Focus Area 1: Maternal and Infant Health
- Goal #1: Reduce premature births
- Goal #2: Increase breastfeeding
- Goal #3: Reduce rate of maternal deaths
Improving the health of mothers and babies is an important public health priority for New York State. Key population indicators of maternal and infant health, including low birth weight, prematurity and maternal mortality, have not improved significantly over the last decade in New York, and in some instances have worsened. Even in measures where trends are improving, such as reductions in adolescent pregnancy rates and infant mortality rates, there are significant and persistent racial, ethnic and economic disparities.
Three priority maternal and infant health outcomes were established for the 2013-2018 a Prevention Agenda/State Health Improvement Plan: preterm birth, breastfeeding and maternal mortality. These outcomes complement other sections of the State Plan that influence maternal and infant health, including: injury and violence prevention, prevention and management of chronic diseases, prevention and cessation of tobacco use, HIV/STI prevention, preconception/reproductive health, promotion of mental health and prevention of substance abuse.
Goal #1: Reduce premature births in New York State.
Defining the Problem
Preterm birth, defined as any birth before 37 weeks gestation, is the leading cause of infant death and long-term neurological disabilities in children.2 Babies born prematurely or at low birth weight are more likely to have or develop significant health problems, including disabling impairments, compared to children who are born at full term at a normal weight. Preterm infants are vulnerable to respiratory, gastrointestinal, immune system, central nervous system, hearing and vision problems, and often require special care in a neonatal intensive care unit after birth. Longer-term problems may include cerebral palsy, mental retardation, vision and hearing impairments, behavioral and social-emotional concerns, learning difficulties and poor growth.3 More than 70 percent of premature babies are late preterm births, delivered between 34 and <37 weeks gestation. While these infants generally are healthier than babies born earlier, they are still three times more likely than full-term infants to die during their first year.4
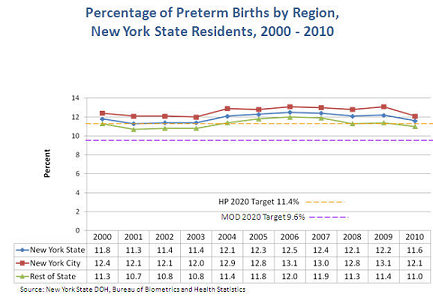
Prematurity can also pose significant emotional and economic burdens on families. In 2010, 11.6 percent of New York State births were preterm.5 Babies who are born preterm cost the US health care system more than $26 billion annually.2 In 2007, about 48 percent of preterm infant hospital stays nationally were paid by Medicaid, the largest source of health insurance for preterm infants.6
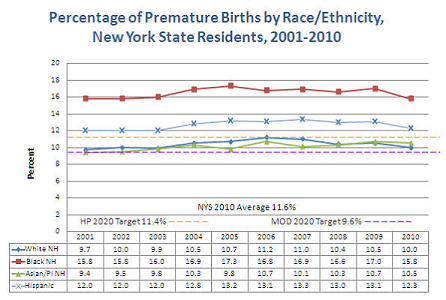
The State's rate of preterm births has been relatively stagnant over the last decade, but significant racial, ethnic and economic disparities persist. Infants of non-Hispanic black mothers are more than 1.5 times more likely to be born preterm than those born to non-Hispanic white mothers, and infants with Medicaid coverage are 1.1 times more likely to be born preterm than infants with other insurance coverage. There are also marked disparities in mortality rates due to prematurity: Infants born to non-Hispanic black mothers were 3.4 times likely to die than white infants.2 The New York State Department of Health has joined the National March of Dimes and Association of State and Territorial Health Officials (ASTHO) in a national challenge to reduce preterm births by eight percent by 2014.7
The causes of preterm birth are not fully understood. Known risk factors include late or no prenatal care, smoking, alcohol use, drug use, domestic violence, lack of social support, stress, long working hours, exposure to environmental pollutants, infections, poor oral health, high blood pressure, diabetes, being underweight before pregnancy, obesity and a short spacing between pregnancies.8 Having a preterm birth is the greatest predictor of a subsequent preterm birth.9 This Action Plan's focus on reducing preterm births complements other efforts in New York State to reduce elective cesarean sections and medical inductions in the 'early term' period, typically defined as between 37 and <39 weeks gestation.10,11 While important in improving birth outcomes for mothers and infants, that work is beyond this Action Plan's scope because it does not specifically target improvements in preterm births, defined as <37 weeks gestation.
