42 CFR 438 MMC Service Authorization and Appeals -
MMC/HIV SNP/HARP
- Presentation is also available in Portable Document Format (PDF)
Hope Goldhaber, Division of Health Plan Contracting and Oversight
Office of Health Insurance Programs
November 30, 2017; REV January 31, 2018
Welcome
- This presentation is for mainstream Medicaid managed care, HIV SNP and HARP products
- Goals for today:
- Describe implementation steps related to full compliance with 42 CFR 438 for service authorization and appeal processes
- Highlight impacts of the 2016 Mega Rule on these processes
- Review appropriate use of the template notices
- Confirm the template notice approval process
Reminders
- This webinar is being recorded
- PLEASE:
- DO NOT PUT YOUR PHONE ON HOLD
- participants may unmute themselves by pressing *6
- please wait for facilitator to acknowledge the next speaker
- Identify yourself when speaking
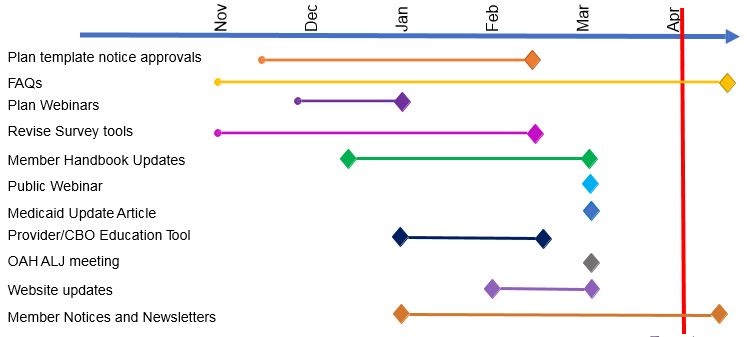
Implementation Timeline
Questions?
Are we speaking the same language?
| 42 CFR 438 | MMC Model Contract | Template |
|---|---|---|
| Service Authorization Request | Services Authorization Request | You asked for [service] |
| Adverse Benefit Determination | Action | Decision to deny, reduce, suspend, stop |
| Notice of Adverse Benefit Determination | Notice of Action | Initial Adverse Determination |
| Appeal | Action Appeal | Plan Appeal |
| Notice of Appeal Resolution | Notice of Action Appeal Determination | Final Adverse Determination |
| Continuation of Benefits | Aid Continuing | Keep your services the same |
| External Medical Review | External Appeal | External Appeal |
| Grievance | Complaint | Complaint |
42 CFR 438 Impact on Service Authorizations and Appeals
| Changed Regulation: | Impact Summary: |
|---|---|
| 438.210(d)(2)(i) | Changes expedited authorization decision/notice timeframe to 72 hours subject to extension |
| 438.210(d)(3) | Refers to SSA § 1927(d)(5)(A) –Requires response by phone or telecommunication device within 24 hours of prior authorization request for outpatient drugs |
| 438.400(b) | Defines adverse benefit determination (replaces "action").
|
| 438.400(b)(7) | Adds denial of a request to dispute a financial liability to the definition of adverse benefit determination. |
| 438.402(b) | Only one level of internal appeal is permitted.
|
| 438.402(c)(1)(i) 438.408(f)(1) |
Establishes the enrollees right to a Fair Hearing regarding an adverse benefit determination after receipt of notice under 438.408 (appeal resolution) that the adverse benefit determination has been upheld.
|
| 438.402(c)(1)(i)(A) 438.408(c)(3) 438.408(f)(1)(i) |
Defines ´deemed exhaustion´ – the enrollee has exhausted the plan´s appeal process if the notice and timing requirements of 438.408 (appeal resolution) have not been met and may request a fair hearing.
|
| 438.402(c)(1)(ii) | Adds requirement for enrollee´s written consent for representatives to request plan appeal, grievance or fair hearing on their behalf. Providers may request appeal, grievance or fair hearing but may not request Aid Continuing.
|
| 438.402(c)(2)(ii) | Requires appeals to be filed within 60 calendar days of the date on the Initial Adverse Determination |
| 438.404(b)(2) | Notices identify the right to request and receive, free of charge, copies of all sources of information relevant to the adverse determination
|
| 438.406(b)(5) | Requires provision of case file free of charge and sufficiently in advance of resolution timeframes for appeals to enrollee and representative.
