Value-Based Payment for Children
- Report is also available in Portable Document Format (PDF)
Report to the NYS Medicaid VBP Workgroup
Children´s Health Subcommittee and Clinical Advisory Group
September 2017 NYS Medicaid Value–Based Payment
Contents
Section 2: Introduction/Context
- Broad goals
The VBP Roadmap
Section 3: The Children´s Health VBP Subcommittee and Clinical Advisory Group
- Charge
Membership and process
Section 4: Overview of Children and Adolescents in New York Medicaid Under the VBP Roadmap
- Background: cost and utilization
Assessing payment models
Section 5: Guiding Principles for Value–Based Payment for Children and Adolescent Health Services
- Principles
Value statement
Section 6: "North Star" Framework
- Linking goals to appropriate measures and care strategies
- Recommendation Process
VBP Principles and Payment Model Recommendations
Recommendation P1: Guiding Framework for Payment Model
Recommendation P2: Pediatric Primary Care Capitation (PPCC)
Recommendation P2.1: Defining the PPCC Population.
Recommendation P2.2: Defining PPCC Costs and Services
Recommendation P2.3: PPCC Disbursement and Withholds
Recommendation P2.4: PPCC Pilot Testing
Recommendation P3: Pediatric Methodology in TCGP and IPC
- VBP Quality Measure Recommendations
- Recommendation M1: Guiding Framework for Measurement
Recommendation M2: Integration with Existing Measures
Recommendation M3: Integration with Maternity Care Episode–Based Arrangement
Recommendation M4: Tracking Progress
Recommendation M5: Developmental Screening
- Recommendation M1: Guiding Framework for Measurement
- Additional Work Recommendations
- Recommendation A1: Focus on Children with Complex Health Needs
Recommendation A2: Iterative Review Process
Recommendation A3: Additional Pilot Testing
- Recommendation A1: Focus on Children with Complex Health Needs
Section 8: Quality Measure Sets
- Principles and criteria
Selection process
Universal Child Measures- Rationale for new vs. existing measures
Universal Child Quality Measure Set (Category 1)
Universal Child Quality Measure Set (Category 2)
- Rationale for new vs. existing measures
- Maternity Measures
- Maternity Measure Set
- Future Measures for Child and Adolescent Health
Section 1: Executive Summary
The New York Medicaid program aims to shift its payment system from a predominantly fee–for–service system to a value–based payment (VBP) system by 2020. This effort is part of a broader national movement to reform health care payment, which is predicated on the belief that changing the way managed care organizations pay providers for health care services should result in improved quality, health care efficiency, and health of vulnerable populations.
The transition is guided by several workgroups and committees that provide the New York Medicaid program with clinical guidance or high–level recommendations on how to implement value–based payment for certain populations (e.g., behavioral health) or with attention to particular issues (e.g., social determinants of health and community–based organizations). In fall 2016, the State established a Children´s Health VBP Subcommittee and Clinical Advisory Group (hereafter "committee") to bring a uniquely child–focused perspective to payment reform.
The committee–including approximately 75 members representing a wide range of primary care and specialty provider organizations, managed care plans, children´s advocacy groups, child welfare organizations, public health agencies, and the NYS Department of Health, Office of Mental Health, Office of Alcoholism and Substance Abuse Services, and Education Department–met seven times between October 20, 2016 and July 10, 2017. The committee developed three products for the State´s consideration over that period:
- A conceptual framework intended to guide the State´s future deliberations about value–based payment for children;
- a set of draft recommendations pertaining to a child–specific VBP model, measures, and future work focused on children with complex needs; and
- a specific set of measures which could be applied to VBP arrangements for children in 2018.
A subset of committee members also began discussions about the appropriateness and design of value– based payment arrangements for children with complex physical and behavioral health needs.
Overview of Children and Adolescents in New York Medicaid Under the VBP Roadmap
In New York´s Medicaid program, 2,037,175 children between the ages of 0 and 20 were enrolled in a mainstream managed care plan (as opposed to a specialty plan) in December 2016. The committee reviewed expenditures and service utilization for this population, and found that:
- Children are generally a low–cost population in comparison to adults; the average expenditure for a child was $4,253 in 2014.
- For 90 percent of the children´s population, the average expenditure is much lower–averaging $2,400 in 2014.
- The remaining 10 percent of the children´s population is much higher–cost and has a heterogeneous set of conditions driving those expenditures, including behavioral health needs, developmental disabilities, and complex chronic conditions.
- Utilization varies by age and race. Children generally have higher inpatient and emergency department utilization in the earliest years of life (age 0–9), and black and Hispanic children have much higher inpatient and emergency department utilization rates than white and Asian or Pacific Islander children.
- Primary care utilization is relatively high for all children; about 85 percent of children receive at least one visit each year.
The committee also reviewed the core value–based payment arrangements already designed for use in New York´s Medicaid program and discussed their possible implications for children in Medicaid. The State´s transition to value–based payment is guided by a document known as the New York State Value– Based Payment Roadmap, which is annually revised and approved by the Centers for Medicare and Medicaid Services. The document identifies four value–based payment models that are considered core to New York´s efforts: Total Care for the General Population (TCGP); Integrated Primary Care (IPC), which includes 14 chronic condition episodes; Maternity Care, an episodic bundle that extends from prenatal care to 60 days post–discharge care for mothers and includes 30 days of post–discharge care for newborns; and Total Care for Special Needs Subpopulations.
Guiding Principles, Value Statement, and "North Star" Framework
The committee concluded that while children will inevitably be included in four of these arrangement types, and that each could offer some benefit to children by encouraging more efficient and higher quality care, none was well suited for promoting the committee´s value statement for children:
"Focusing on the healthy growth and development of children will improve their quality of life. Children require a value–based payment approach that acknowledges the specific needs attendant to each developmental stage and the unique opportunity to improve health and life trajectories, as well as the near–term improvements that are possible from direct health interventions. Support and recognition of families and caregivers are central to improving children´s lives."
This value statement was developed out of eleven principles that are presented on page 14.
The committee identified a dissonance between existing VBP arrangements and the notion of payment models that could be optimal for children: traditional metrics for evaluating the success of value–based payment arrangements–namely, the achievement of cost savings or improvement on clinical quality measures–have shortcomings in the child health context. In aggregate, potential cost savings in children´s health pale in comparison to those from adult health care services, and high expenditure is not widely considered to be the paramount challenge for children´s health services. Existing quality measures, while critical for driving improvement in clinical care, are primarily process–oriented and insufficient for measuring whether the health care system is optimally promoting health and development.
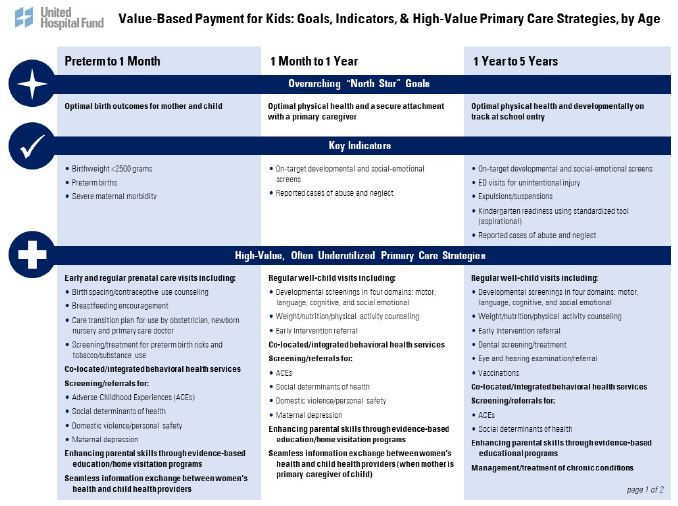
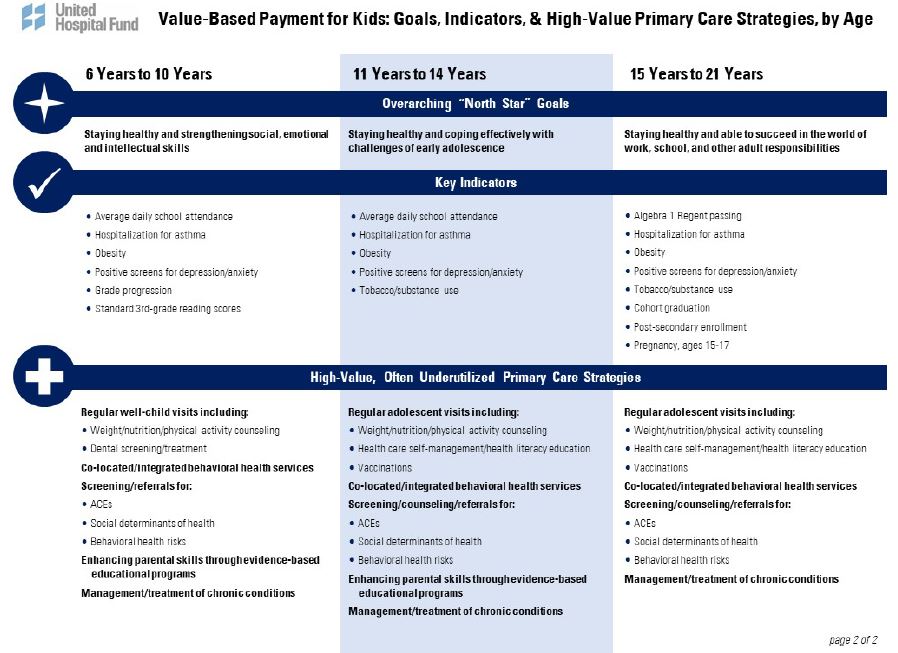
Agreeing that new goals would be needed to guide decisions around value–based payment for children and adolescents, the committee developed a "North Star" Framework presented on pages 17–18 of this report. The framework is divided by developmental stages and contains three elements:
- Overarching "North Star" Goals: a common language goal statement of what the health care system is collectively trying to achieve for every child.