Goals and Objectives
- Objective 1-1:
- By December 31, 2018, reduce the rate of preterm birth in NYS by at least 12% to 10.2%.
- (This target for 2018 is in alignment with the national ASTHO/March of Dimes target of 17.9% improvement by 2020 to achieve a national preterm birth rate of 9.6 %.)
- Objective 1-2:
- By December 31, 2018, reduce the racial, ethnic and economic disparities in preterm birth rates in NYS by at least 10%.
Tracking Indicators:
- Percentage of births that are premature:
- All births
- (Target: 10.2%; Baseline: 11.6%; Year: 2010)
- (Source: NYSDOH Vital Statistics; Data Availability: State, county)
- Ratio of Black non-Hispanic preterm birth rate to White non-Hispanic preterm birth rate.
- (Target: 1.42; Baseline: 1.58; Year: 2010
- Source: (NYSDOH Vital Statistics; Data Availability: State, county)
- Ratio of Hispanic preterm birth rate to White non-Hispanic preterm birth rate.
- (Target: 1.12; Baseline: 1.24; Year: 2010)
- Source: (NYSDOH Vital Statistics; Data Availability: State, county)
- Ratio of Medicaid preterm birth rate to non-Medicaid preterm birth rate.
- (Target: 1.0; Baseline: 1.10; Year: 2010)
- Source: (NYSDOH Vital Statistics; Data Availability: State, county)
Additional Indicators:
- Infant mortality rate per 1,000 live births.
- (Baseline: 5.1 infant deaths per 1,000 live births; Year: 2010)
- Source: (NYSDOH Vital Statistics; Data Availability: State, county)
- Percentage of births that are low birth weight (<2,500 grams).
- (Baseline: 8.2%; Year: 2010)
- Source: (NYSDOH Vital Statistics; Data Availability: State, county)
- Percentage of births for which prenatal care begin in the first trimester of pregnancy.
- (Baseline: 73.2%; Year: 2010)
- Source: (NYSDOH Vital Statistics; Data Availability: State, county)
- Percentage of women who smoke during the last three months of pregnancy.
- (Baseline: 7.2%; Year: 2010)
- Source: (Pregnancy Risk Assessment Monitoring System (PRAMS); Data Availability: State, NYC and rest of State)
Related Healthy People 2020 National Objectives
- MICH-9:
- Reduce total preterm births by at least 10%.
- Target: 11.4%; Baseline: 12.7%; Year: 2007
- Source: (National Vital Statistics System, CDC, NCHS)
- MICH-1.3:
- Reduce the rate of all infant deaths within one year by at least 10%.
- (Target: 6.0 deaths per 1,000 births; Baseline: 6.7 deaths per 1,000 births; Year: 2006;)
- Source: (National Vital Statistics System-Mortality and Natality (NVSS-M, NVSS-N), CDC, NCHS)
Interventions by Health Impact
| Goal #1: Preterm Birth. | |
|---|---|
| Levels of Health Impact Pyramid1 | Interventions |
| Counseling and Education |
|
| Clinical Interventions |
|
| Long-Lasting Protective Interventions |
|
| Changing the Context to Make Individuals' Decisions Healthy |
|
| Socioeconomic Factors |
|
Interventions by Sector
NOTE: The chart below provides a sample of interventions that can be carried out by sector. Please refer to the 'Interventions by Health Impact' grid above for more interventions and references.
