Behavioral Health Chronic Conditions
Behavioral Health Clinical Advisory Group
Value Based Payment Recommendation Report
- Report is also available in Portable Document Format (PDF)
NYS Medicaid Value Based Payment
October 2016
| Contents |
|---|
Introduction
|
Behavioral Health Chronic Condition Clinical Advisory Group (CAG)
|
Recommendation Report Overview and Components
|
Playbook Overview – Behavioral Health Chronic Conditions
|
Behavioral Health Chronic Condition episode Roll–ups
|
| Attachment A: Glossary |
| Behavioral Health Chronic Condition Clinical Advisory Group (CAG) |
| Introduction |
| Categorizing and Prioritizing Quality Measures |
| Overview of Depression & Anxiety Quality Measure Discussion |
| Depression & Anxiety Recommended Quality Measures – Category 1 & 2 |
| Overview of Substance Use Disorder (SUD) Quality Measure Discussion |
| Substance Use Disorder Recommended Quality Measures – Category 1 & 2 |
| Overview of Bipolar Disorder Quality Measure Discussion |
| Bipolar Disorder Recommended Quality Measures – Category 1 & 2 |
| Overview of Trauma & Stressor Quality Measure Discussion |
| Trauma & Stressor CAG Recommended Quality Measures – Category 1 & 2 |
| CAG Categorization and Discussion of Measures – Category 1 & 2 |
| CAG Categorization and Discussion of Measures – Category 3 |
| Appendix A: Meeting Schedule |
Introduction
Delivery System Reform Incentive Payment (DSRIP) Program and Value Based Payment (VBP) Overview
The New York State DSRIP program aims to fundamentally restructure New York State's health care delivery system, reducing avoidable hospital use by 25%, and improving the financial sustainability of New York State's safety net.
To further stimulate and sustain this delivery reform, at least 80–90% of all payments made from Managed Care Organizations (MCOs) to providers will be captured within VBP arrangements by 2020. The goal of converting to VBP arrangements is to develop a sustainable system which incentivizes value over volume. The Centers for Medicare & Medicaid Services (CMS) has approved the State's multi-year VBP Roadmap, which details the menu of options and different levels of VBP that the MCOs and providers can select.
|top of page|Behavioral Health Chronic Condition Clinical Advisory Group (CAG)
CAG Overview
For many VBP arrangements, a subpopulation or defined set of conditions may be contracted on an episodic/condition basis. Clinical Advisory Groups (CAGs) have been formed to review and facilitate the development of each subpopulation or condition. Each CAG comprises leading experts and key stakeholders from throughout New York State, often including representatives from providers, universities, State agencies, medical societies, and clinical experts from health plans.
The Behavioral Health CAG held a series of seven meetings throughout the State and discussed key components of the Behavioral Health VBP arrangement, including episode composition, provider opportunities, and quality measures. For a full list of meeting dates, times, and overview of discussions to date, please see Appendix A in the Quality Measure Summary.
|top of page|Recommendation Report Overview and Components
The following report contains two key components:
Behavioral Health Chronic Condition Playbook
- The playbook provides an overview of the episode definition and clinical descriptions including ICD–9 & ICD–10 codes for the following conditions:
- Depression & Anxiety Disorder
- Substance Use Disorder
- Bipolar Disorder
- Trauma & Stressor Disorder
Behavioral Health Chronic Condition Quality Measure Summary
- The quality measure summary provides a description of the criteria used to determine relevancy, categorization and prioritization of measures, and a listing of the recommended quality measures.
Behavioral Health Chronic Condition Playbook
Behavioral Health Chronic Condition Definition:
- Depression & Anxiety Disorder
- Substance Use Disorder
- Bipolar Disorder
- Trauma & Stressor Disorder
Playbook Overview – Behavioral Health Chronic Conditions
New York State´s VBP Roadmap1 describes how the State will transition 80–90% of all payments from Managed Care Organizations to providers from Fee for Service (FFS) to Value Based Payments.
´Bundles´2 or ´episodes´ group together a range of services performed in the care for a patient with a specific condition. Episodes include services relevant to the condition, including routine and typical care for the specific condition. Services that are required to manage complications potentially occurring during the course of care for the condition are also included. Episodes open with a "trigger code" claim carrying and may require a confirmatory claim to consider an episode of care should be opened. An episode time window is then created to which all relevant claims are attributed. An episode of care is patient centered and time delimited, and becomes a unit of accounting for the purpose of creating a budget, contracting, and quality measurement.
New York State builds on the HCI3 (Prometheus) bundled payment methodology, including the standard episode definitions to maximize compatibility and consistency within the State and nationally. More information on how the episodes are developed is available on HCI3´s Web site3. The HCI3 bundling method is also referred to as "the grouper."
This playbook describes the Behavioral Health Chronic Condition episodes. In practice, these episodes will be contracted together in Integrated Primary Care (IPC) arrangements. They comprise four of the fourteen episodes; the others include physical health conditions such as asthma and diabetes. For more information on those conditions and the IPC arrangement generally, please see the IPC Playbook. The table below provides an overview of the sections in this playbook.
| Section | Short Description |
|---|---|
| Description of Episode | Details on the Depression & Anxiety Disorder, Substance Use Disorder, Bipolar Disorder and Trauma & Stressor Disorder, including episode triggers and timelines, covered services, exclusions, and potentially avoidable complications |
| Attachment A: Glossary | List of all important definitions |
Description of Behavioral Health Chronic Condition Episodes
Members are assigned to the conditions for which they are diagnosed. For example, the Depression & Anxiety Disorder Episode is applicable for Medicaid–only members who are diagnosed with Depression and/or Anxiety Disorder. Similarly, the Substance Use Disorder, Bipolar Disorder and Trauma & Stressor episodes are applicable to the members diagnosed with those conditions.
|top of page|How are the Behavioral Health Chronic Condition Episodes Triggered?
Each of the Behavioral Health Chronic Condition episodes are triggered by one or more claims that carry a diagnosis code for the specific episode and meet the trigger criteria that is specified for the episode. A confirming trigger claim at least 30 days after the initial trigger claim is also necessary to ensure the episode is appropriate for the member.