- Key Indicators: potential indicators for assessing whether progress is being made toward "North Star" goals. Many of these indicators are cross–sector.
- High–Value, Often Underutilized Primary Care Strategies: a non–exhaustive list of potential primary care strategies the Medicaid system, through VBP, could encourage in furtherance of those indicators and the underlying "North Star" goals.
Recommendations
Following these deliberations, the committee turned to developing recommendations in three areas: VBP Principles and Payment Model; Quality Measures; and Additional Work/Deliberation. The full text of the report provides important contextual details for these recommendations on the pages noted.
VBP Principles and Payment Model (pages 20–22)
Building on foundational work done by the consulting group Bailit Health prior to the committee´s creation, the committee proposes the State use the "North Star" Framework as a guide to create an additional, voluntary VBP arrangement for the Roadmap focused on generating health improvements for the 90 percent of children that are considered "low–cost" in Medicaid. This newly proposed Pediatric Primary Care Capitation (PPCC) VBP arrangement would be risk–adjusted and include enhancements to cover care coordination, additional screenings, and efforts associated with addressing the social determinants of health. An additional enhancement should be provided for practices with co–located or integrated behavioral health services. A portion of the prospective capitation payment would be withheld and paid based on improvement and high performance on the child–specific measures described in this report. The committee also developed recommendations on how the potential benefits of the newly proposed option could be extended to child populations served under the existing VBP models.
Quality Measures (pages 23–24)
The committee reviewed the state of child health measurement in New York´s existing VBP arrangements and made recommendations for how child and adolescent quality measures can be improved in the TCGP, IPC, and Maternity Care arrangement measure sets. Again, the committee recommends the State be guided by the North Star Framework as it implements VBP measures for children. The measure recommendations suggest that the same metrics apply for all children, regardless of the underlying VBP arrangement, creating a Universal Child Measure Set applicable to TCGP, IPC, and PPCC arrangements. To address known disparities in children´s health, all measures in this universal set should be reported with relevant race/ethnicity data to the fullest extent possible. The committee also recommends an additional measure for consideration in the Maternity Care set–and that this new measure and four current maternity measures be added to the TCGP set because of their relevance to child health. Finally, the committee felt very strongly that the State should quickly complete the investigations necessary to make developmental screening a Category 1 (to be reported by VBP contractors) measure as soon as possible.
Additional Work/Deliberation (pages 26–27)
Committee members also recommended that the New York Medicaid program support further deliberative work in a few areas, especially in analyzing the appropriateness and potential opportunities of value– based payment for vulnerable subpopulations of children and adolescents. This will require ongoing work by this committee or a similar group with a focus on defining these subpopulations and assessing whether there are VBP models that can work for such small and heterogeneous population subsets. The committee also recommends a process by which child–specific measures and the North Star Framework can be continually updated and adjusted over time. Understanding the need to promote ongoing innovation, the committee also suggests additional pilots and pediatric delivery system transformation efforts towards the longer–term goal of cross–system accountability for broader child well–being.
Quality Measure Sets
The final task of the committee was to select child–focused quality measures for inclusion in VBP arrangements beginning in 2018. Development of the committee´s performance measure sets was shaped by four criteria:
- The measure is relevant to one of the strategies identified to achieve a particular "North Star" goal.
- The measure is evidence–based (i.e., has been tested for validity and reliability, and, preferably, is endorsed for use by the National Quality Forum).
- The measure should be feasible for providers to use and report with minimal additional burden (i.e., does not require expensive medical records review or sophisticated health information technology capacity).
- The final recommended measure set should be parsimonious, with outcome measures having priority.
Consistent with the broad measure recommendations, the committee developed a Universal Child Measure Set that would be applicable to any TCGP, IPC, or PPCC VBP arrangement. This set totals 20 measures, 13 of which are recommended as Category 1 (to be reported by VBP contractors), and 7 of which are recommended for voluntary use (usually because it was not considered feasible to require the measure for all providers engaged in VBP). The set is provided on pages 29–34.
Although the committee´s charge was to focus on child and adolescent health care, there was broad agreement that maternity care is central to children´s health. It therefore reviewed the set of VBP maternity measures for overlap with its own proposed list as well as for any perceived gaps. The group recommended five maternity measures that it felt should be applicable to TCGP as well as to the Maternity Care arrangement. Only one of these measures–behavioral risk assessment for pregnant women–is not already in the Maternity Care set, and the committee requests that the Maternity Clinical Advisory Group review this measure for adoption. A full description of the maternity measures is on pages 35–36.
Finally, the committee identified several areas where the Universal Child Measure Set would ideally be broadened to support achieving the "North Star" goals. Paramount in this discussion was the need to prioritize the development of key indicators and outcome measures that reflect improvements in a child´s developmental trajectory and social–emotional growth. The creation of such measures would represent an important shift from focusing on processes, including the use of specific screening tools and interventions, to focusing on the results of a wide range of services that can be delivered in primary care. A list of future measurement areas for New York State to work on developing is included on page 37.
|top of section| |top of page|Section 2: Introduction/Context
Broad goals
The New York State (NYS) Delivery System Reform Incentive Payment (DSRIP) program aims to fundamentally restructure New York State´s health care delivery system by improving health outcomes for Medicaid members, reducing avoidable hospital use by 25 percent, and improving the financial sustainability of New York State´s safety net.
To further stimulate and sustain this delivery reform, at least 80 to 90 percent of all payments made from managed care organizations to providers will be captured within value–based payment (VBP) arrangements by 2020. The goal of converting to VBP arrangements is to develop a sustainable system that incentivizes value over volume; the current fee–for–service payment system is believed to unduly incentivize a high volume of health care services, even if they are unnecessary. The Centers for Medicare & Medicaid Services (CMS) has approved the State´s multiyear "VBP Roadmap," which details the menu of options and different levels of VBP that managed care organizations and providers can select, and also outlines how the State determines quality measures for VBP arrangements.
The VBP Roadmap
The NYS VBP Roadmap1outlines four core types of VBP arrangements (also known as "on–menu" options):
| Category of Arrangement | Type of Arrangement |
|---|---|
| Population–based arrangement |
|
| Episode–based arrangement |
|
Adapted from Introduction to Value Based Payment (VBP) Arrangements.
In addition to flexibility regarding the type of VBP arrangement, the New York State VBP Roadmap also creates a continuum of increasing levels of value–based payment based on the amount of risk that a provider is willing to accept in a VBP contract with a plan.
Value–Based Payment Methodologies
| Level 0 VBP | Level 1 VBP | Level 2 VBP | Level 3 VBP |
|---|---|---|---|
| FFS with bonus and/or withhold based on quality scores (including PMPM subsidy for integrated primary care) | FFS with upside–only shared savings available when outcome scores are sufficient (FFS may be complemented with PMPM subsidy for integrated primary care) | FFS with risk sharing (upside available when outcome scores are sufficient; downside is reduced or eliminated when quality scores are high) | Capitated payment or bundle (with quality–based component) |
Source: New York State Department of Health. March 2016. A Path Toward Value–Based Payment: Annual Update. Page 18.
In Fall 2016 the NY Medicaid VBP Workgroup established the Children´s Health VBP Subcommittee and Clinical Advisory Group to ensure that value–based payment also transforms the delivery of health care for children.
|top of section| |top of page|Section 3: The Children´s Health VBP Subcommittee and Clinical Advisory Group
Charge
The NY Medicaid VBP Workgroup charged the Children´s Health VBP Subcommittee and Clinical Advisory Group (hereafter "committee") with:
- Reviewing the composition of the child and adolescent population within Medicaid and assessing the relative fit for VBP arrangements;
- Identifying quality measures for potential children´s VBP arrangements;
- Identifying child–specific measures and assessing them for inclusion within existing arrangements; and
- Recommending any necessary policy changes to ensure that the needs of children and adolescents are addressed in a VBP environment.
