DOH REVIEW AND EXECUTIVE SUMMARY OF PPS PRIMARY CARE PLAN
- Response is also available in Portable Document Format (PDF)
Millennium Collaborative Care
Igniting Healthcare Change in WNY
DSRIP Mid-Point Assessment
PPS Response to IA Recommendations
December 21, 2016
1461 Kensington AveBuffalo, New York 14215
716.898.4950
millenniumcc.org
Contents
- Introduction
- IA Analysis: Organizational Assessment
- 2.1 PPS Governance
2.2 Financial Sustainability and Value–Based Payment
2.3 Funds Flow
- 2.1 PPS Governance
- IA Analysis: Project Assessment
- 3.1 Partner Engagement
1 Introduction
- The Independent Assessor (IA) has completed its Mid–Point Assessment review and released its recommendations for public comment. This document will serve as the PPS´ opportunity to respond to the Ia´s recommendations and other commentary as included in the report in an effort to refute some of the recommendations and provide additional information and clarification for PPS partners in relation to the observations and other items noted within.
- The PPS appreciates the opportunity to provide a response that will be reviewed by the IA and considered in the development of the final recommendations to be submitted to DOH.
2 IA Analysis: Organizational Assessment
2.1 PPS Governance
PPS Administration and Project Management Office (PMO): Implementation and Administration Spend
IA Commentary
- "In reviewing the PPS spending on administrative costs, the IA found that Millennium had reported spending of $6,487,040.00 on administrative costs compared to an average spend of $3,758,965.56 on administrative costs for all 25 PPS. As each PPS is operating under different budgets due to varying funding resources associated with the DSRIP valuations, the IA also looked at spending on administrative costs per attributed life, relying on the PPS Attribution for Performance figures. The IA found that Millennium spends $25.67 per attributed life on administrative costs compared to a statewide average spend of $24.23 per attributed life on administrative costs." (p. 8)
PPS Response
- Per review of the calculation in determining the total administrative spend of the PPS, it was noted that a transposition error in the DY2 Q2 Quarterly Report resulted in a significant inflation of the $6,487,040 amount that was reported as administrative in the report. The PPS erroneously switched the amounts reported as "Implementation" and "Administration" in the Budget Reporting module. These categories were reported as $1,422,426 and $3,275,009 for Implementation and Administration, respectively, when it should have been reflected as $3,275,009 and $1,422,429, respectively. The amounts reported in the PIT tool appropriately reflect the funds flowed to our partners. Once this correction is made, the total amount of Administration would be $4,634,457 as reported through DY2 Q2. The PPS recognizes it is slightly above the statewide average, however, there could be a number of factors skewing the average as there are many differences in size, staffing, and structure among the 25 PPSs. On the basis of a normalized attribution, the total administrative spend per attributed life would be $18.34, in comparison to the statewide average of $24.23 per attributed life, which Millennium believes is a more accurate representation.
- Subsequent to the issuance of the initial Mid–Point Assessment Recommendations, the PPS was able to update the DY2 Q2 report in MAPP to reflect the proper amounts of its Administrative spend.
Millennium is requesting that the final report be updated to reflect the correct administrative costs and spend per attributed life as outlined above.
PPS Administration and PMO: PMO Spend
IA Commentary
- "Looking further at the PPS fund distributions to the PPS PMO, Millennium distributed $6,837,028.51 to the PPS PMO out of a total of $16,916,710.23 in funds distributed across the PPS network, accounting for 37.76% of all funds distributed through DY2, Q2. Comparatively, the statewide average for PPS PMO distributions equaled $5,966,502.64 or 42.85% of all funds distributed." (p. 9)
PPS Response
- Per review of the calculation in determining the total PMO spend of the PPS, it was noted that a transposition error was made in this section of the report resulting in the inflation of the amount that was reported as the PMO spend. The amount reported by the IA in this section was $6,837,028.51 when it should have been $6,387,028.51. This appears to have been a typographical error made by the IA. The amount reported in the table on page 11 is correct. The percentage calculation reported in the referenced paragraph on page 9 is also correct.
