Children's Health & Behavioral Health MRT Subcommittee
Quarterly Meeting
NYS OASAS Field Office, New York City
November 3, 2016
- Presentation also available in Portable Document Format (PDF)
Agenda
- Welcome & Introductions
- Health Homes Serving Children
- Key Changes in Managed Care
- Transitioning SPA/HCBS services
- Children´s Transformation Timeline Update
- Foster Care
- SPA Update
- 1115 Amendment
- Medicaid Provider Enrollment & Provider Designation/Authorization
- Plan Qualification Standards
- MC Readiness Funds
- MCTAC Technical Assistance
Health Homes for Children
- Launch date remains on schedule for December 5, 2016
- UAS, which houses the CANS–NY was opened to OMH TCM Providers and certain VFCA for Title IV–E on October 24, 2016 to pre–populate the CANS–NY to facilitate transition to Health Home
- Test environment of MAPP (e.g., Children´s Referral Portal) is now available to MAPP users
- Web–based MAPP training is available now
- Instructor–led Training begins today and into next week
- 16 Contingently Designated Health Homes have been working on readiness activities
- HIT Compliance – Care Management/EHR and Billing Readiness
- Network Adequacy
- ASAs with Managed Care Plans
- Policies and Procedures In Place
- Results of Adult Health Home Designation
- Identified Contingencies
- State is communicating now with Health Homes that have not satisfied the readiness requirements and authorization to begin enrollment will be delayed beyond December 5, 2016
- State is committed to working expeditiously with those Health Homes to get them up and running as soon as possible
- Designation status of Health Homes Serving Children will be posted late next week on the DOH website
Key Changes in Managed Care will Facilitate Implementation of Children´s MRT Transformation
The Children´s MRT Design will :
- Transition the Voluntary Foster Care population to Managed Care
- Provide HCBS services (now only available within Fee–for–Service to enrollees of 1915(c) waivers) under Managed Care via 1115 Waiver and provide Health Home Care Management for children receiving HCBS services
- Expand the MMC benefit package – behavioral health services, new State Plan services, fully aligned array of HCBS Services
All Managed Care Plans will be required to meet new qualification standards for children to implement changes in Managed Care
State Plan Amendment Services:
Proposed New Services
Other Licensed Practitioners (OLP)
- Reimbursement Authority
- Delivery of services in the community
- Services provided outside of the four walls of the agency
State Plan Amendment: Existing services moving into SPA
| Existing OMH Serious Emotional Disturbance (SED) Waiver Services | Existing OCFS Bridges to Health (B2H) Waiver Services | New SPA Service |
|---|---|---|
| Crisis Response Services | Immediate Crisis Response Services | Crisis Intervention |
| Intensive In–Home Services | Crisis Avoidance, Management & Training Intensive In-Home Services | Community Psychiatric Supports & Treatment |
| Psychosocial Rehabilitation Services | ||
| Family Peer Support Services | Family Peer Support Services | |
| Youth Peer Advocate Services | Youth Peer Support and Training |
Children´s Home and Community Based Services: Existing Services Moving into new HCBS benefit array
| Existing Services | Comprehensive Care Coordination (for those ineligible for Health Home or opt out) | Respite (Planned and Crisis) | Habilitative Skill Building | Prevocational Services | Supported Employment | Caregiver/Family Supports and Services | Community Self–Advocacy Training and Support | Habilitation | Adaptive and Assistive Equipment | Accessibility Modifications | Palliative Care | Customized Goods and Services | Non–Medical Transportation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OMH SED Waiver | Individualized Care Coordination | Respite | Skill Building | Prevocational Services | Supported Employment | ||||||||
| OCFS B2H Waiver | Health Care Integration | Crisis and Planned Respite | Skill Building | Prevocational Services | Supported Employment | Family and Caregiver Support Services | Community Advocacy and Support | Day Habilitation | Adaptive and Assistive Equipment | Accessibility Modifications | |||
| CAH I/II Waiver | Care Coordination | Respite Care | Home and Vehicle Modifications | Palliative Care |
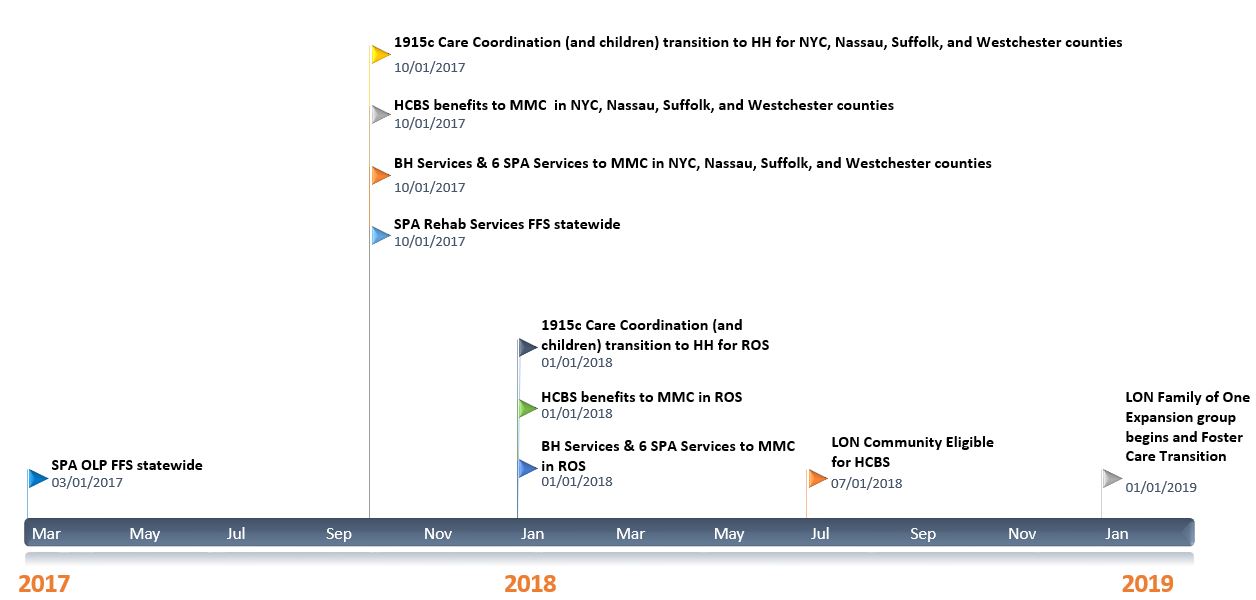
Timeline for Children´s MRT Health and Behavioral Health Transition
