaction with policies related to opioid prescribing. Areas of pain management dissatisfaction included: implementation of a tapering plan due to quantity limits on opioids, the prior authorization process, prescription override process and provider concerns related to opioids. There has been a reduction in the number of complaints in the pharmacy/formulary category since the implementation of the program. Amida Care has also coordinated meetings with the NYS transportation vendor Medical Answering Services (MAS) to form a partnership and plan of action to decrease transportation complaints. Amida Care will continue these activities and search for improvement opportunities via the quarterly Member Complaints Committee. The Department will continue to monitor Amida Care´s corrective action plans and subsequent outcomes.
Long Term Services and Supports
As SSI enrollees typically access long term services and supports, the Department monitors complaints and action appeals filed by this population with Medicaid managed care plans. Of the 6,382 total reported complaints/action appeals, mainstream MMCOs reported 625 complaints and action appeals from their SSI enrollees. This compares to 572 SSI complaints/action appeals from last quarter.
The total number of complaints/action appeals reported for SSI enrollees by category were:
| Category | Number of Complaints/Action Appeals Reported for SSI Enrollees 7/1–9/30/17 |
|---|---|
| Adult Day Care | 0 |
| Advertising/Education/Outreach/Enrollment | 14 |
| AIDS Adult Day Health Care | 0 |
| Appointment Availability – PCP | 5 |
| Appointment Availability – Specialist | 1 |
| Balance Billing | 60 |
| Communications/Physical Barrier | 1 |
| Consumer Directed Personal Assistant | 0 |
| Denial of Behavioral Health Clinical Treatment | 0 |
| Denial of Clinical Treatment | 30 |
| Dental or Orthodontia | 108 |
| Emergency Services | 2 |
| Eye Care | 1 |
| Family Planning | 0 |
| Home Health Care | 7 |
| Mental Health/Substance Abuse Services/ Treatment | 3 |
| Non–covered Services | 26 |
| Non–Permanent Resident Health Care Facility | 2 |
| Personal Care Services | 7 |
| Personal Emergency Response System | 1 |
| Pharmacy | 63 |
| Private Duty Nursing | 0 |
| Provider or MCO Services (Non–Medical) | 52 |
| Quality of Care | 131 |
| Recipient Restriction Program/Plan Initiated Disenrollment | 0 |
| Reimbursement/Billing Issues | 34 |
| Specialist or Hospital Services | 10 |
| Transportation | 7 |
| Waiting Time Too Long at Office | 2 |
| All Other Complaints | 58 |
| Total | 625 |
The top 5 categories of SSI complaints/action appeals reported were:
| Category | Percent of Total Complaints/Appeals Reported for SSI Enrollees |
|---|---|
| Quality of Care | 21% |
| Dental or Orthodontia | 17% |
| Pharmacy | 10% |
| Balance Billing | 10% |
| Provider or MCO Services (Non–Medical) | 8% |
Based on 1st and 2nd quarter trends, the Department has been monitoring the dental or orthodontia category during the Federal fiscal year. (Please note that this category has decreased from 119 complaints (21%) to 108 complaints (17%) and is no longer considered the top complaint category, as it has been replaced with quality of care.)
Annually, the Department has been identifying trends and themes for the SSI dental complaints, and identified MVP as an outlier. The Department reviewed this complaint trend with MVP. Nearly all of MVP´s administrative appeals are associated with endodontics (root canal treatment) for adults and children disputing Medicaid coverage polices for essential dental services. The Department confirmed that MVP is administering the dental benefit according to State dental guidelines. The Department continues to monitor MVP´s dental complaint trend to determine if additional enrollee education efforts are warranted.
The following complaints/action appeals were reported involving difficulty with obtaining long term services and support. The Department did not identify any overall trends impacting enrollees´ access to these services:
| Long Term Services and Supports | Number of Complaints/Action Appeals Reported |
|---|---|
| AIDS Adult Day Health Care | 0 |
| Adult Day Care | 0 |
| Consumer Directed Personal Assistant | 0 |
| Home Health Care | 7 |
| Non–Permanent Residential Health Care Facility | 1 |
| Personal Care Services | 3 |
| Personal Emergency Response System | 1 |
| Private Duty Nursing | 0 |
| Total | 11 |
Complaints Received Directly at NYSDOH
In addition to the MMCO reported complaints, the Department directly received 661 complaints attributable to Medicaid Managed Care lines of business. Annually, the Department directly received 2,554 MMC complaints.
MMC Complaints Received Directly by the Department
| Q1* | Q2* | Q3 | Q4 | Total FFY 17 |
|---|---|---|---|---|
| 484 | 729 | 680 | 661 | 2,554 |
*Q1 was previously reported as 354 MMC complaints and Q2 was previously reported as 490 MMC complaints
During an internal audit, a technical error was discovered that resulted in underreporting of complaints in quarter 1 and 2. As a result, more complaints are now being identified as Medicaid Managed Care and previous quarters have been adjusted. Upon analysis of reported complaints, the Department has not identified any particular trend indicating plan operational deficits.
VIII. Quality Assurance/Monitoring
A. Quality Measurement in Managed Long–Term Care
- In November (2016), as part of the Department´s review process for the publication and public release of its annual Report on quality performance by the Managed Long–Term Care (MLTC) plans, we released the DRAFT data to the MLTC plans as an opportunity for the plans to verify their rates.
- Also in November, the Department release to the MLTC plans, their Crude Percent Reports for the time period of January through June 2016. The Crude Percent Reports provide the plans with a distribution of their members compared to the statewide, for many of the components of the functional assessment tool.
