Focus Area 2: Child Health
Making health a priority for children ensures the health of future generations. During this time of physical and mental growth, children can learn to build a strong foundation for healthy behavior. Research has shown that many medical conditions affecting adults have roots in childhood.76
Consistent with the need to develop a targeted, actionable prevention plan, two priority maternal and infant health outcomes were established for the 2013-2018 Prevention Agenda/State Health Improvement Plan: use of comprehensive well-child care and prevention of dental caries. These outcomes complement other sections of the State Plan related to children's health, including: injury prevention, environmental air quality, obesity prevention, asthma prevention and management, promoting child and adolescent immunizations, prevention of STIs/HIV among youth, preconception/reproductive health care, promotion of mental, emotional and behavioral health and prevention of substance abuse among youth.
Goal #4: Increase the proportion of NYS children who receive comprehensive well-child-care
Defining the Problem

Routine preventive health care visits are essential to promote health in children and youth. Well-child visits allow children and parents to assess and address concerns, obtain information and guidance from pediatricians, reinforce healthy behaviors and parenting practices, identify and address health risks and special needs, receive long-lasting protective interventions, such as immunizations, build health literacy, and establish and maintain positive provider-family relationships. The American Academy of Pediatrics' (AAP) Bright Futures: Guidelines for Health Supervision of Infants, Children and Adolescents (third edition) provides comprehensive, evidence-based and consensus guidelines for preventive health care for children.
 Ensuring that all children receive comprehensive preventive care services in New York State will require attention to both health care access/utilization and content/quality of care. Bright Futures' guidelines address the frequency of care and components of each well-child visit. While elements of a comprehensive well-child visit apply across the age span, the specifics vary by age for medical history, observation of parent-child interaction, physical examination, developmental surveillance, screening, immunizations and anticipatory guidance. In addition, factors that influence whether or not children and families can access well-child care need to be identified and addressed. In particular, health insurance status, including eligibility and continuity of coverage, needs to be considered in any strategy to improve the use of preventive health services.
Ensuring that all children receive comprehensive preventive care services in New York State will require attention to both health care access/utilization and content/quality of care. Bright Futures' guidelines address the frequency of care and components of each well-child visit. While elements of a comprehensive well-child visit apply across the age span, the specifics vary by age for medical history, observation of parent-child interaction, physical examination, developmental surveillance, screening, immunizations and anticipatory guidance. In addition, factors that influence whether or not children and families can access well-child care need to be identified and addressed. In particular, health insurance status, including eligibility and continuity of coverage, needs to be considered in any strategy to improve the use of preventive health services.
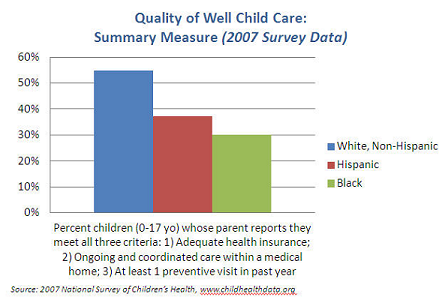
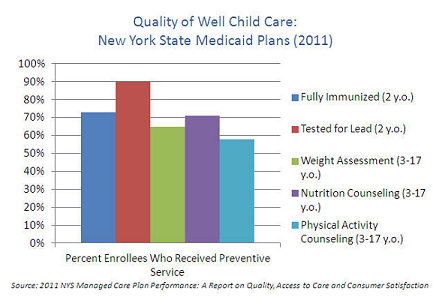
In New York State, data from managed care plans and national parent surveys show that most children receive the recommended number of preventive visits, but there are racial, ethnic and economic disparities. In addition, utilization declines considerably as children age, with only about 60 percent of adolescents getting an annual preventive visit compared to 80-90 percent of younger children. There is also significant variation in how key preventive services are provided as part of routine health care, including immunizations, weight assessment, developmental screening, and counseling/anticipatory guidance.77,78
Goals and Objectives
- Objective 4-1:
- By December 31, 2018 a, increase the percentage of children ages 0-15 months, 3-6 years and 12-21 years who have had the recommended number of well-child visits among NYS Government sponsored managed care health insurance programs by 10%.
- Objective 4-2:
- By December 31, 2018, increase the proportion of NYS children who receive key recommended preventive health services as part of routine well-child care by at least 10%.
