Considerations for Determining HCBS Eligibility for the Serious Emotional Disturbance (SED) Target Population
- Document also available in Portable Document Format (PDF)
April 19, 2023
Meet Today's Speakers
Meredith Ray-LaBatt, MA, MSW
Deputy Director
Division of Integrated Community Services for Children and Families
NYS Department of Mental Health
Colette Poulin, MSSA
Health Program Director
Children's Health Home, Division of Program Development and Management
NY Department of Health
Agenda
- Understanding Designated Mental Illnesses
- Understanding Serious Emotional Disturbance
- When to Assess for HCBS
- SED Target Population
- Q&A
The goal of today's session is to help identify whether a child/youth meet the SED Target Population criteria and who may also be eligible for the HCBS Children's Waiver.
Mental Health Disorders in Children/Youth
Designated Mental Illness
- A child or youth can be determined to have a mental health disorder by a Licensed Practitioner who has the ability to diagnose in their scope of practice.
- This is based on a comprehensive assessment involving a clinical interview to understand the child/youth and family from a holistic perspective with sensitivity to diversity. The assessment process includes the observation of the child/youth known as a mental status examination, where evaluations are made of risk, appearance and behavior. Information may also be obtained from reliable collaterals to inform mental health history and current circumstances.
- Typically, mental health needs can be addressed by community based services, mental health treatment interventions (e.g. cognitive behavioral therapy) and in some cases, if needed, medication.
- Many children/youth with mental health needs can manage their disorder with minimal impact to their well-being or functioning in areas of life
- Schizophrenia Spectrum and Other Psychotic Disorders
- Bipolar and Related Disorders
- Depressive Disorders
- Anxiety Disorders
- Obsessive-Compulsive and Related Disorders
- Trauma-and Stressor-Related Disorders
- Dissociative Disorders
- Somatic Symptom and Related Disorders
- Feeding and Eating Disorders
- Disruptive, Impulse-Control, and Conduct Disorders
- Personality Disorders
- Paraphilic Disorders
- Gender Dysphoria
- Elimination Disorders
- Sleep-Wake Disorders
- Sexual Dysfunctions
- Medication-Induced Movement Disorders
- Attention Deficit/Hyperactivity Disorders
- Tic Disorders
Prevalence of Mental Health Disorders in Children
- Approximately 1 in 6 children (16.5%) between the ages of 6 and 17 has a treatable mental health disorder.
- 3.2% of children aged 3-17 years (approximately 1.9 million) have diagnosed depression.
- 7.4% of children aged 3-17 years (approximately 4.5 million) have a diagnosed behavior problem.
- 7.1% of children aged 3-17 years (approximately 4.4 million) have diagnosed anxiety.
- 9.4% of children aged 2-17 years (approximately 6.1 million) have received an ADHD diagnosis.
Serious Emotional Disturbance
Understanding SED
- "SED" stands for Serious Emotional Disturbance, a clinical determination made by a physician or licensed therapist
- A determination of SED indicates a child/youth has significant mental health needs and may be exhibiting symptoms and/or behaviors that require specialized and/or intensive mental health treatment
- Children with SED often need a higher level of care and intensive treatment interventions, along with medication management
- As a result, many intensive treatment services require an SED determination as part of the eligibility criteria needed for admission to the service
- A CSE classification of ED is DIFFERENT from a SED classification. Eligibility for one does not mean automatic eligibility for the other.
How does SED differ from a MH Diagnosis?
- Children with a mental health diagnosis are not automatically considered to have a serious emotional disturbance
- Children with mental health diagnoses may have needs that are effectively managed by a Pediatrician or therapist
- Children with SED are more likely to experience comorbid psychiatric disorders, and may require medication
- Children with SED often demonstrate challenges in various life domains, such as family and school, and are at increased risk of disengagement in treatment or hospitalization
Prevalence of Children with SED
- One in 10 youth in the United States experience a mental disorder severe enough to limit daily functioning in the family, school, and community setting.
- 10% of youth experience SED with substantial/severe impairment in one or more functional domains
- Approximately 6% of youth experience SED with substantial impairment in two or more domains
Common Challenges Associated with SED
For Youth:
- Academic Experiences: Poor academic outcomes; Inconsistent school attendance/Frequent absence; History of school suspension or expulsion
- Familial/Interpersonal Relationships: Inability to get along with others/make friends; quick to demonstrate frustration or anger with others; struggles to interact positively with classmates and siblings/caregivers
- Psychiatric Comorbidity: Often have multiple diagnoses and presenting problems which impact course of treatment and symptomatology; Comorbidity is one of the most significant predictors of SED in youth
- Medication Use: Often been prescribed psychotropic or antipsychotic medications if they have been managing the symptoms of a mental health condition for some time
For families:
- Families often experience high levels of stress and added responsibilities
- Feelings of "taking over" their lives due to high level of needs/services
- Caregiver strain includes experiencing mental health difficulties, employment interruption, feelings of anger, sadness, guilt, and fatigue, social isolation, and worry about their child's future
- Family Environment: Low SES; Household family members who experience depression; Household family members experienced substance use challenges
For multiple system involvement:
- Children determined to have SED, particularly those with high impairment, are often involved in several systems, including mental health, medical health, education, and juvenile justice which requires increased coordination of services. In some cases, involvement in multiple systems can increase the likelihood of out-of-home care or hospitalization.