- 2016 Managed Long–Term Care Report
The 2016 MLTC Report was publicly released in February 2017. This Report presents information on the 65 plans that were enrolling members during the data collection period. This Report is the basis for the Consumer Guides and the Quality Incentive. - 2016 Managed Long–Term Care Consumer Guides
The 2016 MLTC Consumer Guides were released in March 2017 on the Department´s website. The Guides are also printed by Maximus, our facilitated Medicaid enroller, for inclusion in new member´s packets. The Guides help new members to choose a managed long–term care plan that meets their health care needs. The Guides offer information about the quality of care offered by the different plans, and people´s opinions about the care and services the plans provide. - 2016 Quality Incentive for Managed Long–Term Care (MLTC)
2016 Quality Incentive awards were announced in February 2017. The quality incentive is calculated on the percentage of total points a plan earned in the areas of quality, satisfaction, compliance, and efficiency. Since the MLTC is budget neutral, the bottom tier did not receive any contributed monies back, all the other tiers received back a portion or full amount of contributed monies plus additional award. The awards are retroactive to the April 2016 capitation rates.
| Payer | Plan ID | Plan Name | QI Points, adjusted | Tier |
|---|---|---|---|---|
| partial | 03549135 | Extended MLTC | 74.4 | 3 |
| partial | 03234044 | ElderServe dba RiverSpring | 64.3 | 3 |
| MAP | 03173113 | Elderplan | 63.0 | 3 |
| MAP | 02942923 | GuildNet Medicaid Advantage Plus | 60.5 | 3 |
| PACE | 03072740 | Catholic Health – LIFE | 59.7 | 3 |
| partial | 03506989 | Centers Plan for Healthy Living | 59.2 | 3 |
| PACE | 01519162 | PACE CNY | 59.2 | 3 |
| partial | 02644562 | Empire BCBS HealthPlus MLTC | 57.9 | 3 |
| partial | 03420399 | VillageCareMAX | 57.9 | 3 |
| MAP | 02914056 | VNS CHOICE Total | 57.9 | 3 |
| PACE | 03320725 | Complete Senior Care | 57.9 | 3 |
| partial | 02104369 | Senior Health Partners | 54.6 | 2 |
| MAP | 03420808 | MHI Healthfirst Complete Care | 54.6 | 2 |
| partial | 03253707 | Elderplan dba Homefirst | 54.1 | 2 |
| PACE | 01234037 | CenterLight PACE | 54.1 | 2 |
| partial | 03481927 | AgeWell New York | 52.0 | 2 |
| partial | 01865329 | Independence Care System | 51.5 | 2 |
| partial | 03580307 | North Shore–LIJ Health Plan | 51.5 | 2 |
| PACE | 01674982 | Eddy Senior Care | 50.4 | 2 |
| MAP | 02927631 | Fidelis Medicaid Advantage Plus | 50.3 | 2 |
| partial | 03458546 | Aetna Better Health | 49.5 | 2 |
| partial | 03459881 | Senior Whole Health Partial | 49.0 | 2 |
| MAP | 02932896 | Senior Whole Health | 48.4 | 2 |
| partial | 01778523 | Senior Network Health | 47.7 | 2 |
| PACE | 03114514 | ArchCare Senior Life | 46.4 | 2 |
| partial | 02825230 | WellCare Advocate Partial | 43.9 | 1 |
| PACE | 01278899 | ElderONE | 43.9 | 1 |
| partial | 03475427 | Integra MLTC | 41.3 | 1 |
| partial | 01750467 | VNS CHOICE MLTC | 41.3 | 1 |
| partial | 03594052 | Montefiore MLTC | 39.3 | 1 |
| partial | 01825947 | EverCare Choice | 38.8 | 1 |
| partial | 01827572 | GuildNet | 38.8 | 1 |
| partial | 03529059 | VNA Homecare Options | 38.8 | 1 |
| partial | 01788325 | Fidelis Care at Home | 37.5 | 1 |
| partial | 03439663 | United Health Personal Assist | 36.7 | 0 |
| partial | 03690851 | Kalos Health | 36.5 | 0 |
| partial | 03581413 | Prime Health Choice | 35.3 | 0 |
| partial | 02710185 | CenterLight Select | 33.7 | 0 |
| partial | 03466906 | MetroPlus MLTC | 33.7 | 0 |
| partial | 3466800 | ArchCare Community Life | 31.1 | 0 |
| partial | 03522947 | Hamaspik Choice | 30.6 | 0 |
| partial | 03866960 | iCircle | 28.6 | 0 |
| partial | 03560441 | AlphaCare of New York | 26.5 | 0 |
| PACE | 03056544 | Total Senior Care | 25.4 | 0 |
| partial | 02188296 | Fallon Health Weinberg | 17.5 | 0 |
- 2016 Managed Long–Term Care Crude Percent Reports
- 2016 Managed Long–Term Care Crude Percent Reports
In May, we released Crude Percent Reports for the July through December 2016 time period to the Managed Long–Term Care plans. These reports are plan–specific, reflective of each plan´s July through December 2016 cohort of UAS–NY assessments, and utilize the latest, finalized patient assessment during this six–month time period. - The Crude Percent report provides a breakout by percentage (unless a metric is reported as an average) of each response level for most components of the Community Assessment, Functional Supplement, and Mental Health Supplement across two six– month time periods. Plans were also provided the percentages for the rest of the state with their plan excluded for comparison purposes. Plans were encouraged to review the reports, compare their results to previous data, and look at areas with changes from the previous reporting period to ensure data completeness.
B. Quality Measurement in Medicaid Managed Care
- Child CAHPS with Chronic Care Condition Module
- DataStat administered a CAHPS® 5.0H Medicaid Child with CCC module survey to parents/guardians of children enrolled in Medicaid and Child Health Plus managed care plans. The survey was in the field between September and December 2016. The results indicated continued satisfaction with health care and health plans. In general, families with children with (self–reported) chronic conditions more satisfied than families with children without chronic conditions. Figure 1–3 provide results for the overall responses, and stratifications of Medicaid/Child Health plus and of screened positive or negative for chronic conditions.
