Long-Term Care
Value Based Payment Recommendation Report
Managed Long–Term Care Clinical Advisory Group
- Report is also available in Portable Document Format (PDF)
NYS Medicaid Value Based Payment
December 2016
| Contents |
|---|
Introduction
|
Managed Long–Term Care Clinical Advisory Group (CAG)
|
Playbook Overview
|
| Managed Long–Term Care Clinical Advisory Group (CAG) |
| Introduction |
| Selecting Quality Measures: Criteria used to consider relevance |
| Categorizing and Prioritizing Quality Measures |
| Managed Long–Term Care CAG Recommended Quality Measures – Category 1 & 2 |
| CAG Categorization and Discussion of Measures – Category 1 & 2 |
| CAG Categorization and Discussion of Measures – Category 3 |
| Attachment A: Glossary |
| Appendix B: Meeting Schedule |
Introduction
Delivery System Reform Incentive Payment (DSRIP) Program and Value Based Payment (VBP) Overview
The New York State DSRIP program aims to fundamentally restructure New York State´s healthcare delivery system, reducing avoidable hospital use by 25%, and improving the financial sustainability of New York State´s safety net.
To further stimulate and sustain this delivery reform, at least 80–90% of all payments made from Managed Care Organizations (MCOs) to providers will be captured within VBP arrangements by 2020. The goal of converting to VBP arrangements is to develop a sustainable system which incentivizes value over volume. The Centers for Medicare & Medicaid Services (CMS) has approved the State´s multi–year VBP Roadmap, which details the menu of options and different levels of VBP that the MCOs and providers can select.
The NYS VBP Roadmap outlines two types of VBP arrangements:
- Population–based VBP arrangements
- Episode–based VBP arrangements
This document describes the Long–Term Care Subpopulation
|top of page|Managed Long–Term Care Clinical Advisory Group (CAG)
CAG Overview
For every VBP Arrangement, Clinical Advisory Groups (CAGs) were been formed to discuss the definition of each VBP arrangement and identify relevant, feasible and valid quality measures. Each CAG comprises leading experts and key stakeholders from throughout New York State, including representatives from providers, universities, State agencies, medical societies, and clinical experts.
The Managed Long–Term Care CAG held a series of four meetings throughout the State and discussed key components of the Long–Term Care VBP arrangement, including subpopulation definitions, risk adjustment, and quality measures. For a full list of meeting dates, times, and overview of discussions to date please see Appendix A.
Recommendation Report Overview & Components
The following report contains two key components:
Long–Term Care VBP Arrangement Definition
The playbook provides an overview of the episode definition and clinical descriptions.
Long–Term Care VBP Arrangement Quality Measures Summary
The Quality Measure section provides a description of the criteria used to categorize measures for relevancy, validity, and difficulty of collection. Measures were prioritized, and a listing of the recommended quality measures was prepared and reviewed by the group.
|top of page|Long–Term Care VBP Arrangement Definition
Playbook Overview
New York State´s VBP Roadmap1 details how the State will transition 80–90% of managed care payments from fee for service (FFS) to value based payments (VBP). The NYS VBP Roadmap outlines two types of VBP arrangements:
- Population–based VBP arrangements
- Episode–based VBP arrangements
For the Subpopulations, severe co–morbidity or disability leads to highly specific and costly care needs, so that the majority (or even all) of the care delivered and costs are determined by the specific characteristics of these members. For these subpopulations, a VBP model which includes the total care (and thus total costs) for these often vulnerable members is best suited. As part of the movement towards managed care, the State has already identified several special needs subpopulations that have their own dedicated managed care arrangement:
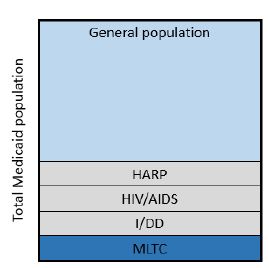
- Members with HIV/AIDS
- Members eligible for Health and Recovery Plans (HARP)
- Members with Intellectual/Developmental Disabilities (I/DD)2
- Members in Managed Long–Term Care (MLTC)
All other members are part of the general population and are eligible for episodic and bundled VBP arrangements such as maternity and integrated primary care.
This document focuses on the MLTC subpopulation arrangement.
The table below provides an overview of the sections in this playbook.
| Section | Short Description |
|---|---|
| Description of subpopulation | Details on the Long–Term Care subpopulation |
| Definition of subpopulation | Detailed definition of the Long–Term Care subpopulation |
| Services included in the subpopulation | Overview of services included in the Long–Term Care subpopulation |
Definition of Long–Term Care subpopulation
This subpopulation includes members enrolled in Managed Long–Term Care plans (home health and nursing home care).
