Partnership Plan Section 1115 Quarterly Report and Annual Report
- Report also available in Portable Document Format (PDF)
Demonstration Year: 16 (10/1/2013 – 9/30/2014)
Federal Fiscal Quarter: 4 (7/01/2014 – 9/30/2014)
I. Introduction
In July 1997, New York State received approval from the Centers for Medicare and Medicaid Services (CMS), for its Partnership Plan Medicaid Section 1115 Demonstration. The Partnership Plan Demonstration was originally authorized for a five–year period and has been extended several times, most recently through December 31, 2014. The primary purpose of the initial Demonstration was to enroll a majority of the State´s Medicaid population into managed care.
There have been a number of amendments to the Partnership Plan Demonstration since its initial approval in 1997.
CMS approved an extension on September 29, 2006 of New York´s 1115 Partnership Plan Waiver for the period beginning October 1, 2006 and ending September 30, 2010. CMS subsequently approved a series of short–term extensions while negotiations continued on renewing the waiver into 2014. CMS approved three waiver amendments on September 30, 2011, March 30, 2012 and August 31, 2012, incorporating changes resulting from the recommendations of Governor Cuomo´s Medicaid Redesign Team.
New York State´s Federal–State Health Reform Partnership (F–SHRP) Medicaid Section 1115 Demonstration expired on March 31, 2014. In accordance with the April 1, 2011 Special Terms and Conditions (STC) Number 50, a final report for the F–SHRP demonstration was submitted to CMS on June 30, 2014. The state has contracted with Rockefeller Institute of Government (RIG) for the F–SHRP demonstration final evaluation report which is due to CMS by April 1, 2015. Populations in the F–SHRP were transitioned into the 1115 Partnership Plan Waiver.
On May 28, 2014, New York State submitted an application requesting an extension of the Partnership Plan 1115 Demonstration for five years. On May 30, 2014, CMS accepted New York´s application as completed and posted the application for a 30 day public comment period. This application will extend the Demonstration until December 31, 2019, thus allowing New York to reinvest federal savings generated by the Medicaid Redesign Team reform initiatives, and to reinvest in the state´s health care system currently authorized by the Partnership Plan.
II. Enrollment: Fourth Quarter
Partnership Plan – Enrollment as of September 2014
| Demonstration Populations (as hard coded in the CMS 64) | Current Enrollees (to date) | # Voluntary Disenrolled in Current Quarter | # Involuntary Disenrolled in Current Quarter |
|---|---|---|---|
| Population 1 – TANF Child 1 – 20 years in Mandatory Counties as of 10/1/06 | 1,524,452 | 16,648 | 76,590 |
| Population 2 – TANF Adults aged 21 through 64 in mandatory MC counties as of 10/1/06Population 2 – TANF Adults 21 – 64 years in Mandatory Counties as of 10/1/06 | 365,140 | 5,799 | 20,872 |
| Population 3 – TANF Child 1 – 20 (´new´ MC Enrollment) | 86,793 | 1,373 | 4,773 |
| Population 4 – TANF Adults 21 – 64 (´new´ MC Enrollment) | 21,144 | 464 | 1,823 |
| Population 5 – Safety Net Adults | 992,217 | 15,565 | 33,256 |
| Population 6 – Family Health Plus Adults with Children | 156,913 | 5,137 | 25,944 |
| Population 7 – Family Health Plus Adults without Children | 41 | 21 | 50 |
| Population 8 – Disabled Adults and Children 0 – 64 (SSI 0–64 Current MC) | 55,189 | 1,069 | 295 |
| Population 9 – Disabled Adults and Children 0 – 64 (SSI 0–64 New MC) | 249,149 | 7,159 | 1,943 |
| Population 10 – Aged or Disabled Elderly (SSI 65+ Current MC) | 3,350 | 249 | 41 |
| Population 11 – Aged or Disabled Elderly (SSI 65+ New MC) | 48,672 | 2,444 | 554 |
Partnership Plan Waiver – Voluntary and Involuntary Disenrollment
| Total # Voluntary Disenrollments in Current Demonstration Year1 | 55,928 |
Reasons for voluntary disenrollment´s include: enrollment in another plan; approved enrollee request to qualify as either exempt or excluded; relocation to residence outside county of enrollment; and Local Department of Social Services (LDSS) approval to disenroll based upon appropriate cause.
| Involuntary Disenrollments | |
|---|---|
| Total # Involuntary Disenrollments in Current Demonstration Year1 | 166,141 |
Reasons for involuntary disenrollment´s include: loss of Medicaid eligibility; eligibility transfers between Family Health Plus (FHPlus) and Medicaid; inappropriate enrollment and death.
III. Outreach/Innovative Activities
The New York State Department of Health (the Department), Maximus and the local departments of social services (LDSS) continue to provide education and outreach in the areas of enrollment and health plan selection to Medicaid eligible individuals that are not enrolled in managed care.
- Mandatory Managed Care Expansion
- The expansion of mandatory Medicaid managed care is complete, with programs operating in all counties of the state, including New York City.
- Outreach Activities
- The total Medicaid eligible population in New York City is approximately 3.2 million. Currently, 2.6 million are enrolled in a managed care plan, including eligible SSI recipients.
- New York Medicaid Choice (NYMC) Field Customer Services Representatives (FCSRs) were conducting outreach activities at 6 HIV/AIDS Services Administration (HASA) sites, 12 Medicaid offices and 17 Job Centers.
- The Education and Enrollment Driven Referral (EED) process was responsible for 88% of 14,000 consumers engaged by NYMC in the last quarter.
- The overall activities at Medicaid offices remained constant averaging five consumers per work session. A work session covers a half day of work activities.
- A total of 2,481 presentations were scheduled by NYMC. Of these, 556 or 23% of the total scheduled presentations were observed by the Contract Monitoring Unit (CMU).
IV. Operational/Policy Developments/Issues
A. Partnership Plan Waiver Amendments
CMS granted approval of several amendments to the Waiver effective January 1, 2014. These changes coincided with continued implementation of the Affordable Care Act.
CMS approved an expenditure authority to allow the state to claim federal matching dollars for the DSHP, which provides premium subsidies to parents and caretaker relatives with incomes between 138%–150% Federal Poverty Level (FPL), who enroll in a Qualified Health Plan (QHP) using Advanced Premium Tax Credits (APTC). Eligibility for this premium assistance is determined by New York´s Marketplace, and the majority of enrollees were determined during the open enrollment period that concluded April 15, 2014.
An additional DSHP was approved that allows federal matching dollars to provide FHPlus benefits to parents and caretaker relatives up to 150% FPL, for continued funding through the full phase–out of the program. The transition is ongoing, and all recipients will be out of the program by December 31, 2014.
B. Health Plans
- Effective July 1, 2014, WellCare of New York, Inc. expanded its Medicaid Managed Care and FHPlus contract service area to include Erie County.
- Effective September 1, 2014, New York State Catholic Health Plan, Inc. expanded its Medicaid Managed Care and FHPlus contract service area to include Jefferson County.
- Changes to Certificates of Authority (COA):
- Fidelis–COA updated 09/01/2014– approval for Medicaid, FHPlus, CHPlus expansion into Jefferson County.
C. Surveillance Activities
Surveillance activity for 4th Quarter FFY 2013–2014 (7/1/14 to 9/30/14) included the following:
- Hudson Health Plan, Inc.: A Targeted Operational Survey completed September 30, 2014. Plan was found to be in compliance.
- MetroPlus and MetroPlus HIV SNP: A joint Targeted Operational Survey was completed June 23, 2014. The Plans were found to be in compliance.
- Member Services Focus Surveys were completed on eleven (11) Managed Care Plans during the 4th Quarter FFY 2014.
- Seven of 11 plans were found to be in compliance: MetroPlus Health Plan, Inc. – SNP, VNS Choice – SNP, WellCare of New York, Inc., United Healthcare of New York, Inc., Hudson Health Plan, Inc., Affinity Health Plan, Inc., and HealthFirst PHSP, Inc.
- Four of 11 plans were issued statements of deficiency and acceptable Plans of Correction have been received: MetroPlus Health Plan, Inc., AMERIGROUP New York, LLC, Amida Care, Inc., and New York State Catholic Health Plan, Inc.
- Provider Directory Information Surveys were completed on fifteen (15) Managed Care Plans during the 4th Quarter FFY 2014.
- Nine of 15 were found to be in compliance: AMERIGROUP New York, LLC, HealthFirst PHSP, Inc., Hudson Health Plan, Inc., MetroPlus Health Plan, Inc., MVP Health Plan, Inc., New York State Catholic Health Plan, Inc., Today´s Option of New York, Inc., United Healthcare of New York, Inc., and WellCare of New York, Inc.
- Six of 15 were issued Statements of Deficiency and Acceptable Plans of Correction have been received: Amida Care, Inc., Capital District Physician´s Health Plan, Inc., Excellus Health Plan, Inc., Independent Health Association, Inc., Univera Community Health, Inc., and VNS Choice – SNP.
- Provider Participation –Directory Surveys were completed on nine Managed Care Plans during the 4th Quarter FFY 2014.
- One of nine was found to be in compliance: MetroPlus Health Plan, Inc
- Eight of nine were issued Statements of Deficiency and Acceptable Plans of Correction have been received: Amida Care, Inc., Capital District Physician´s Health Plan, Inc., Excellus Health Plan, Inc., Independent Health Association, Inc., Today´s Option of New York, Inc., Univera Community Health, Inc., VNS Choice – SNP, and WellCare of New York, Inc.
V. Waiver Deliverables
A. Medicaid Eligibility Quality Control (MEQC) Reviews
- MEQC 2009 – Review of Medicaid Eligibility Determinations and Re–Determinations for Single and Childless Couple Individuals Determined Ineligible for Temporary Assistance
- With CMS approval, the Pacific Health Policy Group (PHPG), the contractor hired to assist the Department with multiple MEQC reviews, implemented an alternate approach for generating the necessary universes of cases. A revised approach was necessary because the availability of DOH system staff continued to be limited due to other system priorities (i.e., system work related to ACA and the NY State of Health Marketplace). Implementation of the revised approach began in September 2013. The process continued for several quarters because the alternate universe identification process was labor intensive and very time consuming.
Initial, peer and supervisory reviews were completed for almost all of the cases during the quarter ending September 30, 2014. During the next quarter, it is anticipated that quality control reviews will be conducted, and preliminary findings will be provided to the appropriate local Department of Social Services (LDSS) offices for feedback.
- With CMS approval, the Pacific Health Policy Group (PHPG), the contractor hired to assist the Department with multiple MEQC reviews, implemented an alternate approach for generating the necessary universes of cases. A revised approach was necessary because the availability of DOH system staff continued to be limited due to other system priorities (i.e., system work related to ACA and the NY State of Health Marketplace). Implementation of the revised approach began in September 2013. The process continued for several quarters because the alternate universe identification process was labor intensive and very time consuming.
- MEQC 2010 – Review of Medicaid Eligibility Determinations and Redeterminations for Persons Identified as Having a Disability
- A summary report was forwarded to the regional CMS office on January 31, 2014.
- MEQC 2011 – Review of Medicaid Self Employment Calculations
- A summary report was forwarded to the regional CMS office on June 28, 2013.
- MEQC 2012 – Review of Medicaid Income Calculations and Verifications
- A summary report was forwarded to the regional CMS office on July 25, 2013.
- MEQC 2013 – Review of Documentation Used to Assess Immigration Status and Coding
- A summary report was forwarded to the regional CMS office on August 1, 2014.
B. Benefit Changes/Other Program Changes
- Twelve Month Continuous Coverage
- In 2007, revisions were made to Chapter 58 of the New York State Social Services Law to provide continuous coverage for certain Medicaid beneficiaries for a period of twelve months from the date of initial eligibility and subsequent redetermination of eligibility. The intent of the policy is to provide stability and continuity of coverage and care to certain adults in the same way it has for children on Medicaid. Twelve months continuous coverage was effective January 1, 2014, for New York´s Marketplace for most Medicaid beneficiaries in Modified Adjusted Gross Income (MAGI) categories, including pregnant women, parents/caretaker relatives, children and other adults under age 65.
C. Federally Qualified Health Services (FQHC) Lawsuit
- The Court issued a decision October 7th that granted summary judgment to the Department on several issues. In the first instance, the Court held that the Department could require dental visits to FQHCs to be bundled for the purpose of reimbursement. "Bundling” is the practice of offering a single reimbursement payment for all services provided during a single patient visit. The Department sought to require all dental services that could be provided during a single patient visit, actually be performed during such visit. The Court agreed. The Court also upheld NY specific PPS rates for offsite and group psychotherapy services. Delving deeper into reimbursement issues, the Court found that the Department appropriately calculated the wrap payment for FQHC´s and allowed the Department to do so prospectively. The wrap payment is the difference between the PPS payment that the FQHC is statutorily entitled to and the payment negotiated by the Managed Care Organization. The Court next addressed denials of payment by MCOs and the Department´s responsibility thereof. The Court found that where an MCO denies payment, the Department must provide a complaint procedure for the aggrieved FQHC. Further, when an FQHC has been denied payment, the Department is responsible for the full PPS rate and not just the wrap payment. The Department had submitted a remedial plan for complaint resolution that was approved by the lower court and that plan was not disturbed by the Second Circuit. The Second Circuit returned to the lower court the question of how payment denials may affect the prospective wrap payment calculation, but otherwise upheld the lower court in all respects. Presently, the Department will not be appealing this decision; however, the plaintiff has filed for a rehearing and en banc review. If such review is granted, the Department will object to the adverse rulings related to FQHC complaint resolution and reimbursement of the PPS rate for improperly denied claims.
D. Managed Long Term Care Program
- All MLTCP models provide a person–centered plan of care, integration of health care, environmental and social services and a supportive transition from the previous, fragmented, FFS process to coordinated managed care.
- Accomplishments
- Expanded MLTCP availability. During the period July 2014 through September 2014 availability was expanded by approving one Service Area Expansion that extended to three new counties, along with one new Certificate of Authority. Total expansion of availability for the annual period of October 2013 through September 2014: two new Certificates of Authority and eight Service Area Expansions.
- New York´s Enrollment Broker, NYMC, conducted the MLTC Post Enrollment Outreach Survey which contains specific questions specifically designed to measure the rate at which consumers are able to maintain their relationship with their personal care aide or home attendant. For the period July 2014 through September 2014 post enrollment surveys were completed for 652 enrollees and 80% of respondents are receiving services from the same caregivers. Post enrollment surveys conducted over the annual period October 2013 through September 2014 reflect that 82% of respondents received services from the same caregivers.
- During the period July 2014 through September 2014 the complaint hotline staffing was further expanded, and the unit is now referred to as the Technical Assistance Center (TAC). A BML email address was created to enhance access to the TAC, and a plan will be formulated to communicate this electronic access to appropriate parties. Internal TAC quality protocols were developed to monitor consistency of investigations and timely resolution. This will be utilized to identify areas for improvement. Over the annual period October 2013 through September 2014, the TAC has developed internal operational protocols to ensure all staff are trained and receive information on pertinent changes in a timely and uniform basis.
- Activity for the period July 2014 through September 2014: the original MLTC timeline to achieve transition to mandatory transition throughout the State by December 2014 was revised and no additional counties transitioned during the month of July 2014. A revised transition timeline was submitted to CMS which projects transition for the remainder of the state to conclude during February 2015. With CMS approval, we have begun expansion of mandatory MLTC to include Dutchess, Montgomery, Broome, Fulton, and Schoharie during August 2014; Delaware and Warren during September 2014. CMS approval was requested to transition Niagara, Madison, and Oswego during October 2014; and planning with the districts and MLTC plans commenced.
- Annual activity during the period October 2013 through September 2014 reflects mandatory transition activities to MLTC as follows:
- October 2013: continued activity in Rockland and Orange, which began during September 2013;
- December 2013: Albany, Erie, Monroe, Onondaga;
- April 2014: Columbia, Putnam, Sullivan, Ulster;
- May 2014: Rensselaer, Cayuga, Herkimer, Oneida;
- June 2014: Greene, Schenectady, Washington, Saratoga;
- August 2014: Dutchess, Montgomery, Broome, Fulton, Schoharie;
- September 2014: Delaware, Warren.