Membership and process
The committee was co–chaired by Dr. Jeanne Alicandro2, former Medical Director for Managed Care at IPRO; Kate Breslin, President & CEO of the Schuyler Center for Analysis and Advocacy; and Dr. Jeffrey Kaczorowski3, Professor of Pediatrics and Vice Chair for Government and Community Relations at Golisano Children´s Hospital at the University of Rochester School of Medicine and Dentistry, and Senior Advisor to The Children´s Agenda. Consulting firm KPMG staffed the committee from October 2016 to December 2016, followed by the nonprofit United Hospital Fund from January 2017 to the present.
Committee deliberations benefited from robust participation by its members. There were approximately 75 members of the committee, including representatives from a wide range of primary care and specialty provider organizations, managed care plans, children´s advocacy groups, child welfare organizations, and public health agencies, as well as from the New York State Department of Health (NYSDOH), Office of Mental Health, Office of Alcoholism and Substance Abuse Services, and Education Department. Each meeting was attended by approximately 40 members, on average. Committee members also provided extensive written feedback on draft materials between meetings.
The committee met seven times between October 20, 2016, and July 10, 2017. At the committee´s first meeting, following presentations on the broader movement toward VBP in New York´s Medicaid program and on children´s health care utilization and spending, the group coalesced around a set of key principles and a value statement that would guide its work (see Section 5, page 15).
At subsequent meetings in November and December 2016 there was significant discussion of the current state of quality measures for children, and of potential VBP models that could be responsive to children´s unique needs. Following a presentation about NYSDOH´s participation in an Albany Promise pilot on developmental screenings, the December meeting culminated in a group brainstorm session outlining ideal "North Star" goals at each developmental stage and cross–sector indicators linked to achievement of those goals. The committee then considered potential primary care strategies that the Medicaid system, through VBP, could encourage in furtherance of those indicators and the underlying "North Star" goals. This framework was refined over the following months.
Following a winter of work by the co–chairs, NYSDOH, and the United Hospital Fund, the committee reconvened in May 2017 to consider: 1) a framework outlining the "North Star" goals, indicators, and primary care strategies; 2) a set of draft recommendations pertaining to a child–specific VBP model, measures, and future work focused on complex children; and 3) a specific set of measures that could be applied to VBP arrangements for children in 2018.
Through two June webinars and a final in–person meeting in July 2017 the committee achieved unanimous consensus on the framework, recommendations, and measures that are included in this report for the VBP Workgroup´s consideration.4
In parallel to the committee´s formal meetings, a subset of committee members also began meeting to discuss the important issue of how to address the needs of children living in families with complex behavioral health needs as part of VBP arrangements. While the committee elected to initially focus on the "general" pediatric population for reasons described in Section 7 of this report, committee members who desired to work on VBP for children in complex families were encouraged to do so. This small group made significant progress in developing a vision and model for improving the quality of care and outcomes, and generating system savings, for children and caregivers by treating the entire family as the client in a single episode of care. The work of those committee members is ongoing and, as discussed in the recommendations section, warrants additional support. Additional work is also needed to consider the fit and appropriateness of VBP for other children with different complex health needs, including medically fragile children and children with intellectual and developmental disabilities.
|top of section| |top of page|Section 4: Overview of Children and Adolescents in New York Medicaid Under the VBP Roadmap
Background: cost and utilization
In New York´s Medicaid program, 2,037,175 children between the ages of 0 and 20 were enrolled in a mainstream managed care plan (as opposed to a specialty plan) in December 2016. This group of children was the focus of the committee´s deliberations, given the State´s goal of having 80 to 90 percent of managed care payments being value–based by 2020. The committee´s decisions on recommendations and measures in this report were informed by a broad understanding of the following top–line summaries of spending and utilization for children in New York Medicaid.5
- Children are generally a low–cost population, compared to adults.
- The average expenditure for a continuously enrolled child (a child enrolled in the program for a full year) in 2014 was $4,253.
- Adults continuously enrolled in the program in that year had average expenditures of $11,154.
- Within the child population, most children have expenditures well below the $4,253 average.
- The average expenditure for 90 percent of the population was $2,400.
- The remaining 10 percent of child enrollees accounted for a full 50% of total Medicaid expenditures for children in 2014.
- The high–cost child population (the top 10%) is heterogeneous in terms of the conditions driving those expenditures.
- Behavioral health needs, developmental disabilities, and complex chronic conditions drive a large portion of the health care utilization for this high–need population.
- Children with these conditions have much higher rates of inpatient and emergency department utilization than other continuously enrolled children.
- Utilization also varies by age and race.
- The age distribution of the child population is as follows:
Age Bracket Percent of Child Population Within Medicaid Program Under age 1 6% 1–4 22% 5–9 26% 10–13 18% 14–17 17% 18–20 11% - Age affects utilization: children generally have higher inpatient and emergency department utilization in their early years (0–4). Utilization then declines through age 13, then increases slightly from age 14 and older, mostly due to behavioral health conditions.
- Primary care utilization is relatively high for all children: about 85 percent of children receive at least one visit each year. The percentage of children with at least one visit begins to decline after age 4; only 70 percent of 18 to 20 year–olds had at least one primary care visit in 2014.
- The age distribution of the child population is as follows:
- Utilization also varies by race.
- Black and Hispanic children have much higher inpatient and emergency department utilization rates than white and Asian or Pacific Islander children:
Emergency Department and Inpatient Visit Rates by Race/Ethnicity for Children Ages 0–20 Continuously Enrolled (CE) in New York Medicaid in 2014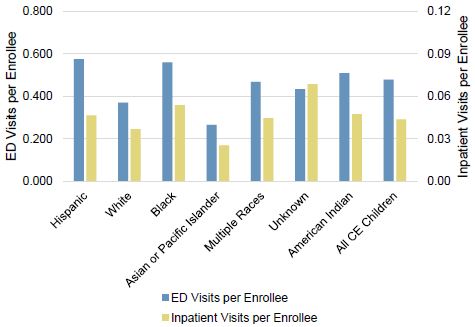
- Differences in primary care utilization are much smaller: black children have a slightly lower percentage of at least one primary care visit compared to all other races.
- Black and Hispanic children have much higher inpatient and emergency department utilization rates than white and Asian or Pacific Islander children:
Assessing payment models
Before considering a VBP model specifically for children, the committee also assessed how current VBP Roadmap arrangements apply to children, and the alignment of the incentives within those arrangements with the guiding principles and "North Star" framework presented in Sections 5 and 6 below.
Total Care for the General Population (TCGP) arrangements create a target budget for providers accounting for all costs of an attributed population (likely including large numbers of children). The arrangement encourages providers to focus on reducing costs below that target budget for purposes of generating savings that can be shared between the managed care plan and participating providers. When considering the 90 percent of children who average only $2,400 a year in total expenditures, the committee openly queried whether it is reasonable to assume there are savings to be obtained from the relatively low cost of attributed children in a TCGP arrangement.
Utilization analysis suggests there are some likely areas for acute care utilization reduction and cost savings even in this low–cost population, especially asthma and gastroenteritis in younger children and behavioral health in older children. That said, the committee remained concerned that, by definition, the savings focus in a TCGP arrangement would undoubtedly be on high–need, high–cost adult populations, potentially undermining the need for additional focus on children, as discussed later in this report.
Integrated Primary Care (IPC) arrangements are designed to cover the costs of preventive care, sick care, and chronic care (though 14 chronic condition episodes). The committee considered how this VBP menu option might be amenable to meeting the unique needs of children, especially with asthma as one of the chronic condition episodes. While the primary care focus of this arrangement might appeal broadly to child health providers, the underlying shared savings/risk nature of the agreement still raises questions regarding the incentive to focus on high–cost adults, rather than on low–cost children.
The committee was especially interested in understanding the maternity care VBP arrangement, given the impact of maternal health on early childhood health and development. The maternity care episode– based arrangement includes prenatal care, delivery, and 60–day post–discharge care for the mother. It also includes the first 30 days of post–discharge care for the newborn. Recognizing the short length of time a newborn would be in this arrangement, the committee concentrated on measures for this arrangement that could directly affect a child´s birth outcomes, as described later in this report.
There are very few children served by the Medicaid special needs plans who are the target of "total care for special needs populations" VBP arrangements. Children are ineligible for Health and Recovery Plans (HARPs) and the managed care system is not yet in place for the Intellectual and Developmental Disabilities (I/DD) population. A small number of children are enrolled in HIV/AIDS special needs plans and Managed Long–Term Care plans; but, consistent with its decision to focus on the lower–cost 90 percent of children, the committee did not broadly consider the implications of these subpopulation arrangements on the child population. The committee did note, however, that this segmentation is complicated, as a small number of children already enrolled in mainstream Medicaid Managed Care incur high claims costs as a result of being medically fragile or having other extensive medical needs.