Enrollment in an MLTC plan is mandatory for those who are dually eligible for Medicaid and Medicare, over 21 years of age, and in need of community–based long–term care services for more than 120 days. Enrollment is also mandatory for nursing home occupants who become permanent residents after July 1, 2015. The Long–Term Care (LTC) subpopulation includes all these Medicaid members. It does not include Medicaid members who are eligible but are not (yet) enrolled. The LTC subpopulation can (but does not have to) be subdivided in two groups:
- Members assigned by their MLTC to home care
- Members assigned by their MLTC to nursing home care
Enrollment in MLTC plans grew from about 134,300 to 148,000 members during the 2014 plan year, an increase of 13,700 members, or 10%. Average annual Medicaid cost per member in 2014 was approximately $41,750, or about $3,500 per member per month (PMPM), excluding Medicare costs. Nursing home benefits are gradually transitioning from FFS to MLTC plans. During the transition, MLTC membership and costs will rise significantly.
Which services are included in the Long–Term Care subpopulation?
MLTC plans cover services such as home care, adult day care, home–delivered meals, medical equipment, certain home modifications, non–emergent medical transportation, podiatry, audiology, dentistry, optometry, nursing home care and care coordination. All services available through MLTC plans are included in the subpopulation VBP arrangement. Services covered by Medicare are not included at this point. Efforts to align New York State´s Medicaid VBP arrangements with Medicare, to allow for VBP arrangements to span across the Medicaid–Medicare divide, will continue.
Value Based Payment and LTC
Unique for NYS Medicaid VBP is the focus on the entire trajectory of the member: the total cost and outcomes throughout the different ´silos´ of care (nursing homes, home care, personal care, acute care, medications and so forth). For the LTC population, this approach is hindered by the inability to integrate Medicare services and costs with Medicaid services and costs. In addition, an evident opportunity to improve outcomes and reduce overall costs is to prevent avoidable hospitalizations or (re)admissions from nursing homes and homecare settings. However, preventing unnecessary hospitalizations results in savings for Medicare that cannot be captured by Medicaid providers unless CMS and NYS set up specific initiatives to make this possible (such as Fully Integrated Dual Advantage (FIDA) plans). Efforts to more fully align with Medicare have thus far been unsuccessful, although they will continue.
Anticipating this challenge, the Roadmap states:
"Preventing avoidable hospital use in this population is part of DSRIP´s goals, and should be equally incentivized through payment reform. Improving palliative care, for example, can greatly enhance the quality of care and quality of life for some patients. […T]he State aims to treat potentially avoidable hospital use as ´quality outcomes´ for this subpopulation, improving the quality of life for these members, and rewarding MLTC providers when certain levels of reduced avoidable hospital use are reached. Such arrangements could be treated as Level 1 VBP arrangements, and would be eligible for financial incentives. Even if the savings would primarily accrue to Medicare, the State will not pass on the opportunity to make significant strides in meeting the needs of this part of the dual eligible population."
The State intends to create an additional Quality Pool to be reward higher rates of avoidable hospital use (see the Quality Measures section for metrics under consideration for this purpose).
Value Based Payment within Medicaid
Although realizing Medicare–related savings remains a priority, the CAG concluded that significant savings while improving quality of life within the Medicaid portion of MLTC were also possible. For members in need of home care, savings could be realized by extending the period the member is able to stay at home (i.e., admission to the nursing home is delayed or avoided all together). For those members living in a nursing home, Medicaid savings could be realized primarily by transitioning residents who are able to do so back into the community, supported by home care if needed. The savings here would be realized by ´beating the premium´ for these members: lowering admission rates and care costs below what is projected in the premium. In these ways total costs of care for the LTC member would decrease, and the savings realized can be shared between MLTC plan and the provider.
The discussions in the CAG led to the recommendation to allow the VBP arrangements to cover only one component of LTC:
- Home Health providers contracting total (Medicaid) costs of care for those members assigned by the MLTC to home care
- Nursing Home providers contracting total (Medicaid) costs of care for those members assigned by the MLTC to a Nursing Home.
Ideally, VBP contracts would span the entire spectrum of MLTC care, so as to maximally incentivize LTC providers to optimize costs versus quality of care. Yet the CAG had three main concerns:
- The organizational infrastructure in the MLTC provider world is not yet well enough integrated to support total cost of care arrangements;
- The cost profile of members within these two care settings is very different, thus creating potentially irresponsible insurance risk for VBP contractors;
- Creating the right incentives is possible without full integration, and the MLTC plan should already be incentivized to assign the member to the appropriate site of care. The MLTC plan can facilitate creating expected costs for the member in question (including both home health and nursing home costs) and calculate potential shared savings accordingly. During the start of VBP contracting in MLTC, the State will support both VBP contractors and plans by providing data across the continuum of care and e.g. monitoring patterns of care (e.g., transitions between home care and nursing home care, quality scores).