EnrollmentOctober Niagara, Madison, Oswego November Chenango, Cortland, Livingston, Ontario, Steuben, Tioga, Tompkins, Wayne December Genesee, Orleans, Otsego, Wyoming January Chautauqua, Chemung, Seneca, Schuyler, Yates Allegany, Cattaraugus February Clinton, Essex, Franklin, Hamilton, Jefferson, Lewis, St. Lawrence, - Total enrollment in MLTC Partial Capitation Plans (see attachment 3) for the period October 2013 through September 2014 is 123,566. Plan specific enrollment on a monthly basis for the period is submitted in the attachment. For the same period, 32,903 individuals who were being transitioned into Managed Long–Term Care from fee for service made an affirmative choice.
- Significant Program Developments
- Developed and expanded information available to participants selecting plans to include a Consumer Guide for Plans in NYC based on assessment data submitted. This Consumer Guide is also being developed for other regions of the state. During the period October 2013 through September 2014, Consumer Guides were developed for other regions of the State: Central, Hudson Valley, Long Island, Northeast, and Western.
- Enhanced oversight of Social Day Care utilization and plan contract monitoring continues.
- Submitted preliminary proposal to develop independent clinical assessment process for MLTC enrollment. Formulating process guidelines to inform development of strategic goals and objectives. During the second quarter completed steps finalized the infrastructure, including roles and responsibilities, with goal to operationalize the process by October 2014 in the New York City region. Refining work–plan to finalize an implementation schedule that will lead to statewide operations. During the period July 2014 through September 2014 final steps were taken to operationalize the process by the target date of October 1, 2014. Outreach, training and education was conducted with stakeholders through a series of web–based sessions.
- Conducted analysis of complaints received by Technical Assistance Center and identified plan specific trends and problem area. Formulated process to commence an in depth focus audit of plan during third quarter. Developing strategies to further expand the focus audit activities. During the period July 2014 through September 2014 in depth focus audit was conducted, findings will be released next quarter.
- Completed development of a Request for Application to address the requirement for an Independent Consumer Support Program. Review and selection process has commenced and remains ongoing. Vendor has been selected and work plan is being finalized. Initial roll out will begin during next quarter.
- During the month of September 2014, developed concept to create a plan member services ‘secret shopper´ process. A standardized survey tool will be designed to test the effectiveness of a plan´s member services toll–free access phone number. Areas of focus will be quality of access, accuracy of information provided. Standards will be created, and protocols developed to for potential statement of deficiency and corrective action plan.
- Issues and Problems
Hurricane Sandy had a devastating impact on New York State´s health resources and the aftermath of the storm continues to affect health care needs and outcomes.- In response to various allegations of improprieties relating to utilization of Social Day Care in MLTC, SDOH, the Attorney General´s Office and the Office of the Medicaid Inspector General are cooperating in ongoing audits and investigations. Focused activities are being expanded on an ongoing basis as issues are identified.
- Summary of Self–Directed Options
This policy document was created in conjunction with a CDPAS Workgroup reflective of numerous stakeholders that met a number of times to discuss issues and develop policies for this new benefit:- Contracting During the Transition Period: For the period October 1 2012– September 30, 2013 (Transition Period), Health Plans are required to contract with Fiscal Intermediaries (FIs) that currently have a contract or MOU with a LDSS and currently provide fiscal intermediary services to the health plan´s member(s). The rate of payment must be at least the FFS rate of payment provided for in the contract or MOU between the FI and the LDSS. The MLTC/MCO is not required to contract with FIs unwilling to accept the applicable Medicaid FFS rate as long as the MLTC/MCO maintains two (2) FIs for each county. To adequately meet the needs of members who are newly assessed and considered eligible to receive CDPAS, the MLTC/MCO may also include in the MLTC/MCO´s network FIs that do not have a contract or MOU with the LDSS.
- Consumer Continuity of Care and Choice during the Transition Period: The Department provided a list of FIs currently providing FI services to FFS and MCO´s enrolled members. To promote and maintain consumer choice, members may, during the Transition Period, change to any FI in the county that has a contract with the MCO.
If, at the time of transition, an FI serves less than five (5) members in a county, MLTC/MCOs may encourage the members to use an alternative FI to minimize the number of FIs an MLTC/ MCO must have under contract. However, during the transition period, the expectation is that a member is not required to transition to a different consumer directed personal assistant due to the lack of an MLTC/MCO/FI contract. MLTC/ MCOs are prohibited from coercing or threatening the member or the worker to change FIs. - Network Adequacy during the Transition Period: An MLTC/ MCO that does not have members participating in CDPAS in a particular LDSS must have at least two (2) FI contracts. This will ensure that members will have the option to participate in CDPAS.
- FI Contracting and Network Adequacy after the Transition Period: Beginning October 1, 2013, MLTC/MCOs may contract with two (2) FIs to cover members in multiple counties.
- Model FI Contract and Department of Health Review: The Department supports the use of the MLTC/MCO/FI model contract developed by the parties. However, each MLTC/MCO/FI may negotiate the terms of the model contract, except that no agreement may contain provisions that would be considered management functions under 10 NYCRR 98–1.11 or a provider agreement per 10 NYCRR 98–1 and the Provider Contract Guidelines without the express written approval of the Department. The MCO were required to submit to the Department the name(s) of the contracted FIs for each county prior to October 1, 2012 and the fourth quarter of each year thereafter, or upon request of the Department.
- Acknowledgement of the Roles and Responsibilities of the Consumer/Designated Representative: Each member prior to receiving CDPAS must sign a consumer acknowledgement of the roles and responsibilities of the MLTC/MCO and the member. The Department has provided a sample acknowledgment form with the minimum requirements for its use by the MLTC/MCO.
- Transition of Consumer Direct Services continues throughout the mandatory counties.
- Department is preparing guidelines to share with all MLTCs regarding Consumer Direct Services to supplement existing educational materials shared previously.
- Posting of Consumer Direct Services guidelines to the Department of Health website for clarification.
- Required Quarterly Reporting
- Critical incidents: There were 214 critical incidences reported for the period July 2014 through September 2014. For the period October 2013 through September 2014 reporting of critical incidents has varied from 85 to 215. During the next quarter the Department will review criteria for reporting elements to identify potential areas for improvement and determine if there are seasonal trends to consider.
- Grievance and Appeals Annual Summary: During the period January 2014 through March 2014 the Department instituted additional quality control measures to oversee the submission of the data. Key areas of concern are consistently dissatisfaction with quality of home care and transportation. Once the data collection improved, numbers have been fairly consistent quarter to quarter. During the quarter July 2014 through September 2014, further analysis began towards identification of trends and referral to plan managers to analyze and probe further with plan; with additional actions as indicated. This is a continuous process that will be monitored and utilized to increase the quality of data. The data does not include Fair Hearing information. Fair Hearing data has been available through the State agency that administers the process, and efforts are currently underway to develop a comprehensive data set and tracking system.
Period: 7/01/14 – 9/30/14 Grievances Total for this period: Resolved Resolved % # Same Day 6810 6810 100% # Standard/Expedited 1207 935 77% Total for this period: 8017 7745 97%
Period: 7/01/14 – 9/30/14 Appeals Total appeals filed for this period: Total for this period: 10
Period: 7/01/14 – 9/30/14 Grievances Reason for Grievances Total Dissatisfaction with quality of home care (other than lateness or absences) 1178 # Same Day 845 # Standard 333 # Expedited 0 Home care aides late/absent on scheduled day of service 627 # Same Day 522 # Standard 105 # Expedited 0 Dissatisfaction with quality of day care 11 # Same Day 4 # Standard 7 # Expedited 0 Dissatisfaction with quality of other covered services 381 # Same Day 231 # Standard 149 # Expedited 1 Dissatisfaction with transportation 4822 # Same Day 4566 # Standard 256 # Expedited 0 Travel time to services too long 12 # Same Day 10 # Standard 2 # Expedited 0 Wait too long to get appointment or service 48 # Same Day 15 # Standard 33 # Expedited 0 Waiting time too long in provider´s office 10 # Same Day 9 # Standard 1 # Expedited 0 Dissatisfaction with care management 244 # Same Day 118 # Standard 126 # Expedited 0 Dissatisfaction with member services and plan operations 213 # Same Day 187 # Standard 26 # Expedited 0 Dissatisfied with choice of providers in network 33 # Same Day 30 # Standard 3 # Expedited 0 Misinformed about plan benefits or rules by marketing or other plan staff 4 # Same Day 3 # Standard 1 # Expedited 0 Language translation services not available 4 # Same Day 1 # Standard 3 # Expedited 0 Hearing/vision needs not accommodated 4 # Same Day 4 # Standard 0 # Expedited 0 Disenrollment issues 18 # Same Day 5 # Standard 13 # Expedited 0 Enrollment issues 7 # Same Day 3 # Standard 4 # Expedited 0 Plan staff rude or abusive 53 # Same Day 39 # Standard 14 # Expedited 0 Provider staff rude or abusive 71 # Same Day 63 # Standard 8 # Expedited 0 Violation of other enrollee rights 24 # Same Day 21 # Standard 3 # Expedited 0 Denial of expedited appeal 0 # Same Day 0 # Standard 0 # Expedited 0 Other: 253 # Same Day 134 # Standard 118 # Expedited 1 Total for this period: 8017 # Same Day 6810 # Standard 1205 # Expedited 2
Period: 7/01/14 – 9/30/14 Reason for Appeal Total Denial or limited authorization of service including amount, type or level of service 152 # of Standard Filed 148 # of Expedited Filed 4 Reduction, suspension or termination of previously authorized service 1149 # of Standard Filed 961 # of Expedited Filed 188 Denial in whole or part of payment for service 4 # of Standard Filed 4 # of Expedited Filed 0 Failure to provide services in a timely manner 0 # of Standard Filed 0 # of Expedited Filed 0 Failure of plan to act upon grievance or appeal of grievance in a timely manner 0 # of Standard Filed 0 # of Expedited Filed 0 Failure of plan to act upon appeal of plan action in a timely manner 0 # of Standard Filed 0 # of Expedited Filed 0 Other 3 # of Standard Filed 2 # of Expedited Filed 1 Total appeals filed for this period: 1308 # of Standard Filed 1115 # of Expedited Filed 193
Period: 7/01/14 – 9/30/14 Fraud and Abuse Complaints Reported during Quarter 20
Period: 7/01/14 – 9/30/14 Fraud and Abuse Complaints Reported during Quarter 20 - Fraud and Abuse: For the period July 2014 through September 2014, there were 20 Fraud and Abuses cases reported. For the annual period of October 2013 through September 2014, there were spikes noted in the second and third quarters relating to one organization´s findings regarding a practitioner group.
- Technical Assistance Center (TAC) Complaints: For the period July 2014 through September 2014 the highest concentration of complaints were in the following areas:
- Billing issues related to plan subcontracted provider claims
- Member Dissatisfaction with Home Care or Network Providers
- Referrals relating to durable medical equipment (DME)
- Assessment for enrollment: For the period July through September 2014 the total number of assessments for enrollment performed by the plans is 20,646 with 1,330 who did not qualify to enroll in an MLTC plan. For the annual period October 2013 through September 2014; 8% of assessments conducted resulted in not qualifying for enrollment. The conflict free enrollment center will begin during October 2014, and operations will be incrementally expanded; therefore, data collection will be adjusted to accommodate the new processes.
- Referrals and 30–day assessment: The establishment of the reporting system and training of Plans to assure data completeness and quality is an ongoing effort. The State will review the finalized data to determine if actions need to be taken. Quality of data will be verified then remedial action pursued. Data reporting has improved. For the period July 2014 through September 2014, total assessments conducted by MLTC plans during the period is 10,309. 87.8% were within the 30–day time frame. For the annual period October 2013 through September 2014, data collection improved, as did the percentage of assessments conducted within the 30–day time frame; consistent throughout the final three quarters.
- Referrals outside enrollment broker: During the period July through September of 2014, 8,487 people were not referred by the enrollment broker and contacted the plan directly and were provided MLTC materials. For the annual period October 2013 through September 2014, numbers were consistent. With the conflict free enrollment center beginning October 2014, this data collection element will be reviewed to ensure accurate information is obtained.
- Rebalancing efforts: For the annual period of October 2013 through September 2014: the number of individuals enrolled in plan from a NH, returning to the community has been consistent. Since data collection processes improved during January 2014, number of MLTC enrollees permanently placed in NHs has also been consistent.
Period: 7/01/14 – 9/30/14 Rebalancing Efforts Number of Individuals enrolled in the plan from a nursing home 178 Number of Enrollees admitted to a nursing home but returned to the community 920 Number of Enrollees permanently admitted to a nursing home 651
VI. Financial, Budget Neutrality Development/Issues
- Quarterly Expenditure Report Using CMS–64
- See attachment 1. NYS Partnership Plan Projected 1115 Waiver Budget Neutrality Impact.
- Designated State Health Programs
- Although the primary source of state match is Inter Governmental Transfers (IGTs), the state proposes to use some previously approved DSHPs to ensure that the complete needs of the state are addressed through the MRT waiver amendment. Sources of DSHP funding, cited in STC 15, include previously approved F–SHRP fund, previously approved Partnership Plan DSHPs, and recently approved DSHPs not utilized for DD Transformation.
- Total value for Designated Year 0 is $188,000,000.
- Clinic Uncompensated Care
- The Department processed Clinic Uncompensated Care distributions in the amount of $34,165,504, $17,082,754 FFP, during the quarter that ended March 31, 2012.
- The Department processed Clinic Uncompensated Care distributions in the amount of $9,196,209, $4,598,105 FFP, during the quarter that ended June 30, 2012.
- The Department processed Clinic Uncompensated Care distributions in the amount of $1,790,919, $895,459 FFP, during the quarter that ended September 30, 2012. Cumulative distributions to date total $45,152,632, $22,576,316 FFP.
- The Department processed Clinic Uncompensated Care distributions in the amount of $79,428,341, $39,714,171 FFP, during the quarter that ended December 31, 2012.
- The Department processed Clinic Uncompensated Care distributions in the amount of $28,385,795, $14,192,898 FFP, during the quarter that ended March 31, 2013.
- The Department processed Clinic Uncompensated Care distributions in the amount of $896,912, $448,456 FFP, during the quarter that ended June 30, 2013.
- Cumulative disbursements to date total $153,863,680, $76,931,843 FFP.
- The Department processed Clinic Uncompensated Care distributions in the amount of $108,751,308, $54,375,690 FFP, during the quarter that ended December 2013.
- The uncompensated care program provides over $108 million in payments to qualifying clinic providers, including mental health (MH) clinics, to assist in covering the uncompensated costs of services provided to the uninsured population. In order to receive these funds, each provider must deliver a comprehensive range of health care or mental health services; have at least 5% of their annual visits providing services to uninsured individuals; have a process in place to collect payments from third party payors. For the year 2013, 133 Diagnostic & Treatment Centers (DTC´s) and 200 MH clinics were determined to be potentially eligible to receive funding for this program. Of the award amounts, the DTC´s were awarded $92,429,009 while the MH clinics received $10,205,991 for a total of $102,635,000. In addition, the Supplemental award amount of $5,880,000 was distributed between 12 DTC´s. This brings the total amount awarded in 2013 to $108,515,000.
- New York requested an amendment to the Partnership Plan to extend the Clinic Uncompensated Care Funding authorized in STC 58, which expired December 31, 2013. The amendment extended the federal funding agreement through December 31, 2014.
- New York received authorization to transition and extend certain Designated State Health Programs (DSHPs) which were authorized under the Federal–State Health Reform Partnership (F–SHRP) Demonstration which expired March 31, 2014. Continuance of these DSHP´s will occur under the Partnership Plan due to expire December 31, 2014.
- Hospital–Medical Home Demonstration (see attachment 4)
Background:
- The Hospital–Medical Home Demonstration announced awards for funding and participation to 64 hospitals in early October 2012. Hospitals submitted work plans on December 3, 2012 for review. Hospitals officially began work plan implementation on January 1, 2013. The initial timeline was extended due to Hurricane Sandy. Twenty–one months into the project, 158 resident clinics training over 5,000 primary care residents affiliated with 61 hospitals serving approximately 1,000,000 Medicaid members in all regions of New York State continue actively implementing residency changes, patient–centered medical home transformation of participating outpatient sites, and the chosen care coordination and inpatient projects contained in their work plans to meet the program requirements.