This exploration of how children and adolescents fit into existing VBP arrangements informed the rest of the committee´s discussions.
|top of section| |top of page|Section 5: Guiding Principles for Value–Based Payment for Children and Adolescent Health Services
Principles
The applicability of VBP approaches for children and adolescent health services has not been widely interrogated in academic policy circles or by most state Medicaid programs. In this sense, New York´s Medicaid program is a pioneer and innovator. To ensure recommendations to the State would reflect the ways in which children´s health differs from adult health–and therefore how "value" might differ for children´s health services–committee members elected to develop a set of observations and principles to keep in mind as they pursued their work. These observations and principles are detailed here.
- Children are not "little adults." Typical value–enhancing strategies and disease–oriented quality measures may miss key aspects of child well–being and might not be appropriate for all developmental stages.
- An efficient and effective way to achieve the Triple Aim is to identify opportunities in childhood for health improvement, thereby reducing demand for health care services in the future.
- Evidence–based childhood interventions can be linked to improvement in overall lifetime health and well–being.
- Maximizing the healthy growth and development of children today will reduce future health care needs and bring long–term value to Medicaid and other public systems, including but not limited to education, child welfare, and juvenile justice. For these reasons a longer horizon for assessing cost savings must be considered.
- VBP participation and quality measurement across child–serving sectors will yield better improvements in child health, development, and well–being.
- Due to rapid brain growth during early childhood and adolescence, social determinants of health are especially important for children. Reducing exposure to–and mitigating effects of–Adverse Childhood Experiences is also critical.
- Strengthening systems of care, including family systems, is fundamental to improving outcomes for children.
- The health and mental health of parents/caregivers significantly influences the health and mental health of children. In particular, quality maternity care and behavioral health care for caregivers is critical for setting children on an equal footing toward lifelong health.
- Access to high–quality primary care is essential.
- Access to specialty care, especially for maternal and child behavioral health, should be integrated into primary care settings to ensure appropriate access. Access to community–based services that support health should also be improved.
- Current investment in children´s health may not be sufficient to fully meet the unique needs of children.
Value statement
Building upon the principles above, the committee coalesced around the following value statement:
"Focusing on the healthy growth and development of children will improve their quality of life. Children require a value–based payment approach that acknowledges the specific needs attendant to each developmental stage and the unique opportunity to improve health and life trajectories, as well as the near–term improvements that are possible from direct health interventions. Support and recognition of families and caregivers are central to improving children´s lives."|top of section| |top of page|
Section 6: "North Star" Framework
Linking goals to appropriate measures and care strategies
As it began discussing potential recommendations and quality measures, the committee found it necessary to first clarify the desired outcomes that would stem from high–value children´s health services before proceeding with its work. This step was considered particularly important because traditional metrics for evaluating the success of value–based payment arrangements–namely, the achievement of cost savings and/or improvement on clinical quality measures–have shortcomings in the child health context. Potential cost savings pale in comparison to those from adult health care services, and high expenditure is not widely considered to be the paramount challenge with children´s health services.
Existing quality measures, while critical for driving improvement in clinical care, are primarily process– oriented and insufficient for measuring whether the health care system is optimally promoting health and development6 (see Section 8 for further discussion). Grappling with these challenges, the committee determined it was necessary to identify "North Star" goals to keep its deliberations on track.
The framework below is the product of that exercise. The framework should be read from left to right and top to bottom. Each column represents a childhood developmental stage and contains the following elements:
- Overarching "North Star" Goals: a common language goal statement of what the health care system is collectively trying to achieve for every child.
- Key Indicators: potential indicators for assessing whether progress is being made toward "North Star" goals. Many of these indicators are cross–sector.
- High–Value, Often Underutilized Primary Care Strategies: a non–exhaustive list of potential primary care strategies the Medicaid system, through VBP, could encourage in furtherance of those indicators and the underlying "North Star" goals.
Above all, this framework shows the complexity of children´s care. From the outset, a child´s health and well–being is intertwined with that of parents and caregivers, and as that child ages, the role of school in ensuring health becomes more prominent. Opportunities for primary care to influence child health and well–being also shift over this time.
While this framework was developed to guide committee deliberations, members felt it could also be useful in guiding future children´s health transformation work by New York´s Medicaid program. The committee offers this draft framework to the State, recognizing that it could still benefit from additional revision and refinement, particularly in the "key indicators" section.
Section 7: Recommendations
Recommendation process
Armed with an understanding of the Medicaid child population and existing VBP models – and with a set of principles, a value statement, and "North Star" framework in hand – the committee moved to develop recommendations for value–based payments and quality measures. In the process of developing and discussing these recommendations, it quickly became clear that given the tight timeframe it would also be important for the committee to recommend future work for this or a similar committee and/or the State. As a result, the committee developed recommendations in three areas:
- VBP Principles and Payment Model
- Quality Measures
- Additional Work/Deliberation
Building on the model used by previously convened subcommittees, the remainder of this section lays out specific recommendations and provides background descriptions to provide context for each recommendation. The information presented here is not in any way designed to reflect the full range of discussion that led to the final, unanimous consensus achieved on each recommendation. The level of detail in these recommendations is designed to provide appropriate implementation guidance to the State, while giving NYSDOH the leeway necessary to implement these recommendations effectively and in a way that is consistent with its own internal processes for adjusting payment policies, in collaboration with participating managed care plans.
Also, consistent with previous committee work, it was important to classify recommendations in such a way that the State and its managed care plans could easily determine where the committee believes it is vital for implementation to directly comply with recommendation language and where the committee believes it is necessary for managed care plans and providers to have some leeway in VBP contracting. There are also a number of recommendations that are not specific to the managed care / provider relationship. As a result, the terminology described below is used throughout the recommendations. In a few instances, the committee determined that it was especially important to note the strength with which a specific suggestion is made directly to the State.
Types of Recommendations Made in This Report
- A Standard is required when it is crucial to the success of the VBP Roadmap that all MCOs and providers follow the same method.
- A Guideline is sufficient when it is useful for providers and MCOs to have a starting point for the discussion, but MCOs and providers may deviate as local flexibility may contribute to the overall success of the VBP Roadmap.
- A Suggestion is a recommendation directed at the State that is not directly related to MCO and provider standards and guidelines.
VBP Principles and Payment Model Recommendations
Consideration of a payment model for children was heavily informed by a discussion at the November 2016 committee meeting, which featured a presentation by Marge Houy of Bailit Health on its seminal report, Value–Based Payment Models for Medicaid Child Health Services.7Based on an environmental scan, interviews with state experts, and a review of national and New York Medicaid data, the Bailit paper findings and value definition were similar to the guiding principles and value statement already developed by the committee. While the committee discussed modification of the existing VBP roadmap models to best meet the unique needs of children and adolescents, the alternative model presented by Ms. Houy quickly led the discussion towards developing a new, child–specific VBP approach for New York Medicaid.
Specifically, the Bailit analysis recognized an important distinction between the generally healthy population that could be appropriately managed in the primary care space, and the small and heterogeneous subpopulations of children that likely require highly specialized care. Ms. Houy presented two proposed models to address the differing needs of these populations: an enhanced pediatric primary care capitation model for the former, and a total cost of care model for the latter. These proposed models, combined with the utilization information presented above and the fact that managed care does not yet cover all children and services for the specialized population, led to the committee deciding to focus on creating a VBP model for the 90 percent of generally low–cost children.
Critically, the Bailit analysis arrived at three other key findings for child–serving VBP approaches. First, the value proposition for pediatric care must recognize the long–term (and not just the immediate) impact of care provided. This is different from adult value propositions that focus on improving value by reducing inpatient and emergency department utilization. Second, pediatric primary care would benefit from flexible funding arrangements that allow for financing non–traditional services, particularly those that address the underlying causes of health problems. Third, pediatricians are in a unique position to have an impact on early childhood development and to identify and help address social determinants of health.
The recommendations that follow reflect the committee´s decision to create an additional core VBP arrangement (alongside those presented on page 7 of this report) for the NYS VBP Roadmap, primarily building off of Bailit Health´s foundational work. The committee recognizes a fair amount of additional detailed work will need to be undertaken between the State, managed care plans, and providers to further work out the operational details of how to implement this arrangement. The committee also recognizes the fact that providers and plans may, in fact, choose to serve children through existing TCGP and IPC arrangements, so the recommendations also consider how the potential benefits of the newly proposed option could be extended to child populations served under the existing models.
Recommendation P1: Guiding Framework for Payment Model
Type: Suggestion
Recommendation P1: The State should adopt the "North Star" framework as the guiding framework for a VBP approach that recognizes: (1) the unique needs of children at different developmental stages; (2) the overarching role of primary care in both the delivery of health care services to children and the promotion of overall child well–being; and (3) the role of caregivers and nonmedical factors in shaping long–term health. Adoption of current and future payment models should be guided by this framework and by the American Academy of Pediatrics "Bright Futures" guidelines.
