Aid to Continue
42 CFR 438 MMC Service Authorization and Appeals
MMC/HIV SNP/HARP/MLTC/Medicaid Advantage/Medicaid Advantage Plus
- Presentation is also available in Portable Document Format (PDF)
Hope Goldhaber, Division of Health Plan Contracting and Oversight
Donna Lochner, Division of Long Term Care
Office of Health Insurance Programs
April 13, 2018
Reminders
- This webinar is being recorded
- Due to the large number of participants, all lines are muted
- No beeps on entry
- We will post these slides on health.ny.gov after the presentation
- Please send questions through Q&A feature
- Questions may also be sent to 438reg@health.ny.gov
Welcome
- This presentation is for Medicaid managed care plans subject to 42 CFR 438
- MMC
- HIV SNP
- HARP
- MLTC Medicaid
- Medicaid Advantage
- Medicaid Advantage Plus
- Goals for today:
- Review requirements for enrollee appeal rights, deemed exhaustion, fair hearing rights, aid to continue and case files
- Review most frequently asked questions on these issues
Are we speaking the same language?
| 42 CFR 438 | MMC Model Contract | Template |
|---|---|---|
| Service Authorization Request | Services Authorization Request | You asked for [service] |
| Adverse Benefit Determination | Action | Decision to deny, reduce, suspend, stop |
| Notice of Adverse Benefit Determination | Notice of Action | Initial Adverse Determination |
| Appeal | Action Appeal | Plan Appeal |
| Notice of Appeal Resolution | Notice of Action Appeal Determination | Final Adverse Determination |
| Continuation of Benefits | Aid Continuing | Keep your services the same |
| External Medical Review | External Appeal | External Appeal |
| Grievance | Complaint | Complaint |
Steps to take if a service request is denied
This is the regular Medicaid Managed Care appeals process. If enrollee´s health is at risk, ask for fast track review. See plan´s member handbook for full information.
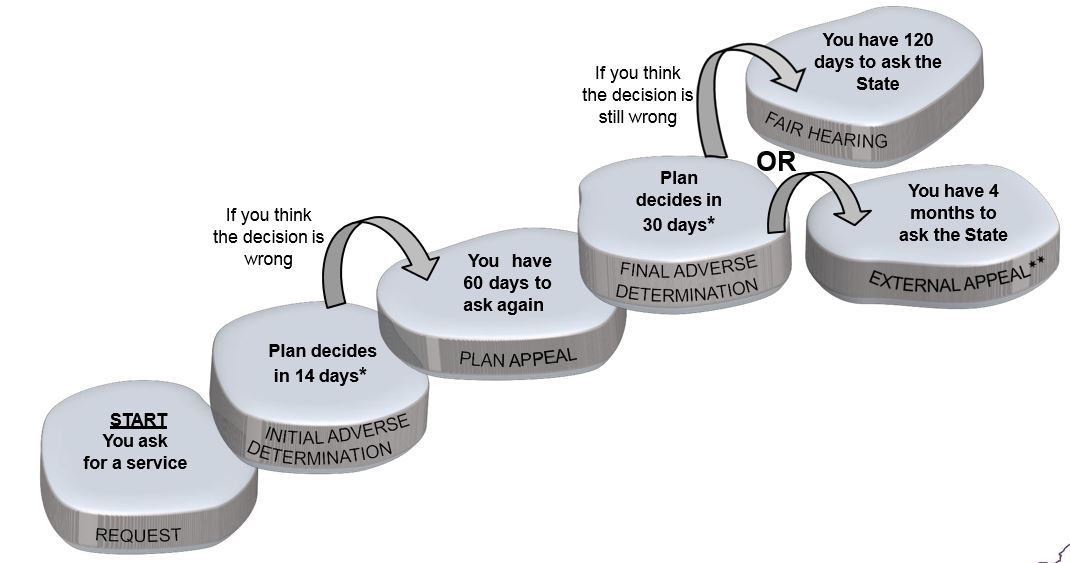
*May take up to 14 days longer if more information is needed
**External appeal is not available for some decisions
When can an enrollee ask for a Plan Appeal about Adverse Benefit Determinations?
Adverse Benefit Determination
42 CFR 438.400 defines as any of the following:
- The denial or limited authorization of a requested service, including determinations based on the type or level of service, requirements for medical necessity, appropriateness, setting, or effectiveness of a covered benefit
- The reduction, suspension, or termination of a previously authorized service.