Program Accomplishments:
- 156/158 of sites (99%) became recognized by the National Commission for Quality Assurance (NCQA) as Level II or III Patient–Centered Medical Homes by 2011 standards by the July 1, 2014 deadline. The two hospitals that were unable to meet the milestone were Niagara Falls Memorial Medical Center and Interfaith Medical Center. Niagara Falls was only able to achieve Level 1 recognition, but hopes to be recognized as Level 2 before the end of the project. The status of Interfaith continues to be in flux, but they will plan to achieve Level 2 by the end of the project, as long as they remain open.
- Reallocation of funding among the 61 remaining hospitals continues to occur based on meeting of program milestones, hospital closures and mergers, and residency program and continuity clinic changes.
- All hospital–reported data submitted through the web tool continues to be aggregated in summary reports for each domain. Summary reports are used to determine the quality and completeness of reporting as well as site progress. (The content in the reports vary by domain, but generally display the number of sites improving on certain metrics since the previous quarter, the number of sites reporting on a given metric, and the number of sites answering either ´yes´ or ´no´ to required questions about meeting milestones in each domain).
- Developed measure categories and composite measures in each domain to better evaluate demonstration effects and individual hospital/clinic achievements.
- Received and reviewed the Year 2, 2nd quarter submission from sites and provided feedback to the hospitals regarding the quarterly metric and narrative information. All feedback letters are posted on the Hospital Medical Home website on the welcome back page after each logging in. Penalties were assessed related to continued decline for Clinical Performance Metrics for both Sisters of Charity Hospital and Mercy Hospital. Niagara Falls Memorial Medical Center and Interfaith Medical Center received penalties due to not meeting the PCMH deliverable by 7/1/14.
- Continued to work with hospital, professional and community organizations such as the Hospital Association of New York, The Greater New York Hospital Association, the Primary Care Development Corporation, the NYS American Academy of Family Physicians, the New York Academy of Physicians and others to support hospitals in their transformation efforts.
- Conducted weekly meetings with a work plan review team, as well as several ad hoc specialty advisors, consisting of clinical and administrative staff both from IPRO and within the NYS DOH. Provided continuous clinical and technical support to 61 hospitals and 158 sites.
- Refined the project website to ensure all reports were directly accessible on the web portal ensuring that Quarterly Hospital Feedback Letters, Hospital Ranking Reports and Hospital Performance Reports are available to all project participants with user access to the portal.
- Coordinated and arranged for 7/9/14 Hospital Medical Home Coaching call presentation on Diabetic Retinopathy Screening. Presenters included David M. Rubaltelli, M.D., M.B.A., Assistant Professor of Ophthalmology, Department of Ophthalmology and Visual Sciences and Jon Swartz MD, MBA, FAAFP, Regional Medical Director, Montefiore Medical Center. This call was held following an informational update with Hospitals involved in the project prior to the Portal Opening for the quarter. Individuals from 110 phone lines participated in the call.
- On 7/30/14, organized a Hospital Medical Home Coaching call presentation on Resident Continuity/Attribution: "Who is My Patient and What Does That Mean?” Three hospitals participating in the project presented including Tom Campbell, MD, from Highland Hospital, George Clifford, PhD MPA from Albany Medical Center Hospital, and Joseph Truglio, MD from Mount Sinai Medical Center. Following the presentation, Dr. Marietta Angelotti provided guidance on the newly required Resident Continuity Measures sites would be expected to report. Individuals from 113 phone lines participated in the call.
- On 8/8/14, held a Hospital–Medical Home Coaching call presentation on Preventing Readmission for High Risk Patients – Post Discharge 48 hour follow up visits. Coaching call presenters included Brenda Matti–Orozco, MD from Mount Sinai St. Luke´s & Mount Sinai Roosevelt Hospital, JoAnne Gottridge, MD, FACP from Northshore University Hospital, and William Pagano, MD, MPH from Lutheran Medical Center. This call was held following a question/answer call prior to Portal closure with Hospitals involved in the project. Individuals from 83 phone lines participated in the call.
- Continued hospital and clinic site visits throughout NYS to learn about the accomplishments, changes and challenges hospitals are facing during this demonstration program. During this quarter, the NYSDOH OQPS Medical Director, Associate Medical Director, Program Manager, Program Specialist, and other specialty advisors conducted six site visits at St. Barnabas Hospital, New York Presbyterian Hospital, Mount Sinai Hospital, Mount Sinai Beth Israel Hospital, Mount Sinai St. Luke´s & Mount Sinai Roosevelt Hospital, and Phelps Hospital Medical Center. Hospital presentations for all visits are posted publicly on the Hospital Medical Home website under Resources. The site visits completed to date represent a collective total award of $225M.
- Conducted teleconferences to educate participants on upcoming changes prior to the Year 2, 2ndt quarter (2014) portal opening on 7/10/14 and provided an educational call one week prior to the portal closing on 8/8/14 to allow for opportunities for question and answer to all hospitals/sites involved in project.
- Distributed scheduled payment to participating hospitals in September 2014, which included 75% of Year 2 payment for all hospitals achieving PCMH Level 2 or 3 by deadline as well as up to 25% of Year 3 payment for the first quarter of Year 2 payment to the hospitals.
- The Department processed Hospital Medical Home distributions in the amount of $25,254,235 on January 2, 2013. This represented 25% of the First Year Award amount.
- The Department processed Hospital Medical Home distributions in the amount of $75,762,705 on October 16, 2013. This represented 75% of the First Year Award amount.
- The Department processed Hospital Medical Home distributions in the amount of $19,084,775 on April 16, 2014. This represented 25% of the Second–Year award amount.
- Cumulative Distributions awarded to date total $120,101,715.
- The Department plans to process Hospital Medical Home distributions in the amount of $75,000,000 in September 2014. That amount represents 75% of the Second–Year award amount and 25% of the Third–Year award amount.
- The Department plans to process Hospital Medical Home distributions in the amount of $56,000,000 in December 2014. That amount will represent 75% of the Year Three award amount.
- The two tentative amounts still to be awarded total $131,000,000.
Provisional Summary based on self–reported data received in the 2014 Quarter 2–time frame:
- Of the 54 sites participating in the Improved Access and Coordination between Primary and Specialty Care project,
- 72% of sites showed improvement in decreasing the amount of time required to see a specialist as compared to baseline.
- Sites most often implemented the following measures to improve access to specialists: onsite specialist clinic/Co–location of services (identified by 24 sites (44%)), same day specialist appointments (identified by 18 sites (33%)), and clinical advice to PCP by telephone (identified by 15 sites (28%)).
- Resident Continuity Metrics: On Average, sites are reporting that 53% of resident visits are with patients on their panel, and 53% of patient visits are with their assigned PCP.
- 82% of sites showed improvement in breast cancer screening and 80% of sites showed improvement in colorectal cancer screening since baseline.
- 75% of sites reporting improved rates of tobacco use screening and/or tobacco cessation counseling.
- 76 clinics are restructuring their care transitions to ensure all patients have medication reconciliation on admission and discharge, including at a clinic follow–up, and that high–risk patients have a follow–up call or visit at their PCPs office within 48 hours of discharge from the hospital.
- On average, these sites are reporting that a follow–up phone call within 48 hours of discharge occurred 73% of the time (up from 47% of the time in Q3 2013)
- 59 clinics are reporting meeting their goals for receiving a hospital transition record to the PCP within 24 hours after discharge (up from 50 last quarter). On average, sites are reporting timely transmission of the discharge record 87% of the time.
- 71 clinics are administering the CTM–15 to clinic patients routinely to assess the quality of their care transitions. The average score is over 3.2 (out of 1–4 scale.)
- 25 clinics committed to ensuring interpreter wait time is 15 minutes or less and 20 clinics report this is true 99% of the time or greater.
- 25 clinics are committed to completing cultural competency training for all providers. On average, as of quarter 2, 2014, 79% of staff at participating sites have received this training within the past 12 months (up from an average rate of 35% in quarter 2, 2013).
- 33 clinics are participating in Collaborative Care to integrate behavioral health into primary care. On average, sites report 85% of adult patients are being screened for depression at the outpatient site. 32 clinics report having depression care managers at their site, and 19 sites report that staff care management time is the equivalent of 1 FTE or more. Nearly half of sites report that 90% or more of their patients see a behavioral health provider within the timeframe requested by their PCP.
- Out of 53 sites committed to improving coordination between primary and specialty care, 36 sites (68%) have documentation of referrals 100% of the time. 52 sites report a rejected referral rate of 10% or less. On average, sites report that only 1% of referrals from the outpatient sites are rejected by the specialist.
Annual Hospital Medical Home Trends in Metrics and Composite Scores
- DOH Hospital–Medical Home data was analyzed for all Care Coordination projects related to metrics and composite scores for hospitals participating in the four coordination projects listed below. All graphs for each project show the progress from Quarter 3, 2013 through Quarter 2, 2014. Graphs and "about reports” are included in appendix of this report.
- Care Transitions / Medication Reconciliation
- Behavioral Health
- Culturally Competent Care
- Coordination between Primary and Specialty Care
Highlights of Annual Trends
- Care Transitions and Medication Reconciliation: the rate of follow up phone calls within 48 hours of discharge improved from 47% in Q3 2013 to 73% in Q2 2014.
- Behavioral Health: From Q3 2013 to Q2 2014, there was a 41% increase in the average rate of patients enrolled in the collaborative care initiative who´s PHQ–9 decreased below 10 in 16 weeks
- Behavioral Health: In the last 4 quarters, the average site–level composite score for behavioral health report card projects has improved by 30%.
- Culturally Competent Care: The average rate of prescription labels being written in the preferred language of the patient has increased 67% in the last year. This has been a challenge for many sites and has been addressed in multiple site visits as well as on coaching calls.
- Coordination between Primary and Specialty Care: Measures for complete referrals in the requested timeframe as well as completed post–specialty visits within the recommended timeframe have shown a steady trend of improvement in the last 4 quarters.
Administrative and Policy Challenges – Annual
- Clinical Performance Metrics: Hospitals need continuing guidance and clarification regarding tracking performance on measures. Hospitals that have measures that do not indicate improvement for two consecutive quarters are asked to conduct a root cause analysis for the areas of concern. NYS DOH continues to provide assistance with root cause analysis.
- Although the majority of hospitals and clinics are exchanging information successfully with their Regional Health Information Organization (RHIO), there continues to be challenges connecting with one particular region of the state associated with the Taconic Health Information Network and Community (THINC) RHIO and with one large hospital system. NYS DOH Office of Health Information Technology and Hospital Medical Home program staff continue to provide assistance and consultation with challenges.
- The portal has been continuously updated to respond to the needs of the project as it evolves including refinements to data collections, new measures, resources for hospital and residency use, etc.
- Plans for best placement and storage as well as long term viewing of the Hospital Medical Home website/portal after the project ends is under discussion. Decisions have not yet been made the permanent location and ongoing functionality of the website/portal.
- Sustainability is a challenge for all participants–hospitals and sites. Hospitals have been asked to supply an explanation regarding what steps are being taken to ensure that improvements made in each area of the project will continue beyond the end of the project.
Planned actions for the next Quarter and remainder of the Demonstration
- Continue planning for the Hospital Medical Home Demonstration Conference to be held on March 19, 2015. This conference will bring together participants from more than 61 hospitals, 115 residency programs, and 158 outpatient clinics across NYS. The program will consist of plenary and panel presentations, keynote Speaker Andrew Morris Singer, M.D., and a poster session. Successes will be celebrated, such as the 99% rate of transformation to high level patient centered medical homes and the numerous projects to improve transitions of care, behavioral health integration, access to specialists, and cultural competence as well as inpatient quality and safety, and next steps for transforming primary care in the context of the SHIP and DSRIP.
- Beginning with this quarter, all sites must report on the strategies undertaken to ensure improvements exist beyond the end of the project in each area of the project.
- Provide ongoing support and education regarding project implementation & reporting processes via teleconferencing and web conferencing.
- Receive and review Year 2 (2014) Quarter 3 report.
- Continue site visits with hospitals and outpatient primary care sites.
- Continue to collaborate with Hospital and Professional Associations to clarify the demonstration components, support hospitals, and plan Hospital–Medical–Home conference.
- Continued refinements adding additional resources to the demonstration´s portal website for participant use. In addition, Hospital–Medical Home staff will provide training on utilizing the Clinical Performance Metrics Hospital Performance report card which allow hospitals to compare their rates with other hospitals and sites for a specific quarter to be used for quality improvement purposes.
- Complete analysis for data and continue to develop final evaluation due in April 2015.
VII. Consumer Issues
A. Complaints
Medicaid managed care plans reported 5,357 complaints/action appeals this quarter, a decrease of 1.8% from the previous quarter. Of these complaints/appeals, 329 were FHPlus complaints/appeals. The most frequent category of complaint/appeal was balance billing disputes, accounting for 26% of the total. There were 139 complaints/appeals reported by the HIV SNPs. The majority of these complaints (35) were in the category of quality of care. The Department directly received 426 Medicaid managed care complaints and 2 FHPlus complaints this quarter.
The top 5 most frequent categories of complaints were as follows:
- 26% Balance Billing
- 22% Reimbursement/Billing Issues
- 7% Provider or MCO Services (Non–Medical)
- 7% Pharmacy
- 6% Emergency Services
This quarter, mainstream Medicaid managed care plans reported the following complaints and action appeals regarding long term services and supports. The Department did not identify any overall trends impacting enrollees´ access to services:
| Long Term Services and Supports | Number of Complaints/ Action Appeals Reported |
|---|---|
| AIDS Adult Day Health Care | 0 |
| Adult Day Care | 0 |
| Consumer Directed Personal Assistant | 0 |
| Home Health Care | 5 |
| Non-Permanent Residential Health Care Facility | 2 |
| Personal Care Services | 14 |
| Personal Emergency Response System | 0 |
| Private Duty Nursing | 0 |
| Total | 21 |
As SSI enrollees typically access long term services and supports, the Department monitors complaints and action appeals filed by this population with managed care plans. Of the 5,357 total reported complaints/action appeals, mainstream Medicaid managed care plans reported 544 complaints and action appeals from their SSI enrollees. This compares to 589 SSI complaints/action appeals from last quarter. The top 5 categories of SSI complaints/action appeals reported were:
| Category | Percent of Total Complaints/ Appeals Reported for SSI Enrollees |
|---|---|
| Balance Billing | 20% |
| Reimbursement/Billing Issues | 19% |
| Quality of Care | 11% |
| Provider or MCO Services (Non–medical) | 10% |
| Emergency Services | 6% |
The total number of complaints/action appeals reported for SSI enrollees by category were:
| Category | Number of Complaints/ Action Appeals Reported For SSI Enrollees |
|---|---|
| Adult Day Care | 0 |
| Advertising/Education/Outreach/Enrollment | 17 |
| AIDS Adult Day Health Care | 0 |
| Appointment Availability – PCP | 0 |
| Appointment Availability – Specialist | 1 |
| Balance Billing | 109 |
| Communications/Physical Barrier | 3 |
| Consumer Directed Personal Assistant | 0 |
| Denial of Clinical Treatment | 24 |
| Dental or Orthodontia | 18 |
| Emergency Services | 30 |
| Eye Care | 0 |
| Family Planning | 0 |
| Home Health Care | 3 |
| Mental Health or Substance Abuse Services/ Treatment | 1 |
| Non–covered Services | 16 |
| Non–Permanent Residential Health Care Facility | 1 |
| Personal Care Services | 13 |
| Personal Emergency Response System | 0 |
| Pharmacy | 18 |
| Private Duty Nursing | 0 |
| Provider or MCO Services (Non–Medical) | 52 |
| Quality of Care | 58 |
| Recipient Restriction Program/Plan Initiated Disenrollment | 0 |
| Reimbursement/Billing Issues | 105 |
| Specialist or Hospital Services | 5 |
| Transportation | 18 |
| Waiting Time Too Long at Office | 1 |
| All Other Complaints | 51 |
| Total | 544 |
B. Medicaid Managed Care Advisory Review Panel (MMCARP) Meetings
The Medicaid Managed Care Advisory Review Panel (MMCARP) met on September 17, 2014. The September meeting included presentations provided by state staff and discussions of the following: Delivery System Reform Incentive Payment (DSRIP) and Performing Provider Systems (PPS), and an update on FIDA and managed long–term care.
