DOH REVIEW AND EXECUTIVE SUMMARY OF PPS PRIMARY CARE PLAN
- Response is also available in Portable Document Format (PDF)
FLPPS
FINGER LAKES PERFORMING PROVIDER SYSTEM
FLPPS Response to 2016 Independent Assessor
Mid–Point Assessment Report
December 21, 2016
Opening Narrative
The Finger Lakes Performing Provider System (FLPPS) is the second largest Performing Provider System in New York State´s Delivery System Reform Incentive Payment (DSRIP) program with a regional span of 13 counties in the Finger Lakes Region and an awarded total valuation of $565,448,177. FLPPS has an attributed Medicaid population of 413,289 for valuation and 269,058 for performance, served by approximately 6,700 providers and 19 hospitals.
FLPPS selected the following 11 projects from the DSRIP Toolkit:
| FLPPS Project | Project Description |
|---|---|
| 2.a.i | Integrated Delivery System |
| 2.b.iii | ED Care Triage |
| 2.b.iv | Care Transitions |
| 2.b.vi | Transitional Supportive Housing |
| 2.d.i | Patient Activation |
| 3.a.i | Integration of Behavioral Health and Primary Care |
| 3.a.ii | Community Crisis Stabilization |
| 3.a.v | Behavioral Interventions Paradigm in Nursing Homes |
| 3.f.i | Maternal and Child Health |
| 4.a.iii | Mental Health and Substance Abuse |
| 4.b.ii | Chronic Disease Preventative Care |
FLPPS´s geographically expansive region, comprised of rural and urban areas, has presented a series of communication and collaboration challenges for project implementation and organizational work streams. Though FLPPS has taken several strategic and tactical steps to mitigate these challenges, [most notably the Naturally Occurring Care Network (NOCN) strategy described below, as well as targeted funds flow payments to Partners that began in DY2 Q2 for immediate, necessary work to achieve project speed and scale and clinical outcome targets] the Independent Assessor (IA) in its Mid–Point Assessment Report identifies correlated recommendations for the PPS.
As such, FLPPS respectfully presents its response to the DSRIP Independent Assessor´s Mid–Point Assessment Organizational and Project Recommendations in the following pages.
Organizational Recommendations
Partner Engagement
Recommendation 1: The IA requires the PPS to develop an action plan to increase partner engagement. The plan needs to provide specific details by each project for partner engagement.
FLPPS recognizes and remains committed to engagement of its large and diverse partnership spanning a 13–county region. At its formation, FLPPS established a unique role, a "Partner Relations Associate", with responsibility to educate, connect with and understand the varied Partners within a specific FLPPS Naturally Occurring Care Network (NOCN). FLPPS has five such NOCNs given the breadth and scope of the PPS´s geography:
- Finger Lakes (inclusive of Cayuga, Ontario, Seneca, Wayne and Yates Counties)
- Monroe (inclusive of Monroe County)
- Southeastern (inclusive of Chemung County and a portion of Steuben County)
- Southern (inclusive of Allegany and Livingston Counties, and a portion of Steuben County)
- Western (inclusive of Genesee, Orleans and Wyoming Counties)
As the measures for DSRIP move from reporting–focused measures in DY1 to outcomes–focused measures in DY2 and DY3, so too has FLPPS shifted its focus on Partner engagement. The role of the Partner Relations Associate has evolved from educating, connecting and understanding the varied Partners within a NOCN, to leading the identification of project implementation and outcome measure risks in each of the NOCNs and vetting possible solutions, as well as which FLPPS Partners are suitable for the execution of these solutions.
This vast engagement of FLPPS Partners, as well as associated flow of funds to this wide and diverse Partnership, is not easily captured in a central tool such as the Provider Import Table (PIT), as referenced by the IA in the FLPPS Mid–Point Assessment with regard to Partner engagement. FLPPS acknowledges the complexity of this information and submits its assessment of Partner engagement by project, with the caveat of the assumptions outlined below:
- Partner engagement, as defined for the Mid–Point Assessment, relates to the flow of funds to FLPPS Partner organizations
- Medicaid Analytics Performance Portal (MAPP), which appears to be a one hierarchy database that is based on Medicaid claims against all National Provider Identifiers (NPIs) under which an organization may bill, is the basis for the FLPPS Provider Import Table (PIT), appears to be the primary source that the IA referenced to measure FLPPS´s Partner engagement
- FLPPS believes that MAPP, and thus the PIT, is not reflective of "parent–child" organizational relationships
- The FLPPS region has many such "parent–child" relationships within its Partnership that FLPPS believes are not reflected accurately in the PIT and thus may have unintentionally skewed the Partner engagement measurement
Though there are many examples of FLPPS Partners that have "parent–child" organizational relationships, two prominent examples of this are the RU System Inc., d/b/a Rochester Regional Health, and the University of Rochester. Both of these Partner organizations participate in all 11 FLPPS projects. In the IA Mid–Point Assessment Report, Figure 5 (PPS Funds Flow Through DY2 Q2), both Rochester Regional Health and the University of Rochester are categorized as "Hospital". However, as demonstrated below, both organizations provide a wide spectrum of clinical services, encompassing a number of provider types. The constitution of these two Partner organizations is as follows:
Rochester Regional Health
- Practitioner – Primary Care Physician (PCP)
- Practitioner – Non–Primary Care Physician (PCP)
- Hospital
- Clinic
- Case Management/Health Home
- Mental Health
- Substance Abuse
- Nursing Home
- Pharmacy
University of Rochester Medicine
- Practitioner – Primary Care Physician (PCP)
- Practitioner – Non–Primary Care Physician (PCP)
- Hospital
- Clinic
- Case Management/Health Home
- Mental Health
- Substance Abuse
- Nursing Home
- Pharmacy
- Hospice
Additionally, both Rochester Regional Health and the University of Rochester have an Independent Practice Association (IPA) through which approximately 70 percent of regional primary care providers are employed or affiliated.
FLPPS recalculated Partner engagement based on additional information the PPS has gathered and maintained from its Partners, including the "parent–child" organizational relationships in the FLPPS region. FLPPS executed this recalculation using the following process and assumptions:
- Partner engagement, as defined for the Mid–Point Assessment, relates to the flow of funds to FLPPS Partner organizations
- FLPPS has collected and maintained a database of NPIs, aligned with "parent–child" organizational relationships in the FLPPS Partnership
- FLPPS also maintains data on the provider type for each "parent–child" organizational relationship in the FLPPS Partnership
- FLPPS aligned these "parent–child" organizational relationships within its Partnership
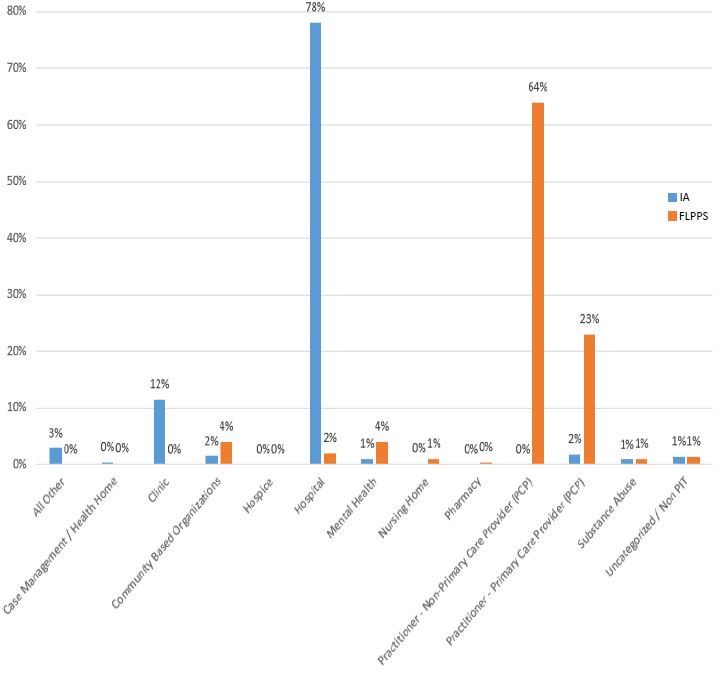
The following table demonstrates FLPPS´s recalculation of Partner engagement with consideration to the "parent–child" organizational relationships in the FLPPS region:
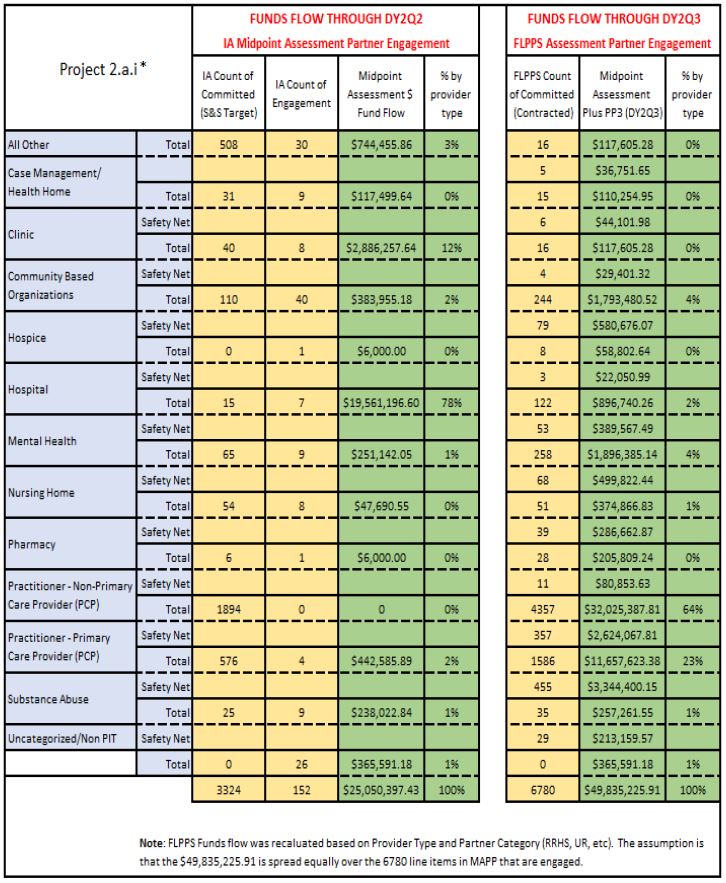
*Project 2.a.i provider type categories are reflective of IA Mid–Point Assessment Report, Figure 5 (PPS Funds Flow through DY2 Q2).
IA Mid–Point Assessment Funds Flow vs. FLPPS Assessment Funds Flow
Under the current FLPPS Partner Funds Flow model, FLPPS Partners are contracted for work by project through one or all of the following methodologies:
- Partner Contracts: Performance–based contracts for FLPPS Partners with contract metrics that are consistent by project and provider type; attribution–based, as consistent with VBP arrangements
- Patient Engagement Fund: Contract–based payment to FLPPS Partners who participate in specific projects to incent the collection and reporting of patient engagement data to FLPPS
- Targeted (Special) Contracting Arrangements: Contract–based payment to FLPPS Partners to mitigate identified project implementation and outcome measure risks
The following table outlines the applicability of each of the FLPPS Projects for the above–described methodologies in progress, unless noted otherwise:
| FLPPS Project | Partner Contracts | Patient Engagement Fund | Targeted (Special) Contracting Arrangements |
|---|---|---|---|
| 2.a.i – Integrated Delivery System | X | ||
| 2.b.iii – ED Care Triage | X | ||
| 2.b.iv – Care Transitions | X | ||
| 2.b.vi – Transitional Supportive Housing | X | X | |
| 2.d.i – Patient Activation | X | X | (future) |
| 3.a.i – Integration of Behavioral Health and Primary Care | X | X | |
| 3.a.ii – Community Crisis Stabilization | X | X | |
| 3.a.v – Behavioral Interventions Paradigm in Nursing Homes | X | (future) | |
| 3.f.i – Maternal and Child Health | X | X | |
| 4.a.iii – Mental Health and Substance Abuse | |||
| 4.b.ii – Chronic Disease Preventative Care | X |
FLPPS identifies project implementation and outcome measure risks, as well as mitigation strategies, through the following process:
- FLPPS Partners report patient engagement, by project, to the PPS monthly
- FLPPS analyzes patient engagement and provider engagement monthly against quarterly targets
- Where patient engagement or provider engagement is at risk of not meeting target, FLPPS prioritizes this risk for discussion at the NOCN level
- At the next convening of the NOCN Partners
- NOCN Partners identify barriers to implementation that are causing patient engagement and/or provider engagement to be at risk
- Where applicable, NOCN Partners identify providers who should be, but are not yet, engaged with FLPPS for that project
- FLPPS utilizes an internal process to recommend to the FLPPS governing bodies targeted flow of funds through the Patient Engagement Fund or Targeted (Special) Contracting Arrangements
The aforementioned process has been implemented in the Finger Lakes, Southeastern, Southern and Western NOCNs, and will be implemented in the Monroe NOCN in January 2017.
Expansion of the Patient Engagement Fund and Targeted (Special) Contracting Arrangement models continue to be considered along with ongoing project and outcome risk assessment. Additionally, FLPPS is developing a FLPPS Innovation Fund, intended to foster sustainable, high–value population health interventions beyond the FLPPS DSRIP project implementation model. FLPPS has identified both short– term (through DY3) and long–term (DY4 and DY5) objectives for the Innovation Fund:
Short–Term (through DY3)
- Rapid deployment of funds for initiatives designed to address gaps and move FLPPS performance metrics across the five NOCNs
- Measure and report achievements from FLPPS Innovation Fund initiatives to the Partnership to stimulate the recruitment and expansion of additional initiatives
Long–Term (DY4 and DY5)
- Create a sustainable funding structure to regionally move outcomes
- Create a learning collaborative designed to share information and leverage processes across the Partnership in support of the NYS DOH mandates around social determinants of health
- FLPPS´s achievement of DSRIP goals to move the Partnership to VBP and risk sharing arrangements, through demonstration
As FLPPS works through its overall funds flow strategy, the PPS is identifying which Partners are most central to impacting projects and clinical outcomes, and creating funds flow mechanisms to incent the work in DY3, DY4 and DY5. This work will result in action plans that will increase Partner engagement for all 11 FLPPS projects.
Cultural Competency and Health Literacy
Recommendation 1: The IA recommends that the PPS develop an action plan to roll out its trainings to workforce and partners with specific dates.
FLPPS has been developing an action plan to roll out the Cultural Competency and Health Literacy (CC/HL) trainings, detailed in the FLPPS CC/HL Training Strategy, to the PPS workforce and Partners. The FLPPS CC/HL Training Strategy, focused on addressing the drivers of health disparities, was approved by the FLPPS Board of Directors in July 2016 and submitted for DSRIP Independent Assessor review, thus completing the DSRIP CC/HL workstream Milestone #2: Develop a training strategy focused on addressing the drivers of health disparities (beyond the availability of language appropriate material).1 The FLPPS CC/HL Training Strategy was accepted by the IA in the FLPPS DY2 Q1 Achievement Value (AV) Scorecard. The FLPPS CC/HL Project Manager has partnered with the FLPPS CC/HL vendor, Coordinated Care Services, Inc. (CCSI), whose team includes a nationally recognized Director of Cultural and Linguistic Competence, Lenora Reid–Rose, to develop an implementation plan for the FLPPS CC/HL Training Strategy. The FLPPS CC/HL Training Strategy Implementation Plan, including target dates, will be finalized by January 15, 2017, and presented to the FLPPS Board of Directors for approval at the February 1, 2017, FLPPS Board Meeting. The FLPPS CC/HL Training Strategy Implementation Plan is a comprehensive action plan that proposes employing several different approaches to accomplish the goals expressed in the FLPPS CC/HL Training Strategy. The CC/HL Training Strategy Implementation Plan identifies that a number of Community Based Organizations (CBOs) in the FLPPS region have patient engagement and social determinants of health expertise, and that expertise will be used to train the FLPPS workforce and Partners on a contracted basis. In November 2016, FLPPS released a Request for Information (RFI) to 250 Partner organizations and included the RFI information in the FLPPS Newsletter. The RFI responses are being used to establish the CC/HL training resources available in the FLPPS 13–county region, including information related to the CBOs that are conducting the existing trainings or are able to create and deliver future trainings. In addition, activities to support the FLPPS CC/HL Training Strategy Implementation Plan are currently underway and the progress–to–date is as follows:
- One hundred and three FLPPS Partner organizations have completed the Organizational CC/HL Readiness Questionnaire. This questionnaire provided the FLPPS Team and CCSI with the information necessary to design a customized approach for each Partner organization to complete the more comprehensive Organizational CC/HL Assessment.
- Thirty–five FLPPS Partner organizations completed the comprehensive Organizational CC/HL Assessment. The FLPPS Team and CCSI are scheduled to review with each organization the results of their Assessment and will provide recommendations to each organization by December 31, 2016. The recommendations will be used by FLPPS´s Partner organizations to incorporate prioritized CC/HL practices into their organizational infrastructure, or enhance their existing CC/HL organizational practices, including CC/HL training plans for each organization.
- One hundred fifty–one FLPPS Partner organizations have reported to FLPPS the selection of a Cultural Competency Champion. This Champion is the liaison between FLPPS and their organization for CC/HL, and promotes CC/HL practices within their organization.
- A FLPPS CC/HL Resource Repository is listed on the FLPPS website and contains tools for both FLPPS Partners and Consumers. This is located at https://flpps.org/Workstreams/Cultural–Competency–Health–Literacy under "CC/HL Resources".
- FLPPS planned and completed two Partnership–wide learning sessions on two target CC/HL populations for the FLPPS region: In September 2016, "The Amish Lifestyle" with Allegany County Historian Craig Braack, and in December 2016, "The Refugee Population" with Jennifer Pincus, Program Coordinator for the Rochester Regional Health Office of Community Medicine.
- The FLPPS DY2 Partner contracts will include contract metrics for payment that ask Partners to report current CC/HL trainings taking place within their organizations.
- In Spring 2017, FLPPS will host its first annual PPS–wide Cultural Competency and Health Literacy Conference to discuss with the FLPPS Partnership the progress of the FLPPS CC/HL Strategy and the FLPPS CC/HL Training Plan, as well as best practices and success stories.
FLPPS submission of the FLPPS CC/HL Training Strategy Implementation Plan to the DSRIP Independent Assessor for review is anticipated for the DY2 Q4 reporting cycle.
Recommendation 1 (cont´d): FLPPS must also develop metrics to assess its most effective strategies to engage Medicaid members and the uninsured and report out on these strategies to the IA.
FLPPS recognizes the importance of engaging Medicaid members and the uninsured as the region participates in the DSRIP Waiver Program, and transforms the delivery system. To that end, Medicaid member´s and uninsured advocate´s input must be present in the governance model, and represented in the development of strategies that aim to improve care and Consumer satisfaction.
The FLPPS region is unique as it encompasses one of the few health systems planning agencies in New York State, the Finger Lakes Health Systems Agency (FLHSA). Throughout the DSRIP period, FLPPS and FLHSA have formally and informally partnered on initiatives that benefit the stakeholders for both organizations, and the region at large, including the administering of the Community Needs Assessment. One such initiative is the collaborative effort to address Consumer engagement and health disparities, in pursuit of overall improvement of health outcomes for regional Medicaid members and the uninsured. A significant benefit of this collaboration is FLPPS´s ability to leverage long–standing and well–established regional Consumer advocacy groups inclusive of: The African American Health Coalition, The Latino Health Coalition, and The Partnership for the Uninsured. This collaboration will also focus on an expanded advocacy network that spans the FLPPS 13–county region.
As a network, FLPPS will focus on assisting providers in providing culturally competent care that is patient– centered. This effort will be led by the FLPPS CC/HL Committee and the FLPPS Project 4.a.iii (Strengthen Mental Health and Substance Abuse Infrastructure Across Systems) Subcommittee, and supplemented by the activities of the FLPPS/FLHSA collaboration. As a first step, FLPPS, with CBO Partners, co–sponsored two community forums in February 2016, to gather information from Medicaid members and uninsured individuals about how they currently access care, and what they would like to see in a future system.
FLPPS is also mindful of the recommendations from the NYS Advocacy and Engagement Subcommittee under the VBP Roadmap. The Subcommittee has specifically guided the DOH and providers to consider:
- The creation of a member incentive program
- The development of Patient Reported Outcomes (PRO)
- Defining what the Medicaid member has a right to know about VBP
This guidance includes methods to activate members, educate around proper system utilization, engage in dialogue around health behaviors that impact outcomes, and provide information on preventative care, and disease management. The FLPPS Consumer Engagement Strategy incorporates this guidance and, in addition to the regional Consumer advocacy groups identified above, FLPPS will recruit a diverse group of individual Consumers – who reflect the breadth of experiences and opinions of the 13–county region – to small–group consumer education forums, community stakeholder forums, consumer focus groups (inclusive of Medicaid members and uninsured individuals) and for representation in FLPPS governance committees and workgroups.
Leveraging the expertise of our collaborating organization, FLHSA, and the subject matter experts from our Partner organizations, FLPPS will evaluate the effectiveness of our strategies and interventions through program design and "Plan, Do, Study, Act (PDSA)" tools. FLPPS will continue to document progress and include progress reports to NYS and the IA through the remainder of the DSRIP program.
FLPPS is highly involved in community–wide activities that address the social needs of FLPPS Consumers and specifically the social determinants of health through the following tables and initiatives:
- Invest Health, a project of the Robert Wood Johnson Foundation and Reinvestment Fund
- Re–Think Health Ventures, a project of the Fannie E. Rippel Foundation
- Rochester–Monroe Anti–Poverty Initiative (50% of the FLPPS attributed lives reside in Monroe County)
- Finger Lakes Regional Economic Development Council´s Pathways to Prosperity
Lastly, FLHSA is assisting FLPPS in identifying metrics of success to augment the prescribed measures under the Domain 1 Requirements in Project 2.d.i (Patient Activation) and the CC/HL workstream to assess the most effective strategies to engage Medicaid members and the uninsured. These metrics will be included in FLPPS´s Consumer Engagement Strategy. FLPPS´s submission of the FLPPS Consumer Engagement Strategy to the DSRIP Independent Assessor for review is anticipated for the DY2 Q4 reporting cycle.
Financial Sustainability and VBP
Recommendation 1: The IA recommends that the PPS create an action plan to address the assessment of its network partners for VBP readiness.
In accordance with the Financial Sustainability workstream Milestone #4, Develop detailed baseline assessment of revenue linked to value–based payment, preferred compensation modalities for different provider–types and functions and Managed Care Organization (MCO) strategy, FLPPS´s governing committee for finance, the Finance Committee, developed a robust VBP Readiness Assessment and Baseline Assessment for distribution to FLPPS Partners. This assessment was a first step in FLPPS´s action plan to address the assessment of its Partners for VBP readiness, and provide information on Partners´ needs for future education, support and implementation assistance as the Partnership transitions to a VBP environment. In August 2016, the NYS DOH announced that this milestone was delayed, indicating further guidance was forthcoming. Due to the pending guidance from the NYS DOH on Financial Sustainability workstream Milestone #4, and the large and complex nature of the FLPPS Partnership, the FLPPS Finance Committee held off on distribution of the VBP Readiness Assessment and Baseline Assessment until such time that guidance was received. FLPPS anticipates that this recently distributed new guidance will significantly increase FLPPS´s understanding of the NYS DOH´s definition of VBP readiness and development of VBP preparedness for FLPPS Partners. FLPPS looks forward to fulfilling Financial Sustainability workstream Milestone #4 under the new NYS DOH guidance.
Recommendation 2: The IA recommends the PPS establish a plan to further educate and support their partners´ moves toward VBP arrangements.
In its efforts to further educate and support its Partners´ moves towards VBP arrangements, FLPPS, as a newly formed 501(c)3 entity (Newco), has a unique challenge given the structure of the PPS´s Partners. FLPPS´s corporate members ("Members") are competing health systems (Rochester Regional Health and University of Rochester Medicine) that require careful consideration around sharing of VBP arrangement details in order to protect themselves from potential anti–trust–related implications. Due to this unique structure, the Members take precautions when being asked to incorporate other organizations, including FLPPS, into the preparation, risk discussions and contracting, between themselves and the MCOs during this move to VBP.
These limitations, in addition to the DSRIP Implementation Plan language that refers to MCO contracting which appear to be tailored to PPSs that are single health system entities, challenged FLPPS´s ability to execute the VBP milestones as they were written in the DSRIP Implementation Plan. With the additional and continued guidance received from the NYS DOH on FLPPS´s role in its Partners´ move toward VPB arrangements, FLPPS will continue to customize and tailor its VBP project plan to focus on educating and supporting the non–Member Partners on VBP readiness and preparation.
Despite the limitations of working across separate health systems, as described above, the work of DSRIP and FLPPS has enabled one regional IPA to negotiate and execute a VBP Medicaid contract with its largest MCO. This IPA, as well as others in the FLPPS 13–county region, are in discussions with other MCOs with regard to VBP Medicaid contracts. In addition, FLPPS has provided resources to support the integration of the newly formed Finger Lakes IPA (FLIPA) with DSRIP–related activities, specifically related to clinical and information technology population health management. The FLIPA, as well, is beginning discussions with an MCO for VBP contracting.
Furthermore, FLPPS DSRIP project implementation has yielded direct contracting between the aforementioned health systems and CBOs for services addressing social determinants of health, such as housing for discharged patients who have no other safe housing option. This collaboration between the health systems and CBOs on project 2.b.vi (Transitional Supportive Housing) is an early example of FLPPS´s ability to educate and support Partners´ moves toward VBP arrangements.
FLPPS will continue to convene key Partners in its network who are anticipated to enter into VBP arrangements with MCOs to establish reasonable community standards for such arrangements.
Since its inception, FLPPS has taken steps to educate and support Partners´ move toward VBP arrangements. These steps include:
- Targeted one–to–one conversations with CBO executives to engage and educate on potential roles for CBOs in VBP arrangements
- Provided encouragement and assistance to FLPPS Partners to attend the NYS DOH–hosted VBP Boot Camp
- Hosted a "Managing Risk in Value Based Payment" webinar with Francois de Brantes, Executive Director for the Health Care Incentives Improvement Institute (HCI3)
- Partnership–wide presentations in Regional NOCN Summits (March 2016) and FLPPS Full Partnership Summit (June 2016)
- Technical support for the DOH Office of Health Insurance Programs Request for Applications for the Community Based Organization (CBO) Planning Grant, which was awarded to FLPPS Partner S2AY Rural Health Network in the "Rest of State" category
- CBO asset mapping in preparation for the creation of a FLPPS CBO digital directory, which will connect CBO participation with DSRIP project implementation, population health and care management strategies
- Formation and meetings of the FLPPS CBO Advisory Council, whose charter is to advise FLPPS on CBOs´ participation in FLPPS implementation, preparation for VBP arrangements and the creation of Information Technology systems that include the social determinants of health
In addition, in September 2016, FLPPS formed a dedicated team to address strategic community initiatives and engagement, staffed by a director and senior project manager, chartered to support the FLPPS Partner CBOs by educating them on their vital role in the DSRIP program and FLPPS. This team will execute FLPPS´s plan to further educate the Partners´ move towards VBP arrangements.
Project Recommendations
Recommendation 1: The IA recommends the PPS develop an action plan to increase CBO and other partner participation in the 2.d.i (Implementation of Patient Activation Activities to Engage, Educate and Integrate the uninsured and low/non–utilizing Medicaid populations into Community Based Care) project.
FLPPS has taken steps to increase CBO and other Partner participation in the 2.d.i project through various outreach activities intended to increase Partner engagement. These steps include:
- Multiple Partner educational sessions and webinars during DY1 and DY2 that detailed outcomes of the 2.d.i project and information on CBO Partner´s roles in participation. These webinars, including one focused specifically on how to implement the 2.d.i project requirements as a CBO, are available on the FLPPS website at https://flpps.org/Projects/Patient–Activation and YouTube.
- FLPPS developed a Partner webpage that has detailed project information, past webinars, FAQs and registration information for future Patient Activation Measure (PAM) trainings. This webpage can be found on FLPPS´s main website: https://flpps.org/Projects/Patient–Activation.
- Actively participated in "Homeless Connect", a Monroe County initiative that brings a continuum of services together for the homeless in Rochester, including medical, mental health, housing, legal counsel, supplemental security income benefits and employment counseling. The FLPPS project 2.d.i Project Manager disseminated information on FLPPS projects, including 2.d.i and organization´s role in the Integrated Delivery System.
- Twelve PAM Train the Trainer sessions for 211 employees of Partner organizations (free for FLPPS Partners participating in project 2.d.i) in all five NOCN regions of FLPPS during 2016; multiple provider types, including CBOs, attended. These FLPPS–sponsored Train the Trainer sessions enable the FLPPS Partner to train their staff on:
- How to administer the PAM
- How to engage patients/clients using activation techniques
- Motivational interviewing
- Cultural competency and health literacy
- A FLPPS Patient Engagement Fund was established for the 2.d.i project in September 2016 that provides incentive funds to FLPPS Partners, including CBOs (20 Partner organizations received money through the FLPPS Patient Engagement Fund, 18 of those organizations are non–health system entities or CBOs) for patient engagement measures. FLPPS´s patient engagement outcomes positively increased as a result of these incentive funds, and FLPPS plans to continue with this model through DY2.