|
| 438.408(b)(3) | Changes expedited appeal determination/notice timeframe to 72 hours |
| 438.408(c)(2) | Plans must make reasonable efforts to give prompt oral notice of an extension and written notice within 2 calendar days |
| 438.408(f) | Provides enrollees 120 calendar days from the date of an adverse appeal resolution notice to request a fair hearing. |
| 438.420 | Provides enrollees the right to Aid Continuing upon timely filing of an appeal – 10 days of the notice of adverse benefit determination or by the effective date of the adverse benefit determination, whichever is later. Provides aid continuing without interruption if the enrollee requests a fair hearing within 10 days of the plan´s sending the written adverse appeal resolution notice.
|
| 438.424(a) | If the fair hearing decision reverses the plan´s adverse benefit determination, and the disputed services were not provided while the appeal and hearing were pending, the plan must authorize or provide the disputed services promptly and as expeditiously as the enrollee´s condition requires but no later than 72 hours from the date the plan receives the fair hearing decision. |
Standard MMCO Prior Authorizations and Appeals Process*
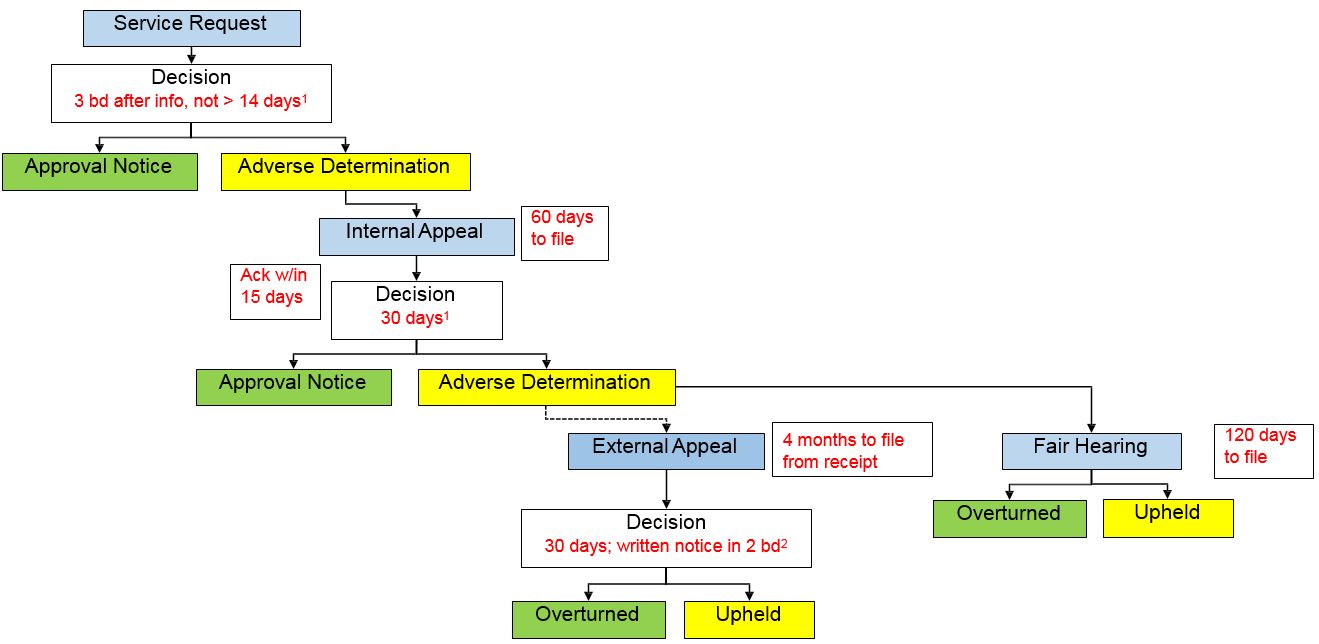
1 possible extension of up to 14 days
2 possible extension of up to 5 bd
*Please see for NYS MMC Service Authorization and Appeals Timeframe Comparison for more information
Standard MMCO Complaint Process*
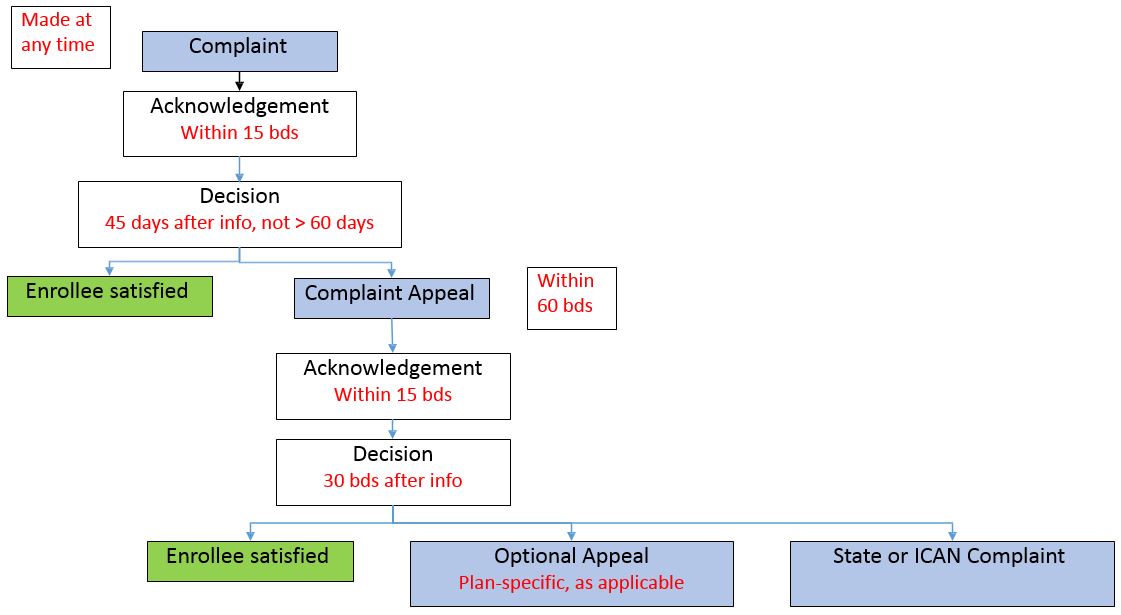
*Please see Grievances Timeframe Chart for more information
Questions?
Template Notices – Purpose and Use
- 42 CFR 438.10(c)(4)(ii) requires the use of model enrollee notices
- The State developed the template notices with significant input of the Service Authorization and Appeals Stakeholder Workgroup
- There are now eight model templates:
- Approval: approval of a services authorization request or whole overturn of an adverse benefit determination on appeal
- Extension: extension for more information during service authorization request review or appeal
- Initial Adverse Determination No AC: notice of adverse benefit determination
- Initial Adverse Determination With AC
- Final Adverse Determination No AC: adverse notice of appeal resolution (adverse benefit determination upheld in whole or in part)
- Final Adverse Determination With AC
- Complaint Resolution
- Complaint Appeal Resolution
- 2014 IAD combined all rights, with separate appeals attachment and fair hearing form to be used for any type of denial
- 2017 templates for IADs and FADs are split by decisions where the enrollee does or does not have a right to aid continuing
