Information for ALJs
42 CFR 438 & 2018–19 Budget Initiatives Impacting Medicaid Managed Care
Information for ALJs
- Presentation is also available in Portable Document Format (PDF)
Erin Kate Calicchia, Division of Long Term Care
Hope Goldhaber, Division of Health Plan Contracting and Oversight
Patricia Sheppard, Division of Health Plan Contracting and Oversight
Office of Health Insurance Programs
April 20, 2018
Reminders
- Participants have been muted upon entry
- Please submit questions through the Q&A function
- Submit any questions not addressed today to: 438reg@health.ny.gov
Welcome
- This presentation describes initiatives impacting:
- Mainstream Medicaid Managed Care Plans
- HIV Special Needs Plans
- Health and Recovery Plans (HARP)
- Managed Long Term Care Partial Capitation Plans
- Medicaid benefit of Medicaid Advantage Plans; and
- Medicaid benefit of Medicaid Advantage Plus Plans
Agenda
Part I: May 6, 2016 Final Rule by the US Health and Human Services Center for Medicare and Medicaid Services (CMS) for Medicaid and Children´s Health Insurance Programs
- In Lieu of Services
- Service Authorization and Appeals
- Deemed Exhaustion
- Aid to Continue
Part II: FY 2018–19 Health and Medicaid Budget Initiatives Chapter 57 of the Laws of 2018
- Benefit changes
- Long Term Care
Part I: May 6, 2016 Final Rule by the US Health and Human Services Center for Medicare and Medicaid Services (CMS) for Medicaid and Children´s Health Insurance Programs
In Lieu of Services
42 CFR 438.3(e): In Lieu of Services
Cost–Effective Alternative Services aka "In Lieu of Services" (ILS) are alternative services or settings that are not included in the State Plan but are medically appropriate, cost–effective substitutes for covered services or settings.
- Currently only applicable to Mainstream, HIV SNP, HARP
- Plans may volunteer to provide ILS, with DOH approval, to a defined population
- Enrollees may elect to utilize ILS offered by plan
More information at: https://www.health.ny.gov/health_care/managed_care/plans/index.htm
- DOH approved ILS will be posted on the health.ny.gov website and be included in the MMC plan contract Appendix M.
- Web posting will include the start date, service definition, service area, provider type, and population criteria
- MMC plans may not be required to:
- offer same ILS as another plan
- offer ILS to all of their enrollees; may limit to enrollees that meet the ILS criteria
- provide ILS where the enrollee does not agree to use the ILS instead of the Benefit Package service or setting
- MMC plans may be required to:
- provide DOH approved ILS where the enrollee meets the ILS criteria, the ILS is medically necessary, and the enrollee agrees to use the ILS instead of the Benefit Package service or setting
- If the plan is contracted to offer an ILS in their area, the enrollee has right to fair hearing if:
- the plan denies a request for the ILS
- the enrollee believes that they meet the criteria for the ILS
- the enrollee meets the criteria and believes the ILS is medically necessary for them
- the plan requires the enrollee to use or try ILS before providing a service included in the plan´s Benefit Package
Medicaid Managed Care Service Authorization, Appeals and Fair Hearing Under 42 CFR 438
42 CFR 438 Regulation Changes
- Impact New York´s Medicaid managed care service authorization and appeal process for enrollees
- Key changes that start May 1, 2018 in NYS and apply to:
- Medicaid Managed Care
- HIV Special Needs Plan
- Health and Recovery Plan (HARP)
- MLTC Medicaid Plan
- Medicaid Advantage
- Medicaid Advantage Plus
- 42 CFR 438 provisions supersede NYS SSL, NYS PHL, 10 NYCRR 360–10.8, and the Model Contracts
- Because plans also have to follow New York State Law, 42 CFR 438 requirements are blended with State requirements for plans
42 CFR 438 Impact on Service Authorizations and Appeals
| Changed Regulation: | Impact Summary: |
|---|---|
| 438.210(d)(2)(i) | Changes expedited authorization decision/notice timeframe to 72 hours subject to extension |
| 438.210(d)(3) | Refers to SSA § 1927(d)(5)(A) –Requires response by phone or telecommunication device within 24 hours of prior authorization request for "covered outpatient drugs" (as defined in SSA § 1927) |
| 438.400(b) | Defines adverse benefit determination (replaces "action").
|
| 438.400(b)(7) | Adds denial of a request to dispute a financial liability to the definition of adverse benefit determination. |
| 438.402(b) | Only one level of internal appeal is permitted.
