Diabetes
Chronic Condition Clinical Advisory Group
Value Based Payment Recommendation Report
- Report is also available in Portable Document Format (PDF)
NYS Medicaid Value Based Payment
September 2016
Introduction
Delivery System Reform Incentive Payment (DSRIP) Program and Value Based Payment (VBP) Overview
The New York State (NYS or the State) DSRIP program aims to fundamentally restructure New York State´s healthcare delivery system, reducing avoidable hospital use by 25%, and improving the financial sustainability of New York State´s safety net.
To further stimulate and sustain this delivery reform, at least 80 - 90% of all payments made from Managed Care Organizations (MCOs) to providers will be captured within VBP arrangements by 2020. The goal of converting to VBP arrangements is to develop a sustainable system, which incentivizes value over volume. The Centers for Medicare & Medicaid Services (CMS) has approved the State´s multiyear VBP Roadmap, which details the menu of options and different levels of VBP that the MCOs and providers can select.
|top of page|Diabetes Episode Clinical Advisory Group (CAG)
CAG Overview
For many VBP arrangements, a subpopulation or defined set of conditions may be contracted on an episodic/bundle basis. Clinical Advisory Groups (CAGs) have been formed to review and facilitate the development of each subpopulation or bundle. Each CAG comprises leading experts and key stakeholders from throughout New York State, often including representatives from providers, universities, State agencies, medical societies, and clinical experts from health plans.
The Diabetes Episode CAG held a series of two meetings throughout the State and discussed key components of the Diabetes Episode VBP arrangement, including bundle definition, risk adjustment, and the Diabetes Episode bundle outcome measures. In order to help ensure a comprehensive discussion that captured unique attributes specific to Diabetes Episode and as well as areas of overlap with chronic heart disease, key stakeholders in the area of Diabetes Episode leveraged the chronic heart disease CAG to continue the discussion focusing on diabetes. For a full list of meeting dates, and an overview of discussions, please see the Appendix A at the end of the Quality Measure Summary.
|top of page|Recommendation Report Overview & Components
The following report contains two key components:
Diabetes Episode Playbook
- The playbook provides an overview of the episode definition and clinical descriptions, including ICD-9 and ICD-10 codes.
Diabetes Episode Outcome Measure Summary
- The outcome measure summary provides a description of the criteria used to determine relevancy, categorization, and prioritization of outcome measures, as well as a listing of the recommended outcome measures.
Diabetes Playbook
Diabetes Episode Definition
Playbook Overview – Diabetes
New York State´s VBP Roadmap1 describes how the State will transition 80 – 90% of all payments from MCOs to providers from Fee for Service (FFS) to Value Based Payments. "Bundles" or "episodes"2 group together the wide range of services performed for a patient with a specific condition. Episodes only include those services that are relevant to the condition, including services that are routine and typical for the care of the condition. The episode also takes into account services that are required to manage complications that could potentially occur during the course and care of the condition. Episodes open with a claim carrying a "trigger code." Sometimes a confirmatory claim is required in addition to the initial trigger code to confirm an episode exists. Once the episode is opened, it creates a time window where all relevant claims are attributed. Thus, an episode of care is patient–centered and time–delimited. It can be considered as a unit of accounting for budgeting purposes, unit of care for contracting purposes, and a unit for accountability for quality measurement purposes.
New York State uses the HCI3 (Prometheus)–bundled payment methodology, including the standard episode definitions to maximize compatibility and consistency within the State and nationally. More information on how the episodes are developed is available on HCI3´s Web site.3 The HCI3–bundled payment methodology is also referred to as "the grouper."
This playbook describes the Diabetes Episode (Asthma Episode and COPD Episode). The table below provides an overview of the sections in this playbook.
| Section | Short Description |
|---|---|
| Description of Episode | Details on the Diabetes Episode, including episode triggers and time lines, covered services, exclusions, and potentially avoidable complications |
| Attachment A: Glossary | List of all important definitions |
| Attachment B: Workbooks with Codes for the Diabetes Episode | Overview of all diabetes specific ICD–9 codes as well as their cross–walk to ICD–10 codes |
Description of Episode – Diabetes
This episode targets Medicaid–only members who have diabetes.
How is a Diabetes Episode triggered?