CCC Composites by Sub–Population
(related to care for chronic conditions)
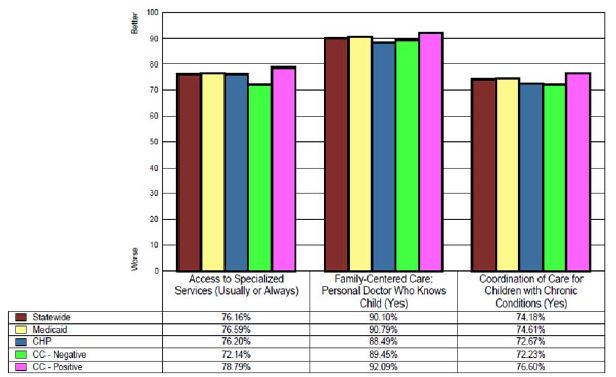
- 2016 Quality Incentive for Medicaid Managed Care
- 2016 Quality Incentive awards were announced in June 2017. The quality incentive is calculated on the percentage of total points a plan earned in the areas of quality, satisfaction and efficiency (Prevention Quality Indicators). Points for issues with Compliance are subtracted from the total plan points before calculating the percentage of total points. The 2016 awards included one plan receiving all of the award, fourteen plans receiving some portion of the award, and two plans not receiving any of the award. The awards will be implemented in April 2017 capitation rates.
| MMC Quality Incentive 2016 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Quality Points NORMALIZED to 100 based on highest score | ||||||||
| March 13, 2017 | ||||||||
| Incentive Tier | Incentive Premium Award* (%) | Plan Name | Normalized Quality Points = Quality Points/Highest Score | Satisfaction Points (30 points possible) | PQI Points (20 points possible) | Compliance Points (20 points possibly subtracted) | Total Points | Percent (up to 100%) |
| Tier 1 | 2.11% | CDPHP | 71.19 | 30 | 10 | –2 | 109.19 | 72.80 |
| Tier 1 | 2.11% | Healthfirst PHSP, Inc. | 99.43 | 15 | 0 | –6 | 108.43 | 72.28 |
| Tier 1 | 2.11% | MetroPlus Health Plan | 100.00 | 10 | 0 | –6 | 104.00 | 69.33 |
| Tier 2 | 1.59% | Fidelis Care New York, Inc. | 84.70 | 10 | 5 | –6 | 93.70 | 62.46 |
| Tier 2 | 1.59% | Hudson Health Plan | 54.01 | 20 | 12.5 | 0 | 86.51 | 57.67 |
| Tier 2 | 1.59% | Excellus BlueCross BlueShield | 47.87 | 25 | 12.5 | –2 | 83.37 | 55.58 |
| Tier 3 | 0.26% | Empire BlueCross BlueShield HealthPlus | 71.19 | 10 | 0 | –2 | 79.19 | 52.80 |
| Tier 3 | 0.26% | UnitedHealthcare Community Plan | 65.06 | 5 | 12.5 | –6 | 76.56 | 51.04 |
| Tier 3 | 0.26% | HealthNow New York Inc. | 44.30 | 15 | 15 | 0 | 74.30 | 49.54 |
| Tier 3 | 0.26% | MVP Health Care | 35.28 | 25 | 15 | –2 | 73.28 | 48.85 |
| Tier 4 | 0.00% | WellCare of New York | 50.33 | 10 | 0 | –2 | 58.33 | 38.88 |
| Tier 4 | 0.00% | Affinity Health Plan | 46.64 | 20 | 0 | –10 | 56.64 | 37.76 |
| Tier 4 | 0.00% | Independent Health´s MediSource | 33.14 | 20 | 5 | –2 | 56.14 | 37.43 |
| Tier 5 | 0.00% | Total Care, a Today´s Options of New York Health Plan | 37.98 | 15 | 7.5 | –8 | 52.48 | 34.98 |
| Tier 5 | 0.00% | YourCare Health Plan | 20.87 | 15 | 15 | –2 | 48.87 | 32.58 |
| Tier 5 | 0.00% | HIP (EmblemHealth) | 34.37 | 10 | 0 | –2 | 42.37 | 28.25 |
* Incentive premium awards were impacted by enacted budget actions for SFY 17?18 and may change to meet program fiscal targets
Quality Assurance Reporting Requirements (QARR)
We had 25 Managed Care Organizations submit Quality Assurance Reporting Requirement (QARR) data on June 15, 2017. This includes 14 of Qualified Health Plans operating through the NY State of Health Marketplace with enough eligible populations to report quality data. Data has been reviewed for completeness and accuracy and final results were published this quarter on our eQARR webpages and our consumer guides data. These reports are available here.
QUALITY IMPROVEMENT
External Quality Review
Over the past year, IPRO has continued to provide EQR services related to required, optional, and supplemental activities, as described by CMS in 42 CFR, Part 438, Subparts D and E, expounded upon in NYS´s consolidated contract with IPRO. Ongoing activities include: 1) validation of performance improvement projects (PIPs); 2) validation of performance measures; 3) review of MCO compliance with state and federal standards for access to care, structure and operations, and quality measurement and improvement; 4) validating encounter and functional assessment data reported by the MCOs; 5) overseeing collection of provider network data; 6) administering and validating consumer satisfaction surveys; 7) conducting focused clinical studies; and 8) developing reports on MCO technical performance. In addition to these specified activities, NYSDOH requires our EQR contractor to also conduct activities including, performing medical record reviews in MCOs, hospitals, and other providers; administering additional surveys of enrollee experience; and providing data processing and analytical support to the Department. EQR activities cover services offered by New York´s MMC plans, HIV– SNPs, MLTC plans, FIDAs, FIDA–IIDs, HARPs, and BHOs as well as plans that offer the state´s Child Health Insurance Program (CHP). Some projects may also include the Medicaid FFS population or on occasion, the commercial managed care population for comparison purposes.