In tandem with the action plan described above, FLPPS´s funds flow strategy through DY3 is designed to support and provide incentive money to CBOs that provide outreach to project 2.d.i eligible populations. The FLPPS CBO Engagement Strategy identifies CBOs as an integral part of community navigation process and linking individuals to insurance, and recommends specific actions to engage and flow funds to CBOs for this work.
Recommendation 2: The IA recommends the PPS develop an action plan to educate CBOs on their vital role in the DSRIP program.
Given the importance of CBOs in the NYS DSRIP model for success, FLPPS has, since its inception, made a concerted effort to include CBOs and CBO input in the governance model, and design and implementation of projects. Under the definition of Community Based Organizations used in the VBP Roadmap2, FLPPS is actively contracted with 88 CBO Partners. Out of FLPPS´s 176 total contracts, these 88 CBO Partners equate to approximately 50 percent of the contracts extended to organizations in the network.
In September 2016, FLPPS formed a dedicated team to address strategic community initiatives and engagement, staffed by a director and senior project manager, to support the FLPPS Partner CBOs by educating them on their vital role in the DSRIP program and FLPPS. This team is responsible for the execution of the FLPPS CBO Engagement Strategy, which was approved by the FLPPS Board of Directors at the December 7, 2016, FLPPS Board Meeting3. The strategy is in accordance with the DSRIP Governance workstream Milestone #8: Inclusion of CBOs in PPS implementation. The FLPPS CBO Engagement Strategy details FLPPS´s plans to:
- Maximize the earning of all achievement values (AVs) tied to CBO–related FLPPS Implementation Plan milestones and tasks, recognizing the critical role of CBOs and community–based services
- Increase CBO engagement in the FLPPS network and inclusion in the FLPPS Integrated Delivery System
- Identify and execute outreach activities to augment the education of CBO executives, frontline staff, and boards on the value of participating in DSRIP and the Value–Based Payment Roadmap
- Develop community–wide quality standards for strategic activities to measure and demonstrate the value of social and human non–billable services to health outcomes
- Prepare CBOs to participate in VBP arrangements through a FLPPS–guided process, in conjunction with strategic community partners
FLPPS submission of the CBO Engagement Strategy to the DSRIP Independent Assessor for review is anticipated for the DY2 Q4 reporting cycle.
Recommendation 1: The IA recommends that the PPS develop an action plan for project 3.a.i (Integration of Primary Care and Behavioral Health Services) to identify and introduce opportunities for mental health professionals to partner with primary care providers, especially in more rural parts of their region. The data in this assessment indicates that FLPPS has only engaged five Mental Health and Primary Care Providers to date. The PPS´ success in implementing this project will not only impact its ability to earn performance funding but also High Performance Funds.
FLPPS has taken a number of steps to identify and introduce opportunities for mental health professional providers to partner with primary care providers, especially in more rural parts of the FLPPS 13–county region. These steps include:
- FLPPS designed and executed a gap analysis in October 2016 to gather data on which Primary Care Providers in the FLPPS region did not have integrated behavioral health services. These results allowed for targeted outreach, to date, to 30 providers. Continued outreach is ongoing to Primary Care Providers in rural areas to address barriers to integration and educate them on the 3.a.i project implementation.
- Multiple Partner educational sessions and webinars during DY1 and DY2 that detailed the FLPPS 3.a.i project goals and information on Partner´s roles in participation. Additionally, FLPPS has developed a Partner web page that has detailed project information and resources for Partners; this webpage can be found on FLPPS´s main website: https://flpps.org/Projects/Integration–of–Behavioral–Health–and–Primary–Care.
- FLPPS has pursued multiple waivers on behalf of the FLPPS Partners to address regulatory barriers that inhibit Primary Care and Behavioral Health Services integration. This has been met with limited success due to the complexities of implementing both Federal and New York State regulations within the boundaries of DSRIP.
- A FLPPS Patient Engagement Fund was established for the 3.a.i project in September 2016 that provides incentive funds to FLPPS Partners, including mental health professionals and primary care providers, for patient engagement measures. FLPPS´s patient engagement outcomes positively increased as a result of these incentive funds, and FLPPS plans to continue with this model through DY2.
Additionally, FLPPS submits below its assessment of the total number of mental health providers engaged as determined by a contractual relationship with the PPS and DSRIP funds received. FLPPS´s assessment demonstrates a total of 53 mental health providers engaged in contrast to the five mental health providers identified in the IA Mid–Point Assessment Project 3.a.i Partner Engagement table. FLPPS Project 3.a.i mental health provider sites:
| Mental Health Provider | Number of Mental Health Provider Sites |
|---|---|
| Anthony L Jordan Health Center | 4 |
| Arnot Health | 2 |
| Brown Square Health Center | 1 |
| CASA of Livingston County | 1 |
| Finger Lakes Addictions Counseling & Referral Agency | 1 |
| Finger Lakes Community Health | 7 |
| Franklin Educational Campus | 1 |
| Genesee Council on Alcoholism and Substance Abuse | 1 |
| Genesee County Mental Health | 1 |
| Highland Hospital of Rochester | 3 |
| Hillside Family of Agencies | 1 |
| Huther Doyle | 1 |
| Orleans County Department of Mental Health | 1 |
| Rochester Primary Care Network Inc | 1 |
| Rochester Regional Health | 19 |
| Steuben County Community Services | 1 |
| Strong Memorial Hospital | 5 |
| Trillium Health | 1 |
| Woodward Health Center | 1 |
| Total | 53 |
FLPPS believes that the action plan articulated above, in combination with the recalculation of the PPS´s engaged mental health and primary care providers, demonstrates an intentionally planned path to success for implementing project 3.a.i and the potential earning of performance funding and High Performance Funds.
__________________________________________________________________
1. Appendix Exhibit A: FLPPS CC/HL Training Strategy. 1
2. As defined by the Department of Health DSRIP A Path toward Value Based Payment: Annual Update, June 2016: Year 2, New York State Roadmap for Medicaid Payment Reform June 2016, page 42:
• Tier 1: Non–profit, non–Medicaid billing, community based social and human service organization (e.g. housing, social services, religious organizations, food banks)
• Tier 2: Non–profit, Medicaid billing, non–clinical service providers (e.g. transportation, care coordination)
• Tier 3: Non–profit, Medicaid billing, clinical and clinical support service providers (licensed by the NYS Department of Health, NYS Office of Mental Health, NYS Office for Persons with Disabilities, or NYS Office of Alcoholism and Substance Abuse Services) 2
3. Appendix Exhibit B: FLPPS CBO Engagement Strategy 3
Appendix
Cultural Competence and Health Literacy Training Strategy
Prepared by Coordinated Care Services, Inc.
June 2016
EXHIBIT A
Acknowledgements
Finger Lakes Performing Provider System, Inc. (FLPPS) in collaboration with the guidance and expertise of Coordinated Care Services, Inc. (CCSI) developed and shaped this Cultural Competence and Health Literacy (CC/HL) Training Strategy. In addition, the thoughtful input of the FLPPS Central Team, workgroups and community stakeholders vested in transforming our healthcare delivery system, such as Patients and Consumers (i.e. focus groups, community engagement forums and outreach), FLPPS Cultural Competence and Health Literacy Committee (regional key stakeholders with CC/HL expertise), Community Members, Faith and Spiritual Leaders, Faith–Based Organizations, Community–Based Organizations, and Partner Organizations, were instrumental in the development of this training strategy.
Table of Contents
Acknowledgements
Rationale for Cultural Competence & Health Literacy Training
Center of Excellence for Cultural Competence & Health Literacy
Appendices
APPENDIX A: Organizational Support
- Organizational Infrastructure Support Needed to Achieve Cultural Competency & Health Literacy
- Population Health Management & Analytics/Health Information Technology (HIT)
- Cultural Competence and Health Literacy Champion
APPENDIX B: Foundational Support
- Strategy for Engaging Community–Based Organizations (CBOs)
- Strategy for Engaging Faith and Spiritual Leaders
- Diversifying the Workforce – Supporting Career Ladders & Strategies for Engaging Colleges and Universities
APPENDIX C: FLPPS Stakeholder Engagement
- FLPPS Network Partners – Cultural Competence and Health Literacy Organizational Self–Assessment & Readiness Questionnaires Partner Themes
- Patients/Consumers – Community Stakeholder Forums
- Faith and Spiritual Leaders
- University of Rochester Center for Experiential Learning (CEL)
- Monroe County Medical Society
- FLPPS Central Team
APPENDIX D: Targeted Training Audience, Groups and Sectors
APPENDIX E Qualities of a Health Literate Organization
APPENDIX F: Social Determinants of Health
APPENDIX G: Cultural Competence & Health Literacy Educational Resource Repository
References
Executive Summary
Based on a comprehensive review of available research, including theory–based best practices, cultural competence and health literacy education intervention toolkits and resource books, and regional and national disparities reports, we have shaped a promising Cultural Competence and Health Literacy Training Strategy focused on addressing the drivers of health disparities, beyond the availability of language–appropriate material (Milestone 2 of NYS requirement for CC/HL).
While health equity remains to be the ultimate goal of the healthcare1 delivery system (AHRQ, 2014), health disparities in disease incidence and prevalence, health outcomes, access to care and quality of care continue to persist among the most vulnerable groups within the Finger Lakes Region. Health care only represents 10% of the contributing factors that lead to premature death. "Research provides clear evidence that residents of [communities] characterized by [social factors such] as persistent poverty, low educational attainment, exposure to greater levels of violence and environmental hazards, and lack of access to health care providers, nutritious foods, and exercise facilities generally have significantly poorer health outcomes than residents of [communities] that are not affected by such conditions" (Joint Center for Political and Economic Studies, 2014). Although improvements in the economy, social conditions or physical environment lend to making substantial contributions to achieving health equity, we recognize that a multimodal, collective impact approach is essential to reducing health disparities (Figure 3. Brach & Fraserirector, 2000):
Diverse Populations
|
+ | Cultural Competency
|
→ | Appropriate Services for Minority Group Members
|
→ | Improved Outcomes for Minority Group Members
|
→ | Reduction of Health Disparities |
FIGURE 3 Reducing Health Disparities Through the Implementation of Cultural Competency
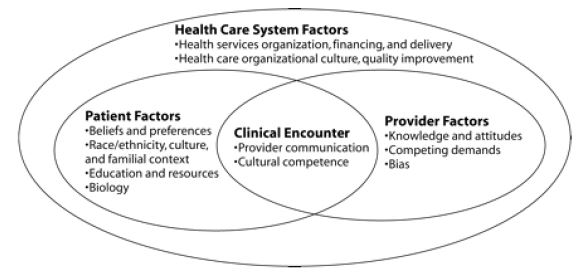
In addition, "although many health services researchers have addressed health disparities among vulnerable populations, there is [no universal framework] to follow for advancing a research agenda within the context of the health care system. [However], the key factors to understanding the root causes of health disparities [are] multilevel determinants of health, including patient/consumer factors, the clinical encounter, provider factors and health care system factors" (Kilbourne, Switzer, Hyman, Crowley–Matoka & Fine, 2006):
Am J Public Health. 2006 December, 96(12): 2113–2121
Finger Lakes Performing Provider System, Inc. (FLPPS) is committed to promoting patient voice and patient choice, while ensuring high value, equitable care. As our partnership works to build a robust integrated delivery system, we need to ensure that the network is grounded in attention to culture, language and health literacy, as these elements are essential to improving patient outcomes and eliminating disparities. Often community–based organizations (CBOs) are underutilized resources. However, we recognize them as vital ´community assets´, which have established trusting relationships with the communities whom they serve, offering/providing health and social services to many of our vulnerable populations on a daily basis. The ultimate goal is a health care network and workforce that can deliver the highest quality of care to every patient/consumer regardless of race, ethnicity, nationality, language, gender identity, socioeconomic status, physical, mental or intellectual ability, sexual orientation, and occupation. Within this system clinicians, other workforce groups, patients/consumers and communities employ a collective impact approach to address the drivers of health disparities, improve health outcomes and reduce costs.
Reducing disparities is identified as a priority in the U.S. Department of Health and Human Services (HHS) Disparities Action Plan, Healthy People 2020, HHS Language Access Plan, Centers for Medicare & Medicaid Services (CMS) Quality Strategy and key provisions in the Affordable Care Act (ACA). "[Cultural competence and health literacy training], related to race, ethnicity, language, disability, sexual orientation, and gender identity is critical for all members of the patient/consumer care team (CMS, 2015)." As a result, funding agencies as well as state and federal laws have all established standards to eliminate disparities and to achieve health equity through cultural competence and health literacy practices, policies and procedures.
With the increasing diversity of our population, and the interconnected barriers and challenges within our healthcare service delivery systems and communities, there must be a focused and sustained effort to create a system of care that is sensitive and responsive to different cultures, including the cultural attributes of priority groups and the varying degree of health literacy among the patients/consumers in our region. To that end, earlier this year, FLPPS developed a comprehensive Cultural Competence and Health Literacy Strategic Plan (Milestone 1 of NYS requirement for CC/HL) that sets forth a vision and outlines the steps that must be taken over the next four years to ensure that the redesign of the Medicaid service delivery system achieves the intended results.
During this process, FLPPS has paid particular attention to vulnerable groups experiencing significant health disparities within the Finger Lakes region. Key findings are recapped briefly below:
Disparities: Significant disparities exist among Black and Hispanic populations living in the Finger Lakes region, including higher rates of mortality and premature death.
Evidence of disparities also extends to potentially avoidable hospitalizations. People of color have substantially higher rates of Prevention Quality Indicators (PQI), regardless of type.
Social Determinants of Health: According to regional stakeholders, social determinants of health are key influences on the health of the Medicaid population and significant contributors to population health. To improve access to quality primary health, behavioral health and preventive health care, addressing social determinants of health and socioeconomic barriers to health will be essential in improving health care disparities and achieving greater health outcomes.
Behavioral Health: Behavioral health conditions are prevalent in the Finger Lakes region, especially among the Medicaid population. Most notably, the region has a higher prevalence of depression, schizophrenia, and stress and anxiety disorders than the New York State Medicaid population as a whole. Additionally, the Medicaid population in the Finger Lakes region has over twice the rate of Attention Deficit Hyperactivity Disorder (ADHD). The co–occurrence of chronic conditions and other significant health concerns among the behavioral health population introduces further complexity in ensuring this subset of the population has access to the range of services needed to reduce the use of acute services.
Perinatal Health: Perinatal health is also an area of concern for the region. The Finger Lakes region historically experiences higher rates of infant mortality than either New York State or Upstate New York. Explanations for this phenomenon have been difficult to ascertain, as the region demonstrates relatively low rates of teen pregnancy (except in Monroe and Chemung counties) and higher percentages of parents receiving prenatal care.
Populations with Special Health Needs: Based on the regional data reviewed we identified a number of populations with special needs, based on their increased risk of poor health outcomes, as a result of poverty, limited resources, inadequate access to care, limited education and language proficiency (Supporting Document: FLPPS CC/HL Implementation Plan Priority Groups Summary Report). These identified groups warrant particular focus: American Indian/Alaska Native/American Indians; Blacks/African Americans; Amish; Mennonite; Deaf and Hard of Hearing; Hispanics/Latinos; Homeless; Individuals that Identify as Lesbian, Gay, Bisexual, Transgender, Questioning (LGBTQ); Individuals w/Mental, Emotional or Behavioral (MEB) Health Disorders; Individuals with Physical, Intellectual or Developmental Disabilities; Mothers, Infant & Children; Refugees; and Rural Migrant and Seasonal Farmworkers.
Priorities: The CNA identified four primary gaps in the Finger Lakes region: (1) the need for an Integrated Delivery System (IDS) to address chronic conditions; (2) need for integration between physical and behavioral health; (3) need to address social determinants of health; and (4) the need to support women, infants and children.
County–Specific Priorities: In addition, the CNA also leveraged a wealth of information gleaned from existing county–specific planning activities, which identified a range of local findings relative to health and wellness priorities, as well as gaps in the healthcare service delivery system and related essential social and community supports.
This Cultural Competence and Health Literacy Training Strategy (Milestone 2 of NYS requirement for CC/HL) builds on the work of the strategic plan, taking a systemic approach and articulating training plans for clinicians and other workforce groups, hospitals/health care systems, patients/consumers, community stakeholders (including community–based organizations). The strategy outlined in the sections that follow is grounded in the work conducted over the past year by FLPPS in partnership and collaboration with Coordinated Care Services, Inc. (CCSI), which has allowed us to deepen our understanding of the populations served by the Medicaid system, conduct organizational provider/partner–level assessments, and to establish baseline measures to describe the current state of cultural competence and health literacy within our partnership. We have engaged with FLPPS Central Team and other external stakeholders, including:
- 36 out of 37 FLPPS Partners that completed the Organizational CC/HL Self–Assessment (representing a cross–section of FLPPS network partners, consisting of physical health, behavioral health and community– based organizations)
- 103 out of 200 FLPPS Partners that completed the Organizational CC/HL Readiness Questionnaire
- Patients/Consumers via focus groups and community forums
- Faith and Spiritual Leaders via individual and community stakeholder meetings
- University of Rochester Center for Experiential Learning (CEL)
- Monroe County Medical Society
- Community–Based Organizations (CBOs)
- The FLPPS CC/HL Committee that consists of healthcare and community based providers with expertise in cultural competency and health literacy practices
This process helped to identify training priorities, but also highlighted areas that must be taken into consideration while implementing the training strategy including: (a) the current lack of access to adequate training resources (including but not limited to culturally appropriate educational materials, incentives, easily accessible resource repositories or information, and infrastructural capacity), (b) time constraints, (c) the desire for multiple training methods and formats to accommodate different learning styles and preferences, (d) the need for audience–specific training topics (based on the interests of participants/audience for easy adoption and incorporation) and (e) the desire for a training process that includes interactive engagement. The feedback and input received from these stakeholder groups (Appendix C: Stakeholder Engagement) has been instrumental in shaping the cultural competence and health literacy training strategy outlined in this document.
In order to achieve DSRIP´s goal of improving clinical outcomes and reducing avoidable hospital use by 25% within 5 years the patients´ voice and patients´ choice must be incorporated in the transformation of the healthcare delivery system. A comprehensive cultural competence and health literacy approach is required to increase awareness and knowledge, build skills and competencies, and to drive practice change within our communities. As such, this training strategy is aimed at broad scale transformation across the health care system, organizations addressing social determinants of health through social services, communities, and patients/consumers – all essential elements in creating a robust integrated delivery system and network of care.
In the sections that follow, we outline a multi–year training strategy aimed at strengthening cultural competence and health literacy practices across the FLPPS DSRIP Projects, Partnership and Region. The strategy includes:
- The development of a Center of Excellence for the Cultural Competence and Health Literacy, to provide leadership, disseminate best practices, and support system–wide practice change;
- An outline of training topics tailored for each audience; and
- A plan for evaluating outcomes and assessing the impact of training efforts
Understanding that time constraints pose significant challenges to implementing an effective, system–wide training initiative, the strategy focuses heavily on forming the strategic partnerships needed to ensure that CC/HL approaches are not siloed efforts, but rather an integral component of all training, education and practice.
OVERALL TRAINING STRATEGY
The sections that follow outline a training strategy that includes the development of training plans for clinicians, focused on available evidenced–based research and addressing the health disparities of the priority groups described in our Cultural Competence and Health Literacy (CC/HL) Strategic Plan, as well as training plans for other sectors of the workforce on specific population needs and effective patient engagement approaches (Milestone 2 of NYS requirement for CC/HL). The transition to an integrated health care delivery system will be most effective and sustainable if it is accompanied by intentional efforts to reconstruct and build on the strengths of its workforce and workflows to a culturally competent and health literate state.
To be effective in our efforts to eliminate health care disparities and ensure equitable outcomes, it is important that our workforce understands the role each sociocultural factor plays in how we interact, engage and communicate with each other, as service providers, health care professionals, peers and individuals. As we partner with patients/consumers to deliver health care and social services, it is critical that we understand their unique perspectives and health beliefs to enhance the quality of care and service we provide. This can be accomplished only by embedding cultural competence and health literacy principles and practices into organizational infrastructures, and routine service delivery.
In developing our training strategy for strengthening cultural competence and health literacy, we acknowledge the value of developing our current workforce, organizational infrastructure, and strategic partnerships to support a more integrated and responsive health care delivery system. It is imperative that we train, educate and develop the current workforce and those entering the workforce, through sustained efforts, to enhance their knowledge, skills and capacity to effectively engage with and meet the needs of our diverse communities and patient/consumer populations.
"Just as place matters in health outcomes, relationships also matter in health outcomes. If relationships in a community are strong, its residents are more likely to engage collectively, through organized and intentional actions, to significantly influence public policies related to social determinants of health. And, in fact, the commitment of a core group of dedicated [key community stakeholders, including clinicians/providers, patients/consumers, spiritual/faith– based organizations, social service agencies, colleges/universities, cultural brokers, local residents, and community–based organizations], working closely together, can bring enduring change" (Joint Center for Political and Economic Studies, 2014). As a result, our training approach will emphasize inter–professional education that applies cultural and linguistic core competencies across all service delivery roles, responsibilities and functions (from front desk to organizational leadership and infrastructure). Addressing the keys to operational success includes high quality, improved customer satisfaction, better patient outcomes, and monitoring for continuous improvement through enhanced cultural competence. This will equip our organization, workforce, partners and patients with the knowledge, skills and resources that best support the delivery of culturally competent services.
In an effort to develop an effective training approach focused on addressing the drivers of health disparities, we have chosen to adopt and modify the conceptual framework of Horvat et al, as described in Cultural Competence Education for Health Professionals. This framework captures the core components of a cultural competence education intervention, such as: (1) training audience, (2) training approach, (3) training methods, (4) organizational support, 5) foundational support and (6) evaluation. Based on the FLPPS Community Needs Assessment (CNA), selected DSRIP Project and Associated Clinical Outcomes, FLPPS and Partner assessment data, and other evidence–based research addressing the identified priority groups experiencing health disparities within the Finger Lakes Region (Supporting Document: FLPPS CC/HL Implementation Plan Priority Groups Summary Report), we have identified the following audiences for cultural competence and health literacy training and implementation support:
- Organizations:
- Health Care Practices, Leadership and Staff2
- Hospitals/Health Care Systems, Leadership and Staff
- Clinicians:
- Primary Care (MDs, NPs, RNs, LPNs, etc.)
- OB/GYN (MDs, NPs, RNs, LPNs, Midwives, Doulas – non–clinical, etc.)
- Behavioral Health (LMSWs, LCSWs, Psychologists, Psychiatrists, Mental Health Therapists, Clinical Mental Health Counselors (MHCs), Credentialed Alcoholism and Substance Abuse Counselor (CASAC), etc.)
- Other Workforce Groups:
– Care Management (Care Managers, Care Coordinators, Community Health Workers, Peer Counselors, Patient Navigators, etc.)
- Patients/Consumers:
- Vulnerable Populations/Priority Groups
- Community Stakeholders:
- Spiritual and Faith–Based Organization Leaders/Members
- Community Members
- Social Service Agencies
- Colleges/Universities
- Cultural Brokers – "Influencers"
- Other Community Leaders/Members
Recognizing the diversity among the key stakeholders comprising the FLPPS Region and Network Partnership, this comprehensive training strategy will be adapted to meet the diverse backgrounds, educational levels, functions, learning styles and special needs of each of the targeted audiences. Training approaches, training methods and professional development opportunities will encompass cultural competence and health literacy core competencies through knowledge–based, attitudes–based, and skills–based training. These approaches will be supported by methods for evaluation and measuring success.
It is a critical element of FLPPS´s overarching strategy to reduce disparities in health care outcomes across the region. However, it is important to remember that, while critical, training is but one element. In order to have an impact on reducing disparities, the training must be coupled with incentives that recognize and reward service providers for making progress in addressing health disparities in the targeted performance measures (See Figure 1. Selected Performance Measures for FLPPS CC/HL Dashboard); through improvement in clinical practices/outcomes, as well as improved patient experience and health outcomes.
When implemented, this training strategy will provide a platform to formalize cultural competence and health literacy practices for FLPPS and its partner organizations, resulting in an integrated service delivery system where core cultural competency and health literacy concepts are incorporated and embedded as a part of routine service delivery practices.
|top of section| |top of appendix| |top of page|Rationale for Cultural Competence & Health Literacy Training
____________________________________________________________________________________________________________
Clinicians, other workforce groups, hospitals/healthcare systems and community–based organizations are delivering care and services to increasingly diverse populations. Social determinants of health contribute to disparities in health and health care among vulnerable populations/priority groups, particularly racial and ethnic minorities. These differences are driven by social determinants of health, for example, race, ethnicity, nationality, language, gender, socioeconomic status, physical, mental or intellectual ability, sexual orientation, and occupation (Appendix F: Social Determinants of Health). In addition, provider–patient relationships and barriers within the healthcare system are seen as potential causes of disparities in health outcomes and status (Betancourt, Green, Carrillo & Park, 2005; Smedley, Stith, & Nelson, 2003; Somnah, Arbelaez, & Cooper, 2002). These social and systemic factors influence the direct and indirect effects on our patients´/consumers´ health, wellness, outcomes, experience and satisfaction, such as:
- Access to care (e.g. locale, transportation)
- Availability of convenient, timely appointments
- Barriers/Challenges to seeking care (including the impact of discrimination, embarrassment, mistrust, racism, shame, stigma, classism)
- Expectations of care (including preferences for or against treatment options, including diagnostic or therapeutic procedures, medications, treatment plans)
- Language/Communication barriers (including translation/interpreter services/literacy levels)
- Variations in patients´ ability to recognize clinical symptoms of disease and illness
- Variations in patients´ perceptions, understanding and beliefs about disease and illness
Cultural competence and health literacy will improve knowledge, attitudes, behaviors and skillset in delivering services that ensures that disparities are eliminated and that all individuals receive equitable and effective health care services, especially vulnerable populations/priority groups currently experiencing poor health outcomes. The principles of valuing diversity, respecting individual differences, developing and institutionalizing cultural and linguistic knowledge, and adapting cultural competent and health literacy practice approaches can be created and applied at every level of an organization – board members, committees, administrators, leadership, partners, clinicians/practitioners, direct care support staff, front–line staff, patients/consumers and family members.
On an individual level, becoming culturally competent and health literate allows us to gain a deeper understanding of the social and cultural influences that affect the quality of services we provide and the quality of care patients/consumers receive.
On an organizational/systems level, becoming culturally competent and health literate helps to position an agency, organization or program as a role model and a leader within the community.
Formally incorporating cultural competency and health literacy practices, policies and procedures into routine service delivery results in social, health and business benefits for the entire Finger Lakes region:
| Social Benefits | Health Benefits | Business Benefits |
|---|---|---|
|
|
|
Source: American Hospital Association, 2013
The FLPPS Community Needs Assessment (CNA) completed early in the planning process identified four primary opportunities to aid in achieving DSRIP´s goal of improving clinical outcomes and reducing avoidable hospital use by 25% within 5 years: (1) an integrated delivery system to address chronic conditions; (2) integration between physical and behavioral health care systems; (3) addressing social determinants of health; and (4) supporting populations with unique needs.
This strategy aims to maximize our collective strengths to improve outcomes and reduce avoidable hospital use by educating and developing the current workforce – as well as those entering the workforce – through sustained efforts to enhance their knowledge, skills and capacity to effectively engage with and meet the needs of our diverse communities and patient/consumer populations. This training strategy provides a platform to formalize cultural competency and health literacy practices for FLPPS and our partner organizations, with the ultimate goal of creating an integrated service delivery system through:
- Supporting inter–collaboration between community–based organizations, health care providers and the surrounding communities to address social determinants of health;
- Supporting practice change at the organizational level to integrate cultural competence and health literacy into the organization infrastructure;
- Enhancing skills and knowledge among clinicians and other workforce groups; and
- Educating and empowering patients/consumers to self–manage their personal health and wellness
Conceptual Framework
____________________________________________________________________________________________________________
Eliminating racial and ethnic disparities within the healthcare delivery system is a complex, multifaceted process. A key cornerstone is assuring staff training supports the development of culturally competent clinicians, health professionals and other key stakeholders. To develop an effective cultural competence and health literacy training strategy focused on addressing the drivers of health disparities (beyond the availability of language–appropriate material) the framework needs to be inclusive of and responsive to the diverse backgrounds, educational levels, functions, learning styles and special needs of the groups being trained.
We utilized the work of Horvat et al, as described in Cultural Competence Education for Health Professionals, first published in May of 2014, as a guide in developing our cultural competence and health literacy training strategy approach. The researchers assessed the effects of cultural competence education for health professionals on patient–related outcomes via five studies. The five studies involved 337 health professionals (including general practitioners/clinicians, primary care teams and counselors) and 8400 patients (at least 3,000 patients represented diverse cultural and linguistic groups) in the United States, Canada and The Netherlands.