Health Care Delivery System
- Ask all pregnant women about tobacco use and provide augmented, pregnancy-tailored counseling for smokers.
- Provide timely, continuous and comprehensive prenatal care services to pregnant women in accordance with NYS Medicaid prenatal care standards and other professional guidelines.
- Work with paraprofessionals, including peer counselors, lay health advisors, and community health workers to reinforce health education and health care service utilization and enhance social support to high-risk pregnant women.
- Implement innovative models of prenatal care, such as Centering Pregnancy, demonstrated to improve preterm birth rates and other adverse pregnancy outcomes.
- Provide clinical management of preterm labor in accordance with current clinical guidelines.
- Implement practices to expedite enrollment of low-income women in Medicaid, including presumptive eligibility for prenatal care and family planning coverage.
- Utilize health information technology to facilitate more robust intake/enrollment, screening/risk assessment, referral, follow up and care coordination practices across health and human service providers.
- Refer high-risk pregnant women to home visiting services in the community.
Employers, Businesses, and Unions
- Provide comprehensive health insurance for employees and their families that covers comprehensive primary care, prenatal care and enhanced supportive, e.g., home visit, services.
- Provide paid time off for employees to attend prenatal care visits.
- Provide paid maternity and family leave.
Media
- Provide comprehensive health insurance for employees and their families that covers comprehensive primary care, prenatal care and enhanced supportive, e.g., home visit, services.
- Provide paid time off for employees to attend prenatal care visits.
- Provide paid maternity and family leave.
Academia
- Develop and evaluate educational messages and formats that have demonstrated positive impact on changes in knowledge, attitudes/beliefs, skills and behaviors related to preterm birth among target populations.
- Conduct translational research to support effective evaluation, replication, dissemination and implementation of evidence-based interventions to reduce preterm births.
- Facilitate community-based participatory research to engage affected populations in raising awareness of health disparities and identifying, developing and implementing collective solutions to community health issues.
- Develop and evaluate professional education messages, vehicles and tools to improve health and human service providers' knowledge, skills and delivery of evidence-based interventions and clinical practices.
Community-Based Organizations
- Implement evidence-based home visiting programs for high-risk pregnant women.
- Use trained paraprofessionals, including peer counselors, community health workers and promotoras to reinforce health education and health care service utilization and enhance social support to high-risk pregnant women.
- Implement practices to expedite enrollment of low-income women in Medicaid, including presumptive eligibility for both prenatal care and family planning coverage.
- Utilize health information technology to facilitate more robust intake/enrollment, screening/risk assessment, referral, follow up and care coordination practices across health and human service providers.
- Identify and promote educational messages in formats that have demonstrated to improve knowledge, attitudes, skills and behavior related to prevention of preterm birth among target populations.
Other Governmental Agencies
- Provide comprehensive, evidence-based health education for children and youth in schools that include health literacy, healthy relationships and consumer skills for use of health care services.
- Assess health insurance status and source of regular health care for all clients served in government programs and connect uninsured pregnant or preconception women to facilitated enrollers within the community.
- Ensure that pregnant youth in foster care have access to timely and comprehensive prenatal care and other supportive services, including home visiting programs where available.
Governmental Public Health
- Develop and conduct effective health communications/social marketing campaigns that promote norms of healthy behaviors before, between and during pregnancies.
- Support implementation of State-wide Medicaid standards for comprehensive prenatal care.
- Support or conduct public health detailing to improve health and human service providers™ knowledge, beliefs and skills related to improved use of evidence-based clinical and community-based interventions to reduce preterm birth.
- Support the expansion and integration of evidence-based home visiting programs and the use of trained paraprofessionals, including lay health advisors, community health workers and promotoras to enhance social support to high-risk pregnant women.
- Support policies, systems and local practices to expedite enrollment of low-income women in Medicaid, including presumptive eligibility for prenatal care and family planning coverage.
- Support the use of health information technology to facilitate more robust intake/enrollment, screening/risk assessment, referral, follow up and care coordination practices across health and human service providers.