- Objective 4-3:
- By December 2018, increase the percentage of children ages less than 19 years with any kind of health coverage to 100%.
- Tracking Indicators:
-
- Percentage of children ages 0-15 months, 3-6 years and 12-21 years who have had the recommended number of well-child visits among NYS Government sponsored managed care health insurance programs.
- Target: 76.9%; Baseline: 69.9%; Year: 2011
- Source: NYSDOH Office of Patient Quality and Safety; Data Availability: State, county)
- The percentage of children ages less than 19 years with any kind of health coverage.
- (Baseline: 94.9%, Year: 2010, Source: U.S. Census Bureau, Small Area Health Insurance Estimates
- Data Availability: State, county.
- Additional Indicators
-
- Percentage of children ages 0-15 months, three to six years and 12-21 years who have had the recommended number of well-child visits among individual or employer-sponsored managed care health insurance.
- Baseline: 62%; Year: 2012
- Source: NYS eQARR ; Data Availability: State only
- Percentage of children who have had the recommended number of well-child visits.
- Source: NYS eQARR ; Data Availability: health plan):
- ages 0-15 months
- 3-6 years
- 12-21 years
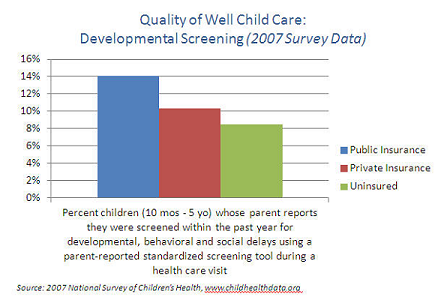
- Percentage of children age ten months to five years whose parent reports screenings for developmental, behavioral and social delays using an age-appropriate standardized screening tool during a health care visit.
- Baseline: 11.7%; Year: 2007
- Source: National Survey of Children's Health; Data Availability: State only)
- Percentage of children tested for lead exposure at least twice by age three.
- Baseline : 52.9%; Year: 2010 (birth cohort 2007); Source: NYSDOH Childhood Blood Lead Registry; Data Availability: State, county)
- Percentage of 19-35 month olds who have received the 4:3:1:3:3:1:4 immunization series (4 DTaP, 3 polio, 1 MMR, 3 Hep B, 3 Hib, 1 Varicella, 4 PCV13) by 23% to 80% or higher.
- (Baseline: 65.1%; Year: 2011
- Data Source: NIS
- Data Availability: State, county (NYSIIS/CIR)
- Percentage of adolescent females age 13-17 years who have received the three-dose HPV immunization series.
- Baseline: 34.2%, Year: 2011; Data Source: NIS; Data Availability: State, county (NYSIIS/CIR)
- Percentage of children ages 2 to 17 years enrolled in managed care plans who had a visit with a health care provider and whose weight was assessed by Body Mass Index. (BMI)
- Baseline: 65% (Medicaid); 64% (Child Health Plus); 62% (Commercial); Year: 2010
- Source: eQARR Managed Care Plan Performance
- Data Availability: State only
- Percentage of children enrolled in managed care plans, ages 3-17 years, who were counseled on nutrition or referred for nutrition education by their health care provider.
- Baseline: 71% (Medicaid); 70% (Child Health Plus); 66% (Commercial); Year: 2010
- Source: eQARR Managed Care Plan Performance; Data Availability: State only
- Percentage of children ages 3-17 years enrolled in managed care plans that were counseled on physical activity or referred for physical activity by their health care provider.
- Baseline: 58% (Medicaid); 61% (Child Health Plus); 59% (Commercial); Year: 2010
- Source: eQARR Managed Care Plan Performance; Data Availability: State only)
- Percentage of adolescents ages 12-17 years enrolled in managed care plans who had at least one visit with a PCP or OB/GYN provider during the measurement year, and who received assessment, counseling, and/or education on:
-
- Risk behaviors and preventive actions associated with sexual activity.
- Baseline: 60% (Medicaid); 59% (Child Health Plus); 54% (Commercial); Year: 2010
- Source: eQARR Managed Care Plan Performance; Data Availability: State only)
- Depression
- Baseline: 52% (Medicaid); 49% (Child Health Plus); 44% (Commercial); Year: 2010
- Source: eQARR Managed Care Plan Performance; Data Availability: State only)
- Tobacco use, including cigarettes, chew or cigars.