| Current Timeline | Revised Timeline | |
|---|---|---|
| SPA Other Licensed Practitioners (OLP) – FFS (1 of 6 new SPA Services) | 1/1/17 | 3/1/17 |
|
7/1/17 Downstate 1/1/18 Upstate | 10/1/17 Downstate 1/1/18 Upstate – No Change |
NYC, Nassau, Suffolk, Westchester
|
7/1/17 | 10/1/17 |
Rest of State
|
1/1/18 | No Change 1/1/18 |
| LON Community Eligible – begin to receive HCBS benefits | 7/1/18 | No Change 7/1/18 |
| LON Family of One – expansion group begins eligibility & access | 1/1/19 | No Change 1/1/19 |
| Foster Care Population Transition to Managed Care (See Foster Care Licensure Timeline) | 7/1/17 Downstate 1/1/18 Upstate | 1/1/19 ( Accommodates Legislation and Licensing VFCA Required for MC Transition Under Corporate Practice of Medicine) |
Children´s Transformation Timeline
Actions to Facilitate the Transition of the Foster Care Population to Managed Care
- Corporate Practice of Medicine (CPOM) Requirements in New York State
- New York State statute, regulations and case law prohibit Managed Care Plans from contracting with unlicensed agencies that provide, contract or arrange for medical services with physicians or licensed practitioners
- Goals for Transition of Foster Care Population to Managed Care
- Provide the choice for VFCAs to preserve the existing relationships they have with medical providers that have the knowledge and expertise to provide medical services to the child welfare population, including:
- Services provided via contract with providers in the community
- Services provided by direct employees of the agency
- Note: Services provided under Articles 28, 31, 32 and 16 are not impacted by CPOM
- Facilitate the payment by the Plan to the VFCA of a residual per diem to cover VFCA Medicaid costs that are not transferrable to the Plan as Managed Care benefits
- Provide the choice for VFCAs to preserve the existing relationships they have with medical providers that have the knowledge and expertise to provide medical services to the child welfare population, including:
- Facilitate the transition of the foster care population by providing Plans the ability to contract with VFCA by seeking legislation and regulations to authorize and implement a specialized licensed for voluntary foster care agencies that provide medical services to children enrolled in foster care
- Timeframes for implementing legislation, regulations, licensing requirements and licensing process will move the date that the statewide VFCA population will transition to Managed Care to January 2019
- Other timelines impacting VFCA will not change – expansion of services, including SPA and HCBS and waiver care coordination transition to Health Home will occur and payments will be made through fee–for–service
- DOH and OCFS are working together to draft legislation and licensing requirements
State Plan Amendment Update
Medically Complex Children: Youth and Family Peer Services and Palliative Care
- Youth and Family Peer Services – will be available to children with complex medical needs
- Requires foundational work:
- Capacity/ providers interested in providing peer services to children with medical needs will need to be assessed
- New credentialing process will need to be developed – CMS requires credentialing process for Youth and Family Peer Service providers
- Palliative Care – End of life requirement is being eliminated – service definitions and utilization requirements under development
Children´s Medicaid State Plan Amendment
- Revised DRAFT SPA Provider Manual will be released with Designation Application
- Six New SPA Services (available in FFS & MMC after implementation)*
- Other Licensed Practitioner (OLP)
- Crisis Intervention (CI)
- Community Psychiatric Supports and Treatment (CPST)
- Psychosocial Rehabilitation (PSR)
- Family Peer Support Services (FPSS)
- Youth Peer Support and Training Services (YPST)
*Services require CMS approval
State Plan Amendment Submission
- Phase in approach for new SPA services to minimize disruption of 1915c programs (i.e., HCBS services that will transition to SPA services)
- NYS will submit two SPAs to CMS
- Other Licensed Practitioner (OLP) SPA with effective date of March 1, 2017 – Under final approval process within the State
- Rehab SPA (Crisis Intervention, CPST, PSR, Family Peer, and Youth Peer) with effective date of October 1, 2017 – Will follow submission of OLP SPA to CMS
- There will continue to be a single process for designating SPA providers – process in not broken out based on the separation of the SPAs
