NEW YORK STATE MONEY FOLLOWS THE PERSON REBALANCING DEMONSTRATION
- Plan is also available in Portable Document Format (PDF, 801KB)

SUSTAINABILITY PLAN
Presented: April 2015
Revised: October 2017

Money Follows the Person (MFP) Rebalancing Demonstration
URL: www.health.ny.gov/health_care/medicaid/redesign/nys_money_follows_person_demonstration.htm
Email: MFP@health.ny.gov
Phone: (518) 486–6562
Table of Contents
- Executive Summary
- Stakeholder Involvement
- Population Rebalancing
- Home and Community Based Services
- Administrative Staffing
- Fund Utilization
- Projected Timeline
- Estimated Budget Summary
1. Executive Summary
Purpose and Contents
The New York State Money Follows the Person Rebalancing Demonstration (Demonstration) – Sustainability Plan, as developed by the New York State Department of Health (DOH) in cooperation with the New York State Office for People With Developmental Disabilities (OPWDD), is designed to serve as a dynamic strategic framework for the continuation of rebalancing services to members of vulnerable populations. Topics discussed within this Sustainability Plan include:
- Executive Summary
- Stakeholder Involvement
- Population Rebalancing
- Demonstration Services
- Administrative Staffing
- Fund Utilization
- Projected Timeline
- Estimated Budget Summary
- Strategic Map
National Background
The Money Follows the Person (MFP) Rebalancing Demonstration grant, established and awarded by the Centers for Medicare and Medicaid Services (CMS), is designed to stimulate a rebalancing of Medicaid long–term care systems at the state level. Currently, forty–four states and the District of Columbia participate in the national initiative.
On the national level, between 2008 through the end of 2016, more than 75, 000 people with chronic conditions and disabilities have transitioned from institutions back into community settings through these various MFP programs.
New York State MFP Mission Statement
Approved by the Centers for Medicare and Medicaid Services (CMS) in 2007 and operating under the auspices of the New York State DOH, the New York State MFP Rebalancing Demonstration is the focal point for rebalancing long–term care in New York State, especially in Medicaid and for vulnerable populations. The Demonstration promotes an ongoing collaborative approach towards driving a substantive consumer–driven rebalancing of the Empire State’s long–term care systems.
Since its inception, the New York State MFP Demonstration is proud to have successfully transitioned more than 2600 individuals with chronic conditions and disabilities from traditional – and often more costly – institutional settings back into the community.
The Demonstration’s current partnerships with constituent programs assure that members of vulnerable populations (e.g., seniors; individuals with physical, intellectual, and/or developmental disabilities; and individuals with traumatic brain injury) have access to home and community–based services (HCBS). New York State continues to articulate a long–term care agenda designed to restructure healthcare priorities by shifting the focus from institutional care to a patient–centered system of quality homecare via a number of mechanisms. This includes the New York State Nursing Home Transition and Diversion (NHTD) and Traumatic Brain Injury (TBI) waivers, the New York State OPWDD waiver, and through the Managed Care and Managed Long–Term Care programs.
OPWDD, as part of its Transformation Agreement with CMS, is participating in the New York State MFP Demonstration within this larger context of de–institutionalization. It is expected that OPWDD’s participation in MFP will continue to support transitions of individuals who will be leaving the limited number of campus–based opportunities that OPWDD will continue to operate, skilled nursing facilities, or individuals who are aging out of specialized Children’s Residential Programs.
After Demonstration participants have received 365 days of qualified home and community–based services during the transition period, they will continue to receive services through any of the waivers mentioned above, or through Managed Care/Managed Long–Term Care, as long as they continue to meet all of the eligibility requirements of the plan/waiver in which they are enrolled.
Project Initiatives
The New York Association of Independent Living and Open Doors
New York State currently contracts with The New York Association of Independent Living (NYAIL) to administer transition efforts through the Open Doors program. The purpose of this program is to identify potential participants in nursing facilities, educate them on their return–to–community options and facilitate successful transitions to their community of choice.
Twenty–Four Regional Transition Centers (9 Regional Lead and 15 Auxiliary Independent Living Centers) have been established to identify and assist individuals from vulnerable populations who express a desire to leave an institutional setting and return to the community. To supplement the formal process of identifying individuals who express a desire to leave institutional settings, NYAIL has also established a Peer Outreach and Referral program to assist in identifying individuals who express a desire to leave institutional settings and to provide peer support to these individuals through the transition process.
Additional funding was added this year to support these complementary Open Doors programs. These programs have expanded their ability to reach–out to the frail elderly, and physically and/or intellectually disabled individuals in New York State nursing homes, as well as Veterans, the elderly with mental health challenges, and New Yorkers residing in out–of–state (OOS) nursing facilities. This expanded funding level is expected to continue throughout the demonstration period and beyond.
New York State plans to continue its contract with NYAIL to operate Open Doors through the contract term ending in 2019. The state plans a competitive re–procurement for the Transition Center and Peer Outreach and Referral projects using Medicaid administrative funds to sustain these successful transition programs beyond the end of the MFP demonstration.
Marketing
Many individuals and caregivers are unaware of the long–term services and supports available to them in their homes and communities especially those supports that can help them avoid institutionalization.
Raising awareness of the MFP program has been important for outreaching to individuals who may qualify for supports to transition back into their homes and communities.
New York State has used a variety of marketing strategies to promote MFP/Open Doors to increase recruitment and enrollment, and ultimately transitions, including: a public website, promotional toolkit for Transition Center and Peer Program staff, radio and local cable television advertising campaign, outreach videos, and ongoing outreach to nursing homes, ombudsman, and managed long–term care managers.
Quality of Life Survey
The Quality of Life Survey is an essential part of an evaluation of the MFP Program and provides valuable information on quality of life satisfaction. The survey was instituted in 2007 as part of the national evaluation of the Demonstration by Mathematica Policy Research (Mathematica). The survey was modified within New York State to better align with plans for continued use following the end of the national evaluation. The revisions made extensive use of Mathematica’s annual evaluation reports to retain questions with statistical significance. The modified QoL was implemented in January 2017 and will continue beyond the end of the grant period.
Section Q Outreach Education
Data has demonstrated that nursing facilities are the favored referral source to result in successful transitions to community living. At the same time, data indicates that nursing facilities are not in compliance with MDS Section Q requirements to administer Section Q during each MDS assessment (unless the resident has requested the question not be asked on quarterly assessments). This lack of compliance results in missed opportunities for potential transition screening by the Local Contact Agency (NYAIL) for those residents who answer ‘yes’ to the community question.
The need for education on this topic was addressed through a Public Health Live Webcast which took place on 2/16/17. (Public Health Live is a monthly webcast series providing continuing education opportunities on public health issues. Webcasts are free and available to all who are interested.) Curriculum for the forum focused on MFP, rebalancing, and MDS Section Q, and presenters represented both local and national perspectives. In addition, MFP staff is working closely with New York State DOH’s Division of Nursing Homes and Intermediate Care Facilities/IID to provide education regarding Section Q referral to the State’s Nursing Home Provider Associations and approved providers of MDS training in the State. Other Section Q education efforts include the creation of a dedicated outreach and education team within the Open Doors program to coordinate and focus outreach to nursing facilities and managed care plans.
Managed Care and Managed Long–Term Care
Contributing to the increase in Transition Center and Peer support referrals, is the approval, obtained in January 2016, retroactive to July 1, 2015, to include managed care participants as MFP constituents.
Both Demonstration and NYAIL staff have invested in facilitating multi–faceted collaboration with managed care and managed long–term care plans to identify and assist their members. This has involved the development of relationships, policy, and reporting at the State level, as well as outreach presentations, information sharing, and other efforts to facilitate direct collaboration between Open Doors and the plans. The number of MFP participants receiving their health care services through a managed care or managed long–term care plan is steadily increasing. The Demonstration is committed to supporting this continued growth throughout the demonstration period and beyond.
Geriatric Mental Health
In anticipation of the expected continuing rise in the need for behavioral health services for adults 65 years or older, the Open Doors program has begun working with community behavioral health resources in order to address this trend. Transition Specialists collaborate with the New York State Office of Mental Health’s (OMH) Single Point of Access to facilitate transitions from nursing facilities involving individuals with mental health needs throughout New York State, and expedites linkages to Health and Recovery Plans (HARP), a managed care product that manages behavioral health needs. In addition, NYAIL is working with the Mental Health Association of New York to provide training and education for Transition Specialists and peers in their work with individuals with mental health needs. At the State level, MFP staff are collaborating both internally and with OMH around HARP and PASRR (Pre–Admission Screening and Resident Review). MFP has been identified as a referral target for nursing facility residents with mental health needs for whom a Level II PASRR has recommended community placement. Resources will continue to be directed to building a sustainable platform of Transition Specialist training and ongoing collaboration with partners in the behavioral health service system.
Veterans
The New York State Division of Veterans´ Affairs (DVA) is the lead advocate for Veterans regarding medical, social, and economic matters impacting Veterans and seeks to educate others to the special skills and needs of Veterans. In addition, DVA assists New York State Veterans who may be eligible for services and benefits based on their military service and disability and age status.
As the need for such services mount and the age of Veterans continues to climb, the New York State MFP Demonstration has engaged in a collaborative relationship with the DVA to address transition needs of veterans currently living in nursing facilities. Cross–training of staff has occurred, and cross– referrals are actively pursued through ongoing collaboration between Veterans Benefit Advisors and Transition Specialists. In addition, the Open Doors Peer Outreach and Referral program is actively recruiting veteran peers to match on Veteran’s status; an effective strategy for engaging Veterans who may be interested in community living.
New York State Office for the Aging
New York State DOH has partnered with the New York State Office for the Aging (SOFA) to facilitate increased access to information about available long–term services and supports through a No–Wrong Door model. The State Office for the Aging expanded its NY Connects program (New York’s Aging and Disability Resource Centers) to include all populations needing long–term services and supports.
Transition Center staff use SOFA’s local NY Connects programs (New York’s Aging and Disability Resource Center’s) to help identify available resources in the community. MFP staff at the State level serve as the liaison between New York State DOH and New York State OFA to support the ongoing development and improved usability of the NY Connects network, and to support continued collaboration at the local level.
Office for People With Developmental Disabilities
OPWDD administers a HCBS 1915(c) waiver through which it provides a wide range of home and community–based supports and services. These supports are provided to individuals through an extensive network of not–for–profit providers and some State–provided services. OPWDD participates in the New York State MFP Demonstration within the larger context of de–institutionalization. OPWDD’s participation in MFP is expected to support continued transitions of individuals who will be leaving the limited number of campus–based intermediate care facilities which continue to be operated by OPWDD, as well as those elderly individuals residing in skilled nursing facilities. Transition efforts for this population will continue post–Demonstration.
Repatriation
Open Doors has begun to outreach to Out–of–State (OOS) nursing facilities and work with partners from the Regional Resource Development Centers (on behalf of New York State’s waiver programs) and New York State’s managed care and managed long–term care plans to facilitate transitions to participants’ communities of choice within New York State. In addition, MFP is aligning with other DOH and Statewide initiatives in an effort to successfully repatriate New York State residents whose placements in OOS nursing facilities is supported by Medicaid. Special expertise is needed to address the unique and increased challenges and barriers faced by New York State residents in OOS nursing facilities when attempting to transition to their home communities. For this reason, MFP is planning to support two assessor positions, a Nurse Evaluator and a Behavioral Specialist, to facilitate needs assessment and care planning for this difficult–to–transition population. These are intended to be contract positions within the Department, initially supported by MFP rebalancing funds and later transitioning to Medicaid administrative funding, as they demonstrate effectiveness.
TRAID
To promote a long–term care system in which individuals at risk of institutional placement or those individuals interested in transitioning from institutional settings have access to needed durable medical equipment and assistive technology, the Demonstration has partnered with the New York State Justice Center to provide additional funding for the Technology–Related Assistance for Individuals with Disabilities (TRAID) Project. TRAID serves to increase well–timed access to and acquisition of assistive technologies (AT), such as durable medical equipment (DME), in support of individuals wishing to remain in or transition to a community setting. A significant barrier traditionally facing these individuals is the delay in receiving AT via typical funding mechanisms such as through State Plan services, HCBS waivers or non–Medicaid services. Currently supported by MFP rebalancing funds, New York State plans to continue its current level of funding for the TRAID project beyond the close of the MFP Demonstration through Medicaid administrative funds.
Lifespan–Community Care Connections
To better support a common goal of helping older adults remain healthy within their own homes, Lifespan of Greater Rochester’s Community Care Connections demonstration initiative integrates a community–based aging services provider into the health care delivery through collaboration with service providers focusing on primary and secondary prevention. The initiative strives to reduce hospital admissions/readmissions and emergency department use, and to reduce caregiver burden.
The Lifespan Demonstration is scheduled for the period of 2015–2018 and will produce a comprehensive evaluation report with recommendations for the development of a model plan for successful replication throughout New York State.
Person–Centered Planning Comprehensive Training Initiative
Enhancing person–centered practice and planning, i.e., an individualized approach to supporting the frail elderly and individuals with disabling conditions, is an important priority for New York State.