The Diabetes Episode is initially triggered by either (1) an inpatient claim with diabetes as the principal diagnosis, or (2) an outpatient or professional billing claim with an evaluation and management (E&M) service listing diabetes as the diagnosis. The confirming trigger must adhere to the same parameters as the initial trigger and follow at least 30 days after the initial trigger.4
|top of page|Which services are included in the Diabetes Episode?
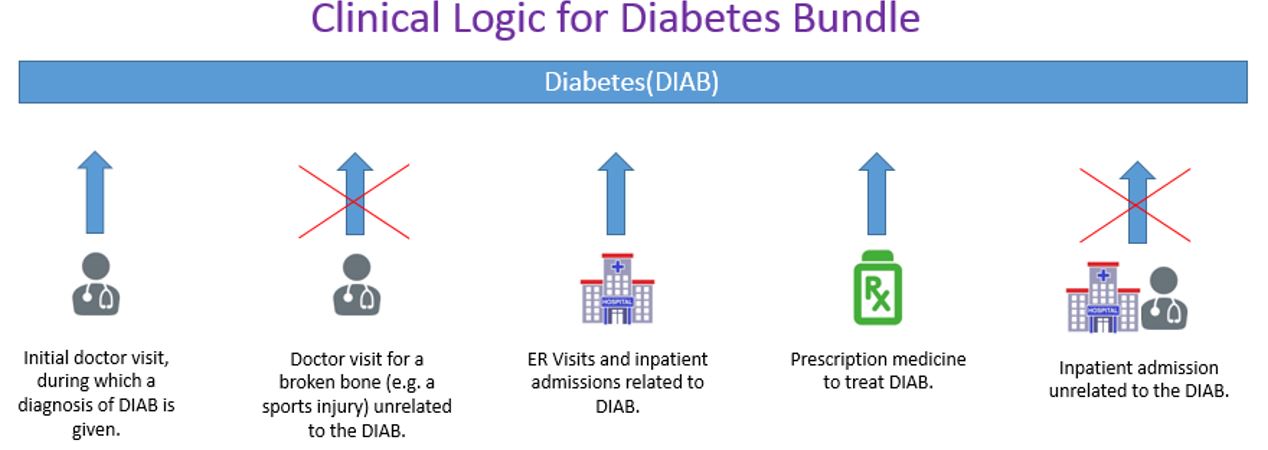
The Diabetes Episode included all services (inpatient services, outpatient services, ancillary, laboratory, radiology, pharmacy, and professional billing services) related to the care for diabetes.4 The visual below provides an example of the services that are/are not included in an episode. The episode includes all care related to that episode, while it excludes encounters where services are provided for unrelated care as defined by the diagnoses (see crossed out services in the example below).
What are the exclusion criteria for the Diabetes Episode?
Some episodes have specific exclusion criteria; these are either exclusions from the episode based on clinical reasons or exclusions from eligibility for Medicaid. Episodes might be excluded from analysis if they are incomplete due to:
- Administrative Exclusion: Incomplete set of claims within the episode time window due to coverage/enrollment gap or lack of episode completion.
- Age: The Diabetes Episode excludes Medicaid members who are younger than 5 or are 65 years and older.
- Cost Upper and Lower Limit: To create adequate risk models, individual episodes where the episode cost is below the first percentile or higher than the ninety–ninth percentile are excluded.
- Coverage Gap: For the Diabetes Episode, continuous member/patient enrollment eligibility is checked for the episode period. If a patient has any enrollment gap during an episode with an episode window 90 days or less or a gap greater than 30 days during episodes with episode window greater than 90 days, then the episode is flagged as not meeting the coverage/enrollment gap criteria.
What is the timeline for a Diabetes Episode?
Starting from the moment the episode is triggered, there is a 30–day look–back period for care related to diabetes. As diabetes are a chronic episodes, the episodes can be open until the patient is deceased. For reporting purposes, the episode can be assessed on a yearly rolling basis. However, if there are no services related to this episode in a given year, then the episode will not be triggered. If the patient becomes deceased, the date of death marks the end of the episode.

Which potentially avoidable complications (PACs) are related to the Diabetes Episode?