- Support development and implementation of local service networks and coordination strategies to ensure that women with identified risk factors are linked to appropriate community resources.
- Make local and State data available more timely through electronic birth certificates to drive quality improvement.
Non-Governmental Public Health
- Ask all pregnant women about tobacco use and provide augmented, pregnancy-tailored counseling to smokers.
- Work with paraprofessionals such as lay health advisors, community health workers and promotoras to reinforce health education and health care service utilization and enhance social support to high-risk pregnant women.
- Promote or implement innovative models of prenatal care demonstrated to improve preterm birth rates and other adverse pregnancy outcomes, such as Centering Pregnancy.
- Implement practices to expedite enrollment of low-income women in Medicaid, including presumptive eligibility for prenatal care and family planning coverage.
- Use health information technology to facilitate more robust intake/enrollment, screening/risk assessment, referral, follow up and care coordination practices across health and human service providers.
- Conduct public health detailing to improve health and human service providers™ knowledge, beliefs and skills related to improved use of evidence-based clinical and community-based interventions to reduce preterm birth.
- Implement evidence-based home visiting programs.
- Support development and implementation of local service networks and coordination strategies to ensure that women with identified risk factors are linked to community resources.
Policymakers and Elected Officials
- Support policies that facilitate easy and early enrollment into Medicaid for pregnant and reproductive-age women, including presumptive eligibility.
- Support policies that promote and facilitate comprehensive preconception, prenatal and inter-conception health care for high-risk, low-income women.
Communities
- Promote consistent health messages, behaviors and policies throughout communities.
- Engage affected populations in local strategies to raise awareness of health disparities and to identify, develop, implement and evaluate collective solutions to community health issues.
- Assist in identifying paraprofessionals from affected communities who can serve in community health promotional programs.
- Help build effective local systems and networks for outreach, engagement, referral and coordinated follow-up.
Philanthropy
- Fund the engagement of affected populations in local strategies to assess their needs and challenges, such as community focus groups of women who did not use prenatal care, and disseminate findings to State and local partners to spur development of more effective intervention strategies.
- Fund the development, evaluation, replication and dissemination of evidence-based and innovative strategies to improve population health.
- Fund strategies, such as training programs and quality improvement collaborations to strengthen capacity and improve effectiveness of health and human services providers.
- Provide leadership and funding to convene multi-sector partners and promote the sharing of information to support expansion of effective strategies to improve population health.
Goal #2: Increase the proportion of NYS babies who are breastfed.
Defining the Problem

Breast milk is the optimal food for infants. Breastfed infants are less likely to develop medical problems such as childhood obesity, respiratory and gastrointestinal infections and are at lower risk for childhood cancers, asthma and Sudden Infant Death Syndrome (SIDS).41 Breastfeeding benefits mothers by decreasing risks of breast and ovarian cancers, osteoporosis and postpartum depression, and by increasing the likelihood of returning to pre-pregnancy weight.41
In addition to health benefits for the mother and infant, breastfeeding can also benefit employers and society. Employers who invest in breastfeeding support programs see increased productivity, reduced absenteeism, higher employee loyalty and lower health care costs. If 90 percent of infants were exclusively breastfed for six months, the US health care system could save as much as $13 billion annually.42
Not breastfeeding carries health risks for mothers, including increased incidence of premenopausal breast cancer, ovarian cancer, retained gestational weight gain, Type-2 diabetes, heart attack, and metabolic syndrome (a set of factors that raise a person's risk for health problems such as heart disease, diabetes and stroke).43 For infants, lack of breastfeeding contributes to higher incidence of ear infections, respiratory and gastrointestinal infections, overweight and obesity. Infants who are not breastfed during their first nine months have a nearly 50 percent greater risk of becoming overweight than children who are breastfed.44
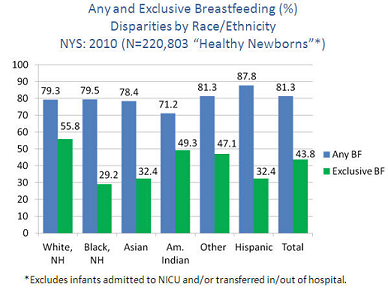
Despite evidence of breastfeeding's benefits, far too many New York infants are receiving infant formula supplementation. NYS ranks among the highest of states for formula supplementation within the first two days of life, and NYS's exclusive breastfeeding rates at three and six months are below the national average.45 Inadequate maternity leave contributes to decreased breastfeeding duration; hourly-wage workers face different challenges than salaried workers and often have less control over their schedules.46 Additionally, women with certain health concerns, such as spinal cord injuries, multiple sclerosis and arthritis, may require specialized breastfeeding supports.