Rebalancing efforts rely on participant choice to guide the shift towards Home and Community Based services. In addition, person–centered planning aligns with an increasing number of regulatory requirements, such as the Home and Community–Based Services Final Rule. This initiative is in the development phase of a planned 3–year project, and is expected to produce resource materials, curriculum, and procedures that will be sustainable beyond the project’s end–date to support the efforts of the Transition Centers to interface with a person–centered health care service system.
Caregiver Guide
The Caregiver Guide has been developed by the New York State DOH to serve as a practical handbook for all caregivers in New York State, particularly seniors 65+ and their caregivers. The guide is intended to support caregivers of individuals needing long–term services and support in their communities. The content has been completed and the guide is currently in the publication design phase of development. Initial plans for distribution include a print run of 2000 copies as a pilot test of the guide. Following feedback from the pilot copies, plans for a larger print run and distribution will be finalized.
MFP Organizational Enhancements
The Demonstration has been working to enhance its organizational structure in an effort to provide greater flexibility and responsiveness to our partners in support of both current and upcoming initiatives. At the core of this organizational change is the concerted effort to recruit and retain talented staff to the Demonstration. Additional Full Time Equivalents (FTEs) were added to the organization during the grant period to support the growth and development of the overall rebalancing infrastructure. In order to support sustainability, it is essential to convert contractor positions, which are temporary in nature, to permanent State FTEs in order to maintain the operation of rebalancing activities.
|top of section 1.| |top of page|2. Stakeholder Involvement
History of Outreach
Since its inception, the Demonstration has routinely hosted or actively participated in an array of outreach, marketing, and educational activities during the pre–implementation and implementation phases. Such activities have included but have not been limited to presentations to nursing home discharge planners, managed care organizations, and community–based providers; organizing and conducting intra– and inter–agency meetings and statewide conferences; and reaching out to potential constituents. In addition, the Demonstration routinely communicates with Local Departments of Social Services and the State’s Medicaid Redesign Team.
As the Demonstration shifts its focus from serving as a catalyst for transitional pilot initiatives towards being a champion for long–term sustainability, the significance of maintaining effective communications with stakeholders is now more important than ever. In an effort to drive and maintain a high level of communications with its stakeholders, the Demonstration formed the MFP Stakeholder Advisory Committee (Committee). Comprised of representatives ranging from individuals, families, and service provider associations, the Committee meets on a regular basis and fosters knowledgeable guidance and dialogue regarding the development and sustainable utilization of rebalancing initiatives.
Stakeholder Summary
Committee members were identified and recruited to ensure fair representation across constituent groups. Members were identified by MFP constituent programs, MFP contractors, and other community partners. Stakeholder feedback and involvement is solicited at quarterly meetings as well as on an ongoing basis through direct communication between stakeholders and MFP staff. As the Waiver Transition to managed care progresses, specific feedback is solicited, and updated information is provided on an ongoing basis as warranted.
The following is a current list of participating stakeholders; however, the Committee meeting is conducted in an open format which allows for enhancement through inclusion of new stakeholders and the public at any point.
| Stakeholder Groups | |
|---|---|
|
|
|
|
|
|
|
|
|
|
Sustainability Process
Representatives of the Committee were called upon to actively engage in the development of the Demonstration’s Sustainability Plan at several points in the process. The planning process has been a major topic at quarterly meetings where beneficial feedback has been received from stakeholders to guide efforts and address identified problems/areas of need. Much of the discussion at the June 2014 meeting involved generating ideas for sustainability. At the meeting in March 2015, Committee members were given an overview of the timetable for submission of the Plan to CMS, highlighting the importance of creating a workable plan to ensure continued MFP funding, and were updated on the current status of ensuring that the various demonstrations remain viable after MFP funds run out in 2020.
Very few dissenting or conflicting opinions were noted regarding sustainability planning itself. Discussions that generated differing viewpoints generally pertained to whether or not specific issues of concern could or should be addressed by MFP within the scope of the Demonstration’s activities, or whether the issues were best addressed through other entities or channels. In those cases, MFP staff have ensured that the concerns were communicated to the appropriate people in order to have these issues moved onto other and often more appropriate programmatic agendas. MFP staff have also encouraged stakeholders to consider how best to frame issues in ways that make them uniquely eligible for MFP consideration.
Takeaways
Stakeholders have identified several areas of need in the community which require urgent attention and enhancement. Three issues in particular: (1) transportation for people with disabilities, (2) affordable and accessible housing, and (3) employment for people with disabilities are at the top of the list of barriers both to people transitioning back to the community from institutions, and for people fully integrating into their communities once there. Since the scope of these issues is vast and not necessarily unique to MFP populations, the Demonstration is considering ways to partner with other entities to address the particular issues that are within the scope of MFP, while also communicating these constituent concerns to other entities that may be able to address the problems from other angles.
Transportation
A lack of accessible, affordable, and reliable transportation is a major barrier for people with disabilities– both those transitioning out of institutions, and those already living independently in the community.
The New York State DOH is represented on both the Most Integrated Setting Coordinating Council (MISCC) and the Olmstead Cabinet which have focused attention on these transportation issues. As part of the Olmstead Plan, the Governor proposed a study of transportation issues for persons with disabilities. This study was completed and presented to the MISCC on May 11, 2017. Recommendations from this study addressed the need for a more coordinated transportation infrastructure, and a focus on broader mobility management strategies. MFP will continue to follow the MISCC’s discussions/decisions as they grapple with the issues and recommendations in this area.
Housing
Stakeholders have identified a lack of affordable, safe, and accessible housing as a barrier to transitioning into the community. These concerns have been heard throughout the State, and the Medicaid Redesign team, in conjunction with the Bureau of Housing and Partnership for Long–Term Care, are taking action by providing many more Supported Housing opportunities for our target populations, as well as allocating funds for modifications to existing apartments/houses to increase the number of accessible units available to people with disabilities.
Among these opportunities provided by the Medicaid Redesign team is a pilot initiative that launched in August of 2016. This initiative, known as the Olmstead Housing Subsidy (OHS), is designed to help address the needs of participants in transitioning from nursing home settings or preventing reinstitutionalization. MFP participants are uniquely targeted to benefit from this initiative as OHS eligibility criteria was designed to closely approximate MFP eligibility. These criteria include requirements for Medicaid enrollment, nursing home level of care needs, homeless or unstably housed, at least one hundred and twenty (120) consecutive days in a nursing home over the most recent two– year period, and the ability to live safely in the community. The initiative provides for a housing subsidy, staffing of ‘housing coordinators’ to develop housing options, and funding for "community transition services” including security deposits, moving expenses, utility payments and household establishment purchases. The Olmstead Housing subsidy is currently funded by the State as a Medicaid Redesign initiative. The potential for supplementing the initiative with MFP rebalancing funds may be explored as a period of planning around the sustainability of the housing pilot is approaching.
MFP has also worked in conjunction with OPWDD to provide training for Certified Housing Specialists across the State. This training, took place in June 2015 and provided the opportunity for individuals to become certified in Homeownership Counseling, and provided sustainable expertise in navigating local housing markets and locating affordable, accessible housing for people with disabilities.
Employment
Another main concern raised by stakeholders is the availability and accessibility of employment for individuals with disabilities. MFP staff have advocated to ensure that the importance of addressing this problem has been conveyed to the Olmstead Committee, and the Most Integrated Settings Coordinating Council (MISCC), the New York State Department of Labor, and others. This issue is currently being addressed primarily in the form of education and support to employers and employees alike. The MISCC is also participating in OMH’s Employment First Commission. MFP, through Open Doors and the OPWDD partnership, continues to ensure that employment services are made available to MFP I/DD participants as needed.
OPWDD has a number of initiatives underway to increase opportunities for people with intellectual and developmental disabilities. Pathway to Employment assists individuals in creating a career plan appropriate with their skills and interests. The redesign of Supported Employment will include an increase in the reimbursement rate for providers as incentive to provide enhanced job development and coaching. A new Community Prevocational service will provide services to individuals who need long– term job readiness services. OPWDD is investing a larger number of resources to build the capacity of providers to offer employment services by training supervisors, job developers and job coaches.
As more people with disabilities enter the workforce and begin looking for employment, it is important that business owners and/or operators understand the benefits of hiring employees of all abilities. EmployAbility: A Toolkit for Employers is a handbook that provides information for employers to begin employing people of all abilities, including financial and tax incentives, how and why hiring people of all abilities would be good for their business and where to find qualified employees.
|top of section 2.| |top of page|3. Population Rebalancing
Service Model
MFP is a state–operated, federal Demonstration that partners with constituent programs providing support for home and community–based living. The CMS Federal MFP Demonstration reimburses the State when individuals move from long–term, institutional placements to integrated settings such as individual homes and apartments in the community. Participation in the Demonstration is transparent to all individuals who express a desire to leave an institutional setting and receive a combination of home and community–based services and Medicaid State Plan services through any of the currently– partnered constituent programs (NHTD, TBI, and OPWDD 1915(c) Waivers, and MC/MLTC).
Projections
The chart below represents the actual and currently projected number (in bold) of eligible individuals in each target group to be assisted in transitioning from an institutional setting to a qualified residence during each year of the Demonstration. Participants will transition from institutional care (nursing home, hospital, or ICF–IID) to community–based care through enrollment in a constituent program (NHTD, TBI, MC/MLTC, or OPWDD). In partnership with the Demonstration, the State serves older adults, and individuals of all ages with physical, intellectual and/or developmental disabilities, who are receiving Medicaid benefits for inpatient services and have resided in a qualified institution (nursing facility, hospital, or ICF/IID) for a least ninety (90) consecutive days, excluding Medicare covered rehabilitative care that is expected to be short term in nature.
| Participant Classification | CY 2009 | CY 2010 | CY 2011 | CY 2012 | CY 2013 | CY 2014 | CY 2015 | CY 2016 | CY 2017 | CY 2018 |
|---|---|---|---|---|---|---|---|---|---|---|
| People with Physical Disabilities (PD) | 47 | 59 | 96 | 137 | 92 | 69 | 41 | 117 | 116 | 54 |
| Seniors | 32 | 46 | 72 | 102 | 91 | 65 | 61 | 128 | 135 | 43 |
| Other (TBI/Dually Diagnosed) | 8 | 60 | 72 | 103 | 102 | 85 | 73 | 85 | 104 | 46 |
| People with Developmental Disabilities (DD) | 0 | 0 | 0 | 0 | 89 | 140 | 150 | 93 | 75 | 100 |
Post–MFP
Participation in the Demonstration begins the day the individual successfully transitions to the community and starts receiving services through the respective constituent program´s provider. The first 365 days of service utilization through the constituent program constitutes the participant´s ´Demonstration period´. At any point in time, all individuals currently in the 365–day Demonstration period are considered ´active´. Any individual that has completed the 365–day period is considered inactive for the Demonstration; but may continue to receive services through the constituent program.
Demonstration participants will continue participation in the respective constituent programs´ services or receive services through the State´s Managed Care and Managed Long–Term Care model. As such, the State will therefore continue its efforts to transition individuals from institutional settings to community–based settings via Managed Long–Term Care or other programs following the conclusion of the Demonstration. New York State plans to continue this transition work with the assistance of the Transition Center and Peer Outreach and Referral Programs will continue to track and report on these transition efforts to MFP stakeholders.
|top of section 3.| |top of page|4. Home and Community Based Services
Background
New York State continues to articulate a long–term care agenda designed to restructure healthcare priorities by shifting the focus from institutional care to a patient–centered system of quality home and community–based services. These services are delivered via a number of mechanisms, including the New York State DOH Nursing Home Transition and Diversion (NHTD) and Traumatic Brain Injury (TBI) waivers, the New York State OPWDD waiver, and through the Managed Care and Managed Long–Term Care programs. Managed Long–Term Care is a program that provides care management and streamlines the delivery of long–term services to people who are chronically ill or disabled and who wish to reside in their homes and communities rather than in institutional settings. MFP participants are increasingly enrolled in Managed Long–Term Care plans as New York State continues the transition of its long–term care system to one that ensures care management for all.
The following home and community–based services will continue to operate, through the constituent programs identified above, within New York State´s long–term care health care system as the transition to managed care in New York State progresses. The 1915(c) waiver services that are not yet available under the 1115 authority will become available through managed care plans when the waiver programs transition into managed care. Leading up to, and beyond, the transfer of authorities, MFP will continue to facilitate community transitions in the same manner as currently occurs.
