DOH REVIEW AND EXECUTIVE SUMMARY OF PPS PRIMARY CARE PLAN
- Response is also available in Portable Document Format (PDF)
COMMUNITY PARTNERS OF WNY
Performing Provider System
December 21, 2016
Ms. Megan Rurak & Mr. Edward McGillPublic Consulting Group
99 Washington Avenue, Suite 704
Albany, NY 12210
Sent via email to dsrip_midpoint@pcgus.com
Dear Ms. Rurak and Mr. McGill:
Thank you for the opportunity to respond and give comment to the "DSRIP Independent Assessor (IA) Mid–Point Assessment Report" for Community Partners of Western New York.
Attached are our itemized comments with originating page numbers referenced for ease of review. Thank you for your consideration of our comments and please contact us with questions or concerns at awhitestorfer@chsbuffalo.org or pgunning@chsbuffalo.org
Thank you,
Amy White–Storfer, MBA, PMP
Director, Project Management Office
Phyllis G.M. Gunning, MPH
Director, Clinical Programs
I. Introduction
Community Partners of WNY (also known as "Sisters of Charity Hospital Performing Provider System (PPS)") appreciates the opportunity to respond to the "DSRIP Independent Assessor (IA) Mid–Point Assessment Report" for Community Partners of Western New York (CPWNY). The following summary is compiled from input by the CPWNY Project Management Office (PMO) staff and key project stakeholder input.
II. Recommendations and Responses
A. Organizational Recommendations (p 28):
Partner Engagement
Recommendation 1: "The IA recommends that the PPS develop a strategy to increase partner engagement throughout the PPS network. The limited partner engagement across multiple projects is a significant risk to the ability of the PPS to implement its DSRIP projects and meet the DSRIP goals."
CPWNY Response: The PPS acknowledges the IA´s recommendation and is developing a plan to address this area of need. In addition, the PPS requests a formal definition universally applicable to all PPS´s from the IA and New York State Department of Health on "partner engagement" in order to comply with this recommendation.
Background Information: The PPS acknowledges that the Mid–Point Assessment reviews materials for 6 quarters of a 20 quarter project. Early assessments about partner engagement show expected gaps in our PPS goals to gain network participation and a concerted effort to address these gaps is underway.
The PPS has created a structured definition of engagement in order to begin measuring partner engagement across projects. PPS teams across the State must define their own meaning for engagement in lieu of a formal definition from the IA or its designees.
Financial Sustainability and VBP
Recommendation 1: "The IA recommends that the PPS establish a plan to further educate and support their partners move toward VBP arrangements."
CPWNY Response: The PPS requests that the IA removes and omits all recommendations related to VBP planning from the IA report.
Background Information: The PPS understands and values the work required to support its network efforts to obtain value based contracts and has made significant progress to that end. It was understood, however, that the VBP plan milestone had been delayed. The PPS received initial communication on August 29, 2016 regarding the delay in final guidance from NYS on value based payment efforts. The PPS received final revised guidance from the New York State Department of Health on December 9, 2016. Although the PPS had started to formulate the plan as part of its work in early DY2, PPS teams were instructed not to submit the plan on the MAPP tool under Financial Stability Milestone 4 until final guidance was supplied.
A brief overview of the PPS structure and its plans to support the network is provided here for background. These plans and efforts will be submitted formally as part of the new guidance received by the PPS on December 9, 2016:
There are two major sets of physician teams inside Community Partners of WNY PPS. First, Catholic Medical Partners (CMP) IPA is approximately 990 independent primary care physicians, pediatricians and specialists. Second, the Chautauqua County Health Network (CCHN) is a health care innovations organization partnering with CPWNY to provide primary care support to key practices that serve large portions of the Medicaid population in Chautauqua County. Additionally, CCHN provides practice level support for key projects of CPWNY.
Both groups already participate in value based payment (VBP) arrangements either directly or through IPA arrangements. Currently, CMP is the only member of the PPS participating in VBP arrangements targeted to the Medicaid managed care population. CMP has approximately 30,000 Medicaid patients enrolled in its provider network, who are part of existing health plan contracts. These contracts are being converted into Value Based Payment (VBP) arrangements with a planned complete date of DY2 Q4.