Which services are included in each Behavioral Health Chronic Condition?
Each of the Behavioral Health Chronic episodes includes all services (e.g. inpatient services, outpatient services, ancillary, laboratory, radiology, pharmacy, and professional billing services) related to the care for the disorder. The graphic below provides an example of the services that are included in an episode. The episode excludes services for unrelated care as indicated by the diagnoses associated with the claim (the services crossed out in the example below).

What are the exclusion criteria for the Behavioral Health Chronic Conditions?
Some episodes have specific exclusion criteria based on clinical reasoning or ineligibility for Medicaid. Episodes can be excluded from analysis due to age or upper and lower cost limits as follows:
- The Behavioral Health Chronic Condition episodes excludes Medicaid members who are younger than 12 or older than 65;
- To create adequate risk models episodes with costs that are below the 1st percentile or above the 99th percentile for all episodes are excluded.
What is the timeline for the Behavioral episodes?
There is a 30-day look-back period from the trigger for each Behavioral Health Chronic episode. Chronic episodes remain open until the end of the period of analysis (one year) or until the patient is deceased. If no services occur in a given year the episode is not triggered. If the member dies, the date of death is the endpoint of the episode.

Potentially Avoidable Complications (PACs) related to Behavioral Health Chronic Conditions
Services (and costs) included in the episode are considered either a part of typical care or indicative of a Potentially Avoidable Complication (PAC). To be classified a PAC, the claim must include complication diagnosis codes that either (1) directly relate to the index condition or (2) indicate a failure in patient safety. A hospital admission for acute alcohol intoxication, for example, is a PAC; as is a medication overdose in a patient treated for depression. PACs, however, are not about the site of service, but about the clinical outcome: PACs can include hospitalizations, emergency room visits, outpatient or office visits, professional services and pharmacy costs. PACs also include patient safety failures such as those captured in CMS' Hospital Acquired Conditions (HACs) measures and the Agency for Healthcare Research and Quality's Patient Safety Indicators (PSIs).
As the "potentially" in the term indicates, a PAC indicates that services were performed related to a clinical event that may or may not have been preventable. As such, the goal is not to eliminate PACs but to reduce them as much as possible. Benchmarking the risk-adjusted occurrence of PACs for VBP contractors and MCOs also provides helpful information on possible areas of improvement.
To help formulate the list of PACs and develop the BH Chronic Condition episodes, New York State convened a Clinical Validation Group (CVG) made up of clinical experts from around the state. The CVG reviewed the analysis from the 2014 NYS claims data in detail and made recommendations about what codes to include in the episodes and what types of conditions to categorize as PACs. The preliminary results of the CVG were reviewed with the CAG and additional work on the PACs was recommended. The CVG has reconvened and PACS continue to be refined. For example, one key issue under consideration is the classification of all inpatient admissions for Substance Use Disorder as PACs. CAG members concurred that inpatient admission for detoxification services in particular is in many cases appropriate, even desirable, and should not be discouraged among providers. Refinements to separate or "sort" admissions for detoxification from all admissions within the SUD episode are under development.
|top of section| |top of page|Behavioral Health Chronic Condition episode Roll–ups
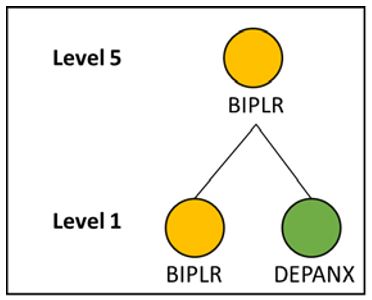
The overarching clinical logic of HCI3´s PROMETHEUS Analytics© allows a member to have multiple concurrent episodes open that can be linked together when they are clinically related. Episodes can be analyzed individually – "level 1" – or roll up into more comprehensive bundles – "level 5" – because of a clinical association.
Depression & Anxiety Disorder
No episodes roll up to Depression & Anxiety Disorder at level 5.
Substance Use Disorder
No episodes roll up to Substance Use Disorder at level 5.
Bipolar Disorder
The costs for Depression & Anxiety Disorder (identified in the graphic below as DEPANX) roll up to the Bipolar Disorder (identified in the graphic below as BIPLR) episode. At level 5 the costs of care for Depression & Anxiety are included as part of the members bipolar disorder.
Trauma & Stressor Disorder
No episodes roll up to Trauma & Stressor Disorder at level 5.
|top of page|What Subtypes are in Use for the Behavioral Health Chronic Conditions?
"Subtypes" are groupings that stratify a population into various "types" for analytic purposes and risk adjustment purposes. Examples of subtypes for the Behavioral Health Chronic episodes are below.
| Depression & Anxiety Disorder |
|---|
|
| Bipolar Disorder |
|---|
|
| Substance Use Disorder |
|---|
|
| Trauma & Stressor Disorder |
|---|
|
How is the Risk Adjustment for the Behavioral Health Chronic Conditions Performed?
Risk adjustment takes into account the profile of the population insured (e.g. member demographics and comorbid conditions). The HCI3's PROMETHEUS Analytics© severity adjustment is used for the risk adjustment of individual episodes and can be refined during pilots and subsequently. HCI3's severity adjustment is computed for each of the State's nine managed care regions as provided by the DOH. Each region has its own estimation model. For episodes where traditional severity adjustment is not appropriate, the regional average is used as the expected cost for all episodes for members within the region.
In order to calculate the risk–adjusted expected cost of an episode, the total cost of the episode is calculated using a regression analysis that includes a set of demographic and clinical risk variables. The regression analysis serves to predict the expected total cost for the episode.
|top of page|ICD–9 and ICD–10 Codes
A list of all relevant codes contained in each HCI episode definition can be found by visiting HCI3's website.
|top of section| |top of page|Attachment A: Glossary
- Complication Code: These are ICD–9 and ICD–10 diagnosis codes, which are used to identify a Potentially Avoidable Complication (PAC) services during the episode time window.