SPA Providers – Authorization for Designation Process
- Title 18 (Social Services Law) Authority for interagency designation of SPA providers
- Joint Development of Children´s SPA regulations for Authorization of designated providers
- Child serving agencies and practitioners that operate within child serving agency with children´s behavioral health and health experience that are licensed, certified, or designated by DOH, OMH, or OASAS, or in the case of voluntary foster care agencies licensed or approved by OCFS and that meet other required qualifications may seek designation
- Providers that seek designation to provide SPA services may be also be subject to additional licensure/authorization requirements including:
- Authorization or licensure by OMH if they provide SPA services to members that need mental health services
- Authorization or licensure by OASAS if they provide SPA services to members that need substance use disorder services
- Details around the additional licensure/authorization being developed by OMH and OASAS
- VFCA that provide SPA services to members that need mental health and substance use disorder services and are in foster care and/or discharged from foster care will not be subject to such additional licensure/authorization requirements
- VFCA that provide SPA services to members that need mental health and substance use disorder services not enrolled in foster would be subject to such requirements
- VFCA that provide SPA services under Managed Care via licensed practitioners will need to have specialize licensed to address CPOM (potentially could impact OLP, crisis intervention, and CPST)
EBP Provider Survey & Rate Development
- Aim: To understand the extent to which Evidence–Based Practices are currently used, their associated monetary costs, and to gauge a provider´s desire to implement (or sustain) an evidence–based practice
- Survey Period: 9/1/16–9/30/16
- Respondents: 233 individually completed surveys
- EBP Experience and use
- 64% Currently Implementing an EBP
- 5% have implemented an EBP in the past but not currently
- 31% have not had experience implementing an EBP
- Top Concerns regarding EBP implementation
- Limited or lack of adequate reimbursement
- Cost for training, certification, and technical assistance associated with an EBP
- Staff turnover resulting in trained clinicians leaving the agency
- Survey will inform the prospective EBP rate development and designation process
- EBP Designation is anticipated to open in Spring 2017
1115 Amendment
- Finalizing outstanding Policy Questions
- Informing Plan Qualification Standards development
- Planned submission to CMS in November 2016
Finalized 1115 Target Populations
Level of Care
- Serious Emotional Disturbance
- Developmentally Disabled in Foster Care
- Medically Complex
Level of Need
- Serious Emotional Disturbance
- Abuse, Neglect and Complex Trauma
Customized Goods and Services Pilot
- Transition of current ´Flexible Service Dollars´ available in the OMH Waiver/TCM
- Mirroring the Adult 1115 Self–Directed Care Pilot (pending final CMS approval)
- Fiscal Intermediary under consideration to manage budgets & process goods/services payments
- Annualized dollar amount per child
Medicaid Provider Enrollment and Provider Designation & Authorization
Medicaid Provider Enrollment
- Guidance and Technical Assistance will be issued for providers that are not currently enrolled in Medicaid
- Upcoming Webinar
- Recommend such providers immediately begin provider enrollment application/process
Tools to Inform Provider Decisions
- Release of Revised SPA Provider Manual and Draft HCBS Provider Manual
- Both Provider Manuals will be released with the Provider Designation Application
- HCBS Benefits Overview I/II Webinar – November 11/16 & 11/18
- Provider Designation Application Overview Webinar
- Medicaid Provider Enrollment Webinar
- SPA/HCBS Rates & Methodology Webinar
- Will be pre–recorded and posted on MCTAC.org
- MCTAC TA Tour for Application Preparation & Planning Assistance
- Additional Upcoming Webinars include:
- Plan Qualification Standards
- 1115 Amendment Overview
Designation of SPA and HCBS Providers
OMH User ID will be required to complete application
- Release of step–by–step instructions sent out on 10/25 explaining how to begin this process, for providers that do not have an OMH user ID
- Also located on Children´s Transformation Website here.