Members of the CMP executive team meet regularly with MCOs in the local community, including Fidelis Care, Independent Health Association (IHA), YourCare, HealthNow NY, and WellCare. They represent the primary care providers within their network, as well as other types of providers. CMP will use its experience with VBP to educate and guide the PPS partners, including primary care providers, through the transition to VBP.
Of the regional MCOs, CMP currently participates in VBP arrangements for the Medicaid patient population with:CCHN will work with its physician partners to obtain VBP for their Medicaid populations independently of the work of CMP. CCHN´s contracting entity is their IPA, the Chautauqua Integrated Delivery System (IDS). IDS has plans to pursue VBP contracts for Medicaid lines of business for its provider members and can serve as a guide as other partner´s transition to VBP. CCHN has been educating providers on VBP programs and their potential impacts. This spring, CCHN will hold a county–wide educational event that will highlight initiatives available to providers, as well as provide tools to remain viable and effective in this environment.
- Fidelis Care, serving 25,000 PPS patients
- Independent Health Association, serving 17,000 PPS patients
- WellCare, a new payer in the region building its patient market share.
CPWNY PMO staff has already begun providing guidance and mentoring, to PPS partners to educate them about being engaged in contracting with Medicaid MCOs through educational sessions at our PAC meetings and online videos. CPWNY will be expanding our efforts in line with the updated guidance from the DOH with focused attention on WCA Hospital, Bertrand Chafee Hospital, Medina Hospital, and other CBO partners including but not limited to our behavioral health partners. CPWNY will also continue to support the CCHN team in pursuing VBP arrangements, including risk based value added contracts, for its IPA, the Chautauqua Integrated Delivery System.
CPWNY will continue to build partnerships with the CMP IPA and its existing VBP agreements. This will include working with CMP IPA´s membership committee to determine the appropriate recruitment of new members to the CMP IPA so they may participate in the VBP arrangements in place now and in the future.
The PPS has created a structured definition of engagement in order to begin measuring partner engagement across projects. PPS teams across the State must define their own meaning for engagement in lieu of a formal definition from the IA or its designees.
B. Project Recommendations (p 28–29)
B.i.) Project 2.b.iii.: ED care triage for at–risk populations
Recommendation 1: The IA recommends the PPS create a systematic process of triaging patients who are not linked to a Health Home, to a PCP in order to (1) Increase engagement of a broad patient population; (2) Meet patient engagement targets; and (3) Ensure access to services before getting linked to a Health Home.
CPWNY Response: The PPS requests that the IA rewords the recommendation to allow for flexibility in PPS planning, such as "The IA recommends the PPS create a systematic process of triaging patients who are not linked to a Health Home, to a PCP in order to (1) Increase engagement of patients who visit the ED with low acuity complaints. (2) Meet patient engagement targets; and (3) Ensure access to services before getting linked to a Health Home." Additionally, the PPS requests clarity on this recommendation.
Background: The PPS does not dispute the recommendations listed above, as the PPS already has reported and identified these needs and is actively working on developing new process flows to address them. It is important to note, however, that in the PPS´s original implementation plan, the PPS designed process flows surrounding referrals of all potential patients to the Health Homes. This referral process to Health Homes was used in the original projection of patient engagement numbers.
In June 2016, clarity on the engagement definition was finalized and distributed by NYS, which removed a large source of potential engagement numbers for the PPS. This new rule states that new referrals can not to be counted in patient engagements, as only patients linked to a Health Home at the time of ED admission could be counted. This finalized definition required the PPS to re–think its implementation, as the original plan was no longer a viable to meet patient engagement targets. Since this time, the PPS developed and implemented new process flows to reach the goals set forth in the project. These newly designed process flows will also enable greater data acquisition and patient management for those patient unnecessarily utilizing the ED.
Recommendation 2: The Independent Assessor recommends the PPS create a plan to address the shortage of primary care physicians engaged in this project.
CPWNY Response: The PPS acknowledges the IA´s recommendation and is developing a plan to address this area of need.
Background: The PPS does not dispute the recommendations listed above, as the PPS already has reported and identified these needs and is actively working on developing new process flows to address them. It is important to note, however, that in the PPS´s original implementation plan, the PPS designed process flows surrounding referrals of all potential patients to the Health Homes. This referral process to Health Homes was used in the original projection of patient engagement numbers.
