Quality Strategy for the New York State Medicaid Managed Care Program
2015
- Document is also available in Portable Document Format (PDF, 1.3MB)
Prepared by
The New York State Department of Health
Office of Quality and Patient Safety
September 2015
Table of Contents
- Introduction
- Background
- Managed Care Program Objectives
- Approach
- Measurement and Assessment
- QARR Measurement Set
- Encounter Data
- Data on Race, Ethnicity and Primary Language
- Uniform Assessment System – New York
- Member Satisfaction Surveys
- Prevention Quality Indicators
- MLTC Specific Performance Measurement
- DISCO Specific Performance Measurement
- Behavioral Health Specific Performance Measurement
- Improvement
- Focused Clinical Studies
- Performance Improvement Projects
- Pay for Performance – Quality Incentive
- PQI Improvement
- Quality Performance Matrix
- Publication of Quality Performance Reports
- Quality Improvement Conferences and Trainings
- Plan Manager Technical Assistance
- DISCO Quality Improvement
- Delivery System Transformation
- Contract Compliance and Oversight
- Participating Provider Network Reports
- Adherence to Clinical Standards/Guidelines
- External Quality Review – Technical Report
- Review of Managed Care Organizations
- Complaint Reports
- Fraud and Abuse Reports
- Quarterly and Annual Financial Statements
- Council on Quality and Leadership (CQL)
- Member Participation on DISCO Governing Board
- SAMM Index
- Membership on MCO/HARP Subcommittees
- Health Information Technology
- Enforcement
- Measurement and Assessment
- Review of Quality Strategy
- Public Input
- Strategy Assessment Timeline
- Achievements and Opportunities
- Managed Care Performance
- Satisfaction with Care
- Access to Care
- Integrating Service Settings
Appendix 1 – Contract Compliance of MCOs/PIHPs
Appendix 2 – Internal Quality Assurance Plan (QAP)
Appendix 2a Credentialing Criteria – Recommended Guidelines
Appendix 3 – NYS DOH QARR Measures, 2014
Appendix 4 – NYS MLTC Report Measure Descriptions
Appendix 5 – DISCO Specific Performance Measures
Appendix 6 – Behavioral Health Performance Measures
Appendix 7 – NYS Managed Care Published Journal Articles
I. Introduction
In 1997, New York State (NYS) received approval from the Center for Medicare and Medicaid Services (CMS), through an 1115 Waiver, to implement a mandatory Medicaid managed care (MMC) program. The program, entitled the Partnership Plan Demonstration, set out to improve the health status of low–income New Yorkers by: increasing access to health care for the Medicaid population; improving the quality of health care services delivered; and expanding coverage to additional low–income New Yorkers with resources generated through managed care efficiencies. The Quality Strategy for the New York State Medicaid Managed Care Program (the Quality Strategy), a requirement of the 1115 Waiver, delineates the goals of the NYS Medicaid managed care program and the actions taken by the New York State Department of Health (NYS DOH) to ensure the quality of care delivered to Medicaid managed care enrollees. The Quality Strategy has evolved over time as a result of programmatic changes, member health needs, clinical practice guidelines, federal and state laws, lessons learned, and best practices; it has been successful as measurable improvements in the quality of health care being provided to enrollees have been noted.
New York State is currently undertaking significant delivery system transformation with innovative and ambitious activities of the Medicaid Redesign Team (MRT), managed care programing, and state plan amendment (SPA). The state´s approach to quality assessment, measurement, oversight, and improvement in the Medicaid managed care program increasingly necessitates interweaving the individualized efforts of several state agencies responsible for specialized care of distinct populations. As previously exempt or excluded populations, such as dual–eligibles and those living with developmental disabilities or behavioral health conditions, are enrolled into specialized managed care plans, the Quality Strategy for the Medicaid managed care program will expand. Agency specific quality strategies may also be developed and maintained, consistent with the Quality Strategy.
The state´s current quality strategy encompasses the traditional plans (including Child Health Plus (CHP) and Family Health Plus (FHP) populations), Managed Long Term Care (MLTC) plans (including Medicaid Advantage Plus, Program of All–inclusive Care for the Elderly (PACE), and partially capitated MLTC plans), HIV/AIDS Special Needs Plans (SNPs), behavioral health special needs Health and Recovery Plans (HARPs), and Developmental Disabilities Individual Support and Care Coordination Organizations (DISCOs). Several of these plans are new, therefore their measurement systems and quality monitoring are not as established as those of the traditional plans. As such, the goals of the MMC program, and the activities related to the Quality Strategy, have expanded accordingly. A separate quality strategy for Developmental Disability services, entitled the Quality Management and Improvement Strategy for the New York State Office for People with Developmental Disabilities (OPWDD), is maintained by OPWDD and is referenced herein where appropriate. As part of the integration of behavioral health services into managed care, the Office of Mental Health (OMH) and the Office for Alcoholism and Substance Abuse Services (OASAS) will maintain a separate quality strategy for behavioral health based on values that address person–centered care, recovery–oriented services and cultures, integrated care, data driven quality improvement, and evidence–based practices.
|top of section I| |table of contents|II. Background
New York´s Medicaid population is both culturally and clinically diverse, with varied and sometimes complex clinical care needs ranging from preventive care for children and adults, perinatal care, long term care, chronic care including HIV/AIDS management, behavioral health care, and assistance with activities of daily living for the elderly and developmentally disabled. Medicaid enrollees include foster children, a significant population of homeless individuals, individuals with serious and chronic substance use disorder, those with serious and persistent mental illness, and those with intellectual and developmental disabilities. Many of these individuals have co–occurring health conditions. The management of services for NYS Medicaid recipients has traditionally been handled across several different state agencies, including: NYS DOH, OASAS, OMH, and OPWDD. Each agency provides specialized services for individuals meeting certain eligibility criteria, based on need. Historically, services were billed for on a fee– for–service basis.
With the approval of the Partnership Plan Demonstration in 1997, the NYS DOH began mandatory enrollment of Medicaid recipients in need of acute care health services into traditional MMC plans. Initially, mandatory enrollment was limited to the Temporary Assistance for Needy Families (TANF) and Safety Net Populations. Individuals with special needs and those qualifying for the specialized services outside of the traditional benefit package, including those living with HIV/AIDS, were exempt from mandatory enrollment.
In 2001, the FHP Program was implemented, providing comprehensive health coverage to low– income uninsured adults, with and without children. Coverage of these services was delivered through the MMC model and qualifying individuals were mandatorily enrolled. In 2005, the Federal–State Health Reform (F–SHRP) Demonstration was approved. Operating separately but complementary to the Partnership Plan, the F–SHRP Demonstration provided additional financial and regulatory support for health reform in NYS while introducing a requirement that most mandatory and optional state plan populations in 14 counties enroll in a managed care organization (MCO). Subsequently, the state continued to increase the number of counties with a mandatory enrollment requirement. As additional populations were required to enroll, all counties participating under the mandatory enrollment rule were subject to the expansion.
In 2006, the NYS DOH began mandatory enrollment of all aged and disabled adults and children (Supplemental Security Income (SSI) eligible) into MMC. In 2011, enrollees with HIV/AIDS were no longer exempt from the program and were mandatorily enrolled in their choice of a HIV/AIDS Special Needs Plan (SNP) or a "Mainstream" (traditional) plan. In 2012, the NYS DOH began to mandatorily enroll dual eligible recipients in need of community–based long–term care services into MLTC plans.
With CMS approval of Partnership Plan and F–SHRP amendments in April 2013, NYS DOH– regulated managed care organizations began designing a system to provide long–term supports and services to the developmentally disabled (DD) population through a benefit package that included services from the OPWDD, NYS DOH´s MLTC program, and behavioral health services through NYS OMH. The transition of developmental disability services into a formalized managed care framework is being realized through a pending Home and Community Based Service (HCBS) waiver between OPWDD and CMS: the People First Waiver. New managed care organizations known as DISCOs will provide holistic, person–centered care planning, and delivery of coordinated supports and services, under the expertise of the current OPWDD service provider community. DISCOs will provide day habilitation, residential–based services and other long–term support services, as well as important clinic and therapy services. Individuals who are dually eligible for Medicare and Medicaid and in need of disability services will be able to enroll in a new plan type called Fully Integrated Duals Advantage for Persons with Intellectual and other Developmental Disabilities (FIDA–IID).
Many of the recent improvements to the Medicaid program can be largely credited to the work of the MRT. Created by Governor Cuomo under an amendment to the Partnership Plan in 2011, the MRT consists of provider, payer, and consumer stakeholders working together to address underlying cost and health care quality in NYS. As a result of their recommendations, several additional plans and populations have been transitioned into a managed care program, including the approximately 100,000 enrollees who were nursing home eligible and in need of more than 120 days of community–based long–term care services into MLTC plans that provide community– based long–term care services.
The MRT also recommended integration of specialty behavioral health services into mainstream Medicaid managed care plans, and the development of new product lines, including special needs Health and Recovery Plans (HARPS), and Fully–Integrated Duals Advantage (FIDA) plans. In 2015, CMS approved a waiver to the Partnership Plan allowing for the integration of behavioral health services into managed care. Under this waiver, behavioral health services were carved into mainstream MCOs and HIV SNPs, and special needs HARPs were created. HARPs are a distinctly qualified, specialized, and integrated managed care product for adults meeting the serious mental illness (SMI) and Substance Use Disorder (SUD) targeting criteria and risk factors. These specialized managed care product lines provide services under the oversight of the state agency specializing in the special needs of the applicable population. In addition to all Medicaid behavioral health and physical health benefits, HARP enrolled individuals who meet specific targeting, risk factor, and functional criteria are offered access to Home and Community Based Services (HCBS). These services are designed to provide support to participants in community–based settings. HARP eligible individuals who are enrolled in HIV SNPs and meet eligibility criteria will also have access to HCBS.
The paramount success of the MRT in New York State not only transformed healthcare delivery for millions of New Yorkers, it also resulted in over $8 billion in federal savings. A 2014 amendment to the Partnership Plan allows the state to reinvest those savings into activities aimed to further transform NYS´s health care delivery system, increasing quality while stabilizing the system and driving down cost, and ensuring access to quality care for all Medicaid members. The waiver amendment dollars are being reinvested over a five–year period, addressing critical issues throughout the state and allowing for comprehensive reform. In addition, the special terms and conditions commit the state to comprehensive payment reform, continuing New York´s effort to effectively manage its Medicaid program within the confines of the Medicaid Global Spending Cap.
Enrollment in MMC currently exceeds 4.5 million people. All 62 counties in NYS, including the five counties that make up New York City, have implemented mandatory enrollment for some type of Medicaid managed care program.
The NYS DOH is now sharing the responsibility with other state agencies for managed care plan oversight. Though inclusive of all managed care programs in NYS, this quality strategy is complemented by one maintained by OPWDD, pursuant to their People First Waiver. OPWDD´s quality strategy for the developmentally disabled population incorporates the needs and demands of the changing developmental disability landscape, while building upon New York State´s Quality Strategy for the Medicaid Managed Care Program so that quality oversight of DISCOs are tailored to the unique needs of this population. The OMH and OASAS quality strategy, will allow for quality oversight that is based on values that address person–centered care, recovery– oriented services and cultures, integrated care, data–driven quality improvement, and evidence–based practices. Research has noted that, compared to measures for general health, there are relatively few behavioral health metrics; and within behavioral health, there are even fewer SUD specific measures.
Effective and efficient quality assurance, oversight, and improvement depends on the efforts of each state agency, internally and cross–agency, in the management of unique needs of the populations served. New York has developed and implemented rigorous standards for plan participation to ensure that NYS health plans have networks and quality management programs necessary to adequately serve all enrolled populations. The NYS DOH performs periodic reviews of the Quality Strategy to determine the need for revision and to assure managed care organizations (MCOs) are in contract compliance and have committed adequate resources to perform internal monitoring and ongoing quality improvement. The Quality Strategy is updated regularly to reflect the maturing of the quality measurement systems for new plan types, as well as new plans and populations that may be developed in the future. Examples of results of analyses and evaluations are described throughout this document.
|top of section II| |table of contents|III. Managed Care Program Objectives
Data collected since 1993 demonstrate that Medicaid beneficiaries enrolled in managed care plans receive better quality care than those in fee–for–service Medicaid. Studies of those who have voluntarily enrolled in managed care and other evaluations have repeatedly shown a steady improvement in quality of care and a dramatic improvement in chronic care disease management for those in Medicaid managed care plans.
The following lists some objectives of the Medicaid managed care program. Through these objectives, the program seeks to improve health care services and population health and reduce costs consistent with the MRT and CMS´ Triple Aim objectives.
Program Initiative Objectives:
- Create and sustain an integrated, high performing health care delivery system that can effectively and efficiently meet the needs of Medicaid beneficiaries and low income uninsured individuals in their local communities by improving care, improving health and reducing costs.
- Continue to expand on the assessment, measurement, and improvement activities for all existing managed care plans while incorporating new managed care plans as they become operational, including HARPs, FIDA–IIDs, and DISCOs.
- Demonstrate an increase of at least 5 percentage points in the statewide rate of diabetics who received all four required tests for the monitoring of diabetes.
- Decrease the prevalence of self–identified smokers on the Consumer Assessment Health Care Provider Systems (CAHPS®) survey.
- Increase the measurement, reporting and improvement initiatives associated with preventable events such as Prevention Quality Indicators (PQIs), potentially preventable readmissions (PPRs) and emergency department use for preventive care (PPVs).
- Increase measurement in behavioral health by developing and implementing a more robust measurement set and incorporating expanded populations such as Health Homes into the Quality Assurance Reporting Requirements (QARR) measurement.
- Continue to publish data by race and ethnicity, as well as aid category, age, gender, special needs, and region in order to develop meaningful objectives for improvement in preventive and chronic care. Engage the plans in new ways to improve care by focusing on specific populations whose rates of performance are below the statewide average.
- Decrease any disparity in health outcomes between the Medicaid and commercial populations.
- Expand access to managed long–term care for Medicaid enrollees who are in need of long term services and supports (LTSS).
- Increase MLTC measurement with the implementation of HEDIS®/QARR reporting on fully capitated plans and the development of additional measures using UAS–NY data.
- Decrease the percentage of MLTC enrollees who experienced daily pain from 52 percent to 45 percent.
- Decrease the percentage of MLTC enrollees who had one or more falls so that no plan has a rate above 20 percent.
- Identify and reduce disparities in access and outcomes for individuals with serious behavioral health conditions (individuals enrolled in HARPs).
- Increase provider implementation of evidence–based practices that integrate behavioral and physical health services, including addiction pharmacotherapy.