Risk adjustment for MLTC VBP Contracts
Risk adjustment takes into account the profile of the population insured (e.g., member demographics such as gender and age), the acuity of a member´s condition(s), and the functional capability of the member. The risk adjustment methodology used in VBP will be identical to the risk adjustment used by the State to calculate MLTC premiums.
In addition to the demographic variables used in traditional risk adjustment, select model predictors are used to assign a risk score to plan members and calculate a Long Term Care Cost Index (LTCCI) for the MLTC plans. The model predictors are selected from the Uniformed Assessment System (UAS) – NY, a comprehensive assessment tool developed by interRAI. A member´s ability to complete activities of daily living such as meal preparation, ambulation, toileting, and dressing are factored in the calculation. Also included are the presence of various diagnoses such as Alzheimer´s, history of stroke, and Parkinson´s disease. Points are assigned to the various factors and serve to weight the formulas for the degree of need of plan members.
|top of section| |top of page|Long–Term Care Quality Measure Summary
Managed Long–Term Care Clinical Advisory Group (CAG)
Quality Measure Recommendations
Introduction
The CAG discussed key factors related to delivering high quality care for MLTC members and reviewed a comprehensive list of quality measures from multiple reputable sources. Recognizing the advantage of selecting measures from those in use for New York State´s ongoing quality improvement programs, including the MLTC Quality Incentive Initiative and Nursing Home Quality Initiative (NHQI), begun in 2014 and 2015, respectively, and overseen by the Office of Quality and Patient Safety, the CAG recommended a subset of these measures.
Many of the MLTC (home/community care) measures considered are derived from the Uniform Assessment System for New York (UAS–NY). The federal Nursing Home Minimum Data Set (MDS) was a primary source for the nursing home measures. The UAS–NY standardizes and automates needs assessment for home and community–based programs, establishing a unique record for all enrollees. UAS records are updated at intervals specified by program or when circumstances change for the member, allowing for patient–level performance comparisons. The MDS 3.0 is part of the federally mandated process for clinical assessment of all residents in Medicare and Medicaid certified nursing homes. It includes comprehensive assessment of each resident´s functional capabilities and helps nursing home staff identify health problems. MDS assessments are required for residents on admission to the nursing facility, periodically, and upon discharge.
The CAG also discussed measures from other sources, including the CMS 5–Star Quality Rating System; Agency for Healthcare Research and Quality (AHRQ) measures; CMS´ Outcome and Assessment Information Set (OASIS); CMS Home Health Quality Reporting Program, and; the National Quality Forum (NQF). The CAG reviewed a large number of measures categorized by topic and used clinical relevance, reliability and validity, and feasibility of collection as the criteria for its recommendations.
In addition, the group discussed the importance of including a range of hospital use measures in MLTC VBP arrangements. A selection of measures is included in the recommendations. The pilot phase will be used to investigate and refine these measures. Avoidable hospital use was identified as a key value opportunity for both community and nursing home residents.
|top of page|Selecting Quality Measures: Criteria used to consider relevance
Standard criteria for measure selection were used for all CAGs. The criteria are presented below along with examples.
Clinical relevance
Focused on key outcomes of integrated care process
- Outcome measures (e.g., postpartum depression) are preferred over process measures (e.g., screening for postpartum depression);
- Outcomes of the total care process are preferred over outcomes of a single component of the care process (e.g., the quality of one type of professional´s care)
For process measures: crucial evidence-based steps in integrated care process that may not be reflected in the patient outcomes measured should be reflected (e.g., focus on postpartum contraceptive care is key but will not be captured in outcomes of current maternity episode).
Existing variability in performance and/or possibility for improvement (e.g., blood pressure measurement during pregnancy is unlikely to be lower than >95% throughout the State).
Reliability and Validity
Measure is well established by reputable organization
By focusing on established measures – those collected by the. NYS Office of Patient Quality and Safety (OQPS), endorsed by the National Quality Forum (NQF), part of the Healthcare Effectiveness Data and Information Set (HEDIS) measures, for example – validity and reliability of measures are assumed acceptable.
Outcome measures are adequately risk–adjusted (e.g., measuring ´% preterm births´ without adequate risk adjustment makes it impossible to compare performance among providers).
Feasibility
Claims–based measures are preferred over non–claims based measures (e.g. clinical data, surveys)
- Ease of data collection data is an important consideration and measures should not place undue burden on providers.
Existing sources are preferable when clinical data or surveys are required (e.g., the vital statistics repository based on birth certificates).