- Diagnosis Codes: These are unique codes based on ICD–9 (or ICD–10) that are used to group and categorize diseases, disorders, symptoms, etc. These identify clinically–related inpatient, outpatient, and professional typical services to be included in the episode in conjunction with the relevant procedure codes. These may include trigger codes, signs and symptoms and other related conditions and are used to steer services into an open episode.
- Episode: An episode of medical care that spans a predefined period of time for a particular payer–provider–patient triad, as informed by clinical practice guidelines and/or expert opinion. The episode starts after there is a confirmed trigger for that episode (e.g. a diagnosis).
- Episode Type: Episodes are grouped into four main categories:
- Chronic Condition – care for a chronic medical condition.
- Acute Condition – care for an acute medical condition.
- Procedural (Inpatient (IP) or Outpatient (OP)) – a surgical procedure and its follow–up care; the procedure may treat a chronic or acute condition.
- Other Condition – care for pregnancy and cancer episodes.
- In addition, there is one generic episode type included:
- System–Related Failures – inpatient and follow–up care for a condition caused by a systemic patient–safety failure.
- Exclusions: Some episodes have specific exclusion criteria, which are either based on clinical or administrative (eligibility/coverage) criteria.
- ICD–10 Codes: The ICD–9 diagnosis codes and the ICD–9 procedure codes for the above categories of codes have been cross–walked to ICD–10 codes leveraging the open–source GEM (Generalized Equivalence mapping) tables published by CMS.
- Index Condition: The index condition refers to the specific episode that the PAC relates to.
- Initial and Confirming Triggers: An initial trigger initiates an episode based on diagnosis and / or procedure codes found on institutional or non–institutional claims. For many episodes, a second trigger, the confirming trigger, is necessary to actually trigger the episode. Sometimes an episode itself could serve as a trigger for another episode, e.g., pregnancy episode in delivery episode.
- Clinical Association: HCI3´s PROMETHEUS Analytics© allows episodes to be connected to one another based on clinical relevance. For any individual patient, conditions and treatments, all of which trigger different episodes, are often related to one another from a clinical perspective. Episodes can be linked together for the analysis of their costs as either typical or complication.
- Look–Back & Look–Forward: From the point at which an episode is triggered, episode costs / volume are evaluated within the associated time window for a predetermined number of days before and after the trigger date. Costs, volume, and other episode components that fall within this range are captured within the episode.
- Pharmacy Codes: These are codes used to identify relevant pharmacy claims to be included in the episode. HCI3´s PROMETHEUS Analytics© groups pharmacy NDC codes into higher categories using the National Library of Medicine´s open–source RxNorm system of drug classification.
- Potentially Avoidable Complication (PAC): An episode contains services that are classified as typical care for the condition or as Potentially Avoidable Complications (PACs) of the condition. PACs include complication diagnosis codes that either (1) directly relate to the index condition; or, (2) indicate a failure in patient safety. PACs include hospitalizations, emergency room visits, and professional services related to these hospitalizations. PACs can also occur in outpatient settings. PACs also include failures to comply with patient safety guidelines, such as CMS' Hospital Acquired Conditions (HACs) and the Agency for Healthcare Research and Quality's Patient Safety Indicators (PSIs). Other patient safety failures (e.g. avoidable infections, drug interactions) may also be included as PACs.
As the "potentially" in the term indicates, a PAC indicates that services were performed related to a clinical event that may or may not have been preventable. As such, the goal is not to eliminate PACs but to reduce them as much as possible. Benchmarking the risk–adjusted occurrence of PACs for VBP contractors and MCOs also provides helpful information on possible areas of improvement. - Procedure Codes: These are codes used to identify clinically–related services to be included in the episode in conjunction with the typical diagnosis codes. These include CPT, HCPCS, and ICD–9 and ICD–10 procedure codes.
- Roll–Ups: Some episodes are associated with each other through HCI3's PROMETHEUS Analytics© clinical logic and are then grouped together under an 'umbrella' episode (called "level 5") to permit member–level analysis. Rolled–up costs include all costs/volume of associated episodes.
- Subtypes (code): Episodes often have subtypes or variants, which are useful to adjust for the severity of that episode, and reduce the need to have multiple episodes of the same type.
- Time–Window: This defines the time that an episode is open. It includes the trigger event, a look–back period and a look–forward period and could be extended based on rules and criteria.
- Trigger Code: A trigger code is the diagnosis or procedure code indicating the condition in question is present or procedure in question has occurred. Trigger codes are used to open new episodes and assign a time window for the start and end dates of each episode (depending on the episode type). Trigger codes can be ICD–9 or ICD–10 diagnosis or procedure codes, CPT or HCPCS codes, and could be present on an inpatient facility, outpatient facility, or professional claim.
Behavioral Health Chronic Conditions Quality Measure Summary
Behavioral Health Chronic Condition Clinical Advisory Group (CAG)
Quality Measure Recommendations
Introduction
Over the course of seven meetings the Behavioral Health CAG reviewed, discussed, and provided feedback on five individual Behavioral Health Chronic episodes. Four will be used for VBP contracting at this juncture. These are: 1) Depression & Anxiety Disorder; 2) Substance Use Disorder; 3) Bipolar Disorder, and; 4) Trauma & Stressor Disorder. An episode for Schizophrenia has been created and information pertaining to it will be released when contracting parameters have been developed.
The discussions in the CAG focused on reviewing quality measures is use currently, as well as measures under development by a variety of national measure stewards. Process and claims–based measures from New York State sources – including QARR and DSRIP – were also discussed. This document summarizes the CAG's recommendations.
The measures contained in this report pertain to treatment associated with each disorder. Screening measures for behavioral health conditions more appropriately handled by primary care physicians are included in the IPC Quality Measure Summary.
Selecting Quality Measures: criteria used to determine relevance:
Standard criteria for measure selection were used for all CAGs. The criteria are presented below along with examples.
Clinical relevance criteria
Focused on key outcomes of an integrated care process.