Millennium is requesting that the amount in the final report be updated to report actual PMO spend.
Community–Based Organization (CBO) Contracting
IA Commentary
- "While the PPS indicated that it would be contracting with and compensating 21 Community Based Organization partners, the funds distributed to date have been primarily paid to six organizations. It will be important for the PPS to expand its fund distributions across all of its CBO partners to maintain engagement of these key partners." (p. 9)
PPS Response
- Millennium is working with and compensating more than 21 CBOs, each of whom participate in one or more projects and submit patient engagement registries. This is not apparent from the funds flow reporting provided through the PIT.
- For some CBOs, we have a MPA in place but report funds flow to them under what we consider their "primary" provider type designation (typically primary care or behavioral health). For others, we are flowing funds to them via a contract with another organization (e.g., through our lead entity, ECMC), and only the top–level funds flow is reported in the PIT. (The limitations of reporting funds flow via the PIT, which contribute to a skewed picture of funds distribution, are discussed further in section 3.3, Funds Flow.)
- The following CBOs have received or will receive funds from Millennium:
- Allegany Council on Alcohol and Substance Abuse*
- Buffalo Federation of Neighborhood Centers Inc.
- Buffalo Municipal Housing Authority
- Buffalo Prenatal-Perinatal Network
- Buffalo Psychiatric Center
- Cattaraugus Council on Alcohol and Substance Abuse*
- Chautauqua Council on Alcohol and Substance Abuse*
- Community Action Organization of Erie County Inc.
- Community Health Center of Buffalo
- Community Services for the Developmentally Disabled
- Compeer*
- Crisis Services
- Erie County Council for the Prevention of Alcohol and Substance Abuse*
- Erie Niagara AHEC
- Evergreen Health Services
- GBUAHN Health Home
- Genesee Council on Alcohol and Substance Abuse*
- Healthy Community Alliance
- Horizon Health Services
- Jericho Road Community Health Center
- Lake Plains Community Care Network
- Mental Health Association of Erie County*
- Native American Community Services*
- Niagara Falls Health Home
- Northpointe Council
- People Inc.
- Person–Centered Services of Western New York
- Planned Parenthood
- Prevention Focus*
- Rural AHEC
- Southern Tier Community Health (Universal Primary Care)
- Spectrum Human Services
- The Chautauqua Center
- The National Witness Project, Inc.
- The Resource Center
- Western New York Independent Living*
- Western New York United Against Drugs and Alcohol*
* Funds are flowed to these CBOs through our partnership with neighboring PPS Community Partners of Western New York on the Mental, Emotional, and Behavioral Well–Being project (4ai).
Millennium requests that the CBO portion of the recommendations be amended to reflect that the PPS is contracting with more than 21 CBOs.
2.2 Financial Sustainability and Value–Based Payment
Financial Sustainability
IA Commentary
- "The Financial Committee created a plan to identify and assist financially fragile partners. They performed an initial assessment in DY1 and created a ´watch–list´ that included 4 partners who were all identified as VAPAP, and all had corrective action plans in place. They meet with these partners quarterly. The PPS is currently preparing a second annual assessment to be conducted in the Fall of 2016.
- "The IA encourages the PPS to continue monitoring its partners and develop creative solutions to address its financially fragile partners." (p. 10)
PPS Response
- The PPS has and continues to meet its requirements regarding the financial viability of its partners and evaluate ways in which the PPS can assist those who may be financially unstable. The Finance Committee of the PPS has created a policy and procedure for this oversight. Each PPS Partner, upon meeting certain review criteria, will be subject to an initial evaluation and subsequent periodic reviews of financial performance for the specific purpose of evaluating financial sustainability. The financial performance metrics utilized are consistent with the standard DSRIP lead entity application process. A color–coded "concern score" is determined by Millennium management through the review of audited financial statements and other relevant supporting documentation. A red, yellow, or green score will then be assigned to each provider based on the established criteria. Green will indicate "no concern;" yellow will indicate "some concern;" and red will indicate "much concern" along with recommendations for the Watch List. Watch List members are PPS partners that do not meet the established ratio targets or who automatically qualify for Watch List status based on certain circumstances (like bankruptcy filing or being IAAF/VAPAP recipients). This review process for evaluated partners will occur no less than annually.