This past year, at the request of the DOH, IPRO worked closely with the DOH Certification and Surveillance program to combine the existing Provider Directory Survey work with the Survey of Access and Provider Availability. Planning for a consolidated survey came on the heels of successfully completing these activities independently earlier in the year, and in light of an identified need for greater efficiencies. IPRO also assisted the DOH in conducting our own in–house Provider Directory survey, supplemental to one completed earlier in the year. Also related to oversight of adequate access to care, a plan Member Services survey was completed by IPRO this year. Finally, IPRO completed a survey to ensure adequate appointment availability among those providers operating at a high–volume ratio of patients to clinician. This year, that ratio was set at 2500:1. The results of all surveys were shared with the DOH and disseminated to MCO´s, with formal requests for Plans of Correction (POCs), as necessary.
Regarding provider network data oversight, IPRO is now finishing the second year of a complete rebuild of the State´s Provider Network Data System (PNDS). The rebuilt PNDS became operational this past year (on–line October 2016), and has been collecting data from MCO´s since then. A Provider Look Up tool was launched in May 2017. IPRO has been diligent in overseeing two sub–contracts for the management of this work, and has facilitated the ongoing adjustments and fixes required as new unanticipated issues arise.
Throughout this year, IPRO conducted recurring group calls to facilitate MMC and MLTC plan completion of required Performance Improvement Projects (PIPs). Plans rolled out 2017 PIP projects and IPRO continued to oversee plan completion of final reports and outstanding final reports from earlier projects. IPRO facilitated the launch of a new HARP PIP, and has been working closely with the DOH and the HARP plans to ensure a smooth start to these projects. Specific information about the MMC and HARP PIP work completed in this quarter can be found under the Performance Improvement Project description.
A new data collection platform for an ongoing Prenatal Care quality improvement project was finalized and brought on–line earlier this year. A pilot round of data entry was conducted with several plans successfully. Upon launch of a new cohort, unforeseen issues experienced by private physician practices, related to insufficient IT infrastructure to support data entry onto this new platform, resulted in an extended hold on the project. IPRO remained actively engaged with the DOH in discussing solutions to the immediate problem, and is currently supporting a work around so the project can continue without additional delays.
This year, IPRO finalized a contract with the National Committee for Quality Assurance (NCQA) to allow health plans to submit NYS quality measurement data (QARR) directly to NCQA through its IDSS tool, as they do for HEDIS measures. IPRO oversaw MCO submission of the QM data to NCQA, and collected Live Birth files. This fall, IPRO hosted an all plan technical webinar for the 2017 measurement year QARR reporting requirements, and developed Access and Utilization Reports for DOH review and dissemination.
Regarding assessment of consumer satisfaction, IPRO continues to oversee a sub–contract with DataStat for the design and administration of a Medicaid CAHPS surveys. This year, IPRO worked closely with the DOH to ensure satisfactory completion of a 2016 child CAHPS survey, and to facilitate the roll–out of a fall 2017 adult CAHPS survey.
They also administered a MLTC satisfaction survey, complete with telephonic follow–up to enhance response rates. In addition, for the first time, IPRO facilitated and administered a non–CAHPS perceptions of care survey of the HARP population, working directly with the Office of Mental Health.
IPRO continues to be involved in an audit of the State´s Uniform Assessment System (UAS), and is currently working with the MLTC program to plan an MLTC Focused Clinical Study to validate assessments being completed by Maximus nurse reviewers. IPRO is also helping DOH programs plan a new Managed Care Focused Clinical Study, examining care management of select conditions.
Performance Improvement Projects (PIPs) for Medicaid Managed Care Plans (MMC)
The Prenatal Care quality improvement project was on hold from August 2017 until November 2017, while IPRO created an alternative excel file for practices experiencing technical issues when submitting their medical record review data. The 47 practices are to complete their reviews in December 2017. The aggregate data will be reported back to the participating practices to be able to compare their performance to their peers.
Performance Improvement Projects (PIPs) for Medicaid Managed Care Plans (MMC)
For 2015–2016, the two–year common–themed PIP to address smoking cessation among Medicaid managed care (MMC) enrolled smokers was implemented. Identification of MCO enrollees who are smokers was included as a major focus of the projects.
Additionally, all plans were required to specifically improve access (and reduce barriers) to existing evidence based Medicaid benefits that reduce tobacco dependence and increase quit rates. The Final PIP Reports were submitted to IPRO in July 2017. The Final Reports are currently under review. Once they are finalized a Compendium of abstracts will be prepared and available on the public website.
For the 2017–2018 Health and Recovery Plan (HARP) and HIV Special Needs Plan (SNP) PIP the selected common topic is Inpatient Care Transitions. Fifteen PIP Proposals were submitted and have been reviewed and accepted by IPRO, NYSDOH, the Office of Mental Health (OMH) and the Office of Alcohol and Substance Abuse Services (OASAS). Oversight calls with IPRO and individual HARP plans and HIV SNP plans were conducted in July 2017. Each plan submitted a written summary of progress to IPRO before the call was conducted.
For the 2017–2018 PIP for the MMC plans the selected common topic is Perinatal Care. There are four priority focus areas to be addressed in this PIP: history of prior spontaneous preterm birth; unintended pregnancy suboptimal birth spacing; maternal smoking; and maternal depression. Fifteen Medicaid managed care plans submitted their Perinatal PIP Proposals and IPRO and NYSDOH have reviewed and accepted them. The IPRO oversight calls were conducted in August 2017. Each plan submitted a written summary of progress to IPRO before the call was conducted. On May 11, 2017, a webinar was conducted and the March of Dimes presented on national and New York state examples of initiatives to promote the use of 17P for the prevention of preterm birth in eligible women. In addition, there was discussion of the many resources available to assist the Medicaid managed care plans in implementing their interventions, such as provider toolkits, provider surveys, 17P brochures and fact sheets. The topic of birth spacing was also addressed and a provider toolkit was presented. On June 27, 2017, a webinar by the American Congress of Obstetricians and Gynecologists (ACOG) was conducted. The presentation focused on the prevention of preterm deliveries. The epidemiology of preterm labor and risk factors to assess for were presented. The appropriate use of 17P only for eligible women was discussed. Additional interventions for other high–risk conditions, e.g. short cervix, were presented. ACOG resources were presented, including Preventing Preterm Birth Video Series, and a toolkit for enhancing access to Long–Acting Reversible Contraception (LARC) in the office setting. ACOG also presented a Perinatal Depression Toolkit that is available. Finally, ACOG presented an eToolkit for Smoking Cessation: Enhancing Early Assessment, Diagnosis and Treatment of the Casual Smoker. On October 23, 2017, a required Perinatal PIP webinar was conducted. Three Medicaid managed care plans presented their Perinatal PIP progress to the group. There are three additional webinars scheduled for the other plans to present on their PIP progress in 2018.