- Baseline: 64% (Medicaid); 63% (Child Health Plus); 58% (Commercial); Year: 2010
- Source: eQARR Managed Care Plan Performance; Data Availability: State only
- Substance use, including alcohol, street drugs, non-prescription drugs, prescription drug misuse and inhalant use.
- Baseline: 60% (Medicaid); 62% (Child Health Plus); 57% (Commercial); Year: 2010
- Source: eQARR Managed Care Plan Performance; Data Availability: State only)
- Percentage of children enrolled in public health insurance managed care plans who have a primary care provider that is a NCQA-certified Patient-Centered Medical Home:
-
- Medicaid Managed Care plans
- Baseline: 40%; Year: 2011
- Source: NYSDOH Office of Patient Quality and Safety; Data Availability: State, county
- Child Health Plus plans
- Baseline: 36%; Year: 2011
- Source: NYSDOH Office of Patient Quality and Safety; Data Availability: State, county
- Percentage of children under 19 without health insurance.
- Baseline: 5.1%, Year: 2010
- Source: U.S. Census Bureau, Small Area Health Insurance Estimates; Data Availability: State, county
- Closely Related Healthy People 2020 National Objectives
-
- AH-1:
- Proportion of adolescents who have had a wellness check up in the past 12 months.
- Target: 75.6%; Baseline: 68.7%; Year: 2008
- Source: National Health Interview Survey, CDC, NCHS
- MICH-29.1:
- Proportion of young children who are screened for Autism Spectrum Disorder (ASD) and other developmental delays by 24 months of age.
- Target: 21.5%; Baseline: 19.5%; Year: 2007
- Source: National Survey on Children's Health), HRSA, MCHB and CDC, NCHS
Interventions by Health Impact
| Goal #4: Use of Comprehensive Well-Child Care | |
|---|---|
| Levels of Health Impact Pyramid1 | Interventions |
| Counseling and Education |
|
| Clinical Interventions |
|
| Long-Lasting Protective Interventions |
|
| Changing the Context to Make Individuals' Decisions Healthy |
|
| Socioeconomic Factors |
|
Interventions by Sector
NOTE: The chart below provides a sample of interventions that can be carried out by sector. Please refer to the 'Interventions by Health Impact' grid above for more interventions and references.
Health Care Delivery System
- Utilize the American Academy of Pediatrics' Bright Futures guidelines and resources.
- Implement reminder systems for routine well-child visits.
- Obtain NCQA patient-centered medical home certification.
- Participate in structured, evidence-based learning collaborations to identify and address areas for improvement in clinical practice and its management, such as increased developmental screenings and reducing no-show rates.
- Adopt electronic health records and connect to regional health information systems to improve service quality and coordination.
- Maintain and expand the availability of school-based health centers in high-need, underserved communities.
Employers, Businesses, and Unions
- Provide health insurance for employees and their families that covers preventive and disease management services for children and youth.
- Provide employees with paid time off, flextime and other incentives for their children's well-child visits.
Media
- Help government and community-based organizations develop effective marketing campaigns that promote routine well-child visits.
- Develop innovative marketing strategies to promote well-child care.
- Make increased advertising space and resources available for health promotion campaigns.
Academia
- Develop and evaluate educational messages and vehicles that have demonstrated increased knowledge, attitudes/beliefs, skills and behaviors about well-child care among target populations.
- Develop and evaluate messages, vehicles and tools to improve health and human service providers' knowledge, skills and delivery of Bright Futures guidelines and other evidence-based clinical practices, with an emphasis on new standards and areas with lowest quality measures.
- Conduct focus groups to understand better why families do not use recommended well-child services, and disseminate findings to practitioners and policymakers to inform improvement strategies.
Community-Based Organizations
- Utilize the American Academy of Pediatrics' Bright Futures research on family care resources.
- Facilitate initial and continuous enrollment of low-income children in Medicaid and Child Health Plus, including use of presumptive eligibility.
- Promote educational messages and vehicles that have demonstrated increased knowledge, attitudes/beliefs, skills and behaviors about well-child health care among target populations.