- The denial, in whole or in part, of payment for a service
- The failure to provide services in a timely manner, as defined by the State
- The failure of an MCO, PIHP, or PAHP to act within the timeframes provided in
- §438.408(b)(1) and (2) regarding the standard resolution of grievances and appeals
- For a resident of a rural area with only one MCO, the denial of an enrollee´s request to exercise his or her right, under §438.52(b)(2)(ii), to obtain services outside the network
- The denial of an enrollee´s request to dispute a financial liability, including cost sharing, copayments, premiums, deductibles, coinsurance, and other enrollee financial liabilities
These events are adverse benefit determinations whether or not the plan sends notice
Adverse Benefit Determination and Appeals
- 42 CFR 438.404 requires timely and adequate notice of adverse benefit determinations (Initial Adverse Determination)
- 42 CFR 438.400 defines Appeal as a review by an MCO, PIHP, or PAHP of an adverse benefit determination
- 42 CFR 438.402 provides an enrollee 60 days from the date of the notice of an Adverse Benefit Determination to ask for a Plan Appeal
What if the Initial Adverse Determination notice is not sent?
- If the plan makes an adverse benefit determination and fails to notify the enrollee, or does not provide timely notice, the enrollee may ask for an appeal
- Plans should accept and review enrollee appeals where the plan failed to provide adequate and timely notice of the adverse benefit determination
When can an enrollee ask for a Plan Appeal of an Adverse Benefit Determination?
- An enrollee can ask for a Plan Appeal of an Adverse Benefit Determination*:
- Up to 60 days from the date of the Initial Adverse Determination
- When the enrollee requests a service, and the plan does not respond or response is late
- When the plan made an adverse benefit determination without adequate notice, or notice was late
- MMC/HARP/HIV SNP only: After filing a complaint that a provider denied a service (which must be handled as a service authorization request), and the plan does not respond, or the response is late
*Not an exhaustive list of appeal rights; enrollees have right to appeal other plan decisions
Plan Appeals of an Adverse Benefit Determination
- 42 CFR 438.406 requires plans to provide reasonable assistance to enrollees in taking procedural steps related to appeals
- Plan policies and procedures should ensure acceptance and review of enrollee appeals
- Plans should not base intake procedures on hearing the word "appeal"
- Plans should ensure internal referrals are accurately made for prompt intake of appeals by appropriate staff
When can an enrollee ask for a Fair Hearing about plan adverse benefit determinations?
Right to Fair Hearing
- DOH guidance issued December 15, 2017
- 42 CFR 438.402 establishes that
- An enrollee may request a State Fair Hearing after receiving an appeal resolution that an adverse benefit determination has been upheld
- An enrollee may be deemed to have exhausted the plan´s appeal process and may request a state fair hearing where notice and timeframe requirements under 42 CFR 438.408 have not been met
- 42 CFR 438.408 provides the enrollee no less than 120 days from the date of the appeal resolution to request a state fair hearing
- An enrollee may request a State Fair Hearing after receiving an appeal resolution that an adverse benefit determination has been upheld
- This means when the plan decides to make an adverse benefit determination, the enrollee must first ask for a Plan Appeal, and allow time for a response, before they can ask for a fair hearing
What if the enrollee receives no response to the Plan Appeal or the response is late?
- An enrollee may be deemed to have exhausted the plan´s appeal process and may request a state fair hearing where notice and timeframe requirements under 42 CFR 438.408 have not been met
Deemed Exhaustion
The Plan´s appeal process is deemed exhausted when:
- An enrollee requests a Plan Appeal, verbally or in writing, and does not receive an appeal resolution notice or extension notice from the plan;
- An enrollee requests a Plan Appeal, verbally or in writing, and does not receive an appeal resolution notice or extension notice from the plan within State–specified timeframes; or
- A plan´s appeal resolution or extension notice does not meet noticing requirements identified in 42 CFR §438.408
When can an enrollee ask for a Fair Hearing about plan adverse benefit determination?
- An enrollee may request a state fair hearing:
- After receiving an appeal resolution that an adverse benefit determination has been upheld (Final Adverse Determination)
- After asking for a Plan Appeal, and the time for the plan´s decision has expired, including noticed extension.
- After asking for a Plan Appeal, and receiving an inadequate notice of the plan´s appeal resolution
- After asking for an expedited Plan Appeal, and the time for the plan´s decision has expired (no notification that the request for expedited appeal was denied, and plan handled in regular time)
- After attempting to ask for a Plan Appeal about an adverse benefit determination, and the plan refuses to accept or review the appeal
What if the enrollee asks for a fair hearing without first exhausting the appeal process?