|
| 438.402(c)(1)(i) 438.408(f)(1) |
Establishes the enrollees right to a Fair Hearing regarding an adverse benefit determination after receipt of notice under 438.408 (appeal resolution) that the adverse benefit determination has been upheld.
|
| 438.402(c)(1)(i)(A) 438.408(c)(3) 438.408(f)(1)(i) |
Defines ´deemed exhaustion´ – the enrollee has exhausted the plan´s appeal process if the notice and timing requirements of 438.408 (appeal resolution) have not been met and may request a fair hearing.
|
| 438.402(c)(1)(ii) | Adds requirement for enrollee´s written consent for representatives to request plan appeal, grievance or fair hearing on their behalf. Providers may request appeal, grievance or fair hearing but may not request Aid Continuing.
|
| 438.402(c)(2)(ii) | Requires appeals to be filed within 60 calendar days of the date on the Initial Adverse Determination |
| 438.404(b)(2) | Notices identify the right to request and receive, free of charge, copies of all sources of information relevant to the adverse determination
|
| 438.406(b)(5) | Requires provision of case file free of charge and sufficiently in advance of resolution timeframes for appeals to enrollee and representative.
|
| 438.408(b)(3) | Changes expedited appeal determination/notice timeframe to 72 hours |
| 438.408(c)(2) | Plans must make reasonable efforts to give prompt oral notice of an extension and written notice within 2 calendar days |
| 438.408(f) | Provides enrollees 120 calendar days from the date of an adverse appeal resolution notice to request a fair hearing. |
| 438.420 | Provides enrollees the right to Aid Continuing upon timely filing of an appeal – 10 days of the notice of adverse benefit determination or by the effective date of the adverse benefit determination, whichever is later. Provides aid continuing without interruption if the enrollee requests a fair hearing within 10 days of the plan´s sending the written adverse appeal resolution notice.
|
| 438.424(a) | If the fair hearing decision reverses the plan´s adverse benefit determination, and the disputed services were not provided while the appeal and hearing were pending, the plan must authorize or provide the disputed services promptly and as expeditiously as the enrollee´s condition requires but no later than 72 hours from the date the plan receives the fair hearing decision. |
Implementing 42 CFR 438 changes for Medicaid Managed Care Service Authorization, Appeal and Fair Hearing Processes
MMC Template Notices
- 42 CFR 438.10(c)(4)(ii) requires the use of model enrollee notices
- DOH developed new template notices in 2017 with significant input of the Service Authorization and Appeals Stakeholder Workgroup
- Same templates for MMC and MLTC plans
- Separate notices for denials and reductions/suspensions/terminations
- Initial Adverse Determinations include a standardized Plan Appeal form
- Final Adverse Determinations integrates Fair Hearing rights and request form into one notice
- There are now eight model templates for use with MMC/MLTC plans:
- Approval: approval of a services authorization request or whole overturn of an adverse benefit determination on appeal
- Extension: extension for more information during service authorization request review or appeal
- Initial Adverse Determination No AC: notice of adverse benefit determination
- Initial Adverse Determination With AC
- Final Adverse Determination No AC: adverse notice of appeal resolution (adverse benefit determination upheld in whole or in part)
- Final Adverse Determination With AC
- Complaint Resolution
- Complaint Appeal Resolution
- DOH model templates are posted here.
- All 42 CFR 438.10 and 438.210; 438.404 notice content included – plus NYS required content
Are we speaking the same language?
| 42 CFR 438 | MMC Model Contract | Template |
|---|---|---|
| Service Authorization Request | Services Authorization Request | You asked for [service] |
| Adverse Benefit Determination | Action | Decision to deny, reduce, suspend, stop |
| Notice of Adverse Benefit Determination | Notice of Action | Initial Adverse Determination |
| Appeal | Action Appeal | Plan Appeal |
| Notice of Appeal Resolution | Notice of Action Appeal Determination | Final Adverse Determination |
| Continuation of Benefits | Aid Continuing | Keep your services the same |
| External Medical Review | External Appeal | External Appeal |
| Grievance | Complaint | Complaint |
Steps to take if a service request is denied
This is the regular Medicaid Managed Care appeals process. If enrollee´s health is at risk, ask for fast track review. See plan´s member handbook for full information.