- Improve care coordination for individuals with complex behavioral and physical health needs
These objectives are designed for the benefit of the entire Medicaid population of NYS and thus encompass all managed care plan types. As specialized managed care plans develop and operationalize, additional managed care objectives need to be considered. Traditional managed care techniques have the potential to facilitate higher quality cost effective services for people with special needs. But this will be the case only if service delivery policies are well designed, effectively implemented, tailored to the unique interests, needs, and challenges of the population, and achieve cost savings by improving outcomes and eliminating inefficiencies, not by reducing the quality or availability of services.
According to the National Council on Disabilities´ March 18, 2013 report titled "Medicaid Managed Care for People with Disabilities: Policy and Implementation Considerations for State and Federal Policymakers", a state´s quality management strategy must be capable of:
- Continuously monitoring the performance of all managed care contractors and subcontractors and ensuring that prompt remedial actions are taken when deficiencies are identified;
- Reporting, tracking, investigating, and analyzing incident patterns and trends in order to pinpoint and promptly remediate threats to health and safety of managed care beneficiaries; and
- Assessing the quality of services and supports provided on an individualized basis using valid and reliable clinical and quality of life measures and preparing and issuing periodic statistical reports on personal outcomes and system performance, analyzing trends, and managing quality improvement initiatives.
The performance measures identified in this quality strategy are designed to accomplish these vital aspects of the quality management. The design and operation of a specialized managed care system for people with intellectual and developmental disabilities poses unique challenges. People with intellectual and developmental disabilities often have complex, multi–dimensional, and highly diverse needs, and NYS recognizes that a medical model of care is not sufficient and that a person–centered model is needed that builds upon advances and quality of life for these individuals.
OPWDD´s quality strategy for DISCOs is available on the OPWDD website: http://www.opwdd.ny.gov/transformation–agreement/quality–strategy–october–2013.
The OPWDD quality strategy will be updated to reflect state–federal agreements related to managed care and the People First waiver and will be made available on the NYS DOH MRT website upon approval. The strategy sets out to build upon a foundation of core principles that promote independence, community inclusion, self–determination, and productivity. As people with developmental disabilities are further integrated into managed care, OPWDD will continue to enhance the focus of quality oversight to how well individuals are progressing toward their personal goals, how satisfied individuals and families are with the services received, how well DISCOs are promoting quality outcomes and quality improvement within their provider networks, and using data related to these measures to effect individual, provider, DISCO, and system improvements.
Specific objectives of managed care for people with intellectual and developmental disabilities relate to:
- Making the system more person centered ––supports and services that match each person´s unique identified interests and needs, including opportunities for self–direction,
- Serving people in the most integrated settings possible,
- Provision of better integrated, holistic planning and supports to individuals, and
- Measuring quality based on individualized outcomes.
The quality strategy being developed by OMH and OASAS will focus on behavioral health populations and services managed by qualified mainstream plans, HARPs, and HIV SNPs. This quality strategy will use a data–driven approach to monitor requirements, including behavioral health network adequacy, and behavioral health– specific reporting requirements for utilization management, quality management, and financial management, as well as administrative and clinical performance metrics. The recovery focus will promote "a process of change through which individuals improve their health and wellness, live a self– directed life, and strive to reach their full potential" (SAMHSA Definition of Recovery 02/12). Performance metrics will reflect this recovery focus and therefore include indicators beyond those related to acute care.
|top of section III| |table of contents|IV. Approach
To achieve the overall objectives of MMC and to ensure the highest quality health care among Medicaid recipients in NYS, the NYS Quality Strategy focuses on measurement and assessment, improvement, redesign, contract compliance and oversight, and enforcement as described below.
Through these activities, the state complies with CFR 438.204, Elements of State Quality Strategies, by detailing:
- The MCO and Prepaid Inpatient Health Plan (PIHP) contract provisions that incorporate the standards specified in this subpart.
- Procedures that:
- Assess the quality and appropriateness of care and services furnished to all Medicaid enrollees under the MCO and PIHP contracts, and to individuals with special health care needs.
- Identify the race, ethnicity, and primary language spoken of each Medicaid enrollee. States must provide this information to the MCO and PIHP for each Medicaid enrollee at the time of enrollment.
- Regularly monitor and evaluate the MCO and PIHP compliance with the standards.
- National performance measures and levels that may be identified and developed by CMS in consultation with States and other relevant stakeholders.
- Arrangements for annual, external independent reviews of the quality outcomes and timeliness of, and access to, the services covered under each MCO and PIHP contract.
- Appropriate use of intermediate sanctions.
- An information system that supports initial and ongoing operation and review of the State´s quality strategy.
- Standards for access to care, structure and operations, and quality measurement and improvement.
1. Measurement and Assessment
Demonstrating success and identifying challenges in meeting objectives of managed care are based on data that reflects:
- Health plan quality performance,
- Access to covered services,
- Extent and impact of care management,
- Use of person–centered care planning (DISCO specific), and
- Enrollee satisfaction with care.
The NYS DOH has developed several systems to collect data from MCOs. MCOs are required to have information systems capable of collecting, analyzing, and submitting the required data and reports. Focused clinical studies and Performance Improvement Projects (PIPs) additionally capture quality of care information for specific populations and diseases.
To ensure the accuracy, integrity, reliability, and validity of the data submitted, the state contracts with an External Quality Review Organization (EQRO). The EQRO audits data submissions and provides technical assistance to MCOs in collecting and submitting requested information.
DISCOs will be the primary entity for quality reporting on managed care for people with intellectual and developmental disabilities. Each DISCO will be required to measure and report its performance to NYS annually, using standardized measures that incorporate the requirements of § 438.204(c) and 438.240(a)(2).
Quality assurance for HARPs will be monitored in two ways. NYS DOH´s QARR measures will be reported both overall and for individuals in HARPs so that any disparities in plan performance for individuals in HARPs compared to performance overall can be identified. In addition, HARPs have a quality assurance program that is separate and distinct from the traditional MCO quality assurance program. It must meet all requirements and conditions of the 1115 Partnership Plan. In addition to QARR, new required recovery outcome measures in areas such as employment, housing, criminal justice status, and functional status will be reported. These recovery outcome measures will be derived from the interRAI Community Mental Health Assessment eligibility screenings for Home and Community Based Services, ongoing re–evaluations, and consumer self–reports.
Measures used to evaluate quality performance in NYS are largely based on The National Committee for Quality Assurance´s (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS), the Medicaid Encounter Data System (MEDS), PQIs– measures developed by the Agency for Healthcare Research and Quality (AHRQ), the Uniform Assessment System for New York (UAS–NY), the National Core Indicators Survey (NCI), and consumer satisfaction surveys including the CAHPS survey. In addition to national measures obtained from these sources, NYS has expanded its evaluation of managed care objectives to include state–specific measures. The QARR quality measurement set and other data sources used for assessment of the managed care delivery system in NYS are described below.
a) QARR Measurement Set
NYS DOH staff developed the QARR in 1993 to monitor quality in managed care plans. QARR consists of 74 measures from the NCQA´s HEDIS®, CAHPS®, and New York State–specific measures.
QARR focuses on health outcome and process measures, and includes clinical data relating to prenatal care, preventive care, acute and chronic illnesses, and mental health and substance abuse for children and adults in Medicaid/CHIP.
The major areas of performance included in QARR are:
- Effectiveness of Care
- Access to/Availability of Care
- Satisfaction with the Experience of Care
- Use of Services
- Health Plan Descriptive Information
- NYS–specific measures: (HIV/AIDS Comprehensive Care, Adolescent Preventive Care, and Prenatal Care measures from the Live Birth file).
All measures address health care needs of traditional MMC, Medicaid MLTC, and special needs populations (SNP). Applicable measures are rotated largely following the HEDIS rotation schedule. A list of the QARR measurements collected by NYS can be seen in appendix (3).
QARR is submitted annually, in June of the year following the measurement year and published in web–based formats.
b) Encounter Data
All MCOs are required to submit monthly encounter data to the MEDS. MEDS is consistent with national standards for a national uniform core data set. MEDS data provide a source of comparative information for MCOs and are used for purposes such as monitoring service utilization, evaluating access and continuity of service issues, monitoring and developing quality and performance indicators, studying special populations and priority areas, applying risk adjustment, and setting capitation rates. OMH and OASAS will also collaborate with DOH to monitor the timeliness and completion of encounter data submissions.
c) Data on Race, Ethnicity and Primary Language
New York Medicaid obtains race, ethnicity, and primary language spoken from several sources: the eligibility system, the enrollment form completed by the recipient, and the enrollee health assessment form mailed to new enrollees by both the social services district and the MCO. Completed enrollment forms are forwarded to the MCO. MCOs are now required to submit member–level QARR and CAHPS® (satisfaction) data to the NYS DOH which enables the calculation of QARR rates by demographic characteristics including race/ethnicity and Medicaid aid category.
These demographic level reports allow further evaluation of the quality of care received by populations of significant and or discrepant healthcare needs, including Safety Net and SSI populations. The most recent report is available here.
d) Uniform Assessment System– New York
In October 2013, the NYS DOH began requiring all MLTCs to use the newly developed UAS–NY. The UAS–NY is an interRAI tool that standardizes and automates needs assessments for home and community–based programs in New York. InterRAI is a collaborative network of researchers in over 30 countries committed to improving health care for persons who are elderly, frail, or disabled. Their goal is to promote evidence–based clinical practice and policy decisions through the collection and interpretation of high quality data. The interRAI organization and its assessment tools are used in many states as well as Canada and other countries.
The UAS–NY system establishes a single, unique medical record for all enrollees of the state´s Medicaid home and community–based long–term care network, further enabling comprehensive assessments. Additionally, the UAS–NY facilitates access to programs and services, eliminates duplicative assessment data, and improves consistency in the assessment process. Fragmentation in the delivery of long term care services will be addressed by the standardized assessment of functional and other needs through an empirically tested and validated means.
The UAS–NY system will also contain the interRAI Community Mental Health Assessment being used to determine HCBS eligibility and HCBS plans of care for HARPs and HARP eligible individuals enrolled in HIV SNPs.
e) Member Satisfaction Surveys
The state conducts an annual CAHPS® survey with a certified CAHPS® vendor, under arrangement by the state´s EQRO. With the EQRO, NYS DOH has also conducted several other surveys focused on specific populations such as enrollees with diabetes or SSI recipients who were mandatorily enrolled for the first time.
Enrollees of the MLTC plans were surveyed in 2007, 2011 and 2013. A new enrollee survey is currently being administered in New York City to determine the satisfaction levels of individuals who were enrolled mandatorily in MLTC. Questions focus on their satisfaction with managed care versus fee–for–service.
These surveys allow the NYS DOH to evaluate the enrollees´ perceptions of quality, access, and timeliness of health care services. Because the results are presented by plan, comparisons to the statewide average are possible, and plans can be held accountable for performance. Plans whose results are meaningfully and statistically below acceptable thresholds may be required to develop a corrective action plan that NYS DOH staff will review and monitor. The results of the surveys are made available to Medicaid recipients to assist them in the process of selecting an appropriate MCO.
HARP members will be surveyed annually to measure perception of care and quality of life outcomes. Data from this survey will allow the State and plans to monitor HARP members´ perception of services and how their behavioral health services affect different areas of their life. Specific survey domains include Perception of Outcomes, Daily Functioning, Access to Services, Appropriateness of Services, Social Connectedness, and Quality of Life. Items addressing family relationship functioning and education of family members are included. Findings will be reported at the survey domain and item level for each plan. Demographics will be collected, which will allow HARPS to monitor disparities.
f) Prevention Quality Indicators
The PQIs are a set of measures developed by the AHRQ used to identify ambulatory care sensitive conditions. These are conditions for which good outpatient care can potentially prevent the need for hospitalizations, or for which early intervention and treatment would prevent complications or severe disease. While the hospital admission is used to identify the PQI, the PQIs can be used to flag problems in the health care system outside the hospital. The NYS DOH calculates and provides PQI data to MMC plans on a yearly basis as part of a quality improvement activity described later
g) MLTC Specific Performance Measurement
Following biannual submission of UAS–NY data, the NYS DOH creates summary reports containing descriptive information about members´ status. The quality performance component of these reports is divided into two sections: 1) Current plan performance– Functional status and rates of performance based on the current submission and 2) Performance over time - Changes in the functional status of the MLTC population over a 6 to 12–month period. One of the primary objectives of long–term care is to improve or stabilize functional status, with stabilization being the most likely outcome for this population. For this reason, positive outcomes for most items are defined as either a member showing improvement over the measurement period or maintaining his/her initial level of functioning/ symptoms. Domains of measurement include:
- Activities of Daily Living
- Quality of Life
- Effectiveness of Care
- Emergent Care
- Utilization and Patient Safety
A complete list of these performance measures can be seen in Appendix 4.
h) DISCO Specific Performance Measurement
A subset of performance measures specific to the special needs of individuals with intellectual and developmental disabilities will be incorporated into the Quality Management and Improvement Strategy for the New York State Office for People with Developmental Disabilities. Established by OPWDD, the DISCO specific performance measures address the following quality domain areas:
- Personal Outcome Measures– Assess the degree to which the DISCO´s care coordination and supports provided are contributing to individual outcome achievement.
- Individual Outcome Measures– Clinical and Functional Outcome Measures derived from the OPWDD Needs Assessment Tool, based upon the InterRAI Consolidated Assessment System.
- OPWDD System Reform Measures– Benchmark the state´s progress toward the developmental disabilities transformation milestones, as they relate to: deinstitutionalization, access to community–based services, self– direction, accessible housing, appropriate supports, and employment opportunities.
- 1915 C Waver Assurance Measures– Assess compliance with HCBS waiver assurances in accordance with CMS´s evidentiary approach to quality reviews.
- National Core Indicators (NCI) – Measures performance of New York State´s developmental disability system at the system´s level and enables comparisons between New York State´s system and other state developmental disability systems.
- Other Structural/Process Measures
The National Core Indicator Survey was launched as a joint venture, by the National Association of State Directors of Developmental Disabilities Services (NASDDDs) and the Human Services Research Institute (HSRI) in 1997. NCI is a common set of data collection protocols that gathers information about the outcomes of state service delivery systems for people with intellectual and developmental disabilities.
New York State will continue to conduct the annual NCI Survey for people with intellectual and developmental disabilities through OPWDD. The Consumer Survey consists of indicators in the following domains: Home, Employment, Health and Safety, Choice, Community Participation, Relationships, Rights, and Individual Satisfaction.
A complete list of these performance measures can be seen in Appendix 5.
i) Behavioral Health Specific Performance Measurement
The quality strategy for behavioral health maintained by OMH and OASAS includes measures specific to behavioral health services in mainstream managed care plans as well as to HARPs. In addition to examination of consumer satisfaction survey results in the behavioral health population, the following elements will be addressed:
- Claims and Encounter Based Measures – These measures will be reported for both MCOs and HARPs. Measures under review such as behavioral health readmission; continuity and engagement in aftercare following discharge from mental health inpatient and SUD crisis (detox) and inpatient programs; Screening, Brief Intervention and Referral to Treatment (SBIRT) screening; continuity of care for SUD; and medication– assisted treatment for SUD.
