CHCANYS Conference
- Presentation is also available in Portable Document Format (PDF)
October 21, 2014
Agenda
Rate Setting Process
Statewide Rate Processing
- Statewide Rate Processing Steps:
- Analyst develops rate package
- Extraction of data
- Impact development
- Rate sheet development
- Division of the Budget letter
- Dear Administrator letter
- Statewide rate package is completed and submitted for internal department review
- Supervisor
- Chief Health Care Fiscal Analyst
- Bureau Director
- Assistant Division Director
- Division Director
- Medicaid Director
- Rates provided to Managed Care Unit for wrap rate development
- Appeal packet submitted to the Division of the Budget for review and approval
- Similar chain as the Department of Health
- When Division of the Budget approval received
- Rates prepared for loading to eMedNY system
- Transmittal document with electronic transmission of rate
- All rate codes, All locations
- Approval requested from Division office for loading of rate due to Global Cap affect
- Rate transmitted and documentation forwarded
- Overnight load process
- Electronic file run thru edits
- Edit review
- Thursday cycle processing
- Health Commerce System
- Programming developed for posting
- Dear Administrator letter
- Rate Sheet
Appeal Rate Processing
- Appeal Rate Processing Steps:
- Providers submit an appeal request to BAMCR
- Mr. Michael Ogborn
Director
Bureau of Acute and Managed Care Rate–Setting One Commerce Plaza – Room 1405
99Washington Avenue
Albany, New York 12210
- Change to be implemented
- Appeal request is reviewed for appropriateness by rate analyst
- Appeal number assigned and acknowledgement letter sent to provider
- Appeal is developed for Fee–for–Service rate:
- Fee–for–Service Rate Calculations
- Bureau Recommendation
- Appeal Medicaid Managed Care Wrap Rate developed
- Analyst calculate
- Supervisor reviewed
- Appeal packet is completed and submitted for internal department review
- Fee–for–Service Supervisor
- Chief Health Care Fiscal Analyst
- Bureau Director
- Assistant Division Director
- Division Director
- Medicaid Director
- Appeal packet submitted to the Division of the Budget for review and approval
- Similar chain as the Department of Health
- When Division of the Budget approval received
- Rate prepared for loading to eMedNY system
- Transmittal document with electronic transmission of rate
- Division office approval for loading of rate due to Global Cap affect
- Rate transmitted and documentation forwarded
- Overnight load process
- Electronic file run thru edits
- Edit review
- Thursday cycle processing
- Bureau recommendation mailed to Provider
- Recommendation letter, appeal packet and attachments, if applicable
- Hardcopy mailed – certified
Adding a Rate to eMedNY for a New Provider or New Location
- Processing Steps:
- Location rate establishment
- New Provider
- Provider submits enrollment application (refer to Contacts)
- Provider Enrollment forwards a "Rate Setter Notification" to the BAMCR contacts with eMedNY details
- Rate loaded when provider´s appeal has received Division of the Budget approval
- New location based on Certificate of Need Application
- Provider Enrollment forwards a "Rate Setter Notification" to the BAMCR contacts with eMedNY details
- Provider Enrollment contact: providerenrollment@health.ny.gov
- If a provider with FQHC locations
- Provider contacted for HRSA approval
- Copy of "Rate Setter Notification" provided to Medicaid managed care for wrap rate