B. iii.) Project 2.c.ii.: Expand usage of telemedicine in underserved areas to provide access to otherwise scarce services
Recommendation 1: The Independent Assessor recommends the PPS develop an action plan to shorten the credentialing process of providers in order to improve the patient and partner engagement shortcomings.
CPWNY Response: The PPS recognizes shortcomings of the patient engagement numbers for the telemedicine project. The PPS requests that the IA rewords the telemedicine project recommendation to allow for flexibility in addressing implementation challenges, such as "The IA recommends the PPS develop an action plan to improve the patient and partner engagement shortcomings within the scope of telemedicine projects."
Background: The PPS acknowledges the IA´s recommendations regarding the shortening of the credentialing process. Woman´s Christian Association (WCA) Hospital is the pilot location for the largest implementation of the PPS´s telemedicine services, and shortening of the credentialing process would require this institution to change its by–laws and regulations. WCA Hospital is currently reviewing this option. However, the PPS has no authority to regulate or direct this partner hospital regarding its credentialing process.
In addition to the credentialing delays, another area for improvement identified by the PPS is the need to engage additional providers in other areas of telemedicine services. With additional pilot programs, the PPS will have greater success meeting the patient engagement requirements. Gap analyses have been completed, and currently the PPS is working on development of process flows for identified areas of need.
The PPS project team is proud to report that this project continues to be a platform that inspires innovation on many levels. Potential areas of interest include behavioral health, the developmentally disabled population, subspecialty care in rural areas, and others. PPS staff continues to explore these ideas and have partnered with members of the community to achieve these goals.
B. iv.) Project 3.a.i: Integration of primary care and behavioral health services
Recommendation: The Independent Assessor notes that the PPS has marked milestones related to EHR operability as on hold. The Independent Assessor recommends the PPS develop a plan to address interoperability requirements.
CPWNY Response: The PPS requests that the IA removes and omits all recommendations related to interoperability for project 3.a.i from CPWNY´s report.
Background: The PPS does not have interoperability milestones as part of its approved implementation plans. The PPS has correctly marked these milestones as "On Hold." This is noted by the IA on page 14 of the Mid–Point Assessment Report, "Further assessment of the PPS project implementation status for project 3.a.i. indicates that many of the project milestones with a status of ´On Hold´ are related to the PPS not pursuing Model 3 for this project. Therefore, for the models the PPS is pursing, there is no risk of project implementation meeting the required completion dates at this time."
B. v.) Project 3.f.i.: Increase support programs for maternal & child health (including high risk pregnancies) (Example: Nurse–Family Partnership)
Recommendation 1: The Independent Assessor recommends that the PPS explore opportunities to expand the services for this project into Erie County which is a part of the PPS service area and impacts a significant portion of the patient population.
CPWNY Response: The PPS acknowledges the IA´s recommendation and is implementing a plan to address this area of need.
Background: The initial intent for this project was to expand the Nurse–Family Partnership (NFP) program to Erie County. The experience with the NFP model in Chautauqua County has been very positive and effective; however, the NFP model is proprietary requiring adherence to nurse caseload limits and other guidelines which make expansion cost prohibitive. Recognizing that Erie County holds the greatest number of attributed lives, the PPS reviewed alternative models which had the potential to serve significantly more mothers and children. The Community Health Worker model was chosen after careful consultation with key stakeholders, including hospital–based clinic providers, community organizations, and other subject matter experts. This model employs a community health worker on the care team who provides patient support beyond the clinic walls to affect key project outcomes. A pilot program began in late November 2016.
Recommendation 2: The Independent Assessor notes that the PPS has marked milestones related to EHR operability as on hold. The Independent Assessor recommends the PPS develop a plan to address interoperability requirements.
CPWNY Response: The PPS requests that the IA removes and omits all recommendations related to interoperability for project 3.f.i from CPWNY´s Mid–Point assessment reports.
Background: The PPS requests that the IA removes and omits all recommendations related to interoperability for project 3.f.i from CPWNY´s Mid–Point assessment reports.
"...for project 3.f.i., the PPS is only implementing Model 1 and all milestones that have a current status of ´On Hold´ are associated with Model 2. As such, the IA has not identified any risks of project implementation meeting the required completion dates at this time."