Patient–level data sources are preferable
- Measures that require random samples (e.g. sampling patient records or using surveys) are not ideal because they do not drill down to the patient level and/or allow for adequate risk adjustment, and may add to the data collection burden. An exception is made for measures that are already part of DSRIP/QARR.
Data must be available without significant delay
- In general, measure data sources should not have a longer lag than claims–based measures (about six months). This is an issue with the vital statistics repository, for example, which has a one–year lag for New York City data.
Meaningful and actionable to provider improvement in general
Measures should not only be related to the goals of care but be usable by the provider to improve care.
|top of page|Categorizing and Prioritizing Quality Measures
Based on the above criteria, the CAG discussed the quality measures in the framework of three categories:
- Category 1 – Category 1 comprises approved quality measures that are felt to be clinically relevant, reliable, valid, and feasible.
- Category 2 – Category 2 quality measures were felt to be clinically relevant, valid, and probably reliable, but the feasibility could be problematic. These quality measures will likely be investigated during pilots but will likely not be implementable in the immediate future.
- Category 3 – Category 3 measures were decided to be insufficiently relevant, valid, reliable, and/or feasible.
The use of these measures, particularly in Category 1 and 2, will be developed and further refined during the pilot phase. The CAG will be reconvened in 2017 to further refine the measures.
|top of section| |top of page|Managed Long–Term Care CAG Recommended Quality Measures – Category 1 and 2
| No. | Measure | Measure Steward/Source | MLTC QI3 or NHQI4 | |
|---|---|---|---|---|
| Category 1 | 1 | Percentage of members who did not have an emergency room visit in the last 90 days | UAS–NY | MLTC QI |
| 2 | Percentage of members who did not have falls resulting in medical intervention in the last 90 days | UAS–NY | MLTC QI | |
| 3 | Percentage of members whose pain was controlled | UAS–NY | MLTC QI | |
| 4 | Percentage of members who were not lonely and distressed | UAS–NY | MLTC QI | |
| 5 | Percentage of members who received an influenza vaccination in the last year | UAS–NY | MLTC QI | |
| 6 | Percentage of members who responded that a health plan representative talked to them about appointing someone to make decisions about their health if they are unable to do so | Member Satisfaction Survey | MLTC QI | |
| 7 | Percentage of members who remained stable or demonstrated improvement in pain intensity | UAS–NY | MLTC QI | |
| 8 | Percentage of members who remained stable or demonstrated improvement in Nursing Facility Level of Care (NFLOC) score | UAS–NY | MLTC QI | |
| 9 | Percentage of members who remained stable or demonstrated improvement in urinary continence | UAS–NY | MLTC QI | |
| 10 | Percentage of members who remained stable or demonstrated improvement in shortness of breath | UAS–NY | MLTC QI | |
| 11 | Percent of long stay high risk residents with pressure ulcers | CMS / MDS 3.0/NYS risk–adjusted | NHQI | |
| 12 | Percent of long stay residents who received the pneumococcal vaccine | CMS / MDS 3.0 | NHQI | |
| 13 | Percent of long stay residents who received the seasonal influenza vaccine | CMS / MDS 3.0 | NHQI | |
| 14 | Percent of long stay residents experiencing one or more falls with major injury | CMS / MDS 3.0 | NHQI | |
| 15 | Percent of long stay residents who have depressive symptoms | CMS / MDS 3.0 | NHQI | |
| 16 | Percent of long stay low risk residents who lose control of their bowel or bladder | CMS / MDS 3.0 | NHQI | |
| 17 | Percent of long stay residents who lose too much weight | CMS / MDS 3.0/NYS risk–adjusted | NHQI | |
| 18 | Antipsychotic use in persons with dementia | Pharmacy Quality Alliance (PQA) / MDS 3.0 | NHQI | |
| 19 | Percent of long stay residents who self–report moderate to severe pain | CMS / MDS 3.0/NYS risk–adjusted | NHQI | |
| 20 | Percent of long stay residents whose need for help with daily activities has increased | CMS / MDS 3.0 | NHQI | |
| 21 | Percent of long stay residents with a urinary tract infection | CMS / MDS 3.0 | NHQI | |
| 22 | Percentage of members who responded that they were usually or always involved in making decisions about their plan of care | NYS DOH / Improving Healthcare for the Common Good® (IPRO) | MLTC QI | |
| 23 | Percentage of members who reported that within the last 6 months the home health aide or personal care aide services were always or usually on time | NYS DOH / Improving Healthcare for the Common Good® (IPRO) Member Satisfaction survey | MLTC QI | |
| 24 | Percentage of members who rated the quality of home health aide or personal care aide services within the last 6 months as good or excellent | NYS DOH / Improving Healthcare for the Common Good® (IPRO) Member Satisfaction survey | MLTC QI | |