- Rate Loading
- Rate prepared for loading to eMedNY system
- Transmittal document with electronic transmission of rate
- Approval requested from Division office for loading of rate due to Global Cap affect
- Rate transmitted and documentation forwarded
- Overnight load process
- Electronic file run thru edits
- Edit review
- Thursday cycle processing
Processing Order
- Processing Order:
- Prioritize
- Payment Issues
- Appeals
- Provider does not have a Medicaid rate
- Provider is converting to an FQHC rate
- Added Capital or Scope of Services
- Appeals:
By Appeal Type
| Appeal Type |
FQHC |
Non‐ FQHC |
Total |
| New Provider / Convert to FQHC |
2 |
12 |
14 |
| Added Capital / Capital Revisions |
4 |
12 |
16 |
| Scope of Services |
2 |
N/A |
2 |
| Total |
8 |
24 |
32 |
By Status
| Status |
FQHC |
Non‐ FQHC |
Total |
| Waiting Processing / Initial Review |
5 |
17 |
22 |
| At the Division of the Budget |
1 |
1 |
2 |
| Final Processing |
2 |
6 |
8 |
| Total |
8 |
24 |
32 |
Additional Processing Information
- Information to facilitate processing:
- Use email account
- Health Commerce System (HCS)
- Facilities need to have access
- Subscribe to the Department´s website (APG)
- Medicaid Provider Enrollment applications submitted
- Future consideration for appeals processing
Health Commerce System (HCS)
- Health Commerce System: https://commerce.health.state.ny.us/hcsportal/hcs_home.portal
- Communication Tool
- Secure network for posting provider information
- FQHC & APG Capital Rate Sheets, AHCF Cost Report, Indigent Care
- Keep email address current
- Facility’s responsibility
- Email blast separate from public website Electronic Mailing List
- Removal of employee when they leave your employment
- HCS Contacts
- Commerce Accounts Management Unit (CAMU): 1–866–529–1890
- HCS accounts
- Password resets
- removal of employee
- New DTC to get established on the HCS
- DTC does not have a Director or Coordinator
- General HCS inquiries: 518–473–1809
- Ask for Commerce Trainers
- BAMCR at dtcffsunit@health.ny.gov
- Receiving access to the D&TC applications 12
Contacts
- Bureau of Acute & Managed Care Rate Setting (BAMCR)
- Contacts outside of BAMCR:
- Contact Computer Sciences Corporation (CSC) at 800–343–9000
- Has my Provider Enrollment application been received?
- What is the status of my Provider Enrollment application?
- How do I submit a claim or why did my claim deny?
- Medicaid Financial Management at mfm@health.ny.gov
- Liability balance
- Payment on a liability
- Contact Provider Enrollment at providerenrollment@health.ny.gov
- Is my location established on eMedNY?
- Bureau of Vital Access Provider Reimbursement at bvapr@health.ny.gov
- Questions regarding AHCF Cost Report
- Bureau of Federal Relations and Provider Assessments at william.hogan@health.ny.gov
- Questions regarding Indigent Care
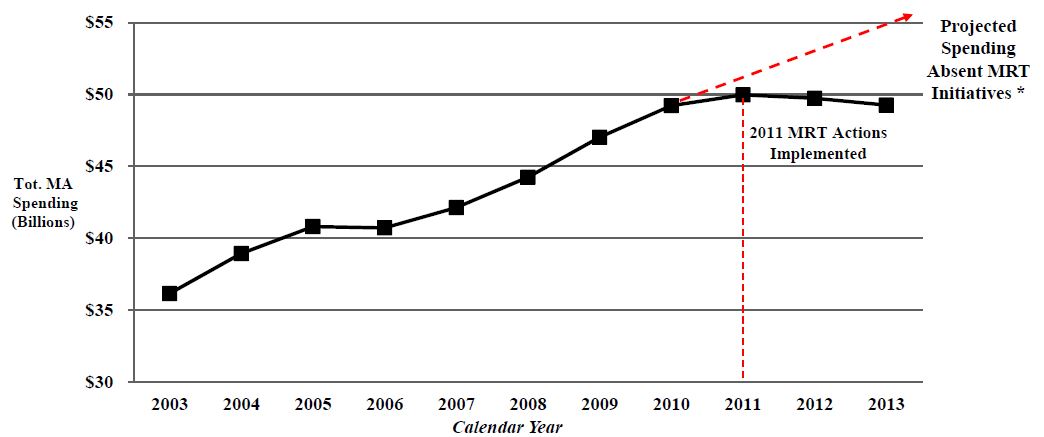
Total Medicaid Spending Over Time
State Fiscal Years 2003–13
NYS Statewide Total Medicaid Spending (CY2003–2013)
| |
2003 |
2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013 |
| # of Recipients |
4,267,573 |
4,594,667 |
4,733,617 |
4,730,167 |
4,622,782 |
4,657,242 |
4,911,408 |
5,212,444 |
5,398,722 |
5,598,237 |
5,792,568 |
| Cost per Recipient |
$8,469 |
$8,472 |
$8,620 |
$8,607 |
$9,113 |
$9,499 |
$9,574 |
$9,443 |
$9,257 |
$8,884 |
$8,504 |
*Projected Spending Absent MRT Initiatives was derived by using the average annual growth rate between 2003 and 2010 of 4.28%.