The services within an episode are assigned as either typical or as potentially avoidable complications. In order to be considered a potentially avoidable complication, or PAC, services must include complication diagnosis codes that either (1) directly relate to the index condition or (2) indicate a failure in patient safety. PACs can occur as hospitalizations, emergency room visits, and professional services related to these hospitalizations, but they can also occur in outpatient settings. As the term indicates, a PAC does not mean that something has gone wrong: it means that a type of care was delivered related to a clinical event that may have been preventable. As such, the goal is not to reduce PACs to zero, but to reduce PACs as much as possible, and to benchmark the risk-adjusted occurrences of these PACs between VBP contractors and MCOs.
Additionally, from a quality perspective, PACs can be identified by failure to comply with patient safety guidelines, such as HACs (CMS defined Hospital–Acquired Conditions) and PSIs (Agency for Healthcare Research and Quality (AHRQ) defined Patient Safety Indicators). Likewise, failure to avoid other situations related to patient safety (e.g. avoidable infection or drug interaction) may also be considered a PAC.
The top 10 PACs (based on cost) related to diabetes in NYS Medicaid are:
- Diabetes, poor control
- HAC: Manifestations of poor glycemic control
- Sepsis
- Cellulitis, skin infection
- Stroke
- Pneumonia
- Urinary tract infection
- Acute myocardial infarction
- Hypotension/syncope
- Acute pancreatitis, Pseudocyst
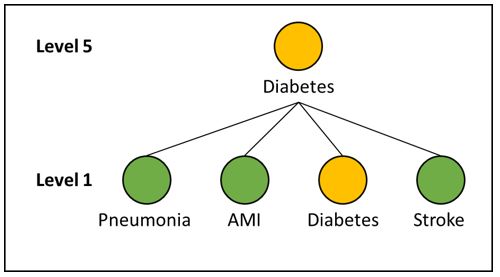
Which episodes roll up under the Diabetes Episode?
The HCI3 grouper looks at episodes at different levels. At level 1, all episodes are analyzed individually. At higher levels (2 to 5), different episodes are rolled up under one specific episode as PACs.
Which subtypes of the Diabetes Episode exist?
"Subtypes" are subgroupings that could help stratify a population for analytic purposes and are used for functions such as risk adjustment.
A few examples of common subtypes for the diabetes episode are:
- Diabetes mellitus with neurologic manifestations
- Diabetes mellitus with ophthalmic manifestations
- Diabetes mellitus with peripheral circulatory disorders
- Diabetes mellitus with renal manifestations
- Type I diabetes
The overview of all subtypes of the diabetes episode can be found in Attachment B.
|top of page|How is the risk adjustment of the Diabetes Episode done?
Separate risk adjustment models are created for "typical" services and for PACs. Risk factors that are taken into account include patient demographics, pre–existing co–morbidities, and subtypes.5 Using these factors, the episode grouper calculates an "expected" total cost that is unique for every individual patient. The difference between the actual cost and the expected cost determines the savings/losses incurred in the care for that individual patient. 6
|top of page|Attachment A: Glossary
- Complication Code: These are ICD–9 and ICD–10 diagnosis codes, which are used to identify a Potentially Avoidable Complication (PAC) services during the episode time window.
- Diagnosis Codes: These are unique codes based on ICD–9 (or ICD–10) that are used to group and categorize diseases, disorders, symptoms, etc. These identify clinically–related inpatient, outpatient, and professional typical services to be included in the episode in conjunction with the relevant procedure codes. These may include trigger codes, signs and symptoms and other related conditions and are used to steer services into an open episode.
- Episode: An episode of medical care that spans a predefined period of time for a particular payer–provider–patient triad, as informed by clinical practice guidelines and/or expert opinion. The episode starts after there is a confirmed trigger for that episode (e.g. a diagnosis).
- Episode Type: Episodes are grouped into four main categories:
- Chronic Condition – care for a chronic medical condition.
- Acute Condition – care for an acute medical condition.
- Procedural (Inpatient (IP) or Outpatient (OP)) – a surgical procedure and its follow–up care; the procedure may treat a chronic or acute condition.
- Other Condition – care for pregnancy and cancer episodes.
- In addition, there is one generic episode type included:
- System–Related Failures – inpatient and follow–up care for a condition caused by a systemic patient–safety failure.
- Exclusions: Some episodes have specific exclusion criteria, which are either based on clinical or administrative (eligibility/coverage) criteria.
- ICD–10 Codes: The ICD–9 diagnosis codes and the ICD–9 procedure codes for the above categories of codes have been cross–walked to ICD–10 codes leveraging the open–source GEM (Generalized Equivalence mapping) tables published by CMS.