Although the quality of evidence was insufficient to draw generalizable conclusions, due to different educational intervention methods (scope, design, duration, implementation and outcomes selected), studies show great promise:
- 1:5 Studies showed improvement in care, which measured mutual understanding between minority patients and their doctors
- 1:5 Studies showed a change in health behavior among female patients whose counselors had received education; which were three times more likely to attend planned counseling sessions
The diagram below outlines our conceptual framework adopted and modified from the work of Horvat et al. This framework captures the core components of cultural competence education interventions: (1) training audience, (2) training approach, (3) training methods, (4) foundational support, (5) organizational support and (6) evaluation – which is key in measuring success, as well as advancing evidence–based research within the context of the healthcare delivery system.
Training Strategy – Conceptual Framework**
| Training Audience | Training Approach | Training Methods | Foundational Support | Organizational Support |
|---|---|---|---|---|
|
|
|
|
|
**Adapted from Horvat, L, Horey, D., & Kis–Rigo, J, 2014.
Finger Lakes Performing Provider System, Inc. (FLPPS) has chosen to use this modified conceptual framework as a guide in developing our cultural competence and health literacy training strategy approach outlined in this plan. This strategy will focus on improving the current performance within the FLPPS network, and harness the resources, knowledge and expertise within the community through training and professional development opportunities for service providers, including clinicians, other workforce sectors and key stakeholders. Trainings will be integrated and comprehensive, consisting of knowledge–based, attitudes– based and skills–based trainings.
Additionally, as we emphasize an integrated, collective impact approach this training framework incorporates strategies for developing organizational culture (Appendix A: Organizational Support) and foundational supports (Appendix B: Foundational Support) within FLPPS Central, as well as our partner organizations and communities. Each of these strategies will be essential in addressing the drivers of health disparities (Appendix F: Social Determinants of Health), by supporting careers ladders to diversify the workforce, engaging community–based organizations, faith & spiritual leaders and colleges & universities. These sectors will be necessary in embedding cultural competence and health literacy practices across the FLPPS DSRIP Projects, Partnership and Region to achieve DSRIP´s goal of improving clinical outcomes and reducing avoidable hospital use by 25% within 5 years.
|top of section| |top of appendix| |top of page|Training Audience
____________________________________________________________________________________________________________
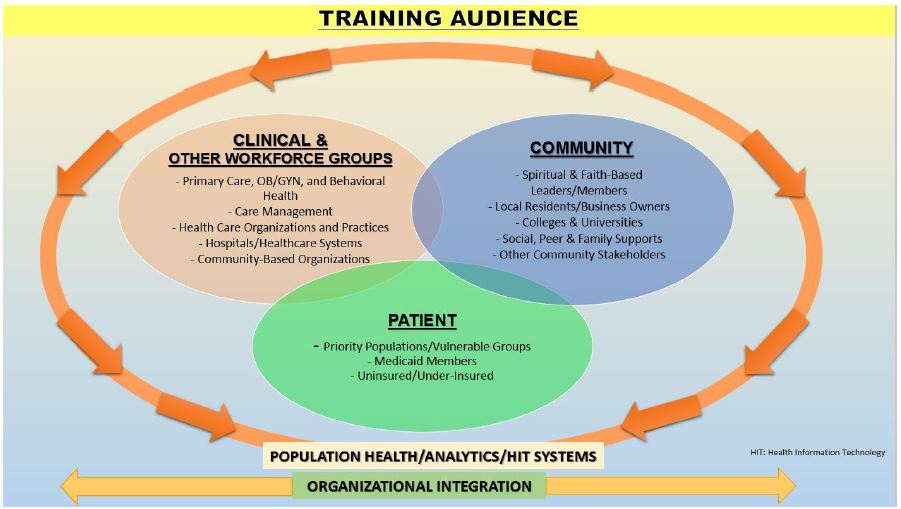
Bringing cultural competence and healthy literacy to fruition within the FLPPS network requires action by various sectors – clinical, community and patient. As noted above, FLPPS is a partnership representing a cross–section of physical health, behavioral health and community–based partner organizations – consisting of 19 hospitals, 6,700 health care providers, and more than 600 health care and community–based organizations in a 13 county region of Upstate New York (Allegany, Cayuga, Chemung, Genesee, Livingston, Monroe, Ontario, Orleans, Seneca, Steuben, Wayne, Wyoming and Yates counties). Given this breadth of partners, service providers and organizations, there is considerable diversity in the nature and scope of their roles, responsibilities and functions in delivering care.
Everyone involved in the service delivery of care, beyond clinical and health professionals, including other workforce sectors (i.e. non–clinical direct support/front–line staff – from the security officer to the information technology (IT) technician) can play a significant role in reducing disparities in disease incidence and prevalence, improving clinical and patient outcomes, and increasing access to high quality, equitable care (Collective Impact, 2015; The Council on Linkages Between Academic and Public Health Practice, 2014).
The goal of a comprehensive cultural competence and health literacy training and professional development strategy is to create a healthcare system and workforce that is equipped with the knowledge and skills to deliver the highest quality of care/service to every patient/consumer, community and population we serve, regardless of sociocultural factors (e.g., race, ethnicity, nationality, language, gender, socioeconomic status, physical, mental or intellectual ability, sexual orientation, and occupation, etc.). This can be accomplished only by embedding cultural competency and health literacy principles and practices into organizational infrastructures and routine service delivery through sustained efforts to eliminate health care disparities and ensure equitable outcomes.
It is important that all members of the service delivery system (Appendix D: Targeted Training Audience, Groups and Sectors) understand the role that culture plays in how we interact, engage and communicate with each other. Hospitals, healthcare practices and other partner organizations and healthcare/organizational leaders will be key in the training efforts for clinicians (See Training Methods) by leading the charge and being a role model. By tending to the needs of staff training and supporting that training with practice/organizational changes, the entire practice/organization focuses on achieving positive outcomes for patients/consumers, clinicians/health professionals and the infrastructure as a whole. To that end, cultural competence and health literacy training and professional development opportunities will be targeted and tailored for specific groups:
- Organizations:
- Health Care Practices and Staff3
- Hospitals/Health Care Systems and Staff
- Clinicians:
- Primary Care (MDs, NPs, RNs, LPNs, etc.)
- OB/GYN (MDs, NPs, RNs, LPNs, Midwives, Doulas – non–clinical, etc.)
- Behavioral Health (LMSWs, LCSWs, Psychologists, Psychiatrists, Mental Health Therapists, Clinical Mental Health Counselors (MHCs), Credentialed Alcoholism and Substance Abuse Counselor (CASAC), etc.)
- Other Workforce Groups:
- Care Management (Care Managers, Care Coordinators, Community Health Workers, Peer Counselors, Patient Navigators, etc.)
- Patients/Consumers:
- Vulnerable Populations/Priority Groups
- Community Stakeholders:
- Spiritual and Faith–Based Organization Leaders/Members
- Community Members
- Social Service Agencies
- Colleges/Universities
- Cultural Brokers – "Influencers"
- Other Community Leaders/Members
Training Modules
____________________________________________________________________________________________________________
In developing training curricula for clinicians, focused on available evidenced–based research addressing health disparities for particular groups, and training plans for other workforce sectors regarding specific population needs and effective patient engagement approaches, FLPPS has paid particular attention to the vulnerable populations/priority groups throughout the Finger Lakes region where significant disparities exists, reviewed available evidenced– based research and obtained the input of key stakeholders.
Research has shown that the key factors to understanding the root causes of health disparities [are] multi–level determinants of health, including patient/consumer factors, the clinical encounter, provider factors and healthcare system and organizational factors (Kilbourne, Switzer, Hyman, Crowley–Matoka & Fine, 2006; Like, Barrett & Moon, 2007). According to available evidence–based research addressing health disparities, better–designed studies are necessary to advance evidence–based research within the context of the healthcare delivery system. However, there is great promise in addressing health disparities through cultural competence and health literacy principles and practices to improve clinical and patient health outcomes. (Angelotti et al, 2015; Horvat et al, 2014; Like, Barrett & Moon, 2007; Goode, Dunne, & Bronheim, 2006; Kilbourne et al, 2006; Blasé & Fixsen, 2003; Brach & Fraserirector, 2000):
- 3 out of 9 cancer studies suggests that utilizing culturally relevant patient education approaches, designed with and tailored for the intended audience´s values, beliefs and preferred ways of receiving information, significantly increased behavior change
- 3 out of 8 diabetes studies suggests that the effects of culturally competent interventions reported significantly improved outcomes in terms of physiological measures associated with better long–term outcomes in diabetes
- effects of cultural competence education for health professionals on patient–related outcomes via five studies
- 1 of 5 studies assessing the effects of cultural competence education for health professionals on patient–related outcomes:
- showed an improvement in care, which measured mutual understanding between minority patients and their doctors
- showed a change in health behavior among female patients whose counselors had received education; which were three times more likely to attend planned counseling sessions
- Studies reporting on health outcomes showed a significant positive relationship between cultural competence policies at sites caring for children with appropriate use of preventive asthma medications and parent satisfaction with care
- The concept of liability – and specifically, of decreasing the liability of providers or organizations through cultural and linguistic competency – is showing some strong preliminary evidence
- Broader literature on physician communication documents providing language access services mandated by Title VI the Civil Rights Act of 1964 as a key factor in avoiding malpractice suits and managing risk
- An essential element of cultural competence is the capacity of an organization to involve patients, families and their communities systematically in designing, implementing and evaluating services, supports and resources
- Within one study, 10% increase in workforce recruitment and retention of diverse staff, particularly African American full–time staff, was associated with a 12% increase in the odds of clients receiving a physical exam
Using the available studies and the valuable input and feedback received from a cross–section of key partners and community stakeholders (Appendix C: Stakeholder Engagement) FLPPS has developed a CC/HL training strategy that includes integrated and comprehensive training modules, consisting of knowledge–based, attitudes–based and skills–based trainings as described below:
Knowledge–Based Training: Focuses on providing information such as introductions to cultural competence, health literacy, cultural humility, social determinants of health, cross–cultural communication and various health belief models and practices. "A key challenge for cultural competence is to clarify the relationship between specific knowledge about particular communities, and generic knowledge required in any clinical encounter at any time and with any/all patients, without resorting to stereotypes or a need for encyclopedic knowledge of many cultures" (Horvat, Horey, Romios & Kis–Rigo, 2014).
Attitudes–Based Training: Focuses on improving awareness of the impact of socio– cultural factors on patients´ values and behaviors, and how these affect care (Horvat et al, 2014).
Skills–Based Training: Focuses on learning communication skills with both patient and culturally specific communities. "Skill development is comprised of two subsets: (1) interpersonal skill development and (2) intrapersonal skill development. This training can teach interpersonal skills to help people work with others, such as advanced communication, negotiation or collaboration (e.g., shared decision making).
Additionally, an example is building skills to work effectively with interpreters. Training can also teach intrapersonal skills to help individuals cope with situations. This can include cultural self–assessment and reflection, mindfulness, deconstructing stereotypes and de–escalation (Horvat et al, 2014).
The table below outlines the training curriculum modules for core cultural competence and health literacy competency training areas. These modules have been modified and adapted using the Association of American Medical Colleges (AAMC) Tool for Assessing Cultural Competence Training (TACCT) (AAMC, 2005). This content addresses and expands upon the important domains identified by the Association of American Medical Colleges (AAMC), Institute of Medicine (IOM) and Georgetown´s National Center for Cultural Competence (NCC):
- A context for the training; common definitions of cultural competence, race, ethnicity, and culture; and tools for self–assessment
- An appreciation for the traditions and beliefs of diverse patient populations at multiple levels–as individuals, in families, and as part of a larger community
- An understanding of the impact that stereotyping can have on medical–decision making
- Strategies for recognizing patterns of healthcare disparities and eliminating factors influencing them through organizational processes, policies and procedures
- Patient–centered care (responsive to the individual patient preferences, needs, and values while insuring that patients´ values guide all clinical decisions)
- Equitable care (providing care that does not vary in quality because if personal characteristics such as gender, ethnicity, geographic location or socioeconomic status)
It is important to note that, while each of the training modules presented below have been tailored to each of our identified target audiences, groups and sectors, we will identify and utilize existing trainings (including those offered by partner organizations) that align with our training curricula (will make modifications as applicable).
| CULTURAL COMPETENCE AND HEALTH LITERACY CORE TRAINING AREAS | |
|---|---|
| ORGANIZATIONAL INFRASTRUCTURE (OI) (including Leadership and other staff) |
FOCUS AREAS |
| MODULE I (OI): ORGANIZATIONAL Assessment |
Willingness to assess the organizational gaps to achieving cultural competence and health literacy Creating a cultural competence and health literate strategic plan Identifying a champion for cultural competence and health literacy Allocating resources – financial and personnel to embed cultural competence and health literacy in all aspects of the organization Be willing to be transparent in activities and outcomes relating to the cultural competence, health literacy, and patient outcomes Workforce Diversity – Human Resources Recruitment, Hiring and Retention |
| MODULE II (OI): Cultural Competence – Rationale, Context and Definition |
Definition and understanding of the importance of cultural competence; how cultural issues affect health and health care quality and cost, and the consequences of cultural barriers Definitions of race, ethnicity and culture Describe own cultural background and biases Valuing the importance of diversity in health care and address the challenges and opportunities |
| MODULE III (OI): Value of Plain Language for your audience/target population (Plain Writing Act 2010) |
Techniques on how to identify, write and provide appropriate materials |
| MODULE IV (OI): National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care |
Understanding and valuing the CLAS standards Connecting the CLAS standards to the elimination of disparities Connecting the CLAS standards to delivering quality care and achieving equitable outcomes |
| MODULE V (OI): Making Meaningful Use of Data |
Understanding the role of health information technology and population health data management in service delivery, patient health outcomes and patient experience Understanding how to use data to enhance continuous quality improvement (CQI) processes Electronic Health Records – introduction and overview; benefits, and applications Understanding how to use data to address/prevent health care disparities among vulnerable populations within communities we serve Meeting the needs of diverse patient population through patient portals Enhancing the Team Approach to care with EHR systems Increasing communication between patient and providers through patient portals Learn how to assess, align and effectively integrate cultural competency and health literacy into the organization culture |
| MODULE VI (OI): Change Management |
Learn how to assess, align and effectively integrate cultural competence and health literacy into the organization culture |
| MODULE VII (OI): Aspects of Cultural Competence & Health Literacy |
Epidemiology of population health History of bias, stereotyping, discrimination, stigma and racism, including limited access to health care and education Deconstructing stereotypes – effects of assumptions, bias and stereotypes on service delivery Institutional cultural issues Understanding the impact of power and privilege Understanding the constructs of racism and prejudice Information on the history of the patient and their community Understanding the community, its assets, social determinants and the impact on health outcomes |
| MODULE VIII (OI): Socio–Cultural Context of Health Disparities; Health Disparities and Factors Influencing Health |
History of health–care design and discrimination – Factors underlying health and health–care disparities, both local and national Social determinants of health Collaborating and partnering with communities to eliminate disparities – through community experiences Partnering with Community Based Organizations |
| MODULE V (OI): Cross–Cultural Interactions |
Having Difficult Conversations – eliciting the patient´s social, medical history and preferences; negotiating and problem–solving Diagnosis, management, and patient–adherence skills leading to patient compliance Understanding the impact of bias and strategize ways to counteract bias Value the importance of the link between effective communication and quality care De–escalation – dealing with hostility and discomfort Working with interpreters Valuing the historical impact on racism Valuing eliminating disparities Valuing the concept of equitable outcomes Motivational interviewing processes – engaging, focusing, evoking and planning |
| MODULE VI (OI): Delivering Trauma Informed Care, Understanding Vicarious Trauma & Mindfulness |
Trauma Informed Care In Practice Adverse Childhood Events (ACEs) & Brain Development: The evidential basis for a trauma informed approach Principles of Trauma Informed Care: Introduction to the core principles of trauma–informed care: safety, trustworthiness, choice, collaboration, and empowerment. Trauma & Resiliency: Building resilience—the ability to adapt well to adversity, trauma, tragedy, threats or even significant sources of stress—can help our clients, and ourselves, manage stress and feelings of anxiety and uncertainty. Self–Care & Mindfulness: Vicarious trauma is a common occupational hazard for professionals working with people with a history of trauma. |
| ORGANIZATIONAL – CLINICIANS & OTHER WORKFORCE GROUPS (O–CLIN/OW) | FOCUS AREAS |
| MODULE I (O–CLIN/OW): Cultural Competence – Rationale, Context and Definition |
Definition and understanding of the importance of cultural competence; how cultural issues affect health and health care quality and cost, and, the consequences of cultural issues. Definitions of race, ethnicity, and culture, including the culture of medicine Discuss race, ethnicity, and culture in the context of the medical interview and health care Clinicians´ self–assessment, reflection, and self–awareness of own culture, assumptions, stereotypes, biases Describe your personal cultural background and biases Valuing the importance of diversity in health care and addressing the challenges and opportunities it poses |
| MODULE II (O–CLIN/OW): Aspects of Cultural Competence & Health Literacy |
Epidemiology of population health Patient/family–centered vs. physician–centered care: emphasis on patients´/families´ healing traditions and beliefs (for example, ethno– medical healers) Institutional cultural issues Health literacy, plain language, culture and communication are essential for anyone working in health information, professions, services and organizations Information on the history of the patient and his/her community of people |
| MODULE III (O–CLIN/OW): Understanding the Impact of Stereotyping on Service Delivery/Patient–Provider Relationships |
Mental Models & Worldviews Power and privilege Cultural humility History of stereotyping, including limited access to health care and education Bias, stereotyping, discrimination, and racism Effects of stereotyping on medical decision–making: Physician´s own potential bias; physician–patient power imbalance; physician effect on health disparities Eliciting patient preferences and respond appropriately to patient feedback about key cross–cultural issues. Elicit additional information about ethno–medical conditions and ethno–medical healers |
| MODULE IV (O–CLIN/OW): Socio–Cultural Context of Health Disparities; Health Disparities and Factors Influencing Health |
History of health–care design and discrimination Epidemiology of specific health and healthcare disparities Factors underlying health and healthcare disparities, both local and national Social determinants of health Collaborating with communities to eliminate disparities – through community experiences Partnering with Community Based Organizations |
| MODULE V (O–CLIN/OW): Cross–Cultural Interactions |
Having Difficult Conversations – eliciting the patient´s social, medical history and preferences; negotiating and problem–solving Diagnosis, management, and patient–adherence skills leading to patient compliance Valuing the impact of bias and strategize ways to counteract bias Value the importance of the link between effective communication and quality care De–escalation – dealing with hostility and discomfort Working with interpreters Understanding the historical impact of racism Valuing eliminating disparities Valuing the concept of equitable outcomes Motivational interviewing processes – engaging, focusing, evoking and planning |
| MODULE VI (O–CLIN/OW): Delivering Trauma Informed Care, Understanding Vicarious Trauma & Mindfulness |
Trauma Informed Care In Practice Adverse Childhood Events (ACEs) & Brain Development: The evidential basis for a trauma informed approach Principles of Trauma Informed Care: Introduction to the core principles of trauma–informed care: safety, trustworthiness, choice, collaboration, and empowerment. Trauma & Resiliency: Building resilience—the ability to adapt well to adversity, trauma, tragedy, threats or even significant sources of stress—can help our clients, and ourselves, manage stress and feelings of anxiety and uncertainty. Self–Care & Mindfulness: Vicarious trauma is a common occupational hazard for professionals working with people with a history of trauma. |
| MODULE VII (O–CLIN/OW): Shared–Decision Making |
Knowing how to seek the patient´s participation; helping patients explore and compare treatment options; assessing patient´s values and preferences; reaching a decision with patients and evaluating the patient´s decision (Cultural Activation Prompts) |
| HEALTH INFORMATION & DATA MANAGEMENT (HIT) | FOCUS AREAS |
| MODULE I (HIT): Learning Management Systems |
Orientation and technical assistance to Learning Management Systems (LMS) that houses training content and tracks completion of required training components across the regional workforce |
| MODULE II (HIT): Data Collection, Analysis and Management |
Engaging patients to share social, cultural and medical information Accurate collection and storage of data describing the ethnic and cultural attributes of the population of focus Accurate collection of the associated social determinants of health Data analysis, by race, ethnicity, and socio demographic factors, providing information to drive change |
| MODULE III (HIT): Performance Reporting |
Developing meaningful performance metrics Deploying PDSA cycles to continuous quality improvement |
| MODULE IV (HIT): Human Resources |
Assessing HR systems to ensure that CC/HL is appropriately incorporated into staff professional development and performance appraisal |
| PATIENTS/CONSUMERS (P/C) | FOCUS AREAS |
| MODULE l (P/C): Shared–Decision Making MODULE II (P/C): Self–Management of Health and Wellness |
Understanding the concept of shared–decision making Participating in decisions about own health outcome Knowing, understanding and accepting the decision made with your caregiver Reaching a decision with your care giver Understanding the concepts of health Understanding the concepts of health and wellness Understanding how and what drives health seeking behaviors Understanding the barrier to one´s health outcomes Knowing how to engage with one´s care givers and asking for help Working with one´s social support in getting help Knowing when one is not well and seeking care Knowing about preventive care resources Understanding diagnosis, treatment and documentation: knowing when to ask for help Knowing about health insurance |
| MODULE III (P/C): Cultural Activation Prompts |
Being cognizant of and aware of cultural strengths and cultural stressors and their impact on health outcome Being comfortable in expressing what matters most in your health care to those who provide care Knowing one´s own cultural cues Knowing one´s rights and demanding the services more appropriate to you |
| MODULE IV (P/C): Trauma and Mindfulness MODULE V (P/C): Self–Advocacy |
Adverse Childhood Events (ACEs) & Brain Development: The evidential basis for a trauma informed approach. Principles of Trauma Informed Care: Introduction to the core principles of trauma–informed care: safety, trustworthiness, choice, collaboration, and empowerment. Self–Care & Mindfulness: Learn techniques that can help you thrive despite life´s challenges. Knowing and understanding what self–advocacy is Knowing how to "speak up." Asking the right questions for you and your care Goal setting Sharing your goals with others Knowing and understanding the gaps between where you are and achieving your goals |
| COMMUNITY (C) | FOCUS AREAS |
| MODULE I (C): Stakeholder Engagement |
Understanding the cultural attributes and nuances of the population in the FLPPS Network Understanding the cultural attributes of priority populations Strategies for effective two–way communication and how to applying them to communicating with the population of focus Planning for, implementing and evaluating community forums with stakeholders to include patients Planning for, implementing and evaluating community meetings Use the PDSA model to engender success |
| MODULE II (C): Collective Impact: Developing Strategic Alliances to Address and Prevent Health Disparities |
Provide educational opportunities to FLPPS partners about the value of establishing strategic partnerships between community–based organizations and the healthcare system to address healthcare disparities Network partners understanding the nuances of the climate in which CBOs operate; how success is measured by both their customers/patients and metrics used to evaluate success CBOs as strategic partners – CBOs will be included in the framework of the modified learning collaborative and have the opportunity to present their organizations and the work they do, including illustrating client outcomes achieved. Providers will have the opportunity to engage with CBOs and employ strategies to eliminate disparities and achieve equitable outcomes |
| MODULE III (C): Community Hot Spotting |
Understanding the concept of "hot spotting" as it relates to health care cost and elimination of disparities – Knowing where the hot spots for priority groups exist – by NOCN Knowing and understanding the challenges and barriers to health and health care for "hot spotters" Using data to measure and drive decision making relating to the elimination of disparities within the hot spots Applying information technology to advance health |
Training Methods
____________________________________________________________________________________________________________
We recognize the value of addressing the drivers of health disparities (Appendix F: Social Determinants of Health) through a focused and sustained effort to create a system of care that is sensitive and responsive to the varying degree of cultures within the Finger Lakes region, including patients/consumers, communities, healthcare professionals and practices/organizations. These demographic and sociocultural differences have implications for the delivery of primary and specialized health care and highlight the need for clinicians/practitioners, healthcare systems and practices/organizations to be more aware than ever of how an understanding of their organizational culture and patients´/consumers´ culture will impact the care they deliver and those receiving the care delivered. Cultural competence and health literacy training and professional development opportunities alone are not all that is necessary to address the drivers of health disparities and poor outcomes. In order to have an impact on reducing disparities, the training must be coupled with incentives that recognize and reward service providers for making progress in addressing health disparities in the targeted performance measures (See Figure 1. Selected Performance Measures for FLPPS CC/HL Dashboard); through improvement in clinical practices/outcomes, as well as improved patient experience and health outcomes.
Given the considerable diversity in the nature and scope of the roles, responsibilities and functions among our network partner organizations and their staff (representing a cross–section of physical health, behavioral health and community–based organizations), we will utilize a multimodal, collective impact approach. This approach incorporates strategies for enhancing knowledge, skills and attitudes through professional development opportunities, developing organizational culture (Appendix A: Organizational Support) and foundational supports (Appendix B: Foundational Support) within FLPPS Central, as well as within our network partner organizations and communities. Training methods will consist of in–person and web–based approaches via train–the–trainer workshop series, modified learning collaborative, annual community stakeholder forums, bi–monthly community meetings, e– learning opportunities, cohort–based cultural competence and health literacy webinars, educational cultural competence and health resource repositories and technical assistance for partners to ensure appropriate application and operationalization. In implementing these methods, the following factors will need to be taken into consideration:
- Engaging and Activating Hospitals, Healthcare Practices and Other Partner Organizations and Leadership: Hospitals, healthcare practices and other partner organizations and healthcare/organizational leaders are key to ensuring that cultural competence and health literacy are embedded within the FLPPS network. "To reduce bias and increase diversity, [some] organizations are relying on the same [programs, practices, processes and interventions they´ve been using for the last 40 years. [However], such efforts make matters worse, rather than better" (Harvard Business Review, 2016). Serving as role models, organizations will be leading the charge in the training efforts for clinicians and other workforce sectors. By tending to the needs of staff training and supporting that training with organizational changes, the entire organization focuses on achieving positive outcomes for patients/consumers, clinicians/health professionals and the infrastructure as a whole. According to Georgetown National Center for Cultural Competence (NCC), all organizations should "have a defined set of values and principles, and demonstrate behaviors, attitudes, policies and structures that enable them to work effectively cross–culturally with [diverse patients/consumers, professionals and organization types]. They should also have the capacity to: value diversity, conduct organizational self–assessment, manage the dynamics of difference, acquire and institutionalize cultural knowledge, and adapt to diversity and the cultural contexts of the communities they serve" (Like, Barrett & Moon, 2007). The degree to which we can create the type of system–wide change needed to move our evolving integrated delivery system to a higher level of cultural competence will depend on the support and commitment of organizational leaders in setting expectations for their system, practice, or agency. FLPPS will continue working to develop strategies to activate leaders at this level (Appendix A: Organizational Support; Appendix E: Qualities of a Health Literate Organization).
- Use of Cultural Brokers and Other Less Traditional Training Mechanisms: Given the significant time constraints providers and organizations face, the ability to participate in traditional in–person training sessions will likely continue to be challenging. As such, the training strategy must incorporate a range of strategies to create opportunities for learning – large and small – in the course of daily practice. This may include maximizing e–learning opportunities, embedding key cultural competence and health literacy elements in other required training curricula, and the use of cultural brokers and/or community "influencers" to spread and sustain knowledge. Within the healthcare delivery system, cultural brokers have become an emerging approach to effectively addressing cultural differences in the goal to eliminating racial and ethnic health disparities (National Center for Cultural Competence, 2015). Cultural brokers are influential community members who serve as bridges, linkages and mediators between groups or persons of different cultural backgrounds. While the roles of cultural brokers vary, their intended goal is to strengthen the patient–provider relationship by supporting shared–decision making. In this capacity, cultural brokers can be instrumental in facilitating the communication needed to enhance the sharing of knowledge and development of skills, attitudes and behaviors.
- Ongoing Assessment of the Training Needs of the Network: It will be important to continue to stay abreast of trends in the health care industry and in population health to maintain training curricula that can arm the workforce and community stakeholders with the information, knowledge and tactics needed to accomplish the initiative´s goals.