For the healthcare system:
- Increased health costs
- Complexity of treating
Need for More Comprehensive Services
Increased Coordination of Care:
- Increased risk for treatment failure and dropout requires enhanced engagement strategies, appointment reminders, and assistance with minimizing barriers to care.
- Challenges in daily functioning highlight the importance of coordinating all primary, acute, behavioral health, and long-term services and supports to treat the whole person.
- Involvement in multiples systems and services require increased coordination of care, communication between treatment providers, and monitoring of progress.
Coordinated Services/ Multidisciplinary Team Approach:
- Mental health diagnosis and functional limitations require both clinical treatment AND support services
- Greater support needed by caregivers/parents to manage their child's needs and behaviors.
SED Target Population
Serious Emotional Disturbance Criteria
- SED is the presence of a designated mental illness that has resulted in functional impairment(s) which substantially interfere with or limits the child/youth's role or functioning in family, school, and/or community activities
- Based on the demonstration of functional limitations for past 12 months on a continuous or intermittent basis; AND
- The functional limitations must be moderate in at least two areas or severe in at least one area
- A clinical determination made by a Licensed Practitioner of the Healing Arts (LPHA) through a comprehensive evaluation or routine treatment
- A mental health diagnosis alone is not sufficient to meet the criteria for a SED determination
Functional Limitations
The Medicaid member has experienced functional limitations due to serious emotional disturbance over the past 12 months on a continuous or intermittent basis. The functional limitations must be moderate in at least two of the following areas or severe in at least one of the following areas:
- Ability to care for self (e.g., personal hygiene; obtaining and eating food; dressing; avoiding injuries); or
- Family life (e.g., capacity to live in a family or family like environment; relationships with parents or substitute parents, siblings and other relatives; behavior in family setting); or
- Social relationships (e.g., establishing and maintaining friendships; interpersonal interactions with peers, neighbors and other adults; social skills; compliance with social norms; play and appropriate use of leisure time); or
- Self-direction/self-control (e.g., ability to sustain focused attention for a long enough period of time to permit completion of age-appropriate tasks; behavioral self-control; appropriate judgment and value systems; decision- making ability); or
- Ability to learn (e.g., school achievement and attendance; receptive and expressive language; relationships with teachers; behavior in school).
Co-Occurring Disorders
- In order to be enrolled in HCBS under the SED Target Population, a child/youth who may have an I/DD, SUD or medical diagnosis must still ALSO have:
- A qualifying designated mental health illness,
- Meet the SED criteria for functional limitations due to their mental health condition,
- And be at risk of hospitalization/out of home placement due to their mental health needs.
If the mental health need is not primary or the reason for being at risk of hospitalization or out of home care, other target populations or HCBS Waivers may be more appropriate.
When to Assess for HCBS
Determining What Services are Needed
- Children and youth with newly identified or progressing mental health needs can be met with "state plan" and other community mental health services, and those services should be used first
- Children and Family Treatment and Support Services (CFTSS), Mental Health Outpatient Treatment and Rehabilitative Service Program (MHOTRS)/OMH clinic, locally funded services, etc.
- Home and Community Based Services (HCBS) are intended for children with significant and chronic disorders that have put them at risk of hospitalization or out-of-home treatment/placement
- HCBS services CANNOT be used in place of "state plan" services; they are intended to supplement and support the use of treatment services and help avert more restrictive services and settings and maintain children and home and in their community
Confirming Level of Mental Health Need
- Does the child have a current mental health diagnosis?
- Do they need a diagnostic evaluation from a licensed mental health practitioner?
- If not in services, has the child been referred for mental health treatment and supports?
- Is the child currently engaged and in receipt of mental health supports and services?
- Can their needs be met with more community mental heath services?
- Have they been determined to meet SED criteria and demonstrating increased, complex mental health needs.
- What that may "look" like…
Indicators of Complex Needs (Risk Factors)
- The child/youth has had multiple recent presentations to the ED/CPEP due to mental health/psychiatric crises to be assessed for admission (applied) for inpatient admission.
- The child/youth has had a recent (past 6 months) inpatient psychiatric stay or been discharged from an inpatient hospitalization.
- The child/youth has been referred/applied for admission to/is on a waitlist for a mental heath facility (RTF, QRTP, Community Residence) within past 6 months.