B. vi.) Project 3.g.i: Integration of palliative care into the PCMH Model
Recommendation 1: The Independent Assessor recommends that the PPS create an action plan to increase the presence of palliative team members in primary care practices in order to increase referrals, which will further improve patient engagement shortcomings.
CPWNY Response: The PPS requests that the IA rewords the recommendation to allow for flexibility in PPS planning, such as "The Independent Assessor recommends that the PPS create an action plan for improving patient engagement shortcomings. This plan may include elements such as increasing the presence of palliative care team members in primary care settings, education and training for primary care providers on palliative care procedures and patient identification, and the development of a method for documenting and tracking engagements performed by primary care staff."
Background: The PPS notes that its partners´ primary care practices have elected to perform palliative care services using their own internal staff. The recommendation of the IA limits action planning. The PPS´s palliative care team is exploring ways of capturing palliative care services performed by primary care staff in a systematic and reportable manner. The IA´s recommendation does not provide the PPS program staff planning flexibility for providers who may choose to deliver services within their own clinical team and not through the use of an outside vendor/party. A specific re–wording of this recommendation will allow for flexibility in palliative care service delivery in a practice setting.
Recommendation 2: The PPS should also create a plan to continue partner engagement beyond the original training.
CPWNY Response: The PPS acknowledges the IA´s recommendation and is developing a plan to address this area of need.
Background: Regarding the patient engagement numbers cited on page 16 for project 3.gi, the PPS would like to clarify that the 3gi project was implemented on a phased roll–out basis. The project started with Erie County and gradually expanded to include the remaining PPS geographic area, Chautauqua and Niagara Counties. The first few quarters of reporting only reflect the pilot model data from Erie County.
Project leadership´s expectation was that once all three palliative care programs from the three counties were participating, we would see sufficient enrollment in their programs to meet patient engagement targets. Unfortunately, enrollment volume ended up lower than expected.
Each of the palliative care programs provided general trainings to primary care explaining what palliative care is, how to identify eligible patients, and how to initiate a conversation. Some primary care providers have chosen to use this training to provide palliative care services using their internal staff. These engagements are not currently being captured in a way that they can be quantified for reporting purposes. This contributes to the inability to capture and report those project level patient engagements. Next steps for this team include managing a work group to identify gaps in the current EHR reporting and develop tools for creating a systematic way to capture palliative care engagements performed by primary care staff.
On page 23, the IA states, "They (CPWNY) states that many primary care practices accept the initial training and education sessions, but few are willing to offer time and space to palliative care staff on an ongoing basis."
The PPS team would like to clarify their statement noted by the IA. Many partner practices accepted the initial palliative care training and education but chose to use this education to offer palliative care services using their own internal staff at the primary care practice. The project´s key issue is not that the engagements are not occurring, but rather that the palliative care services provided at primary care sites are not systematically documented and tracked for engagement reporting purposes. Manual data collection is not possible, as it would require review of individual clinical notes in private practice EHRs. Next steps for this team will be development of a process to address documentation.
III. General Findings
CPWNY would like to highlight a few general issues of concern.
Waiver Versus Non–Waiver Revenue (p3)
CPWNY requests a revision to the Midpoint Assessment Report that clearly states that Non–Waiver funds are not included and the reported funds distributed do not reflect total funds distributed by CPWNY between DY1 Q1 and DY2 Q2. Alternatively, we request that the report be revised to include both the Waiver and Non–Waiver funds.
Background: The Mid–Point Assessment report does not state that the report only addresses the Waiver portion of revenue and expenditures. In general, it appears that the DSRIP IA report for CPWNY only addresses the waiver portion (Net Project Value, Net High Performance Fund, and Additional High Performance Fund) of revenue and expenditures. For example, the total funds distributed in PPS PMO section on Page 8, the total PMO expenditures and total administrative cost on Page 8, and the PPS funds flow table on Page 12 only reflect the Waiver portion. This is an underrepresentation of total funds distributed by CPWNY. However, the Introduction paragraph on Page 3 shows the total award of approximately $92.3 million over the 5 year project which includes both the Waiver and Non–Waiver funds.
CPWNY is one of the PPSs receiving Safety Net Equity funds, which are Non–Waiver funds. Non–Waiver funds (including Equity Infrastructure Program and Equity Performance Program) account for 43.1% of CPWNY´s total potential revenue over the five Demonstration Years. In DY2, the Non–Waiver portion accounts for 50.2% of expected revenue and expected expenditure.