- Plan procedures must ensure that the notice issued is appropriate to the type of denial, or the notice will be inadequate
- Termination, suspension or reduction of a previously authorized service, or any adverse change in LTSS/Nursing home must include right to AC and be issued in advance of the effective date.
- 2017 templates are designed to be used for both administrative and utilization review determinations – external appeal information in the FAD is deleted for administrative decisions.
- 2017 FADs are one notice – combined plan decision and Fair Hearing rights – no separate fair hearing form.
Notice Process and Timeframes
- New charts have been finalized indicating the blended time frames for compliance with PHL and 42 CFR 438 for service authorization requests, appeals, complaints and complaint appeals.
- Plan procedures must be updated to comply with the new timeframes
- New notices and exhaustion/AC processes may not be utilized prior to April 1, 2018. These apply to adverse benefit determination made on April 1, 2018 and thereafter.
- For enrollees who receive an action taken notice prior to April 1, 2018 and subsequently appeals or requests a fair hearing after April 1, 2018, the appeal or fair hearing will be considered timely and handled pursuant to the rights issued in the action notice (old rules).
- If the enrollee appeals, the plan´s appeal resolution will be the new FAD and the enrollee will receive the right to request a fair hearing within 120 days (new rules).
Template Notices – Clinical rationale/specific reason for denial
- During the stakeholder workgroup meeting 3, we reviewed poor clinical rationales and explored ways to improve noticing, including emphasis on plain language and reduction of extraneous information
- DOH restructured model notice templates placeholder language to improve the inclusion of all required elements for these decisions
Specific Denial Reason Requirements:
For administrative or benefit denials
- 4th–6th grade reading level
- Grounds for appeal must be easily identifiable
- For benefit denial, must include the specific service that is not covered
- For benefit coverage that is dependent on the enrollee´s condition, must include the specific benefit criteria that is not being met (e.g., dental, orthodontia, personal care, etc.)
- For administrative denials, such as no prior authorization, must include plan requirement that was not met
- Examples:
- Family planning services are not covered under our benefit package. You may use your
- Medicaid card to obtain this service from any provider that accepts Medicaid.