Service Listing
| MFP Qualified Service | Service Description | Constituent Program | Target Population | Status |
|---|---|---|---|---|
| Adult Day Health Care | The provision of medically supervised services to individuals with physical or mental impairment who need health maintenance and restorative services to enhance their ability to remain in the community. | STATE PLAN SERVICES (FFS) | All | Retain |
| Assistive Technology | Equipment that will improve the participant´s independence, decrease reliance on staff, and will be a cost–effective aid for community integration. This waiver service supplements State Plan Provided Durable Medical Equipment. | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain |
| Assistive Technology – Adaptive Devices* | Assistive technology provides devices, aids, controls, and appliances to enhance independence. | OPWDD HCBS WAIVER | ID/DD | Retain |
| CHHA services | Certified Home Health Agencies (CHHAs) provide part–time, intermittent health care and support services to individuals who need intermediate and skilled health care. CHHAs can also provide long– term nursing and home health aide services, can help patients determine the level of services they need, and can either provide or arrange for other services including physical, occupational, and speech therapy, medical supplies and equipment, and social worker and nutrition services. | STATE PLAN SERVICES (FFS) | All | Retain |
| Community Habilitation Agency Managed Self–Directed | Habilitation supports, and services provided to individuals that occur largely in the community and promote independence and community integration. An individual may choose to self–direct Community Habilitation Services. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Community Integration Counseling | Assistance to help the waiver participant cope with altered abilities and skills, revision of long–term expectations, and/or changes in their roles in relation to significant others. | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain in Waiver; Include in Managed Care |
| Community Transition Services | A service that provides non–recurring set–up expenses for individuals who are transitioning from an institutional or other provider–operated living arrangement to a living arrangement in a private residence in the community where the person is directly responsible for his or her own living expenses. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Community Transitional Services | Assistance in transition from a nursing home back to the community: including the cost of moving, essential furnishings, deposits for utilities, security deposits or health and safety assurances, such as pest eradication, allergen control or one– time cleaning prior to occupancy. | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain in Waiver; Include in Managed Care |
| Congregate and Home Delivered Meals | Meals for waiver participants who cannot prepare or obtain nutritionally adequate meals for themselves, or when the provision of such meals will decrease the need for more costly supports to provide in–home meal preparation. | NHTD WAIVER | Elderly, PD | Retain |
| Consumer Directed Personal Assistance Services | The Consumer Directed Personal Assistance Program is a self– directed model for nursing, home health, and personal care services. This Medicaid program provides services to chronically ill or physically disabled individuals who have a medical need for help with activities of daily living (ADLs) or skilled nursing services. Services can include any of the services provided by a personal care aide (home attendant), home health aide, or nurse. Recipients have flexibility and freedom in choosing their caregivers and the consumer or the person acting on the consumer´s behalf (e.g. the parent of a disabled or chronically ill child) assumes full responsibility for hiring, training, supervising, and – if need be – terminating the employment of persons providing the services. | STATE PLAN SERVICES (FFS) | All | Retain |
| Day Habilitation* Group Supplemental Individual | Habilitation services that assist with acquisition, retention or improvement in self–help, socialization and adaptive skills including communication, travel and adult education that regularly takes place in a non–residential setting. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Durable Medical Equipment (DME) | Durable medical equipment are devices and equipment, other than prosthetic or orthotic appliances, which have been ordered by a practitioner in the treatment of a specific medical condition and which have all the following characteristics: can withstand repeated use for a protracted period of time; are primarily and customarily used for medical purposes; are generally not useful in the absence of an illness or injury; are not usually fitted, designed or fashioned for a particular individual´s use; and where equipment is intended for use by only one patient, it may be either custom–made or customized. | STATE PLAN SERVICES (FFS) | All | Retain |
| Environmental Modifications (Home Accessibility) * | Environmental modifications are physical adaptations to a person´s home that are necessary to ensure the health, welfare and safety of the participant or that enable the participant to function with greater independence. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Environmental Modifications Services | Internal and external physical adaptations to the home necessary to enable the person to function with greater independence, to assure health and welfare, and/or to prevent institutionalization | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain in Waiver; Include in Managed Care |
| Family Care Residential Habilitation* | Living arrangement which places an individual with a family. Individualized habilitation services and supports assist with the acquisition, retention or improvement in skills related to living in the community | OPWDD HCBS WAIVER | ID/DD | Retain |
| Family Education and Training* | Educational programs for parents, siblings, and other relatives designed to enhance a family´s capacity to care and support a family member with a developmental disability living at home. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Fiscal Intermediary* | The Fiscal Intermediary supports the self–directing individual with billing and payment of approved goods and services, fiscal accounting and reporting, ensuring Medicaid and corporate compliance, and general administrative supports. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Home and Community Support Services | Assistance and/or supervision with activities of daily living as well as supervision and oversight. | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain in Waiver; Include in Managed Care |
| Home Visits by Medical Personnel | Needed medical care and evaluation of the participant´s environment and the capacity of natural supports to support the participant. This service is provided by a physician, nurse practitioner or physician´s assistant to waiver participants who are unable to leave their home. | NHTD WAIVER | Elderly, PD | Retain in Waiver; Include in Managed Care |
| Independent Living Skills Training | Training to improve or maintain the waiver participant´s ability to live as independently as possible by focusing on essential community living skills such as task completion, including Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs). | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain in Waiver; Include in Managed Care |
| Individual Directed Goods and Services* | Services, equipment and supplies not otherwise provided through HCBS Waiver or Medicaid State Plan services that addresses an identified need in an individual´s service plan. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Intensive Behavioral Service | Short–term, outcome–oriented services focused on developing effective behavioral management strategies to ensure health and safety and/or improve quality of life. Services are available in the person´s home and are designed to achieve community stabilization and avoid the individual´s placement in a more restrictive living environment due to challenging behavior episodes. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Live–in Caregiver *(42CFR §441.303(f)(8)) | An unrelated care provider who resides in the same household as the waiver participant and provides supports as needed. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Medicaid Service Coordination (MSC) Basic, Willowbrook, Transition–Basic, Transition– Willowbrook | Service coordination assists persons with developmental disabilities and their families in gaining access to services and supports appropriate to their needs. OPWDD delivers almost all service coordination through its Medicaid Service Coordination program (MSC). MSC is provided by qualified service coordinators and uses a person– centered planning process in developing, implementing, and maintaining an Individualized Service Plan. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Moving Assistance | Transport of the participant´s possessions and furnishings when moving from an inadequate or unsafe housing situation or to a location where more natural supports will be available. | NHTD WAIVER | Elderly, PD | Retain in Waiver; Include in Managed Care |
| Nutritional Counseling | Assessment, planning, education and counseling for the waiver participant´s nutritional needs and food patterns. | NHTD WAIVER | Elderly, PD | Retain |
| Pathway to Employment* | Time–limited services designed to provide individuals with the skills and training necessary for competitive employment. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Peer Mentoring | Education, information sharing and self–advocacy training to increase the waiver participant´s self– sufficiency in the community and access to needed services, goods and opportunities. | NHTD WAIVER | Elderly, PD | Retain in Waiver; Include in Managed Care |
| Personal Care Services | Personal care services involve providing assistance to individuals with personal hygiene, dressing, feeding and household tasks essential to his/her health. Nutritional, environmental support and personal care functions such as meal preparation, housekeeping represent additional types of personal care services offered. | STATE PLAN SERVICES (FFS) | All | Retain |
| Personal Emergency Response Services (PERS) | The provision and maintenance of electronic communication equipment in the home of an individual which signals a monitoring agency for help when activated by the individual or after a period of time if a timer mechanism has not been reset. PERS provides for continuous monitoring of such signals by a trained operator and when indicated, the immediate notification of such emergency response organizations or persons, if necessary, that the individual had previously specified. | STATE PLAN SERVICES (FFS) | All | Retain |
| Plan of Care Support Services* | Support with the Individualized Service Plan development and maintenance for individuals not opting for comprehensive service coordination. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Positive Behavioral Interventions and Supports | Interventions provided to waiver participants whose significant maladaptive behaviors, if continued, would result in the individual being removed from the community. | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain in Waiver; Include in Managed Care |
| Prevocational Services | Habilitation services that provide learning and work experiences, including volunteering, where participants can develop general, non–job–task– specific strengths and skills that contribute to employability in paid employment in integrated community settings | OPWDD HCBS WAIVER | ID/DD | Retain |
| Private Duty Nursing | The provision of continuous nursing services by a Registered Nurse or Licensed Practical Nurse that are beyond the scope of a CHHA. Under other circumstances, patient´s may need only intermittent nursing services which are normally provided by a CHHA but which are unavailable at the time the patient needs them. | STATE PLAN SERVICES (FFS) | All | Retain |
| Residential Habilitation (Supervised)* | Habilitation services that occur in small–sized certified l settings that assist with the acquisition, retention or improvement in skills related to living in the community. Supervised model residences provide staff support whenever individuals are present in the home. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Residential Habilitation (Supportive)* | Habilitation services that occur in small–sized certified settings that assist with the acquisition, retention or improvement in skills related to living in the community. Supportive model residences provide staff support that varies according to an individual´s need. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Respiratory Therapy | Services providing preventative, maintenance and rehabilitative airway–related techniques and procedures. | NHTD WAIVER TBI WAIVER | Elderly, PD | Retain |
| Respite Care Services | Relief for non–paid primary caregivers of a waiver participant. | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain |
| Respite* Agency Managed Self– Directed | Services provided to participants unable to care for themselves that are furnished on a short–term basis because of the absence or need for relief of those persons who normally provide care for the participant. May be provided in the individual´s home or at a certified site. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Service Coordination | Assistance with the development and implementation of a person– centered individualized Service Plan that will lead to participant´s greater independence and integration into the community. | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain |
| Structured Day Program | Outpatient congregate services including a wide array of interventions and supports ranging from building task–related skills to socially–oriented activities. | NHTD WAIVER TBI WAIVER | Elderly, PD, Dual/TBI | Retain in Waiver; Include in Managed Care |
| Substance Abuse Program Services | Individually designed interventions to reduce/eliminate the use of alcohol and/or other substances, provided in an outpatient, congregate setting. | TBI WAIVER | Elderly, PD, Dual/TBI | Retain in Waiver; Include in Managed Care |
| Support Brokerage* | Support brokers assist waiver participants, or the participant´s family or representative as appropriate, to self–direct and manage some or all of their waiver services and/or to experience the greatest degree of community integration possible. They may assist in development of a service plan and budget, in the transition to self–direction and in learning about alternatives for receiving services in the most integrated settings. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Supported Employment (SEMP)* Agency Provided Self– Directed | Individualized services and supports to assist people with developmental disabilities in obtaining or maintaining a job in competitive employment. | OPWDD HCBS WAIVER | ID/DD | Retain |
| Transportation Services | This service is offered in addition to medical transportation services required under State Plan. Enables individuals to gain access to waiver and other community services, activities and resources as specified in the Service Plan. | TBI WAIVER | Dual/TBI | Retain in Waiver; Include in Managed Care |
| Wellness Counseling Service | Intermittent evaluation, counseling and training by a Registered Nurse of waiver participants who have a chronic illness but do not need skilled nursing services. | NHTD WAIVER | Elderly, PD | Retain in Waiver; Include in Managed Care |
| Adult Day Care Includes both: Adult Day Health Care and Social Day Care | Adult Day Health Care: Care and services provided in a residential health care facility or approved extension site under the medical direction of a physician to a person who is functionally impaired, not homebound, and who requires certain preventive, diagnostic, therapeutic, rehabilitative or palliative items or services. Adult day health care includes the following services: medical, nursing, food and nutrition, social services, rehabilitation therapy, leisure time activities which are a planned program of diverse meaningful activities, dental pharmaceutical, and other ancillary services. Social Day Care: A structured, comprehensive program which provides functionally impaired individuals with socialization; supervision and monitoring; personal care; and nutrition in a protective setting during any part of the day, but for less than a 24–hour period. Additional services may include and are not limited to maintenance and enhancement of daily living skills, transportation, caregiver assistance, and case coordination and assistance. | MLTC MMC | Elderly, PD | Retain |
| Audiology/Hearing Aids | Audiology services include audiometric examination or testing, hearing aid evaluation, conformity evaluation and hearing aid prescription or recommendations if indicated. Hearing aid services include selecting, fitting and dispensing of hearing aids, hearing aid checks following dispensing and hearing aid repairs. Products include hearing aids, earmolds, batteries, special fittings and replacement parts. | MLTC | Elderly, PD | Retain |
| Care Management | Care management is a process that assists Enrollees to access necessary covered services as identified in the care plan. It also provides referral and coordination of other services in support of the care plan. Care management services will assist Enrollees to obtain needed medical, social, educational, psychosocial, financial and other services in support of the care plan irrespective of whether the needed services are covered under the capitation payment of this Agreement. | MLTC | Elderly, PD | Retain |