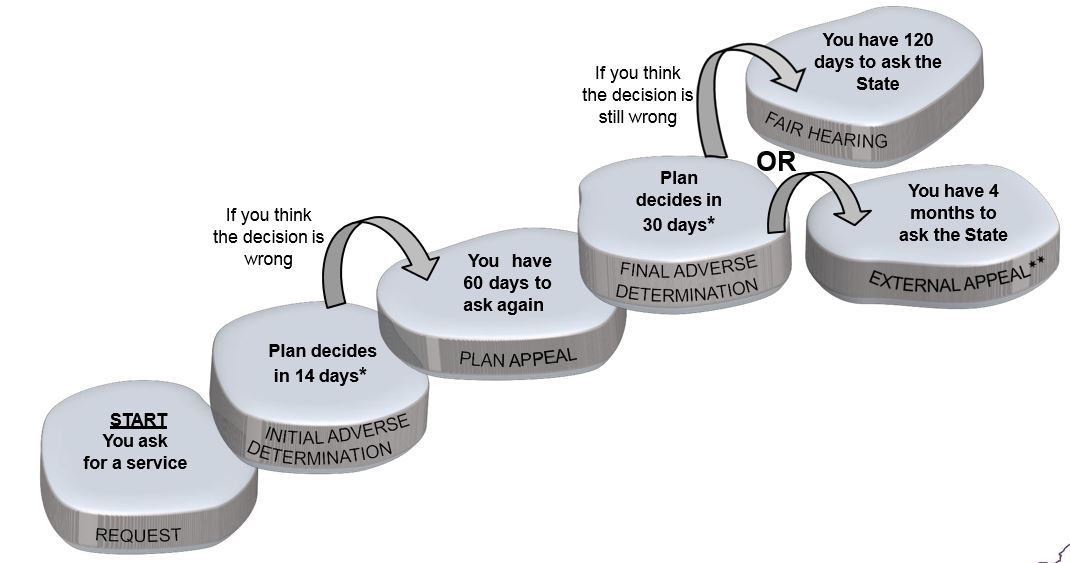
*May take up to 14 days longer if more information is needed
**External appeal is not available for some decisions
If plan decision is to reduce suspend or stop a service and enrollee wants to keep services the same during appeal
Enrollee may have to pay the cost of care received while waiting for the decision. If enrollee´s health is at risk, ask for fast track review. See plan´s member handbook for full information.
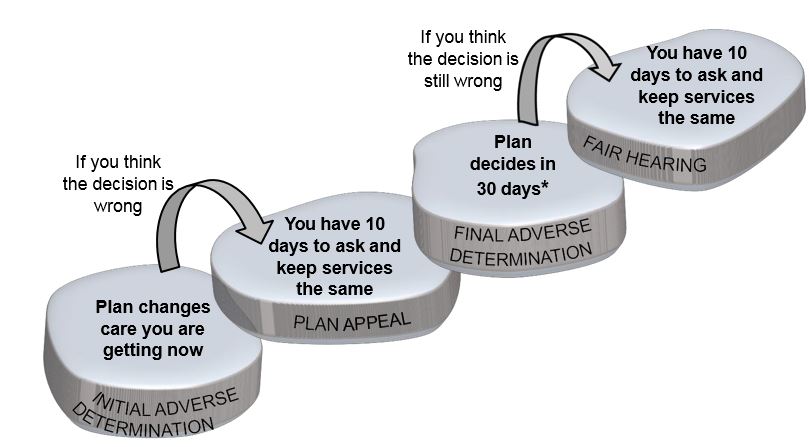
*May take up to 14 days longer if more information is needed
Service Authorization Request
- Plans must respond to a service authorization and provide notice by phone and in writing to the enrollee within 14 days
- If the enrollee´s health is at risk, the plan must Fast Track, and decide in 72 hours
- If the request is for more of, or extension of, a service the enrollee is getting now – the plan will Fast Track these requests
- If the plan needs more information and it´s in the enrollee´s best interest to delay, it may take up to 14 days longer to decide. The plan will notify the enrollee in writing if this happens.
- State law provides special timeframes for some requests; like home care after a hospital admission, and more inpatient substance use disorder treatment.
- These special times are listed in the plan´s member handbook
- Review time frame chart posted here.