- Root canals for tooth #18 (wisdom tooth) are not covered by Medicaid unless the tooth is needed to support a dental device or you need the tooth to be able to chew. You do not wear a dental device, and you have at least eight teeth in contact with each other and are able to chew without this tooth.
- The provider is required to get approval from the plan before performing an MRI. No authorization was issued for your MRI on January 15, 2017, so this claim will not be paid. You are not responsible for payment of this bill.
Out of Network (OON) IAD – Administrative Denial
For administrative or benefit denials
- 4th–6th grade reading level
- Grounds for appeal must be easily identifiable
- OON service denials for service that are not materially different must include a description of the service available in–network, why it is not materially different, and how to access the in–network service.
- OON referral denials for services requested based on the training and experience of a provider must include contact information for in–network providers available and able to provide the requested service.
Out–of–Network Examples:
- OON Not Materially Different Service Denial:
- You asked for 3–D Magnetic Resonance Imaging (MRI) of the temporal lobe because you have been having symptoms that may come from seizures. You want to know if times where you are unresponsive or your mood suddenly changes are related to epilepsy. You would like to find out if there are signs of epilepsy in this part of your brain.
- The following in–network service is available to treat your condition: a standard MRI of the temporal lobe. We believe that this service is not very different from the service you requested because a standard MRI will still show whether or not there are signs of seizure activity. This service can identify whether there is damage to the temporal lobe linked to a diagnosis of epilepsy. You can get this service by contacting one of our in–network providers. A list of these providers is available on our website. You do not need to get approval before getting this service from an in–network provider.
- OON Referral Denial:
- You asked for outpatient physical therapy from Great PT Inc. to help you recover from breaking your left femur (leg).
- The in–network providers listed below are available to provide outpatient physical therapy and have the correct training and experience to meet your needs. You can check the provider directory or call us for other provider options.
111 Main Street
New York, NY 10101
Phone: 212–555–5555 Dr. Brown
99 First Street
New York, NY 10001
Phone: 212–555–7777
Previous Clinical Rationale Requirements:
- For utilization review (PHL 49) decisions
- A statement of clinical rationale for an adverse determination must, at a minimum, identify:
- The enrollee and the nature of his/her medical condition;
- The medical service, treatment or procedure in question; and
- The basis or bases on which the utilization review agent determined that the service, treatment or procedure is or was not medically necessary or experimental/investigational, which shall demonstrate that the agent considered enrollee–specific clinical information in its determination.
- A statement of reasons and clinical rational for adverse determination must be sufficiently specific to enable the enrollee and the enrollee´s health care provider to make an informed judgment regarding 1) whether or not to appeal the adverse determination, and 2) the grounds for such an appeal.
Updated Clinical Rationale Requirements:
- For utilization review (PHL 49) decisions
- 4th–6th grade reading level
- Grounds for appeal must be easily identifiable
- Must include:
- the service requested;
- the enrollee´s condition;
- why the service was requested or how the service was intended to treat or ameliorate the enrollee´s condition;
- the specific criteria that must be met for the service to be approved including the identification/ name of the criteria and a description of what is actually necessary to get the service approved;
- enrollee–specific information about why the decision was made including how the criteria was not met; and
- If this is a change to a service that has already been approved, the change to the enrollee´s condition impacting the level of care needed and when the change occurred must be included.
Updates to Specific Denial Reason/ Clinical Rationale Placeholders
INSERT IF THE DECISION IS CLINICAL AND ABOUT A REQUEST/CLAIM FOR A NEW SERVICE INCLUDING PARTIAL APPROVALS, AND IS NOT ABOUT LTSS, OR DELETE THIS SEGMENT
- You asked for [service] because [Insert the nature of the enrollee´s condition].
- To approve this service, {insert for partial approvals} [in full] the following criteria must be met: [Insert criteria required for the service to be approved].
- These criteria are not met because [Insert enrollee–specific details from the enrollee´s unique clinical/social profile to show why/how the enrollee does not meet the required criteria for service approval (necessitating a service denial) or why/how it does not fully meet the required criteria for service approval (necessitating a partial service approval) or Insert model prescriber prevails language or case–specific information about why the service is experimental/investigational.].
{Note: The clinical rationale must be sufficiently specific to enable the enrollee to determine the basis for appeal.}
Clinical Rationale New Partial Approval Example:
- You asked for outpatient physical therapy services 1 hour per day, 3 days per week from, 8/1/17– 9/12/17, for a total of 18 hours of outpatient physical therapy services because you broke your left wrist. You want this service to help recover so that you can use your injured hand to complete daily living tasks on your own.