| 25 | Care for Older Adults (COA) – Medication Review | NCQA | No | |
| 26 | Percentage PAC Costs (upon availability and analytical integration of Medicare data ) | Altarum Institute (Formerly HCI3) | No | |
| Category 2 | 27 | Medication Adherence: Always adherent, 80% or more of the time adherent, Less than 80% of the time adherent | UAS–NY | No |
| 28 | Use of High–Risk Medications in the Elderly | NCQA | No | |
| 29 | CMS five–star quality rating for staffing | CMS | N/A | |
| 30 | Acute Care Hospitalization During the First 60 Days of Home Health | CMS | No | |
| 31 | Acute Care Hospitalization | CMS | No | |
| 32 | Emergency Department Use with Hospitalization | CMS | No | |
| 33 | Proportion of patient with cancer admitted to the ICU in the last 30 days of life | American Society of Clinical Oncology | No | |
| 34 | Inpatient and ICU Days per Decedent During the Last Six Months of Life, by Gender and Level of Care Intensity | Dartmouth Atlas of Health Care / CMS | No | |
| 35 | Total Medicare Spend in last year / 6 months of life | Dartmouth Atlas of Health Care / CMS | No | |
| 36 | Proportion with more than one emergency room visit in the last days of life | American Society of Clinical Oncology | No | |
| 37 | Hospital–Wide All–Cause Unplanned Readmission Measure | CMS | No |
CAG Categorization and Discussion of Measures – Category 1 & 2
| Topic | # | Quality Measure (* = NQF Endorsed) | Type of Measure | Measure Steward/ Source | Data Required | Quality Measure Categorization & Notes | ||
|---|---|---|---|---|---|---|---|---|
| Medicaid Claims Data | Clinical Data | Category | Notes | |||||
| MLTC Quality Incentive–Quality Measures | 1 | Percentage of members who did not have an emergency room visit in the last 90 days | Outcome | UAS–NY | No | Yes | 1 | This measure scores high on all criteria |
| 2 | Percentage of members who did not have falls resulting in medical intervention in the last 90 days | Outcome | UAS–NY | No | Yes | 1 | This measure scores high on all criteria | |
| 3 | Percentage of members whose pain was controlled | Outcome | UAS–NY | No | Yes | 1 | This measure scores high on all criteria | |
| 4 | Percentage of members who were not lonely and distressed | Outcome | UAS–NY | No | Yes | 1 | This measure scores high on all criteria | |
| 5 | Percentage of members who received an influenza vaccination in the last year | Outcome | UAS–NY | No | Yes | 1 | This measure scores high on all criteria | |
| 6 | Percentage of members who responded that a health plan representative talked to them about appointing someone to make decisions about their health if they are unable to do so | Outcome | UAS–NY | No | Yes | 1 | The CAG commented that although the focus should be at the member level, this measure ensures alignment of appropriate decision making. | |
| 7 | Percentage of members who remained stable or demonstrated improvement in pain intensity | Outcome | UAS–NY | No | Yes | 1 | This measure scores high on all criteria. | |
| 8 | Percentage of members who remained stable or demonstrated improvement in Nursing Facility Level of Care (NFLOC) score | Outcome | UAS–NY | No | Yes | 1 | This measure scores high on all criteria. The CAG noted that improvement in NFLOC score could translate into reduced hospitalizations. | |
| 9 | Percentage of members who remained stable or demonstrated improvement in urinary continence | Outcome | UAS–NY | No | Yes | 1 | The CAG commented that in home care where a family member has responsibility of caring for the member, loss of urinary continence has been a main reason for transitioning to a nursing home. This measure scores high on all criteria. |
|
| 10 | Percentage of members who remained stable or demonstrated improvement in shortness of breath | Outcome | UAS–NY | No | Yes | 1 | This measure scores high on all criteria. | |
| Nursing Home Quality Initiative– | 11 | Percent of long stay high risk residents with pressure ulcers* | Outcome | CMS / MDC 3.0 | No | Yes | 1 | This measure scores high on all criteria. |
| 12 | Percent of long stay residents who received the pneumococcal vaccine* | Outcome | CMS / MDC 3.0 | No | Yes | 1 | This measure scores high on all criteria. | |
| 13 | Percent of long stay residents who received the seasonal influenza vaccine* | Outcome | CMS / MDC 3.0 | No | Yes | 1 | This measure scores high on all criteria. | |
| 14 | Percent of long stay residents experiencing one or more falls with major injury* | Outcome | CMS / MDC 3.0 | No | Yes | 1 | The CAG noted that there is a large spend associated with falls. This measure scores high on all criteria. |
|
| 15 | Percent of long stay residents who have depressive symptoms | Outcome | CMS / MDS 3.0 | No | Yes | 1 | This measure scores high on all criteria. | |
| 16 | Percent of long stay low risk residents who lose control of their bowel or bladder | Outcome | CMS / MDS 3.0 | No | Yes | 1 | This measure scores high on all criteria. | |