C. Managed Care Policy and Planning Meetings
Managed Care Policy and Planning Meetings were held on July 17, August 14, and September 11, 2014. The July meeting included the following presentations: MLTC and FIDA update; finance and rate development, including nursing home reimbursement issues and mix adjustment; Behavioral Health and Recovery Plan (HARP) stop–loss and rate development, and mainstream Sovaldi cost analysis and financing mechanism; health home bridge proposal and Salient outcomes; an update by the Office for People with Developmental Disabilities (OPWDD) on the progress of the development of Developmental Disabilities Individual Support and Care Coordination Organizations (DISCOs) and the transition the OPWDD populations into managed care; behavioral health/HARP transition; and oncotype Dx test for breast cancer. The August meeting agenda included: New York State of Health (SoH) enrollment reconciliation; update on transition of nursing home benefit and population into managed care; finance and rate development; update on Delivery System Reform Incentive Payment (DSRIP) planning grants and Performing Provider Systems (PPS); MLTC and FIDA update; and status of behavioral health/HARP. Presentations, updates and discussions at the September meeting included: DSRIP and PPS; transition of Nursing Home benefit and population to managed care; MCO compliance monitoring requirements related to due process for enrollees receiving long term supports and services (LTSS); MLTC and FIDA update; conflict free evaluation and enrollment center for individuals seeking community–based LTSS; finance and rate development, including mainstream behavioral health, HARP, and pharmacy impacts; children´s behavioral health design; and Certificate of Authority application and start–up grant application process for DISCOs.
VIII. Quality Assurance/Monitoring
A. Quality Measurement
Sixteen Medicaid managed care plans and three Medicaid HIV Special Needs Plans (SNP) submitted 2013 measurement year QARR data in June 2014. All plan data was audited by an NCQA licensed audit organization prior to submission. The following table reflects the State overall results for the two products for measurement year.
National benchmarks for Medicaid are from NCQA´s State of Health Care Quality 2014 report. Of the 58 measures with national comparison data, State Medicaid average exceeds national average for 53 measures, is consistent with national average for one measure, and is below national average for four measures. Comparison of State averages to national averages is indicated in the cell shading for Medicaid. Green cells indicate State average is higher than national average, yellow cells indicate State average is the same as national, and red cells indicate State average is lower than national average. National benchmarks for HIV SNP plans are not available.
2014 QARR Results (2013 Measurement Year – MY) New York State Medicaid Managed Care Plans
| Measure | HIV SNP 2013 MY Average | Medicaid 2013 MY Average | 2013 MY National Average |
|---|---|---|---|
| Adherence to Antipsychotic Medications for Individuals with Schizophrenia | 58 | 63 | 60 |
| Adolescent Immunization Combo | 68 | 72 | 70 |
| Adolescent Immunization HPV | SS | 27 | 20 |
| Adolescent Well–Care Visits | 55 | 64 | 50 |
| Adult BMI Assessment | 84 | 85 | 76 |
| Advising Smokers to Quit | 93 | 78 | 76 |
| Annual Monitoring for Patients on Persistent Medications– ACE Inhibitors/ARBs | 99 | 92 | 88 |
| Annual Monitoring for Patients on Persistent Medications– Anticonvulsant | 66 | 67 | 66 |
| Annual Monitoring for Patients on Persistent Medications– Combined Rate | 98 | 91 | 86 |
| Annual Monitoring for Patients on Persistent Medications– Digoxin | SS | 93 | 91 |
| Annual Monitoring for Patients on Persistent Medications– Diuretics | 99 | 91 | 88 |
| Antidepressant Medication Management– Effective Acute Phase Treatment | 54 | 50 | 51 |
| Antidepressant Medication Management– Effective Continuation Phase Treatment | 40 | 35 | 35 |
| Appropriate Testing for Pharyngitis | SS | 87 | 67 |
| Appropriate Treatment for Upper Respiratory Infection (URI) | 96 | 92 | 85 |
| Asthma Medication Ratio (Ages 5–64) | 41 | 64 | 65 |
| Avoidance of Antibiotics Therapy in Adults with Acute Bronchitis | NA | 26 | 27 |
| Breast Cancer Screening | 74 | 72 | 58 |
| Cardiovascular Monitoring for People with Cardiovascular Disease and Schizophrenia | SS | 82 | 79 |
| Childhood Immunization Status (Combo 3) | 79 | 73 | 71 |
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 12–19 Years) | 90 | 94 | 89 |
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 12–24 months) | 87 | 97 | 96 |
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 25 Mos–6 Years) | 87 | 94 | 88 |
| Children and Adolescents´ Access to Primary Care Practitioners (Ages 7–11 Years) | 92 | 97 | 90 |
| Chlamydia Screening (Ages 16–24) | 73 | 72 | 55 |
| Cholesterol Level Controlled (<100 mg/dL) | 45 | 46 | 41 |
| Cholesterol Screening Test | 91 | 88 | 81 |
| Counseling for Nutrition | 72 | 77 | 59 |
| Counseling for Physical Activity | 49 | 68 | 51 |
| Diabetes Monitoring for People with Diabetes and Schizophrenia | 85 | 77 | 69 |
| Diabetes Screening for People w/ Schizophrenia or Bipolar Disorder Using Antipsychotic Meds | 99 | 82 | 79 |
| Discussing Smoking Cessation Medications | 79 | 56 | 47 |
| Discussing Smoking Cessation Strategies | 75 | 47 | 42 |
| Drug Therapy for Rheumatoid Arthritis | NA | 79 | 71 |
| Follow–Up After Hospitalization for Mental Illness Within 30 Days | 58 | 78 | 61 |
| Follow–Up After Hospitalization for Mental Illness Within 7 Days | 40 | 63 | 42 |
| Follow–Up Care for Children Prescribed ADHD Medication: Continuation Phase | SS | 65 | 46 |
| Follow–Up Care for Children Prescribed ADHD Medication: Initiation Phase | SS | 56 | 40 |
| Lead Testing | 97 | 87 | 67 |
| Managing Diabetes Outcomes – Blood pressure controlled (<140/80 mm Hg) | 45 | 46 | 39 |
| Managing Diabetes Outcomes – Blood pressure controlled (<140/90 mm Hg) | 63 | 69 | 60 |
| Managing Diabetes Outcomes – HbA1C Control (<7.0%) for Selected Populations | 50 | 41 | 34 |
| Managing Diabetes Outcomes – HbA1C Control (<8.0%) | 58 | 57 | 46 |
| Managing Diabetes Outcomes – Lipids Controlled (<100 mg/dL) | 44 | 43 | 34 |
| Managing Diabetes Outcomes –Poor HbA1c Control | 35 | 32 | 46 |
| Medical Management for People with Asthma 75% Days Covered (Ages 5–64) | 61 | 36 | 31 |
| Monitoring Diabetes – Dilated Eye Exam | 42 | 63 | 54 |
| Monitoring Diabetes – HbA1c Testing | 93 | 89 | 84 |
| Monitoring Diabetes – Lipid Profile | 94 | 87 | 76 |
| Monitoring Diabetes – Nephropathy Monitoring | 79 | 83 | 79 |
| Persistence of Beta–Blocker Treatment | 78 | 85 | 84 |
| Pharmacotherapy Management of COPD Exacerbation– Bronchodilator | 94 | 88 | 81 |
| Pharmacotherapy Management of COPD Exacerbation– Corticosteroid | 69 | 75 | 66 |
| Use of Appropriate Medications for People with Asthma (Ages 5–64) | 65 | 83 | 84 |
| Use of Imaging Studies for Low Back Pain | 77 | 77 | 76 |
| Use of Spirometry Testing in the Assessment and Diagnosis of COPD | 24 | 51 | 31 |
| Weight Assessment– BMI Percentile | 78 | 75 | 57 |
| Well–Child & Preventive Care Visits in 3rd, 4th, 5th & 6th Year of Life | 69 | 83 | 72 |
B. MLTC Quality Incentive Workgroup
The Department continues to convene a workgroup of health plan representatives, advocates and associations on the development of the MLTC Quality Incentive. The workgroup and the Department reviewed measures of quality, satisfaction, compliance and efficiency related to performance. The Department shared the methodology for the Quality Incentive with the MLTC plans in September and the payment of the Quality Incentive is on target for 1/1/ 2015.
C. External Quality Review
The current External Quality Review (EQR) contract with the Island Peer Review Organization (IPRO) was given an extension through March 31, 2014, while a Request for Proposals (RFP) was prepared. The RFP will solicit bids for a new five–year contract to conduct Medicaid managed care external quality review as per the Balanced Budget Act of 1997 and CMS published EQR regulations. Because of delays in the State procurement process, the new contract was not in place by the intended date of April 1, 2014. The current contract has received two additional extensions, through November 30, 2014, while the new contract is finalized.
D. Performance Improvement Projects (PIPs)
For 2013–2014, a collaborative PIP includes two parts. Part 1, the Medicaid Incentives for the Prevention of Chronic Disease (MIPCD), includes testing the effectiveness of patient incentives on improving health behaviors and outcomes in the following clinical areas: diabetes prevention and management, smoking cessation, and hypertension management. Part 2 focuses on implementing interventions to improve care in one of the four clinical areas noted above. For Part 1, MIPCD, bi–monthly individual calls with each Medicaid managed care plan were conducted to accelerate progress and facilitate obstacles/barriers. To date, 457 Medicaid recipients are enrolled in the study, of which 180 are in the diabetes prevention study arm, 183 are in the diabetes management study arm, and 94 are in the hypertension management arm. For Part 2, IPRO is conducting conference calls with the health plans to monitor their progress. All plans are on track with proposed interventions
E. Breast Cancer Selective Contracting
Staff successfully completed the Breast Cancer Selective Contracting process for contract year 2014–2015. This included: refining the computer programs used to extract and analyze inpatient and outpatient surgical data from the Statewide Planning and Research Cooperative System (SPARCS); determining restricted facilities; notifying restricted facilities of their low–volume status; overseeing the appeals processing and notifying facilities about appeal decisions; and, sharing the list of restricted facilities with staff at eMedNY to restrict Medicaid fee–for–service payment to restricted facilities.
In total, the 2014–2015 annual review of breast cancer surgical volume involved 219 facilities where breast cancer surgery is occurring. Facility designations were as follows: 116 high– volume facilities, 29 low–volume access facilities, 66 low–volume restricted facilities, and eight closed facilities. Appeals were received from eight low–volume facilities, of which six were approved and two were denied.
In addition, a first annual summer data release was instituted in August, to provide facilities with a projected status of their volume designations (low or high) while allowing facilities sufficient time to correct any discrepancies between facility–calculated volume and SPARCS reported volume. The goal of the new process is to reduce the number of appeals and make the contracting process more efficient.
Staff also worked on updating the protocols and computer programs that will be used in the fall of 2014 to determine restricted facilities for the 2015–2016 contract year.
F. Eliminating Disparities in Asthma Care (EDAC)
The five–year Eliminating Disparities in Asthma Care (EDAC) Collaboration came to a close on August 31, 2014. Grant activities during the final year of funding were focused on completing an in–depth evaluation of the project and assessing the Collaboration´s effectiveness in meeting four objectives: 1) Has an effective collaboration that includes the Department, health plans, primary care practices, the community, and Medicaid recipients, been established and sustained in order to successfully accomplish the stated project goals; 2) Has asthma care been improved across selected indicators within population of focus; 3) Have racial/ethnic disparities in asthma care been reduced among the population of focus; and 4) Have a set of tools and successful strategies been produced and disseminated related to eliminating racial and ethnic disparities in asthma health care outcomes?
Of the 26 indicators employed in the evaluation, 10 met or exceeded the standards of success that were set by the EDAC Leadership Team. Success was noted in the following indicators: existence of shared mission/planning/goals among stakeholders; at least 95 percent of patients with asthma having a documented severity classification in their medical record; and no statistically significant differences noted in rates of asthma inpatient hospitalization or emergency department visits across racial/ethnic groups. However, indicators related to increased distribution of Asthma Action Plans, evaluation of environmental triggers, and smoking status assessment fell below the standards of success.
G. Managed Long Term Care (MLTC)
The EQRO conducted and completed both a focused clinical study and patient satisfaction survey during the last year. The focused clinical study reviewed individuals who were mandatorily enrolled in MLTC plans, both those who chose their plan and those auto–assigned, and who received the same level of service within the initial 60 days of enrollment in an MLTC plan, as they had received under their fee–for–service (FFS) service plan. This ensured compliance with two Centers for Medicare and Medicaid Services (CMS)–based terms and conditions related to the expansion of the MLTC program; eligibility and transition of care. The study commenced in May 2013 and concluded in September 2013. Data analysis completed on the survey reflected virtually no difference in the level of care between the auto–assigned and non–auto–assigned groups when transitioning from FFS to an MLTC plan. A final report was issued in September 2014.
An enrollee satisfaction survey was administered by the EQRO examining the experience of care for MLTC recipients newly enrolled in a managed long–term care plan through the mandatory expansion of MLTC. The survey aimed to measure enrollee´s satisfaction with their plan, both pre– and post–enrollment in the MLTC program. The survey commenced in December 2013 and closed in June 2014. Data analysis was conducted, and a final draft report was issued in September 2014, reflecting that 95 percent of respondents said, overall, that the quality of their health care services is either the same or better since joining the plan.
H. Patient Centered Medical Home (PCMH)
In May 2013, the Department and IPRO began planning a study to look at the differences in experience of care between patients who had visits with a PCMH provider and those with visits to a provider without the PCMH designation. The Clinician and Group CAHPS survey with the additional PCMH group of questions was chosen for this study. A random sample of 6,000 Medicaid members was selected, divided equally between children and adults, and between those with a visit to a PCMH provider and a visit with a non–PCMH provider. Surveys were sent to enrollees following a combined mail and phone methodology in September 2013, resulting in a 35.4 percent response rate. The final report from that study was received in March 2014. Results indicate satisfaction somewhat higher among the non–PCMH group for many questions; however, most differences were not statistically significant. PCMH respondents were more satisfied in the areas of the comprehensiveness of their care.
IX. Transition Plan Updates
Please see attachment 2, which contains the Department´s updated Transition Plan indicating how the Department will transition enrollees to a coverage option under the Affordable Care Act, as required by the Section 1115 Partnership Plan demonstration.
X. Other
A. Medicaid Managed Care/Family Health Plus/HIV SNP Model Contract
On July 11, 2014, the Department submitted to CMS for approval a summary of changes that are to be included in the March 1, 2014 – February 28, 2019 Medicaid Managed Care/Family Health
Plus/HIV SNP model contract. The revised model contract includes contract language changes related to various MRT initiatives and other programmatic changes. The Department is in the process of preparing a response to comments and questions that CMS sent to the Department on September 19, 2014 regarding the Department´s draft revisions.