- Index Condition: The index condition refers to the specific episode that the PAC relates to.
- Initial and Confirming Triggers: An initial trigger initiates an episode based on diagnosis and / or procedure codes found on institutional or non–institutional claims. For many episodes, a second trigger, the confirming trigger, is necessary to actually trigger the episode. Sometimes an episode itself could serve as a trigger for another episode, e.g., pregnancy episode in delivery episode.
- Clinical Association: HCI3´s PROMETHEUS Analytics© allows episodes to be connected to one another based on clinical relevance. For any individual patient, conditions and treatments, all of which trigger different episodes, are often related to one another from a clinical perspective. Episodes can be linked together for the analysis of their costs as either typical or complication.
- Look–Back & Look–Forward: From the point at which an episode is triggered, episode costs / volume are evaluated within the associated time window for a predetermined number of days before and after the trigger date. Costs, volume, and other episode components that fall within this range are captured within the episode.
- Pharmacy Codes: These are codes used to identify relevant pharmacy claims to be included in the episode. HCI3´s PROMETHEUS Analytics© groups pharmacy NDC codes into higher categories using the National Library of Medicine´s open–source RxNorm system of drug classification.
- Potentially Avoidable Complication (PAC): An episode contains services that are assigned as either typical or as potentially avoidable complications. In order to be considered a potentially avoidable complication, or PAC, services must include complication diagnosis codes that either (1) directly relate to the index condition or (2) indicate a failure in patient safety. PACs can occur as hospitalizations, emergency room visits, and professional services related to these hospitalizations, but they can also occur in outpatient settings. As the term indicates, a PAC does not mean that something has gone wrong: it means that a type of care was delivered related to a clinical event that may have been preventable. As such, the goal is never to reduce PACs to zero, but to reduce PACs as much as possible, and to benchmark the risk–adjusted occurrences of these PACs between VBP contractors and MCOs.
Additionally, PACs can be identified by failure to comply with patient safety guidelines, such as HACs (CMS defined Hospital–Acquired Conditions) and PSIs (Agency for Healthcare Research and Quality (AHRQ) defined Patient Safety Indicators). Likewise, failure to avoid other situations related to patient safety (e.g. avoidable infection or drug interaction) may also be considered a PAC. - Procedure Codes: These are codes used to identify clinically–related services to be included in the episode in conjunction with the typical diagnosis codes. These include CPT, HCPCS, and ICD–9 and ICD–10 procedure codes.
- Roll–Ups: Some episodes are associated with each other through HCI3´s PROMETHEUS Analytics© clinical logic and grouped under an ´umbrella´ episode, including the grouped episode´s costs/volume.
- Subtypes (code): Episodes often have subtypes or variants, which are useful to adjust for the severity of that episode, and reduce the need to have multiple episodes of the same type.
- Time–Window: This defines the time that an episode is open. It includes the trigger event, a look–back period and a look–forward period and could be extended based on rules and criteria.
- Trigger Code: A trigger code is the diagnosis or procedure code indicating the condition in question is present or procedure in question has occurred. Trigger codes are used to open new episodes and assign a time window for the start and end dates of each episode (depending on the episode type). Trigger codes can be ICD–9 or ICD–10 diagnosis or procedure codes, CPT or HCPCS codes, and could be present on an inpatient facility, outpatient facility, or professional claim.
Attachment B: Workbook with Codes for the Diabetes Episode
The file below includes all ICD–9 diabetes specific codes
The files below include all ICD–10 diabetes specific codes.
(Coming Soon)
|top of page|Diabetes Quality Measure Summary
Diabetes Clinical Advisory Group (CAG)
Quality Measure Recommendations
Introduction
Over the course of two meetings, the Diabetes Episode CAG reviewed, discussed, and provided feedback on the proposed Diabetes Episode Episodes (diabetes) to be used to inform VBP contracting for levels one through three. Both episodes concern lung–related conditions and include significant overlap of quality measures that are relevant for several conditions simultaneously. To help ensure a comprehensive discussion that captured both unique attributes specific to each bundle as well as areas of overlap (such as quality measures), one Diabetes Episode CAG was assembled and the outcomes are included here within one comprehensive document.