- Outcome measures (e.g., postpartum depression) are preferred over process measures (e.g., screening for postpartum depression);
- Outcomes of the total care process are preferred over outcomes of a single component of the care process (e.g., the quality of one type of professional's care)
For process measures: crucial evidence–based steps in integrated care process that may not be reflected in the patient outcomes measured should be reflected (e.g., focus on postpartum contraceptive care is key but will not be captured in outcomes of current maternity episode).
Existing variability in performance and/or possibility for improvement (e.g., blood pressure measurement during pregnancy is unlikely to be lower than >95% throughout the State)..
Reliability and validity criteria
Measure is well established by reputable organization
By focusing on established measures – those collected by the. NYS Office of Patient Quality and Safety (OQPS), endorsed by the National Quality Forum (NQF), part of the Healthcare Effectiveness Data and Information Set (HEDIS) measures, for example – validity and reliability of measures are assumed acceptable.
Outcome measures are adequately risk–adjusted (e.g., measuring '% preterm births' without adequate risk adjustment makes it impossible to compare performance among providers).
Feasibility criteria
Claims–based measures are preferred over non–claims based measures (e.g. clinical data, surveys)
- Ease of data collection data is an important consideration and measures should not place undue burden on providers.
Existing sources are preferable when clinical data or surveys are required (e.g., the vital statistics repository based on birth certificates).
Patient–level data sources are preferable
- Measures that require random samples (e.g. sampling patient records or using surveys) are not ideal because they do not drill down to the patient level and/or allow for adequate risk adjustment, and may add to the data collection burden. An exception is made for measures that are already part of DSRIP/QARR.
Data must be available without significant delay
- In general, measure data sources should not have a longer lag than claims–based measures (about six months). This is an issue with the vital statistics repository, for example, which has a one–year lag for New York City data.
Meaningful and actionable criteria
Measures should not only be related to the goals of care but be usable by the provider to improve care.
|top of section| |top of page|Categorizing and Prioritizing Quality Measures
Based on the criteria above, the CAG discussed the quality measures and placed them in three categories:
- Category 1 – Category 1 comprises recommended quality measures that were judged clinically relevant, reliable, valid, and feasible;
- Category 2 – Category 2 quality measures were judged clinically relevant, valid, and likely reliable but presented feasibility problems. These quality measures could be targeted for further development including investigation during the 2016 or 2017 pilots.
- Category 3 – Category 3 measures were judged irrelevant, invalid, unreliable, and/or infeasible.
All Category 1 and 2 will be examined in VBP arrangements during the pilot phase in 2016 and 2017. During this time the CAG will be reassembled periodically to reflect on and further refine the Category 1 and 2 measures.
The HCI3 grouper creates condition–specific scores for Potentially Avoidable Complications (PACs) for each condition. The "percentage of total episode costs" that PACs comprise is a useful measure for the identification of potential improvement areas, although it cannot be interpreted as a specific quality measure. However, "PAC counts" (capturing the frequency of PAC occurrence in episodes) is in use as a quality measure nationally and can be used by New York State.
|top of section| |top of page|Overview of Depression & Anxiety Quality Measure Discussion
The Clinical Advisory Group evinced strong support for the IMPACT model, recommending the screening/diagnosis, initiation and adjustment of treatment, and symptom reduction measures. The group also emphasized the importance of suicide risk assessment and management of suicidal ideations for the at–risk segment of depressed members. More generally, the CAG reflected on the need to establish strong feedback mechanisms from diagnosis to follow–up and reassessment to ensure that practitioners are connecting appropriately with affected members.
|top of section| |top of page|Depression & Anxiety Recommended Quality Measures – Category 1 & 2
| No. | Measure | Measure Steward/Source | |
|---|---|---|---|
| Category 1 | 1 | Diagnosis (IMPACT Model) | University of Washington |
| 2 | Initiation of Treatment (IMPACT Model) | University of Washington | |
| 3 | Adjustment of Treatment Based on Outcomes (IMPACT Model) | University of Washington | |
| 4 | Symptom Reduction (IMPACT Model) | University of Washington | |
| 5 | Adult Major Depressive Disorder (MDD): Suicide Risk Assessment (note: only for use if suicide risk is assessed to be present) | AMA-PCPI | |
| 6 | Follow-Up After Hospitalization for Mental Illness within 7 Days and 30 Days | HEDIS | |
| 7 | Follow-up after Discharge from the Emergency Department for Mental Health or Alcohol or Other Drug Dependence | NCQA | |
| 8 | Readmission to mental health inpatient care within 30 days of discharge | IPRO | |
| 9 | Potentially Avoidable Complications | HCI3 | |
| 10 | Generalized Anxiety Disorder 7-item (GAD 7) Scale | Substance Abuse and Mental Health Services Administration |
Overview of Substance Use Disorder (SUD) Quality Measure Discussion
The CAG discussed the importance of aligning with quality measurement efforts underway at the NYS Office of Alcoholism and Substance Abuse Services (OASAS) and with other measure sets currently in use (e.g. HEDIS/QARR). In general, the group acknowledged a dearth of validated measures in the SUD field and the need to improve quality measurement. OASAS is working to develop a more comprehensive SUD measure framework to comport with the model espoused by the Institute of Medicine (IOM).
|top of section| |top of page|Substance Use Disorder Recommended Quality Measures – Category 1 & 2
| No. | Measure | Measure Steward/Source | |
|---|---|---|---|
| Category 1 | 11 | Continuing Engagement in Treatment (CET) | Washington Circle Group |
| 12 | Continuity of care within 14 days of discharge from any level of SUD inpatient care (COC) | Washington Circle Group | |
| 13 | Follow–Up After Emergency Department Visit for Alcohol and Other Drug Dependence | NCQA | |
| 14 | Initiation of MAT for Alcohol Dependence | Washington Circle Group | |
| 15 | Initiation of MAT for Opioid Dependence | Washington Circle Group | |
| 16 | Potentially Avoidable Complications | HCI3 | |
| Category 2 | 17 | Utilization of MAT for Opioid Dependence | Washington Circle Group |
| 18 | Utilization of MAT for Alcohol Dependence | Washington Circle Group | |
| 19 | Connection to Community Recovery Supports | OASAS |
Overview of Bipolar Disorder Quality Measure Discussion
The CAG reviewed existing NCQA/HEDIS measures and noted the need for more robust measures. The group drew from a larger, developmental measure set from the Center for Quality Assessment and Improvement in Mental Health. These measures are not in widespread use currently but could provide a basis for the development of a more comprehensive quality framework for individuals with bipolar disorder. For this reason, these measures were placed in Category 2.