- Understanding the Learning Process: Even if trainers are subject matter experts or have years of experience, there is still an opportunity to grow their expertise. The training strategy will need to allow for enough time for assimilation and practice of their new knowledge. In addition, implementation will incorporate a mentoring process whereby a seasoned trainer is paired with a newer one to help them grow their skills and competencies
Train–the–Trainer Approach
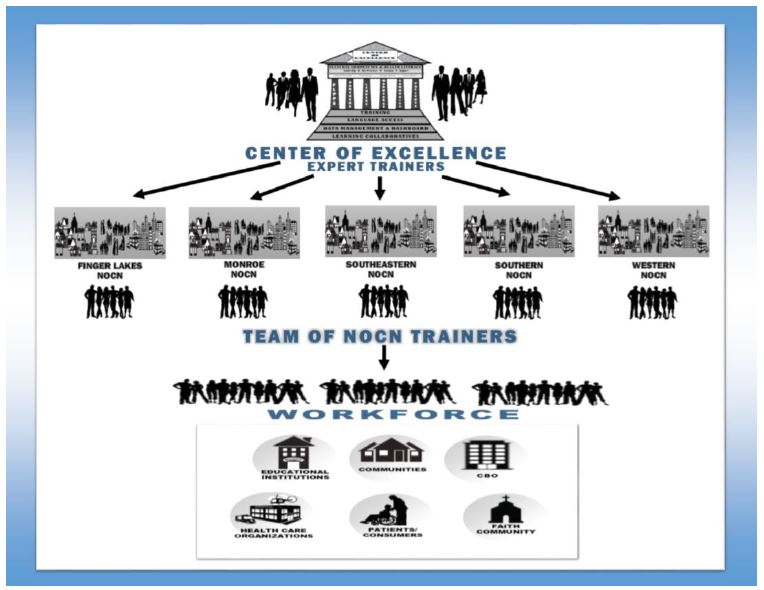
"Train– the– Trainer" (TTT) model involves "training a person or people who, in turn, train other people at their home agency," (Suhrheinrich, 2011). As applied to FLPPS, subject–matter experts will share their expertise with a group of potential trainers who are representative of the five Naturally Occurring Care Networks (NOCNs). These potential trainers will then use the information to instruct individuals from FLPPS partner organizations in their sub–region (NOCN).
FLPPS has elected to use this model because it is efficient and cost–effective in scaling quality skill–based training and professional development across the FLPPS Network. The model has been effectively used with multiple types of trainers and trainees. Potential trainers will be passionate about the subject matter, believe in social justice and equitable outcomes for all, and have some basic skill for effectively delivering any training. The TTT process will provide a framework where potential trainers will develop and strengthen subject matter expertise and the areas of cultural competence and health literacy and be able to effectively share this knowledge with stakeholders in their areas.
BENEFITS OF THIS APPROACH:
- Instead of relying on one individual or costly consultants to train and provide professional development to the network, FLPPS will build a team of trainers who are representative of the population in each Naturally Occurring Care Network (NOCN) and who appreciate the cultural nuances and idiosyncrasies of their region.
- Train–the–Trainer (TTT) curriculum will be developed in a way that allows it to be easily adapted and modified to reflect the nuances of the respective NOCN. This will allow for training goals to be accomplished in a shorter amount of time and for training content to be contextualized to address demographic characteristics and regional trends.
- FLPPS will set the tone for the network´s transformation through the training content and tactics. The (TTT) approach will standardize the content being offered to a large training audience, by providing the training team with essential tools for understanding what to teach and effective approaches on how to teach the content.
- The model will also allow FLPPS to strengthen and sustain knowledge within the workforce. Using Trainers from the region to train others in the region can also help form new alliances and teams.
PROCESS:
- Once established, the TTT model will be embedded in FLPPS Center of Excellence for Cultural Competence and Health Literacy.
- FLPPS will work with the CC/HL committee and NOCN representatives to define the requirements and to develop job descriptions for potential trainers.
- Based on the Medicaid population represented in each NOCN and the community needs, FLPPS will recruit several individuals from each NOCN, resulting in a core group of trainers. Potential trainers will also be representative of the identified priority groups in each region, and could include staff at CBO Partner organizations or from the community at large.
- FLPPS will create a budget to support the TTT model.
- Within the Center of Excellence structure a plan for evaluating the TTT programs and workshops will be developed and implemented.
- FLPPS and the Center of Excellence will use the evaluation results to foster a PDSA cycle to monitor and improve the trainings and their impact.
- Courses taught will be submitted for certification to the University of Rochester´s Center for Experiential Learning, so that participants completing the training are eligible to receive Continuing Medical Education (CME) credits as part of their professional development requirements.
Modified Learning Collaborative
As a complement to the training curriculum described above, FLPPS will support a broad scale transformation across the health care system via a modified learning collaborative. More specifically, we will utilize an adaptive model of the Medicaid Accelerated eXchange (MAX) series for achieving breakthrough improvements in practice, service delivery and equitable outcomes for our patients/consumers. Key components of the MAX series, include (NYSDOH, 2015):
- Multidisciplinary Teams (To Include CBOs)
- Clinical Inter–Professional Collaboration
- Applying Best Practices
- Utilizing and Yielding Subject Matter Experts (To Include CBOs)
Collaborative efforts have become necessary for organizations performing complex work with emerging technologies and rapidly changing environments. The FLPPS modified learning collaborative will create a forum for pooling resources and sharing ideas to promote large– scale change in a cost effective manner. Participants will receive intense, on–going technical support, learn from experts, and learn from and support each other. This approach will ensure understanding of the most effective ways of promoting the adoption, implementation and spread of evidence–based/community defined/best practices. These modified learning collaboratives will be designed as team–based, inter–professional forums in which information and experiences can be shared in an effort to incorporate cultural competency and health literacy in the system of care. Community–based organizations will serve as community assets, to provide guidance in identifying and validating effective interventions/best practices our respective vulnerable populations/priority groups. This will create the opportunity for our partners to learn from each other, trainers and subject matter experts, while setting and achieving bold goals for their own organization to advance the improvement of care, elimination of health care disparities and achieve equitable outcomes efforts.
GOALS OF THE MODIFIED LEARNING COLLABORATIVE, INCLUDE:
- Creating opportunities for intense and rapid learning.
- Broad scale transformation across the health care system driven by decisions supported by data.
- Utilizing and refining existing performance metrics that support the monitoring of health care disparities among the identified priority populations within the FLPPS region. Employ PDSA processes for continuous quality improvement.
- Opportunities for participating partner organizations to work with their peers to accomplish the shared goal of eliminating disparities and achieving equitable outcomes for patients/consumers, while setting and achieving bold goals for their own organization.
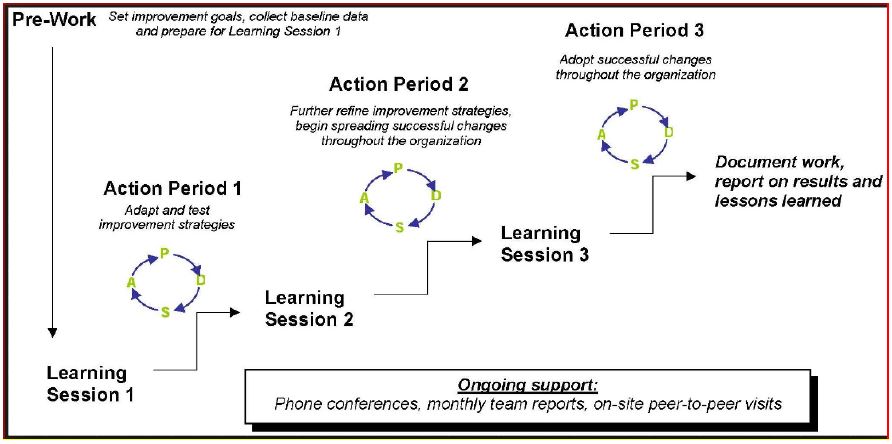
As defined by this modified learning collaborative model (modified and adapted from the Institute for Healthcare Improvement, 2003), the following are the expectations for participating partner organizations and their identified teams:
- There will be Modified Learning Collaborative groups from each of the (5) NOCN regions.
- Each Learning Collaborative will consist of no more than 5–6 partner organizations
- Partner organization teams of 3–4 (minimum) individuals will commit to participating (the FLPPS Patient–Centered Medial Home (PCMH) staff have had some success with this approach).
- Participating staff should represent individuals from the following roles – Administration, Professional, Para professional and Technical
- Participating organizations will select at least (2) performance metrics of focus within the scope of their services related to elimination of disparities
- Participating organizations will commit to the cultural competence and health literacy model
- Outcomes will be defined and agreed to within the framework of eliminating disparities and achieving improved client outcomes for priority groups
- Participating organizations will agree on collaborative benchmarks to meet Learning Collaborative goals
- Learning Collaborative measures will be integrated into the broader set of organizational and FLPPS performance goals
- There will be initial and ongoing participant training on the curriculum modules to support the achievement of outcomes
- Identify challenges, strategies and interventions for practice and system improvements
- Use a Plan–Do–Study–Act (PDSA) cycle to allow for integrating ongoing feedback and adapting tools and strategies to best suit the needs of the partner organization and buy– in from both staff and patients.
- Use data collected to measure progress and share results on a regular basis with the Learning Collaborative.
- Provide participants with a range of ongoing support options, including telephone conferences, list serves, assessments, monthly team reports, face–to–face sessions and onsite peer–to–peer visits
Community Stakeholder Forums and Meetings
Improving access to quality primary, behavioral and preventive healthcare is a continuous process that involves engagement with patients, communities, community stakeholders and network partners. Based on feedback from community members and partners FLPPS is committed to hosting community stakeholder forums and monthly community meetings. These community stakeholder forums and community meetings will serve as two–way communication methods to share information about services offered within the community, to provide updates on key community initiatives, to conduct coordinated patient and community health education, and to obtain feedback/input to refine strategies to support community building and improve access to high quality, equitable health care.
Patient/Consumer Advisory Councils
Patient/Consumer Advisory Councils will also serve as a two–way communication method. In addition to advising FLPPS on patient/consumer communication and marketing materials, the Patient Advisory Council will review patient/consumer grievances and offer input into FLPPS project workflows.
E–Learning
Research "emphasizes the importance of pursuing the development of innovative activities that help implement and assess cultural and linguistic competence in health care organizations and among health care professionals. Recommended activities include developing core competencies for health care professionals at all levels of education and raising awareness of and promoting adoption of the National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care" (Beamon, C.J., Devisetty, V., Fornica Hill, J.M., Huang, W., and Shumate, J.A., 2006).
FLPPS will need to be very creative in ways to engage clinicians in professional development opportunities regarding cultural competence and health literacy. Due to the varying demands and nature of their work, clinicians and other healthcare professionals are "notoriously busy and hardworking, and finding time for training is often problematic, especially for those whose roles in the hospital, clinic or practice are often invaluable and cannot easily take time off of work to attend trainings" (Efront, 2015). Even putting aside compensation – most primary care clinicians go home and work and finish charting from home for several hours on their electronic health records. Given how stretched for time they are, clinicians are apprehensive about attending face–to–face trainings. ´Grand Rounds´, the traditional format for training and education for clinicians and other workforce sectors, has experienced a decrease in attendance regardless of the topic. Clinicians and other workforce sectors have become extremely protective of their time.
For past several years, e–Learning has become one of the most popular method of training within the healthcare industry. Besides core medical training, e–Learning can be used to train clinicians and other workforce sectors in various focus areas regarding cultural competence, health literacy, specific population needs, effective patient education approaches, making meaningful use of data and organizational change management. In addition, "e–Learning can have a tremendous impact on the cost, convenience, time saved, reliability and accountability of [this] training strategy" (EFront, 2015). Clinicians will be receptive to this method of professional development. Accordingly, in implementing the CC/HL training strategy described in this document, FLPPS will ensure that opportunities for e–learning are readily available.
Cohort–Based Webinars will be audience specific trainings focused on various topic areas to increase participants´ knowledge, skills and attitudes to effectively address the drivers of healthcare disparities (beyond language).
Cultural Competence & Health Literacy Training/Educational Resource Repository will be developed to provide partners, patients/consumers and community access to culturally relevant and appropriate educational materials trainings, best practices, and resources for shared–decision making and self–management of health/wellness.
|top of section| |top of appendix| |top of page|Training Goals and Outcomes
This section outlines the training goals and outcomes for: 1) clinicians and other workforce sector goals, 2) organizational goals, 3) patient/consumer goals, and 4) community goals. Within each of these subsections, we detail the activities necessary to achieve these goals as well as the outcome indicators used to assess progress. It is important to note that goals and associated activities contained in this training strategy are both guided by and linked to the goals articulated in the Cultural Competence and Health Literacy Strategic Plan created earlier this year. We will work to create a crosswalk of the goals and objectives from both documents to ensure efficient implementation, synergy and alignment of project activities.
CLINICIANS AND OTHER WORKFORCE SECTORS GOAL: Contracted clinicians and other workforce sectors in the FLPPS Network will receive and have access to cultural competence and health literacy training plans.
Associated Activities:
- Collect, review and analyze information to understand training needs of the Network.
- Utilize information from the FLPPS Community Needs Assessment
- Conduct Individual Interviews, Community Forums and Focus Groups to better understand barriers and challenges to healthcare shared by patients/consumers, providers and community residents and other stakeholders
- Align DSRIP goals with training opportunities through gap analysis process to create and address needed training opportunities.
- Training modules: Incorporate collected information into trainings offered to the Network.
- Training methods: Trainings will address areas that impact health disparities and the producing of equitable outcomes for priority groups.
- Training modes: In–person trainings offered by locally trained experts (train– the–trainer model) and Web–Based training to incorporate flexibility.
- Obtain buy–in of Network leadership, workforce, and community stakeholders.
- Buy–in will be achieved through the following FLPPS activities:
- Outreach and Engagement
- Targeted communication (social marketing techniques, webinars, newsletters, community forums, etc.)
- FLPPS incentivizing cultural competence and health literacy activities completed by partners
- Buy–in will be achieved through the following FLPPS activities:
- Identify and position organizational resources.
- Through the organization´s CC/HL Strategic Planning activities, establish a budget line to accommodate the CC/HL training needs of the workforce.
- Determine what resources are currently available – human capital, infrastructure, materials/collaterals, meeting space, time, etc.
- Identify any possible impediments in the process and develop mitigating strategies to address and plan for these potential barriers. Determine if the mitigation strategies require a cost in additional resources.
- Through the organization´s CC/HL Strategic Planning activities, establish a budget line to accommodate the CC/HL training needs of the workforce.
- As part of the continuous quality improvement process, include data collection and evaluation of the trainings and the trainers through participant surveys.
Achievement Outcome Indicators:
- Contracted clinicians and other workforce Individuals will receive and have access to cultural competence and health literacy training plans.
ORGANIZATIONAL GOAL: Contracted hospitals, healthcare practices and other partner organizations will adopt and implement cultural competency and health literacy concepts and practices by DY5.
Associated Activities:
- FLPPS to obtain buy–in of Network leadership and workforce.
- Buy–in will be achieved through the following FLPPS activities:
- Outreach and engagement
- Targeted communication (social marketing techniques, webinars, newsletters, community forums, etc.)
- FLPPS incentivizing CC/HL activities completed by Partners
- Buy–in will be achieved through the following FLPPS activities:
- Partners will commit to sustaining cultural competence and health literacy concepts and practices.
- Present the CLAS standards to Network Partners as a guide to achieving cultural and linguistic appropriate services.
- FLPPS will cultivate Network Partners´ commitment to organizational cultural competence and health literacy efforts through their CC/HL strategic planning processes, to include:
- Assign a senior management level person to oversee the organizational development of culturally responsive and health literate practices and services.
- Identify a Champion within the organization for CC/HL.
- Invest in long–range fiscal planning to promote cultural competence and health literacy.
- Develop outreach strategies to improve access to high quality, equitable care.
- Review and update mission, vision and value statements to include cultural competence and health literacy principles.
- Review annually and develop policies and procedures to ensure culturally responsive organizational practices.
- Conduct an organizational cultural competence and health literacy self– assessment.
- Create a demographic profile of the community, patients/consumers, staff and Board.
- Develop culturally responsive and diverse staff recruitment, retention and promotion strategies.
- Manage the organizational training requirements and include annual training requirements for cultural competency, diversity and other trainings that focus on enhancing staff´s ability to demonstrate attitudes and behaviors that are culturally responsive.
- Establish practice and training guidelines for language accommodations.
- Develop cultural competence and health literacy governing boards, patient advisory committees and CC/HL Committee.
- Engage clients, staff, and community in the planning, development and implementation of culturally responsive services.
- Language Access Tasks: Plan for language services proactively and establish practice and training guidelines.
Achievement Outcome Indicators:
- FLPPS Contracted hospitals, healthcare practices and other partner organizations will complete the Organizational CC/HL Self–Assessment Tool.
- FLPPS Contracted hospitals, healthcare practices and other partner organizations will complete the CC/HL Readiness Questionnaire.
- FLPPS Contracted hospitals, healthcare practices and other partner organizations will establish cultural competence and health literacy policies and procedures.
- FLPPS Contracted hospitals, healthcare practices and other partner organizations will have a CC/HL Strategic Plan in place with an associated budget and individual responsible for carrying out the CC/HL related activities.
PATIENT/CONSUMER GOAL: Patients/Consumers in the FLPPS region will have access to education, training, resources and support to promote self–management of conditions, reduce health disparities and improve health outcomes.
Associated Activities:
- Establish and sustain FLPPS Patient/Consumer Advisory Councils:
- Identify and recruit a diverse group of individuals that reflect the community they reside in, represent the FLPPS priority/vulnerable groups, and are Medicaid Members or Uninsured.
- In addition to advising FLPPS on patient/consumer communication and marketing materials, patient/consumer grievances and input into project workflows, patients/consumers will receive education and training on:
- how to actively and successfully participate on Boards and Committees as consumers
- techniques for effective communication and self–advocacy
- self–management of conditions and health disparities affecting the FLPPS priority/vulnerable populations
- rights to language access
- new and existing healthcare and community initiatives/services focused on patients and consumers
- other Trainings as Identified
- FLPPS to develop a standard brochure for patient/consumers and partner organizations containing information educating individuals on self–management of conditions, health disparities affecting FLPPS priority/vulnerable populations and information pertaining to access to care (health insurance/navigators, links to local providers accepting patients, information on appropriate use of healthcare facilities and language access rights, etc.)
- In partnership with the Patient/Consumer Advisory Council and CC/HL Committee, FLPPS will host annual community stakeholder forums and bi–monthly community meetings in communities where access has been an identified concern, to educate and create meaningful opportunities for discussion and dialogue in a less threatening environment.
- Utilize targeted social marketing techniques as method to communicate critical health–related messages to the patient/consumers and community members:
- Written collateral (e.g. handbooks, pamphlets, infographics, brochures, manuals) – with LEP (Limited English Proficiency), LRS (Limited Reading Skills) and cultural accommodations
- Media materials – Videos, Radio Ad, Billboards, Social Media (in languages, beyond English, that are most prevalent in the broadcast region)
- Support patients/consumers by developing guidelines for informing patients´ choice in the selection of health plans, providers and other health care services, through interpersonal communication, decision coaching/motivational interviewing and decision aids, which take patient initial/informed preferences into consideration.
- Provide partner/patient evidenced–based and community–defined evidence education related to shared–decision making, patient advocacy, and self– management of health/wellness to create health equity and address health disparities among priority groups.
- Establish a CC/HL resource repository – housed on the FLPPS website, for providers/partners and patients/consumers to access culturally relevant and appropriate best and promising evidenced–based and community– defined evidence self–management practices and resources for shared– decision making and self–management of health/wellness, including culturally, linguistically, and health literacy appropriate patient educational materials.
Achievement Outcome Indicators:
- Patients/Consumers are recruited and have committed to participate in the Patient/Consumer Advisory Council.
- Community Stakeholder Forums conducted annually.
- A CC/HL resource repository will be housed on the FLPPS website.
- All patients/consumers and partner organizations will have access to the FLPPS standard brochure for patients/consumers available on the FLPPS website and at partner locations. FLPPS will establish social marketing methods to provide information and education on healthcare and health promotion to patient/consumer and the community.
- Shared Decision–Making training and information will be available via training workshops and the CC/HL resource repository on the FLPPS website.
COMMUNITY GOAL: Increase community awareness of health disparities and population health and utilize community feedback to refine strategies to improve access to primary, behavioral health and preventive health care.
Associated Activities:
- In partnership with the Patient/Consumer Advisory Council and CC/HL Committee, FLPPS will host annual community stakeholder forums and bi–monthly community meetings to share information about services offered within the community, provide updates on key community initiatives, conduct coordinated patient/consumer and community health education, and obtain feedback/input from patients/consumers and community members to refine strategies to support community building and improve access to high quality, equitable care.
- Identify and form strategic alliances with existing community resources, cultural brokers, community–based organizations, spiritual/religious leaders and colleges/universities.
- FLPPS will partner with partners/partner organizations to develop a standard brochure for patients/consumers and partner organizations containing information educating individuals on self–management of conditions, health disparities affecting FLPPS priority/vulnerable populations and information pertaining to access to care (health insurance/navigators, links to local providers accepting patients, information on appropriate use of healthcare facilities, etc.)
- Community trainings will include the following topics:
- Introduction to Cultural Competence, Health Literacy and Cultural Humility
- Definition of Race, Culture and Ethnicity
- Cross–Cultural Communication
- Mental Models & Worldviews
- Social Determinants of Health
- Having Difficult Conversations
- Shared–Decision Making
- Address/Prevent Healthcare Disparities Among Vulnerable Populations Within the Communities We Serve
- Value of Plain Language (Plain Writing Act 2010)
- Cultural Competence & Health Literacy Planning
Achievement Outcome Indicators:
- Key community stakeholders engaged in developing and implementing educational opportunities and communication strategies to address drivers of healthcare disparities (beyond language).
- Community Stakeholder Forums conducted.
- FLPPS will conduct community training.
Evaluation – Measuring Impact
The "continuous quality improvement (CQI) process is designed to raise the standards of the delivery of preventive, diagnostic, therapeutic, and rehabilitative measures to maintain, restore, or improve the health outcomes of individuals and populations" (AHRQ, 2012).
This Cultural Competence and Health Literacy Training Strategy (Milestone 2 of NYS requirement for CC/HL) will focus on improving the current performance of the healthcare delivery system within the FLPPS network, and harness resources, knowledge and expertise within the FLPPS region to reduce disparities and improve clinical outcomes. Trainings will endeavor to ensure that skill sets exist among key sectors of the community, including:
- Organizations:
- Health Care Practices, Leadership and Staff
- Hospitals/Health Care Systems, Leadership and Staff
- Clinicians and other workforce sectors groups
- Patients/Consumers
- Community Stakeholders
As a result, trainings must be evaluated to assess the impact on the intended audiences with respect to changes in knowledge, attitudes and behaviors, as well as the impact on reducing avoidable hospitalizations, eliminating healthcare disparities and achieving equitable outcomes.
The skill sets learned will aid us in achieving health equity by addressing the drivers of healthcare disparities through:
- Supporting practice change at the organizational level;
- Enhancing skills and knowledge among clinicians and other workforce groups; and
- Working to eliminate health disparities in disease incidence and prevalence, health outcomes, access to care and quality of care among the most vulnerable populations within the Finger Lakes region;
- Empowering patients/consumers to self–manage their personal health and wellness.
Measuring Success
The success of the Cultural Competence and Health Literacy Training will be measured by instruments created to answer the following questions:
- How and to what extent has FLPPS successfully delivered the proposed Cultural Competence and Health Literacy Training Strategy?
- How have participants/audiences/groups/sectors responded to Cultural Competence and Health Literacy Trainings [Pre–Test/Post–Test]?
- According to training audiences, their supervisors and their patients/consumers, how and to what extent have the knowledge, attitudes and practices changed while they are involved in the Cultural Competence and Health Literacy Training [Pre–Test/Post–Test]?
- How and to what extent have the changes in training audiences contributed to changes in patient/consumer health outcomes (including the clinical outcome measures used to assess progress for the initiative as a whole), access and utilization of services?
- What changes in patient/consumer outcome measures have occurred while trainees were involved in the various training opportunities?
- How do training audiences/participants account for these changes?
Training participants and their respective organizations will evaluate trainings to identify successful experiences, areas needing improvement, and to determine whether new skills, techniques, practices, concepts and information were effectively incorporated and implemented.
Performance will also be measured from the organizational perspective by examining progress in priority areas identified through the Cultural Competence and Health Literacy Self– Assessment. Organizations will establish a baseline of their level of cultural competence and health literacy on the Cultural Competence and Health Literacy Continuum through the Organizational Cultural Competence and Health Literacy Self–Assessment process, then assess their growth through comparative analysis with baseline and current state in DY4. Each assessment will be used to identify organizational successes, best practices and areas for improvement. Results will be displayed on FLPPS´s Cultural Competence website via Cultural Competence and Health Literacy Dashboards and Organizational Report Cards.
Finally, the impact of the training will also be assessed by monitoring changes in the performance measures identified for inclusion in the Cultural Competence and Health Literacy Dashboard as outlined in the Cultural Competence and Health Literacy Strategic Plan (See Figure 1 on the following page).
|top of section| |top of appendix| |top of page|Figure 1. Selected Performance Measures for FLPPS CC/HL Dashboard
| Selected Performance Measure for FLPPS CC/HL Dashboard | Description | Source | Reportable for DSRIP Project | Detail Required | Reference Page in Delivery System Reform Incentive Payment (DSRIP): Measure Specification and Reporting Manual Where Measure is Located |
|---|---|---|---|---|---|
| Age–adjusted preventable hospitalizations rate per 10,000 | To track the reduction in reliance on inpatient services by FLPPS region over time. | FLPPS/DSRIP Medicaid Spending on ER and Inpatient Services; Age– adjusted preventable hospitalizations rate per 10,000 – Aged 18+ years | 4.a.iii.; 4.b.ii | Calculated and displayed for each vulnerable population | 48 |
| Potentially avoidable Emergency Room Visits | To track the reduction in reliance on ER use by the FLPPS region over time | FLPPS/DSRIP Potentially Avoidable Emergency Room Visits | 2.a.i.; 2.b.iii.; 2.b.iv; 2.b.vi | Calculated and displayed for each vulnerable population | 25 |
| Follow–up after hospitalization for mental illness – within 7 days & within 30 days (composite of 2 measures) | To assess the success of the FLPSS region in providing continuity of care for those discharged from a mental health inpatient admission | FLPPS/DSRIP Follow–up after hospitalization for Mental Illness – within 30 days; Follow–up after hospitalization for Mental Illness – within 7 days | 3.a.i.; 3.a.ii; 3.a.v. | Calculated and displayed for each vulnerable population | 34 |
| Screening for Clinical Depression and follow up | To track success in addressing clinical depression needs when identified in screening | FLPPS/DSRIP Screening for Clinical Depression and follow–up | 3.a.i.; 3.a.ii; 3.a.v. | Calculated and displayed for each vulnerable population | 35 |
| Well Care Visits in the first 15 months (5 or more visits) | To track the success of the region in linking newborns to health services | FLPPS/DSRIP Well Care Visits in the first 15 months (5 or more Visits) | 3.f.i | Calculated and displayed for each vulnerable population | 35 |
| Initiation of Alcohol and Other Drug Dependence Treatment (initiation and 2 visits within 44 days; composite pf 2 measures) | To track success of system in engaging individual in Alcohol or Drug treatment when the need is identified | FLPPS/DSRIP Engagement of Alcohol and Other Drug Dependence Treatment (initiation and 2 visits within 44 days) | 3.a.i.; 3.a.ii; 3.a.v. | Calculated and displayed for each vulnerable population | 35 |
| Adult access to Preventive or Ambulatory Care 20 to 65 and older (composite of 3 measures) | To track the success of the region in linking adults to routine health services | FLPPS/DSRIP Adult Access to Preventive or Ambulatory Care – 20 to 44 years; Adult Access to Preventive or Ambulatory Care – 45 to 64 years; Adult Access to Preventive or Ambulatory Care – 65 and older | 2.a.i; 2.b.iii; 2.b.iv; 2.b.vi | Calculated and displayed for each vulnerable population | 27 |
| Patient experience survey (composite measure) | To track the success of the region in providing patients with an appropriate health care services experience (getting timely appointments, care and health information. | TBD–many items/measures exist within FLPPS/DSRIP (e.g., C&G CAHPS by PPS for uninsured) | Relevant to all, specific composite components reported to 2.d.i | Calculated and displayed for each vulnerable population | Multiple pages |
| Health Literacy (QHL13, 14 and 16) | To assess change in health literacy over time | FLPPS/DSRIP Health Literacy (QHL13, 14, and 16) | Recommended by CC/HL committee due to high impact on vulnerable populations | Calculated and displayed for each vulnerable population | 40 |
Communication Plan
FLPPS will create an approach to develop activities aimed at changing and/or maintaining behaviors of network partnership and our patients/consumers to ensure that the system continues to move forward in embedding cultural competence and health literacy. Influencing and sustaining behavior in a cost effective way is essential to FLPPS achieving its objectives towards eliminating health care disparities and achieving equitable outcomes. Once defined, the Communication Plan will help us confirm the following:
- Who are our constituents? With whom do we work?
- What behaviors are we trying to influence?
- What are the key messages?
- What are the vehicles to get this message across?
- How will we get the messages out?
- How do we go about it?
- How will we measure our success?