- If the plan denies or partially approves the request, the written notice is called the Initial Adverse Determination
Reduction, Suspension, and Termination
- Upon review of the enrollee´s services, the plan may send notice of an Initial Adverse Determination when:
- When the plan makes a decision to reduce, suspend or stop a previously authorized service during the period for which the service was approved
- When the plan makes a decision to partially approve, reduce, suspend or stop the level or quantity of long term services and supports (LTSS) or nursing home stay in the next authorization period
Initial Adverse Determination
- The enrollee´s appeal rights are described in the Initial Adverse Determination, including:
- the specific reason for the decision
- How and when to ask for a Plan Appeal, including an appeal form
- How to get help understanding the notice and asking for an appeal
- If the enrollee thinks the plan´s decision is wrong, they must first ask for a Plan Appeal, and allow time for an answer, BEFORE asking for a Fair Hearing
- The plan´s member handbook has full information about the enrollee´s appeal rights
Plan Appeals
- The enrollee has 60 days from the date of the Initial Adverse Determination to ask for a Plan Appeal
- If the plan is reducing, suspending, or stopping a service, the enrollee has 10 days from the date of the Initial Adverse Determination, or the effective date of the decision, whichever is later, to ask for a Plan Appeal and keep their service the same
- The Plan Appeal can be made by: mail, phone, or fax. The plan may also take requests in–person, by email, or online.
- If the enrollee asks for a Plan Appeal by phone, the enrollee must follow up in writing, unless the appeal will be Fast Tracked.
- The enrollee can choose someone else to ask for the Plan Appeal for them.
- This could be anybody, like a family member, doctor or representative. The enrollee and that person must sign and date a paper saying the enrollee wants that person to ask for them
- If the enrollee already told the plan that someone may represent them, that person may ask for the Plan Appeal
- The plan must write to the enrollee to let them know the plan received the Plan Appeal – this acknowledgement may be combined with the determination notice
- The plan must send the enrollee a copy of the enrollee´s case file. The case file has all the information the plan looked at about the service and the Plan Appeal
Case Files – During Plan Appeal
- 42 CFR 438.406 Requires provision of case file free of charge and sufficiently in advance of resolution timeframes for appeals to enrollee and representative.
- The case file includes all medical records and other documents relied upon or generated in connection with the appeal of an adverse benefit determination.
- Case files must be automatically sent to enrollee and their representative after the request for a Plan Appeal and before the plan´s appeal determination. May be combined with the acknowledgment notice
Plan Appeals
- The plan has 30 days to decide the Plan Appeal
- Plans must send written notice within 2 business days of their decision
- Fast Track appeal are decided in 72 hours
- Enrollees are told the decision by phone. The written notice is sent within 24 hours of the decision.
- If the plan needs more information and its in the enrollee´s best interest to delay, it may take up to 14 days longer to decide. The plan must notify the enrollee in writing if this happens.
Final Adverse Determination
- If the enrollee lost, or partially lost the Plan Appeal, the plan will send the enrollee a Final Adverse Determination notice, including:
- the specific reason for the decision
- Information about the enrollee´s Fair Hearing rights
- For some decisions, the enrollee´s right to External Appeal
- Ways for the enrollee to get help understanding the notice and their rights.
- The plan´s member handbook also has information about the enrollee´s Fair Hearing and External Appeal rights
External Appeals
- An External Appeal is a review of the enrollee´s case by health professionals that do not work for the plan or the state.
- An enrollee can ask for an External Appeal if the plan said the service was:
- not medically necessary;
- experimental or investigational;
- not different from care you can get in the plan´s network; or
- available from a participating provider who has the necessary training and experience.
- Before asking for an External Appeal:
- An enrollee must file a Plan Appeal and get the plan´s Final Adverse Determination; or
- If the enrollee asks for a fast track Plan Appeal, he or she may also ask for a fast track External Appeal at the same time; or
- The enrollee and plan may jointly agree to skip the Plan Appeal process and go directly to the External Appeal.
- The enrollee has 4 months to ask for an External Appeal from getting the Final Adverse Determination, or from agreeing to skip the Plan Appeal process.
- Requesting an External Appeal does not extend timeframes to ask for a Fair Hearing.
- There are no Aid to Continue rights provided by asking for an External Appeal.