| Dentistry | Dentistry includes but shall not be limited to preventive, prophylactic and other dental care, services and supplies, routine exams, prophylaxis, oral surgery, and dental prosthetic and orthotic appliances required to alleviate a serious health condition including one which affects employability. | MLTC MMC | Elderly, PD | Retain |
| DME | Durable Medical Equipment (DME), includes medical/surgical supplies, prosthetics and orthotics, and orthopedic footwear, enteral and parenteral formula and hearing aid batteries. | MLTC MMC | Elderly, PD | Retain |
| Home Care– Home Health Aide | Home health aide means a person who carries out health care tasks under the supervision of a registered nurse or licensed therapist and who may also provide assistance with personal hygiene, housekeeping and other related supportive tasks to an Enrollee with health care needs in his home. Qualifications of home health aides are defined in 10 NYCRR 700.2(b) (9). | MLTC | Elderly, PD | Retain |
| Home Care – Nursing | Nursing services include intermittent, part–time and continuous nursing services provided in accordance with an ordering physician´s treatment plan as outlined in the physician´s recommendation. Nursing services must be provided by RNs and LPNs in accordance with the Nurse Practice Act. Nursing services include care rendered directly to the individual and instructions to his family or caretaker in the procedures necessary for the patient´s treatment or maintenance. | MLTC | Elderly, PD | Retain |
| Home Care – Occupational Therapy | Occupational therapy: Rehabilitation services provided by a licensed and registered occupational therapist for the purpose of maximum reduction of physical or mental disability and restoration of the Enrollee to his or her best functional level. Medicaid coverage of occupational therapy provided in a setting other than a home is limited to 20 visits per calendar year, except for children under age 21 and the developmentally disabled. A MLTC plan may authorize additional visits. | MLTC | Elderly, PD | Retain |
| Home Care – Physical Therapy | Physical therapy: Rehabilitation services provided by a licensed and registered physical therapist for the purpose of maximum reduction of physical or mental disability and restoration of the Enrollee to his or her best functional level. Medicaid coverage of physical therapy provided in a setting other than a home is limited to 20 visits per calendar year, except for children under age 21 and the developmentally disabled. A MLTC plan may authorize additional visits. | MLTC | Elderly, PD | Retain |
| Home Care – Speech Pathology | Speech–language pathology: A licensed and registered speech–language pathologist provides rehabilitation services for the purpose of maximum reduction of physical or mental disability and restoration of the Enrollee to his or her best functional level. Medicaid coverage of speech therapy provided in a setting other than a home is limited to 20 visits per calendar year, except for children under age 21 and the developmentally disabled. A MLTC plan may authorize additional visits. | MLTC | Elderly, PD | Retain |
| Home Delivered or Congregate Meals | Meals: Home–delivered and congregate meals provided in accordance with each individual Enrollee´s plan of care. | MLTC | Elderly, PD | Retain |
| Medical Social Services | Social services are information, referral, and assistance with obtaining or maintaining benefits which include financial assistance, medical assistance, food stamps, or other support programs provided by the LDSS, Social Security Administration, and other sources. Social services also involve providing supports and addressing problems in an Enrollee´s living environment and daily activities to assist the Enrollee to remain in the community. | MLTC | Elderly, PD | Retain |
| Non–emergent Transportation | Transportation: shall mean transport by ambulance, ambulance, taxi or livery service or public transportation at the appropriate level for the Enrollee´s condition for the Enrollee to obtain necessary medical care and services reimbursed under the New York State Plan for Medical Assistance or the Medicare Program. The Contractor is required to use only approved Medicaid ambulance vendors to provide ambulance transportation services to Enrollees. | MLTC | Elderly, PD | Retain |
| Nutrition | Nutrition means the assessment of nutritional needs and food patterns, or the planning for the provision of foods and drink appropriate for the individual´s physical and medical needs and environmental conditions, or the provision of nutrition education and counseling to meet normal and therapeutic needs. | MLTC | Elderly, PD | Retain |
| Optometry/ Eyeglasses | Optometry includes the services of an optometrist and an ophthalmic dispenser and includes eyeglasses; medical necessary contact lenses and polycarbonate lenses, artificial eyes (stock or custom made) and low vision aids. The optometrist may perform an eye exam to detect visual defects and eye disease as necessary or as required by the Enrollee´s condition. Examinations which include refraction are limited to every two years unless otherwise justified as medically necessary. | MLTC | Elderly, PD | Retain |
| Outpatient Therapies – PT, OT, SP or other therapies provided in a setting other than a home | Rehabilitation services in an outpatient setting provided by licensed and registered therapists for maximum reduction of physical disability and restoration or maintenance of the member to their best functional level. Report each time an enrollee receives therapy services regardless of the number of procedures or clinicians seen. This includes physical, occupational and speech therapies, but excludes mental health, drug and alcohol therapy. | MLTC MMC | Elderly, PD | Retain |
| Personal Care and CDPAP | Personal care means some or total assistance with such activities as personal hygiene, dressing and feeding, and nutritional and environmental support function tasks. Personal care must be medically necessary, ordered by the Enrollee´s physician and provided by a qualified person as defined in 10 NYCRR 700.2(b) (14), in accordance with a plan of care. | MLTC MMC | Elderly, PD | Retain |
| Personal Emergency Response System (PERS) | Personal Emergency Response System (PERS): PERS is an electronic device which enables certain high– risk patients to secure help in the event of a physical, emotional or environmental emergency. A variety of electronic alert systems now exist which employ different signaling devices. Such systems are usually connected to a patient´s phone and signal a response center once a "help" button is activated. In the event of an emergency, the signal is received and appropriately acted on by a response center. | MLTC MMC | Elderly, PD | Retain |
| Podiatry | Podiatry means services by a podiatrist which must include routine foot care when the Enrollee´s physical condition poses a hazard due to the presence of localized illness, injury or symptoms involving the foot, or when they are performed as necessary and integral part of medical care such as the diagnosis and treatment of diabetes, ulcers, and infections. Routine hygienic care of the feet, the treatment of corns and calluses, the trimming of nails, and other hygienic care such as cleaning or soaking feet, is not covered in the absence of pathological condition. | MLTC MMC | Elderly, PD | Retain |
| Private duty nursing | Private duty nursing services as medically necessary are continuous and skilled nursing care provided in an Enrollee´s home, or under certain conditions a Hospital or Nursing Home, by properly licensed registered professional or licensed practical nurses. | MLTC | Elderly, PD | Retain |
| Respiratory therapy | Respiratory therapy means the performance of preventive, maintenance and rehabilitative airway– related techniques and procedures including the application of medical gases, humidity, and aerosols, intermittent positive pressure, continuous artificial ventilation, the administration of drugs through inhalation and related airway management, patient care, instruction of patients and provision of consultation to other health personnel. These services must be provided by a qualified respiratory therapist as defined in 10 NYCRR 700.2(b) (33). | MLTC | Elderly, PD | Retain |
| Social and Environmental Supports | Social and environmental supports are services and items that support the medical needs of the Enrollees and are included in an Enrollee´s plan of care. These services and items include but are not limited to the following: home maintenance tasks, homemaker/chore services, housing improvement, and respite care. | MLTC | Elderly, PD | Retain |
| Community Integration Counseling | An individually designed service intended to assist Participants who are experiencing significant problems in managing the emotional difficulties inherent in adjusting to a significant disability and/or living in the community. It is a counseling service provided to the Participant who is coping with altered abilities and skills, a revision of long– term expectations, or changes in roles in relation to significant others. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Community Transitional Services | Assistance in transition from a nursing home back to the community: including the cost of moving furniture and other belongings, purchase of certain essential items such as linen and dishes, security deposits, including broker´s fees required to obtain a lease on an apartment or home; purchasing essential furnishings; set–up fees or deposits for utility or service access (e.g. telephone, electricity, heating); and health and safety assurances such as pest removal, allergen control or one time cleaning prior to occupancy. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Environmental Modifications | Internal and external physical adaptations to the home necessary to enable the person to function with greater independence, to assure health and welfare, and/or to prevent institutionalization. E– mods may include: installation of ramps and grab bars; widening of doorways; modifications of bathroom facilities; installation of specialized electrical or plumbing systems to accommodate necessary medical equipment; or any other modification necessary to assure the Participant´s health, welfare or safety. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Home and Community Support Services | Assistance with ADLs and IADLs with oversight/supervision services or oversight/supervision as a discrete service, primarily delivered at a Participant´s home. HCSS is provided to a Participant who requires assistance with personal care services tasks and whose health and welfare in the community is at risk because oversight/supervision of the Participant is required when no personal care task is being performed. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Home Visits by Medical Personnel | Individually designed services to provide diagnosis, treatment and wellness monitoring in order to preserve the Participant´s functional capacity to remain in the community. Home Visits by medical personnel are expected to decrease the likelihood of exacerbation of chronic medical conditions and unnecessary and costly emergency room visits, hospitalizations and nursing facility placement. In addition to assessing the Participant, this service will also include the evaluation of the home environment from a medical perspective, and the Participant´s informal support system´s ability to maintain and/or assume the role of caregiver. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Independent Living Skills Training | Training to improve or maintain the Participant´s ability to live as independently as possible in the community by focusing on essential community living skills such as task completion, including Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs). May be provided in the Participant´s residence and in the community on an individual basis. Services may include assessment, training, and supervision of or assistance to, an individual with self–care, medication management, task completion, communication skills, interpersonal skills, socialization, sensory/motor skills, mobility, community transportation skills, reduction/elimination of maladaptive behaviors, problem solving skills, money management, prevocational skills and ability to maintain a household. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Moving Assistance | Transport of the Participant´s possessions and furnishings when moving from an inadequate or unsafe housing situation or to a viable environment which more adequately meets the Participant´s health and welfare needs. May also be utilized when the Participant is moving to a location where more natural supports will be available, and thus allows the Participant to remain in the community in a supportive environment. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Non–Medical Transportation Services | This service is offered in addition to medical transportation services required under State Plan. Enables individuals to gain access to non–medical and community services, such as religious services, community activities, supermarkets, etc. as specified in the Service Plan. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Peer Mentoring | Education, information sharing and self–advocacy training to increase the waiver participant´s self– sufficiency, self–reliance and ability to access needed services, goods and opportunities in the community. This will be accomplished through education, teaching, instruction, information sharing, and self–advocacy training. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Positive Behavioral Interventions and Supports | Interventions provided to Participants who have significant behavioral difficulties that jeopardize their ability to remain in the community of choice due to inappropriate responses to events in their environment. Services include a comprehensive assessment of the individual´s behavior (in the context of their medical diagnosis as determined by the appropriate health or mental health professional), skills and abilities, existing and potential natural and paid supports and the environment; the development and implementation of a holistic structured behavioral treatment plan including specific realistic goals which can also be utilized by other Providers and natural supports; the training of family, natural supports and other providers so that they can also effectively use the basic principles of the behavioral plan; and regular reassessment of the effectiveness of the behavioral treatment plan, making adjustments to the plan as needed. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Structured Day Programs | Outpatient congregate services to improve or maintain the Participant´s skills and ability to live as independently as possible in the community, including assessment, training and supervision to an individual with self–care, task completion, communication skills, interpersonal skills, problem– solving skills, socialization, sensory/motor skills, mobility, community transportation skills, reduction/elimination of maladaptive behaviors, money management skills and ability to maintain a household. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Substance Abuse Program Services | Individually designed interventions to reduce/eliminate the use of alcohol and/or other substances, provided in an outpatient, congregate setting, including an assessment of the individual´s substance abuse history; learning/behavioral assessment; development of a structured treatment plan which reflects an understanding of the Participant´s substance abuse history and cognitive abilities; implementation of the plan; on– going education and training of the Participant, family members, natural supports and all other service Providers; individualized relapse strategies; periodic reassessment of the plan; and ongoing support. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
| Wellness Counseling | Intermittent evaluation, counseling and training by a Registered Nurse intended to assist the medically stable Participant in maintaining an optimal health status. Delivered to Participants who have a chronic illness but are medically stable and do not need skilled nursing services. A Registered Professional Nurse assists the Participant to identify his/her health care needs and provides guidance to minimize, or in some cases prevent acute episodes of disease and utilize health care resources efficiently and effectively. | MLTC–FIDA | Elderly, PD, TBI | Retain in Waiver; Include in Managed Care |
5. Administrative Staffing
Background
The New York State DOH is designated as the single agency responsible for the administration of the Medicaid program. Within NYSDOH, the Deputy Commissioner of the Office of Health Insurance Programs (OHIP) also serves as the Director of the State Medicaid Program. Under OHIP is the Division of Long–Term Care (DLTC) and under DLTC is the Bureau of Community Integration and Alzheimer´s Disease (BCIAD). The Demonstration is operationally housed within the BCIAD.
Placement of the Demonstration under the strategic auspices of the DLTC encourages effective management and coordination with other State entities and similar stakeholders. The Director of the DLTC reports directly to the State Medicaid Director, who has the final authority with regard to the administration of all aspects of the Medicaid program in New York State. The MFP Demonstration Project Director is also the Bureau Director for the BCIAD.