Excluded from the 2013 total Medicaid spending estimate is approximately $5 billion in "off–line spending" (DSH, etc.)
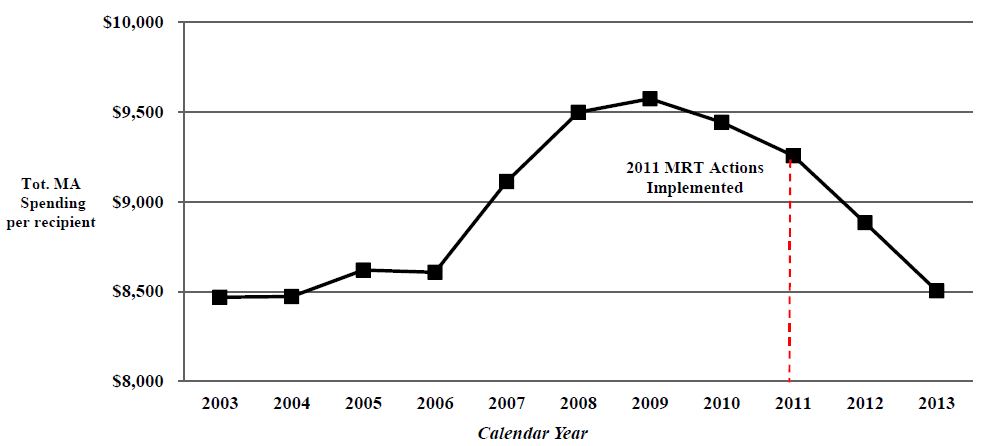
NYS Statewide Total Medicaid Spending per Recipient (CY 2003–2013)
| |
2003 |
2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013 |
| # of Recipients |
4,267,573 |
4,594,667 |
4,733,617 |
4,730,167 |
4,622,782 |
4,657,242 |
4,911,408 |
5,212,444 |
5,398,722 |
5,598,237 |
5,792,568 |
| Cost per Recipient |
$8,469 |
$8,472 |
$8,620 |
$8,607 |
$9,113 |
$9,499 |
$9,574 |
$9,443 |
$9,257 |
$8,884 |
$8,504 |
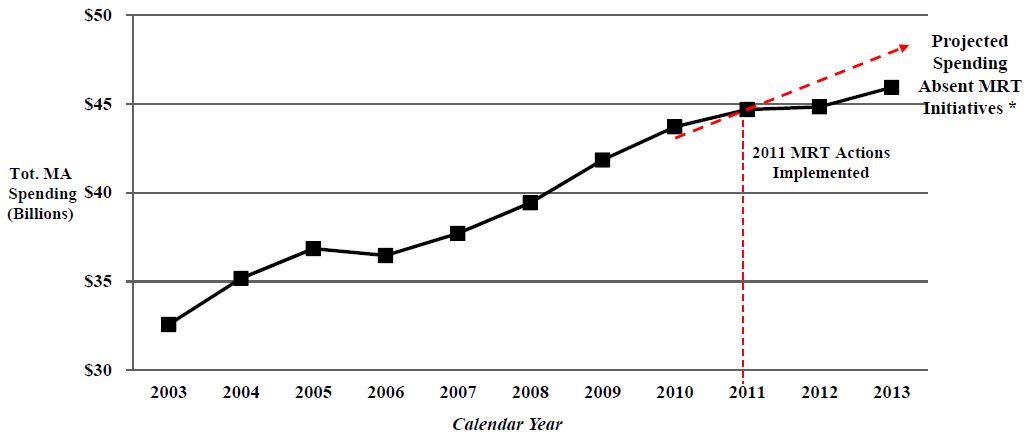
NYS Statewide Total Medicaid Spending for All Categories of Service Under the Global Spending Cap (CY 2003–2013)
| |
2003 |
2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013 |
| # of Recipients |
4,266,538 |
4,593,566 |
4,732,564 |
4,729,167 |
4,621,911 |
4,656,361 |
4,910,528 |
5,211,559 |
5,397,870 |
5,597,551 |
5,791,893 |
| Cost per Recipient |
$7,635 |
$7,657 |
$7,787 |
$7,710 |
$8,158 |
$8,467 |
$8,520 |
$8,386 |
$8,277 |
$8,008 |
$7,929 |
*Projected Spending Absent MRT Initiatives was derived by using the average annual growth rate between 2003 and 2010 of 4.28%.
