Post-Payment Audit Home
The purpose of Post-Payment Audit is to confirm the eligibility and integrity of the provider´s EHR Incentive Payment information submitted within the attestation portal. Recoupment of fees issued is determined through an auditor's investigation of eMedNY, the Medicaid Data Warehouse (MDW), encounter data and supporting documentation. Providers are mandated by regulation to keep all related records for a minimum of six years from the date the attestation is submitted. Compliance with this federally approved audit requires supporting information to be accurate, complete and verifiable. Failure to submit requested documentation will result in repayment of incentive issued and additional sanctions may apply. Listed below are four main categories of information on the post-payment audit process. Each category has multiple links that give access to further resources and data. Using the material below you can get a more detailed understanding of the post-payment audit process.
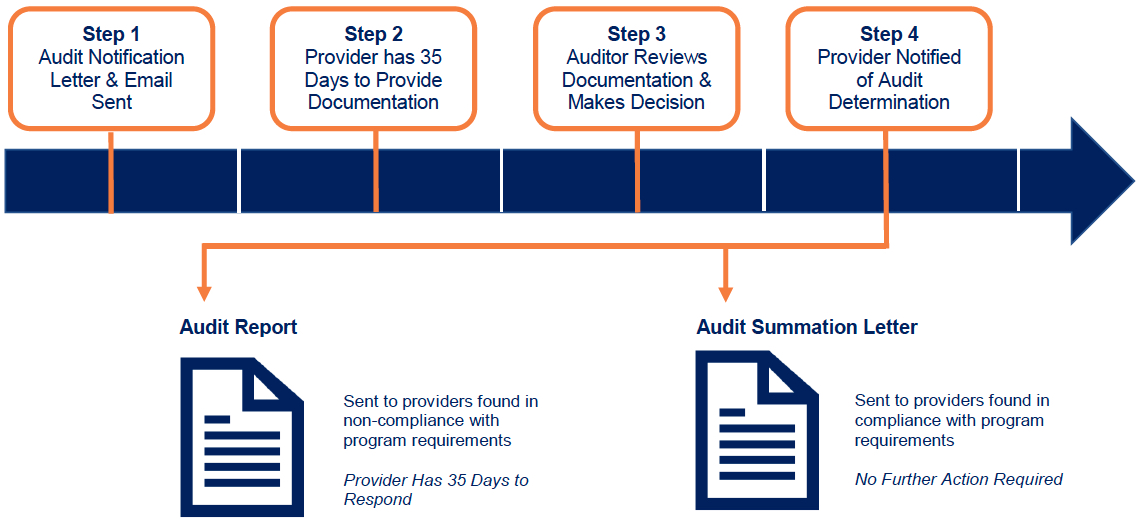
Figure 1: Steps for Standard Audit Process
Audit Communications
Audit Documentation
Audit Educational Materials
- How to Use SendVault for: Chrome Users - Firefox Users - (PDFs)
- Audit Overview Timeline Quick Reference Guide (PDF)
- Audit Notification Email (AIU) Quick Reference Guide (PDF)
- Audit Notification Email (MU) Quick Reference Guide (PDF)
- Completing the Medicaid Patient Volume Spreadsheet Quick Reference Guide (PDF)
- Tutorial 1: Audit Process Overview Tutorial (YouTube)
- Tutorial 2: Understanding the Audit Notification Email - Adopt, Implement, or Upgrade (AIU) Tutorial (YouTube)
- Tutorial 3: Understanding the Audit Notification Email - Meaningful Use (MU) Tutorial (YouTube)
- Tutorial 4: Completing the Medicaid Patient Volume Spreadsheet Tutorial (YouTube)
Follow Us