Center of Excellence for Cultural Competence & Health Literacy
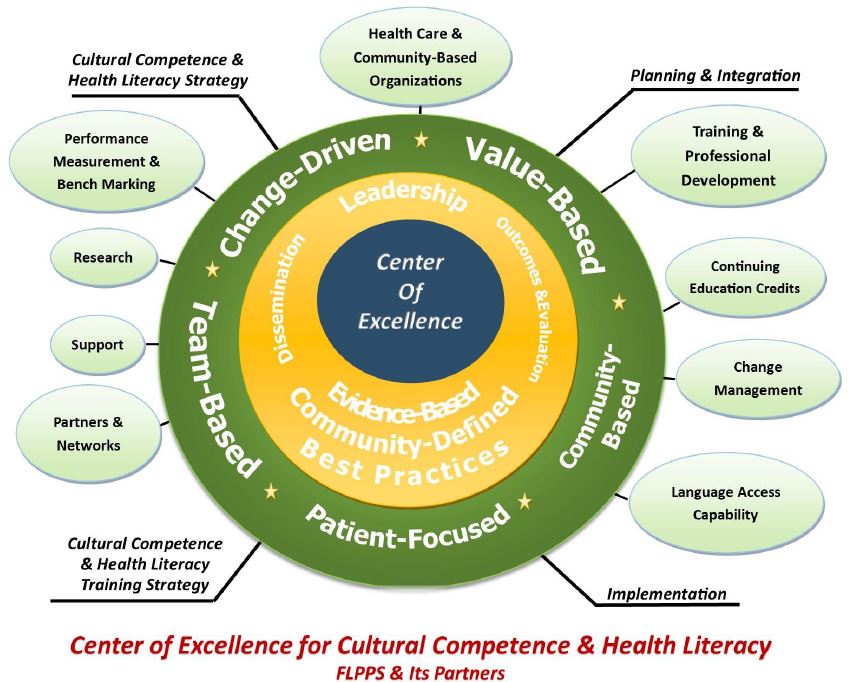
The FLPPS Network aspires to be the leader in removing barriers and providing solutions in cultural competence and health literacy for its Provider Network. This will be accomplished by building and sustaining a Center of Excellence for Cultural Competence and Health Literacy, to provide leadership, best practices, research, language access capability, support and/or training. FLPPS will use this platform to stay abreast of trends in the health care industry especially as it relates to healthy communities, eliminating disparities, achieving equitable patient outcomes and reducing avoidable hospital admissions by 25%. The investigation and dissemination of best practices in the delivery of culturally competent and health literate services to priority populations who are most affected by health disparities, and system and health outcome inequities will be central to the Center of Excellence´s focus.
Center of Excellence (COE) Principles:
- The FLPPS Network Center of Excellence will lead the effort in Delivery System Incentive Payment Program (DSRIP) cultural competence and health literacy proficiency, through contribution of new knowledge based on comprehensive research and compelling evidence regarding culture, race, ethnicity, and the impact of community social determinants that affect health outcomes in the FLPPS network.
- Disseminate obtained knowledge and competency advances in system approaches, clinical practice, program expertise and innovations that offer contributions to the elimination of health disparities and producing health equity for all patients and consumers. Including the following:
- Evidence–Based Practices:
- "The integration of the best research evidence with clinical expertise and patient values" (Institute of Medicine, 2000)
- "The integration of the best available research with clinical expertise in the context of patient characteristics, culture and preferences." (American Psychological Association, 2005)
- Community–Defined Evidence:
- A set of practices that communities have used and determined to yield positive results as determined by community consensus over time and which may or may not have been measured empirically but have reached a level of acceptance by the community.
- Best–Practices:
- A method, approach or technique that has been generally accepted as more effective to any alternatives because it has become a standard way of doing things and has produced results that are superior to those achieved by other means.
- Evidence–Based Practices:
- Apply the principles and practice of cultural competence and health literacy in health care and healthcare delivery.
The Center of Excellence (COE) will work to improve population health resulting in the elimination of health disparities and producing health equity for all, in particular our most vulnerable populations, through the following activities:
- Establishing and communicating the context and community definitions that will provide the blueprint for the transformation of the FLPPS Network
- Providing evidence–based and community–defined knowledge across various domains & technologies
- Identifying tools and frameworks to introduce and share knowledge and emerging best practices
- Adopting and internalizing ´best practices´
- Maintaining a repository of tools and resources
- Conducting Continuing Medical Education (CME) eligible training courses and professional development through University of Rochester Experiential Learning
- Building and supporting ´Train–the–Trainers´ model for delivering training and professional development in cultural competence and health literacy.
- Creating information technology (IT) infrastructure to support standardized data collection
- Utilizing Partner data to share performance metrics on a web–based Dashboard placed on FLPPS´ website
- Utilizing rigorous and credible processes to measure training participant attainment of knowledge/information and to ensure validity of results
- Documenting the processes while strengthening the credibility of the COE
- Training and assessment records
- Record keeping of procedures
- Privacy and confidentiality records
The Center will also promote and support the use of cultural brokering as a key approach to increasing access to and enhancing the delivery of culturally competent care (National Center for Cultural Competence, 2015). Cultural brokers are informal and influential community members who serve as bridges, linkages and mediators between groups or persons of different cultural backgrounds to effect change. In this capacity, cultural brokers are instrumental in facilitating a key method of two–way communication to enhance the sharing of knowledge and development of skills, attitudes and behaviors.
|top of section| |top of appendix| |top of page|Summary
Increasing proficiency in cultural competence and health literacy is not a stand–alone undertaking, but instead, will be integrated throughout FLPPS network – with varying levels of interdependencies among the different projects and workflows. Achieving better health outcomes will depend on how, when, where and to whom services are delivered, the identification and removal of barriers to care, and fostering ongoing collaborative relationships between leaders (organizational and community), partner organizations (including hospitals/healthcare systems and community–based), the community and patients/consumers.
To attain cultural competence and health literacy, clinicians, partners and other partnership staff, patients/consumers and the community must (Betancourt, Green & Carillo, 2002):
- Be made aware of the impact social and cultural factors on health beliefs and behaviors
- Be equipped with the tools and skills to manage social and cultural factors appropriately through training and education
- Empower patients/consumers to be more active partners in the medical encounter
We can achieve this through:
- Supporting the continued professional development of health care providers and community stakeholders in the areas of cultural competence and health literacy.
- Increasing our capacity to effectively educate our 400,000 Medicaid patients/consumers on how to navigate the health care system and become an active participant in their care. This can be accomplished by ensuring culturally and linguistically appropriate health education materials, health promotion and disease prevention interventions.
- Developing quality and performance measures that reflect the needs of priority groups experiencing healthcare disparities within the FLPPS region.
- Implementing the data collection systems needed to help us better describe and understand patient´s racial/ethnic backgrounds and language preferences. These data will also be used to allow FLPPS to monitor racial and ethnic disparities in health care delivery, for reporting to the public, and for quality improvement initiatives.
- Developing mechanisms for community and patient feedback and implementing quality improvement efforts that include culturally and linguistically appropriate patient experience and satisfaction methods.
APPENDICES
APPENDIX A: Organizational Support
To support the successful implementation of the CC/HL Training Strategy, we recognize that cultural competence and health literacy and its successes are dependent on additional supports for successfully addressing the Network´s training needs. Identifying Cultural Competence and Health Literacy Champions, gathering information from our Partners and workforce development are key aspects that aids and sustains infrastructural changes.
Organizational Infrastructure Support Needed to Achieve Cultural Competence & Health Literacy
Cultural competence and health literacy training and professional development opportunities alone are not all that is necessary to address the drivers of health disparities and poor outcomes. In order to have an impact on reducing disparities, the training must be coupled with incentives that recognize and reward service providers for making progress in addressing health disparities in the targeted performance measures (See Figure 1. Selected Performance Measures for FLPPS CC/HL Dashboard); through improvement in clinical practices/outcomes, as well as improved patient experience and health outcomes. The overall structure and functioning of the organization infrastructure must also be examined and modified to support training and professional development and utilization of new skills obtained. It is imperative that everyone in the healthcare organization from direct caregivers, service and support workers, supervisors, managers, and executive staff alike understand and develop a strong sense of empowerment gained through cultural competence and health literacy development. By tending to the needs of staff training and supporting that training with organizational changes, the entire organization focuses on achieving positive outcomes for patients/consumers, clinicians/health professionals and the infrastructure as a whole. In addition, addressing the keys to operational success will positively impact operational performance, including improved patient/consumer satisfaction; improving clinical and patient/consumer outcomes; and monitoring for continuous improvement through enhanced cultural competence.
Cultural competence and health literacy considerations are necessary to qualify programs and routine service delivery as high quality, equitable care. Through more culturally competent and health literate programs, services and treatment methodologies, we can achieve more expedient and better outcomes that can effectively reduce healthcare expenditures and eliminate health care disparities. Moreover, we can also raise the bar on overall consumer satisfaction as the levels increase for more priority groups. Lastly, as with any important initiative it is vitally important that we be able to measure and monitor their effectiveness over time in order to provide future direction and identify areas for continuous improvement
Cultural competence research suggests that [cultural competence trainings] focus largely on improving provider competencies, while agency–level and system–level approaches for meeting the needs of diverse populations are given less attention. As a result, cultural competence training for leadership is critical to promoting and sustaining systemic cultural competence within any organization. Key focus areas to assure sustainability include:
- Provide executive level support and accountability
- Foster patient, community and stakeholder participation and partnerships
- Conduct organizational cultural competence assessments
- Develop incremental and realistic cultural competence action plans
- Ensure linguistic competence
- Diversify, develop, and retain a culturally competent workforce
- Develop an agency or system strategy for managing staff and patient grievances
Cultural competence and health literacy requires that organizations:
- Have a defined set of values and principles, and demonstrate behaviors, attitudes, policies and structures that enable them to effectively work cross–culturally.
- Have the capacity to (1) value diversity, (2) conduct self–assessment, (3) manage the dynamics of difference, (4) acquire and institutionalize cultural knowledge, and (5) adapt to diversity and the cultural contexts of the individuals, families and communities they serve.
- Incorporate the above in all aspects of policy–making, administration, practice, service delivery, systematically involve consumers, families and communities.
Population Health & Analytics/Health Information Technology (HIT)
The current state of healthcare information technology is fragmented. Each provider has their own patient data management systems for patient information. What we need is a way to collect population health4 data/information from each of the provider systems, so we can aggregate and store consolidated information in a central Enterprise Data Warehouse and Care Management Platform.
Implementation of the Cultural Competence and Health Literacy Training Strategy will require continued population health & analytics/health information technology (HIT) investment and development, both within the FLPPS Central Office and across the FLPPS partner network. Key elements will include:
Identifying and deploying a learning management system (LMS) to house training content and to track completion of required training components across the regional workforce. This will be important to FLPPS in monitoring the spread of required training and education and assessing the degree to which provider partners are meeting core training requirements.
Providing training and technical assistance to provider partners to support the standardization and accurate collection and storage of data describing the ethnic and cultural attributes of the population they serve – as well as associated social determinants of health. This will not only require enhancing patient interaction skills across all front line and clinical staff, but as providers become more proficient at obtaining more detailed and comprehensive information about culture, health literacy, and social determinants of health, HIT systems will need to be modified to house and report on an enhanced set of information.
For example, provider EHRs will likely need to be modified to gather more detailed information on client ethnicity, gender identify, or social determinants of health so that this information is incorporated into the patient record and can be taken into consideration in the development of care plans and strategies. Moreover, it will be important that a subset of this information is reported to FLPSS Central to support regional analysis and quality improvement. To that end, standards will have to be developed to ensure consistency in definitions across providers so that reporting and analysis is meaningful.
Expanding performance reporting to allow for the analysis of key indicators by race, ethnicity and sociodemographic factors. A primary aim of the DSRIP initiative is to reduce ethnic and racial disparities in healthcare outcomes. However, at present, the amount of data available to support this type of analysis and reporting is limited. As outlined more fully in the CC/HL strategic plan, as DSRIP implementation continues, it will be critical to examine progress in key areas (e.g., reduction in the use of acute services, reduction in readmissions, timely connection to care post–discharge, and other quality indicators) not only for the region as a whole, but within those populations we know are most vulnerable and more likely to experience negative outcomes. However, this will only be possible if we are collecting these data consistently.
In addition to modification of provider EHRs, as expectations for CC/HL training are defined, it will be important for providers to assess current HR systems to ensure that CC/HL is appropriately incorporated into staff professional development and performance appraisal processes. As noted previously, if as a region we are going to make meaningful and sustained progress in reducing disparities, expectations related to CC/HL must be embedded into the operating practices of all provider organizations. In the same way that HR systems are designed to house data to ensure staff meet required credentialing criteria, it will be important to establish expectations and to assess and incentive improved performance in understanding in the area of CC/HL.
|top of section| |top of appendix| |top of page|Cultural Competence and Health Literacy Champion
The role of the Cultural Competence and Health Literacy Champion is a complex, but essential one. The Champion has a formal leadership role within the organization. The Champion understands and is committed to the Cultural Competence (CC) and Health Literacy (HL) goals and vision of the organization and is able to communicate that clearly with others. The Champion also understands the business imperatives for having a culturally and linguistically competent organization. The Champion is a representative for the leadership of the organization and exemplifies their commitment to making changes that will result in equitable health outcomes. The Champion is also a role model and practitioner of providing culturally competent care. They "walk the walk" and "talk the talk." They demonstrate and educate others about the principles of valuing diversity, respecting individual differences, and work to develop and institutionalize cultural and linguistic knowledge.
The Champion is charged with driving positive change in the organization. They overcome obstacles with creativity and resourcefulness; they persist in the cultural competence and health literacy mission. The Champion is charged with being a spokesperson for health equity concerns and is a passionate advocate that raises awareness for support and promotion of anti– discriminatory practices and strives to improve inclusiveness and understanding. The Champion consistently demonstrates and influences those around them to embrace and practice values such as respect and cultural humility in all interactions. The Champion negotiates all aspects of guiding change within the organization and with stakeholders, with passion and poise knowing that they are leading the charge to achieve the mission of providing appropriate and equitable care for all.
Standards: The Cultural Competence and Health Literacy Champion will adhere to all professional standards of care including confidentiality regulations, HIPAA, data security, and professional conduct.
Qualifications: The Champion is a skilled leader with three or more years of experience working in the organization. They are currently in a leadership role in the organization and are eager to take on the role of Cultural Competence and Health Literacy Champion. They must have superior professional qualifications for their current job and are highly respected for their professional skills and ability to innovate. The ideal candidate possesses strong negotiation, communication and collaboration skills. They must have a demonstrated ability to work effectively with teams.
Qualities of a Cultural Competence and Health Literacy Champion:
DESIRE– Desire to improve the FLPPS system of care to ensure that culturally and linguistically appropriate services are provided and result in eliminating disparities in health outcomes.
CLEAR VISION – Ability to see what can be accomplished and share that vision with passion.
CHANGE AGENT – Ability to help an organization transform itself by focusing on such matters as organizational effectiveness, improvement and development. This individual can be also from outside the organization.
PATIENT – They are patient yet persistent – they understand that change takes time.
COURAGE – They possess internal belief in the importance of the work that enables them to overcome any obstacle and not succumb to discouragement.
COOPERATION – Ability to work as a member of a team and foster collaboration and cooperation among diverse stakeholders; they are extremely approachable.
COMMUNICATION SKILLS –Ability to influence others without power, to communicate persuasively, to coach others, and to listen respectfully to the communication of others.
ASK TOUGH QUESTIONS – Help people think rather than telling them what to do.
RELIABILITY – The drive to perform every duty in a sincere and reliable fashion that fosters the trust and confidence of others.
CONFIDENCE – Confidence is not complacency – it is that feeling that with the proper effort goals will be achieved. Confidence comes from understanding the importance of the work, having training and expertise to share with others, and self–knowledge.
DISCIPLINE – Discipline includes possessing a strong work ethic, having desire to take on challenges, and continually strive to improve performance. It is the ability to remain calm and focused in difficult situations and to put in extra effort, when needed, to accomplish goals.
EFFORT – It takes tremendous effort on a daily basis to be a champion. It can´t be a sometime thing. Level of effort greatly affects level of success.
COMMITMENT – There is no way to achieve change within an organization without a high level of personal commitment on the part of leadership and the Champion. This commitment is seen in the passion one has for the work and the willingness to persevere in difficult circumstances.
|top of section| |top of appendix| |top of page|APPENDIX B: Foundational Support
__________________________________________________________________
Strategy for Engaging Community–Based Organizations (CBOs)
Often primary care providers, physicians and clinicians are not aware of the value and/or importance of collaborations with community–based organizations, including partnerships with programs and services available through local departments of health and human services, which are essential in transforming health care and practices into a more culturally competent and culturally responsive integrated healthcare delivery system. Community assets that complement the healthcare system, such as Community–Based Organizations (CBOs), Managed Care Organizations (MCOs), community stakeholders (e.g. faith & spiritual leaders, faith–based organizations, educational institutions) support patient/consumers in achieving their desired health outcomes in the own neighborhoods.
In collaboration with community–based assets, Finger Lakes Performing Provider System, Inc. (FLPPS) will support culturally relevant, culturally responsive community–based organization programming (e.g. diet, physical activity, and stress management, etc.) and facilitate educational opportunities for community–based organizations, clinicians, partners and other partnership staff, patients/consumers and the community. These opportunities at a minimum will include, but not limited to, the following focus areas:
- Patient Wellness/Self–Management of Illness
- Shared–Decision Making
- Patient Self–Advocacy/Empowerment (Cultural Activation Prompts)
- Patient–Provider Relationship and Service Delivery Approaches
- Patient Engagement/Patient Experience
To achieve productive and meaningful collaboration, FLPPS will engage CBO´s and the Network Partners by educating primary care providers, clinicians, partners and other partnership staff, patients/consumers and the community about the importance of cultural activation and cultural assessments of patients. Trainings and professional development will incorporate:
- Population health and how their work contributes to a healthy population;
- Acknowledging and understanding the culture of their patients;
- Understanding how illness is defined by their patients,
- Stratifying patients´ health outcomes to establish baselines for tracking health disparities and monitoring the effectiveness of interventions to achieve greater health outcomes.
With advisement from the Cultural Competence (CC) and Health Literacy (HL) Committee, Finger Lakes Performing Provider Systems, Inc. (FLPPS) will establish guidelines, and a Memorandum of Understanding (MOUs) and similar type of agreement documents to provide support to primary care providers and clinicians on best practices for establishing essential partnerships. In an effort to sustain these partnerships and collaborations, Finger Lakes Performing Provider Systems, Inc. (FLPPS) will conduct capacity and service gap analysis by hot spots and provider organizations feedback to aid in achieving significant and lasting social change.
Additionally, Finger Lakes Performing Provider Systems, Inc. (FLPPS) will host Modified Learning Collaboratives where community–based organizations (CBOs) will have the opportunity to present their organizations, the work they do, best practices and illustrate patient outcomes achieved, while engaging with primary care providers, clinicians, partners and staff from partner organizations, patients/consumers and the community.
|top of section| |top of appendix| |top of page|Strategy for Engaging Faith and Spiritual Leaders
A congregational health ministry is focused on achieving holistic wellness and disease prevention through education that empowers members and the surrounding community with personal responsibility, self–management, wellness, and stewardship.
Health ministries are an essential part of congregational life. They incorporate the values, beliefs, and practices of a faith community as components in motivating persons toward health and wholeness. Health promotion and religious beliefs are integrated into the normal cycles of life – birth, wellness, development, maturation, illness, and death – to celebrate life; to enhance coping, wholeness, and a sense of peace; and improve community well–being. Intentional contextual practices of caring honor a faith community´s sense of mutual dependence and foster persons´ ability to both give and receive care (Health Ministries Associated, 2012).
Functions of a health ministry as part of the faith community could include:
- Blood pressure screenings
- Coordinating blood drives
- First aid education
- CPR education
- Bereavement care and grief support
- Care calls to members with health issues/concerns
- Weight loss support and education
- Education on the relationship between faith and health
- Walking groups
- Organizing health fairs
- Connecting members with appropriate community resources
- Nutritional education
- Personal health counseling
- Visits made to shut–in or infirmed members through a homebound ministry
- Organizing and training health ministry volunteers
- Stress management classes (emotional and spiritual health)
- Speaking Health and Wellness from the pulpit
Process to engage and educate faith and spiritual leaders:
- Utilizing census data to identify the community´s religious beliefs
- Engage area cultural brokers in assisting with recruitment and offering complementary information
- Identify the Faith and Spiritual Leaders residing and serving within each Finger Lakes Performing Provider System, Inc. (FLPPS) Naturally Occurring Care Network (NOCN), to include faith community health advocates (e.g. Licensed Practical Nurses (LPNs), Dieticians, Physical/Occupational Therapists, Counselors, Social Workers, Athletic Trainers, Coaches, etc.). Faith–based representatives and/or health advocates should possess the following qualities:
- Good communication skills (health literacy)
- Intimate knowledge of the culture of the congregants or a willingness to learn (cultural competence)
- Passion for serving the needs of others
- Non–judgmental attitude
- Excellent listening skills
- Spiritual maturity
- Nurturing spirit
- Understanding of health–related stigma and stereotypes
- FLPPS will convene faith and spiritual leaders listening sessions/focus groups to collect information on the intersection of health/wellness with faith/spirituality.
- Describe what the goals of Delivery System Reform Incentive Payment (DSRIP) Program are and the benefits to their congregants. Explain crucial terms, e.g., health equity, disparities, social determinants, priority groups, cultural competence, health literacy, etc.
- Collect information regarding current health ministries in place and their activities
- Discuss the health challenges and concerns
- Obtain strategies from the Faith and Spiritual Leaders on the best ways to reach and influence their congregants regarding prevention measures, self– management, and wellness.
Diversifying the Workforce – Supporting Career Ladders and Strategies for Engaging Colleges and Universities
While we continue to experience an increasingly diverse population of patients and consumers, the number of racial and ethnic minorities in health care professions and health professional educational programs continues to be underrepresented. Studies suggest that in order to reflect the demographics of the population, the number of non–white physicians would need to be more than doubled (Beamon, et al 2006).
In the provision of an integrated healthcare delivery system through cultural competence and health literacy practice transformation, workforce diversification is essential to ensuring culturally competent and responsive services. Beamon, et al (2006) suggests that it is necessary to develop strategies to recruit, retain and promote staff diversity and leadership who are representative of the demographic characteristics of diverse patients, consumers and communities served at all levels of an organization.
A diverse health care workforce will help to expand health care access for the underserved, foster research in neglected areas of societal need, and enrich the pool of primary care physicians, (clinicians, and other health professionals), managers and policymakers to meet the needs of a diverse populace (Cohen, et all, 2002).
We know that health care providers representative of the patient´s cultural group are more sensitive to cultural nuances and can relate to the experiences of the population. Developing a diverse health care workforce will improve services to cultural groups, as well as engage more people in the workforce at a time when it is difficult to recruit qualified employees.
As Cohen and colleagues noted, "The recruitment of racial and ethnic minorities into the educational pipeline of the health professions is, of course, what determines not only their ultimate representation in the workforce but also their influence on the educational process itself." They identified four practical reasons for attaining greater diversity in the health care workforce:
- Advancing cultural competency and health literacy;
- Increasing access to high–quality health care services;
- Strengthening the medical research agenda; and
- Ensuring optimal management of the health care system (Cohen et al, 2002).
How then can we facilitate the entrée of underserved and vulnerable populations/priority groups into the healthcare workforce given the many compelling reasons for doing so? While there is currently no concerted strategy in the FLPPS region to attract and develop a health care workforce as diverse as the communities we serve, there are many steps that may be taken to do so. The goals of the FLPPS network can provide the impetus for developing collaborations between schools, colleges, the workforce development system, and area employers to create a pipeline into careers in health care as illustrated in the following diagram "Pipeline to Careers in Health Care." Young people from impoverished communities, immigrant, farmworker, and refugee populations, and other priority groups, may never know about or consider the myriad of careers in healthcare unless conscious efforts are undertaken to expose them to these opportunities. These efforts are critical in order to fill the pipeline with potential employees for the health care jobs of the future.
The concept of creating a "Pipeline to Careers in Healthcare" is simple. FLPPS partners, through their community education efforts, will engage with youth from priority groups in their early years of career exploration starting in grade school on into high school. As the youths mature they may engage with an adult mentor who works in the health care industry, the workforce development system, enter school–to–work collaborative programs that engage them with the health care workforce or connect them to college study in a health care field. Community colleges provide the groundwork for advancing to four–year degree programs, and attainment of advanced degrees. Collaborating with the educational institution´s U.S. Department of Education´s TRIO funded programs will be essential in supporting students to be successful in their educational experience. TRIO programs are designed to identify and provide services for individuals from disadvantaged backgrounds. TRIO includes eight programs targeted to serve and assist low–income individuals, first–generation college students, and individuals with disabilities to progress through the academic pipeline from middle school to post–baccalaureate programs. Once employed in health careers, employers support career development ongoing training, tuition assistance and continuing education opportunities.
While no single partner can provide all services, training and professional development, the partnership between FLPPS providers, schools and educational institutions, the workforce development system, and area employers is critical to accomplishing the goal of successful entry into health careers.
The diagram below depicts multiple routes and options that may be utilized to prepare and engage people from vulnerable groups for success in building careers in health care and advancing within their chosen area.
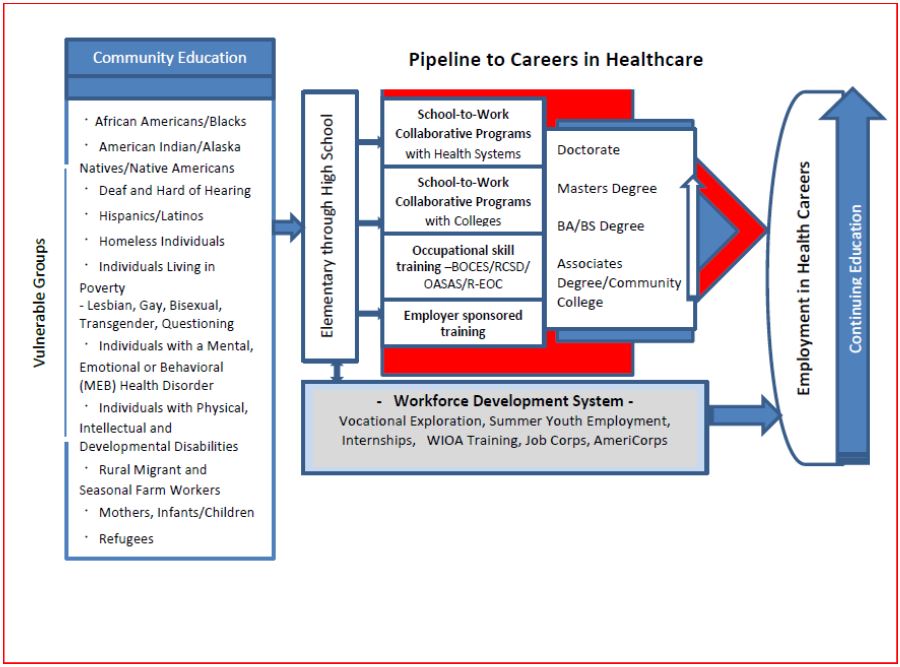
Essential elements in the pipeline to careers in healthcare:
Community education and outreach by FLPPS providers to priority groups. This is the starting point from which to engage youth to envision a career in health care. By collaborating with school guidance counselors FLPPS providers can participate in career fairs, serve as sites for field trips, be available for informational interviews and serve as guest speakers. It is important to introduce health care employment opportunities to young people while they are in the career exploration stage. For example, FLPPS partners could collaborate with local high schools and community colleges to offer a "Careers in Health Care Fair" that features visual and hands–on demonstrations of health care jobs and success stories of current employees who come from backgrounds similar to the students.
Workforce development. It is critically important that community education and outreach efforts conducted by FLPPS providers to vulnerable populations are deliberately linked to local workforce development programs such as Summer Youth Employment, AmeriCorps, and Job Corps. Connecting FLPPS community education and outreach to existing programs such as these will:
- Offer opportunities for FLPPS providers to employ youth and adults from priority groups through subsidized employment programs and incorporate them into community outreach efforts. For example, for a small investment of funding, an AmeriCorps worker could be secured for twelve months to work on a project to promote health careers to priority groups. Through the Summer Youth Employment program, a high school student could assist with community outreach while gaining exposure to potential careers in health care.
- Provide opportunities to co–promote programs so that youth and adults from vulnerable populations can be made aware of current training and employment opportunities in health careers as well as FLPPS provider services.
- Assist with developing and funding training that will meet an identified labor market need where trainees are assured of employment.
- Offer school drop outs a "second chance" at programs like the Rochester Educational Opportunity Center and Job Corps Centers, where they can get their GED and career training in Clinical Medical Assistant (CMA), Certified Nurse´s Assistant (CNA) or Medical Administrative Assistant (MAA).
School–to–Work Collaborative Programs offer rich possibilities for innovative partnerships with FLPPS providers, health systems and colleges. It is important to be aware of existing programs and look for opportunities to replicate or expand successful models to meet the unique needs of specific vulnerable populations.
- School–to Work Collaborative Programs with Health Systems – Some examples in the Rochester area include:
- Rochester General Health System
The Youth Apprenticeship Program and Rochester General Health System give Rochester City School District students an opportunity to succeed and achieve a career in healthcare. Each participant earns not just his/her high school diploma, but also a Certificate of Completion attesting that the students have had youth employment competency training, and have the skills necessary to be a conscientious and productive employee. This "real–life" experience in the medical field 6ukmakes students eligible for entry level positions such as: Patient Care Technician, Pediatric Technician, Material Record Assistant, Respiratory Care Aide, and Transporter and Lab Assistant.