| 17 | Percent of long stay residents who lose too much weight* | Outcome | CMS / MDS 3.0 | No | Yes | 1 | This measure scores high on all criteria. | |
| 18 | Antipsychotic use in persons with dementia* | Outcome | Pharmacy Quality Alliance (PQA) / MDS 3.0 | No | Yes | 1 | This measure scores high on all criteria. | |
| 19 | Percent of long stay residents who self-report moderate to severe pain* | Outcome | CMS / MDS 3.0 | No | Yes | 1 | This measure scores high on all criteria. | |
| 20 | Percent of long stay residents whose need for help with daily activities has increased* | Outcome | CMS / MDS 3.0 | No | Yes | 1 | The CAG noted that increased ADL’s could result in reduction of other services (costs). This measure scores high on all criteria. |
|
| 21 | Percentage of members who responded that they were usually or always involved in making decisions about their plan of care | Outcome | CMS / MDS 3.0 | No | Yes | 1 | This measure scores high on all criteria. | |
| MLTC Quality Incentive | 22 | Percentage of members who responded that they were usually or always involved in making decisions about their plan of care | Survey | NYS DOH / Improving Healthcare for the Common Good® (IPRO) | No | Yes | 1 | This measure scores high on all criteria. Survey Data |
| 23 | Percentage of members who reported that within the last 6 months the home health aide or personal care aide services were always or usually on time | Survey | NYS DOH / Improving Healthcare for the Common Good® (IPRO) | No | Yes | 1 | This measure scores high on all criteria. Survey Data |
|
| 24 | Percentage of members who rated the quality of home health aide or personal care aide services within the last 6 months as good or excellent | Survey | NYS DOH / Improving Healthcare for the Common Good® (IPRO) | No | Yes | 1 | This measure scores high on all criteria. Survey Data |
|
| Medication Measures | 25 | Care for Older Adults (COA) – Medication Review* | Process | NCQA | Yes | Yes | 1 | The CAG determined a medication measure was needed given the high number of members on medications. This measure scores high on all criteria. |
| 26 | Medication Adherence: Always adherent, 80% or more of the time adherent, Less than 80% of the time adherent | Process | UAS–NY | No | Yes | 2 | As noted in the 4th CAG meeting, Medication Adherence from the UAS is being added as a category 2. OQPS reviewed the #’s: 74% for ‘always adherent’ 98.5% for ‘80% or more of the time adherent’ |
|
| 27 | Use of High-Risk Medications in the Elderly* | Process | NCQA | Yes | Yes | 2 | The CAG noted that this measure could lead to unintended consequences where a high-risk medication might not be used when needed. Also noted is there are opportunities to use other medications not classified as ‘high-risk’. |
|
| Nursing Home Quality Rating | 28 | CMS five-star quality rating for staffing | Process | CMS | No | Yes | 2 | The Staffing Domain rating is based on 2 measures:
|
| Hospitalization / Emergency Department | 29 | Acute Care Hospitalization During the First 60 Days of Home Health* | Outcome | CMS | Yes | No | 2 | Hospitalization (ER, associated spends, readmissions, etc.) have been included as a category 2 for purposes of further investigation could be done during pilots. |
| 30 | Acute Care Hospitalization* | Outcome | CMS | Yes | No | 2 | Hospitalization (ER, associated spends, readmissions, etc.) have been included as a category 2 for purposes of further investigation could be done during pilots. | |
| 31 | Emergency Department Use with Hospitalization | Outcome | CMS | No | Yes | 2 | Hospitalization (ER, associated spends, readmissions, etc.) have been included as a category 2 for purposes of further investigation could be done during pilots. | |
| 32 | Proportion admitted to the ICU in the last 30 days of life* | Process | American Society of Clinical Oncology | Yes | Yes | 2 | Hospitalization (ER, associated spends, readmissions, etc.) have been included as a category 2 for purposes of further investigation could be done during pilots. | |
| 33 | Inpatient Days per Decedent During the Last Six Months of Life, by Gender and Level of Care Intensity | Outcome | Dartmouth Atlas of Health Care / CMS | Yes | Yes | 2 | Hospitalization (ER, associated spends, readmissions, etc.) have been included as a category 2 for purposes of further investigation could be done during pilots. | |
| 34 | Total Medicare Spend in last year / 6 months of life | Outcome | Dartmouth Atlas of Health Care / CMS | Yes | Yes | 2 | Hospitalization (ER, associated spends, readmissions, etc.) have been included as a category 2 for purposes of further investigation could be done during pilots. | |
| 35 | Proportion with more than one emergency room visit in the last days of life* | Process | American Society of Clinical Oncology | Yes | Yes | 2 | Hospitalization (ER, associated spends, readmissions, etc.) have been included as a category 2 for purposes of further investigation could be done during pilots. | |