Additionally, OMH and OASAS have developed templates for utilization monitoring reports that will serve as an adjunct to the utilization monitoring done by DOH. These reports will show utilization of services, cost, and encounter volume by behavioral health service. Reports will be done at the plan level. This monitoring will allow OMH and OASAS to determine if services are being provided at an appropriate volume. It is important that the transition of behavioral health services into managed care does not disrupt members´ treatment. These reports will also allow the State to monitor utilization of the new HCBS services.
- Recovery Focused Measures – These measures will be reported for HARPs and HARP eligible individuals in HIV SNPs only and will lead to a better understanding of the plan´s impact on members´ quality of life by examining outcomes such as employment, housing, and social connectedness. HCBS eligibility assessments will serve as the data source for these measures. HCBS assessments will be conducted upon enrollment in the HARP and annually thereafter. Measures will initially be reported as the prevalence of a certain characteristic, such as the percentage of members who are homeless. Eventually measures that look at maintenance of a positive outcome or improvement in outcomes will be reported.
Measure domains will be: employment, education, housing, criminal justice, social connectedness (including assessment of family engagement), self– help group participation, and substance use. Prevalence and outcome metrics will address each of these measure domains.
The interRAI Community Mental Health Assessment includes demographic items that assess gender identity, sexual orientation, religion, race/ethnicity, and preferred language. These items include detailed lists of response options. Prevalence and outcome metrics will be stratified by each demographic in order to identify any disparities. The results of disparity analysis will be shared with plans. Quality improvement efforts will be designed to eliminate identified disparities.
- Transition Monitoring – To help monitor the transition of behavioral health services into managed care, plans will be required to report data related to denials and provider contracting to OMH and OASAS on a regular basis, which will be supplemented by OMH and OASAS with data available to the agencies. These reports will allow OMH and OASAS to assess the impact of the managed care transition on plan members´ access to services. Monitoring of inpatient medically necessary denials during the transition will allow the OMH and OASAS to address related issues expediently. As behavioral health services including new HCBS are brought into managed care, OMH and OASAS will monitor Plan´s behavioral health networks to ensure that standards for choice and access are met. OMH and OASAS will also use administrative data to monitor timeliness of payment to behavioral health providers. A complete list of these performance measures can be seen in Appendix 6.
2. Improvement
Quality Improvement is a continuous process and refers to an organization´s or system´s capacity to improve performance and accountability by systematically collecting and analyzing data and information. Based on the assessments of quality and appropriateness of care, contract compliance, and MCO monitoring activities, the state targets improvement efforts through a number of interventions as described below.
a) Focused Clinical Studies
Focused clinical studies, conducted by the EQRO, usually involve medical record review, surveys, or focus groups. MCOs are required to conduct two or three focused clinical studies a year. With the inclusion of behavioral health services into MCOs and the establishment of HARPs, the NYS DOH will incorporate behavioral health services and HARP populations into the focused clinical studies.
Recommendations for improvement are offered to NYS DOH, plans, and providers. Studies concerning the reduction of falls, the provision of advanced directives, and the administration of flu shots for the MLTC plans, have been conducted as well.
Focused studies are also used to determine whether MLTC plans are conducting timely assessments and maintaining level of services as required by the special terms and conditions of the 1115 waiver.
b) Performance Improvement Projects
Mainstream Medicaid managed care plans are required to conduct one PIP annually using a report template that reflects CMS requirements for a PIP. With the inclusion of behavioral health services into the MCOs and the establishment of HARPs, the NYS DOH will work with the plans and its EQRO to incorporate behavioral health services and HARP populations into the PIPs. The NYS DOH and the EQRO support these collaborative efforts. In the past, each plan has chosen a topic, and with the technical assistance from the EQRO, developed a study methodology and conducted interventions to reach their improvement goals. Recently however, the NYS DOH has encouraged plans to participate in collaborative studies through collaborations with network hospitals across the state.
Study processes and results are presented in final reports due 18 months after each study begins. Conferences are held upon completion of collaborative PIP projects, in which participating health plans are brought together to discuss lessons learned and describe individual experiences with these quality improvement projects.
From 2009–2010, 18 plans worked with NYS DOH and the EQRO to improve the prevention of childhood obesity. From 2011–2012, ten plans worked on addressing potentially preventable hospital readmissions, and six plans worked to reduce disparities in asthma care by partnering with health care practices in Central Brooklyn. Currently, health plans are collaborating on PIPs targeting prevention of chronic diseases. Diabetes management and prevention, hypertension control, and smoking cessation were all topics addressed in the 2013–2014 PIP. A grant titled, Medicaid Incentives for the Prevention of Chronic Disease (MIPCD), was a component of the 2013– 2014 PIP, partnering New York alongside ten other states to determine the effect of offering financial incentives as a means of engaging recipients in preventive health services. Smoking cessation work continues in the 2015–2016 PIP, with a concentration on increasing the utilization of smoking cessation benefits.
MLTC plans also conduct PIPs on a yearly basis. MLTC PIPs focus on clinical and non– clinical areas consistent with the requirements of 42 CFR 438.240 of the Medicaid model contract. One priority project is chosen each year and approved by the Department. PIP topics for 2015 include:
- Depression Management
- Pain Management/Palliative Care
- Falls
- Advanced Directives
- Emergency Preparedness
- Preventive Screenings–Eye, Ear and Dental Exams
MLTC PIPs continue to strive to improve the health and health care of the aged and disabled adult populations. Interventions in past PIPs have included: increased utilization of health informatics in care management and health assessment, increased care coordination, development of multidisciplinary teams to address PIPs within the health plan, increased home care visits; and member, provider, and care manager education through classes and the creation of education materials.
As individuals with intellectual and developmental disabilities are transitioned into managed care, DISCOs will also be required to conduct performance improvement projects that focus on clinical and non–clinical areas consistent with the requirements of 42 CFR 438.240 and CMS and NYS protocol. The purpose of these studies will be to promote quality improvement within health and member outcomes and enrollee satisfaction. At least one (1) PIP each year will be required.
The EQRO will validate the DISCO´s data and methodology for required performance improvement projects.
c) Pay for Performance – Quality Incentive
In 2002, the NYS DOH began rewarding plans that have superior performance by adding up to three percent to plan per member, per month premiums. This Quality Incentive (QI) program uses a standardized algorithm to awards points to health plans for high quality in the categories of: Effectiveness of Care, Access and Availability, and Use of Services. Points are deducted for any Statements of Deficiency (SOD) issued for lack of compliance with managed care requirements. Assessments of quality and satisfaction are derived from HEDIS measures in NYS´s QARR, satisfaction data from CAHPS®, and PQIs.
For HARPs, a modified quality incentive program will be phased in during the first four years of operation. A gradually increasing premium withhold will be used to create a pool for quality incentives determined by OMH and OASAS.
d) PQI Improvement
Each year, the NYS DOH sends plan–specific adult and pediatric PQI reports to health plans. These reports also include enrollee characteristics and PQI rates by hospital. Also included are the PQI statewide rates by hospital. Health plans with a PQI rate higher than the statewide average are required to respond to NYS DOH with a root–cause analysis and action plan. Quality Improvement plan managers at the Office of Quality and Patient Safety (OQPS) oversee the response process and offer guidance on best practices to improve PQI measured performance.
e) Quality Performance Matrix
In order to monitor health plan performance on quality measures, a quality performance matrix was developed and implemented in 1998. The matrix approach provides a framework for benchmarking performance and helps plans prioritize quality improvement planning. The matrix gives a multi–dimensional view of plan performance by comparing rates for selected measures in two ways: 1) by percentile rank among other plans, and 2) trend over two years. The result, as shown in Figure 1, is a 3x3 table where measures are displayed in cells corresponding to a letter grade ranging from A (best performance) to F (worst performance).
Plans are instructed to conduct root–cause analysis and action plan for measures where there is poor performance based on the barriers identified. The action plans are reviewed and approved by OQPS staff and are monitored throughout the year to assure that they are being conducted and evaluated for effectiveness in improving performance.
Figure 1: The Quality Performance Matrix
| Percentile | ||||
|---|---|---|---|---|
| 0 < 50% | 50% < 90% | 90% – 100% | ||
| Trend | ↑ | C | B | A |
| 0 | D | C | B | |
| ↓ | F | D | C | |
| A Performance is notable. No action plan required B, C No action plan required D, F Root cause analysis and action plan required |
||||
f) Publication of Quality Performance Reports
Reports on Medicaid quality performance, patient satisfaction, health plan comparisons, enrollment, quality improvement initiatives, and research results are made available online here.
These easy–to–read reports are designed to help members choose a health plan that meets their needs and the needs of their families, and to inform stakeholders. Data is provided for commercial and government–sponsored managed care. Enrollment reports show the level of consumer participation in various types of managed care plans. Published reports also include results from External Quality Review of the MMC program. Appendix 7, "Published Journal Articles – New York State DOH," presents a bibliography of peer review journal articles published on health plan quality performance.
g) Quality Improvement Conferences and Trainings
NYS DOH is committed to providing MMC plans with tools to conduct successful quality improvement initiatives. One successful approach has been the sharing of other plan experiences in best practice forums. NYS DOH, in collaboration with its EQRO, has conducted conferences on immunization strategies, partnering for quality improvement, understanding CAHPS® (consumer survey) results, adolescent preventive care, physician profiling, ADHD, childhood obesity, asthma, diabetes, and prenatal care. Conferences are also held upon completion of PIPs. Evaluation feedback is always sought, and comments are used when planning future events. The NYS DOH has met with MCOs and other stakeholders to address regional disparities in QARR performance measures.
h) Plan Manager Technical Assistance
Each plan is assigned a plan manager in both the Office of Health Insurance Programs (OHIP) and OQPS. The plan managers act as liaisons with the NYS DOH and managed care plan staff on all issues of quality performance and MCO monitoring. They provide technical assistance to plan staff as they develop their root–cause analyses and action plans in response to the Quality Performance Matrix and PQI measures. They prepare a plan´s Quality Profile for the area office staff prior to their conducting an on–site Comprehensive Operational survey. They also consult with plans concerning their PIPs.
i) DISCO Quality Improvement
For quality improvement in the managed care of people with intellectual and developmental disabilities, OPWDD will use its existing transformation/quality improvement infrastructure that permeates leadership, management, and regional office staff from all divisions. This construct establishes a series of committees that interface, and creates a framework to develop, monitor and revise transformation and quality improvement initiatives throughout the developmental disability service system in New York State. The OPWDD leadership team provides vision and strategic direction for quality management and prioritizes these system improvement activities. This arrangement results in continuous quality improvement across the OPWDD enterprise and the larger developmental disability service system. Ultimately, the OPWDD leadership team prioritizes all agency system improvement activities and is responsible for strategic implementation. The OPWDD leadership team is advised by the Commissioner´s DD Advisory Council established by NYS Mental Hygiene Law (13.05) and comprised of self–advocates, family members, provider representatives, and other stakeholders, and an array of other internal and external stakeholders that represent various constituencies, including the OPWDD Provider Associations; the Self Advocacy Association of New York State; the Statewide Committee for Family Support Services; and many others.
|top of section 2| |top of section IV| |table of contents|3. Delivery System Transformation
An amendment to the Partnership Plan in April of 2014 allowed for the creation of the Delivery System Reform Incentive Payment (DSRIP) program. Its purpose is to provide incentives for Medicaid providers to create and sustain an integrated, high performing health care delivery system that can meet the needs of Medicaid beneficiaries and low income uninsured individuals by improving care, improving health and reducing costs. Broad goals of DSRIP are to:
- Transform the health care safety net at the system and state levels,
- Reduce avoidable hospital use,
- Make improvements in measures of health and public health, and
- Sustain delivery system transformation through managed care payment reform.
Complimentary to existing and routine quality improvement projects previously described, networks of providers will work as unified entities called Performing Provider Systems (PPS), to achieve these goals from within their own practice communities. Each PPS will work to ensure community needs are being met throughout the transformation process, with evidence–based projects addressing or assuming:
- Appropriate infrastructure,
- Integration across settings,
- Responsibility for a defined population,
- Procedures to reduce avoidable hospital use, and
- Managed care contracting reform.
Incentive distribution is based on a PPS meeting the milestones defined. Authority for operations and funding is authorized under renewal of the overall Partnership Plan demonstration, and contingent on satisfactory initial implementation, which includes the state meeting overall milestones. The amendment provides near term financial support for vital safety net providers at risk of closure.
|top of section 3| |top of section IV| |table of contents|4. Contract Compliance and Oversight
As required by CFR 438.204(g) the state must establish standards for MCO/PIHP contracts regarding access to care, structure, operations, and quality measurement and improvement. NYS´s Medicaid model contract systematically addresses how these standards are achieved. Corresponding with CFR components 438.204 – 438.242 the contract details: availability of services, assurances of adequate capacity and services, coordination and continuity of care, coverage and authorization of services, provider selection, enrollee information, confidentiality, enrollment and disenrollment, grievance systems, sub contractual relationships, practice guidelines, quality assessment and performance improvement, and health information systems.
The table in Appendix 1 outlines each required component of the federal regulations and identifies the section of the model contract and/or operational protocol where this requirement is addressed (see Appendix 1 – Contract Compliance of MCOs/PIHPs). New York State´s Operational Protocol for The Partnership Plan is in the process of being updated. If there appears to be a conflict in policy, the model contract and applicable federal or state laws/regulations take precedent. At this time, the OPWDD has not yet finalized its model contract for DISCOs. The model contracts for the behavioral health integration into MCOs and the HARPs will be in place by the implementation date.
New York ensures compliance with the quality strategy by requiring MCOs to have internal quality assurance programs and by monitoring MCO performance. To participate in Medicaid managed care, MCOs must have the structures and processes in place to assure quality performance. Minimum, required components of the MCO´s Quality Assurance Plan (QAP) are listed in Appendix 2. MCO QAPs are reviewed, along with documentation of the activities and studies undertaken as part of the QAP, during both the certification process and pre–contract operational review. (See Appendix 2 – Internal Quality Assurance Plan and 2a – Credentialing Criteria – Recommended Guidelines).
Under §1915(c) of the Social Security Act and 42 CFR §441.302, the approval of an HCBS waiver requires that CMS determine that the state has made satisfactory assurances concerning the protection of participant health and welfare, financial accountability, and other elements of waiver operations. Specific assurances include:
- Participants enrolled in the HCBS waiver meet the level of care criteria consistent with those residing in institutions;
- A person´s needs and preferences are assessed and reflected in a person– centered service plan;
- Agencies and workers providing services are qualified;
- Participants are protected from abuse, neglect and exploitation and get help when things go wrong, or bad things happen;
- The state Medicaid Agency pays only for services that are approved and provided, the cost of which does not exceed the cost of a nursing facility or institutional care on a per person or aggregate basis (as determined by the state); and
- The state Medicaid Agency is fully accountable for HCBS waiver design, operations and performance.