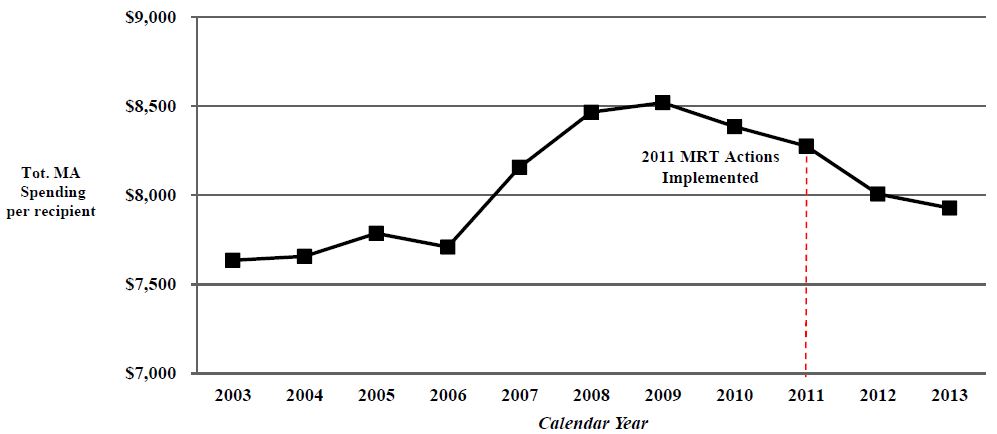
NYS Statewide Total Medicaid Spending per Recipient for All Categories of Service Under the Global Spending Cap (CY 2003–2013)
| |
2003 |
2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013 |
| # of Recipients |
4,266,538 |
4,593,566 |
4,732,564 |
4,729,167 |
4,621,911 |
4,656,361 |
4,910,528 |
5,211,559 |
5,397,870 |
5,597,551 |
5,791,893 |
| Cost per Recipient |
$7,635 |
$7,657 |
$7,787 |
$7,710 |
$8,158 |
$8,467 |
$8,520 |
$8,386 |
$8,277 |
$8,008 |
$7,929 |
*Projected Spending Absent MRT Initiatives was derived by using the average annual growth rate between 2003 and 2010 of 4.28%.
|top of section|
|top of page|
Where We Are
Current State of Medicaid
Current Status of Medicaid Global Cap
| Medicaid Spending – FY 2015 (dollars in millions) |
| Category of Service |
Estimated |
Actual |
Variance
Over /
(Under) |
|
| Medicaid Managed Care |
$1,016 |
$999 |
($17) |
- Total State Medicaid
expenditures under the
Medicaid Global Spending
Cap for FY 2015 through April
are $7 million or 0.5 percent
under projections. Spending
for FY 2015 resulted in total
expenditures of $1.38 billion
compared to the projection
of $1.39 billion.
|
| Mainstream Managed Care |
$750 |
$732 |
($18) |
| Long Term Managed Care |
$266 |
$267 |
$1 |
| Family Health Plus |
$59 |
$62 |
$3 |
| Total Fee For Service |
$686 |
$677 |
($9) |
| Inpatient |
$278 |
$276 |
($2) |
| Outpatient/Emergency Room |
$36 |
$43 |
$7 |
| Clinic |
$56 |
$60 |
$4 |
| Nursing Homes |
$320 |
$307 |
($13) |
| Other Long Term Care |
$73 |
$71 |
($2) |
| Non‐Institutional |
($77) |
($80) |
($3) |
| Medicaid Administration Costs |
$38 |
$33 |
($5) |
| OHIP Budget / State Operations |
$18 |
$7 |
($11) |
| Medicaid Audits |
($35) |
($32) |
$4 |
| All Other |
$315 |
$344 |
$29 |
| Local Funding Offset |
($709) |
($709) |
$0 |
| TOTAL |
$1,388 |
$1,381 |
($7) |
Global Cap Risk Factors
- ACA enrollment – We are now serving more people than ever before: 6,269,841 (for Calendar Year 2013).