Matrix of Administrative Positions
The following tables provide a listing of Administrative Staff positions funded via MFP Administrative funds. Each job position includes the following data elements:
- Functional position title
- Job description
- Current status
- Number of FTEs
- Location
- Type of employee (State or contractor)
- Post–MFP status
- State´s decision to retain, reduce or combine the number of FTEs, or delete the position
- Number of FTEs
- Location
- Type of employee (State or contractor)
- Source of funding for position post–MFP
- Entity that will secure funding
- Date to commence work to secure funding
- Projected date to secure funding
| MFP Demonstration Project Director | |
|---|---|
| Job Description: | The State MFP Demonstration Project Director is dedicated to and acts as the overall director of New York´s MFP Demonstration. The Director is responsible for assuring that all of the activities of the MFP Demonstration are successfully completed, in addition to duties associated with other titles. This includes supervising professional and non–professional staff, coordinating activities and reporting with other State entities and partners, assuring compliance with the MFP Operational Protocol, assuring that the State has satisfied all of the CMS reporting requirements, assuring compliance with fiscal requirements, providing content expertise, providing overall direction of contractors for MFP–related initiatives, and facilitating collaboration with other State agencies, advocates, providers and other stakeholders. |
| Current Status | |
| Number of FTEs: | 1.0 FTE at 51% |
| Location: | NYS Department of Health, Albany |
| Type: | State employee, permanent |
| Post–MFP | |
| Status: | Retain |
| Number of FTEs: | 1.0 FTE at 31% |
| Location: | NYS Department of Health, Albany |
| Type: | State employee, permanent |
| Funding Source: | Medicaid Administrative Funds |
| Securing Entity: | NYS Department of Health |
| Date to Seek Funding: | 01/01/2018 |
| Date to Secure Funding: | 06/30/2020 |
| Project Directors | |
|---|---|
| Job Description: | Provides oversight of the MFP teams (DOH and OPWDD) in restructuring and rebalancing activities. Responsibilities include daily management of the MFP Demonstration staff and activities, preparation of revisions to the Operational Protocol as needed, ensures preparation and submittal of all CMS– and State–required reports on time. Provides oversight of the MFP Demonstration to assure accountability and timely delivery of project components, provides expertise in shaping program decisions. |
| Current Status | |
| Number of FTEs: | 2.0 FTEs at 100% each |
| Location: | 1 – NYS Department of Health, Albany 1 – NYS Office for People with Developmental Disabilities, Albany |
| Type: | State employee, permanent |
| Post–MFP | |
| Status: | Retain |
| Number of FTEs: | 2.0 FTE at 100% each |
| Location: | 1 – NYS Department of Health, Albany 1 – NYS Office for People with Developmental Disabilities, Albany |
| Type: | State employee, permanent |
| Funding Source: | Medicaid Administrative Funds |
| Securing Entity: | 1 – NYS Department of Health 1 – NYS Office for People with Developmental Disabilities |
| Date to Seek Funding: | 01/01/2018 |
| Date to Secure Funding: | 06/30/2020 |
| MFP Supervisor | |
|---|---|
| Job Description: | Assists the Project Director in the supervision of Coordinators and Assistants in the oversight of the MFP Demonstration to ensure the ability to meet Federal program requirements. Duties include supervisory activities in all aspects of program implementation in the administration of Project related activities, including public outreach and education, training and technical assistance; supervision, guidance, including oversight of assigned MFP staff; MOU execution; single/sole source contract requests; drafting of Requests for Applications, review of protocols/oversight of vendor selections; coordination of financial/statistical data for CMS reports; development of policies and procedures related to MFP participants and related LTC rebalancing activities; development of Operational Protocol updates for NYSDOH management for submission to CMS; reconciliation of vendor payment vouchers and program reports to assure meeting contract deliverables; overseeing completion of the MFP Quality of Life surveys; compilation of cross contractor survey data; development of annual Project budgets; provision of technical assistance/training to MFP staff and contractors; oversight of NYS statewide Minimum Data Set 3.0 Section Q implementation; represent MFP Project Director in her/his absence. |
| Current Status | |
| Number of FTEs: | 2.0 FTEs at 100% each |
| Location: | 1 – NYS Department of Health, Albany 1 – NYS Office for People with Developmental Disabilities, Albany |
| Type: | 1 – State employee, permanent 1 – Contractor |
| Post–MFP | |
| Status: | Reduction |
| Number of FTEs: | 1.0 FTE at 100% |
| Location: | 1 – NYS Department of Health, Albany |
| Type: | State employee, permanent (to replace contract position) |
| Funding Source: | Medicaid Administrative Funds |
| Securing Entity: | NYS Department of Health |
| Date to Seek Funding: | 01/01/2018 |
| Date to Secure Funding: | 06/30/2020 |
| MFP Coordinator | |
|---|---|
| Job Description: | Reports to the Project Director and Supervisor. Leads the team directly responsible for daily management of MFP Demonstration activities plus maintaining and updating the MFP Operational Protocol ensuring correct and timely reporting to CMS. The Project Coordinator is responsible for managing multiple projects involved in this Demonstration and will be responsible for assisting in oversight of MFP funded contract deliverables. Supervise activities regarding complex federally required data collection, mining, reporting and data base development and management for MFP system change initiatives. |
| Current Status | |
| Number of FTEs: | 5.0 FTEs at 100% each |
| Location: | 3 – NYS Department of Health, Albany (2–State employee; 1– Contractor) 2 – NYS Office for People with Developmental Disabilities, Albany |
| Type: | 4 – State employee, permanent 1 – Contractor |
| Post–MFP | |
| Status: | Reduction |
| Number of FTEs: | 3.0 FTE at 100% each |
| Location: | 2 – NYS Department of Health, Albany 1 – NYS Office for People with Developmental Disabilities, Albany |
| Type: | State employee, permanent |
| Funding Source: | Medicaid Administrative Funds |
| Securing Entity: | 2 – NYS Department of Health 1 – NYS Office for People with Developmental Disabilities |
| Date to Seek Funding: | 01/01/2018 |
| Date to Secure Funding: | 06/30/2020 |
| Project Assistant | |
|---|---|
| Job Description: | Assists the Project Coordinator in CMS required reporting and assists in evolving long–term care service infrastructure. The position is needed to create and administer required satisfaction surveys and other quality/risk assessment tools; assist with tracking of MFP participant data, and assist in administering high profile MFP activities including RFA/Ps, contracts, work plans, etc. |
| Current Status | |
| Number of FTEs: | 1.0 FTE at 100% |
| Location: | NYS Department of Health, Albany |
| Type: | Contractor |
| Post–MFP | |
| Status: | Retain |
| Number of FTEs: | 1.0 FTE at 100% |
| Location: | NYS Department of Health, Albany |
| Type: | State employee, permanent (to replace contract position) |
| Funding Source: | Medicaid Administrative Funds |
| Securing Entity: | NYS Department of Health |
| Date to Seek Funding: | 01/01/2018 |
| Date to Secure Funding: | 06/30/2020 |
| Project Transition Coordinator | |
|---|---|
| Job Description: | Reports to the Project Director and Supervisor. Coordinates and leads efforts between OPWDD Front Door staff and staff planning the move out of the institution to ensure consistency in community transitions and that individual needs are being met in a timely and efficient manner. Develops guidance and provides technical assistance to OPWDD staff and staff assisting with transitions. The Transition Coordinator works with the MFP team and is the liaison with the transition center vendors to ensure clear definition of roles and processes between the vendors and State agency staff. |
| Current Status | |
| Number of FTEs: | 1.0 FTE at 100% |
| Location: | NYS Office for People with Developmental Disabilities, Albany |
| Type: | State employee, permanent |
| Post–MFP | |
| Status: | Retain |
| Number of FTEs: | 1.0 FTE at 100% |
| Location: | NYS Office for People with Developmental Disabilities, Albany |
| Type: | State employee, permanent |
| Funding Source: | Medicaid Administrative Funds |
| Securing Entity: | NYS Office for People with Developmental Disabilities |
| Date to Seek Funding: | 01/01/2018 |
| Date to Secure Funding: | 06/30/2020 |
| Housing Analyst | |
|---|---|
| Job Description: | Meets the MFP Demonstration´s housing related goals, including the Housing Education Initiative. Responsible for MFP rebalancing activities and other projects designed to increase the availability of affordable, accessible and integrated housing. Acts as a resource to NYSDOH NHTD and TBI waiver staff regarding housing subsidy programs and environmental modifications and supports the MRT Supportive Housing Initiative. In addition, the Housing Analyst serves a role as liaison with local Independent Living Center (ILC) Housing Specialists and helps resolve housing accessibility issues that block choice of community–based long–term care. |
| Current Status | |
| Number of FTEs: | 1.0 FTEs at 100% each |
| Location: | NYS Department of Health, Albany |
| Type: | State employee, permanent |
| Post–MFP | |
| Status: | Retain |
| Number of FTEs: | 1.0 FTE at 100% each |
| Location: | NYS Department of Health, Albany |
| Type: | State employee, permanent |
| Funding Source: | Medicaid Administrative Funds |
| Securing Entity: | NYS Department of Health |
| Date to Seek Funding: | 01/01/2018 |
| Date to Secure Funding: | 06/30/2020 |
| Data Analyst | |
|---|---|
| Job Description: | Oversees and manages MFP data reporting requirements with regard to participant information and service expenditures. Oversees the management of Section Q MDS data for the Peer Outreach and Transition Center project. Creates complex queries using the NYSDOH Medicaid Data Warehouse, Salient, and other data sources. Oversees documentation and flowcharting of assigned system projects and manages reconciling financial data collection for CMS required reports and generates statistical and financial reports. |
| Current Status | |
| Number of FTEs: | 1.0 FTE at 100% |
| Location: | NYS Department of Health, Albany |
| Type: | Contractor |
| Post–MFP | |
| Status: | Retain |
| Number of FTEs | 1.0 FTE at 100% |
| Location: | NYS Department of Health, Albany |
| Type: | State employee, permanent (to replace contract position) |
| Funding Source: | Medicaid Administrative Funds |
| Securing Entity: | NYS Department of Health |
| Date to Seek Funding: | 01/01/2018 |
| Date to Secure Funding: | 06/30/2020 |
6. Fund Utilization
Prior Uses of Rebalancing Funds
Accessible Housing Registry
New York State Homes and Community Renewal (HCR) provides, in collaboration with New York State DOH and OPWDD, funding for a web–based Accessible Housing Registry that lists information about accessible rental properties located throughout New York State. Landlords and owners may list their accessible housing units on the website www.NYHousingSearch.gov or through the HCR website at www.nyshcr.org. People with disabilities and seniors, as well as their families and advocates, can search the Accessible Housing Registry by location (town, zip code and major cities) and/or by sorting based on income, age or disability for comprehensive information about housing opportunities that may meet their needs.
State savings achieved, due to the receipt of enhanced Federal Medical Assistance Percentage (FMAP) through the MFP Demonstration, were directed towards activities designed to strengthen the Accessible Housing Registry to make it a more effective tool for posting and researching available accessible housing units. This one–time funding supplemented the balance provided by HCR, the State´s housing agency to support enhancements to the web–based Accessible Housing Registry that resulted in improved functionality, including the development of www.NYHousingSearch.gov. In addition, the funding was used to market NYHousingSearch.gov to people with disabilities and seniors, owners and landlords and other stakeholders such as service coordinators and discharge planners and to verify the accessibility features of properties.
One–time funding for this initiative was provided in Calendar Year 2008. The website is currently sustained with funding provided by HCR. Marketing of the services was included in the MFP Housing Education Initiative. Though the contract ended in mid–2013, the Accessible Housing Registry continues to promote the availability of affordable, accessible and integrated housing for individuals who wish to avoid or transition from nursing home placement by fostering public/private collaboration and increasing the capacity of stakeholders.
Housing Education and Training of Stakeholders
An important aspect of this MFP rebalancing initiative was to increase communication and change at the local level with regard to the housing needs of people with disabilities and seniors. Beginning in Calendar Year 2009, New York State DOH developed training that focused on housing related policies, such as the Consolidated Planning process, and strategies for effective communication with local housing officials so that trainees would have the knowledge needed to navigate the housing system and more effectively interact with local housing officials. In turn, this informed interaction increased the knowledge base of the local housing officials regarding the needs of people with disabilities and seniors, and the need to promote public/private collaboration. Trainees included stakeholders such as local housing officials, seniors, individuals with disabilities, service coordinators, discharge planners and other
interested stakeholders. The project has reached over 2,800 stakeholders, successfully raising awareness of accessible housing issues across the State.
Housing Training (OPWDD)
The cornerstone of independence for people with intellectual and developmental disabilities is having one´s own home – whether it is an apartment, a furnished room, a shared living arrangement, a single– family home or some other type of residential setting. Lack of accessible housing prevents people with all types of special needs from living in a home of their choice and hinders the progress of the transformation agenda within New York State.
To help address the ongoing need for accessible housing within the disability community, OPWDD´s Office of Home & Community Living received MFP funding for the training and certification of Housing Specialists through the services of Neighbor Works America, a nonprofit organization that provides grants and technical assistance to community development organizations and provides training for housing and community development professionals. Training and certification has taken place during June 2015 followed by a regionally–based train–the–trainer program. Training included Homeownership Counseling Certification, Rental Counseling, and a component on “Making Homes that Work.”
Guardianship Project – VERA
Indigent people with disabilities and seniors, who have been adjudicated by a court as incapacitated, may find that the inability to locate a legal guardian has created an artificial barrier to community care as an alternative to unwanted institutionalization. To address this issue, a portion of the rebalancing funds was used to support an Access to Court Appointed Guardians Project, implemented by a single source contract with the New York City based Vera Institute for Justice (Vera). Vera actively strives to assist low income individuals to move out of institutions and back to their home communities. In 2005, the Vera Institute, in collaboration with the New York State Office of Court Administration, established The Guardianship Project to test a new model of institutional guardianship for indigent elderly and people with disabilities who have been adjudicated by a court as incapacitated. The project has served over 100 individuals annually. The partnership with the Demonstration empowered Vera to expand its capacity to additional boroughs within the New York City area.