Renewal of an existing waiver is contingent upon review by CMS and a finding by CMS that the assurances have been met. In completing the HCBS waiver application, the state specifies how it has designed the waiver´s critical processes, structures, and operational features in order to meet these assurances.
The Quality Management and Improvement Strategy for the New York State OPWDD demonstrates compliance with these assurances by delineating:
- The evidence–based discovery activities that will be conducted for each of the six major waiver assurances.
- The remediation activities that will correct individual problems identified in the implementation of each of the assurances.
The strategy describes: 1) the system improvement activities followed in response to aggregated, analyzed discovery and remediation information collected on the assurances, 2) the correspondent roles/responsibilities of those assessing and prioritizing system corrections and improvements, and 3) the processes the state will follow to continuously assess the effectiveness of the QMS and revise it as necessary and appropriate.
For MMC, the NYS DOH has developed a comprehensive program to monitor all aspects of MCO performance. The program incorporates many of the assessment activities previously outlined, but also monitors provider networks, adherence to clinical guidelines, financial statements, complaints, and reports of fraud and abuse. Comprehensive on–site operational reviews, focused on–sight reviews, and annual technical reports produced by the state´s contracted EQRO, assist the state in this regulatory role.
Oversight involves routine analysis and monitoring of QARR data submitted by MCOs, surveys designed to monitor areas of particular concern (such as provider availability and other issues identified through routine monitoring activities), and analysis of functional assessment and consumer satisfaction data. The state utilizes many data sources for oversight of the Medicaid managed care program, including: the NYS DOH´s Statewide Planning and Research Cooperative System (SPARCS), New York Medicaid Choice (the contracted enrollment broker), the state´s Medicaid Data Warehouse (MDW), findings from The External Quality Review Technical Report, and evaluation results from improvement initiatives. Additional activities and components of state oversight of managed care are described below.
a) Participating Provider Network Reports
On a quarterly basis, MCOs must submit updated information on their contracted provider network to NYS DOH. As part of the quarterly reports, MCOs provide information on the number of Medicaid enrollees empaneled to each network Primary Care Provider (PCP). In addition, any material change in network composition must be reported to the state 45 days prior to the change. Provider network reports are used to monitor compliance with access standards, including travel time/distance requirements, network capacity, panel size, and provider turnover. MCOs also submit quarterly rosters for their network PCPs. The PCP is identified for every managed care enrollee, which allows new analyses such as quality of care for enrollees in patient–centered medical homes versus those who are not.
b) Adherence to Clinical Standards/Guidelines
The state requires MCOs to adopt clinical standards consistent with current standards of care, complying with recommendations of professional medical organizations and government agencies, such as: the American Academy of Pediatrics, the American Academy of Family Physicians, the US Task Force on Preventive Care, the Substance Abuse and Mental Health Services Administration, the New York State Child/Teen Health Program (C/THP), the American Medical Association, the US Department of Health and Human Services Center for Substance Treatment, the American College of Obstetricians and Gynecologists, and the American Diabetes Association.
In February 2010, subsequent to the elimination of the Prenatal Care Assistance Program (PCAP) designation, the NYS DOH released new Medicaid Prenatal Care Standards. These standards are based on the American College of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics´ (AAP) guidelines and also address the special needs of the Medicaid population.
Additionally, New York State has standards/guidelines for the following:
- Adult, adolescent, and pediatric HIV care developed by the NYS DOH AIDS Institute.
- Asthma care developed by the NYS Consensus Asthma Guideline Expert Panel and updated at least every two years through a collaboration with professional organizations, health plan representatives, primary care providers, and asthma specialists.
c) External Quality Review – Technical Report
As mentioned previously, the NYS DOH contracts with an EQRO. To comply with Federal regulations, the EQRO´s scope of work includes:
- Validation of QARR, MEDS, UAS, and DISCO specific performance measure submissions,
- Technical assistance and validation of health plan PIPs,
- Development and implementation of focused studies of health service delivery issues such as coordination, continuity, access and availability of needed services, and
- Preparation of the EQRO Technical Report for each MCO including MLTC plans, HARPs, and DISCOs.
Every three years, the EQRO prepares a full report summarizing plan–specific descriptive data incorporating CMS protocols for external review quality reports. Thus far the reports have been created for the mainstream and HIV/SNP plans with MLTC plans forthcoming. The report includes information on trends in plan enrollment, provider network characteristics, QARR performance measures, complaints and grievances, identification of special needs populations, trends in utilization using encounter data, statements of deficiencies and other on–site survey findings, focused clinical study findings, and financial data. Every year, the reports are updated for a subset of this information focusing on strengths and weaknesses. The data are provided by NYS DOH to the EQRO, which then compiles a profile for each plan, including a summary of plan strengths and weaknesses. (For further information reference 42 CFR Part 438.364 External Quality Review Results.) The reports are distributed on CDs within the NYS DOH and to the New York City (NYC) Department of Health and Mental Hygiene. Each plan receives its own technical report. These reports are available on the NYS DOH website
d) Review of Managed Care Organizations
a. On–site operational reviews
Operational reviews are conducted on an annual basis. The review is a comprehensive examination of the operation of an MCO to ensure compliance with statutes, regulations, and government program contract requirements. These reviews also supplement other state monitoring activities by focusing on those aspects of MCO performance that cannot be fully monitored from reported data or documentation. The review focuses on validating reports and data previously submitted by the MCO through a series of review techniques that include an assessment of supporting documentation and conducting a more in– depth review of areas that have been identified as potential problems. One component of the operational survey is the in–depth review of each MCO´s quality assurance activities.
If any deficiencies are identified through the operational review, an MCO will be issued a Statement of Deficiency (SOD) which specifically identifies deficiencies. The MCO will be required to submit a Plan of Correction (POC) that addresses each deficiency specifically and provides a timeline by which corrective action will be completed. Follow–up visits may be conducted as appropriate to assess the MCO´s progress in implementing its POC. In addition to the SODs and resulting POCs, findings from the operational reviews may be used in future qualification processes as indicators of the capacity to provide high–quality and cost–effective services and to identify priority areas for program improvement and refinement.
Consistent with Mental Hygiene Law requirements, NYS OPWDD Division of Quality Improvement will continue to conduct on–site certification/recertification activities for applicable DISCO programs/facilities. Consistent with federal regulations, annual reviews of Intermediate Care Facilities (ICFs) will be completed by NYS DOH or OPWDD to ensure that the provider has maintained the required conditions of participation necessary to meet the ICF standard. On– site reviews of DISCO operations will be conducted periodically to ensure compliance with the DISCO contracts, once established. These reviews may include, but not be limited to, the following components: governance; fiscal and financial reporting and recordkeeping; internal controls; marketing, network contracting and adequacy; program integrity assurances; utilization control and review systems; grievances and complaint systems; quality assessment and assurance systems; care management; enrollment and disenrollment; ADA (Americans with Disabilities Act) compliance; management information systems; and other operational and management components. These reviews may be done by NYS DOH, NYS OPWDD, the EQRO, or another NYS contractor. Also consistent with Mental Hygiene Law requirements, all licensed mental health and SUD programs will be required to maintain current certification requirements.
b. Ad Hoc Focused Reviews
Focused reviews, which may or may not be on–site, are conducted in response to suspected deficiencies that are identified through the routine monitoring processes and QARR data. These studies also provide more detailed information on areas of particular interest to the state such as emergency room visits, behavioral health, utilization management, and problems with data systems.
c. Ongoing Focused Reviews
While particular studies or activities may be developed in response to unique situations, the following are examples of the kinds of focused studies that are conducted on an on–going basis.
- Appointment and Availability Studies
The purpose of these studies is to review provider availability/accessibility and to determine compliance with contractually defined performance standards. To conduct the study, undercover EQRO staff, on behalf of the NYS DOH, attempt to schedule appointments under defined scenarios, such as a pregnant woman requesting an initial prenatal appointment.
MCOs are required to conduct access and appointment availability studies and to follow–up when they identify providers who are not in compliance with 24–hour coverage and appointment availability requirements. MCOs that fall below the NYS DOH mandated access and availability thresholds are issued a SOD. MCOs are then required to submit a POC. Results of the studies and recommended follow–up should be reported to the MCO´s Quality Assurance (QA) committee. The state reviews the MCO follow–up efforts during subsequent on–site operational reviews and the NYS DOH conducts a re– audit of those MCOs that were issued SODs.
Networks are reviewed on a quarterly basis to determine network adequacy and to see if providers are being listed as practicing in a plan´s network when they have been subjected to disciplinary action that would preclude them from participating in the provider network. - Facilitated Enrollment and Outreach/Advertising Studies
The purpose of these studies is to determine adherence to state and local Facilitated Enrollment and Outreach/Advertising guidelines and restrictions. To conduct these studies, staff may visit sites where MCOs are permitted to do facilitated enrollment, to assist the uninsured consumers with enrollment forms and to educate them on NYS sponsored health insurance programs. The NYS DOH staff may pose as uninsured consumers or observe the activities of MCO facilitated enrollers to ensure that the facilitated enrollers are providing required information and are not engaging in any misleading enrollment practices.
As with the operational reviews, MCOs found to be out of compliance are issued an SOD and required to develop a POC. Follow–up studies are conducted for those MCOs that had a serious deficiency and failed to show improvement upon implementation of corrective action (as determined through review of indicators such as enrollment/disenrollment rates, complaints, etc.). MCOs are also required by contract to submit all marketing materials, marketing plans, and certain member notices to the NYS DOH for approval prior to use. This process ensures the accuracy of the information presented to members and potential members. In addition, New York Medicaid Choice, the NYS DOH enrollment broker, is required to track and report enrollment activity for MLTC, including satisfaction with the process. - Annual Care Coordination Review
New York State OPWDD will conduct an annual on–site review of the effectiveness of every DISCO´s care coordination function in conjunction with the NYS DOH reviews. During its on–site review, OPWDD will pull a valid sample of all individuals served by the DISCO and will review the overall effectiveness of care coordination to produce results that reflect the person´s assessed needs, communicated choices and preferences. The on–site Care Coordination Review will include a record review, interviews with the person and their advocates/circles of support, and interviews with DISCO personnel and staff engaged in the care coordination function. This review may also include operational and administrative elements that will be included in the DISCO contract such as a review of the Quality Improvement Plan and the use of Council on Quality Leadership CQL (see page 26) personal outcome measures, policies and procedures, and grievance systems. - DISCO Care Coordination Reviews
Through the NYS OPWDD´s annual care coordination review, NYS OPWDD will review a representative sample of individuals served by each DISCO. Part of this review will include an interview with the individuals to assess their degree of choice of providers, access to needed services, and satisfaction with services. This review will be part of a coordinated review of DISCOs by the NYS Department of Health and OPWDD.
e) Complaint Reports
On a quarterly basis, MCOs must submit a summary of all complaints registered during that quarter, along with a more detailed record of all complaints that had been unresolved for more than forty–five (45) days. A uniform report format was developed to ensure that complaint data is consistent and comparable. NYS DOH uses complaint data to identify developing trends that may indicate a problem in access or quality of care.
DISCO contracts will stipulate that on a quarterly basis, within 15 business days of the close of the quarter, DISCOs will provide OPWDD a summary of all grievances and appeals received during the preceding quarter using a data transmission method that is determined by OPWDD.
NYS DOH will coordinate with OASAS and OMH, providing regular and periodic reports of all complaints that are made regarding HARPs.
f) Fraud and Abuse Reports
The MCO must submit quarterly, via the Health Commerce System (HCS) complaint reporting format, the number of complaints of fraud or abuse that are made to the MCO that warrant preliminary investigation. The plan must also submit to the NYS DOH the following information on an ongoing basis for each confirmed case of fraud and abuse it identifies through complaints, organizational monitoring, contractors, subcontractors, providers, beneficiaries, enrollees, or any other source:
- The name of the individual or entity that committed the fraud or abuse;
- The individual or entity that identified the fraud or abuse;
- The type of provider, entity or organization that committed the fraud or abuse;
- A description of the fraud or abuse;
- The approximate dollar amount of the fraud or abuse;
- The legal and administrative disposition of the case, if available, including actions taken by law enforcement officials to whom the case has been referred; and,
- Other data/information as prescribed by NYS DOH.
Within DISCOs, care coordinators will be mandated reporters, and therefore care coordinators will have responsibility to report incidents and allegations of abuse that are brought to their attention or that they become aware of through their duties and responsibilities. In addition, DISCOs will have responsibility to review data and/or reports on incidents and allegations of abuse involving their members and within their provider network. They will be expected to include actionable quality improvement strategies in the Quality Assurance/Performance Improvement Plan as a result of this analysis.
g) Quarterly and Annual Financial Statements
In order to monitor fiscal solvency, the NYS DOH requires MCOs to submit quarterly and annual financial statements of operations pursuant to the Medicaid Managed Care (MMC)/FHPlus and MLTC contracts.
h) Council on Quality and Leadership (CQL)
Each DISCO will use CQL certified interviewers to conduct interviews using the CQL interview methodology based upon the 21 personal outcome measures on a representative sample of DISCO members annually. CQL´s Personal Outcome Measures offers organizations and service systems a valid, uniform, and reliable system for:
- Identifying quality of life outcomes as defined and described by each person for each of 21 indicators,
- Determining presence or absence of those outcomes in each person´s life, and,
- Identifying the supports that are facilitating or will facilitate the outcomes.
i) Member Participation on DISCO Governing Board
In accordance with NYS requirements in NYCRR Part 98.1–11, within one year of a DISCO becoming operational, at least 20 percent of the governing body of the DISCO must be enrollees or advocates, and/or an advisory body of enrolled members must be established that has direct input to the governing body, including provision of feedback on enrollee satisfaction. Enrollee/advocate board members and /or the advisory body will provide the plan with information regarding enrollee satisfaction and the DISCO´s responsiveness to cultural considerations of the enrollee community.
j) SAMM Index
In 2007, the NYS DOH developed and implemented a functional assessment scoring system based on the Semi–Annual Assessment of Members (SAAM) instrument to establish clinical eligibility for the MLTC program, i.e., determine if the person is nursing home eligible. (Please note that the UAS–NY is now the source for the creation of the SAAM Index.) The SAAM Index is comprised of 13 items from the UAS–NY instrument. These items include the areas of incontinence, cognitive functioning, and activities of daily living. Points are based on the different levels of functioning with the number of points increasing as the functional deficits increase. For example, if a potential enrollee is able to walk with a cane or walker, no points are assigned for this level of functioning. If the enrollee needs human assistance at all times to walk, four points are assigned. One point is awarded if the person experiences incontinence once a week or less. The maximum number of points is 51. SAAM Index of five or more indicates need of services usually provided in a nursing home. A level of care score of five is no longer required for dual–eligible individuals enrolled in partial capitation plans. The current statewide average SAAM Index score is 16.
k) Membership on MCO/HARP Subcommittees
MCOs are required to maintain an active behavioral health QM subcommittee which must include, in an advisory capacity, members, family members, peer specialists, and provider representatives. It is responsible for carrying out the planned activities of the behavioral health QM program and be accountable to and report regularly to the governing board or its designee concerning behavioral health QM activities. The MCO behavioral health QM subcommittee is chaired by the behavioral health medical director and is charged with implementing a process to collect, monitor, analyze, evaluate, and report utilization data consistent with the reporting requirements. The HARPs have a quality assurance program that is separate and distinct from the mainstream MCO quality assurance program and that meets all necessary requirements and conditions of the 1115 Partnership Plan.
l) Health Information Technology
New York State has been successful in aligning and implementing health information systems and health information infrastructure to support program goals. The state has the ability to collect data on encounters, provider networks, complaints, quality, and satisfaction. Financial reports submitted by plans add to the richness of data collected. New data collection efforts include use of New York´s Uniform Assessment System (UAS–NY) in MLTC plans and HARPs and establishing a "roster" of assigned primary care physicians for enrollees in managed care. UAS– NY, is a web–based system with robust data capture that is being implemented across NYS, allowing for direct data flow into the state´s Medicaid data warehouse. State and regional health registries, such as the NYS Immunization Information System (NYSIIS), continue to grow and have been increasingly utilized in quality measurement activities such as evaluations of enrollee compliance with HEDIS immunization standards.