Breast Cancer Selective Contracting
Staff successfully completed the Breast Cancer Selective Contracting process for contract year 2017–2018. Inpatient and outpatient surgical data extracted from the Statewide Planning and Research Cooperative System (SPARCS) were analyzed to identify low–volume restricted, low–volume access, and high–volume facilities. In total, the annual review identified 255 facilities. Facility designations were as follows: 115 high–volume facilities, 26 low–volume access facilities, 73 low–volume restricted facilities, and 41 closed facilities. Appeals were received from 6 low–volume restricted facilities, and only one was accepted.
Results were shared with the following stakeholders: restricted facilities; staff at eMedNY who ensure restricted facilities are denied Medicaid fee–for service payment; and, Medicaid managed care health plans´ Chief Executive Officers and Medical Directors.
Staff also completed the summer review of breast cancer surgical volume designations and the results were shared with facilities´ SPARCS coordinators in August 2017. The release of these data will give the facilities ample time to identify and correct any discrepancies between facility–calculated volume and SPARCS reported volume.
Additionally, progress was made on the evaluation of the Breast Cancer Selective Contracting Policy and the impact of the policy on access to care, quality of care and survival rates.
Patient Centered Medical Home (PCMH)
As of September 2017, there were 7,154 NCQA–recognized PCMH providers in New York State. 249 providers that became recognized in September 2017 were new to the program and have not been recognized previously. Over the past year the program has consistently seen an increase in the number of new providers joining the program who have never participated before. Approximately 91% (6,390) of current PCMH providers are recognized under the newest 2014 set of standards. Between September 2016 and September 2017, the percentage shift of providers recognized under the newest standards increased from 44% to 91%. We expect to see a continued increase in providers recognized under the 2014 standards due to incentives encouraging practices to strive for the highest PCMH standard. About 9% (615) of recognized providers are still under the 2011 standards and they are expected to all expire by mid–2018. On April 1, 2017 NCQA released their 2017 recognition standards, eliminating the leveling structure. There are currently no practices or providers recognized under the 2017 standards but some sites have applied. Under the new program, it can take up to one year for NCQA to grant PCMH–recognition, as opposed to the guaranteed 90–day review process NCQA offered for sites who submitted applications under all previous standards. The incentive rates for the New York Medicaid PCMH Statewide Incentive Payment Program as of September 2017 are:
- 2011 level 2: %0 per member per month (PMPM)
- 2011 level 3: %0 PMPM
- 2014 level 2: %3 PMPM
- 2014 level 3: %7.50 PMPM
- 2017 recognition: %7.50 PMPM
DSRIP requires certain practices participating in primary care transformation projects to become 2014 level 3 PCMH or Advanced Primary Care (APC) recognized by March 31, 2018. Currently, there are no providers that are APC recognized but there are around 1,000 providers engaged in transformation. Some sites (15% or fewer) going for APC recognition are already PCMH recognized.
The Adirondack Medical Home demonstration (´ADK´), a multi–payer medical home demonstration in the Adirondack region, has continued with monthly meetings for participating payers. There is still a commitment across payers and providers to continue through 2019 but discussions around alignment of methods for shared savings models are still not finalized. Some plans will engage in risk arrangements with the sites that are different than what other plans offer to the same sites. All payments will be made to the newly approved Adirondack Accountable Care Organization (ACO) under the new participation agreement. The ACO will also be responsible for maintaining the funds and distributing among the participating practices in the region, as well as coordinating information between payers and providers. The Adirondack Health Institute (AHI) is working with the new data analytics vendor, Health Catalyst, and the payers to get all data use agreements signed. There is a quality subcommittee for this demonstration that has finalized a measure set to measure quality and performance for these sites over the next few years of participation.
The March 2017 PCMH Statewide quarterly report was posted to the DOH website this past quarter. All quarterly and annual reports on NYS PCMH and ADK program growth can be found on the MRT website, available here.
IX. Transition Plan Updates
No updates.
X. Financial, Budget Neutrality Development/Issues
A. Quarterly Expenditure Report Using CMS–64
At the end of December 2016, New York submitted an updated Specifications Manual and a draft remediation plan and timeline for the completion of the budget neutrality reconciliation process, including plans to reconcile with the CMS–64. The budget neutrality remediation efforts are nearing completion, with initial calculations for DY15 and DY16 submitted on April 28, 2017 and June 29, 2017, respectively.
In early June, NYSDOH FMG uncovered an issue concerning data entry for the New Adult Group relating to reporting overlap of this MEG and Group VIII. New York State notified
CMS about this issue and requested expedient guidance, which CMS provided. The State is on track to meet the new project deadline of December 31, 2017 for DY14–DY17 quarter 2 and expects to provide DY17 quarters 3 and 4 by the new July 1, 2018 deadline without issue.
New York remains in regular contact with CMS regarding the progress of this project. At this time, the state budget neutrality team is entirely focused on the remediation effort and on the development and implementation of the internal processes necessary to ensure New York remains in compliance with Quarterly Expenditure Reporting requirements going forward. The state expects to resume timely quarterly expenditure reporting once the reconciliation process is complete.
As detailed in STC X.10, the State has identified a contractor to complete a certified and audited final assessment of budget neutrality for the 10/1/11–3/31/16 period. The audit will commence upon completion of remediation efforts and CMS approval of the audit plan.
B. Designated State Health Programs
No updates this quarter.