- To approve this service in full, you must be assessed as needing the requested amount of physical therapy to meet your goals in a specific time period. Your goals include independently doing laundry, cleaning, and hygiene tasks.
- The criteria are not met because your doctor assessed your needs and abilities on 7/30/17. You have a hairline fracture, which means the break is minor, and your doctor expects you to recover quickly. You are right handed and still able to complete most hygiene and cleaning tasks independently. Your doctor´s assessment shows that you will only need physical therapy services to meet your goals from 8/1/17 to 9/12/17, 1 hour per day, 2 days per week. You have been approved for outpatient physical therapy services for 1 hour per day, 2 days per week, from 8/1/17–9/12/17 for a total of 12 hours of outpatient physical therapy services.
Updates to Specific Denial Reason/ Clinical Rationale Placeholders
Placeholders for LTSS reduction, suspension, or termination determinations:
- Your [service] will be [stopped][reduced][suspended] because:
- [Indicate the change in medical condition, social, or environmental circumstances since the previous authorization was made.]
- [State when the change occurred.]
- [Include the information and criteria relied on to make the decision.]
- You no longer meet the criteria for your current level of service because:
- [Describe why or how the change in medical condition, social, or environmental circumstances no longer meet the criteria for the previous authorization or why/how this change necessitates a change in services.]
{{Note: The rationale must be sufficiently specific to enable the enrollee to determine the basis for appeal.}
Clinical Rationale LTSS Reduction Example:
- Your Level 2 Personal Care Services 4 hours per day, 5 days per week will be reduced because:
- Your hip replacement has improved your condition. You no longer need the same level of help with personal hygiene tasks and mobility.
- During the UAS–NY assessment you had completed on 9/1/17, you indicated your condition changed.
- Your current services were approved based on your 3/1/17 UAS–NY results. At that time, you needed extensive assistance with both personal hygiene tasks and mobility. Now, your most recent UAS–NY shows you need limited assistance with certain personal hygiene tasks and mobility.
- You no longer meet the criteria for your current level of service because:
- Based on your 9/1/17 assessment, you now only need some hands–on help for bathing and dressing. You only need limited assistance when walking around your home and in the community. We are reducing your Personal Care Services because you do not need as much hands–on help.
Questions?
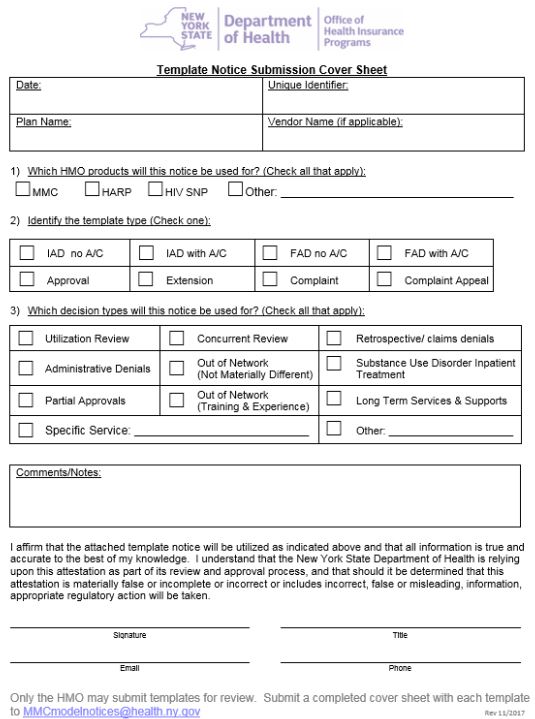
Template Approval Process
- All template notices must be submitted to the Department prior to use
- 2017 templates may not be used prior to April 1, 2018.
- Only MCOs may submit templates for approval
- A Notice Submission Cover Sheet must be submitted for EACH template
- A plan–created unique identifier must appear on the cover sheet and in the footer on each page of the template
- Plans are highly encouraged to follow the model template language
- If additional or revised language is used, the template must be annotated to highlight revisions, including omission of non–applicable placeholders. All changes must be compliant and in plain language (4th to 6th grade reading level).
- The Submission Cover Sheet identifies the intended purpose of each template
- Incomplete submissions will be returned
- Upon completion of the review, the plan will receive a status spreadsheet and, if the notice cannot be approved, a complete checklist highlighting needed changes.
- Plan may be asked to re–start submission process if needed corrections are extensive.
Questions?
Next Steps
- Submit templates no later than December 15, 2017
- Additional webinars and guidance materials
- FAQs
Thank You!
Please send comments or questions to: 438reg@health.ny.gov
Submit template notices to: MMCmodelnotices@health.ny.gov