A key element of these discussions was the review of current, existing, and new quality measures used to measure the quality of care related to the diabetes bundle. The chronic heart and diabetes joint CAG discussed clinically relevant and feasible quality measures for diabetes. This document summarizes the discussion of the CAG and their categorization of quality measures.7
Selecting quality measures: Criteria used to consider relevance:8
In reviewing potential quality measures for utilization as part of a VBP arrangement, a number of key criteria have been applied across all Medicaid member subpopulations and disease bundles. These criteria, and examples of their specific implications for the Diabetes Episode VBP arrangement, are the following:
Clinical relevance
Focused on key outcomes of integrated care process
i.e. outcome measures (postpartum depression) are preferred over process measures (screening for postpartum depression); outcomes of the total care process are preferred over outcomes of a single component of the care process (e.g. the quality of one type of professional´s care)
For process measures: crucial evidence–based steps in integrated care process that may not be reflected in the patient outcomes measured
i.e. focus on postpartum contraceptive care is key but will not be captured in outcomes of current maternity episode
Existing variability in performance and/or possibility for improvement
i.e. blood pressure measurement during pregnancy is unlikely to be lower than >95% throughout the State
Reliability and validity
Measure is well established by reputable organization
By focusing on established measures (owned by e.g. NYS Office of Patient Quality and Safety (OQPS), endorsed by the National Quality Forum (NQF), Healthcare Effectiveness Data and Information Set (HEDIS) measures and/or measures owned by organizations such as the Joint Commission), the validity and reliability of measures can be assumed to be acceptable.
Outcome measures are adequately risk–adjusted
i.e. measuring ´% preterm births´ without adequate risk adjustment makes it impossible to compare outcomes between providers
Feasibility
Claims–based measures are preferred over non–claims based measures (clinical data, surveys)
i.e. ease of data collection data is important and measure information should not add unnecessary burden for data collection
When clinical data or surveys are required, existing sources must be available
i.e. the vital statistics repository (based on birth certificates) is an acceptable source, especially because OQPS has already created the link between the Medicaid claims data and this clinical registry
Data sources preferably are patient–level data
Measures that require random samples (e.g. sampling patient records or using surveys) are less ideal because they do not allow drill–down to patient level and/or adequate risk–adjustment, and may add to the burden of data collection. An exception is made for such measures that are part of DSRIP/QARR.
Data sources must be available without significant delay
i.e. data sources should not have a lag longer than the claims–based measures (which have a lag of six months). This is an issue with the vital statistics repository, for example, which have a one year lag (at least for the NYC data).
Meaningful and actionable to provider improvement in general
Measures should not only be related to the goals of care, but also something the provider can impact or use to change care.
|top of page|Categorizing and prioritizing quality measures
Based on the above criteria, the CAG discussed the quality measures in the framework of three categories:
- Category 1 – Category 1 comprises approved quality measures that are felt to be clinically relevant, reliable, valid, and feasible.
- Category 2 – Category 2 quality measures were felt to be clinically relevant, valid, and probably reliable, but where the feasibility could be problematic. These quality measures will likely be investigated during the 2016 or 2017 pilots but would likely not be implementable in the immediate future.
- Category 3 – Category 3 measures were decided to be insufficiently relevant, valid, reliable, and/or feasible.
Ultimately, the use of these measures, particularly in Category 1 and 2 will be developed and further refined during the 2016 (and possibly 2017 pilots). The CAG will be re-assembled on a yearly basis during at least 2016 and 2017 to further refine the Category 1 and 2 measures.
The HCI3 grouper creates condition–specific scores for Potentially Avoidable Complications (PACs) for each condition. The ´percentage of total episode costs that are PACs is a useful measure to look for potential improvements; it cannot be interpreted as a quality measure. PAC counts however, can be considered clinically relevant and feasible outcome measures.
