DOH REVIEW AND EXECUTIVE SUMMARY OF PPS PRIMARY CARE PLAN
- Response is also available in Portable Document Format (PDF)
On behalf of Albany Medical Center Hospital (AMCH) PPS´s Project Management Office (PMO), this comment is in response to and to ask for clarification on the IA´s recommendation for developing an action plan to implement Cultural Competency and Health Literacy (CCHL) trainings to partners.
In June 2016, our Cultural Competency & Health Literacy Committee (CCHLC) and the PMO developed a Cultural Competency Training Strategy to outline plans to implement cultural competency trainings across the PPS. This document explains identified training areas and a variety of methods for training delivery, as well as mechanisms for continuous feedback to shape future training implementation.
Feedback from partners during the development of the Strategy indicated that there was a lack of adequate introductory training on CCHL. Due to this feedback, initial steps of implementing the Strategy included providing introductory webinar training on CCHL, conducted by a PPS partner with expertise in this area. Participants of this training provided positive feedback and suggestions on the best method to disseminate this information to a larger audience in their organizations. AMCH PPS now plans to work directly with CCHL Champions, liaisons between AMCH PPS and each of our partner organization for CCHL–related activities, to implement this training in organizations´ using their preferred methods (LMS, in–person, etc).
In addition to introductory CCHL training, there are several other trainings that are currently underway or planned for implementation in 2017. Several partners are piloting our learning management system, HealthStream, with a cultural competency module that offers 2 CME/CE credits. Furthermore, we plan to offer Bridges Out of Poverty training opportunities in 2017, with the potential for a train–the–trainer program. This training was prioritized based on partners´ survey responses collected in October 2016. We are also gathering consistent themes from two rounds of Consumer Listening Sessions, where we hear about challenges and barriers to accessible and quality care from underserved patient populations. We take regular feedback from partners and Medicaid beneficiaries as guidance for prioritizing our future CCHL training implementation, as stated in our Strategy.
With stated explanations of implementation progress and immediate plans for 2017, AMCH PPS is seeking clarification on the logic and detail of the IA´s recommended "action plan to implement CCHL trainings to partners." This recommendation is somewhat contradictory to positive verbal feedback we received during the IA´s onsite visit on October 7th, 2016, as well as the Mid–Point Assessment Report that does not mention the deficiency in our CCHL Training Strategy implementation. We would appreciate clarification as to the necessity of this action plan and what elements they are looking for.
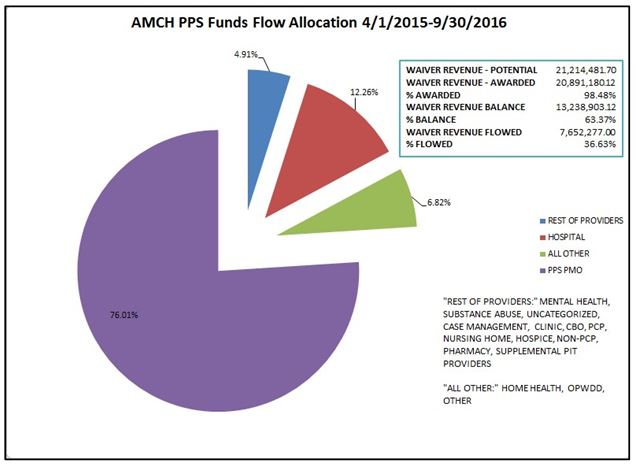
AMCH PPS would like to take the opportunity to provide additional clarifying information regarding the "PPS Progress Report" presented at the Project Approval and Oversight Panel (PAOP) meeting on October 7, 2016. The slide deck contained pie charts and other fiscal statistics for the period of April 1, 2015 through June 30, 2016. The link to the presentation can be found: http://www.health.ny.gov/health_care/medicaid/redesign/dsrip/2016/docs/2016-10-07_pps_progress_report.pdf.
The pie chart on page 4 of the "PPS Progress Report" demonstrates the total potential revenue available, earned revenue, dollars flowed, and the break–down of the funds flowed by provider type as of June 30, 2016. The first point of clarification is in regards to the PMO expense. While it appears that AMCH PPS has flowed 91% of the funds to the PMO, this is misleading. Much of this expense was spent on project implementation costs, such as IT and Clinical Integration consultants, project management software, and required workforce spending. For the same period of time, over 77% of what was designated as PMO expense was actually spent on project implementation, while approximately 13% was spent on administration. As of the quarterly report submitted September 30, 2016, and as shown in the attached pie chart, the percentage of cumulative partner payments rose to 24%, while project implementation and administration costs decreased to 63% and 13%, respectively.
Additionally, the percentage flowed to the Hospital provider type is also ambiguous. Two out of the three Hospitals that partner with AMCH PPS have large primary care practices that are combined with their Hospital contracts. These Master Project Agreements include many activities completed by the primary care practices, however, the funding for these deliverables are flowed solely to the Hospital.
Follow Us