There are also marked disparities among women who breastfeed. Lower rates of breastfeeding initiation, exclusivity and duration exist among younger, less-educated, low-income women. Racial and ethnic minorities and women enrolled in the WIC program also have lower exclusive breastfeeding rates.47
Goals and Objectives
- Objective 2-1:
- By December 31, 2018, increase the percent of infants born in NYS who are exclusively breastfed by at least 10% to 48.1%.
- Objective 2-2:
- By December 31, 2018, improve racial, ethnic and economic disparities in breastfeeding rates in NYS by at least 10%.
Tracking Indicators:
- Percentage of infants exclusively breastfed in the hospital:
-
- All infants
- (Target: 48.1%; Baseline: 43.7%; Year: 2010
- Source: NYSDOH Vital Records
- Data Availability: State, county)
- Ratio of Black non-Hispanic to White non-Hispanic infants exclusively breastfed in the hospital
- (Target: 0.57; Baseline: 0.52; Year: 2010
- Source: NYS Vital Records
- Data Availability: State, county)
- Ratio of Hispanic to White non-Hispanic percentage of infants exclusively breastfed in the hospital
- (Target: 0.64; Baseline: 0.58; Year: 2010
- Source: NYS Vital Records
- Data Availability: State, county)
- Ratio of Medicaid to non-Medicaid percentage of infants exclusively breastfed in the hospital
- (Target: 0.66; Baseline: 0.60; Year: 2010
- Source: NYS Vital Records
- Data Availability: State, county)
Additional Indicators:
- Percentage of infants exclusively breastfed at age 3 months.
- (Baseline: 33.0 %; Year: 2009
- Source: National Immunization Survey
- Data Availability: State, NYC and Rest of State)
- Percentage of infants exclusively breastfed at age 6 months.
- (Baseline: 15.3%; Year: 2009;
- Source: National Immunization Survey
- Data Availability: State, NYC and Rest of State)
- Percentage of infants enrolled in WIC program breastfed for 6 months or longer.
- (Baseline: 39.7%; Year: 2008-10
- Source: NYS Pediatric Nutrition Surveillance System
- Data Availability: State, county).
Related Healthy People 2020 National Objectives
- MICH-21.1:
- Proportion of infants who were ever breastfed.
- Target: 81.9%; Baseline: 74.0%; Year: Birth cohort 2006, as reported in 2007-09.
- Source: National Immunization Survey (NIS), CDC, NCIRD, and NCHS
- MICH-21.4:
- Proportion of infants who were breastfed exclusively through age three months.
- Target: 46.2%; Baseline: 33.6%; Year: Birth cohort 2006, as reported in 2007-09.
- Data Source: National Immunization Survey (NIS), CDC, NCIRD, and NCHS
- MICH-21.5:
- Proportion of infants who were breastfed exclusively through age 6 months.