Early Fair Hearing Requests
Does the enrollee have to exhaust the plan´s appeal process if the plan denies/reduces a service before 5/1/18?
- The enrollee´s right to fair hearing will be honored in accordance with the notice the enrollee received.
- For example: the plan issues the current initial adverse determination notice on 4/23/18 with Managed Care Action Taken fair hearing form.
- If the enrollee timely requests a fair hearing on 5/15/18, the hearing will be handled in accordance with April 2018 processes.
- If the enrollee requests a timely appeal on 5/15/18, and the plan issues a new Final Adverse Determination with the new fair hearing request form, the enrollee will have right to request a fair hearing within 120 days of the FAD.
What if enrollee receives an initial adverse determination (after 5/1/18) – and asks for a fair hearing without first exhausting the appeal process?
- The Office of Administrative Hearings will remind enrollees they must ask for a Plan Appeal before asking for a fair hearing.
- However, depending on the circumstances, a fair hearing may still be scheduled.
What if enrollee receives an initial adverse determination (after 5/1/18) – and asks for a fair hearing without first exhausting the appeal process?
- If the plan receives a fair hearing request notification and the appeal was not exhausted:
- In the evidence packet, the first statement should clearly indicate the enrollee received a timely initial adverse determination and did not exhaust the plan´s internal appeal process
- The plan may contact the enrollee, remind them of the need to ask for a Plan Appeal, and ask if they wish to file a Plan Appeal
- The plan may contact the enrollee and attempt to resolve their dispute prior to the fair hearing
- UNDER NO CIRCUMSTANCES MAY A PLAN INTERFERE WITH THE FAIR HEARING PROCESS OR SUGGEST/DIRECT AN ENROLLEE TO WITHDRAW THEIR FAIR HEARING REQUEST
If plan decision is to reduce suspend or stop a service and enrollee wants to keep services the same during appeal
Enrollee may have to pay the cost of care received while waiting for the decision. If enrollee´s health is at risk, ask for fast track review. See plan´s member handbook for full information.
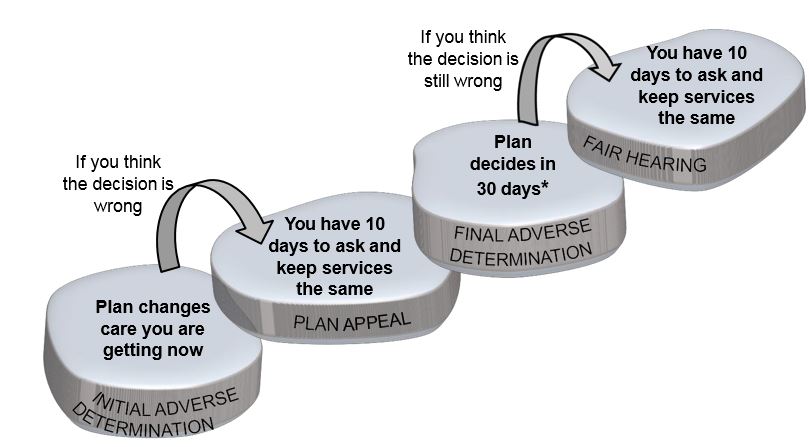
*May take up to 14 days longer if more information is needed
When does the plan have to send notice of an adverse benefit determination 10 Days in advance?
10 Day Notice Requirement
- 42 CFR 438.404 requires the plan to send advance notice when reducing, suspending or terminating a previously authorized service within time frames at 42 CFR 431.211, 431.213, and 431.214
- The notice must be sent at least 10 days before the date of adverse benefit determination, except as permitted under §§431.213 and 431.214.
10 Day Notice Requirement – Exceptions
Notice may be sent not later than the date of adverse benefit determination if–
- The plan has factual information confirming the death of an enrollee;
- The plan receives a clear written statement signed by an enrollee that–
- They no longer wishes services; or
- Gives information that requires termination or reduction of services and indicates that they understand that this must be the result of supplying that information;
- The enrollee has been admitted to an institution where he is ineligible for further services;
- The enrollee´s whereabouts are unknown and the post office returns mail directed to them indicating no forwarding address;
- The enrollee has been accepted for Medicaid by another jurisdiction;
- A change in the level of medical care is prescribed by the enrollee´s physician;
- The date of action will occur in less than 10 days, in accordance with §483.15(b)(4)(ii) and (b)(8), which provides exceptions to the 30 days notice requirements of §483.15(b)(4)(i)
The plan may shorten the period of advance notice to 5 days before the date of action if–
- The plan has facts indicating that action should be taken because of probable fraud by the enrollee; and
- The facts have been verified, if possible, through secondary sources.