Description: Children are not "little adults." Focusing on the healthy growth and holistic development of children will improve their quality of life and long–term outcomes and reduce costs in the long–term and across sectors. Children require a VBP approach that acknowledges the specific needs attendant to each developmental stage and the unique opportunity to improve health and life trajectories, as well as the importance of responding to immediate physical and behavioral health needs. Support and recognition of families and caregivers are central to improving children´s lives.
Recommendation P2: Pediatric Primary Care Capitation (PPCC)
Type: Suggestion
Recommendation P2: The State should create an additional on–menu option in the VBP Roadmap that allows (but does not require) managed care organizations (MCOs) and providers to enter into pediatric primary care capitation (PPCC) arrangements consistent with the sub– recommendations that follow. The model would be deemed a Level 3 VBP arrangement under the Roadmap.
Description: Care for the vast majority of children is low–cost and, therefore, children may be better served by VBP models that do not rely on shared savings/risk. Additional investment in child primary care services is necessary to maximally contribute to the "North Star" goals described above. A wholly separate VBP model should be available to MCOs and providers/practitioners who voluntarily wish to develop unique VBP contracts for the pediatric population.
Recommendation P2.1: Defining the PPCC Population
Type: Guideline
Recommendation P2.1: MCOs and providers should enter into PPCC arrangements only for children who are in the bottom 90th percentile of the MCO´s overall cost/utilization distribution among its child members. Plans and providers should be granted discretion in determining the attributed child population below the 90th percentile, particularly taking into account the share of members that would be considered part of a complex population that should be excluded from the PPCC arrangement. The attributed population methodology should be subject to State review and approval.
Description: PPCC arrangements are not ideal for medically and behaviorally complex children, because they are insufficient to address the specialized needs and service utilization of these children.
Recommendation P2.2: Defining PPCC Costs and Services
Type: Guideline
Recommendation P2.2: The risk–adjusted primary care capitation should include enhancements sufficient to support all necessary screenings, risk–adjusted care coordination, and new workflows to address developmental and behavioral health needs and social determinants. An additional enhancement should be provided to primary care practices with co–located and operationally integrated behavioral health care, taking into account the different operational and staffing costs of various models. While the capitation rate should include nearly all primary care service needs for children, including the previously described enhancements, MCOs and providers can agree to exclude services where there are underutilization concerns (e.g., vaccine costs). Parties may also agree to exclude pediatric services provided by some, but not all, providers that are party to the PPCC arrangement (e.g., suturing).
Description: The capitation rate in PPCC agreements must reflect the role of providers in screening and coordinating care for social, behavioral, and developmental threats to health, in addition to medical needs. The capitation rate in PPCC arrangements should also include the costs of co–located behavioral and developmental services for parents and children.
Recommendation P2.3: PPCC Disbursement and Withholds
Type: Standard/Guideline
Recommendation P2.3:
Standard: MCOs shall implement a withhold from the PPCC rate to be disbursed at least annually based on both improvement and high performance on all Category 1 Pay–for–Performance (P4P) measures, and complete and accurate reporting of Category 1 Pay–for–Reporting (P4R) measures.
Guideline: MCOs and providers shall agree upon a percentage withhold, and the weighting by which performance payments from the withhold are disbursed based on improvement and high performance. In weighting, MCOs and providers should take into account measures of particular relevance to the population being served, and current provider performance on those measures.
Description: In a PPCC model, providers are paid a per–member / per–month payment for an attributed population of children. In order to ensure that providers do not unduly limit child health utilization or reduce the quality of care provided under this model, a percentage withhold and periodic improvement/performance payment based on agreed–to measures is necessary.
Recommendation P2.4: PPCC Pilot Testing
Type: Suggestion
Recommendation P2.4: The State should consider offering pilot opportunities for the PPCC VBP model similar to the pilots offered for the existing VBP Roadmap models.
Description: While PPCC is not an entirely new payment approach to some MCOs and providers, capitation arrangements with the depth and specificity of the approach described in these recommendations are not as widespread. It also may introduce currently unforeseeable effects as it intersects with TCGP/IPC arrangements, or in cases where individual providers are pursuing a multitude of Medicaid and commercial VBP approaches for pediatric populations.
Recommendation P3: Pediatric Methodology in TCGP and IPC
Type: Guideline
Recommendation P3: MCOs and providers in TCGP and IPC arrangements should consider appropriate children´s utilization and cost (including any potential additional enhancements added to MCO rates via a PPCC–related increase) in determining baseline pediatric spending targets in these shared–savings/risk arrangements. The State should review this methodology as part of the VBP contract review process in order to ensure that pediatric primary care providers are not penalized for making appropriate additional investments in child services that are unlikely to generate one–year savings opportunities.
Description: Not all children will be served through a PPCC arrangement. Many will be covered by broader TCGP or IPC arrangements that include shared savings/risk. In those arrangements, pediatric providers should not be put at a financial disadvantage because low–cost children generally do not generate savings. Pediatric providers should also receive any pediatric enhancements envisioned under PPCC.
VBP Quality Measure Recommendations
Reflecting its dual role as a Subcommittee and a Clinical Advisory Group (CAG), the committee was charged with: 1) reviewing the state of child health measurement in NY VBP arrangements, with an eye towards ensuring child and adolescent quality measures are sufficiently included; and 2) developing a child–focused quality measure set. This section focuses on the recommendations that resulted from the committee´s review of New York´s current VBP arrangements and related measure sets. See Section 8, pages 28–33, for discussion of the final proposed Universal Child Measure Set.
The committee focused its review on the VBP Roadmap, the TCGP/IPC measure set, and the Maternity Care measure set. It also considered how quality measurement would fit into the PPCC model outlined on pages 19–22. The need for five actions emerged during this review:
- Aligning new and existing quality measures across VBP arrangements to ensure the same standard of care for all children and adolescents;
- Elevating the importance of high–quality maternity care in determining child health outcomes;
- Encouraging the use of quality measurement for continued clinical improvement and reducing health disparities;
- Further developing child health quality measures that are outcome–oriented, even if they are long– term or cross–sector in nature;
- Continuing to refine VBP quality measure sets as additional and improved quality measures become available, and as high–performing measures are able to be rotated off the sets.
The committee makes the following recommendations to the VBP Workgroup in light of these needs:
Recommendation M1: Guiding Framework for Measurement
Type: Suggestion
Recommendation M1: The State should adopt the "North Star" goals and key indicators at each developmental stage, and the American Academy of Pediatrics "Bright Futures" guidelines as the guiding framework by which the success of VBP for children is measured. These frameworks should be considered as part of all future children´s measure development and implementation for VBP purposes and beyond.
Description: Standard health measures alone are insufficient to fully assess outcomes of high– value well–child care. Cross–sector measures of child development and well–being may be good proxy measures. While it is not currently feasible or appropriate to hold providers accountable for such cross–sector measures of appropriate child development, the State should not lose sight of these larger goals as it advances VBP for children.
Recommendation M2: Integration with Existing Measures
Type: Suggestion (Strongly Recommended)
Recommendation M2: Measures developed for the PPCC model should be integrated with existing measures to create a universal TCGP/IPC/PPCC measure set for 2018 and beyond. PPCC measures in this universal set should be updated at least annually, consistent with the processes used to update TCGP/IPC measures.
Description: Many children will be covered by TCGP/IPC arrangements regardless of the availability of the PPCC VBP model. The current TCGP/IPC measure set does not include sufficient child–focused measures to ensure that providers are striving to improve and achieve high performance for children under those VBP models.
Recommendation M3: Integration with Maternity Care Episode–Based Arrangement
Type: Suggestion (Strongly Recommended)
Recommendation M3: Four specific measures for the current Maternity Care VBP arrangement that are especially relevant for child health should be added to the TCGP measure set as soon as feasible. Relatedly, the maternity CAG should consider adding one new maternity care measure identified by the children´s CAG as particularly relevant to children´s health: behavioral risk assessment for pregnant women. That measure should be added to the TCGP measure set as soon as feasible, as adopted for the Maternity Care arrangement.
Description: Maternal health has a major impact on child health, especially during pre– and post– natal periods and during the first year of a child´s life. Under the VBP Roadmap, maternity services could be provided either through the Maternity Care episodic VBP arrangement or through a TCGP VBP arrangement (maternity costs are specifically excluded from the IPC model). The Maternity Care Measure Set, however, only applies to births covered under a Maternity Care episodic VBP arrangement. Given the dual impact on child and maternal health, and the reality that many births will take place in TCGP arrangements, at least some Maternity Care Measure Set metrics should be included in the TCGP measure set (subject to additional deliberation and recommendation by the Maternity CAG).
Recommendation M4: Tracking Progress
Type: Standard
Recommendation M4: VBP arrangements, regardless of model, should require providers and MCOs to report and track performance on pediatric VBP measures at the most detailed disaggregation of race/ethnicity possible.
Description: The pediatric population is more diverse than the adult population and disparities in care are especially troubling for children. Tracking VBP measures for children with race/ethnicity breakdowns will provide a unique opportunity to assess disparities and identify future opportunities for improved equity through appropriate disparity reduction targets.