XI. Other
A. Transformed Medicaid Statistical Information Systems (T–MSIS)
New York State T–MSIS is current in its submission of production files.
Annual Summary T–MSIS
New York State T–MSIS entered production and sent its first production files on 12/27/2016 to CMS. New York State T–MSIS completed the submission of its twenty months of production catch–up files in March 2017. New York State T–MSIS has several projects on going to address T–MSIS reporting. These projects are:
- T–MSIS – Additional fields from eMedNY
- Social Security Number Removal Initiative (SSNRI)
- Changes to T–MSIS processing for ABP, ADJ_IND and HIPP Claims based on new CMS Guidance
- Changes to T–MSIS processing for Waiver reporting on Claim and Managed files based on new CMS Guidance
- Changes to T–MSIS processing for Money Follows the Person reporting on Claim files based on new DOH Guidance
- T–MSIS Data Quality Report Assessment
- T–MSIS Non–Claims Workgroup
B. Medicaid Managed Care/Family Health Plus/HIV Special Needs Plan Model Contract
On November 18, 2016, New York State submitted to CMS an amendment to the March 1, 2014 Medicaid Managed Care/Family Health Plus/HIV Special Needs Model Contract. This contract amendment includes revisions related to implementation of the adult behavioral health redesign and the Health and Recovery Plan (HARP) product line, as well as new program integrity provisions and other necessary revisions related to implementation of various Medicaid Redesign Team (MRT) initiatives.
C. 1115 Waiver Public Comment Days
With the implementation of the Medicaid Redesign Team in 2011, New York has prioritized transparency and public engagement as a key element of developing and implementing Medicaid policies. The public comments provided at these forums has been shared with the New York teams working on these programs and has informed implementation activities. We will continue to consider these issues and engage stakeholders as part of our ongoing efforts.
On August 14, 2017, the Department of Health conducted a public forum held at the School of Public Health, Rensselaer, NY (Upstate) and again on November 16, 2017 held at the Academy for Medicine, Manhattan, NY.
A recording of the live webcasts, written comments, meeting notes, and presentation slides from each public forum are available for viewing here. To access the information, click on "Latest News" and scroll to "New York´s 1115 Waiver Programs Public Comment Days."
Attachments:
Attachment 1 – MLTC Partial Capitation
Plans Attachment 2 – Critical Incidents
Attachment 3 – Medicaid Managed Care Transition Authorities Analysis
State Contact:
Priscilla Smith
Medical Assistance Specialist III
Division of Program Development and Management
Office of Health Insurance Programs
priscilla.smith@health.ny.gov
Phone (518) 486–5890
Fax# (518) 473–1764
Submitted via email: 12/20/2017
Uploaded to PMDA: 12/20/2017
Managed Long Term Care Partial Capitation Plans
October 2016–September 2017
| Oct–16 | Nov–16 | Dec–16 | Jan–17 | Feb–17 | Mar–17 | Apr–17 | May–17 | Jun–17 | Jul–17 | Aug–17 | Sep–17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Plan Name | Enrollment | Enrollment | Enrollment | Enrollment | Enrollment | Enrollment | Enrollment | Enrollment | Enrollment | Enrollment | Enrollment | Enrollment |
| Aetna Better Health | 3,881 | 3,886 | 3,943 | 4,028 | 4,057 | 4,105 | 4,145 | 4,196 | 4,258 | 4,335 | 4,411 | 4,542 |
| AgeWell New York | 7,355 | 7,524 | 7,663 | 7,828 | 7,939 | 8,079 | 8,227 | 8,409 | 8,522 | 8,542 | 8,607 | 8,690 |
| AlphaCare | 3,154 | 3,263 | 3,347 | 3,428 | 3,528 | 3,627 | 3,735 | 3,856 | 3,951 | 4,134 | 4,282 | 4,459 |
| ArchCare Community Life | 2,175 | 2,219 | 2,231 | 2,273 | 2,298 | 2,339 | 2,400 | 2,509 | 2,623 | 2,695 | 2,783 | 2,871 |
| CCM Select | 5,135 | 5,099 | 4,969 | 4,819 | 50 | 53 | 13 | 1 | 1 | 1 | 0 | 0 |
| Centers Plan for Healthy Living | 7,829 | 8,373 | 8,950 | 9,587 | 14,711 | 15,147 | 15,777 | 16,345 | 16,881 | 17,532 | 18,057 | 18,660 |
| Elant | 829 | 823 | 826 | 839 | 852 | 847 | 843 | 839 | 847 | 854 | 853 | 874 |
| Elderplan | 11,559 | 11,721 | 11,942 | 12,093 | 12,175 | 12,239 | 12,340 | 12,421 | 12,515 | 12,583 | 12,463 | 12,486 |
| Elderserve | 11,033 | 11,037 | 11,072 | 11,084 | 11,113 | 11,158 | 11,207 | 11,196 | 11,231 | 11,248 | 11,265 | 11,277 |
| Elderwood | 62 | 74 | 85 | 88 | 99 | 103 | 107 | 116 | 123 | 140 | 151 | 154 |
| Extended MLTC | 1,613 | 1,692 | 1,771 | 1,819 | 1,913 | 1,983 | 2,098 | 2,307 | 2,475 | 2,660 | 2,800 | 2,895 |
| Fallon Health Weinberg (TAIP) | 419 | 437 | 459 | 466 | 483 | 504 | 521 | 536 | 563 | 573 | 584 | 602 |
| Fidelis Care at Home | 16,073 | 16,454 | 16,804 | 17,184 | 17,421 | 17,655 | 17,959 | 18,278 | 18,622 | 19,092 | 19,226 | 19,487 |
| Guildnet | 16,413 | 16,098 | 15,916 | 15,709 | 15,228 | 14,768 | 14,253 | 12,818 | 11,450 | 10,826 | 10,116 | 9,722 |
| Hamaspik Choice | 1,901 | 1,940 | 1,986 | 2,010 | 2,018 | 2,016 | 2,020 | 2,028 | 2,028 | 2,034 | 2,032 | 2,054 |