|top of page|Diabetes CAG Recommended Quality Measures – Category 1 and 2
| # | Measure | Measure Steward/Source | |
|---|---|---|---|
| Category 1 | 1 | Comprehensive Diabetes Care: Blood Pressure Control (<140/90 mm Hg)* | National Committee for Quality Assurance |
| 2 | Comprehensive Diabetes Care: Medical Attention for Nephropathy* | National Committee for Quality Assurance | |
| 3 | Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%)* | National Committee for Quality Assurance | |
| 4 | Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Poor Control (>9.0%)* | National Committee for Quality Assurance | |
| 5 | Comprehensive Diabetes Care: Eye Exam (retinal) performed* | National Committee for Quality Assurance | |
| 6 | Diabetes: Foot Exam* | National Committee for Quality Assurance | |
| 7 | Smoking Cessation discussed and documented | American Diabetes Association | |
| 8 | Depression screening (PHQ2 or 9) annually | American Diabetes Association | |
| 9 | Comprehensive Diabetes screening – All Four Tests (HbA1c, lipid profile, dilated eye exam, nephropathy monitor) |
National Committee for Quality Assurance | |
| 10 | Diabetes Short–Term Complications Admission Rate (PQI 01) | Agency for Healthcare Research and Quality | |
| Category 2 | 11 | Optimal Diabetes Care (Composite Measure) | Minnesota Community Measurement |
| 12 | BMI/Nutrition Counseling | American Diabetes Association | |
| 13 | Adherence to Statins for Individuals with Diabetes Mellitus* | Centers for Medicare & Medicaid Services | |
| 14 | On ACEI/ARB if hypertension or nephropathy | American Diabetes Association | |
| 15 | Proportion of patients with a chronic condition that have a potentially avoidable complication during a calendar year* | Bridges to Excellence | |
| 16 | Rate of Lower–Extremity Amputation Among Patients With Diabetes (PQI 16) * | Agency for Healthcare Research and Quality | |
| *= NQF Endorsed | |||
CAG categorization and discussion of measures
| Topic | # | Quality Measure (* = NQF Endorsed) | Type of Measure | Measure Steward/ Source | DSRIP | QARR | HEDIS | Data Required | Quality Measure Categorization & Notes | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Medicaid Claims Data | Clinical Data 9 | Category | Notes | ||||||||
| Prevention | 1 | Comprehensive Diabetes Care: Blood Pressure Control (<140/90 mm Hg) * | Outcome | National Committee for Quality Assurance | X | X | Yes | Yes | 1 | The CAG members agreed that this is an essential measure. This is a chart review measure but is already being used by QARR and can be captured with current procedural terminology (CPT) codes. According to NCQA policy update, related to diabetes and blood pressure control < 140/90 mm Hg, CPT codes exist for this measure and should exist in claims data. http://www.ncqa.org/portals/0/PolicyUpdates/HEDIS%20Technical%20Updates/09_CD C_Spec.pdf |
|
| Prevention | 2 | Comprehensive Diabetes Care: Medical Attention for Nephropathy* | Process | National Committee for Quality Assurance | X | Yes | Yes | 1 | This is a comprehensive measure that uses multiple factors for screening, including urine screening, ACEI/ARBs (angiotensin– converting enzyme inhibitor/angiotensin–receptor blocker) use, or referral to a nephrologist. | ||
| Prevention | 3 | Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Control (<8.0%)* | Outcome | National Committee for Quality Assurance | X | X | Yes | Yes | 1 | The CAG members believe that an HbA1c of less than 7.0% as seen in measure #4 is too aggressive. It has the potential to negatively categorize a practice that has a disproportionally large group of patients with comorbidities. They would be unable to realistically achieve the goal of an A1C of less than 7%. The CAG members feel that an HbA1c of less than 8% is a more reasonable measure to use instead of less than 7%. | |
| Prevention | 4 | Hemoglobin A1c Control (HbA1c), (<7.0%) | Outcome | American Diabetes Association | Yes | Yes | 3 | Discussed in measure #3. | |||
| Prevention | 5 | Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) Poor Control (>9.0%)* | Outcome | National Committee for Quality Assurance | X | X | X | Yes | Yes | 1 | The CAG members believe that this measure combined with measure #3 (A1c of less than 8%) provides a balance of controlling diabetes without being too aggressive. It also identifies greater than 9%, which is poorly controlled and unacceptable standards. |
| Prevention | 6 | Comprehensive Diabetes Care: Hemoglobin A1c (HbA1c) testing* | Process | National Committee for Quality Assurance | X | X | Yes | Yes | 3 | This measure is not necessary with measures #3 and #5. | |
| Prevention | 7 | Comprehensive Diabetes Care: Eye Exam (retinal) performed* | Process | National Committee for Quality Assurance | X | X | Yes | Yes | 1 | CAG members believe that this is essential to diabetes care. The measure can be measured through claims data. | |