B. Delivery System Reform Incentive Payment Program
DSRIP is the main mechanism by which the Department will implement the MRT Waiver Amendment. DSRIP´s purpose is to fundamentally restructure the health care delivery system by reinvesting in the Medicaid program, with the primary goal of reducing avoidable hospital use by 25% over five years. Up to $ 6.42 billion dollars are allocated to this program with payouts based upon achieving predefined results in system transformation, clinical management and population health. (Please see attachment 5)
Attachments:
Attachment 1 – Budget Neutrality
Attachment 2 – Transition Plan
Attachment 3 – MLTC Partial Capitation Plans
Attachment 4 – Hospital–Medical Homes
Attachment 5 – DSRIP Quarterly Report
State Contact:
Priscilla Smith
Medical Assistance Specialist III
Division of Program Development and Management
Office of Health Insurance Programs priscilla.smith@health.ny.gov
Phone (518) 486–5890
Fax# (518) 473–1764
Date Submitted to CMS:
December 30, 2014
Attachment 1
New York State Partnership Plan
Projected 1115 Waiver Budget Neutrality Impact Through December 2014
DY13 Actuals 21 Month Lag Final
| Budget Neutrality Cap (Without Waiver) |
DY 1 – 8 (10/1/97 – 9/30/06) Projected |
DY 9 (10/1/06–9/30/07) Actual |
DY 10 (10/1/07–9/30/08) Actual |
DY 11 (10/1/08–9/30/09) Actual |
DY 12 (10/1/09–9/30/10) Actual |
DY 13 (10/1/10–9/30/11) Actual |
|---|---|---|---|---|---|---|
| Demonstration Group 1 – TANF Children under age 1 through 20 | $8,641,454,877 | $9,086,365,132 | $10,048,004,954 | $11,219,968,696 | $12,363,834,697 | |
| Demonstration Group 2 – TANF Adults 21–64 | $3,045,582,094 | $3,217,134,170 | $3,856,757,531 | $4,521,937,580 | $4,941,625,207 | |
| Demonstration Group 6 – FHP Adults w/Children | $1,691,957,919 | $1,813,935,485 | $1,746,457,301 | $1,872,671,502 | $2,098,462,751 | |
| Demonstration Group 8 – Family Planning Expansion | ||||||
| Demonstration Group 10 – MLTC Adult Age 18–64 Duals | ||||||
| Demonstration Group 11 – MLTC age 65+ Duals | ||||||
| W/O Waiver Total | $144,639,878,523 | $13,378,994,889 | $14,117,434,787 | $15,651,219,785 | $17,614,577,777 | $19,403,922,654 |
| Budget Neutrality Cap (With Waiver) |
DY 1 – 8 (10/1/97 – 9/30/06) Projected | DY 9 (10/1/06–9/30/07) Actual | DY 10 (10/1/07–9/30/08) Actual | DY 11 (10/1/08–9/30/09) Actual | DY 12 (10/1/09–9/30/10) Actual | DY 13 (10/1/10–9/30/11) Actual |
|---|---|---|---|---|---|---|
| Demonstration Group 1 – TANF Children under age 1 through 20 | $4,006,367,977 | $4,412,472,964 | $4,828,196,168 | $4,876,699,233 | $4,992,523,251 | |
| Demonstration Group 2 – TANF Adults 21–64 | $2,062,992,139 | $2,222,230,858 | $2,553,996,035 | $2,851,097,035 | $2,980,376,698 | |
| Demonstration Group 5 – Safety Net Adults | $3,017,805,826 | $3,213,033,028 | $3,818,572,584 | $4,479,171,065 | $4,970,515,310 | |
| Demonstration Group 6 – FHP Adults w/Children up tp 150% | $813,927,831 | $884,575,928 | $894,902,321 | $976,122,527 | $1,066,692,312 | |
| Demonstration Group 7 – FHP Adults without Children up to 100% | $587,725,574 | $566,489,543 | $412,034,961 | $322,462,923 | $326,033,807 | |
| Demonstration Group 8 – Family Planning Expansion | $10,471,785 | $10,598,020 | $11,138,799 | $13,378,992 | $12,358,289 | |
| Demonstration Group 9 – Home and Community Based Expansion (HCBS) | N/A | N/A | N/A | N/A | $3,699,108 | |
| Demonstration Group 10 – MLTC Adult Age 18–64 Duals | ||||||
| Demonstration Group 11 – MLTC age 65+ Duals | ||||||
| Demonstration Population 1: State Indigent Care Pool Direct Expenditures (ICP–Direct) | $2,600,000 | |||||
| Demonstration Population 2: Designated State Health Programs to Support Clinic Uncompensated Care Funding (ICP – DSHP) | $2,600,000 | |||||
| Demonstration Population 3: Designated State Health Programs to Support Medical Home Demonstration (DSHP – HMH Demo) | $0 | |||||
| Demonstration Population 4: Designated State Health Programs to Support Potentially Preventable Readmission Demonstration (DSHP – PPR Demo) | $0 | |||||
| Demonstration Population 5: Designated State Health Programs (Various) | ||||||
| DSHP: Orderly Close out of Demo Group 6 | ||||||
| DSHP: APTC Wrap | ||||||
| DSHP For DSRIP | ||||||
| DSRIP | ||||||
| IAAF | ||||||
| With Waiver Total | $123,931,127,812 | $10,499,291,132 | $11,309,400,341 | $12,518,840,867 | $13,518,931,775 | $14,357,398,774 |
| Expenditures (Over)/Under Cap | $20,708,750,711 | $2,879,703,758 | $2,808,034,445 | $3,132,378,919 | $4,095,646,003 | $5,046,523,881 |
| Budget Neutrality Cap (Without Waiver) | DY 14 (10/1/11–9/30/12) Projected | DY 15 (10/1/12–9/30/13) Projected | DY 16 (10/1/13–12/31/13) Projected | DY 17 (1/1/14–3/31/14) Projected | DY 18 (4/1/14 – 12/31/14) Projected | Current Extension Period (10/1/06 – 12/31/14) Projected | DY 1 – DY 18 |
|---|---|---|---|---|---|---|---|
| Demonstration Group 1 – TANF Children under age 1 through 20 | $13,433,986,462 | $14,853,389,777 | $3,975,139,194 | $3,975,139,194 | $12,413,422,113 | $100,010,705,094 | |
| Demonstration Group 2 – TANF Adults 21–64 | $5,353,555,486 | $5,914,379,682 | $1,579,889,213 | $1,579,889,213 | $4,990,265,399 | $39,001,015,574 | |
| Demonstration Group 6 – FHP Adults w/Children | $2,341,067,454 | $2,632,237,613 | $724,658,042 | $14,921,448,066 | |||
| Demonstration Group 8 – Family Planning Expansion | $10,637,764 | $1,845,361 | $12,483,125 | ||||
| Demonstration Group 10 – MLTC Adult Age 18–64 Duals | $247,394,784 | $1,027,336,330 | $260,284,563 | $260,284,563 | $811,742,494 | $2,607,042,734 | |
| Demonstration Group 11 – MLTC age 65+ Duals | $2,554,212,091 | $10,820,566,375 | $2,796,750,566 | $2,796,750,566 | $8,800,737,577 | $27,769,017,175 | |
| W/O Waiver Total | $23,940,854,040 | $35,249,755,138 | $9,336,721,578 | $8,612,063,536 | $27,016,167,583 | $184,321,711,768 | $328,961,590,291 |
| Budget Neutrality Cap (With Waiver) | DY 14 (10/1/11–9/30/12) Projected | DY 15 (10/1/12–9/30/13) Projected | DY 16 (10/1/13–12/31/13) Projected | DY 17 (1/1/14–3/31/14) Projected | DY 18 (4/1/14 – 12/31/14) Projected | Current Extension Period (10/1/06 – 12/31/14) Projected | DY 1 – DY 18 |
|---|---|---|---|---|---|---|---|
| Demonstration Group 1 – TANF Children under age 1 through 20 | $5,426,270,758 | $5,985,938,145 | $1,593,647,093 | $1,592,533,956 | $4,967,097,754 | $42,681,747,299 | |
| Demonstration Group 2 – TANF Adults 21–64 | $3,265,506,602 | $3,601,671,929 | $961,903,936 | $961,993,664 | $3,045,172,437 | $24,506,941,333 | |
| Demonstration Group 5 – Safety Net Adults | $6,027,184,800 | $7,105,677,253 | $1,919,854,079 | $34,551,813,944 | |||
| Demonstration Group 6 – FHP Adults w/Children up tp 150% | $1,194,623,323 | $1,337,606,468 | $366,750,083 | $7,535,200,792 | |||
| Demonstration Group 7 – FHP Adults without Children up to 100% | $373,042,213 | $423,965,223 | $117,318,935 | $3,129,073,179 | |||
| Demonstration Group 8 – Family Planning Expansion | $13,784,643 | $2,435,506 | $74,166,034 | ||||
| Demonstration Group 9 – Home and Community Based Expansion (HCBS) | $3,699,108 | $3,699,108 | $924,777 | $924,777 | $2,774,331 | $15,721,209 | |
| Demonstration Group 10 – MLTC Adult Age 18–64 Duals | $249,276,515 | $999,765,437 | $249,927,129 | $249,927,129 | $780,984,048 | $2,529,880,258 | |
| Demonstration Group 11 – MLTC age 65+ Duals | $2,561,508,288 | $10,403,512,554 | $2,629,869,736 | $2,629,869,736 | $8,298,486,190 | $26,523,246,503 | |
| Demonstration Population 1: State Indigent Care Pool Direct Expenditures (ICP–Direct) | $14,650,000 | $13,700,000 | $3,400,000 | $34,350,000 | |||
| Demonstration Population 2: Designated State Health Programs to Support Clinic Uncompensated Care Funding (ICP – DSHP) | $10,583,333 | $10,583,333 | $2,645,833 | $2,645,833 | $45,791,667 | $74,850,000 | |
| Demonstration Population 3: Designated State Health Programs to Support Medical Home Demonstration (DSHP – HMH Demo) | $100,000,000 | $100,000,000 | $25,000,000 | $25,000,000 | $50,000,000 | $300,000,000 | |
| Demonstration Population 4: Designated State Health Programs to Support Potentially Preventable Readmission Demonstration (DSHP – PPR Demo) | $4,433,333 | $4,433,333 | $1,108,333 | $1,108,333 | $2,216,667 | $13,300,000 | |
| Demonstration Population 5: Designated State Health Programs (Various) | $100,000,000 | $100,000,000 | $300,000,000 | $500,000,000 | |||
| DSHP: Orderly Close out of Demo Group 6 | $363,417,732 | $635,987,007 | $999,404,739 | ||||
| DSHP: APTC Wrap | $7,000,800 | $84,009,600 | $91,010,400 | ||||
| DSHP For DSRIP | $376,000,000 | $376,000,000 | |||||
| DSRIP | $240,000,000 | $240,000,000 | |||||
| IAAF | $1,000,000,000 | $1,000,000,000 | |||||
| With Waiver Total | $19,244,562,917 | $29,992,988,290 | $7,972,349,935 | $5,934,421,960 | $19,828,519,701 | $145,176,705,690 | $269,107,833,502 |
| Expenditures (Over)/Under Cap | $4,696,291,123 | $5,256,766,848 | $1,364,371,644 | $2,677,641,576 | $7,187,647,882 | $39,145,006,077 | $59,853,756,788 |
M:\BPDAR\Special_Populations_Group\1115_Waiver_Info\1115_Annual_and_Quarterly_Report\2014_quarterly–annual_reports\4th_Quarter_Jul_–_Sept\Attachments\Copy_of_BN_1115_Actuals_CMS_1011Final_12/3S0U/2B0M14IT_9T:E2D3_.AxlM
Attachment 2
New York State
Partnership Plan Medicaid Section 1115 Demonstration
Transition Report
I. Introduction
On September 29, 2006, the Centers for Medicare and Medicaid Services (CMS) approved an extension of New York´s 1115 waiver, known as the Partnership Plan, for the period beginning October 1, 2006 and ending September 30, 2010. CMS subsequently approved a series of short–term extensions while negotiations continued on renewing the waiver into 2014. On July 29, 2011, CMS approved a renewal of the Partnership Plan for the period August 1, 2011, through December 31, 2014, with some waiver components expiring earlier to reflect implementation of the Affordable Care Act (ACA).
On January 1, 2014, New York will have made considerable progress in implementing the ACA. Specifically, New York will have expanded coverage, made changes to access to care, and reforms to the payment and delivery system. The ACA expands Medicaid eligibility for individuals under the age of 65, with income at or below 133 percent of the Federal Poverty Level (FPL). In New York State, some of these individuals are currently eligible under New York´s Partnership Plan 1115 Waiver.
II. Transition Plan
Nearly 90 percent of individuals currently covered under New York´s Partnership Plan 1115 waiver will transition to a State Plan eligibility group with coverage through an Alternative Benefit Plan as a result of the Medicaid expansion authorized by the ACA and adopted by New York. For most enrollees in Family Health Plus, the transition to Medicaid using MAGI eligibility rules will occur at renewal. Ideally, the State would choose to switch coverage for the waiver population from Family Health Plus to Medicaid on January 1, 2014. However, this is not possible for all enrollees because not enough information is known to the system about parent/caretaker enrollees to automatically switch them to a MAGI budget on January 1, 2014.
New York intends to stop accepting new applications for Family Health Plus after December 31, 2013. Anyone who submits an application prior to or on that date and are found eligible, will be enrolled in Family Health Plus for 12 months. Effective January 1, 2014, new applications will be evaluated using MAGI eligibility rules, and if eligible, applicants will be enrolled in Medicaid under an Alternative Benefit Plan. New York has chosen the Medicaid State Plan benefit as its Alternative Benefit Plan and will be submitting a SPA for Secretary Approval.
Family Health Plus single and childless couples will have their coverage changed to the Alternative Benefit Plan effective January 1, 2014. Family Health Plus parents and caretaker relatives with income up to 138% FPL will transition to the Alternative Benefit Plan as they renew, effective April 1, 2014. Family Health Plus parents and caretaker relatives with income over 138% FPL to 150% FPL will transition to a qualified health plan, however the State will pay the enrollee´s share of the premium, this does not include the individual´s cost sharing.
As authorized by the waiver under section 1902(e)(14)(A) of the Social Security Act using existing rules, individuals renewing coverage from October 1, 2013 through March 31, 2014, if determined eligible, will enroll in the current plan under the waiver (e.g. Family Health Plus or Medicaid) for twelve months but no longer than through December 31, 2014 for Family Health Plus. Individuals determined ineligible from October 1, 2013 through December 31, 2014, will be sent a notice referring the person to apply for coverage through the Exchange. Individuals renewing from January 1, 2014 through March 31,2014, if found ineligible using existing rules (pre–ACA), must be budgeted using MAGI–like rules following the system migration on February 18, 2014.
New York is building a new eligibility system that automates the MAGI eligibility rules for Medicaid, CHIP, and Advance Premium Tax Credits. The State anticipates over one million individuals are eligible to obtain coverage during the open enrollment period that begins October 1, 2013, and even more may apply. Given the complexity of the system build, the short time for adequately testing all the eligibility permutations and the data services available through the Federal Hub, and the reality that rules and interfaces will continue to be built 3–6 months after open enrollment, New York has decided to mitigate risk by maintaining current Medicaid enrollees in the legacy system until the State is confident it has the automation and system stability to transition over three million current enrollees without a disruption in coverage. New York is prioritizing the ability to provide coverage on January 1, 2014 to the newly eligible populations while doing no harm to current Medicaid enrollees.
To maintain stability in coverage for the over three million Medicaid enrollees whose eligibility will be determined under MAGI, the current legacy system will be modified to calculate budgets using MAGI rules to the maximum extent possible. Effective April 1, 2014, local districts will be able to determine MAGI–like eligibility using the current legacy system for those individuals renewing coverage. Local districts will continue to renew existing enrollees using MAGI–like rules in the legacy system for at least six months or until the new eligibility system is fully automated and is stable enough to handle the transition of over 3 million current recipients. The legacy logic will include:
- No longer counting child support as income
- Not applying income disregards/deductions
- Increased federal poverty levels to comply with ACA income levels
- New AID categories for claiming
- Revised client notices
The current renewal form will be used.
New applications submitted to local departments of social services from October 2013 through December 2013, will have eligibility determined under existing rules in the legacy system and, if eligible, individuals will be enrolled for 12 months of coverage. Individuals that are not eligible due to income will be instructed to reapply through the Exchange. Applications submitted to the Exchange from October 2013 through December 2013, will be determined using MAGI rules and if determined eligible, coverage will be effective January 1, 2014. Applications submitted on or after January 1, 2014, will have eligibility determined through the Exchange under the ACA rules. Individuals who have medical bills or are in need of coverage in the three–month period prior to January 1, 2014, will be referred to the local department of social services for a determination of eligibility for payment/reimbursement of medical bills.
Although New York will transition individuals from the waiver to coverage under the ACA, the State intends to maintain the authority included in the waiver to mandatorily enroll individuals into managed care in counties other than Allegany, Cortland, Duchess, Fulton, Montgomery, Putnam, Orange, Otsego, Schenectady, Seneca, Sullivan, Ulster, Washington and Yates.