- An enrollee can ask for both a Fair Hearing and an External Appeal, but the Fair Hearing decision will be the final answer
Fair Hearings
- An enrollee can ask for a Fair Hearing about a plan decision after going through the Plan Appeal process. This means that the enrollee asked for a Plan Appeal and either:
- Received a Final Adverse Determination; or
- The time for the plan to decide the appeal has expired, including any extensions. If there is no response, or the response is late, the enrollee can ask for Fair Hearing. This is called Deemed Exhaustion
Deemed Exhaustion
The Plan´s appeal process is deemed exhausted when:
- An enrollee requests a Plan Appeal, verbally or in writing, and does not receive an appeal resolution notice or extension notice from the plan;
- An enrollee requests a Plan Appeal, verbally or in writing, and does not receive an appeal resolution notice or extension notice from the plan within State–specified timeframes; or
- A plan´s appeal resolution or extension notice does not meet noticing requirements identified in 42 CFR §438.408
Fair Hearings
- If the enrollee thinks the Plan Appeal decision is still wrong:
- The enrollee has 120 days from the date of the Final Adverse Determination to ask for a Fair Hearing
- If the plan is reducing, suspending, or stopping a service, the enrollee has 10 days from the date of the Final Adverse Determination, or the effective date of the decision, whichever is later, to ask for a Fair Hearing and keep their service the same
- The Fair Hearing decision is final
- 42 CFR 438.424 provides that if the services were not furnished during the review, if the enrollee wins the Plan Appeal or Fair Hearing, the plan must provide or approve the enrollee´s services within 72 hours of the decision, or sooner if the enrollee´s health requires it.
Frequently Asked Questions:
42 CFR 438 Medicaid Managed Care Service Authorization, Appeal, Deemed Exhaustion and Aid to Continue
Adverse Benefit Determination
42 CFR 438.400 defines as any of the following:
- The denial or limited authorization of a requested service, including determinations based on the type or level of service, requirements for medical necessity, appropriateness, setting, or effectiveness of a covered benefit
- The reduction, suspension, or termination of a previously authorized service.
- The denial, in whole or in part, of payment for a service
- The failure to provide services in a timely manner, as defined by the State
- The failure of an MCO, PIHP, or PAHP to act within the timeframes provided in §438.408(b)(1) and (2) regarding the standard resolution of grievances and appeals
- For a resident of a rural area with only one MCO, the denial of an enrollee´s request to exercise his or her right, under §438.52(b)(2)(ii), to obtain services outside the network
- The denial of an enrollee´s request to dispute a financial liability, including cost sharing, copayments, premiums, deductibles, coinsurance, and other enrollee financial liabilities
These events are adverse benefit determinations whether or not the plan sends notice
When can an enrollee ask for a Plan Appeal of an Adverse Benefit Determination?
- An enrollee can ask for a Plan Appeal of an Adverse Benefit Determination*:
- Up to 60 days from the date of the Initial Adverse Determination
- When the enrollee requests a service, and the plan does not respond or response is late
- When the plan made an adverse benefit determination without adequate notice, or notice was late
- MMC/HARP/HIV SNP only: After filing a complaint that a provider denied a service (which must be handled as a service authorization request), and the plan does not respond, or the response is late
* Not an exhaustive list of appeal rights; enrollees have right to appeal other plan decisions
When can an enrollee ask for a Fair Hearing about plan adverse benefit determinations?
- An enrollee may request a state fair hearing:
- After receiving an appeal resolution that an adverse benefit determination has been upheld (Final Adverse Determination)
- After asking for a Plan Appeal, and the time for the plan´s decision has expired, including noticed extension.
- After asking for a Plan Appeal, and receiving an inadequate notice of the plan´s appeal resolution
- After asking for an expedited Plan Appeal, and the time for the plan´s decision has expired (no notification that the request for expedited appeal was denied, and plan handled in regular time)
- After attempting to ask for a Plan Appeal about an adverse benefit determination, and the plan refuses to accept or review the appeal
What if the enrollee asks for a fair hearing without first exhausting the appeal process?
Does the enrollee have to exhaust the plan´s appeal process if the plan denies/reduces a service before 5/1/18?
- The enrollee´s right to fair hearing will be honored in accordance with the notice the enrollee received.
- For example: the plan issues the current initial adverse determination notice on 4/23/18 with Managed Care Action Taken fair hearing form.
- If the enrollee timely requests a fair hearing on 5/15/18, the hearing will be handled in accordance with April 2018 processes.
- If the enrollee requests a timely appeal on 5/15/18, and the plan issues a new Final Adverse Determination with the new fair hearing request form, the enrollee will have right to request a fair hearing within 120 days of the FAD.
What if enrollee receives an initial adverse determination (after 5/1/18) – and asks for a fair hearing without first exhausting the appeal process?
- The Office of Administrative Hearings will remind enrollees they must ask for a Plan Appeal before asking for a fair hearing.
- However, depending on the circumstances, a fair hearing may still be scheduled.
What if enrollee receives an initial adverse determination (after 5/1/18) – and asks for a fair hearing without first exhausting the appeal process?