10 Day Notice Requirement
- DOH guidance issued December 15, 2017
- 10 Day notice must be provided when the plan determines to reduce, suspend or terminate a previously authorized service during the period for which the service was approved
- 10 Day notice must be provided when the enrollee is in receipt of LTSS or nursing home services (short–term or long–term) and the plan determines to partially approve, suspend, terminate or reduce level or quantity of LTSS or nursing home stay (short–term or long–term) for a subsequent authorization period.
When does enrollee have right to Aid to Continue?
Aid to Continue
- DOH guidance issued December 15, 2017
- Right to Aid to Continue exists when:
- the plan determines to reduce, suspend or terminate a previously authorized service during the period for which the service was approved
- when the enrollee is in receipt of LTSS or nursing home services (short– term or long–term) and the plan determines to partially approve, suspend, terminate or reduce level or quantity of LTSS or nursing home stay (short– term or long–term) for a subsequent authorization period.
- 42 CFR 438.420 provides that an enrollee has right to continued benefits while a Plan Appeal or Fair Hearing is pending, if the enrollee timely requests the Plan Appeal and/or Fair Hearing
- Timely filing means:
- The enrollee must ask for a Plan Appeal within 10 days of the Initial Adverse Determination notice or by the effective date of the decision, whichever is later
- The enrollee must ask for a Fair Hearing within 10 days of the Final Adverse Determination, or by the effective date of the appeal decision, whichever is later
Aid to Continue on Plan Appeal
- New York provides Aid to Continue on an "opt out" basis
- Plans must provide Aid to Continue (AC):
- immediately upon receipt of a Plan Appeal disputing the termination, suspension or reduction of a previously authorized service, filed verbally or in writing within 10 days of the date of the notice of adverse benefit determination (Initial Adverse Determination), or the effective date of the action, whichever is later, unless the enrollee indicates they do not wish their services to continue unchanged.
- Plans must provide Aid to Continue:
- immediately upon receipt of a Plan Appeal disputing the partial approval, termination, suspension or reduction in quantity or level of services authorized for long term services and supports or nursing home stay for a subsequent authorization period, filed verbally or in writing within 10 days of the initial adverse determination, or the effective date of the action, whichever is later, unless the enrollee indicates they do not wish their services to continue unchanged.
Aid Continuing on Plan Appeal
- For example: it is 5/22/18 and an enrollee gets care in a nursing home. The plan initially approved nursing home services from 1/1/18 to 6/30/18. The plan receives a request to keep providing nursing home services from 7/1/18 to 8/31/18. After review, the plan decides to deny the request and issues an Initial Adverse Determination on 5/25/18; services will still end on 6/30/18. On 6/25/18 (before the effective date of the termination), the enrollee requests a Plan Appeal and does not opt out of AC. The plan must provide AC.
- Plans should have policies and procedures to ´self–audit´ that AC is provided upon timely filing of Plan Appeals regarding decisions subject to AC.
Aid to Continue on Plan Appeal
What if the enrollee´s provider requests the Plan Appeal on behalf of the enrollee?
- 42 CFR 438.402 prohibits providers from requesting AC
- The plan must ask the enrollee if they wish to continue their services unchanged until the Appeal decision
- The plan may remind the enrollee that if they lose their appeal, they may be liable for the cost of the services they receive while waiting for the decision.
Aid to Continue on Fair Hearing
What if the enrollee requests a Fair Hearing within 10 days of the plan´s Final Adverse Determination?
- The Office of Administrative Hearings will direct the plan to provide AC in the notification of the fair hearing request ("AC" is indicated in the electronic request) unless the enrollee indicates they do not wish their services continue
What if the enrollee has been deemed to have exhausted the plan´s appeal process and there is no Final Adverse Determination?
- The Office of Administrative Hearings may direct the plan to provide AC in the notification of the fair hearing request ("AC" is indicated in the electronic request)
What if the enrollee did not receive AC during the Plan Appeal, but timely filed a Fair Hearing?
- The Office of Administrative Hearings will direct the plan to provide AC in the notification of the fair hearing request ("AC" is indicated in the electronic request) unless the enrollee indicates they do not wish their services continue
- Plans must provide Aid to Continue:
- immediately as directed by the NYS Office of Administrative Hearings (OAH). The enrollee has a right to AC when they have exhausted the plan´s appeal process and have filed a request for a state fair hearing disputing a termination, suspension or reduction of a previously authorized service, or for all long term services and supports and all nursing home stays, partial approval, termination, suspension or reduction in quantity or level of services authorized for a subsequent authorization period. (The OAH may determine other circumstances warrant the provision of AC, including but not limited to a home bound individual who was denied an increase in home care services.)