In the spring of 2011, NYS enacted legislation that allowed for the creation of an All Payer Database (APD). The complexities of the health care system and the lack of comparative information about how services are accessed, provided, and paid for were the driving forces behind this legislation. The state recognized the need for an APD to provide a more complete and accurate picture of the health care delivery system. The APD will support health care finance policy, population health, and health care system comparisons and improvements. New York´s APD will contain health care claims data from insurance carriers, health plans, third–party administrators, pharmacy benefit managers, Medicaid and Medicare that can be synthesized to support the management, evaluation, and analysis of the NYS health care system. Payers will provide information about insured individuals, their diagnoses, services received, and costs of care.
New York´s MCOs have successful information systems that allow them to collect and submit required data and reports. Many health plans have supported the adoption and implementation of electronic health records and established internal registries to assist them in the management of diseases such as diabetes and asthma, as well as conditions such as prenatal care.
The US Department of Health and Human Services, parent agency of the CMS, created the Office of the National Coordinator for Health Information Technology (ONCHIT) in 2004, to advance the President´s agenda of creating an electronic health record for every American by 2014. New York State, in alignment with this agenda, enacted the Healthcare Efficiency and Affordability Law for New Yorkers (HEAL–NY), a grant program promoting broad adoption of the electronic health records, developing the Statewide Health Information Network of New York (SHIN– NY), and defining a governance processes for leveraging Health Information Exchanges to improve population health and reduce health care costs. Through a public/private partnership with the New York eHealth Collaborative (NYeC), a statewide collaborative process is used to continue to move the HIE agenda forward and align with the efforts of the Quality Programs.
Work continues to build an even more efficient statewide network with more robust clinical decision support. Through a statewide collaborative process of diverse stakeholders, NYeC, in partnership with the state, developed a set of privacy and security policies, and technical and operational standards, for health information exchange organizations. The work of NYeC provides the governance framework to make data available, in a consumable electronic format, to clinicians, the state, patients, and plans. The efficient delivery of clinical data at the point of service is again leveraged by the investment in HIT.
The total investment to date in New York´s Health Information Infrastructure is over $980 million, with nearly $400 million in funding through the Health Care Efficiency and Affordability Law, over $400 million in private sector matching funds, and nearly $180 million in other state and federal programs.
|top of section 4| |top of section IV| |table of contents|5. Enforcement
The OQPS, in collaboration with the OHIP has an enforcement policy for data reporting that applies to reporting for quality and appropriateness of care, contract compliance, and monitoring reports. If an MCO cannot meet a reporting deadline, a request for an extension must be submitted in writing to the NYS DOH. The NYS DOH will reply in writing as well, within one week of receiving the request. MCOs that have not submitted mandated data (or requested an extension) are notified within one week of non–receipt that they must: 1) contact the OQPS within one week with an acceptable extension plan; or 2) submit information by one week.
If the data are not submitted within one week of the deadline, enforcement options include:
- Face–to–face meeting with plan to discuss issues,
- Issue SOD and require subsequent POC,
- Deny requests for an expansion,
- Stop auto–assignment to the plan,
- Freeze new enrollment, or,
- Terminate contract.
Upon determination of the appropriate enforcement option, the Bureau of Intergovernmental Affairs shall notify the counties and advise them of the actions to be taken.
|top of section 5| |top of section IV| |table of contents|V. Review of Quality Strategy
A. Public Input
The Quality Strategy is placed on the NYS DOH web site, for a period of no less than 30 days following each update or revision, providing stakeholders and the general public the ability to comment on the content and approach. In addition, the development of the People First Waiver, including these quality strategy elements, has been a transparent and collaborative process with stakeholders. OPWDD´s history of partnership with those it supports has been and will continue to be the key to its ability to effectively support individuals with intellectual and developmental disabilities. OPWDD has used a range of mechanisms to reach as many people as possible with an opportunity to understand the reasons for reform, ask questions and contribute to the future service system. OPWDD established a dedicated People First Waiver webpage to track development for the waiver from its conceptual beginnings to a final agreement with CMS and implementation. The web page became the hub of communication, enhanced by in– person forums, briefings, hearings, and presentations. OMH and OASAS have engaged stakeholders, including the MRT Behavioral Health sub–committee, in the creation of the quality strategy for behavioral health. The agencies formulated a communication plan outlining how partners were informed and included during the development process.
B. Strategy Assessment Timeline
Every three years, NYS DOH will assess the Quality Strategy objectives using QARR/HEDIS results, UAS–NY, case management, CAHPS and other consumer survey results, Access and Availability survey findings, and the EQRO Technical Report Strengths and Opportunities for Improvement section.
Table 1: Timeline for Quality Strategy – Assessment of Objectives 2014 – 2019
| Activity | Date Completed |
|---|---|
| HEDIS/QARR data submitted (annually) | June 2014, 2015, 2016, 2017, 2018, 2019 |
| MEDS III data submitted (monthly) | January – December 2014–2019 |
| CAHPS survey conducted | November 2014–2019 |
| Calculate Rates of Quality Performance | June 2014–2019 |
| Assess Quality Strategy Objectives | December 2014, December 2017 |
| Report changes in the Strategy | Within 90 days of any amendments or changes to the Medicaid managed care program |
VI. Achievements and Opportunities
A. Managed Care Performance
Rates of performance in child health, chronic care, behavioral health, and satisfaction with care have steadily increased over time and are frequently higher than national Medicaid benchmarks published in the NCQA´s State of Healthcare Quality.
Table 2 identifies a list of measures where there was a significant improvement in statewide rates of performance between 2012 and 2014. Significant improvement is defined as having at least a 10% gap between the last reported rate and the current rate. Many additional measures have sustained rates that exceed 90%, as can be seen in Table 3.
Measures with sustained rates that exceed 90%, as can be seen in Table 3.
Table 2: Medicaid Managed Care Measures with at least 10% Improvement from 2012 to 2013 rates.
| Payer | Measure | 2013 Rate |
|---|---|---|
| MEDICAID | ||
| Asthma Ratio (5–year old´s to 64–year old´s) | 64.1 | |
| Medical Management for People with Asthma 50% days Covered (5–18yr) | 53.4 | |
| Medical Management for People with Asthma 75% days Covered (5–18yr) | 28.7 | |
| SNP | ||
| Ambulatory follow up within 30 days | 57.6 | |
| Antidepressant medication management for 84 days | 54.2 | |
| Antidepressant medication management for 180 days | 40.3 | |
| Well–Care for Adolescents | 55.3 | |
Table 3: Medicaid Managed Care Measures with Sustained Rates that Exceed 90%.
| Payer | Measure | 2013 Rate |
|---|---|---|
| MEDICAID | ||
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 12–19 Years) | 93.9 | |
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 12–24 months) | 96.9 | |
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 25 Mos. –6 Years) | 94.2 | |
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 7–11 Years) | 96.6 | |
| Adolescent Immunization Tdap/Td | 92.8 | |
| Adults´ Access to Preventive and Ambulatory Health Services (Ages 45–64) | 90.6 | |
| Adults´ Access to Preventive and Ambulatory Health Services (Ages 65 and over) | 90.1 | |
| Childhood Immunization–MMR | 92.6 | |
| Childhood Immunization –Varicella | 91.7 | |
| Childhood Immunization –3 or more HepB | 90.5 | |
| Childhood Immunization –3 or more Hibs | 93.0 | |
| Childhood Immunization –3 or more IPVs | 93.0 | |
| Annual Monitoring for Patients on Persistent Medications – ACE Inhibitors/ARBs | 92.1 | |
| Annual Monitoring for Patients on Persistent Medications – Combined Rate | 90.6 | |
| Annual Monitoring for Patients on Persistent Medications – Digoxin | 93.5 | |
| Annual Monitoring for Patients on Persistent Medications – Diuretics | 91.1 | |
| Recommend Plan to Others | 92.3 | |
| Appropriate Treatment for Upper Respiratory Infection (URI) | 92.2 | |
| SNP | ||
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 12–19 Years) | 90.4 | |
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 7–11 Years) | 91.6 | |
| Adults´ Access to Preventive and Ambulatory Health Services (Ages 20–44) | 97.2 | |
| Adults´ Access to Preventive and Ambulatory Health Services (Ages 45–64) | 98.8 | |
| Adults´ Access to Preventive and Ambulatory Health Services (Ages 65 and over) | 97.8 | |
| Advising Smokers to Quit | 93.1 | |
| Cholesterol Screening Test | 91.3 | |
| Satisfaction with Provider Communication | 94.1 | |
| Monitoring Diabetes – Lipid Profile | 94.1 | |
| Monitoring Diabetes – HbA1c Testing | 92.9 | |
| Childhood Immunization –MMR | 94.9 | |
| Childhood Immunization –Varicella | 94.9 | |
| Childhood Immunization –3 or more HepB | 94.9 | |
| Childhood Immunization –3 or more Hibs | 92.3 | |
| Childhood Immunization –3 or more IPVs | 92.3 | |
| Lead Testing | 97.4 | |
| Annual Monitoring for Patients on Persistent Medications – ACE Inhibitors/ARBs | 99.3 | |
| Annual Monitoring for Patients on Persistent Medications – Combined Rate | 98.0 | |
| Annual Monitoring for Patients on Persistent Medications – Diuretics | 99.2 | |
| Pharmacotherapy Management of COPD Exacerbation – Bronchodilator | 94.5 | |
| Diabetes Screening for People w/ Schizophrenia or Bipolar Disorder Using Antipsychotic Meds | 98.8 | |
| Appropriate Treatment for Upper Respiratory Infection (URI) | 95.8 | |
New York´s Medicaid managed care plans have continued to close the gap between Medicaid and commercial performance, highlighted in preventive care, prenatal care, women´s health, and care for people with chronic conditions. As of 2014, Medicaid performance results matched or exceeded commercial results for over 52 percent of all measures. The improvements in the timeliness of prenatal care received and control of HbA1C exemplify the progress made and are depicted in figures 2 and 3 below.
For achievements made in children´s health care quality, New York State was recently identified as a "higher performing" state in the May 2015 CMS Medicaid/CHIP Health Quality Measures Analytic Brief. The brief can be accessed here.
The 20–point decrease in persons with diabetes in poor control over the past 20 years has resulted in over 33,000 Medicaid managed care enrollees having better control over their diabetes and avoiding potentially costly complications.
Several initiatives implemented by NYS DOH are believed to have been effective in improving health care quality and service. The QI has been an invaluable tool in improving performance. Public reporting of plan performance has empowered consumers and motivated plans. Plan collaborations, such as the ADHD, childhood obesity, and the readmission collaborative, where plans partnered with network hospitals and shared lessons learned during quarterly conference calls and in–person conferences, provide a useful mechanism for plans to focus on areas of concern to the Medicaid managed care population.
Figure 2: Timeliness of Prenatal Care by Insurance Type since 1994.
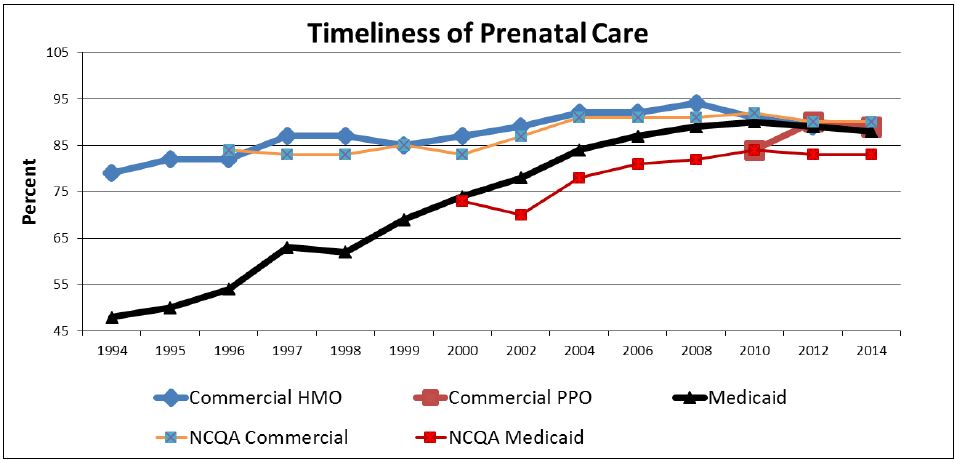
Figure 3: Control of Diabetes by Insurance Type since 2000.
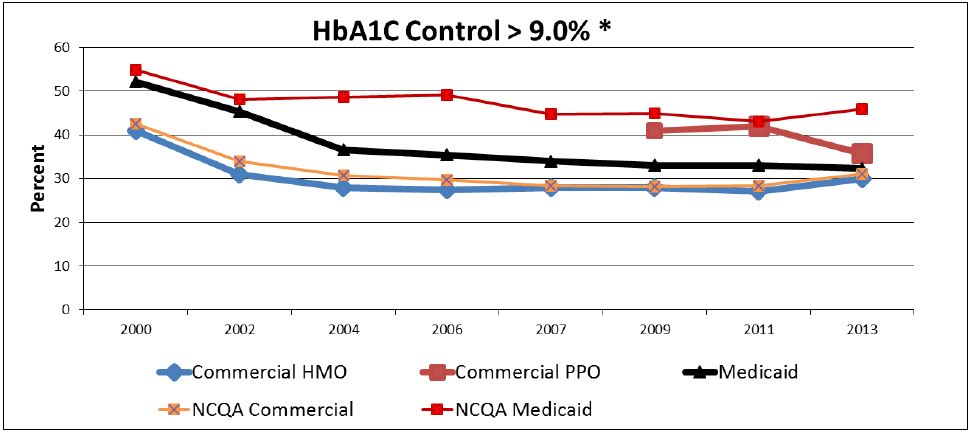
The Quality Performance Matrix has enabled plans to develop internal processes for conducting root cause analyses and implementing actions focused on the identified barriers. While early action plans may have included one or two activities, the overwhelming majority of responses are now multi–faceted, addressing improvement through member, provider, data, and plan– level interventions.