| HealthPlus– Amerigroup | 3,767 | 3,876 | 3,950 | 4,021 | 4,119 | 4,176 | 4,241 | 4,337 | 4,427 | 4,549 | 4,597 | 4,628 |
| iCircle Services | 1,534 | 1,577 | 1,625 | 1,668 | 1,719 | 1,725 | 1,760 | 1,789 | 1,854 | 1,915 | 2,000 | 2,054 |
| Independence Care Systems | 6,348 | 6,447 | 6,514 | 6,574 | 6,593 | 6,504 | 6,535 | 6,558 | 6,569 | 6,579 | 6,606 | 6,600 |
| Integra | 4,241 | 4,438 | 4,607 | 4,794 | 5,064 | 5,279 | 5,516 | 5,890 | 6,190 | 6,500 | 6,852 | 7,191 |
| Kalos Health– Erie Niagara | 874 | 913 | 936 | 961 | 978 | 987 | 1,030 | 1,088 | 1,115 | 1,151 | 1,169 | 1,210 |
| MetroPlus MLTC | 1,300 | 1,355 | 1,382 | 1,413 | 1,439 | 1,460 | 1,506 | 1,528 | 1,573 | 1,609 | 1,623 | 1,653 |
| Montefiore HMO | 1,226 | 1,262 | 1,272 | 1,284 | 1,270 | 1,275 | 1,288 | 1,305 | 1,341 | 1,380 | 1,393 | 1,404 |
| North Shore–LIJ Health Plan | 4,068 | 4,249 | 4,413 | 4,556 | 4,691 | 4,806 | 4,986 | 5,229 | 5,477 | 5,693 | 5,756 | 5,645 |
| Prime Health Choice | 229 | 230 | 235 | 244 | 248 | 263 | 265 | 275 | 276 | 282 | 295 | 301 |
| Senior Health Partners | 12,845 | 12,950 | 13,028 | 13,158 | 13,217 | 13,314 | 13,479 | 13,657 | 13,809 | 13,878 | 13,960 | 14,082 |
| Senior Network Health | 522 | 521 | 514 | 515 | 510 | 521 | 518 | 516 | 527 | 524 | 524 | 530 |
| Senior Whole Health | 6,163 | 6,483 | 6,696 | 6,912 | 7,162 | 7,373 | 7,599 | 7,981 | 8,303 | 8,561 | 8,826 | 9,141 |
| United Healthcare | 2,552 | 2,626 | 2,657 | 2,721 | 2,765 | 2,798 | 2,840 | 2,876 | 2,979 | 3,120 | 3,244 | 3,370 |
| Village Care | 6,773 | 6,986 | 7,190 | 7,304 | 7,455 | 7,466 | 7,667 | 7,906 | 8,102 | 8,328 | 8,525 | 8,713 |
| VNA HomeCare Options | 2,986 | 3,224 | 3,372 | 3,542 | 3,755 | 3,993 | 4,216 | 4,447 | 4,733 | 4,914 | 5,146 | 5,363 |
| VNS Choice | 13,861 | 13,759 | 13,631 | 13,645 | 13,417 | 13,193 | 13,032 | 12,819 | 12,764 | 12,824 | 12,719 | 12,644 |
| WellCare | 6,061 | 6,054 | 6,032 | 6,036 | 5,965 | 5,898 | 5,862 | 5,804 | 5,781 | 5,787 | 5,761 | 5,769 |
| TOTAL | 164,781 | 167,590 | 170,018 | 172,603 | 174,252 | 175,654 | 177,985 | 179,860 | 181,914 | 184,843 | 186,626 | 189,071 |
Critical Incidents
| Plan Name | Plan Type | Total Critical Incidents |
|---|---|---|
| Partial Capitation Plans | ||
| Aetna Better Health | Partial | 0 |
| AgeWell New York ,LLC | Partial | 7 |
| AlphaCare of New York Inc. | Partial | 1 |
| Amerigroup | Partial | 0 |
| ArchCare Community Life | Partial | 12 |
| CenterLight Healthcare Select | Partial | 0 |
| Centers Plan for Healthy Living | Partial | 7 |
| Elant Choice | Partial | 0 |
| ElderServe Health, Inc. | Partial | 1 |
| Elderwood | Partial | 1 |
| Extended | Partial | 0 |
| Fallon Health Weinberg | Partial | 0 |
| FIDELIS Care New York | Partial | 0 |
| GuildNet MLTCP | Partial | 30 |
| Hamaspik Choice | Partial | 0 |
| HomeFirst MLTC, a product of Elderplan | Partial | 2 |
| I Circle | Partial | 0 |
| Independence Care Systems | Partial | 9 |
| Integra MLTC | Partial | 0 |
| Kalos, dba First Choice Health | Partial | 0 |
| Metroplus | Partial | 0 |
| Montefiore Diamond Care | Partial | 4 |
| NSLIJ Health Plan | Partial | 0 |
| Prime Health Choice, LLC | Partial | 35 |
| Senior Health Partners | Partial | 59 |
| Senior Network Health | Partial | 0 |
| Senior Whole Health | Partial | 0 |
| United Healthcare Personal Assist | Partial | 0 |
| VillageCareMAX | Partial | 6 |
| VNA Homecare Options, LLC | Partial | 23 |
| VNSNY CHOICE MLTC | Partial | 0 |
| Wellcare | Partial | 21 |
| Total | 218 | |
| Medicaid Advantage Plus (MAP) | ||
| Elderplan | MAP | 0 |
| Fidelis Medicaid Advantage Plus | MAP | 0 |
| GuildNet GNG | MAP | 0 |
| Healthfirst CompleteCare | MAP | 15 |
| HEALTHPLUS AMERIGROUP | MAP | 0 |
| Senior Whole Health | MAP | 0 |
| VNSNY CHOICE MLTC TOTAL | MAP | 0 |
| Total | 15 | |
| Program of All‐Inclusive Care for the Elderly (PACE) | ||
| ArchCare Senior Life | PACE | 5 |
| Catholic Health LIFE | PACE | 13 |
| CenterLight Healthcare | PACE | 0 |
| Complete Senior Care | PACE | 5 |
| Eddy SeniorCare | PACE | 3 |
| ElderONE | PACE | 0 |
| Fallon Health Weinberg | PACE | 0 |
| Independent Living Services of CNY (PACE CNY) | PACE | 18 |
| Total Senior Care | PACE | 0 |
| Total | 44 | |
| Grand Total | 277 | |
Medicaid Managed Care Authority Transition Analysis
Office of Health Insurance Programs
New York State Department of Health
Medicaid Managed Care Authority Transition Analysis
The Special Terms and Conditions for New York Medicaid Redesign Team (MRT) Section 1115 Waiver (11–W00114/2) requires the State to evaluate which portions of the State´s Medicaid managed care demonstration could be transitioned to another authority under Title XIX of the Social Security Act authority, such as Sections 1915(b),1915(c), or 1932. The State completed this analysis in December 2017, and finds that no portion of the demonstration is appropriate for transition to another Title XIX authority.