- $300 million contribution to the financial plan (tax cut) and $445 million transfer to the Mental Hygiene Stabilization Fund.
- Full implementation of Wage Parity in NYC for SFY14–15 is $420 million. The distribution is as follows:
- MLTC Risk Rates – $225M; MLTC Mandatory Rates – $75M; Fee–For–Service – $50M; Quality Incentive Vital Access Provider Pool (QIVAPP) – $70M
- Complex year with lots of "puts and takes." Need to monitor very closely.
VAP/Safety Net Program
- 2014–15 Enacted Budget includes $194 million in VAP funding of which $30 million continues to be set aside for Financially Disadvantage Nursing Homes.
- Over 180 applications, with a total estimated request of $1.2 billion (excluding capital), have been received to date.
| (dollars in millions) |
2013‐14 |
2014‐15 |
| Total Funding Available |
$182 |
$194 |
| VAP Awards (committed in 2013‐14) |
$156 |
$62 |
| VAP Awards (to be committed in 2014‐15) |
N/A |
$83 |
| Remaining Funding Available |
$26 |
$49 |
| Move 13/14 into 14/15 |
($26) |
$26 |
| Available Funds |
$0 |
$75 |
- Available Funds are to be used to support providers as they transition to DSRIP or those providers that do not qualify for DSRIP.
|top of section|
|top of page|
Big Reforms Ahead:
Agenda for the Next Six Months
- Nursing Home benefit being carved into managed care: January 2015
- FIDA – Fully Integrated Duals Advantage Program:
- NYC/Nassau County: Voluntary enrollment begins on January 1, 2015 with passive in April 2015.
- Westchester/Suffolk Counties: Voluntary enrollment begins April 1,2015 with passive in July 2015.
- HARP/Behavioral Health Carve–In
- April 1, 2015 – BH Adults transition in NYC
- October 1, 2015 – BH Adults transition Rest of State
- April 1, 2016 – BH Children transition Statewide
|top of section|
|top of page|
MRT Waiver Amendment
On April 14, 2014 Governor Andrew M. Cuomo announced that New York finalized agreement with the Federal government for a groundbreaking waiver that will allow the State to reinvest $8 billion in Federal savings generated by Medicaid Redesign Team (MRT) reforms.
- Allows the state to reinvest $8 billion of the $17.1 billion in federal savings generated by MRT reforms.
- Funds will address critical issues throughout the State and allow for comprehensive reform through a Delivery System Reform Incentive Payment (DSRIP) program. The program will:
- Focus on system reform, specifically a goal to achieve a 25 percent reduction in avoidable hospital use over five years.
- Payments are based on performance and outcome milestones.
- Require providers to collaborate to implement innovative projects focusing on system transformation, clinical improvement and population health improvement.
MRT Waiver Allocation Plan
The $8 billion reinvestment will be allocated in the following ways:
- $500 Million for the Interim Access Assurance Fund (IAAF) – Time limited funding to ensure current trusted and viable Medicaid safety net providers can fully participate in the DSRIP transformation without unproductive disruption.
- $6.42 Billion for Delivery System Reform Incentive Payments (DSRIP) – Including DSRIP Planning Grants, DSRIP Provider Incentive Payments, and DSRIP Administrative costs and DSRIP related Workforce Transformation.
- $1.08 Billion for other Medicaid Redesign Purposes – This funding will support Health Home development, and investments in long term care workforce and enhanced behavioral health services, (1915i services).
Value Based Payments
Per Special Terms & Conditions §39, all contracted MCOs must employ non–fee–for–service payment systems that reward value over volume for at least 90% of all their provider payments by Waiver Year 5
- The goals of Value Based Payment Reform is to:
- Create integrated delivery systems that are more accountable for quality of care provided and make providers assume greater financial risk;
- Increase the linkage between quality and cost; and
- Ensure service delivery focuses on high–quality care at a lower cost in a coordinated full continuum of care within emerging Performing Provider Systems (PPS)
|top of section|
|top of page|
Questions?
|top of page|