Despite the impressive gain in many quality measures, there are still areas in need of improvement. Based on the most recent publicly available QARR data (2013 measurement year), the rates for the following measures were seen to have a marginal decline of between 5– 10% from the previous measurement year:
- Mainstream (traditional Medicaid)
- Antidepressant Medication Management – Acute and Long Phase Treatment
- Adolescent Immunization for Meningococcal Disease
The improvement projects, strategies, and collaborations previously described in this state managed care quality strategy are designed to address shortcomings in MMC within NYS. MIPCD provided an excellent opportunity to study strategies for the prevention of chronic diseases; the results of this project will be available in 2016. OQPS is currently partnering with the NYS DOH Bureau of Tobacco Control to monitor and improve utilization of Medicaid smoking cessation benefits. Quality improvement work following a focused clinical study on prenatal care is also ongoing.
In addition, NYS DOH has made a concerted effort to increase the suite of mental health measures, dovetailing new HEDIS measures related to mental health and medication management. Increased measurement is informing quality improvement efforts within the mental health population enrolled in MMC. The integration of behavioral health services into managed care and the creation of HARPs presents an opportunity for NYS DOH to work with OMH and OASAS to further enhance mental health measures, including those focused on SUD. NYS DOH will also continue to work on improving behavioral health outcomes and access to care.
The behavioral health quality strategy establishes and describes an organizational culture and leadership approach that supports a partnership amongst plans, providers, government, members and advocates, and embraces the NYS vision of a system that is person–centered, recovery–oriented, integrated, and outcomes–driven. Plan behavioral health oversight will aim to achieve the following goals:
- Improve access to and engagement in community–based behavioral health services, including services designed to improve and maintain independent functioning and quality of life.
- Increase provider implementation of evidence–based practices that integrate behavioral and physical health services, including addiction pharmacotherapy
- Improve health care coordination that addresses the whole individual and addresses continuity of care.
- Reduce avoidable behavioral health and medical inpatient admissions and readmissions.
- Develop a robust behavioral health monitoring and evaluation system that drives continuous quality improvement at the clinical, program, plan, and population levels.
- Reduce disparities in health outcomes for people with behavioral health conditions as compared to the population at large.
B. Satisfaction with Care
Within NYS, adults in MMC rate their health plans higher than those in commercial products. However, getting care needed and getting care quickly were two satisfaction measures that were lower among MMC recipients than their commercial counterparts in 2011, and the rating of health plan lagged behind national ratings. Parents generally felt, and gave favorable ratings to, that they received the care needed for their children, such as appointments with specialists, physician care, tests, and treatment. Most parents had a favorable assessment of the doctor´s interaction with the child, and of the child´s overall health care. However, parents of children with chronic conditions were generally less satisfied than parents of children without chronic conditions.
The NYS DOH is addressing these opportunities for improvement in patient satisfaction with care through continued promotion of patient surveys to identify relative strengths and weaknesses in health care and health plan services. Attention to patient satisfaction will remain imperative throughout delivery system transformation initiatives. Through greater case management, health homes, patent centered care, and the performing provider practice partnerships in the DSRIP program, NYS DOH believes patient satisfaction with MMC will continue to increase across all measures.
|top of section B| |top of section VI| |table of contents|C. Access to Care
Access to care impacts members´ overall physical, social, and mental health status, and quality of life. It also affects the prevention of disease, preventable death, and promotes detection and treatment of health conditions. Disparities in access to care affect both individuals and the whole society.
Medicaid health plans had high rates of children and adolescents´ accessing primary care when compared with other types of insurance in 2012. CHP health plans exceeded all types of insurance in children and adolescents´ access to care.
NYS hopes to continue to increase the percentage of adult Medicaid members who have a regular health care provider. MMC plans are being encouraged to increase the use of patient reminders and recall systems to maintain regular preventive care visits, and to educate parents about the diseases that can be prevented and detected in the early stages with regular visits to a primary care provider.
|top of section C| |top of section VI| |table of contents|D. Integrating Service Settings
OPWDD has initiated reform efforts that will facilitate compliance with the Olmstead ruling to support all individuals with disabilities in the most integrated settings. The current service system and its underlying fiscal platform were developed to support the provision of care in traditional site–based settings. As a result, NYS has invested approximately 90% of its HCBS waiver resources to support people both residentially and in day services in highly structured certified settings. Over time, the People First Waiver will enable the reform of the service system to better support individuals in the most integrated community settings appropriate to meet their needs.
By including most institutional services in the benefit package, along with the full array of community–based services, the People First Waiver will incentivize more community– based living. In addition, OPWDD will complete its transformation from an institutionally– based system to a community–based system by moving nearly all of the remaining 1,300 people out of large institutions into community settings. It will transform its campus–based services to provide short–term, intensive treatment services to individuals who need this level of care and who will remain only as long as required to develop the supports that will enable them to move back into the community.
OPWDD has committed to achieving significant milestones related to establishing most integrated service settings and a supportive infrastructure through participation in New York State´s Money Follows the Person Demonstration and Balancing Incentive Program. To meet the need for community–based residential settings associated with these reforms, OPWDD will also identify, develop and make available a much broader range of community–based supportive housing options. New care planning practices will also ensure that individuals already living and being supported in community settings are experiencing and engaging in those communities to the fullest extent.
Similarly, OASAS, OMH, and DOH are working to improve care coordination for individuals with mental illness, SUDs, or both, across primary and behavioral health care settings. The expanded behavioral health benefits for traditional Medicaid MCOs will help to ensure that PCPs work closely with behavioral health care providers and community partners to help screen for, refer, and address recipients´ needs at the appropriate level of care. Here, the emphasis is on preventing health problems, particularly those leading to potentially preventable admissions, and, when necessary, supporting and sustaining recovery. HARPs will serve adults meeting serious mental illness and SUD targeting criteria and risk factors through health homes that will provide person–centered care planning and coordination. Care managers and care management teams will help ensure that recipients actively engage with their PCPs, behavioral health providers, and social supports, including those in HCBS settings, to complete appropriate treatment, with the ultimate aim of achieving lifelong recovery and wellness.
|top of section D| |top of section VI| |table of contents|APPENDIX 1
Contract Compliance of MCOs/PIHPs
The following table itemizes the required components of CFR 438.204(g) and identifies where they are addressed in the Medicaid model contract.
| Required Component | Medicaid Managed Care Model Contract Provision | Managed Long Term Care Contract Provision |
|---|---|---|
| 438.204 – Elements of state quality strategy standards at least as stringent as those in the federal regulations, for access to care, structure and operation, and quality measurement and improvement. | Chapter 20 of the Op Prot and the Model Contract. | MLTC Model Contract Article V. Section F. |
438.206 – Availability of services
|
Model Contract: 21.1 15.1, 15.2, 15.3, 15.4, 15.5 and Appendix J (ADA Compliance Plan). 10.12 10.16 and App. K, K.1, 7. and K.2, 7. 21.2 21.4 10.1, 15.2, 15.3, 15.4, 15.5, 15.10, and 21.1 |
MLTC Model Contract Article V. Section A. Article VII. Section A. D. Appendix B – ADA Compliance Plan Not applicable to MLTC Not applicable to MLTC Article V. Section A. Article VII. Section C. Article V. Section E. F. Article VII. Section D. |
438.207 – Assurances of adequate capacity and services
|
Model Contract 18.5 a) viii) and 21.1, Plan Qualification, Network requirements. | MLTC Model Contract Certificate of Authority Process, Network Requirements. Article V. Section A. 4. Article VII. Section D. |
438.208 – Coordination and continuity of care
|
Model Contract: 10.30, 21.8, 21.11, 21.14,10.41 13.6 10.19 – 10.23, 10.41 (c), Appendix T, T.3 (HARP and HIV SNP only) 15.7 |
MLTC Model Contract Article V. Section J. Article VII. Section G. and H. Not applicable to MLTC |
438.210 – Coverage and authorization of services
|
Model Contract: Section 14 & Appendix F | MLTC Model Contract Article V. Section J. Appendix K |
438.214 – Provider selection
|
Model Contract: 21.6 21.4 21.6 (b) 18.9, 21.1 (b) |
MLTC Model Contract Article VII. Section C. Article VII. Section C. |
438.218 – Enrollee information
|
Model Contract: 13.1, 13.2, 13.4, 13.6, 13.7, 13.11, 13.12 | MLTC Model Contract Appendix M |
438.224 – Confidentiality
|
Model Contract: Section 20, Appendix P, P.1, 10 | MLTC Model Contract Article X. Section B. Appendix L |
438.226 – Enrollment and disenrollment
|
Model Contract: Section 7.1, 7.2, 8.6, 8.7 and Appendix H | MLTC Model Contract Article V. Section B.,C.,D. |
438.228 – Grievance systems
|
Model Contract: Section 14 & Appendix F | MLTC Model Contract Article V. Section E. Appendix K. |
438.230 – Sub–contractual relationships and delegation
|
Model Contract: 22.1(b), 22.3, and 22.5 | MTLC Model Contract Article VII. Section B. And C. Provider Contract/Management Guidelines |
438.236 – Practice guidelines
|
Model Contract: 16.2 16.2(c) 14.2, 16.2(b) and Appendix F, F.1, 2. |
MLTC Model Contract Article V. Section A. J. Appendix K. |
438.240 – Quality assessment and performance improvement program
|
Model Contract: 16.1, 16.11 (HARP only), and 18.5 a) x) B) 16.1(b), 16.1 (c), 16.1 (d) & 18.5 a) v) 18.5 a) x) B) 18.5 a) x) B) 18.5 a) x) D) (HARP only) 18.5 a) x) B) |
MLTC Model Contract Article V. Section F. |
438.242 – Health information systems
|
Model Contract: 18.1(a) and 18.1 (c) (HARP only) 18.5 a) iv) 18.1(b) |
MLTC Model Contract Article VIII. Section A., E. |
APPENDIX 2
Internal Quality Assurance Plan (QAP)
MCO Quality Assurance Plans are reviewed, along with documentation of the activities and studies undertaken as part of the QAP during both the certification process and the pre-contract operational review. QAPs must contain, at minimum, the following elements.
- Description of Quality Assurance (QA) Committee structure – The Medical Director must have responsibility for overseeing the QA committee´s activities. The committee must meet regularly, no less than quarterly. Membership must include MCO network providers.
- Designation of individuals/departments responsible for QAP implementation – MCOs must designate a high–level manager with appropriate authority and expertise (such as the Medical Director or the Director´s designee) to oversee QAP implementation.
- Description of network provider participation in QAP – MCOs must involve networks providers in QAP activities. The mechanism for provider participation must be described in the written QAP, and providers must be informed of their right to provide input on MCO policies and procedures.
- Credentialing/re–credentialing procedures – MCOs must institute a credentialing process for their providers that includes, at a minimum, obtaining and verifying information such as valid licenses; professional misconduct or malpractice actions; confirmation that providers have not been sanctioned by Medicaid, Medicare or other state agencies; and the provider´s National Practitioner Data Bank profile. (See Appendix 20.2a.)
- Standards of care – MCOs must develop or adopt practice guidelines consistent with current standards of care, as recommended by professional specialty groups pursuant to the requirements of the MMC/FHPlus Model Contract.
- Standards for service accessibility – MCOs must develop written standards for service accessibility, which at a minimum, meet the standards established by state and local districts as delineated in the MMC/FHPlus Model Contract.
- Medical record standards – The QAP must contain a description of the medical records standards adopted by the MCO as specified in the MMC/FHPlus Model Contract.
- Utilization review procedures – Utilization review policies and procedures must be in accordance with the requirements specified in state law Article 49 of the Public Health Law (PHL).
- Quality indicator measures and clinical studies – The state defines quality measures for MCOs in its Quality Assurance Reporting Requirements (QARR) document. The QARR report is available on the NYS DOH website. MCOs are also required to conduct at least one Performance Improvement Project (PIP) each year in a priority topic area of their choosing. A description of the PIP(s) must be included in the QAP.
- QAP documentation methods – The QAP must contain a description of the process by which all QAP activities will be documented, including performance improvement studies, medical record audits, utilization reviews, etc.
- Integration of quality assurance with other management functions – To be effective, quality assurance must be integrated in all aspects of MCO management and operations. The QAP must describe the process by which this integration will be achieved.
APPENDIX 2a
CREDENTIALING CRITERIA – RECOMMENDED GUIDELINES
The following criteria reflect current observed standards of practice for the credentialing of physicians for participation in a managed care setting:
- List of required licensure, certifications and registrations:
- A copy of a current New York State medical license;
- A copy of current NYS registration (biennial registration as of 1995);
- A copy of current Drug Enforcement Agency (DEA) certificate;
- If the provider is board certified, a copy of the Specialty Board certification must be included and verified by written documentation from the Specialty Board.
- The physician must also have:
- Active hospital admitting privileges at an accredited hospital(s). This can be waived if the physician provides the following information:
- a description of the circumstances that merit consideration of a waiver;
- either a copy of a letter of active hospital appointment other than admitting, or evidence of an agreement between the applicant and a primary care physician who is licensed to practice in New York, has an active admitting privilege and will monitor and provide continuity of care to the applicant´s patients who are hospitalized, and;
- a curriculum vitae, proof of medical malpractice insurance, and two letters of reference from physicians who can attest to the applicant´s qualifications as a practicing physician.
- A current curriculum vitae;
- Graduation from medical school as verified by one of these methods; written documentation from the medical college or AMA Physician Masterfile;
- Completion of a residency program as verified by written documentation from the program;
- Evidence of satisfactory malpractice insurance.
- Active hospital admitting privileges at an accredited hospital(s). This can be waived if the physician provides the following information:
- The physician must submit the following information:
- A waiver by the physician of any confidentiality provisions concerning the information required for the credentialing process and reporting to the Department;
- A verification statement/attestation by the physician indicating that the information he/she is providing is true, accurate and complete;
- The names of any hospital, HMO, PHSP, IPA or medical group the physician was associated with for the purpose of performing, his/her professional duties;
- Reasons for discontinuing associations with any of the aforementioned entities;
- Information regarding pending malpractice actions and/or professional misconduct proceedings in this state or any other state, the substance of these allegations and any other information concerning the proceedings/actions that the physician deems appropriate;
- History of any malpractice and/or professional misconduct judgments and/or settlements within the past 10 years;
- A statement regarding his/her history of loss of professional license, limitation of privileges, disciplinary actions or felony convictions;
- A statement indicating that the practitioner is free from a health impairment that is of potential risk to a patient or that might interfere with the performance of his/her duties, including the habituation or addiction to depressants, stimulants, narcotics, alcohol, or other drugs or substances that may alter the individual´s behavior;
- A statement regarding the lack of present illegal drug use.