- Seamless Transitions
- Determine eligibility under all January 1, 2014, eligibility groups for which the State is required or has opted to provide medical assistance, including the group described in §1902(a)(10)(A)(i)(VIII) for individuals under age 65, regardless of disability status with income at or below 133 percent of the FPL;
The following chart outlines the current waiver population, current coverage, and the coverage options for individuals between 133% FPL and 150% FPL currently enrolled in Family Health Plus. These options include transitioning Family Health Plus enrollees to Advanced Premium Tax Credits. Regardless of which options are available in 2014, all populations will have eligibility determined under the ACA. Table 1: Groups Transitioning from Demonstration to ACA
*The current Partnership Plan 1115 approved NYS comparing income to 160% FPL, but this has not been implemented.Demonstration Eligible Group Current Federal Poverty Level Current Coverage 2014 Coverage Adults who were recipients of or eligible for Safety Net Cash Assistance but are otherwise ineligible for Medicaid (Single individuals and Childless Couples)
[s. 2001(a)(1) and (2)]Income based on Statewide standard of need, approximately 0%–78% FPL Medicaid 0% < 133%
BenchmarkAdults who were recipients of or eligible for Safety Net Cash Assistance but are otherwise ineligible for Medicaid (Single individuals and Childless Couples)
[s. 2001(a)(1) and (2)]Income above the Medicaid income standard but at or below gross 100% FPL Family Health Plus 0% < 133%
BenchmarkChildren 19 and 20 years old
[s. 2001(a)(1) and (2)]Income above the Medicaid income standard but at or below gross 150% FPL* Family Health Plus 0% < 133%
Standard coverage
> 133% < 150%
Standard coverage
>150% APTCParents and caretaker relatives of a child under the age of 21 (who could otherwise be eligible under section 1931 of the Medicaid State Plan)
[s. 2001(a)(1) and (2)]Income above the Medicaid income standard but at or below gross 150% FPL* Family Health Plus 0% < 133%
Benchmark > 133% < 150% State will pay enrollee´s share of APTC premiums and seek federal participation as a designated state health program
>150% APTC (no state assistance) - Identify Demonstration populations not eligible for coverage under the ACA and explain what coverage options and benefits these individuals will have effective January 1, 2014;
All populations currently covered under the waiver will have coverage options under the ACA. In addition, New York plans to implement 12–months of continuous coverage for adults in conjunction with the implementation of the ACA.
In 2007, revisions were made to Chapter 58 of the New York State Social Services Law to provide a 12–month continuous eligibility period to the groups of individuals specified in Table 2, regardless of the delivery system through which they receive Medicaid benefits. Once the State begins exercising this authority, each newly eligible individual´s 12–month period shall begin at the initial determination of eligibility; for those individuals who are redetermined eligible consistent with the Medicaid State plan, the 12–month period begins at that point. At each annual eligibility redetermination thereafter, if an individual is redetermined eligible under the Medicaid State plan, the individual is guaranteed a subsequent 12–month continuous eligibility period.
This proposal will provide stability and continuity of coverage and care to adults in the same way that it has for children on Medicaid. Authority for this population´s eligibility during the 12–month continuous eligibility period is only in the 1115 waiver and therefore, individuals during this period would be eligible for expanded Medicaid levels and benchmark under ACA, and are also subject to continuous coverage. The Department is in the process of exploring the necessary system and program changes and anticipates implementing in January 2014.
Table 2: Groups Eligible for a 12–Month Continuous Eligibility PeriodState Plan Mandatory and Optional Groups Statutory Reference Pregnant women aged 19 or older - 1902(a)(10)(A)(i)(III) or (IV); and
- 1902(a)(10)(A)(ii)(I) and (Ii)
Children aged 19 or 20 1902(a)(10)(A)(ii)(I) and (II) Parents or other caretaker relatives aged 19 or older 1902(a)(10)(A)(ii)(I) and (II) Members of low–income families, except for children 1931 and 1925 - Implement a process for considering, reviewing, and making preliminarily determinations under all January 1, 2014 eligibility groups for new applicants for Medicaid eligibility;
- Local departments of social services will process new applications for Medicaid using current eligibility rules through December 31, 2013.
- New applications submitted to the Exchange from October 2013 through December 2013, will have eligibility determined through the Exchange under ACA rules and, if eligible, enrollment will be effective January 1, 2014. The acceptance notice will inform individuals who have medical bills or are in need of coverage prior to January 1, 2014 to apply at the LDSS. Applicants will be informed of this process online so they may go directly to the LDSS rather than apply through the Exchange before January 1, 2014.
- Beginning January 1, 2014, new applications will go through the Exchange and will be processed through the new integrated eligibility system.
- Conduct an analysis that identifies populations in the Demonstration that may not be eligible for or affected by the ACA and the authorities the State identifies that may be necessary to continue coverage for these individuals;
Nearly all of the populations covered under the waiver will be covered under the ACA and those populations who are subject to continuous coverage will also have it applied under the waiver.
Parents/caretakers with MAGI income between 138% and 150% of FPL will no longer be eligible for a Medicaid waiver category but will be eligible for a tax credit under the ACA provided they do not have access to affordable coverage. CMS approved expenditure authority to allow the state to claim federal matching dollars for the designated state health program (DSHP), this will provide premium subsidies to parents and caretaker relatives with incomes between 138%–150% FPL, who enroll in a silver level Qualified Health Plan using Advanced Premium Tax Credits.
19 and 20–year old´s who are living with parents with MAGI income between 138% and 155% of the FPL will no longer be eligible for a Medicaid waiver category, but will be eligible for Medicaid under MOE requirements.
- Develop a modified adjusted gross income (MAGI) calculation for program eligibility.
New York is developing a new eligibility system that will automate program eligibility based on the MAGI eligibility rules as defined by CMS. All applications submitted to the Exchange after January 1, 2014 will be processed using the MAGI eligibility rules in the new system.
As described above, to maintain stability in coverage for the over three million Medicaid enrollees whose eligibility will be determined under MAGI, the current legacy system will be modified to calculate budgets using MAGI rules to the maximum extent possible. Effective April 1, 2014, local districts will be able to determine MAGI–like eligibility using the current legacy system for individuals renewing coverage. Local districts will continue to renew existing enrollees using MAGI–like rules in the legacy system for at least six months, or, until the new eligibility system is fully automated and is stable enough to handle the transition of over three million current recipients.
New York opted for CMS to develop a modified adjusted gross income (MAGI) equivalency level for converting existing net eligibility levels to MAGI eligibility levels. New York received converted eligibility levels and they are currently in effect.
- Determine eligibility under all January 1, 2014, eligibility groups for which the State is required or has opted to provide medical assistance, including the group described in §1902(a)(10)(A)(i)(VIII) for individuals under age 65, regardless of disability status with income at or below 133 percent of the FPL;
- Access to Care and Provider Payments
- Provider Participation. The State must identify the criteria that will be used for reviewing provider participation in (e.g. demonstrated data collection and reporting capacity) and means of securing provider agreements for the transition;
The service delivery network for a Managed Care Organization ("MCO”) is county specific and is comprised of primary, specialty and ancillary providers as well as related institutions consistent with the benefit package. Each county network must include at least one hospital, one inpatient and outpatient mental health facility as well as at least one substance abuse inpatient and outpatient facility. This applies to HMOs participating in government programs and those that have exclusive commercial membership.
The behavioral health network is required to have both individual providers, outpatient facilities and inpatient facilities. The facilities must include mental health and substance abuse services. In the case of outpatient mental health, at least one facility in the county must be licensed by the Office of Mental Hygiene pursuant to Article 31 of the Mental Hygiene Law, or be a facility operated by the Office of Mental Hygiene. The mental health inpatient facility can be either a psychiatric center under the jurisdiction of the Office of Mental Hygiene, or, a unit or part of a hospital operating under Article 28 of the Public Health Law.
The provision of alcohol and substance abuse services must also be provided in an outpatient facility and an inpatient facility. These facilities must have the capacity to provide substance abuse treatments. The inpatient facilities must have the capacity to provide detoxification and rehabilitation services.
In addition to the above, Medicaid networks must also include traditional Medicaid providers, i.e., presumptive eligibility providers, Designated AIDS Centers and Federally Qualified Health Centers (FQHCs), where available. With the implementation of the homeless population into Medicaid managed care, we also require the MCO to contract with available federally qualified 330 H providers in every county they are available in. - Adequate Provider Supply. The State must provide the process that will be used to assure adequate provider supply for the State plan and Demonstration populations affected by the Demonstration on December 31, 2013;
The MCO is required to have the full array of contracted providers in each county. However, in rural counties, this may not be possible due to a lack of resources within the county. When there is a lack of a provider type in a county the MCOs may contract with providers in adjacent counties, or service area, to fulfill the network requirements. In some cases where counties border neighboring states and the normal access and referral pattern for obtaining medical services in those areas is to go across state boundaries, MCOs may request approval to augment their networks by adding those out of state providers. Attachment 1 provides a listing of the core provider types for all lines of business.
In addition to the full array of required health care providers, the network must include sufficient numbers of each provider type, be geographically distributed and ensure choice of primary and specialty care providers. The Public Health Law requires the MCO member a choice of at least three geographically accessible primary care providers. It is the department´s policy that MCOs are required to contract minimally with two of each required specialist provider types per county. However, additional providers may be required based on enrollment and to ensure geographic accessibility.
The Department of Health has developed time and distance standards for provider networks to which MCOs are required to adhere. For all Medicaid, HIV Special Needs Plans, and Child Health Plus health products, the time and distance standard, is as follows:- metropolitan areas – 30 minutes by public transportation;
- non–Metropolitan areas – 30 minutes or 30 miles by public transportation or by car;
- in rural areas transportation requirements may exceed these standards if justified.
The first part of the review is an electronic analysis based upon program parameters established by the Department to determine if each county has an adequate number of the required core providers. The second part of the analysis is a manual review of reports that are produced. Examples of these reports include whether there are a sufficient number of providers in the county to provide a choice of primary and specialty providers and a comparison of providers not contracting with a specific MCO but who have contracts with other MCOs in the same county. The reports are then summarized and MCOs are notified of any access issues identified within their certified areas of operation. MCOs are required to review the summaries and report back to the Department. The Department will then have MCOs sign an attestation that members may obtain services on an out of network basis to the nearest provider, but not greater than 30 minutes or 30 miles from the members´ residence. This attestation remains in place until the MCO is able to successfully address the noted provider inadequacy. - Provider Payments. The State will establish and implement the necessary processes for ensuring accurate encounter payments to providers entitled to the prospective payment services (PPS) rate (e.g., certain FQHCs and RHCs) or the all–inclusive rate (e.g., certain Indian Health providers);
The State will pay the PPS rate through the eMedNY FFS system for eligible Medicaid enrollees. For enrollees in Medicaid managed care, the State will make supplemental payments to eligible FQHC/RHC´s to make up the difference between the PPS rate and the average managed care payment.
- Provider Participation. The State must identify the criteria that will be used for reviewing provider participation in (e.g. demonstrated data collection and reporting capacity) and means of securing provider agreements for the transition;
- System Development or Remediation. The Transition Plan for the Demonstration is expected to expedite the State´s readiness for compliance with the requirements of the Affordable Care Act and other Federal legislation. System milestones that must be tested for implementation on or before January 1, 2014 include: i. Replacing manual administrative controls with automated processes to help support a smooth interface among coverage and delivery system options that is seamless to beneficiaries;
New York is working to simplify and align both our rules and processes in accordance with the ACA requirements, and to automate MAGI eligibility determinations and verifications to the maximum extent practicable, and to promote a more seamless customer experience. - Progress Updates. After submitting the initial Transition Plan for CMS approval, the State must include progress updates in each quarterly and annual report. The Transition Plan shall be revised as needed;
The State will provide quarterly and annual reports. - Implementation
- By July 1, 2013, the State must begin to implement a simplified, streamlined process for transitioning eligible enrollees in the Demonstration to Medicaid, the Exchange, or other coverage options in 2014. In transitioning these individuals from coverage under the waiver to coverage under the State plan, the State will not require these individuals to submit a new application;
As described above, New York will transition eligible childless adult enrollees in the Demonstration to Medicaid on January 1, 2014. Parents/caretakers will be transitioned at their renewal beginning April 2014 to either Medicaid or QHP coverage. - On or before December 31, 2013, the State must provide notice to the individual of the eligibility determination using a process that minimizes demands on the enrollees;
New York plans to provide appropriate notices that minimize demands on enrollees to the maximum extent possible.
- By July 1, 2013, the State must begin to implement a simplified, streamlined process for transitioning eligible enrollees in the Demonstration to Medicaid, the Exchange, or other coverage options in 2014. In transitioning these individuals from coverage under the waiver to coverage under the State plan, the State will not require these individuals to submit a new application;
December 29, 2014
Attachment 1
Core Provider Types for All Lines of Business.