- Target: 25.5%. Baseline: 14.1%; Year: Birth cohort 2006, as reported in 2007-09;
- Source: National Immunization Survey), CDC, NCIRD and NCHS
Interventions by Health Impact
| Goal #2: Breastfeeding | |
|---|---|
| Levels of Health Impact Pyramid1 | Interventions |
| Counseling and Education |
|
| Clinical Interventions |
|
| Long-Lasting Protective Interventions |
|
| Changing the Context to Make Individuals' Decisions Healthy |
|
| Socioeconomic Factors |
|
Interventions by Sector
NOTE: The chart below provides a sample of interventions that can be carried out by sector. Please refer to the Interventions by Health Impact grid above for more interventions and references.
Healthcare Delivery System
- Implement maternity care practices consistent with WHO's Ten Steps to Successful Breastfeeding and increase the number of Baby Friendly Hospitals in NYS.
- Provide structured, comprehensive breastfeeding education and professional lactation counseling and support, including use of Internal Board Certified Lactation Consultants (IBCLCs) - during pregnancy, in the hospital and at home.
- Address special breastfeeding support needs of women with physical disabilities and other special health needs, such as spinal cord injuries, multiple sclerosis or arthritis.
Employers, Businesses, and Unions
- Create an environment to support breastfeeding/pumping in the workplace and provide lactation support.
- Provide paid maternity and family leave.
- Provide health insurance for employees and their families that cover breastfeeding education, lactation counseling and high-quality breast pumps that meet NYS Medicaid specifications.
Media
- Create or use existing public service announcements to promote breastfeeding.
- Increase the time allotted for programming that supports breastfeeding.
- Help community organizations develop communication strategies to promote breastfeeding.
- Conduct breastfeeding promotion/obesity prevention media campaigns.
Academia
- Train physicians, nurses and other health care providers in the importance of breastfeeding and lactation support.
- Identify and support replication/dissemination of model practices in breastfeeding promotion among NYS employers.
Community-Based Organizations
- Ensure employers create an environment to support breastfeeding-friendly practices in the workplace and advocate for maternity leave policies.
- Implement evidence-based home visiting programs for high-risk pregnant women and families.
- Recruit, train and support peer counselors and community health workers to provide breastfeeding education and support.
Other Governmental Agencies
- Identify and promote educational messages and vehicles that have demonstrated to improve knowledge, attitudes, skills and/or behavior related to successful breastfeeding.
- Increase private and Medicaid reimbursement for births in Baby Friendly Hospitals.
- Collaborate with Child and Adult Care Food Program (CACFP) and WIC to promote breastfeeding-friendly early childcare centers.
- Strengthen laws and regulations that promote, support, and protect breastfeeding.
- Ensure public and private health insurance coverage of, access to, and incentives for breastfeeding education, lactation counseling and support.
Governmental Public Health
- Identify and promote educational messages and vehicles that have demonstrated to improve knowledge, attitudes, skills and/or behavior related to successful breastfeeding.
- Increase private and Medicaid reimbursement for births in Baby Friendly Hospitals.
- Collaborate with Child and Adult Care Food Program (CACFP) and WIC to promote breastfeeding-friendly early childcare centers.
- Strengthen laws and regulations that promote, support, and protect breastfeeding.
- Ensure public and private health insurance coverage of, access to, and incentives for breastfeeding education, lactation counseling and support.
Non-Governmental Public Health
- Support stronger laws and/or regulations to promote, support and protect breastfeeding.
- Help hospitals become 'breastfeeding friendly'.
- Identify and promote educational messages and vehicles that have demonstrated to improve knowledge, attitudes, skills and/or behavior related to successful breastfeeding.
Policymakers and Elected Officials
- Develop and implement paid maternity leave policies.
- Enforce policies of breastfeeding-friendly practices in the workplace.
- Educate and advocate for restrictions on infant formula marketing and distribution of 'gifts' through health care providers and hospitals.
- Strengthen NYS Labor Law and business practices that promote, support and protect breastfeeding at work.
- Adopt regulations and policies to implement standards that will promote, support and protect breastfeeding.
Communities
- Advocate for stronger enforcement of laws supporting breastfeeding at work.
- Advocate for restriction of marketing of baby formula.