|top of section| |top of page|Bipolar Disorder Recommended Quality Measures – Category 1 & 2.
| No. | Measure | Measure Steward/Source | |
|---|---|---|---|
| Category 1 | 20 | Bipolar Disorder and Major Depression: Appraisal for alcohol or chemical substance use | NQF |
| 21 | Cardiovascular Health Screening for People With Schizophrenia or Bipolar Disorder Who Are Prescribed Antipsychotic Medications | NCQA | |
| 22 | Diabetes Screening for People With Schizophrenia or Bipolar Disorder Who Are Using Antipsychotic Medications | HEDIS | |
| 23 | Readmission to mental health inpatient care within 30 days of discharge | OMH Proposed (QARR) | |
| 24 | Follow–Up After Hospitalization for Mental Illness within 7 Days and 30 Days | HEDIS | |
| 25 | Potentially Avoidable Complications | HCI3 | |
| Category 2 | 26 | Adherence to Mood Stabilizers for Individuals with Bipolar I Disorder | CMS |
| 27 | Bipolar disorder: the percentage of patients with Bipolar I Disorder with mania/hypomania, mixed or cycling symptoms and behaviors who have evidence of use of pharmacotherapy agent with antimanic properties during the first 12 weeks of treatment. | Center for Quality Assessment and Improvement in Mental Health | |
| 28 | Bipolar disorder: percentage of patients with Bipolar I Disorder with depressive symptoms and behaviors who have evidence of use of a mood stabilizing or antimanic agent during the first 12 weeks of pharmacotherapy treatment. | Center for Quality Assessment and Improvement in Mental Health | |
| 29 | Bipolar disorder: the percentage of patients diagnosed with bipolar disorder and treated with lithium who have evidence of a lithium serum medication level with 12 weeks of beginning treatment. | Center for Quality Assessment and Improvement in Mental Health | |
| 30 | Bipolar disorder: the percentage of patients with Bipolar I Disorder symptoms and behaviors who received monotherapy with an antidepressant agent during the first 12 weeks of treatment. | Center for Quality Assessment and Improvement in Mental Health | |
| 31 | Bipolar disorder: the percentage of patients with bipolar disorder who receive a recommendation for an adjunctive psychosocial intervention, including evidence-based therapies, within 12 weeks of initiating treatment. | Center for Quality Assessment and Improvement in Mental Health | |
| 32 | Bipolar disorder: the percentage of patients diagnosed and treated for bipolar disorder who are provided with education and information about their illness and treatment within 12 weeks of initiating treatment. | Center for Quality Assessment and Improvement in Mental Health |
Overview of Trauma & Stressor Quality Measure Discussion
The Clinical Advisory Group discussed the episode and noted a dearth of quality measures for trauma treatment in general. Their recommendation is to follow the development of the Primary Care PTSD Screen measure, as it may be able to be used as a quantifiable rating scale in the near future.
|top of section| |top of page|Trauma & Stressor CAG Recommended Quality Measures – Category 1 & 2.
| No. | Measure | Measure Steward/Source | |
|---|---|---|---|
| Category 1 | 33 | Follow–Up After Hospitalization for Mental Illness within 7 Days and 30 Days | HEDIS |
| 34 | Potentially Avoidable Complications | HCI3 | |
| Category 2 | 35 | Primary Care PTSD Screen (PC–PTSD) | National Center for PTSD |
CAG Categorization and Discussion of Measures – Category 1 & 2
| Topic | # | Quality Measure (* = NQF Endorsed) | Type of Measure | Measure Steward/ Source | Data Required | Quality Measure Categorization & Notes | ||
|---|---|---|---|---|---|---|---|---|
| Medicaid Claims Data | Clinical Data | Category | Notes | |||||
| Depression & Anxiety | 1 | Diagnosis (IMPACT Model) | Process | University of Washington | Yes | No | 1 | |
| 2 | Initiation of Treatment (IMPACT Model) | Outcome | University of Washington | Yes | No | 1 | ||
| 3 | Adjustment of Treatment Based on Outcomes (IMPACT Model) | Process | University of Washington | Yes | No | 1 | ||
| 4 | Symptom Reduction (IMPACT Model) | Outcome | University of Washington | Yes | No | 1 | ||
| 5 | Adult Major Depressive Disorder (MDD): Suicide Risk Assessment* (note: only for use if suicide risk is assessed to be present) | Process | AMA–PCPI | No | Yes | 1 | ||
| 6 | Follow–Up After Hospitalization for Mental Illness within 7 Days and 30 Days | Outcome | HEDIS | Yes | Yes | 1 | ||
| 7 | Follow–up after Discharge from the Emergency Department for Mental Health or Alcohol or Other Drug Dependence | Outcome | NCQA | Yes | No | 1 | ||
| 8 | Readmission to mental health inpatient care within 30 days of discharge | Outcome | IPRO | No | Yes | 1 | ||
| 9 | Potentially Avoidable Complications | Outcome | HCI3 | Yes | No | 1 | ||
| 10 | Generalized Anxiety Disorder 7–item (GAD 7) Scale | Process | Substance Abuse and Mental Health Services Administration | No | Yes | 2 | ||
| Substance Use Disorder | 11 | Expansion of IET to Continuing Engagement in Treatment (CET) | Process | NCQA | Yes | No | 1 | |
| 12 | Continuity of care within 14 days of discharge from any level of SUD inpatient care (COC) | Process | Washington Circle Group | Yes | No | 1 | ||
| 13 | Follow–Up After Emergency Department Visit for Alcohol and Other Drug Dependence | Process | NCQA | Yes | No | 1 | ||
| 14 | Initiation of MAT for Alcohol Dependence | Process | Washington Circle Group | Yes | No | 1 | ||
| 15 | Initiation of MAT for Opioid Dependence | Process | Washington Circle Group | Yes | No | 1 | ||
| 16 | Potentially Avoidable Complications | Outcome | HCI3 | Yes | No | 1 | ||