NOTE: Data will be provided when
Attachment 3
Managed Long Term Care
Partial Capitation Plans
October 2013 – September 2014
| Plan Name | Oct–13 Enrollment |
Nov–13 Enrollment |
Dec–13 Enrollment |
Jan–14 Enrollment |
Feb–14 Enrollment |
Mar–14 Enrollment |
Apr–14 Enrollment |
May–14 Enrollment |
Jun–14 Enrollment |
Jul–14 Enrollment |
Aug–14 Enrollment |
Sep–14 Enrollment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aetna Better Health | 1,796 | 1,951 | 2,119 | 2,220 | 2,366 | 2,414 | 2,515 | 2,575 | 2,619 | 2,639 | 2,758 | 2,809 |
| AgeWell New York | 1,870 | 2,101 | 2,287 | 2,466 | 2,609 | 2,766 | 2,909 | 3,103 | 3,234 | 3,355 | 3,471 | 3,601 |
| AlphaCare | 286 | 263 | 248 | 257 | 288 | 322 | 376 | 453 | 554 | 690 | 774 | 879 |
| Amerigroup | 2,875 | 2,893 | 2,895 | 2,857 | 2,827 | 2,807 | 2,827 | 2,799 | 2,798 | 2,828 | 2,839 | 2,854 |
| ArchCare Community Life | 1,408 | 1,559 | 1,731 | 1,775 | 1,818 | 1,861 | 1,845 | 1,871 | 1,867 | 1,885 | 1,899 | 1,921 |
| CCM Select | 9,854 | 10,023 | 10,024 | 10,002 | 9,995 | 9,865 | 9,713 | 9,650 | 9,370 | 8,919 | 8,601 | 8,130 |
| Centers Plan for Healthy Living | 882 | 950 | 1,081 | 1,116 | 1,242 | 1,282 | 1,444 | 1,604 | 1,790 | 1,974 | 2,042 | 2,062 |
| Elant | 381 | 395 | 438 | 464 | 508 | 525 | 550 | 581 | 611 | 639 | 670 | 717 |
| Elderplan | 10,787 | 11,012 | 11,114 | 11,025 | 10,923 | 10,853 | 10,745 | 10,702 | 10,605 | 10,640 | 10,642 | 10,706 |
| Elderserve | 10,064 | 10,166 | 10,238 | 10,277 | 10,319 | 10,268 | 10,349 | 10,358 | 10,369 | 10,400 | 10,443 | 10,433 |
| ErieNiagara MLTCP | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 15 | 60 | 106 | 141 | 165 |
| Extended MLTC | 97 | 132 | 172 | 195 | 207 | 230 | 238 | 246 | 260 | 287 | 298 | 319 |
| Fidelis Care at Home | 7,185 | 7,466 | 7,699 | 7,825 | 7,959 | 8,030 | 8,151 | 8,353 | 8,627 | 8,911 | 9,132 | 9,336 |
| Guildnet | 13,931 | 14,240 | 14,397 | 14,411 | 14,347 | 14,213 | 14,349 | 14,411 | 14,363 | 14,464 | 14,508 | 14,526 |
| Hamaspik Choice | 0 | 3 | 59 | 103 | 116 | 135 | 186 | 220 | 301 | 369 | 419 | 470 |
| HHH Choices | 2,354 | 2,377 | 2,386 | 2,373 | 2,358 | 2,311 | 2,331 | 2,297 | 2,279 | 2,259 | 2,239 | 2,187 |
| HIP of Greater New York | 1,204 | 1,268 | 1,346 | 1,351 | 1,364 | 1,364 | 1,379 | 1,363 | 1,338 | 1,330 | 1,327 | 1,343 |
| Independence Care Systems | 4,925 | 5,008 | 5,046 | 5,076 | 5,067 | 5,009 | 5,055 | 5,077 | 5,081 | 5,091 | 5,118 | 5,179 |
| Integra | 495 | 572 | 670 | 748 | 817 | 951 | 1,076 | 1,174 | 1,263 | 1,476 | 1,595 | 1,813 |
| MetroPlus MLTC | 419 | 429 | 445 | 465 | 472 | 505 | 511 | 536 | 577 | 603 | 627 | 673 |
| Montefiore HMO | 0 | 4 | 25 | 86 | 135 | 194 | 252 | 299 | 339 | 381 | 406 | 444 |
| North Shore– LIJ Health Plan | 0 | 19 | 301 | 481 | 515 | 558 | 605 | 660 | 731 | 818 | 909 | 1,050 |
| Prime Health Choice | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 7 |
| Senior Health Partners | 10,535 | 10,745 | 10,867 | 10,924 | 11,011 | 11,019 | 11,177 | 11,222 | 11,242 | 11,360 | 11,455 | 11,665 |
| Senior Network Health | 437 | 446 | 450 | 458 | 458 | 457 | 466 | 478 | 481 | 479 | 490 | 502 |
| Senior Whole Health | 471 | 523 | 605 | 668 | 704 | 781 | 829 | 885 | 916 | 1,056 | 1,142 | 1,308 |
| Total Aging in Place Program | 124 | 120 | 119 | 119 | 120 | 125 | 124 | 127 | 127 | 139 | 138 | 136 |
| United Healthcare | 461 | 507 | 553 | 604 | 621 | 651 | 687 | 731 | 770 | 826 | 900 | 985 |
| Village Care | 2,287 | 2,346 | 2,461 | 2,550 | 2,631 | 2,703 | 2,800 | 2,851 | 2,944 | 3,043 | 3,161 | 3,237 |
| VNA HomeCare Options | 142 | 156 | 178 | 199 | 202 | 236 | 260 | 305 | 345 | 366 | 392 | 435 |
| VNS Choice | 17,974 | 17,929 | 17,772 | 17,683 | 17,688 | 17,399 | 17,641 | 17,729 | 17,571 | 17,360 | 17,107 | 17,014 |
| WellCare | 5,210 | 5,350 | 5,524 | 5,605 | 5,695 | 5,840 | 6,015 | 6,155 | 6,295 | 6,451 | 6,521 | 6,660 |
| TOTAL | 108,454 | 110,953 | 113,250 | 114,383 | 115,382 | 115,674 | 117,405 | 118,830 | 119,727 | 121,144 | 122,166 | 123,566 |
Attachment 4 – Hospital Medical Home Demonstration
| About This Report |
|---|
| This report displays the average rates of measures and the average site–le vel composite score over time, from Q3 2013 through 02 2014, for measures included in the Improved Access and Coordination Between Primary and Specialty Care project for sites participating in the HMH demonstration. Data presented in this report has not been validated. This report should be used for quality improvement purposes only. |
| Calculating the Composite Score: The site–level composite score is the average rate of 5 required measures in this domain by site. |
| For this domain, the measures that contributed to the composite score are: |
| Post Specialty Visit Care: Numerator: Number of patients from the outpatient site seen for post specialty visit care within the timeframe recommended. Denominator: All patients from the outpatient site being referred. |
| Referrals & Inadequate Documentation: Numerator: Number of referrals from the outpatient site without adequate documentation. Denominator: All referrals from the outpatient sit e. A lower rate is desirable for this measure. |
| Referrals Made and Not Completed: Numerator: Number of referrals from the outpatient site made and not completed. Denominator: All referrals from the outpatient site. A lower rate is desirable for this measure. |
| Rejected Referrals: Numerator: Number of referrals from by the outpatient site rejected by Specialists. Denominator: All referrals from the outpatient site. A lower rate is desirable for this measure. |
| Specialty Care Wait Times: Numerator: Number of patients from the outpatient site seen within the timeframe requested by the primary care provider. Denominator: II patients from the outpatient site being referred. |
| Wait Times for Behavioral Health Services: Numerator: Number of patients from the outpatient site needing behavioral health services seen within the timeframe requested by the primary care provider. Denominator: All patients from the outpatient site being referred. |
| If a site did not report data on a required metric (or reported an invalid rate or a denominator of 9999), their composite score was calculated as the sum of all rates for available required metrics divided by number of rates that contributed to the numerator. |
Trends in HMH Coordination Between Primary and Specialty Care Metrics and Composite Scores
Q3 2013– Q2 2014
*Lower rates are desirable for 3 measures in this graph
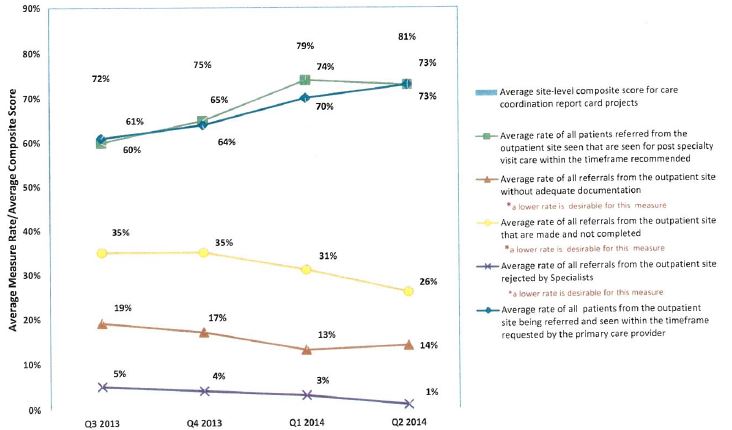
| About This Report |
|---|
| This report displays the average rates of measures and the average site–level composite score over time, from Q3 2013 through Q2 2014, for measures included in the Integration of Physical and Behavioral Health project for sites participating in the HMH demonstration. Data presented in this report has not been validated. This report should be used for quality improvement purposes only. |
| Calculating the Composite Score: The site–level composite score is the average rate of 6 required measures in this domain by site. |
| For this domain, the measures that contributed to the composite score are: |
| Depression and Pain Management: Numerator: Number of primary care clinicians at the outpatient site who have completed a training program in pain management and depression. Denominator: All primary care clinicians at the outpatient site. |
| Depression Screening: Numerator: Number of adult patients per year from the outpatient sit e who received a PHQ–2 or a PHQ–9. Denominator: All patients from the outpatient site. |
| Enrolled Patients with Psychiatric Consult: Numerator: Number of patients enrolled in the Collaborative Care Initiative referred for psychiatric consultation. Denominator: All patients enrolled in the Collaborative Care Initiative. |
| Patients Enrolled in a Physical–Behavioral Health Program: Numerator: Number of patients from the outpatient sit e screening positive for depression who enrolled in physical behavioral health care coordination program (Collaborative Care Initiative). Denominator: All patients from the outpatient site screened positive for depression. |
| PHQ–9 Decrease s Below 10 in 16 Weeks or Greater: Numerator: Number of patients enrolled in the Collaborative Care Initiative whose PHQ–9 went from at >10 to <10 in 16 weeks or greater. Denominator: All patients enrolled in the Collaborative Care Initiative. |
| Wait Times for Behavioral Health Services: Numerator: Number of patients from the outpatient site needing behavioral health services seen with in the timeframe requested by the primary care provider. Denominator: All patients from the outpatient site being referred. |
| If a site did not report data on a required metric (or reported an invalid rat e or a denominator of 9999), their composite score was calculated the sum of all rat es for available required metrics divided by number of rates that contributed to the numerator. Controlled Substances, Care Manager FTE, and Patients Diagnosed with De pression are required measures in this domain, but were not used to calculate the composite score. |
Trends in HMH Behavioral Health Metrics and Composite Scores
Q3 2013 – Q2 2014
*higher rates are desirable for all measures and composites in this graph
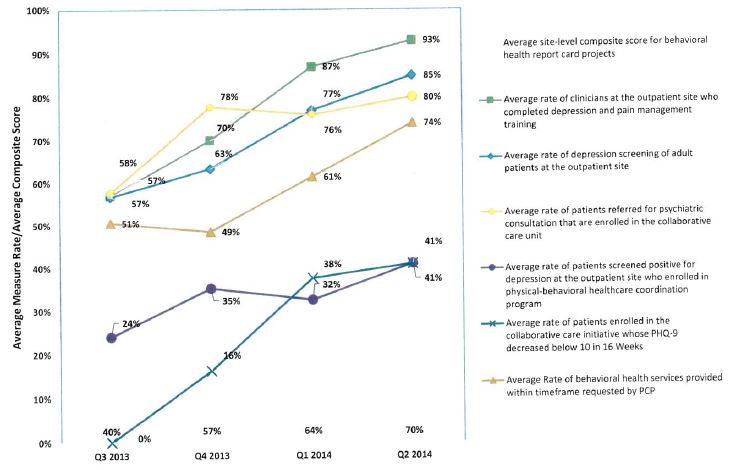
| About This Report |
|---|
| This report displays the average rates of measures and the average site–level composite score over time, from Q3 2013 through Q2 2014, for measures included in the Care Transition and Medication Reconciliation project for sites participating in the HMH demonstration. Data presented in this report has not been validated. This report should be used for quality improvement purposes only. |
| Calculating the Composite Score: The site–level composite score is the average rate of 7 requiredmeasures in this domain by site. |
| For this domain, the measures that contributed to the composite score are: |
| Admission Medication Reconciliation Rate: Numerator: Number of patients from the outpatient site with documentation of medications reconciled on admission. Denominator: Number of patients admitted from the outpatient site. |
| Follow Up Call: Numerator: Number of high–risk Medicaid patients from the outpatient sit e discharged that had a follow up phone call within 48 hours of discharge. Denominator: All high–risk Medicaid patients from the outpatient site discharged from an inpatient facility. |
| Follow Up Visit: Numerator: Number of high–risk Medicaid patients from the outpatient site discharged that completed a follow up PCP visit within 48 hours of discharge. Denominator: All high–risk Medicaid patients from the outpatient site discharged from an inpatient facility. |
| Medicaid Readmission: Numerator: Number high risk Medicaid patients from the outpatient site readmitted within thirty (30) days. Denominator: Number high risk Medicaid patients from that site with an initial admission. A lower rate is desirable for this measure. |
| Reconciled Medication List Received by Discharged Patients: Numerator: Number of patients from the outpatient site discharged from an inpatient facility who received a reconciled medication list at the time of discharge including, at a minimum, medications in the specified categories. Denominator: All patients discharged from an inpatient facility to home/self–care/ or any other site of care. |
| Timely Transmission of Transition Record: Numerator: Number of patients from the outpatient site for whom the specified transition record was transmitted from the hospital within 24 hours of discharge. Denominator: Number of patients from the outpatient site discharged from an inpatient facility. |
| Transition Record with Specified Elements Received by Discharged Patients: Numerator: Number of patients from the outpatient site or their caregiver(s) who received a specified transition record & review at the time of discharge. Denominator: Number of patients from the outpatient site discharged from an inpatient facility. |
| If a site did not report data on a required metric (or reported an invalid rate or a denominator of 9999), their composite score was calculated as the sum of all rates for available required metrics divided by number of rates that contributed to the numerator. |
Trends in HMH Care Transitions and Medication Reconciliation Metrics and Composite Scores
Q3 2013– Q2 2014
*lower rate is desirable for 1 measure in this graph
| About This Report |
|---|
| This report displays the average rates of measures and the average site–level composite score over time, from Q3 2013 through Q2 2014, for measures included in the Enhanced Interpretation Services for Culturally Competent Care project for sites participating in the HMH demonstration. Data presented in this report has not been validated. This report should be used for quality improvement purposes only. |
| Calculating the Composite Score: The site–level composite score is the average rate of 5 required measures in this domain by site. |
| For this domain, the measures that contributed to the composite score are: |
| Cross Cultural Training: Numerator: Number of staff from the outpatient site who have completed training in cross–cultural health, diversity, or cultural competency in the past 12 month s. Denominator: Total number of staff in the outpatient site. |
| Demographic Data Recorded: Numerator: Number of visits in the outpatient site in which the patient´s gender, race, ethnicity, date of birth, and preferred language are recorded. Denominator: All visits in the outpatient site. |
| Discharge Instructions in Language of Patient: Numerator: Number of limited English–proficient patients from the outpatient site receiving both initial assessment and discharge instructions supported by assessed and trained interpretors or from bilingual providers and lingual workers/employees assessed for language proficiency. Denominator: All limited English–proficient patients from the outpatient site being discharged. |
| Interpreter Wait Time: Numerator: Number of interpretor encounters in the outpatient site in which the wait time for an interpreter to arrive is 15 minutes or less. Denominator: The total number of interpreter encounters in the outpatient site. |
| Prescriptions in Language of Patient: Numerator: Number of prescription labels not in English from prescriptions written in the outpatient site. Denominator: Number of prescription labels written in the outpatient site for whom English is not the patient´s preferred language. |
| If a site did not report data on a required metric (or reported an invalid rate or a denominator of 9999), their composite score was calculated as the sum of all rates for available required metrics divided by number of rates that contributed to the numerator. |
Trends in HMH Culturally Competent Care Metrics and Composite Scores
Q3 2013 – Q2 2014
*higher rates are desirable for all measures and composites in this graph
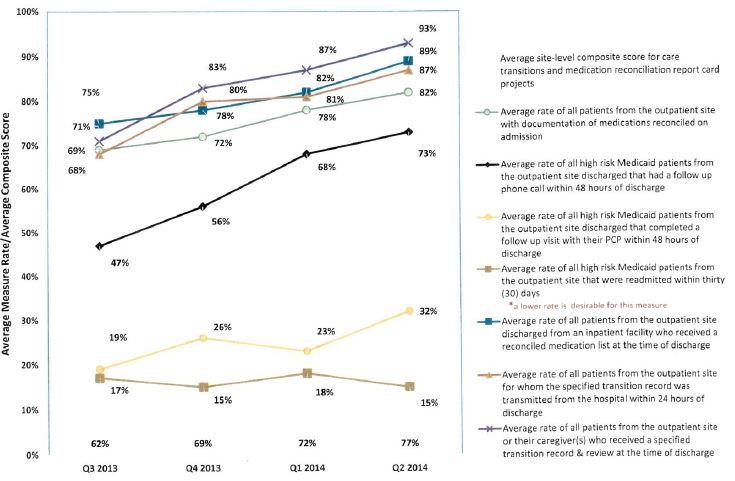
Attachment 5
New York DSRIP 1115 Quarterly Report
July 1, 2014 – September 30, 2014
New York State Department of Health
Office of Health Insurance Programs
Albany, New York
www.health.ny.gov/dsrip
New York DSRIP Section 1115 Quarterly Report
Introduction
On April 14, 2014, New York finalized terms and conditions with the Centers for Medicare and Medicaid Services (CMS) for a groundbreaking amendment that will allow the state to reinvest $8 billion in federal savings generated by Medicaid Redesign Team (MRT) reforms. The MRT waiver amendment amends New York´s Section 1115 Demonstration, the Partnership Plan, and will transform the state´s health care system, bend the Medicaid cost curve, and ensure access to quality care for all Medicaid members. The agreement authorizes funding through the current demonstration end date of December 31, 2014 and will continue upon agreement of the demonstration´s renewal from January 1, 2015 through December 31, 2019.
The Medicaid 1115 waiver amendment will enable New York to fully implement the MRT action plan, facilitate innovation, lower health care costs over the long term, and save scores of essential safety net providers from financial ruin. The waiver allows the state to reinvest over a five–year period $8 billion of the $17.1 billion in federal savings generated by MRT reforms.
The waiver amendment dollars will address critical issues throughout the state and allow for comprehensive reform through a Delivery System Reform Incentive Payment (DSRIP) program. The DSRIP program will promote community–level collaborations and focus on system reform, specifically a goal to achieve a 25 percent reduction in avoidable hospital use over five years. Safety net providers will be required to collaborate to implement innovative projects focusing on system transformation, clinical improvement and population health improvement. Single providers will be ineligible to apply. All DSRIP funds will be based on performance linked to achievement of project milestones.