- If the plan receives a fair hearing request notification and the appeal was not exhausted:
- In the evidence packet, the first statement should clearly indicate the enrollee received a timely initial adverse determination and did not exhaust the plan´s internal appeal process
- The plan may contact the enrollee, remind them of the need to ask for a Plan Appeal, and ask if they wish to file a Plan Appeal
- The plan may contact the enrollee and attempt to resolve their dispute prior to the fair hearing
- UNDER NO CIRCUMSTANCES MAY A PLAN INTERFERE WITH THE FAIR HEARING PROCESS OR SUGGEST/DIRECT AN ENROLLEE TO WITHDRAW THEIR FAIR HEARING REQUEST
When does the plan have to send notice of an adverse benefit determination 10 Days in advance?
10 Day Notice Requirement
- 42 CFR 438.404 requires the plan to send advance notice when reducing, suspending or terminating a previously authorized service within time frames at 42 CFR 431.211, 431.213, and 431.214
- The notice must be sent at least 10 days before the date of adverse benefit determination, except as permitted under §§431.213 and 431.214.
10 Day Notice Requirement – Exceptions
Notice may be sent not later than the date of adverse benefit determination if–
- The plan has factual information confirming the death of an enrollee;
- The plan receives a clear written statement signed by an enrollee that–
- They no longer wish services; or
- Gives information that requires termination or reduction of services and indicates that they understand that this must be the result of supplying that information;
- The enrollee has been admitted to an institution where he is ineligible for further services;
- The enrollee´s whereabouts are unknown and the post office returns mail directed to them indicating no forwarding address;
- The enrollee has been accepted for Medicaid by another jurisdiction;
- A change in the level of medical care is prescribed by the enrollee´s physician;
- The date of action will occur in less than 10 days, in accordance with §483.15(b)(4)(ii) and (b)(8), which provides exceptions to the 30 days´ notice requirements of §483.15(b)(4)(i)
The plan may shorten the period of advance notice to 5 days before the date of action if–
- The plan has facts indicating that action should be taken because of probable fraud by the enrollee; and
- The facts have been verified, if possible, through secondary sources.
10 Day Notice Requirement
- DOH guidance issued December 15, 2017
- 10 Day notice must be provided when the plan determines to reduce, suspend or terminate a previously authorized service during the period for which the service was approved
- 10 Day notice must be provided when the enrollee is in receipt of LTSS or nursing home services (short–term or long–term) and the plan determines to partially approve, suspend, terminate or reduce level or quantity of LTSS or nursing home stay (short–term or long–term) for a subsequent authorization period.
When does enrollee have right to Aid to Continue?
- DOH guidance issued December 15, 2017
- Right to Aid to Continue exists when:
- the plan determines to reduce, suspend or terminate a previously authorized service during the period for which the service was approved
- when the enrollee is in receipt of LTSS or nursing home services (short– term or long–term) and the plan determines to partially approve, suspend, terminate or reduce level or quantity of LTSS or nursing home stay (short– term or long–term) for a subsequent authorization period.
Aid to Continue
- 42 CFR 438.420 provides that an enrollee has right to continued benefits while a Plan Appeal or Fair Hearing is pending, if the enrollee timely requests the Plan Appeal and/or Fair Hearing
- Timely filing means:
- The enrollee must ask for a Plan Appeal within 10 days of the Initial Adverse Determination notice or by the effective date of the decision, whichever is later
- The enrollee must ask for a Fair Hearing within 10 days of the Final Adverse Determination, or by the effective date of the appeal decision, whichever is later
Aid to Continue on Plan Appeal
- New York provides Aid to Continue on an "opt out" basis
- Plans must provide Aid to Continue (AC):
- immediately upon receipt of a Plan Appeal disputing the termination, suspension or reduction of a previously authorized service, filed verbally or in writing within 10 days of the date of the notice of adverse benefit determination (Initial Adverse Determination), or the effective date of the action, whichever is later, unless the enrollee indicates they do not wish their services to continue unchanged.
- Plans must provide Aid to Continue:
- immediately upon receipt of a Plan Appeal disputing the partial approval, termination, suspension or reduction in quantity or level of services authorized for long–term services and supports or nursing home stay for a subsequent authorization period, filed verbally or in writing within 10 days of the initial adverse determination, or the effective date of the action, whichever is later, unless the enrollee indicates they do not wish their services to continue unchanged.