| 36 | Hospital-Wide All-Cause Unplanned Readmission Measure* | Outcome | CMS | Yes | No | 2 | Hospitalization (ER, associated spends, readmissions, etc.) have been included as a category 2 for purposes of further investigation could be done during pilots. The CAG specifically recommended an all-cause readmission measure. | |
CAG Categorization and Discussion of Measures – Category 3
| Topic | # | Quality Measure (* = NQF Endorsed) | Type of Measure | Measure Steward/ Source | Data Required | Quality Measure Categorization & Notes | ||
|---|---|---|---|---|---|---|---|---|
| Medicaid Claims Data | Clinical Data | Category | Notes | |||||
| MLTC Quality Incentive–Satisfaction Measures | 37 | Percentage of members who rated their managed long-term care plan as good or excellent | Survey | NYS DOH / Improving Healthcare for the Common Good® (IPRO) | No | Yes | 3 | The CAG determined that Plan level measures should be category 3 as they are not member focused. |
| 38 | Percentage of members who rated the helpfulness of the plan in assisting them and their family to manage their illnesses as good or excellent | Survey | NYS DOH / Improving Healthcare for the Common Good® (IPRO) | No | Yes | 3 | The CAG determined that Plan level measures should be category 3 as they are not member focused. | |
| 39 | Percentage of members who rated the quality of care manager or case manager services within the last six months as good or excellent | Survey | NYS DOH / Improving Healthcare for the Common Good® (IPRO) | No | Yes | 3 | The CAG determined that Plan level measures should be category 3 as they are not member focused. | |
| MLTC & NH QI Efficiency Measure | 40 | MLTC/NH QI Efficiency Measure - Potentially Avoidable Hospitalization (PAH): hospitalizations identified as potentially avoidable if the primary diagnosis is any one of the following conditions: heart failure, respiratory infection, electrolyte imbalance, sepsis, anemia, or urinary tract infection. | Outcome | CMS/NYS DOH | Yes | No | 3 | The CAG has recommended an ‘All Cause Hospitalization’ measure over the PAH from the MLTC Quality Incentive. CMS potentially expanding to 19 conditions however it has not been confirmed nor has a timetable been established. |
| Compliance Measures | 41 | Percent of contract/agency staff used | Process | NYS DOH | No | Yes | 3 | The CAG determined that staff level measures should be category 3 as they are not member focused. |
| 42 | Percent of employees vaccinated for influenza | Process | NYS DOH | No | Yes | 3 | The CAG determined that staff level measures should be category 3 as they are not member focused. | |
| 43 | CMS Five-Star Quality Rating for Health Inspections (regionally adjusted) | Process | CMS | No | Yes | 3 | The CAG determined that facility level measures should be category 3 as they are not member focused. Poor facility ratings would likely show up in member level measurement. | |
| 44 | Timely submission of employee influenza vaccination data | Process | NYDOH | No | Yes | 3 | The CAG determined that facility level measures should be category 3 as they are not member focused. | |
| 45 | Timely submission of certified and complete nursing home cost reports | Process | NYS DOH | No | Yes | 3 | The CAG determined that facility level measures should be category 3 as they are not member focused. | |
| Medication Measures | 46 | Drug Education on all Medications Provided to Patient/Caregiver | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. |
| 47 | Medication Administration | Process | OQPS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 48 | Drug Education on High Risk Medications Provided To Patient/Caregiver at Start of Episode | Process | CMS | No | Yes | 3 | The CAG selected a separate high-risk medication measure. | |
| 49 | Improvement in Management of Oral Medications* | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 50 | Stabilization in Management of Oral Medications | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3.The CAG determined this measure should be category 3. | |
| 51 | Substantial Decline in Management of Oral Medications | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 52 | Emergent Care for Improper Medication Administration or Medication Side Effects | Outcome | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 53 | Medication Reconciliation Post-Discharge (MRP)* | Process | NCQA | Yes | Yes | 3 | The CAG determined this measure should be category 3. | |
| 54 | Adherence to Chronic Medications* | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 55 | Annual Monitoring for Patients on Persistent Medications (MPM)* | Process | NCQA | Yes | Yes | 3 | The CAG determined this measure should be category 3. | |