The $8 billion reinvestment will be allocated in the following ways:
- $500 Million for the Interim Access Assurance Fund – temporary, time limited funding to ensure current trusted and viable Medicaid safety net providers can fully participate in the DSRIP transformation without disruption
- $6.42 Billion for Delivery System Reform Incentive Payments (DSRIP) – including DSRIP Planning Grants, DSRIP Provider Incentive Payments, and DSRIP Administrative costs
- $1.08 Billion for other Medicaid Redesign purposes – this funding will support Health Home development, and investments in long term care, workforce and enhanced behavioral health services
In addition, the special terms and conditions also commit the state to comprehensive payment reform and continuing New York´s effort to effectively manage its Medicaid program within the confines of the Medicaid Global Spending Cap.
This quarterly report summarizes the program development and implementation activities for the DSRIP program for the period from July 1, 2014 through September 30, 2014.
Year 0 Focus
This report summarizes the activities from the second quarter of Year 0. The agreement between New York and CMS includes a pre–implementation year, known as Year 0, which is the period between April 14, 2014 and March 31, 2015. Stakeholder education and engagement, planning activities, procurement of DSRIP contractors and development of key DSRIP policies and procedures are the main areas of focus during Year 0. An extensive DSRIP website was launched on April 14, 2014 and is available at www.health.ny.gov/dsrip. A high–level Year 0 timeline outlining key activities is available on the website and included with this report. (Attachment A).
Stakeholder Engagement Activities, Transparency, and Public Forums
The period covering July 1, 2014 through September 30, 2014 included extensive stakeholder engagement activity conducted by DOH and by its selected vendors for the DSRIP Support Team and DSRIP Independent Assessor.
- On August 1, 2014, DOH hosted a DSRIP Attribution and Valuation Webinar to walk through Project 2.d.i ("the 11th Project”) and provide updates on the DSRIP attribution and valuation methodologies. This webinar was recorded on Friday, August 1, 2014 was co–led by Jason Helgerson, NYS Medicaid Director and Greg Allen, Director of the Division of Program Development and Management within the NYS Office of Health Insurance Programs (OHIP). The slides and recorded webinar are available on the DSRIP website.
- In September 2014, the Westchester Medical Center led a webinar on the planning process they have gone through in developing their comprehensive DSRIP Project Plan. The slides and recorded webinar are available on the DSRIP website.
- In August 2014, DOH hosted the second half of a two–part webinar series that details the steps and processes a PPS should take in carrying out their DSRIP Community Needs Assessment in order to help drive proper project selection in their DSRIP application.
- On September 10, 2014, DOH hosted a webinar to provide information on the integral role of Health Homes in DSRIP Performing Provider Systems (PPS), including the role of downstream Health Home care managers.
- On September 29, 2014, DOH, with the Independent Assessor, released the DSRIP Project Plan Application, Project Milestones and Metrics, and Scoring Guide for Public Comment.
- Public comments on Attachments I and J were incorporated into redlined versions of the STCs.
- New York collected comment on a draft of the DSRIP Evaluation Plan through July 21, 2014
- The DSRIP Support Team (DST) developed an online survey to be filled out by all PPSs to gather preliminary information about their current status and needs. The data collected from the survey helped understand the level of support potentially required for each PPS and also helped guide the subsequent development of support materials.
- The DST performed outreach to DSRIP stakeholders to ensure their awareness of and involvement in the DSRIP Program. Stakeholders included other DOH bureaus, other NYS agencies, industry associations, and downstream providers.
- The DST formed, trained and deployed teams to the regions to support PPSs with application development.
- The DST assisted DOH with the development of the Midpoint Deliverable questionnaire that provided DOH insight regarding the PPSs´ progress in becoming compliant with DSRIP requirements. In addition, DOH used the finalized, DOH–developed questionnaire as a trigger for second design grant payment.
- The DST developed an online PPS status reporting tool. The tool is used by the PPSs to provide their current progress against DSRIP objectives. It is also used by the DST members to supplement the PPSs´ self–assessment and gathers information weekly for reporting to DOH.
- The DST conducted workshops with DOH on establishing a digital forum for PPSs to share information, collectively solve challenges and claim ownership over the DSRIP process (MRT Innovation Exchange).
Interim Access Assurance Fund
The purpose of the Interim Access Assurance Fund (IAAF), part of the DSRIP program, is to assist safety net hospitals in severe financial distress and major public hospital systems to sustain key health care services as they participate with other providers to develop proposals for systems of integrated services delivery to be funded and implemented under the DSRIP.
$500 million in temporary funding is available in Year 0 through the IAAF will enable recipient hospitals to work toward sustainable operations and, to maintain critical services to their community as they work with other partner providers to develop integrated Performing Provider Systems (PPS) eligible for DSRIP funding.
In accordance with the waiver amendment Special Terms & Conditions (STCs) the State is required to, within 10 days of initiating Interim Access Assurance Fund (IAAF) payments, submit a report to the Centers for Medicare & Medicaid Services (CMS) that states the total amount of the payment or payments, the amount of FFP that the state will claim, the source of the non– Federal share of the payments, and documentation of the needs and purposes of the funds to assure CMS of non–duplication. The report must include all other Medicaid payments (e.g. base, supplemental, VAP, DSH) the provider receives to demonstrate that existing payments are not sufficient to meet financial needs of the providers.
IAAF payments for Large Public Providers began on June 18, 2014 while IAAF payments for Safety Net providers began June 27, 2014. All of the IAAF payment reports submitted to CMS are included as Attachment B.
More information is also available on the IAAF web page.
DSRIP Project Design Grants
The state has made available funding to emerging Performing Provider Systems to develop comprehensive DSRIP Project Plans. Applications for these planning funds were due on Thursday, June 26, 2014 and were collected by the state. Applications for DSRIP Project Design Grants were received from 49 entities across the state.
The DOH announced awards on August 6, 2014, with 42 of the 49 applicants receiving awards. The DOH included conditions with awards to certain applicants including considerations for merging or partnering with other PPSs and for geographic overlap with other PPSs.
Attachment C contains the final award allocation of the DSRIP Design Grant Awards as of September 3, 2014. The regional map and a schedule of the DSRIP Design Grant Awards are available here
DSRIP Safety Net and Vital Access Providers
The DSRIP safety net appeal process continued during this quarter. NYS had created preliminary safety net lists from cost report information. The lists that were posted were developed based upon data readily available to the DOH from various reports filed either with DOH, OASAS, OMH or OPWDD that contained the data needed to determine if a provider meets the respective criteria to be classified as a safety net provider. The providers on those lists could then utilize the appeal form process to provide documentation for DOH to reevaluate that provider and determine that they may in fact meet the specific safety net criteria.
The initial DSRIP Safety Net Appeal process closed on June 11, 2014. This did not include the physicians and pharmacies. The first physician and pharmacy appeal process ended on July 15, 2014. The second DSRIP safety net appeal process ended on August 27, 2014. This included every provider group.
The Vital Access Provider (VAP) Exception process opened on September 29, 2014 and ended on October 24, 2014 for all Medicaid providers, physicians and pharmacies for facilities that did not qualify by the Safety Net Definition by calculation or by appeal. If the exception is granted, then the applicant will be qualified and can fully participate in the DSRIP program. Non– qualifying facilities are limited; they may only receive up to 5% (as a group) of their PPS´s award.
Complete lists of approved safety net providers and VAP exception appeals can be found on the DSRIP website.
In the upcoming quarter, DOH will collect DSRIP Program Design Grant Midpoint deliverable reports from awarded Performing Provider System ("PPS"). The DSRIP program Design Grant Midpoint deliverable will be due October 15, 2014 and will include a questionnaire which will be used to evaluate if the PPS would be awarded the second half of the design grant award to be disbursed on November 3, 2014. The original questionnaires and responses will be made publically available on the DSRIP website.
DSRIP Fund
The DOH incorporated public comment in finalizing the DSRIP Project Toolkit in August 2014. The DSRIP Project Toolkit was also updated to include project 2.d.i (the 11th project). The DSRIP Project Toolkit was further updated in October 2014 to align with the reporting measures outlined in Attachment J.
The DOH, with the Independent Assessor, developed comprehensive DSRIP Project Plan application and Scoring Guide during this quarter. The DSRIP Project Plan application also included a comprehensive Project Requirements Milestones and Metrics document that outlined the Domain 1 process measures for each of the 44 projects across Domains 2 through 4. The DSRIP Project Plan application with accompanying Scoring Guide and Project Requirements Milestones and Metrics documents were released for public comment on 9/29
All materials for the DSRIP Project Plan application are available on the DSRIP website.
Quarterly expenditures related to IAAF, DSRIP Project Design Grants, and DSRIP Fund
IAAF payments began for Large Public Providers began on June 18, 2014 while IAAF payments for Safety Net providers began June 27, 2014. Subsequent IAAF payments were based on three separate categories of providers and made at the following times:
- Large Publics (excluding HHC): July 22, 2014; September 15, 2014
- Large Publics (HHC only): July 24, 2014; August 22, 2014; August 29, 2014
- Safety Net: August 1, 2014; August 25, 2014; September 15, 2014
Attachment B contains all of the IAAF payments made during the July 1, 2014 through September 30, 2014 quarter.
DSRIP Project Design Grant funds for the 42 approved applications were initially distributed on August 22, 2014. Attachment C contains the DSRIP Project Design Grant payments made during the July 1, 2014 through September 30, 2014 quarter.
DSRIP Fund performance payments are scheduled to begin April 1, 2015 for approved DSRIP Project Plan Applications.
Other New York State DSRIP Program Activity
DSRIP Project Management
DSRIP project management efforts continued in to this quarter with the continuation of the use of the successfully established MRT process and work plan format, with key DSRIP staff meeting twice weekly and reporting on progress of DSRIP activity to New York´s Medicaid Director. DSRIP project management meetings have now expanded to include staff from the DSRIP Independent Assessor and the DSRIP Support Team as well as CMS, the vendor tasked with creating the DSRIP project Plan Application web tool. Meetings will continue through the end of Year 0, and will likely continue through DSRIP Years 1 – 5.
New York has also established additional, separate project management meetings with their vendors for the DSRIP Independent Assessor and the DSRIP Support Team and a joint meeting involving key staff from New York, the DSRIP Independent Assessor, and the DSRIP Support Team. These meetings allow for more in–depth reviews of project deliverables with each vendor and to address any policy considerations requiring New York input.
Independent Assessor
New York released a Funding Availability Solicitation (FAS) for the purpose of procuring the services of an entity to serve as the DSRIP Independent Assessor on May 20, 2014. Through the FAS procurement process, New York selected Public Consulting Group (PCG) to serve as the DSRIP Independent Assessor. Notification of the award was made on July 31, 2014 and PCG began work on August 4, 2014.
The DSRIP Independent Assessor´s tasks include, but are not limited to, creating an application and application review tool as well as a process for a transparent and impartial review of all proposed project plans, making project approval recommendations to the state using CMS– approved criteria, assembling an independent review panel chosen by the Department of Health based on standards set forth in the DSRIP STCs, conducting a transparent and impartial mid–point assessment of project performance during the third year to determine whether the DSRIP project plans merit continued funding or need plan alterations, and assisting with the ongoing monitoring of performance and reporting deliverables for the duration of the DSRIP program. State review of proposals was underway at the close of this quarter and additional detail on the contract award will be provided in future reports.
Since beginning work on August 4, 2014, PCG has worked extensively on the development of the DSRIP Project Plan Application, the Project Metrics and Milestones, Scoring Guide, and PPS Lead Financial Stability Test. Throughout the development of these documents, PCG has worked closely with Department of Health staff to ensure the DSRIP Project Plan and all accompanying documents have been consistent with the STCs, Attachments I and J, and the DSRIP project Toolkit.
DSRIP Support Team
New York released a Funding Availability Solicitation (FAS) for the purpose of procuring the services of a vendor to serve as the DSRIP Support Team (DST) on May 21, 2014. Through the FAS procurement process, New York selected KPMG to serve as the DST. KPMG began work on August 1, 2014.
The DSRIP Support Team´s responsibilities include, but are not limited to, under the direction of New York´s DSRIP team, working with providers to strategically think through their potential DSRIP Project Plans to transition to effective and efficient high performing health care delivery systems, developing DSRIP Project Plan prototypes, "how to” guides and other tools to help providers as they prepare their Project Plan applications and then supporting providers from shortly after DSRIP Design Grant awards until final submission of these Project Plan applications.
Since beginning work as the DSRIP Support Team, KPMG has provided the following key functions as the DST:
- The DSRIP Support Team (DST) developed an online survey to be filled out by all PPSs to gather preliminary information about their current status and needs. The data collected from the survey helped understand the level of support potentially required for each PPS and also helped guide the subsequent development of support materials.
- The DST performed outreach to DSRIP stakeholders to ensure their awareness of and involvement in the DSRIP Program. Stakeholders included other DOH bureaus, other NYS agencies, industry associations, and downstream providers.
- The DST formed, trained and deployed teams to the regions to support PPSs with application development.
- The DST assisted DOH with the development of the Midpoint Deliverable questionnaire that provided DOH insight regarding the PPSs´ progress in becoming compliant with DSRIP requirements. In addition, DOH used the finalized, DOH–developed questionnaire as a trigger for second design grant payment.
- The DST developed the Governance How to Guide aimed at providing direction and content to the PPSs when setting up their governance models.
- The DST developed a Community Needs Assessment checklist to help assess the completeness of the PPSs´ CNA reports.
- The DST developed an online PPS status reporting tool. The tool is used by the PPSs to provide their current progress against DSRIP objectives. It is also used by the DST members to supplement the PPSs´ self–assessment and gathers information weekly for reporting to DOH.
- The DST conducted workshops with DOH on establishing a digital forum for PPSs to share information, collectively solve challenges and claim ownership over the DSRIP process (MRT Innovation Exchange).
- The DST commenced the development of the DSRIP Application Prototype to help provide the PPSs with a clear understanding of what an actual application will look like.
Requests for Regulatory Waivers
New York State has not received any requests for regulatory waivers. Future reports will identify any requests for regulatory waivers submitted by PPSs.
Capital Restructuring Finance Program (CRFP) Request for Applications (RFA)
The 2014–15 New York State budget authorized the establishment of the CRFP to allow the DOH and the Dormitory Authority of the State of New York (DASNY), in consultation with the Office of Mental Health ("OMH”), the Office for People with Developmental Disabilities ("OPWDD”) and the Office of Alcoholism and Substance Abuse Services ("OASAS”), to make awards totaling up to $1.2 billion in state funds to support capital projects to help strengthen and promote access to essential health services, including projects to improve infrastructure, promote integrated health systems, and support the development of additional primary care capacity. Awards of CRFP funding may be made to DSRIP participating entities as well as to non–DSRIP participating entities.
The CRFP RFA is scheduled to be released on November 18, 2014. Additional information regarding the CRFP RFA will be included in subsequent quarterly reports.
Other Issues
Other issues arising in this quarter include concerns raised by major general public hospitals regarding valuation. During the time period covered in this report, New York staff met with those affected parties and provided regular updates to CMS. In the next quarter, the issue was resolved through revisions to Attachment I and the development of an additional DSRIP project to serve low– and non–utilizers and the uninsured. Those developments will be included in the next DSRIP quarterly report.
Upcoming Activities
Year 0 implementation and planning activities will continue through March 31, 2015.
- Potential PPSs will complete the PPS Lead Financial Stability Test by November 10, 2014
- Public comments on the DSRIP Project Plan, Project Milestones and Metrics, and Scoring Guide will be collected and summarized for public release
- DST will complete a prototype DSRIP Project Plan Application for evaluation by the DSRIP Independent Assessor and results will be released for public review
- PPSs will complete the DSRIP project Plan Application and submit for review by the DSRIP Independent Assessor by December 22, 2014
- IAAF payments will continue for qualifying hospitals
- Preliminary attribution will be calculated for emerging PPSs
- Safety Net provider lists will continue to be updated
- New York will continue working with CMS on finalizing the MRT waiver extension
Future reports will also include updates on additional activities as required by the MRT Waiver Amendment and related attachments.
Additional Resources
More information on the New York State DSRIP Program is available here.
Interested parties can sign up to be notified of DSRIP program developments, release of new materials, and opportunities for public comment through the Medicaid Redesign Team listserv. Instructions are available here.
Follow Us