School–to–Work Collaborative Programs with Colleges – Monroe County´s largest employer, the University of Rochester has several innovative programs that work in collaboration with the Rochester City School District and others.
University of Rochester Medical Center – The Office of Human Resources–Multicultural Affairs and Inclusion has collaborated since September 2007 with the Rochester City School District to offer the Healthcare and Technology Youth Apprenticeship Program (HTYAP). This two–year apprenticeship program provides work experiences for underrepresented junior and senior high school students interested in medicine, healthcare, and associated technological professions. Student apprentices rotate through several departments at the Medical Center during their first year and a half in the program. The goal is for each student to be placed in a position in one department at the beginning of the second semester of his or her senior year. Students receive stipends provided by the Office of Human Resources–Multicultural Affairs and Inclusion for the entire two–year program. To be eligible to participate in the program, students must achieve at least a 3.0 GPA. During the school year, students work between 12 – 20 hours per week. During the summer, they participate in volunteer community engagement activities to gain awareness of the needs of the community and to increase their understanding of the importance of giving back to the community. Parent involvement is a key component of the success of the apprenticeship program. Evening workshops-well attended by both students and parents-are offered on college selection, financial aid, and professional development.
The URMC Teen Health and Success Partnership (THSP). This partnership provides opportunities for Rochester´s youth to develop hands–on job skills, while laying the foundation for future employment and career development within health care, research, and academic settings. The partnership provides long–term advocacy, academic resources, life skills development, and job training. Mentoring is an integral part of the University of Rochester´s approach.
- Be Employed Be Successful is a Teen Health and Success Partnership offered in concert with the Hillside Youth Scholarship program. The program is focused on increasing the 51% high school graduation rate of Rochester City School District teens by providing academic resources, life skills development, and job training. Resources include free tutoring, career shadowing, monthly enrichment learning sessions, college preparation, wellness programs and career coaching. Participating youth are at least 16 years old and enrolled in the Rochester City School District. THSP young adults employed at the UR have access to tutoring, college and career preparation, monthly enrichments, healthcare resource connections, wellness programs and more.
- The Young Men of Rochester: UR BOLD (Building Outstanding Leadership & Distinction) program is collaboration between the Rochester City School District´s Leadership Academy for Young Men and the University of Rochester´s Teen Health and Success Partnership program. UR BOLD focuses on improving the 47% African–American male and the 42% Latino male graduation rate in the Rochester City School District. This program provides mentorship, resource connection, college immersion and skill–building seminars, which emphasizes personal development and career success.
Occupational Skill Training – Board of Cooperative Educational Services (BOCES), the Office of Adult and Career Education Services and the Rochester Educational Opportunity Center (R–EOC) all offer opportunities for skill training in a variety of entry level health careers to meet current labor market demand. These training providers frequently offer one or more of the following programs: Certified Nursing Assistant, Emergency Medical Technician, Home health Aide, Licensed Practical Nursing, Medical Secretary, and Pharmacy Technician. They are open to working with area employers to customize training to meet the needs of specific groups of trainees or employers. They also offer English as a Second Language, TASC preparation, and work readiness skill development services.
Health Professional Opportunities Grant (HPOG) – Action for a Better Community manages a federally funded training program that will work with 1,500 local residents to provide a pathway out of poverty and jobs in health care. The goal is to recruit, train and place these individuals into good paying and career–ladder jobs over the next five years (2016–2021). The program not only provides education and training to low–income individuals for occupations in the health care field, but also addresses a major barrier – outside support for items such as child care. The program involves more than a dozen partners from the community, with other non– profit agencies and higher education institutions joining in. Some serve as recruiters of sorts, identifying individuals who fit the program and matching them with navigators who help them through the process of applying for services and enrolling in training programs. The program also brings in employers who will match program graduates with jobs in the health care field.
Employer Sponsored Training – Area employers, particularly those that offer home care and facility based care, often provide entry level Home Health Aide and Certified Nursing Assistant training prior to employment. They are open to customizing training to meet the needs of specific cultural groups and are willing to collaborate with community based organizations, the workforce development system, and others to recruit trainees. FLPPS providers can develop relationships with these employers to assist with recruitment for these positions as part of their community outreach efforts to vulnerable populations.
Community College – The role of the community college in providing a foundation for continuing academic success cannot be overstated. It is at the Community College that youth from vulnerable populations begin to master the "hidden rules" of the dominant culture that will help them through their careers. By "hidden rules," we mean the unspoken habits and social cues of a group that let you know if you do or do not belong (Payne, 1996). At the Community College they gain the competencies to succeed not just academically but socially. Here advisors and advocates can play an important role in their success; educational success is more than just getting good grades. The Community College offers youth from disadvantaged backgrounds an affordable education, training for jobs that offer immediate entre to the workforce, an academic foundation in preparation for enrollment into a four–year college, and access to scholarship opportunities. Upon completing a four–year degree it is reasonable to expect that many of those who enter the health careers "pipeline" will obtain Masters Degrees and PhD´s and continue to enrich the field of health care with their experience, cultural background and sensitivity to the needs of vulnerable populations.
Continuing Education – Once employed, career ladders can be designed to support the training and promotion of these employees and others within the health care system by providing continuing education opportunities and on–the–job training. Educational benefits provided by health care employers can provide rich opportunities for adults to advance to obtain multiple degrees and professional certifications over the course of their careers.
In addition, FLPPS partners can play an important role in initiating the development of a local process to facilitate the recruitment of exceptionally capable applicants that are representative of the groups who come to them for health care services. This process will bring in new employees who speak languages other than English, further reducing the costs of health care and improving communication as they advance in their careers in health care. With the myriad of growth opportunities available through careers in health care, it is possible for individuals, once they enter the pipeline, to obtain employment, advanced degrees and benefit from continuing education. However, the first step is still the most important...get them into the pipeline.
Opportunities for Collaboration with Colleges and Universities to enhance instruction in Cultural Competence and Health Literacy:
For colleges and universities, engagement with local FLPPS providers offers many opportunities to enrich program offerings. There may be informal arrangements already in place where educational institutions contact FLPPS providers for guest speakers or FLPPS professional staff serve as adjunct faculty. It is unlikely that academic institutions are fully aware of the broad range of opportunities that exist within the FLPPS provider network to enhance instruction in CC/HL. Some strategies for working with academic institutions to add CC/HL training modules to their required courses for professional practice preparation include:
- FLPPS providers host field trips and service learning opportunities in health care careers. In a service learning project students serve part of a clinical rotation in the surrounding community where they work to address specific health problems of disadvantaged and underserved populations of focus.
- FLPPS will encourage partner organizations to serve as guest speakers at local colleges.
- FLPPS will connect training programs, continuing education opportunities and professional conferences to college and university representatives.
APPENDIX C: Stakeholder Engagement
__________________________________________________________________
Over the past year, Finger Lakes Performing Provider System, Inc. (FLPPS) in partnership and collaboration with Coordinated Care Services, Inc. (CCSI) has engaged with various internal and external community stakeholders. The feedback and input received has been instrumental and incorporated within this cultural competence and health literacy training strategy.
FLPPS Network Partners – CC/HL Organizational Assessment & Readiness Questionnaires
On behalf of Finger Lakes Performing Provider System (FLPPS), Coordinated Care Services, Inc. (CCSI) developed the Organizational Cultural Competence (CC) and Health Literacy (HL) Self– Assessment Tool and Cultural Competence and Health Literacy Organizational Readiness Questionnaire. Partners were given the opportunity to complete the assessment tools to assess the cultural competence and health literacy baseline of their organizational infrastructure, as well as key organizational dimensions of cultural competence and health literacy. The participating partners represented a cross–section of FLPPS network partners, consisting of physical health, behavioral health and community– based organizations. A total of 37 network partners were administered the Organizational Cultural Competence (CC) and Health Literacy (HL) Self–Assessment Tool, which 36 completed the assessment. A total of 103 network partners completed the Cultural Competence and Health Literacy Organizational Readiness Questionnaire. Based on our analysis of partner responses, we identified the following common themes, current gaps and network training needs:
- Foundational Cultural Competence and Health Literacy Training to define, explain and process what cultural competence is and how to incorporate these concepts and approaches into all aspects of the partners´ organization and practices
- Establishment of Board Governance
- Drafting Cultural Competence and Health Literacy Policies
- Data Collection and Making Meaningful Use of Data to Improve Service Delivery, Patient Health Outcomes & Patient Experience
- Continuous Quality Improvement (CQI) Processes
- Language Accommodations/Interpretive and Translation Services
- Building a Diverse and Culturally Respectful Workforce
- Establishing and Convening Internal Cultural Competence and Health Literacy Committees, Patient Advisory Boards and Quality Assurances (QA) and Quality Improvement (QI) Committees
- Patient Prescription Literacy
- Patients´ Rights and Responsibilities
- Health Literacy
- Social Determinants of Health
Patients/Consumers – Community Stakeholder Forums
To promote patient voice and patient choice, we conducted community stakeholder forums to better understand: (1) healthcare challenges/barriers faced by patients/consumers, (2) A vision, from the patient/consumer perspective, of how the patient´s/community´s health and well–being would/could improve, if challenges/barriers were addressed, (3) existing community resources, services and assets that have been beneficial in assisting patients/communities achiever better health outcomes, and (4) key community stakeholders.
Topics discussed during these forums consisted of, but not limited to:
- Women´s Health
- Taking Charge of Your Health (Health Literacy; Community Education; Social Marketing)
- Violence and Trauma (A Public Health Issue)
- The Faith Community (How The Faith Community Impacts Behavior Change; Their Role In The Community)
- Seeking Services in the Community (Physical/Mental And Social Services)
- Youth & Adolescent Health
- Aging & Elder Care
- People With Disabilities (Deaf/Hard Of Hearing; Mobility Challenges; Blind/Visually Impaired)
- LGBTQ Health
- Men´s Health (In A Barber Shop Setting)
- Cultural Competence
- Health Literacy
- Social Determinants of Health
- Transportation
- Mental Health
- Amish & Mennonite
- Insurance & Insurance Enrollment
- Migrant Farmworker Health
- Open Topic
Some resonating themes from these forums consisted of:
- Strengthening Patient–Provider/Healthcare Professionals Cultural Competence
- Increasing awareness/understanding of the intersection of poverty and health – social determinants of health
- Increasing understanding of stigma/perceptions associated with providing care
- Increasing understanding of how the social and emotional needs of individuals and health play a role in health–seeking behaviors and following up with health care needs
- Increasing awareness of patient knowledge/perceptions of different diseases
- Increasing awareness/sensitivity to challenges/barriers that may exist in accessing health care and social services
- Encouraging shared decision–making
- Encouraging/supporting patient education and patient self–advocacy
- Increasing understanding of the challenges that patients/consumers confront with navigating the health care system and the surrounding community–based supports
- Increasing awareness of the cultural and language barriers that impede the patient/consumers ability to interact in cross–cultural clinical encounters
Faith and Spiritual Leaders
A "Spiritual Leaders Breakfast" was hosted with attendees from local faith and spiritual leaders, representatives and laypersons from surrounding area health ministries, faith–based organizations, churches and faith houses. This was an informal community meeting to discuss how we can work together to improve the health of parishioners, congregants and the communities in which we all live, work and play. Topics of discussion consisted of, but were not limited to: (1) health ministries, (2) the health challenges and concerns of parishioners, congregants and their respective communities, (3) health and healing from the pulpit, and (4) successes, feedback and suggestions to aid in the transformation of our healthcare delivery system, and (5) opportunities for partnerships.
The following themes were identified based on feedback received:
- Desire for on–going interfacing with faith & spiritual leaders in an effort to "connect the connectors"
- Opportunities to partner with and establish faith groups (e.g. Interdenominational Health Ministry)
- Addressing the disconnect of the "church" and the community – faith & spiritual leaders are often not present at decision–making tables
- Building Trusting Relationships are Key – people prefer to express their concern in places and with people that they already have established a relationship with
- Desire to use "Home Health Educators" to provide support and health education to people in their homes
- Need for health club access in the various neighborhoods – easily accessible, safe places to participate in fitness activities
- Desire to streamline cross–communication between FLPPS and faith houses to understand how to connect and collaborate on efforts
- Need for an easily accessible resource repository for area organizations and community resources, to include who provides services, where are services provided and available, what types of services are available, when are these services available
- Desire for FLPPS to collaborate with health ministries´ street outreach efforts (e.g. "Clergy on Patrol")
University of Rochester Center for Experiential Learning (CEL)
The Center for Experiential Learning (CEL) creates and supports inter–professional educational programs and partnerships between Strong Memorial Hospital, Highland Hospital, Eastman Institute for Oral Health, the School of Nursing, School of Medicine and Dentistry, Nursing Practice, Graduate Medical Education, community providers, and beyond. The Center for Experiential Learning serves as a resource aimed at both improving the way professionals are taught throughout their careers and supporting innovative educational programs. These activities are designed to provide healthcare providers at every stage in their careers with information they need to improve their level of patient care (URMC, 2015).
We discussed existing cultural competence and health literacy trainings, the continuing medical education (CME) accreditation process for cultural competence and health literacy training and available educational resources.
|top of section| |top of appendix| |top of page|Monroe County Medical Society
The Monroe County Medical Society is a professional organization for physicians, surgeons, residents and medical students, which advocates for the betterment of patients and the community through professional development. During our meeting we discussed popular training topic areas for professional development, best practices for training medical professionals, residents and medical students and opportunities to work in partnership and collaboration with Monroe County Medical Society to meet the training needs of clinicians and other workforce sectors within our region. Currently, the Medical Society provides training in (7) counties (urban and rural) within New York State. It was expressed that rural clinicians, health organizations and service providers display an eagerness and dedication to participate in trainings to ´make things better´ for their patients/consumers, however, many lack the time and convenient accessibility to trainings and best practices resources.
Based on assessment of training participants´ evaluations, some key components of training and professional development opportunities should include:
- Audience–specific training topics (topics based on the interests of participants/audience)
- Flexibility (multiple training methods and formats)
- Interactive Engagement
- Collective Problem–Solving (less lecture, more opportunities for training participants to brainstorm, collaborate and problem solve as a group)
- Relevance and Applicability (for easy adoption and incorporation)
- Holistic Approach
In addition, clinicians and other workforce sectors (i.e., healthcare professionals – primary care, behavioral health, care management, direct/non–direct support, community–based organizations, etc.) experience service provider ´burn–out´ due to the nature of their jobs.
Over the last 5 years, four physicians have committed suicide as a result of ´provider burn–out´ – resulting in a growing interest in Mindfulness and De–Escalation Trainings. Therefore, it is essential that we address the fundamental needs of the participants´ mental, physical and spiritual health and wellness to aid them in providing patients/consumers with high quality, equitable care.
|top of section| |top of appendix| |top of page|FLPPS Central Team
To be successful in implementing our Cultural Competence and Health Literacy Strategic Plan and Training Strategy, multiple work streams are essential to addressing the drivers of healthcare disparities through improved clinical outcomes and reducing avoidable hospitalizations. Several internal meetings were convened with FLPPS Central Team (MEB, Workforce, Information Technology (IT), Medical Director, Patient Centered Medical Homes (PCMH), Leadership and Communications). Based on feedback and input, we acknowledge that cultural competence and health literacy training and professional development opportunities must be integrated into all aspects of FLPPS operations, infrastructure, projects and network partnerships Population Health & Analytics/Health Information Technology (HIT) Systems and Processes; Workforce; Practitioner Engagement; Population Health Management; Clinical Integration; Patient Engagement and Activation; Communication; and FLPPS Organizational Infrastructure). Professional development must be grounded in the context of cultural competence and health literacy, which characterizes the diffusion of professional knowledge to build sustainable work environments focused on improving the health outcomes of FLPPS´ patients/consumers.
|top of section| |top of appendix| |top of page|APPENDIX D: Targeted Training Audience, Groups and Sectors
| Administrative Support | |
| Office Clerks | |
| Secretaries and Administrative Assistants | |
| Coders/Billers | |
| Dietary/Food Service | |
| Financial Service Representatives | |
| Housekeeping | |
| Medical Interpreters | |
| Patient Service Representatives | |
| Transportation | |
| Other | |
| Maintenance Workers, Janitors and Cleaners | |
| Health Information Technology | |
| Health Information Technology Managers | |
| Hardware Maintenance | |
| Software Programmers | |
| Technical Support | |
| Other | |
| Home Health Care | |
| Certified Home Health Aides | |
| Personal Care Aides | |
| Other | |
| Other Allied Health | |
| Nutritionists/Dieticians | |
| Occupational Therapists | |
| Occupational Therapy Assistants/Aides | |
| Pharmacists | |
| Pharmacy Technicians | |
| Physical Therapists | |
| Physical Therapy Assistants/Aides | |
| Respiratory Therapists | |
| Speech Language Pathologists | |
| Other | |
| Nursing Care Managers/Coordinators/Navigators/Coaches | |
| RN Care Coordinators/Case Managers/Care Transitions | |
| LPN Care Coordinators/Case Managers | |
| Social Worker Case Management/Care Management | |
| Bachelor´s Social Work | |
| Licensed Masters Social Workers | |
| Social Worker Care Coordinators/Case Managers/Care Transition | |
| Other | |
| Non–licensed Care Coordination/Case Management/Care Management/Patient Navigators/Community Health Workers (Except RNs, LPNs, and Social Workers) | |
| Care Manager/Coordinator | |
| Care or Patient Navigator | |
| Community Health Worker | |
| Peer Support Worker | |
| Patient Education | |
| Certified Asthma Educators | |
| Certified Diabetes Educators | |
| Health Coach | |
| Health Educators | |
| Other | |
| Administrative Staff ––All Titles | |
| Executive Staff | |
| Financial | |
| Human Resources | |
| Other | |
| Physicians | |
| Primary Care | |
| Other Specialties (Except Psychiatrists) | |
| Physician Assistants | |
| Primary Care | |
| Other Specialties | |
| Nurse Practitioners | |
| Primary Care | |
| Other Specialties (Except Psychiatric NPs) | |
| Nursing | |
| Nurse Managers/Supervisors | |
| Staff Registered Nurses | |
| Other Registered Nurses (Utilization Review, Staff Development, etc.) | |
| Midwives | |
| LPNs | |
| Other | |
| Clinical Support | |
| Medical Assistants | |
| Nurse Aides/Assistants | |
| Patient Care Techs | |
| Clinical Laboratory Technologists and Technicians | |
| Other | |
| Behavioral Health (Except Social Workers providing Case/Care Management, etc.) | |
| Psychiatrists | |
| Psychologists | |
| Psychiatric Nurse Practitioners | |
| Licensed Clinical Social Workers | |
| Substance Abuse and Behavioral Disorder Counselors | |
| Other Mental Health/Substance Abuse Titles Requiring Certification | |
| Social and Human Service Assistants | |
| Psychiatric Aides/Techs | |
| Other | |
| Spiritual Care | |
| Clergy | |
| Deacon/Lay leader | |
| Chaplain | |
| Other | |
| Holistic health practitioner; Herbalist | |
| Patient/Consumer | |
APPENDIX E: Qualities of a Health Literate Organization
Although health literacy is commonly defined as an individual (patient/consumer) trait–the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions (Ratzan and Parker, 2000)–there is a growing appreciation that health literacy does not depend on the skills of individuals (patients/consumers) alone (IOM, 2003). Health literacy is the product of individuals´ capacities and the health literacy– related demands and complexities of the health care system (Baker, 2006; Rudd 2003). System changes are needed to align health care demands better with the public´s skills and abilities (Parker, 2009; Rudd, 2007). Thus, some critical onus of achieving health literacy lies with the healthcare organization.
Attributes about Leadership, Priorities, Training, Access, and Special Situations
- Has leadership that makes health literacy integral to its mission, structure, and operations.
The organization makes advancing health literacy a high priority and part of the organizational values, culture, and day–to–day operations. Committed, continuous, knowledgeable leadership is key to effectively implement and sustain health literacy improvement activities. - Integrates health literacy into strategic and operational planning, quality improvement, goals, and measures.
The organization makes sure that health literacy is explicitly integrated into all relevant activities, and that health literacy informs both strategic and operational planning, execution, and evaluation. The organization assesses success with vulnerable populations as part of its overall organizational performance measures. - Prepares the workforce to address health literacy issues and monitors progress.
The organization recognizes and meets staff health literacy training needs. The training contributes to a culture in which everyone values and promotes effective communication. The organization measures the training´s impact on advancing health literacy and other goals. - Provides easy access to health information and services and help finding the way in facilities.
The organization uses techniques to make it easy for people to find information in facilities, such as health departments, clinics, and social service agencies, and on Web sites and other communication channels. Help finding the way in facilities can mean providing clear signs, directions, forms, and helpful staff who provide information in plain language.
Best practices in Web design and social media communication help the organization make its electronic materials, messages, and systems, such as patient portals or online databases, easy for people to find, understand, and use.
If the organization provides telephone–based information or services, such as appointment scheduling or toll–free information lines, it can make sure staff use plain language when talking with the public. - Addresses health literacy in high–risk situations, such as emergency preparedness, crisis and emergency response, and clinical emergencies or transitions.
The organization puts processes in place to make sure that people receive clear and useful communication when they are at their most vulnerable or under emotional or physical stress. Planning for emergencies, crises and stressful transitions anticipates the audience´s health literacy issues and prepares for the types of basic information and services people will need to respond to high–risk situations. - Communicates clearly available health services and costs.
The organization uses clear communication techniques to explain a person´s choices among health services and the costs, if relevant, for each service. If a person must complete forms to receive services, the forms are in plain language with information design techniques that make it easy to understand and complete the forms.
Attributes about Audience and Group Participation and Feedback in Health Communication and Information Activities
- Includes members of groups served in the design, implementation, and evaluation of health information and services.
The organization invites members of the groups it serves to be part of the processes that result in health information and services. It pays special attention to including people with limited literacy and numeracy skills when planning programs and preparing materials. - Meets the needs of audiences with a range of health literacy skills while avoiding stigmatization.
The organization makes information and communication clear and culturally and linguistically appropriate for all audiences. It uses audience feedback to verify comprehension and information usefulness. The organization selects formats and channels with the greatest reach for the intended audience. Staff don´t demean, criticize, or call negative attention to people with limited literacy and numeracy skills. - Uses health literacy strategies in oral communication.
The organization uses clear communication techniques in spoken communication, such as conversations, interviews, oral presentations, and podcasts and videos. It reinforces spoken information and communication with other formats that help people remember the information and learn how to find more information when they need it. The organization uses various audience feedback methods to verify comprehension and information usefulness. - Designs and distributes print, audiovisual, and social media content that is easy to understand and act on.
The organization asks the intended users of the information and communication to contribute to all steps of the content process. It uses multiple channels for information and communication so that people can use their preferred channels as well as be exposed to the information multiple times to help learning and recall. The materials have a clear message and actions the audience can take to protect and promote their health. The materials use words, number and concepts familiar to the intended audience.
Summarized from:
Brach, C., Keller, D., Hernandez, L.M., Baur, C., Parker, R., Dreyer, B., Schyve, P., Lemerise, A.J., & Schillinger, D. (2012). Ten attributes of health literate health care organizations. Institute of Medicine. Retrieved from:
http://www.ahealthyunderstanding.org/Portals/0/Documents1/IOM_Ten_Attributes_HL_Paper.pdf
EXHIBIT A
Adapted from: Institute of Medicine of the National Academies
Advising the nation * Improving health
The Activities of a...HEALTH LITERATE ORGANIZATION:
Meets Needs of All
Meets needs of population with a range of health literacy skills while avoiding stigmatization. Paying close attention to the specific needs of vulnerable populations.
Communicates Effectively
Uses health literacy strategies in interpersonal communications and confirms understanding at all points of contact.
Includes Patients/Consumers
Includes populations served in the design, implementation, and evaluation of health information and services and operations.
Plans, Evaluates & Improves
Integrates health literacy into planning, evaluation, measures, patient safety and quality improvement.
Prepares Workforce
Prepares the workforce to be health literate and monitors progress.
Focused on High Risk
Addresses health literacy in high–risk situations, including care transitions and communications regarding medications.
Explains Coverage and Costs
Communicates clearly what health plans cover and what individuals will have to pay to receive services.
Ensures Easy Access
Provids easy access to health information and services and navigation/language assistance.
Leadership Promotes
Has leadership that makes health literacy integral to its mission, policies, structure, and operations.
Designs Easy to Use Materials
Designs and distributes print, audiovisual, and social media content that is easy to understand and act on.
BUILDING A FOUNDATION → PATIENT VOICE AND CHOICE
CCSI Coordinated Care Services, Inc. * Innovative Solutions in Human Service Delivery
APPENDIX F: Social Determinants of Health
As explained in Healthy People 2020, health starts in our homes, schools, workplaces, neighborhoods, and communities. We know that taking care of ourselves by eating well and staying active, not smoking, getting the recommended immunizations and screening tests, and seeing a doctor when we are sick all influence our health. Our health is also determined in part by access to social and economic opportunities; the resources and supports available in our homes, neighborhoods, and communities; the quality of our schooling; the safety of our workplaces; the cleanliness of our water, food, and air; and the nature of our social interactions and relationships. The conditions in which we live explain in part why some Americans are healthier than others and why Americans more generally are not as healthy as they could be (Healthy People 2020, 2014).
Healthy People 2020 highlighted the importance of addressing the social determinants of health by including "Create social and physical environments that promote good health for all" as one of the four overarching goals for the decade.
Understanding Social Determinants of Health
Social determinants of health are conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality– of–life outcomes and risks. Conditions (e.g., social, economic, and physical) in these various environments and settings (e.g., school, church, workplace, and neighborhood) have been referred to as "place."
In addition to the more material attributes of "place," the patterns of social engagement and sense of security and well–being are also affected by where people live. Resources that enhance quality of life can have a significant influence on population health outcomes. Examples of these resources include safe and affordable housing, access to education, public safety, availability of healthy foods, local emergency/health services, and environments free of life– threatening toxins.
Understanding the relationship between how population groups experience "place" and the impact of "place" on health is fundamental to the social determinants of health-including both social and physical determinants.
EXHIBIT A
SOCIAL DETERMINANTS
HEALTH
Social, Economic & Political Factors
- Racism
- Social Cohesion
- Political Participation
- Segregation
- Inequality
- Poverty
Living & Working Conditions
- Housing
- Access to Food
- Disease Vectors
- Air, Water & Soil Quality
- Work Environment
- Job Availability
- Wages & Benefits
- Violence & Crime
Public Services & Infrastructure
- Parks
- Education
- Community Center
- Transportation
- Economic Development
- Health Care
Individual Behaviors
- Exercise
- Diet
- Coping
- Addiction
Individual Factors
- Race, Age, Gender, Culture
"Factors that contribute to a person´s current state of health. These factors may be biological, socioeconomic, psychosocial, behavioral, or social in nature."