| 56 | Potential Medication Issues Identified And Timely Physician Contact at Start of Episode | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 57 | Potential Medication Issues Identified And Timely Physician Contact | Process | CMS | Yes | Yes | 3 | The CAG determined this measure should be category 3. | |
| Weight Measurement | 58 | Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow-Up* | Process | CMS | Yes | Yes | 3 | The CAG determined this measure should be category 3. |
| CMS 5 Star | 59 | Percent of residents whose need for help with activities of daily living has increased* | Outcome | CMS | No | Yes | 3 | Duplicative measure |
| 60 | Percent of high risk residents with pressure ulcers (sores)* | Outcome | CMS | No | Yes | 3 | Duplicative measure | |
| 61 | Percent of residents who have/had a catheter inserted and left in their bladder* | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 62 | Percent of residents who were physically restrained* | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 63 | Percent of residents with a urinary tract infection* | Outcome | CMS | No | Yes | 3 | Duplicative measure | |
| 64 | Percent of residents who self-report moderate to severe pain (Long Stay)* | Outcome | CMS | No | Yes | 3 | Duplicative measure | |
| 65 | Percent of residents who received an antipsychotic medication | Process | CMS | No | Yes | 3 | Duplicative measure | |
| 66 | Percent of residents with pressure ulcers (sores) that are new or worsened* | Outcome | CMS | No | Yes | 3 | Duplicative measure | |
| 67 | Percent of residents who self-report moderate to severe pain (Short Stay)* | Outcome | CMS | No | Yes | 3 | The CAG determined that a similar long stay measure would allow for more flexibility in improvement. | |
| 68 | Percent of residents who newly received an antipsychotic medication | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 69 | Percentage of short-stay residents who were successfully discharged to the community | Outcome | CMS | Yes | No | 3 | The CAG determined this measure should be category 3. | |
| 70 | Percentage of short-stay residents who have had an outpatient emergency department visit | Outcome | CMS | Yes | No | 3 | The CAG determined this measure should be category 3. | |
| 71 | Percentage of short-stay residents who were re-hospitalized after a nursing home admission | Outcome | CMS | Yes | No | 3 | The CAG determined this measure should be category 3. | |
| 72 | Percentage of short-stay residents who made improvements in function | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
| 73 | Percentage of long-stay residents whose ability to move independently worsened | Process | CMS | No | Yes | =3 | The CAG determined this measure should be category 3. | |
| 74 | Percentage of long-stay residents who received an antianxiety or hypnotic medication | Process | CMS | No | Yes | 3 | The CAG determined this measure should be category 3. | |
Attachment A: Glossary
- Delivery System Reform Incentive Payments (DSRIP): A five–year program that reinvests up to $6.42B in Medicaid savings in groups of NYS healthcare organizations to reduce hospitalizations, reduce emergency room visits, and improve outcomes. The goal of DSRIP is to move provider Medicaid payments from Fee–for–Service ("FFS") to Value–Based Payments ("VBP").
- Fee for Service (FFS): The prevailing payment model where physicians and other state agency licensed/certified providers are paid for each service rendered. Proven to incentivize volume over value.
- Medicaid Redesign Team (MRT): Medicaid Redesign Team (MRT) is a State team organized by Governor Cuomo to find savings in the long–term. The MRT estimates to generate $17.1 B in federal Medicaid savings over a period of five years, which enabled the State to obtain an 1115 Waiver to reinvest half into delivery system reform programs.
- Value Based Payment (VBP): VBP is a sophisticated payment mechanism design to incentivize physicians to provide more value and better outcomes while reducing costs.
- VBP Roadmap: To ensure the long–term sustainability of the improvements made possible by the DSRIP investments in the waiver, the Terms and Conditions (T&Cs) (§ 39) require the State to submit a multiyear Roadmap for comprehensive Medicaid payment reform including how the State will amend its contracts with Managed Care Organizations (MCOs).
Appendix B:
Meeting Schedule
| Date | Agenda | |
|---|---|---|
| CAG #1 | 11/12/2015 |
|
| CAG #2 | 12/18/2015 |
|
| CAG #3 | 02/09/2016 |
|
| CAG #4 | 04/18/2016 |
|
______________________________________________________
1. https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/docs/vbp_roadmap_final.pdf. 1
2. Total cost of care subpopulation arrangements for the I/DD population will not be contracted until specialty services for those members have transitioned to managed care. 2
3. New York State Department of Health Managed Long-Term Care Quality Incentive (MLTC QI) 3
4. New York State Department of Health Nursing Home Quality Initiative (NHQI) 4
Follow Us