- The Plan conducts the following:
- Validation of all of the aforementioned requirements;
- Search for medical sanctions by the Office of Professional Misconduct and the Office of Medicaid Inspector General;
- Search of the National Practitioners Data Bank.
- The credentialing process, as part of the total Quality Assurance/Quality Improvement program, must be directed by a peer review committee or a comparable designated committee.
- The practitioner´s credentials must be reviewed at least every three years.
APPENDIX 3
New York State Department of Health QARR Measures, 2014
✓: Required measure
NR: Not required
| Method | Measure | Flag | Product Lines | Specifications To Use | Member Level File Required | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Commercial | FHP EBI | CHP only | Medicaid | |||||||||||
| PPO | HMO/ POS | HMO/ PHSP | HIV SNP | C P P O |
C H M O |
C H P |
M A |
H I V |
||||||
| Effectiveness of Care | ||||||||||||||
| A | Adherence to Antipsychotic Medications for People with Schizophrenia | NR | NR | NR | NR | √ | √ | HEDIS 2014 | • | • | ||||
| H | Adolescent Preventive Care Measures | 1 | √ | √ | NR | √ | √ | √ | NYS Specific | • | • | • | • | • |
| H | Adult BMI Assessment | √ | √ | NR | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| A | Annual Monitoring for Patients on Persistent Medications | √ | √ | √ | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| A | Antidepressant Medication Management | √ | √ | √ | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| A | Appropriate Asthma Medications 3 or more controller dispensing events | 8 | NR | NR | NR | NR | NR | NR | NYS Specific | |||||
| A | Appropriate Testing for Children with Pharyngitis | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • | |
| A | Appropriate Treatment for Children with Upper Respiratory Infection | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • | |
| S | Aspirin Discussion and Use | 4 | √ | √ | NR | NR | √ | √ | CAHPS 5.0H | |||||
| A | Asthma Medication Ratio | √ | √ | √ (19–64) |
√ (5–18) |
√ | √ | HEDIS 2014 | • | • | • | • | • | |
| A | Avoidance of Antibiotic Treatment in Adults with Acute Bronchitis | √ | √ | √ | NR | √ | NR | HEDIS 2014 | • | • | • | |||
| A | Breast Cancer Screening | √ | √ | √ | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| A | Cardiovascular Monitoring for People with Cardiovascular Disease and Schizophrenia | NR | NR | NR | NR | √ | √ | HEDIS 2014 | • | • | ||||
| H | Cervical Cancer Screening | 2 | √ | √ | NR | NR | √ | √ | HEDIS 2014 | • | • | • | • | |
| H | Childhood Immunization Status | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • | |
| A | Chlamydia Screening in Women | 2 | √ | √ | √ | √ (16–20) |
√ | √ | HEDIS 2014 | • | • | • | • | • |
| H | Cholesterol Management for Patients with Cardiovascular Conditions | √ | √ | NR | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| H | Colorectal Cancer Screening | 2 | √ | √ | NR | NR | √ | √ | HEDIS 2014 | • | • | • | • | |
| H | Comprehensive Diabetes Care | √ | √ | NR | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| H | Controlling High Blood Pressure | 3 | NR | NR | NR | NR | NR | NR | HEDIS 2014 | |||||
| A | Diabetes Monitoring for People with Diabetes and Schizophrenia | NR | NR | NR | NR | √ | √ | HEDIS 2014 | • | • | ||||
| A | Diabetes Screening for People with Schizophrenia or Bipolar Disorder Using Antipsychotic Medications | NR | NR | NR | NR | √ | √ | HEDIS 2014 | • | • | ||||
| A | Disease–Modifying Anti–Rheumatic Drugs for RA | √ | √ | √ | NR | √ | NR | HEDIS 2014 | • | • | • | |||
| S | Flu Shots for Adults Ages 50 – 64 | 4 | √ | √ | NR | NR | √ | √ | CAHPS 5.0H | |||||
| A | Follow–Up After Hospitalization for Mental Illness | 2 | √ | √ | √ | √ (6–18) |
√ | √ | HEDIS 2014 | • | • | • | • | • |
| A | Follow–Up Care for Children Prescribed ADHD Medication | 2 | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • |
| A | HIV/AIDS Comprehensive Care | NR | NR | NR | NR | √ | √ | NYS Specific | • | • | ||||
| H | HPV Vaccine for Female Adolescents | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • | |
| H | Immunizations for Adolescents | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • | |
| H | Lead Screening in Children | 7 | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • |
| S | Medical Assistance with Smoking Cessation | 4 | √ | √ | NR | NR | √ | √ | CAHPS 5.0H | |||||
| A | Medication Management for People with Asthma | √ | √ | √ (19–64) |
√ (5–18) |
√ | √ | HEDIS 2014 | • | • | • | • | • | |
| A | Non–Recommended Cervical Cancer Screening in Adolescent Females | √ | √ | NR | √ | √ | NR | HEDIS 2014 | • | • | • | • | ||
| A | Persistence of Beta–Blocker Treatment After a Heart Attack | √ | √ | √ | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| A | Pharmacotherapy Management of COPD Exacerbation | √ | √ | √ | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| A | Use of Appropriate Medications for People with Asthma | √ | √ | √ (19–64) |
√ (5–18) |
√ | √ | HEDIS 2014 | • | • | • | • | • | |
| A | Use of Imaging Studies for Low Back Pain | √ | √ | √ | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| A | Use of Spirometry Testing in The Assessment and Diagnosis of COPD | √ | √ | √ | NR | √ | √ | HEDIS 2014 | • | • | • | • | ||
| H | Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • | |
| Access / Availability of Care | ||||||||||||||
| A | Adult Access to Preventive/Ambulatory Care | √ | √ | √ | NR | √ | √ | HEDIS 2014 | ||||||
| A | Annual Dental Visit | NR | NR | NR | √ | √ | NR | HEDIS 2014 | • | • | ||||
| A | Children´s Access to PCPs | √ | √ | NR | √ | √ | √ | HEDIS 2014 | ||||||
| A | Initiation and Engagement of Alcohol & Other Drug Dependence Treatment | √ | √ | √ (18+) |
NR | NR | NR | HEDIS 2014 | ||||||
| H | Prenatal and Postpartum Care | 3 | NR | NR | NR | NR | NR | NR | HEDIS 2014 | |||||
| Health Plan Descriptive Information | ||||||||||||||
| Board Certification | √ | √ | √ | √ | √ | √ | HEDIS 2014 | |||||||
| Enrollment by Product Line | √ | √ | √ | √ (ENP–1a) |
√ (ENP–1a) |
√ (ENP–1a) |
HEDIS 2014 | |||||||
| Cost of Care | ||||||||||||||
| Relative Resource Use for People with Asthma | 3 | NR | NR | NR | NR | NR | NR | HEDIS 2014 | ||||||
| Relative Resource Use for People with COPD | 3 | NR | NR | NR | NR | NR | NR | HEDIS 2014 | ||||||
| Relative Resource Use for People with Diabetes | 3 | NR | NR | NR | NR | NR | NR | HEDIS 2014 | ||||||
| Relative Resource Use for People with Hypertension | 3 | NR | NR | NR | NR | NR | NR | HEDIS 2014 | ||||||
| Use of Services | ||||||||||||||
| A | Well–Child Visits in the First 15 Months of Life | 5 | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • |
| A | Well–Child Visits in the 3rd, 4th, 5th & 6th Year | 5 | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • |
| A | Adolescent Well–Care Visits | 5 | √ | √ | NR | √ | √ | √ | HEDIS 2014 | • | • | • | • | • |
| A | Ambulatory Care | √ | √ | √ | √ | √ | √ | HEDIS 2014 | ||||||
| H | Frequency of Ongoing Prenatal Care | 3 | NR | NR | NR | NR | NR | NR | HEDIS 2014 | |||||
| Frequency of Selected Procedures | ||||||||||||||
| Bariatric Weight Loss Surgery | √ | √ | √ | √ | √ | √ | HEDIS 2014 | |||||||
| Tonsillectomy | √ | √ | NR | √ | √ | √ | HEDIS 2014 | |||||||
| Hysterectomy, vaginal & abdominal | √ | √ | √ | NR | √ | √ | HEDIS 2014 | |||||||
| Cholecystectomy, open & laparoscopic | √ | √ | √ | NR | √ | √ | HEDIS 2014 | |||||||
| Back Surgery | √ | √ | √ | NR | √ | √ | HEDIS 2014 | |||||||
| Percutaneous Coronary Intervention (PCI) | 6 | √ | √ | √ | NR | √ | √ | HEDIS 2014 | ||||||
| Cardiac Catheterization | 6 | √ | √ | √ | NR | √ | √ | HEDIS 2014 | ||||||
| Coronary Artery Bypass Graft (CABG) | 6 | √ | √ | √ | NR | √ | √ | HEDIS 2014 | ||||||
| Prostatectomy | 6 | √ | √ | √ | NR | √ | √ | HEDIS 2014 | ||||||
| Mastectomy | √ | √ | √ | NR | √ | √ | HEDIS 2014 | |||||||
| Lumpectomy | √ | √ | √ | NR | √ | √ | HEDIS 2014 | |||||||
| Identification of Alcohol and Other Drug Services | √ | √ | √ (18+) |
NR | NR | NR | HEDIS 2014 | |||||||
| All Cause Readmission | √ | √ | √ | NR | NR | NR | HEDIS 2014 | |||||||
| Inpatient Utilization (General Hospital–Acute Care) | √ | √ | √ | √ | √ | √ | HEDIS 2014 | |||||||
| Mental Health Utilization | √ | √ | √ | √ | √ | √ | HEDIS 2014 | |||||||
| Antibiotic Utilization | √ | √ | √ | √ | √ | √ | HEDIS 2014 | |||||||
| Satisfaction with the Experience of Care | ||||||||||||||
| Satisfaction Survey | 4 | √ | √ | NR | NR | √ | √ | CAHPS 5.0H | De–identified member file | |||||
| NYS–Specific Prenatal Care Measures | ||||||||||||||
| Risk–Adjusted Low Birth Weight | These prenatal care measures will be calculated by the Office of Quality and Patient Safety using the birth data submitted by plans and the Department's Vital Statistics Birth File. Commercial PPO, HMO/POS, FHP EBI, Child Health Plus, Medicaid HMO/PHSP and Medicaid HIV SNP are required to submit live birth files. | |||||||||||||
| Prenatal Care in the First Trimester | ||||||||||||||
| Risk–Adjusted Primary Cesarean Section | ||||||||||||||
| Vaginal Births after Cesarean Section | ||||||||||||||
| Method A – admin, H – hybrid, S – survey Product lines PPO – Preferred Provider Organization HMO/POS – Health Maintenance Organization/Point of Service FHP EBI – Family Health Plus Employer Buy–In PHSP – Prepaid Health Services Plan HIV SNP – HIV Special Needs Plan |
Flag 1 = Use members in WCC for 12–17 stratum. 2 = Enhanced for Medicaid; file may be needed. 3 = Rotated for 2014 per HEDIS or DOH. 4 = DOH conducting Medicaid CAHPS. 5 = Administrative method only for QARR. 6 = Medicaid follow commercial specifications. 7 = Commercial plans follow Medicaid specs. 8 = Retired for QARR. |
Member Level File CHMO = Commercial HMO/POS CHP = Child Health Plus–only MA = Medicaid HMO/PHSP HIV = Medicaid HIV SNP Shading – Purple – Not required Orange – New |
APPENDIX 4
New York State MLTC Report Measure Descriptions
| Domain | Variable Name (SAAM Item Number) | Current Status and Performance | Trended Status and Performance |
|---|---|---|---|
| Overall Functioning | SAAM Index (Calculated from ML0520a, L0535, ML0540b, ML0560, ML0570, ML0580, ML0650, ML0660, ML0670, ML0680, ML0690a, ML0700a, ML0710) | Composite measure of Activities of Daily Living, Incontinence and Cognitive Functioning. | Percentage of members whose SAAM Index was stable or improved over the follow–up period. |
| Activities of Daily Living (Included in SAAM Index) | Activities of Daily Living (ADL) Composite | Percentage of members whose SAAM Index ADL Functioning composite was stable or improved over the follow–up period. | |
| Ambulation (ML0700a) | Member´s ability to walk on various surfaces. Average score on a scale of 0–6. | Percentage of members whose ability to safely walk or use wheelchair on a variety of surfaces was stable or improved over the follow–up period. | |
| Bathing (ML0670) | Member´s ability to bathe him/herself. Average score on a scale of 0–6. | Percentage of members whose ability to wash their entire body was stable or improved over the follow–up period. | |
| Transferring (ML0690a) | Member´s ability to move from a seated position to another location. Average score on a scale of 0–6. | Percentage of members whose ability to move from one location to another, such as from a bed to a chair, was stable or improved over the follow–up period. | |
| Dressing Upper Body (ML0650) Dressing Lower Body (ML0660) | Member´s ability to dress his/her upper and lower bodies with or without dressing aids. Average score on a scale of 0–3. | Percentage of members whose ability to dress their upper and/or lower body was stable or improved over the follow–up period. | |
| Toileting (ML0680) | Member´s ability to use the bathroom or bedside commode. Average score on a scale of 0–4. | Percentage of members whose ability to use a toilet or bedside commode was stable or improved over the follow–up period. | |
| Feeding/Eating (ML0710) | Member´s ability to feed him/herself. (Does not include meal preparation.) Average score on0–5 scale. | Percentage of members whose ability to feed themselves was stable or improved over the follow–up period. | |
| Incontinence (Included in SAAM Index) | Urinary Incontinence/ Catheter Presence (ML0520a) | Percentage of members who remained stable or improved in presence of incontinence or catheter need over the follow–up period. | |
| Urinary Incontinence Frequency (L0535) | Percentage of members who are incontinent more than once a week. | Percentage of members who remained stable or improved in frequency of urinary incontinence over the follow–up period. | |
| Bowel Incontinence Frequency (ML0540b) | Percentage of members who had any bowel incontinence less than once a week (excluding those who very rarely or never had bowel incontinence). | ||
| Neurological/ Emotional/ Behavioral Status (Included in SAAM Index) | Cognitive Functioning (ML0560) | Percentage of members who are not alert, i.e., need prompting or assistance in routine situations, are disoriented, or in a vegetative state. | |
| When Confused (ML0570) | Percentage of members who were confused in new situations or at various times of the day. | ||
| When Anxious (ML0580) | Percentage of members who were anxious at least occasionally. | ||
| Living Arrangements and Sensory/ Emotional Status | Living Arrangements (ML0340) | Percentage of members living alone. | |
| Frequency of Pain (ML0420) | Percentage of members who experience any pain at least daily. A higher percentage indicates greater care needs of the population. | Percentage of members who remained stable or improved in frequency of pain. | |
| Depressive Feelings (ML0590) | Percentage of members who experienced some depression feelings. A higher percentage indicates greater care needs of the population. | Percentage of members who remained stable or improved in experiencing depressive feelings over the follow–up period. | |
| Quality of Life Effectiveness of Care Emergent Care | Flu Immunization Status (L0300) | Percentage of members who received an influenza vaccination in the past year. | |
| Oral Medication Management (ML0780) | Percentage of members who are independently managing oral medication. | Percentage of members whose ability to independently manage oral medications remained stable or improved over the follow–up period. | |
| Number of Falls (L0550) | Percentage of members who had one or more falls in the last six months. | ||
| Falls Not Resulting in Medical Intervention (L0555) | Percentage of members who had falls that did not result in medical intervention. | ||
| No Known Hospital Emergent Care (ML0830) | Percentage of members who did not receive hospital emergent care. | Percentage of members for whom no hospital emergent care was reported during the follow–up period. | |
| Shortness of Breath (ML0490) | Percentage of members who remained stable or improved in experiencing shortness of breath over the follow–up period. | ||
| Utilization and Patient Safety (Nursing Home Care and Hospital Care) | Nursing Home Admissions (ML0900) | Percentage of members who had a nursing home admission. | |
| Reason for Nursing Home Admission (ML0900) | Percentage of members who had a nursing home admission for either therapy service, respite care, end of life care, permanent placement, unsafe for care at home, other, or unknown reasons. | ||
| Hospital Admissions (ML0890) | Percentage of members who had one hospital admission (emergent, urgent, or elective). | ||
| Two Hospital Admissions (ML0890) | Percentage of members who have two hospital admissions (emergent, urgent, or elective). | ||
| Percentage of members who were hospitalized for either injuries caused by falls/accidents at home, hypoglycemia/hyperglycemia/diabetes out of control, exacerbation of CHF/fluid overload/heart failure, or respiratory problems. | |||
APPENDIX 5
DISCO Specific Performance Measures
These Measures align with those approved by CMS and published in the Quality Management and Improvement Strategy for the New York State Office for People with Developmental Disabilities (OPWDD) available on the OPWDD website. The full document is available here. With the upcoming submission of the 1915 B/C waiver in early 2015, these measures may be updated based on discussions with CMS.