- Once the sustainability review process is initially completed for each review period, the results are reported to the Finance Committee. Furthermore, the Director of Finance, Executive Director, and Finance Committee Chair meet with the executive leadership of each Watch List entity in order to evaluate their membership on the list and to review their transformation and survivability plans.
- Of the four entities that were named to the Watch List for DY1, all have significant transformation plans to which they appear to be making substantial progress on. Additionally, all of the entities have established varying relationships with a large regional health system in this area to support certain aspects of said transformation. Furthermore, the four entities on this list have also received considerable support from NYS on their transformation, receiving awards of approximately $65 million in total from the Capital Restructuring Finance Program. The PPS is working directly with these entities to implement DSRIP– related initiatives and assist in their already–established transformation plans, if such circumstances are presented.
Value Based Payments (VBP)
IA Commentary/Recommendation
- "The PPS has established a VBP Subcommittee within the Finance Committee. This subcommittee has 4 workgroups to address: 1. MCO strategy, 2. Education, 3. Payment Models/Partner Readiness, 4. Communication. At this time, the PPS indicated that it has two partners that are exploring participation in a VBP Pilot, however the IA could not confirm that these partners had moved forward in that process based on the information available. Additionally, Millennium stated that it intends to incorporate VBP requirements in to their Master Participation Agreements with partners. Likewise, the IA was not able to confirm the inclusion of these requirements in the Master Participation Agreements." (p. 10)"The IA recommends that the PPS establish a plan to further educate and support their partners move toward VBP arrangements." (p. 26)
PPS Response
- Value–Based Payments Sub–Committee
- The Value–Based Payment Sub–Committee ("Sub–Committee") was established by the Finance Committee to align with PPS management as it embarked on the initiative to lead value based contracting arrangements. The primary responsibility of the Sub–Committee is to assess readiness, educate partners and offer expertise to the Finance Committee, management and partners on a value based contracting strategy. The Sub–Committee is comprised of a diverse group of representatives from varying provider and service types with a wide range of experience. Finance Committee members may participate on the Sub–Committee at any time and will serve as the Steering Committee of the group. The Sub–Committee established four workgroups to deal with the various education topics and strategies and balance the initial workload of the Sub–Committee. These workgroups include: Education, Communication, Payment Models/Partner Readiness, and Managed Care Organization (MCO) Strategy.
- Education Workgroup: The purpose of the Education Workgroup is to:
- Create an educational tool for explaining New York State´s VBP goals, including, but not limited to, summarizing the state´s roadmap and breaking it down into digestible portions to maximize learning, explaining the various types and levels of VBP contract approaches, etc.
- Describe how VBP can drive additional revenues.
- Consider various stakeholders when developing content and venue.
- The Education Workgroup has since developed an initial easy–to–understand VBP educational presentation and created a plan to establish an ongoing education library or best practices, pilots, and examples to progressively educate and engage stakeholders. Potential future courses include: Educating the Consumer, Social Determinants of Health, Understanding Types of VBP, Reporting, Understanding Risk, Understanding Total Cost of Care, MCO Contracting and Penalties, Attribution and Target Budgets, Implications of VBP for CBOs, etc. A preliminary course catalog and meeting minutes are available to the IA upon request.
- Additionally, the PPS–recognizing that education may be the most important piece of successfully implementing VBP–has requested feedback from the Sub– Committee and its partners for what educational needs they have and courses they would like to see established. This feedback has been requested in Sub– Committee meetings, one–on–one interactions, and in a quarterly newsletter communication from the PPS.