- The child/youth is currently in, will be discharged/recently discharged (within past 6 months) from a mental health facility.
Indicators of Increasing Needs
- The child has had several years of mental health treatment history and is demonstrating a significant increase in MH needs, but may have recently disengaged from treatment.
- The child/youth is currently engaged in a mental health treatment from a community practitioner or other mental health professional and is demonstrating a significant increase in MH needs.
- The child/youth has recently received multiple community crisis services (mobile crisis, crisis residence, crisis stabilization services) for mental health/psychiatric crises.
If these children are also engaged in other child serving systems and have multiple complex needs, they are at increased risk for hospitalization and/or out-of-home care
Multi-systems Involvement*
- If the member is receiving more than one mental health service, this would only count as one system involvement, inclusive of school-based behavioral health services.
- Other systems can include:
- Child welfare (e.g., CPS, Foster care),
- juvenile justice (e.g., Probation),
- Department of Homeless Services,
- OASAS clinics or residential treatment facilities or institutions*,
- OPWDD services or residential facilities or institutions*, or
- having an established school IEP and in receipt of services through the school district.
- However, multi-systems involvement does not include systems/services that all children should receive such as school or primary care services.
- Enrollment in a Medicaid managed care plan, Health Homes/C-YES, HCBS, or other care coordination services also does not count toward multi-systems involvement.
*Please note that children/youth with an I/DD or SUD diagnosis must have a co-occurring qualifying mental health diagnosis, meet the SED criteria, and be at risk of hospitalization/out of home placement due to their mental health needs, in order to be enrolled in HCBS under the SED Target Population.
When Does a Child Need HCBS?
- They have significant social, emotional and behavioral challenges that have put them at risk of hospitalization or out-of-home care due their mental heath needs
- Their community mental health services are not adequate enough to meet their complex and growing mental health needs
- They require additional Home and Community Based Services to:
- Allow access to an expanded array of services within the Medicaid benefit to address their complex needs
- Help to maintain them within their home and community and avoid long term residential and institutional stays.
- Provide ample services and supports to them and their families in order to avoid hospitalizations or out-of-home care
- Assist them within an institution access to supportive services to be able to return back to their home and community.
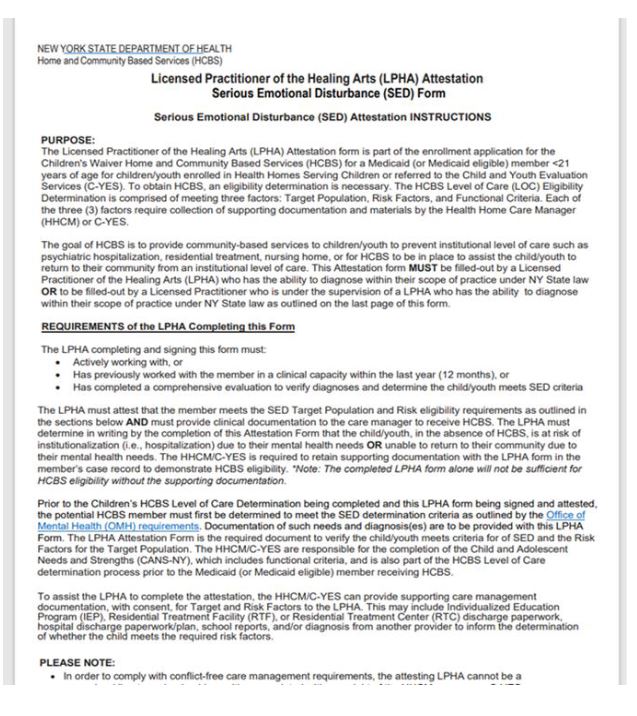
LPHA Attestation
Only the following practitioners can complete the HCBS LPHA Attestation Form and MUST provide supporting documentation regarding their role with the member:
- A clinician who is actively serving the child/youth, and who will have to indicate for how long they have been serving the member, or
- A clinician who has previously worked with the member in a clinical capacity within the last 12 months, or
- A clinician, that was referred for the purpose of completing the comprehensive evaluation in order to verify diagnoses and determine the child meets SED criteria.*
- *For this response, please attached the relevant supporting document
- Date of evaluation is required
OR
- If the child is identified as having significant needs by the HHCM/C-YES, and they and their supervisors/ agency have been unsuccessful in getting a treating clinician to complete the form, HHCM/C-YES may contact the county Children's Single Point of Access (C-SPOA) for assistance. The C-SPOA can work with the HHCM/C-YES to collect required information to complete/sign the form. (Documentation will be required to demonstrate efforts the member/family and care manager has attempted to obtain treatment)
Q&A
Thank you!
- For questions about HH, reach out to healthhomes@health.ny.gov
- HHCMs and HH CMAs should first talk with their Lead Health Home regarding questions and issues they may have.
- For questions about HCBS, reach out to BH.Transition@health.ny.gov