Volunteer Caregiver Project
Support and services provided by family members, friends, neighbors and volunteers to the elderly and people with disabilities can often make the difference on whether someone can remain in the community or will have to seek unwanted and costly institutional care. Community Caregivers, Inc. is a non–for–profit organization, funded by donations, charitable gifts, grants and fund–raising activities. The organization matches volunteers with clients in need of non–medical assistance. Rebalancing funds were used to expand the capacity to provide free home–based, non–clinical support services to residents across northwestern and central Albany County. These services enabled individuals of all ages to maintain their independence, dignity, and quality of life within their homes and communities. This assistance often helped those in need avoid hospitalization or institutionalization; as well as, help family members and friends cope with the challenge of long–term caregiving. Services were provided free of charge to eligible individuals. Uses of the funding included volunteer recruitment, training, stipends, supplies and administrative expenses.
Community Transitions Video Project (OPWDD)
The goal of the Community Transitions Video was to portray, through personal stories, successful transitions of I/DD individuals receiving OPWDD services from segregated institutional settings to integrated community–based opportunities. The personal stories focus on their living situation, workplace, daily activities, relationships and how OPWDD supports and services are assisting them with their transition to a community–based setting. Interviews with the individuals are supported by video testimony from anyone who has assisted with the transition including but not limited to: family members, staff, agency administrators, Medicaid Service Coordinators, friends, acquaintances, employers, etc.
The Community Transitions video is used for multiple purposes: as an example of success stories for presentation to providers, individuals and families to encourage others to make the transition, on the OPWDD website to show transition success stories to the general public, increase public trust in the system, and inform and encourage OPWDD staff, as background video for conference displays, and in other potential uses such as training, outreach, awareness and advocacy.
Currently, many within the service system question the system´s ability to support people with significant needs successfully in community settings. The video demonstrates how this is being done with real stories of how people´s lives have positively changed as they receive the supports they need to experience life in their communities.
The video showcases the following:
- Individuals with significant support needs – behavioral, medical, intellectual – living in community settings;
- Individuals who have left institutional settings and are now living in smaller support settings – small (less than 4 person) group homes, their own apartments or their family home;
- People who have entered and retained employment and other community involvement;
- How the move to community supports has affected the individuals and improved their lives;
- How people with significant support needs are being assisted to self–direct their services; and
- How people are moving to and now living in non–certified settings such as their own apartment (could come from an institution or from a group home – IRA).
Current and Future Uses of Rebalancing Funds
The New York Association of Independent Living and Open Doors
The New York Association of Independent Living (NYAIL) operates the Open Doors program as the backbone of New York State´s MFP Demonstration. The purpose of the Open Doors project is to identify potential participants in nursing facilities, educate them on their return–to–community options and facilitate successful transitions to their community of choice.
NYAIL was chosen as the Contractor for the program through a competitive procurement which awarded the contract for program implementation in February of 2015. Through this contract, NYAIL has established 24 statewide Transition Centers based throughout the local Independent Living Center network to identify and assist individuals from vulnerable populations who express a desire to leave an institutional setting and return to the community. NYAIL has also established a Peer Outreach and Referral program to assist in identifying individuals who express a desire to leave institutional settings and to provide peer support to these individuals through the transition process. Collectively, the Transition Centers and Peer Outreach and Referral program are known by the moniker ´Open Doors´.
Both facets of Open Doors have been fully engaged in the ongoing work of facilitating the transition of elderly and disabled individuals from institutional to community living with the support of MFP rebalancing funds. With additional funding added this year and planned to continue throughout the demonstration period and beyond, the complementary Open Doors programs have expanded their ability to reach–out to the frail elderly, and physically and/or intellectually disabled individuals in New York State nursing homes, as well as Veterans, the elderly with mental health challenges, and New Yorkers residing in out–of–state (OOS) nursing facilities.
Enhancements to the program will continue throughout the remaining grant years and into the sustainability period as interventions and supports are identified that lead to successful transitions and improve the outcomes for long–term transitions. Similarly, the Transition Centers and Peer Outreach and Referral projects will continue to partner with the MFP constituent programs and State agency partners to impact rebalancing efforts at all levels. Expansion of capacity for the Open Doors project parallels the collaborative work of DOH in many areas, including:
- Increasing the capacity of Transition Centers to meet the demand for community preparedness education and transition assistance, particularly in the New York City region where demand is exceptionally high.
- Creating a dedicated outreach and education unit to coordinate and focus outreach to nursing facilities (and care managers), to provide education on Section Q referral requirements.
- Facilitating multi–faceted collaboration with managed care and managed long–term care plans to identify and assist their members.
- Expanding the Transition Center services to effectively serve elderly adults with mental health and behavioral challenges by identifying and linking them to the resources they need to live successfully in the community.
- Expanding Peer support services to identify Veteran participants and effectively match peers on Veteran status.
New York State will continue to operate NYAIL´s Open Doors program through September 2019, supported by MFP rebalancing funds. Based on the rebalancing success achieved by this model of assistance in New York, New York State plans to continue the operation of the Transition Centers and Peer Outreach and Referral programs beyond the end of the MFP Demonstration and into the future by transferring the program support to Medicaid administrative funds in 2020. Towards this end, the development of a competitive re–procurement packet will begin in 2018 to ensure a smooth transition and continuous operation of the Transition Centers and Peer Outreach and Referral services.
Transition Assistance for Institutionalized Individuals
Individuals currently residing in skilled nursing facilities and ICF/IIDs may have limited access to knowledgeable and consistent resources for promoting safe and timely discharge to a community of choice. With the support of the MFP funding, NYAIL´s 24 transition centers identify and assist individuals from vulnerable populations who express a desire to leave an institutional setting and return to the community. An institutionalized individual may or may not possess the self–advocacy skill set necessary to pursue discharge from the facility on her/his own, which may, in some cases, prevent a successful discharge from the facility. This experience has been noted during stakeholder meetings, discussions with service providers, and observations from surveys.
NYAIL´s Transition Centers provide transition planning and community readiness training to educate and support institutionalized individuals to prevent a potential “disconnect” between facility discharge planners and the community–based service providers. Transition Centers are responsible for informing, supporting, and bridging the transition of individuals from pre–discharge while in the facility to early establishment within their community of choice.
The Transition Center program has been so successful that the quantity of referrals has begun to outpace the current resources of the local Transition Centers. During this contract year, the Demonstration has supported increasing the capacity of Transition Centers to meet the demand for community preparedness education and assistance with transition, particularly in the New York City region where the demand for this assistance is exceptionally high.
Peer Outreach and Support to Institutionalized Individuals
Despite various efforts in the field to provide information about HCBS options, there have remained individuals who are unaware of these options, including any new resources, opportunities and/or policy developments related to HCBS services, since being admitted to a facility. The Demonstration has directed rebalancing funds toward an initiative designed to identify and provide peer outreach and support to these institutionalized individuals across all the currently served target populations, including the frail elderly, physically disabled, individuals with an intellectual/developmental disability, and individuals suffering from the sequelae of traumatic brain injury. The Peer Outreach program provides an opportunity to build relationships between a peer and the residents of a particular facility. Not only can currently identified individuals be provided with peer support, but additional residents also reap the benefit of Peers through easy access to information and support. Peer presence in the institution helps to further build relationships between institutional and community care providers. The Peer program, as does the Transition Center program, also empowers and supports individualized choice (via an array of long–term services and supports) through person–centered transition planning.
The partnership of this rebalancing initiative with the recruitment strategies of the constituent programs enables the State to identify, contact, and provide outreach and support to individuals interested in transitioning to the community.
Marketing
As mentioned above, many individuals and caregivers are unaware of the long–term services and supports available to them in their homes and communities, especially those supports that can help them both transition and avoid re–institutionalization. Raising awareness of the MFP/Open Doors program has been important for outreaching to individuals who may qualify for supports to transition back into their homes and communities. Marketing can provide individuals and caregivers the information that they need to reach out to Open Doors and make informed decisions about services and supports needed for sustainable community living.
New York State has used a variety of marketing strategies through the Open Doors program to promote MFP/Open Doors and increase recruitment and enrollment, and ultimately transitions, including:
- Public websites that house information, policy documents and other resources for the MFP program;
- Promotional toolkit for Transition Center and Peer Program staff including flyers, brochures and postcards targeted to different audiences and populations;
- Radio advertising campaign;
- Local cable television advertising campaign that included a 30–second video showcasing 3 different transition stories;
- A series of outreach videos for families and providers;
- Ongoing educational meetings to engage nursing home discharge planners, ombudsman, other long–term care stakeholders, and managed long–term care managers.
Quality of Life Survey
New York State has been very pleased with the results of the Quality of Life (QoL) survey and the information that it has provided to MFP stakeholders via Mathematica´s annual evaluation report. The Demonstration is continuing to support the administration of the QoL survey by the Open Doors´ Transition Specialists beyond the end date of the national evaluation and the grant close–out to measure program success and inform New York State stakeholders on an ongoing basis. The survey has been modified to better align with the plans for continued use, including elimination of the 24–month survey, simplification of the survey process for easier administration by the Transition Specialists, and additional instructions to the Transition Specialists to support the validity of the results. The revisions made extensive use of Mathematica´s annual evaluation reports in order to retain questions with statistical significance. This modified QoL was implemented January 1, 2017 and is intended to continue beyond the demonstration period to provide rebalancing information on an ongoing basis to MFP stakeholders.
Collaboration and Partnerships
Collaboration is a cost–effective strategy for accomplishing program goals. Open Doors partnership in collaborative inter– or intra–agency efforts are supported by the NYAIL contract. Collaborative efforts of DOH MFP staff may involve sub–allocation of funding to a partner agency when needed (included in description), or, where possible, may be achieved by an in–kind exchange of information, referral, and complementary service delivery.
Section Q Outreach Education
Data has demonstrated that nursing facilities are the favored referral source to result in successful transitions to community living. At the same time, data indicates that nursing facilities are not in compliance with MDS Section Q requirements to administer Section Q during each MDS assessment (unless the resident has requested the question not be asked on quarterly assessments) and to refer to the Local Contact Agency (NYAIL) those residents who answer ´yes´ to the community question.
Significant effort was made to address the need for education on this topic through a Public Health Live Webcast which took place on 2/16/17. Curriculum for the forum focused on MFP, rebalancing, and MDS Section Q, and presenters represented both local and national perspectives. With over 600 registrants, the event was very successful with abundant positive feedback obtained. In addition, MFP staff is working closely with New York State DOH´s Division of Nursing Homes and Intermediate Care
Facilities/IID to provide education regarding Section Q referral to the State´s Nursing Home Provider Associations. MFP has also contributed Section Q referral information and resources to the development of curriculum for delivery of MDS training throughout the State.
To more comprehensively address the need for efforts to support Section Q compliance on the local level, a dedicated outreach and education team is being created within Open Doors to coordinate and focus outreach to nursing facilities, including discharge planners, and managed care plans, including care managers, to provide education on Section Q referral requirements.
Managed Care and Managed Long–Term Care
Contributing to the increase in Transition Center and Peer support referrals, is the approval, obtained in January 2016, retroactive to July 1, 2015, to include Managed Care and Managed Long–Term Care as MFP constituent programs. Early identification of an individual´s needs and preferences is essential to successful community living and avoiding reinstitutionalization. Open Doors Transition Specialists and nursing home discharge planners collaborate with plan Care Managers to ensure that MFP participants experience a seamless and successful transition to the community.
Both DOH and NYAIL staff have invested in significant efforts to facilitate multi–faceted collaboration with managed care and managed long–term care plans to identify and assist their members. This has involved the development of relationships, policy, and reporting at the State level, as well as outreach presentations, information sharing, and other efforts to facilitate direct collaboration between Open Doors and the plans. The number of MFP participants receiving their health care services through a managed care or managed long–term care plan is steadily increasing. Processes for verifying enrollment/ plan status have been developed to identify eligible participants. The Demonstration is committed to supporting this continued growth throughout the demonstration period and beyond.
Geriatric Mental Health
According to the New York State OMH, the number of New York State residents aged 65 or older is expected to increase more than 50 percent, from 2.5 million to 3.9 million people, by 2030. Within this demographic, the number of adults aged 65 or older who have mental illness in New York State is expected to increase by 56 percent, from 495,000 in 2000 to 772,000 people in 2030.
The New York State Demonstration´s contractor, NYAIL, through the Open Doors program, has developed a relationship with New York State OMH´s Single Point of Access process. The Single Point of Access has established a uniform process for receiving and evaluating referrals, matching individuals to the services they need, triaging access so that those most in need get priority access and monitoring the results. Transition Specialists use this resource to facilitate transitions involving elderly individuals with mental health needs throughout New York State. NYAIL also works to link participants to Health and Recovery Plans (HARP), a managed care product that manages physical health, mental health, and substance use services in an integrated way for adults with significant behavioral health needs (mental health or substance use). In addition, NYAIL is partnering with the Mental Health Association of New York to provide training and education for Transition Specialists and Peers to support them in their work with individuals with mental health needs. These trainings not only provide education but also offer strategies and information to directly support both the staff and participant.