- Back to example: Enrollee gets care in a nursing home. The plan initially approved nursing home services from 1/1/18 to 6/30/18. The plan receives a request on 5/22/18 to keep providing nursing home services from 7/1/18 to 8/31/18. After review, the plan decides to deny the request and issues an Initial Adverse Determination on 5/25/18; services will still end on 6/30/18. On 6/25/18 (before the effective date of the termination), the enrollee requests a Plan Appeal and does not opt out of AC. The plan must provide AC.
- The plan reviews the Plan Appeal and determines to uphold their decision. On 6/30/18 the plan issues a Final Adverse Determination. The plan is required to continue services for at least 10 days; the effective date of the termination is 7/10/18.
- this allows for 10 day advanced notice of a termination in a subsequent authorization period for a nursing home stay and
- allows at least 10 days for the enrollee to ask for a Fair Hearing and AC
- The enrollee timely requests a Fair Hearing with AC on 7/1/18. The plan must continue to provide AC.
How long must the plan provide Aid to Continue?
Aid to Continue
- DOH guidance issued December 15, 2017
- NYS Social Service Law 365–a(8) applies
- The plan must continue the enrollee´s services under AC until one of the following occurs:
- the enrollee withdraws the request for AC, the plan appeal or the fair hearing;
- the enrollee fails to request a fair hearing within 10 days of the plan´s Final Adverse Determination or the effective date of the decision, whichever is later;
- OAH determines that the Enrollee is not entitled to aid continuing;
- OAH completes the administrative process and/or issues a fair hearing decision adverse to the enrollee; or
- the provider order has expired, except in the case of a home bound enrollee.
Can the member be held liable for the cost of service received while the Plan Appeal and/or
Fair Hearing was under review?
Aid to Continue – Enrollee Liability
- 42 CFR 438.424 provides that if services were not furnished while the Plan Appeal or Fair Hearing was pending, and the enrollee wins the Plan Appeal or Fair Hearing, the plan must restore services within 72 hours of the decision
- 42 CFR 438.420 provides the enrollee may be held liable for cost of services provided while the Plan Appeal or Fair Hearing was pending
- Plan recoveries must be consistent with the State´s policies on recoveries
- The plan may not begin recovery of these costs from the enrollee until at least 10 days have passed from the Final Adverse Determination, and the enrollee has not requested a Fair Hearing
- If the enrollee requests a Fair Hearing within 120 days of the Final Adverse Determination, the plan must cease any collection activity pending the Fair Hearing decision
Case Files vs Evidence Packets
Case Files – During Plan Appeal
- 42 CFR 438.406 Requires provision of case file free of charge and sufficiently in advance of resolution timeframes for appeals to enrollee and representative.
- The case file includes all medical records and other documents relied upon or generated in connection with the appeal of an adverse benefit determination.
- Case files must be automatically sent to enrollee and their representative after the request for a Plan Appeal and before the plan´s appeal determination. May be combined with acknowledgment
Where should the case file be sent if the enrollee is in an inpatient or facility setting?
- The plan may either:
- Contact the enrollee and verify where to send the case file OR
- The plan may send the case file to the enrollee´s home, the enrollee´s designee, and to the provider (where the provider has accepted responsibility to inform the enrollee/share this information)
Evidence Packet – During Fair Hearing
- Plans must automatically send the enrollee the evidence packet within 10 business days of receipt of notification from OAH that a fair hearing has been requested
- If due to the scheduling of the fair hearing, the evidence packet cannot be prepared at least 5 business days before the hearing, and there is not sufficient time for the evidence packet to be mailed, the plan must provide the enrollee or the enrollee´s representative the evidence packet no later than at the time of the hearing
- The evidence packet contains all of the documents the plan will present at the fair hearing
Case File – During Fair Hearing
- Once the enrollee requests a Fair Hearing, the plan must provide access to the enrollee´s case file upon request.
- If requested, copies of the case file must be provided free of charge within a reasonable time before the date of the hearing
- If request for copies is made less than 5 business days before the hearing, the plan must provide the enrollee and the enrollee´s representative the copies no later than at the time of the hearing
- If requested, the case file must be mailed, if there is insufficient time for the case file to be mailed and received before the date of the hearing, the documents may be presented at the hearing instead of being mailed
Questions?
Thank You!
For More Information Contact: 438reg@health.ny.gov