Electronic Application forthcoming
Must meet specific provider agency qualifications
- Designation by joint State agency team
- Provider Medicaid enrollment direction provided in application
- Additional training specific to service delivery, billing and other implementation details to come
Children´s Plan Qualification Standards
Children´s Plan Qualification Standards
- Describes the MCO responsibilities for the delivery of the expanded Medicaid–covered services for all Medicaid enrolled children meeting HCBS target, risk, and functional criteria.
- Outlines additional standards and modifications to the existing Behavioral Health adult standards to which MCOs are contractually obligated.
- NYS expects that Plans continue to operate per the requirements in the Medicaid Managed Care Model Contract and comply with all new Children´s standards.
- NYS will qualify MCOs to serve children in 2 rounds based on geographic region and population characteristics:
- The first round will be in New York City (NYC), and Nassau, Suffolk, and Westchester Counties; and
- The second round will be for the rest of the state (ROS).
Children´s Plan Qualification Standards Structure
NYS will review the following areas to determine MCO organizational and administrative readiness
- 3.1 Organizational Capacity
- 3.2 Contract Personnel
- 3.4 Member Services
- 3.5–3.8 Network Service and Contract Requirements
- 3.9 Utilization Management
- 3.10 Clinical Management
- 3.11 Cross System Collaboration
- 3.12 Quality Management
- 3.13 Reporting and Performance Measurement
- 3.14 Claims
- 3.15 Information Systems and Website Capabilities
- 3.16 Financial Management
Timeline
- Releasing the Children´s Plan Qualification Standards for stakeholder feedback in the next few weeks
- Stakeholders will have 30 days from release to review and submit feedback on Children´s Plan Qualification Standards
- Criteria described in the Children´s Plan Qualification Standards are draft and subject to change based on stakeholder feedback and negotiations with the federal government
- Written feedback will be due to bho@omh.ny.gov by the deadline provided
Children´s Managed Care Readiness Funds
CANS Institute RFP
- Final decisions regarding awardee will be coming in near future; NYS is currently still in the black–out period until all components have been fully approved.
- This procurement is up to $1 million per year, for a total of up to $5 million over the five–year life of the contract.
- High Level deliverables of this contract include:
- Part A:
- Support for individuals trained and certified in the use of the CANS–NY
- Create and maintain an organized network of trained CANS–NY coaches to carry out the work of the CANS–NY Institute
- Provide forums and venues for CANS–NY users to provide information and feedback on the CANS–NY tool
- PART B:
- Establish an analytic process to monitor quality, create reports and provide revisions recommendations for the CANS–NY tool
- Part A:
Managed Care Readiness Funds (OASAS/OMH)
- Round 2 HIT funding to 31 providers of $49,850 each was released in October 2016
- Final recommendations for fund use in process
- Federal match strategy – under discussion
- More information to come
MCTAC Technical Assistance Schedule – coming to your email box soon
New Children´s Managed Care Mailbox
Children´s Transformation Website
Visit the Children´s Managed Care Website here
RESOURCES TO STAY INFORMED:
Subscribe to children´s managed care listserv
Subscribe to DOH Health Home listserv
Health Home Bureau Mail Log (BML)