- Communication Workgroup: The purpose of the Communication Workgroup is to:
- Develop a communication plan to inform the PPS partners regarding the VBP program and milestone requirements
- Identify communication tools, including the frequency of such communications, and content
- Coordinate the communications for the Sub–Committee with PPS management
- The Communication Workgroup has since identified, with the assistance of PPS management, the communication content and priorities, communication vehicles and strategies for VBP education and potential programs to benefit stakeholders, and a strategy to gain participating in the readiness assessment survey. Minutes of the workgroup meetings are available upon request from the IA.
- Additionally, on a quarterly basis, a member of the Millennium leadership team, composes a VBP–related messages to keep partners up to date on VBP happenings. A VBP–specific email address has also been established for two–way communication between the PPS and partners and a separate section of the PPS website has been created as a VBP resource.
- Payment Models/Partner Readiness Workgroup: The purpose of the Payment Models/Partner Readiness Workgroup is to:
- Design plan to assess readiness of providers in PPS network to engage in various levels of VBP contracting, including development of provider assessment instrument
- Work with communication workgroup to develop plan for assessment questions
- Evaluate VBP models utilizing NYS VBP roadmap
- Determine VBP options available to providers
- The Payment Models/Partner Readiness Workgroup has since established and distributed partner readiness assessment. The PPS is currently pursuing non– responders. Additionally, the results of the assessment are being used not only to assess initial readiness but also to facilitate conversations related to VBP and future strategic initiatives with our major partners. A meeting will be arranged with those organizations to facilitate this dialogue. Millennium has also begun these in–person meetings with partners discussing each organization´s progress towards VBP, readiness, and how the PPS can act as a resource for VBP implementation.
- Managed Care Organization (MCO) Strategy Workgroup: The purpose of the MCO Strategy Workgroup is to:
- Create formal structure to work with MCOs on development of VBP payment program
- Develop written MCO strategy to be presented to and approved by Finance Committee and Board of Managers
- Develop principles to achieve 90% VBP across network by DSRIP Year 5
- Develop VBP transition plan
- The MCO Strategy Workgroup has since begun identifying strategies to engage stakeholder and MCOs in pilot programs, worked with management in brainstorming for monthly MCO meetings, created guiding principles, and developed an initial draft MCO strategy. Furthermore, the group, in conjunction with management, worked to coordinate an "All MCO" meeting bringing together three of the four MCOs that the PPS works with to discuss VBP at a high level including: common goals, standardization, MCO and partner readiness, priorities for payment models, and data. It is the goal of the PPS to work with the MCOs and strategize, as much as possible, to align and assist each other with the goals of VBP and the Roadmap. Minutes of the workgroup meetings are available upon request from the IA.
- Millennium Management
- External to the above–referenced committees and workgroups, Millennium management has taken a number of steps to establish the infrastructure needed to support our partners in their transitions into VBP. This first includes building the resources to provide administrative support, analytics, and educational tools to the PPS´ partners. The PPS will continue to facilitate a dialogue with its regional payers to create VBP pilots targeted at high utilization populations with minimal levels of risk to help its partners be successful with VBP arrangements and gain experience to transform to higher levels of risk.
- Additionally, members of Millennium management will be meeting with identified partners, whereby the results of readiness assessments will be reviewed, and a VBP transition plan will be discussed for each organization. The plan will include the potential VBP arrangements, achievable timelines, gaps in achieving goals, and mitigation strategies to reduce such gaps. The plan will also address organizational administrative capacity, "buy–in", clinical integration, and technology capabilities to create an individual organizational roadmap to achieve the PPS VBP goals. The PPS will focus on maximizing clinical integration capabilities, providing analytics, and network support for its partners.
- Furthermore, the PPS will explore the feasibility for Millennium to form a contracting vehicle. Exploration of collaborative data sharing strategies with the MCOs will also be investigated. A task force has been created with Millennium staff, executives from major partners, and members of the Millennium Board of Managers Executive Committee, with the action steps to be accomplished. The task force is to perform due diligence, develop planning documentation, and socialize recommendations with relevant governing boards, based on direction. Further detail and organizational structure will be developed to include accountabilities, resource effort, and appropriate timelines.