- Encourage the awareness of and demand for breastfeeding counseling/education messages that have demonstrated to improve knowledge, attitudes, skills and/or behavior.
Philanthropy
- Support programs for health care staff on breastfeeding related regulations and legislation.
- Support the development of educational messages.
Goal #3: Reduce the rate of maternal deaths in New York State.
Defining the Problem
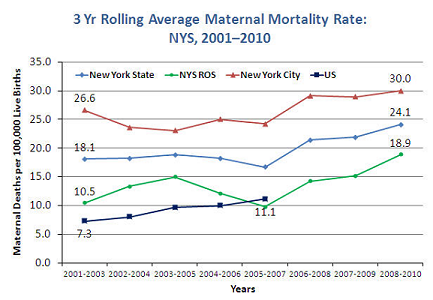
The World Health Organization defines maternal death as the death of a woman while pregnant or within 42 days of the end of a pregnancy, from any cause related to the pregnancy or its management. Maternal death is devastating, with profound impact on infants, other children, partners, families and health care teams. The US ranks behind 40 nations in maternal deaths, and New York's maternal mortality rate is unacceptably high, ranking the State 47 out of 50. In 2010, there were 23.1 maternal deaths per 100,000 live births in New York State.63 Healthy People 2020 calls for a reduction in the maternal mortality rate to 11.4 maternal deaths per 100,000 live births.
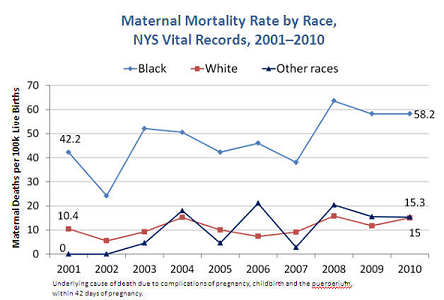
There are dramatic racial, ethnic, socioeconomic and geographic disparities in New York's maternal mortality rate. In New York City, pregnancy-related mortality rates were seven times higher for Blacks and twice as high for Hispanics and Asian/Pacific islanders than for Whites.64 For New York State overall, the maternal mortality rate for black women was approximately 3.7 times the rate for White women.65 Additionally, some poorest neighborhoods had rates almost five times higher than affluent neighborhoods. Women without health insurance had pregnancy-related death rates almost four times higher, than those covered by Medicaid or private insurance.64
The leading causes of maternal death in New York are hemorrhage, pregnancy-induced hypertension, cardiac disorders and embolism.66 Cesarean deliveries, induced preterm births, and obesity increase the risk for complications during delivery. Many of the deaths reviewed are believed to have been preventable. For prevention measures to work, the review system will require a major overhaul to provide more detailed information to providers and communities. The links between underlying maternal health, chronic medical conditions and maternal mortality highlight the importance of addressing the preconception and inter-conception health of high-risk women, as well as prenatal and intra-partum health and clinical care.67
Goals and Objectives
- Objective 3-1:
- By December 31, 2018, reduce the rate of maternal mortality in NYS by at least 10%.
- Objective 3-2:
- By December 31, 2018, improve racial and ethnic disparities in maternal mortality rates in NYS by at least 10%.
Tracking Indicators:
- Number of maternal deaths per 100,000 live births:
-
- All maternal deaths
- Target: 21.0 deaths per 100,000 births; Baseline: 23.3; Year: 2008-2010 (3-year average)
- Source: NYSDOH Vital Statistics; Data Availability: State, county
- Ratio of Black non-Hispanic to White non-Hispanic maternal mortality.
- Target: 4.76; Baseline: 5.29; Year: 2008-2010 (3-year average)
- Source: NYSDOH Vital Statistics; Data Availability: State
Related Healthy People 2020 National Objectives
- MICH-5:
- Maternal deaths per 100,000 live births.