The funds flow table on page 12 has been revised by the PPS and a table has been added as attachment A (figure 5A) to the PPS comments. The revised table clearly indicates the differences in funds flow when all sources of funding to PPS are represented.
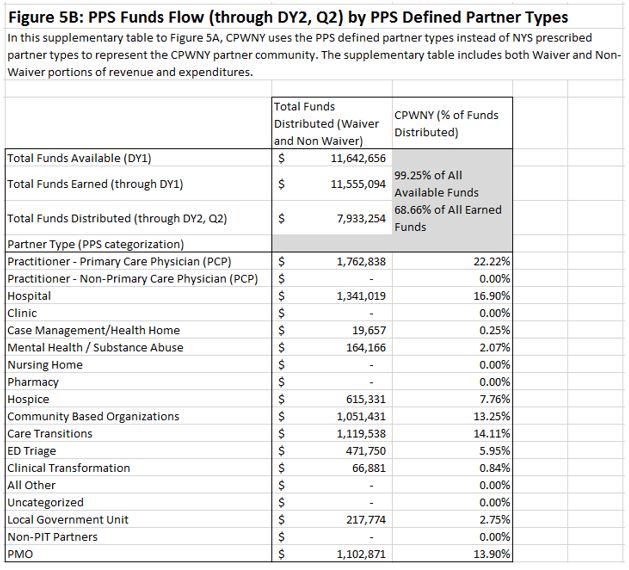
Provider Type Categorizations
CPWNY requests an update to the Midpoint Assessment Report that states the existence of provider type discrepancies and takes into account the Provider Type Categorization Appeal Form submitted in March 2016. It is also requested that the PPS Funds Flow table on Page 12 be replaced. Please see attachment A (figure 5A and 5B) for the requested revised table from the PPS.
Background: There have been systematic discrepancies between how CPWNY identifies partners´ provider types and how NYSDOH categorized PPS partners primarily based on claims. CPWNY identifies partners as a hospital, or a clinic, or a primary care practitioner, etc., based on their operating license, network participating documentations, and self–identified provider types. In general, CPWNY identifies each partner in one provider type based on partner engagement in appropriate project(s). We understand that NYS categorized the PPS partners primarily based on services indicated in claims data, and that NYS may categorize one partner in multiple provider types.
CPWNY submitted a Provider Type Categorization Appeal Form in March 2016 to request changes for 72 partners. Most of the requested changes were between "Practitioner – PCP" and "Practitioner - Non PCP". Some other requested changes include clinic categorized as substance abuse, case management categorized as hospice, nursing home categorized as pharmacy, etc. It appears that most of the requested changes are not yet implemented in MAPP or PIT.
The provider type discrepancies are related to multiple issues in the Midpoint Assessment Report, including but not limited to:
- PPS Funds Flow on Page 12 misrepresents CPWNY´s funds flows because of the partner type discrepancies, among other reasons. Page 12 also indicates the PPS has not distributed funds to Behavioral Health (Mental Health and Substance Abuse). That is incorrect for the following reasons:
First, in most reporting quarters CPWNY used the Primary Funds Flow method for reporting, which showed 100% of funds flow through the lead organization or the PMO, thus no secondary fund flows to Behavioral Health providers, or others were reported in MAPP/PIT.
Second, when CPWNY reported Secondary Funds Flow, funds to Behavioral Health providers are not correctly represented in MAPP/PIT either because NYS did not categorize them as Behavioral Health or because they have other provider types (e.g. Hospital) which took priority over Behavioral Health when the PPS reported the funds flow. - The Partner Engagement per Project tables from Page 18 to Page 22 misrepresent CPWNY´s current status of engagement partners by provider type. The Practitioner – Primary Care Provider type is particularly underrepresented in engaged numbers in each project because many of them are categorized by NYS as Practitioner – Non PCP.
360 Survey Results: Partners´ Experience with the PPS (p 4–6)
Generally, the PPS is concerned that the independent assessor is drawing conclusions such as "Community Based Providers have a negative perception towards PPS engagement, communication and effectiveness" based on a small sample set that may not give a full picture of the work of the PPS. Page 6 shows the number of 360 Survey responses for each category of provider. The n size for the survey is very small. The PPS feels that due to the n size, responses do not represent a fair and reasonable sample of partner opinions.