- Master Participation Agreements
- Millennium´s Master Participation Agreements ("MPAs") govern its contractual relationships with its safety net partners. In each MPA for the DSRIP Year 2 timeframe, 10% of the total award for each organizational type was designated for VBP preparation (see Figure 1).
Figure 1. Screenshot of a behavioral health MPA showing that 10% of payment to Millennium´s
behavioral health partners is allocated for VBP preparation. The same item is included for all provider types.
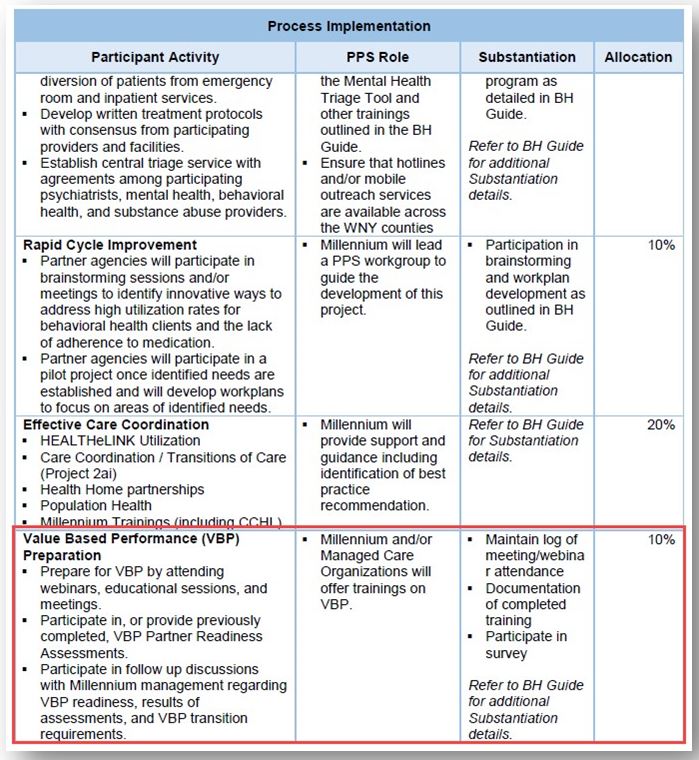
The requirements include attending VBP webinars, educational sessions and meetings, participating in or providing previously completed readiness assessments, and participating in discussions with Millennium management regarding VBP readiness, results of assessments, and VBP transition requirements (see Figure 2).
Figure 2. Screenshot from the acute care Reference Guide detailing the VBP activities required
of partners. The same VBP activities are required of all partners.
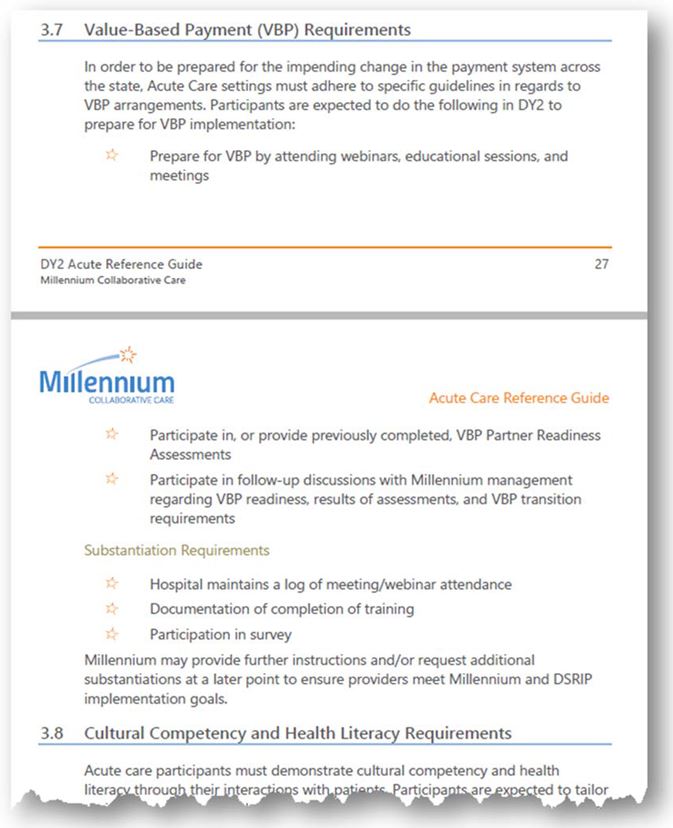
The potential value for MPA awardees is approximately $1.2 million for DSRIP Year 2. All MPA exhibits and reference guides are available upon request of the IA.