Aid Continuing on Plan Appeal
- For example: it is 5/22/18 and an enrollee gets care in a nursing home. The plan initially approved nursing home services from 1/1/18 to 6/30/18. The plan receives a request to keep providing nursing home services from 7/1/18 to 8/31/18. After review, the plan decides to deny the request and issues an Initial Adverse Determination on 5/25/18; services will still end on 6/30/18. On 6/25/18 (before the effective date of the termination), the enrollee requests a Plan Appeal and does not opt out of AC. The plan must provide AC.
Aid to Continue on Plan Appeal
What if the enrollee´s provider requests the Plan Appeal on behalf of the enrollee?
- 42 CFR 438.402 prohibits providers from requesting AC
- The plan must ask the enrollee if they wish to continue their services unchanged until the Appeal decision
- The plan may remind the enrollee that if they lose their appeal, they may be liable for the cost of the services they receive while waiting for the decision.
Aid to Continue on Fair Hearing
What if the enrollee requests a Fair Hearing within 10 days of the plan´s Final Adverse Determination?
- As appropriate, the Office of Administrative Hearings will direct the plan to provide AC unless the enrollee indicates they do not wish their services continue
What if the enrollee has been deemed to have exhausted the plan´s appeal process and there is no Final Adverse Determination?
- As appropriate, the Office of Administrative Hearings may direct the plan to provide AC
What if the enrollee did not receive AC during the Plan Appeal, but timely filed a Fair Hearing?
- As appropriate, the Office of Administrative Hearings will direct the plan to provide AC unless the enrollee indicates they do not wish their services continue
- Plans must provide Aid to Continue:
- immediately as directed by the NYS Office of Administrative Hearings (OAH). The enrollee has a right to AC when they have exhausted the plan´s appeal process and have filed a request for a state fair hearing disputing a termination, suspension or reduction of a previously authorized service, or for all long term services and supports and all nursing home stays, partial approval, termination, suspension or reduction in quantity or level of services authorized for a subsequent authorization period. (The OAH may determine other circumstances warrant the provision of AC, including but not limited to a home bound individual who was denied an increase in home care services.)
- Back to example: Enrollee gets care in a nursing home. The plan initially approved nursing home services from 1/1/18 to 6/30/18. The plan receives a request on 5/22/18 to keep providing nursing home services from 7/1/18 to 8/31/18. After review, the plan decides to deny the request and issues an Initial Adverse Determination on 5/25/18; services will still end on 6/30/18. On 6/25/18 (before the effective date of the termination), the enrollee requests a Plan Appeal and does not opt out of AC. The plan must provide AC.
- The plan reviews the Plan Appeal and determines to uphold their decision. On 6/30/18 the plan issues a Final Adverse Determination. The plan is required to continue services for at least 10 days; the effective date of the termination is 7/10/18.
- this allows for 10–day advanced notice of a termination in a subsequent authorization period for a nursing home stay and
- allows at least 10 days for the enrollee to ask for a Fair Hearing and AC
- The enrollee timely requests a Fair Hearing with AC on 7/1/18. The plan must continue to provide AC.
How long must the plan provide Aid to Continue?
- DOH guidance issued December 15, 2017
- NYS Social Service Law 365–a(8) applies
- The plan must continue the enrollee´s services under AC until one of the following occurs:
- the enrollee withdraws the request for AC, the plan appeal or the fair hearing;
- the enrollee fails to request a fair hearing within 10 days of the plan´s Final Adverse Determination or the effective date of the decision, whichever is later;
- OAH determines that the Enrollee is not entitled to aid continuing;
- OAH completes the administrative process and/or issues a fair hearing decision adverse to the enrollee; or
- the provider order has expired, except in the case of a home bound enrollee.
Can the member be held liable for the cost of service received while the Plan Appeal and/or
Fair Hearing was under review?