| 17 | Utilization of MAT for Opioid Dependence | Process | Washington Circle Group | Yes | No | 2 | ||
| 18 | Utilization of MAT for Alcohol Dependence | Process | Washington Circle Group | Yes | No | 2 | ||
| 19 | Connection to Community Recovery Supports | Process | OASAS | No | Yes | 2 | ||
| Bipolar Disorder | 20 | Bipolar Disorder and Major Depression: Appraisal for alcohol or chemical substance use | Process | NQF | Yes | Yes | 1 | |
| 21 | Cardiovascular Health Screening for People With Schizophrenia or Bipolar Disorder Who Are Prescribed Antipsychotic Medications | Process | NCQA | Yes | Yes | 1 | ||
| 22 | Diabetes Screening for People With Schizophrenia or Bipolar Disorder Who Are Using Antipsychotic Medications | Process | HEDIS | Yes | No | 1 | ||
| 23 | Readmission to mental health inpatient care within 30 days of discharge | Outcome | OMH Proposed (QARR) | Yes | Yes | 1 | OMH has proposed a mental health readmission measure (readmissions after 30 days), would like to follow up with the state on if this measure will be entered into QARR. | |
| 24 | Follow–Up After Hospitalization for Mental Illness within 7 Days and 30 Days | Outcome | HEDIS | Yes | Yes | 1 | ||
| 25 | Potentially Avoidable Complications | Outcome | HCI3 | Yes | No | 1 | ||
| 26 | Adherence to Mood Stabilizers for Individuals with Bipolar I Disorder | Process | CMS | Yes | Yes | 2 | Very relevant if feasible | |
| 27 | Bipolar disorder: the percentage of patients with Bipolar I Disorder with mania/hypomania, mixed or cycling symptoms and behaviors who have evidence of use of pharmacotherapy agent with antimanic properties during the first 12 weeks of treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 2 | The CAG wants to conduct further research to see if this is available through claims data. | |
| 28 | Bipolar disorder: percentage of patients with Bipolar I Disorder with depressive symptoms and behaviors who have evidence of use of a mood stabilizing or antimanic agent during the first 12 weeks of pharmacotherapy treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 2 | The CAG agrees more information is required to see if this is feasible. | |
| 29 | Bipolar disorder: the percentage of patients diagnosed with bipolar disorder and treated with lithium who have evidence of a lithium serum medication level with 12 weeks of beginning treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 2 | The CAG agrees more information is required to see if this is feasible. | |
| 30 | Bipolar disorder: the percentage of patients with Bipolar I Disorder symptoms and behaviors who received monotherapy with an antidepressant agent during the first 12 weeks of treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 2 | The CAG agrees more information is required to see if this is feasible. | |
| 31 | Bipolar disorder: the percentage of patients with bipolar disorder who receive a recommendation for an adjunctive psychosocial intervention, including evidence–based therapies, within 12 weeks of initiating treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 2 | The CAG would like to see if this is available through pharmacy data. | |
| 32 | Bipolar disorder: the percentage of patients diagnosed and treated for bipolar disorder who are provided with education and information about their illness and treatment within 12 weeks of initiating treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 2 | The CAG agreed, this is critical measure. However there needs to be a feasible way to implement and collect a measure on the education and information component of bipolar. | |
| Trauma & Stressor | 33 | Follow–Up After Hospitalization for Mental Illness within 7 Days and 30 Days | Outcome | HEDIS | Yes | Yes | 1 | |
| 34 | Potentially Avoidable Complications | Outcome | HCI3 | Yes | No | 1 | ||
| 35 | Primary Care PTSD Screen (PC–PTSD) | Process | National Center for PTSD | No | Yes | 2 | ||
CAG Categorization and Discussion of Measures – Category 3
| Topic | # | Quality Measure (* = NQF Endorsed) | Type of Measure | Measure Steward/ Source | Data Required | Quality Measure Categorization & Notes | ||
|---|---|---|---|---|---|---|---|---|
| Medicaid Claims Data | Clinical Data | Category | Notes | |||||
| Depression & Anxiety | 1 | Depression Response at Twelve Months – Progress Towards Remission* | Outcome | MN Community Measurement | No | Yes | 3 | |
| 2 | Depression Remission at Six Months | Process | MN Community Measurement | Yes | No | 3 | ||
| 3 | Depression Remission at Twelve Months | Process | MN Community Measurement | Yes | No | 3 | ||
| 4 | Measurement of Treatment Outcomes (IMPACT Model) | Outcome | University of Washington | Yes | No | 3 | ||
| 5 | Timely filling of appropriate medication prescriptions post discharge (30 days and 100 days) | Outcome | BHO I | No | No | 3 | ||
| 6 | Potentially preventable ED visits (for persons with BH diagnosis) | Outcome | 3M | Yes | No | 3 | ||
| 7 | Potential preventable readmission for SNF (skilled nursing facilities) patients | Outcome | 3M | Yes | No | 3 | ||
| 8 | Percent of Long Stay Residents who have Depressive Symptoms | Outcome | CMS | Yes | Yes | 3 | ||
| 9 | Initiation and Engagement of Alcohol and Other Drug Dependence Treatment | Outcome | NCQA | Yes | No | 3 | ||
| 10 | Child and Adolescent Major Depressive Disorder (MDD): Suicide Risk Assessment* | Process | AMA–PCPI | No | Yes | 3 | ||
| 11 | Major Depressive Disorder (MDD): Diagnostic Evaluation | Process | AMA–PCPI | No | Yes | 3 | ||
| 12 | Preventive Care and Screening for Clinical Depression and Follow–up Plan | Process | CMS | Yes | Yes | 3 | ||