CCSI Coordinated Care Services, Inc. * Innovative Solutions in Human Service Delivery
|top of section| |top of appendix| |top of page|
APPENDIX G: Cultural Competence & Health Literacy Educational Resource Repository
| Resource Title | Audience | Authors | Synopsis | Link |
|---|---|---|---|---|
| Promoting Cultural and Linguistic Competence: Self– Assessment Checklist for Personnel Providing Primary Health Care Services | Clinicians, Other Workforce Sections, Community | Tawara D. Goode, National Center for Cultural Competence, Georgetown University Center for Child & Human Development and University Center for Excellence in Developmental Disabilities, Education, Research & Service | Tool for personnel providing primary health care services. | http://nccc.georgetown.edu/documents/Checklist%20PHC.pdf |
| Training and Technical Assistance Tools | Clinicians, Other Workforce Sections, Community | Substance Abuse and Mental Health Services Administration (SAMSHA) | Find training and technical assistance tools to support your prevention efforts and help you use the Strategic Prevention Framework (SPF). Search training and technical assistance tools by keyword, prevention topic, SPF step, and location at tools and other learning resources. | http://www.samhsa.gov/capt/tools–learning–resources/training–technical–assistance |
| What is Cultural Competence & How Is It Measured? | Clinicians, Other Workforce Sections, Community, Patients/Consumers | Diversity Officer Magazine | This article summarizes a unique approach to designing and developing high impact diversity education. It utilizes a cultural competence framework. Cultural competence is defined and a description of how to assess it at the individual and organizational levels is offered. | http://diversityofficermagazine.com/cultural–competence/what–is–cultural–competence–how–is–it–measured/ |
| Cross–Cultural Challenges: Improving Quality of Care for Diverse Populations | Clinicians, Other Workforce Sectors, Community | Institute for Healthcare Improvement | Cross–cultural challenges are just a few examples of how the subject of cultural competence "is attracting increased attention given the concern with improving access, eliminating racial and ethnic health disparities, and providing more culturally competent, high–quality care to diverse populations," according to Robert C. Like, MD, MS, a family physician with a background in medical anthropology. | http://www.ihi.org/resources/Pages/ImprovementStories/CrossCulturalChallengesImprovingtheQualityofCareforDiversePopulations.aspx |
| Institute for Healthcare Improvement Tools | Clinicians, Other Workforce Sectors, Community | Institute for Healthcare Improvement | The Institute for Healthcare Improvement has developed and adapted tools to help organizations accelerate improvement. In addition, many organizations have developed tools in the course of their improvement efforts — for example, successful protocols, order sets and forms, instructions and guidelines for implementing key changes — and are making them available on IHI.org for others to use or adapt in their own organizations. | http://www.ihi.org/resources/Pages/Tools/default.aspx |
| Center for Public Health Education (CPHCE) | Clinicians, Other Workforce Sectors, Community, Patients/Consumers | University of Albany – School of Public Health | The Center for Public Health Continuing Education (CPHCE) strives to be one of the primary sources of continuing education for the public health workforce. Many of our training opportunities are available free via distance learning. Check out the on–demand webcasts from Public Health Live, the certificate program at Public Health Nurse Ready, the online courses at the Empire State Public Health Training Center, and the Northeast Public Health Leadership Institute as well as our many other programs. | http://www.albany.edu/sph/cphce/index.shtml |
| AMA: Steps Forward | Clinicians, Other Workforce Sectors, Community | American Medical Association (AMA) | STEPS Forward™ is a practice–based initiative brought to you by the American Medical Association. Our goal is to provide you with proven strategies that can improve practice efficiency and help you reach the Quadruple Aim — better patient experience, better population health and lower overall costs with improved professional satisfaction. | https://www.stepsforward.org/how–it–works |
| TRAIN National: Public Health and Training Opportunities | Clinicians, Other Workforce Sectors, Community, Patients/Consumers | Public Health Foundation – TRAIN National | TRAIN, the premier learning management system (LMS) for professionals and volunteers who protect the public´s health, would like to invite public health, workforce development, public safety, and emergency preparedness leaders to a monthly webinar demonstration on TRAIN´s functions and features as well as the benefits of utilizing an LMS. TRAIN is a free service of Public Health Foundation and operates through collaborative partnerships with state and federal agencies, local and national organizations, and educational institutions. Through this site, you can: Quickly find and register for many courses listed on Train.org and participating TRAIN affiliate sites; Track your learning with personal online transcripts; Access valuable materials, course reviews, and discussions to improve your learning experience, and Stay informed of the latest public health trainings for your area or expertise. | https://www.train.org/DesktopShell.aspx?tabId=191&goto=browse&browse=subject&lookfor=3&clinical=both&local=all&ByCost=1 |
| Disability Diversity Training | Clinicians, Other Workforce Sectors, Community, Patients/Consumers | Stand Among Friends | Have you ever questioned whether or not you should open the door for someone ahead of you who is in a wheelchair? Or have felt uncomfortable sitting next to someone with an apparent physical disability? These experiences are very common and ones that many of us have worked through. The need for people to be educated about people living with disabilities is ever growing in our society. At some point in all of our lives, we will be confronted with a situation where we will have to serve the needs of someone who has a disability. Sadly, stereotypes and prejudice impact the way in which we interact with and serve others who have disabilities. Discrimination and negative attitudes towards people with disabilities comes from a general lack of information and misunderstanding about who these people are and the best practices for serving their unique needs as individuals. | https://standamongfriends.org/programs/disability–diversity–training/ |
| National Information Center on Health Services Research and Health Care Technology | Clinicians, Other Workforce Sectors, Community, Patients/Consumers | National Institute of Health, U.S. National Library of Medicine | Serving the information needs of health services research community. | https://www.nlm.nih.gov/hsrinfo/health_literacy.html |
| CDC: Health Literacy, Plain Language, Culture and Communication Training Repository | Clinicians, Other Workforce Sectors, Community, Patients/Consumers | Centers for Disease Control and Prevention | Training in health literacy, plain language, and culture and communication is essential for anyone working in health information and services. Whether you are new to these topics, need a refresher, or want to train your entire staff, the following courses are a good place to start. | http://www.cdc.gov/healthliteracy/gettraining.html |
| What Works for Health: Cultural Competence Training for Health Care Professionals | Clinicians, Other Workforce Sectors, Community, Patients/Consumers | County Health Rankings & Roadmaps: Building a Culture of Health, County by County | Cultural competence training for health care professionals focuses on skills and knowledge to value diversity, understand and respond to cultural differences, and increase awareness of providers´ and care organization´s cultural norms. Trainings can provide facts about patient cultures or include more complex interventions such as intercultural communication skills training, exploration of potential barriers to care, and institution of policies that are sensitive to the needs of patients from culturally and linguistically diverse (CALD) backgrounds (Cochrane–Horvat 2014). | http://www.countyhealthrankings.org/policies/cultural–competence–training–health–care–professionals |
| Cultural Competency Training and Resources | Clinicians, Other Workforce Sectors, Community, Patients/Consumers | Cigna | Cigna believes in providing health care professionals with the tools necessary to help treat their patients. By being culturally competent in health care, health care professionals can understand a patient´s diverse values, beliefs, and behaviors, and customize treatment to meet the patients´ social, cultural, and linguistic needs. | http://www.cigna.com/healthcare–professionals/resources–for–health–care–professionals/health–equity |
| Cultural Competency: Importance, Social Stigma and Its Impact on Cultural Competence & What is Structural Competence | Clinicians, Other Workforce Sectors, Community, Patients/Consumers | Community Partners of WNY: Performing Provider System | Community Partners of WNY is a network of more than 100 health, human service, and educational organizations; the Catholic Health System plus five community hospitals; and over 1,000 physicians from across the region that will focus on transforming the delivery of healthcare in Western New York. Community Partners of Western New York will develop our human resource capabilities by training and empowering our workforce to use best clinical and operational science, health information technology, and a proactive approach to patient care in order to achieve our goals. | http://wnycommunitypartners.org/cultural–competency–and–health–literacy/ |
| Teaching and Training Materials: Improving Practice | Clinicians, Other Workforce Sectors, Community | National Center for the Study of Adult Learning and Literacy | These materials are designed for teachers and professional development staff. Part of NCSALL´s effort to link research and practice, they have been developed using findings emerging from NCSALL research. All materials have been piloted with adult students or teachers and revised on the basis of their feedback. Teaching materials are guides for training activities that trainers can use to develop trainees´ literacy skills and knowledge of particular content. Training materials are guides for professional development activities, such as study circles, that help teachers develop their own knowledge and skills in a specific area. | http://www.ncsall.net/index.html@id=25.html |
| Expecting the Best | Clinicians, Other Workplace Sectors, Community | University of Tennessee – Center for Literacy Studies | Expecting the Best is a program that teaches adults with limited English proficiency about health and wellness through English as a Second Language classes. The program is designed to improve health literacy, functional literacy, and communication skills. It is also expected to strengthen students´ ability to seek health care and make sound health– related decisions. | http://www.cls.utk.edu/expectthebest.html |
| Good Questions for Good Health | Clinicians, Other Workforce Sectors, Community | University of Georgia´s Center for Health and Risk Communication: A National Institute on Aging funded project | The Center for Health and Risk Communication at the University of Georgia advances knowledge about the role of communication processes in enhancing human health and safety. | http://chrc.uga.edu/resources/good–questions–for–good–health/ |
| Talking With Your Doctor Presentation Toolkit | Community, Patients/Consumers | National Institute on Aging | The toolkit (slides, speaker notes, and handouts is for a senior center administrator, nurse, or another intermediary to lead a 45– minute interactive session that builds older adults´ capacity for navigating the healthcare system. The kit includes practical tips to make the most of medical visits, including how to get ready for an appointment, share health concerns, and make collaborative decisions about care. It´s evidence–based and repurposed from the popular booklet on doctor–patient communication. | https://www.nia.nih.gov/health/publication/talking–your–doctor–presentation–toolkit |
| Health Literacy Special Collection: Tools and Resources for Health Literacy Initiatives | Clinicians, Other Workforce Sectors, Community | World Education | World Education has collected links to many health literacy curricula for a variety of learners and learning objectives. Two sections include links to curricula for teaching health literacy skills to adult learners and the general public. A third section includes training for literacy and health professionals to better address health literacy in their settings. | http://healthliteracy.worlded.org/curricula.htm |
| Is Our Pharmacy Meeting Patients´ Needs? Pharmacy Health Literacy Assessment Tool User´s Guide | Clinicians, Other Workforce Sectors, Community | Agency for Healthcare Research and Quality (AHRQ) | This pharmacy health literacy tool was designed to capture perspectives of three critical audiences–objective auditors, pharmacy staff, and patients. The three parts of the assessment are complementary and designed to form a comprehensive assessment. Although the assessment was designed to be used in outpatient pharmacies of large, urban, public hospitals that primarily serve a minority population, it can be adapted for use in other pharmacy and non–pharmacy environments. | http://www.ahrq.gov/professionals/quality–patient–safety/pharmhealthlit/pharmlit/index.html |
| AHRQ Pharmacy Health Literacy Center | Clinicians, Other Workforce Sectors, Community | Agency for Healthcare Research and Quality (AHRQ) | This site provides pharmacists with recently released health literacy tools and other resources from the Agency for Healthcare Research and Quality (AHRQ). Pharmacy health literacy is the degree to which individuals are able to obtain, process and understand basic health and medication information and pharmacy services needed to make appropriate health decisions. | http://www.ahrq.gov/professionals/quality–patient–safety/pharmhealthlit/index.html |
| AHRQ Health Literacy Universal Precautions Toolkit | Clinicians, Other Workforce Sectors, Community | Agency for Healthcare Research and Quality (AHRQ) | The AHRQ Health Literacy Universal Precautions Toolkit, 2nd edition, can help primary care practices reduce the complexity of health care, increase patient understanding of health information, and enhance support for patients of all health literacy levels. This toolkit provides step–by–step guidance for examining health literacy in clinical practice settings. It provides tools for assessing practice and improving interactions with patients at all literacy levels. | http://www.ahrq.gov/professionals/quality–patient–safety/quality–resources/tools/literacy–toolkit/index.html |
| Clear Communication Index Widget | Clinicians, Other Workforce Sectors, Community | Center s for Disease Control and Prevention (CDC) | The CDC Clear Communication Index (Index) is a research–based tool to help you develop and assess public communication materials. The Index has 4 introductory questions and 20 scored items drawn from scientific literature in communication and related disciplines. The items represent the most important characteristics that enhance and aid people´s understanding of information. | http://www.cdc.gov/ccindex/ccindex.html |
| CAHPS Surveys and Tools to Advance Patient–Centered Care | Clinicians, Other Workforce Sectors, Community | Agency for Healthcare Research and Quality (AHRQ) | Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys ask consumers and patients to report on and evaluate their experiences with health care. These surveys cover topics that are important to consumers and focus on aspects of quality that consumers are best qualified to assess, such as the communication skills of providers and ease of access to health care services. All CAHPS surveys are in the public domain, which means that anyone can download and use these surveys to assess experiences with care. Users of CAHPS survey results include patients and consumers, quality monitors and regulators, provider organizations, health plans, community collaboratives, and public and private purchasers of health care. These individuals and organizations use the survey results to inform their decisions and to improve the quality of health care services. | http://www.ahrq.gov/cahps/index.html |
| NIH Plain Language Training | Clinicians, Other Workforce Sectors, Community | National Institutes of Health (NIH) | The NIH offers a free plain language internet– based training that introduces you to the basics of plain language. The goal of this training is to help you learn to organize your ideas, use a clear writing style, and become a more effective communicator. | https://plainlanguage.nih.gov/CBTs/PlainLanguage/login.asp |
| The SHARE Approach | Clinicians, Other Workforce Sectors, Community | Agency for Healthcare Research and Quality (AHRQ) | The SHARE approach is a five–step process for shared decision making. Health professionals can sign up for a webinar or in–person workshop or use the online materials. | http://www.ahrq.gov/professionals/education/curriculum–tools/shareddecisionmaking/index.html |
| Tell Others About Health Literacy | Clinicians, Other Workforce Sectors | Center s for Disease Control and Prevention (CDC) | You are a health literacy ambassador. It is up to you to make sure your colleagues, staff, leadership, and community are aware of the issues. Whether to review for yourself, present to others, or convince your leadership, the following resources may help you talk about health literacy. | http://www.cdc.gov/healthliteracy/shareinteract/tellothers.html |
| Culture, Language & Health Literacy Resources: Research and Education | Clinicians, Other Workforce Sectors, Community, Patients/Consumers | U.S. Department of Health and Human Services, Health Resources Administration | Effective health communication is as important to health care as clinical skill. To improve individual health and build healthy communities, health care providers need to recognize and address the unique culture, language and health literacy of diverse consumers and communities. | http://www.hrsa.gov/CulturalCompetence/research.html |
| Health Literacy and Public Health: Introduction | Clinicians, Other Workforce Sectors, Community | New York–New Jersey Public Health Training Center | This training is the first of two that address health literacy and public health. After completing this training, it is recommended that you enroll in Health Literacy & Public Health: Strategies for Addressing Low Health Literacy. This training contains four sections. The content and activities demonstrate how the public´s literacy skills affect interactions with medical and public health staff. | http://www.empirestatephtc.org/learning/pages/catalog/phlit01/default.cfm |
| Pathways to Safer Opioid Use Training | Clinicians, Other Workforce Sectors, Community | U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion | Pathways to Safer Opioid Use is an immersive, interactive training tool that was designed using the opioid–related recommendations outlined in the National Action Plan for Adverse Drug Event Prevention (ADE Action Plan). The training uses the principles of health literacy and a multimodal, team–based approach to promote the appropriate, safe, and effective use of opioids to manage chronic pain. | http://health.gov/hcq/training–pathways.asp |
| A Physician´s Practical Guide to Culturally Competent Care | Clinicians, Other Workforce Sectors | U.S. Department of Health and Human Services (HHS), Office of Minority Health (OMH) | This is a self–directed training course for physicians and other health care professionals with a specific interest in cultural competency in the provision of care. | https://cccm.thinkculturalhealth.hhs.gov/ |
| Cultural Competency Program for Oral Health Professionals | Clinicians, Other Workforce Sectors | U.S. Department of Health and Human Services (HHS), Office of Minority Health (OMH) | This e–learning program provides oral health professionals with basic knowledge and skills related to cultural and linguistic competency, based on the HHS Office of Minority Health´s National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care. | https://oralhealth.thinkculturalhealth.hhs.gov/ |
| Culturally Competent Nursing Care: A Cornerstone of Caring | Clinicians, Other Workforce Sectors | U.S. Department of Health and Human Services (HHS), Office of Minority Health (OMH) | This course discusses the behaviors, attitudes, and skills that enable nurses to work effectively in cross–cultural situations. | https://ccnm.thinkculturalhealth.hhs.gov/ |
| Preventing Adverse Drug Events: Individualizing Glycemic Targets Using Health Literacy Strategies | Clinicians, Other Workforce Sectors, Community | U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion | Preventing Adverse Drug Events: Individualizing Glycemic Targets Using Health Literacy Strategies is an e–Learning course that teaches health care providers how to reduce hypoglycemic adverse drug events (ADEs) in patients with diabetes. | http://health.gov/hcq/trainin g–prevent–ade.asp |
| Helping Older Adults Search for Health Information Online: A Toolkit for Trainers | Clinicians, Other Workforce Sectors, Community | National Institutes of Health | Use these free, easy–to–use training materials to help older adults find reliable, up–to–date online health information on their own. The training features three websites from the National Institutes of Health — NIHSeniorHealth.gov, MedlinePlus.gov and Go4Life®. Trainers can use the toolkit with beginning and intermediate students of the Web. | http://nihseniorhealth.gov/to olkit/toolkit.html |
| Staying Healthy Curriculum for English Learners and Adult Learners´ Handbooks on Women´s Health and Coping with Stress | Clinicians, Other Workforce Sectors, Community | Florida Literacy Coalition | As a statewide umbrella literacy organization and the host of Florida´s State Literacy Resource Center, FLC provides a range of services to support more than 300 adult education, literacy and family literacy providers throughout Florida. Special emphasis is placed on assisting community based literacy organizations with their training and program development needs. | http://www.floridaliteracy.org/health_literacy_curriculum.html |
| Federal Plain Language Guidelines | Clinicians, Other Workforce Sectors | The Plain Language Action and Information Network | These slides offer a self–study option for learning and implementing the Federal Plain Language Guidelines in your work. The five major topics covered are audience, organization, writing principles, writing for the web, and testing techniques. | http://www.plainlanguage.gov/howto/guidelines/FederalPLGuidelines/TOC.cfm |
| The Health Literacy Environment of Hospitals and Health Centers: Partners for Action: Making Your Healthcare Facility Literacy– Friendly | Clinicians, Other Workforce Sectors, Community | Rima E. Rudd, Jennie E. Anderson (Harvard School of Public Health) | This guide and the review tools found within it offer an approach for analyzing literacy–related barriers to healthcare access and navigation. We designed this guide to assist chief executive officers, presidents, program directors, administrators, and healthcare workers at hospitals or health centers to consider the health literacy environment of their facilities and to analyze ways to better serve their patients. | https://cdn1.sph.harvard.edu/wp–content/uploads/sites/135/20 12/09/healthliteracyenvironment.pdf |
| The Health Literacy Environment Activity Packet: First Impressions and A Walking Interview | Clinicians, Other Workforce Sectors, Community | Rima E. Rudd (Harvard School of Public Health) | This packet focuses on four activities designed to help staff members consider the health literacy environment of their workplace. First impressions focus on the phone, the web and the walk to the facility. The walking interview is a navigation exercise | https://cdn1.sph.harvard.edu/wp–content/uploads/sites/135/2012/09/activitypacket.pdf |
| Navigating Hospitals: Literacy Barriers | Clinicians, Other Workforce Sectors, Community | Rima E. Rudd (Harvard School of Public Health) | This report is a result of a small exploratory examination of hospital navigation issues in order to garner insight into the literacy environment of hospitals. Walking interviews were conducted around the public areas of ten municipal hospitals | https://cdn1.sph.harvard.edu/wp–content/uploads/sites/135/20 12/09/rudd_r.e._2004._navig ating_hospitals._literacy_harvest.pdf |
__________________________________________________________________
1. Healthcare (noun or adjective): a system, industry, or field that facilitates the logistics of health care for patients/consumers.
Health care (noun): a set of actions by a person or persons to maintain or improve the health of a patient/consumer. 1
2. Includes individuals who have direct/non–direct contact with each patient/consumer and who carry out the day–to–day tasks in organizations (e.g., Communications, Customer Service, Data Collection and Analysis, Community Health Workers, Hospitality, Intake, Registration, Reception, Outreach, Program Planning, Program Support, Security, etc.) 2
3. Includes individuals who have direct/non–direct contact with each patient/consumer and who carry out the day–to–day tasks in organizations (e.g., Communications, Customer Service, Data Collection and Analysis, Community Health Workers, Hospitality, Intake, Registration, Reception, Outreach, Program Planning, Program Support, Security, etc.) 3
4. Population health: The health outcomes of a group of individuals, including the distribution of such outcomes within the group. It is an approach to health that aims to improve the health of an entire human population. 4
References
- Agency for Healthcare Research and Quality. (2014). Improving Cultural Competence to Reduce Health Disparities for Priority Populations. https://effectivehealthcare.ahrq.gov/ehc/products/573/1934/cultural–competence–protocol–140709.pdf
- Agency for Healthcare Research and Quality. (2012). Quality Improvement Interventions to Address Health Disparities: Closing the Quality Gap – Revisiting the State of Science. AHRQ Evidence Report/Technology Assessment, Number 208. https://effectivehealthcare.ahrq.gov/ehc/products/386/1243/EvidenceReport208_CQGHealthDisparities_ExecutiveSummary_20120824.pdf
- Angelotti, M., Bliss, K., Schiffman, D., Weaver, E., Graham, L., Bliss, K., Lemme, T., Pryor, V., & Gesten, F. (2015). Transforming the Primary Care Training Clinic: New York State´s Hospital Medical Home Demonstration Pilot. Journal of Medical Graduate Education, (June 2015), 247– 252. http://www.jgme.org/doi/pdf/10.4300/JGME–D–14–00782.1
- Association of American Medical Colleges. (2005). Cultural Competence Education. https://www.aamc.org/download/54338/data/culturalcomped.pdf
- Beamon, C., Devisetty, V., Fornica Hill, J.M., Huang, W., & Shumate, J.A. (2005). A Guide to Incorporating Cultural Competency into Health Professionals´ Education and Training. A Cultural Competency Guide, 1–28. http://njms.rutgers.edu/culweb/medical/documents/CulturalCompetencyGuide.pdf
- Betancourt, J.R., Green, A.R., & Carrillo, E. (2002). Cultural Competence in Health Care: Emerging Frameworks and Practical Approaches. The Commonwealth Fund Field Report (October 2002), 1–30. http://www.commonwealthfund.org/usr_doc/betancourt_culturalcompetence_576.pdf
- Blasé, K.A., & Fixsen, D.L. (2003). Evidence–Based Programs and Cultural Competence. National Implementation Research Network. http://nirn.fpg.unc.edu/sites/nirn.fpg.unc.edu/files/resources/NIRN–EBPAndCulturalCompetence–07–2003.pdf
- Brach, C., & Fraserirector, I. (2000). Can Cultural Competency Reduce Racial and Ethnic Health Disparities? A Review and Conceptual Model. Medical Care Research and Review, 57(November 2000) pp.181–217. http://med–brando.med.uiuc.edu/FacultyDev/ClinicalEnviron/CulturalCompetence/CCCModelToReduceDisparitiesBrach.pdf
- Brach, C., Keller, D., Hernandez, L.M., Baur, C., Parker, R., Dreyer, B., Schyve, P., Lemerise, A.J., & Schillinger, D. (2012). Ten Attributes Of Health Literate Health Care Organizations. Institute of Medicine. Retrieved from: http://www.ahealthyunderstanding.org/Portals/0/Documents1/IOM_Ten_Attributes_HL_Paper.pdf
- Braverman, M.T., & Arnold, M.E. (2008). An Evaluator´s Balancing Act: Making decisions about methodological rigor. New Directions for Evaluation, 120, 71–86.
- Centers for Medicare and Medicaid Services Office of Minority Health. (2015). The CMS Equity Plan for Improving Quality in Medicare. September 2015, 1–17. https://www.cms.gov/About–CMS/Agency–Information/OMH/OMH_Dwnld–CMS_EquityPlanforMedicare_090615.pdf
- Cohen, J.J., Gabriel, B.A., & Terrell, C. (2002). The Care for Diversity in the Health Care Workforce. Health Affairs, 21(5) pp. 90–105. doi: 10.1377/hlthaff.21.5.90. http://content.healthaffairs.org/content/21/5/90.full
- Collective Impact. (2015). Collaborating to See All Constituents Reach Their Full Potential: A Memorandum on Research and Resources on Equity and Collective Impact. https://collectiveimpactforum.org/resources/collaborating–see–all–constituents–reach–their–full–potential–memorandum–research–and
- Dobbin, F., & Kalev, A. (2016). Why Diversity Programs Fail: And What Works Better. Harvard Business Review (July – August 2016 Issue), 52–60. https://hbr.org/2016/07/why–diversity–programs–fail
- Elwyn, G., Frosch, D., Thomson, R., Joseph–Williams, N., Lloyd, A., Kinnersley, P., Barry, M. (2012). Shared Decision Making: A Model for Clinical Practice. Journal of General Internal Medicine, 27(10), 1361–1367. http://doi.org/10.1007/s11606–012–2077–6
- Goode, T.D., Dunne, M.C., & Bronheim, S.M. (2006). Evidence Based for Cultural and Linguistic Competency in Healthcare. The Commonwealth Fund Field Report (October 2006), 1–46. http://www.commonwealthfund.org/usr_doc/Goode_evidencebasecultlinguisticcomp_962.pdf
- Healthy People 2020 [Internet]. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Retrieved from https://www.healthypeople.gov/2020/topics–objectives/topic/social–determinants–of–health
- Horvat, L., Horey, D, Romios, P. & Kis–Rigo, J. (2014). Cultural Competence Education for Health Professionals. May 5, (5), 1–98. doi: 10.1002/14651858.CD009405.pub2
- Institute for Healthcare Improvement. (2003). The Breakthrough Series: IHI´s Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series White Paper. Boston: Institute for Healthcare Improvement; 2003. http://www.ihi.org/ihi
- Joint Center for Political and Economic Studies. (2012). Place Matters: Ensuring Opportunities for Good Health for All – A Summary of Place Matter´s Community Health Equity Reports. September 2012. http://www.racialequitytools.org/resourcefiles/PlaceMattersCommunity.pdf
- Kilbourne, A.M., Switzer, G., Hyman, K., Crowley–Matoka, M., & Fine, M.J. (2006). Advancing Health Disparities Research within the Health Care System: A Conceptual Framework. American Journal of Public Health, December 2006; 96(12), 2113–2121.
- Like, R.C., Barret, T.J., & Moon, J. (2008). CME Clinical View: Educating Physicians to Provide Culturally Competent, Patient–Centered Care. Perspectives: A View of Family Medicine in New Jersey (Summer 2008), 1–20. http://www.ncsl.org/documents/health/njafphandout52013.pdf
- Monroe County Medical Society. [Internet]. Mission & By–Laws: (2014). http://www.mcms.org/mission_by_laws
- National Center for Cultural Competence Georgetown University Center for Child and Human Development Georgetown University Medical Center. (2004).Bridging the Cultural Divide in HealthCare Settings the Essential Role of Cultural Broker Programs. Rockville, MD: http://www.culturalbroker.info/Cultural_Broker_EN.pdf1
- New York State Department of Health. (2015). Medicaid Accelerated eXchange (MAX) Series: Accelerate Transformation and Lasting Change. NYS Medicaid Redesign Team. https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/docs/max_all_pps_meeting–20150617.pdf
- Saha, S., Arbelaez, J. J., & Cooper, L. A. (2003). Patient–Physician Relationships and Racial Disparities in the Quality of Health Care. American Journal of Public Health, 93(10), 1713– 1719.
- Smedley, B.D., Stith, A.Y., & Nelson, A.R. (2003). Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, D.C.: National Academy Press.
- Suhrheinrich, J. (2011). Examining the Effectiveness of a Train–the–Trainer Approach: Training Teachers to Use Pivotal Response Training. Society for Research on Educational Effectiveness http://files.eric.ed.gov/fulltext/ED518863.pdf
- The Council on Linkages between Academia and Public Health Practice. (2014). Core Competencies for Public Health Professionals. http://www.phf.org/resourcestools/Documents/Core_Competencies_for_Public_Health_Professionals_2014June.pdf
- University of Rochester Medical Center – Center for Experiential Learning. [Internet]. About Us: (2015). http://www.mcms.org/mission_by_laws
EXHIBIT B
FLPPS FINGER LAKES PERFORMING PROVIDER SYSTEM
FLPPS CBO ENGAGEMENT STRATEGY
DECEMBER 7, 2016
PRESENTED BY: ERIN BARRY
FLPPS DIRECTOR, STRATEGIC COMMUNITY INITIATIVES
FLPPS CBO ENGAGEMENT STRATEGY
INTRODUCTION
It has been cited in numerous studies and publications that the social determinants of health are a key component of population health improvement. In fact, sources such as County Health Rankings Modeli demonstrate that while clinical care accounts for only 20 percent of individual morbidity and mortality, social and economic factors account for 40 percent, and health behaviors and physical environment account for the other 40 percent, of health status. In light of this reality, it is important to recognize that no single service provider (medical or otherwise) can have a significant impact on health and well–being without accounting for the influence of contiguous systems and programs. As such, there is tremendous power in building an Integrated Delivery System ("IDS") that is mindful of the Social Determinants of Health, and incorporates physical, behavioral as well as social and human services.
Since its inception, FLPPS has understood the importance of community based organizations ("CBOs") and has made a concerted effort to include and fund CBOs delivering services across the 13–county region. Going forward, the organization is committing a dedicated team to the work of Community, Consumer and CBO strategy and engagement. The purpose of this document is to illustrate a path forward to encourage and promote the successful participation of CBOs in Projects and the FLPPS Integrated Delivery System, and to maximize the earning of Achievement Values ("A/Vs"), the mechanism to draw–down DSRIP Award.
Further, as FLPPS maintains the work of DSRIP project implementation, the inclusion of CBOs in design, implementation and governance will assist in demonstrating the efficacy of an integrated system, while also organizing CBOs towards the transition to VBP. This body of work includes the strengthening of existing referral relationships while also building new connections, so that the region´s patients can benefit from tight coordination between social/human services, medical services and behavioral health services to provide a true person–centered approach to care. The team will use the NYS´ Value Based Payment ("VBP") Roadmap as the primary source to understand the State agenda and prepare both providers and CBOs´ for formal inclusion in Medicaid VBP arrangements.