Millennium is requesting that the comments relating to the lack of inclusion of VBP requirements into the MPA be revised based on the information outlined above. Millennium would also like the IA to reconsider the inclusion of VBP as a formal organizational recommendation in the final report, in light of the substantial activities that have been outlined in our comments that do not appear to have been fully articulated in the initial review.
- VBP Pilot
- Millennium has been involved in facilitating the potential engagement a number of partners in the NYS VBP pilot from the time of its formation. Throughout the transition of the program, Millennium has worked with said partners and KPMG to provide PPS assistance and resources where available and when applicable. We are also actively engaged with a number of partners around the identification of additional VBP programs. Verification of our participation in the pilot process can be confirmed by KPMG and the DOH. The PPS will solicit verification of our participation from our provider partners upon request of the IA.
2.3 Funds Flow
IA Commentary
- "In further reviewing the Millennium funds flow distributions, the distributions are largely directed towards the PPS PMO, Hospital, and CBO partner categories, with 61.50% of the funds being directed to those three partner categories. While the PPS has distributed funds to most partner categories, the limited amount of funds distributed to PCP partners is an area the PPS could improve upon in future funding distributions. It will be important that these key partners remain engaged to ensure the successful implementation of the DSRIP projects." (p. 11)
PPS Response
- The funds flow by partner type as reported in the PIT Tool can be misleading for a number of reasons.
- Primary Care Designation: The Primary Care designation in the PIT is for individual providers ONLY. The PPS, at this time, will send aggregated payments associated with primary care performance to a group, clinic, or employment entity (i.e., hospital). It heavily supports primary care clinics as they are the cornerstone of the transformation initiatives to which DSRIP is based upon. For example, the DSRIP Year 1 and Year 2 MPA allocations for primary care were approximately $3.4 million and $4.3 million, respectively, which is 34% of the total funds allocated to our partners for years 1 and 2. This funding for these years for primary care clinic locations is associated with 277 individual providers. It is the position of the PPS that it will fund organizations directly to transform their practices to implement the requirements of the MPAs and reward the successful completion of DSRIP–related milestones.
- Improper Designations in the PIT Tool: A number of PPS partners are misclassified in the PIT Tool. For example, a partner may have been listed as an Additional Provider, as they were not included in the PIT or fall into another designation as that was the only available choice for the PPS to make for that organization.
- For example, the DSRIP Year 1 MPA allocation, based on Millennium classifications, were approximately:
| Primary Care | $ 3,435,000 |
| Home Health Agencies | $ 705,000 |
| Behavioral Health | $ 2,060,000 |
| Developmental Disability Organizations | $ 343,000 |
| Hospital | $ 1,845,000 |
| Skilled Nursing Facilities | $ 1,740,000 |
| Note: DY 1 allocation payments were made from DY2Q1-DY2Q3. | |
The same allocations, based on the designations in the PIT Tool, would be mapped
to the following provider categories:
| Clinic | $ 1,234,000 |
| Nursing Home | $ 715,000 |
| All Other | $ 1,225,000 |
| Substance Abuse | $ 343,000 |
| Mental Health | $ 1,922,000 |
| Hospital | $ 2,349,000 |
| Additional Provider * | $ 2,340,000 |
| * May include multiple designations like clinic, hospital, skilled nursing, etc. | |
- Additionally, in some cases, payments for multiple allocations (primary care, skilled nursing, hospital, etc.) would be made to one legal entity. Generally, the highest rollup in these instances is at the hospital level, which can skew the perception of where funds are flowing.