- 42 CFR 438.420 provides the enrollee may be held liable for cost of services provided while the Plan Appeal or Fair Hearing was pending
- Plan recoveries must be consistent with the State´s policies on recoveries
- The plan may not begin recovery of these costs from the enrollee until at least 10 days have passed from the Final Adverse Determination, and the enrollee has not requested a Fair Hearing
- If the enrollee requests a Fair Hearing within 120 days of the Final Adverse Determination, the plan must cease any collection activity pending the Fair Hearing decision
Summary of Changes From 42 CFR 438
- New time frame for Fast Track initial decisions: 72 hours
- Outpatient Pharmacy** 24 hours
- If no notice of adverse benefit determination, or the notice is late, the enrollee may file a Plan Appeal
- Enrollee must first ask for a Plan Appeal and allow time for response, BEFORE asking for a Fair Hearing
- Enrollee has 60 days from the Initial Adverse Determination to ask for a Plan Appeal
- If plan decision is to reduce, suspend or stop a service, an enrollee must ask for a Plan Appeal within 10 days of the Initial Adverse Determination to keep their services unchanged until the decision (aid to continue)
- The enrollee must provide written authorization to designate someone, including their provider, to ask for a Plan Appeal or complaint on their behalf
- New time frame for Fast Track Plan Appeal decisions: 72 hours
- Enrollee has 120 days from Final Adverse Determination to ask for a Fair Hearing
- If Plan Appeal decision is to reduce, suspend or stop a service, an enrollee must ask for a Fair Hearing within 10 days of the Final Adverse Determination to keep their services unchanged until the decision (aid to continue)
- If no response to Plan Appeal or if response is late, the enrollee may ask for a Fair Hearing
- If Enrollee wins Plan Appeal or Fair Hearing, plan must authorize services in 72 hours
**as defined by SSA §1927
Part II: FY 2018–19 Health and Medicaid Budget Initiatives
Chapter 57 of the Laws of 2018
Benefit Changes
Physical Therapy Cap
Effective July 1, 2018, the physical therapy cap under both Medicaid fee–for–service and mainstream managed care will be increased from 20 visits to 40 visits per year.
Telehealth
Effective July 1, 2018.
Telehealth Providers were Expanded to Include:
- Residential health care facilities serving special needs populations;
- Credentialed alcoholism and substance abuse counselors credentialed by the Office of Alcoholism and Substance Abuse Services or by a credentialing entity approved by such office, pursuant to Section 19.07 of the Mental Hygiene law;
- Providers authorized to provide services and service coordination under the Early Intervention Program, pursuant to Article 25 of Public Health law;
- Clinics licensed or certified under Article 16 of the Mental Hygiene law;
- Certified and non–certified day and residential programs funded or operated by the Office for People with Developmental Disabilities; and
- Any other provider as determined by the Commissioner pursuant to regulation or, in consultation with the Commissioner, by the Commissioner of the Office of Mental Health, the Commissioner of the Office of Alcoholism and Substance Abuse Services or the Commissioner of the Office for People with Developmental Disabilities.
Originating Sites were Expanded to Include:
- Certified and non–certified day and residential programs funded or operated by the Office for People with Developmental Disabilities.
- The patient´s place of residence located within the state of New York or other temporary location located within or outside the state of New York.
Remote Patient Monitoring (RPM) was Expanded to Include:
- Additional interaction, triggered by previous RPM transmissions, such as interactive queries conducted through communication technologies or by telephone.
- The Department of Health, the Office of Mental Health, the Office of Alcoholism and Substance Abuse Services, and the Office for People with Developmental Disabilities will issue a single guidance document to assist consumers, providers and health plans in identifying and understanding any differences in telehealth regulations and policies issued by the agencies.
Long Term Care
Long Term Services and Supports (LTSS)
LTSS: facility and community based long term services and supports, including but not limited to short– and long–term nursing home stays; adult day care services; private duty nursing in the home; therapies in the home; home health aide services; personal care services; and consumer directed personal assistance services
Mainstream Managed Care
- LTSS is included in the comprehensive Benefit Package for Mainstream Managed Care Plan, HIV SNP and HARP (no long–term NH)
Managed Long Term Care Plans
- only enroll individuals who need community based LTSS
Receipt of LTSS does not automatically mean the enrollee is in an MLTC plan
2018–2019 Enacted Budget – DLTC Summary
- Limit the number of LHCSA (Licensed Home Care Services Agencies) that Contract with MLTC Plans
- Require Continuous 120 days of CBLTC for Plan Eligibility
- Restrict MLTC Members from Transitioning Plans for 12 Months After Initial Enrollment
- Authorization vs. Utilization Adjustment for MLTC
2018–2019 Enacted Budget – NH Benefit
- Limit MLTC Nursing Home Permanent Placement Benefit to Three Months (3 Prong– Approach)
- Closing the front door to new permanent placement NH residents (returning the exclusion)
- Individuals will no longer be auto assigned upon entry to the NH
- Limitation of the Partial Cap NH Benefit to 3 months for permanently placed enrollees once Medicare is maximized
- DOH is working with New York Medicaid CHOICE to get notices to all enrollees on the change
- DOH will provide plans with a model notice to enrollees in NH
- Transition of NH enrollees from MLTC to FFS
- Enrollees that are permanently placed as of April 1 will be disenrolled in July 2018
- Closing the front door to new permanent placement NH residents (returning the exclusion)