To ensure success in this arena, FLPPS intends to collaborate with its strategic partners to: (1) Continue rapidly connecting social/human service agencies to the FLPPS Integrated Delivery System (Delivery & IT); (2) Compile standardized data on both program cost and benefit; and (3) Determine the impact that CBOs have on population health using collectively prioritized measures. These activities will benefit the larger FLPPS network, as all contracting organizations (per the June release of the VBP Roadmap) must include CBOs in VBP payment arrangements Level 2 and above, starting in 2018; the quality/value driven establishment of provider networks that include CBO sub–contracting arrangements will be paramount to the success of the newly re–designed Medicaid system.
| Community Based Organizations (CBO) | Engagement Strategy |
|---|---|
| Accountable1: | Erin Budd Barry, Director of Strategic Community Initiatives, FLPPS |
| Responsible: | John Paul Perez, Jose Rosario, Joshua Jinks, Meredith Rutherford, Twylla Dillion, Juanita Lyde, Partner Organizations, including but not limited to United Way and FLHSA |
| Consult: | Carol Tegas, Sahar Elezabi, Peter Bauman, Janet King, 2.a.i Project Manager (position open at the time of submission), Courtney Spitz, FLPPS Project Managers, FLPPS Central Regional Managers |
| Inform: | FLPPS Central Contracting, Reporting |
__________________________________________________________________
WORK PLAN OBJECTIVE(S)
- Maximize the earning of all A/Vs tied to CBO–related FLPPS Implementation Plan Milestones and Tasks
- Increase CBO engagement in FLPPS network and inclusion in the FLPPS Integrated Delivery System (Delivery & IT)
- Outreach activities to enhance education of CBO Executives, frontline staff and Boards on the value of participating in DSRIP, and the Value–Based Payment Roadmap
- Clearly demonstrate value of social & human, non–billable services, through strategic activities that connect services to health outcomes, using community–wide (developed and measured) quality standards and IT Platforms
- Prepare CBOs to participate in Value Based Payment arrangements through FLPPS–guided process, in conjunction with Strategic Partners such as The United Way and FLHSA;
__________________________________________________________________
TARGETED PARTNERS AND STAKEHOLDERS
- Tier 1 and Tier 2 Community Based Organizations; Targeted Tier 3 CBOs that provide a hybrid of billable and non–billable services2
- Other Stakeholders including: Strategic Partners, Government Leaders and Professional Organizations
CBO DEFINITIONS PER THE STATE ii
Tier 1: Non–profit, non–Medicaid billing, community based social and human service organization (e.g. housing, social services, religious organizations, food banks)
Tier 2: Non–profit, Medicaid billing, non–clinical service providers (e.g. transportation, care coordination)
Tier 3: Non–profit, Medicaid billing, clinical and clinical support service providers (licensed by the NYS Department of Health, NYS Office of Mental Health, NYS Office for Persons with Disabilities, or NYS Office of Alcoholism and Substance Abuse Services)
__________________________________________________________________
DESIRED OUTCOMES / MEASURES OF SUCCESS
Immediate Priorities (through Q12017)
- Map all CBO services in FLPPS Region, in digital directory that is segmented by county, NOCN, and directly linked to state–prioritized Social Determinants of Health – understand volume of consumers served to prioritize those CBOs that have the most impact and reach
- Identify gaps in DSRIP Project participation (Domain 1), and performance around Domain 2 – 4 Outcome Measures, where CBOs can immediately take action and contribute to FLPPS´ ability to draw down DSRIP award; provide technical assistance to CBOs to increase chances of success
- Prioritize the connection of contracted, key CBOs to RHIO, or through direct linkage to FLPPS IT Care Management Platform, to quickly implement data collection and analytics
- Standardize data points (units of service) for collection to enhance analytics and better understand linkages to health outcomes
- Develop FLPPS Innovation Fund Structure in conjunction with Courtney Spitz (Controller), Carol Tegas, Funds Flow Workgroup, and Finance Committee; clearly define CBO´s ability to participate and contribute to achievement of A/Vs through up–front investment of "grant" dollars and a mechanism to track efficacy of spend (ROI) toward PPS´ goals
- Participate in planning activities around FLPPS contracting deliverables and funding to ensure correct incentives for CBOs as they participate in Phase II and beyond; prioritize activity that influences successful completion of projects and movement of outcome metrics; this will also include any related activities, interventions that CBOs can complete in support of the CC/HL Organizational Work Stream and Training Strategy
- Coordination with FLPPS Population Health Strategy, Care Management Strategy and Regional Prevention Agendas
- Formation of FLPPS CBO Advisory Council, co facilitated with Rochester–area United Way (Laura Gustin); included parties to date: United Way, FLHSA, CCSI, RHIO, Greater Rochester Health Foundation, RMAPI, City Innovation Team, S2AY, City of Rochester´s Innovation Team, NYS Assembly Majority Leader Morelle´s Office, Council of Agency Executives and select CBO Executives
Short–Term Outcomes (18 months)
- Common understanding around the relationship between social services and health outcomes, by service category
- A coordinated community–wide investment strategy is built and deployed
- Social/human service providers have a common understanding about the role, responsibility, risk and reward of participating in the FLPPS Integrated Delivery System.
- Social Determinants of Health/Social Service Providers are included in the FLPPS Population Health Platform and Care Management Platform (IT Build and Implementation)
- An evaluation strategy is designed and implemented, which includes measurement of program cost and benefit
- Coordination and buy–in across key stakeholders and complimentary community initiatives, including: Providers, Insurers, CBO´s, Local Foundations, Patients, Rochester–Monroe Anti–Poverty Initiative and Regional Economic Council´s Pathways to Prosperity Workgroup, Finger Lakes Health Systems Agency, Invest Health, Rethink Health, CMMI: Accountable Health Communities, CMMI: Practice Transformation, NYS Value–Based Payment Roadmap; Implementation of Home and Community–Based Waivers etc.
Medium–Term Outcomes (3 years)
- High–value community–based services and organizations are supported by sustainable funding streams
- A closed–loop referral system between physical, behavioral and social service providers is in place, creating an integrated delivery system with "no wrong door"
- Person–Centered Delivery of Care: All services are delivered at the right time, at the right place to the right person, coordinated through as–needed care management, determined by level of risk
- Data systems support the evaluation of costs and benefit of social/human services, by risk cohort
- Plan–Do–Study–Act (PDSA) cycle applied to cost–benefit analysis across sectors, services and interventions, ensuring continuous evaluation and improvement of quality, cost and satisfaction
Long–Term Outcome (DY5+)
- Improve Health outcomes and generate savings in pursuit of the ´quadruple aim´ for the Medicaid and Uninsured population in the FLPPS region, accomplished by incorporating a strategy to address the social determinants of health and community–based services/organizations into the building of the FLPPS integrated delivery system
- Support other Community Initiatives that aim at the reduction of poverty and other social determinants of health through targeted partnership and community–table participation. Examples: RMAPI and Pathways to Prosperity
__________________________________________________________________
PROJECT PLAN TO ACHIEVE SHORT–TERM OUTCOMES 3
ACTIVITIES,
Milestone 1: Common understanding around the relationship between social services and health outcomes by service category
| Tasks/Sub–Tasks | End Date 4 | Responsible |
|---|---|---|
Define Priority Social Determinates of Health (listed in DOH VBP Roadmap) and tie to Social/Human Services:
|
December 2016 February 2017 TBD |
Lead(s): Erin Barry, Director of Strategic Community Initiatives JP Perez, Senior Project Manager, Community Engagement (FLPPS) Support: Laura Gustin, Director of Systems Integration (UW) |
Create an asset map and capacity analysis of priority social service providers, by county.
|
January/February 2017 February 2017 |
Lead(s): Erin Barry JP Perez Coordinate With: United Way of Greater Rochester, City of Rochester; RMAPI/ESPRI Implementation, Monroe County DSS |
Conduct an Environmental Analysis:
|
January 2016 | Lead(s): Erin Barry John Paul Perez Janet King (CM) Support: United Way, FLHSA and Others |
Milestone 2: A coordinated investment strategy is deployed to balance DSRIP Dollars & community investments
| Tasks/Sub–Tasks | End Date | Responsible |
|---|---|---|
| Conduct an analysis of cross–sector investment priorities and strategies including but not limited to DSRIP, RMAPI, ESPRI, Regional Economic Development, local insurers, local foundations, New York State, etc., to ensure all available resources are appropriately documented, leveraged and brought to bear. | January 2016 | Lead: Laura Gustin |
Build Financial Models to Guide Investments
Contract with CBOs for FLPPS project–related activities, as applicable |
February 2017 1st Round: Q12017 Ongoing |
Lead(s): John Paul Perez Erin Barry Courtney Spitz Carol Tegas |
Coordinated discussions with MCOs and ACOs to understand their priorities for Value Based Payment Arrangements, included in investment strategy
|
Ongoing | Lead: Carol Tegas Erin Barry In coordination with: Laura Gustin and United Way |
| Develop and deploy a coordinated Resource Development Strategy to fill funding gaps using new and diverse funding streams. (e.g. grant development) | February 2017 | Lead: Laura Gustin Erin Barry (coordination) |
Milestone 3: Social Services providers have a common understanding about the role, responsibility, risk and reward of participating in the FLPPS Integrated Delivery System.
| Tasks/Sub–Tasks | End Date | Responsible |
|---|---|---|
Use all influencers to educate CBO Executives, Boards and Staff on the importance of preparing for VBP through participation in DSRIP/FLPPS project and network engagement to transform and prepare
|
December 2016 – January 2017 January 2017 Ongoing |
Lead: Erin Barry Meredith Rutherford Laura Gustin John Paul Perez Support: CBO Advisory Council |
Milestone 4: Social Determinants of Health/Social Service Providers are included in the FLPPS Population Health Platform & Care Management Platform
| Tasks/Sub–Tasks | End Date | Responsible |
|---|---|---|
Begin creation of a digital directory of all prioritized social service providers in FLPPS region, leveraging 211 as applicable (Accountable Health Communities Grant requirement)
|
February 2017 Dec 2016 – Jan 2017 |
Lead: John Paul Perez |
Design and deploy data sharing agreements and patient consent forms
|
March 2017 | Lead: Jose Rosario, Sr. Director of IT and Analytics Coordinate With: Monroe County DSS (Integrated Eligibility), RMAPI/UW, RHIO, NYS DOH |
Right–size IT infrastructure across priority social service providers, as necessary
|
Q32016 – Q12017 Q12017 Ongoing |
Lead: Jose Rosario Coordinate with: RMAPI/UW, FLHSA, City of Rochester Innovation Team & Others |
| Standardized data collected and shared per evaluation strategy (see Milestone 5) | Q1, Q2 2017 | Lead: Jose Rosario Twylla Dillion |
Milestone 5: An evaluation strategy is designed and implemented, which includes measurement of program cost and benefit.
| Tasks/Sub–Tasks | End Date | Responsible |
|---|---|---|
Collect data from prioritized social service providers to measure impact of services and interventions.
|
March 2017 | Recommended Lead: Joint strategy between FLPPS/FLHSA/UW; Joint implementation between FLHSA/UW |
Milestone 6: Coordination and buy–in across key stakeholders and complimentary community initiatives, including: Providers (ACOs, and Independent Organizations), Insurers (MCOs), CBO´s, Local Foundations, Patients, RMAPI and ESPRI, FLHSA, Invest Health, Rethink Health, CMMI: Accountable Health Communities, CMMI: Practice Transformation, NYS Value–Based Payment Roadmap; Implementation of Home and Community-Based Waivers etc.
| Tasks/Sub–Tasks | End Date | Responsible |
|---|---|---|
Establish an Advisory Council to support the Strategic Work plan:
|
Inaugural Meeting held in September 2016; Permanent Council formed by end of January 2017 | Co–Leads: Erin Barry, and Laura Gustin, Integration |
Coordination with NYS Funded CBO Planning Grant
|
Ongoing | Erin Barry John Paul Perez Andrea Haradon |
Establish Intra–Agency MOUS between FLPPS and Strategic Partners, as applicable:
|
As–needed | Accountable: Carol Tegas, Executive Director (FLPPS) Lead: Erin Barry, Director of Strategic Community Initiatives (FLPPS) |
FLPPS LEADERSHIP & BOARD APPROVAL
Approved by FLPPS Board on December 7, 2016
| Title | Name | Date |
|---|---|---|
| Executive Director | Carol Tegas | 12/7/16 |
| Board Chair | Kathy Parrinello | 12/7/16 |
__________________________________________________________________
i Source: University of Wisconsin Population Health Institute. County Health Rankings 2013. Accessible at www.countyhealthrankings.org i
ii Department of Health DSRIP A Path toward Value Based Payment: Annual Update, June 2016: Year 2, New York State Roadmap for Medicaid Payment Reform June 2016, Page 42 ii
__________________________________________________________________
1. FLPPS is applying the RACI model to all work streams and departments (Responsible, Accountable, Consult and Inform). For the purposes of this document, the Responsible Lead(s) are defined as the "R" in the RACI model. Erin Barry is the defined "A" for the overall work plan and will work with other FLPPS members to accomplish deliverables. 1
2. Tier 3 CBOs (other than hybrids) and non–CBO Partners are managed by the FLPPS Central Operations Team, under Peter Bauman´s leadership (at the time this document was submitted to the State) 2
3. Some of the tasks included in the Short Term Milestones and Activities have been prioritized by FLPPS Leadership and will be included in "Immediate Priorities" section for completion in the December 2016, January 2017 timeframe 3
4. Dates are subject to change until Strategy goes through full planning cycle and approval of FLPPS Leadership 4
FLPPS 2nd Tier Funds Flow
December 21, 2016
| PPS Identification Information | Partner Information | Partner Funds Flow Data | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PPS ID | PPS Name | Partner Category | Entity ID | MMIS ID | NPI | CBO Tier for VBP | Partner Name | DY2, Q2 Quarterly Amount Update | Funds Flow DY2 – YTD | Funds Flow All DSRIP Periods |
| 9 | Finger Lakes Performing Provider Systems, Inc. | Clinic | E0176804 | A C CENTER INC | 24,142.00 | 24,142.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | E0230736 | ACTION FOR A BETTER COMMUNITY | 3,000.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1750593539 | Tier 3 | AIM Independent Living Center | 3,000.00 | 3,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | E0028175 | ALL METRO HOME CARE SERVICES OF NEW | 3,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0083104 | Tier 3 | ALLEGANY CO CHAP NYSARC SMP | 10,643.00 | 16,738.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0171131 | ALLEGANY CO COMMUNITY SVCS MH | 4,048.00 | 4,048.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Substance Abuse | E0237864 | Tier 3 | ALLEGANY COUNCIL ON ALCOHOL | 3,000.00 | 6,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0170710 | Tier 3 | ALLEGANY REHAB ASSOC MH | 38,703.27 | 71,442.27 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1013209253 | Tier 1 | ALLEGANY/WESTERN STEUBEN RURAL HEALTH NETWORK, INC. | 5,137.50 | 5,137.50 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Clinic | E0260739 | ANTHONY L JORDAN HEALTH CTR | 1,046,128.40 | 1,948,056.40 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 2 | Arbor Housing and Development | 3,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0012848 | Tier 3 | ARC OF MONROE COUNTY, THE | 8,459.28 | 11,459.28 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0323829 | Tier 3 | ARC OF ORLEANS COUNTY CSSZ01 | 7,625.00 | 7,625.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospital | E0262911 | ARNOT OGDEN MEDICAL CENTER | 702,478.39 | 1,372,734.39 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | Autism Up | 4,250.00 | 4,250.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0091545 | Tier 3 | BADEN STREET SETTLEMENT | 7,999.98 | 10,999.98 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | E0240231 | BETHANY NURSING HOME HRF | 2,625.00 | 5,625.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | E0268058 | BLOSSOM HEALTH CARE CENTER | 3,000.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | 1376948893 | Blossom Road Medicine PLLC | 6,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0103989 | Tier 3 | CAH HERITAGE CHRISTIAN SERVIC | 2,625.00 | 7,875.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1316914104 | Tier 1 | Canandaigua Emergency Squad | 5,250.00 | 5,250.00 | 5,250.00 | ||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | 1952442519 | Canandaigua Medical Group | 4,700.00 | 4,700.00 | 4,700.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | Canisteo (aka Bruce MacKellar MD PC) | 6,000.00 | 6,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1487649471 | Tier 3 | CAPABILITIES INC SMP | 2,000.00 | 2,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 3 | Catholic Charites of Steuben | 8,000.00 | 10,750.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0026257 | Tier 3 | CATHOLIC CHARITIES COMMUNITY | 5,000.00 | 47,741.35 | 75,149.35 | ||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0181893 | Tier 3 | CATHOLIC CHARITIES ROCHESTER | 3,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 3 | Cayuga Counseling Services, Inc. | 3,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1528383239 | Tier 3 | CDS Monarch | 7,625.00 | 7,625.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | Centers Health Care | 3,000.00 | 3,000.00 | 3,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0207097 | Tier 3 | CHEMUNG CO NYS ARC CHILDREN´S | 5,129.87 | 5,129.87 | 9,284.87 | ||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1225434491 | Tier 1 | COMPEER ROCHESTER, INC. | 3,000.00 | 3,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | Compeer, Inc. / NYS Programs | 5,000.00 | 8,000.00 | 10,750.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Substance Abuse | E0230733 | Tier 3 | COUNCIL ALCOHOL SUB ABUSE LIVINGSTN | 16,533.65 | 29,758.65 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | E0263637 | CREST MANOR LIVING & REHAB CTR | 3,974.55 | 6,974.55 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 3 | Daystar | 2,250.00 | 2,250.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | ´00711064´ | 1871573378 | DEAHN DALE L MD | 3,000.00 | 5,750.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Substance Abuse | E0070195 | DELPHI DRUG ALCOHOL COUNCIL | 8,163.43 | 11,163.43 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0156742 | Tier 3 | DICK VAN DYKE A T C | 3,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0169550 | Tier 3 | EAST HOUSE CORPORATION | 7,624.97 | 10,249.97 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1548416803 | Tier 3 | Epilepsy–Pralid,Inc. | 5,250.00 | 5,250.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | Episcopal Church Home | 2,500.00 | 5,500.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0315532 | ERIE COUNTY SOUTH EAST CORP V | 12,057.00 | 12,057.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | Exercise Express LLC | 6,000.00 | 6,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0240643 | Tier 3 | F L A C R A | 22,488.00 | 41,817.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | E0129684 | FAIRPORT BAPTIST HOMES ADHC | 2,250.00 | 5,250.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1417035387 | Tier 3 | Family counseling Services of Finger Lakes | 5,625.00 | 5,625.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0086000 | Tier 3 | FAMILY SER OF CHEMUNG CNTY MH | 82,116.53 | 153,076.53 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1326147968 | Tier 1 | Finger Lakes Ambulance | 4,750.00 | 4,750.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 3 | Finger Lakes Cerebral Palsy, Inc. | 2,625.00 | 5,625.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospital | E0061832 | FINGER LAKES MEDICAL GRP LLC | 56,871.38 | 107,370.38 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Clinic | E0038170 | FINGER LAKES MIGRANT HLTH | 207,540.91 | 392,971.91 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0037941 | Tier 3 | FINGERLAKES PARENT NTWRK RSP | 2,250.00 | 5,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | ´01058424´ | 1972572477 | FLENDER JOAN ELLEN MD | 25,743.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | E0263589 | GENESEE CNTY SNF BATAVIA | 5,000.00 | 5,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Substance Abuse | E0219856 | GENESEE COUNCIL ON ALCOHOLISM | 5,962.42 | 17,200.42 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 3 | Genesee County Chapter NYSARC, Inc. | 4,395.83 | 4,395.83 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | Genesee County Office for the Aging | 6,000.00 | 6,000.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0183386 | GENESEE CTY MH | 35,375.83 | 35,375.83 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0147071 | Tier 3 | GENESEE REG HOME CARE ONT CTY | 28,422.54 | 28,422.54 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | Genesee Valley Health Partnership | 11,000.00 | 11,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Pharmacy | E0262757 | GEROULDS PROF PHARM INC | 3,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | Grace Lutheran Residential Services | 2,250.00 | 5,250.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Case Management / Health Home | E0380015 | GREATER ROCHESTER HLTH HOME NETWORK | 25,864.29 | 25,864.29 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0335619 | Tier 2 | HEALTH HOME PARTNERS OF WNY LLC | 7,850.00 | 7,850.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | 1669865671 | HEALTH REACH PLUS | 10,000.00 | 10,000.00 | 10,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Non–Primary Care Provider (PCP) | Hickok Center for Brain Injury | 2,750.00 | ||||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 3 | Hillside Family of Agencies | 42,070.33 | 78,100.33 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | 1134477334 | His Branches Health Services – Grace Family Medicine | 24,929.68 | 24,929.68 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1073718011 | Tier 3 | Home & Health Care Services, Inc. | 5,125.00 | 5,125.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Substance Abuse | E0204306 | HUTHER–DOYLE MEM INSTITUTE | 62,603.34 | 112,327.34 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | ´03308183´ | Tier 3 | Ibero American Action League | 3,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | E0007172 | INNOVATIVE SERVICES INC | 3,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | Institute for Human Services, Inc. | 4,950.00 | 4,950.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | E0005457 | INTERIM HEALTHCARE OF ROCHESTER INC | 2,785.98 | 2,785.98 | 8,785.98 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | Irondequoit Ambulance, Inc | 5,000.00 | 5,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | 1164727475 | Irondequoit Pediatrics | 4,750.00 | 4,750.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | E0107158 | JEFFERSON FAMILY MEDICINE PC | 29,647.00 | 29,647.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | E0240871 | JEWISH HOME INFIRMARY NON OCC | 2,250.00 | 2,250.00 | 5,250.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Substance Abuse | E0157812 | JOHN L NORRIS A T C | 3,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospital | E0263739 | JONES MEMORIAL HOSPITAL | 40,780.24 | 75,549.24 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | ´02055278´ | 1629085592 | KASSAS MOHAMAD–ZAHI MUSTAPHA | 26,315.89 | 45,225.89 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | 1962417352 | Keuka Family Practice | 5,250.00 | 5,250.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | Keuka Housing Council | 5,625.00 | 5,625.00 | 5,625.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | ´01881025´ | 1962469387 | KILIMNICK JOSEPH B MD | 5,375.00 | 5,375.00 | 5,375.00 | ||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospice | E0338878 | L WOERNER INC | 16,755.63 | 27,183.63 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | Lake Plains Community Care Network, Inc. | 5,625.00 | 5,625.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0148197 | Tier 3 | LAKEVIEW MENTAL HEALTH ICM MH | 31,884.68 | 57,957.68 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 3 | Learning Disabilities of CNY /LDA Life and Learning Services | 8,000.00 | 11,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | E0263562 | LEROY VILLAGE GREEN RHCF INC | 3,000.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0001939 | Tier 3 | LIBERTY RESOURCES INC | 2,625.10 | 5,375.10 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1174951297 | Tier 3 | Lifespan of Greater Rochester, Inc. | 3,000.00 | 3,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0126055 | Tier 3 | LIFETIME ASSISTANCE INC HCBS3 | 12,231.25 | 23,480.25 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0085356 | LIVING OPP OF DEPAUL MH | 4,120.78 | 11,904.78 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | Livingston County Department of Social Services | 39,418.06 | 39,418.06 | 39,418.06 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1134294978 | Tier 3 | Loyola Recovery Foundation, Inc. | 34,946.80 | 34,946.80 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0263513 | Tier 3 | MARY CARIOLA CHILD CTR BROWNC | 3,000.00 | 6,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | 1225375470 | Medical Solutions Inc | 5,250.00 | 10,250.00 | 10,250.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | Mental Health Association of Rochester/Monroe County Inc | 6,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0086760 | MID ERIE MENTAL HEALTH SVC | 2,250.00 | 5,250.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | 1780935502 | Monroe Plan for Medical Care | 5,375.00 | 5,375.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | E0251627 | MOREHOUSE WILLIAM RAYMOND MD | 17,081.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospital | E0263732 | NICHOLAS H NOYES MEM HOSP | 46,174.04 | 86,216.04 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Clinic | NYS Vets & Pembroke Family Med | 10,999.98 | 10,999.98 | 10,999.98 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Clinic | E0016782 | OAK ORCHARD COMMUNITY HEALTH CTR | 2,867.00 | 142,612.46 | 311,967.46 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | 1205187002 | Ogden Pediatrics | 6,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0028423 | Tier 2 | ONONDAGA CASE MANAGEMENT INC | 1,594.00 | 1,594.00 | 1,594.00 | ||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Case Management / Health Home | E0099667 | Tier 3 | ONTARIO ARC | 12,068.05 | 18,766.05 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0263437 | ONTARIO CNTY DEPT OF M H | 8,218.40 | 8,218.40 | 8,218.40 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospital | Orleans Community Health – Medina Hospital Article 28 Clinic | 12,082.00 | 12,082.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0186041 | ORLEANS COUNTY COMM SVC MH | 26,840.65 | 26,840.65 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | 1851700264 | Pathway Houses of Rochester | 3,000.00 | 3,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | E0173809 | Tier 3 | PATHWAYS INC | 7,120.00 | 14,335.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0344096 | Tier 3 | PEOPLE INC CSSZ38 | 2,061.00 | 4,686.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | Perinatal Network of Monroe County | 5,625.00 | 5,625.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Substance Abuse | E0320685 | Tier 3 | RECOVERY COUNSELING, LLC | 2,125.00 | 4,875.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | RGRTA/Regional Transit Service | 6,000.00 | 6,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospital | E0268752 | ROCHESTER GENERAL HOSPITAL | 5,087,220.15 | 10,169,440.15 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 3 | Rochester Monroe Recovery Network Program (Center for Community Alternatives) | 2,250.00 | 2,250.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0263655 | Tier 3 | ROCHESTER REHABILITATION CTR | 4,826.00 | 9,417.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | Rochester School of the Holy Childhood, Inc | 2,813.00 | 5,438.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | E0308694 | RUSHVILLE HEALTH CENTER INC | 70,055.42 | 70,055.42 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | S2AY Rural Health Network, Inc | 11,000.00 | 11,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | Samaritan Women | 5,250.00 | 5,250.00 | 5,250.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0340198 | Tier 3 | SENECA CAYUGA COUNTIES CHAPTER NYSA | 2,850.00 | 2,850.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Clinic | 1588809636 | SENECA COUNTY HEALTH DEPARTMENT | 5,750.00 | 5,750.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospice | E0202369 | SOUTHERN TIER HOSPICE/PALL CA | 6,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | E0206493 | SOUTHERN TIER PEDIATRICS | 234,993.65 | 431,331.65 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospital | E0262914 | ST JAMES MERCY HOSPITAL | 85,868.00 | 166,553.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0009228 | Tier 3 | ST JOSEPHS VILLA OF ROCHESTE | 4,173.94 | 8,118.94 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | St. Ann´s Community | 4,966.00 | ||||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Clinic | E0263648 | STEUBEN BOARD OF SUPERVISO CO | 66,945.45 | 66,945.45 | 187,641.45 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | CBO | Steuben County Chapter, NYSARC Inc | 7,156.00 | 12,782.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | 1841364288 | Stony Brook Pediatrics | 26,547.20 | 26,547.20 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospital | E0271171 | STRONG MEMORIAL HOSPITAL | 3,851,685.32 | 7,698,370.32 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0301217 | Tier 3 | SUBURBAN ADULT SERVICES INC SPT | 2,475.00 | 5,475.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0230730 | Tier 3 | SYRACUSE BRICK HOUSE INC | 2,625.00 | 2,625.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | The Center for Youth | 5,000.00 | 5,000.00 | 5,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1033541107 | Tier 3 | The Community Place of Greater Rochester Inc. | 2,250.00 | 2,250.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0368462 | Tier 3 | THE HEALING CONNECTION INC | 6,000.00 | 6,000.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | E0160154 | Tier 3 | UCP DIAGNOSTIC AND TRT CTR | 14,555.00 | 17,555.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1619062304 | Tier 3 | Venture Forthe | 2,625.00 | 2,625.00 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Primary Care Provider (PCP) | Virdee, Tejinder | 2,625.00 | 5,625.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Practitioner – Non–Primary Care Provider (PCP) | Visiting Nurse Assoc. Batavia | 6,000.00 | 6,000.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | 1336328129 | Wayne Behavioral Health Network | 5,250.00 | 5,250.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Case Management / Health Home | E0013162 | Tier 3 | WAYNE CO CHP NYSARC INC | 12,435.15 | 19,494.15 | |||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | E0261361 | WAYNE COUNTY NURSING HOME | 6,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | 1851490411 | Wayne County Public Health | 6,000.00 | 6,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 3 | Western New York Independent Living (dba Independent Living of the Genesee Region) | 7,624.98 | 10,624.98 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Nursing Home | E0139286 | WNYS VETERANS HM AT BATAVIA | 5,625.00 | 5,625.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Hospital | E0268011 | WYOMING COMMUNITY HOSP CO | 22,519.46 | 39,438.46 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Mental Health | 1285803239 | Wyoming County Mental Health | 7,250.00 | 7,250.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | All Other | Wyoming County Office of the Aging | 2,625.00 | 2,625.00 | |||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | Tier 1 | YMCA of Greater Rochester | 5,250.00 | 8,000.00 | ||||
| 9 | Finger Lakes Performing Provider Systems, Inc. | Community Based Organizations | 1417028622 | Tier 3 | YWCA OF ROCHESTER AND MONROE COUNTY | 2,750.00 | 2,750.00 | |||
Follow Us