Recommendation M5: Developmental Screening
Type: Suggestion
Recommendation M5: The State should expedite its efforts to work with providers and plans through its School Readiness VBP Pilot, New York´s Early Childhood Comprehensive Systems federal grant, and other related efforts, in order to refine its approach to using Developmental Screening in the First Three Years of Life (NQF #1448). The State should consider lessons learned from other states that have modified their billing policies for this measure, including Maine, Massachusetts, Minnesota, North Carolina, and Connecticut. The goal of this work should be on reasonably resolving concerns related to NQF #1448´s measure specifications and updating related clinical guidance for providers and plans, in order to adopt a developmental screening measure as a Category 1 measure by Measurement Year 2019.
Description: Developmental screening (understood to include four domains: motor, language, cognitive, and social–emotional development) is widely recognized as an important clinical strategy for early identification of children experiencing developmental delays and challenges. When combined with access to appropriate interventions, developmental screening is a critical strategy for ensuring that children are able to achieve their maximum potential. Developmental Screening in the First Three Years of Life (NQF #1448) is included in the CMS Child Core Set of quality measures; 22 states reported annual data on developmental screening as part of that process in fiscal 2015. While acknowledging that there are concerns with developmental screening measure NQF #1448, particularly the validity of using the billing code CPT 96110 to collect appropriate measurement data, the committee believes it is important to overcome these barriers to encourage developmental screening in clinical practice.
Payment and Measure Recommendations:
Note for VBP Workgroup Consideration
In general, the payment and measure recommendations presented above were developed as a complementary set of recommendations designed to ensure that, regardless of which VBP model children are served by, they receive the same advantages generated by these incentives and metrics. For example, recommendations P1 and M1 are mirror recommendations recognizing the importance of the “North Star” goals in both payment and measurement. Adopting either the payment or measure recommendations without the other could greatly undermine the ability of New York Medicaid to fully achieve its child health and development goals.
Additional Work Recommendations
Despite making significant progress over the year, committee members are keenly aware that further work is needed. In particular, significant attention needs to be given to considering the appropriateness and potential opportunities of value–based payment for vulnerable subpopulations of children and adolescents, especially those who require higher intensity health services. Additional work is also needed to develop and test additional alternative approaches to optimizing child health and well–being through VBP.
The committee makes the following recommendations to the VBP Workgroup:
Recommendation A1: Focus on Children with Complex Health Needs
Type: Suggestion
Recommendation A1: The State should utilize this committee or a subgroup thereof, or develop a new advisory group, to make recommendations on payment models and measures for children with complex health needs. This process should specifically consider:Description: The committee discussed a number of options for addressing the unique needs of complex children and families through VBP and worked with a subset of members to brainstorm potential models for the behaviorally complex subpopulation. Given time and data constraints, the heterogeneity of subpopulations within the group of complex children and families (e.g., medically complex, medically fragile, behaviorally complex, and children with social services involvement), and the recognition that some of these children are not yet in managed care and that some relevant services remain carved–out, additional deliberation is required.
- The definition of children with complex health needs for VBP purposes and the issue of feasibility of VBP models for small and unique population subsets (e.g., children with medically and/or behaviorally complex needs, children who fall under the State´s definition of "medically fragile," and children with social services involvement) and substantial regression to the mean.
- Whether a payment model for families with behaviorally complex needs (which would include children and their caretakers on Medicaid) is viable and feasible, and whether it should be piloted.
- What measures from the TCGP/IPC/PPCC measure set should apply to children with complex health needs (and/or redefined subsets thereof) and what additional measures are required.
- Whether centers of excellence for very small subsets of children with complex health needs (e.g., medically fragile) could be a viable strategy for achieving VBP goals without creating unnecessary risk for providers and MCOs.
Recommendation A2: Iterative Review Process
Type: Suggestion
Recommendation A2: The State should utilize the existing CAG expertise but consider a centralized and streamlined process for: 1) reconsidering VBP measures annually; 2) adopting new measures as they become available and/or appropriate; 3) encouraging further development of Category 1 P4R and Category 2 measures so that they can become P4P; and 4) developing additional measures that are important to VBP goals, but not currently feasible. This group or a subgroup thereof could be charged with refinement of the pediatric "North Star" goals and indicators and developing pathways for cross–sector measurement with the involvement of appropriate cross–sector stakeholders including, for example, education partners. The Oregon Metrics and Scoring Committee is an example the State should consider as a model.
Description: Ongoing measure review, development, and implementation are required to continue to push the envelope for improvement and to ensure that the measures being utilized are valid and appropriate. Outside of the current CAGs there is no obvious venue for this vital, ongoing work.
Recommendation A3: Additional Pilot Testing
Type: Suggestion|top of section| |top of page|
Recommendation A3: The State should build on its early efforts (e.g., the "Connections: A value–driven project to build strong brains" pilot) to develop additional pilots, programs, and technical assistance efforts that (1) test, evaluate and spread optimum pediatric primary care delivery models or (2) evaluate new funding approaches (considered "off–menu" for the VBP Roadmap) that are focused on achieving the "North Star" goals. Opportunities to be explored through new pilots include developing delivery system models for two–generation (caregiver and child) health services, testing a VBP model for complex families, and assessing whether cross– sector systems integration and blended funding streams can result in child–related shared savings.
Description: Many efforts are underway in New York to transform the delivery system, strengthen primary care, and promote payment innovation. Few of those efforts focus specifically on the unique needs of pediatric patients or pediatric primary care practices. Yet promising pediatric–specific delivery system models, such as Healthy Steps, exist in New York. The State should learn from practices that are currently implementing these approaches in order to develop guidance on how to generalize and spread these models, then support the scaling of such models through pilot programs and technical assistance. Additionally, more work is needed to test and evaluate emerging delivery system ideas and payment innovations that might result in improved outcomes for children and their caregivers. These new innovations could be supported by some form of pediatric innovation fund.
Section 8: Quality Measure Sets
Principles and criteria
The final task of the committee was to select child–focused quality measures for inclusion in VBP arrangements beginning in 2018. Development of the committee´s performance measure sets was shaped by four criteria:
- The measure is relevant to one of the strategies identified to achieve a particular "North Star" goal.
- The measure is evidence–based (i.e., has been tested for validity and reliability, and, preferably, is endorsed for use by the National Quality Forum).
- The measure should be feasible for providers to use and report with minimal additional burden (i.e., does not require expensive medical records review or sophisticated health information technology capacity).
- The final recommended measure set should be parsimonious, with outcome measures having priority.
The committee also wished to align its recommendations, as much as possible, with other performance measure reporting programs, such as New York´s Quality Assurance Reporting Requirements (QARR) for health plans, DSRIP measures, the federal Medicaid Child Health Measurement Set, NCQA´s Healthcare Effectiveness Data and Information Set (HEDIS), and other New York VBP measure sets, notably those used for maternity care and the TCGP/IPC.
Selection process
The selection process began with assembling a measure "library" of more than 70 measures culled from these diverse sources. That list was augmented by specific suggestions from committee members, and the entire list was reviewed for relevance to the identified "North Star" goals and strategies. Staff from the state Office of Health Insurance Programs and the Office of Quality and Patient Safety also worked with committee staff to identify issues related to the feasibility, validity or modification of particular measures that were under discussion.
Although the committee´s charge was to focus on child and adolescent health care, there was broad agreement that maternity care is central to children´s health. It therefore reviewed the set of VBP maternity measures for overlap with its own proposed list, as well as for any perceived gaps. For reader convenience, the maternity–related measures are presented separately, after the child measure set, in this report.
Identifying appropriate outcome measures proved to be especially difficult. It is a common complaint in the health care quality community that most health care performance measures currently in use– including those used in pediatrics–are measures of process, not outcome. Developing satisfactory outcome measures for pediatrics is especially challenging, since the impact of good quality care is often felt outside the health care system itself–for example, in school or athletic performance–and over many years of life. The feasibility of implementing measures that require linking data from diverse sources, such as effective management of a chronic condition with school attendance, is significant, and can involve issues of data system compatibility, security, and confidentiality that are difficult to resolve quickly. Unfortunately, the committee was unable to identify any such cross–sector outcome measures ready for adoption at this time, but strongly recommends that future development of such measures has a high priority in New York.
Consistent with previous CAG deliberations, measures can be categorized as Category 1, 2, or 3 based on their feasibility. Category 1 measures can further be classified as Pay–for–Performance (P4P) or Pay– for–Reporting (P4R). Category 1 measures are to be reported by VBP contractors. Category 2 measures present at least some concern regarding feasibility but could be included in VBP contract agreements between providers and plans. Category 3 measures are not currently feasible, and they have been removed from the measure sets presented below.
Universal Child Measures
Consistent with recommendation M2 presented earlier, the final child measure set would be applicable to any TCGP, IPC or PPCC VBP arrangement. This universal child set totals 20 measures, 13 of which are in Category 1 and 7 in Category 2 (see summary chart below).