- Assess health insurance status and source of regular health care for all client children, and connect families in need to facilitated enrollers and community health care providers.
- Implement evidence-based home visiting programs with documented improvements in the use of well-child health care services.
- Use peer counselors, lay health advisors, community health workers and promotoras to reinforce health education and service utilization and enhance social support to high-risk children and their families.
Other Governmental Agencies
- Provide comprehensive, evidence-based health education in schools that includes health literacy and consumer skills for use of health care services.
- Assess health insurance status and source of regular health care for all client children, and connect families in need to facilitated enrollers.
- Ensure that all children in foster care have a regular source of health care, including comprehensive, age-appropriate well-child and preventive care services.
Governmental Public Health
- Support the expansion and integration of evidence-based home visiting programs.
- Support expedited enrollment of low-income children in Medicaid and Child Health Plus, including presumptive eligibility.
- Facilitate the adoption of electronic medical records and connections to regional health information systems to improve the timeliness, quality and coordination of care for children.
- Continue implementation of quality assurance and improvement strategies for child health measures in managed care plans, and adopt additional new quality measures for key preventive services, such as developmental screening.
- Support or conduct public health detailing to improve health and human service providers' knowledge, beliefs and skills related to delivery of comprehensive well-child care in accordance with Bright Futures guidelines.
- Incentivize primary care practices that serve low-income children to obtain NCQA certification as patient-centered medical homes and the enrollment of publicly insured children in these certified practices.
- Support continued viability and targeted expansion of State-wide network of school-based health centers in high-need, underserved communities.
Non-Governmental Public Health
- Implement evidence-based home visiting programs with documented improvements in the use of well-child health care services.
- Conduct public health detailing to improve health and human service providers' knowledge, beliefs and skills related to improved use of evidence-based clinical and community-based interventions to improve use of well-child care.
- Support streamlining and simplifying enrollment and renewal of health insurance.
Policymakers and Elected Officials
- Implement Affordable Care Act reforms to ensure comprehensive, affordable health insurance for all children.
- Support the viability and targeted expansion of school-based health centers in high-need, underserved communities.
Communities
- Gather direct input from families to understand better why families do not use all well-child services, and share information with practitioners and policymakers to inform improvements.
- Disseminate information to community members about the importance of well-child care, including health insurance resources and health care providers.
- Assess health insurance status and regular source of health care for all children in early care and education programs, and connect families in need to facilitated enrollers.
Philanthropy
- Fund the development, evaluation, replication and dissemination of evidence-based and innovative strategies to improve use of well-child care among affected populations.
- Fund training programs and quality improvement collaboration to help health care providers effectively deliver well-child care that meets Bright Futures guidelines.
- Provide leadership and funding to support community-wide, cross-sector practices, networks and systems to ensure that all children are enrolled in health insurance and have a usual source of primary health care.
Goal #5: Reduce the prevalence of dental caries among NYS children
Defining the Problem
Dental caries, or tooth decay, is the most common chronic disease among children82, dental care being the greatest unmet service need. If untreated, dental caries is often painful and can disrupt learning, school performance and daily activities. In extreme cases, dental caries is fatal. Dental care accounts for almost 15 percent of all health care expenditures among school-aged children. Insurance coverage is uneven and out-of-pocket expense is significant.