| Prevention | 8 | Comprehensive diabetes care: LDL–c control (<100mg/dL) * | Process | National Committee for Quality Assurance | X | Yes | Yes | 3 | The NCQA no longer uses this measure. Furthermore the use of statins, rather than an LDL target goal, is more important. An associated and more relevant quality measure is captured in measure #20, (Adherence to Statins for Individuals with Diabetes Mellitus) –– which is a Category 2 measure. | ||
| Prevention | 9 | Comprehensive Diabetes screening – All Four Tests (HbA1c, lipid profile, dilated eye exam, nephropathy monitor) | Process | National Committee for Quality Assurance | X | Yes | Yes | 1 | The CAG believes that this composite measure is important to include as it truly represents a patient centered focus. The results of this measure speak to how the patient is doing (as reflected in compliance with all 4 measure components on a per patient basis). | ||
| Prevention | 10 | Optimal Diabetes Care (Composite Measure)* | Process | Minnesota Community Measurement | Yes | Yes | 2 | The CAG believes that the threshold for compliance of the different components of this measure are low. Therefore, compliance with this measure is a challenge and may not be reasonable to hold providers accountable. Therefore, the CAG believes that this measure should likely be included in the pilot phase to be further evaluated. | |||
| Prevention | 11 | Diabetic Retinopathy: Communication with the Physician Managing Ongoing Diabetes Care* | Process | American Medical Association (AMA)– convened Physician Consortium for Performance Improvement | Yes | Yes | 3 | The CAG advises against including this measure due to the difficulty of obtaining testing reports from the eye exam provider. The CAG discussed that this information can be collected through claims data. However, it is felt by the CAG that there is a discrepancy in the communication between the eye exam provider and the Medicaid members´ physician. For example, many Medicaid members obtain eye exams through vision care programs that are independent of a referring provider, and these reports may never be received by the member´s physician. | |||
| Prevention | 12 | Diabetic Retinopathy: Documentation of Presence or Absence of Macular Edema and Level of Severity of Retinopathy* | Process | AMA–convened Physician Consortium for Performance Improvement | Yes | Yes | 3 | Similar to measure #11, the CAG is concerned about the difficulty of obtaining eye exam reports and advises against including this measure. | |||
| Prevention | 13 | Diabetes: Foot Exam* | Process | National Committee for Quality Assurance | Yes | Yes | 1 | The CAG believes an annual foot exam is essential for diabetes care. | |||
| Prevention | 14 | Diabetic Foot and Ankle Care, Ulcer Prevention – Evaluation of Footwear* | Process | American College of Cardiology | Yes | Yes | 3 | An annual foot exam is included in this measure; however, the CAG does not believe that it is feasible for the Medicaid member´s primary provider to evaluate for proper footwear. Physicians are not trained to do so; therefore, the analysis may be too subjective. | |||
| Prevention | 15 | Smoking Cessation discussed and documented | Process | American Diabetes Association | No | Yes | 1 | The CAG advises to include this measure. However, there is a concern about the completeness of the data. CAG members suggest it might be possible to use CPT codes for counselling for claims analysis. | |||
| Prevention | 16 | BMI/Nutrition Counseling | Process | American Diabetes Association | No | Yes | 2 | The CAG advises to include this measure. This is a Category 2 because the issue of how to capture nutritional counseling will need to be addressed in the pilot phase. | |||
| Prevention | 17 | Depression screening (PHQ2 or 9) annually | Process | American Diabetes Association | Yes | Yes | 1 | The CAG advises to include this measure. CPT codes for counseling can be used for claims analysis. Data could also be obtained via EMR. | |||
| Medication | 18 | Adherence to ACEIs/ARBs for Individuals with Diabetes Mellitus* | Process | Centers for Medicare & Medicaid Services | Yes | Yes | 3 | The CAG does not feel strongly about holding a physician responsible for medication adherence; medication compliance is low (especially within the Medicaid population) despite physicians encouraging patients, or even giving patients medication to go home with. | |||
| Medication | 19 | Adherence to Oral Diabetes Agents for Individuals with Diabetes Mellitus* | Process | Centers for Medicare & Medicaid Services | Yes | Yes | 3 | Same as measure #19. | |||