To conduct this evaluation, the State reviewed each specific waiver included in the MRT 1115 and each expenditure authority permitted under the Special Terms and Conditions, and compared these allowances to the possible waivers and/or service delivery options allowed under alternate Title XIX authorities, based on CMS published guidance. In addition, the State reviewed its 1115 MRT demonstration program design elements, such as benefits not included in the State Plan, mandatory enrollment, and health care system transformation activities to determine if these objectives could be achieved under existing federal regulation or alternate Title XIX authority.
The State´s analysis shows that other available Title XIX authorities which permit mandatory Medicaid managed care programs are insufficient in scope to support the State´s MRT 1115 initiatives to increase quality of care; increase overall coverage; increase access to and stabilize service delivery networks; prevent breaks in coverage for low–income individuals; and improve health outcomes. While the four Social Security Act sections waived: statewideness, income comparability, service comparability, and freedom of choice, may be possible under an alternate authority, the MRT 1115 demonstration combines these specific waivers with expenditure authorities in a manner that remains unsupported outside of the Section 1115 authority. For example, the MRT 1115 demonstration provides a twelve–month continuous eligibility period for certain populations; provides HCBS to at–risk adult populations through HARPs and HIV SNPs; and requires value based payment plan–provider contracting targets in support of DSRIP objectives and metrics. In addition, the State´s 1115 amendments, submitted to CMS in 2017, further expand covered populations and services to those not available under the State Plan or 1915(c) authority. Results of this evaluation appear in the following table:
| Title XIX Authority | New York State Analysis |
|---|---|
| Section 1932(a) State Plan Amendment Authority | The MRT 1115 demonstration provides Medicaid coverage through enrollment in Medicaid Managed Care plans for most populations, including SSI children and children in foster care, and will be expanded to other children with special health care needs, pending approval of the children´s 1115 amendment submitted to CMS in May 2017. Section 1932(a) State Plan authority does not permit children with special health care needs to be enrolled in Medicaid managed care. |
| Section 1915(a) Exception to State Plan Requirements for Voluntary Managed Care | The MRT 1115 demonstration enrolls most populations on a mandatory basis statewide in Medicaid managed care. This authority does not permit mandatory enrollment. |
| Section 1915(b) Waivers | The MRT 1115 demonstration includes several provision integral to the success of the demonstration including continuous eligibility for adults, facilitated enrollment services by MCOs, at–risk populations for HARP, and IMD services for substance use disorder treatment. These are not permitted under this authority, even in combination with 1915(c) and 1915(i) waivers. This authority does support Medicaid Redesign and DSRIP activities. |
| Section 1915(c) "Home and Community–Based Services (HCBS)" Waivers | The MRT 1115 demonstration provides comprehensive coverage for most populations. This authority is for HCBS only. |
| Concurrent 1915(a)/(c) Authority | The MRT 1115 demonstration enrolls most populations on a mandatory basis statewide. This combined authority does not permit mandatory enrollment. |
| Concurrent 1915(b)/(c) Waivers | The MRT 1115 demonstration provides comprehensive coverage through Medicaid managed care for most populations. This combined authority manages only the HCBS permitted in the contract on a mandatory basis. |
| Section 1915(i) "Home and Community–Based Services" State Plan Option | The MRT 1115 demonstration provides comprehensive coverage for most populations. This authority is for HCBS only. |
| 1915(j) Self Directed Personal | The MRT 1115 demonstration provides |
| Assistance Services (PAS) | comprehensive coverage for most populations. This authority is not specific to operation and managed care delivery system; it is to offer consumer directed services only. |
| 1915(k) Community First Choice | The MRT 1115 demonstration provides comprehensive coverage for most populations. This authority is not specific to operating a managed care delivery system; it is to offer CFCO services. |
| 1937 Benchmark/ Benchmark– | The MRT 1115 demonstration provides nearly all |
| Equivalent Benefit Plans | NY Medicaid benefits through Medicaid managed care, expands eligibility of some populations, offers HCBS to some populations, and pending approval of the 1115 amendments submitted to CMS, will offer HCBS to additional populations in 2018. This authority is to offer more limited coverage through HMOs, equivalent to federal, state employee, or commercial enrollment. |
| Section 1945 Health Home State Plan Option | The MRT 1115 demonstration provides comprehensive coverage for most populations through Medicaid managed care. This authority is not specific to operating a managed care delivery system; it is to offer Health Home services. |
| Section 1115 Demonstrations | The MRT 1115 demonstration continues to include eligibility, benefits, quality, health care system transformation, and evaluation objectives intrinsically tied to enrollment in comprehensive Medicaid managed care for most populations. |
___________________________________________
1 *These surveys were inadvertently omitted from the previously submitted quarterly reports. 1
Follow Us