Universal Child Measure Set: Summary Chart
| Category | Type | Already included in TCGP/IPC set |
Newly Recommended |
Total Measures |
|---|---|---|---|---|
| 1 1 1 |
Pay for Performance Pay for Reporting Category 1 subtotal |
4 1 |
4 4 |
13 |
| 2 2 |
Category 2 (all types) Category 2 subtotal |
1 |
6 |
7 |
| TOTAL | 20 | |||
Rationale for new vs. existing measures
Fourteen of the measures in the universal child set are newly recommended measures–that is, they are not already included in the current Total Care for General Population and Integrated Primary Care (TCGP/IPC) set of measures. Eight of these fourteen measures are designated as Category 1, four of which are Pay for Performance measures and four of which are Pay for Reporting. Most of these measures, however, are not "new" to pediatric providers or managed care plans in New York, as they have been included in the state´s QARR program requirements for at least several years.
The exception is measure #7, the rate of inpatient admissions of children with a principal diagnosis of asthma. This measure is a subset of a larger pediatric composite measure that includes four conditions: asthma, diabetes, gastroenteritis, and urinary tract infections. The committee concluded that in light of the high prevalence of asthma among children in New York, and the extent to which hospitalization can be minimized with appropriate management, only the rate of asthma hospitalizations should be recommended.
Seven of the eight Category 2 measures are newly recommended measures. Measure #14, screening for reduced visual acuity and referral in children under age 6, was approved late in 2015 by NQF as an e– measure for trial use. The measure is intended for use in the primary care setting to encourage early identification of vision impairments in preschool children and appropriate referral to eye care specialists. The committee recognized that this measure is not ideal–preferably there would be a claims–based measure of the number of children receiving an eye examination–but such a measure does not exist.
The committee ultimately agreed that failure to include any kind of vision measure, even one that is only in the trial stage, would be a significant omission.
Measure #20, use of first–line psychosocial care for children and adolescent on antipsychotics, was endorsed by NQF in 2016 and incorporated into both the New York State QARR set and the CMS Child Core Set in 2017. Measures #18 and #19, relating to follow–up after an ED visit, are new HEDIS measures and have also been incorporated in the New York State QARR set for 2017. The committee agreed that all four of these measures can be important in identifying opportunities for improvement and that, despite their relatively recent introduction to the library of available measures, they are appropriate Category 2 measures.
The committee discussed the remaining two measures at some length before arriving at its final recommendation. Measure #15, maternal depression screening during the child´s first six months of life, was initially proposed as a Category 1 measure. The state Medicaid program has a policy that the pediatrician can receive reimbursement for the mother´s screen during the first year of a child´s life (the inconsistency between this state policy and the quality measure–which is focused on the child´s first six months of life–prompted calls among several committee members for a revised national measure) and pilot–testing of the measure is currently underway. However, the measure is an electronic Clinical Quality Measure, which New York´s current quality measurement infrastructure does not support. The committee therefore recommended that the measure be included in Category 2, and that it be moved to Category 1 once the State has the capacity to collect electronic Clinical Quality Measures.
Measure #17, developmental screening during the first 36 months of life, is perhaps the most extensively discussed measure of the entire set. This measure has been in the CMS Child Core Set for more than five years and, as of 2015, more than 20 state Medicaid programs were using it. New York State does not currently use the measure. The measure developer cautioned that ambiguity in coding and lack of clarity about which screening tools constituted an acceptable comprehensive screen could result in scores that were not really comparable across providers. Given the importance of such a measure to identify problems as early as possible in a child´s life, the committee felt it was essential to include the measure at least at the Category 2 level and urge the State to work towards its adoption (see Recommendation M5, page 24).
The committee also discussed four measures that are not recommended at this time but are worth noting. NQF measure #0576, follow–up after hospitalization for mental illness, was not recommended because it was deemed not feasible to hold primary care providers accountable for the measure at the VBP contractor level. NQF #2695, follow–up after ED visits for dental caries, was not recommended for a similar reason – the follow–up rests with the dental community, not with pediatricians – and two other preventive dental health measures were prioritized in the set. Given the importance of detecting hearing problems prior to school entry, the committee considered NQF #1360, audiological evaluation no later than three months of age, but felt it was not distinct enough from NQF #1354 (hearing screening prior to hospital discharge), which has high performance across the state. Similar to the discussion above about the need for a standardized vision examination measure, it is the opinion of the committee that a hearing measure for early childhood needs to be developed. Finally, the committee decided against recommending measures based on the child version of the CAHPS survey of care at the clinician and group level. New York State does biennially administer, and report results based on a CAHPS survey at the health plan level, but administering one at the individual provider level is expensive and could pose significant small–number problems.
Note on Universal Child Quality Measure Set Color Coding
| Green | This measure is already included in the TCGP/IPC measure set. The committee recommends these measures for inclusion in a universal TCGP/IPC/PPCC child set. |
| Orange | This measure is newly recommended by the committee for inclusion in a universal TCGP/IPC/PPCC child set. |
Universal Child Quality Measure Set (Category 1)
| # | Measure (NQF #) | Steward | Data Source | Category |
|---|---|---|---|---|
| 1 | Adolescent well–care visit rate Percentage of enrolled members 12–21 years of age who had at least one comprehensive well–care visit with a primary care provider or an OB/GYN practitioner during the measurement year. |
NCQA | Claims | 1 P4R |
| 2 | Assessment and counseling of adolescents on sexual activity, tobacco use, alcohol and drug use, depression (four–part measure) Percentage of adolescents ages 12–17 who had at least one outpatient visit with a primary care provider or OB/GYN practitioner during the measurement year and received assessment, counseling or education on sexual activity, depression, tobacco use, and alcohol or other drug use. |
NYS | Claims, Medical Record | 1 P4R |
| 3 | BMI assessment and counseling (NQF 0024)* Percentage of patients 3–17 years of age who had an outpatient visit with a Primary Care Physician (PCP) or Obstetrician/Gynecologist (OB/GYN) and who had evidence of the following during the measurement period. Three rates are reported.
|
NCQA | Medical Record | 1 P4P |
| 4 | Child immunization status, age 2 (combo 3) (NQF 0038)* Percentage of children 2 years of age who had four diphtheria, tetanus and acellular pertussis (DtaP); three polio (IPV); one measles, mumps and rubella (MMR); three H influenza type B (HiB); three hepatitis B (HepB); one chicken pox (VZV); four pneumococcal conjugate (PCV); one hepatitis A (HepA); two or three rotavirus (RV); and two influenza (flu) vaccines by their second birthday. The measure calculates a rate for each vaccine and nine separate combination rates. |
NCQA | Claims, Medical Record | 1 P4P |
| 5 | Children ages 2–20 having annual dental visit Percentage of children ages 2–20 who have at least one dental visit during the year. |
NYS | Dental Claims | 1 P4R |
| 6 | Chlamydia screening, ages 16–21 (NQF 0033)* The percentage of women 16–20 years of age who were identified as sexually active and who had at least one test for chlamydia during the measurement year. |
NCQA | Claims | 1 P4P |
| 7 | PDI #14 asthma admission rate, ages 2 through 17 years Rate of inpatient admissions of children with a principal diagnosis of asthma per 100,000 population, ages 2 through 17 years. |
AHRQ | Hospital discharge data | 1 P4P |
| 8 | Follow–up care for children prescribed Rx for ADHD (NQF 0108) Two part measure: initiation phase and continuation phase Percentage of children newly prescribed attention– deficit/hyperactivity disorder (ADHD) medication who had at least three follow–up care visits within a 10–month period after the first ADHD medication was dispensed. The measure includes two separate rates: an initiation phase rate (follow–up visit within the 30 days after starting the medication) and a continuation and maintenance phase rate (children who remained on the medication for 7 months and who, in addition to the visit in the initiation phase had at least two follow–up visits in the 9 month period after the initiation phase ended). |
NCQA | Claims | 1 P4R |
| 9 | Frequency of well–child visits, ages 3 to 6 (NQF 1516) Percentage of children 3–6 years of age who had one or more well– child visits with a primary care provider during the measurement year. |
NCQA | Claims | 1 P4P |
| 10 | Frequency of well–child visits during the first 15 months of life (NQF 1392) Percentage of children 15 months old who had the recommended number of well–child visits with a primary care provider during their first 15 months of life. |
NCQA | Claims | 1 P4P |
| 11 | Medication management for children with asthma, ages 5–18 (NQF 1799)* 2 part measure: The percentage of patients 5–18 years of age during the measurement year who were identified as having persistent asthma and were dispensed appropriate medications that they remained on during the treatment period. Two rates are reported.