MFP staff are working in collaboration with DOH and OMH colleagues administering the HARPs. MFP is also collaborating internally and with OMH around the PASRR assessment process and has been established as a referral target for nursing facility residents with mental health needs for whom a Level II PASRR screen has recommended community placement. Ongoing collaboration will work on development of an automated and efficient referral process.
New York State plans to continue this work to link elderly adults with the mental health and behavioral resources they need to live successfully in the community throughout the remaining grant years and through sustainability.
Veterans
The New York State Division of Veterans´ Affairs is the lead advocate for Veterans regarding medical, social, and economic matters and seeks to educate others to the special skills and needs of Veterans, particularly those men and women who served in combat and who may have specific needs resulting from wartime experience. DVA assists New York State Veterans who may be eligible for services and benefits based on their military service and disability and age status. It is the mission of the State´s network of Veterans Benefits Advisors to provide education and assistance to Veterans to facilitate their access to supports and services available through this service system. Additionally, the New York State Veterans´ Homes are skilled nursing facilities owned and operated by the New York State DOH for Veterans and their dependents in need of skilled nursing care and rehabilitative services.
As the age of Veterans in New York State continues to climb, and services offered through the assistance of the Division of Veterans´ Affairs can support Veterans in their communities, the New York State MFP Demonstration has partnered with the New York State Division of Veterans´ Affairs to increase awareness of the transition needs of veterans currently living in nursing facilities. Cross–training of staff among the two service systems has occurred, and cross–referrals are actively pursued, with ongoing collaboration between the Veterans Benefit Advisors and Transition Specialists actively occurring. In addition, the Open Doors Peer Outreach and Referral program is actively recruiting veteran peers to match on Veteran´s status; an effective strategy for engaging Veterans who may be interested in community living.
New York State Office for the Aging
New York State DOH has partnered with the New York State Office for the Aging (SOFA) to facilitate increased access to information about available LTSS through a No–Wrong Door model. The State Office for the Aging expanded its NY Connects program (New York´s Aging and Disability Resource Centers) to include all populations needing LTSS. Transition Center staff use SOFA´s local NY Connects programs (New York´s Aging and Disability Resource Center´s) to help identify available resources in the community.
Collaboration between New York State DOH and SOFA forms a natural partnership, given the agencies´ overlapping constituents and the long–term care needs of those constituents. MFP staff at the State level serve as the liaison between New York State DOH and SOFA to support the ongoing development and improved usability of the NY Connects network, and to support continued collaboration at the local level between the local Area Offices on Aging and the Transition Center network housed within the local Independent Living Centers.
Office for People With Developmental Disabilities
The New York State OPWDD provides programmatic supports and services to enable individuals with developmental disabilities to live in the community as an alternative to Intermediate Care Facilities (ICFs). OPWDD administers a HCBS 1915(c) waiver through which it provides a wide range of community–based supports and services. These supports are provided to individuals through an extensive network of not–for–profit providers and some State–provided services.
OPWDD participates in the New York State MFP Demonstration within the larger context of de–institutionalization. OPWDD´s participation in MFP is expected to support continued transitions of individuals who will be leaving the limited number of campus–based intermediate care facilities which continue to be operated by OPWDD, as well as those elderly individuals residing in skilled nursing facilities.
As part of its system transformation plan, OPWDD may also oversee important and ongoing rebalancing projects that have been supported by the MFP Demonstration and which enhance OPWDD´s ability to meet individuals´ needs in the most integrated community settings possible and enable them to continue meaningful engagement in their communities. Transition efforts for this population will continue post–Demonstration supported by continued sub–allocated funding at a reduced level.
Repatriation
MFP is aligning with other DOH and Statewide initiatives in an effort to successfully repatriate New York State residents whose placements in out–of–State (OOS) nursing facilities are supported by Medicaid.
Open Doors receives referrals from OOS facilities and works with partners from the Regional Resource Development Centers (on behalf of New York State´s waiver programs) and New York´s managed care and managed long–term care plans to facilitate successful transitions to participants´ communities of choice within New York State. Special expertise is needed to address the unique and increased challenges and barriers faced by New York State residents in OOS nursing facilities when attempting to transition to their home communities. For this reason, MFP is planning to support two assessor positions, a Nurse Evaluator and a Behavioral Specialist, to facilitate needs assessment and care planning for this difficult–to–transition population. These are planned as contract positions within the Department, initially supported by MFP rebalancing funds and later transitioning to Medicaid administrative funding as they demonstrate effectiveness. These specialists will use their expertise working with individuals with complex health care needs, in collaboration with Open Doors, to facilitate the navigation of the most complex elements of the healthcare system and successfully transition OOS participants to community living. MFP continues participation in the Repatriation subcommittee of the Traumatic Brain Injury Coordinating Council to support the efforts to repatriate this constituent population to communities within New York State.
Availability of Assistive Technology (TRAID)
A significant barrier facing individuals who wish to avoid or transition from institutional care is the delay in receiving durable medical equipment (DME) and other assistive technology despite typical funding mechanisms such as State Plan services, HCBS waivers or non–Medicaid services. In many cases, the availability of equipment to use in the interim period is necessary to establish and maintain the individual´s independence in the community. As stated in a CMS letter to State Medicaid Directors, “Purchases of DME are typically made after the individual has moved into the community. However, the delay in receiving and adapting to such equipment often causes hardships for the individual and/or the caregiver(s). The delay may introduce unnecessary hazards into the transition and the first few weeks of community dwelling.”
In order to meet the increasing needs of New Yorkers for assistive technology to support independence in the community, the Demonstration has partnered with the New York State Justice Center to provide additional funding for the Technology–Related Assistance for Individuals with Disabilities (TRAID) Project. This funding is used for a variety of activities including the purchase of new inventory to increase needed equipment loans to New Yorkers and increase staffing to provide device demonstrations. This enhanced funding opportunity has allowed the TRAID Project to secure and maintain AT and DME that will be available long after the Demonstration period in New York State. Additionally, this project is unique in that it allows for the recycling and reuse of equipment which is more cost–effective than repeated purchase of new items.
The current MOU that is in effect provides rebalancing funding to the Justice Center for the TRAID project for the period January 2016 through September 2020. The Department intends to support MFP´s continued collaboration with the Justice Center beyond 2020, through efforts to extend the existing MOU using Medicaid administrative funds.
Time–Limited Initiatives
Lifespan–Community Care Connections
Lifespan of Greater Rochester´s Community Care Connections demonstration initiative is intended to effectively integrate a community–based Aging Services provider as an authentic member of the evolving health care delivery system to help older adults remain in their own homes, reduce hospital admissions/readmissions and emergency department use, and to reduce caregiver burden. Lifespan leverages its existing collaborations with other service providers focusing on primary and secondary prevention in order to better support a common goal of helping older adults remain healthy within their own homes.
Lifespan is conducting a robust data collection and comprehensive evaluation during the demonstration which will drive the development of a model plan for successful replication throughout New York State. The Lifespan demonstration is funded by rebalancing funds for the period of 2015–2017 and will produce a comprehensive evaluation report with recommendations for replication.
Person–Centered Planning Comprehensive Training Initiative
Enhancing person–centered practice and planning, i.e., an individualized approach to supporting the frail elderly and individuals with disabling conditions, is an important priority for New York State. The MFP demonstration, in particular, relies on the health care system´s responsiveness to the expressed preferences of individuals with special health care needs to drive the rebalancing of the long–term care system away from institutional placements and towards HCBS delivered in community settings. In addition, person–centered planning aligns with an increasing number of regulatory requirements, such as the Home and Community–Based Services Final Rule. It also serves to help New York State meet a primary goal of our Medicaid Redesign – improving patient experience of satisfaction and quality of life.
This initiative is in the development phase and is planned as a 3–year project using rebalancing funds to support a system–wide training initiative. The project is expected to produce resource materials, curriculum, and processes that will be sustainable beyond the project´s end–date and will support the efforts of the Transition Centers to interface with a health care service system that is increasingly person–centered.
Caregiver Guide
The Caregiver Guide has been developed by the New York State DOH to serve as a practical handbook for all caregivers in New York State, particularly seniors 65+ and their caregivers. For the purposes of the guide, caregivers are defined as spouses, partners, adult children, family members, friends, neighbors, or others who provide support to an adult. Conditions that often require the help of a caregiver, and to which the guide applies, include developmental disabilities, mental health or psychiatric disorders, addiction, chronic conditions such as diabetes or dementia, or a traumatic brain injury. The guide is intended to support caregivers of individuals needing long–term services and support in their communities.
The guide contains a list of resources, medical terms and definitions (including Medicare and Medicaid), information on caregiver´s rights (policy action such as FMLA), as well as tips and strategies for communicating with healthcare professionals, collaborating with family, care options, coping with the stress, legal and financial planning, and creating a safe environment for the individual.
The content has been completed and the guide is currently in the publication design phase of development. Initial plans for distribution include a print run of 2000 copies as a pilot test of the guide. This initial print run will be distributed through the use of New York State DOH partner agencies and contractors, including the Open Doors project, who serve caregivers throughout New York State.
Following feedback from the pilot copies, plans for a large print run and distribution will be finalized.
|top of section 6.| |top of page|7. Projected Timeline
Background
The following is an estimated dynamic project timeline, identifying the specific activities and milestones anticipated within each time period. As such, activities and milestones are, where applicable, subject to change.
This timeline carries through the end of CY 2020.