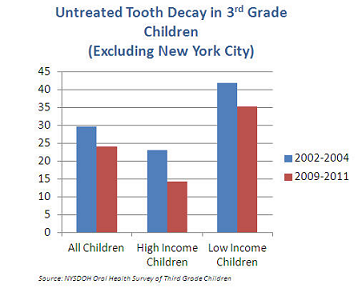
Through water fluoridation, improved oral hygiene and access to dental care, New York State has reduced the prevalence and severity of tooth decay. Approximately 80 percent of untreated tooth decay has been found in 25 percent of children aged 5-17.83 Applying the national estimates to State population counts,84 approximately 3.4 million New York children will experience tooth decay by high school graduation.85
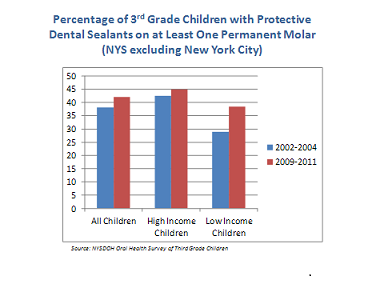
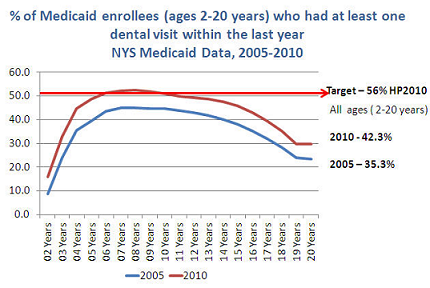
A survey of third-grade children conducted every five years delineates the economic disparities in oral health and unmet needs in New York State. Compared to children in higher income groups, low-income children have more caries experience, including evidence of untreated tooth decay, fewer dental visits, fewer sealants and lower use of fluoride tablets83 (Figure 1 and 2). Among Medicaid enrollees ages 2-20 years, only 42.3 percent visited a dentist in 2010 (Figure 3). Children with special health care needs are also disproportionately susceptible to dental caries.85
Goals and Objectives
Objective 5-1:By December 31, 2018, reduce the prevalence of tooth decay among NYS children by at least 10%.
Objective 5-2:By December 31, 2018, increase the proportion of NYS children who have protective dental sealants by at least 10%.
Objective 5-3:By December 31, 2018, increase the proportion of NYS children who receive regular dental care by at least 10%.
Objective 5-4: By December 31, 2018, increase the percentage of NYS population receiving fluoridated water by 10%.
Objective 5-5: By December 31, 2018, strengthen systems to improve the oral health of people with special health needs.
Tracking Indicators
- Percentage of third-grade children with evidence of untreated tooth decay.
- All third-grade children. (Target: 21.6%; Baseline: 24%; Year: 2009-2011; Source: NYSDOH Oral Health Survey of Third-Grade Children; Data Availability: State, county)
- Ratio of low-income children to high-income children. (Target: 2.21; Baseline: 2.46; Year: 2009-2011; Source: NYSDOH Oral Health Survey of Third-Grade Children; Data Availability: State, county)
Additional Indicators
- Percentage of third-grade children with evidence of treated or untreated tooth decay. (Baseline: 45%; Year: 2009-2011; Source: NYSDOH Oral Health Survey of Third-Grade Children; Data Availability: State, county)
- Percentage of third-grade children who have protective dental sealants on at least one permanent molar. (Baseline: 42%; Year: 2009-2011; Source: NYSDOH Oral Health Survey of Third-Grade Children; Data Availability: State, county)
- Percentage of children and youth enrolled in Medicaid, age 2-20 years, who at least one dental visit within the last year. (Baseline: 40.8 %; Year: 2008-2010; Source: NYSDOH Medicaid Data; Data Availability: State, county)
- The percentage of residents served by community water systems with optimally fluoridated water (Baseline: 71.4%; Year: 2012; Target: 78.5%; Source: CDC Water Fluoridation Reporting System; Data Availability: State, county).
- Proportion of Children with Special Health Care Needs (CSHCN) ages 0-17 years who received any preventive dental service during the past year. (Baseline: 86%; Year: 2009-10; Data Source: National Survey of Children with Special Health Care Needs; Data Availability: State only)
- Proportion of Children with Special Health Care Needs (CSHCN) ages 0-17 years who reported an unmet need for dental care or orthodontia service during the past year. (Baseline: 5%; Year: 2009-10; Data Source: National Survey of Children with Special Health Care Needs; Data Availability: State only)
Closely Related Healthy People 2020 National Objectives
- OH-1.2: Children ages six to nine with dental caries experience. (Target: 49.0 percent; Baseline: 54.4% of children ages 6-9 who had dental caries experience in at least one primary or permanent tooth; Years: 1999-2004; Data Source: National Health and Nutrition Examination Survey, CDC, NCHS)
- OH-2.2: Children aged six to nine with untreated decay in at least one tooth. (Target: 25.9;. Baseline: 28.8%; Years: 1999-2004: Data Source: National Health and Nutrition Examination Survey, CDC, NCHS)
Interventions by Health Impact
| Goal #5: Reducing the Prevalence of Dental Caries | |
|---|---|
| Levels of Health Impact Pyramid | Interventions |
| Counseling and Education |
|
| Clinical Interventions |
|
| Long-Lasting Protective Interventions |
|
| Changing the Context to Make Individuals' Decisions Healthy |
|
| Socioeconomic Factors |
|
Interventions by Sector
NOTE: The chart below provides a sample of interventions that can be carried out by sector. Please refer to the 'Interventions by Health Impact' grid above for more interventions and references.