PPS Administration & PMO Office (p 8)
It was noted that the PPS has experienced lower than average administrative costs. Both the lead organization, Sisters of Charity Hospital, and well as the PMO Catholic Medical Partners have significant experience with existing integrated delivery systems that allow for efficiency in operations and reduced administrative costs for the DSRIP program.
Community Based Organization Contracting (p 9)
On page 9 the IA wrote "However, of those distributions, the IA found that the PPS has been primarily distributing funds under the Community Based Organizations partner category to two entities, Catholic Medical Partners (CMP) and Catholic Health Systems (CHS), both of which are not featured on the list of Community Based Organizations with which CPWNY has contracted"
The PPS does not have CBO agreements with CMP and CHS because CMP is the PMO and CHS is the grant recipient. The reason that CMP and CHS are listed as CBOs in the MAPP and PIT tool is because that was how they were categorized by New York State in the PIT tool via MAPP. Also CMP acts as the PPS´s major safety net provider so many funds pass through CMP first and then are subject to a secondary distribution to a variety of partners and project related costs.
Cultural Competency and Health Literacy (CCHL) (p 9–10)
The PPS requests correction to the following statements:
- Statement indicates PPS works with State Troopers to provide education on Mental Health First Aid. Comment should read: "As part of cultural competency and health literacy imbedded in the MEB project and the effort to reduce Mental Health stigma, CPWNY provides Mental Health First Aid training that can be attended by the public and private sectors. One such course was attended by NYS Troopers and well received."
- Statement indicates PPS is planning to perform poverty simulation training in conjunction with United Way. Comment should read: "Currently, RMAC is investigating a Poverty Simulation Training that could be offered to our clinicians or CBOs in line with United Way trainings."
- Statement indicates no hospitals in the PPS/CPWNY network had a CCHL program. Comment should read: "One hospital had a mandatory training and all others did not address this topic. CPWNY is implementing the training program incrementally, focusing on Erie County and Niagara Counties first followed by Chautauqua County. (Milestone #1 is being addressed in all counties)
Financial Sustainability & VBP (p 10–11)
On page 10 the IA wrote, "The PPS performed a subsequent financial health assessment of its partners, and determined that one partner was in financial distress." The PPS performed an annual baseline Financial Sustainability test for the hospital partners and their associated practitioners, and at that time no partner had been deemed in financial distress. The PPS is in the process of performing the second annual Financial Sustainability test for the 2015 calendar year (as that information becomes publicly available). In the meantime, other measures have been performed by the PPS to assess and assist partners. The IA correctly stated that the PPS provided assistance to a partner as noted on page 10; however, this was done by the PPS proactively to prevent the partner from becoming financially fragile.
Funds Flow (p 11–12)
The amount reported in the Mid–point Assessment report for the total funds distributed across the PPS network of $6,444,472 only includes the waiver portion of funds distributed, and does not reconcile to what CPWNY reported in the MAPP, which was $6,466,637. If the Non–Waiver funds were included, the amount would be $7,933,254 as reported in the MAPP on an accrual basis.
The table that was presented by the IA in Figure 5 on Page 12 of the report, PPS Funds Flow (through DY2, Q2) had some inconsistencies, which we have revised. (See attachment A, Figures 5A and 5B)
On page 12 the IA wrote, "While the PPS has distributed funds to many partner types, funding distributions to Behavioral Health (Mental Health and Substance Abuse) have not occurred. It will be important for the PPS to address this in future funding distributions to ensure the continued engagement of these partners in the successful implementation of the DSRIP projects."