Timeline for 1/1/15–12/31/16
| PERIOD | PLANNED ACTIVITY | MILESTONE(S) |
|---|---|---|
| Period 1 2015 |
|
|
| Period 2 2015 |
|
|
| Period 1 2016 |
|
|
| Period 2 2016 |
|
|
Timeline for 1/1/17–9/3/20
| Time Period | Activity/Goal | Tasks | Milestones |
|---|---|---|---|
| Period 1 2017 |
Facilitate transition of MLTC members. |
|
|
| Maximize resources to support the sustainability of New York State´s rebalancing efforts. |
|
|
|
| Implement new rebalancing initiative under the Demonstration to promote Person–Centered practice and planning using rebalancing funds. |
|
|
|
| Support MFP participant access to housing services, including the services of a housing specialist, housing subsidies, and community transition services. |
|
|
|
| Provide oversight of funded activities through established partnerships with vendors, State agency stakeholders, and participant input. |
|
|
|
| Develop a robust referral process for Minimum Data Set 3.0 Section Q referrals. |
|
|
|
| Support the transition of specialized populations, including elderly individuals with mental health diagnoses, and veterans and families of veterans. |
|
|
|
| Advance efforts to repatriate individuals placed in OOS nursing facilities to their home communities in New York State by addressing barriers to transition. |
|
|
|
| Inform stakeholders regarding the impact of community transition through a redesigned Quality of Life survey. |
|
|
|
| Support the expansion of the transition work of the Open Doors program. |
|
|
|
| Period 2 2017 |
Enhance data collection methods and streamline data maintenance efforts to effectuate transition to managed care/managed long– term care. |
|
|
| Facilitate transition of MLTC members. |
|
|
|
| Continue to maximize resources to support the sustainability of New York State´s rebalancing efforts. |
|
|
|
| Provide oversight of funded activities through established partnerships with vendors, State agency stakeholders, and participant input. |
|
|
|
| Support MFP participant access to housing services, including the services of a housing specialist, housing subsidies, and community transition services. |
|
|
|
| Implement new rebalancing initiative under the Demonstration to promote Person–Centered practice and planning using rebalancing funds. |
|
|
|
| Inform stakeholders regarding the impact of community transition through a redesigned Quality of Life survey. |
|
|
|
| Improve inventory tracking and reporting to support continued rebalancing funding of the TRAID assistive technology loan project. |
|
|
|
| Extend the Lifespan– Community Care Connections demonstration for an additional 6 months to support program evaluation. |
|
|
|
| Analyze current Demonstration staffing level. Project changes to staffing for the duration of the Demonstration and beyond 2020. |
|
|
|
| Support the expansion of the transition work of the Open Doors program. |
|
|
|
| Develop a robust referral process for Minimum Data Set 3.0 Section Q referrals. |
|
|
|
| Period 1 2018 |
Enhance data collection methods and streamline data maintenance efforts to effectuate transition to managed care/managed long– term care. |
|
|
| Facilitate transition of MLTC members. |
|
|
|
| Continue to maximize resources to support the sustainability of New York State´s rebalancing efforts. |
|
|
|
| Provide oversight of funded activities through established partnerships with vendors, State agency stakeholders, and participant input. |
|
|
|
| Support MFP participant access to housing services, including the services of a housing specialist, housing subsidies, and community transition services. |
|
|
|
| Implement new rebalancing initiative under the Demonstration to promote Person–Centered practice and planning using rebalancing funds. |
|
|
|
| Inform stakeholders regarding the impact of community transition through a redesigned Quality of Life survey. |
|
|
|
| Implement contract closeout activities for Lifespan– Community Care Connections. |
|
|
|
| Develop a robust referral process for Minimum Data Set 3.0 Section Q referrals. |
|
|
|
| Period 2 2018 |
Re–procure vendor for the Transition Center and Peer Outreach and Support programs to continue transitions from institutional to community settings to rebalance the Long–Term Care system. |
|
|
| Continue to maximize resources to support the sustainability of New York State´s rebalancing efforts. |
|
|
|
| Provide oversight of funded activities through established partnerships with vendors, State agency stakeholders, and participant input. |
|
|
|
| Support MFP participant access to housing services, including the services of a housing specialist, housing subsidies, and community transition services. |
|
|
|
| Implement new rebalancing initiative under the Demonstration to promote Person–Centered practice and planning using rebalancing funds. |
|
|
|
| Inform stakeholders regarding the impact of community transition through a redesigned Quality of Life survey. |
|
|
|
| Implement demonstration close–out activities and prepare for transition to State leadership. |
|
|
|
| Implement contract closeout activities for Lifespan– Community Care Connections |
|
|
|
| Period 1 2019 |
Re–procure vendor for the Transition Center and Peer Outreach and Support programs to continue transitions from institutional to community settings to rebalance the Long–Term Care system. |
|
|
| Implementation of the transition of the NHTD and TBI waiver programs and participants into managed care. |
|
|
|
| Continue to maximize resources to support the sustainability of New York State´s rebalancing efforts. |
|
|
|
| Provide oversight of funded activities through established partnerships with vendors, State agency stakeholders, and participant input. |
|
|
|
| Inform stakeholders regarding the impact of community transition through a redesigned Quality of Life survey. |
|
|
|
| Facilitate access to access to assistive technology to support rebalancing efforts beyond the demonstration period. |
|
|
|
| Period 2 2019 |
Re–procure vendor for the Transition Center and Peer Outreach and Support programs to continue transitions from institutional to community settings to rebalance the Long–Term Care system. |
|
|
| Continue to maximize resources to support the sustainability of New York State´s rebalancing efforts. |
|
|
|
| Implement demonstration close–out activities and prepare for transition to State leadership. |
|
|
|
| Provide oversight of funded activities through established partnerships with vendors, State agency stakeholders, and participant input. |
|
|
|
| Inform stakeholders regarding the impact of community transition through a redesigned Quality of Life survey. |
|
|
|
| Period 1 2020 |
Plan for transition of ongoing rebalancing contracts to State–supported funding. |
|
|
| Provide oversight of funded activities through established partnerships with vendors, State agency stakeholders, and participant input. |
|
|
|
| Ensure adequate staffing level to continue to support the Demonstration rebalancing activities beyond 2020. |
|
|
|
| Facilitate access to access to assistive technology to support rebalancing efforts beyond the demonstration period. |
|
|
|
| Inform stakeholders regarding the impact of community transition through a redesigned Quality of Life survey. |
|
|
|
| Period 2 2020 |
Implement demonstration close–out activities. |
|
|
| Implement contract closeout activities for the Person– Centered Planning Comprehensive Training Initiative. |
|
|
|
| Continue oversight of funded activities through established partnerships with vendors, State agency stakeholders, and participant input. |
|
|
|
| Continue to inform stakeholders regarding the impact of community transition through a redesigned Quality of Life survey. |
|
|
|
| Ensure adequate staffing level to continue to support the Demonstration rebalancing activities beyond 2020. |
|
|
Color Key:
Red = managed care–related activities
Purple = administrative/compliance activities
Blue = rebalancing activities
Brown = housing support
Green = outreach and identification activities Maroon = stakeholder feedback
Pink = Demonstration close–out activities
8. Estimated Budget Summary
| Grantee Name: | New York State Department of Health | |||||
|---|---|---|---|---|---|---|
| Public Name: | Money Follows the Person (MFP) Demonstration | |||||
| Award Number: | 1LICMS300140 | |||||
| 6. Object Class Categories | CY 2016 | CY 2017 | CY 2018 | CY 2019 | CY 2020 | TOTAL |
| a. Personnel | $839,287.96 | $839,287.96 | $839,287.96 | $839,287.96 | $839,287.96 | $4,196,439.80 |
| b. Fringe Benefits | $449,690.49 | $449,690.49 | $449,690.49 | $449,690.49 | $449,690.49 | $2,248,452.45 |
| c. Travel | $9,470.00 | $9,470.00 | $9,470.00 | $9,470.00 | $9,470.00 | $47,350.00 |
| d. Equipment | $2,500.00 | $2,500.00 | $2,500.00 | $2,500.00 | $2,500.00 | $12,500.00 |
| e. Supplies | $1,500.00 | $1,500.00 | $1,500.00 | $1,359.07 | $1,200.00 | $7,059.07 |
| f. Contractual | $4,653,966.00 | $4,652,562.00 | $3,645,222.00 | $3,631,068.00 | $3,611,914.00 | $20,194,732.00 |
| g. Construction | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 | $0.00 |
| h. Services | $24,153,373.13 | $21,323,977.99 | $16,769,341.91 | $11,731,638.38 | $4,140,578.25 | $78,118,909.66 |
| i. Total Direct Charges (sum of 6a – 6h) |
$30,109,787.58 | $27,278,988.44 | $21,717,012.36 | $16,665,013.90 | $9,054,640.70 | $104,825,442.98 |
| j. Indirect Charges | $262,951.60 | $262,951.60 | $262,951.60 | $262,951.60 | $262,951.60 | $1,314,758.00 |
| k. Total Federal Budget (sum of 6i – 6j) |
$30,372,739.18 | $27,541,940.04 | $21,979,963.96 | $16,927,965.50 | $9,317,592.30 | $106,140,200.98 |
NOTES & ASSUMPTIONS:
- Personnel:
- Revisions expected with the anticipated addition of new State staff as well as the elimination of contracted positions as part of the overall sustainability process and strategic transition to Managed Long–Term Care.
- Fringe Benefits:
- Rates are based upon information published by the NYS Office of State Comptroller´s Bureau of State Accounting Operations and are current as of SFY 2016–2017.
- Travel:
- Assumed that two State staff will attend annual MFP Conferences.
- Assumed that all Demonstration staff will be claiming in–State mileage expenses.
- Equipment:
- Assumed that ad hoc needs will arise to support the work of the MFP team.
- Supplies:
- Assumed that the Demonstration will have a recurring need for office supplies relevant to the number of staff.
- Computers will be needed for additional hires.
- Computers will need to be replaced during CY 2017 for those Demonstration staff with unsupported equipment.
- Contractual:
- Revisions expected as the contract with NYAIL for Peer Outreach and Transition services is being expanded and extended through 2019.
- Services:
- Qualified HCBS services include individuals from the following target populations: Physically Disabled, Elderly, Other/TBI & Dually Diagnosed, and Developmental Disabilities.
- Individuals receiving MFP qualified HCBS services through the demonstration grant will decline through CY 2018.
Appendix A: Strategic Map
Overview
Supplemental Federal funding for the New York State MFP Demonstration program is slated to discontinue in 2020, and the savings achieved due to the receipt of the enhanced Federal Medical Assistance Percentage (FMAP) are being directed towards a variety of State rebalancing initiatives and policy change designed to overcome identified barriers. Driven by a determination to further rebalance the long–term care system, the Demonstration team has developed a strategic map to serve as a visual guide for the strategic methodology for sustaining the long–lasting benefits that the MFP Demonstration brings to the long–term care population within New York State.
Strategic Goals
The overarching purpose of the strategic sustainability framework is to identify and implement policy and program changes resulting in long–lasting, sustainable benefits supporting community reintegration. As part of New York State´s development of this strategic framework, a strategic map was designed to help identify and target key focal points in sustaining the MFP mission during and after the Demonstration.
Stakeholder involvement, which forms the foundation of the Demonstration´s strategic framework, is crucial in identifying areas of potential policy and programmatic change. As noted in Chapter 2 – Stakeholder Involvement, the Demonstration conducts a quarterly stakeholder meeting in order to provide updates on current initiatives and to invite constructive suggestions and feedback from stakeholders regarding improvement opportunities and to brainstorm future potential initiatives.
Stakeholder feedback is then focused into the five different sections of long–term care that the Demonstration team has identified as the main areas of concern in sustaining the benefits of the Demonstration. These five areas of focus include housing, access to services, vulnerable populations, AT, and transition supports. Four goals guide policy and procedural changes for each of these areas of focus; those goals are:
- Self–Direction,
- Define and Implement Focused Approaches that are Culturally Competent,
- Develop and Implement a Communications Plan for the Public and Providers, and
- Quality Improvement, Quality Assurance.
Housing
The first area of focus is housing. There are four main focal points within the area of housing that will be addressed in order to sustain the benefits of community reintegration. After considering stakeholder input, as well as New York State DOH input, the first focal point is to support involvement of the Medicaid Redesign Team (MRT). This has resulted in the development and implementation of the Olmstead Housing Subsidy program discussed earlier in this plan. Other foci that were identified are training for capacity building, as well as the development of tools and resources. Efforts to address these needs are discussed in an earlier section of this plan.
Access to Services
The second area within the strategic plan is access to services. A focal point has been implementing the policy of No Wrong Door/Single Point of Entry alignment with the Transition Centers. New York State continues working to ensure that the policy of No Wrong Door/Single Point of Entry ties in smoothly with the Transition Centers currently run by the New York Association on Independent Living. Supporting caregivers of individuals who are receiving HCBS is another important implementation; this is occurring through the development and distribution of the caregiver guide, discussed earlier in this plan. Lastly, to help make more of the necessary services available, building the HCBS workforce is another key focal point in sustaining these benefits. New York State´s Workforce Investment Program (WIP) makes available funds through the State´s 1115 waiver for initiatives to retrain, recruit and retain healthcare workers in the long–term care sector. The WIP targets direct care workers, with the goals of supporting the critical long–term healthcare workforce infrastructure through retraining, redeployment, and enhancing skillsets. The WIP supports the expansion of home care and respite care, enabling those in need of long–term care to remain in their homes and communities and reduce New York´s Medicaid costs associated with long–term care.
Vulnerable Populations
The first focal group within the topic of vulnerable populations, is cultural vulnerability. The State will focus on reaching populations that may have less information on their choices for end of life care, due to cultural barriers. The second focal group are individuals with geographic vulnerability, meaning more rural communities who have less access to the public information being provided on long–term care options. The third focus, program target populations, speaks to the populations that are currently served by the program through the NHTD, TBI, and OPWDD waivers. The fourth focal group within vulnerable populations is the elderly with behavioral health needs or those supported through OMH or HARP services. The fifth focal group is veterans. The Demonstration has expanded its program to include these target populations.
Assistive Technology
Another major area of concern in supporting community reintegration and sustaining the benefits of HCBS is the assistive technology (AT) that will be used by the participants. AT can be employment related if the individual wishes to return to work, or housing related to help an individual function independently in their home. The State plans to sustain the availability of these different forms of AT to help promote self–management amongst participants. Not only do individuals need the appropriate AT to be available to them, but in most cases, they also need to be taught how to operate and maintain their equipment to ensure that it functions properly and efficiently. The State plans to continue to support the Justice Center´s TRAID program (described earlier in this plan) to continue to address these needs.
Transition Supports
MFP´s contract with NYAIL´s Transition Centers helps the State focus on the assistance people need during their transition back into the community, or once they are already back in a community setting. A focal point within the transition support area is employment. Giving individuals the opportunity to earn an income once they are back residing in the community can help sustain the benefits of community reintegration. Another concern is community preparedness training (e.g., what are the individual´s needs post transition, and what will they need to prevent a re–institutionalization). Do they know how to do essential daily tasks like bathe, cook, and take medication, among other things? NYAIL´s transition specialists assist each individual with the individualized community preparedness education that he or she may need. Along with the Transition Centers, there is also a Peer Outreach component to NYAIL´s contract with MFP. NYAIL will be focusing on promoting peer outreach to help inform and educate individuals still residing in facilities, as well as individuals who may be newly faced with making end of life care choices, about their options for HCBS. The last major concern within transition supports is legal services. For example, helping a relative obtain power of attorney on behalf of a loved one. The Transition Centers are aware of these concerns with regards to transition supports and sustaining the benefits of community reintegration and focus on addressing these concerns with individuals whom they assist.
|top of section 9.| |top of page|NYS MFP Strategic Map
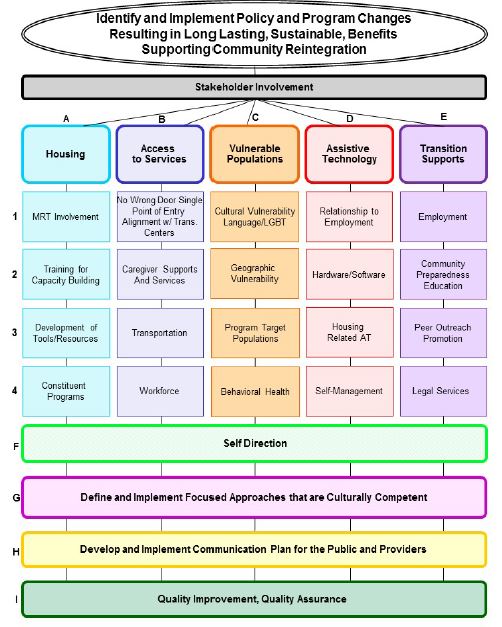
Follow Us