Healthcare Delivery System
- Integrate oral health preventive practices, such as application of fluoride varnish, into pediatric primary care. Establish referral links with community dental providers.
- Maintain and expand the availability of school-based preventive dental programs in targeted high-need, underserved communities.
- Participate in structured, evidence-based learning collaborations to identify and address areas for improvement in clinical practice, including the management of early childhood caries and dental sealant and reductions in no-show rates.
- Adopt electronic health records and connect to regional health information systems to improve quality and coordination of services.
Employers, Businesses, and Unions
- Provide dental insurance for employees and their families, including oral health preventive and treatment services.
Media
- Help government and community-based organizations develop effective marketing campaigns that improve oral health literacy, knowledge, attitudes and skills.
- Make increased advertising space and resources available for health promotion/social marketing campaigns.
- Develop strategies to educate stakeholders about the unique oral health challenges facing low-income children and children with special health needs.
Academia
- Provide clinical training and continuing education to general dentists to expand services for children.
- Encourage educational and training programs to update competencies and standards to enhance the treatment of children with special health care needs.
- Integrate oral health in training for medical students and primary care residents. Support continuing education/professional development for primary care practitioners on preventive dental health practices that can be provided as part of pediatric primary care.
Community-Based Organizations
- Integrate oral health messages across all providers and programs that serve children, including childcare, home visiting and WIC, and establish linkages with community dental providers to refer families in need of services.
- Conduct annual community assessments to determine availability of dental practices, including capacity for new clients, and what insurances are accepted, and distribute information in up to date local resource guides.
Other Governmental Agencies
- Require dental examinations as part of school and Head Start examinations, with referral networks and linkages to dental providers.
- Promote healthy school lunch standards and prohibit vending machines and soda pouring rights in schools.
- Integrate oral health messages across all providers and programs that serve children, including childcare, home visiting and WIC, and establish linkages with community dental providers to refer families in need of services.
Governmental Public Health
- Implement an essential dental health benefit package that includes coverage for oral health preventive and treatment services.
- Support efforts to enroll low-income children in Medicaid and Child Health Plus, including presumptive eligibility.
- Support continued viability and targeted expansion of State-wide network of school-based dental sealant and fluoride programs in high-need, underserved communities.
- Promote acceptance of Medicaid reimbursement among dentists to expand the supply of dental providers for low-income children.
- Facilitate co-location of medical and dental health services.
- Maintain and expand fluoridation of public water supplies in high-need communities.
Non-Governmental Public Health
- Support efforts to enroll low-income children in Medicaid and Child Health Plus, including presumptive eligibility.
- Promote acceptance of Medicaid reimbursement among dentists to expand the supply of dental providers for low-income children.
- Support efforts to maintain and expand fluoridation of public water supplies in high-need communities.
Policymakers and Elected Officials
- Implement Affordable Care Act reforms to assure comprehensive, affordable health insurance that includes coverage for dental health services for all NYS children.
- Develop and implement innovative policies for maintaining and expanding water fluoridation.
- Explore innovative workforce solutions to address the shortage of dental professionals in underserved communities and inefficient use of existing providers.
Communities
- Integrate oral health messages across all providers and programs that serve children, including child care, home visiting, and WIC, and est
- Implement quality standards for early care and education programs that promote healthy meals and snacks.
Philanthropy
- Fund the development, evaluation, replication and dissemination of evidence-based and innovative strategies to improve oral health literacy, behaviors and use of preventive dental services among affected populations.
- Fund training programs and quality improvement collaboration to strengthen capacity and improve effectiveness of children's oral health services.
- Provide leadership and funding to support community-wide, cross-sector efforts to maintain and expand fluoridation of public water supplies.
a The Prevention Agenda 2013-2017 has been extended to 2018 to align its timeline with other state and federal health care reform initiatives.