The PPS did distribute funds to at least eight behavioral health providers. This funds flow was not evident because 1) funds were categorized under distributions to Community Based Organizations and Case Management/Health Homes rather than Mental Health and Substance Abuse providers and 2) For all but one reporting period, the PPS provided funds flow at the primary level which did not breakout spending to secondary payees such as Behavioral Health organizations. The correct funds flow categorization is provided in the revised table, Figure 5B. (See attachment A)
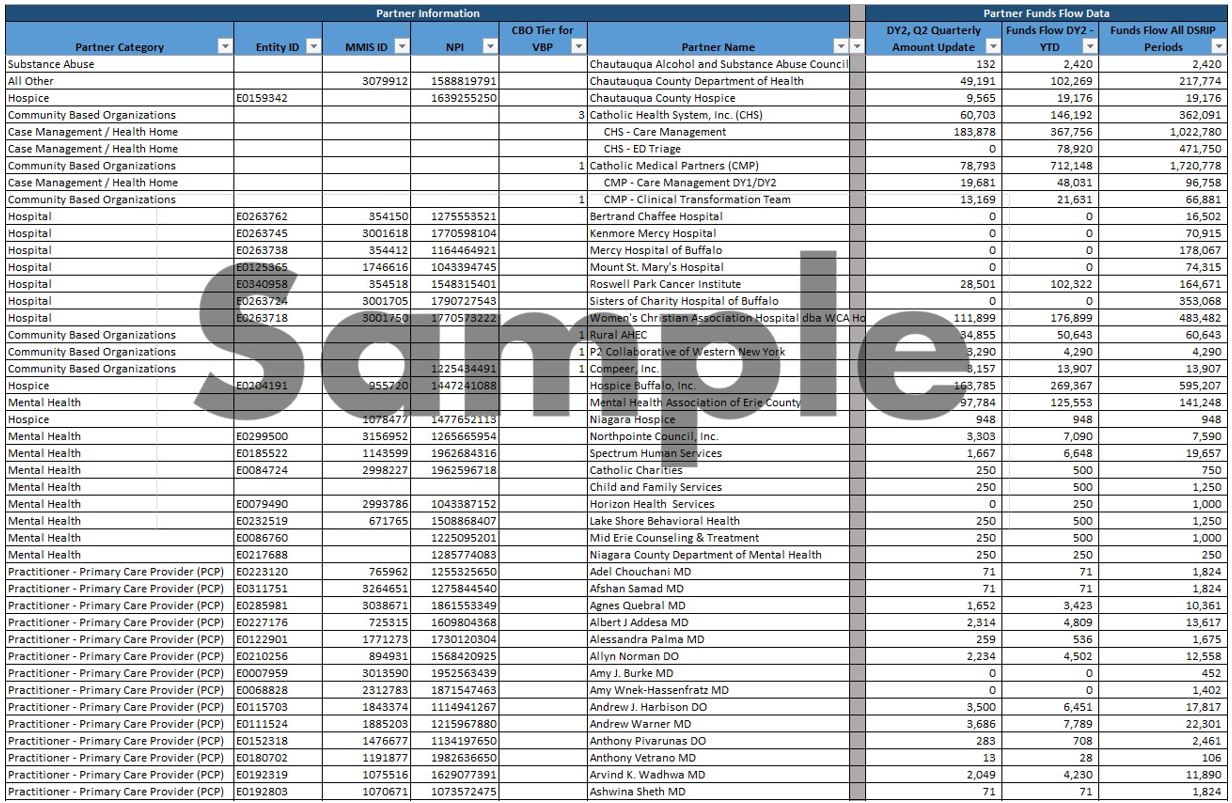
A detailed secondary funds flow document is also provided as part of the PPS response, please see attachment B.
Attachment A: Figure 5A
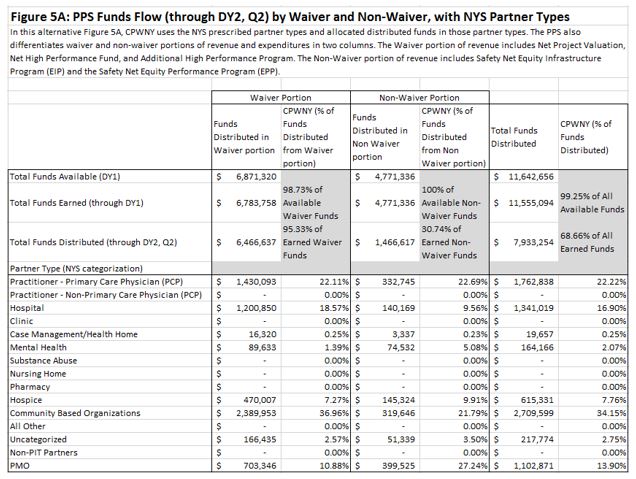
Attachment A: Figure 5B
Attachment B–Secondary Funds Flow Detail
See spreadsheet entitled "Attachment B – PPS 2nd Tier Funds Flow Reporting Template.xlsx"
Follow Us