Millennium is requesting that the PCP dollars be revised to reflect the actual dollars associated with these providers or a comment be included in the final report indicating that the current PIT tool may require reporting in a manner that is not fully reflective of the actual dollars associated with primary care performance and requirements.
3 IA Analysis: Project Assessment
3.1 Partner Engagement
IA Commentary/Recommendation
- "As the data in Figures 8 through 14 above indicate, the PPS has engaged network partners on a limited basis for each of the projects highlighted. Of further concern is the limited engagement of PCPs across multiple projects. The PPS has made significant commitments to engage PCPs across each project, up to 620 PCPs for project 2.a.i., yet has only indicated the engagement of 115 PCPs for any project through the DY2, Q2 PPS Quarterly Report. For project 3.a.i., the PPS committed to engaging 107 Mental Health partners and 571 PCP partners to implement this significant project, however, through the DY2, Q2 PPS Quarterly Report, the PPS has indicated engagement of eight Mental Health partners and zero PCP partners. This lack of partner engagement across projects presents a significant risk to the PPS´ successful implementation of the DSRIP projects.
- "Of the projects highlighted in the tables above, only project 3.b.i. was also highlighted for the PPS failure to meet Patient Engagement targets consistently through the PPS Quarterly Reports. The combination of the PPS failure to meet Patient Engagement targets and the limited Partner Engagement across project 3.b.i indicates an elevated level of risk for the successful implementation of these projects." (p. 21)
- "The PPS must develop a plan for more actively engaging its network partners across all projects to ensure the successful completion of project milestones and meeting all DSRIP performance goals." (p. 26)
PPS Response
- Millennium has made a significant investment in engaging our network partners, and primary care providers in particular. There are several reasons this high level of engagement is not apparent.
- As with CBO engagement and funds flow, the true extent of provider engagement is not well communicated via the PIT. We report funds flow (and participation) at an organizational level, so while a practice may have dozens of physicians associated with it and engaged in our projects, only one entity is marked in the PIT as participating. For example, while it appears we have only engaged eight mental health partners, those organizations represent at least 66 individual providers. The same is true for primary care: we have contracts with safety net practices which represent many individual providers.
- In the absence of satisfactory guidance around how partner engagement is defined and substantiated (particularly in cases without provider–type–specific milestones), the PPS adopted an intentionally conservative approach to reporting engagement. Our focus when completing the PIT was mostly limited to capturing funds flowed.
- In the quarterly reporting cycle, there appeared to be little value to reporting incremental progress towards engagement, and no consequence for not doing so. No AV or payment is tied to incremental provider engagement and the interim targets previously established were removed-points and dollars are only earned when milestones/projects are completed. Given the incredible quantity of mandatory information PPSs report, it seemed irresponsible to expend great effort to report non–value–driving information.
- For all these reasons, and because incremental progress towards provider engagement was not identified as one of the criteria for mid–point assessment, we did not make a concerted effort to capture all providers engaged with all projects every quarter.
- The PPS subsequently made a concerted effort to report all providers that are participating in all projects in an updated PIT file which is being provided to the IA separately. The new PIT more accurately reflects the current scope of provider engagement across projects at the individual level, not just the group level. Our quarterly updates to the PIT will continue to detail individual providers´ participation.
- Cross–project participation is expected of our partners. Our MPAs specify which projects (and workstreams) each provider type must participate in. For example, primary care physicians are required to participate in the following:
- Integrated Delivery System (IDS) (Project 2ai)
- CVD Management/Million Hearts® (Project 3bi)
- Primary Care and Behavioral Health Integration (Project 3ai)
- Patient Activation Measures (PAM)® (Project 2di)
- Emergency Department Care Triage (Project 2biii)
- Maternal and Child Health (Project 3fi) (if applicable)
- Cultural Competency and Health Literacy
- Value–Based Payment
- Workforce
Millennium is requesting that the partner engagement data be revised to reflect the updated PIT tool. Millennium would also like the IA to reconsider the inclusion of partner engagement as a formal project recommendation in the final report, in light of the revised data.
Follow Us