|
NCQA | Claims, EMR | 1 P4P |
| 12 | Screen for depression using age appropriate tool and follow–up, ages 12+ (NQF 0418)* Percentage of patients aged 12 years and older screened for clinical depression using an age appropriate standardized tool AND follow– up plan documented. |
CMS | Claims, registry | 1 P4R |
| 13 | Adolescent immunization rate, including rate for HPV (NQF 1407) Percentage of adolescents 13 years of age who had one dose of meningococcal vaccine, one Tdap, and 3 doses of HPV by their 13th birthday. The measure calculates a rate for each vaccine and two combination rates. |
NCQA | Claims | 1 P4P |
Universal Child Quality Measure Set (Category 2)
| # | Measure (NQF #) | Steward | Data Source | Category |
|---|---|---|---|---|
| 14 | Screening for Reduced Visual Acuity and Referral in Children (NQF 2721—approved for trial use) The percentage of children who received visual acuity screening at least once by their 6th birthday; and if necessary, were referred appropriately. |
CMS | EMR | 2 |
| 15 | Maternal depression screen done during child´s first 6 months of life Percentage of children who turned 6 months of age during the measurement year, who had a face–to–face visit between the clinician and the child during the child´s first 6 months, and who had a maternal depression screening for the mother at least once between 0 and 6 months of life. |
NCQA | EMR, CMS eCQM #82 | Cat 2, with recommendation that upon completion of ECQM this measure immediately becomes Cat 1 P4R. |
| 16 | Children at elevated risk of caries who received fluoride varnish applications (NQF 2528)* Percentage of enrolled children aged 1–21 years who are at "elevated" risk (i.e. "moderate" or "high") who received at least 2 topical fluoride applications as a dental OR oral health service within the reporting year. |
American Dental Association (ADA) | Claims | 2 |
| 17 | Developmental screening using standardized tool, first 36 months of life (NQF 1448) Percentage of children screened for risk of developmental, behavioral and social delays using a standardized screening tool in the first three years of life. The measure includes three, age–specific indicators assessing whether children are screened by 12 months of age, by 24 months of age and 36 months of age. |
Oregon HSU | Claims or Medical Record | 2 |
| 18 | Follow–up after ED visit for mental illness, ages 6 and older Percentage of ED visits with a primary diagnosis of mental illness for which the patient received follow–up care with any practitioner within specified time frames. Reported in two separate rates: within 7 days of the ED visit and within 30 days of the visit. |
NCQA | Claims | 2 |
| 19 | Follow–up after ED visit for alcohol and other drug dependence, ages 13 and older Percentage of ED visits with a primary diagnosis of alcohol or other drug dependence for which the patient received follow–up care with any practitioner within specific time frames. Reported in two separate rates: within 7 days of the ED visit and within 30 days of the visit. |
NCQA | Claims | 2 |
| 20 | Use of first–line psychosocial care for children and adolescents on antipsychotics (NQF 2801) Percentage of patients, ages 1–17, who had a new prescription for an antipsychotic medication and had documentation of psychosocial care as first–line treatment. |
NCQA | Claims | 2 |
Maternity Measures
As noted earlier in this report, the committee also decided to recommend a group of maternity measures it considers equally relevant for child health quality, and which therefore should be applicable to TCGP as well as the Maternity Care arrangement (consistent with Recommendation M3). The committee recognizes that this may require additional deliberation and recommendations from the Maternity CAG to the VBP Workgroup. This child relevant maternity set, a total of five measures, includes only one that is not already in the Maternity Care list.
Maternity Measure Set: Summary Chart
| Category | Type | Already included in TCGP/IPC set |
Newly Recommended |
Total Measures |
|---|---|---|---|---|
| 1 1 1 |
Pay for Performance Pay for Reporting Category 1 subtotal |
1 3 |
0 0 |
5 |
| 2 2 |
Category 2 (all types) Category 2 subtotal |
0 |
1 |
0 |
| TOTAL | 5 | |||
The one newly recommended measure, behavioral risk assessment for pregnant women, generated considerable discussion within the committee, as it is a measure based on an electronic medical record and its suitability for widespread use across the state is untested. However, the committee consensus was to recommend that it be endorsed by the Maternity CAG as a Category 1 P4R measure. The measure has recently lost its steward and may be removed from Child Core Set due to a flaw in the measure identified during medical record review. As a result, the final committee recommendation is that the Maternity CAG endorse the measure as Category 2 recognizing the importance of the risk assessment for pregnant women. The committee considered recommending another measure, hearing screening of newborns before hospital discharge, but decided not to include it due to high performance and because the measure does not include referral to a specialist when problems are detected.
Note on Maternity Measure Set Color Coding
| Blue | This measure is already included in the Maternity Care set. It is recommended for broader inclusion in TCGP but not PPCC. |
| Orange | This measure is newly recommended. The committee recommends this measure for inclusion in TCGP and Maternity Care arrangements. |
Maternity Measure Set
| # | Measure (NQF #) | Steward | Data Source | Category |
|---|---|---|---|---|
| 1 | Infants exclusively fed with breast milk in hospital (NQF 480)* The number of newborns exclusively fed with breast milk during the newborn´s entire hospitalization. |
Joint Commission | Claims, Medical Record | 1 P4R |
| 2 | Live births less than 2500 grams (NQF 1382)* The adjusted rate for live infants weighing less than 2500 grams among all deliveries by women continuously enrolled in a plan for 10 or more months. |
AHRQ | PQI #9 | 1 P4R |
| 3 | Timeliness and frequency of prenatal and postpartum care visits* Prenatal Care: The percentage of deliveries that received a prenatal care visit as a patient of the organization in the first trimester or within 42 days of enrollment in the organization. Postpartum Care: The percentage of deliveries that had a postpartum visit on or between 21 and 56 days after delivery. |
NCQA | Claims, Medical Record | 1 P4P |
| 4 | Women provided most or moderately effective methods of contraceptive care within 3 to 60 days of delivery (NQF 2902)* Among women aged 15–21 who had a live birth, the percentage that is provided a most effective (sterilization, contraceptive implants, intrauterine devices or systems (IUD/IUS)) or moderately (injectables, oral pills, patch, ring, or diaphragm) effective method of contraception within 3 and 60 days of delivery. |
OPA | Claims | 1 P4R |
| 5 | Behavioral risk assessment for pregnant women Percentage of women who gave birth during a 12–month period who were seen at least once for prenatal care and who were screened for depression, alcohol use, tobacco use, drug use, and intimate partner violence. |
No Current Steward | EMR | Recommend to Maternity CAG as Category 2 |
Future Measures for Child and Adolescent Health
During its discussions the committee identified several areas where the Universal Child Measure Set would ideally be broadened to support achieving the "North Star" goals. Paramount in this discussion was the need to prioritize the development of key indicators and outcome measures that reflect improvements in a child´s developmental trajectory and social–emotional growth. The creation of such measures would represent an important shift from focusing on processes, including the use of specific screening tools and interventions, to focusing on the results of a wide range of services that can be delivered in primary care. In a number of areas this will require actual development and testing of a measure before it can be recommended for use. Measures that require data collection outside of the traditional health care domain will also require working through complicated data–sharing relationships that will protect patient privacy but also permit enhanced learning and accountability between systems that serve children.
The committee´s "wish list" of future measures includes:
- Measures linked to school–based data sets, such as absence due to illness or suspension/expulsion and scores on kindergarten–ready assessments;
- Measures related to improvements in family strengthening and reduction of toxic stress in a child´s life;
- Measures that help evaluate the impact of primary prevention interventions and behavioral health services on family involvement with the child welfare system or juvenile justice system;
- Measures of care coordination quality for children with medically complex conditions, including measures based on patient– or parent–reported data, and measures that assess coordination among medical settings, schools, day care facilities, and community–based organizations;
- Measures based on data derived from adolescents´ self–assessment of their health status and capability of functioning successfully in school or workplace;
- Measures that are more amenable to measurement–based primary care–e.g., measures that have shorter time frames and can be administered repeatedly visit by visit; and
- Measures of individual or economic mobility–including but not limited to metrics such as employment rates, workforce participation rates, and percent of families relying on low–cost food–as a long–term outcome measure of early childhood interventions.
______________________________________________________________
1. New York State Department of Health, " A Path Toward Value–Based Payment: Annual Update", June 2016 version as approved by CMS in March 2017. 1
2. Dr. Alicandro served as co–chair from October 2016 – June 2017, at which time she joined the NYSDOH Office of Quality and Patient Safety and stepped down as committee co–chair. 2
3. Dr. Kaczorowski began his service as co–chair in July 2017 following Dr. Alicandro´s term. 3
4. The full set of committee meeting materials can be accessed here. 4
5. L. Kennedy–Shaffer and C. Shearer. "http://www.uhfnyc.org/publications/881143Understanding Medicaid Utilization for Children in New York State: A Chartbook", United Hospital Fund, July 2016: 5
6. S. Brundage, "You Get What You Pay For: Measuring Quality in Value–Based Payment for Children´s Health Care" United Hospital Fund, June 2016. 6
7. Bailit Health, "Value–Based Payment Models for Child Health Services: Report to the Schuyler Center for Analysis and Advocacy and the United Hospital Fund," July 2016. 7
Follow Us