- Target: 11.4 deaths per 100,000 births
- Baseline: 12.7s; Year: 2007; Source: National Vital Statistics System, CDC, NCHS
Interventions by Health Impact
| Goal #3: Maternal Mortality | |
|---|---|
| Levels of Health Impact Pyramid1 | Interventions |
| Counseling and Education |
|
| Clinical Interventions |
|
| Long-Lasting Protective Interventions |
|
| Changing the Context to Make Individuals' Decisions Healthy |
|
| Socioeconomic Factors |
|
Interventions by Sector
NOTE: The chart below provides a sample of interventions that can be carried out by sector. Please refer to the 'Interventions by Health Impact' grid above for more interventions and references.
Healthcare Delivery System
- Assess and address pregnancy planning, including the use of effective contraception, among women with severe chronic conditions that make pregnancy a life-threatening event.
- Use guidelines for clinical management of chronic diseases and other risk factors or events, such as obesity, hypertension and hemorrhage, during pregnancy and delivery.
- Identify high-risk women upon entry into prenatal care to refer to experienced prenatal care providers with specialized services.
- Flag high-risk pregnant women upon arrival at the emergency rooms or other hospital portals to assure appropriate level of care.
- Provide routine preconception and inter-conception health visits for women of reproductive age that include screening and follow up for risk factors, management of chronic medical conditions and use of contraception to plan pregnancies.
Employers, Businesses, and Unions
- Provide comprehensive health insurance (for employees and their families) which covers preventive, disease management and enhanced supportive services.
- Provide incentives for employees and their families to access clinical and community preventive and disease self-management programs and services, including time off or flextime.
- Provide employees with comprehensive wellness programs.
Media
- Help government and community-based organizations develop effective health communications/social marketing campaigns that promote norms of health and healthy behaviors before, between and during pregnancies.
- Conduct health communications and social marketing campaigns on women's health, chronic disease, domestic violence and pregnancy planning.
- Increase time/space allotted for programming that supports health promotion messages targeting high-risk women of reproductive age and pregnant women.
Academia
- Partner with public health to conduct research to increase the understanding of the causes of maternal death, emphasizing disparities.
- Improve medical education to include the social determinants of women's health.
- Expand health education for young women that addresses reproductive health and chronic disease.
Community-Based Organizations
- Implement evidence-based home visiting programs for high-risk pregnant women.
- Utilize paraprofessionals, such as lay health advisors, community health workers, and promotoras, to reinforce health education and health care service utilization and enhance social support to high-risk pregnant women.
- Link women with community resources, such as safe housing, nutritional services, drug treatment and mental health services.
Other Governmental Agencies
- Increase Outreach to link women in need to services from other State agencies their local counterparts.
- Partner with other agencies in translation of maternal mortality review findings to develop and implement prevention initiatives.
Governmental Public Health
- Continue State-wide maternal mortality review efforts.
- Enhance surveillance to identify all cases of maternal mortality.
- Identify gaps in health services and systems to prevent future deaths.
- Disseminate DOH Guidelines on Hypertensive Disorders of Pregnancy and Managing Maternal Hemorrhage.
- At the local level, use outreach and existing programs in high-risk communities to educate, provide support and connect women to services.
Non-Governmental Public Health
- Partner with public health to disseminate information on women's and reproductive health.
- Advocate for resources to address the needs of high-risk communities and populations on reproductive health.
Policymakers and Elected Officials
- Support policies that facilitate easy and early enrollment into Medicaid for pregnant and reproductive age women, including presumptive eligibility.
- Support policies that promote and facilitate comprehensive preconception, prenatal and inter-conception health care for high-risk, low-income women.
- Support policies that promote housing, nutritional services and safe communities.
Communities
- Support educational messages and outreach to high-risk women.
- Provide social and emotional support to affected families throughout the community.
- Improve access to healthy housing and foods.
Philanthropy
- Support efforts to reduce maternal mortality.
- Support educational initiatives on women's health and reproductive health.
- Support public health efforts to enhance maternal mortality review.
a The Prevention Agenda 2013-2017 has been extended to 2018 to align its timeline with other state and federal health care reform initiatives.