| Assurance and/or Quality Domain Area | Description of What will Be Measured | Anticipated Data Sources | |
|---|---|---|---|
| Personal Outcome Measures: (Assess the degree to which the DISCO´s care coordination and supports provided are contributing to individual outcome achievement) |
|||
| 21 CQL POMs | CQL POMs Measure if People: | DISCOs annual CQL data aggregation; as validated by OPWDD and/or the EQRO | |
| Are connected to natural support networks | Have meaningful relationships | ||
| Exercise Rights | Are safe | ||
| Are free from abuse and neglect | Are treated fairly | ||
| Decide when to share personal information | Experience continuity and security | ||
| Choose where they work | Choose where and with whom they live | ||
| Live in integrated settings | Use their environments | ||
| Perform different social roles | Interact with other members of community | ||
| Choose personal goals | Choose services | ||
| Participate in the life of the community | Realize personal goals | ||
| Are respected | Have friends | ||
| Individual Outcome Measures: (Clinical and Functional Outcome Measures derived from data from the OPWDD Needs Assessment Tool based upon the InterRAI known as the Coordinated Assessment System when fully implemented) |
|||
| Clinical | Select scales measure depression, behavioral needs, and cognitive performance | OPWDD CAS | |
| Functional | Select scales measure adaptive skills, communication skills, and activities of daily living | OPWDD CAS | |
| OPWDD System Reform Measures: | |||
| Self–Direction |
|
OPWDD surveys and data systems | |
| Employment |
|
OPWDD data systems | |
| Most Integrated Settings |
|
OPWDD Surveys and tracking systems | |
| 1915 C Waiver Assurance Measures: (Measures compliance with HCBS waiver assurances in accordance with CMS´s evidentiary approach to quality reviews of HCBS waiver programs). |
|||
| Level of Care |
|
OPWDD Care Coordination Review | |
| Service Planning |
|
OPWDD Care Coordination review | |
| Qualified Providers |
|
OPWDD Care Coordination Review | |
| Health and Welfare |
|
OPWDD´s Incident Reporting and Management Application including mortality review information | |
| Other Structural/Process Measures: | |||
| OPWDD Fire Safety and Physical Plant Requirements | Proportion of OPWDD–certified sites that comply with physical plant, fire safety and other requirements integral to OPWDD certification standards. | OPWDD MHL site visit protocol review | |
| Rights | Proportion of individuals who received information about their rights and the process to express concerns/objections in accordance with requirements. | OPWDD Care Coordination Review | |
| Access to Health Care | Proportion of individuals who had a primary care doctor visit for an annual physical in the last 12 months) | Encounter Data | |
| Workforce competencies | Proportion of direct support professionals that meet competencies. | OPWDD Survey Activity | |
| National Core Indicators: | |||
| Measures performance of New York State´s developmental disability system at the systems level and enables comparisons between New York State´s system and other state developmental disability systems). The NCI enhances OPWDD´s quality improvement process on a systems level by analyzing and sharing data on outcomes that are important to stakeholders, including people served and family members. Information related to National Core Indicators and recent results for NYS can be found here. | |||
APPENDIX 6
Behavioral Health Performance Measures
Social and Recovery Outcome Measures
The data source for all measures in the table below is the interRAI Community Mental Health Assessment. Measures listed as Prevalence (P) require one data point to calculate, while measures listed as Follow–Up (F) require two data points to calculate.
| Domain | Measure Name | Prevalence or Follow–Up |
|---|---|---|
| Employment | The percentage of members currently employed | P |
| The percentage of members currently competitively employed | P | |
| The percentage of members who prefer change in their employment situation | P | |
| The percentage of members who prefer change in employment supports | P | |
| The percentage of members employed at least 35 hours per week in the past month | P | |
| The percentage of members employed at or above the minimum wage | P | |
| The percentage of members who maintained or obtained employment | F | |
| The percentage of members interested in obtaining employment support who received HCBS employment supports | F | |
| The percentage of members who maintained or obtained full–time employment (averaging 35 hours per week in the past month) | F | |
| The percentage of members who maintained or obtained employment at or above the minimum wage | F | |
| Education | The percentage of members currently enrolled in a formal education program | P |
| The percentage of members who prefer change in their level of education | P | |
| The percentage of members who prefer a change in educational support services | P | |
| The percentage of members interested in receiving education supports who received HCBS education supports | F | |
| Housing | The percentage of members who are homeless | P |
| The percentage of members with residential instability in the past two years | P | |
| The percentage of members with maintenance of stable or improved housing status | F | |
| Criminal Justice | The percentage of members who were arrested within the past 30 days | P |
| The percentage of members who were arrested within the past year | P | |
| The percentage of members who were incarcerated within the past 30 days | P | |
| The percentage of members who were incarcerated within the past year | P | |
| The percentage of members on probation or parole at time of assessment | P | |
| The percentage of members with reduced arrests – 30 days | F | |
| The percentage of members with reduced arrests – past year | F | |
| Social Connectedness | The percentage of members with social interaction in the past week | P |
| The percentage of members with one or more social strengths | P | |
| The percentage of members with maintained or improved social interaction in the past week | F | |
| The percentage of members with maintained or improved social strengths | F | |
| Self–Help Group Participation | The percentage of members who attended a self–help or peer group in the past 30 days | P |
| Inpatient Treatment | The percentage of members who were discharged from a psychiatric hospital within the past 90 days | P |
| The percentage of members who had an inpatient stay for substance use disorder in the past 6 months | P | |
| Substance Use | The percentage of members with reduced substance use | F |
| Activities of Daily Living | The percentage of members with improved performance on and capacity for activities of daily living from baseline measurement to 12 months | F |
Behavioral Health Medicaid Managed Care Performance Measures
The following measures will be produced by OMH on a quarterly basis. Populations are either MH (mental health), Substance Use Disorder (SUD), or Behavioral Health (BH). Medicaid encounter data will be the data source for all measures in this table.
| Domain | Population | Measure Name |
|---|---|---|
| Mental Health Readmission | MH | Readmission to mental health inpatient treatment within 30 days of discharge. |
| MH | Readmission to mental health inpatient treatment within 90 days of discharge. | |
| BH Continuity of Care/ Ambulatory Follow–up | MH | The percentage of mental health inpatient discharges followed by an outpatient visit for mental health treatment within 7 and 30 days of discharge. |
| SUD | The percentage of SUD detoxification discharges followed by a lower level SUD service within 14 days of discharge. | |
| SUD | The percentage of SUD inpatient rehab discharges followed by a lower level SUD service within 14 days of discharge. | |
| BH | The percentage of individuals seen in a medical emergency department for a suicide attempt or drug overdose who are discharged from the medical ED and/or a medical surgical unit to the community who are seen for behavioral health services/treatment within 48 hours of discharge | |
| Engagement in Care | MH | The percentage of mental health inpatient discharges followed by two or more outpatient visits for mental health treatment within 30 days of discharge. |
| Psychiatric Medication Management | MH | The percentage of MH Discharges where a prescription for a psychotropic medication was filled within 30 days. |
| Addiction Medication | SUD | The percentage of SUD Detox or Rehabilitation discharges where a prescription for an anti–addiction medication was filled within 30 days. |
| SUD | Utilization of pharmacotherapy for alcohol dependence | |
| SUD | Utilization of pharmacotherapy for opioid dependence | |
| SUD | Initiation of pharmacotherapy for alcohol dependence | |
| SUD | Initiation of pharmacotherapy for opioid dependence | |
| Length of Stay | BH | Mean and median length of stay |
| MH | The percentage of MH inpatient discharges who meet short and long stay criteria (criteria TBD) | |
| Outpatient Care | BH | The percentage of members with at least 2 BH outpatient visits in a year |
| MH | The percentage of HARP members who didn't receive any MH outpatient treatment for 6 months | |
| MH | The percentage of HARP members who didn't receive any MH outpatient treatment for 12 months | |
| MH | The percentage of members who had at least three MH outpatient treatments during a year period, with a gap of no more than three months between each visit | |
| MH | The percentage of MH inpatient discharges who enrolled into ACT within 30 days after discharge. | |
| Adult Access to Preventive/Ambulatory Health Services | BH | The percentage of members with at least one physical health visit in a year |
| MH | The percentage of MH inpatient discharges who had chronic physical condition as secondary or other diagnoses followed by a physical health visit within 30/60/90 days. | |
| SBIRT (Alcohol Use) | SUD | Screening for Substance Use Disorder and Referral |
APPENDIX 7
Published Journal Articles – New York State Managed Care
Emergency Department Reliance Among Rural Children in Medicaid in New York State. Uva JL, Wagner VL, Gesten FC. J Rural Health. 2012 Spring; 28(2): 152–61.
Cogan LW, Josberger, RE, Gesten, FC Roohan, PJ. Can Prenatal Care Impact Future Well–Child Visits? The Experience of a Low–Income Population in New York State Medicaid Managed Care. Matern Child Health J (2012) 16:92–99.
Morris LS, Schettine A, Roohan PJ, & Gesten F (2011). Preventive Care for Chronically Ill Children in Medicaid Managed Care. American Journal of Managed Care. 17 (11): e435–e442.
Anarella J, Roohan P, Balistreri E, Gesten F. A survey of Medicaid recipients with asthma: perceptions of self–management, access, and care. Chest. 2004 Apr;125(4):1359–67.
Gesten F, Leonard M, Schettine A. Seeking to understand case management in New York. Case Manager. 2006 Jul–Aug;17(4):55–8, 62.
Klein JD, Sesselber TS, Gawronski B, Handwerker L, Gesten F, Schettine A. Improving adolescent preventive services through state, managed care, and community partnerships. J Adolesc Health. 2003 Jun;32(6 Suppl):91–7.
Pasley B, Roohan PJ, Wagner V, Novak J, Gesten F. Identifying areas for improvement: results of a Medicaid managed care diabetes survey. J Health Care Poor Underserved. 2005 Nov;16(4):691–719.
Radigan M, Lannon P, Roohan P, Gesten F. Medication patterns for attention– deficit/hyperactivity disorder and comorbid psychiatric conditions in a low–income population. J Child Adolesc Psychopharmacol. 2005 Feb;15(1):44–56.
Roohan, P. Integration of data and management tools into the new york state medicaid managed care encounter data system. J Ambul Care Manage. 2006 Oct–Dec;29(4):291–9.
Roohan PJ, Butch JM, Anarella JP, Gesten F, Shure K. Quality measurement in medicaid managed care and fee–for–service: the New York State experience. Am J Med Qual. 2006 May– Jun;21(3):185–91.
Roohan PJ, Anarella JP, Gesten FC. Quality oversight and improvement in Medicaid managed care. J Public Health Manag Pract. 2004 Jul–Aug;10(4):321–9.
Roohan PJ, Josberger RE, Acar J, Dabir P, Feder HM, Gagliano PJ. Validation of birth certificate data in New York State. J Community Health. 2003 Oct;28(5):335–46.
Roohan PJ, Franko SJ, Anarella JP, Dellehunt LK, Gesten FC. Do commercial managed care members rate their health plans differently than Medicaid managed care members? Health Serv Res. 2003 Aug;38(4):1121–34.
Roohan PJ, Gesten F, Pasley B, Schettine AM. The quality performance matrix: New York State´s model for targeting quality improvement in managed care plans. Qual Manag Health Care. 2002 Winter;10(2):39–46.
Roohan PJ, Josberger RE, Gesten FC. Risk–adjusted primary cesarean delivery rates for managed care plans in New York State, 1998. Matern Child Health J. 2001 Sep;5(3):169–77.
Roohan PJ, Conroy MB, Anarella JP, Butch JM, Gesten FC. Commercial managed care plans leaving the Medicaid managed care program in New York State: impact on quality and access. J Urban Health. 2000 Dec;77(4):560–72.
Schettine, A. Seeking to understand case management in New York. Case Manager. 2006 Nov– Dec;17(6):13.
Wagner VL, Radigan MS, Roohan PJ, Anarella JP, Gesten FC. Asthma in Medicaid managed care enrollees residing in New York City: results from a post–World Trade Center disaster survey. J Urban Health. 2005 Mar;82(1):76–89. Epub 2005 Feb 28.
|top of appendix 7| |table of contents|
Follow Us