| Medication | 20 | Adherence to Statins for Individuals with Diabetes Mellitus* | Process | Centers for Medicare & Medicaid Services | Yes | Yes | 2 | Similar to measures #18 and #19; however, the CAG feels that there is currently mixed opinions on statin use and would like to test this measure in the pilot phase. | |||
| Medication | 21 | Glycemic Control – Hyperglycemia* | Outcome | Centers for Medicare & Medicaid Services | No | Yes | 3 | The CAG feels that many patients who are hospitalized with primary diagnoses other than diabetes often have hyperglycemia. This leads to a positively skewed view of hyperglycemia and, therefore, does not properly reflect how well the diabetic population is being controlled. | |||
| Medication | 22 | Glycemic Control – Hypoglycemia* | Outcome | Centers for Medicare & Medicaid Services | No | Yes | 3 | Hypoglycemia (blood sugar of less than 40) would require clinical records to capture data, and the CAG feels that the value gained is not worth the effort since the rate of hypoglycemic events is low. | |||
| Medication | 23 | Proportion of Days Covered (PDC): 3 rates by therapeutic category (% of patients who met the PDC threshold of 80% during the measurement year (at least 91 days) for RAS antagonists, diabetes medication, or statins)* | Process | American Diabetes Association | Yes | Yes | 3 | Similar to measures #18 and #19, this measure covers statins, diabetes medications, and ACE/ARBS for at least two prescriptions filled annually. | |||
| Medication | 24 | On ACEI/ARB if hypertension or nephropathy | Process | American Diabetes Association | Yes | Yes | 3 | This is already included in measure #2. | |||
| Treatment | 25 | Proportion of patients with a chronic condition that have a PAC during a calendar year* | Outcome | Bridges to Excellence | Yes | No | 2 | The CAG believes that no matter how good the provider´s treatment is, due to the long–term multiple organ effects of diabetes disease and the issue of patients who are noncompliant, it is difficult to hold providers and plans accountable. However, this measure is helpful to analyze aggregate level data and to see the medication member population as a whole. The CAG would like to test it in the pilot phase. | |||
| Treatment | 26 | Diabetes Short–Term Complications Admission Rate (PQI 01)* | Outcome | Agency for Healthcare Research and Quality | X | Yes | No | 1 | The CAG feels that this measure would be helpful since the providers have a greater impact on short–term complication rates as opposed to long–term complication rates (long–term complication rate discussed in measure #27). | ||
| Treatment | 27 | Diabetes Long–Term Complications Admission Rate (PQI 03)* | Outcome | Agency for Healthcare Research and Quality | Yes | No | 3 | The CAG feels that providers should not be accountable for this measure. The variability of long–term extent of diabetes is high, and the CAG feels that the provider may inherit patients with significant uncontrollable disease that they should not be financially responsible for. | |||
| Treatment | 28 | Uncontrolled Diabetes Admission Rate (PQI 14)* | Outcome | Agency for Healthcare Research and Quality | Yes | No | 3 | The CAG discussed that most hospital admissions do not occur as a result of uncontrolled diabetes, and therefore, this measure is not applicable. | |||
| Treatment | 29 | Rate of Lower–Extremity Amputation Among Patients With Diabetes (PQI 16)* | Outcome | Agency for Healthcare Research and Quality | Yes | No | 2 | The CAG would like to test this measure in the pilot phase to see if better controlled diabetes can slow down the amputation rate. | |||
Appendix A:
Meeting Schedule
| Date | Agenda | |
|---|---|---|
| CAG #1 (Webinar) |
10/14/2015 | Part I
|
| CAG #2 | 10/20/2015 |
|
______________________________________________________
1. https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/docs/vbp_roadmap_final.pdf. 1
2. The terms can be used interchangeably. Sometimes, the term "bundle" is used to refer to a combination of individual episodes. 2
3. http://www.hci3.org/content/online–courses 3
4. Attachment B lists all codes for the Asthma Episode and COPD Episode. 4
5. For details on risk adjustment, visit the HCI3 Web site (http://www.hci3.org/content/online–courses) 5
6. The overall total savings/losses per bundle are calculated by adding all these savings/losses at the individual episode level. 6
7. The following sources were used to establish the list of measures to evaluate: existing DSRIP/QARR measures; AHRQ PQI/IQI/PSI/PDI measures; CMS Medicaid Core set measures; other existing statewide measures; NQF endorsed measures; measures suggested by the CAG. 7
8. After the Measurement Evaluation Criteria established by the National Quality Forum (NQF), 8
9. Clinical data refers to non–claims data and is information that is often captured on a patient´s individual chart or record. 9
Follow Us