| 13 | (Screening, Brief Intervention, and Referral to Treatment) SBIRT screening | Process | MASBIRT | No | Yes | 3 | ||
| 14 | Multidimensional Mental Health Screening Assessment | Process | M3 Information LLC | No | Yes | 3 | ||
| 15 | Bipolar Disorder and Major Depression: Appraisal for alcohol or chemical substance use | Process | Center for Quality Assessment and Improvement in Mental Health | Yes | Yes | 3 | ||
| 16 | Acute Stress Disorder Interview (ASDI) 1 | Process | PTSD: National Center for PTSD | No | Yes | 3 | 1 Quality Measures recommended by the National Center for PTSD for assessing Acute Stress Disorder (ASD). More information found at: http://www.ptsd.va.gov/professional/treatment/early/acute–stress–disorder.asp | |
| 17 | Acute Stress Disorder Scale (ASDS) 1 | Process | PTSD: National Center for PTSD | No | Yes | 3 | ||
| 18 | Social Phobia Inventory (SPIN) 2 | Process | ICHOM | No | Yes | 3 | 2Additional Quality Measures recommended in the International Consortium for Health Outcomes Measurement (ICHOM) – Depression & Anxiety Standard Set. | |
| 19 | Mobility Inventory for Agoraphobia (MIA) 2 | Process | ICHOM | No | Yes | 3 | ||
| 20 | Panic Disorder Severity Scale (PDSS–SR) 2 | Process | ICHOM | No | Yes | 3 | ||
| 21 | Obsessive–Compulsive Inventory (OCI–R) 2 | Process | ICHOM | No | Yes | 3 | ||
| 22 | Recommended to track via the World Health Organization Disability Assessment 2.0 (WHODAS 2.0) 2 | Process | ICHOM | No | Yes | 3 | ||
| Substance Use Disorder | 23 | 14–Day Follow–up after Initiating Substance–related Treatment | Process | Washington Circle Group | No | Yes | 3 | |
| 24 | 1–Month Retention Rate for Chemical Dependency Treatment | Process | NY State Office of Alcoholism and Substance Abuse Services/CQAIMH | No | Yes | 3 | ||
| 25 | 1–Week Retention Rate for Chemical Dependency Treatment | Process | NY State Office of Alcoholism and Substance Abuse Services/CQAIMH | No | Yes | 3 | ||
| 26 | 1–Year Retention Rate for Chemical Dependency Treatment | Process | NY State Office of Alcoholism and Substance Abuse Services/CQAIMH | No | Yes | 3 | ||
| 27 | 3–Month Retention Rate for Chemical Dependency Treatment | Process | NY State Office of Alcoholism and Substance Abuse Services/CQAIMH | No | Yes | 3 | ||
| 28 | 60–day Continuation of Substance Abuse Treatment | Process | NY State Office of Alcoholism and Substance Abuse Services/CQAIMH | No | Yes | 3 | ||
| 29 | 6–Month Retention Rate for Chemical Dependency Treatment | Process | NY State Office of Alcoholism and Substance Abuse Services/CQAIMH | No | Yes | 3 | ||
| 30 | Identification Alcohol & Drug Services (IAD) | Process | OASAS | Yes | No | 3 | ||
| 31 | Adult Current Smoking Prevalence | Process | Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion | No | Yes | 3 | ||
| 32 | Ambulatory Follow–up Attended within 30 Days of Discharge Substance Abuse | Process | American Managed Behavioral Healthcare Association | No | Yes | 3 | ||
| 33 | Availability of Alcohol Counseling and Education | Process | Foundation for Accountability | No | Yes | 3 | ||
| 34 | Blood Pressure Control (<140/90 mm Hg) (SUD Link: Alcohol, cocaine, amphetamine use – raised BP) | Process | NCQA | Yes | Yes | 3 | ||
| 35 | Chemical Dependency Utilization– % of Members Receiving Inpatient, Day/Night Care & Ambulatory Services | Process | NCQA | No | Yes | 3 | ||
| 36 | Completion of Treatment for Substance Abuse | Process | Texas Commission on Alcohol and Drug Abuse | No | Yes | 3 | ||
| 37 | Connectivity to Primary Care | Process | OASAS | No | Yes | 3 | ||
| 38 | Counseling Regarding Psychosocial and Pharmacologic Treatment Options for Opioid Addiction | Process | AMA–PCPI | No | Yes | 3 | ||
| 39 | Follow–up after Discharge from the Emergency Department for Mental Health or Alcohol or Other Drug Dependence | Process | NCQA | Yes | No | 3 | ||
| 40 | Functional Outcome Assessment | Process | CMS | Yes | Yes | 3 | ||
| 41 | GAD–7 | Outcome | Substance Abuse and Mental Health Services Administration | No | Yes | 3 | ||
| 42 | Improvement / Stability in Activities of Daily Living (ADL) Functioning | Process | NY State–specified measure | No | Yes | 3 | ||
| 43 | Initiation measure: Opioid Parameters: Number of individuals who initiate pharmacotherapy with at least one prescription for an opioid treatment medication within 30 days following index visit with a diagnosis of opioid dependence. | Process | OASAS | Yes | Yes | 3 | ||
| 44 | Maintenance Pharmacotherapy for Substance Abuse | Process | American Psychiatric Association | No | Yes | 3 | ||
| 45 | Measures from MRT/Behavioral Health Medicaid Managed Care Phase I (BHO 1): Continuity of Care (CoC) from Detox or Inpatient Rehab to a lower level of SUD treatment (within 14 days). | Process | OASAS | No | Yes | 3 | ||
| 46 | Multiple Outpatient Visits after Substance–Related Hospitalization | Process | Department of Veterans Affairs– Palo Alto Health Care System | No | Yes | 3 | ||
| 47 | Outpatient Follow–up after Initial Substance–Related Visit (2 or more visits) | Process | Department of Veterans Affairs–Palo Alto Health Care System | No | Yes | 3 | ||
| 48 | Outpatient Visit within 3 Days of Discharge (Substance Abuse) | Process | Department of Veterans Affairs– Palo Alto Health Care System | No | Yes | 3 | ||
| 49 | PHQ–9 | Outcome | Center for Quality Assessment and Improvement in Mental Health (CQAIMH) | No | Yes | 3 | ||
| 50 | Prenatal & Postpartum Care (PPC) (SUD Link: SUD impact on pregnancy and postpartum care) | Process | NCQA | Yes | Yes | 3 | ||
| 51 | Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow–Up (SUD Link: Alcohol – Glucose intolerance) | Process | CMS | Yes | Yes | 3 | ||
| 52 | Preventive Care and Screening: Unhealthy Alcohol Use: Screening & Brief Counseling | Process | AMA–convened Physician Consortium for Performance Improvement | No | Yes | 3 | ||
| 53 | Program Completion for Chemical Dependency Treatment | Process | NY State Office of Alcoholism and Substance Abuse Services/CQAIMH | No | Yes | 3 | ||
| 54 | Promoting Healthy Development Survey (PHDS) | Process | Oregon Health & Science University | No | Yes | 3 | ||
| 55 | Proposed Pay–for–Reporting measure: To support decreases in inpatient crisis (detox) with corresponding uptake in ancillary withdrawal services. | Process | OASAS | No | Yes | 3 | ||
| 56 | Proposed Refinement of Measures (with OQPS/OMH) for MRT/Behavioral Health Medicaid Managed Care Phase II (BHO 2): Continuity of Care (CoC) measures to include residential and all OASAS treatment modalities. | Process | OASAS | No | Yes | 3 | ||
| 57 | Readmission Rates for Chemical Dependency | Process | NCQA | No | Yes | 3 | ||
| 58 | Risky Behavior Assessment or Counseling by Age 13 Years | Process | NCQA | No | Yes | 3 | ||
| 59 | Risky Behavior Assessment or Counseling by Age 18 Years | Process | NCQA | No | Yes | 3 | ||
| 60 | Screening for MH/PH Disorder | Process | OASAS | No | Yes | 3 | ||
| 61 | Opioid and Alcohol parameters: Number of individuals with at least one prescription for appropriate pharmacotherapy at any time during the measurement year | Process | OASAS | Yes | Yes | 3 | ||
| 62 | Initiation measure: Alcohol Parameter: Number of individuals who initiate pharmacotherapy with at least one prescription for an alcohol treatment medication within 30 days following index visit with a diagnosis of alcohol dependence | Process | OASAS | Yes | Yes | 3 | ||
| 63 | SUB–1 Alcohol Use Screening | Process | The Joint Commission | No | Yes | 3 | ||
| 64 | SUB–2 Alcohol Use Brief Intervention Provided or offered SUB–2a Alcohol Use Brief Intervention | Process | The Joint Commission | No | Yes | 3 | ||
| 65 | SUB–3 Alcohol & Other Drug Use Disorder Treatment Provided or Offered at Discharge SUB–3a Alcohol & Other Drug Use Disorder Treatment at Discharge | Process | The Joint Commission | No | Yes | 3 | ||
| 66 | Substance Abuse Treatment Following Detoxification | Process | Washington Circle Group | No | Yes | 3 | ||
| 67 | Substantial Decline in 3 or more Activities of Daily Living | Process | CMS | No | Yes | 3 | ||
| Bipolar Disorder | 68 | Bipolar disorder: the percentage of patients with bipolar disorder who receive an initial assessment that considers alcohol and chemical substance use. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 3 | –Not feasible |
| 69 | Bipolar disorder: the percentage of patients diagnosed with bipolar disorder who receive an initial assessment that considers the risk of suicide. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 3 | –Not feasible | |
| 70 | Bipolar disorder: the percentage of patients diagnosed with bipolar disorder and treated with an atypical antipsychotic agent who received at least one assessment for hyperlipidemia within the initial 16 week period of treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 3 | Have QARR measures on this | |
| 71 | Bipolar disorder: the percentage of patients diagnosed with bipolar disorder and treated with an antipsychotic agent who were assessed for the presence of extrapyramidal symptoms twice within the first 24 weeks of treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 3 | Not Feasible | |
| 72 | Bipolar disorder: the percentage of patients diagnosed with bipolar disorder and treated with an atypical antipsychotic agent who receive at least one screening for hyperglycemia within the initial 16 weeks of treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 3 | Have HEDIS measure on treatment | |
| 73 | Bipolar disorder: the percentage of patients diagnosed and treated for bipolar disorder who are monitored for change in their symptom complex within 12 weeks of initiating treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 3 | Not Feasible | |
| 74 | Bipolar disorder: the percentage of patients diagnosed and treated for bipolar disorder who are monitored for change in their level–of–functioning in response to treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 3 | Not Feasible | |
| 75 | Bipolar disorder: the percentage of patients with bipolar disorder who were monitored for weight gain during initial 12 week period of treatment. | Process | Center for Quality Assessment and Improvement in Mental Health | No | Yes | 3 | Not Feasible | |
| 76 | Potentially preventable readmissions (PPR) for SNF patients | Outcome | 3M | Yes | No | 3 | This specific measure is not relevant for use for just the bipolar population. | |
| Trauma & Stressor | 77 | Primary Care PTSD Screen (PC–PTSD) | Process | National Center for PTSD | No | Yes | 3 | |
| 78 | PTSD Checklist for DSM–5 (PCL–5) | Process | National Center for PTSD | No | Yes | 3 | ||
| 79 | Clinician–Administered PTSD Scale for DSM–5 (CAPS–5) | Process | National Center for PTSD | No | Yes | 3 | ||
Appendix A: Meeting Schedule
| Date | Agenda | |
|---|---|---|
| CAG #1 | 8/12/2015 |
|
| CAG #2 | 9/15/15 |
|
| CAG #3 | 10/6/2015 |
|
| CAG #4 | 4/28/2016 |
|
| CAG #5 | 6/23/2016 |
|
| CAG #6 | 7/8/2016 |
|
| CAG #7 (Webinar) | 8/24/2016 |
|
______________________________________________________
1. https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/2016/docs/2016–jun_annual_update.pdf. 1
2. The term "bundle" is used to refer to a combination of individual episodes. 2
3. http://www.HCI3.org/content/online–courses 3
Follow Us